User login
Remove the black-box warning for depot medroxyprogesterone acetate!
- Update on contraception
Rachel B. Rapkin, MD; Mitchell D. Creinin, MD (August 2011) - 10 (+1) practical, evidence-based recommendations for you to improve contraceptive care now
Colleen Krajewski, MD; Mark D. Walters, MD (August 2011) - Levonorgestrel or ulipristal: Is one a better emergency contraceptive than the other?
Robert L. Barbieri, MD (Editorial; March 2011) - IUD use in nulliparous and adolescent women
Jennefer A. Russo, MD; Mitchell D. Creinin, MD (Update on Contraception, August 2010)
The Food and Drug Administration (FDA) should remove the black-box warning regarding skeletal health that the agency inserted into labeling for the injectable contraceptive depot medroxyprogesterone acetate (DMPA; Depo-Provera) in 2004. The black box 1) indicates that use of DMPA for longer than 2 years may reduce peak bone mass and place a woman at increased risk of osteoporotic fracture and 2) suggests that ObGyns order bone-density assessment in women who use DMPA long-term.
This warning is not based on scientific evidence. By depriving women of long-term use of a safe, effective contraceptive, the black-box warning damages women’s health and the public health.
The scientific argument for removing the black box
Although DMPA does cause reduced ovarian estradiol production, with a decline in bone mineral density (BMD), complete recovery of BMD occurs approximately 1 or 2 years after discontinuation in adolescent girls1,2 and 3 years after discontinuation in adult women.3,4 BMD trends observed with the use of DMPA parallel those associated with another normal but hypoestrogenic state: breastfeeding. Although BMD declines noted in nursing mothers are similar to those associated with DMPA, breastfeeding one or more infants has not been reported to increase the risk of subsequent osteoporotic fractures.5 The FDA does not warn women against breastfeeding for fear of a theoretical negative impact on skeletal health.
BMD can help predict a risk of osteoporotic fracture in menopausal women, but it is not a valid surrogate endpoint for fracture in women of reproductive age.6 Basing clinical recommendations on invalid surrogate endpoints can cause harm.7-9 Clinical recommendations, including those from the FDA, should be based on sound studies that address important clinical outcomes.
No convincing evidence links the use of DMPA for contraception to fracture. Studies of menopausal women have not suggested that prior use of DMPA increased their risk of osteoporosis.10-12 Two recently published case-control studies, one using a Danish National Patient Registry13 and one based on the United Kingdom Family Practice Research database,14 have demonstrated that DMPA is associated with an elevated risk of fracture in reproductive-age women. However, a cohort analysis using the same British Family Practice database clarifies that the elevated fracture risk observed in women using DMPA occurred before initiation of injectable contraception and was not the result of DMPA use.15

A clearly harmful effect on women’s health
The black-box warning for DMPA has caused clinicians and women to reduce use of this effective method of contraception. The 2008 National Survey of Family Growth shows that the overall percentage of US women, 15 to 44 years of age, who now use DMPA has declined—from 3.3% in 2002 to 2.0% in 2006 to 2008.16
In fact, a survey of ObGyns in Florida found that 1) almost one half of respondents place a time limit on duration of DMPA and 2) two thirds of those respondents base that restriction on the black-box warning.17 Restricting the use of DMPA can lead to more unintended pregnancies and induced abortions.
In the Florida survey, two thirds of respondents order BMD assessment in women who use DMPA, with 58% of those physicians who do so attributing their decision to, again, the black-box warning. Indeed, more than 5% of respondents reported that they selectively prescribe bisphosphonates to women of reproductive age who use DMPA—an expensive practice that is not evidence-based and is potentially dangerous.
FDA guidance is far out of step
The black-box warning for DMPA is not in accord with the guidance provided major medical and public health organizations. The World Health Organization,6 the American College of Obstetricians and Gynecologists,18 the Society for Adolescent Medicine,19 and the Society of Obstetrics and Gynecology of Canada,20 have all stated that skeletal health concerns shouldn’t restrict the use of DMPA, including the duration of use.
In the US Medical Eligibility Criteria for contraceptive use, the Centers for Disease Control and Prevention declared that use of DMPA is Category 1 (no restriction on use) in women 18 to 45 years of age and Category 2 (advantages of the method generally outweigh theoretical or proven risks) in younger women.21 The FDA’s black-box warning is therefore inconsistent with the recommendation of its sister agency.
An opportunity to improve the health of women
The FDA appropriately takes action when a pharmaceutical company mislabels a product or promotes it in a way that isn’t based on sound evidence. Shouldn’t the FDA apply the same scientific standards to itself? Guidance included in DMPA’s black box is not evidence-based—and that reduces use of DMPA in US women and increases the potential for harm. Removing the black box would encourage use of this convenient, effective, and safe contraceptive22 and, in turn, improve the health of women and their families.
Again: We urge the FDA to promptly remove the black-box warning from labeling for DMPA.
Do you agree? We want to hear your opinion: Write to us in care of The Editors, at [email protected]!
Long-acting reversible contraceptives are safe, effective for most women, study shows
But most use other methods because of lack of knowledge and cost concerns
Long-acting reversible contraceptives (LARC) are safe and effective for almost all women of reproductive age, according to an ACOG practice bulletin published in the July issue of Obstetrics & Gynecology.
Eve Espey, MD, MPH, and Rameet H. Singh, MD, MPH, from ACOG in Washington, DC, and colleagues compiled the latest recommendations on LARC use. The recommendations identify candidates for LARCs and help obstetricians and gynecologists manage LARC-related clinical issues.
The investigators reported that the LARC methods currently available have few contraindications, and that most women are eligible to use them. Intrauterine devices (IUDs) are suitable for women with a previous ectopic pregnancy and for women immediately after abortion or miscarriage. Routine antibiotic prophylaxis is not recommended before IUD insertion.
Copper IUD inserted up to 5 days after unprotected intercourse is the most effective method of postcoital contraception. The copper IUD can be used and remains effective for up to 10 continuous years. The levonorgestrel IUD may be effective for up to 7 years.
IUD complications are rare and include expulsion, method failure, and perforation. Implants can be safely inserted at any time after childbirth in non-breastfeeding women, or after 4 weeks for breastfeeding mothers. All LARC methods are safe for nulliparous women and adolescents.
The use of IUDs increased from 1.3% to 5.5% from 2002 to 2006-2008. Despite the benefits of LARCs, the majority of women choose other birth control methods, probably due to lack of knowledge about LARCs and cost concerns.
“LARC methods are the best tool we have to fight against unintended pregnancies, which currently account for 49% of US pregnancies each year,” Espey said in a statement.
Copyright © 2011 HealthDay. All rights reserved.
Has the FDA’s warning about DMPA had a chilling effect? Does the black-box warning prevent you from prescribing DMPA? Or does it alter your approach to using it? How?
To tell us, click here
1. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatric Adolesc Med. 2005;159(2):139-144.
2. Harel Z, Johnson CC, Gold MA, et al. Recovery of bone mineral density in adolescents following the use of depot medroxyprogesterone acetate contraceptive injections. Contraception. 2010;81(4):281-291.
3. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Injectable hormone contraception and bone density: Results from a prospective study. Epidemiology. 2002;13(5):581-7.
4. Kaunitz AM, Miller PD, Rice VM, Ross D, McClung MR. Bone mineral density in women aged 25-35 years receiving depot medroxyprogesterone acetate: recovery following discontinuation. Contraception. 2006;74(2):90-99.
5. Schnatz PF, Barker KG, Marakovits KA, O’Sullivan DM. Effects of age at first pregnancy and breast-feeding on the development of postmenopausal osteoporosis. Menopause. 2010;17(6):1161-1166.
6. World Health Organization WHO Epidemiological Record No. 35: WHO statement on hormonal contraception and bone health. Geneva Switzerland: World Health Organization. 2005;80(35):302-304.
7. Grimes DA, Schulz KF. Surrogate end points in clinical research: hazardous to your health. Obstet Gynecol. 2005;105(5 pt 1):1114-1118.
8. Grimes DA, Schulz KF, Raymond EG. Surrogate end points in women’s health research: science protoscience, and pseudoscience. Fertil Steril. 2010;93(6):1731-1734.
9. Shulman LP, Bateman LH, Creinin MD, et al. Surrogate markers, emboldened and boxed warnings, and an expanding culture of misinformation: evidence-based clinical science should guide FDA decision making about product labeling. Contraception. 2006;73(5):440-442.
10. Cundy T, Cornish J, Roberts H, Reid IR. Menopausal bone loss in long-term users of depot medroxyprogesterone acetate contraception. Am J Obstet Gynecol. 2002;186(5):978-983.
11. Orr-Walker BJ, Evans MC, Ames RW, Clearwater JM, Cundy T, Reid IR. The effect of past use of the injectable contraceptive depot medroxyprogesterone acetate on bone mineral density in normal post-menopausal women. Clin Endocrinol (Oxf). 1998;49(5):615-618.
12. Viola AS, Castro S, Marchi NM, Bahamondes MV, Viola CFM, Bahamondes L. Long-term assessment of forearm bone mineral density in postmenopausal former users of depot medroxyprogesterone acetate. Contraception. In press.
13. Vestergaard P, Rejnmark L, Mosekilde L. The effects of depot medroxyprogesterone acetate and intrauterine device use on fracture risk in Danish women. Contraception. 2008;78(6):459-464.
14. Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot medroxyprogesterone acetate and fracture risk. J Clin Endocrin Metab. 2010;95(11):4909-4916.
15. Kaunitz AM, Harel Z, Bone H, et al. Retrospective cohort study of DMPA and fractures in reproductive age women. Paper presented at: Association of Reproductive Health Professional Annual Meeting; September 24, 2010; Atlanta, GA.
16. Mosher WD, Jones J. Use of contraception in the United States: 1982-2008. National Center for Health Statistics. Vital Health Stat 23. 2010;23(29):1-44.
17. Paschall S, Kaunitz AM. Depo-Provera and skeletal health: A survey of Florida obstetrics and gynecologist physicians. Contraception. 2008;78(5):370-376.
18. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 415: Depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2008;112(3):727-730.
19. Cromer BA, Scholes D, Berenson A, Cundy T, Clark MK, Kaunitz AM; Society for Adolescent Medicine. Depot medroxyprogesterone acetate and bone mineral density in adolescent—the black box warning: A position paper of the Society for Adolescent Medicine. J Adolesc Health. 2006;39(2):296-301.
20. Black A; Ad Hoc DMPA Committee of the Society of Obstetricians and Gynaecologists of Canada. Canadian contraception consensus: update on depot medroxyprogesterone acetate (DMPA). J Obstet Gynaecol Can. 2006;28(4):305-313.
21. Centers for Disease Control and Prevention. US medical eligibility criteria contraceptive use 2010. MMWR. 2010;59 (RR04);1:6.
22. Kaunitz AM, Grimes DA. Removing the black box warning for depot medroxyprogesterone acetate [published online ahead of print February 21 2011]. Contraception. doi:10.1016/j.contraception.2011.01.009.
- Update on contraception
Rachel B. Rapkin, MD; Mitchell D. Creinin, MD (August 2011) - 10 (+1) practical, evidence-based recommendations for you to improve contraceptive care now
Colleen Krajewski, MD; Mark D. Walters, MD (August 2011) - Levonorgestrel or ulipristal: Is one a better emergency contraceptive than the other?
Robert L. Barbieri, MD (Editorial; March 2011) - IUD use in nulliparous and adolescent women
Jennefer A. Russo, MD; Mitchell D. Creinin, MD (Update on Contraception, August 2010)
The Food and Drug Administration (FDA) should remove the black-box warning regarding skeletal health that the agency inserted into labeling for the injectable contraceptive depot medroxyprogesterone acetate (DMPA; Depo-Provera) in 2004. The black box 1) indicates that use of DMPA for longer than 2 years may reduce peak bone mass and place a woman at increased risk of osteoporotic fracture and 2) suggests that ObGyns order bone-density assessment in women who use DMPA long-term.
This warning is not based on scientific evidence. By depriving women of long-term use of a safe, effective contraceptive, the black-box warning damages women’s health and the public health.
The scientific argument for removing the black box
Although DMPA does cause reduced ovarian estradiol production, with a decline in bone mineral density (BMD), complete recovery of BMD occurs approximately 1 or 2 years after discontinuation in adolescent girls1,2 and 3 years after discontinuation in adult women.3,4 BMD trends observed with the use of DMPA parallel those associated with another normal but hypoestrogenic state: breastfeeding. Although BMD declines noted in nursing mothers are similar to those associated with DMPA, breastfeeding one or more infants has not been reported to increase the risk of subsequent osteoporotic fractures.5 The FDA does not warn women against breastfeeding for fear of a theoretical negative impact on skeletal health.
BMD can help predict a risk of osteoporotic fracture in menopausal women, but it is not a valid surrogate endpoint for fracture in women of reproductive age.6 Basing clinical recommendations on invalid surrogate endpoints can cause harm.7-9 Clinical recommendations, including those from the FDA, should be based on sound studies that address important clinical outcomes.
No convincing evidence links the use of DMPA for contraception to fracture. Studies of menopausal women have not suggested that prior use of DMPA increased their risk of osteoporosis.10-12 Two recently published case-control studies, one using a Danish National Patient Registry13 and one based on the United Kingdom Family Practice Research database,14 have demonstrated that DMPA is associated with an elevated risk of fracture in reproductive-age women. However, a cohort analysis using the same British Family Practice database clarifies that the elevated fracture risk observed in women using DMPA occurred before initiation of injectable contraception and was not the result of DMPA use.15

A clearly harmful effect on women’s health
The black-box warning for DMPA has caused clinicians and women to reduce use of this effective method of contraception. The 2008 National Survey of Family Growth shows that the overall percentage of US women, 15 to 44 years of age, who now use DMPA has declined—from 3.3% in 2002 to 2.0% in 2006 to 2008.16
In fact, a survey of ObGyns in Florida found that 1) almost one half of respondents place a time limit on duration of DMPA and 2) two thirds of those respondents base that restriction on the black-box warning.17 Restricting the use of DMPA can lead to more unintended pregnancies and induced abortions.
In the Florida survey, two thirds of respondents order BMD assessment in women who use DMPA, with 58% of those physicians who do so attributing their decision to, again, the black-box warning. Indeed, more than 5% of respondents reported that they selectively prescribe bisphosphonates to women of reproductive age who use DMPA—an expensive practice that is not evidence-based and is potentially dangerous.
FDA guidance is far out of step
The black-box warning for DMPA is not in accord with the guidance provided major medical and public health organizations. The World Health Organization,6 the American College of Obstetricians and Gynecologists,18 the Society for Adolescent Medicine,19 and the Society of Obstetrics and Gynecology of Canada,20 have all stated that skeletal health concerns shouldn’t restrict the use of DMPA, including the duration of use.
In the US Medical Eligibility Criteria for contraceptive use, the Centers for Disease Control and Prevention declared that use of DMPA is Category 1 (no restriction on use) in women 18 to 45 years of age and Category 2 (advantages of the method generally outweigh theoretical or proven risks) in younger women.21 The FDA’s black-box warning is therefore inconsistent with the recommendation of its sister agency.
An opportunity to improve the health of women
The FDA appropriately takes action when a pharmaceutical company mislabels a product or promotes it in a way that isn’t based on sound evidence. Shouldn’t the FDA apply the same scientific standards to itself? Guidance included in DMPA’s black box is not evidence-based—and that reduces use of DMPA in US women and increases the potential for harm. Removing the black box would encourage use of this convenient, effective, and safe contraceptive22 and, in turn, improve the health of women and their families.
Again: We urge the FDA to promptly remove the black-box warning from labeling for DMPA.
Do you agree? We want to hear your opinion: Write to us in care of The Editors, at [email protected]!
Long-acting reversible contraceptives are safe, effective for most women, study shows
But most use other methods because of lack of knowledge and cost concerns
Long-acting reversible contraceptives (LARC) are safe and effective for almost all women of reproductive age, according to an ACOG practice bulletin published in the July issue of Obstetrics & Gynecology.
Eve Espey, MD, MPH, and Rameet H. Singh, MD, MPH, from ACOG in Washington, DC, and colleagues compiled the latest recommendations on LARC use. The recommendations identify candidates for LARCs and help obstetricians and gynecologists manage LARC-related clinical issues.
The investigators reported that the LARC methods currently available have few contraindications, and that most women are eligible to use them. Intrauterine devices (IUDs) are suitable for women with a previous ectopic pregnancy and for women immediately after abortion or miscarriage. Routine antibiotic prophylaxis is not recommended before IUD insertion.
Copper IUD inserted up to 5 days after unprotected intercourse is the most effective method of postcoital contraception. The copper IUD can be used and remains effective for up to 10 continuous years. The levonorgestrel IUD may be effective for up to 7 years.
IUD complications are rare and include expulsion, method failure, and perforation. Implants can be safely inserted at any time after childbirth in non-breastfeeding women, or after 4 weeks for breastfeeding mothers. All LARC methods are safe for nulliparous women and adolescents.
The use of IUDs increased from 1.3% to 5.5% from 2002 to 2006-2008. Despite the benefits of LARCs, the majority of women choose other birth control methods, probably due to lack of knowledge about LARCs and cost concerns.
“LARC methods are the best tool we have to fight against unintended pregnancies, which currently account for 49% of US pregnancies each year,” Espey said in a statement.
Copyright © 2011 HealthDay. All rights reserved.
Has the FDA’s warning about DMPA had a chilling effect? Does the black-box warning prevent you from prescribing DMPA? Or does it alter your approach to using it? How?
To tell us, click here
- Update on contraception
Rachel B. Rapkin, MD; Mitchell D. Creinin, MD (August 2011) - 10 (+1) practical, evidence-based recommendations for you to improve contraceptive care now
Colleen Krajewski, MD; Mark D. Walters, MD (August 2011) - Levonorgestrel or ulipristal: Is one a better emergency contraceptive than the other?
Robert L. Barbieri, MD (Editorial; March 2011) - IUD use in nulliparous and adolescent women
Jennefer A. Russo, MD; Mitchell D. Creinin, MD (Update on Contraception, August 2010)
The Food and Drug Administration (FDA) should remove the black-box warning regarding skeletal health that the agency inserted into labeling for the injectable contraceptive depot medroxyprogesterone acetate (DMPA; Depo-Provera) in 2004. The black box 1) indicates that use of DMPA for longer than 2 years may reduce peak bone mass and place a woman at increased risk of osteoporotic fracture and 2) suggests that ObGyns order bone-density assessment in women who use DMPA long-term.
This warning is not based on scientific evidence. By depriving women of long-term use of a safe, effective contraceptive, the black-box warning damages women’s health and the public health.
The scientific argument for removing the black box
Although DMPA does cause reduced ovarian estradiol production, with a decline in bone mineral density (BMD), complete recovery of BMD occurs approximately 1 or 2 years after discontinuation in adolescent girls1,2 and 3 years after discontinuation in adult women.3,4 BMD trends observed with the use of DMPA parallel those associated with another normal but hypoestrogenic state: breastfeeding. Although BMD declines noted in nursing mothers are similar to those associated with DMPA, breastfeeding one or more infants has not been reported to increase the risk of subsequent osteoporotic fractures.5 The FDA does not warn women against breastfeeding for fear of a theoretical negative impact on skeletal health.
BMD can help predict a risk of osteoporotic fracture in menopausal women, but it is not a valid surrogate endpoint for fracture in women of reproductive age.6 Basing clinical recommendations on invalid surrogate endpoints can cause harm.7-9 Clinical recommendations, including those from the FDA, should be based on sound studies that address important clinical outcomes.
No convincing evidence links the use of DMPA for contraception to fracture. Studies of menopausal women have not suggested that prior use of DMPA increased their risk of osteoporosis.10-12 Two recently published case-control studies, one using a Danish National Patient Registry13 and one based on the United Kingdom Family Practice Research database,14 have demonstrated that DMPA is associated with an elevated risk of fracture in reproductive-age women. However, a cohort analysis using the same British Family Practice database clarifies that the elevated fracture risk observed in women using DMPA occurred before initiation of injectable contraception and was not the result of DMPA use.15

A clearly harmful effect on women’s health
The black-box warning for DMPA has caused clinicians and women to reduce use of this effective method of contraception. The 2008 National Survey of Family Growth shows that the overall percentage of US women, 15 to 44 years of age, who now use DMPA has declined—from 3.3% in 2002 to 2.0% in 2006 to 2008.16
In fact, a survey of ObGyns in Florida found that 1) almost one half of respondents place a time limit on duration of DMPA and 2) two thirds of those respondents base that restriction on the black-box warning.17 Restricting the use of DMPA can lead to more unintended pregnancies and induced abortions.
In the Florida survey, two thirds of respondents order BMD assessment in women who use DMPA, with 58% of those physicians who do so attributing their decision to, again, the black-box warning. Indeed, more than 5% of respondents reported that they selectively prescribe bisphosphonates to women of reproductive age who use DMPA—an expensive practice that is not evidence-based and is potentially dangerous.
FDA guidance is far out of step
The black-box warning for DMPA is not in accord with the guidance provided major medical and public health organizations. The World Health Organization,6 the American College of Obstetricians and Gynecologists,18 the Society for Adolescent Medicine,19 and the Society of Obstetrics and Gynecology of Canada,20 have all stated that skeletal health concerns shouldn’t restrict the use of DMPA, including the duration of use.
In the US Medical Eligibility Criteria for contraceptive use, the Centers for Disease Control and Prevention declared that use of DMPA is Category 1 (no restriction on use) in women 18 to 45 years of age and Category 2 (advantages of the method generally outweigh theoretical or proven risks) in younger women.21 The FDA’s black-box warning is therefore inconsistent with the recommendation of its sister agency.
An opportunity to improve the health of women
The FDA appropriately takes action when a pharmaceutical company mislabels a product or promotes it in a way that isn’t based on sound evidence. Shouldn’t the FDA apply the same scientific standards to itself? Guidance included in DMPA’s black box is not evidence-based—and that reduces use of DMPA in US women and increases the potential for harm. Removing the black box would encourage use of this convenient, effective, and safe contraceptive22 and, in turn, improve the health of women and their families.
Again: We urge the FDA to promptly remove the black-box warning from labeling for DMPA.
Do you agree? We want to hear your opinion: Write to us in care of The Editors, at [email protected]!
Long-acting reversible contraceptives are safe, effective for most women, study shows
But most use other methods because of lack of knowledge and cost concerns
Long-acting reversible contraceptives (LARC) are safe and effective for almost all women of reproductive age, according to an ACOG practice bulletin published in the July issue of Obstetrics & Gynecology.
Eve Espey, MD, MPH, and Rameet H. Singh, MD, MPH, from ACOG in Washington, DC, and colleagues compiled the latest recommendations on LARC use. The recommendations identify candidates for LARCs and help obstetricians and gynecologists manage LARC-related clinical issues.
The investigators reported that the LARC methods currently available have few contraindications, and that most women are eligible to use them. Intrauterine devices (IUDs) are suitable for women with a previous ectopic pregnancy and for women immediately after abortion or miscarriage. Routine antibiotic prophylaxis is not recommended before IUD insertion.
Copper IUD inserted up to 5 days after unprotected intercourse is the most effective method of postcoital contraception. The copper IUD can be used and remains effective for up to 10 continuous years. The levonorgestrel IUD may be effective for up to 7 years.
IUD complications are rare and include expulsion, method failure, and perforation. Implants can be safely inserted at any time after childbirth in non-breastfeeding women, or after 4 weeks for breastfeeding mothers. All LARC methods are safe for nulliparous women and adolescents.
The use of IUDs increased from 1.3% to 5.5% from 2002 to 2006-2008. Despite the benefits of LARCs, the majority of women choose other birth control methods, probably due to lack of knowledge about LARCs and cost concerns.
“LARC methods are the best tool we have to fight against unintended pregnancies, which currently account for 49% of US pregnancies each year,” Espey said in a statement.
Copyright © 2011 HealthDay. All rights reserved.
Has the FDA’s warning about DMPA had a chilling effect? Does the black-box warning prevent you from prescribing DMPA? Or does it alter your approach to using it? How?
To tell us, click here
1. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatric Adolesc Med. 2005;159(2):139-144.
2. Harel Z, Johnson CC, Gold MA, et al. Recovery of bone mineral density in adolescents following the use of depot medroxyprogesterone acetate contraceptive injections. Contraception. 2010;81(4):281-291.
3. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Injectable hormone contraception and bone density: Results from a prospective study. Epidemiology. 2002;13(5):581-7.
4. Kaunitz AM, Miller PD, Rice VM, Ross D, McClung MR. Bone mineral density in women aged 25-35 years receiving depot medroxyprogesterone acetate: recovery following discontinuation. Contraception. 2006;74(2):90-99.
5. Schnatz PF, Barker KG, Marakovits KA, O’Sullivan DM. Effects of age at first pregnancy and breast-feeding on the development of postmenopausal osteoporosis. Menopause. 2010;17(6):1161-1166.
6. World Health Organization WHO Epidemiological Record No. 35: WHO statement on hormonal contraception and bone health. Geneva Switzerland: World Health Organization. 2005;80(35):302-304.
7. Grimes DA, Schulz KF. Surrogate end points in clinical research: hazardous to your health. Obstet Gynecol. 2005;105(5 pt 1):1114-1118.
8. Grimes DA, Schulz KF, Raymond EG. Surrogate end points in women’s health research: science protoscience, and pseudoscience. Fertil Steril. 2010;93(6):1731-1734.
9. Shulman LP, Bateman LH, Creinin MD, et al. Surrogate markers, emboldened and boxed warnings, and an expanding culture of misinformation: evidence-based clinical science should guide FDA decision making about product labeling. Contraception. 2006;73(5):440-442.
10. Cundy T, Cornish J, Roberts H, Reid IR. Menopausal bone loss in long-term users of depot medroxyprogesterone acetate contraception. Am J Obstet Gynecol. 2002;186(5):978-983.
11. Orr-Walker BJ, Evans MC, Ames RW, Clearwater JM, Cundy T, Reid IR. The effect of past use of the injectable contraceptive depot medroxyprogesterone acetate on bone mineral density in normal post-menopausal women. Clin Endocrinol (Oxf). 1998;49(5):615-618.
12. Viola AS, Castro S, Marchi NM, Bahamondes MV, Viola CFM, Bahamondes L. Long-term assessment of forearm bone mineral density in postmenopausal former users of depot medroxyprogesterone acetate. Contraception. In press.
13. Vestergaard P, Rejnmark L, Mosekilde L. The effects of depot medroxyprogesterone acetate and intrauterine device use on fracture risk in Danish women. Contraception. 2008;78(6):459-464.
14. Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot medroxyprogesterone acetate and fracture risk. J Clin Endocrin Metab. 2010;95(11):4909-4916.
15. Kaunitz AM, Harel Z, Bone H, et al. Retrospective cohort study of DMPA and fractures in reproductive age women. Paper presented at: Association of Reproductive Health Professional Annual Meeting; September 24, 2010; Atlanta, GA.
16. Mosher WD, Jones J. Use of contraception in the United States: 1982-2008. National Center for Health Statistics. Vital Health Stat 23. 2010;23(29):1-44.
17. Paschall S, Kaunitz AM. Depo-Provera and skeletal health: A survey of Florida obstetrics and gynecologist physicians. Contraception. 2008;78(5):370-376.
18. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 415: Depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2008;112(3):727-730.
19. Cromer BA, Scholes D, Berenson A, Cundy T, Clark MK, Kaunitz AM; Society for Adolescent Medicine. Depot medroxyprogesterone acetate and bone mineral density in adolescent—the black box warning: A position paper of the Society for Adolescent Medicine. J Adolesc Health. 2006;39(2):296-301.
20. Black A; Ad Hoc DMPA Committee of the Society of Obstetricians and Gynaecologists of Canada. Canadian contraception consensus: update on depot medroxyprogesterone acetate (DMPA). J Obstet Gynaecol Can. 2006;28(4):305-313.
21. Centers for Disease Control and Prevention. US medical eligibility criteria contraceptive use 2010. MMWR. 2010;59 (RR04);1:6.
22. Kaunitz AM, Grimes DA. Removing the black box warning for depot medroxyprogesterone acetate [published online ahead of print February 21 2011]. Contraception. doi:10.1016/j.contraception.2011.01.009.
1. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Change in bone mineral density among adolescent women using and discontinuing depot medroxyprogesterone acetate contraception. Arch Pediatric Adolesc Med. 2005;159(2):139-144.
2. Harel Z, Johnson CC, Gold MA, et al. Recovery of bone mineral density in adolescents following the use of depot medroxyprogesterone acetate contraceptive injections. Contraception. 2010;81(4):281-291.
3. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Injectable hormone contraception and bone density: Results from a prospective study. Epidemiology. 2002;13(5):581-7.
4. Kaunitz AM, Miller PD, Rice VM, Ross D, McClung MR. Bone mineral density in women aged 25-35 years receiving depot medroxyprogesterone acetate: recovery following discontinuation. Contraception. 2006;74(2):90-99.
5. Schnatz PF, Barker KG, Marakovits KA, O’Sullivan DM. Effects of age at first pregnancy and breast-feeding on the development of postmenopausal osteoporosis. Menopause. 2010;17(6):1161-1166.
6. World Health Organization WHO Epidemiological Record No. 35: WHO statement on hormonal contraception and bone health. Geneva Switzerland: World Health Organization. 2005;80(35):302-304.
7. Grimes DA, Schulz KF. Surrogate end points in clinical research: hazardous to your health. Obstet Gynecol. 2005;105(5 pt 1):1114-1118.
8. Grimes DA, Schulz KF, Raymond EG. Surrogate end points in women’s health research: science protoscience, and pseudoscience. Fertil Steril. 2010;93(6):1731-1734.
9. Shulman LP, Bateman LH, Creinin MD, et al. Surrogate markers, emboldened and boxed warnings, and an expanding culture of misinformation: evidence-based clinical science should guide FDA decision making about product labeling. Contraception. 2006;73(5):440-442.
10. Cundy T, Cornish J, Roberts H, Reid IR. Menopausal bone loss in long-term users of depot medroxyprogesterone acetate contraception. Am J Obstet Gynecol. 2002;186(5):978-983.
11. Orr-Walker BJ, Evans MC, Ames RW, Clearwater JM, Cundy T, Reid IR. The effect of past use of the injectable contraceptive depot medroxyprogesterone acetate on bone mineral density in normal post-menopausal women. Clin Endocrinol (Oxf). 1998;49(5):615-618.
12. Viola AS, Castro S, Marchi NM, Bahamondes MV, Viola CFM, Bahamondes L. Long-term assessment of forearm bone mineral density in postmenopausal former users of depot medroxyprogesterone acetate. Contraception. In press.
13. Vestergaard P, Rejnmark L, Mosekilde L. The effects of depot medroxyprogesterone acetate and intrauterine device use on fracture risk in Danish women. Contraception. 2008;78(6):459-464.
14. Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot medroxyprogesterone acetate and fracture risk. J Clin Endocrin Metab. 2010;95(11):4909-4916.
15. Kaunitz AM, Harel Z, Bone H, et al. Retrospective cohort study of DMPA and fractures in reproductive age women. Paper presented at: Association of Reproductive Health Professional Annual Meeting; September 24, 2010; Atlanta, GA.
16. Mosher WD, Jones J. Use of contraception in the United States: 1982-2008. National Center for Health Statistics. Vital Health Stat 23. 2010;23(29):1-44.
17. Paschall S, Kaunitz AM. Depo-Provera and skeletal health: A survey of Florida obstetrics and gynecologist physicians. Contraception. 2008;78(5):370-376.
18. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. ACOG Committee Opinion No. 415: Depot medroxyprogesterone acetate and bone effects. Obstet Gynecol. 2008;112(3):727-730.
19. Cromer BA, Scholes D, Berenson A, Cundy T, Clark MK, Kaunitz AM; Society for Adolescent Medicine. Depot medroxyprogesterone acetate and bone mineral density in adolescent—the black box warning: A position paper of the Society for Adolescent Medicine. J Adolesc Health. 2006;39(2):296-301.
20. Black A; Ad Hoc DMPA Committee of the Society of Obstetricians and Gynaecologists of Canada. Canadian contraception consensus: update on depot medroxyprogesterone acetate (DMPA). J Obstet Gynaecol Can. 2006;28(4):305-313.
21. Centers for Disease Control and Prevention. US medical eligibility criteria contraceptive use 2010. MMWR. 2010;59 (RR04);1:6.
22. Kaunitz AM, Grimes DA. Removing the black box warning for depot medroxyprogesterone acetate [published online ahead of print February 21 2011]. Contraception. doi:10.1016/j.contraception.2011.01.009.
IN THIS ARTICLE
UPDATE ON MENOPAUSE
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
- Is hormone therapy still a valid option? 12 ObGyns address this question
Members of the OBG MANAGEMENT Virtual Board of Editors and Janelle Yates, Senior Editor (May 2011)
Dr. Kaunitz receives grant or research support from Bayer, Agile, Noven, Teva, and Medical Diagnostic Laboratories, is a consultant to Bayer, Merck, and Teva, and owns stock in Becton Dickinson.
Among the developments of the past year in the care of menopausal women are:
- updated guidelines from the Institute of Medicine regarding vitamin D requirements—suggesting that fewer women are deficient in this nutrient than experts had believed
- new data from Europe on hormone therapy (HT) that highlight the safety of transdermal estrogen in comparison with oral administration
- a recent analysis from the Women’s Health Initiative (WHI), confirming a small elevated risk of breast cancer mortality with use of combination estrogen-progestin HT
- confirmation that age at initiation of HT determines its effect on cardiovascular health
- clarification of the association between HT and dementia
- new data demonstrating modest improvement in hot flushes when the serotonin reuptake inhibitor (SRI) escitalopram is used
- a brand new report from the WHI estrogen-alone arm that shows a protective effect against breast cancer.
The new data on HT suggest that we still have much to learn about its benefits and risks. We also are reaching an understanding that, for many young, symptomatic, menopausal patients, HT can represent a safe choice, with much depending on the timing and duration of therapy.
For more on how your colleagues are managing menopausal patients with and without hormone therapy, see “Is hormone therapy still a valid option? 12 ObGyns address this question,” on the facing page.
Menopausal women need less vitamin D than we thought
Institute of Medicine. Dietary reference intakes for calcium and vitamin D. Washington, DC: IOM; December 2010. http://www.iom.edu/~/media/Files/Report%20Files/2010/Dietary-Reference-Intakes-for-Calcium-and-Vitamin-D/Vitamin%20D%20and%20Calcium%202010%20Report%20Brief.pdf. Accessed March 24, 2011.
In the 2010 Update on Menopause, I summarized recent findings on vitamin D requirements, including recommendations that menopausal women should take at least 800 IU of vitamin D daily. I also described the prevailing expert opinion that many North American women are deficient in this nutrient.
What a difference a year can make! In late November, the Institute of Medicine (IOM) released a comprehensive report on vitamin D. Here are some of its conclusions:
- Vitamin D plays an important role in skeletal health but its role in other areas, including cardiovascular disease and cancer, is uncertain
- An intake of 600 IU of vitamin D daily is appropriate for girls and for women as old as 70 years; an in-take of 800 IU daily is appropriate for women older than 70 years
- A serum level of 25-hydroxy vitamin D of 20 ng/mL is consistent with adequate vitamin D status; this is lower than the threshold many have recommended
- With few exceptions, all people who live in North America—including those who have minimal or no exposure to sunlight—are receiving adequate calcium and vitamin D
- Ingestion of more than 4,000 IU of vitamin D daily can cause renal damage and injure other tissues.
The IOM report will likely prompt multivitamin manufacturers to increase the amount of vitamin D contained in their supplements to 600 IU daily. In addition, the report will probably discourage the common practice of checking serum 25-hydroxy vitamin D levels and prescribing a high dosage of vitamin D supplementation when the level is below 30 ng/mL.
I continue to recommend multivitamin supplements that include calcium and vitamin D (but no iron) to my menopausal patients. However, I no longer routinely recommend that they take additional calcium and vitamin D or undergo assessment of serum vitamin D levels.
Is transdermal estrogen safer than oral administration?
Canonico M, Fournier A, Carcaillon L, et al. Postmenopausal hormone therapy and risk of idiopathic venous thromboembolism: results from the E3N cohort study. Arterioscler Thromb Vasc Biol. 2010;30(2):340–345.
Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010;340:c2519. doi: 10.1136/bmj.c2519.
In the WHI, the combination of oral conjugated equine estrogen and medroxyprogesterone acetate more than doubled the risk of deep venous thrombosis and pulmonary embolism and modestly increased the risk of stroke, compared with nonuse.1
A year after publication of the initial findings of the WHI estrogen-progestin arm, the Estrogen and THromboEmbolism Risk Study Group (ESTHER) case-control study from France provided evidence that transdermal estrogen does not increase the risk of venous thrombosis.2 In France, many menopausal women use HT, and the transdermal route of administration is common.
In 2010, the E3N cohort study from France also assessed the risk of thrombosis associated with oral and transdermal HT. Investigators followed more than 80,000 postmenopausal women and found that, unlike oral HT, the transdermal route did not increase the risk of venous thrombosis.
More recent evidence also suggests a safety advantage for transdermal HT. The newest data come from the United Kingdom General Practice Research Database, which includes information on more than 870,000 women who were 50 to 70 years old from 1987 to 2006. Investigators identified more than 15,000 women who were given a diagnosis of stroke during this period and compared the use of HT in these women with that of almost 60,000 women in a control group. The risk of stroke associated with current use of transdermal HT was similar to the risk associated with nonuse of HT. Women who used a patch containing 0.05 mg of estradiol or less had a risk of stroke 19% lower than women who did not use HT.
In contrast, the risk of stroke in users of patches that contained a higher dosage of estradiol was almost twice the risk in nonusers of HT. Current users of oral HT had a risk of stroke 28% higher than that of nonusers of HT.
The WHI assessed the risks and benefits of oral HT only. Although no randomized, clinical trial has compared cardiovascular risks among users of oral and transdermal HT, I believe that a preponderance of evidence points to a superior safety profile for the transdermal route, particularly at a dosage of 0.05 mg of estradiol or less.
I encourage my patients who are initiating HT to consider the transdermal route—particularly women who have an elevated risk of cardiovascular disease, including those who are overweight, smoke cigarettes, or who have hypertension or diabetes. I suggest the transdermal route despite its higher cost (oral micronized estradiol can be purchased for as little as $4 for a month’s supply at a chain pharmacy).
When a patient prefers to avoid a patch (because of local irritation), I offer her estradiol gel or spray or the vaginal ring. (Femring is systemic estradiol, whereas Estring is local.) These formulations should provide the same safety benefits as the patch.
Estrogen-progestin HT raises the risk of death from breast cancer
Chlebowski RT, Anderson GL, Gass M, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304(15):1684–1692.
Toh S, Hernandez-Diaz S, Logan R, Rossouw JE, Hernan MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin: does the increased risk ever disappear? Ann Intern Med. 2010;152(4):211–217.
In the estrogen-progestin arm of the WHI, initially published in 2002, the risk of invasive breast cancer was modestly elevated (hazard ratio [HR], 1.26) among women who had used HT longer than 5 years.3
In 2010, investigators reported on breast cancer mortality in WHI participants at a mean follow-up of 11 years. They found that combination HT users had breast cancer histology similar to that of nonusers. However, the tumors were more likely to be node-positive in combination HT users (23.7% vs 16.2%). In addition, breast cancer mortality was slightly higher among users of HT (2.6 vs 1.3 deaths in every 10,000 woman-years) (HR, 1.96; 95% confidence interval, 1.00–4.04).
Earlier observational studies had suggested that the death rate from breast cancer is lower in users of combination HT than in nonusers. Consistent with the UK Million Women Study, however, a 2010 report from the WHI found a higher mortality rate among women who have used HT.4
These new WHI findings reinforce the importance of assessing whether micronized progesterone combined with estrogen might lower the risk of death from breast cancer—a possibility suggested by findings of the French E3N cohort study.5
In addition, given the possibility that HT may be cardioprotective when it is initiated within 10 years after the onset of menopause, a WHI report that addresses long-term all-cause mortality would allow us to better counsel our menopausal patients who are trying to decide whether to start or continue HT. See, for example, the data from the California Teachers Study (below) and the estrogen-alone arm of the WHI (page 46).
The findings of this important WHI publication have strengthened the resolve of some clinicians to stop prescribing HT for menopausal women. I continue to prescribe HT to patients who have bothersome vasomotor and related symptoms, however. I also counsel women about the other benefits of HT, which include alleviation of genital atrophy and prevention of osteoporotic fractures. For patients considering or using estrogen-progestin HT, I include discussion of the small increase in their risk of developing, and dying from, breast cancer.
Age at initiation of HT determines its effect on CHD
Stram DO, Liu Y, Henderson KD, et al. Age-specific effects of hormone therapy use on overall mortality and ischemic heart disease mortality among women in the California Teachers Study. Menopause 2011;18(3):253-261.
Allison MA, Manson JE. Age, hormone therapy use, coronary heart disease, and mortality [editorial]. Menopause. 2011;18(3):243-245.
The initial findings of the WHI estrogen-progestin arm suggested that menopausal HT increases the risk of CHD. Since then, however, further analyses from the WHI and other HT trials, as well as reports from the observational Nurses’ Health Study, have suggested that the timing of initiation of HT determines its effect on cardiovascular health.
In this study from the California Teachers Study (CTS), investigators explored the effect of age at initiation of HT on cardiovascular and overall mortality. The CTS is a prospective study of more than 133,000 current and retired female teachers and administrators who returned an initial questionnaire in 1995 and 1996. Participants were then followed until late 2004, or death, whichever came first. More than 71,000 participants were eligible for analysis.
Current HT users were leaner, less likely to smoke, and more likely to exercise and consume alcohol than nonusers were. The analysis was adjusted for a variety of potential cardiovascular and other confounders.
Youngest HT users had the lowest risk of death
During follow-up, 18.3% of never-users of HT died, compared with 17.9% of former users. In contrast, 6.9% of women taking HT at the time of the baseline questionnaire died during follow-up.
Overall, current HT use was associated with a reduced risk of death from CHD (hazard ratio [HR], 0.84; 95% confidence interval, 0.74–0.95). This risk reduction was most notable (HR, 0.38) in the youngest HT users (36 to 59 years old). The risk of death from CHD gradually increased with the age of current HT users, reaching a hazard ratio of approximately 0.9 in current users who were 70 years and older. However, the CHD mortality hazard ratio did not reach or exceed the referent hazard ratio (1.0) assigned to never users of HT of any age.
The overall mortality rate was lowest for the youngest HT users (HR, 0.54) and approached 1.0 in the oldest current HT users.
The associations between overall and CHD mortality were similar among users of estrogen-only and estrogen-progestin HT.
As Allison and Manson point out in an editorial accompanying this study, the findings from the CTS are congruent with an extensive body of evidence from women and nonhuman primates. These data provide robust reassurance that HT does not increase the risk of death from CHD when it is used by recently menopausal women who have bothersome vasomotor symptoms.
Hormone therapy and dementia: Earlier use is better
Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169.
Alzheimer’s disease is more common among women than men. In addition, caregivers to those who have dementia are more likely to be women. Therefore, it’s no surprise that women are especially concerned about their risk of dementia. Menopausal patients in my practice often ask whether use of HT might alter this risk.
Because vasomotor symptoms usually arise in late perimenopause or early menopause, women in observational studies (which reflect clinical practice) tend to begin HT when they are in their late 40s or early 50s. Overall, observational studies have suggested that HT is associated with a reduced risk of dementia. In contrast, the WHI clinical trial, in which the mean age of women who were randomized to HT or placebo was 63 years, found that the initiation of HT later in life increased the risk of dementia.
These observations led to the “critical window” theory regarding HT and dementia: Estrogen protects against dementia when it is taken by perimenopausal or early menopausal women, whereas it is not protective and may even accelerate cognitive decline when it is started many years after the onset of menopause.
In this recent study from the California Kaiser Permanente health maintenance organization, investigators assessed the long-term risk of dementia by timing of HT. From 1964 through 1973, menopausal “midlife” women who were 40 to 55 years old and free of dementia reported whether or not they used HT. Twenty-five to 30 years later, participants were reassessed for “late life” HT use.
Women who used HT in midlife only had the lowest prevalence of dementia, whereas those who used HT only in late life had the highest prevalence. Women who used HT at both time points had a prevalence of dementia similar to that of women who had never used HT.
Given these important findings, I believe it is now reasonable to counsel women in late perimenopause and early menopause that the use of HT may lower their risk of dementia. How long we should continue to prescribe HT depends on individual variables, including the presence of vasomotor symptoms, the risk of osteoporosis, and concerns about breast cancer.
I encourage women to taper their dosage of HT over time, aiming at complete discontinuation or a low maintenance dosage.
Are SRIs an effective alternative to HT for hot flushes?
Freeman EW, Guthrie K, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. JAMA. 2011;305(3):267–274.
Interest in nonhormonal management of menopausal vasomotor symptoms continues to run high, although only hormonal therapy has FDA approval for this indication. Many trials of serotonin reuptake inhibitors (SRIs) for the treatment of vasomotor symptoms have focused on breast cancer survivors, many of whom use anti-estrogen agents that increase the prevalence of these symptoms. In contrast, this well-conducted multicenter trial, funded by the National Institutes of Health, enrolled healthy, symptomatic, menopausal women.
In the trial, 205 perimenopausal or postmenopausal women 40 to 62 years old who had at least 28 bothersome or severe episodes of hot flushes and night sweats a week were randomized to 10 mg daily of the SRI escitalopram (Lexapro) or placebo for 8 weeks. Women who did not report a reduction in hot flushes and night sweats of at least 50% at 4 weeks, or a decrease in the severity of these symptoms, were increased to a dosage of 20 mg daily of escitalopram or placebo. The mean baseline frequency of vasomotor symptoms was 9.79.
Within 1 week, women taking the SRI experienced significantly greater improvement than those taking placebo. By 8 weeks, the daily frequency of vasomotor symptoms had diminished by 4.6 hot flushes among women taking the SRI, compared with 3.20 among women taking placebo (P < .01).
Overall, adverse effects were reported by approximately 58% of participants. The pattern of these side effects was similar in the active and placebo treatment arms. No adverse events serious enough to require withdrawal from the study were reported in either arm.
Patient satisfaction with treatment was 70% in the SRI group, compared with 43% among women taking placebo (P < .001).
Although Freeman and colleagues convincingly demonstrate that escitalopram is more effective than placebo, the drug is less effective than HT. I agree with Nelson and coworkers, who, in a meta-analysis of nonhormonal treatments for vasomotor symptoms, concluded: “These therapies may be most useful for highly symptomatic women who cannot take estrogen but are not optimal choices for most women.”6
Unopposed estrogen appears to protect against breast cancer
LaCroix AZ, Chlebowski RT, Manson JE, et al; WHI Investigators. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy. A randomized controlled trial. JAMA. 2011;305(13):1305–1314.
The WHI continues to surprise with its findings almost a decade after publication of initial data. In this brand new report from the estrogen-alone arm, postmenopausal, hysterectomized women who were followed for a mean of 10.7 years experienced a reduced risk of breast cancer after a mean of 5.9 years of use of conjugated equine estrogens (CEE).
They experienced no increased or diminished risk of coronary heart disease (CHD), deep venous thrombosis, stroke, hip fracture, colorectal cancer, or total mortality after post-intervention follow-up.
Keep in mind that the women in this arm were instructed to discontinue the study medication at the time the intervention phase was halted because of an increased risk of stroke among CEE users. The elevated risk of stroke attenuated with the longer follow-up.
All ages experienced a reduced risk of breast cancer
Some subgroup analyses from the WHI have found differential effects of HT by age of the user, with younger women experiencing fewer risks and more benefits than those who are more than 10 years past the menopausal transition. In this analysis, all three age groups (50–59 years, 60–69 years, and 70–79 years) of women who used CEE had a reduced risk of breast cancer, compared with placebo users.
Other risks did appear to differ by age. For example, the overall hazard ratio for CHD was 0.59 among CEE users 50 to 59 years old, but it approached unity among the older women.
As new and seemingly conflicting data are published, many clinicians and their menopausal patients may feel confused and frustrated. My perspective: It is becoming clear that age during HT use matters with respect to CHD and dementia, and that estrogen-only HT has a different impact on breast cancer risk than does combination estrogen-progestin HT. When this new information from the WHI is considered in aggregate with earlier WHI reports, as well as with data from the Nurses Health Study, the California Teachers Study, and Kaiser Permanente, we can, with growing confidence, advise our patients that menopausal HT does not increase the risk of fatal CHD and may reduce the risk of dementia when used by younger menopausal women with bothersome symptoms. I would define “younger” here as an age younger than 60 years or within 10 years of the onset of menopause.
In regard to breast cancer, it is now clear that, although estrogen-only HT lowers risk, use of combination estrogen-progestin therapy for more than approximately 5 years modestly elevates risk. Each menopausal woman may use this information to make an individual decision regarding use of HT.
In sum, current evidence allows me to feel comfortable counseling most young menopausal women who have bothersome symptoms that the initiation of HT for symptom relief is a safe and reasonable option.
We want to hear from you! Tell us what you think.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
1. Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative Randomized Controlled Trial. JAMA. 2002;288(3):321-333.
2. Scarabin PY, Oger E, Plu-Bureau G. Estrogen and THromboembolism Risk (ESTHER) Study Group. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362(9382):428-432.
3. Anderson GL, Chlebowski RT, Rossouw JE, et al. Prior hormone therapy and breast cancer risk in the Women’s Health Initiative randomized trial of estrogen and progestin. Maturitas. 2006;55(2):103-115.
4. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003;362(9382):419-427.
5. Fournier A, Fabre A, Misrine S, et al. Use of different postmenopausal hormone therapies and risk of histology- and hormone receptor-defined invasive breast cancer. J Clin Oncol. 2008;26(8):1260-1268.
6. Nelson HD, Vesco KK, Haney E, et al. Nonhormonal therapies for menopausal hot flashes: systematic review and meta-analysis. JAMA. 2006;295(17):2057-2071.
Is population-based screening for endometrial cancer feasible?
- At what thickness is the endometrial stripe cause for concern in a woman who has postmenopausal bleeding?
Linda R. Duska, MD (Examining the Evidence, October 2010) - Update on endometrial cancer
David G. Mutch, MD; B. J. Rimel, MD (July 2009)
Although endometrial cancer is the most common gynecologic malignancy in the United States, population-based screening has not been recommended. In this study—the only large-scale study to focus on the use of TVS in endometrial cancer screening—Jacobs and colleagues correlated endometrial thickness and any endometrial abnormalities detected during screening with a subsequent diagnosis of endometrial neoplasia (cancer or atypical hyperplasia). In an analysis of 96 asymptomatic women who were found to have endometrial neoplasia at the time of TVS, a cutoff for endometrial thickness of 5 mm or more was associated with 77.1% sensitivity and 85.8% specificity.
Among the variables associated with a higher risk of endometrial neoplasia were weight, age, and a personal history of breast cancer. Among those associated with a lower risk of neoplasia were use of oral contraceptives, age at menarche, and parity.
Jacobs and colleagues used these risk factors to divide women into quartiles. Women in the highest quartile had a relative risk (RR) of endometrial neoplasia of 1.98, and 39.5% of cases fell into this quartile. In this quartile, a cutoff for endometrial thickness of 6.75 mm or more was associated with sensitivity of 84.3% and specificity of 89.9%.
One finding is inexplicable
In an editorial accompanying this study, Vergote and colleagues call attention to what they consider to be an inexplicable finding: The optimal cutoff for endometrial thickness in the highest-risk quartile was greater than it was for the lower-risk women.1 They also point to the lack of data on subsequent procedures, such as endometrial biopsy and hysteroscopy, in women who had falsely positive TVS findings. And they emphasize their belief that the study should not lead clinicians to perform biopsies in asymptomatic women who are found to have an endometrial thickness greater than 5 mm.
Last, the editorialists, all of whom are gynecologic oncologists, appropriately point out that not all endometrial neoplasia is life-threatening. Therefore, the long-term survival advantage of detecting endometrial neoplasia in asymptomatic women is uncertain.
The findings of Jacobs and colleagues form the basis for further large-scale study of screening for endometrial cancer in asymptomatic women. But until such studies are conducted and reported (and then only if findings support a benefit from screening), there is no justification for screening asymptomatic postmenopausal women using TVS.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Vergote I, Amant F, Timmerman D. Should we screen for endometrial cancer? Lancet Oncol. 2011;12(1):4-5.
- At what thickness is the endometrial stripe cause for concern in a woman who has postmenopausal bleeding?
Linda R. Duska, MD (Examining the Evidence, October 2010) - Update on endometrial cancer
David G. Mutch, MD; B. J. Rimel, MD (July 2009)
Although endometrial cancer is the most common gynecologic malignancy in the United States, population-based screening has not been recommended. In this study—the only large-scale study to focus on the use of TVS in endometrial cancer screening—Jacobs and colleagues correlated endometrial thickness and any endometrial abnormalities detected during screening with a subsequent diagnosis of endometrial neoplasia (cancer or atypical hyperplasia). In an analysis of 96 asymptomatic women who were found to have endometrial neoplasia at the time of TVS, a cutoff for endometrial thickness of 5 mm or more was associated with 77.1% sensitivity and 85.8% specificity.
Among the variables associated with a higher risk of endometrial neoplasia were weight, age, and a personal history of breast cancer. Among those associated with a lower risk of neoplasia were use of oral contraceptives, age at menarche, and parity.
Jacobs and colleagues used these risk factors to divide women into quartiles. Women in the highest quartile had a relative risk (RR) of endometrial neoplasia of 1.98, and 39.5% of cases fell into this quartile. In this quartile, a cutoff for endometrial thickness of 6.75 mm or more was associated with sensitivity of 84.3% and specificity of 89.9%.
One finding is inexplicable
In an editorial accompanying this study, Vergote and colleagues call attention to what they consider to be an inexplicable finding: The optimal cutoff for endometrial thickness in the highest-risk quartile was greater than it was for the lower-risk women.1 They also point to the lack of data on subsequent procedures, such as endometrial biopsy and hysteroscopy, in women who had falsely positive TVS findings. And they emphasize their belief that the study should not lead clinicians to perform biopsies in asymptomatic women who are found to have an endometrial thickness greater than 5 mm.
Last, the editorialists, all of whom are gynecologic oncologists, appropriately point out that not all endometrial neoplasia is life-threatening. Therefore, the long-term survival advantage of detecting endometrial neoplasia in asymptomatic women is uncertain.
The findings of Jacobs and colleagues form the basis for further large-scale study of screening for endometrial cancer in asymptomatic women. But until such studies are conducted and reported (and then only if findings support a benefit from screening), there is no justification for screening asymptomatic postmenopausal women using TVS.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
- At what thickness is the endometrial stripe cause for concern in a woman who has postmenopausal bleeding?
Linda R. Duska, MD (Examining the Evidence, October 2010) - Update on endometrial cancer
David G. Mutch, MD; B. J. Rimel, MD (July 2009)
Although endometrial cancer is the most common gynecologic malignancy in the United States, population-based screening has not been recommended. In this study—the only large-scale study to focus on the use of TVS in endometrial cancer screening—Jacobs and colleagues correlated endometrial thickness and any endometrial abnormalities detected during screening with a subsequent diagnosis of endometrial neoplasia (cancer or atypical hyperplasia). In an analysis of 96 asymptomatic women who were found to have endometrial neoplasia at the time of TVS, a cutoff for endometrial thickness of 5 mm or more was associated with 77.1% sensitivity and 85.8% specificity.
Among the variables associated with a higher risk of endometrial neoplasia were weight, age, and a personal history of breast cancer. Among those associated with a lower risk of neoplasia were use of oral contraceptives, age at menarche, and parity.
Jacobs and colleagues used these risk factors to divide women into quartiles. Women in the highest quartile had a relative risk (RR) of endometrial neoplasia of 1.98, and 39.5% of cases fell into this quartile. In this quartile, a cutoff for endometrial thickness of 6.75 mm or more was associated with sensitivity of 84.3% and specificity of 89.9%.
One finding is inexplicable
In an editorial accompanying this study, Vergote and colleagues call attention to what they consider to be an inexplicable finding: The optimal cutoff for endometrial thickness in the highest-risk quartile was greater than it was for the lower-risk women.1 They also point to the lack of data on subsequent procedures, such as endometrial biopsy and hysteroscopy, in women who had falsely positive TVS findings. And they emphasize their belief that the study should not lead clinicians to perform biopsies in asymptomatic women who are found to have an endometrial thickness greater than 5 mm.
Last, the editorialists, all of whom are gynecologic oncologists, appropriately point out that not all endometrial neoplasia is life-threatening. Therefore, the long-term survival advantage of detecting endometrial neoplasia in asymptomatic women is uncertain.
The findings of Jacobs and colleagues form the basis for further large-scale study of screening for endometrial cancer in asymptomatic women. But until such studies are conducted and reported (and then only if findings support a benefit from screening), there is no justification for screening asymptomatic postmenopausal women using TVS.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Vergote I, Amant F, Timmerman D. Should we screen for endometrial cancer? Lancet Oncol. 2011;12(1):4-5.
1. Vergote I, Amant F, Timmerman D. Should we screen for endometrial cancer? Lancet Oncol. 2011;12(1):4-5.
Just how much does screening mammography reduce mortality from breast cancer?
In its 2009 assessment of the benefits of screening mammography among women 50 to 69 years old, the US Preventive Services Task Force (USPSTF) estimated that the modality reduces mortality from breast cancer by 14% to 32%. However, that estimate is based on studies conducted more than 20 years ago.1
In 1996, some parts of Norway began to offer screening mammography. By 2005, screening had become universally available in the country, with more than 75% of the eligible population participating. During that decade, Norway also established multidisciplinary teams to improve the management of women given a diagnosis of breast cancer.
To determine the effects of modern screening, investigators in Norway compared breast cancer mortality in four groups:
- women who lived, from 1996 through 2005, in counties in that country that offered mammography screening
- those who lived, from 1986 through 1995, in these same counties
- those who lived, from 1996 through 2005, in counties that did not offer screening
- those who lived, from 1986 through 1995, in these same counties.
The impact of the combination of mammography screening and multidisciplinary management of breast cancer cases was a 10% reduction in breast cancer mortality. Women who did not undergo mammography screening but whose cancers were treated according to the new paradigm experienced an 8% reduction in breast cancer mortality. That suggests that the reduction in mortality that can be attributed solely to screening mammography is a surprisingly low 2%. In other words, mammography may prevent as few as 2.4 deaths for every 100,000 person-years.
Although these numbers may appear to be strikingly low, the authors point out that they are consistent with those from Britain’s national screening program.
Can the low figures be good news?
Although some practitioners may view these data with confusion or even hostility, I see the findings of this study as good news: We have improved our treatment of breast cancer so dramatically over the past few decades that the benefits of early diagnosis have become attenuated. As an editorial accompanying the Norwegian study postulates, “It is quite plausible that screening mammography was more effective in the past than it is now. If women with new breast lumps now present earlier for evaluation, the benefit of screening will be less. If treatment of clinically detected breast cancer (i.e., tumors that are detected by means other than screening) has now improved, the benefit of screening will be less. Thus, the increased awareness about the importance of promptly seeking care for overt breast abnormalities (there is no debate about diagnostic mammography) and the widespread use of adjuvant therapy may have combined to make screening now less important.”2
What about women under 50?
Breast cancer is uncommon in women in their 40s, and screening mammograms are associated with a high rate of false-positive results and unnecessary additional imaging and biopsies in this age group. In late 2009, these observations led the USPSTF to recommend against routinely screening women 40 to 49 years old.3
Now, a study from Sweden provides data that contradict that position.4 In Sweden, a screening-mammography program was initiated for women 40 to 74 years old between 1986 and 1997. In 1987 and 1988, national guidelines were revised to allow counties that faced financial challenges to curtail screening for women younger than 50 years. At that time, about 50% of Swedish counties discontinued screening of younger women. The remaining counties continued screening women in their 40s at intervals ranging from 18 to 24 months.
From 1986 through 2005, 803 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were screened by mammography (7.3 million person-years). During the same period, 1,238 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were not screened by mammography (8.8 million person-years).
Investigators calculated the odds ratio (OR) for fatal breast cancer among women who were screened in their 40s: 0.71 (95% confidence interval [CI], 0.62–0.80). They also estimated that, over a 10-year period (roughly six screening mammograms), one case of fatal breast cancer was prevented among every 1,252 women screened.
Picture remains a bit murky
Coming less than a year after the aforementioned USPSTF recommendations against screening women under 50, and right on the heels of the Norwegian study minimizing the value of screening in women 50 to 69 years old, these new data have ignited controversy.
Unlike their Norwegian counterparts, Swedish investigators failed to report mortality rates, making interpretation of the data difficult. Nor did they detail the health costs of mammograms among women in their 40s.
Note: For more on the debate over screening mammography, see Dr. Kaunitz’s earlier commentary on the subject, “I’ve been rethinking my zeal for breast cancer screening,” in the December 2009 issue of OBG Management, and Dr. Robert L. Barbieri’s distinctive viewpoint, “Access to screening mammography: Priceless,” in the January 2010 issue at obgmanagement.com.
For the foreseeable future, most clinicians will continue to recommend regular screening for women 50 to 69 years old, and most women will continue to choose to have mammograms. In my practice, however, I plan to spend less time nagging women who are reluctant to get mammograms. I now feel more comfortable recommending screening consistent with the US Preventive Services Task Force guidelines from late 2009.
As for women 40 to 49 years old, I plan to continue following USPSTF guidelines. However, I will also continue to order screens for women in their 40s who are at increased risk of breast cancer due to family history or other reasons and for those who prefer to be screened despite awareness of the high rate of false-positive findings.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
2. Welch HG. Screening mammography—a long run for a short slide? N Engl J Med. 2010;363(13):1276-1278.
3. US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(10):716-726.
4. Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40–49 years: evaluation of the Swedish Mammography Screening in young women (SCRY) cohort [published online ahead of print September 29, 2010]. Cancer. doi:10.1002/cncr.25650.
In its 2009 assessment of the benefits of screening mammography among women 50 to 69 years old, the US Preventive Services Task Force (USPSTF) estimated that the modality reduces mortality from breast cancer by 14% to 32%. However, that estimate is based on studies conducted more than 20 years ago.1
In 1996, some parts of Norway began to offer screening mammography. By 2005, screening had become universally available in the country, with more than 75% of the eligible population participating. During that decade, Norway also established multidisciplinary teams to improve the management of women given a diagnosis of breast cancer.
To determine the effects of modern screening, investigators in Norway compared breast cancer mortality in four groups:
- women who lived, from 1996 through 2005, in counties in that country that offered mammography screening
- those who lived, from 1986 through 1995, in these same counties
- those who lived, from 1996 through 2005, in counties that did not offer screening
- those who lived, from 1986 through 1995, in these same counties.
The impact of the combination of mammography screening and multidisciplinary management of breast cancer cases was a 10% reduction in breast cancer mortality. Women who did not undergo mammography screening but whose cancers were treated according to the new paradigm experienced an 8% reduction in breast cancer mortality. That suggests that the reduction in mortality that can be attributed solely to screening mammography is a surprisingly low 2%. In other words, mammography may prevent as few as 2.4 deaths for every 100,000 person-years.
Although these numbers may appear to be strikingly low, the authors point out that they are consistent with those from Britain’s national screening program.
Can the low figures be good news?
Although some practitioners may view these data with confusion or even hostility, I see the findings of this study as good news: We have improved our treatment of breast cancer so dramatically over the past few decades that the benefits of early diagnosis have become attenuated. As an editorial accompanying the Norwegian study postulates, “It is quite plausible that screening mammography was more effective in the past than it is now. If women with new breast lumps now present earlier for evaluation, the benefit of screening will be less. If treatment of clinically detected breast cancer (i.e., tumors that are detected by means other than screening) has now improved, the benefit of screening will be less. Thus, the increased awareness about the importance of promptly seeking care for overt breast abnormalities (there is no debate about diagnostic mammography) and the widespread use of adjuvant therapy may have combined to make screening now less important.”2
What about women under 50?
Breast cancer is uncommon in women in their 40s, and screening mammograms are associated with a high rate of false-positive results and unnecessary additional imaging and biopsies in this age group. In late 2009, these observations led the USPSTF to recommend against routinely screening women 40 to 49 years old.3
Now, a study from Sweden provides data that contradict that position.4 In Sweden, a screening-mammography program was initiated for women 40 to 74 years old between 1986 and 1997. In 1987 and 1988, national guidelines were revised to allow counties that faced financial challenges to curtail screening for women younger than 50 years. At that time, about 50% of Swedish counties discontinued screening of younger women. The remaining counties continued screening women in their 40s at intervals ranging from 18 to 24 months.
From 1986 through 2005, 803 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were screened by mammography (7.3 million person-years). During the same period, 1,238 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were not screened by mammography (8.8 million person-years).
Investigators calculated the odds ratio (OR) for fatal breast cancer among women who were screened in their 40s: 0.71 (95% confidence interval [CI], 0.62–0.80). They also estimated that, over a 10-year period (roughly six screening mammograms), one case of fatal breast cancer was prevented among every 1,252 women screened.
Picture remains a bit murky
Coming less than a year after the aforementioned USPSTF recommendations against screening women under 50, and right on the heels of the Norwegian study minimizing the value of screening in women 50 to 69 years old, these new data have ignited controversy.
Unlike their Norwegian counterparts, Swedish investigators failed to report mortality rates, making interpretation of the data difficult. Nor did they detail the health costs of mammograms among women in their 40s.
Note: For more on the debate over screening mammography, see Dr. Kaunitz’s earlier commentary on the subject, “I’ve been rethinking my zeal for breast cancer screening,” in the December 2009 issue of OBG Management, and Dr. Robert L. Barbieri’s distinctive viewpoint, “Access to screening mammography: Priceless,” in the January 2010 issue at obgmanagement.com.
For the foreseeable future, most clinicians will continue to recommend regular screening for women 50 to 69 years old, and most women will continue to choose to have mammograms. In my practice, however, I plan to spend less time nagging women who are reluctant to get mammograms. I now feel more comfortable recommending screening consistent with the US Preventive Services Task Force guidelines from late 2009.
As for women 40 to 49 years old, I plan to continue following USPSTF guidelines. However, I will also continue to order screens for women in their 40s who are at increased risk of breast cancer due to family history or other reasons and for those who prefer to be screened despite awareness of the high rate of false-positive findings.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
In its 2009 assessment of the benefits of screening mammography among women 50 to 69 years old, the US Preventive Services Task Force (USPSTF) estimated that the modality reduces mortality from breast cancer by 14% to 32%. However, that estimate is based on studies conducted more than 20 years ago.1
In 1996, some parts of Norway began to offer screening mammography. By 2005, screening had become universally available in the country, with more than 75% of the eligible population participating. During that decade, Norway also established multidisciplinary teams to improve the management of women given a diagnosis of breast cancer.
To determine the effects of modern screening, investigators in Norway compared breast cancer mortality in four groups:
- women who lived, from 1996 through 2005, in counties in that country that offered mammography screening
- those who lived, from 1986 through 1995, in these same counties
- those who lived, from 1996 through 2005, in counties that did not offer screening
- those who lived, from 1986 through 1995, in these same counties.
The impact of the combination of mammography screening and multidisciplinary management of breast cancer cases was a 10% reduction in breast cancer mortality. Women who did not undergo mammography screening but whose cancers were treated according to the new paradigm experienced an 8% reduction in breast cancer mortality. That suggests that the reduction in mortality that can be attributed solely to screening mammography is a surprisingly low 2%. In other words, mammography may prevent as few as 2.4 deaths for every 100,000 person-years.
Although these numbers may appear to be strikingly low, the authors point out that they are consistent with those from Britain’s national screening program.
Can the low figures be good news?
Although some practitioners may view these data with confusion or even hostility, I see the findings of this study as good news: We have improved our treatment of breast cancer so dramatically over the past few decades that the benefits of early diagnosis have become attenuated. As an editorial accompanying the Norwegian study postulates, “It is quite plausible that screening mammography was more effective in the past than it is now. If women with new breast lumps now present earlier for evaluation, the benefit of screening will be less. If treatment of clinically detected breast cancer (i.e., tumors that are detected by means other than screening) has now improved, the benefit of screening will be less. Thus, the increased awareness about the importance of promptly seeking care for overt breast abnormalities (there is no debate about diagnostic mammography) and the widespread use of adjuvant therapy may have combined to make screening now less important.”2
What about women under 50?
Breast cancer is uncommon in women in their 40s, and screening mammograms are associated with a high rate of false-positive results and unnecessary additional imaging and biopsies in this age group. In late 2009, these observations led the USPSTF to recommend against routinely screening women 40 to 49 years old.3
Now, a study from Sweden provides data that contradict that position.4 In Sweden, a screening-mammography program was initiated for women 40 to 74 years old between 1986 and 1997. In 1987 and 1988, national guidelines were revised to allow counties that faced financial challenges to curtail screening for women younger than 50 years. At that time, about 50% of Swedish counties discontinued screening of younger women. The remaining counties continued screening women in their 40s at intervals ranging from 18 to 24 months.
From 1986 through 2005, 803 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were screened by mammography (7.3 million person-years). During the same period, 1,238 women died from breast cancer that was diagnosed when they were 40 to 49 years old and who were not screened by mammography (8.8 million person-years).
Investigators calculated the odds ratio (OR) for fatal breast cancer among women who were screened in their 40s: 0.71 (95% confidence interval [CI], 0.62–0.80). They also estimated that, over a 10-year period (roughly six screening mammograms), one case of fatal breast cancer was prevented among every 1,252 women screened.
Picture remains a bit murky
Coming less than a year after the aforementioned USPSTF recommendations against screening women under 50, and right on the heels of the Norwegian study minimizing the value of screening in women 50 to 69 years old, these new data have ignited controversy.
Unlike their Norwegian counterparts, Swedish investigators failed to report mortality rates, making interpretation of the data difficult. Nor did they detail the health costs of mammograms among women in their 40s.
Note: For more on the debate over screening mammography, see Dr. Kaunitz’s earlier commentary on the subject, “I’ve been rethinking my zeal for breast cancer screening,” in the December 2009 issue of OBG Management, and Dr. Robert L. Barbieri’s distinctive viewpoint, “Access to screening mammography: Priceless,” in the January 2010 issue at obgmanagement.com.
For the foreseeable future, most clinicians will continue to recommend regular screening for women 50 to 69 years old, and most women will continue to choose to have mammograms. In my practice, however, I plan to spend less time nagging women who are reluctant to get mammograms. I now feel more comfortable recommending screening consistent with the US Preventive Services Task Force guidelines from late 2009.
As for women 40 to 49 years old, I plan to continue following USPSTF guidelines. However, I will also continue to order screens for women in their 40s who are at increased risk of breast cancer due to family history or other reasons and for those who prefer to be screened despite awareness of the high rate of false-positive findings.
—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
2. Welch HG. Screening mammography—a long run for a short slide? N Engl J Med. 2010;363(13):1276-1278.
3. US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(10):716-726.
4. Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40–49 years: evaluation of the Swedish Mammography Screening in young women (SCRY) cohort [published online ahead of print September 29, 2010]. Cancer. doi:10.1002/cncr.25650.
1. Nelson HD, Tyne K, Naik A, et al. Screening for breast cancer: an update for the US Preventive Services Task Force. Ann Intern Med. 2009;151(10):727-737.
2. Welch HG. Screening mammography—a long run for a short slide? N Engl J Med. 2010;363(13):1276-1278.
3. US Preventive Services Task Force. Screening for breast cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2009;151(10):716-726.
4. Hellquist BN, Duffy SW, Abdsaleh S, et al. Effectiveness of population-based service screening with mammography for women ages 40–49 years: evaluation of the Swedish Mammography Screening in young women (SCRY) cohort [published online ahead of print September 29, 2010]. Cancer. doi:10.1002/cncr.25650.
An ObGyn’s guide to aromatase inhibitors as adjuvant therapy for breast CA
Think breast cancer survivors are unlikely to show up in your practice? You should think again.
At last official count, 2.5 million women in the United States had a history of breast cancer.1 Most of them are now free of malignancy, but others are still grappling with the disease in some form or fashion.2 All need continuing health care.
Roughly two thirds of women who have breast cancer have disease that is hormone-receptor–positive.2,3 Recently updated guidelines from the American Society of Clinical Oncology (ASCO) recommend that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI) (see a summary of these guidelines on page 36). That makes it likely that a good number of breast cancer survivors who visit your practice are taking one of these medications: anastrozole (Arimidex), letrozole (Femara), or exemestane (Aromasin). These drugs are antiestrogens, given to postmenopausal women to reduce the likelihood of disease recurrence and progression.
The antiestrogenic properties of these drugs are what make them lifesavers. But the same qualities can create a range of health issues, from increased risk of osteoporosis and fracture to vasomotor and joint symptoms. And although ObGyns are not the physicians who prescribe these drugs, you may be the provider one of these women consults about their side effects and related issues.
To find out the latest on the management of women who are taking one of these agents, we inserted ourselves into the busy schedule of Andrew M. Kaunitz, MD, who agreed to address some fundamental—and some not so basic—questions about the drugs. In this extended Q&A, Dr. Kaunitz touches on mechanism of action, benefits versus risks, common side effects, compliance with therapy, and the ill effects of early discontinuation.
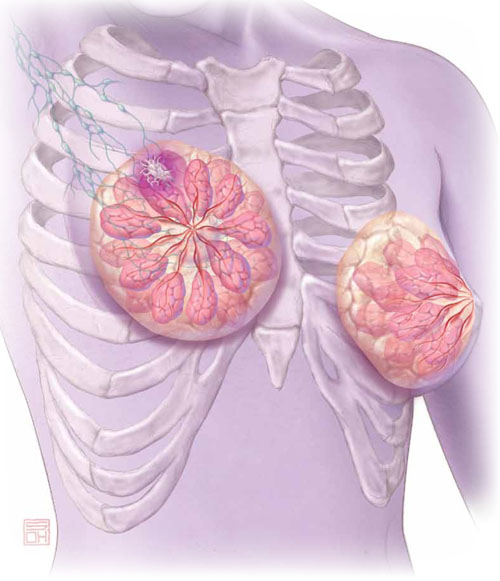
Aromatase inhibitors are better than tamoxifen at reducing the risk of breast cancer recurrence in postmenopausal women who have hormone-receptor–positive disease. But, they increase the risk of osteoporosis and fracture and often cause arthralgias and other complaints that ObGyn practitioners may be called upon to manage.
OBG Management: What is the overall aim of adjuvant endocrine therapy in the setting of breast cancer?
Dr. Kaunitz: Endocrine therapy—specifically, use of an AI—prevents the stimulation of breast cancer cells by endogenous estrogen. In other words, aromatase inhibitors suppress the growth of cancer cells that have estrogen receptors. These drugs also inhibit aromatase near any breast tumor and reduce estrogen levels in breast tissue.
OBG Management: What is the mechanism of action of adjuvant endocrine therapy?
Dr. Kaunitz: In postmenopausal women, androgens are converted to estrogens via the aromatase enzyme, which is present in adipose tissue and other sites. By blocking this enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
OBG Management: How does that differ from the mechanism of action of tamoxifen, another drug used in breast cancer patients?
Dr. Kaunitz: Tamoxifen is a selective estrogen receptor modulator (SERM). It blocks estrogen in breast tissue selectively, by competitively binding to estrogen receptors.5 However, tamoxifen has estrogenic effects in the uterus, bone, and liver, as well as other tissues.
The efficacy of AIs in preventing breast cancer recurrence in the first 2 years after breast cancer surgery is higher than that of tamoxifen. And unlike tamoxifen, the AIs do not increase the risk of venous thromboembolism or cause endometrial disease.
OBG Management: What effects do aromatase inhibitors have in premenopausal women?
Dr. Kaunitz: These agents are not recommended for use in premenopausal women because, in that population, the lion’s share of estrogen production takes place in the ovary rather than in adipose tissue and muscle. If you were to administer an AI to a premenopausal woman, the reduced hypothalamic and pituitary estrogen feedback could lead to ovarian stimulation—which could increase ovarian steroid production.
OBG Management: What about women who become amenorrheic as a result of chemotherapy or other cancer treatment? Do most oncologists assume that they are postmenopausal and prescribe an aromatase inhibitor?
Dr. Kaunitz: Clinicians should not assume that chemotherapy-induced amenorrhea signals permanent cessation of ovarian function. It is common for ovarian function to return in this setting. Accordingly, follicle-stimulating hormone (FSH) and estradiol levels should be assessed before an AI is considered as adjuvant therapy. Some investigators have suggested that the use of an AI in women who have chemotherapy-induced amenorrhea may actually increase the likelihood that ovarian function will return.6
OBG Management: Do all AIs produce the same effects?
Dr. Kaunitz: The AIs used in women with breast cancer are third-generation drugs. These AIs are classified as steroidal (type 1; exemestane) or nonsteroidal (type 2; anastrozole, letrozole). Exemestane, a steroid derived from androstenedione, inhibits the aromatase enzyme irreversibly. The nonsteroidal AIs are reversible.
Although all three AIs have numerous similarities, there are other distinctions between them in pharmacokinetics, mechanism of action, and toxicity—so they are not completely interchangeable.7 However, from our perspective as ObGyns caring for breast cancer survivors, we can assume that all three AIs will have similar effects on skeletal health and produce similar side effects in postmenopausal women.
- The American Society of Clinical Oncology recommends that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI).
- AIs are not recommended for use in premenopausal women.
- By blocking the aromatase enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
- AIs are more effective than tamoxifen at preventing recurrence in the first 2 years after breast cancer surgery. Postmenopausal women taking an AI have a longer disease-free survival and time to recurrence than do women taking tamoxifen. They also have a lower incidence of contralateral breast cancer.
- The most prominent side effects of AI therapy include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD). However, endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.
- The FDA strongly discourages the use of estrogen therapy—systemic or local—in women who are taking an AI. Accordingly, bisphospho-nate therapy is recommended as first-line treatment of low bone mineral density. Vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy. And gabapentin, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors are the mainstay of therapy for vasomotor flushes.
- Roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32 Early discontinuation is associated with an increase in mortality.33
How much do we know about these drugs?
OBG Management: How long does a woman typically take an AI?
Dr. Kaunitz: At present, in women treated for early-stage, hormone-positive breast cancer, the optimal duration of treatment is unknown. Most oncologists prescribe an AI for 5 years, the length of treatment in a prominent trial of the drugs.8
OBG Management: Is that duration likely to increase as more data come in?
Dr. Kaunitz: The optimal duration of adjuvant AI therapy will be determined by the findings of long-term clinical trials. The National Surgical Adjuvant Breast and Bowel Project B-42 trial may provide new insights into optimal duration of AI treatment after initial tamoxifen therapy.9
OBG Management: How thoroughly have AIs been studied in regard to their use in breast cancer survivors and women who have early-stage disease? How would you characterize the quantity and quality of data that we have so far?
Dr. Kaunitz: AIs have been extensively studied. The most important clinical trials of AIs in this setting, including the Anastrozole, Tamoxifen Alone or in Combination (ATAC) trial (over 6,000 participants, median follow-up of 100 months) and the Breast International Group (BIG) trial (almost 5,000 participants, median follow-up of 76 months) have been detailed in the recent ASCO report.10 These two large landmark trials, in particular, formed the basis for ASCO’s recommendations to routinely incorporate AIs into the therapy of postmenopausal women who have hormone-receptor–positive breast cancer.
OBG Management: In treating breast cancer, what other applications are AIs used for?
Dr. Kaunitz: AIs appear to be slightly more effective than tamoxifen in treating postmenopausal women who have metastatic breast cancer.11
They are approved as first-line therapy for breast cancer in:
- postmenopausal women who have hormone-receptor–positive disease
- postmenopausal women who have locally advanced disease when the hormone receptor is unknown
- postmenopausal women who have metastatic disease.
In addition, they are approved as second-line treatment of advanced breast cancer in postmenopausal women who have disease progression following tamoxifen therapy.12
How effective is AI therapy?
OBG Management: What do we know about the efficacy of these drugs?
Dr. Kaunitz: Most of the studies that have explored efficacy compare an AI with tamoxifen rather than with placebo. In the ATAC trial, after a median follow-up of 33 months, women who were taking anastrozole for early-stage breast cancer had longer disease-free survival and time to recurrence and a lower incidence of contralateral breast cancer than did women taking tamoxifen.8
After 4 years of follow-up in the ATAC trial, women taking anastrozole continued to have more favorable disease-free survival (86.9% vs 84.5% for anastrozole and tamoxifen, respectively; hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.76–0.99; P =.03).13 They also had a more favorable time to recurrence than did women taking tamoxifen (HR, 0.83; 95% CI, 0.71–0.96; P =.015). And women taking anastrozole had a lower incidence of contralateral breast cancer, as well, although this different did not achieve statistical significance (HR, 0.62; 95% CI, 0.38–1.02; P =.062).13
In the BIG study, women taking letrozole had a 5-year disease-free survival estimate of 84.0%, compared with 81.4% for women taking tamoxifen.14 In addition, women taking letrozole were significantly less likely than those taking tamoxifen to experience an event that ended a period of disease-free survival (HR, 0.81; 95% CI, 0.70–0.93; P =.003), especially the event of distant recurrence (HR, 0.73; 95% CI, 0.60–0.88; P =.001).14
And a phase-3 study of exemestane versus tamoxifen in women who had metastatic breast cancer found that the AI produced a superior response rate (46% vs 31% for exemestane and tamoxifen, respectively; odds ratio [OR], 1.85; 95% CI, 1.21–2.82; P =.005). In addition, median progression-free survival was greater with exemestane (9.9 months; 95% CI, 8.7–11.8 months) than with tamoxifen (5.8 months; 95% CI, 5.3–8.1 months). However, there was no difference between arms in progression-free survival or overall survival.
Postmenopausal women who have hormone-receptor–positive breast cancer should consider taking an aromatase inhibitor (AI) to lengthen disease-free survival and lower the risk of recurrence. That’s one of the recommendations in updated guidelines issued earlier this year by the American Society of Clinical Oncology (ASCO). The guidelines suggest a duration of AI therapy of 5 years. In the event that a woman discontinues AI therapy before 5 years are up, she should consider using tamoxifen to bring the total duration of treatment to 5 years.
Other recommendations in the guidelines include:
- Women who have taken tamoxifen for 5 years stand to benefit from switching to an AI for as long as 5 additional years.
- When advising a woman about adjuvant therapy with an AI, clinicians should consider the potential adverse effects, which include osteoporosis, fracture, and arthralgias.
- The third-generation AIs on the market today have not been found to have clinically important differences between them. A woman who cannot tolerate a particular AI should consider switching to a different AI.
- Switching from an AI to tamoxifen (or vice versa) may be an appropriate option for patients who cannot tolerate a drug’s adverse effects. In the event of a switch to tamoxifen, the clinician should counsel the patient about its adverse effects, which include venous thromboembolism and endometrial polyps, hyperplasia, and cancer.
The full guidelines can be accessed at http://jco.ascopubs.org/content/early/2010/07/12/JCO.2009.26.3756.full.pdf.
—Andrew M. Kaunitz, MD
How well tolerated are AIs?
OBG Management: What adverse effects are associated with AIs?
Dr. Kaunitz: Although AIs, overall, are safe medications, their use is associated with a number of adverse events. The most prominent side effects include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD).
However, the drugs are generally perceived as being easier to tolerate than tamoxifen. That’s because endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.8,13
For overweight women, who face an elevated baseline risk of thromboembolism, the availability of AIs represents a major advantage over tamoxifen. Similarly, AIs offer advantages over tamoxifen for women who have an intact uterus. In addition, postmenopausal women who are taking a selective serotonin reuptake inhibitor (SSRI) such as paroxetine should take an AI rather than tamoxifen, because the concomitant use of SSRIs attenuates the efficacy of tamoxifen.15
What can be done about the most prominent risks?
OBG Management: Let’s focus on what’s probably the best-known adverse effect of AIs—the heightened risk of osteoporosis and fracture. How significant is this effect?
Dr. Kaunitz: Because use of an AI is associated with a profound reduction in endogenous estrogen levels, it also decreases BMD and can lead to osteoporotic fractures. All major phase-3 trials of adjuvant use of AIs in women who have early breast cancer found an increased risk of fracture, with no significant differences between AIs.16
Fortunately, bisphosphonate therapy (oral or intravenous) has been found to reduce bone loss associated with AI therapy.17,18
Assessing baseline BMD is important as women initiate AI therapy. Although no consensus exists regarding follow-up BMD assessment in the setting of AI use, an interval of 2 years is prudent, with the follow-up study preferably performed at the same imaging center and by the same technician as the first. If baseline osteoporosis is observed at the lumbar spine or hip, bisphosphonate therapy is appropriate. If a woman taking an AI has low bone mass (osteopenia) but not osteoporosis, bisphosphonate therapy should be considered if any of the following risk factors are present:
- advanced age
- history of fracture
- glucocorticoid therapy
- parental history of hip fracture
- low body weight
- current smoking status
- excess alcohol consumption
- rheumatoid arthritis
- known risk factors for secondary osteoporosis.19
In breast cancer survivors initiating or continuing AI therapy, it is also appropriate to check a serum vitamin D level and ensure that intake of this nutrient is adequate.
Bisphosphonates may offer oncologic benefits, as well; preliminary evidence suggests that the drugs may prevent recurrence of the cancer and prolong survival.20
OBG Management: What can an ObGyn offer to a woman who complains of significant AI-related arthralgia?
Dr. Kaunitz: Bone and joint symptoms, including aches, pain, and stiffness that is bilateral and not associated with other evidence of rheumatologic disorders, are among the most common side effects of AI therapy. On the plus side of the equation, these symptoms are more likely to be mild to moderate than severe. On the negative side, no specific treatment has been found to be effective in relieving these symptoms, which usually resolve within 2 months or so after discontinuing AI therapy.10
OBG Management: Do AIs have a negative impact on cardiovascular health?
Dr. Kaunitz: Unlike tamoxifen, AIs do not increase the risk of thromboembolic disease. Although the use of an AI may modestly increase the risk of ischemic cardiovascular disease (and lipid changes), compared with tamoxifen, AIs do not appear to increase cardiovascular risk compared with placebo.21,22
OBG Management: Do the antiestrogenic effects of AIs have a significant impact on vaginal health and sexual desire?
Dr. Kaunitz: A review of published reports did not find that the use of AIs has a predictable impact on vaginal dryness or sexual desire.10 However, symptomatic genital atrophy is common in postmenopausal breast cancer survivors, whether or not they use adjuvant therapy.
Although the FDA considers the use of any estrogen (systemic or vaginal) following a diagnosis of breast cancer to be contraindicated, some breast cancer survivors who have symptomatic genital atrophy express an interest in the use of vaginal estrogen. Use of 25-μg estradiol tablets (Vagifem) is associated with a short-term increase in serum estradiol levels.23 This finding has reinforced caution among medical oncologists about the safety of vaginal estrogen in breast cancer survivors. (The 25-μg tablets are no longer marketed.) The lowest dosage of vaginal estrogen available for the treatment of genital atrophy is found in 10-μg estradiol tablets (Vagifem) and the estradiol (2-mg) 3-month vaginal ring (Estring). Nonetheless, in the absence of data, oncologists will likely continue to be concerned that even the lowest dosage of vaginal estrogen could attenuate the favorable impact of AIs on breast cancer. Accordingly, use of vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy.
OBG Management: What about the ubiquitous hot flush? Vasomotor symptoms may be more common in women who take tamoxifen, but women on AIs are also bothered by flushes. What are the alternatives to estrogen therapy?
Dr. Kaunitz: Both nonprescription and prescription alternatives are available. Nonprescription options include soy extract and red clover isoflavones, black cohosh, and Chinese herbs. However, none of these over-the-counter approaches has been found to be more effective than placebo in the treatment of menopausal hot flushes.24-26
As for prescription nonhormonal options, ObGyns should recognize that all such treatments are off-label and that none attain the efficacy of hormone therapy in the treatment of vasomotor symptoms. The best-studied and most effective medications include gabapentin, SSRIs (especially paroxetine), and serotonin-norepinephrine reuptake inhibitors (venlafaxine and desvenlafaxine).24,27
OBG Management: Is there any evidence that AIs impair cognitive function in postmenopausal women?
Dr. Kaunitz: Because estrogen is important for cognition, one might anticipate that the profound reduction in background estrogen associated with AI use would impair cognition. Fortunately, the evidence to date is reassuring. Substudies of the BIG trial and the Tamoxifen and Exemestane Adjuvant Multinational Trial indicate that, compared with tamoxifen (which is associated with declines in cognitive function in postmenopausal women), letrozole and exemestane do not diminish cognitive function.28,29
OBG Management: Overall, what is the typical impact of an AI on a woman’s quality of life?
Dr. Kaunitz: Most women do very well on an AI, finding it easier to tolerate than tamoxifen, as we have discussed. However, a significant minority of women is seriously bothered by the adverse effects, with arthralgias usually leading the pack of complaints.30,31
OBG Management: Do some women discontinue adjuvant endocrine therapy because of adverse effects?
Dr. Kaunitz: Regrettably, the answer is “Yes.” A recent study from Kaiser Permanente of northern California found that roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32
OBG Management: What can an ObGyn do to encourage compliance with and completion of AI therapy?
Dr. Kaunitz: First, it is critical that patients understand that AIs are lifesaving drugs. As a recent paper points out, early discontinuation or noncompliance with AI therapy is associated with higher mortality.33
Clinicians should also help breast cancer patients understand what common side effects to anticipate with these medications.
Finally, clinicians who understand the financial toll a breast cancer diagnosis and treatment can take are better positioned to help women overcome challenges that may interfere with long-term compliance with AI therapy.
OBG Management: Do you expect the use of AIs in breast cancer survivors to become more commonplace?
Dr. Kaunitz: Given how common breast cancer is, and given the new ASCO guidelines and the extensive literature upon which they are based, ObGyns will be seeing more women using AIs. Although we are not the physicians who prescribe AIs, we need to remain up to date on their benefits and side effects. This important class of drugs is positioned to improve outcomes for postmenopausal women with breast cancer.
- Do certain SSRIs reduce the benefits of tamoxifen in breast cancer survivors?
Examining the Evidence
Andrew M. Kaunitz, MD - Does the clinical breast exam boost the sensitivity of mammography?
Examining the Evidence
Jennifer Griffin, MD, and Mark Pearlman, MD - A guide to lotions and potions for treating vaginal atrophy
Danielle D. Marshall, MD, and Cheryl Iglesia, MD
We want to hear from you! Tell us what you think.
1. Horner MJ, Ries LAG, Krapcho M, et al. eds. SEER Cancer Statistics Review, 1975–2006. Bethesda, Md: National Cancer Institute; 2009.http://seer.cancer.gov/csr/1975_2006. Accessed August 18, 2010.
2. American Cancer Society. Breast cancer facts and figures, 2009–2010. Atlanta, Ga: American Cancer Society; 2010. http://www.cancer.org/Research/CancerFactsFigures/BreastCancerFactsFigures/breast-cancer-facts—figures-2009-2010. Accessed August 18, 2010.
3. Li CI, Daling JR, Malone KE. Incidence of invasive breast cancer by hormone receptor status from 1992 to 1998. J Clin Oncol. 2003;21(1):28-34.
4. Miller WR. Aromatase inhibitors: mechanism of action and role in the treatment of breast cancer. Semin Oncol. 2003;30(4 suppl 14):3-11.
5. Peng J, Sengupta S, Jordan VC. Potential of selective estrogen receptor modulators as treatments and preventives of breast cancer. Anticancer Agents Med Chem. 2009;9(5):481-499.
6. Smith IE, Dowsett M, Yap YS, et al. Adjuvant aromatase inhibitors for early breast cancer after chemotherapy-induced amenorrhea: caution and suggested guidelines. J Clin Oncol. 2006;24(16):2444-2447.
7. Nabholtz JM, Mouret-Reynier MA, Durando X, et al. Comparative review of anastrozole, letrozole and exemestane in the management of early breast cancer. Expert Opin Pharmacother. 2009;10(9):1435-1447.
8. Baum M, Budzar AU, Cuzick J, et al. ATAC Trialists’ Group. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomized trial. Lancet. 2002;359(9324):2131-2139.
9. Letrozole in treating postmenopausal women who have received hormone therapy for hormone receptor-positive breast cancer. National Cancer Institute Web site.http://www.cancer.gov/clinicaltrials/NSABP-B-42. Published August 16, 2010. Accessed August 18, 2010.
10. Burstein HJ, Prestrud AA, Seidenfeld J, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone-receptor–positive breast cancer. J Clin Oncol. 2010;28(23):3784-3796.
11. Mauri D, Pavlidis N, Polyzos NP, Ioanidis JP. Survival with aromatase inhibitors and inactivators versus standard hormonal therapy in advanced breast cancer: meta-analysis. J Natl Cancer Inst. 2006;98(18):1285-1291.
12. Arimidex [package insert]. AstraZeneca; 2009.
13. Baum M, Buzdar A, Cuzick J, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Taxoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer. 2003;98(9):1802-1810.
14. Thurlimann B, Keshaviah A, Coates AS, et al. Breast International Group (BIG) 1-98 Collaborative Group. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353(26):2747-2757.
15. Kelly CM, Juurlink DM, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population-based cohort study. 2010;340:c693.-doi: 10.1136/bmj.c693.
16. Geisler J, Lonning PE. Impact of aromatase inhibitors on bone health in breast cancer patients. J Steroid Biochem Mol Biol. 2010;118(4–5):294-299.
17. Van Poznak C, Hannon RA, Mackey JR, et al. Prevention of aromatase inhibitor-induced bone loss using risedronate: the SABRE trial. J Clin Oncol. 2010;28(6):967-975.
18. Brufsky AM, Bosserman LD, Caradonna RR, et al. Zoledronic acid effectively prevents aromatase-inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole. Z-FAST study 36-month follow-up results. Clin Breast Cancer. 2009;9(2):77-85.
19. Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporosis Int. 2005;16(6):581-589.
20. Reeder JG, Brufsky AM. The role of bisphosphonates in the adjuvant setting for breast cancer. Oncology. 2010;24(6):462-467,475.
21. Nabholtz JM. Long-term safety of aromatase inhibitors in the treatment of breast cancer. Ther Clin Risk Manag. 2008;4(1):189-204.
22. Cuppone F, Bria E, Verma S, et al. Do adjuvant aromatase inhibitors increase the cardiovascular risk in postmenopausal women with early breast cancer? Meta-analysis of randomized trials. Cancer. 2008;112(2):260-267.
23. Kendall A, Dowsett M, Folkerd E, Smith I. Caution: Vaginal estradiol appears to be contraindicated in postmenopausal women on adjuvant aromatase inhibitors. Ann Oncol. 2006;17(4):584-587.
24. Nelson HD. Menopause. Lancet. 2008;371(9614):760-770.
25. Geller SE, Shulman LP, van Breemen RB, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Menopause. 2009;16(6):1156-1166.
26. Kaunitz AM. Effective herbal treatment of vasomotor symptoms—are we any closer? Menopause. 2009;16(3):428-429.
27. Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S. Study 319 Investigators. Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, randomized, placebo-controlled trial of efficacy and safety. Am J Obstet Gynecol. 2009;200(3):238.e1-e10.
28. Phillips KA, Ribi K, Sun Z, et al. Cognitive function in postmenopausal women receiving adjuvant letrozole or tamoxifen for breast cancer in the BIG 1-98 randomized trial [published online ahead of print April 10, 2010]. Breast. doi:10.1016/j.breast.2010.03.025.
29. Schilder CM, Seynaeve C, Beex LV, et al. Effects of tamoxifen and exemestane on cognitive functioning of postmenopausal patients with breast cancer: results from the neuropsychological side study of the Tamoxifen and Exemestane Adjuvant Multinational Trial. J Clin Oncol. 2010;28(8):1294-1300.
30. Din OS, Dodwell D, Wakefield RJ, Coleman RE. Aromatase inhibitor-induced arthralgia in early breast cancer: what do we know and how can we find out more? Breast Cancer Res Treat. 2010;120(3):525-538.
31. Burstein HJ. Aromatase inhibitor-associated arthralgia syndrome. Breast. 2007;16(3):223-234.
32. Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients [published online ahead of print June 28, 2010]. J Clin Oncol. doi: 10.1200/JCO.2009.25.9655.
33. Hershman DL, Shao T, Kushi LH, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer [published online ahead of print August 28, 2010]. Breast Cancer Res Treat. doi: 10.1007/ s10549-010-1132-4.
Think breast cancer survivors are unlikely to show up in your practice? You should think again.
At last official count, 2.5 million women in the United States had a history of breast cancer.1 Most of them are now free of malignancy, but others are still grappling with the disease in some form or fashion.2 All need continuing health care.
Roughly two thirds of women who have breast cancer have disease that is hormone-receptor–positive.2,3 Recently updated guidelines from the American Society of Clinical Oncology (ASCO) recommend that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI) (see a summary of these guidelines on page 36). That makes it likely that a good number of breast cancer survivors who visit your practice are taking one of these medications: anastrozole (Arimidex), letrozole (Femara), or exemestane (Aromasin). These drugs are antiestrogens, given to postmenopausal women to reduce the likelihood of disease recurrence and progression.
The antiestrogenic properties of these drugs are what make them lifesavers. But the same qualities can create a range of health issues, from increased risk of osteoporosis and fracture to vasomotor and joint symptoms. And although ObGyns are not the physicians who prescribe these drugs, you may be the provider one of these women consults about their side effects and related issues.
To find out the latest on the management of women who are taking one of these agents, we inserted ourselves into the busy schedule of Andrew M. Kaunitz, MD, who agreed to address some fundamental—and some not so basic—questions about the drugs. In this extended Q&A, Dr. Kaunitz touches on mechanism of action, benefits versus risks, common side effects, compliance with therapy, and the ill effects of early discontinuation.
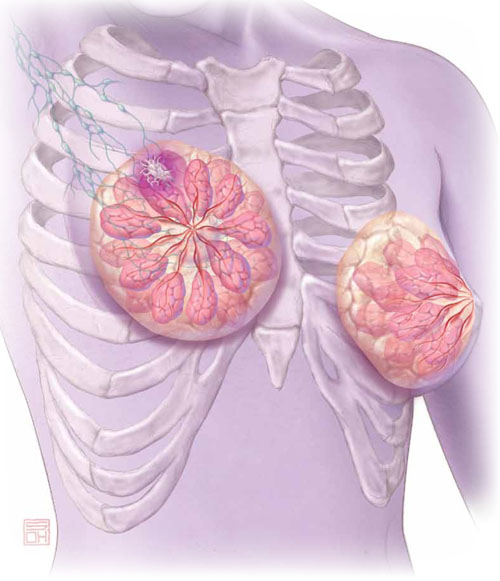
Aromatase inhibitors are better than tamoxifen at reducing the risk of breast cancer recurrence in postmenopausal women who have hormone-receptor–positive disease. But, they increase the risk of osteoporosis and fracture and often cause arthralgias and other complaints that ObGyn practitioners may be called upon to manage.
OBG Management: What is the overall aim of adjuvant endocrine therapy in the setting of breast cancer?
Dr. Kaunitz: Endocrine therapy—specifically, use of an AI—prevents the stimulation of breast cancer cells by endogenous estrogen. In other words, aromatase inhibitors suppress the growth of cancer cells that have estrogen receptors. These drugs also inhibit aromatase near any breast tumor and reduce estrogen levels in breast tissue.
OBG Management: What is the mechanism of action of adjuvant endocrine therapy?
Dr. Kaunitz: In postmenopausal women, androgens are converted to estrogens via the aromatase enzyme, which is present in adipose tissue and other sites. By blocking this enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
OBG Management: How does that differ from the mechanism of action of tamoxifen, another drug used in breast cancer patients?
Dr. Kaunitz: Tamoxifen is a selective estrogen receptor modulator (SERM). It blocks estrogen in breast tissue selectively, by competitively binding to estrogen receptors.5 However, tamoxifen has estrogenic effects in the uterus, bone, and liver, as well as other tissues.
The efficacy of AIs in preventing breast cancer recurrence in the first 2 years after breast cancer surgery is higher than that of tamoxifen. And unlike tamoxifen, the AIs do not increase the risk of venous thromboembolism or cause endometrial disease.
OBG Management: What effects do aromatase inhibitors have in premenopausal women?
Dr. Kaunitz: These agents are not recommended for use in premenopausal women because, in that population, the lion’s share of estrogen production takes place in the ovary rather than in adipose tissue and muscle. If you were to administer an AI to a premenopausal woman, the reduced hypothalamic and pituitary estrogen feedback could lead to ovarian stimulation—which could increase ovarian steroid production.
OBG Management: What about women who become amenorrheic as a result of chemotherapy or other cancer treatment? Do most oncologists assume that they are postmenopausal and prescribe an aromatase inhibitor?
Dr. Kaunitz: Clinicians should not assume that chemotherapy-induced amenorrhea signals permanent cessation of ovarian function. It is common for ovarian function to return in this setting. Accordingly, follicle-stimulating hormone (FSH) and estradiol levels should be assessed before an AI is considered as adjuvant therapy. Some investigators have suggested that the use of an AI in women who have chemotherapy-induced amenorrhea may actually increase the likelihood that ovarian function will return.6
OBG Management: Do all AIs produce the same effects?
Dr. Kaunitz: The AIs used in women with breast cancer are third-generation drugs. These AIs are classified as steroidal (type 1; exemestane) or nonsteroidal (type 2; anastrozole, letrozole). Exemestane, a steroid derived from androstenedione, inhibits the aromatase enzyme irreversibly. The nonsteroidal AIs are reversible.
Although all three AIs have numerous similarities, there are other distinctions between them in pharmacokinetics, mechanism of action, and toxicity—so they are not completely interchangeable.7 However, from our perspective as ObGyns caring for breast cancer survivors, we can assume that all three AIs will have similar effects on skeletal health and produce similar side effects in postmenopausal women.
- The American Society of Clinical Oncology recommends that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI).
- AIs are not recommended for use in premenopausal women.
- By blocking the aromatase enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
- AIs are more effective than tamoxifen at preventing recurrence in the first 2 years after breast cancer surgery. Postmenopausal women taking an AI have a longer disease-free survival and time to recurrence than do women taking tamoxifen. They also have a lower incidence of contralateral breast cancer.
- The most prominent side effects of AI therapy include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD). However, endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.
- The FDA strongly discourages the use of estrogen therapy—systemic or local—in women who are taking an AI. Accordingly, bisphospho-nate therapy is recommended as first-line treatment of low bone mineral density. Vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy. And gabapentin, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors are the mainstay of therapy for vasomotor flushes.
- Roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32 Early discontinuation is associated with an increase in mortality.33
How much do we know about these drugs?
OBG Management: How long does a woman typically take an AI?
Dr. Kaunitz: At present, in women treated for early-stage, hormone-positive breast cancer, the optimal duration of treatment is unknown. Most oncologists prescribe an AI for 5 years, the length of treatment in a prominent trial of the drugs.8
OBG Management: Is that duration likely to increase as more data come in?
Dr. Kaunitz: The optimal duration of adjuvant AI therapy will be determined by the findings of long-term clinical trials. The National Surgical Adjuvant Breast and Bowel Project B-42 trial may provide new insights into optimal duration of AI treatment after initial tamoxifen therapy.9
OBG Management: How thoroughly have AIs been studied in regard to their use in breast cancer survivors and women who have early-stage disease? How would you characterize the quantity and quality of data that we have so far?
Dr. Kaunitz: AIs have been extensively studied. The most important clinical trials of AIs in this setting, including the Anastrozole, Tamoxifen Alone or in Combination (ATAC) trial (over 6,000 participants, median follow-up of 100 months) and the Breast International Group (BIG) trial (almost 5,000 participants, median follow-up of 76 months) have been detailed in the recent ASCO report.10 These two large landmark trials, in particular, formed the basis for ASCO’s recommendations to routinely incorporate AIs into the therapy of postmenopausal women who have hormone-receptor–positive breast cancer.
OBG Management: In treating breast cancer, what other applications are AIs used for?
Dr. Kaunitz: AIs appear to be slightly more effective than tamoxifen in treating postmenopausal women who have metastatic breast cancer.11
They are approved as first-line therapy for breast cancer in:
- postmenopausal women who have hormone-receptor–positive disease
- postmenopausal women who have locally advanced disease when the hormone receptor is unknown
- postmenopausal women who have metastatic disease.
In addition, they are approved as second-line treatment of advanced breast cancer in postmenopausal women who have disease progression following tamoxifen therapy.12
How effective is AI therapy?
OBG Management: What do we know about the efficacy of these drugs?
Dr. Kaunitz: Most of the studies that have explored efficacy compare an AI with tamoxifen rather than with placebo. In the ATAC trial, after a median follow-up of 33 months, women who were taking anastrozole for early-stage breast cancer had longer disease-free survival and time to recurrence and a lower incidence of contralateral breast cancer than did women taking tamoxifen.8
After 4 years of follow-up in the ATAC trial, women taking anastrozole continued to have more favorable disease-free survival (86.9% vs 84.5% for anastrozole and tamoxifen, respectively; hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.76–0.99; P =.03).13 They also had a more favorable time to recurrence than did women taking tamoxifen (HR, 0.83; 95% CI, 0.71–0.96; P =.015). And women taking anastrozole had a lower incidence of contralateral breast cancer, as well, although this different did not achieve statistical significance (HR, 0.62; 95% CI, 0.38–1.02; P =.062).13
In the BIG study, women taking letrozole had a 5-year disease-free survival estimate of 84.0%, compared with 81.4% for women taking tamoxifen.14 In addition, women taking letrozole were significantly less likely than those taking tamoxifen to experience an event that ended a period of disease-free survival (HR, 0.81; 95% CI, 0.70–0.93; P =.003), especially the event of distant recurrence (HR, 0.73; 95% CI, 0.60–0.88; P =.001).14
And a phase-3 study of exemestane versus tamoxifen in women who had metastatic breast cancer found that the AI produced a superior response rate (46% vs 31% for exemestane and tamoxifen, respectively; odds ratio [OR], 1.85; 95% CI, 1.21–2.82; P =.005). In addition, median progression-free survival was greater with exemestane (9.9 months; 95% CI, 8.7–11.8 months) than with tamoxifen (5.8 months; 95% CI, 5.3–8.1 months). However, there was no difference between arms in progression-free survival or overall survival.
Postmenopausal women who have hormone-receptor–positive breast cancer should consider taking an aromatase inhibitor (AI) to lengthen disease-free survival and lower the risk of recurrence. That’s one of the recommendations in updated guidelines issued earlier this year by the American Society of Clinical Oncology (ASCO). The guidelines suggest a duration of AI therapy of 5 years. In the event that a woman discontinues AI therapy before 5 years are up, she should consider using tamoxifen to bring the total duration of treatment to 5 years.
Other recommendations in the guidelines include:
- Women who have taken tamoxifen for 5 years stand to benefit from switching to an AI for as long as 5 additional years.
- When advising a woman about adjuvant therapy with an AI, clinicians should consider the potential adverse effects, which include osteoporosis, fracture, and arthralgias.
- The third-generation AIs on the market today have not been found to have clinically important differences between them. A woman who cannot tolerate a particular AI should consider switching to a different AI.
- Switching from an AI to tamoxifen (or vice versa) may be an appropriate option for patients who cannot tolerate a drug’s adverse effects. In the event of a switch to tamoxifen, the clinician should counsel the patient about its adverse effects, which include venous thromboembolism and endometrial polyps, hyperplasia, and cancer.
The full guidelines can be accessed at http://jco.ascopubs.org/content/early/2010/07/12/JCO.2009.26.3756.full.pdf.
—Andrew M. Kaunitz, MD
How well tolerated are AIs?
OBG Management: What adverse effects are associated with AIs?
Dr. Kaunitz: Although AIs, overall, are safe medications, their use is associated with a number of adverse events. The most prominent side effects include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD).
However, the drugs are generally perceived as being easier to tolerate than tamoxifen. That’s because endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.8,13
For overweight women, who face an elevated baseline risk of thromboembolism, the availability of AIs represents a major advantage over tamoxifen. Similarly, AIs offer advantages over tamoxifen for women who have an intact uterus. In addition, postmenopausal women who are taking a selective serotonin reuptake inhibitor (SSRI) such as paroxetine should take an AI rather than tamoxifen, because the concomitant use of SSRIs attenuates the efficacy of tamoxifen.15
What can be done about the most prominent risks?
OBG Management: Let’s focus on what’s probably the best-known adverse effect of AIs—the heightened risk of osteoporosis and fracture. How significant is this effect?
Dr. Kaunitz: Because use of an AI is associated with a profound reduction in endogenous estrogen levels, it also decreases BMD and can lead to osteoporotic fractures. All major phase-3 trials of adjuvant use of AIs in women who have early breast cancer found an increased risk of fracture, with no significant differences between AIs.16
Fortunately, bisphosphonate therapy (oral or intravenous) has been found to reduce bone loss associated with AI therapy.17,18
Assessing baseline BMD is important as women initiate AI therapy. Although no consensus exists regarding follow-up BMD assessment in the setting of AI use, an interval of 2 years is prudent, with the follow-up study preferably performed at the same imaging center and by the same technician as the first. If baseline osteoporosis is observed at the lumbar spine or hip, bisphosphonate therapy is appropriate. If a woman taking an AI has low bone mass (osteopenia) but not osteoporosis, bisphosphonate therapy should be considered if any of the following risk factors are present:
- advanced age
- history of fracture
- glucocorticoid therapy
- parental history of hip fracture
- low body weight
- current smoking status
- excess alcohol consumption
- rheumatoid arthritis
- known risk factors for secondary osteoporosis.19
In breast cancer survivors initiating or continuing AI therapy, it is also appropriate to check a serum vitamin D level and ensure that intake of this nutrient is adequate.
Bisphosphonates may offer oncologic benefits, as well; preliminary evidence suggests that the drugs may prevent recurrence of the cancer and prolong survival.20
OBG Management: What can an ObGyn offer to a woman who complains of significant AI-related arthralgia?
Dr. Kaunitz: Bone and joint symptoms, including aches, pain, and stiffness that is bilateral and not associated with other evidence of rheumatologic disorders, are among the most common side effects of AI therapy. On the plus side of the equation, these symptoms are more likely to be mild to moderate than severe. On the negative side, no specific treatment has been found to be effective in relieving these symptoms, which usually resolve within 2 months or so after discontinuing AI therapy.10
OBG Management: Do AIs have a negative impact on cardiovascular health?
Dr. Kaunitz: Unlike tamoxifen, AIs do not increase the risk of thromboembolic disease. Although the use of an AI may modestly increase the risk of ischemic cardiovascular disease (and lipid changes), compared with tamoxifen, AIs do not appear to increase cardiovascular risk compared with placebo.21,22
OBG Management: Do the antiestrogenic effects of AIs have a significant impact on vaginal health and sexual desire?
Dr. Kaunitz: A review of published reports did not find that the use of AIs has a predictable impact on vaginal dryness or sexual desire.10 However, symptomatic genital atrophy is common in postmenopausal breast cancer survivors, whether or not they use adjuvant therapy.
Although the FDA considers the use of any estrogen (systemic or vaginal) following a diagnosis of breast cancer to be contraindicated, some breast cancer survivors who have symptomatic genital atrophy express an interest in the use of vaginal estrogen. Use of 25-μg estradiol tablets (Vagifem) is associated with a short-term increase in serum estradiol levels.23 This finding has reinforced caution among medical oncologists about the safety of vaginal estrogen in breast cancer survivors. (The 25-μg tablets are no longer marketed.) The lowest dosage of vaginal estrogen available for the treatment of genital atrophy is found in 10-μg estradiol tablets (Vagifem) and the estradiol (2-mg) 3-month vaginal ring (Estring). Nonetheless, in the absence of data, oncologists will likely continue to be concerned that even the lowest dosage of vaginal estrogen could attenuate the favorable impact of AIs on breast cancer. Accordingly, use of vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy.
OBG Management: What about the ubiquitous hot flush? Vasomotor symptoms may be more common in women who take tamoxifen, but women on AIs are also bothered by flushes. What are the alternatives to estrogen therapy?
Dr. Kaunitz: Both nonprescription and prescription alternatives are available. Nonprescription options include soy extract and red clover isoflavones, black cohosh, and Chinese herbs. However, none of these over-the-counter approaches has been found to be more effective than placebo in the treatment of menopausal hot flushes.24-26
As for prescription nonhormonal options, ObGyns should recognize that all such treatments are off-label and that none attain the efficacy of hormone therapy in the treatment of vasomotor symptoms. The best-studied and most effective medications include gabapentin, SSRIs (especially paroxetine), and serotonin-norepinephrine reuptake inhibitors (venlafaxine and desvenlafaxine).24,27
OBG Management: Is there any evidence that AIs impair cognitive function in postmenopausal women?
Dr. Kaunitz: Because estrogen is important for cognition, one might anticipate that the profound reduction in background estrogen associated with AI use would impair cognition. Fortunately, the evidence to date is reassuring. Substudies of the BIG trial and the Tamoxifen and Exemestane Adjuvant Multinational Trial indicate that, compared with tamoxifen (which is associated with declines in cognitive function in postmenopausal women), letrozole and exemestane do not diminish cognitive function.28,29
OBG Management: Overall, what is the typical impact of an AI on a woman’s quality of life?
Dr. Kaunitz: Most women do very well on an AI, finding it easier to tolerate than tamoxifen, as we have discussed. However, a significant minority of women is seriously bothered by the adverse effects, with arthralgias usually leading the pack of complaints.30,31
OBG Management: Do some women discontinue adjuvant endocrine therapy because of adverse effects?
Dr. Kaunitz: Regrettably, the answer is “Yes.” A recent study from Kaiser Permanente of northern California found that roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32
OBG Management: What can an ObGyn do to encourage compliance with and completion of AI therapy?
Dr. Kaunitz: First, it is critical that patients understand that AIs are lifesaving drugs. As a recent paper points out, early discontinuation or noncompliance with AI therapy is associated with higher mortality.33
Clinicians should also help breast cancer patients understand what common side effects to anticipate with these medications.
Finally, clinicians who understand the financial toll a breast cancer diagnosis and treatment can take are better positioned to help women overcome challenges that may interfere with long-term compliance with AI therapy.
OBG Management: Do you expect the use of AIs in breast cancer survivors to become more commonplace?
Dr. Kaunitz: Given how common breast cancer is, and given the new ASCO guidelines and the extensive literature upon which they are based, ObGyns will be seeing more women using AIs. Although we are not the physicians who prescribe AIs, we need to remain up to date on their benefits and side effects. This important class of drugs is positioned to improve outcomes for postmenopausal women with breast cancer.
- Do certain SSRIs reduce the benefits of tamoxifen in breast cancer survivors?
Examining the Evidence
Andrew M. Kaunitz, MD - Does the clinical breast exam boost the sensitivity of mammography?
Examining the Evidence
Jennifer Griffin, MD, and Mark Pearlman, MD - A guide to lotions and potions for treating vaginal atrophy
Danielle D. Marshall, MD, and Cheryl Iglesia, MD
We want to hear from you! Tell us what you think.
Think breast cancer survivors are unlikely to show up in your practice? You should think again.
At last official count, 2.5 million women in the United States had a history of breast cancer.1 Most of them are now free of malignancy, but others are still grappling with the disease in some form or fashion.2 All need continuing health care.
Roughly two thirds of women who have breast cancer have disease that is hormone-receptor–positive.2,3 Recently updated guidelines from the American Society of Clinical Oncology (ASCO) recommend that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI) (see a summary of these guidelines on page 36). That makes it likely that a good number of breast cancer survivors who visit your practice are taking one of these medications: anastrozole (Arimidex), letrozole (Femara), or exemestane (Aromasin). These drugs are antiestrogens, given to postmenopausal women to reduce the likelihood of disease recurrence and progression.
The antiestrogenic properties of these drugs are what make them lifesavers. But the same qualities can create a range of health issues, from increased risk of osteoporosis and fracture to vasomotor and joint symptoms. And although ObGyns are not the physicians who prescribe these drugs, you may be the provider one of these women consults about their side effects and related issues.
To find out the latest on the management of women who are taking one of these agents, we inserted ourselves into the busy schedule of Andrew M. Kaunitz, MD, who agreed to address some fundamental—and some not so basic—questions about the drugs. In this extended Q&A, Dr. Kaunitz touches on mechanism of action, benefits versus risks, common side effects, compliance with therapy, and the ill effects of early discontinuation.
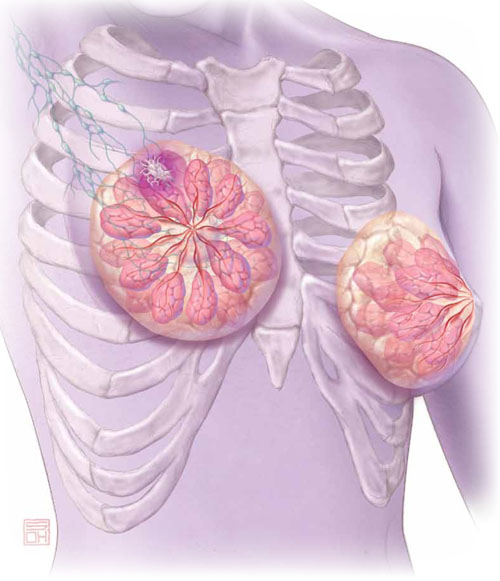
Aromatase inhibitors are better than tamoxifen at reducing the risk of breast cancer recurrence in postmenopausal women who have hormone-receptor–positive disease. But, they increase the risk of osteoporosis and fracture and often cause arthralgias and other complaints that ObGyn practitioners may be called upon to manage.
OBG Management: What is the overall aim of adjuvant endocrine therapy in the setting of breast cancer?
Dr. Kaunitz: Endocrine therapy—specifically, use of an AI—prevents the stimulation of breast cancer cells by endogenous estrogen. In other words, aromatase inhibitors suppress the growth of cancer cells that have estrogen receptors. These drugs also inhibit aromatase near any breast tumor and reduce estrogen levels in breast tissue.
OBG Management: What is the mechanism of action of adjuvant endocrine therapy?
Dr. Kaunitz: In postmenopausal women, androgens are converted to estrogens via the aromatase enzyme, which is present in adipose tissue and other sites. By blocking this enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
OBG Management: How does that differ from the mechanism of action of tamoxifen, another drug used in breast cancer patients?
Dr. Kaunitz: Tamoxifen is a selective estrogen receptor modulator (SERM). It blocks estrogen in breast tissue selectively, by competitively binding to estrogen receptors.5 However, tamoxifen has estrogenic effects in the uterus, bone, and liver, as well as other tissues.
The efficacy of AIs in preventing breast cancer recurrence in the first 2 years after breast cancer surgery is higher than that of tamoxifen. And unlike tamoxifen, the AIs do not increase the risk of venous thromboembolism or cause endometrial disease.
OBG Management: What effects do aromatase inhibitors have in premenopausal women?
Dr. Kaunitz: These agents are not recommended for use in premenopausal women because, in that population, the lion’s share of estrogen production takes place in the ovary rather than in adipose tissue and muscle. If you were to administer an AI to a premenopausal woman, the reduced hypothalamic and pituitary estrogen feedback could lead to ovarian stimulation—which could increase ovarian steroid production.
OBG Management: What about women who become amenorrheic as a result of chemotherapy or other cancer treatment? Do most oncologists assume that they are postmenopausal and prescribe an aromatase inhibitor?
Dr. Kaunitz: Clinicians should not assume that chemotherapy-induced amenorrhea signals permanent cessation of ovarian function. It is common for ovarian function to return in this setting. Accordingly, follicle-stimulating hormone (FSH) and estradiol levels should be assessed before an AI is considered as adjuvant therapy. Some investigators have suggested that the use of an AI in women who have chemotherapy-induced amenorrhea may actually increase the likelihood that ovarian function will return.6
OBG Management: Do all AIs produce the same effects?
Dr. Kaunitz: The AIs used in women with breast cancer are third-generation drugs. These AIs are classified as steroidal (type 1; exemestane) or nonsteroidal (type 2; anastrozole, letrozole). Exemestane, a steroid derived from androstenedione, inhibits the aromatase enzyme irreversibly. The nonsteroidal AIs are reversible.
Although all three AIs have numerous similarities, there are other distinctions between them in pharmacokinetics, mechanism of action, and toxicity—so they are not completely interchangeable.7 However, from our perspective as ObGyns caring for breast cancer survivors, we can assume that all three AIs will have similar effects on skeletal health and produce similar side effects in postmenopausal women.
- The American Society of Clinical Oncology recommends that adjuvant therapy for postmenopausal women who have hormone-positive breast cancer include an aromatase inhibitor (AI).
- AIs are not recommended for use in premenopausal women.
- By blocking the aromatase enzyme, AIs reduce endogenous estrogen levels by as much as 95%.4
- AIs are more effective than tamoxifen at preventing recurrence in the first 2 years after breast cancer surgery. Postmenopausal women taking an AI have a longer disease-free survival and time to recurrence than do women taking tamoxifen. They also have a lower incidence of contralateral breast cancer.
- The most prominent side effects of AI therapy include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD). However, endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.
- The FDA strongly discourages the use of estrogen therapy—systemic or local—in women who are taking an AI. Accordingly, bisphospho-nate therapy is recommended as first-line treatment of low bone mineral density. Vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy. And gabapentin, selective serotonin reuptake inhibitors, and serotonin norepinephrine reuptake inhibitors are the mainstay of therapy for vasomotor flushes.
- Roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32 Early discontinuation is associated with an increase in mortality.33
How much do we know about these drugs?
OBG Management: How long does a woman typically take an AI?
Dr. Kaunitz: At present, in women treated for early-stage, hormone-positive breast cancer, the optimal duration of treatment is unknown. Most oncologists prescribe an AI for 5 years, the length of treatment in a prominent trial of the drugs.8
OBG Management: Is that duration likely to increase as more data come in?
Dr. Kaunitz: The optimal duration of adjuvant AI therapy will be determined by the findings of long-term clinical trials. The National Surgical Adjuvant Breast and Bowel Project B-42 trial may provide new insights into optimal duration of AI treatment after initial tamoxifen therapy.9
OBG Management: How thoroughly have AIs been studied in regard to their use in breast cancer survivors and women who have early-stage disease? How would you characterize the quantity and quality of data that we have so far?
Dr. Kaunitz: AIs have been extensively studied. The most important clinical trials of AIs in this setting, including the Anastrozole, Tamoxifen Alone or in Combination (ATAC) trial (over 6,000 participants, median follow-up of 100 months) and the Breast International Group (BIG) trial (almost 5,000 participants, median follow-up of 76 months) have been detailed in the recent ASCO report.10 These two large landmark trials, in particular, formed the basis for ASCO’s recommendations to routinely incorporate AIs into the therapy of postmenopausal women who have hormone-receptor–positive breast cancer.
OBG Management: In treating breast cancer, what other applications are AIs used for?
Dr. Kaunitz: AIs appear to be slightly more effective than tamoxifen in treating postmenopausal women who have metastatic breast cancer.11
They are approved as first-line therapy for breast cancer in:
- postmenopausal women who have hormone-receptor–positive disease
- postmenopausal women who have locally advanced disease when the hormone receptor is unknown
- postmenopausal women who have metastatic disease.
In addition, they are approved as second-line treatment of advanced breast cancer in postmenopausal women who have disease progression following tamoxifen therapy.12
How effective is AI therapy?
OBG Management: What do we know about the efficacy of these drugs?
Dr. Kaunitz: Most of the studies that have explored efficacy compare an AI with tamoxifen rather than with placebo. In the ATAC trial, after a median follow-up of 33 months, women who were taking anastrozole for early-stage breast cancer had longer disease-free survival and time to recurrence and a lower incidence of contralateral breast cancer than did women taking tamoxifen.8
After 4 years of follow-up in the ATAC trial, women taking anastrozole continued to have more favorable disease-free survival (86.9% vs 84.5% for anastrozole and tamoxifen, respectively; hazard ratio [HR], 0.86; 95% confidence interval [CI], 0.76–0.99; P =.03).13 They also had a more favorable time to recurrence than did women taking tamoxifen (HR, 0.83; 95% CI, 0.71–0.96; P =.015). And women taking anastrozole had a lower incidence of contralateral breast cancer, as well, although this different did not achieve statistical significance (HR, 0.62; 95% CI, 0.38–1.02; P =.062).13
In the BIG study, women taking letrozole had a 5-year disease-free survival estimate of 84.0%, compared with 81.4% for women taking tamoxifen.14 In addition, women taking letrozole were significantly less likely than those taking tamoxifen to experience an event that ended a period of disease-free survival (HR, 0.81; 95% CI, 0.70–0.93; P =.003), especially the event of distant recurrence (HR, 0.73; 95% CI, 0.60–0.88; P =.001).14
And a phase-3 study of exemestane versus tamoxifen in women who had metastatic breast cancer found that the AI produced a superior response rate (46% vs 31% for exemestane and tamoxifen, respectively; odds ratio [OR], 1.85; 95% CI, 1.21–2.82; P =.005). In addition, median progression-free survival was greater with exemestane (9.9 months; 95% CI, 8.7–11.8 months) than with tamoxifen (5.8 months; 95% CI, 5.3–8.1 months). However, there was no difference between arms in progression-free survival or overall survival.
Postmenopausal women who have hormone-receptor–positive breast cancer should consider taking an aromatase inhibitor (AI) to lengthen disease-free survival and lower the risk of recurrence. That’s one of the recommendations in updated guidelines issued earlier this year by the American Society of Clinical Oncology (ASCO). The guidelines suggest a duration of AI therapy of 5 years. In the event that a woman discontinues AI therapy before 5 years are up, she should consider using tamoxifen to bring the total duration of treatment to 5 years.
Other recommendations in the guidelines include:
- Women who have taken tamoxifen for 5 years stand to benefit from switching to an AI for as long as 5 additional years.
- When advising a woman about adjuvant therapy with an AI, clinicians should consider the potential adverse effects, which include osteoporosis, fracture, and arthralgias.
- The third-generation AIs on the market today have not been found to have clinically important differences between them. A woman who cannot tolerate a particular AI should consider switching to a different AI.
- Switching from an AI to tamoxifen (or vice versa) may be an appropriate option for patients who cannot tolerate a drug’s adverse effects. In the event of a switch to tamoxifen, the clinician should counsel the patient about its adverse effects, which include venous thromboembolism and endometrial polyps, hyperplasia, and cancer.
The full guidelines can be accessed at http://jco.ascopubs.org/content/early/2010/07/12/JCO.2009.26.3756.full.pdf.
—Andrew M. Kaunitz, MD
How well tolerated are AIs?
OBG Management: What adverse effects are associated with AIs?
Dr. Kaunitz: Although AIs, overall, are safe medications, their use is associated with a number of adverse events. The most prominent side effects include arthralgias and hot flushes, while the most serious health impact appears to be a decrease in bone mineral density (BMD).
However, the drugs are generally perceived as being easier to tolerate than tamoxifen. That’s because endometrial cancer, vaginal bleeding and discharge, cerebrovascular events, venous thromboembolic events, and hot flushes all are less common among women taking an AI than among those taking tamoxifen.8,13
For overweight women, who face an elevated baseline risk of thromboembolism, the availability of AIs represents a major advantage over tamoxifen. Similarly, AIs offer advantages over tamoxifen for women who have an intact uterus. In addition, postmenopausal women who are taking a selective serotonin reuptake inhibitor (SSRI) such as paroxetine should take an AI rather than tamoxifen, because the concomitant use of SSRIs attenuates the efficacy of tamoxifen.15
What can be done about the most prominent risks?
OBG Management: Let’s focus on what’s probably the best-known adverse effect of AIs—the heightened risk of osteoporosis and fracture. How significant is this effect?
Dr. Kaunitz: Because use of an AI is associated with a profound reduction in endogenous estrogen levels, it also decreases BMD and can lead to osteoporotic fractures. All major phase-3 trials of adjuvant use of AIs in women who have early breast cancer found an increased risk of fracture, with no significant differences between AIs.16
Fortunately, bisphosphonate therapy (oral or intravenous) has been found to reduce bone loss associated with AI therapy.17,18
Assessing baseline BMD is important as women initiate AI therapy. Although no consensus exists regarding follow-up BMD assessment in the setting of AI use, an interval of 2 years is prudent, with the follow-up study preferably performed at the same imaging center and by the same technician as the first. If baseline osteoporosis is observed at the lumbar spine or hip, bisphosphonate therapy is appropriate. If a woman taking an AI has low bone mass (osteopenia) but not osteoporosis, bisphosphonate therapy should be considered if any of the following risk factors are present:
- advanced age
- history of fracture
- glucocorticoid therapy
- parental history of hip fracture
- low body weight
- current smoking status
- excess alcohol consumption
- rheumatoid arthritis
- known risk factors for secondary osteoporosis.19
In breast cancer survivors initiating or continuing AI therapy, it is also appropriate to check a serum vitamin D level and ensure that intake of this nutrient is adequate.
Bisphosphonates may offer oncologic benefits, as well; preliminary evidence suggests that the drugs may prevent recurrence of the cancer and prolong survival.20
OBG Management: What can an ObGyn offer to a woman who complains of significant AI-related arthralgia?
Dr. Kaunitz: Bone and joint symptoms, including aches, pain, and stiffness that is bilateral and not associated with other evidence of rheumatologic disorders, are among the most common side effects of AI therapy. On the plus side of the equation, these symptoms are more likely to be mild to moderate than severe. On the negative side, no specific treatment has been found to be effective in relieving these symptoms, which usually resolve within 2 months or so after discontinuing AI therapy.10
OBG Management: Do AIs have a negative impact on cardiovascular health?
Dr. Kaunitz: Unlike tamoxifen, AIs do not increase the risk of thromboembolic disease. Although the use of an AI may modestly increase the risk of ischemic cardiovascular disease (and lipid changes), compared with tamoxifen, AIs do not appear to increase cardiovascular risk compared with placebo.21,22
OBG Management: Do the antiestrogenic effects of AIs have a significant impact on vaginal health and sexual desire?
Dr. Kaunitz: A review of published reports did not find that the use of AIs has a predictable impact on vaginal dryness or sexual desire.10 However, symptomatic genital atrophy is common in postmenopausal breast cancer survivors, whether or not they use adjuvant therapy.
Although the FDA considers the use of any estrogen (systemic or vaginal) following a diagnosis of breast cancer to be contraindicated, some breast cancer survivors who have symptomatic genital atrophy express an interest in the use of vaginal estrogen. Use of 25-μg estradiol tablets (Vagifem) is associated with a short-term increase in serum estradiol levels.23 This finding has reinforced caution among medical oncologists about the safety of vaginal estrogen in breast cancer survivors. (The 25-μg tablets are no longer marketed.) The lowest dosage of vaginal estrogen available for the treatment of genital atrophy is found in 10-μg estradiol tablets (Vagifem) and the estradiol (2-mg) 3-month vaginal ring (Estring). Nonetheless, in the absence of data, oncologists will likely continue to be concerned that even the lowest dosage of vaginal estrogen could attenuate the favorable impact of AIs on breast cancer. Accordingly, use of vaginal lubricants and moisturizers are the mainstay strategy for symptomatic genital atrophy.
OBG Management: What about the ubiquitous hot flush? Vasomotor symptoms may be more common in women who take tamoxifen, but women on AIs are also bothered by flushes. What are the alternatives to estrogen therapy?
Dr. Kaunitz: Both nonprescription and prescription alternatives are available. Nonprescription options include soy extract and red clover isoflavones, black cohosh, and Chinese herbs. However, none of these over-the-counter approaches has been found to be more effective than placebo in the treatment of menopausal hot flushes.24-26
As for prescription nonhormonal options, ObGyns should recognize that all such treatments are off-label and that none attain the efficacy of hormone therapy in the treatment of vasomotor symptoms. The best-studied and most effective medications include gabapentin, SSRIs (especially paroxetine), and serotonin-norepinephrine reuptake inhibitors (venlafaxine and desvenlafaxine).24,27
OBG Management: Is there any evidence that AIs impair cognitive function in postmenopausal women?
Dr. Kaunitz: Because estrogen is important for cognition, one might anticipate that the profound reduction in background estrogen associated with AI use would impair cognition. Fortunately, the evidence to date is reassuring. Substudies of the BIG trial and the Tamoxifen and Exemestane Adjuvant Multinational Trial indicate that, compared with tamoxifen (which is associated with declines in cognitive function in postmenopausal women), letrozole and exemestane do not diminish cognitive function.28,29
OBG Management: Overall, what is the typical impact of an AI on a woman’s quality of life?
Dr. Kaunitz: Most women do very well on an AI, finding it easier to tolerate than tamoxifen, as we have discussed. However, a significant minority of women is seriously bothered by the adverse effects, with arthralgias usually leading the pack of complaints.30,31
OBG Management: Do some women discontinue adjuvant endocrine therapy because of adverse effects?
Dr. Kaunitz: Regrettably, the answer is “Yes.” A recent study from Kaiser Permanente of northern California found that roughly 50% of women who are prescribed adjuvant endocrine therapy with tamoxifen or an AI discontinue the drug early.32
OBG Management: What can an ObGyn do to encourage compliance with and completion of AI therapy?
Dr. Kaunitz: First, it is critical that patients understand that AIs are lifesaving drugs. As a recent paper points out, early discontinuation or noncompliance with AI therapy is associated with higher mortality.33
Clinicians should also help breast cancer patients understand what common side effects to anticipate with these medications.
Finally, clinicians who understand the financial toll a breast cancer diagnosis and treatment can take are better positioned to help women overcome challenges that may interfere with long-term compliance with AI therapy.
OBG Management: Do you expect the use of AIs in breast cancer survivors to become more commonplace?
Dr. Kaunitz: Given how common breast cancer is, and given the new ASCO guidelines and the extensive literature upon which they are based, ObGyns will be seeing more women using AIs. Although we are not the physicians who prescribe AIs, we need to remain up to date on their benefits and side effects. This important class of drugs is positioned to improve outcomes for postmenopausal women with breast cancer.
- Do certain SSRIs reduce the benefits of tamoxifen in breast cancer survivors?
Examining the Evidence
Andrew M. Kaunitz, MD - Does the clinical breast exam boost the sensitivity of mammography?
Examining the Evidence
Jennifer Griffin, MD, and Mark Pearlman, MD - A guide to lotions and potions for treating vaginal atrophy
Danielle D. Marshall, MD, and Cheryl Iglesia, MD
We want to hear from you! Tell us what you think.
1. Horner MJ, Ries LAG, Krapcho M, et al. eds. SEER Cancer Statistics Review, 1975–2006. Bethesda, Md: National Cancer Institute; 2009.http://seer.cancer.gov/csr/1975_2006. Accessed August 18, 2010.
2. American Cancer Society. Breast cancer facts and figures, 2009–2010. Atlanta, Ga: American Cancer Society; 2010. http://www.cancer.org/Research/CancerFactsFigures/BreastCancerFactsFigures/breast-cancer-facts—figures-2009-2010. Accessed August 18, 2010.
3. Li CI, Daling JR, Malone KE. Incidence of invasive breast cancer by hormone receptor status from 1992 to 1998. J Clin Oncol. 2003;21(1):28-34.
4. Miller WR. Aromatase inhibitors: mechanism of action and role in the treatment of breast cancer. Semin Oncol. 2003;30(4 suppl 14):3-11.
5. Peng J, Sengupta S, Jordan VC. Potential of selective estrogen receptor modulators as treatments and preventives of breast cancer. Anticancer Agents Med Chem. 2009;9(5):481-499.
6. Smith IE, Dowsett M, Yap YS, et al. Adjuvant aromatase inhibitors for early breast cancer after chemotherapy-induced amenorrhea: caution and suggested guidelines. J Clin Oncol. 2006;24(16):2444-2447.
7. Nabholtz JM, Mouret-Reynier MA, Durando X, et al. Comparative review of anastrozole, letrozole and exemestane in the management of early breast cancer. Expert Opin Pharmacother. 2009;10(9):1435-1447.
8. Baum M, Budzar AU, Cuzick J, et al. ATAC Trialists’ Group. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomized trial. Lancet. 2002;359(9324):2131-2139.
9. Letrozole in treating postmenopausal women who have received hormone therapy for hormone receptor-positive breast cancer. National Cancer Institute Web site.http://www.cancer.gov/clinicaltrials/NSABP-B-42. Published August 16, 2010. Accessed August 18, 2010.
10. Burstein HJ, Prestrud AA, Seidenfeld J, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone-receptor–positive breast cancer. J Clin Oncol. 2010;28(23):3784-3796.
11. Mauri D, Pavlidis N, Polyzos NP, Ioanidis JP. Survival with aromatase inhibitors and inactivators versus standard hormonal therapy in advanced breast cancer: meta-analysis. J Natl Cancer Inst. 2006;98(18):1285-1291.
12. Arimidex [package insert]. AstraZeneca; 2009.
13. Baum M, Buzdar A, Cuzick J, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Taxoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer. 2003;98(9):1802-1810.
14. Thurlimann B, Keshaviah A, Coates AS, et al. Breast International Group (BIG) 1-98 Collaborative Group. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353(26):2747-2757.
15. Kelly CM, Juurlink DM, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population-based cohort study. 2010;340:c693.-doi: 10.1136/bmj.c693.
16. Geisler J, Lonning PE. Impact of aromatase inhibitors on bone health in breast cancer patients. J Steroid Biochem Mol Biol. 2010;118(4–5):294-299.
17. Van Poznak C, Hannon RA, Mackey JR, et al. Prevention of aromatase inhibitor-induced bone loss using risedronate: the SABRE trial. J Clin Oncol. 2010;28(6):967-975.
18. Brufsky AM, Bosserman LD, Caradonna RR, et al. Zoledronic acid effectively prevents aromatase-inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole. Z-FAST study 36-month follow-up results. Clin Breast Cancer. 2009;9(2):77-85.
19. Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporosis Int. 2005;16(6):581-589.
20. Reeder JG, Brufsky AM. The role of bisphosphonates in the adjuvant setting for breast cancer. Oncology. 2010;24(6):462-467,475.
21. Nabholtz JM. Long-term safety of aromatase inhibitors in the treatment of breast cancer. Ther Clin Risk Manag. 2008;4(1):189-204.
22. Cuppone F, Bria E, Verma S, et al. Do adjuvant aromatase inhibitors increase the cardiovascular risk in postmenopausal women with early breast cancer? Meta-analysis of randomized trials. Cancer. 2008;112(2):260-267.
23. Kendall A, Dowsett M, Folkerd E, Smith I. Caution: Vaginal estradiol appears to be contraindicated in postmenopausal women on adjuvant aromatase inhibitors. Ann Oncol. 2006;17(4):584-587.
24. Nelson HD. Menopause. Lancet. 2008;371(9614):760-770.
25. Geller SE, Shulman LP, van Breemen RB, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Menopause. 2009;16(6):1156-1166.
26. Kaunitz AM. Effective herbal treatment of vasomotor symptoms—are we any closer? Menopause. 2009;16(3):428-429.
27. Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S. Study 319 Investigators. Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, randomized, placebo-controlled trial of efficacy and safety. Am J Obstet Gynecol. 2009;200(3):238.e1-e10.
28. Phillips KA, Ribi K, Sun Z, et al. Cognitive function in postmenopausal women receiving adjuvant letrozole or tamoxifen for breast cancer in the BIG 1-98 randomized trial [published online ahead of print April 10, 2010]. Breast. doi:10.1016/j.breast.2010.03.025.
29. Schilder CM, Seynaeve C, Beex LV, et al. Effects of tamoxifen and exemestane on cognitive functioning of postmenopausal patients with breast cancer: results from the neuropsychological side study of the Tamoxifen and Exemestane Adjuvant Multinational Trial. J Clin Oncol. 2010;28(8):1294-1300.
30. Din OS, Dodwell D, Wakefield RJ, Coleman RE. Aromatase inhibitor-induced arthralgia in early breast cancer: what do we know and how can we find out more? Breast Cancer Res Treat. 2010;120(3):525-538.
31. Burstein HJ. Aromatase inhibitor-associated arthralgia syndrome. Breast. 2007;16(3):223-234.
32. Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients [published online ahead of print June 28, 2010]. J Clin Oncol. doi: 10.1200/JCO.2009.25.9655.
33. Hershman DL, Shao T, Kushi LH, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer [published online ahead of print August 28, 2010]. Breast Cancer Res Treat. doi: 10.1007/ s10549-010-1132-4.
1. Horner MJ, Ries LAG, Krapcho M, et al. eds. SEER Cancer Statistics Review, 1975–2006. Bethesda, Md: National Cancer Institute; 2009.http://seer.cancer.gov/csr/1975_2006. Accessed August 18, 2010.
2. American Cancer Society. Breast cancer facts and figures, 2009–2010. Atlanta, Ga: American Cancer Society; 2010. http://www.cancer.org/Research/CancerFactsFigures/BreastCancerFactsFigures/breast-cancer-facts—figures-2009-2010. Accessed August 18, 2010.
3. Li CI, Daling JR, Malone KE. Incidence of invasive breast cancer by hormone receptor status from 1992 to 1998. J Clin Oncol. 2003;21(1):28-34.
4. Miller WR. Aromatase inhibitors: mechanism of action and role in the treatment of breast cancer. Semin Oncol. 2003;30(4 suppl 14):3-11.
5. Peng J, Sengupta S, Jordan VC. Potential of selective estrogen receptor modulators as treatments and preventives of breast cancer. Anticancer Agents Med Chem. 2009;9(5):481-499.
6. Smith IE, Dowsett M, Yap YS, et al. Adjuvant aromatase inhibitors for early breast cancer after chemotherapy-induced amenorrhea: caution and suggested guidelines. J Clin Oncol. 2006;24(16):2444-2447.
7. Nabholtz JM, Mouret-Reynier MA, Durando X, et al. Comparative review of anastrozole, letrozole and exemestane in the management of early breast cancer. Expert Opin Pharmacother. 2009;10(9):1435-1447.
8. Baum M, Budzar AU, Cuzick J, et al. ATAC Trialists’ Group. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomized trial. Lancet. 2002;359(9324):2131-2139.
9. Letrozole in treating postmenopausal women who have received hormone therapy for hormone receptor-positive breast cancer. National Cancer Institute Web site.http://www.cancer.gov/clinicaltrials/NSABP-B-42. Published August 16, 2010. Accessed August 18, 2010.
10. Burstein HJ, Prestrud AA, Seidenfeld J, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone-receptor–positive breast cancer. J Clin Oncol. 2010;28(23):3784-3796.
11. Mauri D, Pavlidis N, Polyzos NP, Ioanidis JP. Survival with aromatase inhibitors and inactivators versus standard hormonal therapy in advanced breast cancer: meta-analysis. J Natl Cancer Inst. 2006;98(18):1285-1291.
12. Arimidex [package insert]. AstraZeneca; 2009.
13. Baum M, Buzdar A, Cuzick J, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Taxoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer. 2003;98(9):1802-1810.
14. Thurlimann B, Keshaviah A, Coates AS, et al. Breast International Group (BIG) 1-98 Collaborative Group. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353(26):2747-2757.
15. Kelly CM, Juurlink DM, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population-based cohort study. 2010;340:c693.-doi: 10.1136/bmj.c693.
16. Geisler J, Lonning PE. Impact of aromatase inhibitors on bone health in breast cancer patients. J Steroid Biochem Mol Biol. 2010;118(4–5):294-299.
17. Van Poznak C, Hannon RA, Mackey JR, et al. Prevention of aromatase inhibitor-induced bone loss using risedronate: the SABRE trial. J Clin Oncol. 2010;28(6):967-975.
18. Brufsky AM, Bosserman LD, Caradonna RR, et al. Zoledronic acid effectively prevents aromatase-inhibitor associated bone loss in postmenopausal women with early breast cancer receiving adjuvant letrozole. Z-FAST study 36-month follow-up results. Clin Breast Cancer. 2009;9(2):77-85.
19. Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporosis Int. 2005;16(6):581-589.
20. Reeder JG, Brufsky AM. The role of bisphosphonates in the adjuvant setting for breast cancer. Oncology. 2010;24(6):462-467,475.
21. Nabholtz JM. Long-term safety of aromatase inhibitors in the treatment of breast cancer. Ther Clin Risk Manag. 2008;4(1):189-204.
22. Cuppone F, Bria E, Verma S, et al. Do adjuvant aromatase inhibitors increase the cardiovascular risk in postmenopausal women with early breast cancer? Meta-analysis of randomized trials. Cancer. 2008;112(2):260-267.
23. Kendall A, Dowsett M, Folkerd E, Smith I. Caution: Vaginal estradiol appears to be contraindicated in postmenopausal women on adjuvant aromatase inhibitors. Ann Oncol. 2006;17(4):584-587.
24. Nelson HD. Menopause. Lancet. 2008;371(9614):760-770.
25. Geller SE, Shulman LP, van Breemen RB, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Menopause. 2009;16(6):1156-1166.
26. Kaunitz AM. Effective herbal treatment of vasomotor symptoms—are we any closer? Menopause. 2009;16(3):428-429.
27. Archer DF, Dupont CM, Constantine GD, Pickar JH, Olivier S. Study 319 Investigators. Desvenlafaxine for the treatment of vasomotor symptoms associated with menopause: a double-blind, randomized, placebo-controlled trial of efficacy and safety. Am J Obstet Gynecol. 2009;200(3):238.e1-e10.
28. Phillips KA, Ribi K, Sun Z, et al. Cognitive function in postmenopausal women receiving adjuvant letrozole or tamoxifen for breast cancer in the BIG 1-98 randomized trial [published online ahead of print April 10, 2010]. Breast. doi:10.1016/j.breast.2010.03.025.
29. Schilder CM, Seynaeve C, Beex LV, et al. Effects of tamoxifen and exemestane on cognitive functioning of postmenopausal patients with breast cancer: results from the neuropsychological side study of the Tamoxifen and Exemestane Adjuvant Multinational Trial. J Clin Oncol. 2010;28(8):1294-1300.
30. Din OS, Dodwell D, Wakefield RJ, Coleman RE. Aromatase inhibitor-induced arthralgia in early breast cancer: what do we know and how can we find out more? Breast Cancer Res Treat. 2010;120(3):525-538.
31. Burstein HJ. Aromatase inhibitor-associated arthralgia syndrome. Breast. 2007;16(3):223-234.
32. Hershman DL, Kushi LH, Shao T, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy in a cohort of 8,769 early-stage breast cancer patients [published online ahead of print June 28, 2010]. J Clin Oncol. doi: 10.1200/JCO.2009.25.9655.
33. Hershman DL, Shao T, Kushi LH, et al. Early discontinuation and nonadherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer [published online ahead of print August 28, 2010]. Breast Cancer Res Treat. doi: 10.1007/ s10549-010-1132-4.
Are ObGyns offering the range of treatment options for early pregnancy failure?
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
One in every four women experiences EPF. Although office uterine evacuation and misoprostol administration are less invasive and less expensive alternatives to traditional OR evacuation, it is not clear how extensively clinicians employ these options in the United States.1,2
In 2008, Dalton and colleagues surveyed ObGyns, certified nurse midwives (CNMs), and family physicians (FPs) in the United States who had evaluated or treated, or both, a woman for EPF in the preceding 6 months. They achieved response rates of 51.0%, 70.9%, and 53.5%, respectively. Evaluable respondents had a mean age of 49 to 50 years and included 309 ObGyns (46.9% of whom were female), 368 CNMs (97.8% female), and 299 FPs (43.6% female).
Overall, approximately one third of respondents believe that office evacuation is riskier than OR evacuation. In addition, 65.7% of ObGyns believe that most patients prefer OR evacuation, compared with 46.2% and 43.1% of CNMs and FPs, respectively (P < .001). Among ObGyns, an adjusted analysis estimated the likelihood of providing office evacuation to be five times higher among those who have undergone training in induced abortion (P < .05). As for misoprostol for EPF, about two thirds of respondents overall believe that it is safe.
Dalton and associates posit that providers “perceive that their personal treatment preferences are different than their patients’. Whether this discordance results in women undergoing operating room uterine evacuation more often than is necessary or preferred could not be assessed by this study.” However, the authors also assert that, “given that providers affect treatment choice greatly, it is plausible that provider treatment preferences are an important influence on current treatment patterns.”
Certainly, women have diverse preferences for how EPF is managed, but many do find office evacuation and misoprostol to be acceptable methods. Accordingly, we should offer all options to them. As the investigators in this study suggest, we may need to focus on correcting inaccurate beliefs about these modalities among providers to increase their willingness to offer them.
The findings of this survey also underscore the fact that training programs that do not teach induced abortion—or that allow trainees to opt out of such training—can compromise the care provided to women who have EPF.—ANDREW M. KAUNITZ, MD
We want to hear from you! Tell us what you think.
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
1. Zhang J, Gilles JM, Barnhart K, et al. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005;353(8):761-769.
2. Harris LH, Dalton VK, Johnson TR. Surgical management of early pregnancy failure: history, politics, and safe, cost-effective care. Am J Obstet Gynecol. 2007;196(5):445.e1–e5.-
A new treatment for menorrhagia enters the US market
CASE: Heavy bleeding and apprehension over hormones
Your patient, R.L., 34 years old, has been bothered by gradually worsening menorrhagia for 2 years when she schedules an appointment to discuss treatment options. She prefers to avoid surgery, if at all possible, and is reluctant to use hormonal medications because she’s concerned about side effects. Nonsteroidal anti-inflammatory drugs provide inadequate relief.
R.L. asks if there is any other agent that can reduce her menstrual blood loss.
What can you offer to her?
Heavy menstrual bleeding (menorrhagia) impairs quality of life and prompts many women such as R.L. to seek a gynecologic consultation—many of them hoping to avoid surgery.
In the United States, medical-management options for the treatment of heavy menstrual bleeding include nonsteroidal anti-inflammatory drugs (NSAIDs) and off-label use of oral contraceptives, injectable depot medroxyprogesterone acetate, and high-dose oral progestin (e.g., norethindrone acetate, 5-mg tablets). The levonorgestrel intrauterine system (LNG-IUS; Mirena) is also widely used to treat heavy menstrual bleeding in women and was approved for this indication in October 2009. FDA approval of the LNG-IUS for heavy menstrual bleeding was based on a pivotal randomized trial demonstrating high efficacy.1,2
Very soon an additional option will be available—the antifibrinolytic agent tranexamic acid (to be sold by Ferring Pharmaceuticals under the brand name Lysteda). Although the LNG-IUS remains first-line treatment for heavy menstrual bleeding, tranexamic acid is appropriate for women who need to, or prefer to, avoid hormones.
How tranexamic acid works
Women who experience heavy menstrual bleeding have an elevated level of plasminogen activators in the endometrium, enzymes that facilitate the dissolution of clots. These enzymes can be inhibited by antifibrinolytic agents such as tranexamic acid, which competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis (FIGURE).3
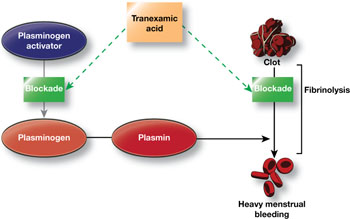
FIGURE How tranexamic acid stanches heavy menstrual bleeding
Tranexamic acid (Lysteda) competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis.Clinical trials of tranexamic acid to treat menorrhagia were first performed in the 1960s. The agent proved to be superior to placebo, NSAIDs, and cyclic oral progestin.4 However, the LNG-IUS has been found to be more effective than tranexamic acid in reducing menstrual blood loss.5
In the United States, until very recently, tranexamic acid was FDA-indicated only as an injectable agent for use at the time of dental extraction in hemophilic patients. However, an oral formulation has been widely used abroad, including in Canada, to treat heavy menstrual bleeding. In Sweden, the agent is available over the counter.
In November 2009, the FDA approved 650-mg tablets of tranexamic acid as a treatment for heavy menstrual bleeding.6
Recommended dosage
In women who have normal renal function, the recommended dosage of tranexamic acid is 1,300 mg (two 650-mg tablets) three times daily (a total of 3,900 mg) for as long as 5 days during menstruation. In women who have impaired renal function, the dosage should be adjusted according to the package insert.
In randomized clinical trials, tranexamic acid did not produce more side effects than placebo did. However, because of concerns that tranexamic acid may increase risk of venous thromboembolism (VTE), the agent is contraindicated in women who have a history of VTE.
Although women who use hormonal contraception have not been included in clinical trials of tranexamic acid, the FDA recommends that they take tranexamic acid only if there is “a strong medical need and the benefit of treatment will outweigh the potential increased risk of a thrombotic event.”6
Tranexamic acid will likely be of particular utility for women who desire treatment for heavy menstrual bleeding but who should, or would prefer to, avoid hormonal agents. British guidelines recommend that, when medical management is appropriate in the treatment of heavy menstrual bleeding, the LNG-IUS be considered first-line treatment, with tranexamic acid representing a second-line strategy.7
CASE: Resolved
When she hears about tranexamic acid, R.L. is eager to try it. She is pleased that it does not contain hormones and needs to be taken only 5 days or fewer each month. You give her a prescription and schedule a follow-up visit 3 months later, at which time she reports being satisfied with the drug.
1. FDA approves additional use for IUD Mirena to treat heavy menstrual bleeding in IUD users [press release]. Rockville, Md: FDA; Oct. 1, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm184747.htm. Accessed May 3, 2010.
2. Kaunitz AM, Bissonette F, Monteiro I, Lukkari-Lax E, Muysers C, Jensen J. Levonorgestrel intrauterine system and medroxyprogesterone acetate for treatment of heavy menstrual bleeding. Poster No. 49 Presented at Reproductive Health 2009, Association of Reproductive Health Professionals annual meeting, September 30–October 3, 2009, Los Angeles, Calif. Contraception. 2009;80(2):212.-
3. Grimes DA, Davis AR, Ramos DE. Heavy menstrual bleeding: Assessing impact, evaluating management options. OBG Management. 2009;21(10)(supple).-http://www.obgmanagement.com/article_pages.asp?filename="2206OBG_Article2" aid=7971. Accessed May 3, 2010.
4. Lethaby A, Farquhar C, Cooke I. Antifibrinolytics for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000;(4):CD000249.-
5. Milsom I, Andersson K, Andersch B, Rybo G. A comparison of flurbiprofen, tranexamic acid, and a levonorgestrel-releasing intrauterine contraceptive device in the treatment of idiopathic menorrhagia. Am J Obstet Gynecol. 1991;164(3):879-883.
6. FDA approves Lysteda to treat heavy menstrual bleeding [press release]. Rockville, Md: FDA; Nov. 13, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm190551.htm. Accessed May 3, 2010.
7. National Institute for Health and Clinical Excellence. Heavy menstrual bleeding. January 2007.http://www.nice.org.uk/CG44. Accessed May 3, 2010.
CASE: Heavy bleeding and apprehension over hormones
Your patient, R.L., 34 years old, has been bothered by gradually worsening menorrhagia for 2 years when she schedules an appointment to discuss treatment options. She prefers to avoid surgery, if at all possible, and is reluctant to use hormonal medications because she’s concerned about side effects. Nonsteroidal anti-inflammatory drugs provide inadequate relief.
R.L. asks if there is any other agent that can reduce her menstrual blood loss.
What can you offer to her?
Heavy menstrual bleeding (menorrhagia) impairs quality of life and prompts many women such as R.L. to seek a gynecologic consultation—many of them hoping to avoid surgery.
In the United States, medical-management options for the treatment of heavy menstrual bleeding include nonsteroidal anti-inflammatory drugs (NSAIDs) and off-label use of oral contraceptives, injectable depot medroxyprogesterone acetate, and high-dose oral progestin (e.g., norethindrone acetate, 5-mg tablets). The levonorgestrel intrauterine system (LNG-IUS; Mirena) is also widely used to treat heavy menstrual bleeding in women and was approved for this indication in October 2009. FDA approval of the LNG-IUS for heavy menstrual bleeding was based on a pivotal randomized trial demonstrating high efficacy.1,2
Very soon an additional option will be available—the antifibrinolytic agent tranexamic acid (to be sold by Ferring Pharmaceuticals under the brand name Lysteda). Although the LNG-IUS remains first-line treatment for heavy menstrual bleeding, tranexamic acid is appropriate for women who need to, or prefer to, avoid hormones.
How tranexamic acid works
Women who experience heavy menstrual bleeding have an elevated level of plasminogen activators in the endometrium, enzymes that facilitate the dissolution of clots. These enzymes can be inhibited by antifibrinolytic agents such as tranexamic acid, which competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis (FIGURE).3
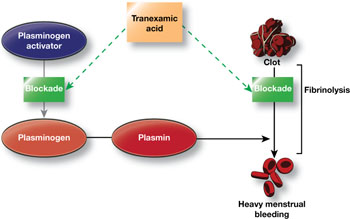
FIGURE How tranexamic acid stanches heavy menstrual bleeding
Tranexamic acid (Lysteda) competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis.Clinical trials of tranexamic acid to treat menorrhagia were first performed in the 1960s. The agent proved to be superior to placebo, NSAIDs, and cyclic oral progestin.4 However, the LNG-IUS has been found to be more effective than tranexamic acid in reducing menstrual blood loss.5
In the United States, until very recently, tranexamic acid was FDA-indicated only as an injectable agent for use at the time of dental extraction in hemophilic patients. However, an oral formulation has been widely used abroad, including in Canada, to treat heavy menstrual bleeding. In Sweden, the agent is available over the counter.
In November 2009, the FDA approved 650-mg tablets of tranexamic acid as a treatment for heavy menstrual bleeding.6
Recommended dosage
In women who have normal renal function, the recommended dosage of tranexamic acid is 1,300 mg (two 650-mg tablets) three times daily (a total of 3,900 mg) for as long as 5 days during menstruation. In women who have impaired renal function, the dosage should be adjusted according to the package insert.
In randomized clinical trials, tranexamic acid did not produce more side effects than placebo did. However, because of concerns that tranexamic acid may increase risk of venous thromboembolism (VTE), the agent is contraindicated in women who have a history of VTE.
Although women who use hormonal contraception have not been included in clinical trials of tranexamic acid, the FDA recommends that they take tranexamic acid only if there is “a strong medical need and the benefit of treatment will outweigh the potential increased risk of a thrombotic event.”6
Tranexamic acid will likely be of particular utility for women who desire treatment for heavy menstrual bleeding but who should, or would prefer to, avoid hormonal agents. British guidelines recommend that, when medical management is appropriate in the treatment of heavy menstrual bleeding, the LNG-IUS be considered first-line treatment, with tranexamic acid representing a second-line strategy.7
CASE: Resolved
When she hears about tranexamic acid, R.L. is eager to try it. She is pleased that it does not contain hormones and needs to be taken only 5 days or fewer each month. You give her a prescription and schedule a follow-up visit 3 months later, at which time she reports being satisfied with the drug.
CASE: Heavy bleeding and apprehension over hormones
Your patient, R.L., 34 years old, has been bothered by gradually worsening menorrhagia for 2 years when she schedules an appointment to discuss treatment options. She prefers to avoid surgery, if at all possible, and is reluctant to use hormonal medications because she’s concerned about side effects. Nonsteroidal anti-inflammatory drugs provide inadequate relief.
R.L. asks if there is any other agent that can reduce her menstrual blood loss.
What can you offer to her?
Heavy menstrual bleeding (menorrhagia) impairs quality of life and prompts many women such as R.L. to seek a gynecologic consultation—many of them hoping to avoid surgery.
In the United States, medical-management options for the treatment of heavy menstrual bleeding include nonsteroidal anti-inflammatory drugs (NSAIDs) and off-label use of oral contraceptives, injectable depot medroxyprogesterone acetate, and high-dose oral progestin (e.g., norethindrone acetate, 5-mg tablets). The levonorgestrel intrauterine system (LNG-IUS; Mirena) is also widely used to treat heavy menstrual bleeding in women and was approved for this indication in October 2009. FDA approval of the LNG-IUS for heavy menstrual bleeding was based on a pivotal randomized trial demonstrating high efficacy.1,2
Very soon an additional option will be available—the antifibrinolytic agent tranexamic acid (to be sold by Ferring Pharmaceuticals under the brand name Lysteda). Although the LNG-IUS remains first-line treatment for heavy menstrual bleeding, tranexamic acid is appropriate for women who need to, or prefer to, avoid hormones.
How tranexamic acid works
Women who experience heavy menstrual bleeding have an elevated level of plasminogen activators in the endometrium, enzymes that facilitate the dissolution of clots. These enzymes can be inhibited by antifibrinolytic agents such as tranexamic acid, which competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis (FIGURE).3
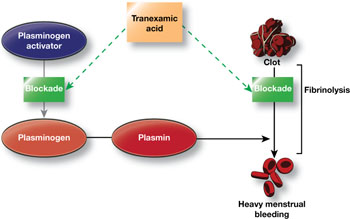
FIGURE How tranexamic acid stanches heavy menstrual bleeding
Tranexamic acid (Lysteda) competitively blocks the conversion of plasminogen to plasmin, thereby reducing fibrinolysis.Clinical trials of tranexamic acid to treat menorrhagia were first performed in the 1960s. The agent proved to be superior to placebo, NSAIDs, and cyclic oral progestin.4 However, the LNG-IUS has been found to be more effective than tranexamic acid in reducing menstrual blood loss.5
In the United States, until very recently, tranexamic acid was FDA-indicated only as an injectable agent for use at the time of dental extraction in hemophilic patients. However, an oral formulation has been widely used abroad, including in Canada, to treat heavy menstrual bleeding. In Sweden, the agent is available over the counter.
In November 2009, the FDA approved 650-mg tablets of tranexamic acid as a treatment for heavy menstrual bleeding.6
Recommended dosage
In women who have normal renal function, the recommended dosage of tranexamic acid is 1,300 mg (two 650-mg tablets) three times daily (a total of 3,900 mg) for as long as 5 days during menstruation. In women who have impaired renal function, the dosage should be adjusted according to the package insert.
In randomized clinical trials, tranexamic acid did not produce more side effects than placebo did. However, because of concerns that tranexamic acid may increase risk of venous thromboembolism (VTE), the agent is contraindicated in women who have a history of VTE.
Although women who use hormonal contraception have not been included in clinical trials of tranexamic acid, the FDA recommends that they take tranexamic acid only if there is “a strong medical need and the benefit of treatment will outweigh the potential increased risk of a thrombotic event.”6
Tranexamic acid will likely be of particular utility for women who desire treatment for heavy menstrual bleeding but who should, or would prefer to, avoid hormonal agents. British guidelines recommend that, when medical management is appropriate in the treatment of heavy menstrual bleeding, the LNG-IUS be considered first-line treatment, with tranexamic acid representing a second-line strategy.7
CASE: Resolved
When she hears about tranexamic acid, R.L. is eager to try it. She is pleased that it does not contain hormones and needs to be taken only 5 days or fewer each month. You give her a prescription and schedule a follow-up visit 3 months later, at which time she reports being satisfied with the drug.
1. FDA approves additional use for IUD Mirena to treat heavy menstrual bleeding in IUD users [press release]. Rockville, Md: FDA; Oct. 1, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm184747.htm. Accessed May 3, 2010.
2. Kaunitz AM, Bissonette F, Monteiro I, Lukkari-Lax E, Muysers C, Jensen J. Levonorgestrel intrauterine system and medroxyprogesterone acetate for treatment of heavy menstrual bleeding. Poster No. 49 Presented at Reproductive Health 2009, Association of Reproductive Health Professionals annual meeting, September 30–October 3, 2009, Los Angeles, Calif. Contraception. 2009;80(2):212.-
3. Grimes DA, Davis AR, Ramos DE. Heavy menstrual bleeding: Assessing impact, evaluating management options. OBG Management. 2009;21(10)(supple).-http://www.obgmanagement.com/article_pages.asp?filename="2206OBG_Article2" aid=7971. Accessed May 3, 2010.
4. Lethaby A, Farquhar C, Cooke I. Antifibrinolytics for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000;(4):CD000249.-
5. Milsom I, Andersson K, Andersch B, Rybo G. A comparison of flurbiprofen, tranexamic acid, and a levonorgestrel-releasing intrauterine contraceptive device in the treatment of idiopathic menorrhagia. Am J Obstet Gynecol. 1991;164(3):879-883.
6. FDA approves Lysteda to treat heavy menstrual bleeding [press release]. Rockville, Md: FDA; Nov. 13, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm190551.htm. Accessed May 3, 2010.
7. National Institute for Health and Clinical Excellence. Heavy menstrual bleeding. January 2007.http://www.nice.org.uk/CG44. Accessed May 3, 2010.
1. FDA approves additional use for IUD Mirena to treat heavy menstrual bleeding in IUD users [press release]. Rockville, Md: FDA; Oct. 1, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm184747.htm. Accessed May 3, 2010.
2. Kaunitz AM, Bissonette F, Monteiro I, Lukkari-Lax E, Muysers C, Jensen J. Levonorgestrel intrauterine system and medroxyprogesterone acetate for treatment of heavy menstrual bleeding. Poster No. 49 Presented at Reproductive Health 2009, Association of Reproductive Health Professionals annual meeting, September 30–October 3, 2009, Los Angeles, Calif. Contraception. 2009;80(2):212.-
3. Grimes DA, Davis AR, Ramos DE. Heavy menstrual bleeding: Assessing impact, evaluating management options. OBG Management. 2009;21(10)(supple).-http://www.obgmanagement.com/article_pages.asp?filename="2206OBG_Article2" aid=7971. Accessed May 3, 2010.
4. Lethaby A, Farquhar C, Cooke I. Antifibrinolytics for heavy menstrual bleeding. Cochrane Database Syst Rev. 2000;(4):CD000249.-
5. Milsom I, Andersson K, Andersch B, Rybo G. A comparison of flurbiprofen, tranexamic acid, and a levonorgestrel-releasing intrauterine contraceptive device in the treatment of idiopathic menorrhagia. Am J Obstet Gynecol. 1991;164(3):879-883.
6. FDA approves Lysteda to treat heavy menstrual bleeding [press release]. Rockville, Md: FDA; Nov. 13, 2009.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm190551.htm. Accessed May 3, 2010.
7. National Institute for Health and Clinical Excellence. Heavy menstrual bleeding. January 2007.http://www.nice.org.uk/CG44. Accessed May 3, 2010.
IN THIS ARTICLE
UPDATE: MENOPAUSE
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
Much has changed in the management of menopausal women. The Women’s Health Initiative (WHI) and other trials shed light on the risk-benefit ratio of hormone therapy (HT) and significantly altered patterns of usage. A new fracture risk-assessment tool devised by the World Health Organization is now available for widespread use; it continues to be refined so that it can be applied to specific populations with greater accuracy. And the management of low bone mass and osteoporosis has evolved so that we can determine with greater precision exactly who merits our attention.
This year, the Update on Menopause describes:
- a reanalysis of WHI data, focusing on the relationship between hormone therapy and the risk of coronary artery disease (CAD)
- a study from Finland that explores the risk of endometrial cancer associated with various progestin regimens in women who are taking estrogen and who have an intact uterus
- guidance from the North American Menopause Society and the National Osteoporosis Foundation on who, how, and when to evaluate for a likelihood of fracture
- insight into the benefits of and need for vitamin D among menopausal women
- information on a new selective estrogen-receptor modulator under development.
Hormone therapy and CAD: Is the glass half full…or half empty?
Toh S, Hernández-Díaz S, Logan R, Rossouw JE, Hernán MA. Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear? A randomized trial. Ann Intern Med. 2010;152(4):211–217.
North American Menopause Society. Position Statement: Estrogen and progestogens use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(2):242–255. DOI: 10.1097/gme.0b013e3181d0f6b9. http://www.menopause.org/PSht10.pdf. Accessed April 1, 2010.
When estrogen therapy is initiated within 10 years of menopause, it may reduce the risk of CAD, according to data from the WHI randomized trial and observational data.
The picture isn’t as clear in regard to estrogen-progestin HT. In a just-published study, Toh and colleagues reassessed data from the WHI trial of continuous oral conjugated equine estrogen plus medroxyprogesterone acetate versus placebo. They also compared the WHI findings with those of the large observational Nurses’ Health Study (NHS). Here are some of their findings:
- participants became less consistent in taking study medication over time—a finding of many long-term studies. This trend prompted Toh and colleagues to adjust their analysis for adherence
- among women who used HT within 10 years after the menopausal transition, the hazard ratio (HR) for CAD was 0.64 (95% confidence interval [CI], 0.21, 1.99) in the WHI and 0.68 (95% CI, 0.24, 1.91) in the NHS. Both hazard ratios suggest that the risk of CAD is lower in Ht users than in nonusers—although the difference is not significant
- when investigators pooled the WHI and NHS findings, the hazard ratio for CAD associated with combination HT was 0.66 (95% CI, 0.31, 1.42). Note that, as the number of participants increases, the confidence limits narrow.
Toh and colleagues concluded that their analysis demonstrated no diminished risk of CAD with HT use. My reading of these data is different: Combination HT does not increase the risk of CAD in women who have been postmenopausal for less than 10 years.
Focus on risk was unbalanced
The question of whether combination HT reduces the risk of CAD in younger women is somewhat moot. I am not aware of any ObGyn in the United States who uses HT to prevent CAD, and the great majority of symptomatic women who consider initiating HT have been menopausal for less than a decade. For these reasons, I find the conclusions drawn by Toh and colleagues a bit mystifying—and the title they chose for their study may be misleading:
Coronary heart disease in postmenopausal recipients of estrogen plus progestin therapy: Does the increased risk ever disappear?
Nevertheless, fear that HT might increase the risk of CAD is common among symptomatic menopausal women and their physicians. What this important analysis can offer is reassurance to symptomatic women who have been menopausal for less than 10 years: namely, that HT—estrogen alone or estrogen plus progestin—does not increase the risk of myocardial infarction or death from CAD.
You should counsel symptomatic women who have been menopausal less than 10 years that short-term use of estrogen therapy or estrogen-progestin therapy does not appear to increase their risk of CAD.
In women taking estrogen, sequential progestin therapy raises the risk of endometrial cancer
Jaakkola S, Lyytinen H, Pukkala E, Ylikorkala O. Endometrial cancer in postmenopausal women using estradiol-progestin therapy. Obstet Gynecol. 2009;114(6):1197–1204.
Because unopposed estrogen raises the risk of endometrial hyperplasia and adenocarcinoma, we prescribe progestational therapy when a menopausal woman who has an intact uterus decides to use estrogen.
Some ObGyns prescribe continuous progestin in this setting; others, sequential progestin (e.g., continuous estrogen along with 14 days of progestin each month). Still others prescribe “long-cycle” sequential regimens comprising continuous estrogen plus 2 weeks of progestin every 3 months. However, the long-term endometrial safety of these regimens has not been adequately explored.
In a national cohort study in Finland, Jaakkola and coworkers followed more than 200,000 menopausal women who used estrogen plus progestin (E+P) HT from 1994 to 2006. The incidence of endometrial cancer in these women was compared with that of all women in Finland. Overall, 1,400 newly diagnosed cases of endometrial cancer were identified.
Investigators found that, compared with the general population:
- E+P users overall had a 54% greater risk of endometrioid endometrial adenocarcinoma, the tumor most closely associated with use of unopposed estrogen
- monthly sequential E+P users had a 69% (5 years’ use) and 156% (10 years’ use) greater risk of this tumor
- at 5 and 10 years of use, long-cycle sequential HT was associated with a substantially higher risk of endometrial adenocarcinoma than was monthly sequential HT
- the endometrial safety profiles of transdermal and oral sequential HT were comparable; so were those of medroxyprogesterone acetate and norethindrone acetate
- in contrast to sequential HT regimens, continuous E+P was associated with a lower risk of endometrial cancer than that found in the overall population (76% risk reduction after 3 to 5 years of use).
These important findings clarify the safety profiles of long-term continuous E+P, which is protective, and sequential E+P, which substantially raises the risk of endometrial adenocarcinoma.
The authors estimate that, for every 1,000 women who use E+P for 10 years, eight additional cases of cancer will be diagnosed if that therapy is sequential and monthly; on the other hand, three or four fewer cases will be diagnosed if HT is continuous.
Women who use E+P hormone therapy should take the progestin continuously rather than sequentially.
Any woman who uses sequential progestin over the long term should undergo regular endometrial monitoring via transvaginal ultrasonography, endometrial biopsy, or both.
Guidance on who to assess for osteoporosis—and when to treat them
The North American Menopause Society. NAMS continuing medical education activity: Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17(1):23–24.
National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, D.C.: NOF: 2008. http://www.nof.org/professionals/NOF_Clinicians_Guide.pdf. Accessed April 1, 2010.
Kaunitz AM, McClung MR, Feldman RG, Wysocki S. Postmenopausal osteoporosis: fracture risk and prevention. OBG Management. 2009;21(10)(suppl):S1–6.
The North American Menopause Society (NAMS) has updated its position statement on the management of osteoporosis in postmenopausal women, incorporating many recommendations from guidelines issued in 2008 by the National Osteoporosis Foundation. You may find the recommendations on bone mineral density (BMD) assessment and use of medications to prevent fractures of particular interest.
BMD assessment should focus on women at high risk of fracture
In the United States, many women at low risk of fracture begin BMD assessment in their 50s via dual-energy x-ray absorptiometry (DXA) imaging of the lumbar spine and hip (FIGURE). As a result, many of these menopausal women are given a diagnosis of low bone mass (often termed “osteopenia” when in fact their DXA findings do not meet the criteria for osteoporosis) and are given a prescription for a bisphosphonate, often of indefinite duration.
FIGURE When DXA imaging reveals low BMD
DXA scan of the lumbar spine and both hips showing osteoporosis in a 69-year-old woman. The colored graphs show the range of bone mineral density (BMD) across eight decades. The blue bars represent normal bone density; the white squares within the orange and red bars denote this patient’s low BMD. NAMS’s latest position statement clarifies exactly which women should be assessed, concluding that BMD measurement is appropriate in postmenopausal women who are not only at least 50 years old, but who also have one or more of the following risk factors for fracture:
- a history of fracture after menopause
- body mass index (BMI) <21 kg/m2 or weight <127 lb
- parental history of hip fracture
- current smoking, rheumatoid arthritis, or excessive alcohol intake (i.e., three or more drinks per day).
In the absence of these risk factors, BMD assessment should begin at 65 years of age.
Once initiated, treatment is usually long-term
The NAMS statement indicates that drug therapy—using bisphosphonates as first-line agents—is appropriate in postmenopausal women who have any of the following:
- a history of osteoporotic hip or vertebral fracture
- DXA-defined T-score lower than –2.5, indicating osteoporosis
- T-score from –1.0 to –2.5 (low bone mass) plus either a FRAX score that indicates a 10-year risk of hip fracture of at least 3% or a 10-year overall risk of osteoporotic fracture of at least 20%.
The World Health Organization (WHO) Fracture Risk Algorithm (FRAX) was developed to calculate the 10-year risk of hip fracture and the 10-year overall risk of osteoporotic fracture (online at http://www.shef.ac.uk/FRAX/). (For a description of two menopausal cases in which this Web site was used to determine appropriate clinical management, see the article by Kaunitz and colleagues cited above. Also, be aware that use of the FRAX Web site is inappropriate for making clinical decisions about women who are already using prescription antifracture therapy.)
NAMS points out that 1) treatment should usually span a period of years and 2) the risk of fracture after discontinuation of treatment has not been adequately studied.
Lasofoxifene seems unlikely to offer net benefits greater than what women obtain from existing therapies
Clinicians and menopausal women would welcome any agent that can prevent osteoporotic fracture with minimal adverse outcomes. Lasofoxifene appears to fulfill the first half of this equation, but its potential risks and questionable long-term effects cast doubt on its overall utility.
In a manufacturer-sponsored international trial, investigators randomized 8,556 women (mean age, 67 years) who met BMD criteria for osteoporosis to the selective estrogen-receptor modulator (SERM) lasofoxifene (0.25 mg daily or 0.5 mg daily) or placebo for 5 years. Women who received 0.5 mg daily of lasofoxifene had a substantially lower risk of vertebral (HR, 0.58) and nonvertebral (HR, 0.76) fracture than did women who received placebo.1
This dosage of lasofoxifene was also associated with a lower risk of estrogen-receptor–positive breast cancer (HR, 0.19), CAD events (HR, 0.68), and stroke (HR, 0.64), but a twofold higher risk of venous thromboembolic events overall and more than fourfold higher risk of pulmonary embolism. The incidence of endometrial cancer and endometrial hyperplasia was low (fewer than three women in each group), but endometrial polyps and hypertrophy were substantially more common among women who received either dosage of lasofoxifene.1
At 3 years, questionable benefit
Although these findings indicate that lasofoxifene lowers the risk of radiologically confirmed vertebral fracture, data submitted to the FDA reveal that the risk of clinical vertebral fracture was not reduced at 3 years.
Both raloxifene and lasofoxifene are associated with a heightened risk of venous thromboembolic events. Although lasofoxifene did not raise the risk of endometrial neoplasia or hyperplasia in the trial just described, the rates of other endometrial outcomes suggest that this agent has a proliferative effect on the endometrium.1
The reduced risk of estrogen-receptor–positive breast cancer and CAD events is intriguing. However, as an editorial writer points out, a clinician would need to treat 492 women for 1 year to prevent one major CAD event.2
Lasofoxifene does not seem to offer any clinically important benefit over existing SERMs. Moreover, alendronate, a generic bisphosphonate proven to prevent clinical vertebral and nonvertebral fracture, often fills the bill for the prevention of osteoporotic fracture in menopausal women.
References
1. Cummings SR, Ensrud K, Delmas PF, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686-696.
2. Becker C. Another selective estrogen-receptor modulator for osteoporosis. N Engl J Med. 2010;362(8):752-754.
BMD reassessment should be minimal
BMD assessment by means of DXA imaging to monitor the effects of therapy is appropriate after 1 or 2 years of treatment. Thereafter, repeat measurement is of little value in women whose BMD has stabilized or increased on therapy. A follow-up DXA scan is of limited use in predicting the effectiveness of antiresorptive therapy in lowering the risk of fracture. Moreover, changes in BMD can lag behind actual therapeutic benefits (i.e., fracture prevention).
In menopausal women who are not taking prescription antifracture therapy, the follow-up measurement of BMD is not useful until 2 to 5 years after initial testing. Although BMD may be lost rapidly in the initial years after menopause (or after discontinuation of HT), subsequently it plateaus or declines slowly.
If a woman is not using prescription antifracture therapy and is within 2 or 3 years of menopause (or if she has discontinued menopausal HT in the past 2 to 3 years), retesting in 2 years is prudent. However, if the same woman were 5 or more years post-menopausal and had not recently discontinued HT, follow-up BMD assessment can be deferred for 3 to 5 years.
This updated guidance from NAMS emphasizes that BMD need not be assessed in women younger than 65 years unless they have specific risk factors. FRAX evaluation also makes it possible to estimate the 10-year risk of fracture in women who have low bone mass but who do not meet criteria for osteoporosis. FRAX evaluation indicates that prescription therapy is rarely required for women in their 50s or 60s who have low bone mass (but not osteoporosis). For women in their 70s or 80s who have low bone mass (but not osteoporosis), however, FRAX evaluation often leads to a recommendation to initiate prescription antifracture treatment.
Many postmenopausal women who are in their 50s or 60s and who have T-scores of –1.0 to –2.5 are given bisphosphonates, despite being at low risk of fracture. Adherence to the NAMS guidelines will help prevent unnecessary assessment and treatment. In particular, the NAMS recommendations for follow-up BMD assessment—i.e., one-time evaluation 1 to 2 years after initiating therapy and no further assessment in women found to have stable BMD at the first follow-up DXA—should simplify clinical management in this setting.
Hold off on ordering DXA testing until women meet criteria for BMD assessment. In women who do not have osteoporosis, limit use of bisphosphonates to those who have an elevated 10-year risk of fracture, as assessed using the FRAX tool.
Our menopausal patients should be taking more vitamin D supplements
Bischoff-Ferrari H. Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23(6):789.
Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;339:b3692.
Stewart JW, Alekel DL, Ritland LM, et al. Serum 25-hydroxyvitamin D is related to indicators of overall physical fitness in healthy postmenopausal women. Menopause. 2009;16(6):1093–1101.
Office of Dietary Supplements. Dietary Supplement Fact Sheet: Vitamin D. National Institutes of Health Web site. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Updated November 13, 2009. Accessed April 2, 2010.
We have long recognized the important role vitamin D plays in promoting calcium absorption from the gut and maintaining adequate serum calcium and phosphate concentrations to enable normal bone mineralization. Now, studies reveal that the vitamin also helps prevent falls and promotes overall fitness in menopausal women. It has also become clear that traditional targets for vitamin D supplementation are inadequate.
Two recent meta-analyses of double-blind, randomized trials concluded that vitamin D reduces the risk of falls in a dose-dependent manner. Dr. Heike Bischoff-Ferrari, a Swiss scientist and a leading vitamin D researcher, points out that 1) a minimum of 700 to 1,000 IU of vitamin D supplementation daily is appropriate in menopausal women and 2) a higher amount is indicated for those who are obese or deficient in vitamin D.
Compare the current recommended dietary allowance (RDA) for adults 51 to 70 years old: 400 IU daily. The federal Food and Nutrition Board is expected to update the vitamin D RDA this spring. The 2010 NAMS statement on osteoporosis recommends a daily vitamin D intake of 800 to 1,000 IU for menopausal women.
Ask your patient to add up the aggregate daily amount of vitamin D she ingests with her multivitamin and calcium and vitamin D supplements. If it is less than 800 IU, have her purchase over-the-counter vitamin D supplements (available in 400, 1,000, and 2,000 IU capsules). Obese patients and those known to be deficient may need to ingest higher daily amounts of vitamin D.
Do certain SSRIs reduce the benefits of tamoxifen in breast cancer survivors?
Tamoxifen is widely used by women who have receptor-positive breast cancer to lower their risk of recurrence. Tamoxifen is a prodrug converted by the hepatic cytochrome P450 enzyme system (particularly isoenzyme CYP2D6) to active metabolites, which have much higher affinity for the estrogen receptor than the parent prodrug has. Selective serotonin reuptake inhibitors (SSRIs) inhibit CYP2D6 to variable degrees, with paroxetine thought to be the most potent inhibitor.
The fact that SSRIs inhibit CYP2D6 is important because as many as one in every four women who have breast cancer experiences depression as well.1 SSRIs are widely prescribed for these patients—not only as treatment for their depressive disorder but also because the drugs have been shown to offer some relief from hot flashes.
In this cohort study from Ontario, where health care is delivered in a centralized fashion, Kelly and colleagues assessed the survival of breast cancer survivors 66 years and older who were treated with both tamoxifen and an SSRI, or with both tamoxifen and venlafaxine (which inhibits reuptake of both serotonin and norepinephrine).
The median age of the 2,430 eligible and evaluable women at the time of tamoxifen initiation was 74 years. These women began using tamoxifen between 1993 and 2005, with a median duration of use of 4 years. Paroxetine was the most commonly used SSRI in this study (25.9%), followed by sertraline (Zoloft, 22.3%), citalopram (Celexa, 19.2%), venlafaxine (Effexor, 15.0%), fluoxetine (Prozac, Sarafem, 10.4%), and fluvoxamine (Luvox, 7.2%).
Neither duloxetine (Cymbalta) nor escitalopram (Lexapro) were included in this analysis.
By the end of follow-up, 1,074 women (44.2%) in the cohort had died, 374 of them from breast cancer.
When taken with tamoxifen, paroxetine increased breast cancer mortality
Concomitant use of paroxetine and tamoxifen was associated with a significantly increased risk of death from breast cancer. In addition, as the proportion of concomitant use of the drugs increased to 25%, 50%, and 75% of total tamoxifen use, the adjusted risk of death increased 24%, 54%, and 91%, respectively. Among women taking tamoxifen, concomitant use of other SSRIs or venlafaxine was not associated with an increased risk of death.
Based on their data, the investigators determined that use of paroxetine during 41% of tamoxifen treatment (the median overlap observed in this study) would result in one additional breast cancer death at 5 years for every 19.7 women treated in this fashion. If paroxetine were used for the entire duration of tamoxifen treatment—an overlap of 100%—an additional death would occur for every 6.9 women treated.
The authors also noted that fluoxetine is a “strong inhibitor” of tamoxifen, although it was not associated with an increased risk of breast cancer death in this trial. One reason may be the small number of women who took tamoxifen and fluoxetine concomitantly in this study.
“Our results should not be viewed as evidence that fluoxetine can be safely used in combination with tamoxifen,” Kelly and coworkers write. “Similarly, we cannot exclude the possibility that insufficient sample size explains the nonsignificant mortality results with other SSRIs.”
Because fluoxetine is known to strongly inhibit CYP2D6, other antidepressants are more prudent choices for tamoxifen users.
In addition, switch any tamoxifen user who is taking paroxetine to an alternative antidepressant. Venlafaxine may be a sound choice in this setting, given the data indicating its efficacy as a nonhormonal treatment for vasomotor symptoms in breast cancer survivors.—ANDREW M. KAUNITZ, MD
Reference
1. Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30(2):112-126.
Tamoxifen is widely used by women who have receptor-positive breast cancer to lower their risk of recurrence. Tamoxifen is a prodrug converted by the hepatic cytochrome P450 enzyme system (particularly isoenzyme CYP2D6) to active metabolites, which have much higher affinity for the estrogen receptor than the parent prodrug has. Selective serotonin reuptake inhibitors (SSRIs) inhibit CYP2D6 to variable degrees, with paroxetine thought to be the most potent inhibitor.
The fact that SSRIs inhibit CYP2D6 is important because as many as one in every four women who have breast cancer experiences depression as well.1 SSRIs are widely prescribed for these patients—not only as treatment for their depressive disorder but also because the drugs have been shown to offer some relief from hot flashes.
In this cohort study from Ontario, where health care is delivered in a centralized fashion, Kelly and colleagues assessed the survival of breast cancer survivors 66 years and older who were treated with both tamoxifen and an SSRI, or with both tamoxifen and venlafaxine (which inhibits reuptake of both serotonin and norepinephrine).
The median age of the 2,430 eligible and evaluable women at the time of tamoxifen initiation was 74 years. These women began using tamoxifen between 1993 and 2005, with a median duration of use of 4 years. Paroxetine was the most commonly used SSRI in this study (25.9%), followed by sertraline (Zoloft, 22.3%), citalopram (Celexa, 19.2%), venlafaxine (Effexor, 15.0%), fluoxetine (Prozac, Sarafem, 10.4%), and fluvoxamine (Luvox, 7.2%).
Neither duloxetine (Cymbalta) nor escitalopram (Lexapro) were included in this analysis.
By the end of follow-up, 1,074 women (44.2%) in the cohort had died, 374 of them from breast cancer.
When taken with tamoxifen, paroxetine increased breast cancer mortality
Concomitant use of paroxetine and tamoxifen was associated with a significantly increased risk of death from breast cancer. In addition, as the proportion of concomitant use of the drugs increased to 25%, 50%, and 75% of total tamoxifen use, the adjusted risk of death increased 24%, 54%, and 91%, respectively. Among women taking tamoxifen, concomitant use of other SSRIs or venlafaxine was not associated with an increased risk of death.
Based on their data, the investigators determined that use of paroxetine during 41% of tamoxifen treatment (the median overlap observed in this study) would result in one additional breast cancer death at 5 years for every 19.7 women treated in this fashion. If paroxetine were used for the entire duration of tamoxifen treatment—an overlap of 100%—an additional death would occur for every 6.9 women treated.
The authors also noted that fluoxetine is a “strong inhibitor” of tamoxifen, although it was not associated with an increased risk of breast cancer death in this trial. One reason may be the small number of women who took tamoxifen and fluoxetine concomitantly in this study.
“Our results should not be viewed as evidence that fluoxetine can be safely used in combination with tamoxifen,” Kelly and coworkers write. “Similarly, we cannot exclude the possibility that insufficient sample size explains the nonsignificant mortality results with other SSRIs.”
Because fluoxetine is known to strongly inhibit CYP2D6, other antidepressants are more prudent choices for tamoxifen users.
In addition, switch any tamoxifen user who is taking paroxetine to an alternative antidepressant. Venlafaxine may be a sound choice in this setting, given the data indicating its efficacy as a nonhormonal treatment for vasomotor symptoms in breast cancer survivors.—ANDREW M. KAUNITZ, MD
Tamoxifen is widely used by women who have receptor-positive breast cancer to lower their risk of recurrence. Tamoxifen is a prodrug converted by the hepatic cytochrome P450 enzyme system (particularly isoenzyme CYP2D6) to active metabolites, which have much higher affinity for the estrogen receptor than the parent prodrug has. Selective serotonin reuptake inhibitors (SSRIs) inhibit CYP2D6 to variable degrees, with paroxetine thought to be the most potent inhibitor.
The fact that SSRIs inhibit CYP2D6 is important because as many as one in every four women who have breast cancer experiences depression as well.1 SSRIs are widely prescribed for these patients—not only as treatment for their depressive disorder but also because the drugs have been shown to offer some relief from hot flashes.
In this cohort study from Ontario, where health care is delivered in a centralized fashion, Kelly and colleagues assessed the survival of breast cancer survivors 66 years and older who were treated with both tamoxifen and an SSRI, or with both tamoxifen and venlafaxine (which inhibits reuptake of both serotonin and norepinephrine).
The median age of the 2,430 eligible and evaluable women at the time of tamoxifen initiation was 74 years. These women began using tamoxifen between 1993 and 2005, with a median duration of use of 4 years. Paroxetine was the most commonly used SSRI in this study (25.9%), followed by sertraline (Zoloft, 22.3%), citalopram (Celexa, 19.2%), venlafaxine (Effexor, 15.0%), fluoxetine (Prozac, Sarafem, 10.4%), and fluvoxamine (Luvox, 7.2%).
Neither duloxetine (Cymbalta) nor escitalopram (Lexapro) were included in this analysis.
By the end of follow-up, 1,074 women (44.2%) in the cohort had died, 374 of them from breast cancer.
When taken with tamoxifen, paroxetine increased breast cancer mortality
Concomitant use of paroxetine and tamoxifen was associated with a significantly increased risk of death from breast cancer. In addition, as the proportion of concomitant use of the drugs increased to 25%, 50%, and 75% of total tamoxifen use, the adjusted risk of death increased 24%, 54%, and 91%, respectively. Among women taking tamoxifen, concomitant use of other SSRIs or venlafaxine was not associated with an increased risk of death.
Based on their data, the investigators determined that use of paroxetine during 41% of tamoxifen treatment (the median overlap observed in this study) would result in one additional breast cancer death at 5 years for every 19.7 women treated in this fashion. If paroxetine were used for the entire duration of tamoxifen treatment—an overlap of 100%—an additional death would occur for every 6.9 women treated.
The authors also noted that fluoxetine is a “strong inhibitor” of tamoxifen, although it was not associated with an increased risk of breast cancer death in this trial. One reason may be the small number of women who took tamoxifen and fluoxetine concomitantly in this study.
“Our results should not be viewed as evidence that fluoxetine can be safely used in combination with tamoxifen,” Kelly and coworkers write. “Similarly, we cannot exclude the possibility that insufficient sample size explains the nonsignificant mortality results with other SSRIs.”
Because fluoxetine is known to strongly inhibit CYP2D6, other antidepressants are more prudent choices for tamoxifen users.
In addition, switch any tamoxifen user who is taking paroxetine to an alternative antidepressant. Venlafaxine may be a sound choice in this setting, given the data indicating its efficacy as a nonhormonal treatment for vasomotor symptoms in breast cancer survivors.—ANDREW M. KAUNITZ, MD
Reference
1. Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30(2):112-126.
Reference
1. Fann JR, Thomas-Rich AM, Katon WJ, et al. Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry. 2008;30(2):112-126.
OBG Management ©2010 Dowden Health Media
Is new-onset breast tenderness after the start of hormone therapy a sign of elevated cancer risk?
Breast tenderness is a common side effect of postmenopausal hormone therapy (HT); generally, it is dose-dependent. In this study by Crandall and colleagues, investigators assessed self-reported breast tenderness at the beginning of the WHI and after 12 months of HT, exploring any association between that tenderness and the risk of breast cancer. Here is what they found:
- Among women who reported no breast tenderness at study entry, the incidence of breast tenderness after 12 months was three times higher in those assigned to HT than in those assigned to placebo (36.1% vs 11.8%; P <.001).
- Women who reported the onset of breast tenderness after starting HT were older and more likely to be black or Hispanic than were women who did not.
- More than 75% of women who reported new breast tenderness (most often rated as mild) had been assigned to HT.
- Women taking HT who reported new breast tenderness had a risk of breast cancer 48% higher than those who did not report this complaint (P=.02).
- New-onset breast tenderness in women assigned to the placebo group was not associated with an elevated risk of breast cancer.
Does breast tenderness reflect an increase in cell proliferation?
Earlier studies have linked breast tenderness in women taking CEE plus MPA to high mammographic density, an independent risk factor for breast cancer. They have also established a link between estrogen-progestin therapy and breast cell proliferation. Therefore, as Crandall and colleagues observe, “breast discomfort may be a clinical manifestation of increased proliferation that is manifest radiographically as increased breast density.”
Keep in mind that the original WHI estrogen-progestin trial demonstrated that CEE plus MPA is associated with eight additional cases of breast cancer per 10,000 woman-years—a modest increase in risk. Although the study by Crandall and colleagues suggests that new-onset breast tenderness further increases the risk of breast cancer among users of estrogen-progestin therapy, the absolute magnitude of this increased risk is modest.
New-onset breast tenderness has a sensitivity and specificity similar to those of the Gail model for predicting the risk of invasive breast cancer. In this study, based on a mean follow-up of 5.6 years, the sensitivity and specificity of new-onset breast tenderness were 41% and 64%, respectively, and the positive predictive value was 2.7%. In comparison, using a threshold risk of breast cancer of 1.67% over 5 years, the Gail model has sensitivity, specificity, and a positive predictive value of 44%, 66%, and 6.6%, respectively.
Counsel women who are considering or continuing estrogen-progestin hormone therapy (HT) about its risks (including a modestly increased risk of breast cancer) and benefits. Also counsel them that breast tenderness commonly occurs after initiation of HT.
During follow-up visits, any woman reporting breast tenderness should be advised that this side effect suggests that her risk of breast cancer may be higher than that of women who use HT but do not experience breast tenderness. This information may factor into decisions about HT continuation and dosage, as well as strategies for breast-cancer surveillance.—ANDREW M. KAUNITZ, MD
Breast tenderness is a common side effect of postmenopausal hormone therapy (HT); generally, it is dose-dependent. In this study by Crandall and colleagues, investigators assessed self-reported breast tenderness at the beginning of the WHI and after 12 months of HT, exploring any association between that tenderness and the risk of breast cancer. Here is what they found:
- Among women who reported no breast tenderness at study entry, the incidence of breast tenderness after 12 months was three times higher in those assigned to HT than in those assigned to placebo (36.1% vs 11.8%; P <.001).
- Women who reported the onset of breast tenderness after starting HT were older and more likely to be black or Hispanic than were women who did not.
- More than 75% of women who reported new breast tenderness (most often rated as mild) had been assigned to HT.
- Women taking HT who reported new breast tenderness had a risk of breast cancer 48% higher than those who did not report this complaint (P=.02).
- New-onset breast tenderness in women assigned to the placebo group was not associated with an elevated risk of breast cancer.
Does breast tenderness reflect an increase in cell proliferation?
Earlier studies have linked breast tenderness in women taking CEE plus MPA to high mammographic density, an independent risk factor for breast cancer. They have also established a link between estrogen-progestin therapy and breast cell proliferation. Therefore, as Crandall and colleagues observe, “breast discomfort may be a clinical manifestation of increased proliferation that is manifest radiographically as increased breast density.”
Keep in mind that the original WHI estrogen-progestin trial demonstrated that CEE plus MPA is associated with eight additional cases of breast cancer per 10,000 woman-years—a modest increase in risk. Although the study by Crandall and colleagues suggests that new-onset breast tenderness further increases the risk of breast cancer among users of estrogen-progestin therapy, the absolute magnitude of this increased risk is modest.
New-onset breast tenderness has a sensitivity and specificity similar to those of the Gail model for predicting the risk of invasive breast cancer. In this study, based on a mean follow-up of 5.6 years, the sensitivity and specificity of new-onset breast tenderness were 41% and 64%, respectively, and the positive predictive value was 2.7%. In comparison, using a threshold risk of breast cancer of 1.67% over 5 years, the Gail model has sensitivity, specificity, and a positive predictive value of 44%, 66%, and 6.6%, respectively.
Counsel women who are considering or continuing estrogen-progestin hormone therapy (HT) about its risks (including a modestly increased risk of breast cancer) and benefits. Also counsel them that breast tenderness commonly occurs after initiation of HT.
During follow-up visits, any woman reporting breast tenderness should be advised that this side effect suggests that her risk of breast cancer may be higher than that of women who use HT but do not experience breast tenderness. This information may factor into decisions about HT continuation and dosage, as well as strategies for breast-cancer surveillance.—ANDREW M. KAUNITZ, MD
Breast tenderness is a common side effect of postmenopausal hormone therapy (HT); generally, it is dose-dependent. In this study by Crandall and colleagues, investigators assessed self-reported breast tenderness at the beginning of the WHI and after 12 months of HT, exploring any association between that tenderness and the risk of breast cancer. Here is what they found:
- Among women who reported no breast tenderness at study entry, the incidence of breast tenderness after 12 months was three times higher in those assigned to HT than in those assigned to placebo (36.1% vs 11.8%; P <.001).
- Women who reported the onset of breast tenderness after starting HT were older and more likely to be black or Hispanic than were women who did not.
- More than 75% of women who reported new breast tenderness (most often rated as mild) had been assigned to HT.
- Women taking HT who reported new breast tenderness had a risk of breast cancer 48% higher than those who did not report this complaint (P=.02).
- New-onset breast tenderness in women assigned to the placebo group was not associated with an elevated risk of breast cancer.
Does breast tenderness reflect an increase in cell proliferation?
Earlier studies have linked breast tenderness in women taking CEE plus MPA to high mammographic density, an independent risk factor for breast cancer. They have also established a link between estrogen-progestin therapy and breast cell proliferation. Therefore, as Crandall and colleagues observe, “breast discomfort may be a clinical manifestation of increased proliferation that is manifest radiographically as increased breast density.”
Keep in mind that the original WHI estrogen-progestin trial demonstrated that CEE plus MPA is associated with eight additional cases of breast cancer per 10,000 woman-years—a modest increase in risk. Although the study by Crandall and colleagues suggests that new-onset breast tenderness further increases the risk of breast cancer among users of estrogen-progestin therapy, the absolute magnitude of this increased risk is modest.
New-onset breast tenderness has a sensitivity and specificity similar to those of the Gail model for predicting the risk of invasive breast cancer. In this study, based on a mean follow-up of 5.6 years, the sensitivity and specificity of new-onset breast tenderness were 41% and 64%, respectively, and the positive predictive value was 2.7%. In comparison, using a threshold risk of breast cancer of 1.67% over 5 years, the Gail model has sensitivity, specificity, and a positive predictive value of 44%, 66%, and 6.6%, respectively.
Counsel women who are considering or continuing estrogen-progestin hormone therapy (HT) about its risks (including a modestly increased risk of breast cancer) and benefits. Also counsel them that breast tenderness commonly occurs after initiation of HT.
During follow-up visits, any woman reporting breast tenderness should be advised that this side effect suggests that her risk of breast cancer may be higher than that of women who use HT but do not experience breast tenderness. This information may factor into decisions about HT continuation and dosage, as well as strategies for breast-cancer surveillance.—ANDREW M. KAUNITZ, MD



