User login
Breast and Uterine Cancer: Screening Guidelines, Genetic Testing, and Mortality Trends
Breast and Uterine Cancer: Screening Guidelines, Genetic Testing, and Mortality Trends
Click to view more from Cancer Data Trends 2025.
- Shepherd-Banigan M, Zullig LL, Berkowitz TSZ, et al. Improving Cancer Care
for Women Seeking Services in the Veterans Health Administration Through the
Breast and Gynecological Oncology System of Excellence. Mil Med. 2024:usae447.
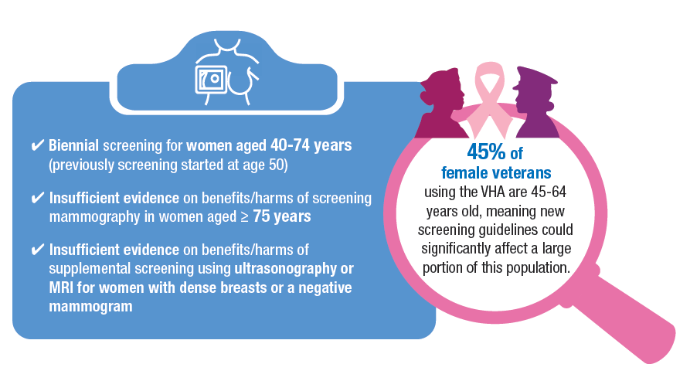
doi:10.1093/milmed/usae447 - US Preventive Services Task Force, Nicholson WK, Silverstein M, et al. Screening
for Breast Cancer: US Preventive Services Task Force Recommendation Statement.
JAMA. 2024;331(22):1918-1930. doi:10.1001/jama.2024.5534 - VA announces steps to increase life-saving screening, access to benefits for
Veterans with cancer. VA News. March 8, 2024. Accessed January 14, 2025. https://
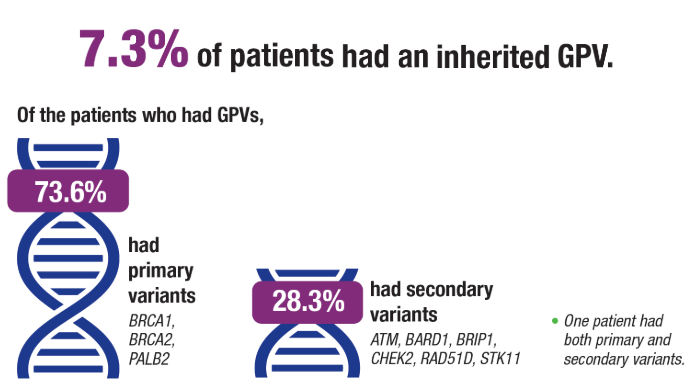
news.va.gov/press-room/va-expands-health-care-benefits-veterans-cancer/ - Rezoug Z, Totten SP, Szlachtycz D, et al. Universal Genetic Testing for Newly
Diagnosed Invasive Breast Cancer. JAMA Netw Open. 2024;7(9):e2431427.
doi:10.1001/jamanetworkopen.2024.31427 - National Institutes of Health. National Cancer Institute. Surveillance, Epidemiology,
and End Results Program. Cancer Stat Facts: Uterine Cancer. Accessed January 14,
2025. https://seer.cancer.gov/statfacts/html/corp.html - Clarke MA, Devesa SS, Hammer A, Wentzensen N. Racial and Ethnic Differences in
Hysterectomy-Corrected Uterine Corpus Cancer Mortality by Stage and Histologic
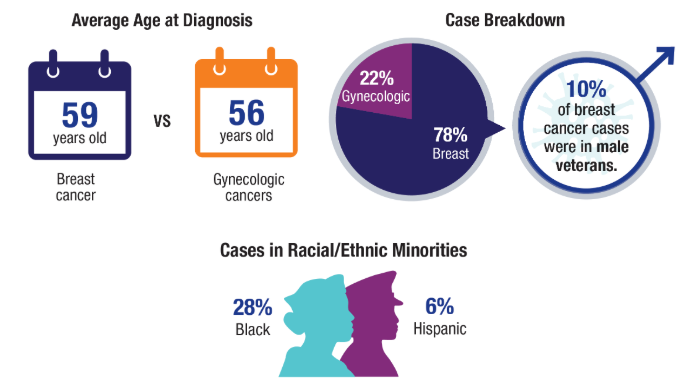
Subtype. JAMA Oncol. 2022;8(6):895-903. doi:10.1001/jamaoncol.2022.0009 - Moss HA, Rasmussen, KM, Patil, V, et al. Demographic Characteristics of Veterans
Diagnosed With Breast and Gynecologic Cancers: A Comparative Analysis With the
General Population. Abstract presented at: Annual Meeting of the Association of
VA Hematology/Oncology (AVAHO); September 29–October 1, 2023; Chicago, IL.
Abstract 47. - Breland JY, Frayne SM, Saechao F, Gujral K, Vashi AA, Shaw JG, Gray KM, Illarmo SS,
Urech T, Grant N, Berg E, Offer C, Veldanda S, Schoemaker L, Dalton AL, Esmaeili
A, Phibbs CS, Hayes PM, Haskell S. Sourcebook: Women Veterans in the Veterans
Health Administration. Volume 5: Longitudinal Trends in Sociodemographics and
Utilization, Including Type, Modality, and Source of Care. Women’s Health Evaluation
Initiative, Office of Women’s Health, Veterans Health Administration, Department of
Veterans Affairs, Washington DC. June 2024. - NCCN: National Comprehensive Cancer Network. Breast Cancer Screening and
Diagnosis. V2.2024 April 9, 2024. Accessed January 14, 2025. https://www.nccn.
org/professionals/physician_gls/pdf/breast-screening.pdf - ACS: American Cancer Society. Breast Cancer Early Detection and Diagnosis.
Revised December 19, 2023. Accessed January 14, 2025. https://www.cancer.org/
cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancersociety-
recommendations-for-the-early-detection-of-breast-cancer.html - Somasegar S, Bashi A, Lang SM, et al. Trends in Uterine Cancer Mortality
in the United States: A 50-Year Population-Based Analysis. Obstet Gynecol.
2023;142(4):978-986. doi:10.1097/AOG.0000000000005321
Click to view more from Cancer Data Trends 2025.
Click to view more from Cancer Data Trends 2025.
- Shepherd-Banigan M, Zullig LL, Berkowitz TSZ, et al. Improving Cancer Care
for Women Seeking Services in the Veterans Health Administration Through the
Breast and Gynecological Oncology System of Excellence. Mil Med. 2024:usae447.
doi:10.1093/milmed/usae447 - US Preventive Services Task Force, Nicholson WK, Silverstein M, et al. Screening
for Breast Cancer: US Preventive Services Task Force Recommendation Statement.
JAMA. 2024;331(22):1918-1930. doi:10.1001/jama.2024.5534 - VA announces steps to increase life-saving screening, access to benefits for
Veterans with cancer. VA News. March 8, 2024. Accessed January 14, 2025. https://
news.va.gov/press-room/va-expands-health-care-benefits-veterans-cancer/ - Rezoug Z, Totten SP, Szlachtycz D, et al. Universal Genetic Testing for Newly
Diagnosed Invasive Breast Cancer. JAMA Netw Open. 2024;7(9):e2431427.
doi:10.1001/jamanetworkopen.2024.31427 - National Institutes of Health. National Cancer Institute. Surveillance, Epidemiology,
and End Results Program. Cancer Stat Facts: Uterine Cancer. Accessed January 14,
2025. https://seer.cancer.gov/statfacts/html/corp.html - Clarke MA, Devesa SS, Hammer A, Wentzensen N. Racial and Ethnic Differences in
Hysterectomy-Corrected Uterine Corpus Cancer Mortality by Stage and Histologic
Subtype. JAMA Oncol. 2022;8(6):895-903. doi:10.1001/jamaoncol.2022.0009 - Moss HA, Rasmussen, KM, Patil, V, et al. Demographic Characteristics of Veterans
Diagnosed With Breast and Gynecologic Cancers: A Comparative Analysis With the
General Population. Abstract presented at: Annual Meeting of the Association of
VA Hematology/Oncology (AVAHO); September 29–October 1, 2023; Chicago, IL.
Abstract 47. - Breland JY, Frayne SM, Saechao F, Gujral K, Vashi AA, Shaw JG, Gray KM, Illarmo SS,
Urech T, Grant N, Berg E, Offer C, Veldanda S, Schoemaker L, Dalton AL, Esmaeili
A, Phibbs CS, Hayes PM, Haskell S. Sourcebook: Women Veterans in the Veterans
Health Administration. Volume 5: Longitudinal Trends in Sociodemographics and
Utilization, Including Type, Modality, and Source of Care. Women’s Health Evaluation
Initiative, Office of Women’s Health, Veterans Health Administration, Department of
Veterans Affairs, Washington DC. June 2024. - NCCN: National Comprehensive Cancer Network. Breast Cancer Screening and
Diagnosis. V2.2024 April 9, 2024. Accessed January 14, 2025. https://www.nccn.
org/professionals/physician_gls/pdf/breast-screening.pdf - ACS: American Cancer Society. Breast Cancer Early Detection and Diagnosis.
Revised December 19, 2023. Accessed January 14, 2025. https://www.cancer.org/
cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancersociety-
recommendations-for-the-early-detection-of-breast-cancer.html - Somasegar S, Bashi A, Lang SM, et al. Trends in Uterine Cancer Mortality
in the United States: A 50-Year Population-Based Analysis. Obstet Gynecol.
2023;142(4):978-986. doi:10.1097/AOG.0000000000005321
- Shepherd-Banigan M, Zullig LL, Berkowitz TSZ, et al. Improving Cancer Care
for Women Seeking Services in the Veterans Health Administration Through the
Breast and Gynecological Oncology System of Excellence. Mil Med. 2024:usae447.
doi:10.1093/milmed/usae447 - US Preventive Services Task Force, Nicholson WK, Silverstein M, et al. Screening
for Breast Cancer: US Preventive Services Task Force Recommendation Statement.
JAMA. 2024;331(22):1918-1930. doi:10.1001/jama.2024.5534 - VA announces steps to increase life-saving screening, access to benefits for
Veterans with cancer. VA News. March 8, 2024. Accessed January 14, 2025. https://
news.va.gov/press-room/va-expands-health-care-benefits-veterans-cancer/ - Rezoug Z, Totten SP, Szlachtycz D, et al. Universal Genetic Testing for Newly
Diagnosed Invasive Breast Cancer. JAMA Netw Open. 2024;7(9):e2431427.
doi:10.1001/jamanetworkopen.2024.31427 - National Institutes of Health. National Cancer Institute. Surveillance, Epidemiology,
and End Results Program. Cancer Stat Facts: Uterine Cancer. Accessed January 14,
2025. https://seer.cancer.gov/statfacts/html/corp.html - Clarke MA, Devesa SS, Hammer A, Wentzensen N. Racial and Ethnic Differences in
Hysterectomy-Corrected Uterine Corpus Cancer Mortality by Stage and Histologic
Subtype. JAMA Oncol. 2022;8(6):895-903. doi:10.1001/jamaoncol.2022.0009 - Moss HA, Rasmussen, KM, Patil, V, et al. Demographic Characteristics of Veterans
Diagnosed With Breast and Gynecologic Cancers: A Comparative Analysis With the
General Population. Abstract presented at: Annual Meeting of the Association of
VA Hematology/Oncology (AVAHO); September 29–October 1, 2023; Chicago, IL.
Abstract 47. - Breland JY, Frayne SM, Saechao F, Gujral K, Vashi AA, Shaw JG, Gray KM, Illarmo SS,
Urech T, Grant N, Berg E, Offer C, Veldanda S, Schoemaker L, Dalton AL, Esmaeili
A, Phibbs CS, Hayes PM, Haskell S. Sourcebook: Women Veterans in the Veterans
Health Administration. Volume 5: Longitudinal Trends in Sociodemographics and
Utilization, Including Type, Modality, and Source of Care. Women’s Health Evaluation
Initiative, Office of Women’s Health, Veterans Health Administration, Department of
Veterans Affairs, Washington DC. June 2024. - NCCN: National Comprehensive Cancer Network. Breast Cancer Screening and
Diagnosis. V2.2024 April 9, 2024. Accessed January 14, 2025. https://www.nccn.
org/professionals/physician_gls/pdf/breast-screening.pdf - ACS: American Cancer Society. Breast Cancer Early Detection and Diagnosis.
Revised December 19, 2023. Accessed January 14, 2025. https://www.cancer.org/
cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancersociety-
recommendations-for-the-early-detection-of-breast-cancer.html - Somasegar S, Bashi A, Lang SM, et al. Trends in Uterine Cancer Mortality
in the United States: A 50-Year Population-Based Analysis. Obstet Gynecol.
2023;142(4):978-986. doi:10.1097/AOG.0000000000005321
Breast and Uterine Cancer: Screening Guidelines, Genetic Testing, and Mortality Trends
Breast and Uterine Cancer: Screening Guidelines, Genetic Testing, and Mortality Trends
MRI-Invisible Prostate Lesions: Are They Dangerous?
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
MRI-invisible prostate lesions. It sounds like the stuff of science fiction and fantasy, a creation from the minds of H.G. Wells, who wrote The Invisible Man, or J.K. Rowling, who authored the Harry Potter series.
But MRI-invisible prostate lesions are real. And what these lesions may, or may not, indicate is the subject of intense debate.
MRI plays an increasingly important role in detecting and diagnosing prostate cancer, staging prostate cancer as well as monitoring disease progression. However, on occasion, a puzzling phenomenon arises. Certain prostate lesions that appear when pathologists examine biopsied tissue samples under a microscope are not visible on MRI. The prostate tissue will, instead, appear normal to a radiologist’s eye.
Some experts believe these MRI-invisible lesions are nothing to worry about.
If the clinician can’t see the cancer on MRI, then it simply isn’t a threat, according to Mark Emberton, MD, a pioneer in prostate MRIs and director of interventional oncology at University College London, England.
Laurence Klotz, MD, of the University of Toronto, Ontario, Canada, agreed, noting that “invisible cancers are clinically insignificant and don’t require systematic biopsies.”
Emberton and Klotz compared MRI-invisible lesions to grade group 1 prostate cancer (Gleason score ≤ 6) — the least aggressive category that indicates the cancer that is not likely to spread or kill. For patients on active surveillance, those with MRI-invisible cancers do drastically better than those with visible cancers, Klotz explained.
But other experts in the field are skeptical that MRI-invisible lesions are truly innocuous.
Although statistically an MRI-visible prostate lesion indicates a more aggressive tumor, that is not always the case for every individual, said Brian Helfand, MD, PhD, chief of urology at NorthShore University Health System, Evanston, Illinois.
MRIs can lead to false negatives in about 10%-20% of patients who have clinically significant prostate cancer, though estimates vary.
In one analysis, 16% of men with no suspicious lesions on MRI had clinically significant prostate cancer identified after undergoing a systematic biopsy. Another analysis found that about 35% of MRI-invisible prostate cancers identified via biopsy were clinically significant.
Other studies, however, have indicated that negative MRI results accurately indicate patients at low risk of developing clinically significant cancers. A recent JAMA Oncology analysis, for instance, found that only seven of 233 men (3%) with negative MRI results at baseline who completed 3 years of monitoring were diagnosed with clinically significant prostate cancer.
When a patient has an MRI-invisible prostate tumor, there are a couple of reasons the MRI may not be picking it up, said urologic oncologist Alexander Putnam Cole, MD, assistant professor of surgery, Harvard Medical School, Boston, Massachusetts. “One is that the cancer is aggressive but just very small,” said Cole.
“Another possibility is that the cancer looks very similar to background prostate tissue, which is something that you might expect if you think about more of a low-grade cancer,” he explained.
The experience level of the radiologist interpreting the MRI can also play into the accuracy of the reading.
But Cole agreed that “in general, MRI visibility is associated with molecular and histologic features of progression and aggressiveness and non-visible cancers are less likely to have aggressive features.”
The genomic profiles of MRI-visible and -invisible cancers bear this out.
According to Todd Morgan, MD, chief of urologic oncology at Michigan Medicine, University of Michigan, Ann Arbor, the gene expression in visible disease tends to be linked to more aggressive prostate tumors whereas gene expression in invisible disease does not.
In one analysis, for instance, researchers found that four genes — PHYHD1, CENPF, ALDH2, and GDF15 — associated with worse progression-free survival and metastasis-free survival in prostate cancer also predicted MRI visibility.
“Genes that are associated with visibility are essentially the same genes that are associated with aggressive cancers,” Klotz said.
Next Steps After Negative MRI Result
What do MRI-invisible lesions mean for patient care? If, for instance, a patient has elevated PSA levels but a normal MRI, is a targeted or systematic biopsy warranted?
The overarching message, according to Klotz, is that “you don’t need to find them.” Klotz noted, however, that patients with a negative MRI result should still be followed with periodic repeat imaging.
Several trials support this approach of using MRI to decide who needs a biopsy and delaying a biopsy in men with normal MRIs.
The recent JAMA Oncology analysis found that, among men with negative MRI results, 86% avoided a biopsy over 3 years, with clinically significant prostate cancer detected in only 4% of men across the study period — four in the initial diagnostic phase and seven in the 3-year monitoring phase. However, during the initial diagnostic phase, more than half the men with positive MRI findings had clinically significant prostate cancer detected.
Another recent study found that patients with negative MRI results were much less likely to upgrade to higher Gleason scores over time. Among 522 patients who underwent a systematic and targeted biopsy within 18 months of their grade group 1 designation, 9.2% with negative MRI findings had tumors reclassified as grade group 2 or higher vs 27% with positive MRI findings, and 2.3% with negative MRI findings had tumors reclassified as grade group 3 or higher vs 7.8% with positive MRI findings.
These data suggest that men with grade group 1 cancer and negative MRI result “may be able to avoid confirmatory biopsies until a routine surveillance biopsy in 2-3 years,” according to study author Christian Pavlovich, MD, professor of urologic oncology at the Johns Hopkins University School of Medicine, Baltimore.
Cole used MRI findings to triage who gets a biopsy. When a biopsy is warranted, “I usually recommend adding in some systematic sampling of the other side to assess for nonvisible cancers,” he noted.
Sampling prostate tissue outside the target area “adds maybe 1-2 minutes to the procedure and doesn’t drastically increase the morbidity or risks,” Cole said. It also can help “confirm there is cancer in the MRI target and also confirm there is no cancer in the nonvisible areas.”
According to Klotz, if imaging demonstrates progression, patients should receive a biopsy — in most cases, a targeted biopsy only. And, Klotz noted, skipping routine prostate biopsies in men with negative MRI results can save thousands of men from these procedures, which carry risks for infections and sepsis.
Looking beyond Gleason scores for risk prediction, MRI “visibility is a very powerful risk stratifier,” he said.
A version of this article appeared on Medscape.com.
Vulvar and Vaginal Melanoma: A Rare but Important Diagnosis
Cutaneous melanoma is a type of skin cancer typically associated with significant ultraviolet radiation exposure. Melanoma arises from melanocytes, cells found within the lower portion of the epidermis that make the pigment melanin.
While much less common than squamous cell carcinoma or basal cell carcinoma, melanoma is responsible for most deaths from skin cancer. In 2024, there will be more than 100,000 new cases of melanoma and over 8,000 melanoma-related deaths.1 If localized at the time of diagnosis, survival rates are excellent. Cutaneous melanomas are more common in those with fair complexions or who have had long periods of exposure to natural or artificial sunlight.
Melanoma can also occur in mucous membranes. Mucosal melanoma is much less common than cutaneous melanoma and accounts for only a very small percentage of all new melanoma diagnoses. Unlike their cutaneous counterparts, risk factors for mucosal melanomas have yet to be identified. Although there is some disagreement on whether vulvar melanomas represent cutaneous or mucous melanomas, vulvovaginal melanomas have historically been considered to be mucosal melanomas.
Vulvovaginal melanomas are characterized by a high mortality rate, diagnostic challenges, and lack of awareness, making early detection and intervention crucial to improving patient outcomes. The 5-year overall survival rate for vulvar melanoma is 36% and for vaginal melanoma ranges between 5% and 25%.2 Survival rates for vulvovaginal melanomas are lower than for other types of vulvar cancers (72%) or for cutaneous melanomas (72%-81%).2
Racial disparities in survival rates for mucosal and cutaneous melanomas were highlighted in a retrospective study using the Surveillance Epidemiology and End Results (SEER) database. Although the number of Black patients included was small, the median overall survival in that population was less than that in non-Black patients with vulvovaginal melanoma (16 vs. 39 months). Similar findings were noted in Black patients with cutaneous melanoma, compared with non-Black patients (median overall survival, 124 vs 319 months).3
One of the most significant obstacles in the diagnosis of vulvar and vaginal melanoma is its rarity. Both patients and clinicians alike may fail to recognize early warning signs. In a world where skin cancer is heavily publicized, melanoma in the genital area is not as frequently discussed or understood. Postmenopausal patients may have less regular gynecologic care, and unless they present with specific symptoms prompting an exam, melanomas can grow undetected, progressing to more advanced stages before they are discovered.
The median age of patients diagnosed with vulvar and vaginal melanomas is 67-68.4,5 Symptoms can be subtle and nonspecific. Women with vulvar melanoma may experience symptoms that are similar to other vulvar cancers including pruritus, irritation, pain, bleeding, or a new or growing mass. While vaginal melanoma can be asymptomatic, patients frequently present with vaginal bleeding, discharge, and/or pain (including dyspareunia).
Vulvovaginal melanomas may present differently than cutaneous melanomas. Vulvar melanomas are often pigmented and frequently present as ulcerated lesions. In some cases, though, they appear amelanotic (lacking pigment), making them even harder to identify. The ABCDEs of skin cancer (asymmetry, border, color, diameter, evolving) should be applied to these lesions. Change in the size, shape, or pigment of preexisting melanosis (areas of hyperpigmentation caused by increased melanin), should raise concern for possible malignant transformation.
Most vaginal melanomas occur within the distal third of the vagina, frequently along the anterior vaginal wall.6 They can be polypoid or nodular in appearance and may be ulcerated. While biopsy of any suspicious, enlarging/changing, or symptomatic lesion should be performed, it may be prudent to pause prior to biopsy of a vaginal lesion depending on its appearance. Although rare, gestational trophoblastic neoplasia (GTN) can present with vaginal metastases, and these lesions are frequently very vascular and pose a high bleeding risk if biopsied. They may look dark blue or black. If there is any concern for metastatic GTN on vaginal exam, a beta-hCG level should be obtained prior to biopsy.
Treatment of vulvovaginal melanoma may include surgical excision, systemic therapy, radiation therapy, or a combination of treatments. There is growing use of immunotherapy that mirrors cutaneous melanoma therapy.
Vulvar and vaginal melanoma represent a rare yet serious health issue for women and their impact on public health should not be underestimated. Vulvovaginal melanoma often goes unrecognized until it has reached an advanced stage. Increased awareness about these rare forms of melanoma among both patients and healthcare professionals is vital to improve early detection and treatment outcomes. With greater attention to this disease, we can strive for better diagnostic methods, more effective treatments, and ultimately, a reduction in mortality rates associated with vulvar and vaginal melanoma.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. National Cancer Institute. Cancer Stat Facts: Melanoma of the skin. 2024 Dec 2. Available from: https://seer.cancer.gov/statfacts/html/melan.html.
2. Piura B. Lancet Oncol. 2008 Oct;9(10):973-81. .
3. Mert I et al. Int J Gynecol Cancer. 2013;23(6):1118-25.
4. Wang D et al. Am J Cancer Res. 2020 Dec 1;10(12):4017-37.
5. Albert A et al. J Gynecol Oncol. 2020 Sep;31(5):e66.
Cutaneous melanoma is a type of skin cancer typically associated with significant ultraviolet radiation exposure. Melanoma arises from melanocytes, cells found within the lower portion of the epidermis that make the pigment melanin.
While much less common than squamous cell carcinoma or basal cell carcinoma, melanoma is responsible for most deaths from skin cancer. In 2024, there will be more than 100,000 new cases of melanoma and over 8,000 melanoma-related deaths.1 If localized at the time of diagnosis, survival rates are excellent. Cutaneous melanomas are more common in those with fair complexions or who have had long periods of exposure to natural or artificial sunlight.
Melanoma can also occur in mucous membranes. Mucosal melanoma is much less common than cutaneous melanoma and accounts for only a very small percentage of all new melanoma diagnoses. Unlike their cutaneous counterparts, risk factors for mucosal melanomas have yet to be identified. Although there is some disagreement on whether vulvar melanomas represent cutaneous or mucous melanomas, vulvovaginal melanomas have historically been considered to be mucosal melanomas.
Vulvovaginal melanomas are characterized by a high mortality rate, diagnostic challenges, and lack of awareness, making early detection and intervention crucial to improving patient outcomes. The 5-year overall survival rate for vulvar melanoma is 36% and for vaginal melanoma ranges between 5% and 25%.2 Survival rates for vulvovaginal melanomas are lower than for other types of vulvar cancers (72%) or for cutaneous melanomas (72%-81%).2
Racial disparities in survival rates for mucosal and cutaneous melanomas were highlighted in a retrospective study using the Surveillance Epidemiology and End Results (SEER) database. Although the number of Black patients included was small, the median overall survival in that population was less than that in non-Black patients with vulvovaginal melanoma (16 vs. 39 months). Similar findings were noted in Black patients with cutaneous melanoma, compared with non-Black patients (median overall survival, 124 vs 319 months).3
One of the most significant obstacles in the diagnosis of vulvar and vaginal melanoma is its rarity. Both patients and clinicians alike may fail to recognize early warning signs. In a world where skin cancer is heavily publicized, melanoma in the genital area is not as frequently discussed or understood. Postmenopausal patients may have less regular gynecologic care, and unless they present with specific symptoms prompting an exam, melanomas can grow undetected, progressing to more advanced stages before they are discovered.
The median age of patients diagnosed with vulvar and vaginal melanomas is 67-68.4,5 Symptoms can be subtle and nonspecific. Women with vulvar melanoma may experience symptoms that are similar to other vulvar cancers including pruritus, irritation, pain, bleeding, or a new or growing mass. While vaginal melanoma can be asymptomatic, patients frequently present with vaginal bleeding, discharge, and/or pain (including dyspareunia).
Vulvovaginal melanomas may present differently than cutaneous melanomas. Vulvar melanomas are often pigmented and frequently present as ulcerated lesions. In some cases, though, they appear amelanotic (lacking pigment), making them even harder to identify. The ABCDEs of skin cancer (asymmetry, border, color, diameter, evolving) should be applied to these lesions. Change in the size, shape, or pigment of preexisting melanosis (areas of hyperpigmentation caused by increased melanin), should raise concern for possible malignant transformation.
Most vaginal melanomas occur within the distal third of the vagina, frequently along the anterior vaginal wall.6 They can be polypoid or nodular in appearance and may be ulcerated. While biopsy of any suspicious, enlarging/changing, or symptomatic lesion should be performed, it may be prudent to pause prior to biopsy of a vaginal lesion depending on its appearance. Although rare, gestational trophoblastic neoplasia (GTN) can present with vaginal metastases, and these lesions are frequently very vascular and pose a high bleeding risk if biopsied. They may look dark blue or black. If there is any concern for metastatic GTN on vaginal exam, a beta-hCG level should be obtained prior to biopsy.
Treatment of vulvovaginal melanoma may include surgical excision, systemic therapy, radiation therapy, or a combination of treatments. There is growing use of immunotherapy that mirrors cutaneous melanoma therapy.
Vulvar and vaginal melanoma represent a rare yet serious health issue for women and their impact on public health should not be underestimated. Vulvovaginal melanoma often goes unrecognized until it has reached an advanced stage. Increased awareness about these rare forms of melanoma among both patients and healthcare professionals is vital to improve early detection and treatment outcomes. With greater attention to this disease, we can strive for better diagnostic methods, more effective treatments, and ultimately, a reduction in mortality rates associated with vulvar and vaginal melanoma.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. National Cancer Institute. Cancer Stat Facts: Melanoma of the skin. 2024 Dec 2. Available from: https://seer.cancer.gov/statfacts/html/melan.html.
2. Piura B. Lancet Oncol. 2008 Oct;9(10):973-81. .
3. Mert I et al. Int J Gynecol Cancer. 2013;23(6):1118-25.
4. Wang D et al. Am J Cancer Res. 2020 Dec 1;10(12):4017-37.
5. Albert A et al. J Gynecol Oncol. 2020 Sep;31(5):e66.
Cutaneous melanoma is a type of skin cancer typically associated with significant ultraviolet radiation exposure. Melanoma arises from melanocytes, cells found within the lower portion of the epidermis that make the pigment melanin.
While much less common than squamous cell carcinoma or basal cell carcinoma, melanoma is responsible for most deaths from skin cancer. In 2024, there will be more than 100,000 new cases of melanoma and over 8,000 melanoma-related deaths.1 If localized at the time of diagnosis, survival rates are excellent. Cutaneous melanomas are more common in those with fair complexions or who have had long periods of exposure to natural or artificial sunlight.
Melanoma can also occur in mucous membranes. Mucosal melanoma is much less common than cutaneous melanoma and accounts for only a very small percentage of all new melanoma diagnoses. Unlike their cutaneous counterparts, risk factors for mucosal melanomas have yet to be identified. Although there is some disagreement on whether vulvar melanomas represent cutaneous or mucous melanomas, vulvovaginal melanomas have historically been considered to be mucosal melanomas.
Vulvovaginal melanomas are characterized by a high mortality rate, diagnostic challenges, and lack of awareness, making early detection and intervention crucial to improving patient outcomes. The 5-year overall survival rate for vulvar melanoma is 36% and for vaginal melanoma ranges between 5% and 25%.2 Survival rates for vulvovaginal melanomas are lower than for other types of vulvar cancers (72%) or for cutaneous melanomas (72%-81%).2
Racial disparities in survival rates for mucosal and cutaneous melanomas were highlighted in a retrospective study using the Surveillance Epidemiology and End Results (SEER) database. Although the number of Black patients included was small, the median overall survival in that population was less than that in non-Black patients with vulvovaginal melanoma (16 vs. 39 months). Similar findings were noted in Black patients with cutaneous melanoma, compared with non-Black patients (median overall survival, 124 vs 319 months).3
One of the most significant obstacles in the diagnosis of vulvar and vaginal melanoma is its rarity. Both patients and clinicians alike may fail to recognize early warning signs. In a world where skin cancer is heavily publicized, melanoma in the genital area is not as frequently discussed or understood. Postmenopausal patients may have less regular gynecologic care, and unless they present with specific symptoms prompting an exam, melanomas can grow undetected, progressing to more advanced stages before they are discovered.
The median age of patients diagnosed with vulvar and vaginal melanomas is 67-68.4,5 Symptoms can be subtle and nonspecific. Women with vulvar melanoma may experience symptoms that are similar to other vulvar cancers including pruritus, irritation, pain, bleeding, or a new or growing mass. While vaginal melanoma can be asymptomatic, patients frequently present with vaginal bleeding, discharge, and/or pain (including dyspareunia).
Vulvovaginal melanomas may present differently than cutaneous melanomas. Vulvar melanomas are often pigmented and frequently present as ulcerated lesions. In some cases, though, they appear amelanotic (lacking pigment), making them even harder to identify. The ABCDEs of skin cancer (asymmetry, border, color, diameter, evolving) should be applied to these lesions. Change in the size, shape, or pigment of preexisting melanosis (areas of hyperpigmentation caused by increased melanin), should raise concern for possible malignant transformation.
Most vaginal melanomas occur within the distal third of the vagina, frequently along the anterior vaginal wall.6 They can be polypoid or nodular in appearance and may be ulcerated. While biopsy of any suspicious, enlarging/changing, or symptomatic lesion should be performed, it may be prudent to pause prior to biopsy of a vaginal lesion depending on its appearance. Although rare, gestational trophoblastic neoplasia (GTN) can present with vaginal metastases, and these lesions are frequently very vascular and pose a high bleeding risk if biopsied. They may look dark blue or black. If there is any concern for metastatic GTN on vaginal exam, a beta-hCG level should be obtained prior to biopsy.
Treatment of vulvovaginal melanoma may include surgical excision, systemic therapy, radiation therapy, or a combination of treatments. There is growing use of immunotherapy that mirrors cutaneous melanoma therapy.
Vulvar and vaginal melanoma represent a rare yet serious health issue for women and their impact on public health should not be underestimated. Vulvovaginal melanoma often goes unrecognized until it has reached an advanced stage. Increased awareness about these rare forms of melanoma among both patients and healthcare professionals is vital to improve early detection and treatment outcomes. With greater attention to this disease, we can strive for better diagnostic methods, more effective treatments, and ultimately, a reduction in mortality rates associated with vulvar and vaginal melanoma.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no conflicts of interest.
References
1. National Cancer Institute. Cancer Stat Facts: Melanoma of the skin. 2024 Dec 2. Available from: https://seer.cancer.gov/statfacts/html/melan.html.
2. Piura B. Lancet Oncol. 2008 Oct;9(10):973-81. .
3. Mert I et al. Int J Gynecol Cancer. 2013;23(6):1118-25.
4. Wang D et al. Am J Cancer Res. 2020 Dec 1;10(12):4017-37.
5. Albert A et al. J Gynecol Oncol. 2020 Sep;31(5):e66.
Eye Toxicities Are a Growing Concern With Certain ADCs
Such experts called for greater collaboration between oncologists and ophthalmologists, in interviews with Medscape Medical News.
ADCs combine a monoclonal antibody targeted at an antigen overexpressed on cancer cells with a toxic chemotherapy payload — the aim being to maximize the effectiveness of the drug against the tumor while minimizing the damage to healthy tissues and reducing systemic toxicity.
Yet trastuzumab duocarmazine (T-Duo), a third-generation human epidermal growth factor receptor 2 (HER2)–targeted ADC designed to treat HER2-positive breast cancer, was recently found to have a notable adverse effect in the TULIP trial of 437 patients.
As reported by Medscape Medical News, the drug was associated with a significant increase in progression-free survival over physician’s choice of therapy. However, 78% of patients in the ADC group experienced at least one treatment-emergent ocular toxicity adverse event vs 29.2% of those in the control group.
Moreover, grade 3 or high ocular toxicity events were reported by 21% of patients in the experimental group compared with none of those who received physician’s choice.
Ocular Toxicities Seen on Ocular Surface
Ocular toxicities with these drugs are “not necessarily a new thing,” said Joann J. Kang, MD, director, Cornea and Refractive Surgery, and associate professor of ophthalmology at Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, New York.
“But what we’re seeing with certain ADCs is a lot of ocular toxicity, especially on the ocular surface,” with the degree toxicity varying depending on the ADC in question. “It’s definitely a real concern.”
Kang noted that separate from T-Duo, certain ADCs already come with black box warnings for ocular toxicity, including:
- Belantamab mafodotin (Blenrep) — approved for relapsed or refractory multiple myeloma and carries a warning specifically for keratopathy.
- Tisotumab vedotin (Tivdak) — indicated for recurrent or metastatic cervical cancer and can cause changes in the corneal epithelium and conjunctiva.
- Mirvetuximab soravtansine (Elahere) — used to treat folate receptor (FR) alpha–positive ovarian, fallopian tube, and peritoneal cancers and can lead to keratopathy, blurred vision, and dry eyes.
Indeed, the American Academy of Ophthalmology 2024 annual meeting saw research presented indicating that mirvetuximab was associated with moderate or severe corneal toxicity in 47% of patients treated for primary gynecologic malignancies.
As reported by Medscape Medical News, the study, by researchers at Byers Eye Institute of Stanford University in Stanford, California, was a retrospective analysis of 36 eyes of 18 women who received mirvetuximab for FR alpha–positive, platinum-resistant primary ovarian cancer.
What Are the Causes?
But why would a drug that is targeted specifically to a cancer tumor, thanks to the presence of a monoclonal antibody, cause off-target effects such as ocular toxicity?
Kathy D. Miller, MD, professor of oncology and medicine at Indiana University School of Medicine in Indianapolis, pointed out that they are targeted in a relative and not absolute sense, meaning that the antigen target may not be truly limited to the tumor cells.
There can also be “a lot of ways that you could get systemic toxicities,” she said.
For example, if the linker connecting the antibody and the chemotherapy payload breaks prematurely or is not stable, or if the drug leaches out into the tumor microenvironment and then is “picked up into the circulation, that can give you systemic toxicity,” she said.
In addition, the drug may, once it is in the tumor cells, be metabolized to an active metabolite that could, again, result in systemic exposure.
Side Effects Are Underappreciated and Distressing
Ocular toxicity remains underappreciated among oncologists prescribing these drugs. One reason is that it “did not get enough attention” in the initial clinical trial reports, Miller said she suspects.
Another potential reason for this is that “we’re not used to thinking about it because it’s not particularly common among the drugs that oncologists use frequently,” she added. Additionally, it tends to come up later during treatment, “so people have to be on therapy for some time before you start to see it.”
Nevertheless, Miller underlined that ocular toxicity “can be particularly distressing for patients, as it’s uncomfortable [and] can lead to scarring, so some of the vision issues can be permanent.”
“We often see in these situations that there are different types of ocular toxicities that present in different patients,” said Jane L. Meisel, MD, co-director, Breast Medical Oncology, Department of Hematology and Medical Oncology at Emory University School of Medicine in Atlanta.
“Corneal damage is pretty common, and patients can present with blurry vision, or dry eyes, or light sensitivity. And unlike some side effects, these are things that really impact people at every waking moment of their day.”
“So they’re pretty clinically significant side effects, even if they’re not life-threatening,” Meisel emphasized.
Miller suspects that more heavily pretreated patients may be more likely to experience ocular toxicity, as “there’s a much higher incidence of dry eyes in our patients than we recognize.”
She added: “We don’t usually ask about it, and we certainly don’t routinely do Schirmer’s tests,” which determine whether the eye produces enough tears to keep it moist.
Preventive Measures
For patients receiving tisotumab or mirvetuximab who experience ocular toxicity, Kang said the recommendation is to use steroid eye drops before, during, and after treatment with the ADC.
However, she noted that steroids have not been found to be useful in patients given belantamab, so clinicians have tried vasoconstrictor eye drops immediately prior to the infusion, as well as ocular cooling masks, which “are thought to help by reducing blood supply to the ocular areas.”
Other approaches to minimize ocular toxicity have included longer infusion times, so it’s “not so much of a hefty dose at one time,” Kang added.
She underlined that grade 2 and 3 ocular toxicities can lead to dose delays or dose modifications, and “usually by the time you get a grade 4 event, then you may need to discontinue the medication.”
This can have consequences for the patients because they are often “very sick, and this may be their third agent that they’re trying,” or it may be that their tumor is responding to a new treatment, but it has to be withheld because of an ocular toxicity.
“It can be incredibly frustrating for patients, and also for oncologists, and then for ophthalmologists,” Kang said.
Closer Collaboration Between Specialists Needed
What’s known about ocular side effects in patients taking ADCs underlines that there is a need for closer collaboration between oncologists and ophthalmologists.
“In oncology, especially as immunotherapies came to the forefront, our relationships with our endocrinology colleagues have become stronger because we’ve needed them to help us manage things like thyroid toxicity and pituitary issues related to immunotherapy,” Meisel said.
With toxicities that may be “very impactful for patient quality of life, like ocular toxicity, we will need to learn more about them and develop protocols for management, along with our ophthalmology colleagues, so that we can keep patients as comfortable as possible, while maximizing the efficacy of these drugs.”
Miller agreed, saying oncologists need to have “a conversation with a local ophthalmologist,” although she conceded that, in many areas, such specialists “are in short supply.”
The oncologist “not only needs to be aware” of and looking for ocular toxicity when using these ADCs but also needs to be thinking: “If I run into trouble here, who’s my ophthalmology backup? Are they familiar with this drug? And do we have a plan for the multispecialty management of patients who run into this toxicity?”
Setting Counts When Assessing Toxicities
But do all these considerations mean that ADCs’ potential ocular toxicity should give clinicians pause when considering whether to use these drugs?
“What my patients most want are drugs that work; that are effective in controlling their tumors,” Miller said.
“Every drug we use has potential toxicities, and which toxicities are most physically troublesome [or] are the greatest concern may vary from patient to patient, and it may vary a lot from patients with metastatic disease to those in the curative setting.”
She explained that “toxicities that might not be prohibitive at all in the metastatic setting [may] have to be a much bigger part of our considerations” when moving drugs into the adjuvant or neoadjuvant setting.
This, Miller underlined, is where the ocular toxicity with these ADCs “may be much more prohibitive.”
TULIP was funded by Byondis BV.
Turner declared relationships with Novartis, AstraZeneca, Pfizer, Merck Sharp & Dohme, Lilly, Repare Therapeutics, Roche, GlaxoSmithKline, Gilead Sciences, Inivata, Guardant Health, Exact Sciences, and Relay Therapeutics.
Meisel declared relationships with Novartis, AstraZeneca, Genentech, Seagen, Olema Oncology, GE Healthcare, Pfizer, Stemline, and Sermonix Pharmaceuticals.
A version of this article appeared on Medscape.com.
Such experts called for greater collaboration between oncologists and ophthalmologists, in interviews with Medscape Medical News.
ADCs combine a monoclonal antibody targeted at an antigen overexpressed on cancer cells with a toxic chemotherapy payload — the aim being to maximize the effectiveness of the drug against the tumor while minimizing the damage to healthy tissues and reducing systemic toxicity.
Yet trastuzumab duocarmazine (T-Duo), a third-generation human epidermal growth factor receptor 2 (HER2)–targeted ADC designed to treat HER2-positive breast cancer, was recently found to have a notable adverse effect in the TULIP trial of 437 patients.
As reported by Medscape Medical News, the drug was associated with a significant increase in progression-free survival over physician’s choice of therapy. However, 78% of patients in the ADC group experienced at least one treatment-emergent ocular toxicity adverse event vs 29.2% of those in the control group.
Moreover, grade 3 or high ocular toxicity events were reported by 21% of patients in the experimental group compared with none of those who received physician’s choice.
Ocular Toxicities Seen on Ocular Surface
Ocular toxicities with these drugs are “not necessarily a new thing,” said Joann J. Kang, MD, director, Cornea and Refractive Surgery, and associate professor of ophthalmology at Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, New York.
“But what we’re seeing with certain ADCs is a lot of ocular toxicity, especially on the ocular surface,” with the degree toxicity varying depending on the ADC in question. “It’s definitely a real concern.”
Kang noted that separate from T-Duo, certain ADCs already come with black box warnings for ocular toxicity, including:
- Belantamab mafodotin (Blenrep) — approved for relapsed or refractory multiple myeloma and carries a warning specifically for keratopathy.
- Tisotumab vedotin (Tivdak) — indicated for recurrent or metastatic cervical cancer and can cause changes in the corneal epithelium and conjunctiva.
- Mirvetuximab soravtansine (Elahere) — used to treat folate receptor (FR) alpha–positive ovarian, fallopian tube, and peritoneal cancers and can lead to keratopathy, blurred vision, and dry eyes.
Indeed, the American Academy of Ophthalmology 2024 annual meeting saw research presented indicating that mirvetuximab was associated with moderate or severe corneal toxicity in 47% of patients treated for primary gynecologic malignancies.
As reported by Medscape Medical News, the study, by researchers at Byers Eye Institute of Stanford University in Stanford, California, was a retrospective analysis of 36 eyes of 18 women who received mirvetuximab for FR alpha–positive, platinum-resistant primary ovarian cancer.
What Are the Causes?
But why would a drug that is targeted specifically to a cancer tumor, thanks to the presence of a monoclonal antibody, cause off-target effects such as ocular toxicity?
Kathy D. Miller, MD, professor of oncology and medicine at Indiana University School of Medicine in Indianapolis, pointed out that they are targeted in a relative and not absolute sense, meaning that the antigen target may not be truly limited to the tumor cells.
There can also be “a lot of ways that you could get systemic toxicities,” she said.
For example, if the linker connecting the antibody and the chemotherapy payload breaks prematurely or is not stable, or if the drug leaches out into the tumor microenvironment and then is “picked up into the circulation, that can give you systemic toxicity,” she said.
In addition, the drug may, once it is in the tumor cells, be metabolized to an active metabolite that could, again, result in systemic exposure.
Side Effects Are Underappreciated and Distressing
Ocular toxicity remains underappreciated among oncologists prescribing these drugs. One reason is that it “did not get enough attention” in the initial clinical trial reports, Miller said she suspects.
Another potential reason for this is that “we’re not used to thinking about it because it’s not particularly common among the drugs that oncologists use frequently,” she added. Additionally, it tends to come up later during treatment, “so people have to be on therapy for some time before you start to see it.”
Nevertheless, Miller underlined that ocular toxicity “can be particularly distressing for patients, as it’s uncomfortable [and] can lead to scarring, so some of the vision issues can be permanent.”
“We often see in these situations that there are different types of ocular toxicities that present in different patients,” said Jane L. Meisel, MD, co-director, Breast Medical Oncology, Department of Hematology and Medical Oncology at Emory University School of Medicine in Atlanta.
“Corneal damage is pretty common, and patients can present with blurry vision, or dry eyes, or light sensitivity. And unlike some side effects, these are things that really impact people at every waking moment of their day.”
“So they’re pretty clinically significant side effects, even if they’re not life-threatening,” Meisel emphasized.
Miller suspects that more heavily pretreated patients may be more likely to experience ocular toxicity, as “there’s a much higher incidence of dry eyes in our patients than we recognize.”
She added: “We don’t usually ask about it, and we certainly don’t routinely do Schirmer’s tests,” which determine whether the eye produces enough tears to keep it moist.
Preventive Measures
For patients receiving tisotumab or mirvetuximab who experience ocular toxicity, Kang said the recommendation is to use steroid eye drops before, during, and after treatment with the ADC.
However, she noted that steroids have not been found to be useful in patients given belantamab, so clinicians have tried vasoconstrictor eye drops immediately prior to the infusion, as well as ocular cooling masks, which “are thought to help by reducing blood supply to the ocular areas.”
Other approaches to minimize ocular toxicity have included longer infusion times, so it’s “not so much of a hefty dose at one time,” Kang added.
She underlined that grade 2 and 3 ocular toxicities can lead to dose delays or dose modifications, and “usually by the time you get a grade 4 event, then you may need to discontinue the medication.”
This can have consequences for the patients because they are often “very sick, and this may be their third agent that they’re trying,” or it may be that their tumor is responding to a new treatment, but it has to be withheld because of an ocular toxicity.
“It can be incredibly frustrating for patients, and also for oncologists, and then for ophthalmologists,” Kang said.
Closer Collaboration Between Specialists Needed
What’s known about ocular side effects in patients taking ADCs underlines that there is a need for closer collaboration between oncologists and ophthalmologists.
“In oncology, especially as immunotherapies came to the forefront, our relationships with our endocrinology colleagues have become stronger because we’ve needed them to help us manage things like thyroid toxicity and pituitary issues related to immunotherapy,” Meisel said.
With toxicities that may be “very impactful for patient quality of life, like ocular toxicity, we will need to learn more about them and develop protocols for management, along with our ophthalmology colleagues, so that we can keep patients as comfortable as possible, while maximizing the efficacy of these drugs.”
Miller agreed, saying oncologists need to have “a conversation with a local ophthalmologist,” although she conceded that, in many areas, such specialists “are in short supply.”
The oncologist “not only needs to be aware” of and looking for ocular toxicity when using these ADCs but also needs to be thinking: “If I run into trouble here, who’s my ophthalmology backup? Are they familiar with this drug? And do we have a plan for the multispecialty management of patients who run into this toxicity?”
Setting Counts When Assessing Toxicities
But do all these considerations mean that ADCs’ potential ocular toxicity should give clinicians pause when considering whether to use these drugs?
“What my patients most want are drugs that work; that are effective in controlling their tumors,” Miller said.
“Every drug we use has potential toxicities, and which toxicities are most physically troublesome [or] are the greatest concern may vary from patient to patient, and it may vary a lot from patients with metastatic disease to those in the curative setting.”
She explained that “toxicities that might not be prohibitive at all in the metastatic setting [may] have to be a much bigger part of our considerations” when moving drugs into the adjuvant or neoadjuvant setting.
This, Miller underlined, is where the ocular toxicity with these ADCs “may be much more prohibitive.”
TULIP was funded by Byondis BV.
Turner declared relationships with Novartis, AstraZeneca, Pfizer, Merck Sharp & Dohme, Lilly, Repare Therapeutics, Roche, GlaxoSmithKline, Gilead Sciences, Inivata, Guardant Health, Exact Sciences, and Relay Therapeutics.
Meisel declared relationships with Novartis, AstraZeneca, Genentech, Seagen, Olema Oncology, GE Healthcare, Pfizer, Stemline, and Sermonix Pharmaceuticals.
A version of this article appeared on Medscape.com.
Such experts called for greater collaboration between oncologists and ophthalmologists, in interviews with Medscape Medical News.
ADCs combine a monoclonal antibody targeted at an antigen overexpressed on cancer cells with a toxic chemotherapy payload — the aim being to maximize the effectiveness of the drug against the tumor while minimizing the damage to healthy tissues and reducing systemic toxicity.
Yet trastuzumab duocarmazine (T-Duo), a third-generation human epidermal growth factor receptor 2 (HER2)–targeted ADC designed to treat HER2-positive breast cancer, was recently found to have a notable adverse effect in the TULIP trial of 437 patients.
As reported by Medscape Medical News, the drug was associated with a significant increase in progression-free survival over physician’s choice of therapy. However, 78% of patients in the ADC group experienced at least one treatment-emergent ocular toxicity adverse event vs 29.2% of those in the control group.
Moreover, grade 3 or high ocular toxicity events were reported by 21% of patients in the experimental group compared with none of those who received physician’s choice.
Ocular Toxicities Seen on Ocular Surface
Ocular toxicities with these drugs are “not necessarily a new thing,” said Joann J. Kang, MD, director, Cornea and Refractive Surgery, and associate professor of ophthalmology at Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, New York.
“But what we’re seeing with certain ADCs is a lot of ocular toxicity, especially on the ocular surface,” with the degree toxicity varying depending on the ADC in question. “It’s definitely a real concern.”
Kang noted that separate from T-Duo, certain ADCs already come with black box warnings for ocular toxicity, including:
- Belantamab mafodotin (Blenrep) — approved for relapsed or refractory multiple myeloma and carries a warning specifically for keratopathy.
- Tisotumab vedotin (Tivdak) — indicated for recurrent or metastatic cervical cancer and can cause changes in the corneal epithelium and conjunctiva.
- Mirvetuximab soravtansine (Elahere) — used to treat folate receptor (FR) alpha–positive ovarian, fallopian tube, and peritoneal cancers and can lead to keratopathy, blurred vision, and dry eyes.
Indeed, the American Academy of Ophthalmology 2024 annual meeting saw research presented indicating that mirvetuximab was associated with moderate or severe corneal toxicity in 47% of patients treated for primary gynecologic malignancies.
As reported by Medscape Medical News, the study, by researchers at Byers Eye Institute of Stanford University in Stanford, California, was a retrospective analysis of 36 eyes of 18 women who received mirvetuximab for FR alpha–positive, platinum-resistant primary ovarian cancer.
What Are the Causes?
But why would a drug that is targeted specifically to a cancer tumor, thanks to the presence of a monoclonal antibody, cause off-target effects such as ocular toxicity?
Kathy D. Miller, MD, professor of oncology and medicine at Indiana University School of Medicine in Indianapolis, pointed out that they are targeted in a relative and not absolute sense, meaning that the antigen target may not be truly limited to the tumor cells.
There can also be “a lot of ways that you could get systemic toxicities,” she said.
For example, if the linker connecting the antibody and the chemotherapy payload breaks prematurely or is not stable, or if the drug leaches out into the tumor microenvironment and then is “picked up into the circulation, that can give you systemic toxicity,” she said.
In addition, the drug may, once it is in the tumor cells, be metabolized to an active metabolite that could, again, result in systemic exposure.
Side Effects Are Underappreciated and Distressing
Ocular toxicity remains underappreciated among oncologists prescribing these drugs. One reason is that it “did not get enough attention” in the initial clinical trial reports, Miller said she suspects.
Another potential reason for this is that “we’re not used to thinking about it because it’s not particularly common among the drugs that oncologists use frequently,” she added. Additionally, it tends to come up later during treatment, “so people have to be on therapy for some time before you start to see it.”
Nevertheless, Miller underlined that ocular toxicity “can be particularly distressing for patients, as it’s uncomfortable [and] can lead to scarring, so some of the vision issues can be permanent.”
“We often see in these situations that there are different types of ocular toxicities that present in different patients,” said Jane L. Meisel, MD, co-director, Breast Medical Oncology, Department of Hematology and Medical Oncology at Emory University School of Medicine in Atlanta.
“Corneal damage is pretty common, and patients can present with blurry vision, or dry eyes, or light sensitivity. And unlike some side effects, these are things that really impact people at every waking moment of their day.”
“So they’re pretty clinically significant side effects, even if they’re not life-threatening,” Meisel emphasized.
Miller suspects that more heavily pretreated patients may be more likely to experience ocular toxicity, as “there’s a much higher incidence of dry eyes in our patients than we recognize.”
She added: “We don’t usually ask about it, and we certainly don’t routinely do Schirmer’s tests,” which determine whether the eye produces enough tears to keep it moist.
Preventive Measures
For patients receiving tisotumab or mirvetuximab who experience ocular toxicity, Kang said the recommendation is to use steroid eye drops before, during, and after treatment with the ADC.
However, she noted that steroids have not been found to be useful in patients given belantamab, so clinicians have tried vasoconstrictor eye drops immediately prior to the infusion, as well as ocular cooling masks, which “are thought to help by reducing blood supply to the ocular areas.”
Other approaches to minimize ocular toxicity have included longer infusion times, so it’s “not so much of a hefty dose at one time,” Kang added.
She underlined that grade 2 and 3 ocular toxicities can lead to dose delays or dose modifications, and “usually by the time you get a grade 4 event, then you may need to discontinue the medication.”
This can have consequences for the patients because they are often “very sick, and this may be their third agent that they’re trying,” or it may be that their tumor is responding to a new treatment, but it has to be withheld because of an ocular toxicity.
“It can be incredibly frustrating for patients, and also for oncologists, and then for ophthalmologists,” Kang said.
Closer Collaboration Between Specialists Needed
What’s known about ocular side effects in patients taking ADCs underlines that there is a need for closer collaboration between oncologists and ophthalmologists.
“In oncology, especially as immunotherapies came to the forefront, our relationships with our endocrinology colleagues have become stronger because we’ve needed them to help us manage things like thyroid toxicity and pituitary issues related to immunotherapy,” Meisel said.
With toxicities that may be “very impactful for patient quality of life, like ocular toxicity, we will need to learn more about them and develop protocols for management, along with our ophthalmology colleagues, so that we can keep patients as comfortable as possible, while maximizing the efficacy of these drugs.”
Miller agreed, saying oncologists need to have “a conversation with a local ophthalmologist,” although she conceded that, in many areas, such specialists “are in short supply.”
The oncologist “not only needs to be aware” of and looking for ocular toxicity when using these ADCs but also needs to be thinking: “If I run into trouble here, who’s my ophthalmology backup? Are they familiar with this drug? And do we have a plan for the multispecialty management of patients who run into this toxicity?”
Setting Counts When Assessing Toxicities
But do all these considerations mean that ADCs’ potential ocular toxicity should give clinicians pause when considering whether to use these drugs?
“What my patients most want are drugs that work; that are effective in controlling their tumors,” Miller said.
“Every drug we use has potential toxicities, and which toxicities are most physically troublesome [or] are the greatest concern may vary from patient to patient, and it may vary a lot from patients with metastatic disease to those in the curative setting.”
She explained that “toxicities that might not be prohibitive at all in the metastatic setting [may] have to be a much bigger part of our considerations” when moving drugs into the adjuvant or neoadjuvant setting.
This, Miller underlined, is where the ocular toxicity with these ADCs “may be much more prohibitive.”
TULIP was funded by Byondis BV.
Turner declared relationships with Novartis, AstraZeneca, Pfizer, Merck Sharp & Dohme, Lilly, Repare Therapeutics, Roche, GlaxoSmithKline, Gilead Sciences, Inivata, Guardant Health, Exact Sciences, and Relay Therapeutics.
Meisel declared relationships with Novartis, AstraZeneca, Genentech, Seagen, Olema Oncology, GE Healthcare, Pfizer, Stemline, and Sermonix Pharmaceuticals.
A version of this article appeared on Medscape.com.
New Cancer Drugs: Do Patients Prefer Faster Access or Clinical Benefit?
When the Food and Drug Administration (FDA) grants cancer drugs accelerated approval, a key aim is to provide patients faster access to therapies that can benefit them.
The downside of a speedier approval timeline, however, is that it’s often not yet clear whether the new drugs will actually allow a patient to live longer or better. Information on overall survival and quality of life typically comes years later, after drugs undergo confirmatory trials, or sometimes not at all, if companies fail to conduct these trials.
During this waiting period, patients may be receiving a cancer drug that provides no real clinical benefit but comes with a host of toxicities.
In fact, the odds are about as good as a coin flip. For cancer drugs that have confirmatory trial data, more than half don’t ultimately provide an overall survival or quality of life benefit.
Inherent to the accelerated approval process is the assumption that patients are willing to accept this uncertainty in exchange for faster access.
But is that really the case?
The researchers asked about 870 adults with experience of cancer challenges — either their own cancer diagnosis or that of family or a close friend — whether they valued faster access or certainty that a drug really works.
In the study, participants imagined they had been diagnosed with cancer and could choose between two cancer drugs under investigation in clinical trials but with uncertain effectiveness, and a current standard treatment. Participants had to make a series of choices based on five scenarios.
The first two scenarios were based on the impact of the current standard treatment: A patient’s life expectancy on the standard treatment (6 months up to 3 years), and a patient’s physical health on the standard treatment (functional status restricted only during strenuous activities up to completely disabled).
The remaining three scenarios dealt with the two new drugs: The effect of the new drugs on a surrogate endpoint, progression-free survival (whether the drugs slowed tumor growth for an extra month or 5 additional months compared with the standard treatment), certainty that slowing tumor growth will improve survival (very low to high), and the wait time to access the drugs (immediately to as long as 2 years).
The researchers assessed the relative importance of survival benefit certainty vs wait time and how that balance shifted depending on the different scenarios.
Overall, the researchers found that, if there was no evidence linking the surrogate endpoint (progression-free survival) to overall survival, patients were willing to wait about 8 months for weak evidence of an overall survival benefit (ie, low certainty the drug will extend survival by 1-5 months), about 16 months for moderate certainty, and almost 22 months for high certainty.
Despite a willingness to wait for greater certainty, participants did value speed as well. Overall, respondents showed a strong preference against a 1-year delay in FDA approval time. People who were aged 55 years or more and were non-White individuals made less than $40,000 year as well as those with the lowest life expectancy on a current standard treatment were most sensitive to wait times while those with better functional status and longer life expectancies on a current treatment were less sensitive to longer wait times.
“Our results indicate that some patients (except those with the poorest prognoses) would find the additional time required to generate evidence on the survival benefit of new cancer drugs an acceptable tradeoff,” the study authors concluded.
Although people do place high value on timely access to new cancer drugs, especially if there are limited treatment options, many are willing to wait for greater certainty that a new drug provides an overall survival benefit, lead author Robin Forrest, MSc, with the Department of Health Policy, London School of Economics in England, said in an interview.
In the study, respondents also did not place significant value on whether the drug substantially slowed cancer growth. “In other words, substantial progression-free survival benefit of a drug did not compensate for lack of certainty about a drug’s benefit on survival in respondents’ drug choices,” the authors explained.
“In an effort to move quickly, we have accepted progression-free survival [as a surrogate endpoint],” Jyoti D. Patel, MD, oncologist with Northwestern Memorial Hospital, Chicago, Illinois, who wasn’t involved in the study. But a growing body of evidence indicates that progression-free survival is often a poor surrogate for overall survival. And what this study suggests is that “patients uniformly care about improvements in overall survival and the quality of that survival,” Patel said.
Bishal Gyawali, MD, PhD, was not surprised by the findings.
“I always thought this was the real-world scenario, but the problem is the voices of ordinary patients are not heard,” Gyawali, with Queen’s University, Kingston, Ontario, Canada, who also wasn’t involved in the study, said in an interview.
“What is heard is the loud noise of ‘we need access now, today, yesterday’ — ‘we don’t care if the drug doesn’t improve overall survival, we just need a drug, any drug’ — ‘we don’t care how much it costs, we need access today,’ ” Gyawali said. “Not saying this is wrong, but this is not the representation of all patients.”
However, the voices of patients who are more cautious and want evidence of benefit before accepting toxicities don’t make headlines, he added.
What this survey means from a policy perspective, said Gyawali, is that accelerated approvals that do not mandate survival endpoint in confirmatory trials are ignoring the need of many patients who prioritize certainty of benefit over speed of access.
The study was funded by the London School of Economics and Political Science Phelan United States Centre. Forrest had no relevant disclosures. Gyawali has received consulting fees from Vivio Health. Patel has various relationships with AbbVie, Anheart, AstraZeneca, Bristol-Myers Squibb, Guardant, Tempus, Sanofi, BluePrint, Takeda, and Gilead.
A version of this article first appeared on Medscape.com.
When the Food and Drug Administration (FDA) grants cancer drugs accelerated approval, a key aim is to provide patients faster access to therapies that can benefit them.
The downside of a speedier approval timeline, however, is that it’s often not yet clear whether the new drugs will actually allow a patient to live longer or better. Information on overall survival and quality of life typically comes years later, after drugs undergo confirmatory trials, or sometimes not at all, if companies fail to conduct these trials.
During this waiting period, patients may be receiving a cancer drug that provides no real clinical benefit but comes with a host of toxicities.
In fact, the odds are about as good as a coin flip. For cancer drugs that have confirmatory trial data, more than half don’t ultimately provide an overall survival or quality of life benefit.
Inherent to the accelerated approval process is the assumption that patients are willing to accept this uncertainty in exchange for faster access.
But is that really the case?
The researchers asked about 870 adults with experience of cancer challenges — either their own cancer diagnosis or that of family or a close friend — whether they valued faster access or certainty that a drug really works.
In the study, participants imagined they had been diagnosed with cancer and could choose between two cancer drugs under investigation in clinical trials but with uncertain effectiveness, and a current standard treatment. Participants had to make a series of choices based on five scenarios.
The first two scenarios were based on the impact of the current standard treatment: A patient’s life expectancy on the standard treatment (6 months up to 3 years), and a patient’s physical health on the standard treatment (functional status restricted only during strenuous activities up to completely disabled).
The remaining three scenarios dealt with the two new drugs: The effect of the new drugs on a surrogate endpoint, progression-free survival (whether the drugs slowed tumor growth for an extra month or 5 additional months compared with the standard treatment), certainty that slowing tumor growth will improve survival (very low to high), and the wait time to access the drugs (immediately to as long as 2 years).
The researchers assessed the relative importance of survival benefit certainty vs wait time and how that balance shifted depending on the different scenarios.
Overall, the researchers found that, if there was no evidence linking the surrogate endpoint (progression-free survival) to overall survival, patients were willing to wait about 8 months for weak evidence of an overall survival benefit (ie, low certainty the drug will extend survival by 1-5 months), about 16 months for moderate certainty, and almost 22 months for high certainty.
Despite a willingness to wait for greater certainty, participants did value speed as well. Overall, respondents showed a strong preference against a 1-year delay in FDA approval time. People who were aged 55 years or more and were non-White individuals made less than $40,000 year as well as those with the lowest life expectancy on a current standard treatment were most sensitive to wait times while those with better functional status and longer life expectancies on a current treatment were less sensitive to longer wait times.
“Our results indicate that some patients (except those with the poorest prognoses) would find the additional time required to generate evidence on the survival benefit of new cancer drugs an acceptable tradeoff,” the study authors concluded.
Although people do place high value on timely access to new cancer drugs, especially if there are limited treatment options, many are willing to wait for greater certainty that a new drug provides an overall survival benefit, lead author Robin Forrest, MSc, with the Department of Health Policy, London School of Economics in England, said in an interview.
In the study, respondents also did not place significant value on whether the drug substantially slowed cancer growth. “In other words, substantial progression-free survival benefit of a drug did not compensate for lack of certainty about a drug’s benefit on survival in respondents’ drug choices,” the authors explained.
“In an effort to move quickly, we have accepted progression-free survival [as a surrogate endpoint],” Jyoti D. Patel, MD, oncologist with Northwestern Memorial Hospital, Chicago, Illinois, who wasn’t involved in the study. But a growing body of evidence indicates that progression-free survival is often a poor surrogate for overall survival. And what this study suggests is that “patients uniformly care about improvements in overall survival and the quality of that survival,” Patel said.
Bishal Gyawali, MD, PhD, was not surprised by the findings.
“I always thought this was the real-world scenario, but the problem is the voices of ordinary patients are not heard,” Gyawali, with Queen’s University, Kingston, Ontario, Canada, who also wasn’t involved in the study, said in an interview.
“What is heard is the loud noise of ‘we need access now, today, yesterday’ — ‘we don’t care if the drug doesn’t improve overall survival, we just need a drug, any drug’ — ‘we don’t care how much it costs, we need access today,’ ” Gyawali said. “Not saying this is wrong, but this is not the representation of all patients.”
However, the voices of patients who are more cautious and want evidence of benefit before accepting toxicities don’t make headlines, he added.
What this survey means from a policy perspective, said Gyawali, is that accelerated approvals that do not mandate survival endpoint in confirmatory trials are ignoring the need of many patients who prioritize certainty of benefit over speed of access.
The study was funded by the London School of Economics and Political Science Phelan United States Centre. Forrest had no relevant disclosures. Gyawali has received consulting fees from Vivio Health. Patel has various relationships with AbbVie, Anheart, AstraZeneca, Bristol-Myers Squibb, Guardant, Tempus, Sanofi, BluePrint, Takeda, and Gilead.
A version of this article first appeared on Medscape.com.
When the Food and Drug Administration (FDA) grants cancer drugs accelerated approval, a key aim is to provide patients faster access to therapies that can benefit them.
The downside of a speedier approval timeline, however, is that it’s often not yet clear whether the new drugs will actually allow a patient to live longer or better. Information on overall survival and quality of life typically comes years later, after drugs undergo confirmatory trials, or sometimes not at all, if companies fail to conduct these trials.
During this waiting period, patients may be receiving a cancer drug that provides no real clinical benefit but comes with a host of toxicities.
In fact, the odds are about as good as a coin flip. For cancer drugs that have confirmatory trial data, more than half don’t ultimately provide an overall survival or quality of life benefit.
Inherent to the accelerated approval process is the assumption that patients are willing to accept this uncertainty in exchange for faster access.
But is that really the case?
The researchers asked about 870 adults with experience of cancer challenges — either their own cancer diagnosis or that of family or a close friend — whether they valued faster access or certainty that a drug really works.
In the study, participants imagined they had been diagnosed with cancer and could choose between two cancer drugs under investigation in clinical trials but with uncertain effectiveness, and a current standard treatment. Participants had to make a series of choices based on five scenarios.
The first two scenarios were based on the impact of the current standard treatment: A patient’s life expectancy on the standard treatment (6 months up to 3 years), and a patient’s physical health on the standard treatment (functional status restricted only during strenuous activities up to completely disabled).
The remaining three scenarios dealt with the two new drugs: The effect of the new drugs on a surrogate endpoint, progression-free survival (whether the drugs slowed tumor growth for an extra month or 5 additional months compared with the standard treatment), certainty that slowing tumor growth will improve survival (very low to high), and the wait time to access the drugs (immediately to as long as 2 years).
The researchers assessed the relative importance of survival benefit certainty vs wait time and how that balance shifted depending on the different scenarios.
Overall, the researchers found that, if there was no evidence linking the surrogate endpoint (progression-free survival) to overall survival, patients were willing to wait about 8 months for weak evidence of an overall survival benefit (ie, low certainty the drug will extend survival by 1-5 months), about 16 months for moderate certainty, and almost 22 months for high certainty.
Despite a willingness to wait for greater certainty, participants did value speed as well. Overall, respondents showed a strong preference against a 1-year delay in FDA approval time. People who were aged 55 years or more and were non-White individuals made less than $40,000 year as well as those with the lowest life expectancy on a current standard treatment were most sensitive to wait times while those with better functional status and longer life expectancies on a current treatment were less sensitive to longer wait times.
“Our results indicate that some patients (except those with the poorest prognoses) would find the additional time required to generate evidence on the survival benefit of new cancer drugs an acceptable tradeoff,” the study authors concluded.
Although people do place high value on timely access to new cancer drugs, especially if there are limited treatment options, many are willing to wait for greater certainty that a new drug provides an overall survival benefit, lead author Robin Forrest, MSc, with the Department of Health Policy, London School of Economics in England, said in an interview.
In the study, respondents also did not place significant value on whether the drug substantially slowed cancer growth. “In other words, substantial progression-free survival benefit of a drug did not compensate for lack of certainty about a drug’s benefit on survival in respondents’ drug choices,” the authors explained.
“In an effort to move quickly, we have accepted progression-free survival [as a surrogate endpoint],” Jyoti D. Patel, MD, oncologist with Northwestern Memorial Hospital, Chicago, Illinois, who wasn’t involved in the study. But a growing body of evidence indicates that progression-free survival is often a poor surrogate for overall survival. And what this study suggests is that “patients uniformly care about improvements in overall survival and the quality of that survival,” Patel said.
Bishal Gyawali, MD, PhD, was not surprised by the findings.
“I always thought this was the real-world scenario, but the problem is the voices of ordinary patients are not heard,” Gyawali, with Queen’s University, Kingston, Ontario, Canada, who also wasn’t involved in the study, said in an interview.
“What is heard is the loud noise of ‘we need access now, today, yesterday’ — ‘we don’t care if the drug doesn’t improve overall survival, we just need a drug, any drug’ — ‘we don’t care how much it costs, we need access today,’ ” Gyawali said. “Not saying this is wrong, but this is not the representation of all patients.”
However, the voices of patients who are more cautious and want evidence of benefit before accepting toxicities don’t make headlines, he added.
What this survey means from a policy perspective, said Gyawali, is that accelerated approvals that do not mandate survival endpoint in confirmatory trials are ignoring the need of many patients who prioritize certainty of benefit over speed of access.
The study was funded by the London School of Economics and Political Science Phelan United States Centre. Forrest had no relevant disclosures. Gyawali has received consulting fees from Vivio Health. Patel has various relationships with AbbVie, Anheart, AstraZeneca, Bristol-Myers Squibb, Guardant, Tempus, Sanofi, BluePrint, Takeda, and Gilead.
A version of this article first appeared on Medscape.com.
FROM THE LANCET ONCOLOGY
USPSTF Updates Recommendations on Cervical Cancer Screening
The US Preventive Services Task Force (USPSTF) has posted a draft updated statement on cervical cancer screening. The statement is open for public comment until January 13, 2025, on the task force’s website.
Nearly all cases of cervical cancer are caused by human papilloma virus (HPV) and most occur in women who have not been regularly screened or appropriately treated, the task force stressed.
New Screening Option
In 2024, there will be an estimated 13,820 new cases of cervical cancer and 4360 deaths.
“Evidence shows that screening saves lives, and all women aged 21-65 need to be screened,” task force member Esa Davis, MD, MPH, FAAFP, a professor of family and community medicine and associate vice president for community health at the University of Maryland, Baltimore, said in an interview. A new feature in the 2024 draft statement endorsing self-collection of cervical samples for HPV testing may facilitate broader screening.
“We hope the new effective option of self-collecting will expand screening and allow even more women to get screened regularly,” Davis said. “Some may feel more comfortable collecting samples themselves, and the collection can be office-based or home-based, but it’s very important that it be done under the direction of a clinician.”
In agreement is Diego Aviles, MD, an assistant professor and a gynecologic oncologist with UTHealth Houston. “Self-collection will absolutely expand screening. I think it’s an incredible advancement in medicine that patients are able to collect in the comfort of their own homes with no need to come into the office for an uncomfortable pelvic exam,” he said in an interview. “This empowers the patient and gives her a choice.”
As to concern about potential error, he added that while this is a concern on paper, “a lot of studies have shown that self-collection is just as effective doctor collection.”
Largely consistent with the task force’s 2018 screening recommendations, the updated suggestions also align with those of other organizations such as the American College of Obstetricians and Gynecologists (ACOG), Davis said.
Christopher M. Zahn, MD, ACOG’s chief of clinical practice and health equity and quality, stressed the importance of cervical cancer screening and said his organization will be reviewing the USPSTF recommendations. He urges ACOG members to consider them and offer their comments on the public-input platform.
Drawing on the latest evidence, the task force is also highlighting for the first time that stand-alone HPV screening gives women aged 30-65 years the best balance of benefits and harms when it comes to finding and preventing cervical cancer, while continuing to reinforce that Pap testing and co-testing are also effective screening options for these women.
The current draft statement applies to cisgender women and those assigned female sex at birth, including transgender men and nonbinary individuals. The recommendations do not apply to women at increased risk of cervical cancer such as those with HIV infection, a compromised immune system, or a history of treatment for precancerous lesions or cervical cancer.
Based on a review of evidence on the benefits and harms of screening, the USPSTF’s independent panel of national experts proposed the following:
Recommendations for Screening (Based on Grade A Evidence):
- Ages 21-65 years: All women should get screened regularly for this preventable disease.
- Ages 21-29 years: All women in this age group should undergo a Pap test every 3 years but do not need HPV testing. “In this age group most HPV infections will go away on their own because young women have strong immune systems. Older women are likely to have HPV that lasts longer and so they need testing for the virus,” Davis said.
- Ages 30-65 years: As noted, HPV screening gives women in this age category the best balance of benefits and harms in terms of preventing and finding cervical cancer. Pap testing or co-testing (Pap tests and HPV tests) are also effective screening options for this population. Ideally, these women should have an HPV test every 5 years or, alternatively, a Pap test every 3 years, or a combined HPV and Pap test every 5 years (co-testing).
Recommendations Against Screening (No Benefit or Benefit Outweighed by Harms — Grade D evidence):
- Women aged less than 21 years: Screening is not necessary.
- Other women not needing screening: Nor is screening necessary for those of any age who have had a total hysterectomy with removal of the cervix and those aged > 65 years who have had regular screenings with normal results. That means normal results from their last three Pap tests or their last two HPV tests, completed in the past 10 years, with at least one of the tests done in the past 5 years.
- Women aged 65 or more: These women should continue screening only if they have not been screened regularly or have had abnormal results in the past decade such as a high-grade precancerous lesion (cervical intraepithelial neoplasia grade 2 or 3) or cervical cancer.
Davis noted that none of the current recommendations are likely to be controversial or to spark pushback. “But,” said Aviles, “any time I see recent change in medicine, there’s always a little bit of pushback and it may take some time for everyone to be comfortable with the self-collection option. The recommendations still give doctors the grace to use the screening test they feel comfortable with, but I think eventually everyone will get on board with self-collection.”
As for the future, he added, “Over the next few years we’ll have to look at women who are on immune-weakening medications like Skyrizi [risankizumab] for skin conditions like psoriasis. These are commonly used in young people and can increase the risk of cervical cancer. I haven’t seen a lot of conversation about this, but patients should be aware of this risk and recommendations for this group should be different than for the general population.”
The USPSTF also noted a need to assess the magnitude of the incremental benefit and harms of screening and the interval of multiple rounds of HPV-primary screening in HPV-vaccinated cohorts in US populations.
Davis, Aviles, and Zahn and had no relevant competing interests to disclose.
A version of this article first appeared on Medscape.com.
The US Preventive Services Task Force (USPSTF) has posted a draft updated statement on cervical cancer screening. The statement is open for public comment until January 13, 2025, on the task force’s website.
Nearly all cases of cervical cancer are caused by human papilloma virus (HPV) and most occur in women who have not been regularly screened or appropriately treated, the task force stressed.
New Screening Option
In 2024, there will be an estimated 13,820 new cases of cervical cancer and 4360 deaths.
“Evidence shows that screening saves lives, and all women aged 21-65 need to be screened,” task force member Esa Davis, MD, MPH, FAAFP, a professor of family and community medicine and associate vice president for community health at the University of Maryland, Baltimore, said in an interview. A new feature in the 2024 draft statement endorsing self-collection of cervical samples for HPV testing may facilitate broader screening.
“We hope the new effective option of self-collecting will expand screening and allow even more women to get screened regularly,” Davis said. “Some may feel more comfortable collecting samples themselves, and the collection can be office-based or home-based, but it’s very important that it be done under the direction of a clinician.”
In agreement is Diego Aviles, MD, an assistant professor and a gynecologic oncologist with UTHealth Houston. “Self-collection will absolutely expand screening. I think it’s an incredible advancement in medicine that patients are able to collect in the comfort of their own homes with no need to come into the office for an uncomfortable pelvic exam,” he said in an interview. “This empowers the patient and gives her a choice.”
As to concern about potential error, he added that while this is a concern on paper, “a lot of studies have shown that self-collection is just as effective doctor collection.”
Largely consistent with the task force’s 2018 screening recommendations, the updated suggestions also align with those of other organizations such as the American College of Obstetricians and Gynecologists (ACOG), Davis said.
Christopher M. Zahn, MD, ACOG’s chief of clinical practice and health equity and quality, stressed the importance of cervical cancer screening and said his organization will be reviewing the USPSTF recommendations. He urges ACOG members to consider them and offer their comments on the public-input platform.
Drawing on the latest evidence, the task force is also highlighting for the first time that stand-alone HPV screening gives women aged 30-65 years the best balance of benefits and harms when it comes to finding and preventing cervical cancer, while continuing to reinforce that Pap testing and co-testing are also effective screening options for these women.
The current draft statement applies to cisgender women and those assigned female sex at birth, including transgender men and nonbinary individuals. The recommendations do not apply to women at increased risk of cervical cancer such as those with HIV infection, a compromised immune system, or a history of treatment for precancerous lesions or cervical cancer.
Based on a review of evidence on the benefits and harms of screening, the USPSTF’s independent panel of national experts proposed the following:
Recommendations for Screening (Based on Grade A Evidence):
- Ages 21-65 years: All women should get screened regularly for this preventable disease.
- Ages 21-29 years: All women in this age group should undergo a Pap test every 3 years but do not need HPV testing. “In this age group most HPV infections will go away on their own because young women have strong immune systems. Older women are likely to have HPV that lasts longer and so they need testing for the virus,” Davis said.
- Ages 30-65 years: As noted, HPV screening gives women in this age category the best balance of benefits and harms in terms of preventing and finding cervical cancer. Pap testing or co-testing (Pap tests and HPV tests) are also effective screening options for this population. Ideally, these women should have an HPV test every 5 years or, alternatively, a Pap test every 3 years, or a combined HPV and Pap test every 5 years (co-testing).
Recommendations Against Screening (No Benefit or Benefit Outweighed by Harms — Grade D evidence):
- Women aged less than 21 years: Screening is not necessary.
- Other women not needing screening: Nor is screening necessary for those of any age who have had a total hysterectomy with removal of the cervix and those aged > 65 years who have had regular screenings with normal results. That means normal results from their last three Pap tests or their last two HPV tests, completed in the past 10 years, with at least one of the tests done in the past 5 years.
- Women aged 65 or more: These women should continue screening only if they have not been screened regularly or have had abnormal results in the past decade such as a high-grade precancerous lesion (cervical intraepithelial neoplasia grade 2 or 3) or cervical cancer.
Davis noted that none of the current recommendations are likely to be controversial or to spark pushback. “But,” said Aviles, “any time I see recent change in medicine, there’s always a little bit of pushback and it may take some time for everyone to be comfortable with the self-collection option. The recommendations still give doctors the grace to use the screening test they feel comfortable with, but I think eventually everyone will get on board with self-collection.”
As for the future, he added, “Over the next few years we’ll have to look at women who are on immune-weakening medications like Skyrizi [risankizumab] for skin conditions like psoriasis. These are commonly used in young people and can increase the risk of cervical cancer. I haven’t seen a lot of conversation about this, but patients should be aware of this risk and recommendations for this group should be different than for the general population.”
The USPSTF also noted a need to assess the magnitude of the incremental benefit and harms of screening and the interval of multiple rounds of HPV-primary screening in HPV-vaccinated cohorts in US populations.
Davis, Aviles, and Zahn and had no relevant competing interests to disclose.
A version of this article first appeared on Medscape.com.
The US Preventive Services Task Force (USPSTF) has posted a draft updated statement on cervical cancer screening. The statement is open for public comment until January 13, 2025, on the task force’s website.
Nearly all cases of cervical cancer are caused by human papilloma virus (HPV) and most occur in women who have not been regularly screened or appropriately treated, the task force stressed.
New Screening Option
In 2024, there will be an estimated 13,820 new cases of cervical cancer and 4360 deaths.
“Evidence shows that screening saves lives, and all women aged 21-65 need to be screened,” task force member Esa Davis, MD, MPH, FAAFP, a professor of family and community medicine and associate vice president for community health at the University of Maryland, Baltimore, said in an interview. A new feature in the 2024 draft statement endorsing self-collection of cervical samples for HPV testing may facilitate broader screening.
“We hope the new effective option of self-collecting will expand screening and allow even more women to get screened regularly,” Davis said. “Some may feel more comfortable collecting samples themselves, and the collection can be office-based or home-based, but it’s very important that it be done under the direction of a clinician.”
In agreement is Diego Aviles, MD, an assistant professor and a gynecologic oncologist with UTHealth Houston. “Self-collection will absolutely expand screening. I think it’s an incredible advancement in medicine that patients are able to collect in the comfort of their own homes with no need to come into the office for an uncomfortable pelvic exam,” he said in an interview. “This empowers the patient and gives her a choice.”
As to concern about potential error, he added that while this is a concern on paper, “a lot of studies have shown that self-collection is just as effective doctor collection.”
Largely consistent with the task force’s 2018 screening recommendations, the updated suggestions also align with those of other organizations such as the American College of Obstetricians and Gynecologists (ACOG), Davis said.
Christopher M. Zahn, MD, ACOG’s chief of clinical practice and health equity and quality, stressed the importance of cervical cancer screening and said his organization will be reviewing the USPSTF recommendations. He urges ACOG members to consider them and offer their comments on the public-input platform.
Drawing on the latest evidence, the task force is also highlighting for the first time that stand-alone HPV screening gives women aged 30-65 years the best balance of benefits and harms when it comes to finding and preventing cervical cancer, while continuing to reinforce that Pap testing and co-testing are also effective screening options for these women.
The current draft statement applies to cisgender women and those assigned female sex at birth, including transgender men and nonbinary individuals. The recommendations do not apply to women at increased risk of cervical cancer such as those with HIV infection, a compromised immune system, or a history of treatment for precancerous lesions or cervical cancer.
Based on a review of evidence on the benefits and harms of screening, the USPSTF’s independent panel of national experts proposed the following:
Recommendations for Screening (Based on Grade A Evidence):
- Ages 21-65 years: All women should get screened regularly for this preventable disease.
- Ages 21-29 years: All women in this age group should undergo a Pap test every 3 years but do not need HPV testing. “In this age group most HPV infections will go away on their own because young women have strong immune systems. Older women are likely to have HPV that lasts longer and so they need testing for the virus,” Davis said.
- Ages 30-65 years: As noted, HPV screening gives women in this age category the best balance of benefits and harms in terms of preventing and finding cervical cancer. Pap testing or co-testing (Pap tests and HPV tests) are also effective screening options for this population. Ideally, these women should have an HPV test every 5 years or, alternatively, a Pap test every 3 years, or a combined HPV and Pap test every 5 years (co-testing).
Recommendations Against Screening (No Benefit or Benefit Outweighed by Harms — Grade D evidence):
- Women aged less than 21 years: Screening is not necessary.
- Other women not needing screening: Nor is screening necessary for those of any age who have had a total hysterectomy with removal of the cervix and those aged > 65 years who have had regular screenings with normal results. That means normal results from their last three Pap tests or their last two HPV tests, completed in the past 10 years, with at least one of the tests done in the past 5 years.
- Women aged 65 or more: These women should continue screening only if they have not been screened regularly or have had abnormal results in the past decade such as a high-grade precancerous lesion (cervical intraepithelial neoplasia grade 2 or 3) or cervical cancer.
Davis noted that none of the current recommendations are likely to be controversial or to spark pushback. “But,” said Aviles, “any time I see recent change in medicine, there’s always a little bit of pushback and it may take some time for everyone to be comfortable with the self-collection option. The recommendations still give doctors the grace to use the screening test they feel comfortable with, but I think eventually everyone will get on board with self-collection.”
As for the future, he added, “Over the next few years we’ll have to look at women who are on immune-weakening medications like Skyrizi [risankizumab] for skin conditions like psoriasis. These are commonly used in young people and can increase the risk of cervical cancer. I haven’t seen a lot of conversation about this, but patients should be aware of this risk and recommendations for this group should be different than for the general population.”
The USPSTF also noted a need to assess the magnitude of the incremental benefit and harms of screening and the interval of multiple rounds of HPV-primary screening in HPV-vaccinated cohorts in US populations.
Davis, Aviles, and Zahn and had no relevant competing interests to disclose.
A version of this article first appeared on Medscape.com.
New Cancer Vaccines on the Horizon: Renewed Hope or Hype?
Vaccines for treating and preventing cancer have long been considered a holy grail in oncology.
But aside from a few notable exceptions — including the human papillomavirus (HPV) vaccine, which has dramatically reduced the incidence of HPV-related cancers, and a Bacillus Calmette-Guerin vaccine, which helps prevent early-stage bladder cancer recurrence — most have failed to deliver.
Following a string of disappointments over the past decade, recent advances in the immunotherapy space are bringing renewed hope for progress.
In an American Association for Cancer Research (AACR) series earlier in 2024, Catherine J. Wu, MD, predicted big strides for cancer vaccines, especially for personalized vaccines that target patient-specific neoantigens — the proteins that form on cancer cells — as well as vaccines that can treat diverse tumor types.
said Wu, the Lavine Family Chair of Preventative Cancer Therapies at Dana-Farber Cancer Institute and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
A prime example is a personalized, messenger RNA (mRNA)–based vaccine designed to prevent melanoma recurrence. The mRNA-4157 vaccine encodes up to 34 different patient-specific neoantigens.
“This is one of the most exciting developments in modern cancer therapy,” said Lawrence Young, a virologist and professor of molecular oncology at the University of Warwick, Coventry, England, who commented on the investigational vaccine via the UK-based Science Media Centre.
Other promising options are on the horizon as well. In August, BioNTech announced a phase 1 global trial to study BNT116 — a vaccine to treat non–small cell lung cancer (NSCLC). BNT116, like mRNA-4157, targets specific antigens in the lung cancer cells.
“This technology is the next big phase of cancer treatment,” Siow Ming Lee, MD, a consultant medical oncologist at University College London Hospitals in England, which is leading the UK trial for the lung cancer and melanoma vaccines, told The Guardian. “We are now entering this very exciting new era of mRNA-based immunotherapy clinical trials to investigate the treatment of lung cancer.”
Still, these predictions have a familiar ring. While the prospects are exciting, delivering on them is another story. There are simply no guarantees these strategies will work as hoped.
Then: Where We Were
Cancer vaccine research began to ramp up in the 2000s, and in 2006, the first-generation HPV vaccine, Gardasil, was approved. Gardasil prevents infection from four strains of HPV that cause about 80% of cervical cancer cases.
In 2010, the Food and Drug Administration approved sipuleucel-T, the first therapeutic cancer vaccine, which improved overall survival in patients with hormone-refractory prostate cancer.
Researchers predicted this approval would “pave the way for developing innovative, next generation of vaccines with enhanced antitumor potency.”
In a 2015 AACR research forecast report, Drew Pardoll, MD, PhD, co-director of the Cancer Immunology and Hematopoiesis Program at Johns Hopkins University, Baltimore, Maryland, said that “we can expect to see encouraging results from studies using cancer vaccines.”
Despite the excitement surrounding cancer vaccines alongside a few successes, the next decade brought a longer string of late-phase disappointments.
In 2016, the phase 3 ACT IV trial of a therapeutic vaccine to treat glioblastoma multiforme (CDX-110) was terminated after it failed to demonstrate improved survival.
In 2017, a phase 3 trial of the therapeutic pancreatic cancer vaccine, GVAX, was stopped early for lack of efficacy.
That year, an attenuated Listeria monocytogenes vaccine to treat pancreatic cancer and mesothelioma also failed to come to fruition. In late 2017, concerns over listeria infections prompted Aduro Biotech to cancel its listeria-based cancer treatment program.
In 2018, a phase 3 trial of belagenpumatucel-L, a therapeutic NSCLC vaccine, failed to demonstrate a significant improvement in survival and further study was discontinued.
And in 2019, a vaccine targeting MAGE-A3, a cancer-testis antigen present in multiple tumor types, failed to meet endpoints for improved survival in a phase 3 trial, leading to discontinuation of the vaccine program.
But these disappointments and failures are normal parts of medical research and drug development and have allowed for incremental advances that helped fuel renewed interest and hope for cancer vaccines, when the timing was right, explained vaccine pioneer Larry W. Kwak, MD, PhD, deputy director of the Comprehensive Cancer Center at City of Hope, Duarte, California.
When it comes to vaccine progress, timing makes a difference. In 2011, Kwak and colleagues published promising phase 3 trial results on a personalized vaccine. The vaccine was a patient-specific tumor-derived antigen for patients with follicular lymphoma in their first remission following chemotherapy. Patients who received the vaccine demonstrated significantly longer disease-free survival.
But, at the time, personalized vaccines faced strong headwinds due, largely, to high costs, and commercial interest failed to materialize. “That’s been the major hurdle for a long time,” said Kwak.
Now, however, interest has returned alongside advances in technology and research. The big shift has been the emergence of lower-cost rapid-production mRNA and DNA platforms and a better understanding of how vaccines and potent immune stimulants, like checkpoint inhibitors, can work together to improve outcomes, he explained.
“The timing wasn’t right” back then, Kwak noted. “Now, it’s a different environment and a different time.”
A Turning Point?
Indeed, a decade later, cancer vaccine development appears to be headed in a more promising direction.
Among key cancer vaccines to watch is the mRNA-4157 vaccine, developed by Merck and Moderna, designed to prevent melanoma recurrence. In a recent phase 2 study, patients receiving the mRNA-4157 vaccine alongside pembrolizumab had nearly half the risk for melanoma recurrence or death at 3 years compared with those receiving pembrolizumab alone. Investigators are now evaluating the vaccine in a global phase 3 study in patients with high-risk, stage IIB to IV melanoma following surgery.
Another one to watch is the BNT116 NSCLC vaccine from BioNTech. This vaccine presents the immune system with NSCLC tumor markers to encourage the body to fight cancer cells expressing those markers while ignoring healthy cells. BioNTech also launched a global clinical trial for its vaccine this year.
Other notables include a pancreatic cancer mRNA vaccine, which has shown promising early results in a small trial of 16 patients. Of 16 patients who received the vaccine alongside chemotherapy and after surgery and immunotherapy, 8 responded. Of these eight, six remained recurrence free at 3 years. Investigators noted that the vaccine appeared to stimulate a durable T-cell response in patients who responded.
Kwak has also continued his work on lymphoma vaccines. In August, his team published promising first-in-human data on the use of personalized neoantigen vaccines as an early intervention in untreated patients with lymphoplasmacytic lymphoma. Among nine asymptomatic patients who received the vaccine, all achieved stable disease or better, with no dose-limiting toxicities. One patient had a minor response, and the median time to progression was greater than 72 months.
“The current setting is more for advanced disease,” Kwak explained. “It’s a tougher task, but combined with checkpoint blockade, it may be potent enough to work.”
Still, caution is important. Despite early promise, it’s too soon to tell which, if any, of these investigational vaccines will pan out in the long run. Like investigational drugs, cancer vaccines may show big promising initially but then fail in larger trials.
One key to success, according to Kwak, is to design trials so that even negative results will inform next steps.
But, he noted, failures in large clinical trials will “put a chilling effect on cancer vaccine research again.”
“That’s what keeps me up at night,” he said. “We know the science is fundamentally sound and we have seen glimpses over decades of research that cancer vaccines can work, so it’s really just a matter of tweaking things to optimize trial design.”
Companies tend to design trials to test if a vaccine works or not, without trying to understand why, he said.
“What we need to do is design those so that we can learn from negative results,” he said. That’s what he and his colleagues attempted to do in their recent trial. “We didn’t just look at clinical results; we’re interrogating the actual tumor environment to understand what worked and didn’t and how to tweak that for the next trial.”
Kwak and his colleagues found, for instance, that the vaccine had a greater effect on B cell–derived tumor cells than on cells of plasma origin, so “the most rational design for the next iteration is to combine the vaccine with agents that work directly against plasma cells,” he explained.
As for what’s next, Kwak said: “We’re just focused on trying to do good science and understand. We’ve seen glimpses of success. That’s where we are.”
A version of this article first appeared on Medscape.com.
Vaccines for treating and preventing cancer have long been considered a holy grail in oncology.
But aside from a few notable exceptions — including the human papillomavirus (HPV) vaccine, which has dramatically reduced the incidence of HPV-related cancers, and a Bacillus Calmette-Guerin vaccine, which helps prevent early-stage bladder cancer recurrence — most have failed to deliver.
Following a string of disappointments over the past decade, recent advances in the immunotherapy space are bringing renewed hope for progress.
In an American Association for Cancer Research (AACR) series earlier in 2024, Catherine J. Wu, MD, predicted big strides for cancer vaccines, especially for personalized vaccines that target patient-specific neoantigens — the proteins that form on cancer cells — as well as vaccines that can treat diverse tumor types.
said Wu, the Lavine Family Chair of Preventative Cancer Therapies at Dana-Farber Cancer Institute and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
A prime example is a personalized, messenger RNA (mRNA)–based vaccine designed to prevent melanoma recurrence. The mRNA-4157 vaccine encodes up to 34 different patient-specific neoantigens.
“This is one of the most exciting developments in modern cancer therapy,” said Lawrence Young, a virologist and professor of molecular oncology at the University of Warwick, Coventry, England, who commented on the investigational vaccine via the UK-based Science Media Centre.
Other promising options are on the horizon as well. In August, BioNTech announced a phase 1 global trial to study BNT116 — a vaccine to treat non–small cell lung cancer (NSCLC). BNT116, like mRNA-4157, targets specific antigens in the lung cancer cells.
“This technology is the next big phase of cancer treatment,” Siow Ming Lee, MD, a consultant medical oncologist at University College London Hospitals in England, which is leading the UK trial for the lung cancer and melanoma vaccines, told The Guardian. “We are now entering this very exciting new era of mRNA-based immunotherapy clinical trials to investigate the treatment of lung cancer.”
Still, these predictions have a familiar ring. While the prospects are exciting, delivering on them is another story. There are simply no guarantees these strategies will work as hoped.
Then: Where We Were
Cancer vaccine research began to ramp up in the 2000s, and in 2006, the first-generation HPV vaccine, Gardasil, was approved. Gardasil prevents infection from four strains of HPV that cause about 80% of cervical cancer cases.
In 2010, the Food and Drug Administration approved sipuleucel-T, the first therapeutic cancer vaccine, which improved overall survival in patients with hormone-refractory prostate cancer.
Researchers predicted this approval would “pave the way for developing innovative, next generation of vaccines with enhanced antitumor potency.”
In a 2015 AACR research forecast report, Drew Pardoll, MD, PhD, co-director of the Cancer Immunology and Hematopoiesis Program at Johns Hopkins University, Baltimore, Maryland, said that “we can expect to see encouraging results from studies using cancer vaccines.”
Despite the excitement surrounding cancer vaccines alongside a few successes, the next decade brought a longer string of late-phase disappointments.
In 2016, the phase 3 ACT IV trial of a therapeutic vaccine to treat glioblastoma multiforme (CDX-110) was terminated after it failed to demonstrate improved survival.
In 2017, a phase 3 trial of the therapeutic pancreatic cancer vaccine, GVAX, was stopped early for lack of efficacy.
That year, an attenuated Listeria monocytogenes vaccine to treat pancreatic cancer and mesothelioma also failed to come to fruition. In late 2017, concerns over listeria infections prompted Aduro Biotech to cancel its listeria-based cancer treatment program.
In 2018, a phase 3 trial of belagenpumatucel-L, a therapeutic NSCLC vaccine, failed to demonstrate a significant improvement in survival and further study was discontinued.
And in 2019, a vaccine targeting MAGE-A3, a cancer-testis antigen present in multiple tumor types, failed to meet endpoints for improved survival in a phase 3 trial, leading to discontinuation of the vaccine program.
But these disappointments and failures are normal parts of medical research and drug development and have allowed for incremental advances that helped fuel renewed interest and hope for cancer vaccines, when the timing was right, explained vaccine pioneer Larry W. Kwak, MD, PhD, deputy director of the Comprehensive Cancer Center at City of Hope, Duarte, California.
When it comes to vaccine progress, timing makes a difference. In 2011, Kwak and colleagues published promising phase 3 trial results on a personalized vaccine. The vaccine was a patient-specific tumor-derived antigen for patients with follicular lymphoma in their first remission following chemotherapy. Patients who received the vaccine demonstrated significantly longer disease-free survival.
But, at the time, personalized vaccines faced strong headwinds due, largely, to high costs, and commercial interest failed to materialize. “That’s been the major hurdle for a long time,” said Kwak.
Now, however, interest has returned alongside advances in technology and research. The big shift has been the emergence of lower-cost rapid-production mRNA and DNA platforms and a better understanding of how vaccines and potent immune stimulants, like checkpoint inhibitors, can work together to improve outcomes, he explained.
“The timing wasn’t right” back then, Kwak noted. “Now, it’s a different environment and a different time.”
A Turning Point?
Indeed, a decade later, cancer vaccine development appears to be headed in a more promising direction.
Among key cancer vaccines to watch is the mRNA-4157 vaccine, developed by Merck and Moderna, designed to prevent melanoma recurrence. In a recent phase 2 study, patients receiving the mRNA-4157 vaccine alongside pembrolizumab had nearly half the risk for melanoma recurrence or death at 3 years compared with those receiving pembrolizumab alone. Investigators are now evaluating the vaccine in a global phase 3 study in patients with high-risk, stage IIB to IV melanoma following surgery.
Another one to watch is the BNT116 NSCLC vaccine from BioNTech. This vaccine presents the immune system with NSCLC tumor markers to encourage the body to fight cancer cells expressing those markers while ignoring healthy cells. BioNTech also launched a global clinical trial for its vaccine this year.
Other notables include a pancreatic cancer mRNA vaccine, which has shown promising early results in a small trial of 16 patients. Of 16 patients who received the vaccine alongside chemotherapy and after surgery and immunotherapy, 8 responded. Of these eight, six remained recurrence free at 3 years. Investigators noted that the vaccine appeared to stimulate a durable T-cell response in patients who responded.
Kwak has also continued his work on lymphoma vaccines. In August, his team published promising first-in-human data on the use of personalized neoantigen vaccines as an early intervention in untreated patients with lymphoplasmacytic lymphoma. Among nine asymptomatic patients who received the vaccine, all achieved stable disease or better, with no dose-limiting toxicities. One patient had a minor response, and the median time to progression was greater than 72 months.
“The current setting is more for advanced disease,” Kwak explained. “It’s a tougher task, but combined with checkpoint blockade, it may be potent enough to work.”
Still, caution is important. Despite early promise, it’s too soon to tell which, if any, of these investigational vaccines will pan out in the long run. Like investigational drugs, cancer vaccines may show big promising initially but then fail in larger trials.
One key to success, according to Kwak, is to design trials so that even negative results will inform next steps.
But, he noted, failures in large clinical trials will “put a chilling effect on cancer vaccine research again.”
“That’s what keeps me up at night,” he said. “We know the science is fundamentally sound and we have seen glimpses over decades of research that cancer vaccines can work, so it’s really just a matter of tweaking things to optimize trial design.”
Companies tend to design trials to test if a vaccine works or not, without trying to understand why, he said.
“What we need to do is design those so that we can learn from negative results,” he said. That’s what he and his colleagues attempted to do in their recent trial. “We didn’t just look at clinical results; we’re interrogating the actual tumor environment to understand what worked and didn’t and how to tweak that for the next trial.”
Kwak and his colleagues found, for instance, that the vaccine had a greater effect on B cell–derived tumor cells than on cells of plasma origin, so “the most rational design for the next iteration is to combine the vaccine with agents that work directly against plasma cells,” he explained.
As for what’s next, Kwak said: “We’re just focused on trying to do good science and understand. We’ve seen glimpses of success. That’s where we are.”
A version of this article first appeared on Medscape.com.
Vaccines for treating and preventing cancer have long been considered a holy grail in oncology.
But aside from a few notable exceptions — including the human papillomavirus (HPV) vaccine, which has dramatically reduced the incidence of HPV-related cancers, and a Bacillus Calmette-Guerin vaccine, which helps prevent early-stage bladder cancer recurrence — most have failed to deliver.
Following a string of disappointments over the past decade, recent advances in the immunotherapy space are bringing renewed hope for progress.
In an American Association for Cancer Research (AACR) series earlier in 2024, Catherine J. Wu, MD, predicted big strides for cancer vaccines, especially for personalized vaccines that target patient-specific neoantigens — the proteins that form on cancer cells — as well as vaccines that can treat diverse tumor types.
said Wu, the Lavine Family Chair of Preventative Cancer Therapies at Dana-Farber Cancer Institute and a professor of medicine at Harvard Medical School, both in Boston, Massachusetts.
A prime example is a personalized, messenger RNA (mRNA)–based vaccine designed to prevent melanoma recurrence. The mRNA-4157 vaccine encodes up to 34 different patient-specific neoantigens.
“This is one of the most exciting developments in modern cancer therapy,” said Lawrence Young, a virologist and professor of molecular oncology at the University of Warwick, Coventry, England, who commented on the investigational vaccine via the UK-based Science Media Centre.
Other promising options are on the horizon as well. In August, BioNTech announced a phase 1 global trial to study BNT116 — a vaccine to treat non–small cell lung cancer (NSCLC). BNT116, like mRNA-4157, targets specific antigens in the lung cancer cells.
“This technology is the next big phase of cancer treatment,” Siow Ming Lee, MD, a consultant medical oncologist at University College London Hospitals in England, which is leading the UK trial for the lung cancer and melanoma vaccines, told The Guardian. “We are now entering this very exciting new era of mRNA-based immunotherapy clinical trials to investigate the treatment of lung cancer.”
Still, these predictions have a familiar ring. While the prospects are exciting, delivering on them is another story. There are simply no guarantees these strategies will work as hoped.
Then: Where We Were
Cancer vaccine research began to ramp up in the 2000s, and in 2006, the first-generation HPV vaccine, Gardasil, was approved. Gardasil prevents infection from four strains of HPV that cause about 80% of cervical cancer cases.
In 2010, the Food and Drug Administration approved sipuleucel-T, the first therapeutic cancer vaccine, which improved overall survival in patients with hormone-refractory prostate cancer.
Researchers predicted this approval would “pave the way for developing innovative, next generation of vaccines with enhanced antitumor potency.”
In a 2015 AACR research forecast report, Drew Pardoll, MD, PhD, co-director of the Cancer Immunology and Hematopoiesis Program at Johns Hopkins University, Baltimore, Maryland, said that “we can expect to see encouraging results from studies using cancer vaccines.”
Despite the excitement surrounding cancer vaccines alongside a few successes, the next decade brought a longer string of late-phase disappointments.
In 2016, the phase 3 ACT IV trial of a therapeutic vaccine to treat glioblastoma multiforme (CDX-110) was terminated after it failed to demonstrate improved survival.
In 2017, a phase 3 trial of the therapeutic pancreatic cancer vaccine, GVAX, was stopped early for lack of efficacy.
That year, an attenuated Listeria monocytogenes vaccine to treat pancreatic cancer and mesothelioma also failed to come to fruition. In late 2017, concerns over listeria infections prompted Aduro Biotech to cancel its listeria-based cancer treatment program.
In 2018, a phase 3 trial of belagenpumatucel-L, a therapeutic NSCLC vaccine, failed to demonstrate a significant improvement in survival and further study was discontinued.
And in 2019, a vaccine targeting MAGE-A3, a cancer-testis antigen present in multiple tumor types, failed to meet endpoints for improved survival in a phase 3 trial, leading to discontinuation of the vaccine program.
But these disappointments and failures are normal parts of medical research and drug development and have allowed for incremental advances that helped fuel renewed interest and hope for cancer vaccines, when the timing was right, explained vaccine pioneer Larry W. Kwak, MD, PhD, deputy director of the Comprehensive Cancer Center at City of Hope, Duarte, California.
When it comes to vaccine progress, timing makes a difference. In 2011, Kwak and colleagues published promising phase 3 trial results on a personalized vaccine. The vaccine was a patient-specific tumor-derived antigen for patients with follicular lymphoma in their first remission following chemotherapy. Patients who received the vaccine demonstrated significantly longer disease-free survival.
But, at the time, personalized vaccines faced strong headwinds due, largely, to high costs, and commercial interest failed to materialize. “That’s been the major hurdle for a long time,” said Kwak.
Now, however, interest has returned alongside advances in technology and research. The big shift has been the emergence of lower-cost rapid-production mRNA and DNA platforms and a better understanding of how vaccines and potent immune stimulants, like checkpoint inhibitors, can work together to improve outcomes, he explained.
“The timing wasn’t right” back then, Kwak noted. “Now, it’s a different environment and a different time.”
A Turning Point?
Indeed, a decade later, cancer vaccine development appears to be headed in a more promising direction.
Among key cancer vaccines to watch is the mRNA-4157 vaccine, developed by Merck and Moderna, designed to prevent melanoma recurrence. In a recent phase 2 study, patients receiving the mRNA-4157 vaccine alongside pembrolizumab had nearly half the risk for melanoma recurrence or death at 3 years compared with those receiving pembrolizumab alone. Investigators are now evaluating the vaccine in a global phase 3 study in patients with high-risk, stage IIB to IV melanoma following surgery.
Another one to watch is the BNT116 NSCLC vaccine from BioNTech. This vaccine presents the immune system with NSCLC tumor markers to encourage the body to fight cancer cells expressing those markers while ignoring healthy cells. BioNTech also launched a global clinical trial for its vaccine this year.
Other notables include a pancreatic cancer mRNA vaccine, which has shown promising early results in a small trial of 16 patients. Of 16 patients who received the vaccine alongside chemotherapy and after surgery and immunotherapy, 8 responded. Of these eight, six remained recurrence free at 3 years. Investigators noted that the vaccine appeared to stimulate a durable T-cell response in patients who responded.
Kwak has also continued his work on lymphoma vaccines. In August, his team published promising first-in-human data on the use of personalized neoantigen vaccines as an early intervention in untreated patients with lymphoplasmacytic lymphoma. Among nine asymptomatic patients who received the vaccine, all achieved stable disease or better, with no dose-limiting toxicities. One patient had a minor response, and the median time to progression was greater than 72 months.
“The current setting is more for advanced disease,” Kwak explained. “It’s a tougher task, but combined with checkpoint blockade, it may be potent enough to work.”
Still, caution is important. Despite early promise, it’s too soon to tell which, if any, of these investigational vaccines will pan out in the long run. Like investigational drugs, cancer vaccines may show big promising initially but then fail in larger trials.
One key to success, according to Kwak, is to design trials so that even negative results will inform next steps.
But, he noted, failures in large clinical trials will “put a chilling effect on cancer vaccine research again.”
“That’s what keeps me up at night,” he said. “We know the science is fundamentally sound and we have seen glimpses over decades of research that cancer vaccines can work, so it’s really just a matter of tweaking things to optimize trial design.”
Companies tend to design trials to test if a vaccine works or not, without trying to understand why, he said.
“What we need to do is design those so that we can learn from negative results,” he said. That’s what he and his colleagues attempted to do in their recent trial. “We didn’t just look at clinical results; we’re interrogating the actual tumor environment to understand what worked and didn’t and how to tweak that for the next trial.”
Kwak and his colleagues found, for instance, that the vaccine had a greater effect on B cell–derived tumor cells than on cells of plasma origin, so “the most rational design for the next iteration is to combine the vaccine with agents that work directly against plasma cells,” he explained.
As for what’s next, Kwak said: “We’re just focused on trying to do good science and understand. We’ve seen glimpses of success. That’s where we are.”
A version of this article first appeared on Medscape.com.
Inside the Patient-Oncologist Bond: Why It’s Often So Strong
Rose Gerber was 39, mother to a third grader and a kindergartener, when the diagnosis came: Advanced HER2-positive breast cancer.
“On one of my first or second appointments, I took in a little picture of Alexander and Isabella,” Gerber said. Gerber showed her oncologist the picture and told her: “I’ll do anything. I just want to be there for them.”
That was 21 years ago. Today, her current cancer status is “no evidence of disease.”
Over the past 2 decades, Gerber has gotten to be there for her children. Her youngest is now a television producer and her oldest, a CPA.
In that time,
“I’ve seen multiple physicians over my 21 years, but my oncologist has always been the focal point, guiding me in the right direction,” Gerber said in an interview.
Over the years, Jaga guided Gerber through a range of treatment decisions, including a Herceptin clinical trial that the mom of two views as lifesaving. Jaga often took on the role of both doctor and therapist, even providing comfort in the smaller moments when Gerber would fret about her weight gain.
The oncologist-patient “bond is very, very, very special,” said Gerber, who now works as director of patient advocacy and education at the Community Oncology Alliance.
Gerber isn’t alone in calling out the depth of the oncologist-patient bond.
Over years, sometimes decades, patients and oncologists can experience a whole world together: The treatment successes, relapses, uncertainties, and tough calls. As a result, a deep therapeutic alliance often develops. And with each new hurdle or decision, that collaborative, human connection between doctor and patient continues to form new layers.
“It’s like a shared bonding experience over trauma, like strangers trapped on a subway and then we get out, and we’re now on the other side, celebrating together,” said Saad Khan, MD, an associate professor of medicine (oncology) at Stanford University in California.
Connecting Through Stress
Although studies exploring the oncologist-patient bond are limited, some research suggests that a strong therapeutic alliance between patients and oncologists not only provides a foundation for quality care but can also help improve patients’ quality of life, protect against suicidal ideation, and increase treatment adherence.
Because of how stressful and frightening a cancer diagnosis can be, creating “a trusting, uninterrupted, almost sacred environment for them” is paramount for Khan. “I have no doubt that the most important part of their treatment is that they find an oncologist in whom they have total confidence,” Khan wrote in a blog.
The stress that patients with cancer experience is well documented, but oncologists take on a lot themselves and can also experience intense stress (.
“I consider my patient’s battles to be my battles,” Khan wrote.
The stress can start with the daily schedule. Oncologists often have a high volume of patients and tend to spend more time with each individual than most.
According to a 2023 survey, oncologists see about 68 patients a week, on average, but some oncologists, like Khan, have many more. Khan typically sees 20-30 patients a day and continues to care for many over years.
The survey also found that oncologists tend to spend a lot of time with their patients. Compared with other physicians, oncologists are two times more likely to spend at least 25 minutes with each patient.
With this kind of patient volume and time, Khan said, “you’re going to be exhausted.”
What can compound the exhaustion are the occasions oncologists need to deliver bad news — this treatment isn’t working, your cancer has come roaring back and, perhaps the hardest, we have no therapeutic options left. The end-of-life conversations, in particular, can be heartbreaking, especially when a patient is young and not ready to stop trying.
“It can be hard for doctors to discuss the end of life,” Don Dizon, MD, director of the Pelvic Malignancies Program at Lifespan Cancer Institute and director of Medical Oncology at Rhode Island Hospital, Providence, wrote in a column in 2023. Instead, it can be tempting and is often easier to focus on the next treatment, “instilling hope that there’s more that can be done,” even if doing more will only do harm.
In the face of these challenging decisions, growing a personal connection with patients over time can help keep oncologists going.
“We’re not just chemotherapy salesmen,” Khan said in an interview. “We get to know their social support network, who’s going to be driving them [to and from appointments], where they go on vacation, their cat’s name, who their neighbors are.”
A ‘Special Relationship’
Ralph V. Boccia, MD, is often asked what he does.
The next question that often comes — “Why do I do what I do?” — is Boccia’s favorite.
“Someone needs to take these patients through their journey,” Boccia, the founder of The Center for Cancer and Blood Disorders, Bethesda, Maryland, typically responds. He also often notes that “it is a special relationship you develop with the patient and their families.”
Boccia thinks about one long-term patient who captures this bond.
Joan Pinson, 70, was diagnosed with multiple myeloma about 25 years ago, when patients’ average survival was about 4 years.
Over a quarter century, Pinson has pivoted to different treatments, amid multiple relapses and remissions. Throughout most of this cancer journey, Boccia has been her primary oncologist, performing a stem cell transplant in 2000 and steering her to six clinical trials.
Her last relapse was 2 years ago, and since then she has been doing well on oral chemotherapy.
“Every time I relapsed, by the next appointment, he’d say, ‘here is what we are going to do,’ ” Pinson recalled. “I never worried, I never panicked. I knew he would take care of me.”
Over the years, Pinson and Boccia have shared many personal moments, sometimes by accident. One special moment happened early on in Pinson’s cancer journey. During an appointment, Boccia had “one ear to the phone” as his wife was about to deliver their first baby, Pinson recalled.
Later, Pinson met that child as a young man working in Boccia’s lab. She has also met Boccia’s wife, a nurse, when she filled in one day in the chemotherapy room.
Boccia now also treats Pinson’s husband who has prostate cancer, and he ruled out cancer when Pinson’s son, now in his 40s, had some worrisome symptoms.
More than 2 decades ago, Pinson told Boccia her goal was to see her youngest child graduate from high school. Now, six grandsons later, she has lived far beyond that goal.
“He has kept me alive,” said Pinson.
The Dying Patient
Harsha Vyas, MD, FACP, remembers the first encounter his office had with a 29-year-old woman referred with a diagnosis of stage IV breast cancer.
After just 15 minutes in the waiting room, the woman announced she was leaving. Although office staff assured the woman that she was next, the patient walked out.
Several months later, Vyas was called for an inpatient consult. It was the same woman.
Her lungs were full of fluid, and she was struggling to breathe, said Vyas, president and CEO of the Cancer Center of Middle Georgia, Dublin, and assistant professor at Augusta University in Georgia.
The woman, a single mother, told Vyas about her three young kids at home and asked him, “Doc, do something, please help me,” he recalled.
“Absolutely,” Vyas told her. But he had to be brutally honest about her prognosis and firm that she needed to follow his instructions. “You have a breast cancer I cannot cure,” he said. “All I can do is control the disease.”
From that first day, until the day she died, she came to every appointment and followed the treatment plan Vyas laid out.
For about 2 years, she responded well to treatment. And as the time passed and the trust grew, she began to open up to him. She showed him pictures. She talked about her children and being a mother.
“I’ve got to get my kids in a better place. I’m going to be there for them,” he recalled her saying.
Vyas admired her resourcefulness. She held down a part-time job, working retail and at a local restaurant. She figured out childcare so she could get to her chemotherapy appointments every 3 weeks and manage the copays.
Several years later, when she knew she was approaching the end of her life, she asked Vyas a question that hit hard.
“Doc, I don’t want to die and my kids find me dead. What can we do about it?”
Vyas, who has three daughters, imagined how traumatic this would be for a child. She and Vyas made the shared decision to cease treatment and begin home hospice. When the end was approaching, a hospice worker took over, waiting for bodily functions to cease.
When news of a death comes, “I say a little prayer, it’s almost like a send-off for that soul. That helps me absorb the news ... and let it go.”
But when the bond grows strong over time, as with his patient with breast cancer, Vyas said, “a piece of her is still with me.”
Khan had no relevant disclosures. Boccia and Vyas had no disclosures.
A version of this article appeared on Medscape.com.
Rose Gerber was 39, mother to a third grader and a kindergartener, when the diagnosis came: Advanced HER2-positive breast cancer.
“On one of my first or second appointments, I took in a little picture of Alexander and Isabella,” Gerber said. Gerber showed her oncologist the picture and told her: “I’ll do anything. I just want to be there for them.”
That was 21 years ago. Today, her current cancer status is “no evidence of disease.”
Over the past 2 decades, Gerber has gotten to be there for her children. Her youngest is now a television producer and her oldest, a CPA.
In that time,
“I’ve seen multiple physicians over my 21 years, but my oncologist has always been the focal point, guiding me in the right direction,” Gerber said in an interview.
Over the years, Jaga guided Gerber through a range of treatment decisions, including a Herceptin clinical trial that the mom of two views as lifesaving. Jaga often took on the role of both doctor and therapist, even providing comfort in the smaller moments when Gerber would fret about her weight gain.
The oncologist-patient “bond is very, very, very special,” said Gerber, who now works as director of patient advocacy and education at the Community Oncology Alliance.
Gerber isn’t alone in calling out the depth of the oncologist-patient bond.
Over years, sometimes decades, patients and oncologists can experience a whole world together: The treatment successes, relapses, uncertainties, and tough calls. As a result, a deep therapeutic alliance often develops. And with each new hurdle or decision, that collaborative, human connection between doctor and patient continues to form new layers.
“It’s like a shared bonding experience over trauma, like strangers trapped on a subway and then we get out, and we’re now on the other side, celebrating together,” said Saad Khan, MD, an associate professor of medicine (oncology) at Stanford University in California.
Connecting Through Stress
Although studies exploring the oncologist-patient bond are limited, some research suggests that a strong therapeutic alliance between patients and oncologists not only provides a foundation for quality care but can also help improve patients’ quality of life, protect against suicidal ideation, and increase treatment adherence.
Because of how stressful and frightening a cancer diagnosis can be, creating “a trusting, uninterrupted, almost sacred environment for them” is paramount for Khan. “I have no doubt that the most important part of their treatment is that they find an oncologist in whom they have total confidence,” Khan wrote in a blog.
The stress that patients with cancer experience is well documented, but oncologists take on a lot themselves and can also experience intense stress (.
“I consider my patient’s battles to be my battles,” Khan wrote.
The stress can start with the daily schedule. Oncologists often have a high volume of patients and tend to spend more time with each individual than most.
According to a 2023 survey, oncologists see about 68 patients a week, on average, but some oncologists, like Khan, have many more. Khan typically sees 20-30 patients a day and continues to care for many over years.
The survey also found that oncologists tend to spend a lot of time with their patients. Compared with other physicians, oncologists are two times more likely to spend at least 25 minutes with each patient.
With this kind of patient volume and time, Khan said, “you’re going to be exhausted.”
What can compound the exhaustion are the occasions oncologists need to deliver bad news — this treatment isn’t working, your cancer has come roaring back and, perhaps the hardest, we have no therapeutic options left. The end-of-life conversations, in particular, can be heartbreaking, especially when a patient is young and not ready to stop trying.
“It can be hard for doctors to discuss the end of life,” Don Dizon, MD, director of the Pelvic Malignancies Program at Lifespan Cancer Institute and director of Medical Oncology at Rhode Island Hospital, Providence, wrote in a column in 2023. Instead, it can be tempting and is often easier to focus on the next treatment, “instilling hope that there’s more that can be done,” even if doing more will only do harm.
In the face of these challenging decisions, growing a personal connection with patients over time can help keep oncologists going.
“We’re not just chemotherapy salesmen,” Khan said in an interview. “We get to know their social support network, who’s going to be driving them [to and from appointments], where they go on vacation, their cat’s name, who their neighbors are.”
A ‘Special Relationship’
Ralph V. Boccia, MD, is often asked what he does.
The next question that often comes — “Why do I do what I do?” — is Boccia’s favorite.
“Someone needs to take these patients through their journey,” Boccia, the founder of The Center for Cancer and Blood Disorders, Bethesda, Maryland, typically responds. He also often notes that “it is a special relationship you develop with the patient and their families.”
Boccia thinks about one long-term patient who captures this bond.
Joan Pinson, 70, was diagnosed with multiple myeloma about 25 years ago, when patients’ average survival was about 4 years.
Over a quarter century, Pinson has pivoted to different treatments, amid multiple relapses and remissions. Throughout most of this cancer journey, Boccia has been her primary oncologist, performing a stem cell transplant in 2000 and steering her to six clinical trials.
Her last relapse was 2 years ago, and since then she has been doing well on oral chemotherapy.
“Every time I relapsed, by the next appointment, he’d say, ‘here is what we are going to do,’ ” Pinson recalled. “I never worried, I never panicked. I knew he would take care of me.”
Over the years, Pinson and Boccia have shared many personal moments, sometimes by accident. One special moment happened early on in Pinson’s cancer journey. During an appointment, Boccia had “one ear to the phone” as his wife was about to deliver their first baby, Pinson recalled.
Later, Pinson met that child as a young man working in Boccia’s lab. She has also met Boccia’s wife, a nurse, when she filled in one day in the chemotherapy room.
Boccia now also treats Pinson’s husband who has prostate cancer, and he ruled out cancer when Pinson’s son, now in his 40s, had some worrisome symptoms.
More than 2 decades ago, Pinson told Boccia her goal was to see her youngest child graduate from high school. Now, six grandsons later, she has lived far beyond that goal.
“He has kept me alive,” said Pinson.
The Dying Patient
Harsha Vyas, MD, FACP, remembers the first encounter his office had with a 29-year-old woman referred with a diagnosis of stage IV breast cancer.
After just 15 minutes in the waiting room, the woman announced she was leaving. Although office staff assured the woman that she was next, the patient walked out.
Several months later, Vyas was called for an inpatient consult. It was the same woman.
Her lungs were full of fluid, and she was struggling to breathe, said Vyas, president and CEO of the Cancer Center of Middle Georgia, Dublin, and assistant professor at Augusta University in Georgia.
The woman, a single mother, told Vyas about her three young kids at home and asked him, “Doc, do something, please help me,” he recalled.
“Absolutely,” Vyas told her. But he had to be brutally honest about her prognosis and firm that she needed to follow his instructions. “You have a breast cancer I cannot cure,” he said. “All I can do is control the disease.”
From that first day, until the day she died, she came to every appointment and followed the treatment plan Vyas laid out.
For about 2 years, she responded well to treatment. And as the time passed and the trust grew, she began to open up to him. She showed him pictures. She talked about her children and being a mother.
“I’ve got to get my kids in a better place. I’m going to be there for them,” he recalled her saying.
Vyas admired her resourcefulness. She held down a part-time job, working retail and at a local restaurant. She figured out childcare so she could get to her chemotherapy appointments every 3 weeks and manage the copays.
Several years later, when she knew she was approaching the end of her life, she asked Vyas a question that hit hard.
“Doc, I don’t want to die and my kids find me dead. What can we do about it?”
Vyas, who has three daughters, imagined how traumatic this would be for a child. She and Vyas made the shared decision to cease treatment and begin home hospice. When the end was approaching, a hospice worker took over, waiting for bodily functions to cease.
When news of a death comes, “I say a little prayer, it’s almost like a send-off for that soul. That helps me absorb the news ... and let it go.”
But when the bond grows strong over time, as with his patient with breast cancer, Vyas said, “a piece of her is still with me.”
Khan had no relevant disclosures. Boccia and Vyas had no disclosures.
A version of this article appeared on Medscape.com.
Rose Gerber was 39, mother to a third grader and a kindergartener, when the diagnosis came: Advanced HER2-positive breast cancer.
“On one of my first or second appointments, I took in a little picture of Alexander and Isabella,” Gerber said. Gerber showed her oncologist the picture and told her: “I’ll do anything. I just want to be there for them.”
That was 21 years ago. Today, her current cancer status is “no evidence of disease.”
Over the past 2 decades, Gerber has gotten to be there for her children. Her youngest is now a television producer and her oldest, a CPA.
In that time,
“I’ve seen multiple physicians over my 21 years, but my oncologist has always been the focal point, guiding me in the right direction,” Gerber said in an interview.
Over the years, Jaga guided Gerber through a range of treatment decisions, including a Herceptin clinical trial that the mom of two views as lifesaving. Jaga often took on the role of both doctor and therapist, even providing comfort in the smaller moments when Gerber would fret about her weight gain.
The oncologist-patient “bond is very, very, very special,” said Gerber, who now works as director of patient advocacy and education at the Community Oncology Alliance.
Gerber isn’t alone in calling out the depth of the oncologist-patient bond.
Over years, sometimes decades, patients and oncologists can experience a whole world together: The treatment successes, relapses, uncertainties, and tough calls. As a result, a deep therapeutic alliance often develops. And with each new hurdle or decision, that collaborative, human connection between doctor and patient continues to form new layers.
“It’s like a shared bonding experience over trauma, like strangers trapped on a subway and then we get out, and we’re now on the other side, celebrating together,” said Saad Khan, MD, an associate professor of medicine (oncology) at Stanford University in California.
Connecting Through Stress
Although studies exploring the oncologist-patient bond are limited, some research suggests that a strong therapeutic alliance between patients and oncologists not only provides a foundation for quality care but can also help improve patients’ quality of life, protect against suicidal ideation, and increase treatment adherence.
Because of how stressful and frightening a cancer diagnosis can be, creating “a trusting, uninterrupted, almost sacred environment for them” is paramount for Khan. “I have no doubt that the most important part of their treatment is that they find an oncologist in whom they have total confidence,” Khan wrote in a blog.
The stress that patients with cancer experience is well documented, but oncologists take on a lot themselves and can also experience intense stress (.
“I consider my patient’s battles to be my battles,” Khan wrote.
The stress can start with the daily schedule. Oncologists often have a high volume of patients and tend to spend more time with each individual than most.
According to a 2023 survey, oncologists see about 68 patients a week, on average, but some oncologists, like Khan, have many more. Khan typically sees 20-30 patients a day and continues to care for many over years.
The survey also found that oncologists tend to spend a lot of time with their patients. Compared with other physicians, oncologists are two times more likely to spend at least 25 minutes with each patient.
With this kind of patient volume and time, Khan said, “you’re going to be exhausted.”
What can compound the exhaustion are the occasions oncologists need to deliver bad news — this treatment isn’t working, your cancer has come roaring back and, perhaps the hardest, we have no therapeutic options left. The end-of-life conversations, in particular, can be heartbreaking, especially when a patient is young and not ready to stop trying.
“It can be hard for doctors to discuss the end of life,” Don Dizon, MD, director of the Pelvic Malignancies Program at Lifespan Cancer Institute and director of Medical Oncology at Rhode Island Hospital, Providence, wrote in a column in 2023. Instead, it can be tempting and is often easier to focus on the next treatment, “instilling hope that there’s more that can be done,” even if doing more will only do harm.
In the face of these challenging decisions, growing a personal connection with patients over time can help keep oncologists going.
“We’re not just chemotherapy salesmen,” Khan said in an interview. “We get to know their social support network, who’s going to be driving them [to and from appointments], where they go on vacation, their cat’s name, who their neighbors are.”
A ‘Special Relationship’
Ralph V. Boccia, MD, is often asked what he does.
The next question that often comes — “Why do I do what I do?” — is Boccia’s favorite.
“Someone needs to take these patients through their journey,” Boccia, the founder of The Center for Cancer and Blood Disorders, Bethesda, Maryland, typically responds. He also often notes that “it is a special relationship you develop with the patient and their families.”
Boccia thinks about one long-term patient who captures this bond.
Joan Pinson, 70, was diagnosed with multiple myeloma about 25 years ago, when patients’ average survival was about 4 years.
Over a quarter century, Pinson has pivoted to different treatments, amid multiple relapses and remissions. Throughout most of this cancer journey, Boccia has been her primary oncologist, performing a stem cell transplant in 2000 and steering her to six clinical trials.
Her last relapse was 2 years ago, and since then she has been doing well on oral chemotherapy.
“Every time I relapsed, by the next appointment, he’d say, ‘here is what we are going to do,’ ” Pinson recalled. “I never worried, I never panicked. I knew he would take care of me.”
Over the years, Pinson and Boccia have shared many personal moments, sometimes by accident. One special moment happened early on in Pinson’s cancer journey. During an appointment, Boccia had “one ear to the phone” as his wife was about to deliver their first baby, Pinson recalled.
Later, Pinson met that child as a young man working in Boccia’s lab. She has also met Boccia’s wife, a nurse, when she filled in one day in the chemotherapy room.
Boccia now also treats Pinson’s husband who has prostate cancer, and he ruled out cancer when Pinson’s son, now in his 40s, had some worrisome symptoms.
More than 2 decades ago, Pinson told Boccia her goal was to see her youngest child graduate from high school. Now, six grandsons later, she has lived far beyond that goal.
“He has kept me alive,” said Pinson.
The Dying Patient
Harsha Vyas, MD, FACP, remembers the first encounter his office had with a 29-year-old woman referred with a diagnosis of stage IV breast cancer.
After just 15 minutes in the waiting room, the woman announced she was leaving. Although office staff assured the woman that she was next, the patient walked out.
Several months later, Vyas was called for an inpatient consult. It was the same woman.
Her lungs were full of fluid, and she was struggling to breathe, said Vyas, president and CEO of the Cancer Center of Middle Georgia, Dublin, and assistant professor at Augusta University in Georgia.
The woman, a single mother, told Vyas about her three young kids at home and asked him, “Doc, do something, please help me,” he recalled.
“Absolutely,” Vyas told her. But he had to be brutally honest about her prognosis and firm that she needed to follow his instructions. “You have a breast cancer I cannot cure,” he said. “All I can do is control the disease.”
From that first day, until the day she died, she came to every appointment and followed the treatment plan Vyas laid out.
For about 2 years, she responded well to treatment. And as the time passed and the trust grew, she began to open up to him. She showed him pictures. She talked about her children and being a mother.
“I’ve got to get my kids in a better place. I’m going to be there for them,” he recalled her saying.
Vyas admired her resourcefulness. She held down a part-time job, working retail and at a local restaurant. She figured out childcare so she could get to her chemotherapy appointments every 3 weeks and manage the copays.
Several years later, when she knew she was approaching the end of her life, she asked Vyas a question that hit hard.
“Doc, I don’t want to die and my kids find me dead. What can we do about it?”
Vyas, who has three daughters, imagined how traumatic this would be for a child. She and Vyas made the shared decision to cease treatment and begin home hospice. When the end was approaching, a hospice worker took over, waiting for bodily functions to cease.
When news of a death comes, “I say a little prayer, it’s almost like a send-off for that soul. That helps me absorb the news ... and let it go.”
But when the bond grows strong over time, as with his patient with breast cancer, Vyas said, “a piece of her is still with me.”
Khan had no relevant disclosures. Boccia and Vyas had no disclosures.
A version of this article appeared on Medscape.com.
NCCN Expands Cancer Genetic Risk Assessment Guidelines
Additional cancer types were included in the title and content for both guidelines. Prostate cancer was added to Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate, and endometrial and gastric cancer were added to Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, and Gastric.
For these cancers, the expanded guidelines include information on when genetic testing is recommended and what type of testing may be best. These guidelines also detail the hereditary conditions and genetic mutations associated with elevated cancer risk and include appropriate “next steps” for individuals who have them, which may involve increased screening or prevention surgeries.
“These updates include the spectrum of genes associated with genetic syndromes, the range of risk associated with each pathogenic variant, the improvements in screening and prevention strategies, the role of genetic data to inform cancer treatment, and the expansion of the role of genetic counseling as this field moves forward,” Mary B. Daly, MD, PhD, with Fox Chase Cancer Center, Philadelphia, Pennsylvania, said in a news release. Daly chaired the panel that updated the breast, ovarian, pancreatic, and prostate cancer guidelines.
Oncologists should, for instance, ask patients about their family and personal history of cancer and known germline variants at time of initial diagnosis. With prostate cancer, if patients meet criteria for germline testing, multigene testing should include a host of variants, including BRCA1, BRCA2, ATM, PALB2, CHEK2, HOXB13, MLH1, MSH2, MSH6, and PMS2.
The updated guidelines on genetic risk assessment of colorectal, endometrial, and gastric cancer include new recommendations to consider for hereditary cancer screening in patients with newly diagnosed endometrial cancer, for evaluating and managing CDH1-associated gastric cancer risk, and for managing gastric cancer risk in patients with APC pathogenic variants.
For CDH1-associated gastric cancer, for instance, the guidelines recommend carriers be referred to institutions with expertise in managing risks for cancer associated with CDH1, “given the still limited understanding and rarity of this syndrome.”
“These expanded guidelines reflect the recommendations from leading experts on genetic testing based on the latest scientific research across the cancer spectrum, consolidated into two convenient resources,” said NCCN CEO Crystal S. Denlinger, MD, with Fox Chase Cancer Center, in a news release.
“This information is critical for guiding shared decision-making between health care providers and their patients, enhancing screening practices as appropriate, and potentially choosing options for prevention and targeted treatment choices. Genetic testing guidelines enable us to better care for people with cancer and their family members,” Denlinger added.
A version of this article first appeared on Medscape.com.
Additional cancer types were included in the title and content for both guidelines. Prostate cancer was added to Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate, and endometrial and gastric cancer were added to Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, and Gastric.
For these cancers, the expanded guidelines include information on when genetic testing is recommended and what type of testing may be best. These guidelines also detail the hereditary conditions and genetic mutations associated with elevated cancer risk and include appropriate “next steps” for individuals who have them, which may involve increased screening or prevention surgeries.
“These updates include the spectrum of genes associated with genetic syndromes, the range of risk associated with each pathogenic variant, the improvements in screening and prevention strategies, the role of genetic data to inform cancer treatment, and the expansion of the role of genetic counseling as this field moves forward,” Mary B. Daly, MD, PhD, with Fox Chase Cancer Center, Philadelphia, Pennsylvania, said in a news release. Daly chaired the panel that updated the breast, ovarian, pancreatic, and prostate cancer guidelines.
Oncologists should, for instance, ask patients about their family and personal history of cancer and known germline variants at time of initial diagnosis. With prostate cancer, if patients meet criteria for germline testing, multigene testing should include a host of variants, including BRCA1, BRCA2, ATM, PALB2, CHEK2, HOXB13, MLH1, MSH2, MSH6, and PMS2.
The updated guidelines on genetic risk assessment of colorectal, endometrial, and gastric cancer include new recommendations to consider for hereditary cancer screening in patients with newly diagnosed endometrial cancer, for evaluating and managing CDH1-associated gastric cancer risk, and for managing gastric cancer risk in patients with APC pathogenic variants.
For CDH1-associated gastric cancer, for instance, the guidelines recommend carriers be referred to institutions with expertise in managing risks for cancer associated with CDH1, “given the still limited understanding and rarity of this syndrome.”
“These expanded guidelines reflect the recommendations from leading experts on genetic testing based on the latest scientific research across the cancer spectrum, consolidated into two convenient resources,” said NCCN CEO Crystal S. Denlinger, MD, with Fox Chase Cancer Center, in a news release.
“This information is critical for guiding shared decision-making between health care providers and their patients, enhancing screening practices as appropriate, and potentially choosing options for prevention and targeted treatment choices. Genetic testing guidelines enable us to better care for people with cancer and their family members,” Denlinger added.
A version of this article first appeared on Medscape.com.
Additional cancer types were included in the title and content for both guidelines. Prostate cancer was added to Genetic/Familial High-Risk Assessment: Breast, Ovarian, Pancreatic, and Prostate, and endometrial and gastric cancer were added to Genetic/Familial High-Risk Assessment: Colorectal, Endometrial, and Gastric.
For these cancers, the expanded guidelines include information on when genetic testing is recommended and what type of testing may be best. These guidelines also detail the hereditary conditions and genetic mutations associated with elevated cancer risk and include appropriate “next steps” for individuals who have them, which may involve increased screening or prevention surgeries.
“These updates include the spectrum of genes associated with genetic syndromes, the range of risk associated with each pathogenic variant, the improvements in screening and prevention strategies, the role of genetic data to inform cancer treatment, and the expansion of the role of genetic counseling as this field moves forward,” Mary B. Daly, MD, PhD, with Fox Chase Cancer Center, Philadelphia, Pennsylvania, said in a news release. Daly chaired the panel that updated the breast, ovarian, pancreatic, and prostate cancer guidelines.
Oncologists should, for instance, ask patients about their family and personal history of cancer and known germline variants at time of initial diagnosis. With prostate cancer, if patients meet criteria for germline testing, multigene testing should include a host of variants, including BRCA1, BRCA2, ATM, PALB2, CHEK2, HOXB13, MLH1, MSH2, MSH6, and PMS2.
The updated guidelines on genetic risk assessment of colorectal, endometrial, and gastric cancer include new recommendations to consider for hereditary cancer screening in patients with newly diagnosed endometrial cancer, for evaluating and managing CDH1-associated gastric cancer risk, and for managing gastric cancer risk in patients with APC pathogenic variants.
For CDH1-associated gastric cancer, for instance, the guidelines recommend carriers be referred to institutions with expertise in managing risks for cancer associated with CDH1, “given the still limited understanding and rarity of this syndrome.”
“These expanded guidelines reflect the recommendations from leading experts on genetic testing based on the latest scientific research across the cancer spectrum, consolidated into two convenient resources,” said NCCN CEO Crystal S. Denlinger, MD, with Fox Chase Cancer Center, in a news release.
“This information is critical for guiding shared decision-making between health care providers and their patients, enhancing screening practices as appropriate, and potentially choosing options for prevention and targeted treatment choices. Genetic testing guidelines enable us to better care for people with cancer and their family members,” Denlinger added.
A version of this article first appeared on Medscape.com.
Many Patients With Cancer Visit EDs Before Diagnosis
Researchers examined Institute for Clinical Evaluative Sciences (ICES) data that had been gathered from January 1, 2014, to December 31, 2021. The study focused on patients aged 18 years or older with confirmed primary cancer diagnoses.
Factors associated with an increased likelihood of an ED visit ahead of diagnosis included having certain cancers, living in rural areas, and having less access to primary care, according to study author Keerat Grewal, MD, an emergency physician and clinician scientist at the Schwartz/Reisman Emergency Medicine Institute at Sinai Health in Toronto, Ontario, Canada, and coauthors.
“The ED is a distressing environment for patients to receive a possible cancer diagnosis,” the authors wrote. “Moreover, it is frequently ill equipped to provide ongoing continuity of care, which can lead patients down a poorly defined diagnostic pathway before receiving a confirmed diagnosis based on tissue and a subsequent treatment plan.”
The findings were published online on November 4 in CMAJ).
Neurologic Cancers Prominent
In an interview, Grewal said in an interview that the study reflects her desire as an emergency room physician to understand why so many patients with cancer get the initial reports about their disease from clinicians whom they often have just met for the first time.
Among patients with an ED visit before cancer diagnosis, 51.4% were admitted to hospital from the most recent visit.
Compared with patients with a family physician on whom they could rely for routine care, those who had no outpatient visits (odds ratio [OR], 2.09) or fewer than three outpatient visits (OR, 1.41) in the 6-30 months before cancer diagnosis were more likely to have an ED visit before their cancer diagnosis.
Other factors associated with increased odds of ED use before cancer diagnosis included rurality (OR, 1.15), residence in northern Ontario (northeast region: OR, 1.14 and northwest region: OR, 1.27 vs Toronto region), and living in the most marginalized areas (material resource deprivation: OR, 1.37 and housing stability: OR, 1.09 vs least marginalized area).
The researchers also found that patients with certain cancers were more likely to have sought care in the ED. They compared these cancers with breast cancer, which is often detected through screening.
“Patients with neurologic cancers had extremely high odds of ED use before cancer diagnosis,” the authors wrote. “This is likely because of the emergent nature of presentation, with acute neurologic symptoms such as weakness, confusion, or seizures, which require urgent assessment.” On the other hand, pancreatic, liver, or thoracic cancer can trigger nonspecific symptoms that may be ignored until they reach a crisis level that prompts an ED visit.
The limitations of the study included its inability to identify cancer-related ED visits and its narrow focus on patients in Ontario, according to the researchers. But the use of the ICES databases also allowed researchers access to a broader pool of data than are available in many other cases.
The findings in the new paper echo those of previous research, the authors noted. Research in the United Kingdom found that 24%-31% of cancer diagnoses involved the ED. In addition, a study of people enrolled in the US Medicare program, which serves patients aged 65 years or older, found that 23% were seen in the ED in the 30 days before diagnosis.
‘Unpacking the Data’
The current findings also are consistent with those of an International Cancer Benchmarking Partnership study that was published in 2022 in The Lancet Oncology, said Erika Nicholson, MHS, vice president of cancer systems and innovation at the Canadian Partnership Against Cancer. The latter study analyzed cancer registration and linked hospital admissions data from 14 jurisdictions in Australia, Canada, Denmark, New Zealand, Norway, and the United Kingdom.
“We see similar trends in terms of people visiting EDs and being diagnosed through EDs internationally,” Nicholson said. “We’re working with partners to put in place different strategies to address the challenges” that this phenomenon presents in terms of improving screening and follow-up care.
“Cancer is not one disease, but many diseases,” she said. “They present differently. We’re focused on really unpacking the data and understanding them.”
All this research highlights the need for more services and personnel to address cancer, including people who are trained to help patients cope after getting concerning news through emergency care, she said.
“That means having a system that fully supports you and helps you navigate through that diagnostic process,” Nicholson said. Addressing the added challenges for patients who don’t have secure housing is a special need, she added.
This study was supported by the Canadian Institutes of Health Research (CIHR). Grewal reported receiving grants from CIHR and the Canadian Association of Emergency Physicians. Nicholson reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Researchers examined Institute for Clinical Evaluative Sciences (ICES) data that had been gathered from January 1, 2014, to December 31, 2021. The study focused on patients aged 18 years or older with confirmed primary cancer diagnoses.
Factors associated with an increased likelihood of an ED visit ahead of diagnosis included having certain cancers, living in rural areas, and having less access to primary care, according to study author Keerat Grewal, MD, an emergency physician and clinician scientist at the Schwartz/Reisman Emergency Medicine Institute at Sinai Health in Toronto, Ontario, Canada, and coauthors.
“The ED is a distressing environment for patients to receive a possible cancer diagnosis,” the authors wrote. “Moreover, it is frequently ill equipped to provide ongoing continuity of care, which can lead patients down a poorly defined diagnostic pathway before receiving a confirmed diagnosis based on tissue and a subsequent treatment plan.”
The findings were published online on November 4 in CMAJ).
Neurologic Cancers Prominent
In an interview, Grewal said in an interview that the study reflects her desire as an emergency room physician to understand why so many patients with cancer get the initial reports about their disease from clinicians whom they often have just met for the first time.
Among patients with an ED visit before cancer diagnosis, 51.4% were admitted to hospital from the most recent visit.
Compared with patients with a family physician on whom they could rely for routine care, those who had no outpatient visits (odds ratio [OR], 2.09) or fewer than three outpatient visits (OR, 1.41) in the 6-30 months before cancer diagnosis were more likely to have an ED visit before their cancer diagnosis.
Other factors associated with increased odds of ED use before cancer diagnosis included rurality (OR, 1.15), residence in northern Ontario (northeast region: OR, 1.14 and northwest region: OR, 1.27 vs Toronto region), and living in the most marginalized areas (material resource deprivation: OR, 1.37 and housing stability: OR, 1.09 vs least marginalized area).
The researchers also found that patients with certain cancers were more likely to have sought care in the ED. They compared these cancers with breast cancer, which is often detected through screening.
“Patients with neurologic cancers had extremely high odds of ED use before cancer diagnosis,” the authors wrote. “This is likely because of the emergent nature of presentation, with acute neurologic symptoms such as weakness, confusion, or seizures, which require urgent assessment.” On the other hand, pancreatic, liver, or thoracic cancer can trigger nonspecific symptoms that may be ignored until they reach a crisis level that prompts an ED visit.
The limitations of the study included its inability to identify cancer-related ED visits and its narrow focus on patients in Ontario, according to the researchers. But the use of the ICES databases also allowed researchers access to a broader pool of data than are available in many other cases.
The findings in the new paper echo those of previous research, the authors noted. Research in the United Kingdom found that 24%-31% of cancer diagnoses involved the ED. In addition, a study of people enrolled in the US Medicare program, which serves patients aged 65 years or older, found that 23% were seen in the ED in the 30 days before diagnosis.
‘Unpacking the Data’
The current findings also are consistent with those of an International Cancer Benchmarking Partnership study that was published in 2022 in The Lancet Oncology, said Erika Nicholson, MHS, vice president of cancer systems and innovation at the Canadian Partnership Against Cancer. The latter study analyzed cancer registration and linked hospital admissions data from 14 jurisdictions in Australia, Canada, Denmark, New Zealand, Norway, and the United Kingdom.
“We see similar trends in terms of people visiting EDs and being diagnosed through EDs internationally,” Nicholson said. “We’re working with partners to put in place different strategies to address the challenges” that this phenomenon presents in terms of improving screening and follow-up care.
“Cancer is not one disease, but many diseases,” she said. “They present differently. We’re focused on really unpacking the data and understanding them.”
All this research highlights the need for more services and personnel to address cancer, including people who are trained to help patients cope after getting concerning news through emergency care, she said.
“That means having a system that fully supports you and helps you navigate through that diagnostic process,” Nicholson said. Addressing the added challenges for patients who don’t have secure housing is a special need, she added.
This study was supported by the Canadian Institutes of Health Research (CIHR). Grewal reported receiving grants from CIHR and the Canadian Association of Emergency Physicians. Nicholson reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
Researchers examined Institute for Clinical Evaluative Sciences (ICES) data that had been gathered from January 1, 2014, to December 31, 2021. The study focused on patients aged 18 years or older with confirmed primary cancer diagnoses.
Factors associated with an increased likelihood of an ED visit ahead of diagnosis included having certain cancers, living in rural areas, and having less access to primary care, according to study author Keerat Grewal, MD, an emergency physician and clinician scientist at the Schwartz/Reisman Emergency Medicine Institute at Sinai Health in Toronto, Ontario, Canada, and coauthors.
“The ED is a distressing environment for patients to receive a possible cancer diagnosis,” the authors wrote. “Moreover, it is frequently ill equipped to provide ongoing continuity of care, which can lead patients down a poorly defined diagnostic pathway before receiving a confirmed diagnosis based on tissue and a subsequent treatment plan.”
The findings were published online on November 4 in CMAJ).
Neurologic Cancers Prominent
In an interview, Grewal said in an interview that the study reflects her desire as an emergency room physician to understand why so many patients with cancer get the initial reports about their disease from clinicians whom they often have just met for the first time.
Among patients with an ED visit before cancer diagnosis, 51.4% were admitted to hospital from the most recent visit.
Compared with patients with a family physician on whom they could rely for routine care, those who had no outpatient visits (odds ratio [OR], 2.09) or fewer than three outpatient visits (OR, 1.41) in the 6-30 months before cancer diagnosis were more likely to have an ED visit before their cancer diagnosis.
Other factors associated with increased odds of ED use before cancer diagnosis included rurality (OR, 1.15), residence in northern Ontario (northeast region: OR, 1.14 and northwest region: OR, 1.27 vs Toronto region), and living in the most marginalized areas (material resource deprivation: OR, 1.37 and housing stability: OR, 1.09 vs least marginalized area).
The researchers also found that patients with certain cancers were more likely to have sought care in the ED. They compared these cancers with breast cancer, which is often detected through screening.
“Patients with neurologic cancers had extremely high odds of ED use before cancer diagnosis,” the authors wrote. “This is likely because of the emergent nature of presentation, with acute neurologic symptoms such as weakness, confusion, or seizures, which require urgent assessment.” On the other hand, pancreatic, liver, or thoracic cancer can trigger nonspecific symptoms that may be ignored until they reach a crisis level that prompts an ED visit.
The limitations of the study included its inability to identify cancer-related ED visits and its narrow focus on patients in Ontario, according to the researchers. But the use of the ICES databases also allowed researchers access to a broader pool of data than are available in many other cases.
The findings in the new paper echo those of previous research, the authors noted. Research in the United Kingdom found that 24%-31% of cancer diagnoses involved the ED. In addition, a study of people enrolled in the US Medicare program, which serves patients aged 65 years or older, found that 23% were seen in the ED in the 30 days before diagnosis.
‘Unpacking the Data’
The current findings also are consistent with those of an International Cancer Benchmarking Partnership study that was published in 2022 in The Lancet Oncology, said Erika Nicholson, MHS, vice president of cancer systems and innovation at the Canadian Partnership Against Cancer. The latter study analyzed cancer registration and linked hospital admissions data from 14 jurisdictions in Australia, Canada, Denmark, New Zealand, Norway, and the United Kingdom.
“We see similar trends in terms of people visiting EDs and being diagnosed through EDs internationally,” Nicholson said. “We’re working with partners to put in place different strategies to address the challenges” that this phenomenon presents in terms of improving screening and follow-up care.
“Cancer is not one disease, but many diseases,” she said. “They present differently. We’re focused on really unpacking the data and understanding them.”
All this research highlights the need for more services and personnel to address cancer, including people who are trained to help patients cope after getting concerning news through emergency care, she said.
“That means having a system that fully supports you and helps you navigate through that diagnostic process,” Nicholson said. Addressing the added challenges for patients who don’t have secure housing is a special need, she added.
This study was supported by the Canadian Institutes of Health Research (CIHR). Grewal reported receiving grants from CIHR and the Canadian Association of Emergency Physicians. Nicholson reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM CMAJ