User login
Do Delayed Prescriptions Reduce the Use of Antibiotics for the Common Cold?
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
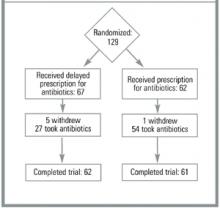
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
OBJECTIVE: To test the use of a delayed prescription compared with instructions to take antibiotics immediately in patients presenting to family physicians with upper respiratory tract infections (common colds).
STUDY DESIGN: Randomized controlled single-blind study.
POPULATION: Subjects were 129 patients presenting with the common cold who requested antibiotics or whose physicians thought they wanted them. All patients were in a family practice in Auckland, New Zealand, consisting of 15 physicians (9 male, 6 female) who had completed medical school between 1973 and 1992.
OUTCOMES MEASURED: Outcomes were antibiotic use (taking at least 1 dose of the antibiotic), symptom scores, and responses to the satisfaction questions asked at the end of the study.
RESULTS: Patients in the delayed-prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than were those instructed to take antibiotics immediately (89%, 95% CI, 76%-94%). Daily body temperature was higher in the immediate-prescription group. The lack of difference in the symptom score between the 2 groups suggests that there is no danger in delaying antibiotic prescriptions for the common cold.
CONCLUSIONS: Delayed prescriptions are a safe and effective means of reducing antibiotic consumption in patients with the common cold. Clarification of patient expectations for antibiotics may result in a lower prescription rate. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education.
- Delaying the prescription of antibiotics reduces antibiotic intake in patients who insist on taking antibiotics for the common cold.
- Giving a delayed prescription and asking the patient to return to the office to fill it may reduce antibiotic consumption further.
Antibiotics continue to be commonly used to treat the common cold1-3 despite longstanding doubts about their efficacy4,5 or ability to prevent complications.6 Upper respiratory tract infection (URTI) is the most common reason for a new consultation in family practice and the second most common reason for the prescribing of an antibiotic.7 Reported prescription rates for antibiotics for treating the common cold range from 17% to 60% in the United Kingdom and United States and 78% in New Zealand.1,8 Ineffective but widespread use of antibiotics is not only a poor use of health care funds but also a cause of morbidity (from adverse effects) and the development of resistant strains of bacteria.8-10
A promising technique to reduce antibiotic use is the delayed prescription. The only published randomized controlled trials of delayed prescription use examined its effect for the treatment of sore throat, acute childhood otitis media, and cough.11-13 In the sore throat study, antibiotics were used by 99% of a group given antibiotics, by 13% of a group not offered any, and 31% of a group given a prescription to be taken after 3 days if symptoms persisted. The authors of the otitis media study noted a 66% reduction of antibiotic use in the delayed-prescription group, who had more symptoms, signs, and sleepless nights than the “take-now” group. In the study with acute cough, the use of antibiotics was reduced by 55% in the group with delayed prescriptions. Our study, undertaken in winter 2000, tested the use of a delayed prescription versus instructions to take antibiotics immediately in patients presenting to general practitioners with URTIs.
Methods
The 15 family physicians (FPs) who recruited patients for this study were selected primarily from a group who had reported in a previous study that they frequently gave delayed prescriptions to patients.14 Ethical approval was given by the Auckland Ethics Committee.
Inclusion and exclusion criteria
Patients of any age were eligible if they presented to their FP with a new case of the common cold and either the FP thought the patient wanted antibiotics or the patient stated that desire. For young children, the parents indicated whether or not they wanted antibiotics. FPs were provided with the diagnostic criteria for URTI from the International Classification of Health Problems in Primary Care (ICHPPC-2), which defines an URTI as including the presence of acute inflammation of the nasal or pharyngeal mucosa in the absence of other specifically defined respiratory infection.15
Patients were excluded if they had suspected streptococcal tonsillitis, sinusitis, bronchitis, or pneumonia. Also excluded were patients with lower respiratory signs, those who needed an x-ray, those with a past history of rheumatic fever, and those who had experienced a serious illness or any antibiotic treatment in the previous 2 weeks. Throat cultures were not required. Eligible patients were invited to participate and signed an informed consent form. Ideally, the offer to join the study was to be made to consecutive patients, but this did not occur in all practices.
Interventions
The intervention group was given a prescription for antibiotics with instructions to fill it after 3 days if symptoms failed to improve. The control group received a prescription with instructions to start taking the antibiotic medication immediately. General practitioners prescribed any antibiotic that they considered most appropriate. In both groups, patients were advised to return to see their doctor if symptoms worsened.
Data collection
At recruitment, the patient’s temperature was taken and the list of symptoms was recorded in duplicate. The patient was asked to take his or her temperature daily with a digital thermometer (Assess Diagnostics Medical Industries Australia Pty. Ltd., 148-152 Regent St., Redfern NSW 2016, Australia) that was provided. Patients were given symptom checklists to complete daily for 10 days after the visit. Symptoms listed were dry cough, night cough, sneezing, sore throat, pain on inspiration, pain when coughing, hoarse voice, headache, staying home from work or unable to do normal daily tasks, unwell, diarrhea, vomiting, and nausea without vomiting. Patients were instructed to record whether they had a runny nose with clear secretions (“clear runny nose”), stuffy (blocked) nose, or runny nose with dark secretions (“colored runny nose”). Patients further checked off whether they had clear sputum only in the morning, colored sputum in the morning, clear sputum all day, or colored sputum all day.
A point was allocated for each symptom. The maximum possible score was 15.16 A study assistant telephoned all participants on day 3, day 7, and day 10 to ask about their temperature and symptoms. At the end of the study, the research assistant asked participants about their level of satisfaction with the consultation, using the questions and scoring system devised by Little et al.11 Although no data were collected about revisit rates, data were collected about the patient’s intention to visit a physician for the next cold.
Outcomes and analysis
The outcomes were antibiotic use, symptom scores, and the responses to satisfaction-related questions asked at the end of the study. Outcomes of intervention and control groups were compared on an intention-to-treat basis.17 Because of the repeated measures, the temperatures and summary scores of symptoms were determined with the general linear mixed model that uses Statistical Analysis System (SAS, Cary, N.C.), version 8, for Windows. Chi-square determinations and the Mantel-Haenszel odds ratio were performed for discrete variables using Statistical Package for the Social Sciences (SPSS), version 10, for Windows. When the final data point for continuous variables was missing, the last recorded value was analyzed as the current value. For discrete values, worst-case and best-case scenarios were performed. The sample size of 212 patients was based on a reduction from 60% of antibiotics consumed immediately to 40% in the delayed-prescription group (alpha 0.05, beta 0.2).
Allocation and masking
The unit of randomization was the patient. N.K., who was not a recruiter, generated the allocation schedule with Excel 97. Letters containing instructions for the intervention strategy pertaining to each patient or allocating the patient to the control group were placed in opaque envelopes and sealed. The study number was written on the outside of the envelope according to the randomization schedule. The envelopes were then given to the research assistant, who placed them in a large brown envelope with the consent forms and information sheets for recruiting family physicians. The recruiters opened each envelope immediately after recruitment of each patient.
Patients were told only that they would be given 1 of 2 sets of instruction about taking antibiotics for their colds. Participants read an information sheet and then completed a consent form. Thus, patients were blind to what the other group would take. The research assistant asked the participants not to tell her which instructions they had been given for taking antibiotics. If both types of blinding had been followed correctly, this study could be described as double blinded. However, because we cannot confirm the effectiveness of blinding the research assistant, we prefer to call this study single blinded. One copy of the allocation schedule was kept in the office of N.K.; another was kept by the departmental secretary.
Results
The Figure shows the trial profile summarizing participant flow. The baseline characteristics of the patients in both groups were similar (Table 1).
Patients in the delayed prescription group were less likely to use antibiotics (48%, 95% CI, 35%-60%) than those in the “take antibiotics now” group (89%, 95% CI, 76%-94%). The odds ratio for not using antibiotics was 0.12 (95% CI, 0.05 to 0.29) using intention-to-treat analysis. By antibiotic use, we mean that the patients consumed at least 1 dose of the antibiotic medication.
Table 2 shows the outcomes for temperature and symptom score using an intention-to-treat model. The general linear model for repeated measures found average temperature significantly higher (by 0.2°C) in the immediate antibiotic use group (P = .039) and no significant difference for the symptom score (P = .29). Reanalyzing with only collected data (without intention to treat) found no significant differences from the intention-to-treat analysis. The power to detect a difference in symptom score of 30% is 80% for an alpha of 0.05, assuming that the study gives measures of variation of the symptom score that are close to the real values. There were no significant adverse effects from taking antibiotics or not. Patients’ beliefs and intentions were not affected by the interventions (Table 3).
TABLE 1
BASELINE CHARACTERISTICS AND SYMPTOMS OF THE 2 GROUPS
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Characteristics | ||
| Number of patients | 62 | 67 |
| Male / female | 22 / 40 | 26 / 41 |
| Mean age (SD) | 27.9 years (3.1) | 23.6 years (2.7) |
| Cigarettes per day | 1.26 (0.47) | 1.17 (0.54) |
| Mean temperature (SD) | 36.9 (0.08) | 36.7 (0.08) |
| Days of illness before doctor’s visit | 4.5 (0.5) | 5.0 (0.7) |
| Total symptom score (SD) | 5.1 (0.28) | 5.4 (0.22) |
| Symptoms | ||
| Dry cough | 31 | 35 |
| Productive cough | ||
| Cough with clear sputum in morning | 8 | 5 |
| Cough with clear sputum all day | 6 | 7 |
| Cough with colored sputum in morning | 8 | 7 |
| Cough with colored sputum all day | 10 | 16 |
| Nasal symptoms | ||
| Clear rhinitis | 27 | 22 |
| Blocked or stuff nose | 21 | 26 |
| Colored runny nose | 12 | 15 |
| Night cough | 29 | 37 |
| Sneezing | 31 | 26 |
| Sore throat | 38 | 31 |
| Pain in chest on breathing in | 6 | 7 |
| Pain on coughing | 17 | 13 |
| Hoarse voice | 28 | 26 |
| Headache | 26 | 28 |
| Unwell* | 44* | 56* |
| Limitation of activities | 25 | 23 |
| Nausea | 7 | 6 |
| Vomiting | 5 | 6 |
| Diarrhea | 6 | 4 |
| * Pearson chi-square 9.134, 1 degree of freedom, P = .0025, 2 sided. | ||
| The number of patients recruited per family physician ranged from 1 to 40. | ||
| SD denotes standard deviation. | ||
TABLE 2
OUTCOMES AT BASELINE AND ON DAYS 3, 7, AND 10
| Immediate Prescription | Delayed Prescription | |
|---|---|---|
| Temperature (C)* | ||
| Baseline | 36.9 (0.1) | 36.7 (0.1) |
| Day 3 | 36.4 (0.1) | 36.2 (0.1) |
| Day 7 | 36.4 (0.1) | 36.1 (0.1) |
| Day 10 | 36.3 (0.1) | 36.1 (0.1) |
| Symptom Score (1 point for each of 15 symptoms in Table 1)* | ||
| Baseline | 5.1 (0.3) | 5.4 (0.2) |
| Day 3 | 2.9 (0.2) | 3.6 (0.3) |
| Day 7 | 1.8 (0.2) | 2.0 (0.3) |
| Day 10 | 1.4 (0.2) | 1.5 (0.2) |
| *The general linear model for repeated measures found the significantly higher temperature of 0.2°C in the immediate-use antibiotic versus that in the delayed-use group (P = .039) and no significant difference for the symptom score (P = .29). | ||
TABLE 3
SATISFACTION, ATTITUDES, AND BELIEFS
| Immediate Prescription | Delayed Prescription | P | |
|---|---|---|---|
| Satisfaction with the consultation; ie, score (1+2) / (1+2+3+4) | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Doctors dealt with worries | 58 / 62 (94%) | 64 / 67 (96%) | .71 * |
| Likely to see doctors for next common cold | 40 / 62 (65%) | 49 / 67 (73%) | .343 † |
| Antibiotics are effective | 47 / 62 (76%) | 51 / 67 (76%) | 1.0 † |
| Importance of seeing doctor to have time off from work or school | 19 / 62 (31%) | 13 / 54 (19%) | .16 † |
| Importance of seeing doctor to explain illness to friends and family | 6 / 62 (10%) | 7 / 60 (12%) | 1.00 † |
| * Fisher’s exact test. | |||
| † Chi-square test. | |||
| 1= very satisfied; 2 = moderately satisfied; 3 = slightly satisfied; 4 = not at all satisfied. For this table, groups responding 1 and 2 have been combined and groups responding 3 and 4 have been combined. | |||
FIGURE
PROGRESS OF PATIENTS THROUGH THE TRIAL
Discussion
We believe that this is the first published randomized controlled trial of delayed prescriptions for antibiotics for the common cold. Asking patients to wait for 3 days before taking their medication reduced consumption of antibiotics from 89% to 48% (P = .0001). The 41% reduction is smaller than that found in the study by Little and colleagues11 of 1% in the take-now group and 69% in the delayed-prescription group. Patients in the UK study returned to the office in 3 days to pick up their prescription, whereas the New Zealand group received the prescription with instructions to wait 3 days before filling it. If the third day had occurred on a weekend, the patients would have had to seek assistance from an after-hours clinic, thereby incurring a direct patient charge.
Our study assessed only the effect of delayed prescriptions, whereas the study by Little and colleagues tested the combined effect of a delayed prescription and the barrier of having to return to the clinic to obtain the prescription. Furthermore, our approach may be more acceptable to a wider group of doctors and patients, although at the expense of a higher consumption rate.
The external validity (generalizability) of this study is difficult to assess. As with the study by Little and colleagues,11 the FPs had different rates of recruitment. One investigator in the current study (B.A.) kept a list of all patients who presented to him with symptoms of the common cold. Of the 44 who were potentially eligible, 4 refused to be part of the study and 10 had other medical problems (eg, heart transplant, previous lung removal) that would have made inclusion potentially hazardous. Thus, 88% of those who had a common cold and were eligible may have participated in the study.
We do not know how many patients were excluded or refused to participate; the recruiting physicians did not supply this information as requested. There was no systematic difference in symptom scores for patients of the different recruiting doctors. As with the study by Little and colleagues, the doctors found themselves too busy to enroll patients. Such problems are always an issue in general practice research.18 Little and colleagues checked the internal validity of their telephone information; therefore, we did not repeat this. In an earlier study,14 the recruiting family physicians’ preference for using delayed prescriptions may have made them more supportive of the delayed prescription than of the immediate prescription. This issue cannot be resolved, since we needed doctors who would prescribe either a delayed prescription or an immediate prescription in order to recruit enough patients.
The strength of this study lies in the blinded nature of the intervention delivery to the patient, the analysis by intention to treat, and the study’s originality. Our intervention had no impact on patients’ satisfaction, concerns, or the likelihood of seeing a doctor for next illness (Table 3). In contrast, Little11 found that antibiotic use predicted future consultations for sore throat and the belief that antibiotics were effective for sore throat.11,19 The differences may relate to the different patient symptoms and geographical differences (common cold in New Zealand versus sore throat in the UK) or the fact that all patients in our study left with a prescription. Another possible reason is that the patients knew they were participating in a study, whereas in the Little study, the instructions were more vague.11
Doctors often misinterpret patient expectations. Improving communications between patient and doctor may be central to reducing patients’ demand for antibiotics. Britten makes the claim that “all the misunderstandings were associated with lack of patients’ participation in the consultation in terms of voicing of expectations and preferences or the voicing of responses to doctors’ decisions and actions.”20 The need for delayed prescriptions had been highlighted as a solution. We know that the common cold presents no great diagnostic dilemma but can produce enormous treatment dilemmas.21 Barry believes that by changing doctors’ views and helping patients to explain what they want from the office visit may lead to changes in treatment patterns.22 We concur with Little that unless patients are very ill, general practitioners should consider exploring their concerns, explaining the natural history of their illness, and avoiding or delaying prescribing antibiotics.11
We were pleased to see a reduction of antibiotics consumed (89% to 48%). However, 48% still represents a high proportion of patients who consumed antibiotics for an illness that is most unlikely to respond to those drugs. More placebo-controlled randomized trials of antibiotics for respiratory tract infections in the primary care setting are needed. We suggest that FPs clarify patients’ expectation for antibiotics and not prescribe them unless the patient insists. For patients who expect to take antibiotics and cannot be persuaded otherwise, a delayed prescription may be the first step in educating them that these medicines are not routinely required.
Conclusions
Delayed prescriptions are a safe and effective means of reducing antibiotic use in patients with the common cold who want antibiotics. The additional barrier of asking the patient to pick up the prescription from the office if symptoms persist after 3 days may reduce antibiotic use even further. When the patient demands a prescription, delaying its delivery has the potential to provide gentle education that antibiotics are an unnecessary treatment.
Acknowledgments
The authors acknowledge the support of the Health Research Council for funding the study, Tania Milne for data collection, and Alistair Stewart for statistical advice. The authors further thank the participating family physicians and patients for their contribution.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.
1. McGregor A, Dovey S, Tilyard M. Antibiotic use in upper respiratory tract infections in New Zealand. Fam Pract 1995;12:166-70.
2. Mainous AG, Hueston WJ, Clark JR. Antibiotics and upper respiratory infections: Do some folks think there is a cure for the common cold? J Fam Pract 1996;42:357-61.
3. Ochoa C, Eiros JM, Inglada L, Vallano A, Guerra L. Assessment of antibiotic prescription in acute respiratory infections in adults. The Spanish study group on antibiotic treatment. J Infect Dis 2000;41:73-80.
4. Spector SL. The common cold: current therapy and natural history. J Allergy Clin Immunol 1995;95:1133-8.
5. Arroll B, Kenealy T. Antibiotics for the common cold (Cochrane Review). The Cochrane Library, issue 4, 2000. Oxford, England: Update Software.
6. Gadomski AM. Potential interventions for preventing pneumonia among young children: lack of effect of antibiotic treatment for upper respiratory infections. Pediatr Infect Dis J 1993;12:115-20.
7. McAvoy B, Davis P, Raymont A, Gribben B. The Waikato Medical Care Survey. N Z Med J 1994;107:387-433.
8. Carrie AC, Zhanel CG. Antibacterial use in community practice: assessing quantity, indications and appropriateness and relationship to the development of resistant bacteria. Drugs 1999;57:871-81.
9. Arason VA, Kristinsson KG, Sigurdsson JA, Stefansdottir G, Molstad S, Gudmundsson S. Do antimicrobials increase the carriage rate of penicillin resistant pneumococci in children? Cross-sectional prevalence study. BMJ 1996;313:387-91.
10. Verkatesum P, Innes JA. Antibiotic resistance in common acute respiratory pathogens. Thorax 1995;50:481-3.
11. Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmouth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ 1997;314:722-7.
12. Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42.
13. Dowell J, Pitkethly M, Bain J, Martin S. A randomised controlled trial as a strategy for managing uncomplicated respiratory tract infection in primary care. Br J Gen Pract 2001;51:200-5.
14. Arroll B, Goodyear-Smith F. General practitioners management of URTIs: when are antibiotics prescribed? N Z Med J 2000;113:493-6.
15. International Classification of Health Problems in Primary Care (ICHPPC-2). International classification of primary care. Oxford, England: Oxford University Press; 1998.
16. Kaiser L, Lew D, Hirschel B, et al. Effects of antibiotic treatment in the subset of common cold patients who have bacteria in nasopharyngeal secretions. Lancet 1996;347:1507-10.
17. Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 1999;319:670-4.
18. McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ 1996;313:732-3.
19. Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmouth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ 1997;315:350-2.
20. Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice. BMJ 2000;320:484-8.
21. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners and patients’ perceptions of antibiotics for sore throats. BMJ 1998;317:637-42.
22. Barry CA, Bradley CP, Britten N, Stevenson FA, Barber N. Patients’ unvoiced agendas in general practice consultations: qualitative study. BMJ 2000;320:1246-50.