User login
Pain in right shoulder
A 44-year-old African-American woman with sickle cell trait presented to the clinic to establish care. She complained of polyarthralgias that she’d had since adolescence; the pain was worst in her right shoulder. She reported morning stiffness that lasted up to 8 hours, an intermittent facial rash, oral ulcers, joint edema (of which she had pictures on her phone), and photosensitivity. She took ibuprofen and acetaminophen as needed for pain. She once worked as a medical assistant but hadn’t been able to work since 2014 due to pain. She reported having been told as a teenager that she might have juvenile arthritis, but she didn’t recall ever having diagnostic tests performed or receiving treatment other than anti-inflammatories.
A couple of weeks after an initial visit with a rheumatologist, the patient returned to the family medicine clinic. She said she was upset that the specialist had x-rayed her hands, but had not checked her shoulder, which was the primary source of her pain. She also had pain in her hands, hips, feet, and knees.
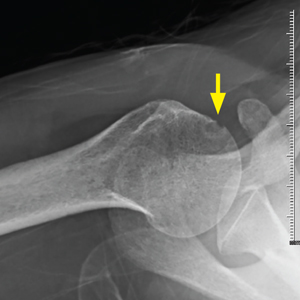
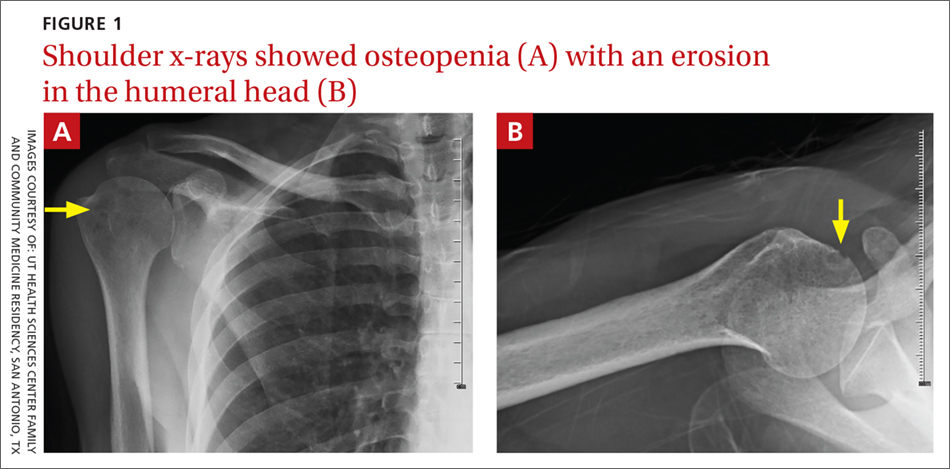
On physical exam, the patient looked fatigued. A musculoskeletal exam revealed no joint effusions or edema, but was significant for right shoulder pain with reduced abduction to 90°. Gross motor strength was 5/5 in all 4 extremities. Laboratory testing revealed an antinuclear antibody titer of 1:160 and was negative for double-stranded DNA. Bilateral hand and foot x-rays showed no joint erosions. An x-ray of the right shoulder was obtained, which showed evidence of osteopenia and an erosion in the humeral head (FIGURES 1A and 1B).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rheumatoid arthritis
The patient’s history of morning stiffness and the joint erosion observed on x-ray were highly suggestive of rheumatoid arthritis (RA).
RA is a symmetric, inflammatory, peripheral polyarthritis of unknown etiology. It is the most common form of inflammatory arthritis, affecting 1% of the population worldwide.1 It causes cartilage and bone to erode, leading to the deformation and destruction of joints. If RA is left untreated or is unresponsive to therapy, it can eventually lead to loss of physical function.
Making the diagnosis
The distinctive signs of RA are joint erosions and rheumatoid nodules, which are often absent on initial presentation.
Classification criteria. The 2010 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) classification criteria for RA2 are based on the presence of synovitis in at least one joint, the absence of an alternative diagnosis that better explains the synovitis, and a cumulative score of at least 6/10 from the following 4 domains:
- Number and site of involved joints
- 2 to 10 large joints (shoulders, elbows, hips, knees, ankles)=1 point
- 1 to 3 small joints (metacarpophalangeal [MCP] joints, proximal interphalangeal [PIP] joints, 2nd-5th metatarsophalangeal joints, thumb interphalangeal joints, wrists)=2 points
- 4 to 10 small joints=3 points
- More than 10 joints (including at least 1 small joint)=5 points
- Serologic abnormality (rheumatoid factor [RF] and anti-cyclic citrullinated peptide)
- Low positive=2 points
- High positive=3 points
- Elevated acute phase response (erythrocyte sedimentation rate [ESR] or C-reactive protein [CRP])=1 point
- Symptom duration of at least 6 weeks=1 point.
These criteria are best suited for early disease. For patients with longstanding symptoms, diagnosis is based on an erosive disease with a history of criteria fulfillment, or a currently inactive longstanding disease, with or without treatment, that has previously fulfilled the criteria.3
Continue to: The differential Dx is extensive
The differential Dx is extensive
The differential includes polyarthralgias such as viral polyarthritis, systemic rheumatic diseases, and osteoarthritis.
Viral polyarthritis is caused by rubella, parvovirus B194, alphaviruses, and hepatitis B. Symptoms can last from 3 days to several weeks, but rarely persist beyond 6 weeks; alphaviruses, however, can last 3 to 6 months.5 The common symptom triad includes fever, arthritis, and rash. Chikungunya is an example of an alphavirus that has become a global disease. Alphavirus arthritis can mimic seronegative RA and even satisfy the classification criteria for RA if the initial symptoms of fever and rash and history of travel to endemic regions are not appreciated.5
Systemic rheumatic diseases. Early RA may mimic the arthritis of systemic lupus erythematosus (SLE), Sjögren’s syndrome, dermatomyositis, or mixed connective tissue disease.6 In contrast to RA, these disorders generally have systemic features, such as rashes, dry mouth and eyes, myositis, or nephritis, and generate autobodies, which are not seen with RA. The CRP is often normal in patients with active SLE, even when the ESR is elevated.
Osteoarthritis (OA) can be confused with RA, particularly when small joints are involved. A thorough history helps elucidate the diagnosis. For example, OA of the fingers affects distal interphalangeal joints and is associated with Heberden’s nodes, while RA more commonly affects MCP and PIP joints. Swelling from OA is typically firm, while swelling due to RA is warm, boggy, and tender. Joint stiffness due to OA is worse with activity and generally lasts only a few minutes, while joint stiffness due to RA is worse at rest and lasts 30 minutes or more. X-rays show joint-space narrowing with OA, but no erosions or cysts. RF may be present at low levels in older patients with OA, while it is usually associated with high levels in patients with seropositive RA.
Continue to: Treat with disease-modifying antirheumatic drugs
Treat with disease-modifying antirheumatic drugs
Immediate treatment of RA with disease-modifying antirheumatic drugs (DMARDs) is important to achieve control of the disease and prevent disability.
Our patient. We ordered a purified protein derivative skin test in preparation for the patient to start therapy with a DMARD. Our patient followed up with Rheumatology and was started on indomethacin, with an initial dose of 25 mg bid. (DMARDs are first-line therapy; indomethacin is a second-line choice. In this case, the patient declined DMARDs after hearing they lowered the body’s ability to fight infection.) An RF level measured 6.74 IU/ml, which is within normal limits. The patient was subsequently lost to follow-up.
CORRESPONDENCE
Barbara Kiersz, DO, 6835 Austin Center Blvd., Austin, TX 78731; [email protected].
1. Rothschild BM, Turner KR, DeLuca MA. Symmetrical erosive peripheral polyarthritis in the Late Archaic Period of Alabama. Science. 1988;241:1498-1501.
2. Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580-1588.
3. Pincus T, Callahan LF. How many types of patients meet classification criteria for rheumatoid arthritis? J Rheumatol. 1994;21:1385-1389.
4. Smith CA, Woolf AD, Lenci M. Parvoviruses: infections and arthropathies. Rheum Dis Clin North Am. 1987;13:249-263.
5. Miner JJ, Aw-Yeang HX, Fox JM, et al. Chikungunya viral arthritis in the United States: a mimic of seronegative rheumatoid arthritis. Arthritis Rheumatol. 2015;67:1214-1220.
6. Cronin ME. Musculoskeletal manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. 1988;14:99-116.
A 44-year-old African-American woman with sickle cell trait presented to the clinic to establish care. She complained of polyarthralgias that she’d had since adolescence; the pain was worst in her right shoulder. She reported morning stiffness that lasted up to 8 hours, an intermittent facial rash, oral ulcers, joint edema (of which she had pictures on her phone), and photosensitivity. She took ibuprofen and acetaminophen as needed for pain. She once worked as a medical assistant but hadn’t been able to work since 2014 due to pain. She reported having been told as a teenager that she might have juvenile arthritis, but she didn’t recall ever having diagnostic tests performed or receiving treatment other than anti-inflammatories.
A couple of weeks after an initial visit with a rheumatologist, the patient returned to the family medicine clinic. She said she was upset that the specialist had x-rayed her hands, but had not checked her shoulder, which was the primary source of her pain. She also had pain in her hands, hips, feet, and knees.
On physical exam, the patient looked fatigued. A musculoskeletal exam revealed no joint effusions or edema, but was significant for right shoulder pain with reduced abduction to 90°. Gross motor strength was 5/5 in all 4 extremities. Laboratory testing revealed an antinuclear antibody titer of 1:160 and was negative for double-stranded DNA. Bilateral hand and foot x-rays showed no joint erosions. An x-ray of the right shoulder was obtained, which showed evidence of osteopenia and an erosion in the humeral head (FIGURES 1A and 1B).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rheumatoid arthritis
The patient’s history of morning stiffness and the joint erosion observed on x-ray were highly suggestive of rheumatoid arthritis (RA).
RA is a symmetric, inflammatory, peripheral polyarthritis of unknown etiology. It is the most common form of inflammatory arthritis, affecting 1% of the population worldwide.1 It causes cartilage and bone to erode, leading to the deformation and destruction of joints. If RA is left untreated or is unresponsive to therapy, it can eventually lead to loss of physical function.
Making the diagnosis
The distinctive signs of RA are joint erosions and rheumatoid nodules, which are often absent on initial presentation.
Classification criteria. The 2010 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) classification criteria for RA2 are based on the presence of synovitis in at least one joint, the absence of an alternative diagnosis that better explains the synovitis, and a cumulative score of at least 6/10 from the following 4 domains:
- Number and site of involved joints
- 2 to 10 large joints (shoulders, elbows, hips, knees, ankles)=1 point
- 1 to 3 small joints (metacarpophalangeal [MCP] joints, proximal interphalangeal [PIP] joints, 2nd-5th metatarsophalangeal joints, thumb interphalangeal joints, wrists)=2 points
- 4 to 10 small joints=3 points
- More than 10 joints (including at least 1 small joint)=5 points
- Serologic abnormality (rheumatoid factor [RF] and anti-cyclic citrullinated peptide)
- Low positive=2 points
- High positive=3 points
- Elevated acute phase response (erythrocyte sedimentation rate [ESR] or C-reactive protein [CRP])=1 point
- Symptom duration of at least 6 weeks=1 point.
These criteria are best suited for early disease. For patients with longstanding symptoms, diagnosis is based on an erosive disease with a history of criteria fulfillment, or a currently inactive longstanding disease, with or without treatment, that has previously fulfilled the criteria.3
Continue to: The differential Dx is extensive
The differential Dx is extensive
The differential includes polyarthralgias such as viral polyarthritis, systemic rheumatic diseases, and osteoarthritis.
Viral polyarthritis is caused by rubella, parvovirus B194, alphaviruses, and hepatitis B. Symptoms can last from 3 days to several weeks, but rarely persist beyond 6 weeks; alphaviruses, however, can last 3 to 6 months.5 The common symptom triad includes fever, arthritis, and rash. Chikungunya is an example of an alphavirus that has become a global disease. Alphavirus arthritis can mimic seronegative RA and even satisfy the classification criteria for RA if the initial symptoms of fever and rash and history of travel to endemic regions are not appreciated.5
Systemic rheumatic diseases. Early RA may mimic the arthritis of systemic lupus erythematosus (SLE), Sjögren’s syndrome, dermatomyositis, or mixed connective tissue disease.6 In contrast to RA, these disorders generally have systemic features, such as rashes, dry mouth and eyes, myositis, or nephritis, and generate autobodies, which are not seen with RA. The CRP is often normal in patients with active SLE, even when the ESR is elevated.
Osteoarthritis (OA) can be confused with RA, particularly when small joints are involved. A thorough history helps elucidate the diagnosis. For example, OA of the fingers affects distal interphalangeal joints and is associated with Heberden’s nodes, while RA more commonly affects MCP and PIP joints. Swelling from OA is typically firm, while swelling due to RA is warm, boggy, and tender. Joint stiffness due to OA is worse with activity and generally lasts only a few minutes, while joint stiffness due to RA is worse at rest and lasts 30 minutes or more. X-rays show joint-space narrowing with OA, but no erosions or cysts. RF may be present at low levels in older patients with OA, while it is usually associated with high levels in patients with seropositive RA.
Continue to: Treat with disease-modifying antirheumatic drugs
Treat with disease-modifying antirheumatic drugs
Immediate treatment of RA with disease-modifying antirheumatic drugs (DMARDs) is important to achieve control of the disease and prevent disability.
Our patient. We ordered a purified protein derivative skin test in preparation for the patient to start therapy with a DMARD. Our patient followed up with Rheumatology and was started on indomethacin, with an initial dose of 25 mg bid. (DMARDs are first-line therapy; indomethacin is a second-line choice. In this case, the patient declined DMARDs after hearing they lowered the body’s ability to fight infection.) An RF level measured 6.74 IU/ml, which is within normal limits. The patient was subsequently lost to follow-up.
CORRESPONDENCE
Barbara Kiersz, DO, 6835 Austin Center Blvd., Austin, TX 78731; [email protected].
A 44-year-old African-American woman with sickle cell trait presented to the clinic to establish care. She complained of polyarthralgias that she’d had since adolescence; the pain was worst in her right shoulder. She reported morning stiffness that lasted up to 8 hours, an intermittent facial rash, oral ulcers, joint edema (of which she had pictures on her phone), and photosensitivity. She took ibuprofen and acetaminophen as needed for pain. She once worked as a medical assistant but hadn’t been able to work since 2014 due to pain. She reported having been told as a teenager that she might have juvenile arthritis, but she didn’t recall ever having diagnostic tests performed or receiving treatment other than anti-inflammatories.
A couple of weeks after an initial visit with a rheumatologist, the patient returned to the family medicine clinic. She said she was upset that the specialist had x-rayed her hands, but had not checked her shoulder, which was the primary source of her pain. She also had pain in her hands, hips, feet, and knees.
On physical exam, the patient looked fatigued. A musculoskeletal exam revealed no joint effusions or edema, but was significant for right shoulder pain with reduced abduction to 90°. Gross motor strength was 5/5 in all 4 extremities. Laboratory testing revealed an antinuclear antibody titer of 1:160 and was negative for double-stranded DNA. Bilateral hand and foot x-rays showed no joint erosions. An x-ray of the right shoulder was obtained, which showed evidence of osteopenia and an erosion in the humeral head (FIGURES 1A and 1B).
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Rheumatoid arthritis
The patient’s history of morning stiffness and the joint erosion observed on x-ray were highly suggestive of rheumatoid arthritis (RA).
RA is a symmetric, inflammatory, peripheral polyarthritis of unknown etiology. It is the most common form of inflammatory arthritis, affecting 1% of the population worldwide.1 It causes cartilage and bone to erode, leading to the deformation and destruction of joints. If RA is left untreated or is unresponsive to therapy, it can eventually lead to loss of physical function.
Making the diagnosis
The distinctive signs of RA are joint erosions and rheumatoid nodules, which are often absent on initial presentation.
Classification criteria. The 2010 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) classification criteria for RA2 are based on the presence of synovitis in at least one joint, the absence of an alternative diagnosis that better explains the synovitis, and a cumulative score of at least 6/10 from the following 4 domains:
- Number and site of involved joints
- 2 to 10 large joints (shoulders, elbows, hips, knees, ankles)=1 point
- 1 to 3 small joints (metacarpophalangeal [MCP] joints, proximal interphalangeal [PIP] joints, 2nd-5th metatarsophalangeal joints, thumb interphalangeal joints, wrists)=2 points
- 4 to 10 small joints=3 points
- More than 10 joints (including at least 1 small joint)=5 points
- Serologic abnormality (rheumatoid factor [RF] and anti-cyclic citrullinated peptide)
- Low positive=2 points
- High positive=3 points
- Elevated acute phase response (erythrocyte sedimentation rate [ESR] or C-reactive protein [CRP])=1 point
- Symptom duration of at least 6 weeks=1 point.
These criteria are best suited for early disease. For patients with longstanding symptoms, diagnosis is based on an erosive disease with a history of criteria fulfillment, or a currently inactive longstanding disease, with or without treatment, that has previously fulfilled the criteria.3
Continue to: The differential Dx is extensive
The differential Dx is extensive
The differential includes polyarthralgias such as viral polyarthritis, systemic rheumatic diseases, and osteoarthritis.
Viral polyarthritis is caused by rubella, parvovirus B194, alphaviruses, and hepatitis B. Symptoms can last from 3 days to several weeks, but rarely persist beyond 6 weeks; alphaviruses, however, can last 3 to 6 months.5 The common symptom triad includes fever, arthritis, and rash. Chikungunya is an example of an alphavirus that has become a global disease. Alphavirus arthritis can mimic seronegative RA and even satisfy the classification criteria for RA if the initial symptoms of fever and rash and history of travel to endemic regions are not appreciated.5
Systemic rheumatic diseases. Early RA may mimic the arthritis of systemic lupus erythematosus (SLE), Sjögren’s syndrome, dermatomyositis, or mixed connective tissue disease.6 In contrast to RA, these disorders generally have systemic features, such as rashes, dry mouth and eyes, myositis, or nephritis, and generate autobodies, which are not seen with RA. The CRP is often normal in patients with active SLE, even when the ESR is elevated.
Osteoarthritis (OA) can be confused with RA, particularly when small joints are involved. A thorough history helps elucidate the diagnosis. For example, OA of the fingers affects distal interphalangeal joints and is associated with Heberden’s nodes, while RA more commonly affects MCP and PIP joints. Swelling from OA is typically firm, while swelling due to RA is warm, boggy, and tender. Joint stiffness due to OA is worse with activity and generally lasts only a few minutes, while joint stiffness due to RA is worse at rest and lasts 30 minutes or more. X-rays show joint-space narrowing with OA, but no erosions or cysts. RF may be present at low levels in older patients with OA, while it is usually associated with high levels in patients with seropositive RA.
Continue to: Treat with disease-modifying antirheumatic drugs
Treat with disease-modifying antirheumatic drugs
Immediate treatment of RA with disease-modifying antirheumatic drugs (DMARDs) is important to achieve control of the disease and prevent disability.
Our patient. We ordered a purified protein derivative skin test in preparation for the patient to start therapy with a DMARD. Our patient followed up with Rheumatology and was started on indomethacin, with an initial dose of 25 mg bid. (DMARDs are first-line therapy; indomethacin is a second-line choice. In this case, the patient declined DMARDs after hearing they lowered the body’s ability to fight infection.) An RF level measured 6.74 IU/ml, which is within normal limits. The patient was subsequently lost to follow-up.
CORRESPONDENCE
Barbara Kiersz, DO, 6835 Austin Center Blvd., Austin, TX 78731; [email protected].
1. Rothschild BM, Turner KR, DeLuca MA. Symmetrical erosive peripheral polyarthritis in the Late Archaic Period of Alabama. Science. 1988;241:1498-1501.
2. Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580-1588.
3. Pincus T, Callahan LF. How many types of patients meet classification criteria for rheumatoid arthritis? J Rheumatol. 1994;21:1385-1389.
4. Smith CA, Woolf AD, Lenci M. Parvoviruses: infections and arthropathies. Rheum Dis Clin North Am. 1987;13:249-263.
5. Miner JJ, Aw-Yeang HX, Fox JM, et al. Chikungunya viral arthritis in the United States: a mimic of seronegative rheumatoid arthritis. Arthritis Rheumatol. 2015;67:1214-1220.
6. Cronin ME. Musculoskeletal manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. 1988;14:99-116.
1. Rothschild BM, Turner KR, DeLuca MA. Symmetrical erosive peripheral polyarthritis in the Late Archaic Period of Alabama. Science. 1988;241:1498-1501.
2. Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580-1588.
3. Pincus T, Callahan LF. How many types of patients meet classification criteria for rheumatoid arthritis? J Rheumatol. 1994;21:1385-1389.
4. Smith CA, Woolf AD, Lenci M. Parvoviruses: infections and arthropathies. Rheum Dis Clin North Am. 1987;13:249-263.
5. Miner JJ, Aw-Yeang HX, Fox JM, et al. Chikungunya viral arthritis in the United States: a mimic of seronegative rheumatoid arthritis. Arthritis Rheumatol. 2015;67:1214-1220.
6. Cronin ME. Musculoskeletal manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. 1988;14:99-116.