User login
Afraid in the Hospital
The Institute of Medicine report linking between 48,000 and 98,000 deaths annually to medical errors1 has raised awareness about medical errors across all areas of medicine. In pediatrics, medical errors in hospitalized children are associated with significant increases in length of stay, healthcare costs, and death.2, 3 While much attention has been paid to the use of hospital systems to prevent medical errors, there has been considerably less focus on the experiences of patients and their potential role in preventing errors.
Studies have suggested that a significant majority of adult patients are concerned about medical errors during hospitalization.4, 5 However, a similar assessment of parents' concerns about medical errors in pediatrics is lacking. Admittedly, for concern to be constructive it must be linked to action. The Joint Commission and the Agency for Healthcare Research and Quality (AHRQ) currently recommend that parents help prevent errors by becoming active, involved and informed members of their healthcare team and taking part in every decision about (their) child's health care.6, 7 However, the extent to which parental concern about medical errors is related to a parent's self‐efficacy, or confidence, interacting with physicians is unknown.
Self‐efficacy is a construct used in social cognitive theory to explain behavior change.8 It refers to an individual's belief in (his/her) capabilities to organize and execute the courses of action required to produce given attainments or a desired outcome.9 Self‐efficacy is not a general concept; it must be discussed in reference to a specific activity. In healthcare it has been associated not only with willingness to adopt preventive strategies,10 but also with treatment adherence,11, 12 behavior change,13 and with greater patient participation in healthcare decision‐making.14, 15
In this study we had 2 objectives. First, we sought to assess the proportion of parents of hospitalized children who are concerned about medical errors. Second, we attempted to examine whether a parent's self‐efficacy interacting with physicians was associated with their concern about medical errors for their child. Given that parents with greater self‐efficacy interacting with physicians might feel more empowered to prevent errors and, as such, be more inclined to take an active role to do so, we hypothesized that such parents would be less concerned about medical errors during a pediatric hospitalization.
Subjects and Methods
Population
We surveyed parents of children <18 years of age (including 2 grandparents who will hereafter be referred to as parents) who were admitted to the general medical service of the Children's Hospital & Regional Medical Center (CHRMC) in Seattle, WA, from July through September 2005. This study was approved by the CHRMC Institutional Review Board. Due to stipulations of the Health Insurance Portability and Accountability Act (HIPAA), we were unable to collect extensive information on those parents who were missed or those who refused to participate in the study.
Exclusions
We excluded parents if: (1) they did not feel comfortable answering a written survey in English or Spanish; (2) their child was transferred to the general medical unit either from the intensive care unit (ICU) or from the inpatient unit of another hospital; or (3) they were not present during the hospitalization.
Study Design
We conducted a cross‐sectional self‐administered written survey of parents. The survey was translated into Spanish by a certified Spanish translator. A second independent translator confirmed the accuracy of the translation. Informed consent was obtained from parents before administration of the survey.
Data Collection
Parents were surveyed with a consecutive sampling methodology Tuesday through Friday from July 2005 through September 2005. We surveyed parents within 48 hours of admission of their child to the hospital, but after they had an opportunity to speak with the inpatient medical team that was caring for their child. A more detailed discussion of the data collection process has been published previously.16
Dependent Variables
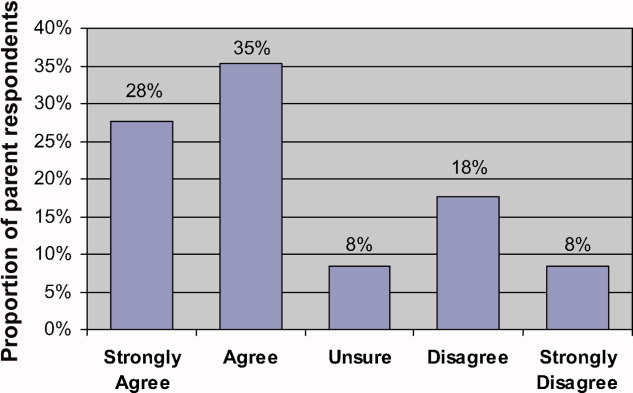
Parental Concern About the Need to Watch for Medical Errors
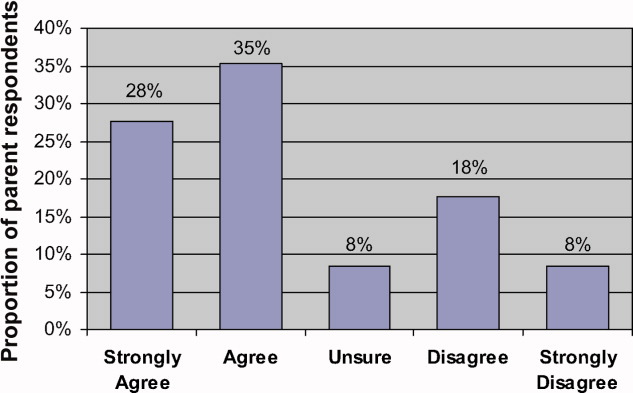
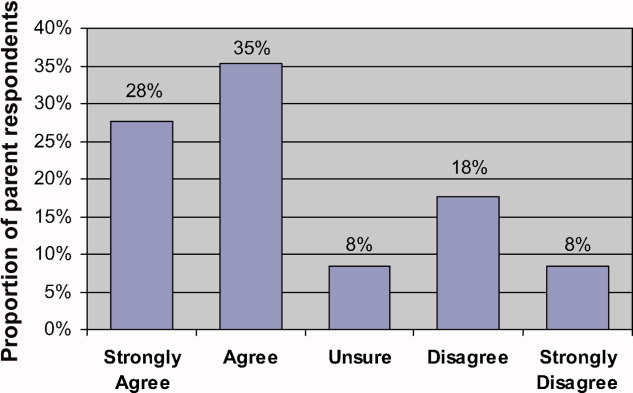
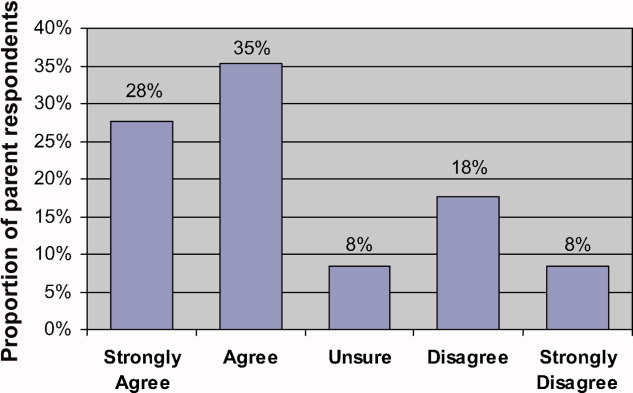
We assessed parental concerns about medical errors during hospitalization by measuring responses to the statement When my child is in the hospital I feel that I have to watch over the care that he/she is receiving to make sure that mistakes aren't made. Parents reported their agreement/disagreement with this statement using a 5‐point Likert scale. For our analysis we dichotomized the dependent variable into those parents who responded Strongly Agree or Agree vs. those who responded Strongly Disagree or Disagree. We chose to focus on parents who expressed a directional response (eg, agree or disagree) because we felt that such responses were more likely to be correlated with behavior. As a result, we excluded from our primary analysis those participants who responded Unsure. In order to determine the effect of exclusion on our results (given its size), we conducted separate post‐hoc analyses in which we included the Unsure respondents in Agree and Disagree categories, respectively.
Independent Variables
Self‐Efficacy in Patient‐Physician Interactions
The Joint Commission's Speak Up initiative7 recommends that patients and parents interact with their healthcare providers in order to prevent errors. We gauged a parent's confidence of interacting with healthcare providers using an adapted scale of the Perceived Efficacy in Patient‐Physician Interactions (PEPPI) self‐efficacy scale. The PEPPI is a 50‐point self‐efficacy scale that has been validated in older adults.17 The response to each question is recorded on a 5‐point Likert scale ranging from 1 to 5 where 1 represents not at all confident and 5 represents very confident. Higher scores on this scale have been associated with greater participation in treatment decisions by women with breast cancer.18 We adapted this scale for use in pediatrics (Appendix 1).
Covariates
Prior Hospitalizations and Chronic Illness History
We asked parents to report how many times their child had been hospitalized prior to this current admission (not including birth). We chose to query parents directly because a search of our institutions' medical record database would not capture hospitalizations at other facilities. We categorized the variable for previous hospitalizations as follows: none, 1, 2, 3.
We asked parents to report if prior to this hospitalization they had ever been told by a nurse or doctor that their child had any of a list of chronic medical conditions such as chronic respiratory disease, mental retardation, and seizure disorder, among others. We gave parents the opportunity to specify a medical condition not provided on this list. The list of conditions was the same as that used in the Child Health Questionnaire PF‐28,19 which has been used in national and international studies to measure quality of life in children with and without chronic conditions20, 21 (Appendix 2).
Limited English Proficiency
We assessed the potential for a language barrier to impede communication between parent and healthcare providers by asking parents the following question: How comfortable are you that you can express your concerns and ask questions of your child's doctors in English? We measured parental responses on a 5‐point Likert scale (very comfortable vs. somewhat comfortable, not sure, somewhat uncomfortable, very uncomfortable). For our analyses, we dichotomized responses into those who reported being very comfortable vs. those who chose any other response category.
Social Desirability
We measured the potential for social desirability to bias responses using the Marlowe‐Crowne 2(10) Scale of Social Desirability.22 The Marlowe‐Crowne 2(10) Scale of Social Desirability is a shorter, validated version of the Marlowe‐Crowne Scale.23 This scale has been recommended by the National Institutes of Health (NIH)'s Behavior Change Consortium for use in behavioral change research related to health.24 It has been used in previous studies to account for social desirability bias in studies which involve patient self‐report of attitudes and beliefs.25 We analyzed scores on a continuous scale with higher scores representing greater social desirability bias in responses.
Demographics
We collected the following demographic data on parents: age, gender, race/ethnicity (white non‐Hispanic vs. other), education (high school or less, some college, college or higher). We also recorded the child's age and gender.
Statistical Analysis
Parental Concern for Medical Errors
Univariate statistics were used to report proportions of parents who were concerned about medical errors and to summarize the data for covariates and demographics. We conducted bivariate logistic regression analyses to assess the association between our outcome variable and the independent variable and each covariate, respectively. We used a Fisher's exact test to examine the association between limited English proficiency and our outcome variable because the absence of participants (eg, a zero cell) who were not very comfortable with English and not concerned about errors precluded the use of bivariate logistic regression. Therefore, to explore the relationship between race and language we used a Fischer's exact test to compare concern about medical errors between white and non‐white participants who were very comfortable with English.
We used multivariate logistic regression to test our hypothesis that greater self‐efficacy would be associated with less concern about medical errors after adjusting for the aforementioned covariates and demographics, excluding child gender. We had no a priori reason to expect that child gender would affect parental self‐efficacy or parental concern about errors and did not include it in the regression model. In order to provide a more clinically relevant interpretation of our results, we calculated adjusted predicted probabilities for the 25%, 50%, and 75% PEPPI scores using the mean for all other variables in the model.
We conducted post‐hoc analysis using a likelihood‐ratio test to determine if the hospitalization variable was significant in the multivariate regression model. We conducted additional post‐hoc analysis using bivariate logistic regression to explore the relationship between concern about medical errors and the following independent variables: hospitalization for >3 days after birth (yes/no); previous hospitalization for >1 week (yes/no); parents' experience with the hospital system (a lot, some, not sure, a little, none); overall perception of child's health (excellent, very good, good, fair); previous hospitalizations for other children (yes, no, no other children); rating of care that child has received (excellent vs. other [very good, good, fair]). We incorporated any significant associations (P < 0.05) into our preexisting multivariate model.
Results
During the time period of our study, 278 parents were eligible to participate. Eighty‐five parents could not be surveyed either because they could not be reached despite multiple attempts (eg, out of the room, speaking with physicians) or because the child had already been discharged. Of the 193 parents approached, 130 agreed to take the survey. Two parents who agreed to complete the survey forgot to return it before their children were discharged. Demographics of respondents and nonparticipants are presented in Table 1. The distribution of self‐efficacy scores was skewed, with a mean score of 45 (median 46, range 5‐50) on a 50‐point scale, consistent with previous studies in adults.18
| Characteristics | Respondents (n = 130) | Number Missed (n = 85) | Number Refused (n = 61) |
|---|---|---|---|
| |||
| Parent's mean age | 34 years (range: 18‐51) | NA | NA |
| Parent sex female, n (%) | 105 (80.8) | NA | NA |
| Parental education, n (%) | |||
| College or higher | 65 (50.4) | ||
| Some college | 34 (26.4) | ||
| High school or less | 30 (23.3) | NA | NA |
| Parental race, n (%) | |||
| White | 86 (67.2) | ||
| Non‐White | 42 (32.8) | NA | NA |
| Parent's social desirability score, mean (SD) | 7.0 (2.0) | NA | NA |
| Child's median age | 21.4 months (range: 1 day‐17.8 years) | 24 months | 24 months |
| Child's sex female, n (%) | 63 (48.5) | 36 (42) | 35 (57) |
| Number of previous hospitalizations (child), n (%) | |||
| None | 68 (53.1) | ||
| 1 | 26 (20.3) | ||
| 2 | 19 (14.8) | ||
| 3 | 15 (11.7) | NA | NA |
| Number of chronic medical conditions (child), n (%) | |||
| None | 56 (48.7) | ||
| 1 | 34 (29.6) | ||
| 2 | 25 (21.8) | NA | NA |
| Parent's comfort expressing concerns in English, n (%) | NA | NA | |
| Very comfortable | 109 (83.9) | ||
| Less than very comfortable | 21 (16.1) | ||
| Self‐efficacy score (parent), mean (SD) | 45 (6.3) | NA | NA |
Eighty‐two parents (63% of respondents) Agreed or Strongly Agreed with the statement When my child is in the hospital I feel that I need to watch over his/her care in order to make sure that mistakes aren't made (Figure 1). In bivariate analyses, non‐white race (Table 2) and English proficiency (P = 0.002) were significantly associated with parental concern about medical errors. Notably, all respondents who were not very comfortable with English agreed that they felt the need to watch over their child's care to ensure that mistakes do not happen. The association between self‐efficacy with physician interactions and concern was nearly significant (Table 2).
| Variable | Crude Odds Ratio | Confidence Interval | P Value | Adjusted Odds Ratio | Confidence Interval | P Value |
|---|---|---|---|---|---|---|
| ||||||
| Parent age (years) | 1.01 | 0.95‐1.06 | 0.79 | 1.05 | 0.95‐1.15 | 0.36 |
| Parent gender | ||||||
| Female | Referent | |||||
| Male | 0.86 | 0.32‐2.35 | 0.77 | 0.76 | 0.20‐2.79 | 0.68 |
| Age of child (months) | 1.00 | 0.99‐1.01 | 0.97 | 1.00 | 0.99‐1.01 | 0.83 |
| Parental education | ||||||
| College or higher | Referent | Referent | ||||
| Some college | 0.48 | 0.18‐1.26 | 0.14 | 0.3 | 0.07‐1.13 | 0.07 |
| High school or less | 1.39 | 0.48‐4.00 | 0.55 | 0.5 | 0.1‐2.2 | 0.38 |
| Parental race | ||||||
| White | Referent | Referent | ||||
| Non‐White | 5.00* | 1.61‐15.56 | 0.005 | 4.9 | 1.19‐20.4 | 0.03 |
| Previous hospitalization (child) | ||||||
| None | Referent | Referent | ||||
| 1 | 0.44 | 0.16‐1.20 | 0.11 | 0.16 | 0.04‐0.69 | 0.01 |
| 2 | 0.89 | 0.27‐2.87 | 0.84 | 0.60 | 0.13‐2.83 | 0.5 |
| 3 | 0.91 | 0.21‐3.84 | 0.90 | 0.79 | 0.12‐5.06 | 0.8 |
| Number of chronic medical conditions | 0.86 | 0.67‐1.11 | 0.26 | 1.05 | 0.74‐1.50 | 0.78 |
| Social desirability score (parent) | 0.99 | 0.81‐1.21 | 0.92 | 0.99 | 0.76‐1.29 | 0.9 |
| Self‐efficacy score (parent) | 0.90 | 0.81‐1.00 | 0.06 | 0.83 | 0.73‐0.95 | 0.006* |
In multivariate analysis, self‐efficacy was independently associated with parental report about the need to watch over a child's care (odds ratio [OR], 0.83; 95% confidence interval [CI], 0.72‐0.92). In prediction models, with self‐efficacy scores of 44 (25th percentile), 46 (50th percentile), and 49 (75th percentile), about 72.2% (59.1‐82.3), 64.2% (51.8‐75.0), and 50.8% (35.3‐66.2) of parents, respectively, would feel the need to watch over their child's care to prevent medical errors.
While respondents of non‐white race had the greatest independent odds of reporting a concern for medical errors occurring while their child was hospitalized (OR, 4.9; 95% CI, 1.19‐20.4), we could not reliably determine how much of this effect was due to language instead of to race because the vast majority of parents who reported being less than very comfortable with English were also non‐white (non‐white 90.5% vs. white 9.5%, P < 0.001). In additional analyses we were unable to find a difference in concern about medical errors between white and non‐white parents who were very comfortable with English (data not shown).
Of note, while having 1 hospitalization compared to none was significantly associated with having decreased concern about medical errors (Table 2), the variable hospitalizations was not significant in the model (P = 0.07).
In post‐hoc analysis, we found no association between hospitalization for >3 days after birth, previous hospitalization for >1 week, parents' experience with the hospital system, and overall perception of child's health, previous hospitalizations for other children. While rating of care that child received was significantly associated with parents' concern about medical errors in the bivariate analysis, it did not remain significant in multivariate analysis and did not substantially change the magnitude or significance of previous associations.
Discussion
In our study, we found that nearly two‐thirds of parents of children admitted to the general pediatric service of a tertiary care children's hospital felt the need to watch over their child's care to ensure that mistakes would not be made. We also found that a parent's self‐efficacy interacting with physicians was associated with less parental concern for medical errors.
To our knowledge, this is the first study to systematically survey parents' concerns about medical errors during a child's hospitalization and to evaluate factors associated with this concern. The immediate question prompted by our findings is whether the fact that 63% of parents are concerned is alarming because it is too low or too high. Some might contend that concern about medical errors is an appropriate and desirable response because it may motivate parents to become more vigilant about the medical care that their child is receiving. However, others may challenge that such concern may indicate a feeling of powerlessness to act to prevent potential errors. In our study, the relationship between higher self‐efficacy and less parental concern raises the possibility that parents with higher levels of self‐efficacy with physician interactions may feel more comfortable communicating with physicians, which in turn may temper parents' concerns about medical errors during hospitalization.
It is equally plausible that concern about medical errors during hospitalization may motivate parents to become involved in their child's medical care and, in turn, lead them to feel empowered to prevent medical errors and so ease their concerns. It is conceivable that experience with past medical errors may fuel a parent's need to watch over their child's care to prevent additional medical errors. Future studies should address the independent effect of past medical errors on parental concern about medical errors.
In this study, all parents who reported being very uncomfortable with English and parents of non‐white race felt the need to watch over their child's care to help prevent errors. A previous survey of a nationally representative sample of U.S. adults found greater proportion of non‐white adults were very concerned about errors or mistakes happening when receiving care at a hospital (blacks 62%, Hispanics 57%, whites 44%).26 However, in our study, the relationship between race and concern is likely mediated by language since many of the parents who described themselves as other than white also reported being not very comfortable with English and we could not find an effect of race on concern among parents who were very comfortable with English. Indeed, previous studies have linked decreased English proficiency to medical errors with potential clinical consequence.27
Given our previous investigation of the relationship between self‐efficacy and parent participation in medical decisions during a child's hospitalization, we conducted post‐hoc analyses exploring the association between parents' self‐report of participation in medical decisions and concern about medical errors during their child's hospitalization.16 Using a simple logistic regression we did not find any association. However, we advise caution in interpreting and generalizing these results because the study was not powered to adequately evaluate this association.
There are additional limitations in our study to be noted. First, this question has not been used previously to assess parental concern about medical errors, so future work will need to focus on assessing its reliability and validity. Second, it is also possible that parents' concern for medical errors is mitigated by the complexity of their child's healthcare.5 We attempted to address this issue by controlling for the child's number of chronic illnesses. However, it is possible that our metric did not capture the level of complexity associated with different types of chronic conditions. Moreover, additional variables such as health insurance type, parental physical and mental health, and quality of interactions with the nursing staff may confound the relationships that we observed. Future studies should examine the effect of these variables on parents' self‐efficacy and their concern about medical errors.
Third, we surveyed parents at a single institution and, as such, differences in demographics and hospital‐specific practices related to patient‐physician interactions may prevent generalization of our findings to other institutions. For example, the parents in our survey had a higher average education level than the general population and the racial makeup of our population was not nationally representative. Also, due to HIPAA constraints, we were unable to collect extensive demographic information on parents and children who were missed or those who refused to participate in the study, which also could conceivably influence the strength of our findings.
Fourth, we adapted a validated adult measure of self‐efficacy for use in pediatrics. The patient‐physician self‐efficacy scale, the PEPPI, did have a skewed distribution in our study, although this performance is consistent with adult studies18 and in post‐hoc analyses, outlier PEPPI scores did not have a significant effect on the magnitude of the relationship we observed between self‐efficacy and parental concern about medical errors. However, the reading level of this instrument is ninth grade, which may impact the generalization of our findings to populations with lower literacy levels.
Fifth, we excluded parents who were unsure about their concern from our analyses. In post‐hoc multivariate regression analyses, reassignment of unsure responses to either agree or disagree did not result in any change in odds ratio for any endpoint.
Finally, it is possible that parental concern was influenced by social desirability bias in that parents may have been less likely to report concern about medical errors during a hospitalization because of fear of the implications it might have for their child's care. We attempted to control for this effect by adjusting for social desirability bias using the Marlowe‐Crowne scale. This scale is commonly used in behavioral science research to account for such response bias and has been recommended by the NIH Consortium on Behavior Change for use in behavioral change research related to health.24
Within the context of these limitations, we feel that our study contributes an important first step toward characterizing the scope of parental concern about medical errors during pediatric hospitalizations and understanding the relationship of self‐efficacy with physician interactions to this concern. Devising a quality initiative program to improve parents' self‐efficacy interacting with physicians might help to temper parents' concerns about medical errors while also encouraging their involvement in their child's medical care. Such a program would likely prove most beneficial if it sought to improve self‐efficacy among parents with lower English proficiency given that this group had the highest concern for medical errors. Possible interventions might include more ready access to interpreters or use of visual aids.
- Institute of Medicine Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,,, et al.Medication errors and adverse drug events in pediatric inpatients.JAMA.2001;285(16):2114–2120.
- ,.Pediatric patient safety in hospitals: a national picture in 2000.Pediatrics.2004;113(6):1741–1746.
- ,,,,,.Brief report: hospitalized patients' attitudes about and participation in error prevention.J Gen Intern Med.2006;21(4):367–370.
- ,,, et al.Patients' concerns about medical errors during hospitalization.Jt Comm J Qual Patient Saf.2007;33(1):5–14.
- Agency for Healthcare Research and Quality.20 Tips to Help Prevent Medical Errors in Children. Patient Fact Sheet. 2009, AHRQ Publication No. 02‐P034.Rockville, MD:Agency for Healthcare Research and Quality.
- Joint Commission on Accreditation of Healthcare Organizations. Speak Up Initiatives. Available at: http://www.jointcommission.org/PatientSafety/SpeakUp. Accessed May 2009.
- .Self‐efficacy: toward a unifying theory of behavioral change.Psychol Rev.1977;84(2):191–215.
- .Self‐Efficacy: The Exercise of Control.New York, NY:W.H. Freeman and Company;1997.
- ,,,.Psychosocial correlates of physical activity in healthy children.Arch Pediatr Adolesc Med.2001;155(8):897–902.
- ,,,,.Self‐efficacy as a mediator variable for adolescents' adherence to treatment for insulin‐dependent diabetes mellitus.Children's Health Care.2000;29(1):47–63.
- ,,.Diabetes regimen behaviors. Predicting adherence.Med Care.1987;25(9):868–881.
- ,,,,,.Pediatrician self‐efficacy for counseling parents of asthmatic children to quit smoking.Pediatrics.2004;113(1 Pt 1):78–81.
- ,,.Examining the relationship of patients' attitudes and beliefs with their self‐reported level of participation in medical decision‐making.Med Care.2005;43(9):865–872.
- ,,,,,.Patient‐physician concordance: preferences, perceptions, and factors influencing the breast cancer surgical decision.J Clin Oncol.2004;22(15):3091–3098.
- ,,.Toward family‐centered inpatient medical care: the role of parents as participants in medical decisions.J Pediatr.2007;151(6):690–695.
- ,,,,.Perceived efficacy in patient‐physician interactions (PEPPI): validation of an instrument in older persons.J Am Geriatr Soc.1998;46(7):889–894.
- ,,,.Determinants of participation in treatment decision‐making by older breast cancer patients.Breast Cancer Res Treat.2004;85(3):201–209.
- ,.The CHQ: A User's Manual (2nd printing).Boston, MA:HealthAct;1999.
- ,,,,.The health and well‐being of adolescents: a school‐based population study of the self‐report Child Health Questionnaire.J Adolesc Health.2001;29(2):140–149.
- ,,.The Child Health Questionnaire in children with diabetes: cross‐sectional survey of parent and adolescent‐reported functional health status.Diabet Med.2000;17(10):700–707.
- ,.Semantic style variance in personality questionnaires.J Psychol.1973;85:109–118.
- ,.A new scale of social desirability independent of psychopathology.J Consult Psychol.1960;24:349–354.
- National Institutes of Health. Behavior Change Consortium‐Recommended Nutrition Measures. Available at:http://www1.od.nih.gov/behaviorchange/measures/nutrition.htm. Accessed May 2009.
- ,,.Response bias influences mental health symptom reporting in patients with obstructive sleep apnea.Ann Behav Med.2001;23(4):313–317.
- Kaiser Family Foundation, Agency for Healthcare Research and Quality.Americans as Health Care Consumers: Update on the Role of Quality Information.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- ,,, et al.Errors in medical interpretation and their potential clinical consequences in pediatric encounters.Pediatrics.2003;111(1):6–14.
The Institute of Medicine report linking between 48,000 and 98,000 deaths annually to medical errors1 has raised awareness about medical errors across all areas of medicine. In pediatrics, medical errors in hospitalized children are associated with significant increases in length of stay, healthcare costs, and death.2, 3 While much attention has been paid to the use of hospital systems to prevent medical errors, there has been considerably less focus on the experiences of patients and their potential role in preventing errors.
Studies have suggested that a significant majority of adult patients are concerned about medical errors during hospitalization.4, 5 However, a similar assessment of parents' concerns about medical errors in pediatrics is lacking. Admittedly, for concern to be constructive it must be linked to action. The Joint Commission and the Agency for Healthcare Research and Quality (AHRQ) currently recommend that parents help prevent errors by becoming active, involved and informed members of their healthcare team and taking part in every decision about (their) child's health care.6, 7 However, the extent to which parental concern about medical errors is related to a parent's self‐efficacy, or confidence, interacting with physicians is unknown.
Self‐efficacy is a construct used in social cognitive theory to explain behavior change.8 It refers to an individual's belief in (his/her) capabilities to organize and execute the courses of action required to produce given attainments or a desired outcome.9 Self‐efficacy is not a general concept; it must be discussed in reference to a specific activity. In healthcare it has been associated not only with willingness to adopt preventive strategies,10 but also with treatment adherence,11, 12 behavior change,13 and with greater patient participation in healthcare decision‐making.14, 15
In this study we had 2 objectives. First, we sought to assess the proportion of parents of hospitalized children who are concerned about medical errors. Second, we attempted to examine whether a parent's self‐efficacy interacting with physicians was associated with their concern about medical errors for their child. Given that parents with greater self‐efficacy interacting with physicians might feel more empowered to prevent errors and, as such, be more inclined to take an active role to do so, we hypothesized that such parents would be less concerned about medical errors during a pediatric hospitalization.
Subjects and Methods
Population
We surveyed parents of children <18 years of age (including 2 grandparents who will hereafter be referred to as parents) who were admitted to the general medical service of the Children's Hospital & Regional Medical Center (CHRMC) in Seattle, WA, from July through September 2005. This study was approved by the CHRMC Institutional Review Board. Due to stipulations of the Health Insurance Portability and Accountability Act (HIPAA), we were unable to collect extensive information on those parents who were missed or those who refused to participate in the study.
Exclusions
We excluded parents if: (1) they did not feel comfortable answering a written survey in English or Spanish; (2) their child was transferred to the general medical unit either from the intensive care unit (ICU) or from the inpatient unit of another hospital; or (3) they were not present during the hospitalization.
Study Design
We conducted a cross‐sectional self‐administered written survey of parents. The survey was translated into Spanish by a certified Spanish translator. A second independent translator confirmed the accuracy of the translation. Informed consent was obtained from parents before administration of the survey.
Data Collection
Parents were surveyed with a consecutive sampling methodology Tuesday through Friday from July 2005 through September 2005. We surveyed parents within 48 hours of admission of their child to the hospital, but after they had an opportunity to speak with the inpatient medical team that was caring for their child. A more detailed discussion of the data collection process has been published previously.16
Dependent Variables
Parental Concern About the Need to Watch for Medical Errors
We assessed parental concerns about medical errors during hospitalization by measuring responses to the statement When my child is in the hospital I feel that I have to watch over the care that he/she is receiving to make sure that mistakes aren't made. Parents reported their agreement/disagreement with this statement using a 5‐point Likert scale. For our analysis we dichotomized the dependent variable into those parents who responded Strongly Agree or Agree vs. those who responded Strongly Disagree or Disagree. We chose to focus on parents who expressed a directional response (eg, agree or disagree) because we felt that such responses were more likely to be correlated with behavior. As a result, we excluded from our primary analysis those participants who responded Unsure. In order to determine the effect of exclusion on our results (given its size), we conducted separate post‐hoc analyses in which we included the Unsure respondents in Agree and Disagree categories, respectively.
Independent Variables
Self‐Efficacy in Patient‐Physician Interactions
The Joint Commission's Speak Up initiative7 recommends that patients and parents interact with their healthcare providers in order to prevent errors. We gauged a parent's confidence of interacting with healthcare providers using an adapted scale of the Perceived Efficacy in Patient‐Physician Interactions (PEPPI) self‐efficacy scale. The PEPPI is a 50‐point self‐efficacy scale that has been validated in older adults.17 The response to each question is recorded on a 5‐point Likert scale ranging from 1 to 5 where 1 represents not at all confident and 5 represents very confident. Higher scores on this scale have been associated with greater participation in treatment decisions by women with breast cancer.18 We adapted this scale for use in pediatrics (Appendix 1).
Covariates
Prior Hospitalizations and Chronic Illness History
We asked parents to report how many times their child had been hospitalized prior to this current admission (not including birth). We chose to query parents directly because a search of our institutions' medical record database would not capture hospitalizations at other facilities. We categorized the variable for previous hospitalizations as follows: none, 1, 2, 3.
We asked parents to report if prior to this hospitalization they had ever been told by a nurse or doctor that their child had any of a list of chronic medical conditions such as chronic respiratory disease, mental retardation, and seizure disorder, among others. We gave parents the opportunity to specify a medical condition not provided on this list. The list of conditions was the same as that used in the Child Health Questionnaire PF‐28,19 which has been used in national and international studies to measure quality of life in children with and without chronic conditions20, 21 (Appendix 2).
Limited English Proficiency
We assessed the potential for a language barrier to impede communication between parent and healthcare providers by asking parents the following question: How comfortable are you that you can express your concerns and ask questions of your child's doctors in English? We measured parental responses on a 5‐point Likert scale (very comfortable vs. somewhat comfortable, not sure, somewhat uncomfortable, very uncomfortable). For our analyses, we dichotomized responses into those who reported being very comfortable vs. those who chose any other response category.
Social Desirability
We measured the potential for social desirability to bias responses using the Marlowe‐Crowne 2(10) Scale of Social Desirability.22 The Marlowe‐Crowne 2(10) Scale of Social Desirability is a shorter, validated version of the Marlowe‐Crowne Scale.23 This scale has been recommended by the National Institutes of Health (NIH)'s Behavior Change Consortium for use in behavioral change research related to health.24 It has been used in previous studies to account for social desirability bias in studies which involve patient self‐report of attitudes and beliefs.25 We analyzed scores on a continuous scale with higher scores representing greater social desirability bias in responses.
Demographics
We collected the following demographic data on parents: age, gender, race/ethnicity (white non‐Hispanic vs. other), education (high school or less, some college, college or higher). We also recorded the child's age and gender.
Statistical Analysis
Parental Concern for Medical Errors
Univariate statistics were used to report proportions of parents who were concerned about medical errors and to summarize the data for covariates and demographics. We conducted bivariate logistic regression analyses to assess the association between our outcome variable and the independent variable and each covariate, respectively. We used a Fisher's exact test to examine the association between limited English proficiency and our outcome variable because the absence of participants (eg, a zero cell) who were not very comfortable with English and not concerned about errors precluded the use of bivariate logistic regression. Therefore, to explore the relationship between race and language we used a Fischer's exact test to compare concern about medical errors between white and non‐white participants who were very comfortable with English.
We used multivariate logistic regression to test our hypothesis that greater self‐efficacy would be associated with less concern about medical errors after adjusting for the aforementioned covariates and demographics, excluding child gender. We had no a priori reason to expect that child gender would affect parental self‐efficacy or parental concern about errors and did not include it in the regression model. In order to provide a more clinically relevant interpretation of our results, we calculated adjusted predicted probabilities for the 25%, 50%, and 75% PEPPI scores using the mean for all other variables in the model.
We conducted post‐hoc analysis using a likelihood‐ratio test to determine if the hospitalization variable was significant in the multivariate regression model. We conducted additional post‐hoc analysis using bivariate logistic regression to explore the relationship between concern about medical errors and the following independent variables: hospitalization for >3 days after birth (yes/no); previous hospitalization for >1 week (yes/no); parents' experience with the hospital system (a lot, some, not sure, a little, none); overall perception of child's health (excellent, very good, good, fair); previous hospitalizations for other children (yes, no, no other children); rating of care that child has received (excellent vs. other [very good, good, fair]). We incorporated any significant associations (P < 0.05) into our preexisting multivariate model.
Results
During the time period of our study, 278 parents were eligible to participate. Eighty‐five parents could not be surveyed either because they could not be reached despite multiple attempts (eg, out of the room, speaking with physicians) or because the child had already been discharged. Of the 193 parents approached, 130 agreed to take the survey. Two parents who agreed to complete the survey forgot to return it before their children were discharged. Demographics of respondents and nonparticipants are presented in Table 1. The distribution of self‐efficacy scores was skewed, with a mean score of 45 (median 46, range 5‐50) on a 50‐point scale, consistent with previous studies in adults.18
| Characteristics | Respondents (n = 130) | Number Missed (n = 85) | Number Refused (n = 61) |
|---|---|---|---|
| |||
| Parent's mean age | 34 years (range: 18‐51) | NA | NA |
| Parent sex female, n (%) | 105 (80.8) | NA | NA |
| Parental education, n (%) | |||
| College or higher | 65 (50.4) | ||
| Some college | 34 (26.4) | ||
| High school or less | 30 (23.3) | NA | NA |
| Parental race, n (%) | |||
| White | 86 (67.2) | ||
| Non‐White | 42 (32.8) | NA | NA |
| Parent's social desirability score, mean (SD) | 7.0 (2.0) | NA | NA |
| Child's median age | 21.4 months (range: 1 day‐17.8 years) | 24 months | 24 months |
| Child's sex female, n (%) | 63 (48.5) | 36 (42) | 35 (57) |
| Number of previous hospitalizations (child), n (%) | |||
| None | 68 (53.1) | ||
| 1 | 26 (20.3) | ||
| 2 | 19 (14.8) | ||
| 3 | 15 (11.7) | NA | NA |
| Number of chronic medical conditions (child), n (%) | |||
| None | 56 (48.7) | ||
| 1 | 34 (29.6) | ||
| 2 | 25 (21.8) | NA | NA |
| Parent's comfort expressing concerns in English, n (%) | NA | NA | |
| Very comfortable | 109 (83.9) | ||
| Less than very comfortable | 21 (16.1) | ||
| Self‐efficacy score (parent), mean (SD) | 45 (6.3) | NA | NA |
Eighty‐two parents (63% of respondents) Agreed or Strongly Agreed with the statement When my child is in the hospital I feel that I need to watch over his/her care in order to make sure that mistakes aren't made (Figure 1). In bivariate analyses, non‐white race (Table 2) and English proficiency (P = 0.002) were significantly associated with parental concern about medical errors. Notably, all respondents who were not very comfortable with English agreed that they felt the need to watch over their child's care to ensure that mistakes do not happen. The association between self‐efficacy with physician interactions and concern was nearly significant (Table 2).
| Variable | Crude Odds Ratio | Confidence Interval | P Value | Adjusted Odds Ratio | Confidence Interval | P Value |
|---|---|---|---|---|---|---|
| ||||||
| Parent age (years) | 1.01 | 0.95‐1.06 | 0.79 | 1.05 | 0.95‐1.15 | 0.36 |
| Parent gender | ||||||
| Female | Referent | |||||
| Male | 0.86 | 0.32‐2.35 | 0.77 | 0.76 | 0.20‐2.79 | 0.68 |
| Age of child (months) | 1.00 | 0.99‐1.01 | 0.97 | 1.00 | 0.99‐1.01 | 0.83 |
| Parental education | ||||||
| College or higher | Referent | Referent | ||||
| Some college | 0.48 | 0.18‐1.26 | 0.14 | 0.3 | 0.07‐1.13 | 0.07 |
| High school or less | 1.39 | 0.48‐4.00 | 0.55 | 0.5 | 0.1‐2.2 | 0.38 |
| Parental race | ||||||
| White | Referent | Referent | ||||
| Non‐White | 5.00* | 1.61‐15.56 | 0.005 | 4.9 | 1.19‐20.4 | 0.03 |
| Previous hospitalization (child) | ||||||
| None | Referent | Referent | ||||
| 1 | 0.44 | 0.16‐1.20 | 0.11 | 0.16 | 0.04‐0.69 | 0.01 |
| 2 | 0.89 | 0.27‐2.87 | 0.84 | 0.60 | 0.13‐2.83 | 0.5 |
| 3 | 0.91 | 0.21‐3.84 | 0.90 | 0.79 | 0.12‐5.06 | 0.8 |
| Number of chronic medical conditions | 0.86 | 0.67‐1.11 | 0.26 | 1.05 | 0.74‐1.50 | 0.78 |
| Social desirability score (parent) | 0.99 | 0.81‐1.21 | 0.92 | 0.99 | 0.76‐1.29 | 0.9 |
| Self‐efficacy score (parent) | 0.90 | 0.81‐1.00 | 0.06 | 0.83 | 0.73‐0.95 | 0.006* |
In multivariate analysis, self‐efficacy was independently associated with parental report about the need to watch over a child's care (odds ratio [OR], 0.83; 95% confidence interval [CI], 0.72‐0.92). In prediction models, with self‐efficacy scores of 44 (25th percentile), 46 (50th percentile), and 49 (75th percentile), about 72.2% (59.1‐82.3), 64.2% (51.8‐75.0), and 50.8% (35.3‐66.2) of parents, respectively, would feel the need to watch over their child's care to prevent medical errors.
While respondents of non‐white race had the greatest independent odds of reporting a concern for medical errors occurring while their child was hospitalized (OR, 4.9; 95% CI, 1.19‐20.4), we could not reliably determine how much of this effect was due to language instead of to race because the vast majority of parents who reported being less than very comfortable with English were also non‐white (non‐white 90.5% vs. white 9.5%, P < 0.001). In additional analyses we were unable to find a difference in concern about medical errors between white and non‐white parents who were very comfortable with English (data not shown).
Of note, while having 1 hospitalization compared to none was significantly associated with having decreased concern about medical errors (Table 2), the variable hospitalizations was not significant in the model (P = 0.07).
In post‐hoc analysis, we found no association between hospitalization for >3 days after birth, previous hospitalization for >1 week, parents' experience with the hospital system, and overall perception of child's health, previous hospitalizations for other children. While rating of care that child received was significantly associated with parents' concern about medical errors in the bivariate analysis, it did not remain significant in multivariate analysis and did not substantially change the magnitude or significance of previous associations.
Discussion
In our study, we found that nearly two‐thirds of parents of children admitted to the general pediatric service of a tertiary care children's hospital felt the need to watch over their child's care to ensure that mistakes would not be made. We also found that a parent's self‐efficacy interacting with physicians was associated with less parental concern for medical errors.
To our knowledge, this is the first study to systematically survey parents' concerns about medical errors during a child's hospitalization and to evaluate factors associated with this concern. The immediate question prompted by our findings is whether the fact that 63% of parents are concerned is alarming because it is too low or too high. Some might contend that concern about medical errors is an appropriate and desirable response because it may motivate parents to become more vigilant about the medical care that their child is receiving. However, others may challenge that such concern may indicate a feeling of powerlessness to act to prevent potential errors. In our study, the relationship between higher self‐efficacy and less parental concern raises the possibility that parents with higher levels of self‐efficacy with physician interactions may feel more comfortable communicating with physicians, which in turn may temper parents' concerns about medical errors during hospitalization.
It is equally plausible that concern about medical errors during hospitalization may motivate parents to become involved in their child's medical care and, in turn, lead them to feel empowered to prevent medical errors and so ease their concerns. It is conceivable that experience with past medical errors may fuel a parent's need to watch over their child's care to prevent additional medical errors. Future studies should address the independent effect of past medical errors on parental concern about medical errors.
In this study, all parents who reported being very uncomfortable with English and parents of non‐white race felt the need to watch over their child's care to help prevent errors. A previous survey of a nationally representative sample of U.S. adults found greater proportion of non‐white adults were very concerned about errors or mistakes happening when receiving care at a hospital (blacks 62%, Hispanics 57%, whites 44%).26 However, in our study, the relationship between race and concern is likely mediated by language since many of the parents who described themselves as other than white also reported being not very comfortable with English and we could not find an effect of race on concern among parents who were very comfortable with English. Indeed, previous studies have linked decreased English proficiency to medical errors with potential clinical consequence.27
Given our previous investigation of the relationship between self‐efficacy and parent participation in medical decisions during a child's hospitalization, we conducted post‐hoc analyses exploring the association between parents' self‐report of participation in medical decisions and concern about medical errors during their child's hospitalization.16 Using a simple logistic regression we did not find any association. However, we advise caution in interpreting and generalizing these results because the study was not powered to adequately evaluate this association.
There are additional limitations in our study to be noted. First, this question has not been used previously to assess parental concern about medical errors, so future work will need to focus on assessing its reliability and validity. Second, it is also possible that parents' concern for medical errors is mitigated by the complexity of their child's healthcare.5 We attempted to address this issue by controlling for the child's number of chronic illnesses. However, it is possible that our metric did not capture the level of complexity associated with different types of chronic conditions. Moreover, additional variables such as health insurance type, parental physical and mental health, and quality of interactions with the nursing staff may confound the relationships that we observed. Future studies should examine the effect of these variables on parents' self‐efficacy and their concern about medical errors.
Third, we surveyed parents at a single institution and, as such, differences in demographics and hospital‐specific practices related to patient‐physician interactions may prevent generalization of our findings to other institutions. For example, the parents in our survey had a higher average education level than the general population and the racial makeup of our population was not nationally representative. Also, due to HIPAA constraints, we were unable to collect extensive demographic information on parents and children who were missed or those who refused to participate in the study, which also could conceivably influence the strength of our findings.
Fourth, we adapted a validated adult measure of self‐efficacy for use in pediatrics. The patient‐physician self‐efficacy scale, the PEPPI, did have a skewed distribution in our study, although this performance is consistent with adult studies18 and in post‐hoc analyses, outlier PEPPI scores did not have a significant effect on the magnitude of the relationship we observed between self‐efficacy and parental concern about medical errors. However, the reading level of this instrument is ninth grade, which may impact the generalization of our findings to populations with lower literacy levels.
Fifth, we excluded parents who were unsure about their concern from our analyses. In post‐hoc multivariate regression analyses, reassignment of unsure responses to either agree or disagree did not result in any change in odds ratio for any endpoint.
Finally, it is possible that parental concern was influenced by social desirability bias in that parents may have been less likely to report concern about medical errors during a hospitalization because of fear of the implications it might have for their child's care. We attempted to control for this effect by adjusting for social desirability bias using the Marlowe‐Crowne scale. This scale is commonly used in behavioral science research to account for such response bias and has been recommended by the NIH Consortium on Behavior Change for use in behavioral change research related to health.24
Within the context of these limitations, we feel that our study contributes an important first step toward characterizing the scope of parental concern about medical errors during pediatric hospitalizations and understanding the relationship of self‐efficacy with physician interactions to this concern. Devising a quality initiative program to improve parents' self‐efficacy interacting with physicians might help to temper parents' concerns about medical errors while also encouraging their involvement in their child's medical care. Such a program would likely prove most beneficial if it sought to improve self‐efficacy among parents with lower English proficiency given that this group had the highest concern for medical errors. Possible interventions might include more ready access to interpreters or use of visual aids.
The Institute of Medicine report linking between 48,000 and 98,000 deaths annually to medical errors1 has raised awareness about medical errors across all areas of medicine. In pediatrics, medical errors in hospitalized children are associated with significant increases in length of stay, healthcare costs, and death.2, 3 While much attention has been paid to the use of hospital systems to prevent medical errors, there has been considerably less focus on the experiences of patients and their potential role in preventing errors.
Studies have suggested that a significant majority of adult patients are concerned about medical errors during hospitalization.4, 5 However, a similar assessment of parents' concerns about medical errors in pediatrics is lacking. Admittedly, for concern to be constructive it must be linked to action. The Joint Commission and the Agency for Healthcare Research and Quality (AHRQ) currently recommend that parents help prevent errors by becoming active, involved and informed members of their healthcare team and taking part in every decision about (their) child's health care.6, 7 However, the extent to which parental concern about medical errors is related to a parent's self‐efficacy, or confidence, interacting with physicians is unknown.
Self‐efficacy is a construct used in social cognitive theory to explain behavior change.8 It refers to an individual's belief in (his/her) capabilities to organize and execute the courses of action required to produce given attainments or a desired outcome.9 Self‐efficacy is not a general concept; it must be discussed in reference to a specific activity. In healthcare it has been associated not only with willingness to adopt preventive strategies,10 but also with treatment adherence,11, 12 behavior change,13 and with greater patient participation in healthcare decision‐making.14, 15
In this study we had 2 objectives. First, we sought to assess the proportion of parents of hospitalized children who are concerned about medical errors. Second, we attempted to examine whether a parent's self‐efficacy interacting with physicians was associated with their concern about medical errors for their child. Given that parents with greater self‐efficacy interacting with physicians might feel more empowered to prevent errors and, as such, be more inclined to take an active role to do so, we hypothesized that such parents would be less concerned about medical errors during a pediatric hospitalization.
Subjects and Methods
Population
We surveyed parents of children <18 years of age (including 2 grandparents who will hereafter be referred to as parents) who were admitted to the general medical service of the Children's Hospital & Regional Medical Center (CHRMC) in Seattle, WA, from July through September 2005. This study was approved by the CHRMC Institutional Review Board. Due to stipulations of the Health Insurance Portability and Accountability Act (HIPAA), we were unable to collect extensive information on those parents who were missed or those who refused to participate in the study.
Exclusions
We excluded parents if: (1) they did not feel comfortable answering a written survey in English or Spanish; (2) their child was transferred to the general medical unit either from the intensive care unit (ICU) or from the inpatient unit of another hospital; or (3) they were not present during the hospitalization.
Study Design
We conducted a cross‐sectional self‐administered written survey of parents. The survey was translated into Spanish by a certified Spanish translator. A second independent translator confirmed the accuracy of the translation. Informed consent was obtained from parents before administration of the survey.
Data Collection
Parents were surveyed with a consecutive sampling methodology Tuesday through Friday from July 2005 through September 2005. We surveyed parents within 48 hours of admission of their child to the hospital, but after they had an opportunity to speak with the inpatient medical team that was caring for their child. A more detailed discussion of the data collection process has been published previously.16
Dependent Variables
Parental Concern About the Need to Watch for Medical Errors
We assessed parental concerns about medical errors during hospitalization by measuring responses to the statement When my child is in the hospital I feel that I have to watch over the care that he/she is receiving to make sure that mistakes aren't made. Parents reported their agreement/disagreement with this statement using a 5‐point Likert scale. For our analysis we dichotomized the dependent variable into those parents who responded Strongly Agree or Agree vs. those who responded Strongly Disagree or Disagree. We chose to focus on parents who expressed a directional response (eg, agree or disagree) because we felt that such responses were more likely to be correlated with behavior. As a result, we excluded from our primary analysis those participants who responded Unsure. In order to determine the effect of exclusion on our results (given its size), we conducted separate post‐hoc analyses in which we included the Unsure respondents in Agree and Disagree categories, respectively.
Independent Variables
Self‐Efficacy in Patient‐Physician Interactions
The Joint Commission's Speak Up initiative7 recommends that patients and parents interact with their healthcare providers in order to prevent errors. We gauged a parent's confidence of interacting with healthcare providers using an adapted scale of the Perceived Efficacy in Patient‐Physician Interactions (PEPPI) self‐efficacy scale. The PEPPI is a 50‐point self‐efficacy scale that has been validated in older adults.17 The response to each question is recorded on a 5‐point Likert scale ranging from 1 to 5 where 1 represents not at all confident and 5 represents very confident. Higher scores on this scale have been associated with greater participation in treatment decisions by women with breast cancer.18 We adapted this scale for use in pediatrics (Appendix 1).
Covariates
Prior Hospitalizations and Chronic Illness History
We asked parents to report how many times their child had been hospitalized prior to this current admission (not including birth). We chose to query parents directly because a search of our institutions' medical record database would not capture hospitalizations at other facilities. We categorized the variable for previous hospitalizations as follows: none, 1, 2, 3.
We asked parents to report if prior to this hospitalization they had ever been told by a nurse or doctor that their child had any of a list of chronic medical conditions such as chronic respiratory disease, mental retardation, and seizure disorder, among others. We gave parents the opportunity to specify a medical condition not provided on this list. The list of conditions was the same as that used in the Child Health Questionnaire PF‐28,19 which has been used in national and international studies to measure quality of life in children with and without chronic conditions20, 21 (Appendix 2).
Limited English Proficiency
We assessed the potential for a language barrier to impede communication between parent and healthcare providers by asking parents the following question: How comfortable are you that you can express your concerns and ask questions of your child's doctors in English? We measured parental responses on a 5‐point Likert scale (very comfortable vs. somewhat comfortable, not sure, somewhat uncomfortable, very uncomfortable). For our analyses, we dichotomized responses into those who reported being very comfortable vs. those who chose any other response category.
Social Desirability
We measured the potential for social desirability to bias responses using the Marlowe‐Crowne 2(10) Scale of Social Desirability.22 The Marlowe‐Crowne 2(10) Scale of Social Desirability is a shorter, validated version of the Marlowe‐Crowne Scale.23 This scale has been recommended by the National Institutes of Health (NIH)'s Behavior Change Consortium for use in behavioral change research related to health.24 It has been used in previous studies to account for social desirability bias in studies which involve patient self‐report of attitudes and beliefs.25 We analyzed scores on a continuous scale with higher scores representing greater social desirability bias in responses.
Demographics
We collected the following demographic data on parents: age, gender, race/ethnicity (white non‐Hispanic vs. other), education (high school or less, some college, college or higher). We also recorded the child's age and gender.
Statistical Analysis
Parental Concern for Medical Errors
Univariate statistics were used to report proportions of parents who were concerned about medical errors and to summarize the data for covariates and demographics. We conducted bivariate logistic regression analyses to assess the association between our outcome variable and the independent variable and each covariate, respectively. We used a Fisher's exact test to examine the association between limited English proficiency and our outcome variable because the absence of participants (eg, a zero cell) who were not very comfortable with English and not concerned about errors precluded the use of bivariate logistic regression. Therefore, to explore the relationship between race and language we used a Fischer's exact test to compare concern about medical errors between white and non‐white participants who were very comfortable with English.
We used multivariate logistic regression to test our hypothesis that greater self‐efficacy would be associated with less concern about medical errors after adjusting for the aforementioned covariates and demographics, excluding child gender. We had no a priori reason to expect that child gender would affect parental self‐efficacy or parental concern about errors and did not include it in the regression model. In order to provide a more clinically relevant interpretation of our results, we calculated adjusted predicted probabilities for the 25%, 50%, and 75% PEPPI scores using the mean for all other variables in the model.
We conducted post‐hoc analysis using a likelihood‐ratio test to determine if the hospitalization variable was significant in the multivariate regression model. We conducted additional post‐hoc analysis using bivariate logistic regression to explore the relationship between concern about medical errors and the following independent variables: hospitalization for >3 days after birth (yes/no); previous hospitalization for >1 week (yes/no); parents' experience with the hospital system (a lot, some, not sure, a little, none); overall perception of child's health (excellent, very good, good, fair); previous hospitalizations for other children (yes, no, no other children); rating of care that child has received (excellent vs. other [very good, good, fair]). We incorporated any significant associations (P < 0.05) into our preexisting multivariate model.
Results
During the time period of our study, 278 parents were eligible to participate. Eighty‐five parents could not be surveyed either because they could not be reached despite multiple attempts (eg, out of the room, speaking with physicians) or because the child had already been discharged. Of the 193 parents approached, 130 agreed to take the survey. Two parents who agreed to complete the survey forgot to return it before their children were discharged. Demographics of respondents and nonparticipants are presented in Table 1. The distribution of self‐efficacy scores was skewed, with a mean score of 45 (median 46, range 5‐50) on a 50‐point scale, consistent with previous studies in adults.18
| Characteristics | Respondents (n = 130) | Number Missed (n = 85) | Number Refused (n = 61) |
|---|---|---|---|
| |||
| Parent's mean age | 34 years (range: 18‐51) | NA | NA |
| Parent sex female, n (%) | 105 (80.8) | NA | NA |
| Parental education, n (%) | |||
| College or higher | 65 (50.4) | ||
| Some college | 34 (26.4) | ||
| High school or less | 30 (23.3) | NA | NA |
| Parental race, n (%) | |||
| White | 86 (67.2) | ||
| Non‐White | 42 (32.8) | NA | NA |
| Parent's social desirability score, mean (SD) | 7.0 (2.0) | NA | NA |
| Child's median age | 21.4 months (range: 1 day‐17.8 years) | 24 months | 24 months |
| Child's sex female, n (%) | 63 (48.5) | 36 (42) | 35 (57) |
| Number of previous hospitalizations (child), n (%) | |||
| None | 68 (53.1) | ||
| 1 | 26 (20.3) | ||
| 2 | 19 (14.8) | ||
| 3 | 15 (11.7) | NA | NA |
| Number of chronic medical conditions (child), n (%) | |||
| None | 56 (48.7) | ||
| 1 | 34 (29.6) | ||
| 2 | 25 (21.8) | NA | NA |
| Parent's comfort expressing concerns in English, n (%) | NA | NA | |
| Very comfortable | 109 (83.9) | ||
| Less than very comfortable | 21 (16.1) | ||
| Self‐efficacy score (parent), mean (SD) | 45 (6.3) | NA | NA |
Eighty‐two parents (63% of respondents) Agreed or Strongly Agreed with the statement When my child is in the hospital I feel that I need to watch over his/her care in order to make sure that mistakes aren't made (Figure 1). In bivariate analyses, non‐white race (Table 2) and English proficiency (P = 0.002) were significantly associated with parental concern about medical errors. Notably, all respondents who were not very comfortable with English agreed that they felt the need to watch over their child's care to ensure that mistakes do not happen. The association between self‐efficacy with physician interactions and concern was nearly significant (Table 2).
| Variable | Crude Odds Ratio | Confidence Interval | P Value | Adjusted Odds Ratio | Confidence Interval | P Value |
|---|---|---|---|---|---|---|
| ||||||
| Parent age (years) | 1.01 | 0.95‐1.06 | 0.79 | 1.05 | 0.95‐1.15 | 0.36 |
| Parent gender | ||||||
| Female | Referent | |||||
| Male | 0.86 | 0.32‐2.35 | 0.77 | 0.76 | 0.20‐2.79 | 0.68 |
| Age of child (months) | 1.00 | 0.99‐1.01 | 0.97 | 1.00 | 0.99‐1.01 | 0.83 |
| Parental education | ||||||
| College or higher | Referent | Referent | ||||
| Some college | 0.48 | 0.18‐1.26 | 0.14 | 0.3 | 0.07‐1.13 | 0.07 |
| High school or less | 1.39 | 0.48‐4.00 | 0.55 | 0.5 | 0.1‐2.2 | 0.38 |
| Parental race | ||||||
| White | Referent | Referent | ||||
| Non‐White | 5.00* | 1.61‐15.56 | 0.005 | 4.9 | 1.19‐20.4 | 0.03 |
| Previous hospitalization (child) | ||||||
| None | Referent | Referent | ||||
| 1 | 0.44 | 0.16‐1.20 | 0.11 | 0.16 | 0.04‐0.69 | 0.01 |
| 2 | 0.89 | 0.27‐2.87 | 0.84 | 0.60 | 0.13‐2.83 | 0.5 |
| 3 | 0.91 | 0.21‐3.84 | 0.90 | 0.79 | 0.12‐5.06 | 0.8 |
| Number of chronic medical conditions | 0.86 | 0.67‐1.11 | 0.26 | 1.05 | 0.74‐1.50 | 0.78 |
| Social desirability score (parent) | 0.99 | 0.81‐1.21 | 0.92 | 0.99 | 0.76‐1.29 | 0.9 |
| Self‐efficacy score (parent) | 0.90 | 0.81‐1.00 | 0.06 | 0.83 | 0.73‐0.95 | 0.006* |
In multivariate analysis, self‐efficacy was independently associated with parental report about the need to watch over a child's care (odds ratio [OR], 0.83; 95% confidence interval [CI], 0.72‐0.92). In prediction models, with self‐efficacy scores of 44 (25th percentile), 46 (50th percentile), and 49 (75th percentile), about 72.2% (59.1‐82.3), 64.2% (51.8‐75.0), and 50.8% (35.3‐66.2) of parents, respectively, would feel the need to watch over their child's care to prevent medical errors.
While respondents of non‐white race had the greatest independent odds of reporting a concern for medical errors occurring while their child was hospitalized (OR, 4.9; 95% CI, 1.19‐20.4), we could not reliably determine how much of this effect was due to language instead of to race because the vast majority of parents who reported being less than very comfortable with English were also non‐white (non‐white 90.5% vs. white 9.5%, P < 0.001). In additional analyses we were unable to find a difference in concern about medical errors between white and non‐white parents who were very comfortable with English (data not shown).
Of note, while having 1 hospitalization compared to none was significantly associated with having decreased concern about medical errors (Table 2), the variable hospitalizations was not significant in the model (P = 0.07).
In post‐hoc analysis, we found no association between hospitalization for >3 days after birth, previous hospitalization for >1 week, parents' experience with the hospital system, and overall perception of child's health, previous hospitalizations for other children. While rating of care that child received was significantly associated with parents' concern about medical errors in the bivariate analysis, it did not remain significant in multivariate analysis and did not substantially change the magnitude or significance of previous associations.
Discussion
In our study, we found that nearly two‐thirds of parents of children admitted to the general pediatric service of a tertiary care children's hospital felt the need to watch over their child's care to ensure that mistakes would not be made. We also found that a parent's self‐efficacy interacting with physicians was associated with less parental concern for medical errors.
To our knowledge, this is the first study to systematically survey parents' concerns about medical errors during a child's hospitalization and to evaluate factors associated with this concern. The immediate question prompted by our findings is whether the fact that 63% of parents are concerned is alarming because it is too low or too high. Some might contend that concern about medical errors is an appropriate and desirable response because it may motivate parents to become more vigilant about the medical care that their child is receiving. However, others may challenge that such concern may indicate a feeling of powerlessness to act to prevent potential errors. In our study, the relationship between higher self‐efficacy and less parental concern raises the possibility that parents with higher levels of self‐efficacy with physician interactions may feel more comfortable communicating with physicians, which in turn may temper parents' concerns about medical errors during hospitalization.
It is equally plausible that concern about medical errors during hospitalization may motivate parents to become involved in their child's medical care and, in turn, lead them to feel empowered to prevent medical errors and so ease their concerns. It is conceivable that experience with past medical errors may fuel a parent's need to watch over their child's care to prevent additional medical errors. Future studies should address the independent effect of past medical errors on parental concern about medical errors.
In this study, all parents who reported being very uncomfortable with English and parents of non‐white race felt the need to watch over their child's care to help prevent errors. A previous survey of a nationally representative sample of U.S. adults found greater proportion of non‐white adults were very concerned about errors or mistakes happening when receiving care at a hospital (blacks 62%, Hispanics 57%, whites 44%).26 However, in our study, the relationship between race and concern is likely mediated by language since many of the parents who described themselves as other than white also reported being not very comfortable with English and we could not find an effect of race on concern among parents who were very comfortable with English. Indeed, previous studies have linked decreased English proficiency to medical errors with potential clinical consequence.27
Given our previous investigation of the relationship between self‐efficacy and parent participation in medical decisions during a child's hospitalization, we conducted post‐hoc analyses exploring the association between parents' self‐report of participation in medical decisions and concern about medical errors during their child's hospitalization.16 Using a simple logistic regression we did not find any association. However, we advise caution in interpreting and generalizing these results because the study was not powered to adequately evaluate this association.
There are additional limitations in our study to be noted. First, this question has not been used previously to assess parental concern about medical errors, so future work will need to focus on assessing its reliability and validity. Second, it is also possible that parents' concern for medical errors is mitigated by the complexity of their child's healthcare.5 We attempted to address this issue by controlling for the child's number of chronic illnesses. However, it is possible that our metric did not capture the level of complexity associated with different types of chronic conditions. Moreover, additional variables such as health insurance type, parental physical and mental health, and quality of interactions with the nursing staff may confound the relationships that we observed. Future studies should examine the effect of these variables on parents' self‐efficacy and their concern about medical errors.
Third, we surveyed parents at a single institution and, as such, differences in demographics and hospital‐specific practices related to patient‐physician interactions may prevent generalization of our findings to other institutions. For example, the parents in our survey had a higher average education level than the general population and the racial makeup of our population was not nationally representative. Also, due to HIPAA constraints, we were unable to collect extensive demographic information on parents and children who were missed or those who refused to participate in the study, which also could conceivably influence the strength of our findings.
Fourth, we adapted a validated adult measure of self‐efficacy for use in pediatrics. The patient‐physician self‐efficacy scale, the PEPPI, did have a skewed distribution in our study, although this performance is consistent with adult studies18 and in post‐hoc analyses, outlier PEPPI scores did not have a significant effect on the magnitude of the relationship we observed between self‐efficacy and parental concern about medical errors. However, the reading level of this instrument is ninth grade, which may impact the generalization of our findings to populations with lower literacy levels.
Fifth, we excluded parents who were unsure about their concern from our analyses. In post‐hoc multivariate regression analyses, reassignment of unsure responses to either agree or disagree did not result in any change in odds ratio for any endpoint.
Finally, it is possible that parental concern was influenced by social desirability bias in that parents may have been less likely to report concern about medical errors during a hospitalization because of fear of the implications it might have for their child's care. We attempted to control for this effect by adjusting for social desirability bias using the Marlowe‐Crowne scale. This scale is commonly used in behavioral science research to account for such response bias and has been recommended by the NIH Consortium on Behavior Change for use in behavioral change research related to health.24
Within the context of these limitations, we feel that our study contributes an important first step toward characterizing the scope of parental concern about medical errors during pediatric hospitalizations and understanding the relationship of self‐efficacy with physician interactions to this concern. Devising a quality initiative program to improve parents' self‐efficacy interacting with physicians might help to temper parents' concerns about medical errors while also encouraging their involvement in their child's medical care. Such a program would likely prove most beneficial if it sought to improve self‐efficacy among parents with lower English proficiency given that this group had the highest concern for medical errors. Possible interventions might include more ready access to interpreters or use of visual aids.
- Institute of Medicine Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,,, et al.Medication errors and adverse drug events in pediatric inpatients.JAMA.2001;285(16):2114–2120.
- ,.Pediatric patient safety in hospitals: a national picture in 2000.Pediatrics.2004;113(6):1741–1746.
- ,,,,,.Brief report: hospitalized patients' attitudes about and participation in error prevention.J Gen Intern Med.2006;21(4):367–370.
- ,,, et al.Patients' concerns about medical errors during hospitalization.Jt Comm J Qual Patient Saf.2007;33(1):5–14.
- Agency for Healthcare Research and Quality.20 Tips to Help Prevent Medical Errors in Children. Patient Fact Sheet. 2009, AHRQ Publication No. 02‐P034.Rockville, MD:Agency for Healthcare Research and Quality.
- Joint Commission on Accreditation of Healthcare Organizations. Speak Up Initiatives. Available at: http://www.jointcommission.org/PatientSafety/SpeakUp. Accessed May 2009.
- .Self‐efficacy: toward a unifying theory of behavioral change.Psychol Rev.1977;84(2):191–215.
- .Self‐Efficacy: The Exercise of Control.New York, NY:W.H. Freeman and Company;1997.
- ,,,.Psychosocial correlates of physical activity in healthy children.Arch Pediatr Adolesc Med.2001;155(8):897–902.
- ,,,,.Self‐efficacy as a mediator variable for adolescents' adherence to treatment for insulin‐dependent diabetes mellitus.Children's Health Care.2000;29(1):47–63.
- ,,.Diabetes regimen behaviors. Predicting adherence.Med Care.1987;25(9):868–881.
- ,,,,,.Pediatrician self‐efficacy for counseling parents of asthmatic children to quit smoking.Pediatrics.2004;113(1 Pt 1):78–81.
- ,,.Examining the relationship of patients' attitudes and beliefs with their self‐reported level of participation in medical decision‐making.Med Care.2005;43(9):865–872.
- ,,,,,.Patient‐physician concordance: preferences, perceptions, and factors influencing the breast cancer surgical decision.J Clin Oncol.2004;22(15):3091–3098.
- ,,.Toward family‐centered inpatient medical care: the role of parents as participants in medical decisions.J Pediatr.2007;151(6):690–695.
- ,,,,.Perceived efficacy in patient‐physician interactions (PEPPI): validation of an instrument in older persons.J Am Geriatr Soc.1998;46(7):889–894.
- ,,,.Determinants of participation in treatment decision‐making by older breast cancer patients.Breast Cancer Res Treat.2004;85(3):201–209.
- ,.The CHQ: A User's Manual (2nd printing).Boston, MA:HealthAct;1999.
- ,,,,.The health and well‐being of adolescents: a school‐based population study of the self‐report Child Health Questionnaire.J Adolesc Health.2001;29(2):140–149.
- ,,.The Child Health Questionnaire in children with diabetes: cross‐sectional survey of parent and adolescent‐reported functional health status.Diabet Med.2000;17(10):700–707.
- ,.Semantic style variance in personality questionnaires.J Psychol.1973;85:109–118.
- ,.A new scale of social desirability independent of psychopathology.J Consult Psychol.1960;24:349–354.
- National Institutes of Health. Behavior Change Consortium‐Recommended Nutrition Measures. Available at:http://www1.od.nih.gov/behaviorchange/measures/nutrition.htm. Accessed May 2009.
- ,,.Response bias influences mental health symptom reporting in patients with obstructive sleep apnea.Ann Behav Med.2001;23(4):313–317.
- Kaiser Family Foundation, Agency for Healthcare Research and Quality.Americans as Health Care Consumers: Update on the Role of Quality Information.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- ,,, et al.Errors in medical interpretation and their potential clinical consequences in pediatric encounters.Pediatrics.2003;111(1):6–14.
- Institute of Medicine Committee on Quality of Health Care in America.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- ,,, et al.Medication errors and adverse drug events in pediatric inpatients.JAMA.2001;285(16):2114–2120.
- ,.Pediatric patient safety in hospitals: a national picture in 2000.Pediatrics.2004;113(6):1741–1746.
- ,,,,,.Brief report: hospitalized patients' attitudes about and participation in error prevention.J Gen Intern Med.2006;21(4):367–370.
- ,,, et al.Patients' concerns about medical errors during hospitalization.Jt Comm J Qual Patient Saf.2007;33(1):5–14.
- Agency for Healthcare Research and Quality.20 Tips to Help Prevent Medical Errors in Children. Patient Fact Sheet. 2009, AHRQ Publication No. 02‐P034.Rockville, MD:Agency for Healthcare Research and Quality.
- Joint Commission on Accreditation of Healthcare Organizations. Speak Up Initiatives. Available at: http://www.jointcommission.org/PatientSafety/SpeakUp. Accessed May 2009.
- .Self‐efficacy: toward a unifying theory of behavioral change.Psychol Rev.1977;84(2):191–215.
- .Self‐Efficacy: The Exercise of Control.New York, NY:W.H. Freeman and Company;1997.
- ,,,.Psychosocial correlates of physical activity in healthy children.Arch Pediatr Adolesc Med.2001;155(8):897–902.
- ,,,,.Self‐efficacy as a mediator variable for adolescents' adherence to treatment for insulin‐dependent diabetes mellitus.Children's Health Care.2000;29(1):47–63.
- ,,.Diabetes regimen behaviors. Predicting adherence.Med Care.1987;25(9):868–881.
- ,,,,,.Pediatrician self‐efficacy for counseling parents of asthmatic children to quit smoking.Pediatrics.2004;113(1 Pt 1):78–81.
- ,,.Examining the relationship of patients' attitudes and beliefs with their self‐reported level of participation in medical decision‐making.Med Care.2005;43(9):865–872.
- ,,,,,.Patient‐physician concordance: preferences, perceptions, and factors influencing the breast cancer surgical decision.J Clin Oncol.2004;22(15):3091–3098.
- ,,.Toward family‐centered inpatient medical care: the role of parents as participants in medical decisions.J Pediatr.2007;151(6):690–695.
- ,,,,.Perceived efficacy in patient‐physician interactions (PEPPI): validation of an instrument in older persons.J Am Geriatr Soc.1998;46(7):889–894.
- ,,,.Determinants of participation in treatment decision‐making by older breast cancer patients.Breast Cancer Res Treat.2004;85(3):201–209.
- ,.The CHQ: A User's Manual (2nd printing).Boston, MA:HealthAct;1999.
- ,,,,.The health and well‐being of adolescents: a school‐based population study of the self‐report Child Health Questionnaire.J Adolesc Health.2001;29(2):140–149.
- ,,.The Child Health Questionnaire in children with diabetes: cross‐sectional survey of parent and adolescent‐reported functional health status.Diabet Med.2000;17(10):700–707.
- ,.Semantic style variance in personality questionnaires.J Psychol.1973;85:109–118.
- ,.A new scale of social desirability independent of psychopathology.J Consult Psychol.1960;24:349–354.
- National Institutes of Health. Behavior Change Consortium‐Recommended Nutrition Measures. Available at:http://www1.od.nih.gov/behaviorchange/measures/nutrition.htm. Accessed May 2009.
- ,,.Response bias influences mental health symptom reporting in patients with obstructive sleep apnea.Ann Behav Med.2001;23(4):313–317.
- Kaiser Family Foundation, Agency for Healthcare Research and Quality.Americans as Health Care Consumers: Update on the Role of Quality Information.Rockville, MD:Agency for Healthcare Research and Quality;2000.
- ,,, et al.Errors in medical interpretation and their potential clinical consequences in pediatric encounters.Pediatrics.2003;111(1):6–14.
Copyright © 2009 Society of Hospital Medicine
Variation in Ordering CBCs for Bronchiolitis
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
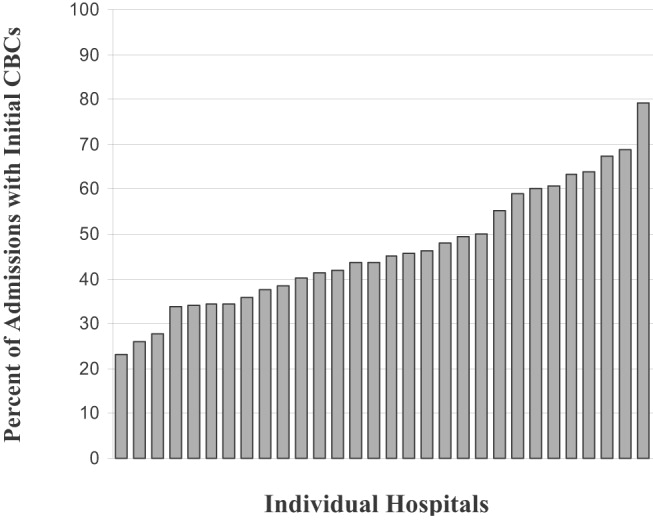
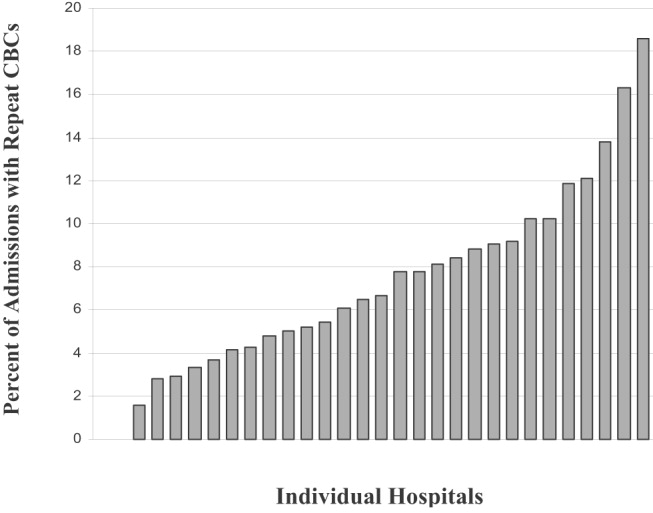
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
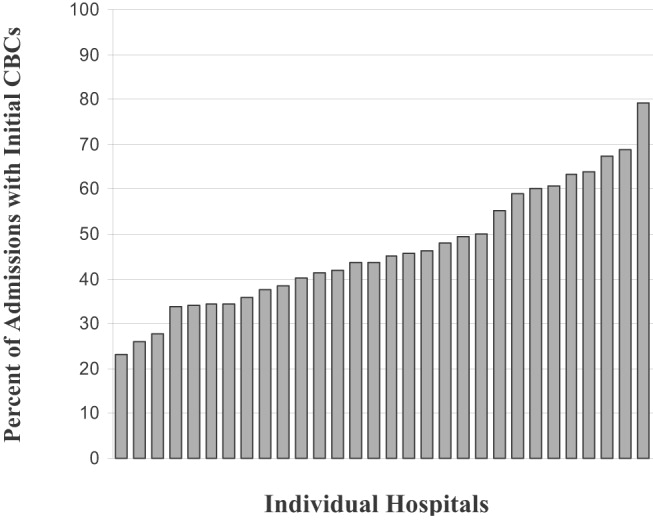
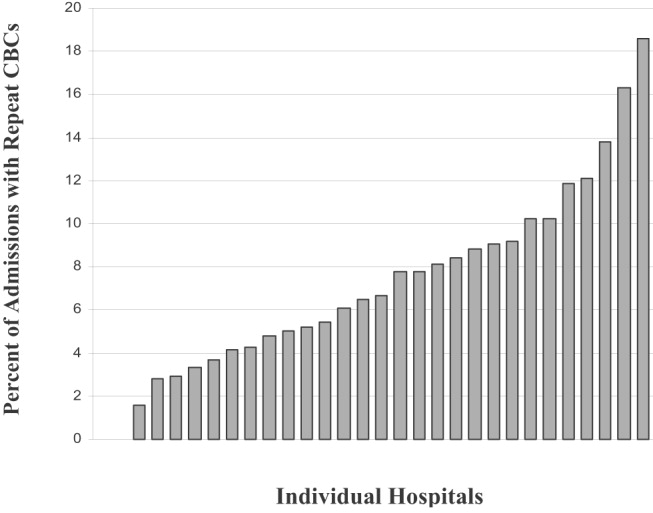
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
Bronchiolitis was the most common primary diagnosis of infants hospitalized in the United States from 2000 to 2001.1 Consequently, much research has focused on the effectiveness of management24 and variation in care, especially the use of unproven diagnostic tests such as chest x‐rays.5 Such variation may have substantial financial and medical impact and has been shown to correlate significantly with hospital costs and length of stay.6
Because bronchiolitis is primarily a clinical diagnosis,7 there is no strong evidence to support the role of diagnostic testing, particularly that of complete blood counts (CBCs).8 Moreover, given the limited diagnostic utility of a single CBC, the benefit of obtaining a second CBC, especially with its associated physical discomfort and additional financial costs, is questionable. Yet despite the lack of evidence and rationale to support initial and repeated ordering of CBCs, we suspect that this practice may be more widespread and variable than currently appreciated.
Using a national database of children's hospitals, we sought to determine the frequency with which CBCs are ordered and repeated during hospitalizations for bronchiolitis, the extent to which these practices vary across institutions, and the relationship of these practices to average charges for a hospital stay.
METHODS
Data Source
We analyzed cases of children with bronchiolitis from the Pediatric Health Information System (PHIS) database of the Child Health Corporation of America.9 This database contains inpatient demographic, administrative, and diagnostic data from 36 freestanding, noncompeting children's hospitals in the United States. However, only 30 of the hospitals provided information on diagnostic testing during the period of our study. To protect the participating hospitals, hospitals were deidentified in this analysis. Diagnoses in the database are provided in the International Classification of Disease, 9th revision (ICD‐9), and the All‐Patient Refined Diagnostic Related Groups (APR‐DRGs), version 15 format.
Cases
We included in our sample children who had a primary ICD‐9 discharge code for bronchiolitis (469.11 or 469.19), an APR‐DRG for bronchiolitis/asthma (141), and a discharge date between October 2001 and September 2003.10 We further restricted cases to children less than 12 months of age because this is the age group most frequently hospitalized for bronchiolitis. Only the first admission per child was included in the analysis.
Outcome and Covariates
We identified the number of CBCs ordered using charge codes in the PHIS data. To avoid double counting, we required that the CBCs be charged on different dates of service, and we counted a maximum of 1 CBC per day per patient. We defined a child as having a repeated CBC if more than 1 CBC was charged during the child's hospital stay. Our outcome variable of repeat CBCs was measured dichotomously. We included age, male sex, Medicaid status, season of admission, intensive care unit (ICU) admission, APR‐DRG‐calculated severity scores for bronchiolitis/asthma (to adjust for disease severity), and length of stay as covariates in the regression and ANOVA analyses. All covariates were measured dichotomously, except for mean age and LOS, which were measured continuously.
Statistical Analyses
Bivariate analysis of baseline characteristics were compared across age groups using 2 tests to compare differences between categorical variables and the Student t test to compare differences between continuous variables.
To examine variability across hospitals in the initial and repeat ordering of CBCs, we performed multivariate ANOVA (MANOVA) controlling for age, sex, Medicaid status, illness severity, season of admission, ICU admission, and length of stay (LOS). Because the factors associated with repeat CBCs are not readily apparent, we performed logistic regression to determine which of these factors were significantly associated (P < .05) with having repeat CBCs performed. To account for the influence of age on the management and epidemiology of children with respiratory distress, we stratified MANOVA and regression analyses by age (< 3 months and 3 months. We clustered our regression analysis by hospital to determine whether there was hospital‐specific variation in repeating CBCs.
We performed post hoc analysis after noting additional variable relationships in our results. To determine whether CBC‐ordering patterns differed by severity, we stratified the analysis of repeat CBCs in both the bivariate and multivariate model by disease severity and ICU admission, respectively.
To determine if the number of CBCs ordered was related to admission charges, we categorized hospitals into tertiles (lowest, intermediate, highest) according to the proportion of admissions in which CBCs were ordered. We then calculated average admission hospital stay charges for each hospital. We used Student t tests to examine the relationship between the charges for admissions in hospitals with the intermediate and highest proportion of admissions with CBCs compared with those hospitals with the lowest proportion of admissions with CBCs.
We used Stata 8.0 to conduct our analyses.11 The Children's Hospital and Regional Medical Center Institutional Review Board (Seattle, WA) approved the analysis of the data for this study.
RESULTS
A total of 17,397 children met the inclusion criteria. Children under 3 months were more likely to be covered by Medicaid, be admitted to the ICU, have a longer length of stay, and have at least 1 CBC (Table 1). Of all children hospitalized, 48.2% had at least 1 CBC, and 7.8% had more than 1 CBC performed during their hospital stay. Notably, the proportion of all admissions with at least 1 CBC varied from 23.2% to 79.2% (Fig. 1), and those with repeat CBCs varied from 0% to 18.6% across hospitals (Fig. 2). This variation was significant when stratified by age and adjusted for covariates, which included length of stay and severity of illness (P < .001). In additional post hoc analyses we found differences in ordering pattern by disease severity that should be noted. The proportion of admissions with repeat CBCs varied significantly across severity groups (mild 3.9%, moderate 10.3%, and severe 21.3%, P < .001) and ICU admission status (ICU admission 5.5%, no ICU admission 23%, P <.001). Stratified analyses indicated an interaction between ICU utilization and disease severity, but neither covariate showed significant interactions with other variables in the model (data not shown).
| < 3 Months of Age | 3‐11 Months of Age | |
|---|---|---|
| ||
| Sample size | 7336 | 10,061 |
| Mean age (months) | 1.4 | 5.8 |
| Male (%) | 58.3 | 59.3 |
| Medicaid (%) | 56.0* | 53.8 |
| Admission Season | ||
| October‐February (%) | 71.0 | 70.4 |
| APG‐DRG severity score | ||
| Mild | 63.0 | 63.4 |
| Moderate | 22.4 | 22.7 |
| Severe | 14.6 | 13.8 |
| ICU admission (%) | 15.7 | 11.2 |
| Mean length of stay (days) | 3.1 | 2.8 |
| Received 1 CBC | 53.8 | 44.1 |
| Received > 1 CBC | 9.2 | 6.8 |
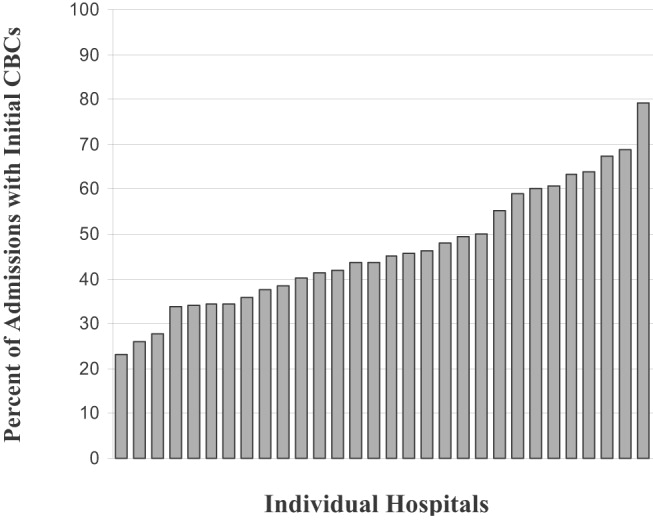
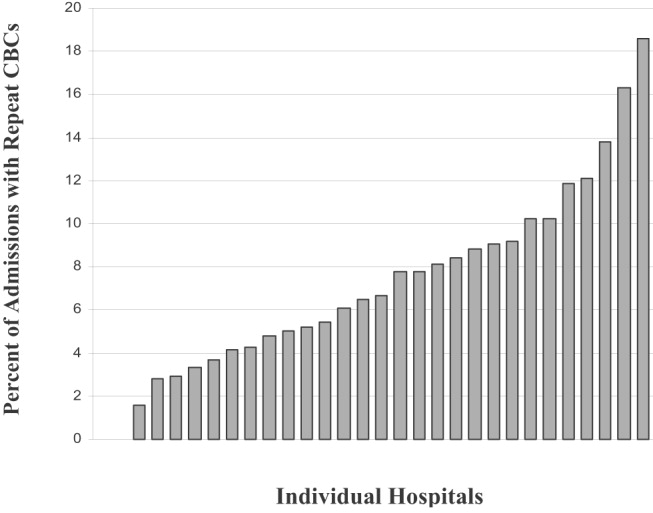
With respect to repeat CBCs, for children at least 3 months old, the strongest predictor was ICU admission (odds ratio [OR] 2.53, 95% CI: 1.69‐3.77), followed by a severe or extreme APR‐DRG severity score (OR 1.75, 95% CI: 1.23‐2.49) and LOS (OR 1.22, 95% CI: 1.15‐1.28). For children less than 3 months old, some of these associations strengthened ICU admission (OR 2.58, 95% CI: 1.84‐3.61), followed by a severe or extreme APR‐DRG severity score (OR 2.31, 95% CI: 1.64‐3.24) and LOS (OR 1.24, 95% CI: 1.16‐1.32). Additional predictors for this age group were a moderate severity score (OR 1.67, 95% CI: 1.29‐2.16) and Medicaid status (OR 1.20, 95% CI: 1.0‐1.43) (Table 2).
| < 3 Months of Age | 311 Months of Age | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted OR* | 95% CI | Adjusted OR* | 95% CI | |||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||
| Mean Age (months) | 1.04 | 0.841.30 | 0.99 | 0.961.03 | ||||||||||||||||||||||||||||||||||||||||
| Male (%) | 1.01 | 0.851.19 | 0.88 | 0.741.05 | ||||||||||||||||||||||||||||||||||||||||
| Medicaid (%) | 1.20 | 1.001.43 | 0.95 | 0.791.15 | ||||||||||||||||||||||||||||||||||||||||
| Admission Season | ||||||||||||||||||||||||||||||||||||||||||||
| OctoberFebruary | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| MarchSeptember (%) | 1.13 | 0.931.37 | 1.11 | 0.811.53 | ||||||||||||||||||||||||||||||||||||||||
| APGDRG severity score | ||||||||||||||||||||||||||||||||||||||||||||
| Mild | Referent | Referent | ||||||||||||||||||||||||||||||||||||||||||
| Moderate | 1.67 | 1.292.16 | 1.28 | 0.941.76 | ||||||||||||||||||||||||||||||||||||||||
| Severe | 2.31 | 1.643.24 | 1.75 | 1.232.49 | ||||||||||||||||||||||||||||||||||||||||
| ICU admission (%) | 2.58 | 1.843.61 | 2.53 | 1.693.77 | ||||||||||||||||||||||||||||||||||||||||
| Length of stay (days) | 1.24 | 1.161.32 | 1.22 | 1.151.28 | ||||||||||||||||||||||||||||||||||||||||
Compared with hospitals that had the lowest proportion of admissions in which CBCs were ordered, hospitals with higher proportions of CBCs ordered had significantly higher mean charges per hospital stay (Table 3).
| Hospital CBC Levels | Patients | Mean Charge (95% CI) | Mean Difference (95% CI) |
|---|---|---|---|
| |||
| Lowest (23%‐40%) | 5838 | $7293 ($70967489) | Referent |
| Middle (41%59%) | 6673 | $8099 ($78598339) | $807* ($491$1122) |
| Highest (60%79%) | 4886 | $8316 ($80548578) | $1024* ($702$1345) |
DISCUSSION
We found that in a nationwide sample of children hospitalized with bronchiolitis, 48% had at least 1 CBC and nearly 8% had a repeat CBC ordered during their hospital stay. Moreover, even after adjusting for covariates, the proportion of children with initial and repeat CBCs during a single admission varied widely and significantly across a nationwide sample of children's hospitals.
We can only speculate on the reasons for institutional variation. Although it is not unusual for some cases of illness to vary from a standard course and so trigger initial or repeat evaluations with a CBC, we do not have any a priori reason to expect the proportion of unusual cases to vary by institution in a national cohort of children's hospitals. One compelling explanation for this variation is differing institutional patterns of practice. For example, it may be that some institutions have protocols that require the ordering of a CBC on admission. This practice could prompt a costly and unnecessary testing cascade14 generated by an initially abnormal CBC and so could trigger additional testing and/or procedures, such as x‐rays and parental antibiotics. Such a cascade of testing and intervention could conceivably lead to additional, and dependent, costs not captured by a simple tally of the costs of individual CBCs. Indeed, in our analysis we found that those hospitals with higher proportion of admissions in which CBCs were ordered also had significantly higher admission charges that exceeded the cost of a CBC. Previous studies support the finding that institutional variation in care for viral respiratory illness is significantly correlated with hospital costs.6
Limitations of this study should be noted. First, the PHIS database does not provide indications for, results of, or hospital location of tests, so we cannot determine whether clinical condition or results prompted initial and/or repeat testing. However, because children with complicated courses or atypical disease presentations likely have longer hospital stays, severe disease, or additional diagnoses, we attempted to control for these factors in our analysis. Second, although we selected cases based on a discharge diagnosis of bronchiolitis, it is possible that admitting physicians obtained an initial CBC to rule out alternative diagnoses, such as bacteremia, which can occur but is rare in this population.12, 13 It is plausible that bacteremia is most likely in children with other comorbidities or higher disease severity. In additional stratified analyses we did find that the proportion of repeat CBCs increased with higher disease severity and that there was an interaction between severe disease status and ICU admission. However, all participating institutions are children's hospitals and so are likely to treat children with a range of severity of illness and comorbidities. Finally, as with other analyses of the PHIS database, we used charges to identify diagnostic tests.5
Given that more than 120,000 U.S. infants are hospitalized annually with bronchiolitis,15 the cost and discomfort associated with unnecessary testing warrants attention. The issue of cost is particularly relevant in light of recent research findings of increased costs for admissions at freestanding children's hospitals.16 We found that mean charges per hospital stay were significantly higher for hospitals that had a higher proportion of admissions during which multiple CBCs were ordered. Although we cannot exclude illness severity and age as explanations for the higher charges, we have no reason to believe that one freestanding children's hospital would have a sicker and younger population than another. An alternative and compelling explanation is that a variation in the standard of care exists across these hospitals.
The institutional variation in and the limited evidence for the utility of the ordering of CBCs in the evaluation of bronchiolitis call into question the necessity of this testing strategy. Exploration of the reasons for this institutional variation will help to create quality initiatives and directed interventions to improve and standardize care in bronchiolitis.
Acknowledgements
Supported by: Robert Wood Johnson (RWJ) Foundation through the Robert Wood Johnson Clinical Scholars Program. The views expressed do not necessarily represent the views of the Robert Wood Johnson Foundation or the University of Washington. The RWJ Foundation provided salary support for Dr. Tarini. The RWJ Foundation did not have a role in the study's design; collection, analysis and interpretation of data; writing of the report; or decision to submit the article for publication. Dr. Tarini wrote the first draft of the manuscript. All authors have seen and agree with the contents of this manuscript.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
- ,,, et al.Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population.Pediatrics. Oct2004;114:e437–e444.
- ,,, et al.Pharmacologic treatment of bronchiolitis in infants and children: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):127–137.
- ,,,.Glucocorticoids for acute viral bronchiolitis in infants and young children.Cochrane Database Syst Rev.2004(3):CD004878.
- ,,.Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old.Cochrane Database Syst Rev.2005;(2):CD004873.
- ,,,,,.Variation in inpatient diagnostic testing and management of bronchiolitis.Pediatrics.2005;115:878–884.
- ,,,,.Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness.Pediatrics.2001;108:851–855.
- .Bronchiolitis. In:Behrman Re KR,Jenson HB, eds.Nelson Textbook of Pediatrics.17th ed.Philadelphia:WB Saunders Co.;2004:1415–1417.
- ,,, et al.Diagnosis and testing in bronchiolitis: a systematic review.Arch Pediatr Adolesc Med.2004;158(2):119–126.
- .Achieving data quality. How data from a pediatric health information system earns the trust of its users.J AHIMA.2004;75(10):22–26.
- ,,,,.A closer look at all‐patient refined DRGs.J AHIMA.2002;73(1):46–50.
- Stata Corp. College Station, TX.
- ,.Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections.Arch Pediatr Adolesc Med.2002;156:322–324.
- ,.Concurrent serious bacterial infections in 912 infants and children hospitalized for treatment of respiratory syncytial virus lower respiratory tract infection.Pediatr Infect Dis J.2004;23:267–269.
- ,.The cascade effect in the clinical care of patients.N Engl J Med.1986;314:512–514.
- ,,,,,.Bronchiolitis‐associated hospitalizations among US children, 1980‐1996.JAMA.1999;282:1440–1446.
- ,,.Lengths of stay and costs associated with children's hospitals.Pediatrics.2005;115:839–844.
Copyright © 2007 Society of Hospital Medicine