User login
Pruritic eruption on the chest
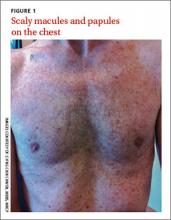
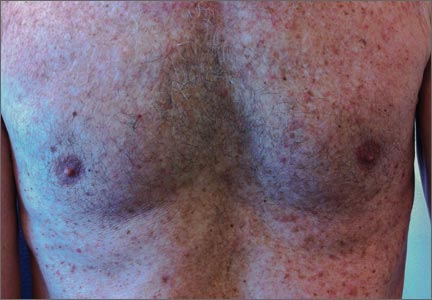
A 61-year-old Caucasian man sought care for a rash that he’d had on and off for the past 5 years. He’d seen several physicians, but none had been able to make a diagnosis. Topical antifungal creams and steroids provided some improvement, but the rash would always come back.
The patient was otherwise healthy and had no personal or family history of atopy or skin disease.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Grover’s disease
A clinical diagnosis of Grover’s disease (transient acantholytic dermatosis) was confirmed by skin biopsy.
First described in 1970,1 Grover’s disease is characterized by a monomorphic papulovesicular eruption that is limited to the trunk and is seen mainly among middle-aged2 Caucasian men.3 Most cases of Grover’s disease are benign and self-limiting, lasting weeks to months, but it can be difficult to manage and has been reported to be recurrent or persistent.4
Some researchers have proposed that Grover’s disease is caused by obstructed sweat glands that lead to pooled sweat urea coming out of the epidermis, resulting in acantholysis.5 However, patients typically present during the winter months when presumably they perspire less frequently.2
There is some evidence linking infection, infestation, ionizing radiation, drugs such as sulfadoxine/pyrimethamine, and recombinant human interleukin-4 with the development of Grover’s disease;3 however, the evidence is weak. Patients with recurrent Grover’s disease often report a history of asteatotic eczema, atopic dermatitis, or contact dermatitis.3
The differential diagnosis includes truncal acne, folliculitis
Because the clinical features of Grover’s disease are often subtle (macules and papules are not florid) and variable (may be red or brown and usually papular but can be acneiform, vesicular, pustular, and even bullous), diagnosis requires a high degree of clinical suspicion. There are many potential differential diagnoses, including:
Truncal acne may present as inflammatory papules. Patient may complain of itchiness. Comedones and pustules are telltale signs of truncal acne, and are not present in Grover’s disease.
Seborrheic dermatitis often presents as greasy, scaly, eczematous patches, and papules. It can be found on the hair-bearing area on the scalp, forehead, eyebrows, nasolabial folds, postauricular skin, and anterior chest wall. Grover’s disease typically presents on the trunk.
Folliculitis may look very similar to Grover’s disease, and its erythematous papules are often found on the trunk. Distinguishing the 2 can be done on biopsy.
Exanthematous drug eruptions, also called maculopapular eruptions, are not limited to the trunk. They are often associated with the use of a new medication within the previous 4 to 21 days.6
Biopsy can confirm the diagnosis
A diagnosis of Grover’s disease is usually made clinically based on the appearance of the rash and the patient’s age and sex (typically seen in middle-aged men). The diagnosis can be confirmed by biopsy. Under a microscope, Grover’s disease has a characteristic appearance of acantholytic dyskeratosis (FIGURE 2); it can be similar in appearance to Darier’s disease, Hailey-Hailey disease, or pemphigus.7
Steroids, other meds are used to reduce itching and inflammation
There are no curative treatments for Grover’s disease. Treatment usually is symptomatic. Local application twice a day of topical steroids, such as triamcinolone acetonide or fluticasone propionate, is often used to relieve the itching and reduce inflammation. Oral steroids, oral retinoids, calcipotriol, phototherapy with ultraviolet B or psoralen plus ultraviolet A light, Grenz radiation, and methotrexate may help clear the eruption in patients with severe itch or extensive or refractory disease.3,8 Antibiotics such as topical fucidin 2 to 3 times a day or oral cloxacillin 500 mg 4 times a day are indicated only if there is secondary impetiginization.
Advise patients to avoid excessive sweating, excessive sun exposure, occlusive clothing, and contact with topical irritants because all of these things are likely to make an outbreak worse.
Our patient was instructed to apply a topical clobetasone butyrate 0.05% cream twice a day. He was also told to take an oral antihistamine, fexofenadine, 180 mg bid for 2 months. The lesions healed, leaving hyperpigmentation. He was advised that the lesions might return in the future.
CORRESPONDENCE
Ch’ng Chin Chwen, MBBS, MRCP, Department of Medicine, Faculty of Medicine, University of Malaya, Lembah Pantai, 50603 Kuala Lumpur, Malaysia; [email protected]
1.Grover RW. Transient acantholytic dermatosis. Arch Dermatol. 1970;101:426-434.
2. Scheinfeld N, Mones J. Seasonal variation of transient acantholytic dyskeratosis (Grover’s disease). J Am Acad Dermatol. 2006;55:263-268.
3. Parsons JM. Transient acantholytic dermatosis: a global perspective. J Am Acad Dermatol. 1996;35(5 pt 1):653-666; quiz 667-670.
4. Streit M, Paredes BE, Braathen LR, et al. Transitory acantholytic dermatosis (Grover disease). An analysis of the clinical spectrum based on 21 histologically assessed cases [in German]. Hautarzt. 2000;51:244-249.
5. Kato N, Furuya K. Two cases of transient acantholytic dermatosis—with the analysis of 20 cases reported in Japan [in Japanese]. Nihon Hifuka Gakkai Zasshi. 1991;101:453-460.
6. Stern RS. Clinical practice. Exanthematous drug eruptions. N Engl J Med. 2012;366:2492-2501.
7. Fernández-Figueras MT, Puig LT, Cannata P, et al. Grover disease: a reappraisal of histopathological diagnostic criteria in 120 cases. Am J Dermatopathol. 2010;32:541-549.
8. Miljkovíc J, Marko PB. Grover’s disease: successful treatment with acitretin and calcipotriol. Wien Klin Wochenschr. 2004;116 suppl 2:81-83.
A 61-year-old Caucasian man sought care for a rash that he’d had on and off for the past 5 years. He’d seen several physicians, but none had been able to make a diagnosis. Topical antifungal creams and steroids provided some improvement, but the rash would always come back.
The patient was otherwise healthy and had no personal or family history of atopy or skin disease.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Grover’s disease
A clinical diagnosis of Grover’s disease (transient acantholytic dermatosis) was confirmed by skin biopsy.
First described in 1970,1 Grover’s disease is characterized by a monomorphic papulovesicular eruption that is limited to the trunk and is seen mainly among middle-aged2 Caucasian men.3 Most cases of Grover’s disease are benign and self-limiting, lasting weeks to months, but it can be difficult to manage and has been reported to be recurrent or persistent.4
Some researchers have proposed that Grover’s disease is caused by obstructed sweat glands that lead to pooled sweat urea coming out of the epidermis, resulting in acantholysis.5 However, patients typically present during the winter months when presumably they perspire less frequently.2
There is some evidence linking infection, infestation, ionizing radiation, drugs such as sulfadoxine/pyrimethamine, and recombinant human interleukin-4 with the development of Grover’s disease;3 however, the evidence is weak. Patients with recurrent Grover’s disease often report a history of asteatotic eczema, atopic dermatitis, or contact dermatitis.3
The differential diagnosis includes truncal acne, folliculitis
Because the clinical features of Grover’s disease are often subtle (macules and papules are not florid) and variable (may be red or brown and usually papular but can be acneiform, vesicular, pustular, and even bullous), diagnosis requires a high degree of clinical suspicion. There are many potential differential diagnoses, including:
Truncal acne may present as inflammatory papules. Patient may complain of itchiness. Comedones and pustules are telltale signs of truncal acne, and are not present in Grover’s disease.
Seborrheic dermatitis often presents as greasy, scaly, eczematous patches, and papules. It can be found on the hair-bearing area on the scalp, forehead, eyebrows, nasolabial folds, postauricular skin, and anterior chest wall. Grover’s disease typically presents on the trunk.
Folliculitis may look very similar to Grover’s disease, and its erythematous papules are often found on the trunk. Distinguishing the 2 can be done on biopsy.
Exanthematous drug eruptions, also called maculopapular eruptions, are not limited to the trunk. They are often associated with the use of a new medication within the previous 4 to 21 days.6
Biopsy can confirm the diagnosis
A diagnosis of Grover’s disease is usually made clinically based on the appearance of the rash and the patient’s age and sex (typically seen in middle-aged men). The diagnosis can be confirmed by biopsy. Under a microscope, Grover’s disease has a characteristic appearance of acantholytic dyskeratosis (FIGURE 2); it can be similar in appearance to Darier’s disease, Hailey-Hailey disease, or pemphigus.7
Steroids, other meds are used to reduce itching and inflammation
There are no curative treatments for Grover’s disease. Treatment usually is symptomatic. Local application twice a day of topical steroids, such as triamcinolone acetonide or fluticasone propionate, is often used to relieve the itching and reduce inflammation. Oral steroids, oral retinoids, calcipotriol, phototherapy with ultraviolet B or psoralen plus ultraviolet A light, Grenz radiation, and methotrexate may help clear the eruption in patients with severe itch or extensive or refractory disease.3,8 Antibiotics such as topical fucidin 2 to 3 times a day or oral cloxacillin 500 mg 4 times a day are indicated only if there is secondary impetiginization.
Advise patients to avoid excessive sweating, excessive sun exposure, occlusive clothing, and contact with topical irritants because all of these things are likely to make an outbreak worse.
Our patient was instructed to apply a topical clobetasone butyrate 0.05% cream twice a day. He was also told to take an oral antihistamine, fexofenadine, 180 mg bid for 2 months. The lesions healed, leaving hyperpigmentation. He was advised that the lesions might return in the future.
CORRESPONDENCE
Ch’ng Chin Chwen, MBBS, MRCP, Department of Medicine, Faculty of Medicine, University of Malaya, Lembah Pantai, 50603 Kuala Lumpur, Malaysia; [email protected]
A 61-year-old Caucasian man sought care for a rash that he’d had on and off for the past 5 years. He’d seen several physicians, but none had been able to make a diagnosis. Topical antifungal creams and steroids provided some improvement, but the rash would always come back.
The patient was otherwise healthy and had no personal or family history of atopy or skin disease.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Grover’s disease
A clinical diagnosis of Grover’s disease (transient acantholytic dermatosis) was confirmed by skin biopsy.
First described in 1970,1 Grover’s disease is characterized by a monomorphic papulovesicular eruption that is limited to the trunk and is seen mainly among middle-aged2 Caucasian men.3 Most cases of Grover’s disease are benign and self-limiting, lasting weeks to months, but it can be difficult to manage and has been reported to be recurrent or persistent.4
Some researchers have proposed that Grover’s disease is caused by obstructed sweat glands that lead to pooled sweat urea coming out of the epidermis, resulting in acantholysis.5 However, patients typically present during the winter months when presumably they perspire less frequently.2
There is some evidence linking infection, infestation, ionizing radiation, drugs such as sulfadoxine/pyrimethamine, and recombinant human interleukin-4 with the development of Grover’s disease;3 however, the evidence is weak. Patients with recurrent Grover’s disease often report a history of asteatotic eczema, atopic dermatitis, or contact dermatitis.3
The differential diagnosis includes truncal acne, folliculitis
Because the clinical features of Grover’s disease are often subtle (macules and papules are not florid) and variable (may be red or brown and usually papular but can be acneiform, vesicular, pustular, and even bullous), diagnosis requires a high degree of clinical suspicion. There are many potential differential diagnoses, including:
Truncal acne may present as inflammatory papules. Patient may complain of itchiness. Comedones and pustules are telltale signs of truncal acne, and are not present in Grover’s disease.
Seborrheic dermatitis often presents as greasy, scaly, eczematous patches, and papules. It can be found on the hair-bearing area on the scalp, forehead, eyebrows, nasolabial folds, postauricular skin, and anterior chest wall. Grover’s disease typically presents on the trunk.
Folliculitis may look very similar to Grover’s disease, and its erythematous papules are often found on the trunk. Distinguishing the 2 can be done on biopsy.
Exanthematous drug eruptions, also called maculopapular eruptions, are not limited to the trunk. They are often associated with the use of a new medication within the previous 4 to 21 days.6
Biopsy can confirm the diagnosis
A diagnosis of Grover’s disease is usually made clinically based on the appearance of the rash and the patient’s age and sex (typically seen in middle-aged men). The diagnosis can be confirmed by biopsy. Under a microscope, Grover’s disease has a characteristic appearance of acantholytic dyskeratosis (FIGURE 2); it can be similar in appearance to Darier’s disease, Hailey-Hailey disease, or pemphigus.7
Steroids, other meds are used to reduce itching and inflammation
There are no curative treatments for Grover’s disease. Treatment usually is symptomatic. Local application twice a day of topical steroids, such as triamcinolone acetonide or fluticasone propionate, is often used to relieve the itching and reduce inflammation. Oral steroids, oral retinoids, calcipotriol, phototherapy with ultraviolet B or psoralen plus ultraviolet A light, Grenz radiation, and methotrexate may help clear the eruption in patients with severe itch or extensive or refractory disease.3,8 Antibiotics such as topical fucidin 2 to 3 times a day or oral cloxacillin 500 mg 4 times a day are indicated only if there is secondary impetiginization.
Advise patients to avoid excessive sweating, excessive sun exposure, occlusive clothing, and contact with topical irritants because all of these things are likely to make an outbreak worse.
Our patient was instructed to apply a topical clobetasone butyrate 0.05% cream twice a day. He was also told to take an oral antihistamine, fexofenadine, 180 mg bid for 2 months. The lesions healed, leaving hyperpigmentation. He was advised that the lesions might return in the future.
CORRESPONDENCE
Ch’ng Chin Chwen, MBBS, MRCP, Department of Medicine, Faculty of Medicine, University of Malaya, Lembah Pantai, 50603 Kuala Lumpur, Malaysia; [email protected]
1.Grover RW. Transient acantholytic dermatosis. Arch Dermatol. 1970;101:426-434.
2. Scheinfeld N, Mones J. Seasonal variation of transient acantholytic dyskeratosis (Grover’s disease). J Am Acad Dermatol. 2006;55:263-268.
3. Parsons JM. Transient acantholytic dermatosis: a global perspective. J Am Acad Dermatol. 1996;35(5 pt 1):653-666; quiz 667-670.
4. Streit M, Paredes BE, Braathen LR, et al. Transitory acantholytic dermatosis (Grover disease). An analysis of the clinical spectrum based on 21 histologically assessed cases [in German]. Hautarzt. 2000;51:244-249.
5. Kato N, Furuya K. Two cases of transient acantholytic dermatosis—with the analysis of 20 cases reported in Japan [in Japanese]. Nihon Hifuka Gakkai Zasshi. 1991;101:453-460.
6. Stern RS. Clinical practice. Exanthematous drug eruptions. N Engl J Med. 2012;366:2492-2501.
7. Fernández-Figueras MT, Puig LT, Cannata P, et al. Grover disease: a reappraisal of histopathological diagnostic criteria in 120 cases. Am J Dermatopathol. 2010;32:541-549.
8. Miljkovíc J, Marko PB. Grover’s disease: successful treatment with acitretin and calcipotriol. Wien Klin Wochenschr. 2004;116 suppl 2:81-83.
1.Grover RW. Transient acantholytic dermatosis. Arch Dermatol. 1970;101:426-434.
2. Scheinfeld N, Mones J. Seasonal variation of transient acantholytic dyskeratosis (Grover’s disease). J Am Acad Dermatol. 2006;55:263-268.
3. Parsons JM. Transient acantholytic dermatosis: a global perspective. J Am Acad Dermatol. 1996;35(5 pt 1):653-666; quiz 667-670.
4. Streit M, Paredes BE, Braathen LR, et al. Transitory acantholytic dermatosis (Grover disease). An analysis of the clinical spectrum based on 21 histologically assessed cases [in German]. Hautarzt. 2000;51:244-249.
5. Kato N, Furuya K. Two cases of transient acantholytic dermatosis—with the analysis of 20 cases reported in Japan [in Japanese]. Nihon Hifuka Gakkai Zasshi. 1991;101:453-460.
6. Stern RS. Clinical practice. Exanthematous drug eruptions. N Engl J Med. 2012;366:2492-2501.
7. Fernández-Figueras MT, Puig LT, Cannata P, et al. Grover disease: a reappraisal of histopathological diagnostic criteria in 120 cases. Am J Dermatopathol. 2010;32:541-549.
8. Miljkovíc J, Marko PB. Grover’s disease: successful treatment with acitretin and calcipotriol. Wien Klin Wochenschr. 2004;116 suppl 2:81-83.