User login
Reorganizing a Hospital Ward
In 2001, the Institute of Medicine called for a major redesign of the US healthcare system, describing the chasm between the quality of care Americans receive and the quality of healthcare they deserve.[1] The healthcare community recognizes its ongoing quality and value gaps, but progress has been limited by outdated care models, fragmented organizational structures, and insufficient advances in system design.[2] Many healthcare organizations are searching for new care delivery models capable of producing greater value.
A major constraint in hospitals is the persistence of underperforming frontline clinical care teams.[3] Physicians typically travel from 1 unit or patient to the next in unpredictable patterns, resulting in missed opportunities to share perspectives and coordinate care with nurses, discharge planning personnel, pharmacists, therapists, and patients. This geographic fragmentation almost certainly contributes to interprofessional silos and hierarchies, nonspecific care plans, and failure to initiate or intensify therapy when indicated.[4] Modern hospital units could benefit from having a standard care model that synchronizes frontline professionals into teams routinely coordinating and progressing a shared plan of care.
EFFECTIVE CLINICAL MICROSYSTEMS REFLECTED IN THE DESIGN OF THE ACCOUNTABLE CARE UNIT
High‐value healthcare organizations deliberately design clinical microsystems.[5] An effective clinical microsystem combines several traits: (1) a small group of people who work together in a defined setting on a regular basis to provide care, (2) linked care processes and a shared information environment that includes individuals who receive that care, (3) performance outcomes, and (4) set service and care aims.[6] For the accountable care unit (ACU) to reflect the traits of an effective clinical microsystem, we designed it with analogous features: (1) unit‐based teams, (2) structured interdisciplinary bedside rounds (SIBR), (3) unit‐level performance reporting, and (4) unit‐level nurse and physician coleadership. We launched the ACU on September 1, 2010 in a high‐acuity 24‐bed medical unit at Emory University Hospital, a 579‐bed tertiary academic medical center. Herein we provide a brief report of our experience implementing and refining the ACU over a 4‐year period to help others gauge feasibility and sustainability.
FEATURES OF AN ACU
Unit‐Based Teams
Design
Geographic alignment fosters mutual respect, cohesiveness, communication, timeliness, and face‐to‐face problem solving,[7, 8] and has been linked to improved patient satisfaction, decreased length of stay, and reductions in morbidity and mortality.[9, 10, 11] At our hospital, though, patients newly admitted or transferred to the hospital medicine service traditionally had been distributed to physician teams without regard to geography, typically based on physician call schedules or traditions of balancing patient volumes across colleagues. These traditional practices geographically dispersed our teams. Physicians would be forced regularly to travel to 5 to 8 different units each day to see 10 to 18 patients. Nurses might perceive this as a parade of different physician teams coming and going off the unit at unpredictable times. To temporally and spatially align physicians with unit‐based staff, specific physician teams were assigned to the ACU.
Implementation
The first step in implementing unit‐based teams was to identify the smallest number of physician teams that could be assigned to the ACU. Two internal medicine resident teams are assigned to care for all medical patients in the unit. Each resident team consists of 1 hospital medicine attending physician, 1 internal medicine resident, 3 interns (2 covering the day shift and 1 overnight every other night), and up to 2 medical students. The 2 teams alternate a 24‐hour call cycle where the on‐call team admits every patient arriving to the unit. For patients arriving to the unit from 6 pm to 7 am, the on‐call overnight intern admits the patients and hands over care to the team in the morning. The on‐call team becomes aware of an incoming patient once the patient has been assigned a bed in the home unit. Several patients per day may arrive on the unit as transfers from a medical or surgical intensive care unit, but most patients arrive as emergency room or direct admissions. On any given day it is acceptable and typical for a team to have several patients off the ACU. No specific changes were made to nurse staffing, with the unit continuing to have 1 nurse unit manager, 1 charge nurse per shift, and a nurse‐to‐patient ratio of 1 to 4.
Results
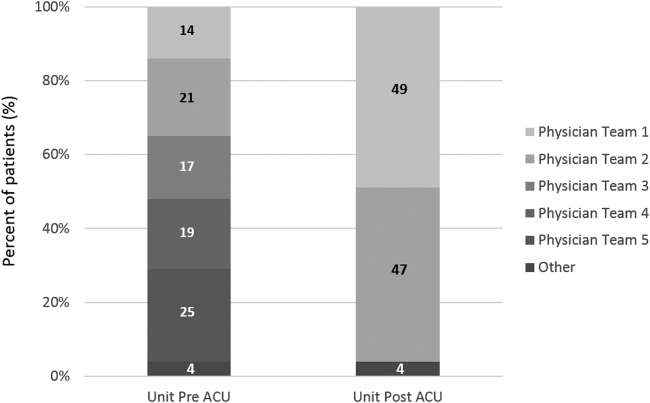
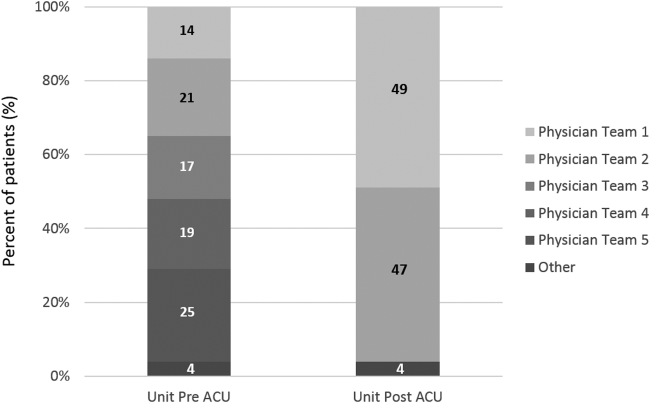
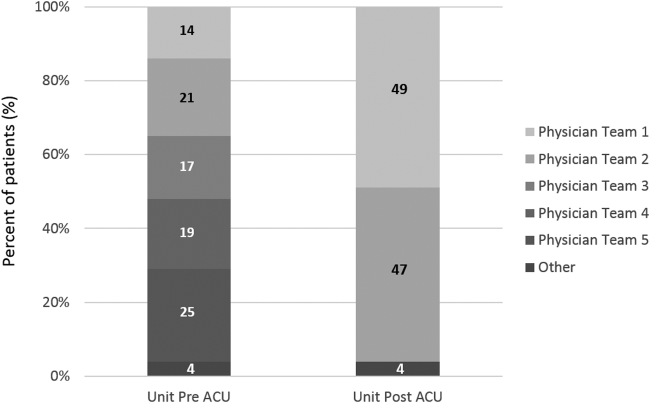
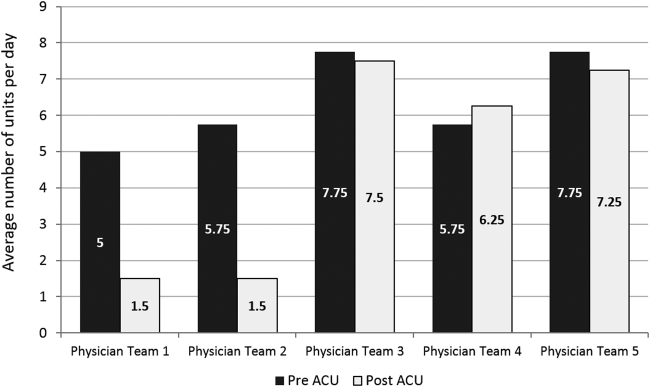
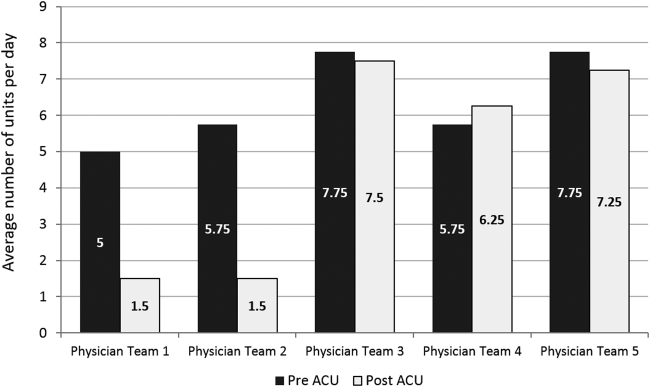
Geographic patient assignment has been successful (Figure 1). Prior to implementing the ACU, more than 5 different hospital medicine physician teams cared for patients on the unit, with no single team caring for more than 25% of them. In the ACU, all medical patients are assigned to 1 of the 2 unit‐based physician teams (physician teams 1 and 2), which regularly represents more than 95% of all patients on the unit. Over the 4 years, these 2 ACU teams have had an average of 12.9 total patient encounters per day (compared to 11.8 in the year before the ACU when these teams were not unit based). The 2 unit‐based teams have over 90% of their patients on the ACU daily. In contrast, 3 attending‐only hospital medicine teams (physician teams 3, 4, and 5) are still dispersed over 6 to 8 units every day (Figure 2), primarily due to high hospital occupancy and a relative scarcity of units eligible to become dedicated hospital medicine units.
Effects of the Change
Through unit‐based teams, the ACU achieves the first trait of an effective clinical microsystem. Although an evaluation of the cultural gains are beyond the scope of this article, the logistical advantages are self‐evident; having the fewest necessary physician teams overseeing care for nearly all patients in 1 unit and where those physician teams simultaneously have nearly all of their patients on that 1 unit, makes it possible to schedule interdisciplinary teamwork activities, such as SIBR, not otherwise feasible.
Structured Interdisciplinary Bedside Rounds
Design
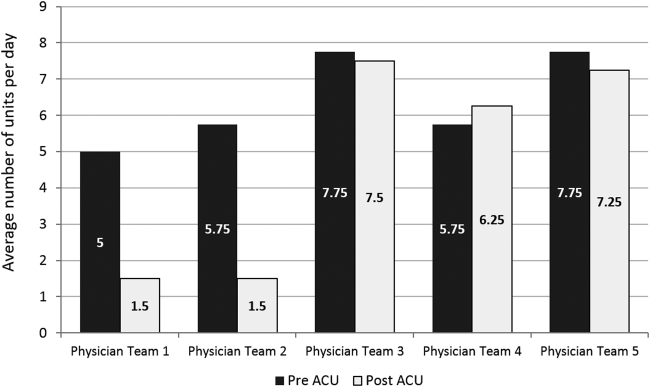
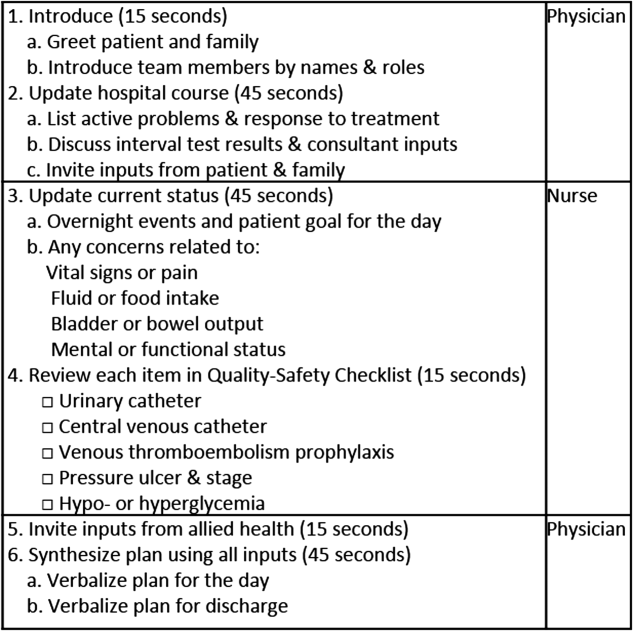
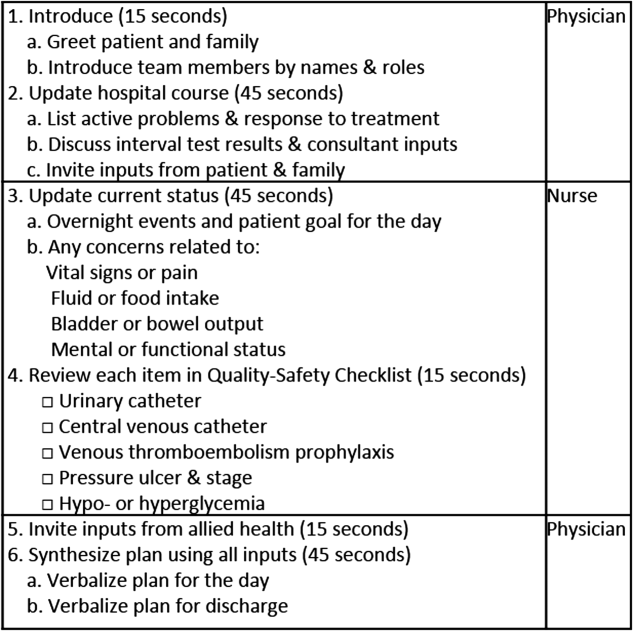
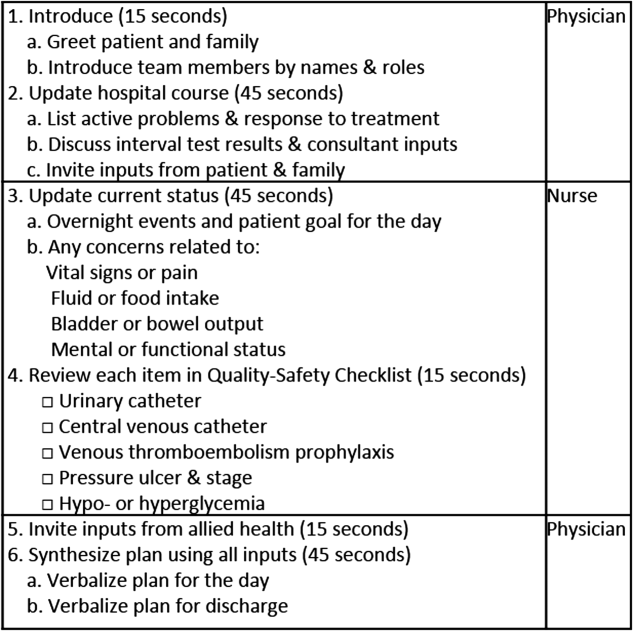
To reflect the second trait of an effective clinical microsystem, a hospital unit should routinely combine best practices for communication, including daily goals sheets,[12] safety checklists,[13] and multidisciplinary rounds.[14, 15] ACU design achieves this through SIBR, a patient‐ and family‐centered, team‐based approach to rounds that brings the nurse, physician, and available allied health professionals to the patient's bedside every day to exchange perspectives using a standard format to cross‐check information with the patient, family, and one another, and articulate a clear plan for the day. Before the SIBR hour starts, physicians and nurses have already performed independent patient assessments through usual activities such as handover, chart review, patient interviews, and physical examinations. Participants in SIBR are expected to give or receive inputs according to the standard SIBR communication protocol (Figure 3), review a quality‐safety checklist together, and ensure the plan of care is verbalized. Including the patient and family allows all parties to hear and be heard, cross‐check information for accuracy, and hold each person accountable for contributions.[16, 17]
Implementation
Each ACU staff member receives orientation to the SIBR communication protocol and is expected to be prepared and punctual for the midmorning start times. The charge nurse serves as the SIBR rounds manager, ensuring physicians waste no time searching for the next nurse and each team's eligible patients are seen in the SIBR hour. For each patient, SIBR begins when the nurse and physician are both present at the bedside. The intern begins SIBR by introducing team members before reviewing the patient's active problem list, response to treatment, and interval test results or consultant inputs. The nurse then relays the patient's goal for the day, overnight events, nursing concerns, and reviews the quality‐safety checklist. The intern then invites allied health professionals to share inputs that might impact medical decision making or discharge planning, before synthesizing all inputs into a shared plan for the day.
Throughout SIBR, the patient and family are encouraged to ask questions or correct misinformation. Although newcomers to SIBR often imagine that inviting patient inputs will disrupt efficiency, we have found teams readily learn to manage this risk, for instance discerning the core question among multiple seemingly disparate ones, or volunteering to return after the SIBR hour to explore a complex issue.
Results
Since the launch of the ACU on September 1, 2010, SIBR has been embedded as a routine on the unit with both physician teams and the nursing staff conducting it every day. Patients not considered eligible for SIBR are those whom the entire physician team has not yet evaluated, typically patients who arrived to the unit overnight. For patients who opt out due to personal preference, or for patients away from the unit for a procedure or a test, SIBR occurs without the patient so the rest of the team can still exchange inputs and formulate a plan of care. A visitor to the unit sees SIBR start punctually at 9 am and 10 am for successive teams, with each completing SIBR on eligible patients in under 60 minutes.
Effects of the Change
The second trait of an effective clinical microsystem is achieved through SIBR's routine forum for staff to share information with each other and the patient. By practicing SIBR every workday, staff are presented with multiple routine opportunities to experience an environment reflective of high‐performing frontline units.[18] We found that SIBR resembled other competencies, with a bell curve of performance. For this reason, by the start of the third year we added a SIBR certification program, a SIBR skills training program where permanent and rotating staff are evaluated through an in vivo observed structured clinical exam, typically with a charge nurse or physician as preceptor. When a nurse, medical student, intern, or resident demonstrates an ability to perform a series of specific high performance SIBR behaviors in 5 of 6 consecutive patients, they can achieve SIBR certification. In the first 2 years of this voluntary certification program, all daytime nursing staff and rotating interns have achieved this demonstration of interdisciplinary teamwork competence.
Unit‐Level Performance Reporting
Design
Hospital outcomes are determined on the clinical frontline. To be effective at managing unit outcomes, performance reports must be made available to unit leadership and staff.[5, 16] However, many hospitals still report performance at the level of the facility or service line. This limits the relevance of reports for the people who directly determine outcomes.
Implementation
For the first year, a data analyst was available to prepare and distribute unit‐level performance reports to unit leaders quarterly, including rates of in‐hospital mortality, blood stream infections, patient satisfaction, length of stay, and 30‐day readmissions. Preparation of these reports was labor intensive, requiring the analyst to acquire raw data from multiple data sources and to build the reports manually.
Results
In an analysis comparing outcomes for every patient spending at least 1 night on the unit in the year before and year after implementation, we observed reductions in in‐hospital mortality and length of stay. Unadjusted in‐hospital mortality decreased from 2.3% to 1.1% (P=0.004), with no change in referrals to hospice (5.4% to 4.5%) (P=0.176), and length‐of‐stay decreased from 5.0 to 4.5 days (P=0.001).[19] A complete report of these findings, including an analysis of concurrent control groups is beyond the scope of this article, but here we highlight an effect we observed on ACU leadership and staff from the reduction in in‐hospital mortality.
Effects of the Change
Noting the apparent mortality reduction, ACU leadership encouraged permanent staff and rotating trainees to consider an unexpected death as a never event. Although perhaps self‐evident, before the ACU we had never been organized to reflect on that concept or to use routines to do something about it. The unit considered an unexpected death one where the patient was not actively receiving comfort measures. At the monthly meet and greet, where ACU leadership bring the permanent staff and new rotating trainees together to introduce themselves by first name, the coleaders proposed that unexpected deaths in the month ahead could represent failures to recognize or respond to deterioration, to consider an alternative or under‐treated process, to transfer the patient to a higher level of care, or to deliver more timely and appropriate end‐of‐life care. It is our impression that this introspection was extraordinarily meaningful and would not have occurred without unit‐based teams, unit‐level performance data, and ACU leadership learning to utilize this rhetoric.
Unit‐Level Nurse and Physician Coleadership
Design
Effective leadership is a major driver of successful clinical microsystems.[20] The ACU is designed to be co‐led by a nurse unit manager and physician medical director. The leadership pair was charged simply with developing patient‐centered teams and ensuring the staff felt connected to the values of the organization and accountable to each other and the outcomes of the unit.
Implementation
Nursing leadership and hospital executives influenced the selection of the physician medical director, which was a way for them to demonstrate support for the care model. Over the first 4 years, the physician medical director position has been afforded a 10% to 20% reduction in clinical duties to fulfill the charge. The leadership pair sets expectations for the ACU's code of conduct, standard operating procedures (eg, SIBR), and best‐practice protocols.
Results
The leadership pair tries explicitly to role model the behaviors enumerated in the ACU's relational covenant, itself the product of a facilitated exercise they commissioned in the first year in which the entire staff drafted and signed a document listing behaviors they wished to see from each other (see Supporting Information, Appendix 1, in the online version of this article). The physician medical director, along with charge nurses, coach staff and trainees wishing to achieve SIBR certification. Over the 4 years, the pair has introduced best‐practice protocols for glycemic control, venous thromboembolism prophylaxis, removal of idle venous and bladder catheters, and bedside goals‐of‐care conversations.
Effects of the Change
Where there had previously been no explicit code of conduct, standard operating procedures such as SIBR, or focused efforts to optimize unit outcomes, the coleadership pair fills a management gap. These coleaders play an essential role in building momentum for the structure and processes of the ACU. The leadership pair has also become a primary resource for intraorganizational spread of the ACU model to medical and surgical wards, as well as geriatric, long‐term acute, and intensive care units.
CHALLENGES
Challenges with implementing the ACU fell into 3 primary categories: (1) performing change management required for a successful launch, (2) solving logistics of maintaining unit‐based physician teams, and (3) training physicians and nurses to perform SIBR at a high level.
For change management, the leadership pair was able to explain the rationale of the model to all staff in sufficient detail to launch the ACU. To build momentum for ACU routines and relationships, the physician leader and the nurse unit manager were both present on the unit daily for the first 100 days. As ACU operations became routine and competencies formed among clinicians, the amount of time spent by these leaders was de‐escalated.
Creating and maintaining unit‐based physician teams required shared understanding and coordination between on‐call hospital medicine physicians and the bed control office so that new admissions or transfers could be consistently assigned to unit‐based teams without adversely affecting patient flow. We found this challenge to be manageable once stakeholders accepted the rationale for the care mode and figured out how to support it.
The challenge of building high‐performance SIBR across the unit, including competence of rotating trainees new to the model, requires individualized assessment and feedback necessary for SIBR certification. We addressed this challenge by creating a SIBR train‐the‐trainer programa list of observable high‐performance SIBR behaviors coupled with a short course about giving effective feedback to learnersand found that once the ACU had several nurse and physician SIBR trainers in the staffing mix every day, the required amount of SIBR coaching expertise was available when needed.
CONCLUSION
Improving value and reliability in hospital care may require new models of care. The ACU is a hospital care model specifically designed to organize physicians, nurses, and allied health professionals into high‐functioning, unit‐based teams. It converges standard workflow, patient‐centered communication, quality‐safety checklists, best‐practice protocols, performance measurement, and progressive leadership. Our experience with the ACU suggests that hospital units can be reorganized as effective clinical microsystems where consistent unit professionals can share time and space, a sense of purpose, code of conduct, shared mental model for teamwork, an interprofessional management structure, and an important level of accountability to each other and their patients.
Disclosures: Jason Stein, MD: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees and royalties for licensed intellectual property to support implementation of the care model described; founder and president of nonprofit Centripital, provider of consulting services to hospital systems implementing the care model described. The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict of interest policies. Liam Chadwick, PhD, and Diaz Clark, MS, RN: recipients of consulting fees through Centripital to support implementation of the care model described. Bryan W. Castle, MBA, RN: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees through Centripital to support implementation of the care model described. The authors report no other conflicts of interest.
- Institute of Medicine. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- , , . The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- . The end of the beginning: patient safety five years after “to err is human”. Health Aff (Millwood). 2004;Suppl Web Exclusives:W4‐534–545.
- , , , et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834.
- . The four habits of high‐value health care organizations. N Engl J Med. 2011;365(22):2045–2047.
- , , , . Using a Malcolm Baldrige framework to understand high‐performing clinical microsystems. Qual Saf Health Care. 2007;16(5):334–341.
- , , , . Relational coordination among nurses and other providers: impact on the quality of patient care. J Nurs Manag. 2010;18(8):926–937.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Reducing cardiac arrests in the acute admissions unit: a quality improvement journey. BMJ Qual Saf. 2013;22(12):1025–1031.
- , , , et al. Evolving practice of hospital medicine and its impact on hospital throughput and efficiencies. J Hosp Med. 2012;7(8):649–654.
- , . Improvement projects led by unit‐based teams of nurse, physician, and quality leaders reduce infections, lower costs, improve patient satisfaction, and nurse‐physician communication. AHRQ Health Care Innovations Exchange. Available at: https://innovations.ahrq.gov/profiles/improvement‐projects‐led‐unit‐based‐teams‐nurse‐physician‐and‐quality‐leaders‐reduce. Accessed May 4, 2014.
- , , , , . The daily goals communication sheet: a simple and novel tool for improved communication and care. Jt Comm J Qual Patient Saf. 2008;34(10):608–613, 561.
- , , , et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence‐based intensive care unit practices. Crit Care Med. 2009;37(10):2775–2781.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88–93.
- , , . Integrating patient safety into the clinical microsystem. Qual Saf Health Care. 2004;13(suppl 2):ii34–ii38.
- , , , . Collaborative‐cross checking to enhance resilience. Cogn Tech Work. 2007;9:155–162.
- , , , et al. Microsystems in health care: Part 1. Learning from high‐performing front‐line clinical units. Jt Comm J Qual Improv. 2002;28(9):472–493.
- , , . Mortality reduction associated with structure process, and management redesign of a hospital medicine unit. J Hosp Med. 2012;7(suppl 2):115.
- , , , et al. Microsystems in health care: part 5. How leaders are leading. Jt Comm J Qual Saf. 2003;29(6):297–308.
In 2001, the Institute of Medicine called for a major redesign of the US healthcare system, describing the chasm between the quality of care Americans receive and the quality of healthcare they deserve.[1] The healthcare community recognizes its ongoing quality and value gaps, but progress has been limited by outdated care models, fragmented organizational structures, and insufficient advances in system design.[2] Many healthcare organizations are searching for new care delivery models capable of producing greater value.
A major constraint in hospitals is the persistence of underperforming frontline clinical care teams.[3] Physicians typically travel from 1 unit or patient to the next in unpredictable patterns, resulting in missed opportunities to share perspectives and coordinate care with nurses, discharge planning personnel, pharmacists, therapists, and patients. This geographic fragmentation almost certainly contributes to interprofessional silos and hierarchies, nonspecific care plans, and failure to initiate or intensify therapy when indicated.[4] Modern hospital units could benefit from having a standard care model that synchronizes frontline professionals into teams routinely coordinating and progressing a shared plan of care.
EFFECTIVE CLINICAL MICROSYSTEMS REFLECTED IN THE DESIGN OF THE ACCOUNTABLE CARE UNIT
High‐value healthcare organizations deliberately design clinical microsystems.[5] An effective clinical microsystem combines several traits: (1) a small group of people who work together in a defined setting on a regular basis to provide care, (2) linked care processes and a shared information environment that includes individuals who receive that care, (3) performance outcomes, and (4) set service and care aims.[6] For the accountable care unit (ACU) to reflect the traits of an effective clinical microsystem, we designed it with analogous features: (1) unit‐based teams, (2) structured interdisciplinary bedside rounds (SIBR), (3) unit‐level performance reporting, and (4) unit‐level nurse and physician coleadership. We launched the ACU on September 1, 2010 in a high‐acuity 24‐bed medical unit at Emory University Hospital, a 579‐bed tertiary academic medical center. Herein we provide a brief report of our experience implementing and refining the ACU over a 4‐year period to help others gauge feasibility and sustainability.
FEATURES OF AN ACU
Unit‐Based Teams
Design
Geographic alignment fosters mutual respect, cohesiveness, communication, timeliness, and face‐to‐face problem solving,[7, 8] and has been linked to improved patient satisfaction, decreased length of stay, and reductions in morbidity and mortality.[9, 10, 11] At our hospital, though, patients newly admitted or transferred to the hospital medicine service traditionally had been distributed to physician teams without regard to geography, typically based on physician call schedules or traditions of balancing patient volumes across colleagues. These traditional practices geographically dispersed our teams. Physicians would be forced regularly to travel to 5 to 8 different units each day to see 10 to 18 patients. Nurses might perceive this as a parade of different physician teams coming and going off the unit at unpredictable times. To temporally and spatially align physicians with unit‐based staff, specific physician teams were assigned to the ACU.
Implementation
The first step in implementing unit‐based teams was to identify the smallest number of physician teams that could be assigned to the ACU. Two internal medicine resident teams are assigned to care for all medical patients in the unit. Each resident team consists of 1 hospital medicine attending physician, 1 internal medicine resident, 3 interns (2 covering the day shift and 1 overnight every other night), and up to 2 medical students. The 2 teams alternate a 24‐hour call cycle where the on‐call team admits every patient arriving to the unit. For patients arriving to the unit from 6 pm to 7 am, the on‐call overnight intern admits the patients and hands over care to the team in the morning. The on‐call team becomes aware of an incoming patient once the patient has been assigned a bed in the home unit. Several patients per day may arrive on the unit as transfers from a medical or surgical intensive care unit, but most patients arrive as emergency room or direct admissions. On any given day it is acceptable and typical for a team to have several patients off the ACU. No specific changes were made to nurse staffing, with the unit continuing to have 1 nurse unit manager, 1 charge nurse per shift, and a nurse‐to‐patient ratio of 1 to 4.
Results
Geographic patient assignment has been successful (Figure 1). Prior to implementing the ACU, more than 5 different hospital medicine physician teams cared for patients on the unit, with no single team caring for more than 25% of them. In the ACU, all medical patients are assigned to 1 of the 2 unit‐based physician teams (physician teams 1 and 2), which regularly represents more than 95% of all patients on the unit. Over the 4 years, these 2 ACU teams have had an average of 12.9 total patient encounters per day (compared to 11.8 in the year before the ACU when these teams were not unit based). The 2 unit‐based teams have over 90% of their patients on the ACU daily. In contrast, 3 attending‐only hospital medicine teams (physician teams 3, 4, and 5) are still dispersed over 6 to 8 units every day (Figure 2), primarily due to high hospital occupancy and a relative scarcity of units eligible to become dedicated hospital medicine units.
Effects of the Change
Through unit‐based teams, the ACU achieves the first trait of an effective clinical microsystem. Although an evaluation of the cultural gains are beyond the scope of this article, the logistical advantages are self‐evident; having the fewest necessary physician teams overseeing care for nearly all patients in 1 unit and where those physician teams simultaneously have nearly all of their patients on that 1 unit, makes it possible to schedule interdisciplinary teamwork activities, such as SIBR, not otherwise feasible.
Structured Interdisciplinary Bedside Rounds
Design
To reflect the second trait of an effective clinical microsystem, a hospital unit should routinely combine best practices for communication, including daily goals sheets,[12] safety checklists,[13] and multidisciplinary rounds.[14, 15] ACU design achieves this through SIBR, a patient‐ and family‐centered, team‐based approach to rounds that brings the nurse, physician, and available allied health professionals to the patient's bedside every day to exchange perspectives using a standard format to cross‐check information with the patient, family, and one another, and articulate a clear plan for the day. Before the SIBR hour starts, physicians and nurses have already performed independent patient assessments through usual activities such as handover, chart review, patient interviews, and physical examinations. Participants in SIBR are expected to give or receive inputs according to the standard SIBR communication protocol (Figure 3), review a quality‐safety checklist together, and ensure the plan of care is verbalized. Including the patient and family allows all parties to hear and be heard, cross‐check information for accuracy, and hold each person accountable for contributions.[16, 17]
Implementation
Each ACU staff member receives orientation to the SIBR communication protocol and is expected to be prepared and punctual for the midmorning start times. The charge nurse serves as the SIBR rounds manager, ensuring physicians waste no time searching for the next nurse and each team's eligible patients are seen in the SIBR hour. For each patient, SIBR begins when the nurse and physician are both present at the bedside. The intern begins SIBR by introducing team members before reviewing the patient's active problem list, response to treatment, and interval test results or consultant inputs. The nurse then relays the patient's goal for the day, overnight events, nursing concerns, and reviews the quality‐safety checklist. The intern then invites allied health professionals to share inputs that might impact medical decision making or discharge planning, before synthesizing all inputs into a shared plan for the day.
Throughout SIBR, the patient and family are encouraged to ask questions or correct misinformation. Although newcomers to SIBR often imagine that inviting patient inputs will disrupt efficiency, we have found teams readily learn to manage this risk, for instance discerning the core question among multiple seemingly disparate ones, or volunteering to return after the SIBR hour to explore a complex issue.
Results
Since the launch of the ACU on September 1, 2010, SIBR has been embedded as a routine on the unit with both physician teams and the nursing staff conducting it every day. Patients not considered eligible for SIBR are those whom the entire physician team has not yet evaluated, typically patients who arrived to the unit overnight. For patients who opt out due to personal preference, or for patients away from the unit for a procedure or a test, SIBR occurs without the patient so the rest of the team can still exchange inputs and formulate a plan of care. A visitor to the unit sees SIBR start punctually at 9 am and 10 am for successive teams, with each completing SIBR on eligible patients in under 60 minutes.
Effects of the Change
The second trait of an effective clinical microsystem is achieved through SIBR's routine forum for staff to share information with each other and the patient. By practicing SIBR every workday, staff are presented with multiple routine opportunities to experience an environment reflective of high‐performing frontline units.[18] We found that SIBR resembled other competencies, with a bell curve of performance. For this reason, by the start of the third year we added a SIBR certification program, a SIBR skills training program where permanent and rotating staff are evaluated through an in vivo observed structured clinical exam, typically with a charge nurse or physician as preceptor. When a nurse, medical student, intern, or resident demonstrates an ability to perform a series of specific high performance SIBR behaviors in 5 of 6 consecutive patients, they can achieve SIBR certification. In the first 2 years of this voluntary certification program, all daytime nursing staff and rotating interns have achieved this demonstration of interdisciplinary teamwork competence.
Unit‐Level Performance Reporting
Design
Hospital outcomes are determined on the clinical frontline. To be effective at managing unit outcomes, performance reports must be made available to unit leadership and staff.[5, 16] However, many hospitals still report performance at the level of the facility or service line. This limits the relevance of reports for the people who directly determine outcomes.
Implementation
For the first year, a data analyst was available to prepare and distribute unit‐level performance reports to unit leaders quarterly, including rates of in‐hospital mortality, blood stream infections, patient satisfaction, length of stay, and 30‐day readmissions. Preparation of these reports was labor intensive, requiring the analyst to acquire raw data from multiple data sources and to build the reports manually.
Results
In an analysis comparing outcomes for every patient spending at least 1 night on the unit in the year before and year after implementation, we observed reductions in in‐hospital mortality and length of stay. Unadjusted in‐hospital mortality decreased from 2.3% to 1.1% (P=0.004), with no change in referrals to hospice (5.4% to 4.5%) (P=0.176), and length‐of‐stay decreased from 5.0 to 4.5 days (P=0.001).[19] A complete report of these findings, including an analysis of concurrent control groups is beyond the scope of this article, but here we highlight an effect we observed on ACU leadership and staff from the reduction in in‐hospital mortality.
Effects of the Change
Noting the apparent mortality reduction, ACU leadership encouraged permanent staff and rotating trainees to consider an unexpected death as a never event. Although perhaps self‐evident, before the ACU we had never been organized to reflect on that concept or to use routines to do something about it. The unit considered an unexpected death one where the patient was not actively receiving comfort measures. At the monthly meet and greet, where ACU leadership bring the permanent staff and new rotating trainees together to introduce themselves by first name, the coleaders proposed that unexpected deaths in the month ahead could represent failures to recognize or respond to deterioration, to consider an alternative or under‐treated process, to transfer the patient to a higher level of care, or to deliver more timely and appropriate end‐of‐life care. It is our impression that this introspection was extraordinarily meaningful and would not have occurred without unit‐based teams, unit‐level performance data, and ACU leadership learning to utilize this rhetoric.
Unit‐Level Nurse and Physician Coleadership
Design
Effective leadership is a major driver of successful clinical microsystems.[20] The ACU is designed to be co‐led by a nurse unit manager and physician medical director. The leadership pair was charged simply with developing patient‐centered teams and ensuring the staff felt connected to the values of the organization and accountable to each other and the outcomes of the unit.
Implementation
Nursing leadership and hospital executives influenced the selection of the physician medical director, which was a way for them to demonstrate support for the care model. Over the first 4 years, the physician medical director position has been afforded a 10% to 20% reduction in clinical duties to fulfill the charge. The leadership pair sets expectations for the ACU's code of conduct, standard operating procedures (eg, SIBR), and best‐practice protocols.
Results
The leadership pair tries explicitly to role model the behaviors enumerated in the ACU's relational covenant, itself the product of a facilitated exercise they commissioned in the first year in which the entire staff drafted and signed a document listing behaviors they wished to see from each other (see Supporting Information, Appendix 1, in the online version of this article). The physician medical director, along with charge nurses, coach staff and trainees wishing to achieve SIBR certification. Over the 4 years, the pair has introduced best‐practice protocols for glycemic control, venous thromboembolism prophylaxis, removal of idle venous and bladder catheters, and bedside goals‐of‐care conversations.
Effects of the Change
Where there had previously been no explicit code of conduct, standard operating procedures such as SIBR, or focused efforts to optimize unit outcomes, the coleadership pair fills a management gap. These coleaders play an essential role in building momentum for the structure and processes of the ACU. The leadership pair has also become a primary resource for intraorganizational spread of the ACU model to medical and surgical wards, as well as geriatric, long‐term acute, and intensive care units.
CHALLENGES
Challenges with implementing the ACU fell into 3 primary categories: (1) performing change management required for a successful launch, (2) solving logistics of maintaining unit‐based physician teams, and (3) training physicians and nurses to perform SIBR at a high level.
For change management, the leadership pair was able to explain the rationale of the model to all staff in sufficient detail to launch the ACU. To build momentum for ACU routines and relationships, the physician leader and the nurse unit manager were both present on the unit daily for the first 100 days. As ACU operations became routine and competencies formed among clinicians, the amount of time spent by these leaders was de‐escalated.
Creating and maintaining unit‐based physician teams required shared understanding and coordination between on‐call hospital medicine physicians and the bed control office so that new admissions or transfers could be consistently assigned to unit‐based teams without adversely affecting patient flow. We found this challenge to be manageable once stakeholders accepted the rationale for the care mode and figured out how to support it.
The challenge of building high‐performance SIBR across the unit, including competence of rotating trainees new to the model, requires individualized assessment and feedback necessary for SIBR certification. We addressed this challenge by creating a SIBR train‐the‐trainer programa list of observable high‐performance SIBR behaviors coupled with a short course about giving effective feedback to learnersand found that once the ACU had several nurse and physician SIBR trainers in the staffing mix every day, the required amount of SIBR coaching expertise was available when needed.
CONCLUSION
Improving value and reliability in hospital care may require new models of care. The ACU is a hospital care model specifically designed to organize physicians, nurses, and allied health professionals into high‐functioning, unit‐based teams. It converges standard workflow, patient‐centered communication, quality‐safety checklists, best‐practice protocols, performance measurement, and progressive leadership. Our experience with the ACU suggests that hospital units can be reorganized as effective clinical microsystems where consistent unit professionals can share time and space, a sense of purpose, code of conduct, shared mental model for teamwork, an interprofessional management structure, and an important level of accountability to each other and their patients.
Disclosures: Jason Stein, MD: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees and royalties for licensed intellectual property to support implementation of the care model described; founder and president of nonprofit Centripital, provider of consulting services to hospital systems implementing the care model described. The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict of interest policies. Liam Chadwick, PhD, and Diaz Clark, MS, RN: recipients of consulting fees through Centripital to support implementation of the care model described. Bryan W. Castle, MBA, RN: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees through Centripital to support implementation of the care model described. The authors report no other conflicts of interest.
In 2001, the Institute of Medicine called for a major redesign of the US healthcare system, describing the chasm between the quality of care Americans receive and the quality of healthcare they deserve.[1] The healthcare community recognizes its ongoing quality and value gaps, but progress has been limited by outdated care models, fragmented organizational structures, and insufficient advances in system design.[2] Many healthcare organizations are searching for new care delivery models capable of producing greater value.
A major constraint in hospitals is the persistence of underperforming frontline clinical care teams.[3] Physicians typically travel from 1 unit or patient to the next in unpredictable patterns, resulting in missed opportunities to share perspectives and coordinate care with nurses, discharge planning personnel, pharmacists, therapists, and patients. This geographic fragmentation almost certainly contributes to interprofessional silos and hierarchies, nonspecific care plans, and failure to initiate or intensify therapy when indicated.[4] Modern hospital units could benefit from having a standard care model that synchronizes frontline professionals into teams routinely coordinating and progressing a shared plan of care.
EFFECTIVE CLINICAL MICROSYSTEMS REFLECTED IN THE DESIGN OF THE ACCOUNTABLE CARE UNIT
High‐value healthcare organizations deliberately design clinical microsystems.[5] An effective clinical microsystem combines several traits: (1) a small group of people who work together in a defined setting on a regular basis to provide care, (2) linked care processes and a shared information environment that includes individuals who receive that care, (3) performance outcomes, and (4) set service and care aims.[6] For the accountable care unit (ACU) to reflect the traits of an effective clinical microsystem, we designed it with analogous features: (1) unit‐based teams, (2) structured interdisciplinary bedside rounds (SIBR), (3) unit‐level performance reporting, and (4) unit‐level nurse and physician coleadership. We launched the ACU on September 1, 2010 in a high‐acuity 24‐bed medical unit at Emory University Hospital, a 579‐bed tertiary academic medical center. Herein we provide a brief report of our experience implementing and refining the ACU over a 4‐year period to help others gauge feasibility and sustainability.
FEATURES OF AN ACU
Unit‐Based Teams
Design
Geographic alignment fosters mutual respect, cohesiveness, communication, timeliness, and face‐to‐face problem solving,[7, 8] and has been linked to improved patient satisfaction, decreased length of stay, and reductions in morbidity and mortality.[9, 10, 11] At our hospital, though, patients newly admitted or transferred to the hospital medicine service traditionally had been distributed to physician teams without regard to geography, typically based on physician call schedules or traditions of balancing patient volumes across colleagues. These traditional practices geographically dispersed our teams. Physicians would be forced regularly to travel to 5 to 8 different units each day to see 10 to 18 patients. Nurses might perceive this as a parade of different physician teams coming and going off the unit at unpredictable times. To temporally and spatially align physicians with unit‐based staff, specific physician teams were assigned to the ACU.
Implementation
The first step in implementing unit‐based teams was to identify the smallest number of physician teams that could be assigned to the ACU. Two internal medicine resident teams are assigned to care for all medical patients in the unit. Each resident team consists of 1 hospital medicine attending physician, 1 internal medicine resident, 3 interns (2 covering the day shift and 1 overnight every other night), and up to 2 medical students. The 2 teams alternate a 24‐hour call cycle where the on‐call team admits every patient arriving to the unit. For patients arriving to the unit from 6 pm to 7 am, the on‐call overnight intern admits the patients and hands over care to the team in the morning. The on‐call team becomes aware of an incoming patient once the patient has been assigned a bed in the home unit. Several patients per day may arrive on the unit as transfers from a medical or surgical intensive care unit, but most patients arrive as emergency room or direct admissions. On any given day it is acceptable and typical for a team to have several patients off the ACU. No specific changes were made to nurse staffing, with the unit continuing to have 1 nurse unit manager, 1 charge nurse per shift, and a nurse‐to‐patient ratio of 1 to 4.
Results
Geographic patient assignment has been successful (Figure 1). Prior to implementing the ACU, more than 5 different hospital medicine physician teams cared for patients on the unit, with no single team caring for more than 25% of them. In the ACU, all medical patients are assigned to 1 of the 2 unit‐based physician teams (physician teams 1 and 2), which regularly represents more than 95% of all patients on the unit. Over the 4 years, these 2 ACU teams have had an average of 12.9 total patient encounters per day (compared to 11.8 in the year before the ACU when these teams were not unit based). The 2 unit‐based teams have over 90% of their patients on the ACU daily. In contrast, 3 attending‐only hospital medicine teams (physician teams 3, 4, and 5) are still dispersed over 6 to 8 units every day (Figure 2), primarily due to high hospital occupancy and a relative scarcity of units eligible to become dedicated hospital medicine units.
Effects of the Change
Through unit‐based teams, the ACU achieves the first trait of an effective clinical microsystem. Although an evaluation of the cultural gains are beyond the scope of this article, the logistical advantages are self‐evident; having the fewest necessary physician teams overseeing care for nearly all patients in 1 unit and where those physician teams simultaneously have nearly all of their patients on that 1 unit, makes it possible to schedule interdisciplinary teamwork activities, such as SIBR, not otherwise feasible.
Structured Interdisciplinary Bedside Rounds
Design
To reflect the second trait of an effective clinical microsystem, a hospital unit should routinely combine best practices for communication, including daily goals sheets,[12] safety checklists,[13] and multidisciplinary rounds.[14, 15] ACU design achieves this through SIBR, a patient‐ and family‐centered, team‐based approach to rounds that brings the nurse, physician, and available allied health professionals to the patient's bedside every day to exchange perspectives using a standard format to cross‐check information with the patient, family, and one another, and articulate a clear plan for the day. Before the SIBR hour starts, physicians and nurses have already performed independent patient assessments through usual activities such as handover, chart review, patient interviews, and physical examinations. Participants in SIBR are expected to give or receive inputs according to the standard SIBR communication protocol (Figure 3), review a quality‐safety checklist together, and ensure the plan of care is verbalized. Including the patient and family allows all parties to hear and be heard, cross‐check information for accuracy, and hold each person accountable for contributions.[16, 17]
Implementation
Each ACU staff member receives orientation to the SIBR communication protocol and is expected to be prepared and punctual for the midmorning start times. The charge nurse serves as the SIBR rounds manager, ensuring physicians waste no time searching for the next nurse and each team's eligible patients are seen in the SIBR hour. For each patient, SIBR begins when the nurse and physician are both present at the bedside. The intern begins SIBR by introducing team members before reviewing the patient's active problem list, response to treatment, and interval test results or consultant inputs. The nurse then relays the patient's goal for the day, overnight events, nursing concerns, and reviews the quality‐safety checklist. The intern then invites allied health professionals to share inputs that might impact medical decision making or discharge planning, before synthesizing all inputs into a shared plan for the day.
Throughout SIBR, the patient and family are encouraged to ask questions or correct misinformation. Although newcomers to SIBR often imagine that inviting patient inputs will disrupt efficiency, we have found teams readily learn to manage this risk, for instance discerning the core question among multiple seemingly disparate ones, or volunteering to return after the SIBR hour to explore a complex issue.
Results
Since the launch of the ACU on September 1, 2010, SIBR has been embedded as a routine on the unit with both physician teams and the nursing staff conducting it every day. Patients not considered eligible for SIBR are those whom the entire physician team has not yet evaluated, typically patients who arrived to the unit overnight. For patients who opt out due to personal preference, or for patients away from the unit for a procedure or a test, SIBR occurs without the patient so the rest of the team can still exchange inputs and formulate a plan of care. A visitor to the unit sees SIBR start punctually at 9 am and 10 am for successive teams, with each completing SIBR on eligible patients in under 60 minutes.
Effects of the Change
The second trait of an effective clinical microsystem is achieved through SIBR's routine forum for staff to share information with each other and the patient. By practicing SIBR every workday, staff are presented with multiple routine opportunities to experience an environment reflective of high‐performing frontline units.[18] We found that SIBR resembled other competencies, with a bell curve of performance. For this reason, by the start of the third year we added a SIBR certification program, a SIBR skills training program where permanent and rotating staff are evaluated through an in vivo observed structured clinical exam, typically with a charge nurse or physician as preceptor. When a nurse, medical student, intern, or resident demonstrates an ability to perform a series of specific high performance SIBR behaviors in 5 of 6 consecutive patients, they can achieve SIBR certification. In the first 2 years of this voluntary certification program, all daytime nursing staff and rotating interns have achieved this demonstration of interdisciplinary teamwork competence.
Unit‐Level Performance Reporting
Design
Hospital outcomes are determined on the clinical frontline. To be effective at managing unit outcomes, performance reports must be made available to unit leadership and staff.[5, 16] However, many hospitals still report performance at the level of the facility or service line. This limits the relevance of reports for the people who directly determine outcomes.
Implementation
For the first year, a data analyst was available to prepare and distribute unit‐level performance reports to unit leaders quarterly, including rates of in‐hospital mortality, blood stream infections, patient satisfaction, length of stay, and 30‐day readmissions. Preparation of these reports was labor intensive, requiring the analyst to acquire raw data from multiple data sources and to build the reports manually.
Results
In an analysis comparing outcomes for every patient spending at least 1 night on the unit in the year before and year after implementation, we observed reductions in in‐hospital mortality and length of stay. Unadjusted in‐hospital mortality decreased from 2.3% to 1.1% (P=0.004), with no change in referrals to hospice (5.4% to 4.5%) (P=0.176), and length‐of‐stay decreased from 5.0 to 4.5 days (P=0.001).[19] A complete report of these findings, including an analysis of concurrent control groups is beyond the scope of this article, but here we highlight an effect we observed on ACU leadership and staff from the reduction in in‐hospital mortality.
Effects of the Change
Noting the apparent mortality reduction, ACU leadership encouraged permanent staff and rotating trainees to consider an unexpected death as a never event. Although perhaps self‐evident, before the ACU we had never been organized to reflect on that concept or to use routines to do something about it. The unit considered an unexpected death one where the patient was not actively receiving comfort measures. At the monthly meet and greet, where ACU leadership bring the permanent staff and new rotating trainees together to introduce themselves by first name, the coleaders proposed that unexpected deaths in the month ahead could represent failures to recognize or respond to deterioration, to consider an alternative or under‐treated process, to transfer the patient to a higher level of care, or to deliver more timely and appropriate end‐of‐life care. It is our impression that this introspection was extraordinarily meaningful and would not have occurred without unit‐based teams, unit‐level performance data, and ACU leadership learning to utilize this rhetoric.
Unit‐Level Nurse and Physician Coleadership
Design
Effective leadership is a major driver of successful clinical microsystems.[20] The ACU is designed to be co‐led by a nurse unit manager and physician medical director. The leadership pair was charged simply with developing patient‐centered teams and ensuring the staff felt connected to the values of the organization and accountable to each other and the outcomes of the unit.
Implementation
Nursing leadership and hospital executives influenced the selection of the physician medical director, which was a way for them to demonstrate support for the care model. Over the first 4 years, the physician medical director position has been afforded a 10% to 20% reduction in clinical duties to fulfill the charge. The leadership pair sets expectations for the ACU's code of conduct, standard operating procedures (eg, SIBR), and best‐practice protocols.
Results
The leadership pair tries explicitly to role model the behaviors enumerated in the ACU's relational covenant, itself the product of a facilitated exercise they commissioned in the first year in which the entire staff drafted and signed a document listing behaviors they wished to see from each other (see Supporting Information, Appendix 1, in the online version of this article). The physician medical director, along with charge nurses, coach staff and trainees wishing to achieve SIBR certification. Over the 4 years, the pair has introduced best‐practice protocols for glycemic control, venous thromboembolism prophylaxis, removal of idle venous and bladder catheters, and bedside goals‐of‐care conversations.
Effects of the Change
Where there had previously been no explicit code of conduct, standard operating procedures such as SIBR, or focused efforts to optimize unit outcomes, the coleadership pair fills a management gap. These coleaders play an essential role in building momentum for the structure and processes of the ACU. The leadership pair has also become a primary resource for intraorganizational spread of the ACU model to medical and surgical wards, as well as geriatric, long‐term acute, and intensive care units.
CHALLENGES
Challenges with implementing the ACU fell into 3 primary categories: (1) performing change management required for a successful launch, (2) solving logistics of maintaining unit‐based physician teams, and (3) training physicians and nurses to perform SIBR at a high level.
For change management, the leadership pair was able to explain the rationale of the model to all staff in sufficient detail to launch the ACU. To build momentum for ACU routines and relationships, the physician leader and the nurse unit manager were both present on the unit daily for the first 100 days. As ACU operations became routine and competencies formed among clinicians, the amount of time spent by these leaders was de‐escalated.
Creating and maintaining unit‐based physician teams required shared understanding and coordination between on‐call hospital medicine physicians and the bed control office so that new admissions or transfers could be consistently assigned to unit‐based teams without adversely affecting patient flow. We found this challenge to be manageable once stakeholders accepted the rationale for the care mode and figured out how to support it.
The challenge of building high‐performance SIBR across the unit, including competence of rotating trainees new to the model, requires individualized assessment and feedback necessary for SIBR certification. We addressed this challenge by creating a SIBR train‐the‐trainer programa list of observable high‐performance SIBR behaviors coupled with a short course about giving effective feedback to learnersand found that once the ACU had several nurse and physician SIBR trainers in the staffing mix every day, the required amount of SIBR coaching expertise was available when needed.
CONCLUSION
Improving value and reliability in hospital care may require new models of care. The ACU is a hospital care model specifically designed to organize physicians, nurses, and allied health professionals into high‐functioning, unit‐based teams. It converges standard workflow, patient‐centered communication, quality‐safety checklists, best‐practice protocols, performance measurement, and progressive leadership. Our experience with the ACU suggests that hospital units can be reorganized as effective clinical microsystems where consistent unit professionals can share time and space, a sense of purpose, code of conduct, shared mental model for teamwork, an interprofessional management structure, and an important level of accountability to each other and their patients.
Disclosures: Jason Stein, MD: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees and royalties for licensed intellectual property to support implementation of the care model described; founder and president of nonprofit Centripital, provider of consulting services to hospital systems implementing the care model described. The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict of interest policies. Liam Chadwick, PhD, and Diaz Clark, MS, RN: recipients of consulting fees through Centripital to support implementation of the care model described. Bryan W. Castle, MBA, RN: grant support from the US Health & Resources Services Administration to support organizational implementation of the care model described; recipient of consulting fees through Centripital to support implementation of the care model described. The authors report no other conflicts of interest.
- Institute of Medicine. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- , , . The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- . The end of the beginning: patient safety five years after “to err is human”. Health Aff (Millwood). 2004;Suppl Web Exclusives:W4‐534–545.
- , , , et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834.
- . The four habits of high‐value health care organizations. N Engl J Med. 2011;365(22):2045–2047.
- , , , . Using a Malcolm Baldrige framework to understand high‐performing clinical microsystems. Qual Saf Health Care. 2007;16(5):334–341.
- , , , . Relational coordination among nurses and other providers: impact on the quality of patient care. J Nurs Manag. 2010;18(8):926–937.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Reducing cardiac arrests in the acute admissions unit: a quality improvement journey. BMJ Qual Saf. 2013;22(12):1025–1031.
- , , , et al. Evolving practice of hospital medicine and its impact on hospital throughput and efficiencies. J Hosp Med. 2012;7(8):649–654.
- , . Improvement projects led by unit‐based teams of nurse, physician, and quality leaders reduce infections, lower costs, improve patient satisfaction, and nurse‐physician communication. AHRQ Health Care Innovations Exchange. Available at: https://innovations.ahrq.gov/profiles/improvement‐projects‐led‐unit‐based‐teams‐nurse‐physician‐and‐quality‐leaders‐reduce. Accessed May 4, 2014.
- , , , , . The daily goals communication sheet: a simple and novel tool for improved communication and care. Jt Comm J Qual Patient Saf. 2008;34(10):608–613, 561.
- , , , et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence‐based intensive care unit practices. Crit Care Med. 2009;37(10):2775–2781.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88–93.
- , , . Integrating patient safety into the clinical microsystem. Qual Saf Health Care. 2004;13(suppl 2):ii34–ii38.
- , , , . Collaborative‐cross checking to enhance resilience. Cogn Tech Work. 2007;9:155–162.
- , , , et al. Microsystems in health care: Part 1. Learning from high‐performing front‐line clinical units. Jt Comm J Qual Improv. 2002;28(9):472–493.
- , , . Mortality reduction associated with structure process, and management redesign of a hospital medicine unit. J Hosp Med. 2012;7(suppl 2):115.
- , , , et al. Microsystems in health care: part 5. How leaders are leading. Jt Comm J Qual Saf. 2003;29(6):297–308.
- Institute of Medicine. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- , , . The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- . The end of the beginning: patient safety five years after “to err is human”. Health Aff (Millwood). 2004;Suppl Web Exclusives:W4‐534–545.
- , , , et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834.
- . The four habits of high‐value health care organizations. N Engl J Med. 2011;365(22):2045–2047.
- , , , . Using a Malcolm Baldrige framework to understand high‐performing clinical microsystems. Qual Saf Health Care. 2007;16(5):334–341.
- , , , . Relational coordination among nurses and other providers: impact on the quality of patient care. J Nurs Manag. 2010;18(8):926–937.
- , , , et al. Unit‐based care teams and the frequency and quality of physician‐nurse communications. Arch Pediatr Adolesc Med. 2011;165(5):424–428.
- , , , et al. Reducing cardiac arrests in the acute admissions unit: a quality improvement journey. BMJ Qual Saf. 2013;22(12):1025–1031.
- , , , et al. Evolving practice of hospital medicine and its impact on hospital throughput and efficiencies. J Hosp Med. 2012;7(8):649–654.
- , . Improvement projects led by unit‐based teams of nurse, physician, and quality leaders reduce infections, lower costs, improve patient satisfaction, and nurse‐physician communication. AHRQ Health Care Innovations Exchange. Available at: https://innovations.ahrq.gov/profiles/improvement‐projects‐led‐unit‐based‐teams‐nurse‐physician‐and‐quality‐leaders‐reduce. Accessed May 4, 2014.
- , , , , . The daily goals communication sheet: a simple and novel tool for improved communication and care. Jt Comm J Qual Patient Saf. 2008;34(10):608–613, 561.
- , , , et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence‐based intensive care unit practices. Crit Care Med. 2009;37(10):2775–2781.
- , , , et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011;171(7):678–684.
- , , , , , . Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. J Hosp Med. 2011;6(2):88–93.
- , , . Integrating patient safety into the clinical microsystem. Qual Saf Health Care. 2004;13(suppl 2):ii34–ii38.
- , , , . Collaborative‐cross checking to enhance resilience. Cogn Tech Work. 2007;9:155–162.
- , , , et al. Microsystems in health care: Part 1. Learning from high‐performing front‐line clinical units. Jt Comm J Qual Improv. 2002;28(9):472–493.
- , , . Mortality reduction associated with structure process, and management redesign of a hospital medicine unit. J Hosp Med. 2012;7(suppl 2):115.
- , , , et al. Microsystems in health care: part 5. How leaders are leading. Jt Comm J Qual Saf. 2003;29(6):297–308.
Find Your Niche
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.
“You must define yourself as a hospitalist.” I smiled uncomfortably at my colleagues across the table as I pondered how best to respond to this statement. This seemingly innocuous comment had me perplexed, despite the fact that I aced the “What I want to be when I grow up” question as a fifth-grader. What had changed in all these years?
It was my first job as a hospitalist. I was two months out of residency and had accepted a position at the large academic hospital where I’d spent the previous three years of my life. The comfort was alluring and the transition appeared mundane. However, I naively did not realize that the difference between residency and the launch of a professional career was far greater than a miraculous transformation of paychecks.
Don’t get me wrong—throughout residency, I knew that I had a wealth of untapped energy and ideas; I was just too exhausted from patient-care duties to put action and plans into place. But as I vaulted into my career, I realized I now had the opportunity to act on these ideas and transcend the physician-in-training stereotype.
And so here I was, sitting with colleagues, attempting to define what would occupy the nonclinical portion of my upcoming career.
You might be wondering, “Isn’t great patient care enough for me as a hospitalist?” Indeed, in residency, we are praised, ranked, and valued almost solely on clinical acuity. As a hospitalist, however, we have the unique opportunity of defining ourselves in ways beyond bedside skills. While we are all astute clinicians, an important secret was kept from you during residency: You can choose another hat to wear and—unlike during your training years—you will have the time to do so.
Not buying it? It’s true. Simply pause and reflect on the hospitalists or general internal-medicine physicians you once admired; odds are they weren’t just clinicians, but they were also clinician-educators, clinician-researchers, clinician-administrators, clinician-fill-in-the-blank. In essence, they found a niche, a path that defined their careers.
And now, it’s time you did the same. But how, you ask? Here are a few pointers to get you started:
No. 1: Take Your Time
Before you go off trying to find your claim to fame, keep in mind that the first few years out of residency are a time of transition. Simply put, taking on too much, too early, could capsize your vessel. Learning to become an attending comes with a myriad of diverse responsibilities and a slow march to confidence in your clinical skills. This is a full-time position and one that requires diligence, both to ensure that you gain a strong clinical footing and fully understand the dimensions and nuances of potential “niches.” Get secure in your new role before beginning the search for your new calling. Once you feel comfortable with the resident-to-attending transition, you might find yourself itching to take on that new role in the hospital.
No. 2: Identify Your Passion
My mentor in residency was Dr. M, an all-star attending who had the energy to inspire by building an effortless bridge over the intern-resident-attending communication gap. As I studied her actions during my intern year, I found myself asking, “Could I ever be that successful in my career?”
As we shared experiences, I realized Dr. M genuinely was happy and passionate about her job every day. Her ability to effectively communicate to residents, nurses, and patients was a simple segue to her niche. So what is her niche? Dr. M is a clinician-communicator. Whether it is blogging about a recent patient experience on the wards or appearing as a physician correspondent for an Atlanta news affiliate, Dr. M’s strength is effective communication. Despite being a great clinician, it was her drive outside the wards that helped me understand she had found, and was living, her passion.
During residency, every physician had that one thing that continued to drive us when the going got tough. For some, it was the eager medical student who deserved to learn about that critical aortic stenosis murmur, even if you were 28 hours into your shift. For others, it was quality-improvement (QI) projects that arose from experiencing firsthand the effects of haphazard care transitions. Still others became passionate about patient advocacy after watching patients struggle to understand complex diseases.
Why are these examples relevant? Because each example represents a pathway to your niche. The first person might find a niche as a clinician-educator, exploring opportunities with the medical school during their first year. The second might align themselves with like-minded colleagues in QI and begin projects that will solve frustrations or improve physician efficiency. The third might get involved with local health fairs or local news stations to promote health awareness. The common link between all of these examples is that a clinician’s niche is based on their passion.
No. 3: Stay in Your Own Orbit
We’ve all been go-getters. We’re used to stretching ourselves thin to show what efficient, all-around superdocs we are. And this drive to say yes to your boss, that clinical nurse specialist, and to your colleague who schedules medical student clinical exams will lead to fruitful clinical ventures. Ultimately, however, this approach will leave you exhausted and will leave your colleagues wondering what it is that you actually do with your nonclinical time.
The solution? Learn to invest yourself, and your time, wisely.
During the first week of my new career (when I was asked that fateful question to define myself), I received the best advice. Dr. S (yes, another mentor—it’s OK to have multiple mentors) drew a series of random dots on a sheet of paper. Each of these dots represented opportunities that would arise during my first year. Circling a dot in the middle of the page, Dr. S looked at me and said, “One of these dots represents your passion. The remaining dots are where others’ interests lie. Pick one of these and work in its orbit only. Sure, you may jump up to another dot for a project, but the more you stay within the orbit of your passion, the happier and more productive you’ll be.”
In your first few years on the job, do say yes to joining committees, taking on projects, and collaborating with colleagues. But as you do, ensure that each of these decisions is within your orbit. Saying yes is easy, but saying yes and making it count twice is a skill that you will develop as your career progresses.
Not sure what your orbit is? I encourage you to refer back to tip No. 2 and start seeking out opportunities that center around your passion, not someone else’s.
No. 4: Master the Network
Networking is an art in which our business-minded friends from college excel. Unfortunately, studying for exams and resting after a 30-hour MICU call is a solo venture that leaves little room to hone networking skills. But now, the onlooker must become the master … of networking.
Networking is an important skill to develop, and you start the very first day of your career. The relationships you forge with successful colleagues and superiors will provide you with opportunities beyond the clinical arena (see “Simple Strategies to Expand Your HM Network,” below).
Not sure where to start? A mentor can help. Look at the well-respected leaders in your department and institution, and take note of how each of these people always talk about their mentors and the role they played in crystallizing their career paths. Good mentors steer you toward other like-minded professionals. They help you navigate the complex relationships that are at the base of a successful networking strategy. A wise strategy is to find multiple mentors who serve different purposes in your career; this usually leads to untold opportunities.
Can’t find a suitable mentor at the workplace? Fear not. Consider networking at local, regional, and national society meetings (www.hospitalmedicine.org/events). When the opportunity arises, do more than just attend the clinical sessions during these meetings. Learn which committees are available through the various societies and contact their leaders to express interest in joining next year’s group. Your fellow committee members will be a natural place to practice your networking skills. High-quality relationships made during this time have the potential to grow, and they could lead to more opportunities as your career progresses.
No. 5: Take Calculated Risks
This might sound simple enough, but it is not easy. It is uncomfortable to make mistakes in front of a public audience (and believe me, we all make mistakes). But you will be successful, too, and you must learn how to promote yourself during these times.
Challenge yourself by attending SHM’s Academic Hospitalist Academy (www.academichospitalist.org), or by taking on that project discussed at the last committee meeting. Say yes to your mentor when they learn your passion is QI and appropriately volunteer you to lead a resident research project. Submit your most recent project to an abstract competition, such as SHM’s Research, Innovation, and Clinical Vignettes (RIV) competition. Before you go, research others in your field with similar interests and seek them out during the meeting to share your experiences. Be ready to explain your pitfalls as well, and use this as an opportunity to learn from experienced colleagues.
Whether it is speaking in front of a group of strangers at the academy, giving a presentation to your colleagues, or meeting HM leaders at the national meeting, opportunities abound and often pay off in the long run.
No. 6: Ready For Change
Wait, change? Back up to tip No. 2. I know you’re saying, “But I’m following my passion.” Remember that, fresh out of residency, your interests likely are somewhat different than those of your future self. Thus, as the saying goes, the only thing that is certain is change.
Through networking and putting yourself in new positions, you will discover a world that was never revealed to you in residency. Case in point: my friend and colleague Dr. H. As a chief resident, Dr. H was exposed to a year of educational opportunities before she embarked on a hospitalist career. Education seemed like a natural fit in her first year as a hospitalist. In fact, she never imagined that it would be her experience with the inner workings of her hospital’s electronic medical record (EMR) during her chief year that would catapult her career as the physician director for information services. Yes, she is now a hospitalist-administrator. The bottom line: Remain resilient and ready to take up that next interesting opportunity.
Residency provides you with the skills to be a confident and effective clinician. But as residency comes to a close, think about what really drives you. Where do you see yourself in five years? How about 10 years?
Plot your course to live your passion at work every day; as you start your new job, find, refine, and define your niche.
Dr. Payne is a hospitalist in the Department of Internal Medicine at Emory University Hospital in Atlanta, and a clinical instructor of medicine at Emory University School of Medicine.