User login
Critical Care in the ED: Mechanical Ventilation, Sepsis, Neurological Hypertensive Emergencies, and Pressors in Shock
Emergency medicine and critical care medicine share a responsibility for the care of acutely ill patients with life-threatening pathologies. The skills required of both emergency physicians (EPs) and critical care specialists to recognize, diagnose, and resuscitate such patients have resulted in many shared guidelines, recommendations, and publications. When critically ill patients enter the hospital through the ED, the care provided by EPs greatly impacts both the early and long-term outcomes. It is not uncommon for critically ill patients to spend several hours under the care of an EP while awaiting an available inpatient bed in the intensive care unit (ICU) or “step down” monitored unit.
This article provides a summary review of current guidelines, evidence-based medicine recommendations, and the results of recent trials involving ventilator management, treatment of sepsis, management of hypertension accompanying neurological emergencies, and the selection of pressors for the treatment of different shock states.
Ventilator Management
Mechanical ventilation is frequently undertaken in the ED for patients with respiratory failure—the origin of which is not always immediately clear. Data from the National Heart, Lung, and Blood Institute’s (NHLBI) acute respiratory distress syndrome (ARDS) clinical network (http://www.ardsnet.org) and other clinical trials have established the benefit of low tidal-volume, “lung-protective” ventilation in the patient with ARDS.1,2 Numerous studies have also shown the benefit of low-tidal-volume (TV), ventilation in patients without ARDS, and its use is now the standard of care for a large range of respiratory conditions causing compromise.3
The prompt initiation of lung-protective ventilation has a significant impact on reducing ICU mortality.4 A recent retrospective review of 3.5 million ED visits showed the median length of stay for patients started on mechanical ventilation in the ED to be greater than 3 hours.5 Such a length of time on mechanical ventilation in this setting can have significant effects on the course of illness; however, it is not clear whether mechanical ventilation performed in the ED typically conforms to evidence-based standards. In one study performed in an academic center, less than one-third of patients with sepsis and respiratory failure received low-volume ventilation in the ED.6 Another study suggested that emergency medicine residents may not receive as much dedicated education on the initial management of ventilators as needed—despite the potentially unforgiving physiologic process of positive-pressure mechanical ventilation.7
The fundamental principles required to safely manage most patients in respiratory failure are not difficult to master. There are several simple evidence-based ventilator strategies for managing patients with respiratory failure. The three primary principles of initiating and providing effective mechanical ventilation are: (1) avoiding traumatic ventilation; (2) maintaining normoxia; and (3) maintaining appropriate acid-base balance. Each of these principles can be achieved in a stepwise fashion.
Step I: Establishing Lung-Protective Settings on the Ventilator
Three central parameters must be selected at the initiation of assist-control mechanical ventilation: TV, respiratory rate (RR), and positive end-expiratory pressure (PEEP). These parameters have been extensively studied, and there is excellent evidence to guide the EP in choosing the correct settings.
Tidal Volume. Although the normal human lung can accommodate about 6 L of air, in cases of respiratory failure, the surface area available for gas exchange is significantly reduced due to a pathologic process undermining entire regions of the air-blood interface. Consequently, a person whose normal lungs are suddenly required to perform the life-sustaining gas exchanges in critical illness with the much smaller lung surface is at a significant disadvantage.
The widely accepted lung-protective volumes range from 6 to 8 mL/kg of predicted body weight (PBW), a height-based calculation.8 For example, in a 6-foot tall man, 6 mL/kg of PBW amounts to a TV of 466 mL; in a 5-foot tall woman, the same amount of PBW amounts to a TV of 273 mL. Volumes may be referenced using PBW tables from the NHLBI ARDS network or by employing the following equations:
Adult men: PBW (kg) = 50 + 2.3 (height [in] – 60)
Adult women: PBW (kg) = 45.5 + 2.3 (height [in] – 60).9
Respiratory Rate. The RR should be set somewhat higher than normal because the TV per breath has been slightly reduced, and also because sick patients in a catabolic state may have larger minute ventilations than they would when healthy. As previously described, since the TV is restricted, RR is the most mobile parameter in maintaining appropriate minute ventilation. Minute ventilation (MV) is the product of RR multiplied by TV (MV = RR x TV), and this should be calculated to approximate the patient’s own efforts, which are dependent upon the clinical circumstances. For example, patients whose bodies are trying to compensate for an acidosis will require much higher rates than those who are simply obtunded and intubated for airway protection. In other words, in order to remove carbon dioxide (CO2) in an acidemic patient, a higher RR rate may be required, whereas a lower rate may be selected to compensate for alkalemia while maintaining appropriate oxygen (O2) levels in both cases.10
Positive End-Expiratory Pressure. Previous recommendations for ventilation in respiratory failure called for large TVs (ie, 10 to 15 mL/kg), partly out of concern that smaller volumes would promote distal airway collapse, thereby increasing the amount of lung that received blood but not air, consequently worsening overall oxygenation.11 Although administering such large volumes has clearly proved harmful, the valid concern about distal airway collapse can be addressed in part by adjustments to PEEP, which acts to “stent” open airways after most of the tidal breath has left the airways.
Positive end-expiratory pressure, however, is not without risks.12 Blood from the rest of the body will encounter resistance returning to a thoracic cavity persistently inflated by positive pressure, and this decrease in preload may contribute to hypotension. Similarly, a weak right ventricle may struggle to push blood into the compressed pulmonary vasculature, increasing the cardiac workload and further compromising hemodynamics.13 In general, PEEP should be set as low as the maintenance of adequate oxygenation permits. The NHLBI ARDS guidelines provide a table on balancing PEEP and the fraction of inspired O2 (FiO2), as well as hypotension, in refractory hypoxemic patients—with the limitation on PEEP set by the patients’ pulmonary compliance (plateau pressures, discussed next).8
After making these selections, several parameters must be monitored closely. Those most relevant to lung-protective ventilation are the peak airway pressure and, most importantly, the plateau pressure. Numerous animal studies now demonstrate serious lung injury in both healthy and diseased lungs from high peak pressures (defined as a plateau pressure >30 cm water [H2O]).14,15 A high-pressure alarm sounding on the ventilator must be promptly addressed by an evaluation for easily reversible causes, such as tube obstruction, pneumothorax, breath stacking, pulmonary edema, or pleural effusions. A full discussion of the causes of elevated peak and plateau pressures is beyond the scope of this review, but if the plateau pressures remain consistently high, a reduction in TV may be necessary.
Step II: Maintaining Normoxia
As a severely hypoxic patient will rapidly decompensate with progression to death, a host of monitoring devices are used to alert the nurse or physician that O2 levels have fallen below the normal range. Strategies to manage refractory hypoxia in the ventilated patient are complex. For most patients, 100% FiO2 is initiated immediately after intubation to increase the safety of the procedure, but there is animal evidence that high O2 levels promote inflammatory responses, and human data suggest hyperoxia can be deleterious to long-term outcomes, particularly following cardiac arrest and stroke.16,17 A persistent O2 saturation of 100% on pulse oximetry or a supraphysiologic partial pressure of O2 (PaO2) on an arterial blood gas (defined as >200 mm Hg) may actually cause the patient more harm than good. Therefore, the fraction of inspired O2 should be titrated to maintain normoxia. The ARDS protocol, for example, targets an O2 saturation of 88% to 95% and a PaO2 of 55 to 80 mm Hg.8
Step III: Maintaining Acid-Base Balance
The basic principles of acid-base physiology should be familiar to EPs. When a patient is sedated and the airway secured, the primary means by which blood pH is maintained is now in the hands of the intubating physician. Patients with respiratory failure may have compensated for a preexisting derangement in their blood pH. If the preexisting condition is not recognized and ventilator settings are not maintained appropriately, they may be vulnerable to developing another derangement. Even on settings that allow the patient to breathe over a set rate, the sedation required to tolerate an endotracheal tube may cause significant respiratory depression, making it impossible for the patient to auto-regulate the respiratory component of acid-base homeostasis (ie, by hyperventilation).
As in the discussion of RR, TVs are “fixed” based on low-TV lung-protective ventilation. Therefore, changing the patient’s set RR is the easiest method to adjust the partial pressure of CO2 (PaCO2), and consequently address any respiratory acidosis. An increase in the RR will increase the patient’s minute ventilation, leading to a decrease in serum PaCO2 levels, whereas a decrease in the RR will have the converse effect. It is important to obtain an arterial blood-gas reading shortly after intubation and to continue to monitor the impact of any ventilator titrations on the patient’s acid-base status.
Studies of “permissive hypercapnia” in ARDS patients have shown that prioritizing lung-protective ventilator settings, even at the expense of a normal CO2, reduce mortality.1,18 Even in situations where it is not necessary to maintain hypercapnia for lung-protective settings, the hypercapnia appears to have beneficial effects.19-21 No upper limits on hypercapnia have been established, and even extreme levels have been associated with successful patient outcomes.22 However, a study by Hickling et al23 demonstrated that an initial trial of lung-protective ventilation demonstrated benefit from unbuffered hypercarbia and acidosis, reporting an average CO2 level of 66 and a pH of 7. These guidelines should be appropriate for use in the ED.
In summary, assuming control of a patient’s respiratory system—with its nuanced and responsive role in acid-base, oxygenation, and cardiopulmonary hemodynamics—is one of the most difficult situations routinely encountered by an EP. While the procedure itself may be life-saving, the next several hours can have significant impact on the patient’s long-term outcome.
Treating Sepsis and Surviving Sepsis: Recommendations Versus the ARISE/ProCESS Trials
Sepsis and Septic Shock
Sepsis is defined as an infection plus systemic inflammatory response syndrome (SIRS). Severe sepsis is sepsis plus sepsis-induced organ dysfunction or tissue hypoperfusion resulting in or caused by lactic acidosis, acute lung injury, altered mental status, or coagulation abnormalities. Septic shock refers to persistent sepsis-induced hypotension despite adequate fluid resuscitation.24 The ambiguity of these definitions may invariably lead to a practitioner’s underappreciation or misconception of the importance of sepsis.
Sepsis is one of the most common, yet least-recognized, entities. In the United States, it is estimated that 3 in 1,000 people annually are affected by sepsis, and every few seconds, a person dies of sepsis.25 Both numbers underestimate the effects on the elderly. Clinical manifestations of sepsis vary, and the condition may originate from both community-acquired and healthcare-associated sources.
In 2001, a landmark study demonstrated that early goal-directed therapy (EGDT) reduced mortality and improved patient outcomes in patients presenting to the ED in severe sepsis.26 The estimated 12% to 16% reduction in mortality reported in this trial began an initiative to broaden the scope and awareness of sepsis.
Current Literature and Evidence-Based Guidelines
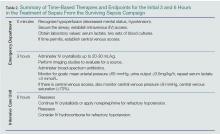
The most recent guidelines for the management of septic shock from the Surviving Sepsis Campaign are summarized in Table 1. With its last revision, the Surviving Sepsis guidelines of 2012 has two main management foci—initiating treatment within the first 3 and the first 6 hours after recognition within the first 3 hours and those within the first 6 hours after sepsis recognition (Table 2). Within the first 3 hours, the treatment team should draw a serum lactate level; obtain cultures prior to the administration of antibiotics; initiate broad-spectrum antibiotics as early as possible; and administer 20 to 30 mL/kg of crystalloid fluids in patients with hypotension or a lactate level greater than 4 mmol/L. Within the first 6 hours, the clinician should administer intravenous (IV) vasopressors, preferentially norepinephrine, for persistent hypotension after a fluid challenge to maintain a mean arterial pressure >65 mm Hg; place a supra-diaphragmatic central venous catheter to measure a serum mixed venous O2 saturation (ScvO2) and central venous pressure (CVP); and measure serial serum lactate levels if they were initially elevated (lactate ≥4 mmol/L [36 mg/dL]).24,30,31 The targets for ScvO2 and CVP are ≥70%, and >8 mm Hg, respectively.
Summary
Sepsis is a prevalent ED presentation associated with mortality that can present in a complex fashion. Early recognition and management is essential and can be condensed into a few key recommendations. Becoming familiar with and incorporating these recommendations into daily practice will enable EPs to deliver quality care to every patient presenting with sepsis, and will also reduce mortality.
Blood Pressure Management for Select Neurological Emergencies
Patients with ischemic stroke, spontaneous intracerebral hemorrhage (ICH), and aneurysmal subarachnoid hemorrhage (SAH) often present with elevated blood pressures (BPs).34-36 In caring for these patients, EPs face the question of how, or even if, the patient’s BP should be managed. What are the appropriate BP targets for each of the aforementioned pathologies? Does aggressive BP management benefit or harm the patient?
Background
The relationship between hypertension and stroke is different for each stroke type. Retrospective data show a U-shaped relationship between BP and mortality in ischemic stroke, with the highest mortality observed at both extremes of the BP curve.34 Data also suggest increased mortality when ICH is accompanied by hypertension.35 Hypertension may also be associated with a higher risk of rebleeding in patients with SAH due to aneurysms.36 Because of the variable relationship between stroke and hypertension, therapeutic recommendations for each type of stroke can be confusing.
Current Literature and Evidence-Based Guidelines
Firm evidence to make therapeutic recommendations remains elusive. The recent American Heart Association (AHA) guidelines covering ischemic stroke, ICH, and SAH were published between late 2010 and early 2013, and several trials investigating the role of BP control in ischemic and hemorrhagic stroke have subsequently been published.37-41
When the Cochrane Collaboration updated its systematic review on vasoactive medications in stroke in 2014 to include recent evidence,42 it ultimately concluded that lowering BP does not improve mortality, neurological deterioration, or quality of life regardless of stroke type, and suggest that further investigations should be undertaken.9 However, the Cochrane authors noted that two recent trials showed a statistically significant association between improved quality of life and BP reduction within 6 hours of stroke onset.38-39 Although the data were compiled from just 2,835 patients of the 15,432 included in the entire Cochrane review, it suggested that interventions initiated in the ED may contribute to any potential beneficial outcomes from intensive BP control.
Ischemic Stroke
The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) investigated the initiation of BP-control measures within 48 hours of onset of ischemic stroke in approximately 4,000 patients and found no significant difference in death or disability between the group that received BP-control interventions and the group that did not.37 The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT) included patients with both ischemic and hemorrhagic strokes. Though it studied only 41 patients, this trial suggests that early BP control is safe and may be associated with lower disability.38 These findings are bolstered by the more recent Efficacy of Nitric Oxide in Stroke (ENOS) trial showing a similar safety profile for BP control in both ischemic and hemorrhagic strokes, though the mean difference in systolic BP after therapy was a mere 7 mm Hg.40 The combined data from the RIGHT and ENOS trials offer little to clarify the question of appropriate BP control.
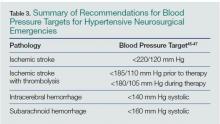
For now, the EP is left with the AHA/American Stroke Association (ASA) guideline’s recommendation “not to lower the BP during the initial 24 hours of acute ischemic stroke unless the BP is greater than 220/120 mm Hg.”34 The recommendation differs in cases when a patient receives thrombolytics and hemorrhagic transformation is a risk. There have been no new data to change the AHA/ASA’s recommendations for patients receiving thrombolytics. In such cases, the EP should ensure the patient’s BP is below 185/110 mm Hg prior to thrombolytic administration and below 180/105 mm Hg during therapy.34 A variety of agents is available to lower BP in this situation, and includes IV labetalol, nicardipine, esmolol, and others.
Intracerebral Hemorrhage
The recent literature on blood pressure control in ICH has also increased since the most recent AHA/ASA recommendations. The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2 included over 2,800 patients randomized to intensive early therapy to reduce BP to less than 140 mm Hg or less than 180 mm Hg and found no significant difference in mortality or safety between the two groups, though intensive therapy was associated with less disability.39 The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial (ICH-ADAPT) trial further clarified the issue of safety during intensive BP control by showing no decrease in perihematomal cerebral blood flow in patients whose BP control was targeted to less than 150 mm Hg compared to those whose BP was less than 180 mm Hg, suggesting that aggressive BP reduction does not cause iatrogenic ischemic stroke.41
These combined data suggest that intensive BP management is safe for patients with ICH, providing reassurance for the AHA/ASA guideline recommendation that “in patients…with a systolic BP of 150 to 220 mm Hg, acute lowering of systolic BP to 140 mm Hg is probably safe.”35 Whether this improves patient outcomes remains unclear. Again, multiple agents are available for BP control, including IV labetalol or nicardipine, with no agent identified as superior in producing better patient outcomes. A continuous infusion is recommended if several boluses are ineffective in achieving and maintaining the target BP, as BP variability has been associated with poorer outcomes.43
Subarachnoid Hemorrhage
There are no large recent studies in the literature on antihypertensive therapy in SAH. The AHA/ASA guidelines updated in 2012 reflect the consensus that elevated BPs are associated with increased risk of aneurysmal rebleeding and thus poorer patient-oriented outcomes. The consensus remains to use a titratable agent to target a systolic BP less than 160 mm Hg until definitive neurosurgical therapy, such as aneurysmal coiling or clipping.36 Given the variability of the sodium nitroprusside dose-response relationship, IV labetalol, and nicardipine, are recommended agents for continuous control, though data showing differences in mortality and/or disability are lacking.36 Again, retrospective data suggest that BP variability negatively impacts mortality and disability, so consider early initiation of continuous infusions to achieve and maintain consistency in the chosen target.44
Summary
Pressors in the Management of Hypotension
Norepinephrine
Norepinephrine is one of the most commonly used agents for shock in the ED, with indications spanning multiple etiologies. It is an endogenous neurotransmitter that works predominantly on a1 receptors as well as exerting some modest effects on b1 and b2 receptors, for combined vasopressor and improved cardiac contractility effect.46-47 Norepinephrine is currently the recommended initial agent for sepsis-induced tissue hypoperfusion.24 However, a recent Cochrane systematic review and meta-analysis supports evidence of limited differences among various pressors.48 Several comparative randomized control trials show norepinephrine is as effective as other agents, but with fewer side effects.24,49 With the ease and familiarity of its use by most EPs, and a wide therapeutic index for targeted effect versus arrhythmias, norepinephrine is a reasonable choice as the initial pressor in managing a wide variety of shock syndromes.
Vasopressin
Another commonly used agent in the treatment of shock, vasopressin is an analogue of the antidiuretic hormone secreted from the posterior pituitary gland, exerting its CV effects primarily as a vasoconstrictor by increasing intracellular calcium.50 Vasopressin doses are 0.03 or 0.04 U/min IV without titration.24,50 Early studies of septic patients demonstrated a relative deficiency of serum vasopressin levels, leading clinicians to utilize it in the treatment of sepsis-induced shock. However, the Vasopressin and Septic Shock Trial (VASST) trial demonstrated that the addition of vasopressin to norepinephrine did not produce any improvements in morbidity or mortality compared with norepinephrine alone.51 Despite these findings, vasopressin is still commonly used as a secondary agent to correct continued hypotension. Vasopressin may be appropriate for patients who specifically require peripheral vasoconstriction in the setting of good cardiac output and volume status, ability to tolerate increases in afterload, or in patients at risk for dysrhythmias.
Dopamine
Dopamine had been previously recommended as the initial choice of pharmacologic support for the management of shock.24,52-54 Dopamine is an adrenergic agonist agent that works via a1 and b1 receptors as well as a precursor to the synthesis of norepinephrine and epinephrine.55 There are dose-dependent effects on various receptors from escalating amounts administered,55-56 but the literature does not support the concept of “renal-dose” dopamine.57-59 A study by DeBaker et al49 suggested no difference in efficacy between dopamine and norepinephrine, but demonstrated a greater tendency toward cardiac dysrhythmias with dopamine. For these reasons noted above, norepinephrine may be the initial agent for pharmaceutical support of shock, particularly in septic syndromes, with dopamine as a secondary or adjunct agent in patients at low risk for tachyarrhythmia or a relative bradycardia. 24, 56
Dobutamine
Dobutamine is another adrenergic agonist that is similar to dopamine but with a greater effect on inotropic cardiac contractility due to a preferential action at b1 receptors.60 It can potentially induce peripheral vasodilatation due to its effect on arterial b1 receptors. Given this balance, dobutamine is an agent that should be utilized for cardiogenic shock when increased contractility is needed. These effects are particularly useful in patients with “wet and cold” heart failure who have a low cardiac output and volume-overloaded status.61, 62 However, it may be necessary to add another agent to provide additional peripheral vasoconstriction should the use of dobutamine affect lead to excessive vasodilatation.
Epinephrine
One of the most powerful vasoactive agents, epinephrine has a high affinity for all b1, b2 and a1 receptors.63 These combined effects lead to increased cardiac output and improved BP by increasing cardiac contractility and peripheral vasoconstriction. The effect of epinephrine in limiting mast cell release of histamine makes it the preferred choice for the treatment of anaphylaxis.64 However, side effects of epinephrine include hypertension, tachydysrhythmias, tissue ischemia from vigorous vasoconstriction, and induced lactic acidosis.63
Phenylephrine
Phenylephrine is an a-adrenergic agonist that activates a1 receptors on arteriole smooth muscle, resulting in vasoconstriction.65 It is currently recommended only for hypotension related to procedural sedation.47 Phenylephrine is not recommended for treating patients with septic shock, except when there are concerns about tachydysrhythmias; persistent hypotension with a high cardiac output after treatment with other vasoconstrictor and inotropic drugs; or when a “pure” vasoconstrictor may be preferred.24,56,65
Summary
Although there are many other vasoactive agents that can be used, the selected agents discussed above represent those most commonly used in the ED. All demonstrate significant crossover effects and receptor activation, as well as impact on cardiac contractility and vasoconstriction. The suggested specific indications for each agent are based on current evidenced-based medicine, clinical guidelines, and theoretical benefits on clinical scenarios. But, as always, clinical decisions should be individualized for critically ill patients.
Conclusion
The resuscitation and initiation of care for critically ill patients must typically be immediately upon their arrival in the ED. While general guidelines or recommendations exist for commonly encountered pathologies, treatment should always be patient-centered, based on the needs and nuances unique to each patient in this vulnerable population. The initiation of mechanical ventilation, treatment of sepsis, management of hypertensive neurosurgical emergencies, and use of pressors in shock states are among the most critically important tasks an EP is called upon to perform. This review of current evidence-based guidelines and recommendations will help EPs provide the appropriate and unique care each patient requires.
Dr Brubaker is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Yu is a fellow of adult critical care medicine – emergency medicine in the department of critical care medicine, University of Pittsburgh Medical Center, Pennsylvania. Dr Goodmanson is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Schott is an assistant professor, department of emergency medicine and critical care medicine; assistant director of ultrasonography; director, critical care elective student rotation; and director, point of care ultrasound elective student rotation, at the University of Pittsburgh, Pennsylvania
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
- Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32(9):1817-1824.
- Brower RG, Rubenfeld GD. Lung-protective ventilation strategies in acute lung injury. Crit Care Med. 2003;31(4):S312-S316.
- Needham DM, Yang T, Dinglas VD. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med. 2015;191(2):177-185.
- Easter BD, Fischer C, Fisher J. The use of mechanical ventilation in the ED. Am J Emerg Med. 2012;30(7):1183-1188.
- Fuller BM, Mohr NM, Dettmer M, et al. Mechanical ventilation and acute lung injury in emergency department patients with severe sepsis and septic shock: an observational study. Acad Emerg Med. 2013;20(7):659-669.
- Wilcox SR, Seigel TA, Strout TD, et al. Emergency medicine residents’ knowledge of mechanical ventilation. J Emerg Med. 2014. doi:10.1016/j.jemermed.2014.09.059. [Epub ahead of print]
- National Institutes of Health’s National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Clinical Network Mechanical Ventilator Protocol Summary. http://www.ardsnet.org/system/files/Ventilator%20Protocol%20Card.pdf. Accessed March 5, 2015.
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (NHLBI ARDS) Network. Predicted body weight calculator. http://www.ardsnet.org/node/77460. Accessed March 5, 2015.
- Boron WF. Acid-base physiology. In: Boron WF, Boulpaep EL, eds. Medical Physiology: A Cellular And Molecular Approach. Philadelphia, PA: Saunders/Elsevier; 2009:647-649.
- Orebaugh, SL. Initiation of mechanical ventilation in the emergency department. Am J Emerg Med. 1996;14(1):59-69.
- Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149(5):1327-1334.
- Marino PL, Sutin KM. Principles of mechanical ventilation. In: Marino PL, ed. The ICU Book. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:457-472.
- Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection with positive end-expiratory pressures. Am Rev Resp Dis. 1974;110(5):556-565.
- Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993;21(1):131-143.
- Bhandari V. Molecular mechanisms of hyperoxia-induced acute lung injury. Front Biosci. 2008;13:6653-6661.
- Kilgannon JH, Jones AE, Shapiro NI, et al; Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165-2171.
- Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
- Laffey JG, Tanaka M, Engelberts D, et al. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med. 2000;162(6):2287-2294.
- Costello J, Higgins B, Contreras M, et al. Hypercapnic acidosis attenuates shock and lung injury in early and prolonged systemic sepsis. Crit Care Med. 2009;37(8):2412-2420.
- Ijland MM, Heunks LM, van der Hoeven JG. Bench-to-bedside review: hypercapnic acidosis in lung injury—from ‘permissive’ to ‘therapeutic.’ Crit Care. 2010;14(6):237.
- Garg SK. Permissive hypercapnia: Is there any upper limit? Indian J Crit Care Med. 2014;18(9):612-614.
- Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med. 1994;22(10):1568-1578.
- Dellinger RP, Levy MM, Rhodes A, et al; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup Surviving Sepsis Campaign. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165-228.
- Peake SL, Delaney A, Bailey M, et al; ARISE Investigators; ANZICS Clinical Trials Group. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496-1506.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;8;345(19):1368-1377.
- Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(21):2063.
- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303-1310.
- Rivers EP, Ahrens T. Improving outcomes for severe sepsis and septic shock: tools for early identification of at-risk patients and treatment protocol implementation. Crit Care Clin. 2008;24(3 Suppl):S1-S47.
- Nguyen HB, Rivers EP, Abrahamian FM, et al; Emergency Department Sepsis Education Program and Strategies to Improve Survival (ED-SEPSIS) Working Group. Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med. 2006;48(1):28-54.
- Jones AE, Puskarich MA. The Surviving Sepsis Campaign guidelines 2012: update for emergency physicians. Ann Emerg Med. 2014;63(1):35-47.
- Yealy DM, Kellum JA, Huang DT, et al.;ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683-1693.
- Huang DT, Angus DC, Barnato A, et al; ProCESS/ARISE/ProMISe Methodology Writing Committee. Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: methodology of ProCESS, ARISE, and ProMISe. Intensive Care Med. 2013;39(10):1760-1775.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al; American Heart Association Stroke Council and Council on Cardiovascular Nursing. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711-1737.
- He J, Zhang Y, Xu T, et al; The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) Investigators. Effects of immediate blood pressure reduction on death and major disability in patients with acute ischemic stroke: the CATIS randomized clinical trial. JAMA. 2014;311(5):479-489.
- Ankolekar S, Fuller M, Cross I, et al. Feasibility of an ambulance-based stroke trial, and safety of glyceryl trinitrate in ultra-acute stroke: The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT, ISRCTN66434824). Stroke. 2013;44(11):3120-3128.
- Anderson CS, Heeley E, Huang Y, et al; The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2) Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355-2365.
- Bath PM, Woodhouse L, Scutt P, et al; ENOS Trial Investigators. Efficacy of nitric oxide, with or without continuing antihypertensive treatment, for management of high blood pressure in acute stroke (ENOS): a partial-factorial randomised controlled trial. Lancet. 2014;385(9968):617-628
- Butcher KS, Jeerakathil T, Hill M, et al; ICH ADAPT Investigators. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke. 2013;44(3):620-626.
- Bath PM, Krishnan K. Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database Syst Rev. 2014;10:CD000039.
- Tanaka E, Koga M, Kobayashi J, et al. Blood pressure variability on antihypertensive therapy in acute intracerebral hemorrhage: the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement-intracerebral hemorrhage study. Stroke. 2014;45(8):2275-2279.
- Beseoglu K, Unfrau K, Steiger HJ, Hänggi D. Influence of blood pressure variability on short-term outcome in patients with subarachnoid hemorrhage. Cent Eur Neurosurg. 2010;71(2):69-74.
- Hinshaw LB, Cox BG, eds. The fundamental mechanisms of shock. Proceedings of a Symposium Held in Oklahoma City, Oklahoma, October 1-2, 1971. In: Advances in Experimental Medicine and Biology, Vol 23. New York, NY: Plenum Press; 1972.
- Norepinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=norepinephrine&x=0&y=0. March 5, 2015.
- Overgaard CB, Dzavik V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008;118(10):1047-1056.
- Havel C, Arrich J, Losert H, et al. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2011;(5):CD003709.
- De Backer D, Biston P, Devriendt J, et al; SOAP II Investigators. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 2010;362(9):779-789.
- Vasopressin. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=vasopressin&x=0&y=0. March 5, 2015.
- Russell JA, Walley KR, Singer J, et al; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
- Martin C, Papazian L, Perrin G, Saux P, Gouin F. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest. 1993;103(6):1826-1831.
- De Backer D, Creteur J, Silva E, Vincent JL. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31(6)1659-1667.
- Day NP, Phu NH, Bethell DP, et al. The effects of dopamine and adrenaline infusions on acid-base balance and systemic haemodynamics in severe infection. Lancet. 1996;348(9022):219-223.
- Dopamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=dopamine&x=0&y=0. March 5, 2015.
- Manaker S. Use of vasopressors and inotropes. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/use-of-vasopressors-and-inotropes?source=search_result&search=Use+of+vasopressors+and+isotopes&selectedTitle=1%7E150. Accessed March 5, 2015.
- Lauschke A, Teichgräber UK, Frei U, Eckardt KU. ‘Low-dose’ dopamine worsens renal perfusion in patients with acute renal failure. Kidney Int. 2006;69(9):1669-1674.
- Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J. Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Australian and New Zealand Intensive Care Society (ANZICS) Clinical Trials Group. Lancet. 2000;356(9248):2139-2143.
- Kellum JA, M Decker J. Use of dopamine in acute renal failure: a meta-analysis. Crit Care Med. 2001;29(8):1526-1531.
- Dobutamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=Dobutamine&x=0&y=0. Accessed March 5, 2015.
- Nohria A, Mielniczuk LM, Stevenson LW. Evaluation and monitoring of patients with acute heart failure syndromes. Am J Cardiol. 2005;96(6A):32G-40G.
- Joseph SM, Cedars AM, Ewald GA, Geltman EM, Mann DL. Acute decompensated heart failure: contemporary medical management. Tex Heart Inst J. 2009;36(6):510-520.
- Epinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=epinephrine. Accessed March 5, 2015.
- Vadas P, Perelman B. Effect of epinephrine on platelet-activating factor-stimulated human vascular smooth muscle cells. J Allergy Clin Immunol. 2012;129(5):1329-1333.
- Phenylephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=65.%09Phenylephrine&x=10&y=10. Accessed March 5, 2015.
Emergency medicine and critical care medicine share a responsibility for the care of acutely ill patients with life-threatening pathologies. The skills required of both emergency physicians (EPs) and critical care specialists to recognize, diagnose, and resuscitate such patients have resulted in many shared guidelines, recommendations, and publications. When critically ill patients enter the hospital through the ED, the care provided by EPs greatly impacts both the early and long-term outcomes. It is not uncommon for critically ill patients to spend several hours under the care of an EP while awaiting an available inpatient bed in the intensive care unit (ICU) or “step down” monitored unit.
This article provides a summary review of current guidelines, evidence-based medicine recommendations, and the results of recent trials involving ventilator management, treatment of sepsis, management of hypertension accompanying neurological emergencies, and the selection of pressors for the treatment of different shock states.
Ventilator Management
Mechanical ventilation is frequently undertaken in the ED for patients with respiratory failure—the origin of which is not always immediately clear. Data from the National Heart, Lung, and Blood Institute’s (NHLBI) acute respiratory distress syndrome (ARDS) clinical network (http://www.ardsnet.org) and other clinical trials have established the benefit of low tidal-volume, “lung-protective” ventilation in the patient with ARDS.1,2 Numerous studies have also shown the benefit of low-tidal-volume (TV), ventilation in patients without ARDS, and its use is now the standard of care for a large range of respiratory conditions causing compromise.3
The prompt initiation of lung-protective ventilation has a significant impact on reducing ICU mortality.4 A recent retrospective review of 3.5 million ED visits showed the median length of stay for patients started on mechanical ventilation in the ED to be greater than 3 hours.5 Such a length of time on mechanical ventilation in this setting can have significant effects on the course of illness; however, it is not clear whether mechanical ventilation performed in the ED typically conforms to evidence-based standards. In one study performed in an academic center, less than one-third of patients with sepsis and respiratory failure received low-volume ventilation in the ED.6 Another study suggested that emergency medicine residents may not receive as much dedicated education on the initial management of ventilators as needed—despite the potentially unforgiving physiologic process of positive-pressure mechanical ventilation.7
The fundamental principles required to safely manage most patients in respiratory failure are not difficult to master. There are several simple evidence-based ventilator strategies for managing patients with respiratory failure. The three primary principles of initiating and providing effective mechanical ventilation are: (1) avoiding traumatic ventilation; (2) maintaining normoxia; and (3) maintaining appropriate acid-base balance. Each of these principles can be achieved in a stepwise fashion.
Step I: Establishing Lung-Protective Settings on the Ventilator
Three central parameters must be selected at the initiation of assist-control mechanical ventilation: TV, respiratory rate (RR), and positive end-expiratory pressure (PEEP). These parameters have been extensively studied, and there is excellent evidence to guide the EP in choosing the correct settings.
Tidal Volume. Although the normal human lung can accommodate about 6 L of air, in cases of respiratory failure, the surface area available for gas exchange is significantly reduced due to a pathologic process undermining entire regions of the air-blood interface. Consequently, a person whose normal lungs are suddenly required to perform the life-sustaining gas exchanges in critical illness with the much smaller lung surface is at a significant disadvantage.
The widely accepted lung-protective volumes range from 6 to 8 mL/kg of predicted body weight (PBW), a height-based calculation.8 For example, in a 6-foot tall man, 6 mL/kg of PBW amounts to a TV of 466 mL; in a 5-foot tall woman, the same amount of PBW amounts to a TV of 273 mL. Volumes may be referenced using PBW tables from the NHLBI ARDS network or by employing the following equations:
Adult men: PBW (kg) = 50 + 2.3 (height [in] – 60)
Adult women: PBW (kg) = 45.5 + 2.3 (height [in] – 60).9
Respiratory Rate. The RR should be set somewhat higher than normal because the TV per breath has been slightly reduced, and also because sick patients in a catabolic state may have larger minute ventilations than they would when healthy. As previously described, since the TV is restricted, RR is the most mobile parameter in maintaining appropriate minute ventilation. Minute ventilation (MV) is the product of RR multiplied by TV (MV = RR x TV), and this should be calculated to approximate the patient’s own efforts, which are dependent upon the clinical circumstances. For example, patients whose bodies are trying to compensate for an acidosis will require much higher rates than those who are simply obtunded and intubated for airway protection. In other words, in order to remove carbon dioxide (CO2) in an acidemic patient, a higher RR rate may be required, whereas a lower rate may be selected to compensate for alkalemia while maintaining appropriate oxygen (O2) levels in both cases.10
Positive End-Expiratory Pressure. Previous recommendations for ventilation in respiratory failure called for large TVs (ie, 10 to 15 mL/kg), partly out of concern that smaller volumes would promote distal airway collapse, thereby increasing the amount of lung that received blood but not air, consequently worsening overall oxygenation.11 Although administering such large volumes has clearly proved harmful, the valid concern about distal airway collapse can be addressed in part by adjustments to PEEP, which acts to “stent” open airways after most of the tidal breath has left the airways.
Positive end-expiratory pressure, however, is not without risks.12 Blood from the rest of the body will encounter resistance returning to a thoracic cavity persistently inflated by positive pressure, and this decrease in preload may contribute to hypotension. Similarly, a weak right ventricle may struggle to push blood into the compressed pulmonary vasculature, increasing the cardiac workload and further compromising hemodynamics.13 In general, PEEP should be set as low as the maintenance of adequate oxygenation permits. The NHLBI ARDS guidelines provide a table on balancing PEEP and the fraction of inspired O2 (FiO2), as well as hypotension, in refractory hypoxemic patients—with the limitation on PEEP set by the patients’ pulmonary compliance (plateau pressures, discussed next).8
After making these selections, several parameters must be monitored closely. Those most relevant to lung-protective ventilation are the peak airway pressure and, most importantly, the plateau pressure. Numerous animal studies now demonstrate serious lung injury in both healthy and diseased lungs from high peak pressures (defined as a plateau pressure >30 cm water [H2O]).14,15 A high-pressure alarm sounding on the ventilator must be promptly addressed by an evaluation for easily reversible causes, such as tube obstruction, pneumothorax, breath stacking, pulmonary edema, or pleural effusions. A full discussion of the causes of elevated peak and plateau pressures is beyond the scope of this review, but if the plateau pressures remain consistently high, a reduction in TV may be necessary.
Step II: Maintaining Normoxia
As a severely hypoxic patient will rapidly decompensate with progression to death, a host of monitoring devices are used to alert the nurse or physician that O2 levels have fallen below the normal range. Strategies to manage refractory hypoxia in the ventilated patient are complex. For most patients, 100% FiO2 is initiated immediately after intubation to increase the safety of the procedure, but there is animal evidence that high O2 levels promote inflammatory responses, and human data suggest hyperoxia can be deleterious to long-term outcomes, particularly following cardiac arrest and stroke.16,17 A persistent O2 saturation of 100% on pulse oximetry or a supraphysiologic partial pressure of O2 (PaO2) on an arterial blood gas (defined as >200 mm Hg) may actually cause the patient more harm than good. Therefore, the fraction of inspired O2 should be titrated to maintain normoxia. The ARDS protocol, for example, targets an O2 saturation of 88% to 95% and a PaO2 of 55 to 80 mm Hg.8
Step III: Maintaining Acid-Base Balance
The basic principles of acid-base physiology should be familiar to EPs. When a patient is sedated and the airway secured, the primary means by which blood pH is maintained is now in the hands of the intubating physician. Patients with respiratory failure may have compensated for a preexisting derangement in their blood pH. If the preexisting condition is not recognized and ventilator settings are not maintained appropriately, they may be vulnerable to developing another derangement. Even on settings that allow the patient to breathe over a set rate, the sedation required to tolerate an endotracheal tube may cause significant respiratory depression, making it impossible for the patient to auto-regulate the respiratory component of acid-base homeostasis (ie, by hyperventilation).
As in the discussion of RR, TVs are “fixed” based on low-TV lung-protective ventilation. Therefore, changing the patient’s set RR is the easiest method to adjust the partial pressure of CO2 (PaCO2), and consequently address any respiratory acidosis. An increase in the RR will increase the patient’s minute ventilation, leading to a decrease in serum PaCO2 levels, whereas a decrease in the RR will have the converse effect. It is important to obtain an arterial blood-gas reading shortly after intubation and to continue to monitor the impact of any ventilator titrations on the patient’s acid-base status.
Studies of “permissive hypercapnia” in ARDS patients have shown that prioritizing lung-protective ventilator settings, even at the expense of a normal CO2, reduce mortality.1,18 Even in situations where it is not necessary to maintain hypercapnia for lung-protective settings, the hypercapnia appears to have beneficial effects.19-21 No upper limits on hypercapnia have been established, and even extreme levels have been associated with successful patient outcomes.22 However, a study by Hickling et al23 demonstrated that an initial trial of lung-protective ventilation demonstrated benefit from unbuffered hypercarbia and acidosis, reporting an average CO2 level of 66 and a pH of 7. These guidelines should be appropriate for use in the ED.
In summary, assuming control of a patient’s respiratory system—with its nuanced and responsive role in acid-base, oxygenation, and cardiopulmonary hemodynamics—is one of the most difficult situations routinely encountered by an EP. While the procedure itself may be life-saving, the next several hours can have significant impact on the patient’s long-term outcome.
Treating Sepsis and Surviving Sepsis: Recommendations Versus the ARISE/ProCESS Trials
Sepsis and Septic Shock
Sepsis is defined as an infection plus systemic inflammatory response syndrome (SIRS). Severe sepsis is sepsis plus sepsis-induced organ dysfunction or tissue hypoperfusion resulting in or caused by lactic acidosis, acute lung injury, altered mental status, or coagulation abnormalities. Septic shock refers to persistent sepsis-induced hypotension despite adequate fluid resuscitation.24 The ambiguity of these definitions may invariably lead to a practitioner’s underappreciation or misconception of the importance of sepsis.
Sepsis is one of the most common, yet least-recognized, entities. In the United States, it is estimated that 3 in 1,000 people annually are affected by sepsis, and every few seconds, a person dies of sepsis.25 Both numbers underestimate the effects on the elderly. Clinical manifestations of sepsis vary, and the condition may originate from both community-acquired and healthcare-associated sources.
In 2001, a landmark study demonstrated that early goal-directed therapy (EGDT) reduced mortality and improved patient outcomes in patients presenting to the ED in severe sepsis.26 The estimated 12% to 16% reduction in mortality reported in this trial began an initiative to broaden the scope and awareness of sepsis.
Current Literature and Evidence-Based Guidelines
The most recent guidelines for the management of septic shock from the Surviving Sepsis Campaign are summarized in Table 1. With its last revision, the Surviving Sepsis guidelines of 2012 has two main management foci—initiating treatment within the first 3 and the first 6 hours after recognition within the first 3 hours and those within the first 6 hours after sepsis recognition (Table 2). Within the first 3 hours, the treatment team should draw a serum lactate level; obtain cultures prior to the administration of antibiotics; initiate broad-spectrum antibiotics as early as possible; and administer 20 to 30 mL/kg of crystalloid fluids in patients with hypotension or a lactate level greater than 4 mmol/L. Within the first 6 hours, the clinician should administer intravenous (IV) vasopressors, preferentially norepinephrine, for persistent hypotension after a fluid challenge to maintain a mean arterial pressure >65 mm Hg; place a supra-diaphragmatic central venous catheter to measure a serum mixed venous O2 saturation (ScvO2) and central venous pressure (CVP); and measure serial serum lactate levels if they were initially elevated (lactate ≥4 mmol/L [36 mg/dL]).24,30,31 The targets for ScvO2 and CVP are ≥70%, and >8 mm Hg, respectively.
Summary
Sepsis is a prevalent ED presentation associated with mortality that can present in a complex fashion. Early recognition and management is essential and can be condensed into a few key recommendations. Becoming familiar with and incorporating these recommendations into daily practice will enable EPs to deliver quality care to every patient presenting with sepsis, and will also reduce mortality.
Blood Pressure Management for Select Neurological Emergencies
Patients with ischemic stroke, spontaneous intracerebral hemorrhage (ICH), and aneurysmal subarachnoid hemorrhage (SAH) often present with elevated blood pressures (BPs).34-36 In caring for these patients, EPs face the question of how, or even if, the patient’s BP should be managed. What are the appropriate BP targets for each of the aforementioned pathologies? Does aggressive BP management benefit or harm the patient?
Background
The relationship between hypertension and stroke is different for each stroke type. Retrospective data show a U-shaped relationship between BP and mortality in ischemic stroke, with the highest mortality observed at both extremes of the BP curve.34 Data also suggest increased mortality when ICH is accompanied by hypertension.35 Hypertension may also be associated with a higher risk of rebleeding in patients with SAH due to aneurysms.36 Because of the variable relationship between stroke and hypertension, therapeutic recommendations for each type of stroke can be confusing.
Current Literature and Evidence-Based Guidelines
Firm evidence to make therapeutic recommendations remains elusive. The recent American Heart Association (AHA) guidelines covering ischemic stroke, ICH, and SAH were published between late 2010 and early 2013, and several trials investigating the role of BP control in ischemic and hemorrhagic stroke have subsequently been published.37-41
When the Cochrane Collaboration updated its systematic review on vasoactive medications in stroke in 2014 to include recent evidence,42 it ultimately concluded that lowering BP does not improve mortality, neurological deterioration, or quality of life regardless of stroke type, and suggest that further investigations should be undertaken.9 However, the Cochrane authors noted that two recent trials showed a statistically significant association between improved quality of life and BP reduction within 6 hours of stroke onset.38-39 Although the data were compiled from just 2,835 patients of the 15,432 included in the entire Cochrane review, it suggested that interventions initiated in the ED may contribute to any potential beneficial outcomes from intensive BP control.
Ischemic Stroke
The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) investigated the initiation of BP-control measures within 48 hours of onset of ischemic stroke in approximately 4,000 patients and found no significant difference in death or disability between the group that received BP-control interventions and the group that did not.37 The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT) included patients with both ischemic and hemorrhagic strokes. Though it studied only 41 patients, this trial suggests that early BP control is safe and may be associated with lower disability.38 These findings are bolstered by the more recent Efficacy of Nitric Oxide in Stroke (ENOS) trial showing a similar safety profile for BP control in both ischemic and hemorrhagic strokes, though the mean difference in systolic BP after therapy was a mere 7 mm Hg.40 The combined data from the RIGHT and ENOS trials offer little to clarify the question of appropriate BP control.
For now, the EP is left with the AHA/American Stroke Association (ASA) guideline’s recommendation “not to lower the BP during the initial 24 hours of acute ischemic stroke unless the BP is greater than 220/120 mm Hg.”34 The recommendation differs in cases when a patient receives thrombolytics and hemorrhagic transformation is a risk. There have been no new data to change the AHA/ASA’s recommendations for patients receiving thrombolytics. In such cases, the EP should ensure the patient’s BP is below 185/110 mm Hg prior to thrombolytic administration and below 180/105 mm Hg during therapy.34 A variety of agents is available to lower BP in this situation, and includes IV labetalol, nicardipine, esmolol, and others.
Intracerebral Hemorrhage
The recent literature on blood pressure control in ICH has also increased since the most recent AHA/ASA recommendations. The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2 included over 2,800 patients randomized to intensive early therapy to reduce BP to less than 140 mm Hg or less than 180 mm Hg and found no significant difference in mortality or safety between the two groups, though intensive therapy was associated with less disability.39 The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial (ICH-ADAPT) trial further clarified the issue of safety during intensive BP control by showing no decrease in perihematomal cerebral blood flow in patients whose BP control was targeted to less than 150 mm Hg compared to those whose BP was less than 180 mm Hg, suggesting that aggressive BP reduction does not cause iatrogenic ischemic stroke.41
These combined data suggest that intensive BP management is safe for patients with ICH, providing reassurance for the AHA/ASA guideline recommendation that “in patients…with a systolic BP of 150 to 220 mm Hg, acute lowering of systolic BP to 140 mm Hg is probably safe.”35 Whether this improves patient outcomes remains unclear. Again, multiple agents are available for BP control, including IV labetalol or nicardipine, with no agent identified as superior in producing better patient outcomes. A continuous infusion is recommended if several boluses are ineffective in achieving and maintaining the target BP, as BP variability has been associated with poorer outcomes.43
Subarachnoid Hemorrhage
There are no large recent studies in the literature on antihypertensive therapy in SAH. The AHA/ASA guidelines updated in 2012 reflect the consensus that elevated BPs are associated with increased risk of aneurysmal rebleeding and thus poorer patient-oriented outcomes. The consensus remains to use a titratable agent to target a systolic BP less than 160 mm Hg until definitive neurosurgical therapy, such as aneurysmal coiling or clipping.36 Given the variability of the sodium nitroprusside dose-response relationship, IV labetalol, and nicardipine, are recommended agents for continuous control, though data showing differences in mortality and/or disability are lacking.36 Again, retrospective data suggest that BP variability negatively impacts mortality and disability, so consider early initiation of continuous infusions to achieve and maintain consistency in the chosen target.44
Summary
Pressors in the Management of Hypotension
Norepinephrine
Norepinephrine is one of the most commonly used agents for shock in the ED, with indications spanning multiple etiologies. It is an endogenous neurotransmitter that works predominantly on a1 receptors as well as exerting some modest effects on b1 and b2 receptors, for combined vasopressor and improved cardiac contractility effect.46-47 Norepinephrine is currently the recommended initial agent for sepsis-induced tissue hypoperfusion.24 However, a recent Cochrane systematic review and meta-analysis supports evidence of limited differences among various pressors.48 Several comparative randomized control trials show norepinephrine is as effective as other agents, but with fewer side effects.24,49 With the ease and familiarity of its use by most EPs, and a wide therapeutic index for targeted effect versus arrhythmias, norepinephrine is a reasonable choice as the initial pressor in managing a wide variety of shock syndromes.
Vasopressin
Another commonly used agent in the treatment of shock, vasopressin is an analogue of the antidiuretic hormone secreted from the posterior pituitary gland, exerting its CV effects primarily as a vasoconstrictor by increasing intracellular calcium.50 Vasopressin doses are 0.03 or 0.04 U/min IV without titration.24,50 Early studies of septic patients demonstrated a relative deficiency of serum vasopressin levels, leading clinicians to utilize it in the treatment of sepsis-induced shock. However, the Vasopressin and Septic Shock Trial (VASST) trial demonstrated that the addition of vasopressin to norepinephrine did not produce any improvements in morbidity or mortality compared with norepinephrine alone.51 Despite these findings, vasopressin is still commonly used as a secondary agent to correct continued hypotension. Vasopressin may be appropriate for patients who specifically require peripheral vasoconstriction in the setting of good cardiac output and volume status, ability to tolerate increases in afterload, or in patients at risk for dysrhythmias.
Dopamine
Dopamine had been previously recommended as the initial choice of pharmacologic support for the management of shock.24,52-54 Dopamine is an adrenergic agonist agent that works via a1 and b1 receptors as well as a precursor to the synthesis of norepinephrine and epinephrine.55 There are dose-dependent effects on various receptors from escalating amounts administered,55-56 but the literature does not support the concept of “renal-dose” dopamine.57-59 A study by DeBaker et al49 suggested no difference in efficacy between dopamine and norepinephrine, but demonstrated a greater tendency toward cardiac dysrhythmias with dopamine. For these reasons noted above, norepinephrine may be the initial agent for pharmaceutical support of shock, particularly in septic syndromes, with dopamine as a secondary or adjunct agent in patients at low risk for tachyarrhythmia or a relative bradycardia. 24, 56
Dobutamine
Dobutamine is another adrenergic agonist that is similar to dopamine but with a greater effect on inotropic cardiac contractility due to a preferential action at b1 receptors.60 It can potentially induce peripheral vasodilatation due to its effect on arterial b1 receptors. Given this balance, dobutamine is an agent that should be utilized for cardiogenic shock when increased contractility is needed. These effects are particularly useful in patients with “wet and cold” heart failure who have a low cardiac output and volume-overloaded status.61, 62 However, it may be necessary to add another agent to provide additional peripheral vasoconstriction should the use of dobutamine affect lead to excessive vasodilatation.
Epinephrine
One of the most powerful vasoactive agents, epinephrine has a high affinity for all b1, b2 and a1 receptors.63 These combined effects lead to increased cardiac output and improved BP by increasing cardiac contractility and peripheral vasoconstriction. The effect of epinephrine in limiting mast cell release of histamine makes it the preferred choice for the treatment of anaphylaxis.64 However, side effects of epinephrine include hypertension, tachydysrhythmias, tissue ischemia from vigorous vasoconstriction, and induced lactic acidosis.63
Phenylephrine
Phenylephrine is an a-adrenergic agonist that activates a1 receptors on arteriole smooth muscle, resulting in vasoconstriction.65 It is currently recommended only for hypotension related to procedural sedation.47 Phenylephrine is not recommended for treating patients with septic shock, except when there are concerns about tachydysrhythmias; persistent hypotension with a high cardiac output after treatment with other vasoconstrictor and inotropic drugs; or when a “pure” vasoconstrictor may be preferred.24,56,65
Summary
Although there are many other vasoactive agents that can be used, the selected agents discussed above represent those most commonly used in the ED. All demonstrate significant crossover effects and receptor activation, as well as impact on cardiac contractility and vasoconstriction. The suggested specific indications for each agent are based on current evidenced-based medicine, clinical guidelines, and theoretical benefits on clinical scenarios. But, as always, clinical decisions should be individualized for critically ill patients.
Conclusion
The resuscitation and initiation of care for critically ill patients must typically be immediately upon their arrival in the ED. While general guidelines or recommendations exist for commonly encountered pathologies, treatment should always be patient-centered, based on the needs and nuances unique to each patient in this vulnerable population. The initiation of mechanical ventilation, treatment of sepsis, management of hypertensive neurosurgical emergencies, and use of pressors in shock states are among the most critically important tasks an EP is called upon to perform. This review of current evidence-based guidelines and recommendations will help EPs provide the appropriate and unique care each patient requires.
Dr Brubaker is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Yu is a fellow of adult critical care medicine – emergency medicine in the department of critical care medicine, University of Pittsburgh Medical Center, Pennsylvania. Dr Goodmanson is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Schott is an assistant professor, department of emergency medicine and critical care medicine; assistant director of ultrasonography; director, critical care elective student rotation; and director, point of care ultrasound elective student rotation, at the University of Pittsburgh, Pennsylvania
Emergency medicine and critical care medicine share a responsibility for the care of acutely ill patients with life-threatening pathologies. The skills required of both emergency physicians (EPs) and critical care specialists to recognize, diagnose, and resuscitate such patients have resulted in many shared guidelines, recommendations, and publications. When critically ill patients enter the hospital through the ED, the care provided by EPs greatly impacts both the early and long-term outcomes. It is not uncommon for critically ill patients to spend several hours under the care of an EP while awaiting an available inpatient bed in the intensive care unit (ICU) or “step down” monitored unit.
This article provides a summary review of current guidelines, evidence-based medicine recommendations, and the results of recent trials involving ventilator management, treatment of sepsis, management of hypertension accompanying neurological emergencies, and the selection of pressors for the treatment of different shock states.
Ventilator Management
Mechanical ventilation is frequently undertaken in the ED for patients with respiratory failure—the origin of which is not always immediately clear. Data from the National Heart, Lung, and Blood Institute’s (NHLBI) acute respiratory distress syndrome (ARDS) clinical network (http://www.ardsnet.org) and other clinical trials have established the benefit of low tidal-volume, “lung-protective” ventilation in the patient with ARDS.1,2 Numerous studies have also shown the benefit of low-tidal-volume (TV), ventilation in patients without ARDS, and its use is now the standard of care for a large range of respiratory conditions causing compromise.3
The prompt initiation of lung-protective ventilation has a significant impact on reducing ICU mortality.4 A recent retrospective review of 3.5 million ED visits showed the median length of stay for patients started on mechanical ventilation in the ED to be greater than 3 hours.5 Such a length of time on mechanical ventilation in this setting can have significant effects on the course of illness; however, it is not clear whether mechanical ventilation performed in the ED typically conforms to evidence-based standards. In one study performed in an academic center, less than one-third of patients with sepsis and respiratory failure received low-volume ventilation in the ED.6 Another study suggested that emergency medicine residents may not receive as much dedicated education on the initial management of ventilators as needed—despite the potentially unforgiving physiologic process of positive-pressure mechanical ventilation.7
The fundamental principles required to safely manage most patients in respiratory failure are not difficult to master. There are several simple evidence-based ventilator strategies for managing patients with respiratory failure. The three primary principles of initiating and providing effective mechanical ventilation are: (1) avoiding traumatic ventilation; (2) maintaining normoxia; and (3) maintaining appropriate acid-base balance. Each of these principles can be achieved in a stepwise fashion.
Step I: Establishing Lung-Protective Settings on the Ventilator
Three central parameters must be selected at the initiation of assist-control mechanical ventilation: TV, respiratory rate (RR), and positive end-expiratory pressure (PEEP). These parameters have been extensively studied, and there is excellent evidence to guide the EP in choosing the correct settings.
Tidal Volume. Although the normal human lung can accommodate about 6 L of air, in cases of respiratory failure, the surface area available for gas exchange is significantly reduced due to a pathologic process undermining entire regions of the air-blood interface. Consequently, a person whose normal lungs are suddenly required to perform the life-sustaining gas exchanges in critical illness with the much smaller lung surface is at a significant disadvantage.
The widely accepted lung-protective volumes range from 6 to 8 mL/kg of predicted body weight (PBW), a height-based calculation.8 For example, in a 6-foot tall man, 6 mL/kg of PBW amounts to a TV of 466 mL; in a 5-foot tall woman, the same amount of PBW amounts to a TV of 273 mL. Volumes may be referenced using PBW tables from the NHLBI ARDS network or by employing the following equations:
Adult men: PBW (kg) = 50 + 2.3 (height [in] – 60)
Adult women: PBW (kg) = 45.5 + 2.3 (height [in] – 60).9
Respiratory Rate. The RR should be set somewhat higher than normal because the TV per breath has been slightly reduced, and also because sick patients in a catabolic state may have larger minute ventilations than they would when healthy. As previously described, since the TV is restricted, RR is the most mobile parameter in maintaining appropriate minute ventilation. Minute ventilation (MV) is the product of RR multiplied by TV (MV = RR x TV), and this should be calculated to approximate the patient’s own efforts, which are dependent upon the clinical circumstances. For example, patients whose bodies are trying to compensate for an acidosis will require much higher rates than those who are simply obtunded and intubated for airway protection. In other words, in order to remove carbon dioxide (CO2) in an acidemic patient, a higher RR rate may be required, whereas a lower rate may be selected to compensate for alkalemia while maintaining appropriate oxygen (O2) levels in both cases.10
Positive End-Expiratory Pressure. Previous recommendations for ventilation in respiratory failure called for large TVs (ie, 10 to 15 mL/kg), partly out of concern that smaller volumes would promote distal airway collapse, thereby increasing the amount of lung that received blood but not air, consequently worsening overall oxygenation.11 Although administering such large volumes has clearly proved harmful, the valid concern about distal airway collapse can be addressed in part by adjustments to PEEP, which acts to “stent” open airways after most of the tidal breath has left the airways.
Positive end-expiratory pressure, however, is not without risks.12 Blood from the rest of the body will encounter resistance returning to a thoracic cavity persistently inflated by positive pressure, and this decrease in preload may contribute to hypotension. Similarly, a weak right ventricle may struggle to push blood into the compressed pulmonary vasculature, increasing the cardiac workload and further compromising hemodynamics.13 In general, PEEP should be set as low as the maintenance of adequate oxygenation permits. The NHLBI ARDS guidelines provide a table on balancing PEEP and the fraction of inspired O2 (FiO2), as well as hypotension, in refractory hypoxemic patients—with the limitation on PEEP set by the patients’ pulmonary compliance (plateau pressures, discussed next).8
After making these selections, several parameters must be monitored closely. Those most relevant to lung-protective ventilation are the peak airway pressure and, most importantly, the plateau pressure. Numerous animal studies now demonstrate serious lung injury in both healthy and diseased lungs from high peak pressures (defined as a plateau pressure >30 cm water [H2O]).14,15 A high-pressure alarm sounding on the ventilator must be promptly addressed by an evaluation for easily reversible causes, such as tube obstruction, pneumothorax, breath stacking, pulmonary edema, or pleural effusions. A full discussion of the causes of elevated peak and plateau pressures is beyond the scope of this review, but if the plateau pressures remain consistently high, a reduction in TV may be necessary.
Step II: Maintaining Normoxia
As a severely hypoxic patient will rapidly decompensate with progression to death, a host of monitoring devices are used to alert the nurse or physician that O2 levels have fallen below the normal range. Strategies to manage refractory hypoxia in the ventilated patient are complex. For most patients, 100% FiO2 is initiated immediately after intubation to increase the safety of the procedure, but there is animal evidence that high O2 levels promote inflammatory responses, and human data suggest hyperoxia can be deleterious to long-term outcomes, particularly following cardiac arrest and stroke.16,17 A persistent O2 saturation of 100% on pulse oximetry or a supraphysiologic partial pressure of O2 (PaO2) on an arterial blood gas (defined as >200 mm Hg) may actually cause the patient more harm than good. Therefore, the fraction of inspired O2 should be titrated to maintain normoxia. The ARDS protocol, for example, targets an O2 saturation of 88% to 95% and a PaO2 of 55 to 80 mm Hg.8
Step III: Maintaining Acid-Base Balance
The basic principles of acid-base physiology should be familiar to EPs. When a patient is sedated and the airway secured, the primary means by which blood pH is maintained is now in the hands of the intubating physician. Patients with respiratory failure may have compensated for a preexisting derangement in their blood pH. If the preexisting condition is not recognized and ventilator settings are not maintained appropriately, they may be vulnerable to developing another derangement. Even on settings that allow the patient to breathe over a set rate, the sedation required to tolerate an endotracheal tube may cause significant respiratory depression, making it impossible for the patient to auto-regulate the respiratory component of acid-base homeostasis (ie, by hyperventilation).
As in the discussion of RR, TVs are “fixed” based on low-TV lung-protective ventilation. Therefore, changing the patient’s set RR is the easiest method to adjust the partial pressure of CO2 (PaCO2), and consequently address any respiratory acidosis. An increase in the RR will increase the patient’s minute ventilation, leading to a decrease in serum PaCO2 levels, whereas a decrease in the RR will have the converse effect. It is important to obtain an arterial blood-gas reading shortly after intubation and to continue to monitor the impact of any ventilator titrations on the patient’s acid-base status.
Studies of “permissive hypercapnia” in ARDS patients have shown that prioritizing lung-protective ventilator settings, even at the expense of a normal CO2, reduce mortality.1,18 Even in situations where it is not necessary to maintain hypercapnia for lung-protective settings, the hypercapnia appears to have beneficial effects.19-21 No upper limits on hypercapnia have been established, and even extreme levels have been associated with successful patient outcomes.22 However, a study by Hickling et al23 demonstrated that an initial trial of lung-protective ventilation demonstrated benefit from unbuffered hypercarbia and acidosis, reporting an average CO2 level of 66 and a pH of 7. These guidelines should be appropriate for use in the ED.
In summary, assuming control of a patient’s respiratory system—with its nuanced and responsive role in acid-base, oxygenation, and cardiopulmonary hemodynamics—is one of the most difficult situations routinely encountered by an EP. While the procedure itself may be life-saving, the next several hours can have significant impact on the patient’s long-term outcome.
Treating Sepsis and Surviving Sepsis: Recommendations Versus the ARISE/ProCESS Trials
Sepsis and Septic Shock
Sepsis is defined as an infection plus systemic inflammatory response syndrome (SIRS). Severe sepsis is sepsis plus sepsis-induced organ dysfunction or tissue hypoperfusion resulting in or caused by lactic acidosis, acute lung injury, altered mental status, or coagulation abnormalities. Septic shock refers to persistent sepsis-induced hypotension despite adequate fluid resuscitation.24 The ambiguity of these definitions may invariably lead to a practitioner’s underappreciation or misconception of the importance of sepsis.
Sepsis is one of the most common, yet least-recognized, entities. In the United States, it is estimated that 3 in 1,000 people annually are affected by sepsis, and every few seconds, a person dies of sepsis.25 Both numbers underestimate the effects on the elderly. Clinical manifestations of sepsis vary, and the condition may originate from both community-acquired and healthcare-associated sources.
In 2001, a landmark study demonstrated that early goal-directed therapy (EGDT) reduced mortality and improved patient outcomes in patients presenting to the ED in severe sepsis.26 The estimated 12% to 16% reduction in mortality reported in this trial began an initiative to broaden the scope and awareness of sepsis.
Current Literature and Evidence-Based Guidelines
The most recent guidelines for the management of septic shock from the Surviving Sepsis Campaign are summarized in Table 1. With its last revision, the Surviving Sepsis guidelines of 2012 has two main management foci—initiating treatment within the first 3 and the first 6 hours after recognition within the first 3 hours and those within the first 6 hours after sepsis recognition (Table 2). Within the first 3 hours, the treatment team should draw a serum lactate level; obtain cultures prior to the administration of antibiotics; initiate broad-spectrum antibiotics as early as possible; and administer 20 to 30 mL/kg of crystalloid fluids in patients with hypotension or a lactate level greater than 4 mmol/L. Within the first 6 hours, the clinician should administer intravenous (IV) vasopressors, preferentially norepinephrine, for persistent hypotension after a fluid challenge to maintain a mean arterial pressure >65 mm Hg; place a supra-diaphragmatic central venous catheter to measure a serum mixed venous O2 saturation (ScvO2) and central venous pressure (CVP); and measure serial serum lactate levels if they were initially elevated (lactate ≥4 mmol/L [36 mg/dL]).24,30,31 The targets for ScvO2 and CVP are ≥70%, and >8 mm Hg, respectively.
Summary
Sepsis is a prevalent ED presentation associated with mortality that can present in a complex fashion. Early recognition and management is essential and can be condensed into a few key recommendations. Becoming familiar with and incorporating these recommendations into daily practice will enable EPs to deliver quality care to every patient presenting with sepsis, and will also reduce mortality.
Blood Pressure Management for Select Neurological Emergencies
Patients with ischemic stroke, spontaneous intracerebral hemorrhage (ICH), and aneurysmal subarachnoid hemorrhage (SAH) often present with elevated blood pressures (BPs).34-36 In caring for these patients, EPs face the question of how, or even if, the patient’s BP should be managed. What are the appropriate BP targets for each of the aforementioned pathologies? Does aggressive BP management benefit or harm the patient?
Background
The relationship between hypertension and stroke is different for each stroke type. Retrospective data show a U-shaped relationship between BP and mortality in ischemic stroke, with the highest mortality observed at both extremes of the BP curve.34 Data also suggest increased mortality when ICH is accompanied by hypertension.35 Hypertension may also be associated with a higher risk of rebleeding in patients with SAH due to aneurysms.36 Because of the variable relationship between stroke and hypertension, therapeutic recommendations for each type of stroke can be confusing.
Current Literature and Evidence-Based Guidelines
Firm evidence to make therapeutic recommendations remains elusive. The recent American Heart Association (AHA) guidelines covering ischemic stroke, ICH, and SAH were published between late 2010 and early 2013, and several trials investigating the role of BP control in ischemic and hemorrhagic stroke have subsequently been published.37-41
When the Cochrane Collaboration updated its systematic review on vasoactive medications in stroke in 2014 to include recent evidence,42 it ultimately concluded that lowering BP does not improve mortality, neurological deterioration, or quality of life regardless of stroke type, and suggest that further investigations should be undertaken.9 However, the Cochrane authors noted that two recent trials showed a statistically significant association between improved quality of life and BP reduction within 6 hours of stroke onset.38-39 Although the data were compiled from just 2,835 patients of the 15,432 included in the entire Cochrane review, it suggested that interventions initiated in the ED may contribute to any potential beneficial outcomes from intensive BP control.
Ischemic Stroke
The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) investigated the initiation of BP-control measures within 48 hours of onset of ischemic stroke in approximately 4,000 patients and found no significant difference in death or disability between the group that received BP-control interventions and the group that did not.37 The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT) included patients with both ischemic and hemorrhagic strokes. Though it studied only 41 patients, this trial suggests that early BP control is safe and may be associated with lower disability.38 These findings are bolstered by the more recent Efficacy of Nitric Oxide in Stroke (ENOS) trial showing a similar safety profile for BP control in both ischemic and hemorrhagic strokes, though the mean difference in systolic BP after therapy was a mere 7 mm Hg.40 The combined data from the RIGHT and ENOS trials offer little to clarify the question of appropriate BP control.
For now, the EP is left with the AHA/American Stroke Association (ASA) guideline’s recommendation “not to lower the BP during the initial 24 hours of acute ischemic stroke unless the BP is greater than 220/120 mm Hg.”34 The recommendation differs in cases when a patient receives thrombolytics and hemorrhagic transformation is a risk. There have been no new data to change the AHA/ASA’s recommendations for patients receiving thrombolytics. In such cases, the EP should ensure the patient’s BP is below 185/110 mm Hg prior to thrombolytic administration and below 180/105 mm Hg during therapy.34 A variety of agents is available to lower BP in this situation, and includes IV labetalol, nicardipine, esmolol, and others.
Intracerebral Hemorrhage
The recent literature on blood pressure control in ICH has also increased since the most recent AHA/ASA recommendations. The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2 included over 2,800 patients randomized to intensive early therapy to reduce BP to less than 140 mm Hg or less than 180 mm Hg and found no significant difference in mortality or safety between the two groups, though intensive therapy was associated with less disability.39 The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial (ICH-ADAPT) trial further clarified the issue of safety during intensive BP control by showing no decrease in perihematomal cerebral blood flow in patients whose BP control was targeted to less than 150 mm Hg compared to those whose BP was less than 180 mm Hg, suggesting that aggressive BP reduction does not cause iatrogenic ischemic stroke.41
These combined data suggest that intensive BP management is safe for patients with ICH, providing reassurance for the AHA/ASA guideline recommendation that “in patients…with a systolic BP of 150 to 220 mm Hg, acute lowering of systolic BP to 140 mm Hg is probably safe.”35 Whether this improves patient outcomes remains unclear. Again, multiple agents are available for BP control, including IV labetalol or nicardipine, with no agent identified as superior in producing better patient outcomes. A continuous infusion is recommended if several boluses are ineffective in achieving and maintaining the target BP, as BP variability has been associated with poorer outcomes.43
Subarachnoid Hemorrhage
There are no large recent studies in the literature on antihypertensive therapy in SAH. The AHA/ASA guidelines updated in 2012 reflect the consensus that elevated BPs are associated with increased risk of aneurysmal rebleeding and thus poorer patient-oriented outcomes. The consensus remains to use a titratable agent to target a systolic BP less than 160 mm Hg until definitive neurosurgical therapy, such as aneurysmal coiling or clipping.36 Given the variability of the sodium nitroprusside dose-response relationship, IV labetalol, and nicardipine, are recommended agents for continuous control, though data showing differences in mortality and/or disability are lacking.36 Again, retrospective data suggest that BP variability negatively impacts mortality and disability, so consider early initiation of continuous infusions to achieve and maintain consistency in the chosen target.44
Summary
Pressors in the Management of Hypotension
Norepinephrine
Norepinephrine is one of the most commonly used agents for shock in the ED, with indications spanning multiple etiologies. It is an endogenous neurotransmitter that works predominantly on a1 receptors as well as exerting some modest effects on b1 and b2 receptors, for combined vasopressor and improved cardiac contractility effect.46-47 Norepinephrine is currently the recommended initial agent for sepsis-induced tissue hypoperfusion.24 However, a recent Cochrane systematic review and meta-analysis supports evidence of limited differences among various pressors.48 Several comparative randomized control trials show norepinephrine is as effective as other agents, but with fewer side effects.24,49 With the ease and familiarity of its use by most EPs, and a wide therapeutic index for targeted effect versus arrhythmias, norepinephrine is a reasonable choice as the initial pressor in managing a wide variety of shock syndromes.
Vasopressin
Another commonly used agent in the treatment of shock, vasopressin is an analogue of the antidiuretic hormone secreted from the posterior pituitary gland, exerting its CV effects primarily as a vasoconstrictor by increasing intracellular calcium.50 Vasopressin doses are 0.03 or 0.04 U/min IV without titration.24,50 Early studies of septic patients demonstrated a relative deficiency of serum vasopressin levels, leading clinicians to utilize it in the treatment of sepsis-induced shock. However, the Vasopressin and Septic Shock Trial (VASST) trial demonstrated that the addition of vasopressin to norepinephrine did not produce any improvements in morbidity or mortality compared with norepinephrine alone.51 Despite these findings, vasopressin is still commonly used as a secondary agent to correct continued hypotension. Vasopressin may be appropriate for patients who specifically require peripheral vasoconstriction in the setting of good cardiac output and volume status, ability to tolerate increases in afterload, or in patients at risk for dysrhythmias.
Dopamine
Dopamine had been previously recommended as the initial choice of pharmacologic support for the management of shock.24,52-54 Dopamine is an adrenergic agonist agent that works via a1 and b1 receptors as well as a precursor to the synthesis of norepinephrine and epinephrine.55 There are dose-dependent effects on various receptors from escalating amounts administered,55-56 but the literature does not support the concept of “renal-dose” dopamine.57-59 A study by DeBaker et al49 suggested no difference in efficacy between dopamine and norepinephrine, but demonstrated a greater tendency toward cardiac dysrhythmias with dopamine. For these reasons noted above, norepinephrine may be the initial agent for pharmaceutical support of shock, particularly in septic syndromes, with dopamine as a secondary or adjunct agent in patients at low risk for tachyarrhythmia or a relative bradycardia. 24, 56
Dobutamine
Dobutamine is another adrenergic agonist that is similar to dopamine but with a greater effect on inotropic cardiac contractility due to a preferential action at b1 receptors.60 It can potentially induce peripheral vasodilatation due to its effect on arterial b1 receptors. Given this balance, dobutamine is an agent that should be utilized for cardiogenic shock when increased contractility is needed. These effects are particularly useful in patients with “wet and cold” heart failure who have a low cardiac output and volume-overloaded status.61, 62 However, it may be necessary to add another agent to provide additional peripheral vasoconstriction should the use of dobutamine affect lead to excessive vasodilatation.
Epinephrine
One of the most powerful vasoactive agents, epinephrine has a high affinity for all b1, b2 and a1 receptors.63 These combined effects lead to increased cardiac output and improved BP by increasing cardiac contractility and peripheral vasoconstriction. The effect of epinephrine in limiting mast cell release of histamine makes it the preferred choice for the treatment of anaphylaxis.64 However, side effects of epinephrine include hypertension, tachydysrhythmias, tissue ischemia from vigorous vasoconstriction, and induced lactic acidosis.63
Phenylephrine
Phenylephrine is an a-adrenergic agonist that activates a1 receptors on arteriole smooth muscle, resulting in vasoconstriction.65 It is currently recommended only for hypotension related to procedural sedation.47 Phenylephrine is not recommended for treating patients with septic shock, except when there are concerns about tachydysrhythmias; persistent hypotension with a high cardiac output after treatment with other vasoconstrictor and inotropic drugs; or when a “pure” vasoconstrictor may be preferred.24,56,65
Summary
Although there are many other vasoactive agents that can be used, the selected agents discussed above represent those most commonly used in the ED. All demonstrate significant crossover effects and receptor activation, as well as impact on cardiac contractility and vasoconstriction. The suggested specific indications for each agent are based on current evidenced-based medicine, clinical guidelines, and theoretical benefits on clinical scenarios. But, as always, clinical decisions should be individualized for critically ill patients.
Conclusion
The resuscitation and initiation of care for critically ill patients must typically be immediately upon their arrival in the ED. While general guidelines or recommendations exist for commonly encountered pathologies, treatment should always be patient-centered, based on the needs and nuances unique to each patient in this vulnerable population. The initiation of mechanical ventilation, treatment of sepsis, management of hypertensive neurosurgical emergencies, and use of pressors in shock states are among the most critically important tasks an EP is called upon to perform. This review of current evidence-based guidelines and recommendations will help EPs provide the appropriate and unique care each patient requires.
Dr Brubaker is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Yu is a fellow of adult critical care medicine – emergency medicine in the department of critical care medicine, University of Pittsburgh Medical Center, Pennsylvania. Dr Goodmanson is a resident in the department of emergency medicine at the University of Pittsburgh, Pennsylvania. Dr Schott is an assistant professor, department of emergency medicine and critical care medicine; assistant director of ultrasonography; director, critical care elective student rotation; and director, point of care ultrasound elective student rotation, at the University of Pittsburgh, Pennsylvania
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
- Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32(9):1817-1824.
- Brower RG, Rubenfeld GD. Lung-protective ventilation strategies in acute lung injury. Crit Care Med. 2003;31(4):S312-S316.
- Needham DM, Yang T, Dinglas VD. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med. 2015;191(2):177-185.
- Easter BD, Fischer C, Fisher J. The use of mechanical ventilation in the ED. Am J Emerg Med. 2012;30(7):1183-1188.
- Fuller BM, Mohr NM, Dettmer M, et al. Mechanical ventilation and acute lung injury in emergency department patients with severe sepsis and septic shock: an observational study. Acad Emerg Med. 2013;20(7):659-669.
- Wilcox SR, Seigel TA, Strout TD, et al. Emergency medicine residents’ knowledge of mechanical ventilation. J Emerg Med. 2014. doi:10.1016/j.jemermed.2014.09.059. [Epub ahead of print]
- National Institutes of Health’s National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Clinical Network Mechanical Ventilator Protocol Summary. http://www.ardsnet.org/system/files/Ventilator%20Protocol%20Card.pdf. Accessed March 5, 2015.
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (NHLBI ARDS) Network. Predicted body weight calculator. http://www.ardsnet.org/node/77460. Accessed March 5, 2015.
- Boron WF. Acid-base physiology. In: Boron WF, Boulpaep EL, eds. Medical Physiology: A Cellular And Molecular Approach. Philadelphia, PA: Saunders/Elsevier; 2009:647-649.
- Orebaugh, SL. Initiation of mechanical ventilation in the emergency department. Am J Emerg Med. 1996;14(1):59-69.
- Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149(5):1327-1334.
- Marino PL, Sutin KM. Principles of mechanical ventilation. In: Marino PL, ed. The ICU Book. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:457-472.
- Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection with positive end-expiratory pressures. Am Rev Resp Dis. 1974;110(5):556-565.
- Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993;21(1):131-143.
- Bhandari V. Molecular mechanisms of hyperoxia-induced acute lung injury. Front Biosci. 2008;13:6653-6661.
- Kilgannon JH, Jones AE, Shapiro NI, et al; Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165-2171.
- Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
- Laffey JG, Tanaka M, Engelberts D, et al. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med. 2000;162(6):2287-2294.
- Costello J, Higgins B, Contreras M, et al. Hypercapnic acidosis attenuates shock and lung injury in early and prolonged systemic sepsis. Crit Care Med. 2009;37(8):2412-2420.
- Ijland MM, Heunks LM, van der Hoeven JG. Bench-to-bedside review: hypercapnic acidosis in lung injury—from ‘permissive’ to ‘therapeutic.’ Crit Care. 2010;14(6):237.
- Garg SK. Permissive hypercapnia: Is there any upper limit? Indian J Crit Care Med. 2014;18(9):612-614.
- Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med. 1994;22(10):1568-1578.
- Dellinger RP, Levy MM, Rhodes A, et al; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup Surviving Sepsis Campaign. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165-228.
- Peake SL, Delaney A, Bailey M, et al; ARISE Investigators; ANZICS Clinical Trials Group. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496-1506.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;8;345(19):1368-1377.
- Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(21):2063.
- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303-1310.
- Rivers EP, Ahrens T. Improving outcomes for severe sepsis and septic shock: tools for early identification of at-risk patients and treatment protocol implementation. Crit Care Clin. 2008;24(3 Suppl):S1-S47.
- Nguyen HB, Rivers EP, Abrahamian FM, et al; Emergency Department Sepsis Education Program and Strategies to Improve Survival (ED-SEPSIS) Working Group. Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med. 2006;48(1):28-54.
- Jones AE, Puskarich MA. The Surviving Sepsis Campaign guidelines 2012: update for emergency physicians. Ann Emerg Med. 2014;63(1):35-47.
- Yealy DM, Kellum JA, Huang DT, et al.;ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683-1693.
- Huang DT, Angus DC, Barnato A, et al; ProCESS/ARISE/ProMISe Methodology Writing Committee. Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: methodology of ProCESS, ARISE, and ProMISe. Intensive Care Med. 2013;39(10):1760-1775.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al; American Heart Association Stroke Council and Council on Cardiovascular Nursing. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711-1737.
- He J, Zhang Y, Xu T, et al; The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) Investigators. Effects of immediate blood pressure reduction on death and major disability in patients with acute ischemic stroke: the CATIS randomized clinical trial. JAMA. 2014;311(5):479-489.
- Ankolekar S, Fuller M, Cross I, et al. Feasibility of an ambulance-based stroke trial, and safety of glyceryl trinitrate in ultra-acute stroke: The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT, ISRCTN66434824). Stroke. 2013;44(11):3120-3128.
- Anderson CS, Heeley E, Huang Y, et al; The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2) Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355-2365.
- Bath PM, Woodhouse L, Scutt P, et al; ENOS Trial Investigators. Efficacy of nitric oxide, with or without continuing antihypertensive treatment, for management of high blood pressure in acute stroke (ENOS): a partial-factorial randomised controlled trial. Lancet. 2014;385(9968):617-628
- Butcher KS, Jeerakathil T, Hill M, et al; ICH ADAPT Investigators. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke. 2013;44(3):620-626.
- Bath PM, Krishnan K. Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database Syst Rev. 2014;10:CD000039.
- Tanaka E, Koga M, Kobayashi J, et al. Blood pressure variability on antihypertensive therapy in acute intracerebral hemorrhage: the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement-intracerebral hemorrhage study. Stroke. 2014;45(8):2275-2279.
- Beseoglu K, Unfrau K, Steiger HJ, Hänggi D. Influence of blood pressure variability on short-term outcome in patients with subarachnoid hemorrhage. Cent Eur Neurosurg. 2010;71(2):69-74.
- Hinshaw LB, Cox BG, eds. The fundamental mechanisms of shock. Proceedings of a Symposium Held in Oklahoma City, Oklahoma, October 1-2, 1971. In: Advances in Experimental Medicine and Biology, Vol 23. New York, NY: Plenum Press; 1972.
- Norepinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=norepinephrine&x=0&y=0. March 5, 2015.
- Overgaard CB, Dzavik V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008;118(10):1047-1056.
- Havel C, Arrich J, Losert H, et al. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2011;(5):CD003709.
- De Backer D, Biston P, Devriendt J, et al; SOAP II Investigators. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 2010;362(9):779-789.
- Vasopressin. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=vasopressin&x=0&y=0. March 5, 2015.
- Russell JA, Walley KR, Singer J, et al; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
- Martin C, Papazian L, Perrin G, Saux P, Gouin F. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest. 1993;103(6):1826-1831.
- De Backer D, Creteur J, Silva E, Vincent JL. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31(6)1659-1667.
- Day NP, Phu NH, Bethell DP, et al. The effects of dopamine and adrenaline infusions on acid-base balance and systemic haemodynamics in severe infection. Lancet. 1996;348(9022):219-223.
- Dopamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=dopamine&x=0&y=0. March 5, 2015.
- Manaker S. Use of vasopressors and inotropes. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/use-of-vasopressors-and-inotropes?source=search_result&search=Use+of+vasopressors+and+isotopes&selectedTitle=1%7E150. Accessed March 5, 2015.
- Lauschke A, Teichgräber UK, Frei U, Eckardt KU. ‘Low-dose’ dopamine worsens renal perfusion in patients with acute renal failure. Kidney Int. 2006;69(9):1669-1674.
- Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J. Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Australian and New Zealand Intensive Care Society (ANZICS) Clinical Trials Group. Lancet. 2000;356(9248):2139-2143.
- Kellum JA, M Decker J. Use of dopamine in acute renal failure: a meta-analysis. Crit Care Med. 2001;29(8):1526-1531.
- Dobutamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=Dobutamine&x=0&y=0. Accessed March 5, 2015.
- Nohria A, Mielniczuk LM, Stevenson LW. Evaluation and monitoring of patients with acute heart failure syndromes. Am J Cardiol. 2005;96(6A):32G-40G.
- Joseph SM, Cedars AM, Ewald GA, Geltman EM, Mann DL. Acute decompensated heart failure: contemporary medical management. Tex Heart Inst J. 2009;36(6):510-520.
- Epinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=epinephrine. Accessed March 5, 2015.
- Vadas P, Perelman B. Effect of epinephrine on platelet-activating factor-stimulated human vascular smooth muscle cells. J Allergy Clin Immunol. 2012;129(5):1329-1333.
- Phenylephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=65.%09Phenylephrine&x=10&y=10. Accessed March 5, 2015.
- The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301-1308.
- Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med. 2004;32(9):1817-1824.
- Brower RG, Rubenfeld GD. Lung-protective ventilation strategies in acute lung injury. Crit Care Med. 2003;31(4):S312-S316.
- Needham DM, Yang T, Dinglas VD. Timing of low tidal volume ventilation and intensive care unit mortality in acute respiratory distress syndrome. A prospective cohort study. Am J Respir Crit Care Med. 2015;191(2):177-185.
- Easter BD, Fischer C, Fisher J. The use of mechanical ventilation in the ED. Am J Emerg Med. 2012;30(7):1183-1188.
- Fuller BM, Mohr NM, Dettmer M, et al. Mechanical ventilation and acute lung injury in emergency department patients with severe sepsis and septic shock: an observational study. Acad Emerg Med. 2013;20(7):659-669.
- Wilcox SR, Seigel TA, Strout TD, et al. Emergency medicine residents’ knowledge of mechanical ventilation. J Emerg Med. 2014. doi:10.1016/j.jemermed.2014.09.059. [Epub ahead of print]
- National Institutes of Health’s National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Clinical Network Mechanical Ventilator Protocol Summary. http://www.ardsnet.org/system/files/Ventilator%20Protocol%20Card.pdf. Accessed March 5, 2015.
- National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (NHLBI ARDS) Network. Predicted body weight calculator. http://www.ardsnet.org/node/77460. Accessed March 5, 2015.
- Boron WF. Acid-base physiology. In: Boron WF, Boulpaep EL, eds. Medical Physiology: A Cellular And Molecular Approach. Philadelphia, PA: Saunders/Elsevier; 2009:647-649.
- Orebaugh, SL. Initiation of mechanical ventilation in the emergency department. Am J Emerg Med. 1996;14(1):59-69.
- Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med. 1994;149(5):1327-1334.
- Marino PL, Sutin KM. Principles of mechanical ventilation. In: Marino PL, ed. The ICU Book. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:457-472.
- Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection with positive end-expiratory pressures. Am Rev Resp Dis. 1974;110(5):556-565.
- Parker JC, Hernandez LA, Peevy KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993;21(1):131-143.
- Bhandari V. Molecular mechanisms of hyperoxia-induced acute lung injury. Front Biosci. 2008;13:6653-6661.
- Kilgannon JH, Jones AE, Shapiro NI, et al; Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165-2171.
- Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347-354.
- Laffey JG, Tanaka M, Engelberts D, et al. Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med. 2000;162(6):2287-2294.
- Costello J, Higgins B, Contreras M, et al. Hypercapnic acidosis attenuates shock and lung injury in early and prolonged systemic sepsis. Crit Care Med. 2009;37(8):2412-2420.
- Ijland MM, Heunks LM, van der Hoeven JG. Bench-to-bedside review: hypercapnic acidosis in lung injury—from ‘permissive’ to ‘therapeutic.’ Crit Care. 2010;14(6):237.
- Garg SK. Permissive hypercapnia: Is there any upper limit? Indian J Crit Care Med. 2014;18(9):612-614.
- Hickling KG, Walsh J, Henderson S, Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med. 1994;22(10):1568-1578.
- Dellinger RP, Levy MM, Rhodes A, et al; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup Surviving Sepsis Campaign. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165-228.
- Peake SL, Delaney A, Bailey M, et al; ARISE Investigators; ANZICS Clinical Trials Group. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014;371(16):1496-1506.
- Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;8;345(19):1368-1377.
- Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(21):2063.
- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303-1310.
- Rivers EP, Ahrens T. Improving outcomes for severe sepsis and septic shock: tools for early identification of at-risk patients and treatment protocol implementation. Crit Care Clin. 2008;24(3 Suppl):S1-S47.
- Nguyen HB, Rivers EP, Abrahamian FM, et al; Emergency Department Sepsis Education Program and Strategies to Improve Survival (ED-SEPSIS) Working Group. Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med. 2006;48(1):28-54.
- Jones AE, Puskarich MA. The Surviving Sepsis Campaign guidelines 2012: update for emergency physicians. Ann Emerg Med. 2014;63(1):35-47.
- Yealy DM, Kellum JA, Huang DT, et al.;ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014;370(18):1683-1693.
- Huang DT, Angus DC, Barnato A, et al; ProCESS/ARISE/ProMISe Methodology Writing Committee. Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: methodology of ProCESS, ARISE, and ProMISe. Intensive Care Med. 2013;39(10):1760-1775.
- Jauch EC, Saver JL, Adams HP Jr, et al; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Peripheral Vascular Disease; Council on Clinical Cardiology. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870-947.
- Morgenstern LB, Hemphill JC 3rd, Anderson C, et al; American Heart Association Stroke Council and Council on Cardiovascular Nursing. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41(9):2108-2129.
- Connolly ES Jr, Rabinstein AA, Carhuapoma JR, et al; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711-1737.
- He J, Zhang Y, Xu T, et al; The China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) Investigators. Effects of immediate blood pressure reduction on death and major disability in patients with acute ischemic stroke: the CATIS randomized clinical trial. JAMA. 2014;311(5):479-489.
- Ankolekar S, Fuller M, Cross I, et al. Feasibility of an ambulance-based stroke trial, and safety of glyceryl trinitrate in ultra-acute stroke: The Rapid Intervention With Glyceryl Trinitrate in Hypertensive Stroke Trial (RIGHT, ISRCTN66434824). Stroke. 2013;44(11):3120-3128.
- Anderson CS, Heeley E, Huang Y, et al; The Second Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage Trial (INTERACT-2) Investigators. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355-2365.
- Bath PM, Woodhouse L, Scutt P, et al; ENOS Trial Investigators. Efficacy of nitric oxide, with or without continuing antihypertensive treatment, for management of high blood pressure in acute stroke (ENOS): a partial-factorial randomised controlled trial. Lancet. 2014;385(9968):617-628
- Butcher KS, Jeerakathil T, Hill M, et al; ICH ADAPT Investigators. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke. 2013;44(3):620-626.
- Bath PM, Krishnan K. Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database Syst Rev. 2014;10:CD000039.
- Tanaka E, Koga M, Kobayashi J, et al. Blood pressure variability on antihypertensive therapy in acute intracerebral hemorrhage: the Stroke Acute Management with Urgent Risk-factor Assessment and Improvement-intracerebral hemorrhage study. Stroke. 2014;45(8):2275-2279.
- Beseoglu K, Unfrau K, Steiger HJ, Hänggi D. Influence of blood pressure variability on short-term outcome in patients with subarachnoid hemorrhage. Cent Eur Neurosurg. 2010;71(2):69-74.
- Hinshaw LB, Cox BG, eds. The fundamental mechanisms of shock. Proceedings of a Symposium Held in Oklahoma City, Oklahoma, October 1-2, 1971. In: Advances in Experimental Medicine and Biology, Vol 23. New York, NY: Plenum Press; 1972.
- Norepinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=norepinephrine&x=0&y=0. March 5, 2015.
- Overgaard CB, Dzavik V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008;118(10):1047-1056.
- Havel C, Arrich J, Losert H, et al. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2011;(5):CD003709.
- De Backer D, Biston P, Devriendt J, et al; SOAP II Investigators. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 2010;362(9):779-789.
- Vasopressin. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=vasopressin&x=0&y=0. March 5, 2015.
- Russell JA, Walley KR, Singer J, et al; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887.
- Martin C, Papazian L, Perrin G, Saux P, Gouin F. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest. 1993;103(6):1826-1831.
- De Backer D, Creteur J, Silva E, Vincent JL. Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: which is best? Crit Care Med. 2003;31(6)1659-1667.
- Day NP, Phu NH, Bethell DP, et al. The effects of dopamine and adrenaline infusions on acid-base balance and systemic haemodynamics in severe infection. Lancet. 1996;348(9022):219-223.
- Dopamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=dopamine&x=0&y=0. March 5, 2015.
- Manaker S. Use of vasopressors and inotropes. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/use-of-vasopressors-and-inotropes?source=search_result&search=Use+of+vasopressors+and+isotopes&selectedTitle=1%7E150. Accessed March 5, 2015.
- Lauschke A, Teichgräber UK, Frei U, Eckardt KU. ‘Low-dose’ dopamine worsens renal perfusion in patients with acute renal failure. Kidney Int. 2006;69(9):1669-1674.
- Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J. Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Australian and New Zealand Intensive Care Society (ANZICS) Clinical Trials Group. Lancet. 2000;356(9248):2139-2143.
- Kellum JA, M Decker J. Use of dopamine in acute renal failure: a meta-analysis. Crit Care Med. 2001;29(8):1526-1531.
- Dobutamine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=Dobutamine&x=0&y=0. Accessed March 5, 2015.
- Nohria A, Mielniczuk LM, Stevenson LW. Evaluation and monitoring of patients with acute heart failure syndromes. Am J Cardiol. 2005;96(6A):32G-40G.
- Joseph SM, Cedars AM, Ewald GA, Geltman EM, Mann DL. Acute decompensated heart failure: contemporary medical management. Tex Heart Inst J. 2009;36(6):510-520.
- Epinephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=epinephrine. Accessed March 5, 2015.
- Vadas P, Perelman B. Effect of epinephrine on platelet-activating factor-stimulated human vascular smooth muscle cells. J Allergy Clin Immunol. 2012;129(5):1329-1333.
- Phenylephrine. UpToDate Web site. Post TW, ed. UpToDate, Waltham, MA. http://www.uptodate.com/contents/search?search=65.%09Phenylephrine&x=10&y=10. Accessed March 5, 2015.