User login
Nail pigmentation and fatigue
A 49-year-old man presented with pigmentation on the nails of both hands during the past 6 months. He had no history of significant medical conditions, but he complained of generalized asthenia, with no fever, during the previous 6 weeks. He said that he was a volcanologist and had recently returned from an expedition in the mountains of Peru that involved intense physical activity at high altitudes. He was a non-smoker and did not drink alcohol; he was not taking any medications or nutritional supplements. A biochemical profile including a white blood cell count 3 months ago was normal.
On physical examination, he had splenomegaly (about 2 cm below the costal margin) and low systolic blood pressure (90 mm Hg, with the diastolic pressure at 60 mm Hg). Heart and lung examinations, including chest radiography, were normal.
Q: What is the diagnosis?
- Addison disease
- Onychotillomania
- Longitudinal melanonychia in human immunodeficiency virus (HIV) infection
- Systemic lupus erythematosus
A: The patient was diagnosed with longitudinal melanonychia with underlying HIV infection.
In addition to the clinical findings noted above, laboratory testing now revealed a low white blood cell count (2.9 × 109/L, reference range 4.5–11.0) and a low CD4+ T-cell count (182 cells/mL). An enzyme-linked immunosorbent assay and a Western blot assay were positive for HIV, and his viral load was 120,000 copies/mL as determined by reverse transcription-polymerase chain reaction testing. On more detailed questioning, the patient admitted to sexual practices that put him at high risk for HIV infection.
Longitudinal melanonychia is characterized by a tan, brown, or black longitudinal streak, originating in the matrix and resulting from increased synthesis of melanin (by either normal or abnormal melanocytes) and its deposition within the nail plate.1
If the cause is not apparent (eg, trauma, application of chemical agents, concomitant onychomycosis or treatments), this pigmentation usually reflects the presence of a benign lesion within the matrix caused by a melanocytic nevus, simple lentigo, or increased activation of benign melanocytes. This finding has been reported in a US study2 to be more common in people with dark skin, occurring in 77% of blacks over age 20 and in almost 100% of those over age 50.
Melanoma and other nonmelanocytic tumors may present as longitudinal melanonychia, but these rarely involve more than one digit simultaneously, and they are usually detected with specific clinical clues, such as the Hutchinson sign, ie, periungual spread of pigmentation into the proximal and lateral nail folds.
A SIGN OF BENIGN AND MALIGNANT CONDITIONS
Longitudinal melanonychia can have benign causes, and these need to be investigated. It can occur with repeated trauma, friction, or pressure on the nails. The physician should question the patient about habits such as picking or chewing of the finger tips or pushing back the cuticles, as well as about athletic activities or manual work that could affect the nails. In addition, blood thinners can cause nail discoloration via subungual hemorrhage.
A number of pathologic conditions can cause longitudinal discoloration of the nails. Infection with certain dermatophytes can cause discoloration, but this pigmentation is usually wider and more distal at the hyponychium rather than proximal, with a black streak with several pointed extensions proximally.
Adrenocortical insufficiency (Addison disease), nutritional disorders (deficiency of folic acid or vitamin B12), and, more rarely, systemic lupus erythematosus and scleroderma should be ruled out, as they are typically associated with cutaneous and mucosal hyperpigmentation.
Chemotherapeutic agents such as doxorubicin (Adriamycin), hydroxyurea (Droxea), and cyclophosphamide and drugs such as antimalarials and tetracyclines can also cause longitudinal melanonychia.1,3
Nail lesions with a similar pattern are often seen in patients (especially black patients) taking zidovudine (Retrovir), and these lesions seem not to be related to drug dosage, HIV risk group, or severity of the infection. Nail discoloration in HIV patients not taking antiretroviral therapy has not been well documented.
The significance of melanonychia in the course of HIV remains unclear. A key role of overexpression of alpha-melanocyte-stimulating-hormone has been proposed.4 Although rare in fair-skinned people, longitudinal melanonychia represents an important clinical sign of disease progression. In reported cases, however, no significant improvement has been noted with treatment despite favorable virologic and immunologic responses.4,5
- Smith DF, Morgan MB, Bettencourt MS. Longitudinal melanonychia. Arch Dermatol 2003; 139:1209–1214.
- Baran R, Kechijian P. Longitudinal melanonychia (melanonychia striata): diagnosis and management. J Am Acad Dermatol 1989; 21:1165–1175.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Ward HA, Russo GG, Shrum J. Cutaneous manifestations of antiretroviral therapy. J Am Acad Dermatol 2002; 46:284–293.
- Ehnzadeh-Cheemeh P, Grimes RM, Rowan P, Huang YJ, Essien EJ, Lewis ST. Melanonychia in patients infected with human immunodeficiency virus original communication. Adv Infect Dis 2011; 1:15–19.
A 49-year-old man presented with pigmentation on the nails of both hands during the past 6 months. He had no history of significant medical conditions, but he complained of generalized asthenia, with no fever, during the previous 6 weeks. He said that he was a volcanologist and had recently returned from an expedition in the mountains of Peru that involved intense physical activity at high altitudes. He was a non-smoker and did not drink alcohol; he was not taking any medications or nutritional supplements. A biochemical profile including a white blood cell count 3 months ago was normal.
On physical examination, he had splenomegaly (about 2 cm below the costal margin) and low systolic blood pressure (90 mm Hg, with the diastolic pressure at 60 mm Hg). Heart and lung examinations, including chest radiography, were normal.
Q: What is the diagnosis?
- Addison disease
- Onychotillomania
- Longitudinal melanonychia in human immunodeficiency virus (HIV) infection
- Systemic lupus erythematosus
A: The patient was diagnosed with longitudinal melanonychia with underlying HIV infection.
In addition to the clinical findings noted above, laboratory testing now revealed a low white blood cell count (2.9 × 109/L, reference range 4.5–11.0) and a low CD4+ T-cell count (182 cells/mL). An enzyme-linked immunosorbent assay and a Western blot assay were positive for HIV, and his viral load was 120,000 copies/mL as determined by reverse transcription-polymerase chain reaction testing. On more detailed questioning, the patient admitted to sexual practices that put him at high risk for HIV infection.
Longitudinal melanonychia is characterized by a tan, brown, or black longitudinal streak, originating in the matrix and resulting from increased synthesis of melanin (by either normal or abnormal melanocytes) and its deposition within the nail plate.1
If the cause is not apparent (eg, trauma, application of chemical agents, concomitant onychomycosis or treatments), this pigmentation usually reflects the presence of a benign lesion within the matrix caused by a melanocytic nevus, simple lentigo, or increased activation of benign melanocytes. This finding has been reported in a US study2 to be more common in people with dark skin, occurring in 77% of blacks over age 20 and in almost 100% of those over age 50.
Melanoma and other nonmelanocytic tumors may present as longitudinal melanonychia, but these rarely involve more than one digit simultaneously, and they are usually detected with specific clinical clues, such as the Hutchinson sign, ie, periungual spread of pigmentation into the proximal and lateral nail folds.
A SIGN OF BENIGN AND MALIGNANT CONDITIONS
Longitudinal melanonychia can have benign causes, and these need to be investigated. It can occur with repeated trauma, friction, or pressure on the nails. The physician should question the patient about habits such as picking or chewing of the finger tips or pushing back the cuticles, as well as about athletic activities or manual work that could affect the nails. In addition, blood thinners can cause nail discoloration via subungual hemorrhage.
A number of pathologic conditions can cause longitudinal discoloration of the nails. Infection with certain dermatophytes can cause discoloration, but this pigmentation is usually wider and more distal at the hyponychium rather than proximal, with a black streak with several pointed extensions proximally.
Adrenocortical insufficiency (Addison disease), nutritional disorders (deficiency of folic acid or vitamin B12), and, more rarely, systemic lupus erythematosus and scleroderma should be ruled out, as they are typically associated with cutaneous and mucosal hyperpigmentation.
Chemotherapeutic agents such as doxorubicin (Adriamycin), hydroxyurea (Droxea), and cyclophosphamide and drugs such as antimalarials and tetracyclines can also cause longitudinal melanonychia.1,3
Nail lesions with a similar pattern are often seen in patients (especially black patients) taking zidovudine (Retrovir), and these lesions seem not to be related to drug dosage, HIV risk group, or severity of the infection. Nail discoloration in HIV patients not taking antiretroviral therapy has not been well documented.
The significance of melanonychia in the course of HIV remains unclear. A key role of overexpression of alpha-melanocyte-stimulating-hormone has been proposed.4 Although rare in fair-skinned people, longitudinal melanonychia represents an important clinical sign of disease progression. In reported cases, however, no significant improvement has been noted with treatment despite favorable virologic and immunologic responses.4,5
A 49-year-old man presented with pigmentation on the nails of both hands during the past 6 months. He had no history of significant medical conditions, but he complained of generalized asthenia, with no fever, during the previous 6 weeks. He said that he was a volcanologist and had recently returned from an expedition in the mountains of Peru that involved intense physical activity at high altitudes. He was a non-smoker and did not drink alcohol; he was not taking any medications or nutritional supplements. A biochemical profile including a white blood cell count 3 months ago was normal.
On physical examination, he had splenomegaly (about 2 cm below the costal margin) and low systolic blood pressure (90 mm Hg, with the diastolic pressure at 60 mm Hg). Heart and lung examinations, including chest radiography, were normal.
Q: What is the diagnosis?
- Addison disease
- Onychotillomania
- Longitudinal melanonychia in human immunodeficiency virus (HIV) infection
- Systemic lupus erythematosus
A: The patient was diagnosed with longitudinal melanonychia with underlying HIV infection.
In addition to the clinical findings noted above, laboratory testing now revealed a low white blood cell count (2.9 × 109/L, reference range 4.5–11.0) and a low CD4+ T-cell count (182 cells/mL). An enzyme-linked immunosorbent assay and a Western blot assay were positive for HIV, and his viral load was 120,000 copies/mL as determined by reverse transcription-polymerase chain reaction testing. On more detailed questioning, the patient admitted to sexual practices that put him at high risk for HIV infection.
Longitudinal melanonychia is characterized by a tan, brown, or black longitudinal streak, originating in the matrix and resulting from increased synthesis of melanin (by either normal or abnormal melanocytes) and its deposition within the nail plate.1
If the cause is not apparent (eg, trauma, application of chemical agents, concomitant onychomycosis or treatments), this pigmentation usually reflects the presence of a benign lesion within the matrix caused by a melanocytic nevus, simple lentigo, or increased activation of benign melanocytes. This finding has been reported in a US study2 to be more common in people with dark skin, occurring in 77% of blacks over age 20 and in almost 100% of those over age 50.
Melanoma and other nonmelanocytic tumors may present as longitudinal melanonychia, but these rarely involve more than one digit simultaneously, and they are usually detected with specific clinical clues, such as the Hutchinson sign, ie, periungual spread of pigmentation into the proximal and lateral nail folds.
A SIGN OF BENIGN AND MALIGNANT CONDITIONS
Longitudinal melanonychia can have benign causes, and these need to be investigated. It can occur with repeated trauma, friction, or pressure on the nails. The physician should question the patient about habits such as picking or chewing of the finger tips or pushing back the cuticles, as well as about athletic activities or manual work that could affect the nails. In addition, blood thinners can cause nail discoloration via subungual hemorrhage.
A number of pathologic conditions can cause longitudinal discoloration of the nails. Infection with certain dermatophytes can cause discoloration, but this pigmentation is usually wider and more distal at the hyponychium rather than proximal, with a black streak with several pointed extensions proximally.
Adrenocortical insufficiency (Addison disease), nutritional disorders (deficiency of folic acid or vitamin B12), and, more rarely, systemic lupus erythematosus and scleroderma should be ruled out, as they are typically associated with cutaneous and mucosal hyperpigmentation.
Chemotherapeutic agents such as doxorubicin (Adriamycin), hydroxyurea (Droxea), and cyclophosphamide and drugs such as antimalarials and tetracyclines can also cause longitudinal melanonychia.1,3
Nail lesions with a similar pattern are often seen in patients (especially black patients) taking zidovudine (Retrovir), and these lesions seem not to be related to drug dosage, HIV risk group, or severity of the infection. Nail discoloration in HIV patients not taking antiretroviral therapy has not been well documented.
The significance of melanonychia in the course of HIV remains unclear. A key role of overexpression of alpha-melanocyte-stimulating-hormone has been proposed.4 Although rare in fair-skinned people, longitudinal melanonychia represents an important clinical sign of disease progression. In reported cases, however, no significant improvement has been noted with treatment despite favorable virologic and immunologic responses.4,5
- Smith DF, Morgan MB, Bettencourt MS. Longitudinal melanonychia. Arch Dermatol 2003; 139:1209–1214.
- Baran R, Kechijian P. Longitudinal melanonychia (melanonychia striata): diagnosis and management. J Am Acad Dermatol 1989; 21:1165–1175.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Ward HA, Russo GG, Shrum J. Cutaneous manifestations of antiretroviral therapy. J Am Acad Dermatol 2002; 46:284–293.
- Ehnzadeh-Cheemeh P, Grimes RM, Rowan P, Huang YJ, Essien EJ, Lewis ST. Melanonychia in patients infected with human immunodeficiency virus original communication. Adv Infect Dis 2011; 1:15–19.
- Smith DF, Morgan MB, Bettencourt MS. Longitudinal melanonychia. Arch Dermatol 2003; 139:1209–1214.
- Baran R, Kechijian P. Longitudinal melanonychia (melanonychia striata): diagnosis and management. J Am Acad Dermatol 1989; 21:1165–1175.
- Haneke E, Baran R. Longitudinal melanonychia. Dermatol Surg 2001; 27:580–584.
- Ward HA, Russo GG, Shrum J. Cutaneous manifestations of antiretroviral therapy. J Am Acad Dermatol 2002; 46:284–293.
- Ehnzadeh-Cheemeh P, Grimes RM, Rowan P, Huang YJ, Essien EJ, Lewis ST. Melanonychia in patients infected with human immunodeficiency virus original communication. Adv Infect Dis 2011; 1:15–19.
More Than a Plantar Wart
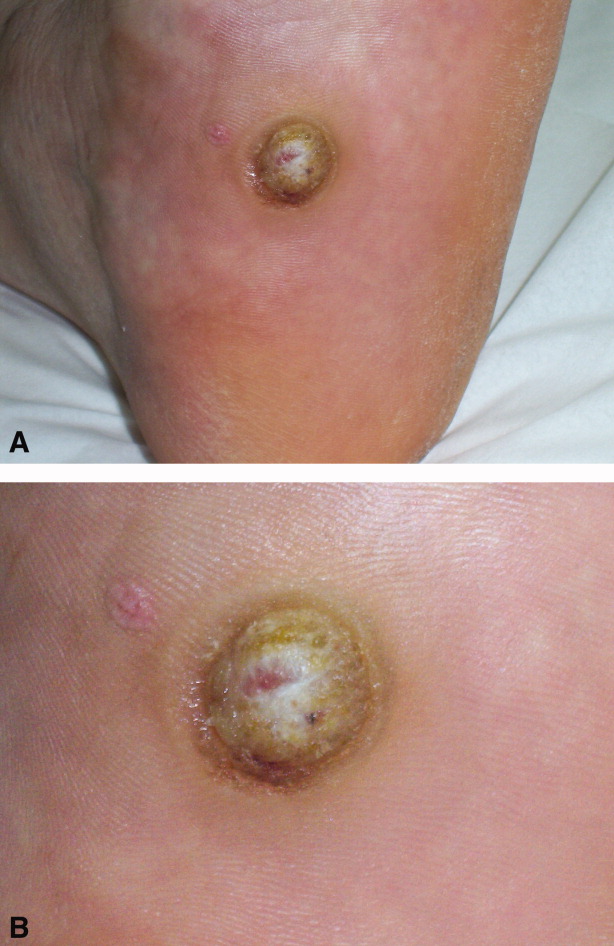
A 56‐year‐old man with a 1‐year history of a verrucous nodule on his left foot presented to our department due to the unexpected growth. He was previously diagnosed with a plantar wart so underwent salicylic ointment application, liquid‐nitrogen cryotherapy and electrocoagulation, with no improvement of the condition.
Clinical examination revealed a 22‐mm flesh‐colored, centrally hypopigmented and ulcerated, exophytic nodule, with an adjacent 5 4 mm pink papule with telangiectasia (Figure 1A and B).

Histological examination established the diagnosis of ulcerated amelanotic malignant melanoma (Clark's level IV, Breslow's thickness of 3 mm) with a satellite nodule. Radical inguinal lymph node dissection yielded a negative result. Total‐body computed tomographic scan was unremarkable. One‐year follow‐up revealed no metastatic disease.
Melanoma of the foot accounts for 3% to 15% of all cutaneous melanoma. In acral skin, melanomas tend to have unusual clinical appearances. Amelanotic variants may masquerade as several benign hyperkeratotic dermatoses (warts, calluses, fungal disorders, foreign bodies, moles, keratoacanthomas, hematomas) increasing misdiagnosis and inadequate treatment rates, with a poorer patient outcome.1 Pedal lesions require close observation and biopsy when diagnostic uncertainty exists or when therapeutic interventions fail.
- ,,,,,.Acral lentiginous melanoma mimicking benign disease: the Emory experience.J Am Acad Dermatol.2003;48:183–188.
A 56‐year‐old man with a 1‐year history of a verrucous nodule on his left foot presented to our department due to the unexpected growth. He was previously diagnosed with a plantar wart so underwent salicylic ointment application, liquid‐nitrogen cryotherapy and electrocoagulation, with no improvement of the condition.
Clinical examination revealed a 22‐mm flesh‐colored, centrally hypopigmented and ulcerated, exophytic nodule, with an adjacent 5 4 mm pink papule with telangiectasia (Figure 1A and B).

Histological examination established the diagnosis of ulcerated amelanotic malignant melanoma (Clark's level IV, Breslow's thickness of 3 mm) with a satellite nodule. Radical inguinal lymph node dissection yielded a negative result. Total‐body computed tomographic scan was unremarkable. One‐year follow‐up revealed no metastatic disease.
Melanoma of the foot accounts for 3% to 15% of all cutaneous melanoma. In acral skin, melanomas tend to have unusual clinical appearances. Amelanotic variants may masquerade as several benign hyperkeratotic dermatoses (warts, calluses, fungal disorders, foreign bodies, moles, keratoacanthomas, hematomas) increasing misdiagnosis and inadequate treatment rates, with a poorer patient outcome.1 Pedal lesions require close observation and biopsy when diagnostic uncertainty exists or when therapeutic interventions fail.
A 56‐year‐old man with a 1‐year history of a verrucous nodule on his left foot presented to our department due to the unexpected growth. He was previously diagnosed with a plantar wart so underwent salicylic ointment application, liquid‐nitrogen cryotherapy and electrocoagulation, with no improvement of the condition.
Clinical examination revealed a 22‐mm flesh‐colored, centrally hypopigmented and ulcerated, exophytic nodule, with an adjacent 5 4 mm pink papule with telangiectasia (Figure 1A and B).

Histological examination established the diagnosis of ulcerated amelanotic malignant melanoma (Clark's level IV, Breslow's thickness of 3 mm) with a satellite nodule. Radical inguinal lymph node dissection yielded a negative result. Total‐body computed tomographic scan was unremarkable. One‐year follow‐up revealed no metastatic disease.
Melanoma of the foot accounts for 3% to 15% of all cutaneous melanoma. In acral skin, melanomas tend to have unusual clinical appearances. Amelanotic variants may masquerade as several benign hyperkeratotic dermatoses (warts, calluses, fungal disorders, foreign bodies, moles, keratoacanthomas, hematomas) increasing misdiagnosis and inadequate treatment rates, with a poorer patient outcome.1 Pedal lesions require close observation and biopsy when diagnostic uncertainty exists or when therapeutic interventions fail.
- ,,,,,.Acral lentiginous melanoma mimicking benign disease: the Emory experience.J Am Acad Dermatol.2003;48:183–188.
- ,,,,,.Acral lentiginous melanoma mimicking benign disease: the Emory experience.J Am Acad Dermatol.2003;48:183–188.