User login
Isolated oligohydramnios at term: Is induction indicated?
- Isolated term oligohydramnios, as defined by an amniotic fluid index (AFI) of less than 5 cm, has not been shown to be associated with poor maternal or fetal outcomes. Management may be individualized based on factors such as parity, cervical ripeness, and patient preference (SOR: B).
- Maternal hydration with oral water has been shown to increase AFI in a few hours, likely due to improved uteroplacental perfusion. This is a reasonable alternative to immediate labor induction in women with isolated term oligohydramnios (SOR: B).
- An isolated finding of a so-called “border-line” AFI (5–8 cm) is not an indication for labor induction (SOR: B).
Family physicians providing maternity care often face a scenario in which an otherwise low-risk, term patient is incidentally noted to have a low amniotic fluid index (AFI). Common reasons for obtaining an AFI in a woman with a low-risk pregnancy include evaluation of decreased fetal movement, spontaneous variable decelerations during monitoring to evaluate for labor, or an ultrasound evaluation for fundal height measurements discordant with gestational age. How should “isolated” oligohydramnios—an AFI <5 cm—be interpreted, and should immediate induction be recommended for such patients?
Oligohydramnios occurs in about 1% to 5% of pregnancies at term.1,2 Because adverse outcomes occur in high-risk pregnancies complicated by low amniotic fluid volume, oligohydramnios commonly prompts labor induction.1,3,4 At one university center, oligohydramnios is now the leading indication for labor induction.5 Many centers may even induce labor when the AFI is between 5 cm and 8 cm, the so-called borderline AFI.3
Labor induction increases the use of cesarean delivery, particularly for the primiparous woman with an unripe cervix.6 Recent studies questioning the safety of labor induction in women who have had a cesarean may increase the number of elective repeat cesarean procedures when delivery is believed indicated for oligohydramnios.7 (See Underlying causes of oligohydramnios.)
By the second trimester, amniotic fluid is being produced primarily through fetal urine production and is primarily resorbed through fetal swallowing. Significant amounts of amniotic fluid are also produced and resorbed by the fetal lung and directly resorbed from the amniotic cavity by the placenta.8,9 Amniotic fluid volume is affected by the status of maternal hydration and maternal plasma osmolality.10-13
Acute oligohydramnios may occur from ruptured membranes, usually diagnosed by clinical signs and vaginal fluid with altered pH and a ferning pattern on microscopic exam.
Chronic oligohydramnios arises from prerenal, renal, and postrenal causes. The latter 2 groups reflect fetal kidney and urogenital abnormalities, which directly decrease fetal amniotic fluid production. Uteroplacental insufficiency is the most common cause of prerenal oligohydramnios, and the decreased amniotic fluid is a direct result of decreased fetal renal perfusion.14 Uteroplacental insufficiency may result in intrauterine growth restriction as the fetus shunts blood away from the growing torso and limbs and to vital organs such as the brain. Preeclampsia and postdate pregnancies both involve pathologic changes in the placenta that may result in uteroplacental insufficiency and oligohydramnios.
Oligohydramnios is difficult to assess
True oligohydramnios can be difficult to confirm due to the questionable accuracy of amniotic fluid measurement by ultrasound. There is controversy, for example, about whether (and how) to include pockets of amniotic fluid containing umbilical cord.15 The AFI was introduced in 19872 to replace the 2 cm “pocket technique” of fluid assessment, and studies continue to question to what extent the AFI reflects actual amniotic fluid volume.
AFI measurements may vary with the amount of pressure applied to the abdomen and with fetal position or movement.16
Serial measurements taken by the same ultrasound operator have been shown to differ from the true volume by 1 cm, or 10.8%; serial measurements taken by multiple operators have differed by as much as 2 cm, or 15.4%.17,18
O’Reilly-Green compared the diagnosis of oligohydramnios in 449 post-term patients with actual amniotic fluid volume measured at rupture of membranes.19 They found a positive predictive value of 50% for oligohydramnios at an AFI of 5 cm as the lower limit of normal. A study of 144 third trimester patients using the dye-dilution technique found that, to achieve 95% confidence for ruling out oligohydramnios, a cutoff AFI of 30 cm would need to be used, a value consistent with polyhydramnios.20
What is the association between oligohydramnios and poor fetal outcomes?
A number of studies over the past 15 years have shown an association between oligohydramnios and poor fetal outcomes. These were predominantly retrospective studies, which failed to control for the presence of factors known to be associated with oligohydramnios such as intrauterine growth restriction (IUGR) and urogenital malformations.
No studies have directly addressed whether labor induction improves outcomes. A meta-analysis of 18 studies examining outcomes of pregnancies with AFI <5 cm found an increased risk of cesarean delivery for fetal distress and low Apgar scores at 5 minutes. Most of these studies, however, had high-risk patients including IUGR (level of evidence [LOE]: 2).21
A recent study of high-risk patients failed to detect a difference in the incidence of nonreactive nonstress tests, meconium-stained amniotic fluid cesarean delivery for fetal distress, low Apgar scores, or infants with a cord pH of <7.10 when oligohydramnios (AFI <5.0 cm) was present (LOE: 1).2 The patients with oligohydramnios were all induced, while many of the other high-risk patients were expectantly managed. The study therefore provides no guidance on the safety of expectant management for patients with oligohydramnios. To eliminate the potential effect of induction versus expectant management the same authors performed a case-control study of 79 high-risk women with AFI <5 cm matched to 79 women with the same high-risk pregnancy complication who had an AFI >5 cm at the time of induction (LOE: 2).23 They failed to detect any significant differences in neonatal outcomes between the groups.
Studies of the “borderline” AFI (between 5 cm and 8 cm) may also demonstrate an association with adverse neonatal outcomes if researchers include fetuses with IUGR or malformations. In one retrospective case review of 214 women with AFI of 5 cm to 10 cm, the only statistically significant finding was an association with IUGR.3 The authors recommended antepartum surveillance twice a week for mothers with borderline AFI, but they did not comment on induction (LOE: 2). Correspondence regarding this study argued that this recommendation was not supported by the evidence and would lead to unnecessary antenatal testing.24
Studies of isolated oligohydramnios
Investigators have conducted studies (Table 1) excluding fetuses with intrauterine growth restriction or anomalies to try to determine if isolated oligohydramnios is associated with poorer outcomes.25-30
Rainford’s study of outcomes in exclusively term, low-risk patients failed to show significant outcome differences in Apgar scores, NICU admissions, or rates of cesarean delivery for non-reassuring fetal heart rate monitoring (LOE: 2).29 This study was limited due to its retrospective design. The authors comment that the relatively good outcomes in the oligohydramnios group may be due to the widespread practice of inducing such patients.
In a case-control study by Conway, 183 low-risk, term parturients with oligohydramnios were matched to 183 women of similar gestational age and parity who presented in spontaneous labor. The patients with isolated oligohydramnios were induced and showed an increased cesarean delivery rate. The increased rate of cesarean delivery was not due to nonreassuring fetal surveillance and was attributed to the induction process (LOE: 2).25
An analysis of woman diagnosed with isolated oligohydramnios (AFI <5) at any gestational age in the multicenter prospective RADIUS trial demonstrated similar perinatal outcomes and fetal growth compared with pregnancies with a normal amniotic fluid (LOE: 2).30
The only randomized clinical trial of labor induction vs expectant management for term isolated oligohydramnios showed similar outcomes in each group. But this study was small (n=61) and has only been published as an abstract.31
TABLE 1
Isolated oligohydramnios and perinatal outcomes
| Study | Design | Study number n vs controls | Patient-oriented outcomes | Comment | LOE | |
|---|---|---|---|---|---|---|
| Population | Significant findings | Non-significant findings | ||||
| Garmel19 | Prospective cohort | N=187 | Increased preterm birth (OR=3.23; 95% CI, 1.4–7.3) in oligohydramnios group | IUGR, asphyxia, death, NICU admit | Delivery recommended at 37 weeks | 2 |
| 17–37 week with subnormal EFW (>10%) | 65 AFI <8 cm vs 122 AFI >8 cm | |||||
| Conway18 | Prospective cohort | N=366 | Increased CS rate (OR=2.7 95% CI, 1.3–5.4) in oligohydramnios group | CS for fetal distress; all neonatal outcomes | Treatment group induced, controls spontaneous | 2 |
| Term, isolated oligohydramnios undergoing induction | 183 AFI <5 cm vs 183 AFI >5 cm | |||||
| Roberts21 | Prospective cohort | N=206 | Increased IUGR (OR=5.2; 95% CI, 1.6–22), induction (OR=34.4, 95% CI, 4–1425.5), NICU admit (OR=9.8; 95% CI, 1.3–432) | Fetal distress requiring CS | Used >5%ile to exclude IUGR. Included some high-risk pts (diabetes or hypertension) | 2 |
| 3rd trimester, isolated oligohydramnios | 103 AFI 3%ile (N=103) vs matched control | |||||
| Rainford22 | Retrospective cohort | N=232 | Induction rate for AFI <5 = 98% vs 51% AFI >5 P<.001; increased meconium staining in controls without oligohydramnios | NICU 2 admissions, 5-minute Apgar scores | 2 | |
| 37–41 week, low-risk. AFI within 4 days of delivery | AFI <5 (n=44) vs >5 (n=188) | |||||
| Zhang23 | Retrospective nested cohort | N=6657 | Malpresentation (RR=3.5, 95% CI 1.8–6.60) | Fetal growth, CS, low Apgar, overall neonatal morbidity | Benefit of routine ultrasound was the primary study outcome study endpoint | 2 |
| Term or near-term, low-risk | AFI <5 (n=86) vs >5 (n=6571) | |||||
| AFI, amniotic fluid index; CI, confidence interval; CS, cesarean section; EFW, estimated fetal weight; IUGR, intrauterine growth restriction; LOE, level of evidence; NICU, neonatal intensive care unit; OR, odds ratio; RR, relative risk. | ||||||
Effect of maternal hydration
Maternal hydration status and plasma osmolality have an affect on amniotic fluid volume (Table 2). Maternal hydration with oral water or intravenous hypotonic solutions has been shown to increase amniotic fluid volume.8,11-13 Oral hydration with hypotonic fluid has been demonstrated to increase fetal urine production in one observational study.32 Another observational study demonstrated increased amniotic fluid volume and uteroplacental perfusion without alteration of fetal urine production suggesting the possibility that transmembranous fluid shifts from the placenta to the amniotic cavity may be involved.12
Two small, randomized controlled trials (RCTs) demonstrated an increase in amniotic fluid volume in women with oligohydramnios after oral hydration.11,13 Doi demonstrated significant increases in AFI in women with oligohydramnios beyond 35 weeks when given oral hydration with free water (increase of 3.8 cm ± 1.9; P<. 001) or hypotonic intravenous solution (increase of 2.8 cm ± 1.9; P<.001) (LOE: 3).11 Interestingly, this study did not demonstrate an increase in amniotic fluid volume with intravenous hydration with isotonic fluid.
Kirkpatrick demonstrated a 30% increase in amniotic fluid compared with controls in women of unspecified gestational age with oligohydramnios given 2 liters of oral water 2 to 5 hours before repeat amniotic fluid index (LOE: 3).13
A randomized trial in women with normal amniotic fluid demonstrated a 16% increase in amniotic fluid index 4 to 6 hours after hydration with 2 liters of oral water, compared with an 8% decrease after fluid restriction during the same period.8
A recent study of daily oral hydration in women with amniotic fluid volume <10% percentile showed increased amniotic fluid volume at 1 week, suggesting long-term benefit, although the study lacked an appropriate control group (LOE: 3).33
There are no studies of clinical outcomes such as fetal heart rate decelerations during labor, or neonatal outcomes. A Cochrane systematic review concluded that maternal hydration appears to increase amniotic fluid and may be beneficial in management of oligohydramnios; however, it recommended controlled trials to assess clinical outcome benefits (LOE: 3).34
TABLE 2
Effect of hydration on amniotic fluid index
| Study | Design | Population | Intervention | Outcome | Comment | LOE |
|---|---|---|---|---|---|---|
| Kilpatrick32 | RCT | N=40, AFI 2.1–6.0; population of patients referred for antenatal testing | Treatment group drank 2 L water and repeat AFI same or next day | Increase of 1.5 ± 1.4 cm (P<.01) in treatment group | Gestational ages of subjects not stated | 3 |
| Kilpatrick37 | RCT | N=40, AFI 7–24 cm, gestational 28 weeks | Treatment group instructed to drink 2 L and restricted group 0.1 L water. AFI repeated in 4–6 h | Increase of 3.0 ± 2.4 cm (P<.0001) in treatment group; decrease of 1.5 ± 2.7cm in controls (P <.02) | Subjects had normal AFI at entry | 3 |
| Flack36 | Prospective cohort | N=20, 10 w/AFI <5 cm, 10 controls AFI >7, 3rd trimester | 2 L oral water over 2 h for treatment and control groups, repeat AFI at 2 h | Increase in 3.2 cm in AFI (95% CI, 1.1–5.3) in oligohydramnios group but not in normal AFI group | Improved uterine perfusion shown by increased uterine artery velocity only in oligohydramnios group | 3 |
| Doi35 | RCT | N=84, AFI <5, at least 35 wks; randomized three maternal hydration methods (2 L oral water, hypotonic saline IV, or isotonic saline IV) | Hydration with 2 L fluid and AFI repeated in 1 h compared with controls | Significant increases in AFI in oral water and hypotonic IV groups by 3.8 cm and 2.8 cm (P<.001) respectively | IV isotonic solutions did not increase amniotic fluid volume in study population | 3 |
| RCT, randomized controlled trial; AFI, amniotic fluid index; CI, confidence interval. | ||||||
Management recommendations
The AFI has low specificity and positive predictive value for oligohydramnios, and there is scant evidence that isolated term oligohydramnios causes adverse fetal outcomes. We recommend that an AFI under 5 cm should prompt additional antenatal testing rather than immediate induction in low-risk term pregnancies (SOR: B).
Though we acknowledge the lack of high-quality studies with patient-oriented outcomes to support observation and maternal hydration, we have developed a management strategy that does not require immediate induction of labor in women with uncomplicated term pregnancies.
The following recommendations apply to women having oligohydramnios as defined by amniotic fluid volume of less than 5 cm and gestational age between 37 and 41 weeks.
Initial assessment
- Assess for premature rupture of membranes with a thorough history and a sterile speculum exam
- Reassess dating as oligohydramnios in post-dates pregnancy (>41 weeks) is an indication for induction (SOR: C)35
- Perform a nonstress test to assess fetal wellbeing
- Assess for IUGR with an ultrasound for estimated fetal weight and for the ratio of head circumference (HC) to abdominal circumference (AC). A comparison with prior ultrasounds can aid in assessing interval growth. An estimated fetal weight below the 10%, an elevated HC/AC ratio, or poor interval growth would suggest IUGR
- Arrange for an ultrasound anatomic survey for fetal anomalies, if not done previously
- Determine if preeclampsia, chronic hypertension, diabetes, or other maternal conditions associated with uteroplacental insufficiency are present.
Action steps
With any positive findings in the initial evaluation, proceed to labor induction, as the patient does not have isolated, term oligohydramnios (SOR: C). If the initial assessment is unremarkable and the AFI is less than 5, consider hydration with oral water and repeating the AFI 2 to 6 hours later (SOR: B).
Persistent oligohydramnios at term, particularly with a ripe cervix, may lead you to consider labor induction. Continued expectant management of isolated term oligohydramnios with twice weekly fetal surveillance may also be a reasonable option due to the paucity of evidence that oligohydramnios is associated with an adverse outcome in this scenario (SOR: C). Normal results with umbilical artery Doppler flow studies have been used to decrease the need for induction in high-risk pregnancies with oligohydramnios, and this technique may eventually have a role in isolated term oligohydramnios.36
It is essential that patients receive counseling and give informed consent regarding the risks and benefits of observation or induction for isolated term oligohydramnios. The ease of induction based on parity and cervical ripeness should be considered.
A primiparous woman with an unfavorable cervix who strongly desires a spontaneous, vaginal birth could be told that, although there may be a small risk for her baby, no study has demonstrated any increased long-term morbidity or mortality associated with low fluid in her situation and that labor induction may double her chance of cesarean delivery.37,38 In such a situation, an acceptable approach for mother and clinician may be rehydration followed by a repeat AFI and close follow-up with testing for fetal well-being according to the algorithm (Figure). In a practical sense, rehydration with 2 liters of oral water for oligohydramnios may be done whether or not immediate induction is chosen, as this is a safe measure that has been shown to significantly increase AFI. Alternatively, the preferred approach for a multiparous woman with a ripe cervix by Bishop score may be labor induction.
As adverse fetal outcomes have not been demonstrated in women with isolated term oligohydramnios, there is no rationale for routinely inducing labor based on an isolated finding of a so called “borderline” amniotic fluid index in the 5-to-8 range. In this situation it is appropriate to perform the initial assessment described above and may be reasonable to repeat the amniotic fluid index in 3 to 4 days to determine if true oligohydramnios has developed.
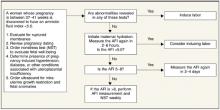
FIGURE
Assessment of the pregnant woman with oligohydramnios at term
Acknowledgments
We appreciate the assistance of George Gilson MD, Lauren Plante MD, and William Rayburn MD in manuscript review.
Corresponding author
Lawrence Leeman, MD, MPH, University of New Mexico Depts of Family and Community Medicine, Obstetrics and Gynecology, 2400 Tucker NE, 3rd floor, Albuquerque, NM 87131. E-mail: [email protected].
1. Moore TR. Clinical assessment of amniotic fluid. Clin Obstet Gynecol 1997;40:303-313.
2. Phelan JP, Smith CV, Broussard P, Small M. Amniotic fluid volume assessment with the four-quadrant technique at 36–42weeks’ gestation. J Reprod Med 1987;32:540-542.
3. Banks EH. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol 1999;180:1461-1463.
4. Casey BM. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks gestation. Am J Obstet Gynecol 2000;182:909-912.
5. Hobbins JC. Oligohydramnios and post-term pregnancy. Ob/Gyn Clinical Alert December 2002;59-60.
6. Johnson DP, Davis NR, Brown AJ. Risk of cesarean delivery after induction at term in nulliparous women with an unfavorable cervix. Am J Obstet Gynecol 2003;188:1565-1572.
7. Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 2001;345:3-8.
8. Kilpatrick SJ, Safford KL. Maternal hydration increases amniotic fluid index in women with normal amniotic fluid. Obstet Gynecol 1993;81:49-52.
9. Gilbert WM, Brace RA. Amniotic fluid volume and normal flows to and from the amniotic cavity. Seminars in Perinatology 1993;17:150-157.
10. Chandra PC, Schiavello HJ, Lewandowski MA. Effect of oral and intravenous hydration on oligohydramnios. J Reprod Med 2000;45:337-340.
11. Doi S, Osada H, Seki K, Sekiya S. Effect of maternal hydration on oligohydramnios: a comparison of three volume expansion methods. Obstet Gynecol 1998;92:525-529.
12. Flack NJ, Sepulveda W, Bower S, Fisk NM. Acute maternal hydration in third-trimester oligohydramnios: effects on amniotic fluid volume, uteroplacental perfusion, and fetal blood flow and urine output. Am J Obstet Gynecol 1995;173:1186-1191.
13. Kilpatrick SJ, Safford KL, Pomeroy T, Hoedt L, Scheerer L, Laros RK. Maternal hydration increases amniotic fluid index. Obstet Gynecol 1991;78:1098-1102.
14. Larmon JE, Ross BS. Clinical utility of amniotic fluid volume assessment. Obstet Gynecol Clin North Am 1998;25:639-661.
15. Hill LM. Oligohydramnios: sonographic diagnosis and clinical implications. Clin Obstet Gynecol 1997;40:314-327.
16. Flack NJ, Dore C, Southwell D, Kourtis P, Sepulveda W, Fisk NM. The influence of operator transducer pressure on ultrasonographic measurements of amniotic fluid volume. Am J Obstet Gynecol 1994;171:218-222.
17. Rutherford SE, Smith CV, Phelan JP, Kawakami K, Ahn MO. Four-quadrant assessment of amniotic fluid volume: interobserver and intraobserver variation. J Reprod Med 1987;32:587-589.
18. Bruner JP, Reed GW, Sarno AP, Harrington RA, Goodman MA. Intraobserver and interobserver variability of the amniotic fluid index. Am J Obstet Gynecol 1993;168:1309-1313.
19. O’Reilly-Green CP, Divon MY. Predictive value of amniotic fluid index for oligohydramnios in patients with prolonged pregnancies. J Matern Fetal Med 1996;5:218-226.
20. Chauhan SP, Magann EF, Morrison JC, Whitworth NS, Hendrix NW, Devoe LD. Ultrasonographic assessment of amniotic fluid does not reflect actual amniotic fluid volume. Am J Obstet Gynecol 1997;177:291-297.
21. Chauhan SP, Sanderson M, Hendrix NW, Magann EF, Devoe LD. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a meta-analysis. Am J Obstet Gynecol 1999;181:1473-1478.
22. Magann EF. Antenatal testing among 1001 patients at high risk: the role of ultrasonographic estimate of amniotic fluid volume. Am J Obstet Gynecol 1999;180:1330-1336.
23. Magann EF. Does an amniotic fluid index of 5 cm necessitate delivery in high-risk pregnancies? A case-control study. Am J Obstet Gynecol 1999;180:1354-1359.
24. Nisell H, Ek S. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol. 2000;182:750-751.
25. Conway DL, et al. Isolated oligohydramnios in the term pregnancy: Is it a clinical entity. J Matern Fetal Med 1998;7:197-200.
26. Garmel SH, Chelmow D, Sha SJ, Roan JT, D’Alton ME. Oligohydramnios and the appropriately grown fetus. Am J Perinatol 1997;14:359-363.
27. Kreiser D, el-Sayed YY, Sorem KA, Chitkara U, Holbrook RH, Jr, Druzin ML. Decreased amniotic fluid index in low-risk pregnancy. J Reprod Med 2001;46:743-746.
28. Roberts D, Nwosu EC, Walkinshaw SA. The fetal outcome in pregnancies with isolated reduced amniotic fluid volume in the third trimester. J Perinat Med 1998;26:390-395.
29. Rainford M, Adair R, Scialli AR, Ghidini A, Spong CY. Amniotic fluid index in the uncomplicated term pregnancy. Prediction of outcome. J Reprod Med 2001;46:589-592.
30. Zhang J, Troendle J, Meikle S, Klebanoff MA, Rayburn WF. Isolated oligohydramnios is not associated with adverse perinatal outcomes. BJOG 2004;111:220-225.
31. Conway DL, Groth S, Adkins WB, Langer O. Management of isolated oligohyramnios in the term pregnancy: a randomized clinical trial. Am J Obstet Gynecol 2000;182:S21.-
32. Oosterhof H, Haak MC, Aarnoudse JG. Acute maternal rehydration increases the urine production rate in the near-term human fetus. Am J Obstet Gynecol 2000;183:226-229.
33. Fait G, Pauzner D, Gull I, Lessing JB, Jaffa AJ, Wolman I. Effect of 1 week or oral hydration on the amniotic fluid index. J Reprod Med 2003;48:187-190.
34. Hofmeyr GJ, Gulmezoglu AM. Maternal hydration for increasing amniotic fluid volume in oligohydramnios and normal amniotic fluid volute (Cochrane Review). In: The Cochrane Library. Issue 4, 2002. Oxford: Update Software.
35. Sherer DM, Langer O. Oligohydramnios: use and misuse in clinical management. Ultrasound Obstet Gynecol 2001;18:411-419.
36. Carroll BC, Bruner JP. Umbilical artery Doppler velocimetry in pregnancies complicated by oligohydramnios. J Reprod Med 2000;45:562-566.
37. Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol 1999;94:600-607.
38. Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol 1999;180:628-633.
- Isolated term oligohydramnios, as defined by an amniotic fluid index (AFI) of less than 5 cm, has not been shown to be associated with poor maternal or fetal outcomes. Management may be individualized based on factors such as parity, cervical ripeness, and patient preference (SOR: B).
- Maternal hydration with oral water has been shown to increase AFI in a few hours, likely due to improved uteroplacental perfusion. This is a reasonable alternative to immediate labor induction in women with isolated term oligohydramnios (SOR: B).
- An isolated finding of a so-called “border-line” AFI (5–8 cm) is not an indication for labor induction (SOR: B).
Family physicians providing maternity care often face a scenario in which an otherwise low-risk, term patient is incidentally noted to have a low amniotic fluid index (AFI). Common reasons for obtaining an AFI in a woman with a low-risk pregnancy include evaluation of decreased fetal movement, spontaneous variable decelerations during monitoring to evaluate for labor, or an ultrasound evaluation for fundal height measurements discordant with gestational age. How should “isolated” oligohydramnios—an AFI <5 cm—be interpreted, and should immediate induction be recommended for such patients?
Oligohydramnios occurs in about 1% to 5% of pregnancies at term.1,2 Because adverse outcomes occur in high-risk pregnancies complicated by low amniotic fluid volume, oligohydramnios commonly prompts labor induction.1,3,4 At one university center, oligohydramnios is now the leading indication for labor induction.5 Many centers may even induce labor when the AFI is between 5 cm and 8 cm, the so-called borderline AFI.3
Labor induction increases the use of cesarean delivery, particularly for the primiparous woman with an unripe cervix.6 Recent studies questioning the safety of labor induction in women who have had a cesarean may increase the number of elective repeat cesarean procedures when delivery is believed indicated for oligohydramnios.7 (See Underlying causes of oligohydramnios.)
By the second trimester, amniotic fluid is being produced primarily through fetal urine production and is primarily resorbed through fetal swallowing. Significant amounts of amniotic fluid are also produced and resorbed by the fetal lung and directly resorbed from the amniotic cavity by the placenta.8,9 Amniotic fluid volume is affected by the status of maternal hydration and maternal plasma osmolality.10-13
Acute oligohydramnios may occur from ruptured membranes, usually diagnosed by clinical signs and vaginal fluid with altered pH and a ferning pattern on microscopic exam.
Chronic oligohydramnios arises from prerenal, renal, and postrenal causes. The latter 2 groups reflect fetal kidney and urogenital abnormalities, which directly decrease fetal amniotic fluid production. Uteroplacental insufficiency is the most common cause of prerenal oligohydramnios, and the decreased amniotic fluid is a direct result of decreased fetal renal perfusion.14 Uteroplacental insufficiency may result in intrauterine growth restriction as the fetus shunts blood away from the growing torso and limbs and to vital organs such as the brain. Preeclampsia and postdate pregnancies both involve pathologic changes in the placenta that may result in uteroplacental insufficiency and oligohydramnios.
Oligohydramnios is difficult to assess
True oligohydramnios can be difficult to confirm due to the questionable accuracy of amniotic fluid measurement by ultrasound. There is controversy, for example, about whether (and how) to include pockets of amniotic fluid containing umbilical cord.15 The AFI was introduced in 19872 to replace the 2 cm “pocket technique” of fluid assessment, and studies continue to question to what extent the AFI reflects actual amniotic fluid volume.
AFI measurements may vary with the amount of pressure applied to the abdomen and with fetal position or movement.16
Serial measurements taken by the same ultrasound operator have been shown to differ from the true volume by 1 cm, or 10.8%; serial measurements taken by multiple operators have differed by as much as 2 cm, or 15.4%.17,18
O’Reilly-Green compared the diagnosis of oligohydramnios in 449 post-term patients with actual amniotic fluid volume measured at rupture of membranes.19 They found a positive predictive value of 50% for oligohydramnios at an AFI of 5 cm as the lower limit of normal. A study of 144 third trimester patients using the dye-dilution technique found that, to achieve 95% confidence for ruling out oligohydramnios, a cutoff AFI of 30 cm would need to be used, a value consistent with polyhydramnios.20
What is the association between oligohydramnios and poor fetal outcomes?
A number of studies over the past 15 years have shown an association between oligohydramnios and poor fetal outcomes. These were predominantly retrospective studies, which failed to control for the presence of factors known to be associated with oligohydramnios such as intrauterine growth restriction (IUGR) and urogenital malformations.
No studies have directly addressed whether labor induction improves outcomes. A meta-analysis of 18 studies examining outcomes of pregnancies with AFI <5 cm found an increased risk of cesarean delivery for fetal distress and low Apgar scores at 5 minutes. Most of these studies, however, had high-risk patients including IUGR (level of evidence [LOE]: 2).21
A recent study of high-risk patients failed to detect a difference in the incidence of nonreactive nonstress tests, meconium-stained amniotic fluid cesarean delivery for fetal distress, low Apgar scores, or infants with a cord pH of <7.10 when oligohydramnios (AFI <5.0 cm) was present (LOE: 1).2 The patients with oligohydramnios were all induced, while many of the other high-risk patients were expectantly managed. The study therefore provides no guidance on the safety of expectant management for patients with oligohydramnios. To eliminate the potential effect of induction versus expectant management the same authors performed a case-control study of 79 high-risk women with AFI <5 cm matched to 79 women with the same high-risk pregnancy complication who had an AFI >5 cm at the time of induction (LOE: 2).23 They failed to detect any significant differences in neonatal outcomes between the groups.
Studies of the “borderline” AFI (between 5 cm and 8 cm) may also demonstrate an association with adverse neonatal outcomes if researchers include fetuses with IUGR or malformations. In one retrospective case review of 214 women with AFI of 5 cm to 10 cm, the only statistically significant finding was an association with IUGR.3 The authors recommended antepartum surveillance twice a week for mothers with borderline AFI, but they did not comment on induction (LOE: 2). Correspondence regarding this study argued that this recommendation was not supported by the evidence and would lead to unnecessary antenatal testing.24
Studies of isolated oligohydramnios
Investigators have conducted studies (Table 1) excluding fetuses with intrauterine growth restriction or anomalies to try to determine if isolated oligohydramnios is associated with poorer outcomes.25-30
Rainford’s study of outcomes in exclusively term, low-risk patients failed to show significant outcome differences in Apgar scores, NICU admissions, or rates of cesarean delivery for non-reassuring fetal heart rate monitoring (LOE: 2).29 This study was limited due to its retrospective design. The authors comment that the relatively good outcomes in the oligohydramnios group may be due to the widespread practice of inducing such patients.
In a case-control study by Conway, 183 low-risk, term parturients with oligohydramnios were matched to 183 women of similar gestational age and parity who presented in spontaneous labor. The patients with isolated oligohydramnios were induced and showed an increased cesarean delivery rate. The increased rate of cesarean delivery was not due to nonreassuring fetal surveillance and was attributed to the induction process (LOE: 2).25
An analysis of woman diagnosed with isolated oligohydramnios (AFI <5) at any gestational age in the multicenter prospective RADIUS trial demonstrated similar perinatal outcomes and fetal growth compared with pregnancies with a normal amniotic fluid (LOE: 2).30
The only randomized clinical trial of labor induction vs expectant management for term isolated oligohydramnios showed similar outcomes in each group. But this study was small (n=61) and has only been published as an abstract.31
TABLE 1
Isolated oligohydramnios and perinatal outcomes
| Study | Design | Study number n vs controls | Patient-oriented outcomes | Comment | LOE | |
|---|---|---|---|---|---|---|
| Population | Significant findings | Non-significant findings | ||||
| Garmel19 | Prospective cohort | N=187 | Increased preterm birth (OR=3.23; 95% CI, 1.4–7.3) in oligohydramnios group | IUGR, asphyxia, death, NICU admit | Delivery recommended at 37 weeks | 2 |
| 17–37 week with subnormal EFW (>10%) | 65 AFI <8 cm vs 122 AFI >8 cm | |||||
| Conway18 | Prospective cohort | N=366 | Increased CS rate (OR=2.7 95% CI, 1.3–5.4) in oligohydramnios group | CS for fetal distress; all neonatal outcomes | Treatment group induced, controls spontaneous | 2 |
| Term, isolated oligohydramnios undergoing induction | 183 AFI <5 cm vs 183 AFI >5 cm | |||||
| Roberts21 | Prospective cohort | N=206 | Increased IUGR (OR=5.2; 95% CI, 1.6–22), induction (OR=34.4, 95% CI, 4–1425.5), NICU admit (OR=9.8; 95% CI, 1.3–432) | Fetal distress requiring CS | Used >5%ile to exclude IUGR. Included some high-risk pts (diabetes or hypertension) | 2 |
| 3rd trimester, isolated oligohydramnios | 103 AFI 3%ile (N=103) vs matched control | |||||
| Rainford22 | Retrospective cohort | N=232 | Induction rate for AFI <5 = 98% vs 51% AFI >5 P<.001; increased meconium staining in controls without oligohydramnios | NICU 2 admissions, 5-minute Apgar scores | 2 | |
| 37–41 week, low-risk. AFI within 4 days of delivery | AFI <5 (n=44) vs >5 (n=188) | |||||
| Zhang23 | Retrospective nested cohort | N=6657 | Malpresentation (RR=3.5, 95% CI 1.8–6.60) | Fetal growth, CS, low Apgar, overall neonatal morbidity | Benefit of routine ultrasound was the primary study outcome study endpoint | 2 |
| Term or near-term, low-risk | AFI <5 (n=86) vs >5 (n=6571) | |||||
| AFI, amniotic fluid index; CI, confidence interval; CS, cesarean section; EFW, estimated fetal weight; IUGR, intrauterine growth restriction; LOE, level of evidence; NICU, neonatal intensive care unit; OR, odds ratio; RR, relative risk. | ||||||
Effect of maternal hydration
Maternal hydration status and plasma osmolality have an affect on amniotic fluid volume (Table 2). Maternal hydration with oral water or intravenous hypotonic solutions has been shown to increase amniotic fluid volume.8,11-13 Oral hydration with hypotonic fluid has been demonstrated to increase fetal urine production in one observational study.32 Another observational study demonstrated increased amniotic fluid volume and uteroplacental perfusion without alteration of fetal urine production suggesting the possibility that transmembranous fluid shifts from the placenta to the amniotic cavity may be involved.12
Two small, randomized controlled trials (RCTs) demonstrated an increase in amniotic fluid volume in women with oligohydramnios after oral hydration.11,13 Doi demonstrated significant increases in AFI in women with oligohydramnios beyond 35 weeks when given oral hydration with free water (increase of 3.8 cm ± 1.9; P<. 001) or hypotonic intravenous solution (increase of 2.8 cm ± 1.9; P<.001) (LOE: 3).11 Interestingly, this study did not demonstrate an increase in amniotic fluid volume with intravenous hydration with isotonic fluid.
Kirkpatrick demonstrated a 30% increase in amniotic fluid compared with controls in women of unspecified gestational age with oligohydramnios given 2 liters of oral water 2 to 5 hours before repeat amniotic fluid index (LOE: 3).13
A randomized trial in women with normal amniotic fluid demonstrated a 16% increase in amniotic fluid index 4 to 6 hours after hydration with 2 liters of oral water, compared with an 8% decrease after fluid restriction during the same period.8
A recent study of daily oral hydration in women with amniotic fluid volume <10% percentile showed increased amniotic fluid volume at 1 week, suggesting long-term benefit, although the study lacked an appropriate control group (LOE: 3).33
There are no studies of clinical outcomes such as fetal heart rate decelerations during labor, or neonatal outcomes. A Cochrane systematic review concluded that maternal hydration appears to increase amniotic fluid and may be beneficial in management of oligohydramnios; however, it recommended controlled trials to assess clinical outcome benefits (LOE: 3).34
TABLE 2
Effect of hydration on amniotic fluid index
| Study | Design | Population | Intervention | Outcome | Comment | LOE |
|---|---|---|---|---|---|---|
| Kilpatrick32 | RCT | N=40, AFI 2.1–6.0; population of patients referred for antenatal testing | Treatment group drank 2 L water and repeat AFI same or next day | Increase of 1.5 ± 1.4 cm (P<.01) in treatment group | Gestational ages of subjects not stated | 3 |
| Kilpatrick37 | RCT | N=40, AFI 7–24 cm, gestational 28 weeks | Treatment group instructed to drink 2 L and restricted group 0.1 L water. AFI repeated in 4–6 h | Increase of 3.0 ± 2.4 cm (P<.0001) in treatment group; decrease of 1.5 ± 2.7cm in controls (P <.02) | Subjects had normal AFI at entry | 3 |
| Flack36 | Prospective cohort | N=20, 10 w/AFI <5 cm, 10 controls AFI >7, 3rd trimester | 2 L oral water over 2 h for treatment and control groups, repeat AFI at 2 h | Increase in 3.2 cm in AFI (95% CI, 1.1–5.3) in oligohydramnios group but not in normal AFI group | Improved uterine perfusion shown by increased uterine artery velocity only in oligohydramnios group | 3 |
| Doi35 | RCT | N=84, AFI <5, at least 35 wks; randomized three maternal hydration methods (2 L oral water, hypotonic saline IV, or isotonic saline IV) | Hydration with 2 L fluid and AFI repeated in 1 h compared with controls | Significant increases in AFI in oral water and hypotonic IV groups by 3.8 cm and 2.8 cm (P<.001) respectively | IV isotonic solutions did not increase amniotic fluid volume in study population | 3 |
| RCT, randomized controlled trial; AFI, amniotic fluid index; CI, confidence interval. | ||||||
Management recommendations
The AFI has low specificity and positive predictive value for oligohydramnios, and there is scant evidence that isolated term oligohydramnios causes adverse fetal outcomes. We recommend that an AFI under 5 cm should prompt additional antenatal testing rather than immediate induction in low-risk term pregnancies (SOR: B).
Though we acknowledge the lack of high-quality studies with patient-oriented outcomes to support observation and maternal hydration, we have developed a management strategy that does not require immediate induction of labor in women with uncomplicated term pregnancies.
The following recommendations apply to women having oligohydramnios as defined by amniotic fluid volume of less than 5 cm and gestational age between 37 and 41 weeks.
Initial assessment
- Assess for premature rupture of membranes with a thorough history and a sterile speculum exam
- Reassess dating as oligohydramnios in post-dates pregnancy (>41 weeks) is an indication for induction (SOR: C)35
- Perform a nonstress test to assess fetal wellbeing
- Assess for IUGR with an ultrasound for estimated fetal weight and for the ratio of head circumference (HC) to abdominal circumference (AC). A comparison with prior ultrasounds can aid in assessing interval growth. An estimated fetal weight below the 10%, an elevated HC/AC ratio, or poor interval growth would suggest IUGR
- Arrange for an ultrasound anatomic survey for fetal anomalies, if not done previously
- Determine if preeclampsia, chronic hypertension, diabetes, or other maternal conditions associated with uteroplacental insufficiency are present.
Action steps
With any positive findings in the initial evaluation, proceed to labor induction, as the patient does not have isolated, term oligohydramnios (SOR: C). If the initial assessment is unremarkable and the AFI is less than 5, consider hydration with oral water and repeating the AFI 2 to 6 hours later (SOR: B).
Persistent oligohydramnios at term, particularly with a ripe cervix, may lead you to consider labor induction. Continued expectant management of isolated term oligohydramnios with twice weekly fetal surveillance may also be a reasonable option due to the paucity of evidence that oligohydramnios is associated with an adverse outcome in this scenario (SOR: C). Normal results with umbilical artery Doppler flow studies have been used to decrease the need for induction in high-risk pregnancies with oligohydramnios, and this technique may eventually have a role in isolated term oligohydramnios.36
It is essential that patients receive counseling and give informed consent regarding the risks and benefits of observation or induction for isolated term oligohydramnios. The ease of induction based on parity and cervical ripeness should be considered.
A primiparous woman with an unfavorable cervix who strongly desires a spontaneous, vaginal birth could be told that, although there may be a small risk for her baby, no study has demonstrated any increased long-term morbidity or mortality associated with low fluid in her situation and that labor induction may double her chance of cesarean delivery.37,38 In such a situation, an acceptable approach for mother and clinician may be rehydration followed by a repeat AFI and close follow-up with testing for fetal well-being according to the algorithm (Figure). In a practical sense, rehydration with 2 liters of oral water for oligohydramnios may be done whether or not immediate induction is chosen, as this is a safe measure that has been shown to significantly increase AFI. Alternatively, the preferred approach for a multiparous woman with a ripe cervix by Bishop score may be labor induction.
As adverse fetal outcomes have not been demonstrated in women with isolated term oligohydramnios, there is no rationale for routinely inducing labor based on an isolated finding of a so called “borderline” amniotic fluid index in the 5-to-8 range. In this situation it is appropriate to perform the initial assessment described above and may be reasonable to repeat the amniotic fluid index in 3 to 4 days to determine if true oligohydramnios has developed.
FIGURE
Assessment of the pregnant woman with oligohydramnios at term
Acknowledgments
We appreciate the assistance of George Gilson MD, Lauren Plante MD, and William Rayburn MD in manuscript review.
Corresponding author
Lawrence Leeman, MD, MPH, University of New Mexico Depts of Family and Community Medicine, Obstetrics and Gynecology, 2400 Tucker NE, 3rd floor, Albuquerque, NM 87131. E-mail: [email protected].
- Isolated term oligohydramnios, as defined by an amniotic fluid index (AFI) of less than 5 cm, has not been shown to be associated with poor maternal or fetal outcomes. Management may be individualized based on factors such as parity, cervical ripeness, and patient preference (SOR: B).
- Maternal hydration with oral water has been shown to increase AFI in a few hours, likely due to improved uteroplacental perfusion. This is a reasonable alternative to immediate labor induction in women with isolated term oligohydramnios (SOR: B).
- An isolated finding of a so-called “border-line” AFI (5–8 cm) is not an indication for labor induction (SOR: B).
Family physicians providing maternity care often face a scenario in which an otherwise low-risk, term patient is incidentally noted to have a low amniotic fluid index (AFI). Common reasons for obtaining an AFI in a woman with a low-risk pregnancy include evaluation of decreased fetal movement, spontaneous variable decelerations during monitoring to evaluate for labor, or an ultrasound evaluation for fundal height measurements discordant with gestational age. How should “isolated” oligohydramnios—an AFI <5 cm—be interpreted, and should immediate induction be recommended for such patients?
Oligohydramnios occurs in about 1% to 5% of pregnancies at term.1,2 Because adverse outcomes occur in high-risk pregnancies complicated by low amniotic fluid volume, oligohydramnios commonly prompts labor induction.1,3,4 At one university center, oligohydramnios is now the leading indication for labor induction.5 Many centers may even induce labor when the AFI is between 5 cm and 8 cm, the so-called borderline AFI.3
Labor induction increases the use of cesarean delivery, particularly for the primiparous woman with an unripe cervix.6 Recent studies questioning the safety of labor induction in women who have had a cesarean may increase the number of elective repeat cesarean procedures when delivery is believed indicated for oligohydramnios.7 (See Underlying causes of oligohydramnios.)
By the second trimester, amniotic fluid is being produced primarily through fetal urine production and is primarily resorbed through fetal swallowing. Significant amounts of amniotic fluid are also produced and resorbed by the fetal lung and directly resorbed from the amniotic cavity by the placenta.8,9 Amniotic fluid volume is affected by the status of maternal hydration and maternal plasma osmolality.10-13
Acute oligohydramnios may occur from ruptured membranes, usually diagnosed by clinical signs and vaginal fluid with altered pH and a ferning pattern on microscopic exam.
Chronic oligohydramnios arises from prerenal, renal, and postrenal causes. The latter 2 groups reflect fetal kidney and urogenital abnormalities, which directly decrease fetal amniotic fluid production. Uteroplacental insufficiency is the most common cause of prerenal oligohydramnios, and the decreased amniotic fluid is a direct result of decreased fetal renal perfusion.14 Uteroplacental insufficiency may result in intrauterine growth restriction as the fetus shunts blood away from the growing torso and limbs and to vital organs such as the brain. Preeclampsia and postdate pregnancies both involve pathologic changes in the placenta that may result in uteroplacental insufficiency and oligohydramnios.
Oligohydramnios is difficult to assess
True oligohydramnios can be difficult to confirm due to the questionable accuracy of amniotic fluid measurement by ultrasound. There is controversy, for example, about whether (and how) to include pockets of amniotic fluid containing umbilical cord.15 The AFI was introduced in 19872 to replace the 2 cm “pocket technique” of fluid assessment, and studies continue to question to what extent the AFI reflects actual amniotic fluid volume.
AFI measurements may vary with the amount of pressure applied to the abdomen and with fetal position or movement.16
Serial measurements taken by the same ultrasound operator have been shown to differ from the true volume by 1 cm, or 10.8%; serial measurements taken by multiple operators have differed by as much as 2 cm, or 15.4%.17,18
O’Reilly-Green compared the diagnosis of oligohydramnios in 449 post-term patients with actual amniotic fluid volume measured at rupture of membranes.19 They found a positive predictive value of 50% for oligohydramnios at an AFI of 5 cm as the lower limit of normal. A study of 144 third trimester patients using the dye-dilution technique found that, to achieve 95% confidence for ruling out oligohydramnios, a cutoff AFI of 30 cm would need to be used, a value consistent with polyhydramnios.20
What is the association between oligohydramnios and poor fetal outcomes?
A number of studies over the past 15 years have shown an association between oligohydramnios and poor fetal outcomes. These were predominantly retrospective studies, which failed to control for the presence of factors known to be associated with oligohydramnios such as intrauterine growth restriction (IUGR) and urogenital malformations.
No studies have directly addressed whether labor induction improves outcomes. A meta-analysis of 18 studies examining outcomes of pregnancies with AFI <5 cm found an increased risk of cesarean delivery for fetal distress and low Apgar scores at 5 minutes. Most of these studies, however, had high-risk patients including IUGR (level of evidence [LOE]: 2).21
A recent study of high-risk patients failed to detect a difference in the incidence of nonreactive nonstress tests, meconium-stained amniotic fluid cesarean delivery for fetal distress, low Apgar scores, or infants with a cord pH of <7.10 when oligohydramnios (AFI <5.0 cm) was present (LOE: 1).2 The patients with oligohydramnios were all induced, while many of the other high-risk patients were expectantly managed. The study therefore provides no guidance on the safety of expectant management for patients with oligohydramnios. To eliminate the potential effect of induction versus expectant management the same authors performed a case-control study of 79 high-risk women with AFI <5 cm matched to 79 women with the same high-risk pregnancy complication who had an AFI >5 cm at the time of induction (LOE: 2).23 They failed to detect any significant differences in neonatal outcomes between the groups.
Studies of the “borderline” AFI (between 5 cm and 8 cm) may also demonstrate an association with adverse neonatal outcomes if researchers include fetuses with IUGR or malformations. In one retrospective case review of 214 women with AFI of 5 cm to 10 cm, the only statistically significant finding was an association with IUGR.3 The authors recommended antepartum surveillance twice a week for mothers with borderline AFI, but they did not comment on induction (LOE: 2). Correspondence regarding this study argued that this recommendation was not supported by the evidence and would lead to unnecessary antenatal testing.24
Studies of isolated oligohydramnios
Investigators have conducted studies (Table 1) excluding fetuses with intrauterine growth restriction or anomalies to try to determine if isolated oligohydramnios is associated with poorer outcomes.25-30
Rainford’s study of outcomes in exclusively term, low-risk patients failed to show significant outcome differences in Apgar scores, NICU admissions, or rates of cesarean delivery for non-reassuring fetal heart rate monitoring (LOE: 2).29 This study was limited due to its retrospective design. The authors comment that the relatively good outcomes in the oligohydramnios group may be due to the widespread practice of inducing such patients.
In a case-control study by Conway, 183 low-risk, term parturients with oligohydramnios were matched to 183 women of similar gestational age and parity who presented in spontaneous labor. The patients with isolated oligohydramnios were induced and showed an increased cesarean delivery rate. The increased rate of cesarean delivery was not due to nonreassuring fetal surveillance and was attributed to the induction process (LOE: 2).25
An analysis of woman diagnosed with isolated oligohydramnios (AFI <5) at any gestational age in the multicenter prospective RADIUS trial demonstrated similar perinatal outcomes and fetal growth compared with pregnancies with a normal amniotic fluid (LOE: 2).30
The only randomized clinical trial of labor induction vs expectant management for term isolated oligohydramnios showed similar outcomes in each group. But this study was small (n=61) and has only been published as an abstract.31
TABLE 1
Isolated oligohydramnios and perinatal outcomes
| Study | Design | Study number n vs controls | Patient-oriented outcomes | Comment | LOE | |
|---|---|---|---|---|---|---|
| Population | Significant findings | Non-significant findings | ||||
| Garmel19 | Prospective cohort | N=187 | Increased preterm birth (OR=3.23; 95% CI, 1.4–7.3) in oligohydramnios group | IUGR, asphyxia, death, NICU admit | Delivery recommended at 37 weeks | 2 |
| 17–37 week with subnormal EFW (>10%) | 65 AFI <8 cm vs 122 AFI >8 cm | |||||
| Conway18 | Prospective cohort | N=366 | Increased CS rate (OR=2.7 95% CI, 1.3–5.4) in oligohydramnios group | CS for fetal distress; all neonatal outcomes | Treatment group induced, controls spontaneous | 2 |
| Term, isolated oligohydramnios undergoing induction | 183 AFI <5 cm vs 183 AFI >5 cm | |||||
| Roberts21 | Prospective cohort | N=206 | Increased IUGR (OR=5.2; 95% CI, 1.6–22), induction (OR=34.4, 95% CI, 4–1425.5), NICU admit (OR=9.8; 95% CI, 1.3–432) | Fetal distress requiring CS | Used >5%ile to exclude IUGR. Included some high-risk pts (diabetes or hypertension) | 2 |
| 3rd trimester, isolated oligohydramnios | 103 AFI 3%ile (N=103) vs matched control | |||||
| Rainford22 | Retrospective cohort | N=232 | Induction rate for AFI <5 = 98% vs 51% AFI >5 P<.001; increased meconium staining in controls without oligohydramnios | NICU 2 admissions, 5-minute Apgar scores | 2 | |
| 37–41 week, low-risk. AFI within 4 days of delivery | AFI <5 (n=44) vs >5 (n=188) | |||||
| Zhang23 | Retrospective nested cohort | N=6657 | Malpresentation (RR=3.5, 95% CI 1.8–6.60) | Fetal growth, CS, low Apgar, overall neonatal morbidity | Benefit of routine ultrasound was the primary study outcome study endpoint | 2 |
| Term or near-term, low-risk | AFI <5 (n=86) vs >5 (n=6571) | |||||
| AFI, amniotic fluid index; CI, confidence interval; CS, cesarean section; EFW, estimated fetal weight; IUGR, intrauterine growth restriction; LOE, level of evidence; NICU, neonatal intensive care unit; OR, odds ratio; RR, relative risk. | ||||||
Effect of maternal hydration
Maternal hydration status and plasma osmolality have an affect on amniotic fluid volume (Table 2). Maternal hydration with oral water or intravenous hypotonic solutions has been shown to increase amniotic fluid volume.8,11-13 Oral hydration with hypotonic fluid has been demonstrated to increase fetal urine production in one observational study.32 Another observational study demonstrated increased amniotic fluid volume and uteroplacental perfusion without alteration of fetal urine production suggesting the possibility that transmembranous fluid shifts from the placenta to the amniotic cavity may be involved.12
Two small, randomized controlled trials (RCTs) demonstrated an increase in amniotic fluid volume in women with oligohydramnios after oral hydration.11,13 Doi demonstrated significant increases in AFI in women with oligohydramnios beyond 35 weeks when given oral hydration with free water (increase of 3.8 cm ± 1.9; P<. 001) or hypotonic intravenous solution (increase of 2.8 cm ± 1.9; P<.001) (LOE: 3).11 Interestingly, this study did not demonstrate an increase in amniotic fluid volume with intravenous hydration with isotonic fluid.
Kirkpatrick demonstrated a 30% increase in amniotic fluid compared with controls in women of unspecified gestational age with oligohydramnios given 2 liters of oral water 2 to 5 hours before repeat amniotic fluid index (LOE: 3).13
A randomized trial in women with normal amniotic fluid demonstrated a 16% increase in amniotic fluid index 4 to 6 hours after hydration with 2 liters of oral water, compared with an 8% decrease after fluid restriction during the same period.8
A recent study of daily oral hydration in women with amniotic fluid volume <10% percentile showed increased amniotic fluid volume at 1 week, suggesting long-term benefit, although the study lacked an appropriate control group (LOE: 3).33
There are no studies of clinical outcomes such as fetal heart rate decelerations during labor, or neonatal outcomes. A Cochrane systematic review concluded that maternal hydration appears to increase amniotic fluid and may be beneficial in management of oligohydramnios; however, it recommended controlled trials to assess clinical outcome benefits (LOE: 3).34
TABLE 2
Effect of hydration on amniotic fluid index
| Study | Design | Population | Intervention | Outcome | Comment | LOE |
|---|---|---|---|---|---|---|
| Kilpatrick32 | RCT | N=40, AFI 2.1–6.0; population of patients referred for antenatal testing | Treatment group drank 2 L water and repeat AFI same or next day | Increase of 1.5 ± 1.4 cm (P<.01) in treatment group | Gestational ages of subjects not stated | 3 |
| Kilpatrick37 | RCT | N=40, AFI 7–24 cm, gestational 28 weeks | Treatment group instructed to drink 2 L and restricted group 0.1 L water. AFI repeated in 4–6 h | Increase of 3.0 ± 2.4 cm (P<.0001) in treatment group; decrease of 1.5 ± 2.7cm in controls (P <.02) | Subjects had normal AFI at entry | 3 |
| Flack36 | Prospective cohort | N=20, 10 w/AFI <5 cm, 10 controls AFI >7, 3rd trimester | 2 L oral water over 2 h for treatment and control groups, repeat AFI at 2 h | Increase in 3.2 cm in AFI (95% CI, 1.1–5.3) in oligohydramnios group but not in normal AFI group | Improved uterine perfusion shown by increased uterine artery velocity only in oligohydramnios group | 3 |
| Doi35 | RCT | N=84, AFI <5, at least 35 wks; randomized three maternal hydration methods (2 L oral water, hypotonic saline IV, or isotonic saline IV) | Hydration with 2 L fluid and AFI repeated in 1 h compared with controls | Significant increases in AFI in oral water and hypotonic IV groups by 3.8 cm and 2.8 cm (P<.001) respectively | IV isotonic solutions did not increase amniotic fluid volume in study population | 3 |
| RCT, randomized controlled trial; AFI, amniotic fluid index; CI, confidence interval. | ||||||
Management recommendations
The AFI has low specificity and positive predictive value for oligohydramnios, and there is scant evidence that isolated term oligohydramnios causes adverse fetal outcomes. We recommend that an AFI under 5 cm should prompt additional antenatal testing rather than immediate induction in low-risk term pregnancies (SOR: B).
Though we acknowledge the lack of high-quality studies with patient-oriented outcomes to support observation and maternal hydration, we have developed a management strategy that does not require immediate induction of labor in women with uncomplicated term pregnancies.
The following recommendations apply to women having oligohydramnios as defined by amniotic fluid volume of less than 5 cm and gestational age between 37 and 41 weeks.
Initial assessment
- Assess for premature rupture of membranes with a thorough history and a sterile speculum exam
- Reassess dating as oligohydramnios in post-dates pregnancy (>41 weeks) is an indication for induction (SOR: C)35
- Perform a nonstress test to assess fetal wellbeing
- Assess for IUGR with an ultrasound for estimated fetal weight and for the ratio of head circumference (HC) to abdominal circumference (AC). A comparison with prior ultrasounds can aid in assessing interval growth. An estimated fetal weight below the 10%, an elevated HC/AC ratio, or poor interval growth would suggest IUGR
- Arrange for an ultrasound anatomic survey for fetal anomalies, if not done previously
- Determine if preeclampsia, chronic hypertension, diabetes, or other maternal conditions associated with uteroplacental insufficiency are present.
Action steps
With any positive findings in the initial evaluation, proceed to labor induction, as the patient does not have isolated, term oligohydramnios (SOR: C). If the initial assessment is unremarkable and the AFI is less than 5, consider hydration with oral water and repeating the AFI 2 to 6 hours later (SOR: B).
Persistent oligohydramnios at term, particularly with a ripe cervix, may lead you to consider labor induction. Continued expectant management of isolated term oligohydramnios with twice weekly fetal surveillance may also be a reasonable option due to the paucity of evidence that oligohydramnios is associated with an adverse outcome in this scenario (SOR: C). Normal results with umbilical artery Doppler flow studies have been used to decrease the need for induction in high-risk pregnancies with oligohydramnios, and this technique may eventually have a role in isolated term oligohydramnios.36
It is essential that patients receive counseling and give informed consent regarding the risks and benefits of observation or induction for isolated term oligohydramnios. The ease of induction based on parity and cervical ripeness should be considered.
A primiparous woman with an unfavorable cervix who strongly desires a spontaneous, vaginal birth could be told that, although there may be a small risk for her baby, no study has demonstrated any increased long-term morbidity or mortality associated with low fluid in her situation and that labor induction may double her chance of cesarean delivery.37,38 In such a situation, an acceptable approach for mother and clinician may be rehydration followed by a repeat AFI and close follow-up with testing for fetal well-being according to the algorithm (Figure). In a practical sense, rehydration with 2 liters of oral water for oligohydramnios may be done whether or not immediate induction is chosen, as this is a safe measure that has been shown to significantly increase AFI. Alternatively, the preferred approach for a multiparous woman with a ripe cervix by Bishop score may be labor induction.
As adverse fetal outcomes have not been demonstrated in women with isolated term oligohydramnios, there is no rationale for routinely inducing labor based on an isolated finding of a so called “borderline” amniotic fluid index in the 5-to-8 range. In this situation it is appropriate to perform the initial assessment described above and may be reasonable to repeat the amniotic fluid index in 3 to 4 days to determine if true oligohydramnios has developed.
FIGURE
Assessment of the pregnant woman with oligohydramnios at term
Acknowledgments
We appreciate the assistance of George Gilson MD, Lauren Plante MD, and William Rayburn MD in manuscript review.
Corresponding author
Lawrence Leeman, MD, MPH, University of New Mexico Depts of Family and Community Medicine, Obstetrics and Gynecology, 2400 Tucker NE, 3rd floor, Albuquerque, NM 87131. E-mail: [email protected].
1. Moore TR. Clinical assessment of amniotic fluid. Clin Obstet Gynecol 1997;40:303-313.
2. Phelan JP, Smith CV, Broussard P, Small M. Amniotic fluid volume assessment with the four-quadrant technique at 36–42weeks’ gestation. J Reprod Med 1987;32:540-542.
3. Banks EH. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol 1999;180:1461-1463.
4. Casey BM. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks gestation. Am J Obstet Gynecol 2000;182:909-912.
5. Hobbins JC. Oligohydramnios and post-term pregnancy. Ob/Gyn Clinical Alert December 2002;59-60.
6. Johnson DP, Davis NR, Brown AJ. Risk of cesarean delivery after induction at term in nulliparous women with an unfavorable cervix. Am J Obstet Gynecol 2003;188:1565-1572.
7. Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 2001;345:3-8.
8. Kilpatrick SJ, Safford KL. Maternal hydration increases amniotic fluid index in women with normal amniotic fluid. Obstet Gynecol 1993;81:49-52.
9. Gilbert WM, Brace RA. Amniotic fluid volume and normal flows to and from the amniotic cavity. Seminars in Perinatology 1993;17:150-157.
10. Chandra PC, Schiavello HJ, Lewandowski MA. Effect of oral and intravenous hydration on oligohydramnios. J Reprod Med 2000;45:337-340.
11. Doi S, Osada H, Seki K, Sekiya S. Effect of maternal hydration on oligohydramnios: a comparison of three volume expansion methods. Obstet Gynecol 1998;92:525-529.
12. Flack NJ, Sepulveda W, Bower S, Fisk NM. Acute maternal hydration in third-trimester oligohydramnios: effects on amniotic fluid volume, uteroplacental perfusion, and fetal blood flow and urine output. Am J Obstet Gynecol 1995;173:1186-1191.
13. Kilpatrick SJ, Safford KL, Pomeroy T, Hoedt L, Scheerer L, Laros RK. Maternal hydration increases amniotic fluid index. Obstet Gynecol 1991;78:1098-1102.
14. Larmon JE, Ross BS. Clinical utility of amniotic fluid volume assessment. Obstet Gynecol Clin North Am 1998;25:639-661.
15. Hill LM. Oligohydramnios: sonographic diagnosis and clinical implications. Clin Obstet Gynecol 1997;40:314-327.
16. Flack NJ, Dore C, Southwell D, Kourtis P, Sepulveda W, Fisk NM. The influence of operator transducer pressure on ultrasonographic measurements of amniotic fluid volume. Am J Obstet Gynecol 1994;171:218-222.
17. Rutherford SE, Smith CV, Phelan JP, Kawakami K, Ahn MO. Four-quadrant assessment of amniotic fluid volume: interobserver and intraobserver variation. J Reprod Med 1987;32:587-589.
18. Bruner JP, Reed GW, Sarno AP, Harrington RA, Goodman MA. Intraobserver and interobserver variability of the amniotic fluid index. Am J Obstet Gynecol 1993;168:1309-1313.
19. O’Reilly-Green CP, Divon MY. Predictive value of amniotic fluid index for oligohydramnios in patients with prolonged pregnancies. J Matern Fetal Med 1996;5:218-226.
20. Chauhan SP, Magann EF, Morrison JC, Whitworth NS, Hendrix NW, Devoe LD. Ultrasonographic assessment of amniotic fluid does not reflect actual amniotic fluid volume. Am J Obstet Gynecol 1997;177:291-297.
21. Chauhan SP, Sanderson M, Hendrix NW, Magann EF, Devoe LD. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a meta-analysis. Am J Obstet Gynecol 1999;181:1473-1478.
22. Magann EF. Antenatal testing among 1001 patients at high risk: the role of ultrasonographic estimate of amniotic fluid volume. Am J Obstet Gynecol 1999;180:1330-1336.
23. Magann EF. Does an amniotic fluid index of 5 cm necessitate delivery in high-risk pregnancies? A case-control study. Am J Obstet Gynecol 1999;180:1354-1359.
24. Nisell H, Ek S. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol. 2000;182:750-751.
25. Conway DL, et al. Isolated oligohydramnios in the term pregnancy: Is it a clinical entity. J Matern Fetal Med 1998;7:197-200.
26. Garmel SH, Chelmow D, Sha SJ, Roan JT, D’Alton ME. Oligohydramnios and the appropriately grown fetus. Am J Perinatol 1997;14:359-363.
27. Kreiser D, el-Sayed YY, Sorem KA, Chitkara U, Holbrook RH, Jr, Druzin ML. Decreased amniotic fluid index in low-risk pregnancy. J Reprod Med 2001;46:743-746.
28. Roberts D, Nwosu EC, Walkinshaw SA. The fetal outcome in pregnancies with isolated reduced amniotic fluid volume in the third trimester. J Perinat Med 1998;26:390-395.
29. Rainford M, Adair R, Scialli AR, Ghidini A, Spong CY. Amniotic fluid index in the uncomplicated term pregnancy. Prediction of outcome. J Reprod Med 2001;46:589-592.
30. Zhang J, Troendle J, Meikle S, Klebanoff MA, Rayburn WF. Isolated oligohydramnios is not associated with adverse perinatal outcomes. BJOG 2004;111:220-225.
31. Conway DL, Groth S, Adkins WB, Langer O. Management of isolated oligohyramnios in the term pregnancy: a randomized clinical trial. Am J Obstet Gynecol 2000;182:S21.-
32. Oosterhof H, Haak MC, Aarnoudse JG. Acute maternal rehydration increases the urine production rate in the near-term human fetus. Am J Obstet Gynecol 2000;183:226-229.
33. Fait G, Pauzner D, Gull I, Lessing JB, Jaffa AJ, Wolman I. Effect of 1 week or oral hydration on the amniotic fluid index. J Reprod Med 2003;48:187-190.
34. Hofmeyr GJ, Gulmezoglu AM. Maternal hydration for increasing amniotic fluid volume in oligohydramnios and normal amniotic fluid volute (Cochrane Review). In: The Cochrane Library. Issue 4, 2002. Oxford: Update Software.
35. Sherer DM, Langer O. Oligohydramnios: use and misuse in clinical management. Ultrasound Obstet Gynecol 2001;18:411-419.
36. Carroll BC, Bruner JP. Umbilical artery Doppler velocimetry in pregnancies complicated by oligohydramnios. J Reprod Med 2000;45:562-566.
37. Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol 1999;94:600-607.
38. Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol 1999;180:628-633.
1. Moore TR. Clinical assessment of amniotic fluid. Clin Obstet Gynecol 1997;40:303-313.
2. Phelan JP, Smith CV, Broussard P, Small M. Amniotic fluid volume assessment with the four-quadrant technique at 36–42weeks’ gestation. J Reprod Med 1987;32:540-542.
3. Banks EH. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol 1999;180:1461-1463.
4. Casey BM. Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks gestation. Am J Obstet Gynecol 2000;182:909-912.
5. Hobbins JC. Oligohydramnios and post-term pregnancy. Ob/Gyn Clinical Alert December 2002;59-60.
6. Johnson DP, Davis NR, Brown AJ. Risk of cesarean delivery after induction at term in nulliparous women with an unfavorable cervix. Am J Obstet Gynecol 2003;188:1565-1572.
7. Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 2001;345:3-8.
8. Kilpatrick SJ, Safford KL. Maternal hydration increases amniotic fluid index in women with normal amniotic fluid. Obstet Gynecol 1993;81:49-52.
9. Gilbert WM, Brace RA. Amniotic fluid volume and normal flows to and from the amniotic cavity. Seminars in Perinatology 1993;17:150-157.
10. Chandra PC, Schiavello HJ, Lewandowski MA. Effect of oral and intravenous hydration on oligohydramnios. J Reprod Med 2000;45:337-340.
11. Doi S, Osada H, Seki K, Sekiya S. Effect of maternal hydration on oligohydramnios: a comparison of three volume expansion methods. Obstet Gynecol 1998;92:525-529.
12. Flack NJ, Sepulveda W, Bower S, Fisk NM. Acute maternal hydration in third-trimester oligohydramnios: effects on amniotic fluid volume, uteroplacental perfusion, and fetal blood flow and urine output. Am J Obstet Gynecol 1995;173:1186-1191.
13. Kilpatrick SJ, Safford KL, Pomeroy T, Hoedt L, Scheerer L, Laros RK. Maternal hydration increases amniotic fluid index. Obstet Gynecol 1991;78:1098-1102.
14. Larmon JE, Ross BS. Clinical utility of amniotic fluid volume assessment. Obstet Gynecol Clin North Am 1998;25:639-661.
15. Hill LM. Oligohydramnios: sonographic diagnosis and clinical implications. Clin Obstet Gynecol 1997;40:314-327.
16. Flack NJ, Dore C, Southwell D, Kourtis P, Sepulveda W, Fisk NM. The influence of operator transducer pressure on ultrasonographic measurements of amniotic fluid volume. Am J Obstet Gynecol 1994;171:218-222.
17. Rutherford SE, Smith CV, Phelan JP, Kawakami K, Ahn MO. Four-quadrant assessment of amniotic fluid volume: interobserver and intraobserver variation. J Reprod Med 1987;32:587-589.
18. Bruner JP, Reed GW, Sarno AP, Harrington RA, Goodman MA. Intraobserver and interobserver variability of the amniotic fluid index. Am J Obstet Gynecol 1993;168:1309-1313.
19. O’Reilly-Green CP, Divon MY. Predictive value of amniotic fluid index for oligohydramnios in patients with prolonged pregnancies. J Matern Fetal Med 1996;5:218-226.
20. Chauhan SP, Magann EF, Morrison JC, Whitworth NS, Hendrix NW, Devoe LD. Ultrasonographic assessment of amniotic fluid does not reflect actual amniotic fluid volume. Am J Obstet Gynecol 1997;177:291-297.
21. Chauhan SP, Sanderson M, Hendrix NW, Magann EF, Devoe LD. Perinatal outcome and amniotic fluid index in the antepartum and intrapartum periods: a meta-analysis. Am J Obstet Gynecol 1999;181:1473-1478.
22. Magann EF. Antenatal testing among 1001 patients at high risk: the role of ultrasonographic estimate of amniotic fluid volume. Am J Obstet Gynecol 1999;180:1330-1336.
23. Magann EF. Does an amniotic fluid index of 5 cm necessitate delivery in high-risk pregnancies? A case-control study. Am J Obstet Gynecol 1999;180:1354-1359.
24. Nisell H, Ek S. Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol. 2000;182:750-751.
25. Conway DL, et al. Isolated oligohydramnios in the term pregnancy: Is it a clinical entity. J Matern Fetal Med 1998;7:197-200.
26. Garmel SH, Chelmow D, Sha SJ, Roan JT, D’Alton ME. Oligohydramnios and the appropriately grown fetus. Am J Perinatol 1997;14:359-363.
27. Kreiser D, el-Sayed YY, Sorem KA, Chitkara U, Holbrook RH, Jr, Druzin ML. Decreased amniotic fluid index in low-risk pregnancy. J Reprod Med 2001;46:743-746.
28. Roberts D, Nwosu EC, Walkinshaw SA. The fetal outcome in pregnancies with isolated reduced amniotic fluid volume in the third trimester. J Perinat Med 1998;26:390-395.
29. Rainford M, Adair R, Scialli AR, Ghidini A, Spong CY. Amniotic fluid index in the uncomplicated term pregnancy. Prediction of outcome. J Reprod Med 2001;46:589-592.
30. Zhang J, Troendle J, Meikle S, Klebanoff MA, Rayburn WF. Isolated oligohydramnios is not associated with adverse perinatal outcomes. BJOG 2004;111:220-225.
31. Conway DL, Groth S, Adkins WB, Langer O. Management of isolated oligohyramnios in the term pregnancy: a randomized clinical trial. Am J Obstet Gynecol 2000;182:S21.-
32. Oosterhof H, Haak MC, Aarnoudse JG. Acute maternal rehydration increases the urine production rate in the near-term human fetus. Am J Obstet Gynecol 2000;183:226-229.
33. Fait G, Pauzner D, Gull I, Lessing JB, Jaffa AJ, Wolman I. Effect of 1 week or oral hydration on the amniotic fluid index. J Reprod Med 2003;48:187-190.
34. Hofmeyr GJ, Gulmezoglu AM. Maternal hydration for increasing amniotic fluid volume in oligohydramnios and normal amniotic fluid volute (Cochrane Review). In: The Cochrane Library. Issue 4, 2002. Oxford: Update Software.
35. Sherer DM, Langer O. Oligohydramnios: use and misuse in clinical management. Ultrasound Obstet Gynecol 2001;18:411-419.
36. Carroll BC, Bruner JP. Umbilical artery Doppler velocimetry in pregnancies complicated by oligohydramnios. J Reprod Med 2000;45:562-566.
37. Seyb ST, Berka RJ, Socol ML, Dooley SL. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol 1999;94:600-607.
38. Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol 1999;180:628-633.