User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Study Spotlights Long-Term Burden of Influenza in Children
SAN DIEGO – Influenza can be deadly even in children with no underlying high-risk conditions, results from a national 8-year study demonstrated.
"Because kids with and without high-risk medical conditions can die quickly from influenza, prevention is the best defense, and all children 6 months of age or older should receive influenza vaccination annually," lead study investigator Dr. Karen K. Wong said in an interview prior to IDWeek 2012, where the research was presented.
Dr. Wong, an epidemic intelligence service officer with the influenza division at the Centers for Disease Control and Prevention, and her associates evaluated data from 829 influenza-associated deaths among children under age 18 that occurred in the United States between Oct. 1, 2004, and Sept. 30, 2012. Their median age was 7 years, and 35% of children died in the emergency department or outside the hospital.
Of the 793 children with a known medical history, 341 (43%) had no high-risk medical conditions, 33% reported neurologic disorders, 26% reported pulmonary disorders including asthma, and 12% reported genetic or chromosomal disorders. These exceeded 100% because more than one medical condition could be reported for a child.
The median duration of illness from symptom onset to death was shorter among children with no underlying high-risk medical conditions than in children with at least one high-risk medical condition (4 vs. 7 days, respectively; P less than .01).
Of 386 children with a specimen collected for bacterial culture from a normally sterile site whose results were available, 153 (40%) had at least one bacterial coinfection. Of those 153 children, the most common bacterial coinfection was Staphylococcus aureus, which was identified in 76 cases (50%).
"Influenza-associated deaths in children are rare," Dr. Wong said. "By including all reported influenza-associated pediatric deaths over an 8-year period in the United States, this study builds on prior smaller studies to describe the children at risk."
She said that she and her associates were surprised to find that 43% of the children who died of influenza-related illness "did not have any medical conditions that placed them at higher risk for influenza complications. Compared with children with high-risk conditions, these otherwise healthy children tended to be younger, and they were more likely to progress to death rapidly before being admitted to the hospital."
Dr. Wong acknowledged certain limitations of the study, including the fact that it was not designed to evaluate the impact of any interventions, such as vaccination or antiviral treatment. "Also, the national influenza-associated pediatric mortality surveillance system likely underestimates the true burden of influenza-associated death in children," she said.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Wong said that she had no relevant financial disclosures.
SAN DIEGO – Influenza can be deadly even in children with no underlying high-risk conditions, results from a national 8-year study demonstrated.
"Because kids with and without high-risk medical conditions can die quickly from influenza, prevention is the best defense, and all children 6 months of age or older should receive influenza vaccination annually," lead study investigator Dr. Karen K. Wong said in an interview prior to IDWeek 2012, where the research was presented.
Dr. Wong, an epidemic intelligence service officer with the influenza division at the Centers for Disease Control and Prevention, and her associates evaluated data from 829 influenza-associated deaths among children under age 18 that occurred in the United States between Oct. 1, 2004, and Sept. 30, 2012. Their median age was 7 years, and 35% of children died in the emergency department or outside the hospital.
Of the 793 children with a known medical history, 341 (43%) had no high-risk medical conditions, 33% reported neurologic disorders, 26% reported pulmonary disorders including asthma, and 12% reported genetic or chromosomal disorders. These exceeded 100% because more than one medical condition could be reported for a child.
The median duration of illness from symptom onset to death was shorter among children with no underlying high-risk medical conditions than in children with at least one high-risk medical condition (4 vs. 7 days, respectively; P less than .01).
Of 386 children with a specimen collected for bacterial culture from a normally sterile site whose results were available, 153 (40%) had at least one bacterial coinfection. Of those 153 children, the most common bacterial coinfection was Staphylococcus aureus, which was identified in 76 cases (50%).
"Influenza-associated deaths in children are rare," Dr. Wong said. "By including all reported influenza-associated pediatric deaths over an 8-year period in the United States, this study builds on prior smaller studies to describe the children at risk."
She said that she and her associates were surprised to find that 43% of the children who died of influenza-related illness "did not have any medical conditions that placed them at higher risk for influenza complications. Compared with children with high-risk conditions, these otherwise healthy children tended to be younger, and they were more likely to progress to death rapidly before being admitted to the hospital."
Dr. Wong acknowledged certain limitations of the study, including the fact that it was not designed to evaluate the impact of any interventions, such as vaccination or antiviral treatment. "Also, the national influenza-associated pediatric mortality surveillance system likely underestimates the true burden of influenza-associated death in children," she said.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Wong said that she had no relevant financial disclosures.
SAN DIEGO – Influenza can be deadly even in children with no underlying high-risk conditions, results from a national 8-year study demonstrated.
"Because kids with and without high-risk medical conditions can die quickly from influenza, prevention is the best defense, and all children 6 months of age or older should receive influenza vaccination annually," lead study investigator Dr. Karen K. Wong said in an interview prior to IDWeek 2012, where the research was presented.
Dr. Wong, an epidemic intelligence service officer with the influenza division at the Centers for Disease Control and Prevention, and her associates evaluated data from 829 influenza-associated deaths among children under age 18 that occurred in the United States between Oct. 1, 2004, and Sept. 30, 2012. Their median age was 7 years, and 35% of children died in the emergency department or outside the hospital.
Of the 793 children with a known medical history, 341 (43%) had no high-risk medical conditions, 33% reported neurologic disorders, 26% reported pulmonary disorders including asthma, and 12% reported genetic or chromosomal disorders. These exceeded 100% because more than one medical condition could be reported for a child.
The median duration of illness from symptom onset to death was shorter among children with no underlying high-risk medical conditions than in children with at least one high-risk medical condition (4 vs. 7 days, respectively; P less than .01).
Of 386 children with a specimen collected for bacterial culture from a normally sterile site whose results were available, 153 (40%) had at least one bacterial coinfection. Of those 153 children, the most common bacterial coinfection was Staphylococcus aureus, which was identified in 76 cases (50%).
"Influenza-associated deaths in children are rare," Dr. Wong said. "By including all reported influenza-associated pediatric deaths over an 8-year period in the United States, this study builds on prior smaller studies to describe the children at risk."
She said that she and her associates were surprised to find that 43% of the children who died of influenza-related illness "did not have any medical conditions that placed them at higher risk for influenza complications. Compared with children with high-risk conditions, these otherwise healthy children tended to be younger, and they were more likely to progress to death rapidly before being admitted to the hospital."
Dr. Wong acknowledged certain limitations of the study, including the fact that it was not designed to evaluate the impact of any interventions, such as vaccination or antiviral treatment. "Also, the national influenza-associated pediatric mortality surveillance system likely underestimates the true burden of influenza-associated death in children," she said.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Wong said that she had no relevant financial disclosures.
AT IDWEEK 2012
Major Finding: Of children in the United States who died from influenza over an 8-year period, 43% had no high-risk medical conditions.
Data Source: This was a national study of data from 829 influenza-associated deaths in children under age 18 that occurred between Oct. 1, 2004, and Sept. 30, 2012.
Disclosures: Dr. Wong said that she had no relevant financial disclosures.
Study Spotlights Benefits of School-Based Flu Shots
SAN DIEGO – Children who received the influenza vaccine at school were three times less likely to become infected with the influenza virus and missed half the of number of school days during the flu season, compared with their counterparts who did not, results from a large study showed.
The finding "supports the implementation of school-located influenza immunization programs to bring down the rates of flu in this age group," lead researcher Dr. Pia S. Pannaraj said during a press telephone conference in advance of IDWeek.
During the 2010-2011 influenza season, Dr. Pannaraj and her associates conducted active influenza surveillance among 4,455 children enrolled at eight elementary schools in the Los Angeles area with similar sociodemographic characteristics. Four of the schools served as controls while the other half served as intervention sites, where school-located influenza vaccination was offered. The researchers conducted polymerase chain reaction (PCR) testing for respiratory viruses on nose and throat swabs collected from febrile children with influenzalike illness to the school nurse or during absenteeism.
"A fundamental difference between this study and previous studies is that [our] research actively documented the reasons for absences and confirmed cases of flu instead of relying on parent surveys," noted Dr. Pannaraj of the department of pediatrics at the University of Southern California, Los Angeles.
Between 27% and 47% of students attending an intervention school received at least one dose of influenza vaccine. Dr. Pannaraj reported findings from 1,021 PCR specimens obtained from 898 children during the 15-week surveillance period. Of these 898 specimens, 21% were positive for influenza, including 2009 H1N1 (31%), H3 (9%), and B (60%). An additional 126 children (12%) tested positive for other respiratory viruses.
Rates of influenza were significantly higher among control schools, compared with schools where vaccination was offered (5.8 vs. 4.0 per 100 children, respectively; P = .011). Unvaccinated children who attended any school were 3.1 times more likely to acquire influenza infection, compared with vaccinated children (5.5 vs. 1.8 per 100 children, respectively; P less than .001).
Rates of absenteeism were higher among control schools compared with schools where vaccination was offered (4.2 vs. 3.9 days per 100 school days, respectively; P = .02), and children with influenza missed more school days, compared with those who had developed other respiratory viruses (a median of 2 days vs. 1 day, respectively; P less than .001).
Protection for unvaccinated children was observed in one school that achieved a vaccination rate of 47% (odds ratio, 2.1; P = .039). In an interview, she speculated that efforts to achieve a 50% vaccination rate in elementary schools "might be a target number to use in planning for pandemics, or even in preparing for the regular flu season. More studies are needed to be sure," she said in advance of the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Pannaraj said that she had no relevant financial conflicts to disclose. One of the study investigators, Dr. Laurene Mascola, disclosed being a member of the speakers bureau and receiving speaker honorarium from Merck and MedImmune.
SAN DIEGO – Children who received the influenza vaccine at school were three times less likely to become infected with the influenza virus and missed half the of number of school days during the flu season, compared with their counterparts who did not, results from a large study showed.
The finding "supports the implementation of school-located influenza immunization programs to bring down the rates of flu in this age group," lead researcher Dr. Pia S. Pannaraj said during a press telephone conference in advance of IDWeek.
During the 2010-2011 influenza season, Dr. Pannaraj and her associates conducted active influenza surveillance among 4,455 children enrolled at eight elementary schools in the Los Angeles area with similar sociodemographic characteristics. Four of the schools served as controls while the other half served as intervention sites, where school-located influenza vaccination was offered. The researchers conducted polymerase chain reaction (PCR) testing for respiratory viruses on nose and throat swabs collected from febrile children with influenzalike illness to the school nurse or during absenteeism.
"A fundamental difference between this study and previous studies is that [our] research actively documented the reasons for absences and confirmed cases of flu instead of relying on parent surveys," noted Dr. Pannaraj of the department of pediatrics at the University of Southern California, Los Angeles.
Between 27% and 47% of students attending an intervention school received at least one dose of influenza vaccine. Dr. Pannaraj reported findings from 1,021 PCR specimens obtained from 898 children during the 15-week surveillance period. Of these 898 specimens, 21% were positive for influenza, including 2009 H1N1 (31%), H3 (9%), and B (60%). An additional 126 children (12%) tested positive for other respiratory viruses.
Rates of influenza were significantly higher among control schools, compared with schools where vaccination was offered (5.8 vs. 4.0 per 100 children, respectively; P = .011). Unvaccinated children who attended any school were 3.1 times more likely to acquire influenza infection, compared with vaccinated children (5.5 vs. 1.8 per 100 children, respectively; P less than .001).
Rates of absenteeism were higher among control schools compared with schools where vaccination was offered (4.2 vs. 3.9 days per 100 school days, respectively; P = .02), and children with influenza missed more school days, compared with those who had developed other respiratory viruses (a median of 2 days vs. 1 day, respectively; P less than .001).
Protection for unvaccinated children was observed in one school that achieved a vaccination rate of 47% (odds ratio, 2.1; P = .039). In an interview, she speculated that efforts to achieve a 50% vaccination rate in elementary schools "might be a target number to use in planning for pandemics, or even in preparing for the regular flu season. More studies are needed to be sure," she said in advance of the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Pannaraj said that she had no relevant financial conflicts to disclose. One of the study investigators, Dr. Laurene Mascola, disclosed being a member of the speakers bureau and receiving speaker honorarium from Merck and MedImmune.
SAN DIEGO – Children who received the influenza vaccine at school were three times less likely to become infected with the influenza virus and missed half the of number of school days during the flu season, compared with their counterparts who did not, results from a large study showed.
The finding "supports the implementation of school-located influenza immunization programs to bring down the rates of flu in this age group," lead researcher Dr. Pia S. Pannaraj said during a press telephone conference in advance of IDWeek.
During the 2010-2011 influenza season, Dr. Pannaraj and her associates conducted active influenza surveillance among 4,455 children enrolled at eight elementary schools in the Los Angeles area with similar sociodemographic characteristics. Four of the schools served as controls while the other half served as intervention sites, where school-located influenza vaccination was offered. The researchers conducted polymerase chain reaction (PCR) testing for respiratory viruses on nose and throat swabs collected from febrile children with influenzalike illness to the school nurse or during absenteeism.
"A fundamental difference between this study and previous studies is that [our] research actively documented the reasons for absences and confirmed cases of flu instead of relying on parent surveys," noted Dr. Pannaraj of the department of pediatrics at the University of Southern California, Los Angeles.
Between 27% and 47% of students attending an intervention school received at least one dose of influenza vaccine. Dr. Pannaraj reported findings from 1,021 PCR specimens obtained from 898 children during the 15-week surveillance period. Of these 898 specimens, 21% were positive for influenza, including 2009 H1N1 (31%), H3 (9%), and B (60%). An additional 126 children (12%) tested positive for other respiratory viruses.
Rates of influenza were significantly higher among control schools, compared with schools where vaccination was offered (5.8 vs. 4.0 per 100 children, respectively; P = .011). Unvaccinated children who attended any school were 3.1 times more likely to acquire influenza infection, compared with vaccinated children (5.5 vs. 1.8 per 100 children, respectively; P less than .001).
Rates of absenteeism were higher among control schools compared with schools where vaccination was offered (4.2 vs. 3.9 days per 100 school days, respectively; P = .02), and children with influenza missed more school days, compared with those who had developed other respiratory viruses (a median of 2 days vs. 1 day, respectively; P less than .001).
Protection for unvaccinated children was observed in one school that achieved a vaccination rate of 47% (odds ratio, 2.1; P = .039). In an interview, she speculated that efforts to achieve a 50% vaccination rate in elementary schools "might be a target number to use in planning for pandemics, or even in preparing for the regular flu season. More studies are needed to be sure," she said in advance of the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Pannaraj said that she had no relevant financial conflicts to disclose. One of the study investigators, Dr. Laurene Mascola, disclosed being a member of the speakers bureau and receiving speaker honorarium from Merck and MedImmune.
AT IDWEEK 2012
Major Finding: Rates of influenza were significantly lower in elementary schools that offered on-site flu shots, compared with schools that did not (4.0 vs. 5.8 per 100 children, respectively; P = .011).
Data Source: This was a study of 4,455 children enrolled at eight elementary schools in the Los Angeles area: Four served as control schools and four offered school-located influenza vaccination during the 2010-2011 flu season.
Disclosures: Dr. Pannaraj said that she had no relevant financial conflicts to disclose. One of the study investigators, Dr. Laurene Mascola, disclosed being a member of the speakers bureau and receiving speaker honorarium from Merck and MedImmune.
UV-C Light Blasts 'Bad Bugs' in Hospital Rooms
SAN DIEGO – A portable device that emits UV-C light destroyed vancomycin-resistant enterococci, Acinetobacter, and C. difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.*
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were only able to evaluate two hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
CORRECTION 10/18/12: This sentence was amended to state the correct number of sensors and bulbs that emit UV-C light.
SAN DIEGO – A portable device that emits UV-C light destroyed vancomycin-resistant enterococci, Acinetobacter, and C. difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.*
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were only able to evaluate two hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
CORRECTION 10/18/12: This sentence was amended to state the correct number of sensors and bulbs that emit UV-C light.
SAN DIEGO – A portable device that emits UV-C light destroyed vancomycin-resistant enterococci, Acinetobacter, and C. difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.*
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were only able to evaluate two hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
CORRECTION 10/18/12: This sentence was amended to state the correct number of sensors and bulbs that emit UV-C light.
AT IDWEEK 2012
Major Finding: UV-C irradiation of hospital rooms with a portable disinfection system reduced colony-forming units of vancomycin-resistant enterococci by 98%, C. difficile by 93%, and Acinetobacter by 98%.
Data Source: Results were taken from a study conducted in 39 hospital rooms at two tertiary medical centers.
Disclosures: The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
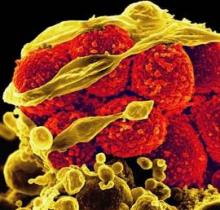
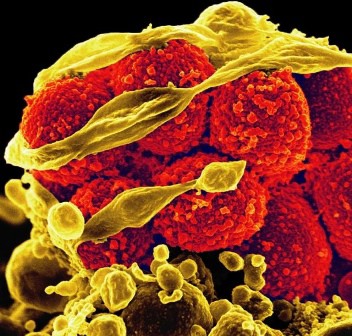
Don't Screen, Clean: MRSA Rates Slashed by ICU Scrub Down
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
SAN DIEGO – The use of antimicrobial soap and ointment on all patients admitted to intensive care units led to a 37% reduction in methicillin-resistant Staphylococcus aureus clinical isolates and a 44% reduction in bloodstream infections caused by all pathogens, results from a large multicenter study demonstrated.
"While earlier, smaller studies have suggested benefit from bathing with antibacterial soap and using nose ointment, this trial provides the first large-scale evaluation of this question and is anticipated to impact on best-practice guidelines for preventing hospital infections," lead researcher Dr. Susan S. Huang said in an interview prior to IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society of Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Huang, medical director of epidemiology and infection prevention at the University of California, Irvine, and her associates randomized 43 hospitals in 16 states to one of three ICU strategies for reducing bloodstream infections: nasal MRSA screening followed by isolation if positive (group 1); targeted decolonization by treating patients who tested positive with chlorhexidine baths and mupirocin for 5 days (group 2); or universal decolonization by elimination of all screening and administration of mupirocin for 5 days and daily chlorhexidine baths for the duration of ICU stay (group 3).
The study, known as the REDUCE MRSA Trial, included a 1-year baseline period and an 18-month intervention period that ended in September 2011.
"Until this trial, there has been debate about whether bathing with antibacterial soap and using nose ointment prevent infections in these high-risk settings," Dr. Huang said. "There has also been debate whether such bathing, if it is helpful, should be used for all ICU patients or only for patients who can be shown to have MRSA on their skin or nose."
Dr. Huang reported results from 48,390 ICU admissions in the baseline period and 74,256 in the intervention period. Between the two time periods, MRSA rates among ICU patients fell by 37% in group 3, compared with a 25% drop in group 2 and an 8% drop in group 1. The difference between groups reached statistical significance (P less than .01).
A similar association was seen when the researchers compared the effect of all interventions on the rate of all bloodstream infections caused by all pathogens. Between the two time periods, the rates of bloodstream infections among ICU patients fell by 44% in group 3, compared with a 22% drop in group 2 and a 1% drop in group 1. The difference between groups reached statistical significance (P less than .00001).
"This trial was almost entirely based in community hospitals and the results are therefore likely to be applicable to nearly all U.S. hospitals," Dr. Huang said. "This is in contrast to prior research, which mainly involved large academic centers that may not be representative of usual medical care."
She went on to note that, until now, it was unclear which strategy – directing prevention strategies at patients who harbor highly resistant organisms or at entire high-risk patient groups – would be better. "This has been a key area of debate among infection prevention experts," she said. "We are pleased to find that the results support a strategy that will benefit more people and prevent more infections than those just due to MRSA."
Dr. Huang acknowledged certain limitations of the study, including the fact that it was conducted exclusively in ICUs. "We do not know the effects of this strategy in other settings," she said. "Formal cost analyses have yet to be done to understand the cost of product compared to the reduction in infection risk. In addition, we have yet to analyze whether wide use of these products caused resistant bacteria to emerge. Even if it did not, continued vigilance for emerging resistance will be required if it is widely implemented."
The study was sponsored by Harvard Pilgrim Health Care and supported by funding from the Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, and Hospital Corporation of America. Dr. Huang said that she had no relevant financial conflicts to disclose.
AT IDWEEK 2012
Major Finding: Universal decolonization with chlorhexidine and mupirocin in adult intensive care units led to a 37% reduced risk of a methicillin-resistant S. aureus clinical isolate and a 44% reduced risk of bloodstream infections caused by all pathogens.
Data Source: These findings come from a study of 43 hospitals in 16 states that were randomized to one of three ICU strategies for reducing bloodstream infections over a period of 18 months.
Disclosures: The study was supported by funding from the Agency for Healthcare Research and Quality and from the Centers for Disease Control and Prevention. Dr. Huang said that she had no relevant financial conflicts.
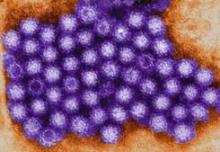
Ten States Dealing With H3N2 Outbreak
SAN FRANCISCO – The H3N2 virus could sicken 500-900 people in the United States by the end of 2012, surveillance studies by the Centers for Disease Control and Prevention suggest.
"Cooler weather is approaching, and it is likely that additional cases of H3N2v will be identified in the coming weeks," said Lyn Finelli, Dr.PH., chief of surveillance and outbreak response in the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta.
Between December 2005 and June of 2012, there have been 36 human cases of swine influenza A virus infection identified, Dr. Finelli said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification has increased since 2009" as novel influenza A became a reportable disease in 2007, better diagnostics became available at state health departments, and there has been greater awareness due to the 2009 pandemic H1N1 virus.
In 2011, public health officials in the United States identified 12 cases of H3N2v with the pandemic M gene from the 2009 pandemic H1N1 virus. Six were associated with exposure at agricultural fairs or farms and six were cases of human to human transmission.
This subtype continues to spike in prevalence. Between July 1 and Sept. 10, 2012, 302 cases of H3N2v infection with the M gene have been confirmed in the United States. The M gene "was thought to contribute to increased transmissibility of the pandemic H1N1 virus," Dr. Finelli noted. "In two animal studies it was shown to increase transmissibility for pandemic H1N1 ... Various serologic studies to date suggest that children under 12 have very little protection against this virus."
An outbreak of H3N2v is occurring in 10 states, and 16 patients have been hospitalized. Indiana has the most confirmed cases, followed by Ohio and Wisconsin. "Ohio also has a large number of probable cases, many of whom are rapid test positive but who have not been tested with PCR, so that state probably has more cases than Indiana at this point," Dr. Finelli said.
The mean age of the 302 cases is 8 years, with a range between 4 months and 74 years, and the incubation period is 2-3 days. "The secondary attack rate is low," she said. "We only have 10 probable cases of human to human transmission. The duration of illness is 3-4 days and the period of infectiousness is unknown. We don’t have enough secondary transmission to tell."
Of the 16 patients who have been hospitalized with H3N2v, 14 (87%) were 0-17 years of age and the remaining 2 were at least 18 years of age. The most common underlying condition is being 5 years of age or younger (38%), followed by asthma (19%), cancer or immune suppression (19%), and neurological disorder (13%). One patient died (7%).
Dr. Finelli and her associates have exposure data on 203 cases. Of these, 198 (98%) had either direct or indirect swine contact, or attended a state or county fair.
Antiviral treatment with oral oseltamivir or inhaled zanamivir is encouraged as soon as possible for patients with suspected H3N2v virus infection, especially hospitalized patients or patients with severe or progressive illness, she said. "All non–high-risk outpatients without underlying medical conditions can be started within 48 hours of illness onset."
"Surveillance guidance for state and local public health has focused on increasing collection of PCR quality specimens from patients presenting with influenza-like illness in high risk groups, such as outbreaks in child care and school settings or in populations where confirmed H3N2v cases have occurred," Dr. Finelli said.
Two candidate H3N2v vaccines have been identified and have been sent to the World Health Organization, the Food and Drug Administration, and vaccine manufacturers, she said. Clinical trials using the National Institutes of Health’s Vaccine and Therapeutics Evaluation Unit are now under way.
The conference was sponsored by the American Society for Microbiology. Dr. Finelli said that she had no relevant financial disclosures to make.
SAN FRANCISCO – The H3N2 virus could sicken 500-900 people in the United States by the end of 2012, surveillance studies by the Centers for Disease Control and Prevention suggest.
"Cooler weather is approaching, and it is likely that additional cases of H3N2v will be identified in the coming weeks," said Lyn Finelli, Dr.PH., chief of surveillance and outbreak response in the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta.
Between December 2005 and June of 2012, there have been 36 human cases of swine influenza A virus infection identified, Dr. Finelli said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification has increased since 2009" as novel influenza A became a reportable disease in 2007, better diagnostics became available at state health departments, and there has been greater awareness due to the 2009 pandemic H1N1 virus.
In 2011, public health officials in the United States identified 12 cases of H3N2v with the pandemic M gene from the 2009 pandemic H1N1 virus. Six were associated with exposure at agricultural fairs or farms and six were cases of human to human transmission.
This subtype continues to spike in prevalence. Between July 1 and Sept. 10, 2012, 302 cases of H3N2v infection with the M gene have been confirmed in the United States. The M gene "was thought to contribute to increased transmissibility of the pandemic H1N1 virus," Dr. Finelli noted. "In two animal studies it was shown to increase transmissibility for pandemic H1N1 ... Various serologic studies to date suggest that children under 12 have very little protection against this virus."
An outbreak of H3N2v is occurring in 10 states, and 16 patients have been hospitalized. Indiana has the most confirmed cases, followed by Ohio and Wisconsin. "Ohio also has a large number of probable cases, many of whom are rapid test positive but who have not been tested with PCR, so that state probably has more cases than Indiana at this point," Dr. Finelli said.
The mean age of the 302 cases is 8 years, with a range between 4 months and 74 years, and the incubation period is 2-3 days. "The secondary attack rate is low," she said. "We only have 10 probable cases of human to human transmission. The duration of illness is 3-4 days and the period of infectiousness is unknown. We don’t have enough secondary transmission to tell."
Of the 16 patients who have been hospitalized with H3N2v, 14 (87%) were 0-17 years of age and the remaining 2 were at least 18 years of age. The most common underlying condition is being 5 years of age or younger (38%), followed by asthma (19%), cancer or immune suppression (19%), and neurological disorder (13%). One patient died (7%).
Dr. Finelli and her associates have exposure data on 203 cases. Of these, 198 (98%) had either direct or indirect swine contact, or attended a state or county fair.
Antiviral treatment with oral oseltamivir or inhaled zanamivir is encouraged as soon as possible for patients with suspected H3N2v virus infection, especially hospitalized patients or patients with severe or progressive illness, she said. "All non–high-risk outpatients without underlying medical conditions can be started within 48 hours of illness onset."
"Surveillance guidance for state and local public health has focused on increasing collection of PCR quality specimens from patients presenting with influenza-like illness in high risk groups, such as outbreaks in child care and school settings or in populations where confirmed H3N2v cases have occurred," Dr. Finelli said.
Two candidate H3N2v vaccines have been identified and have been sent to the World Health Organization, the Food and Drug Administration, and vaccine manufacturers, she said. Clinical trials using the National Institutes of Health’s Vaccine and Therapeutics Evaluation Unit are now under way.
The conference was sponsored by the American Society for Microbiology. Dr. Finelli said that she had no relevant financial disclosures to make.
SAN FRANCISCO – The H3N2 virus could sicken 500-900 people in the United States by the end of 2012, surveillance studies by the Centers for Disease Control and Prevention suggest.
"Cooler weather is approaching, and it is likely that additional cases of H3N2v will be identified in the coming weeks," said Lyn Finelli, Dr.PH., chief of surveillance and outbreak response in the influenza division at the CDC’s National Center for Immunization and Respiratory Diseases, Atlanta.
Between December 2005 and June of 2012, there have been 36 human cases of swine influenza A virus infection identified, Dr. Finelli said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification has increased since 2009" as novel influenza A became a reportable disease in 2007, better diagnostics became available at state health departments, and there has been greater awareness due to the 2009 pandemic H1N1 virus.
In 2011, public health officials in the United States identified 12 cases of H3N2v with the pandemic M gene from the 2009 pandemic H1N1 virus. Six were associated with exposure at agricultural fairs or farms and six were cases of human to human transmission.
This subtype continues to spike in prevalence. Between July 1 and Sept. 10, 2012, 302 cases of H3N2v infection with the M gene have been confirmed in the United States. The M gene "was thought to contribute to increased transmissibility of the pandemic H1N1 virus," Dr. Finelli noted. "In two animal studies it was shown to increase transmissibility for pandemic H1N1 ... Various serologic studies to date suggest that children under 12 have very little protection against this virus."
An outbreak of H3N2v is occurring in 10 states, and 16 patients have been hospitalized. Indiana has the most confirmed cases, followed by Ohio and Wisconsin. "Ohio also has a large number of probable cases, many of whom are rapid test positive but who have not been tested with PCR, so that state probably has more cases than Indiana at this point," Dr. Finelli said.
The mean age of the 302 cases is 8 years, with a range between 4 months and 74 years, and the incubation period is 2-3 days. "The secondary attack rate is low," she said. "We only have 10 probable cases of human to human transmission. The duration of illness is 3-4 days and the period of infectiousness is unknown. We don’t have enough secondary transmission to tell."
Of the 16 patients who have been hospitalized with H3N2v, 14 (87%) were 0-17 years of age and the remaining 2 were at least 18 years of age. The most common underlying condition is being 5 years of age or younger (38%), followed by asthma (19%), cancer or immune suppression (19%), and neurological disorder (13%). One patient died (7%).
Dr. Finelli and her associates have exposure data on 203 cases. Of these, 198 (98%) had either direct or indirect swine contact, or attended a state or county fair.
Antiviral treatment with oral oseltamivir or inhaled zanamivir is encouraged as soon as possible for patients with suspected H3N2v virus infection, especially hospitalized patients or patients with severe or progressive illness, she said. "All non–high-risk outpatients without underlying medical conditions can be started within 48 hours of illness onset."
"Surveillance guidance for state and local public health has focused on increasing collection of PCR quality specimens from patients presenting with influenza-like illness in high risk groups, such as outbreaks in child care and school settings or in populations where confirmed H3N2v cases have occurred," Dr. Finelli said.
Two candidate H3N2v vaccines have been identified and have been sent to the World Health Organization, the Food and Drug Administration, and vaccine manufacturers, she said. Clinical trials using the National Institutes of Health’s Vaccine and Therapeutics Evaluation Unit are now under way.
The conference was sponsored by the American Society for Microbiology. Dr. Finelli said that she had no relevant financial disclosures to make.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
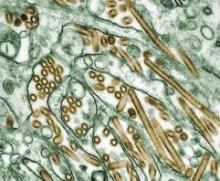
H5N1 Called an Entrenched Threat to Human Health
SAN FRANCISCO – The pathogenic avian influenza A(H5N1) virus remains entrenched in poultry in many countries and is unlikely to be eradicated, according to Dr. Malik Peiris.
"Over the past 15 years the virus has spread through Asia and to part of Africa. Even this year there have been poultry outbreaks in about nine countries, especially in Egypt but also in Asia and Indonesia," said Dr. Peiris, director of the Center of Influenza Research at the University of Hong Kong. "That, I think, is the real cause for concern."
So far, human disease has been uncommon, but the potential for human exposure to H5N1 is massive, he said. The reasons for viral spread are multifactorial, including the prevalence of backyard flocks of poultry and game birds, which are extremely common in parts of Asia, and the fact that the virus can infect ducks. "These ducks are moved from paddy field to paddy field," he said. "They graze on fallen rice in these paddy fields, and they move the virus without any ill effect to themselves. Live poultry markets are also a reservoir and amplifier. Some lineages of this virus can be moved long distances through migration of wild birds, but it is not clear whether wild birds are a true reservoir of this virus."
To date, Dr. Peiris said, 608 human cases of H5N1 infection have been reported from 15 countries in Asia and Africa. Of these, 359 (59%) have been fatal. The incubation period is 2-3 days, and the virus presents as severe viral pneumonia. "It’s rapidly progressing in previously healthy younger persons," he said. "It’s not the type of pneumonia [caused by] complications of influenza that you see with typical seasonal flu, which is at the extremes of age and is often associated with secondary bacterial superinfection. These are perfectly healthy people."
Virus clades from Indonesia seem to carry the greatest severity, Dr. Peiris said, followed by clades from the Middle East and those from other parts of Asia. There appears to be lower mortality among affected children under age 5 and among patients who receive oseltamivir treatment within 2 days of symptom onset.
"The virus strains are generally sensitive to oseltamivir, though different clades have a different range of sensitivity," Dr. Peiris said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "There are cases where antiviral resistance has been detected, with adverse outcomes."
According to World Health Organization guidelines published in 2007, "modified regimens of oseltamivir treatment, including twofold higher dosage, longer duration, and, possibly, combination therapy with amantadine or rimantadine (in countries where A(H5N1) viruses are likely to be susceptible to amantadines), may be considered on a case by case basis, especially in patients with pneumonia or progressive disease."
According to Dr. Peiris, data on this approach "are limited, but observational data suggest that a higher dose of oseltamivir is not associated with lower mortality."
While some experts argue that H5N1 viruses are inherently unable to transmit from human to human, two recent studies of ferrets suggest that airborne transmission is possible (Science 2012;336:1534-41 and Nature 2012;486:420-8). "While combinations of mutations are required for acquisition of mammalian transmissibility, some of these are individually present in some field isolates of H5N1 viruses, highlighting the need for enhanced and continued vigilance," Dr. Peiris noted.
The H5N1 virus "has diversified genetically and antigenically over the years," he said. "This is the challenge that we face in developing a vaccine for H5N1."
The conference was sponsored by the American Society for Microbiology. Dr. Peiris disclosed that he is a scientific adviser for Crucell and is a consultant for GlaxoSmithKline.
SAN FRANCISCO – The pathogenic avian influenza A(H5N1) virus remains entrenched in poultry in many countries and is unlikely to be eradicated, according to Dr. Malik Peiris.
"Over the past 15 years the virus has spread through Asia and to part of Africa. Even this year there have been poultry outbreaks in about nine countries, especially in Egypt but also in Asia and Indonesia," said Dr. Peiris, director of the Center of Influenza Research at the University of Hong Kong. "That, I think, is the real cause for concern."
So far, human disease has been uncommon, but the potential for human exposure to H5N1 is massive, he said. The reasons for viral spread are multifactorial, including the prevalence of backyard flocks of poultry and game birds, which are extremely common in parts of Asia, and the fact that the virus can infect ducks. "These ducks are moved from paddy field to paddy field," he said. "They graze on fallen rice in these paddy fields, and they move the virus without any ill effect to themselves. Live poultry markets are also a reservoir and amplifier. Some lineages of this virus can be moved long distances through migration of wild birds, but it is not clear whether wild birds are a true reservoir of this virus."
To date, Dr. Peiris said, 608 human cases of H5N1 infection have been reported from 15 countries in Asia and Africa. Of these, 359 (59%) have been fatal. The incubation period is 2-3 days, and the virus presents as severe viral pneumonia. "It’s rapidly progressing in previously healthy younger persons," he said. "It’s not the type of pneumonia [caused by] complications of influenza that you see with typical seasonal flu, which is at the extremes of age and is often associated with secondary bacterial superinfection. These are perfectly healthy people."
Virus clades from Indonesia seem to carry the greatest severity, Dr. Peiris said, followed by clades from the Middle East and those from other parts of Asia. There appears to be lower mortality among affected children under age 5 and among patients who receive oseltamivir treatment within 2 days of symptom onset.
"The virus strains are generally sensitive to oseltamivir, though different clades have a different range of sensitivity," Dr. Peiris said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "There are cases where antiviral resistance has been detected, with adverse outcomes."
According to World Health Organization guidelines published in 2007, "modified regimens of oseltamivir treatment, including twofold higher dosage, longer duration, and, possibly, combination therapy with amantadine or rimantadine (in countries where A(H5N1) viruses are likely to be susceptible to amantadines), may be considered on a case by case basis, especially in patients with pneumonia or progressive disease."
According to Dr. Peiris, data on this approach "are limited, but observational data suggest that a higher dose of oseltamivir is not associated with lower mortality."
While some experts argue that H5N1 viruses are inherently unable to transmit from human to human, two recent studies of ferrets suggest that airborne transmission is possible (Science 2012;336:1534-41 and Nature 2012;486:420-8). "While combinations of mutations are required for acquisition of mammalian transmissibility, some of these are individually present in some field isolates of H5N1 viruses, highlighting the need for enhanced and continued vigilance," Dr. Peiris noted.
The H5N1 virus "has diversified genetically and antigenically over the years," he said. "This is the challenge that we face in developing a vaccine for H5N1."
The conference was sponsored by the American Society for Microbiology. Dr. Peiris disclosed that he is a scientific adviser for Crucell and is a consultant for GlaxoSmithKline.
SAN FRANCISCO – The pathogenic avian influenza A(H5N1) virus remains entrenched in poultry in many countries and is unlikely to be eradicated, according to Dr. Malik Peiris.
"Over the past 15 years the virus has spread through Asia and to part of Africa. Even this year there have been poultry outbreaks in about nine countries, especially in Egypt but also in Asia and Indonesia," said Dr. Peiris, director of the Center of Influenza Research at the University of Hong Kong. "That, I think, is the real cause for concern."
So far, human disease has been uncommon, but the potential for human exposure to H5N1 is massive, he said. The reasons for viral spread are multifactorial, including the prevalence of backyard flocks of poultry and game birds, which are extremely common in parts of Asia, and the fact that the virus can infect ducks. "These ducks are moved from paddy field to paddy field," he said. "They graze on fallen rice in these paddy fields, and they move the virus without any ill effect to themselves. Live poultry markets are also a reservoir and amplifier. Some lineages of this virus can be moved long distances through migration of wild birds, but it is not clear whether wild birds are a true reservoir of this virus."
To date, Dr. Peiris said, 608 human cases of H5N1 infection have been reported from 15 countries in Asia and Africa. Of these, 359 (59%) have been fatal. The incubation period is 2-3 days, and the virus presents as severe viral pneumonia. "It’s rapidly progressing in previously healthy younger persons," he said. "It’s not the type of pneumonia [caused by] complications of influenza that you see with typical seasonal flu, which is at the extremes of age and is often associated with secondary bacterial superinfection. These are perfectly healthy people."
Virus clades from Indonesia seem to carry the greatest severity, Dr. Peiris said, followed by clades from the Middle East and those from other parts of Asia. There appears to be lower mortality among affected children under age 5 and among patients who receive oseltamivir treatment within 2 days of symptom onset.
"The virus strains are generally sensitive to oseltamivir, though different clades have a different range of sensitivity," Dr. Peiris said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "There are cases where antiviral resistance has been detected, with adverse outcomes."
According to World Health Organization guidelines published in 2007, "modified regimens of oseltamivir treatment, including twofold higher dosage, longer duration, and, possibly, combination therapy with amantadine or rimantadine (in countries where A(H5N1) viruses are likely to be susceptible to amantadines), may be considered on a case by case basis, especially in patients with pneumonia or progressive disease."
According to Dr. Peiris, data on this approach "are limited, but observational data suggest that a higher dose of oseltamivir is not associated with lower mortality."
While some experts argue that H5N1 viruses are inherently unable to transmit from human to human, two recent studies of ferrets suggest that airborne transmission is possible (Science 2012;336:1534-41 and Nature 2012;486:420-8). "While combinations of mutations are required for acquisition of mammalian transmissibility, some of these are individually present in some field isolates of H5N1 viruses, highlighting the need for enhanced and continued vigilance," Dr. Peiris noted.
The H5N1 virus "has diversified genetically and antigenically over the years," he said. "This is the challenge that we face in developing a vaccine for H5N1."
The conference was sponsored by the American Society for Microbiology. Dr. Peiris disclosed that he is a scientific adviser for Crucell and is a consultant for GlaxoSmithKline.
EXPERT ANALYSIS FROM THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Linezolid May Predict MRSA Pneumonia Treatment Success
SAN FRANCISCO – In a national cohort of VA patients with MRSA pneumonia, treatment with linezolid was the only modifiable variable in predicting clinical success.
"Pneumonia is the No. 1 cause of infectious disease–related deaths in the United States yet there are limited treatment options for pneumonia caused by MRSA," Aisling R. Caffrey, Ph.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification of independent predictors of clinical success can optimize patient care."
In an effort to identify independent predictors of clinical success in MRSA pneumonia, Dr. Caffrey, assistant professor of pharmacoepidemiology at the University of Rhode Island College of Pharmacy, and her associates conducted a retrospective cohort study of VA hospital admissions between January 2002 and September 2010 with diagnosis codes for MRSA and pneumonia. They used pharmacy records to identify initiation of linezolid or vancomycin during admission, with at least 3 days of therapy as dosed per protocol.
Patients who died or were discharged within 3 days of treatment initiation with either agent were excluded from the study, as were those whose treatment was initiated in a nursing home and those who were exposed to more than 2 consecutive days of antibiotic therapy with MRSA activity within 3 days prior to initiation of linezolid or vancomycin or during treatment with either agent.
Clinical success was defined as discharge from the hospital or intensive care unit by day 14 after treatment initiation, in the absence of death, therapy change, or intubation. Nonsuccess was defined as therapy change, intubation, discharge, and readmission, or death between treatment initiation and day 14. They also investigated numerous potential predictors of clinical success, including treatment with linezolid or vancomycin, demographics and admission characteristics, and comorbidities and medical history.
Dr. Caffrey reported data from 231 patients who received linezolid and 3,501 patients who received vancomycin. Their mean age was 70 years and most (98%) were male. Predictors of clinical success included treatment with linezolid (OR 1.53) and having a previous complication of an implant or graft (OR 1.55). Factors associated with nonsuccess included dialysis (OR 0.54), intravenous line (OR 0.76), having three or more inpatient procedures (OR 0.53), inpatient surgery (OR 0.48), urinary tract infection (0.82), previous coagulopathy (0.74), previous endocarditis (0.24), and previous amputation procedure (OR 0.72).
Dr. Caffrey acknowledged certain limitations of the study, including the reliance on diagnostic codes to ascertain the number of MRSA pneumonia cases. "We’re probably only capturing 20%-40% of MRSA diagnoses by using the diagnosis codes," she said at the meeting, which was sponsored by the American Society for Microbiology.
Low generalizability of the findings to other patient populations is another limitation: "The VA is the largest integrated health care system in the United States but it [consists of] mainly older white males with a lot of comorbidities," she explained.
She concluded that patients with MRSA pneumonia "are often complex, and identifying predictors of success is useful in maximizing clinical decision making."
The study was supported by the Department of Veterans Affairs and Pfizer.
SAN FRANCISCO – In a national cohort of VA patients with MRSA pneumonia, treatment with linezolid was the only modifiable variable in predicting clinical success.
"Pneumonia is the No. 1 cause of infectious disease–related deaths in the United States yet there are limited treatment options for pneumonia caused by MRSA," Aisling R. Caffrey, Ph.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification of independent predictors of clinical success can optimize patient care."
In an effort to identify independent predictors of clinical success in MRSA pneumonia, Dr. Caffrey, assistant professor of pharmacoepidemiology at the University of Rhode Island College of Pharmacy, and her associates conducted a retrospective cohort study of VA hospital admissions between January 2002 and September 2010 with diagnosis codes for MRSA and pneumonia. They used pharmacy records to identify initiation of linezolid or vancomycin during admission, with at least 3 days of therapy as dosed per protocol.
Patients who died or were discharged within 3 days of treatment initiation with either agent were excluded from the study, as were those whose treatment was initiated in a nursing home and those who were exposed to more than 2 consecutive days of antibiotic therapy with MRSA activity within 3 days prior to initiation of linezolid or vancomycin or during treatment with either agent.
Clinical success was defined as discharge from the hospital or intensive care unit by day 14 after treatment initiation, in the absence of death, therapy change, or intubation. Nonsuccess was defined as therapy change, intubation, discharge, and readmission, or death between treatment initiation and day 14. They also investigated numerous potential predictors of clinical success, including treatment with linezolid or vancomycin, demographics and admission characteristics, and comorbidities and medical history.
Dr. Caffrey reported data from 231 patients who received linezolid and 3,501 patients who received vancomycin. Their mean age was 70 years and most (98%) were male. Predictors of clinical success included treatment with linezolid (OR 1.53) and having a previous complication of an implant or graft (OR 1.55). Factors associated with nonsuccess included dialysis (OR 0.54), intravenous line (OR 0.76), having three or more inpatient procedures (OR 0.53), inpatient surgery (OR 0.48), urinary tract infection (0.82), previous coagulopathy (0.74), previous endocarditis (0.24), and previous amputation procedure (OR 0.72).
Dr. Caffrey acknowledged certain limitations of the study, including the reliance on diagnostic codes to ascertain the number of MRSA pneumonia cases. "We’re probably only capturing 20%-40% of MRSA diagnoses by using the diagnosis codes," she said at the meeting, which was sponsored by the American Society for Microbiology.
Low generalizability of the findings to other patient populations is another limitation: "The VA is the largest integrated health care system in the United States but it [consists of] mainly older white males with a lot of comorbidities," she explained.
She concluded that patients with MRSA pneumonia "are often complex, and identifying predictors of success is useful in maximizing clinical decision making."
The study was supported by the Department of Veterans Affairs and Pfizer.
SAN FRANCISCO – In a national cohort of VA patients with MRSA pneumonia, treatment with linezolid was the only modifiable variable in predicting clinical success.
"Pneumonia is the No. 1 cause of infectious disease–related deaths in the United States yet there are limited treatment options for pneumonia caused by MRSA," Aisling R. Caffrey, Ph.D., said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "Identification of independent predictors of clinical success can optimize patient care."
In an effort to identify independent predictors of clinical success in MRSA pneumonia, Dr. Caffrey, assistant professor of pharmacoepidemiology at the University of Rhode Island College of Pharmacy, and her associates conducted a retrospective cohort study of VA hospital admissions between January 2002 and September 2010 with diagnosis codes for MRSA and pneumonia. They used pharmacy records to identify initiation of linezolid or vancomycin during admission, with at least 3 days of therapy as dosed per protocol.
Patients who died or were discharged within 3 days of treatment initiation with either agent were excluded from the study, as were those whose treatment was initiated in a nursing home and those who were exposed to more than 2 consecutive days of antibiotic therapy with MRSA activity within 3 days prior to initiation of linezolid or vancomycin or during treatment with either agent.
Clinical success was defined as discharge from the hospital or intensive care unit by day 14 after treatment initiation, in the absence of death, therapy change, or intubation. Nonsuccess was defined as therapy change, intubation, discharge, and readmission, or death between treatment initiation and day 14. They also investigated numerous potential predictors of clinical success, including treatment with linezolid or vancomycin, demographics and admission characteristics, and comorbidities and medical history.
Dr. Caffrey reported data from 231 patients who received linezolid and 3,501 patients who received vancomycin. Their mean age was 70 years and most (98%) were male. Predictors of clinical success included treatment with linezolid (OR 1.53) and having a previous complication of an implant or graft (OR 1.55). Factors associated with nonsuccess included dialysis (OR 0.54), intravenous line (OR 0.76), having three or more inpatient procedures (OR 0.53), inpatient surgery (OR 0.48), urinary tract infection (0.82), previous coagulopathy (0.74), previous endocarditis (0.24), and previous amputation procedure (OR 0.72).
Dr. Caffrey acknowledged certain limitations of the study, including the reliance on diagnostic codes to ascertain the number of MRSA pneumonia cases. "We’re probably only capturing 20%-40% of MRSA diagnoses by using the diagnosis codes," she said at the meeting, which was sponsored by the American Society for Microbiology.
Low generalizability of the findings to other patient populations is another limitation: "The VA is the largest integrated health care system in the United States but it [consists of] mainly older white males with a lot of comorbidities," she explained.
She concluded that patients with MRSA pneumonia "are often complex, and identifying predictors of success is useful in maximizing clinical decision making."
The study was supported by the Department of Veterans Affairs and Pfizer.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Treatment with linezolid (OR 1.53) and having a previous complication of an implant or graft (OR 1.55) are independent predictors of clinical success in patients with MRSA pneumonia.
Data Source: Findings are from a study of 231 patients who received linezolid and 3,501 patients who received vancomycin during Veterans Affairs hospital admission for MRSA pneumonia between January 2002 and September 2010.
Disclosures: The study was supported by the Department of Veterans Affairs and Pfizer.
Analysis Supports First-Line Daptomycin Against Catheter-Related Bacteremia
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
SAN FRANCISCO – Daptomycin demonstrated an overall clinical success rate of 83% when used as a first-line treatment of catheter-related bacteremia, according to analysis of a large European database.
"In Europe, we have seen daptomycin being used as more of a salvage therapy for catheter-related bacteremia," study investigator Mike Allen, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "This is our first opportunity with a reasonable number of patients to ask how it performs as a first-line treatment."
Dr. Allen, senior medical development adviser at Novartis Pharmaceuticals UK, and his associates reported results from 487 patients in the EUCORE (European Cubicin Outcomes Registry and Experience) trial, an ongoing noninterventional multicenter study designed to assess the characteristics and clinical outcomes of patients with catheter-related bacteremia who were treated with at least one dose of daptomycin (Cubicin). Investigators followed protocol criteria and were asked to rate outcomes following daptomycin therapy as improved, failure, or nonevaluable. An outcome of cured or improved was considered a clinical success.
Of the 487 patients, 148 received daptomycin as a first-line therapy. Of these, 59% were male and 34% were aged 65 years or older. The majority (97%) had significant underlying diseases, particularly cardiovascular disease (44%) and oncologic disease (28%).
"This registry includes all comers, so what we have is a snapshot of clinical practice," Dr. Allen said. "It gives us a far better feel for how the drug is actually used. We don’t have the caveats of a clinical trial whereby we’re limited to a certain patient population."
Samples for microbiologic analysis were available for 134 patients, with 117 (87%) yielding positive culture. The two most common pathogens were coagulase-negative staphylococci (55%) and Staphylococcus aureus (27%), followed by enterococci (10%) and other pathogens.
The most frequent initial dose of daptomycin was 6 mg/kg and the median duration of therapy was 10 days. A majority of patients met the definition of clinical success (57% cured, 26% improved). Success rates reached 79% against methicillin-resistant S. aureus and S. epidermidis and 87% against other coagulase-negative staphylococci.
Among all 148 patients who received daptomycin as first-line therapy, 16 (11%) experienced mild to severe adverse events regardless of relationship to daptomycin treatment, including infections and renal and urinary disorders urinary disorders, and two of skin and subcutaneous tissue disorders.
The study was funded by Novartis. Dr. Allen is employed by Novartis Pharmaceuticals UK, which markets daptomycin in the EU.
The meeting was sponsored by the American Society for Microbiology.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Daptomycin was successful in 83% of patients who received it as a first-line treatment for catheter-related bacteremia (57% cured, 26% improved).
Data Source: Results were taken from a multicenter analysis of 148 patients enrolled in the ongoing EUCORE (European Cubicin Outcomes Registry and Experience) study.
Disclosures: The investigator is employed by Novartis Pharmaceuticals UK, which markets daptomycin and funded the study.
Antibiotic Resistance May Drive Cystitis Rx Changes
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
SAN FRANCISCO – Concerns about antibiotic resistance may be driving more physicians to prescribe second-line antibiotics for uncomplicated cystitis in women, a new study indicates.
Between 1998 and 2009, outpatient prescribing of first-line antibiotics for uncomplicated cystitis in women remained constant – yet the number of quinolone prescriptions grew significantly, results from an analysis of national data demonstrated.
The findings "reinforce what our gut instincts have been saying about prescribing for cystitis: Physicians are having more concerns about resistance and are therefore going to the second-line agents like quinolones, cephalosporins, and other medications," Jessina C. McGregor, Ph.D., said in an interview during a poster session at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Dr. McGregor and her associates analyzed data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey, which are nationally representative surveys of ambulatory and emergency department visits. They focused their study on women over age 17, and used linear tests to analyze trends in rates of visits for cystitis and related antibiotic prescribing patterns.
An estimated 124,978,631 visits among adult women were attributable to cystitis between 1998 and 2009, reported Dr. McGregor of the department of pharmacy practice at Oregon State University, Portland. The mean age of patients for these visits was 50 years, 83% were white, 69% presented to a physician’s office for their cystitis, and 48% had private insurance.
The annual rates of cystitis visits were stable between 1998 and 2009, with an average of 195 visits per 1,000 women. Nearly three-quarters of women (71%) received an antibiotic prescription during the study period.
Prescriptions for the first-line urinary anti-infectives trimethoprim/sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin remained constant (P = .10). But prescriptions for quinolones grew by 10%, and prescriptions for cephalosporins grew by 3%, which were statistically significant increases (P less than .01 and P = .02, respectively).
The findings "correlate with other data showing increasing rates of uropathogen resistance," the researchers wrote. "Further research is needed to evaluate empiric antibiotic prescribing in this setting to ensure prudent antibiotic use and limit the spread of resistance."
The conference was sponsored by the American Society for Microbiology.
Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY
Major Finding: Between 1998 and 2009, prescriptions for the first-line urinary anti-infectives trimethoprim/ sulfamethoxazole, trimethoprim, fosfomycin, and nitrofurantoin for uncomplicated cystitis in women remained constant (P = .10); yet prescriptions for quinolones grew by 10% and prescriptions for cephalosporins grew by 3% (P less than .01 and P = .02, respectively).
Data Source: This was an analysis of data from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey related to an estimated 124,978,631 visits for cystitis over the 10-year period.
Disclosures: Dr. McGregor reported that the National Institutes of Health and the National Center for Research Resources supported the study.
Noroviruses Affecting Diverse Populations
SAN FRANCISCO – As the availability of more sensitive diagnostic methods such as reverse transcription-polymerase chain reaction testing become more widespread, noroviruses are increasingly being recognized as important enteric pathogens in diverse populations.
"In the past, much of our knowledge about noroviruses has been hindered because we don’t have a good animal model or method for culturing norovirus," Dr. Hoonmo L. Koo said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "The majority of our current understanding has come from studying human outbreaks, volunteer challenge studies, and evaluating surrogate caliciviruses such as feline and murine caliciviruses, which don’t cause human infection but can be cultured."
Noroviruses (NoVs) are classified into five genetic groups based on their RNA capsid sequences, with genogroup I (GI) and genogroup II (GII) NoVs causing the most human NoV infections. GII.4 NoV strains are the predominant circulating genotype in the United States and worldwide, said Dr. Koo of Baylor College of Medicine, Houston. As reverse transcription-polymerase chain reaction testing (RT-PCR) has become more available in recent years, NoVs "are now recognized as the most definable common cause of acute nonbacterial gastroenteritis worldwide," he said. "They account for approximately half of all food-borne illness in the United States.
"Each year, NoVs cause about 21 million cases of infection in the United States. They occur throughout the year, but they peak in the winter season."
NoV outbreaks are common in children, travelers, restaurant patrons, military personnel, patients, and health care staff at hospitals, nursing homes, and other medical facilities. Dr. Koo and his associates conducted an 8.5-year surveillance study at Texas Children’s Hospital (TCH) investigating NoV, rotavirus (RV), and adenovirus prevalence at the facility before and after introduction of the RV vaccine in 2006. The study evaluated 8,173 stool samples from inpatients and outpatients at TCH from February 2002 to June 2010. The samples were evaluated for RV by antigen detection or electron microscopy and adenoviruses by electron microscopy. In addition, a subset of 3,222 stools were evaluated for NoV by RT-PCR (J. Ped. Infect. Dis. 2012 Aug. 3 [doi:10.1093/jpids/pis070]).
"We found that RV prevalence decreased significantly after the introduction of the RV vaccine in 2006," Dr. Koo said at the meeting, which was sponsored by the American Society for Microbiology. "In more recent years, it decreased from about 9% in 2007 to 3% in 2010." At the same time, he continued, "NoV prevalence increased in 2004 and was consistently between 11% and 17% from 2004 to 2010. There was no significant increase in NoV prevalence after the RV vaccine was introduced in 2006."
The researchers concluded that NoVs have emerged as the most common viral gastroenteritis pathogen at TCH, which is one of the largest pediatric hospitals in the United States. "We believe that as RV prevalence continues to decline with vaccination, NoVs will soon eclipse rotaviruses as the most important cause of pediatric gastroenteritis in the United States and other countries where the RV vaccine is successfully administered," Dr. Koo said.
In a separate study, he and his associates evaluated stools from 571 international travelers who acquired diarrhea in Guatemala, India, and Mexico (J. Clin. Microbiol. 2010;48:1673-6). NoVs were identified in 10% of cases of travelers’ diarrhea, and overall were the second most common pathogen following diarrheagenic Escherichia coli. "We concluded that NoVs are important pathogens of travelers’ diarrhea in multiple developing regions of the world," Dr. Koo said. "However, there was significant variation evident in the prevalence of NoV diarrhea and in the predominant genogroup infecting the travelers, depending on the specific geographic location and time period we looked at."
Immunocompromised patients also have been affected by NoVs. One report described 12 hematopoietic stem cell transplant patients with NoV gastroenteritis who were hospitalized for a median of 73 days (Clin. Infect. Dis. 2009;49:1069-71). Half of the patients required supplemental feeding with enteral or parenteral nutrition, and two patients died: one secondary to malnutrition and chronic NoV gastroenteritis. "Future areas of NoV study include further defining the burden of disease in pediatric and immunocompromised populations," Dr. Koo said. "We need development of sensitive diagnostic assays that can be used by clinical laboratories. Unfortunately, the ELISA assay that we have now for NoV detection is relatively insensitive, and most clinical laboratories cannot perform RT-PCR. We need effective therapeutic agents to be developed, and we need an effective NoV vaccine."
Results from a recent randomized, double-blind, placebo-controlled trial of an investigational NoV vaccine found a significantly lower frequency of viral gastroenteritis among vaccine recipients, compared with placebo recipients (37% vs. 69%, respectively; P = .006). It was found to be safe and well tolerated, and no severe adverse events were reported (N. Engl. J. Med. 2011;365:2178-87). "The vaccine was also found to be immunogenic, with 70% of vaccine recipients producing a fourfold rise in serum total antibody and serum IgA," Dr. Koo said. "However, there are significant challenges to the development of NoV vaccines. In the NEJM study, the frequency and magnitude of serum antibody response with the vaccine was lower than what’s been observed with natural infection. Previous studies have shown that acquired immunity with natural infection may be short-lived: less than 2 years. So how long will the vaccine protection last?"
Another challenge, he said, is that antibodies are only cross-protective within the same genogroup. "Future NoV vaccines will need to be composed of both GI and GII virus–like particles (VLPs)," he said. "Finally, significant antigenic diversity of noroviruses and the constant antigenic drift may require active surveillance similar to what we have for influenza viruses, where we are constantly surveying what strains are in the community and changing the composition of vaccine VLP strains to represent these important community strains."
Dr. Koo disclosed that he has received research support from the National Institute of Diabetes and Digestive and Kidney Diseases, and the Baylor College of Medicine Center for Globalization.
SAN FRANCISCO – As the availability of more sensitive diagnostic methods such as reverse transcription-polymerase chain reaction testing become more widespread, noroviruses are increasingly being recognized as important enteric pathogens in diverse populations.
"In the past, much of our knowledge about noroviruses has been hindered because we don’t have a good animal model or method for culturing norovirus," Dr. Hoonmo L. Koo said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "The majority of our current understanding has come from studying human outbreaks, volunteer challenge studies, and evaluating surrogate caliciviruses such as feline and murine caliciviruses, which don’t cause human infection but can be cultured."
Noroviruses (NoVs) are classified into five genetic groups based on their RNA capsid sequences, with genogroup I (GI) and genogroup II (GII) NoVs causing the most human NoV infections. GII.4 NoV strains are the predominant circulating genotype in the United States and worldwide, said Dr. Koo of Baylor College of Medicine, Houston. As reverse transcription-polymerase chain reaction testing (RT-PCR) has become more available in recent years, NoVs "are now recognized as the most definable common cause of acute nonbacterial gastroenteritis worldwide," he said. "They account for approximately half of all food-borne illness in the United States.
"Each year, NoVs cause about 21 million cases of infection in the United States. They occur throughout the year, but they peak in the winter season."
NoV outbreaks are common in children, travelers, restaurant patrons, military personnel, patients, and health care staff at hospitals, nursing homes, and other medical facilities. Dr. Koo and his associates conducted an 8.5-year surveillance study at Texas Children’s Hospital (TCH) investigating NoV, rotavirus (RV), and adenovirus prevalence at the facility before and after introduction of the RV vaccine in 2006. The study evaluated 8,173 stool samples from inpatients and outpatients at TCH from February 2002 to June 2010. The samples were evaluated for RV by antigen detection or electron microscopy and adenoviruses by electron microscopy. In addition, a subset of 3,222 stools were evaluated for NoV by RT-PCR (J. Ped. Infect. Dis. 2012 Aug. 3 [doi:10.1093/jpids/pis070]).
"We found that RV prevalence decreased significantly after the introduction of the RV vaccine in 2006," Dr. Koo said at the meeting, which was sponsored by the American Society for Microbiology. "In more recent years, it decreased from about 9% in 2007 to 3% in 2010." At the same time, he continued, "NoV prevalence increased in 2004 and was consistently between 11% and 17% from 2004 to 2010. There was no significant increase in NoV prevalence after the RV vaccine was introduced in 2006."
The researchers concluded that NoVs have emerged as the most common viral gastroenteritis pathogen at TCH, which is one of the largest pediatric hospitals in the United States. "We believe that as RV prevalence continues to decline with vaccination, NoVs will soon eclipse rotaviruses as the most important cause of pediatric gastroenteritis in the United States and other countries where the RV vaccine is successfully administered," Dr. Koo said.
In a separate study, he and his associates evaluated stools from 571 international travelers who acquired diarrhea in Guatemala, India, and Mexico (J. Clin. Microbiol. 2010;48:1673-6). NoVs were identified in 10% of cases of travelers’ diarrhea, and overall were the second most common pathogen following diarrheagenic Escherichia coli. "We concluded that NoVs are important pathogens of travelers’ diarrhea in multiple developing regions of the world," Dr. Koo said. "However, there was significant variation evident in the prevalence of NoV diarrhea and in the predominant genogroup infecting the travelers, depending on the specific geographic location and time period we looked at."
Immunocompromised patients also have been affected by NoVs. One report described 12 hematopoietic stem cell transplant patients with NoV gastroenteritis who were hospitalized for a median of 73 days (Clin. Infect. Dis. 2009;49:1069-71). Half of the patients required supplemental feeding with enteral or parenteral nutrition, and two patients died: one secondary to malnutrition and chronic NoV gastroenteritis. "Future areas of NoV study include further defining the burden of disease in pediatric and immunocompromised populations," Dr. Koo said. "We need development of sensitive diagnostic assays that can be used by clinical laboratories. Unfortunately, the ELISA assay that we have now for NoV detection is relatively insensitive, and most clinical laboratories cannot perform RT-PCR. We need effective therapeutic agents to be developed, and we need an effective NoV vaccine."
Results from a recent randomized, double-blind, placebo-controlled trial of an investigational NoV vaccine found a significantly lower frequency of viral gastroenteritis among vaccine recipients, compared with placebo recipients (37% vs. 69%, respectively; P = .006). It was found to be safe and well tolerated, and no severe adverse events were reported (N. Engl. J. Med. 2011;365:2178-87). "The vaccine was also found to be immunogenic, with 70% of vaccine recipients producing a fourfold rise in serum total antibody and serum IgA," Dr. Koo said. "However, there are significant challenges to the development of NoV vaccines. In the NEJM study, the frequency and magnitude of serum antibody response with the vaccine was lower than what’s been observed with natural infection. Previous studies have shown that acquired immunity with natural infection may be short-lived: less than 2 years. So how long will the vaccine protection last?"
Another challenge, he said, is that antibodies are only cross-protective within the same genogroup. "Future NoV vaccines will need to be composed of both GI and GII virus–like particles (VLPs)," he said. "Finally, significant antigenic diversity of noroviruses and the constant antigenic drift may require active surveillance similar to what we have for influenza viruses, where we are constantly surveying what strains are in the community and changing the composition of vaccine VLP strains to represent these important community strains."
Dr. Koo disclosed that he has received research support from the National Institute of Diabetes and Digestive and Kidney Diseases, and the Baylor College of Medicine Center for Globalization.
SAN FRANCISCO – As the availability of more sensitive diagnostic methods such as reverse transcription-polymerase chain reaction testing become more widespread, noroviruses are increasingly being recognized as important enteric pathogens in diverse populations.
"In the past, much of our knowledge about noroviruses has been hindered because we don’t have a good animal model or method for culturing norovirus," Dr. Hoonmo L. Koo said at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy. "The majority of our current understanding has come from studying human outbreaks, volunteer challenge studies, and evaluating surrogate caliciviruses such as feline and murine caliciviruses, which don’t cause human infection but can be cultured."
Noroviruses (NoVs) are classified into five genetic groups based on their RNA capsid sequences, with genogroup I (GI) and genogroup II (GII) NoVs causing the most human NoV infections. GII.4 NoV strains are the predominant circulating genotype in the United States and worldwide, said Dr. Koo of Baylor College of Medicine, Houston. As reverse transcription-polymerase chain reaction testing (RT-PCR) has become more available in recent years, NoVs "are now recognized as the most definable common cause of acute nonbacterial gastroenteritis worldwide," he said. "They account for approximately half of all food-borne illness in the United States.
"Each year, NoVs cause about 21 million cases of infection in the United States. They occur throughout the year, but they peak in the winter season."
NoV outbreaks are common in children, travelers, restaurant patrons, military personnel, patients, and health care staff at hospitals, nursing homes, and other medical facilities. Dr. Koo and his associates conducted an 8.5-year surveillance study at Texas Children’s Hospital (TCH) investigating NoV, rotavirus (RV), and adenovirus prevalence at the facility before and after introduction of the RV vaccine in 2006. The study evaluated 8,173 stool samples from inpatients and outpatients at TCH from February 2002 to June 2010. The samples were evaluated for RV by antigen detection or electron microscopy and adenoviruses by electron microscopy. In addition, a subset of 3,222 stools were evaluated for NoV by RT-PCR (J. Ped. Infect. Dis. 2012 Aug. 3 [doi:10.1093/jpids/pis070]).
"We found that RV prevalence decreased significantly after the introduction of the RV vaccine in 2006," Dr. Koo said at the meeting, which was sponsored by the American Society for Microbiology. "In more recent years, it decreased from about 9% in 2007 to 3% in 2010." At the same time, he continued, "NoV prevalence increased in 2004 and was consistently between 11% and 17% from 2004 to 2010. There was no significant increase in NoV prevalence after the RV vaccine was introduced in 2006."
The researchers concluded that NoVs have emerged as the most common viral gastroenteritis pathogen at TCH, which is one of the largest pediatric hospitals in the United States. "We believe that as RV prevalence continues to decline with vaccination, NoVs will soon eclipse rotaviruses as the most important cause of pediatric gastroenteritis in the United States and other countries where the RV vaccine is successfully administered," Dr. Koo said.
In a separate study, he and his associates evaluated stools from 571 international travelers who acquired diarrhea in Guatemala, India, and Mexico (J. Clin. Microbiol. 2010;48:1673-6). NoVs were identified in 10% of cases of travelers’ diarrhea, and overall were the second most common pathogen following diarrheagenic Escherichia coli. "We concluded that NoVs are important pathogens of travelers’ diarrhea in multiple developing regions of the world," Dr. Koo said. "However, there was significant variation evident in the prevalence of NoV diarrhea and in the predominant genogroup infecting the travelers, depending on the specific geographic location and time period we looked at."
Immunocompromised patients also have been affected by NoVs. One report described 12 hematopoietic stem cell transplant patients with NoV gastroenteritis who were hospitalized for a median of 73 days (Clin. Infect. Dis. 2009;49:1069-71). Half of the patients required supplemental feeding with enteral or parenteral nutrition, and two patients died: one secondary to malnutrition and chronic NoV gastroenteritis. "Future areas of NoV study include further defining the burden of disease in pediatric and immunocompromised populations," Dr. Koo said. "We need development of sensitive diagnostic assays that can be used by clinical laboratories. Unfortunately, the ELISA assay that we have now for NoV detection is relatively insensitive, and most clinical laboratories cannot perform RT-PCR. We need effective therapeutic agents to be developed, and we need an effective NoV vaccine."
Results from a recent randomized, double-blind, placebo-controlled trial of an investigational NoV vaccine found a significantly lower frequency of viral gastroenteritis among vaccine recipients, compared with placebo recipients (37% vs. 69%, respectively; P = .006). It was found to be safe and well tolerated, and no severe adverse events were reported (N. Engl. J. Med. 2011;365:2178-87). "The vaccine was also found to be immunogenic, with 70% of vaccine recipients producing a fourfold rise in serum total antibody and serum IgA," Dr. Koo said. "However, there are significant challenges to the development of NoV vaccines. In the NEJM study, the frequency and magnitude of serum antibody response with the vaccine was lower than what’s been observed with natural infection. Previous studies have shown that acquired immunity with natural infection may be short-lived: less than 2 years. So how long will the vaccine protection last?"
Another challenge, he said, is that antibodies are only cross-protective within the same genogroup. "Future NoV vaccines will need to be composed of both GI and GII virus–like particles (VLPs)," he said. "Finally, significant antigenic diversity of noroviruses and the constant antigenic drift may require active surveillance similar to what we have for influenza viruses, where we are constantly surveying what strains are in the community and changing the composition of vaccine VLP strains to represent these important community strains."
Dr. Koo disclosed that he has received research support from the National Institute of Diabetes and Digestive and Kidney Diseases, and the Baylor College of Medicine Center for Globalization.
AT THE ANNUAL INTERSCIENCE CONFERENCE ON ANTIMICROBIAL AGENTS AND CHEMOTHERAPY