User login
Doug Brunk is a San Diego-based award-winning reporter who began covering health care in 1991. Before joining the company, he wrote for the health sciences division of Columbia University and was an associate editor at Contemporary Long Term Care magazine when it won a Jesse H. Neal Award. His work has been syndicated by the Los Angeles Times and he is the author of two books related to the University of Kentucky Wildcats men's basketball program. Doug has a master’s degree in magazine journalism from the S.I. Newhouse School of Public Communications at Syracuse University. Follow him on Twitter @dougbrunk.
Kidney Disease a Risk Factor for Death in Pregnancy
SAN DIEGO – Pregnant women with kidney disease face an increased risk of adverse maternal outcomes including maternal mortality independent of underlying comorbid conditions that can occur with kidney disease, according to Dr. Shailendra Sharma.
"Any degree of kidney disease during pregnancy should be recognized and should be treated promptly with respect because we now know that can lead to bad outcomes down the road," Dr. Sharma said in an interview during a poster session at the Kidney Week 2012. "This is not something that should be underestimated."
Dr. Sharma, a second-year renal fellow at the University of Colorado, Aurora, and his associates retrospectively studied the records of 646 women with kidney disease who gave birth in Colorado and Utah between 2000 and 2011 at facilities operated by Intermountain Health Care. For comparison, the researchers randomly selected the records of 62,757 pregnancies from women without kidney disease.
Kidney disease was defined by ICD-9 code, and adverse maternal outcomes were defined as preterm delivery (prior to 37 weeks’ gestation), delivery by cesarean section, length of hospital stay, and maternal death. The researchers used multivariate logistic regression analysis to examine the association between kidney disease and adverse maternal outcomes. Covariates included in the fully adjusted model were maternal age, race, history of diabetes, chronic hypertension, liver disease, and connective tissue disorders.
The mean age of patients was 28 years. Compared with women who did not have kidney disease, those who did were significantly more likely to have comorbid conditions including diabetes (12% vs. 1%, respectively); chronic hypertension (2% vs. 7%); liver disease (9% vs. 1%); and connective tissue disorders (7% vs. 0.4%). They also were more likely to have preeclampsia/eclampsia (11% vs. 3%), to have a longer hospital stay (a mean of 3 vs. 2 days), and to give birth to a lower-weight infant (a mean of 3,067 g vs. 3,325 g).
After the investigators adjusted for age, race, history of diabetes, hypertension, liver disease, and connective tissue disorders, Dr. Sharma and his associates found that pregnant women with kidney disease had a significantly increased risk of death (OR, 3.38); preterm delivery (OR, 1.95); delivery via C-section (OR, 1.38); and longer length of hospital stay (OR, 1.39). "The most striking finding was the association of kidney disease with maternal mortality," Dr. Sharma said at the meeting, which was sponsored by the American Society of Nephrology. "The magnitude of this association surprised us."
He said that the retrospective design of the study is a limitation. "If there’s a prospective study moving forward, specifically designed to answer these questions, then it probably would help us establish the causality."
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Sharma said he had no relevant financial conflicts to disclose.
SAN DIEGO – Pregnant women with kidney disease face an increased risk of adverse maternal outcomes including maternal mortality independent of underlying comorbid conditions that can occur with kidney disease, according to Dr. Shailendra Sharma.
"Any degree of kidney disease during pregnancy should be recognized and should be treated promptly with respect because we now know that can lead to bad outcomes down the road," Dr. Sharma said in an interview during a poster session at the Kidney Week 2012. "This is not something that should be underestimated."
Dr. Sharma, a second-year renal fellow at the University of Colorado, Aurora, and his associates retrospectively studied the records of 646 women with kidney disease who gave birth in Colorado and Utah between 2000 and 2011 at facilities operated by Intermountain Health Care. For comparison, the researchers randomly selected the records of 62,757 pregnancies from women without kidney disease.
Kidney disease was defined by ICD-9 code, and adverse maternal outcomes were defined as preterm delivery (prior to 37 weeks’ gestation), delivery by cesarean section, length of hospital stay, and maternal death. The researchers used multivariate logistic regression analysis to examine the association between kidney disease and adverse maternal outcomes. Covariates included in the fully adjusted model were maternal age, race, history of diabetes, chronic hypertension, liver disease, and connective tissue disorders.
The mean age of patients was 28 years. Compared with women who did not have kidney disease, those who did were significantly more likely to have comorbid conditions including diabetes (12% vs. 1%, respectively); chronic hypertension (2% vs. 7%); liver disease (9% vs. 1%); and connective tissue disorders (7% vs. 0.4%). They also were more likely to have preeclampsia/eclampsia (11% vs. 3%), to have a longer hospital stay (a mean of 3 vs. 2 days), and to give birth to a lower-weight infant (a mean of 3,067 g vs. 3,325 g).
After the investigators adjusted for age, race, history of diabetes, hypertension, liver disease, and connective tissue disorders, Dr. Sharma and his associates found that pregnant women with kidney disease had a significantly increased risk of death (OR, 3.38); preterm delivery (OR, 1.95); delivery via C-section (OR, 1.38); and longer length of hospital stay (OR, 1.39). "The most striking finding was the association of kidney disease with maternal mortality," Dr. Sharma said at the meeting, which was sponsored by the American Society of Nephrology. "The magnitude of this association surprised us."
He said that the retrospective design of the study is a limitation. "If there’s a prospective study moving forward, specifically designed to answer these questions, then it probably would help us establish the causality."
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Sharma said he had no relevant financial conflicts to disclose.
SAN DIEGO – Pregnant women with kidney disease face an increased risk of adverse maternal outcomes including maternal mortality independent of underlying comorbid conditions that can occur with kidney disease, according to Dr. Shailendra Sharma.
"Any degree of kidney disease during pregnancy should be recognized and should be treated promptly with respect because we now know that can lead to bad outcomes down the road," Dr. Sharma said in an interview during a poster session at the Kidney Week 2012. "This is not something that should be underestimated."
Dr. Sharma, a second-year renal fellow at the University of Colorado, Aurora, and his associates retrospectively studied the records of 646 women with kidney disease who gave birth in Colorado and Utah between 2000 and 2011 at facilities operated by Intermountain Health Care. For comparison, the researchers randomly selected the records of 62,757 pregnancies from women without kidney disease.
Kidney disease was defined by ICD-9 code, and adverse maternal outcomes were defined as preterm delivery (prior to 37 weeks’ gestation), delivery by cesarean section, length of hospital stay, and maternal death. The researchers used multivariate logistic regression analysis to examine the association between kidney disease and adverse maternal outcomes. Covariates included in the fully adjusted model were maternal age, race, history of diabetes, chronic hypertension, liver disease, and connective tissue disorders.
The mean age of patients was 28 years. Compared with women who did not have kidney disease, those who did were significantly more likely to have comorbid conditions including diabetes (12% vs. 1%, respectively); chronic hypertension (2% vs. 7%); liver disease (9% vs. 1%); and connective tissue disorders (7% vs. 0.4%). They also were more likely to have preeclampsia/eclampsia (11% vs. 3%), to have a longer hospital stay (a mean of 3 vs. 2 days), and to give birth to a lower-weight infant (a mean of 3,067 g vs. 3,325 g).
After the investigators adjusted for age, race, history of diabetes, hypertension, liver disease, and connective tissue disorders, Dr. Sharma and his associates found that pregnant women with kidney disease had a significantly increased risk of death (OR, 3.38); preterm delivery (OR, 1.95); delivery via C-section (OR, 1.38); and longer length of hospital stay (OR, 1.39). "The most striking finding was the association of kidney disease with maternal mortality," Dr. Sharma said at the meeting, which was sponsored by the American Society of Nephrology. "The magnitude of this association surprised us."
He said that the retrospective design of the study is a limitation. "If there’s a prospective study moving forward, specifically designed to answer these questions, then it probably would help us establish the causality."
The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Sharma said he had no relevant financial conflicts to disclose.
AT KIDNEY WEEK 2012
Major Finding: Pregnant women with kidney disease had a significantly increased risk of death (OR, 3.38), preterm delivery (OR, 1.95), delivery via C-section (OR, 1.38), and longer length of hospital stay (OR, 1.39), compared with pregnant women who did not have kidney disease.
Data Source: Data are from a retrospective study comparing 646 women with kidney disease who gave birth in Colorado and Utah between 2000 and 2011 with 62,757 pregnancies from women without kidney disease. The women all gave birth at Intermountain Health Care.
Disclosures: The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Sharma said he had no relevant financial conflicts to disclose.
Pneumonia Prevalence Highest of Health Care-Associated Infections
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
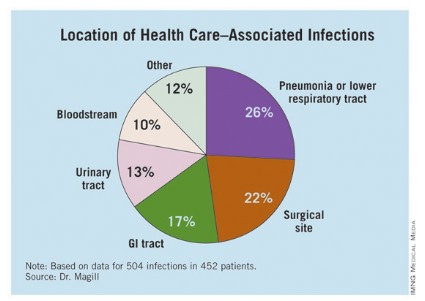
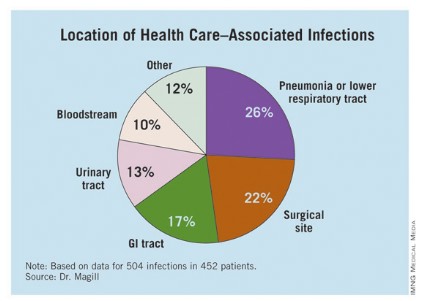
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
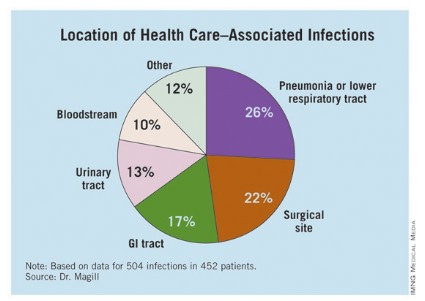
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
SAN DIEGO – The overall prevalence of health care–associated infections among inpatients in the United States stands at 4%, with the most common types of infections being a combination of pneumonia and lower respiratory infections.
Those are key preliminary findings from the Centers for Disease Control and Prevention’s first large-scale health care–associated infection (HAI) prevalence survey in more than 30 years, Dr. Shelley S. Magill reported during IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The data "can help us better understand the factors that influence HAI prevalence," said Dr. Magill of the division of health care quality promotion at the Centers for Disease Control and Prevention, Atlanta. "We can also clarify the burden of different HAI types and pathogens across the hospital, which can suggest areas to target for prevention."
The phase 3 survey was conducted in 2011 in 183 hospitals in 10 states: California, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, New York, Oregon, and Tennessee. Dr. Magill reported results from 11,282 patients who were surveyed in the 183 hospitals. Of these, 452 patients had HAIs, for a prevalence of 4%.
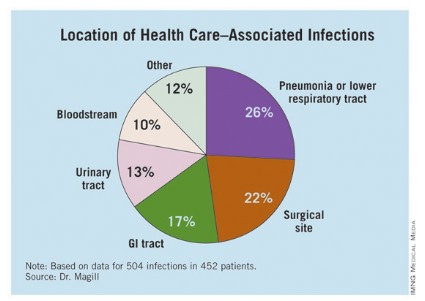
The researchers identified 504 HAIs in the 452 patients. Of these, the highest proportion (26%) were pneumonia or lower respiratory infections. "Of the pneumonia events, 39% were ventilator-associated infections," Dr. Magill said.
Surgical-site infections were the second most common infection type, representing 22% of all HAIs, followed by GI infections (17%), urinary tract infections (13%), and bloodstream infections (10%). "About two-third of UTIs were catheter associated and about 84% of the bloodstream infections were central-line associated," Dr. Magill noted.
Other infections made up the remaining 12% of HAIs.
Dr. Magill also reported that 56% of HAIs were attributed to non-ICU locations in the hospital while 53% were not directly associated with a device or with a procedure.
After multivariable regression analysis, patients with the following factors were at higher risk of having HAIs:
• Older age (risk ratio, 4.60 for patients older than age 77 compared with patients younger than 3 months old).
• Inpatient in a large hospital – defined as having 400 or more beds (RR, 1.24).
• Inpatient in a critical care unit (RR ,1.96 compared with all other units),
• Inpatient for more than 2 weeks at the time of the survey (RR, 26.09 compared with patients in the hospital for 3 days or fewer).
Pathogens were reported for 372 of the 504 HAIs. Clostridium difficile was the most common pathogen, accounting for 12% of all HAIs that were identified. Staphylococcus aureus was the second most common pathogen (11%; about half of these cases were methicillin-resistant S. aureus), followed by Klebsiella pneumoniae and Klebsiella oxytoca (10%).
Dr. Magill acknowledged certain limitations of the survey, including the fact that a small number of patients surveyed in each hospital "make results of limited use to individual facilities," she said. "We also had a relatively small number of hospitals in 10 states participate. This survey method provides a single snapshot of HAIs based on a retrospective review of medical record data, which is sometimes not complete. Finally, we were not able to collect a lot of detailed patient information, such as underlying illnesses and severity of illness."
She and her associates are currently planning a phase 4 survey, anticipated to occur in 2014.
Dr. Magill said she had no relevant financial conflicts to disclose.
AT IDWEEK 2012
Major Finding: The overall prevalence of health care–associated infections among hospitalized patients nationwide was 4%.
Data Source: Preliminary results were obtained from a 2011 survey of 11,282 inpatients at 183 hospitals located in 10 states.
Disclosures: The study was conducted by the Centers for Disease Control and Prevention. Dr. Magill said she had no relevant financial conflicts to disclose.
UV-C Light Blasts 'Bad Bugs' in Hospital Rooms
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Major Finding: UV-C irradiation of hospital rooms with a portable disinfection system reduced colony-forming units of vancomycin-resistant enterococci by 98%, C. difficile by 93%, and Acinetobacter by 98%.
Data Source: Results were taken from a study conducted in 39 hospital rooms at two tertiary medical centers.
Disclosures: The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
Most Gastric Tumors Handled Best With Laparoscopy
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital length of stay, compared with those who had open resection.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (mean of 3.3 days) than in the open group (mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.5), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-powered fields (OR, 4.7).
Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital length of stay, compared with those who had open resection.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (mean of 3.3 days) than in the open group (mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.5), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-powered fields (OR, 4.7).
Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Patients who underwent laparoscopic resection of gastric submucosal neoplasms had shorter operative times, less blood loss, lower postoperative morbidity, and shorter hospital length of stay, compared with those who had open resection.
"Numerous reports not only have assessed the feasibility, but confirmed the long-term oncologic efficacy of laparoscopic resection for gastrointestinal stromal tumors [GISTs]," Dr. Sabha Ganai said at the annual Digestive Disease Week.
"However, in 2004, the European Society of Medical Oncology published a consensus report suggesting that laparoscopic surgery may result in a higher risk of tumor rupture and peritoneal seeding, and suggested that laparoscopic resection may be acceptable in cases of small intramural tumors – those 2 cm or smaller," she added (Ann. Oncol. 2005;16:566-78).
Dr. Ganai, a fellow in surgical oncology and clinical medical ethics at the University of Chicago, noted that concerns exist "regarding the ability to generalize laparoscopic techniques to the spectra of gastric submucosal neoplasms, specifically related to tumor size and location, particularly the GE junction/cardia, the antrum/pylorus, and posteriorly based lesions."
To evaluate patient selection for a minimally invasive approach, Dr. Ganai and her associates compared laparoscopic and open techniques used in the resection of gastric submucosal neoplasms. "We hypothesized that there are predictors of unsuccessful laparoscopic resection, with failures defined by conversions, complications, and recurrences," she said.
The retrospective study involved 106 patients with gastric submucosal neoplasms who underwent operative management at the university from October 2002 to March 2012. There were 79 patients in the laparoscopic group and 27 in the open group. The mean age was 63 years, the mean body mass index was 29 kg/m2, and 57% were male.
There was less preoperative use of ultrasound in the open group vs. the laparoscopic group (67% vs. 87%, respectively), and greater pretreatment lesion size (9.5 cm vs. 3.9 cm). In addition, the open group had a 6-month greater interval from diagnosis to surgery (10.1 months vs. 4.4 months), and more neoadjuvant imatinib was used in the open group (26% vs. 5%).
Most tumors (76%) were GISTs; the rest were leiomyomas (9%), schwannomas (6%), carcinoids (3%), and other types (6%).
There were no significant differences between the groups in terms of tumor location; most were found in the greater curvature (41% open vs. 32% laparoscopic). "There were slightly more posterior lesions in the open group, but this was not statistically significant," she said. "On presentation, patients in the open group had a significantly greater presentation with abdominal pain, while those in the laparoscopic group were more likely to present with GI bleed."
Most patients underwent sleeve or wedge resection, with 11% of patients undergoing transgastric wedge resections. A higher proportion of the open group required a gastroenteric anastomosis (37% vs. 6%) and a multivisceral resection (41% vs. 1%). Overall, operative time was significantly greater in the open group (a mean of 230 minutes vs. 132 minutes), as was the estimated blood loss (a mean of 364 mL vs. 35 mL).
Most GISTs in the laparoscopic group (64%) ranged in size from 2 cm to 5 cm, while the majority in the open group (58%) were greater than 5 cm. In addition, the open group had a higher mitotic index (44% vs. 20%).
Postoperatively, hospital length of stay was significantly shorter in the laparoscopic group (mean of 3.3 days) than in the open group (mean of 8.4 days). The laparoscopic group also had significantly fewer surgical site infections (1% vs. 22%), anastomotic leaks (0% vs. 7%), and postoperative arrhythmias (0% vs. 15%).
Overall complications, evaluated on the basis of the Accordion Severity Grading System of surgical complications, were less severe in the laparoscopic group. "However, there was one perioperative death in the laparoscopic group related to a massive myocardial infarction, as well as two reoperations, one related to a port site hernia and one related to a gastric outlet obstruction in an antral lesion," Dr. Ganai said.
On multivariate analysis, conversion was predicted by tumor size greater than 8 cm (odds ratio, 18.5), while recurrence was predicted by having a mitotic rate of greater than 5 mitoses per 50 high-powered fields (OR, 4.7).
Laparoscopic resection resulted in better perioperative outcomes, with less morbidity, shorter operative times, less blood loss, and shorter lengths of stay (P less than .05). No significant difference was seen in survival; 90% and 81% of patients were alive 3 years after laparoscopic and open resection, respectively (hazard ratio, 0.4; P = .13). "Tumor biology and imatinib may play a greater role in oncologic outcome than technical considerations," Dr. Ganai suggested.
She acknowledged certain limitations of the study, including its retrospective design, the potential for selection bias, and limited follow-up, "especially in the lower-risk tumors."
Dr. Ganai said that she had no relevant financial conflicts to disclose.
Sternal SSIs, Mediastinitis Plummet Under Preop Decolonization Program
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
SAN DIEGO – Conducting preoperative nasal screening and decolonization of Staphylococcus aureus in patients undergoing cardiothoracic surgery led to a significant reduction in the rate of all sternal surgical site infections, including those attributable to S. aureus, results from a large single-center study showed.
"Staphylococcus aureus sternal surgical site infections [SSIs] are associated with significant morbidity and mortality," lead researcher Jennifer Madigan said in an interview following IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Multiple studies in the past have shown that screening and decolonization of S. aureus carriers are associated with a reduction in sternal SSIs."
One recent intervention that identified S. aureus nasal carriers concluded that S. aureus SSIs can be reduced by rapid screening and decolonization of nares on hospital admission (N. Engl. J. Med. 2010;362:9-17). "This study used [polymerase chain reaction testing] for identification of S. aureus nasal carriers, followed by treatment with mupirocin nasal ointment and chlorhexidine soap," said Ms. Madigan of the department of infection prevention and control at St. John Hospital and Medical Center, Detroit. "The results showed more than a 50% reduction in S. aureus infections."
Ms. Madigan and her associates compared the SSI rates 57 months before and 24 months after initiation of an S. aureus decolonization program for cardiothoracic surgery patients. For this program S. aureus nasal carriers were decolonized with mupirocin nasal ointment daily for 5 days and were asked to bathe with chlorhexidine gluconate rinse for 5 days immediately before surgery. The researchers reported results from 580 patients who were screened from April 2010 through March 2012. Of these patients, 118 (20%) tested positive for S. aureus colonization, including 34 (6%) who tested positive for methicillin-resistant S. aureus.
After the S. aureus decolonization program was initiated, the rate of postoperative sternal SSIs following coronary artery bypass grafting (CABG) decreased by 65% (from 76 infections per 1,416 cases before screening to 8 infections per 427 cases after screening; P = .0019), with a 75% drop in the number of mediastinitis cases (from 39 infections per 1,416 cases before screening to 3 infections per 427 cases after screening; P = .0106).
The researchers also found that sternal SSIs attributable to S. aureus dropped by 82% (from 39 infections per 1,416 cases before screening to 2 infections per 427 cases after screening; P = .0044), with S. aureus mediastinitis dropping by 87% (from 21 infections per 1,416 cases before screening to 1 infection per 427 cases after screening; P = .0337).
"We encourage hospitals that perform CABG surgeries to incorporate this [decolonization program] into their process," Ms. Madigan said. "The program is associated with significant reductions in infection, morbidity, and mortality. It provides a great tool to reduce the risk of patient harm. In addition, this may have a positive financial impact on hospitals as mediastinitis is no longer a reimbursable condition."
Ms. Madigan said that she had no relevant financial conflicts.
AT IDWEEK 2012
Major Finding: Following initiation of a preoperative S. aureus decolonization program, the rate of postoperative sternal SSIs following coronary artery bypass grafting dropped by 65%, and the rate of mediastinitis cases dropped by 75%.
Data Source: A single-center study of 580 cardiothoracic surgery patients who were screened from April 2010 through March 2012.
Disclosures: The researchers reported having no relevant financial conflicts.
Postpartum Tdap Acceptance Impacts Infant Vaccine Rates
SAN DIEGO – Maternal acceptance of influenza vaccine during pregnancy and postpartum Tdap immunization both increase infant vaccination rates, results from a large single-center study showed.
"The postpartum period may be an optimal time for education of current threats related to vaccine-preventable infection for mothers and infants," lead study author Gina Calarco said in an interview after IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Getting obstetricians and pediatricians actively discussing and educating their patients during this critical period appears to benefit both maternal and infant vaccination rates."
Ms. Calarco and her coinvestigators enrolled 900 postpartum women-infant dyads cared for at Shawnee Mission (Kan.) Medical Center in a prospective study intended to evaluate Tdap vaccine acceptance. This particular hospital was targeted as the research site because of its "location in a relatively affluent area with higher education and socioeconomic status and the highest birth rates in the bistate area," explained Ms. Calarco, who led the study during her tenure as infectious disease study coordinator at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. "In past studies this type of demographic has been known to be vaccine hesitant and this is why we chose this facility. We compared maternal acceptance of Tdap to the infant’s 3-month vaccine record to determine if there are any early indicators of vaccine-hesitant parents. Our overall question was to determine if mom declined vaccination of herself, is she more likely to not fully vaccinate her infant, or conversely if a mom accepts Tdap, does that impact her infant’s vaccine status at 3 months of age."
The mean age of the study participants was 28 years, 83% were white, 66% were married, and 67% had private insurance. Ms. Calarco, who is now a clinical project manager with Quintiles in Overland Park, Kan., reported that 597 of the mothers (66%) received Tdap prior to discharge and 269 (30%) declined the vaccine, while 34 (4%) had received Tdap within 2 years and thus were not currently eligible to receive the vaccine prior to discharge.
A total of 757 maternal Tdap and infant vaccine records and 740 maternal influenza and infant vaccine records were available for analysis. The records revealed that mothers who accepted Tdap were 13.5 times more likely to fully immunize their infant than not to do so. In addition, mothers who received the influenza vaccine were 1.85 times more likely to fully immunize their children than were mothers who did not receive the influenza vaccine.
When the researchers adjusted for maternal age, they found that mothers older than 28 years had a 6% per year increase in having a fully vaccinated infant (OR, 1.06) However, the 34 mothers who had Tdap within the previous 2 years were less likely to have a fully vaccinated infant, compared with other mothers in the study (OR, 0.28). "This was surprising in that these women had accepted Tdap for themselves previously yet were not as likely to immunize their infant," Ms. Calarco commented. "We haven’t explored this finding further, but it may be that the education supplied when they received Tdap was too far removed from them vaccinating their infant, or maybe they received a required tetanus booster vaccine due to an accident and this wasn’t as much [of] a choice."
The study was supported by a grant from the Kenneth and Eva Smith Foundation. Ms. Calarco said she had no relevant financial disclosures.
SAN DIEGO – Maternal acceptance of influenza vaccine during pregnancy and postpartum Tdap immunization both increase infant vaccination rates, results from a large single-center study showed.
"The postpartum period may be an optimal time for education of current threats related to vaccine-preventable infection for mothers and infants," lead study author Gina Calarco said in an interview after IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Getting obstetricians and pediatricians actively discussing and educating their patients during this critical period appears to benefit both maternal and infant vaccination rates."
Ms. Calarco and her coinvestigators enrolled 900 postpartum women-infant dyads cared for at Shawnee Mission (Kan.) Medical Center in a prospective study intended to evaluate Tdap vaccine acceptance. This particular hospital was targeted as the research site because of its "location in a relatively affluent area with higher education and socioeconomic status and the highest birth rates in the bistate area," explained Ms. Calarco, who led the study during her tenure as infectious disease study coordinator at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. "In past studies this type of demographic has been known to be vaccine hesitant and this is why we chose this facility. We compared maternal acceptance of Tdap to the infant’s 3-month vaccine record to determine if there are any early indicators of vaccine-hesitant parents. Our overall question was to determine if mom declined vaccination of herself, is she more likely to not fully vaccinate her infant, or conversely if a mom accepts Tdap, does that impact her infant’s vaccine status at 3 months of age."
The mean age of the study participants was 28 years, 83% were white, 66% were married, and 67% had private insurance. Ms. Calarco, who is now a clinical project manager with Quintiles in Overland Park, Kan., reported that 597 of the mothers (66%) received Tdap prior to discharge and 269 (30%) declined the vaccine, while 34 (4%) had received Tdap within 2 years and thus were not currently eligible to receive the vaccine prior to discharge.
A total of 757 maternal Tdap and infant vaccine records and 740 maternal influenza and infant vaccine records were available for analysis. The records revealed that mothers who accepted Tdap were 13.5 times more likely to fully immunize their infant than not to do so. In addition, mothers who received the influenza vaccine were 1.85 times more likely to fully immunize their children than were mothers who did not receive the influenza vaccine.
When the researchers adjusted for maternal age, they found that mothers older than 28 years had a 6% per year increase in having a fully vaccinated infant (OR, 1.06) However, the 34 mothers who had Tdap within the previous 2 years were less likely to have a fully vaccinated infant, compared with other mothers in the study (OR, 0.28). "This was surprising in that these women had accepted Tdap for themselves previously yet were not as likely to immunize their infant," Ms. Calarco commented. "We haven’t explored this finding further, but it may be that the education supplied when they received Tdap was too far removed from them vaccinating their infant, or maybe they received a required tetanus booster vaccine due to an accident and this wasn’t as much [of] a choice."
The study was supported by a grant from the Kenneth and Eva Smith Foundation. Ms. Calarco said she had no relevant financial disclosures.
SAN DIEGO – Maternal acceptance of influenza vaccine during pregnancy and postpartum Tdap immunization both increase infant vaccination rates, results from a large single-center study showed.
"The postpartum period may be an optimal time for education of current threats related to vaccine-preventable infection for mothers and infants," lead study author Gina Calarco said in an interview after IDWeek 2012, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. "Getting obstetricians and pediatricians actively discussing and educating their patients during this critical period appears to benefit both maternal and infant vaccination rates."
Ms. Calarco and her coinvestigators enrolled 900 postpartum women-infant dyads cared for at Shawnee Mission (Kan.) Medical Center in a prospective study intended to evaluate Tdap vaccine acceptance. This particular hospital was targeted as the research site because of its "location in a relatively affluent area with higher education and socioeconomic status and the highest birth rates in the bistate area," explained Ms. Calarco, who led the study during her tenure as infectious disease study coordinator at Children’s Mercy Hospitals and Clinics in Kansas City, Mo. "In past studies this type of demographic has been known to be vaccine hesitant and this is why we chose this facility. We compared maternal acceptance of Tdap to the infant’s 3-month vaccine record to determine if there are any early indicators of vaccine-hesitant parents. Our overall question was to determine if mom declined vaccination of herself, is she more likely to not fully vaccinate her infant, or conversely if a mom accepts Tdap, does that impact her infant’s vaccine status at 3 months of age."
The mean age of the study participants was 28 years, 83% were white, 66% were married, and 67% had private insurance. Ms. Calarco, who is now a clinical project manager with Quintiles in Overland Park, Kan., reported that 597 of the mothers (66%) received Tdap prior to discharge and 269 (30%) declined the vaccine, while 34 (4%) had received Tdap within 2 years and thus were not currently eligible to receive the vaccine prior to discharge.
A total of 757 maternal Tdap and infant vaccine records and 740 maternal influenza and infant vaccine records were available for analysis. The records revealed that mothers who accepted Tdap were 13.5 times more likely to fully immunize their infant than not to do so. In addition, mothers who received the influenza vaccine were 1.85 times more likely to fully immunize their children than were mothers who did not receive the influenza vaccine.
When the researchers adjusted for maternal age, they found that mothers older than 28 years had a 6% per year increase in having a fully vaccinated infant (OR, 1.06) However, the 34 mothers who had Tdap within the previous 2 years were less likely to have a fully vaccinated infant, compared with other mothers in the study (OR, 0.28). "This was surprising in that these women had accepted Tdap for themselves previously yet were not as likely to immunize their infant," Ms. Calarco commented. "We haven’t explored this finding further, but it may be that the education supplied when they received Tdap was too far removed from them vaccinating their infant, or maybe they received a required tetanus booster vaccine due to an accident and this wasn’t as much [of] a choice."
The study was supported by a grant from the Kenneth and Eva Smith Foundation. Ms. Calarco said she had no relevant financial disclosures.
AT IDWEEK 2012
Major Finding: Mothers who accepted the Tdap vaccine were 13.5 times more likely to fully immunize their infant than not to do so. Also, mothers who received the influenza vaccine were 1.85 times more likely to fully immunize their infant than were mothers who did not receive the influenza vaccine.
Data Source: Data are from a prospective study of 900 postpartum women-infant dyads at a single community hospital that evaluated Tdap vaccine acceptance.
Disclosures: The study was supported by a grant from the Kenneth and Eva Smith Foundation. Ms. Calarco said she had no relevant financial disclosures.
Serious Bacterial Infections Uncommon in Infants
SAN DIEGO – The incidence rate of serious bacterial infections in infants age 1 week to 3 months is relatively low, at 4.6/1,000 full-term births, results from a long-term study showed.
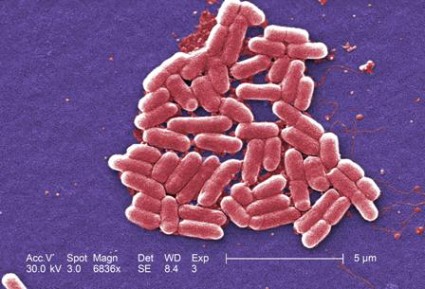
In addition, Escherichia coli is the most common cause of bacteremia, urinary tract infections, and meningitis in this patient population.
Despite decades of research, the incidence rate and current risk factors of serious bacterial infections have not been performed," investigators led by Dr. Tara L. Greenhow wrote in a poster presented during IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Greenhow, a pediatric infectious disease specialist with Kaiser Permanente Northern California, San Francisco, and her associates retrospectively reviewed all blood, urine, cerebral spine fluid, and stool cultures in 216,005 full-term healthy infants aged 1 week to 3 months between Jan. 1, 2005, and Sept. 1, 2011. Cultures were collected in the outpatient setting, emergency department, or first 24 hours of hospitalization. Nonpathogens were excluded from the analysis.
During the study period, 871 infants had a total of 1,004 serious bacterial infections, including 841 urinary tract infections, 125 cases of bacteremia, 22 cases of bacterial gastroenteritis, and 16 cases of bacterial meningitis. A higher proportion of males than females were affected by each infection, with the exception of meningitis, which affected females in 9 cases (56%). No cases of Listeria or meningococcal infection were observed.
The researchers reported that the overall incidence rate of serious bacterial infections was 4.6/1,000 full-term births, while the incidence rate of febrile serious bacterial infections was 3.5/1,000 full-term births. The incidence rate of bacteremia, UTI, meningitis, and gastroenteritis was 0.58, 3.89, 0.08, and 0.10 per 1,000 full-term births, respectively.
E. coli was the culprit in 64% of bacteremia cases, 91% of UTIs, and 44% of meningitis cases, while Salmonella sp. was the most common cause of gastroenteritis (86%).
Other authors on the study were Yun-Yi Hung, Ph.D., and Dr. Arnd Herz. The project was funded by a community benefit grant from Kaiser Permanente Northern California. The investigators had no relevant financial disclosures.
SAN DIEGO – The incidence rate of serious bacterial infections in infants age 1 week to 3 months is relatively low, at 4.6/1,000 full-term births, results from a long-term study showed.
In addition, Escherichia coli is the most common cause of bacteremia, urinary tract infections, and meningitis in this patient population.
Despite decades of research, the incidence rate and current risk factors of serious bacterial infections have not been performed," investigators led by Dr. Tara L. Greenhow wrote in a poster presented during IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Greenhow, a pediatric infectious disease specialist with Kaiser Permanente Northern California, San Francisco, and her associates retrospectively reviewed all blood, urine, cerebral spine fluid, and stool cultures in 216,005 full-term healthy infants aged 1 week to 3 months between Jan. 1, 2005, and Sept. 1, 2011. Cultures were collected in the outpatient setting, emergency department, or first 24 hours of hospitalization. Nonpathogens were excluded from the analysis.
During the study period, 871 infants had a total of 1,004 serious bacterial infections, including 841 urinary tract infections, 125 cases of bacteremia, 22 cases of bacterial gastroenteritis, and 16 cases of bacterial meningitis. A higher proportion of males than females were affected by each infection, with the exception of meningitis, which affected females in 9 cases (56%). No cases of Listeria or meningococcal infection were observed.
The researchers reported that the overall incidence rate of serious bacterial infections was 4.6/1,000 full-term births, while the incidence rate of febrile serious bacterial infections was 3.5/1,000 full-term births. The incidence rate of bacteremia, UTI, meningitis, and gastroenteritis was 0.58, 3.89, 0.08, and 0.10 per 1,000 full-term births, respectively.
E. coli was the culprit in 64% of bacteremia cases, 91% of UTIs, and 44% of meningitis cases, while Salmonella sp. was the most common cause of gastroenteritis (86%).
Other authors on the study were Yun-Yi Hung, Ph.D., and Dr. Arnd Herz. The project was funded by a community benefit grant from Kaiser Permanente Northern California. The investigators had no relevant financial disclosures.
SAN DIEGO – The incidence rate of serious bacterial infections in infants age 1 week to 3 months is relatively low, at 4.6/1,000 full-term births, results from a long-term study showed.
In addition, Escherichia coli is the most common cause of bacteremia, urinary tract infections, and meningitis in this patient population.
Despite decades of research, the incidence rate and current risk factors of serious bacterial infections have not been performed," investigators led by Dr. Tara L. Greenhow wrote in a poster presented during IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Greenhow, a pediatric infectious disease specialist with Kaiser Permanente Northern California, San Francisco, and her associates retrospectively reviewed all blood, urine, cerebral spine fluid, and stool cultures in 216,005 full-term healthy infants aged 1 week to 3 months between Jan. 1, 2005, and Sept. 1, 2011. Cultures were collected in the outpatient setting, emergency department, or first 24 hours of hospitalization. Nonpathogens were excluded from the analysis.
During the study period, 871 infants had a total of 1,004 serious bacterial infections, including 841 urinary tract infections, 125 cases of bacteremia, 22 cases of bacterial gastroenteritis, and 16 cases of bacterial meningitis. A higher proportion of males than females were affected by each infection, with the exception of meningitis, which affected females in 9 cases (56%). No cases of Listeria or meningococcal infection were observed.
The researchers reported that the overall incidence rate of serious bacterial infections was 4.6/1,000 full-term births, while the incidence rate of febrile serious bacterial infections was 3.5/1,000 full-term births. The incidence rate of bacteremia, UTI, meningitis, and gastroenteritis was 0.58, 3.89, 0.08, and 0.10 per 1,000 full-term births, respectively.
E. coli was the culprit in 64% of bacteremia cases, 91% of UTIs, and 44% of meningitis cases, while Salmonella sp. was the most common cause of gastroenteritis (86%).
Other authors on the study were Yun-Yi Hung, Ph.D., and Dr. Arnd Herz. The project was funded by a community benefit grant from Kaiser Permanente Northern California. The investigators had no relevant financial disclosures.
AT IDWEEK 2012
Major Finding: The overall incidence rate of serious bacterial infections was 4.6/1,000 full-term births while the incidence rate of febrile serious bacterial infections was 3.5/1,000 full-term births.
Data Source: This was a study of 871 full-term infants aged 1 week to 3 months who had 1,004 serious bacterial infections between Jan. 1, 2005, and Sept. 1, 2011.
Disclosures: The project was funded by a community benefit grant from Kaiser Permanente Northern California. The investigators had no relevant financial disclosures.
Typhoid Vaccines Estimated to Be 84% Effective
SAN DIEGO – Typhoid vaccines continue to be 84% effective and should be given to patients who are traveling to typhoid endemic areas, based on the results of a survey of case reports to the Centers for Disease Control and Prevention.
Patients also need to be reminded to follow safe food and water precautions, since the vaccine is not 100% effective, Anna Newton, M.P.H., said in an interview during a poster session during IDWeek.
Ms. Newton and her colleagues analyzed the National Typhoid and Paratyphoid Fever Surveillance database from 2008-2010. Managed by Ms. Newton, this database contains demographic information, travel history, and typhoid vaccination status in the 5 years before illness onset in cases of typhoid fever and paratyphoid fever reported to the CDC by state and local health officials. The researchers estimated vaccine effectiveness by comparing vaccination rates in travelers who became infected.
From 2008 to 2010, the CDC received data regarding 977 travelers with typhoid fever and 241 with paratyphoid fever. Vaccination status was available in 65% of travelers with typhoid fever and 50% of those with paratyphoid fever. From this data the researchers estimated the vaccine effectiveness to be 84%, "which is on par with what we expected to find," Ms. Newton said. "The vaccine is moderately effective."
Only 6% of patients with typhoid fever and 29% with paratyphoid fever reported having received a typhoid vaccine within the past 5 years. Asia was the most common region of travel for patients with typhoid fever (94%) and paratyphoid fever (99%), with India being the most commonly reported destination country (57% and 67%, respectively).
Two typhoid vaccines are currently available in the United States: a live attenuated oral vaccine (Vivotif, Crucell/Berna) and an intramuscular polysaccharide vaccine (Typhim Vi, Sanofi Pasteur). Neither is licensed for use in children younger than 2 years of age. Prior to the current analysis little had been known about the effectiveness of either vaccine in U.S. travelers, said Ms. Newton, a surveillance epidemiologist with the Enteric Diseases Epidemiology Branch of the Centers for Disease Control and Prevention, Atlanta.
Ms. Newton acknowledged certain limitations of the study, including the fact that many patients were excluded due to unknown vaccination status. "Improvement in completeness of reporting vaccination status and type of vaccine received could enhance the reliability of these estimates and could facilitate estimation of vaccine effectiveness for each vaccine," the researchers concluded in their abstract.
IDWEEK was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. Ms. Newton said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Typhoid vaccines continue to be 84% effective and should be given to patients who are traveling to typhoid endemic areas, based on the results of a survey of case reports to the Centers for Disease Control and Prevention.
Patients also need to be reminded to follow safe food and water precautions, since the vaccine is not 100% effective, Anna Newton, M.P.H., said in an interview during a poster session during IDWeek.
Ms. Newton and her colleagues analyzed the National Typhoid and Paratyphoid Fever Surveillance database from 2008-2010. Managed by Ms. Newton, this database contains demographic information, travel history, and typhoid vaccination status in the 5 years before illness onset in cases of typhoid fever and paratyphoid fever reported to the CDC by state and local health officials. The researchers estimated vaccine effectiveness by comparing vaccination rates in travelers who became infected.
From 2008 to 2010, the CDC received data regarding 977 travelers with typhoid fever and 241 with paratyphoid fever. Vaccination status was available in 65% of travelers with typhoid fever and 50% of those with paratyphoid fever. From this data the researchers estimated the vaccine effectiveness to be 84%, "which is on par with what we expected to find," Ms. Newton said. "The vaccine is moderately effective."
Only 6% of patients with typhoid fever and 29% with paratyphoid fever reported having received a typhoid vaccine within the past 5 years. Asia was the most common region of travel for patients with typhoid fever (94%) and paratyphoid fever (99%), with India being the most commonly reported destination country (57% and 67%, respectively).
Two typhoid vaccines are currently available in the United States: a live attenuated oral vaccine (Vivotif, Crucell/Berna) and an intramuscular polysaccharide vaccine (Typhim Vi, Sanofi Pasteur). Neither is licensed for use in children younger than 2 years of age. Prior to the current analysis little had been known about the effectiveness of either vaccine in U.S. travelers, said Ms. Newton, a surveillance epidemiologist with the Enteric Diseases Epidemiology Branch of the Centers for Disease Control and Prevention, Atlanta.
Ms. Newton acknowledged certain limitations of the study, including the fact that many patients were excluded due to unknown vaccination status. "Improvement in completeness of reporting vaccination status and type of vaccine received could enhance the reliability of these estimates and could facilitate estimation of vaccine effectiveness for each vaccine," the researchers concluded in their abstract.
IDWEEK was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. Ms. Newton said that she had no relevant financial conflicts to disclose.
SAN DIEGO – Typhoid vaccines continue to be 84% effective and should be given to patients who are traveling to typhoid endemic areas, based on the results of a survey of case reports to the Centers for Disease Control and Prevention.
Patients also need to be reminded to follow safe food and water precautions, since the vaccine is not 100% effective, Anna Newton, M.P.H., said in an interview during a poster session during IDWeek.
Ms. Newton and her colleagues analyzed the National Typhoid and Paratyphoid Fever Surveillance database from 2008-2010. Managed by Ms. Newton, this database contains demographic information, travel history, and typhoid vaccination status in the 5 years before illness onset in cases of typhoid fever and paratyphoid fever reported to the CDC by state and local health officials. The researchers estimated vaccine effectiveness by comparing vaccination rates in travelers who became infected.
From 2008 to 2010, the CDC received data regarding 977 travelers with typhoid fever and 241 with paratyphoid fever. Vaccination status was available in 65% of travelers with typhoid fever and 50% of those with paratyphoid fever. From this data the researchers estimated the vaccine effectiveness to be 84%, "which is on par with what we expected to find," Ms. Newton said. "The vaccine is moderately effective."
Only 6% of patients with typhoid fever and 29% with paratyphoid fever reported having received a typhoid vaccine within the past 5 years. Asia was the most common region of travel for patients with typhoid fever (94%) and paratyphoid fever (99%), with India being the most commonly reported destination country (57% and 67%, respectively).
Two typhoid vaccines are currently available in the United States: a live attenuated oral vaccine (Vivotif, Crucell/Berna) and an intramuscular polysaccharide vaccine (Typhim Vi, Sanofi Pasteur). Neither is licensed for use in children younger than 2 years of age. Prior to the current analysis little had been known about the effectiveness of either vaccine in U.S. travelers, said Ms. Newton, a surveillance epidemiologist with the Enteric Diseases Epidemiology Branch of the Centers for Disease Control and Prevention, Atlanta.
Ms. Newton acknowledged certain limitations of the study, including the fact that many patients were excluded due to unknown vaccination status. "Improvement in completeness of reporting vaccination status and type of vaccine received could enhance the reliability of these estimates and could facilitate estimation of vaccine effectiveness for each vaccine," the researchers concluded in their abstract.
IDWEEK was the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society. Ms. Newton said that she had no relevant financial conflicts to disclose.
AT IDWEEK
Major Finding: The estimated effectiveness of typhoid vaccines in travelers stands at 84%.
Data Source: A study of 649 cases of typhoid fever and 122 cases of paratyphoid fever reported to the National Typhoid and Paratyphoid Fever Surveillance System between 2008 and 2010.
Disclosures: The study was conducted by the Centers for Disease Control and Prevention.
Probiotics Plus High-Risk Antibiotics Increased C. difficile Risk
SAN DIEGO – The concomitant use of probiotics and antibiotics associated with a high risk of acquiring Clostridium difficile infections increased the risk of developing C. difficile by nearly threefold, a single-center retrospective study showed.
"We were very surprised by this finding," Justine E. Dickson, Pharm. D., said in an interview at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Dickson and her colleagues at Yale–New Haven Hospital evaluated 389 adult inpatients who received high-risk antibiotics for 5 days or more between July 1 and Dec. 31, 2010. High-risk antibiotics investigated included ceftriaxone, ciprofloxacin, clindamycin, imipenem-cilastatin, levofloxacin, and meropenem. Formulary probiotics investigated were Lactobacillus GG and Saccharomyces boulardii.
Of the 389 patients, 246 (63%) received antibiotics alone while 143 (37%) received antibiotics and a probiotic. A total of 20 patients (5%) developed a C. difficile infection (CDI) within 90 days of antibiotic use. The average duration of high-risk antibiotic use was 7.3 days among those who received probiotics and 7.7 days among those in the antibiotics-only group.
Dr. Dickson, who is now a PGY-2 ambulatory care pharmacy resident at the University Hospital in Cincinnati, reported that the incidence of CDI was 8.4% among patients who received probiotics compared with 3.3% in the antibiotics-only group. Levofloxacin was the most common high-risk antibiotic used by patients who developed a CDI, representing 65% of cases.
The risk of developing CDI among patients who received probiotics was 2.7 times higher than in patients in the antibiotics-only group, a difference that reached statistical significance. After controlling for the use of levofloxacin (the researchers initially speculated that this antibiotic might be a key culprit), they found that the relative risk remained similar, at 2.6 times higher among patients who received probiotics.
When the researchers factored in the concomitant use of proton pump inhibitors, the incidence of CDI did not differ among patients in the antibiotics-only group, but the concomitant use of probiotics further increased the risk of CDI, "which may suggest a potential interaction between these two drug classes," the researchers wrote in their abstract, which was presented during a poster session.
The investigators stated that they had no relevant financial conflicts to disclose.
SAN DIEGO – The concomitant use of probiotics and antibiotics associated with a high risk of acquiring Clostridium difficile infections increased the risk of developing C. difficile by nearly threefold, a single-center retrospective study showed.
"We were very surprised by this finding," Justine E. Dickson, Pharm. D., said in an interview at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Dickson and her colleagues at Yale–New Haven Hospital evaluated 389 adult inpatients who received high-risk antibiotics for 5 days or more between July 1 and Dec. 31, 2010. High-risk antibiotics investigated included ceftriaxone, ciprofloxacin, clindamycin, imipenem-cilastatin, levofloxacin, and meropenem. Formulary probiotics investigated were Lactobacillus GG and Saccharomyces boulardii.
Of the 389 patients, 246 (63%) received antibiotics alone while 143 (37%) received antibiotics and a probiotic. A total of 20 patients (5%) developed a C. difficile infection (CDI) within 90 days of antibiotic use. The average duration of high-risk antibiotic use was 7.3 days among those who received probiotics and 7.7 days among those in the antibiotics-only group.
Dr. Dickson, who is now a PGY-2 ambulatory care pharmacy resident at the University Hospital in Cincinnati, reported that the incidence of CDI was 8.4% among patients who received probiotics compared with 3.3% in the antibiotics-only group. Levofloxacin was the most common high-risk antibiotic used by patients who developed a CDI, representing 65% of cases.
The risk of developing CDI among patients who received probiotics was 2.7 times higher than in patients in the antibiotics-only group, a difference that reached statistical significance. After controlling for the use of levofloxacin (the researchers initially speculated that this antibiotic might be a key culprit), they found that the relative risk remained similar, at 2.6 times higher among patients who received probiotics.
When the researchers factored in the concomitant use of proton pump inhibitors, the incidence of CDI did not differ among patients in the antibiotics-only group, but the concomitant use of probiotics further increased the risk of CDI, "which may suggest a potential interaction between these two drug classes," the researchers wrote in their abstract, which was presented during a poster session.
The investigators stated that they had no relevant financial conflicts to disclose.
SAN DIEGO – The concomitant use of probiotics and antibiotics associated with a high risk of acquiring Clostridium difficile infections increased the risk of developing C. difficile by nearly threefold, a single-center retrospective study showed.
"We were very surprised by this finding," Justine E. Dickson, Pharm. D., said in an interview at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Dr. Dickson and her colleagues at Yale–New Haven Hospital evaluated 389 adult inpatients who received high-risk antibiotics for 5 days or more between July 1 and Dec. 31, 2010. High-risk antibiotics investigated included ceftriaxone, ciprofloxacin, clindamycin, imipenem-cilastatin, levofloxacin, and meropenem. Formulary probiotics investigated were Lactobacillus GG and Saccharomyces boulardii.
Of the 389 patients, 246 (63%) received antibiotics alone while 143 (37%) received antibiotics and a probiotic. A total of 20 patients (5%) developed a C. difficile infection (CDI) within 90 days of antibiotic use. The average duration of high-risk antibiotic use was 7.3 days among those who received probiotics and 7.7 days among those in the antibiotics-only group.
Dr. Dickson, who is now a PGY-2 ambulatory care pharmacy resident at the University Hospital in Cincinnati, reported that the incidence of CDI was 8.4% among patients who received probiotics compared with 3.3% in the antibiotics-only group. Levofloxacin was the most common high-risk antibiotic used by patients who developed a CDI, representing 65% of cases.
The risk of developing CDI among patients who received probiotics was 2.7 times higher than in patients in the antibiotics-only group, a difference that reached statistical significance. After controlling for the use of levofloxacin (the researchers initially speculated that this antibiotic might be a key culprit), they found that the relative risk remained similar, at 2.6 times higher among patients who received probiotics.
When the researchers factored in the concomitant use of proton pump inhibitors, the incidence of CDI did not differ among patients in the antibiotics-only group, but the concomitant use of probiotics further increased the risk of CDI, "which may suggest a potential interaction between these two drug classes," the researchers wrote in their abstract, which was presented during a poster session.
The investigators stated that they had no relevant financial conflicts to disclose.
AT IDWEEK 2012
Major Finding: The risk of developing Clostridium difficile infection among patients who received probiotics plus high-risk antibiotics was 2.7 times higher than in patients who received antibiotics only, a difference that reached statistical significance.
Data Source: Data are from a single-center study of 389 adult inpatients who received high-risk antibiotics for 5 days or more between July 1 and Dec. 31, 2010.
Disclosures: The researchers stated that they had no relevant financial conflicts to disclose.
Propanolol Guidelines for Infant Hemangiomas Focus on Hospitalization
Inpatient hospitalization is recommended for infants with hemangiomas who are undergoing treatment with propanolol if they are younger than 8 weeks of gestational age, have inadequate social support, or have a comorbid condition affecting the cardiovascular or respiratory system, according to new consensus guidelines on the use of propranolol.
Outpatient initiation with monitoring can be considered for infants older than 8 weeks of age who have adequate social support and who do not have significant comorbidities, noted Dr. Ilona J. Frieden, who presented an overview of the soon-to-be published guidelines at the Women’s and Pediatric Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Dr. Frieden was part of a multispecialty consensus group of experts who met in December 2011 to draft the recommendations on when to admit patients for hospitalization and which patients should be considered for outpatient therapy.
The guidelines also emphasize that all patients who receive propranolol should be monitored with heart rate and blood pressure measurements at baseline and at 1 and 2 hours after receiving the initial dose.
"Clinicians should repeat these measurements with dose increases greater than 0.5 mg/kg per day, including at least one set of measurements after the target dose has been achieved," said Dr. Frieden, professor of dermatology and pediatrics at the University of California, San Francisco. "If heart rate and blood pressure are abnormal, the child should be monitored until the vital signs normalize."
According to Dr. Frieden, the guidelines do not recommend routine glucose testing. "The risk of hypoglycemia is age dependent and begins after 8 hours of fasting in children 0-2 years of age," she said. The guidelines recommend that infants younger than 6 weeks of age be fed every 4 hours, those 6 weeks to 4 months of age every 5 hours, and those older than 4 months every 6-8 hours. They also state that propranolol should be discontinued during intercurrent illness, especially in the setting of restricted oral intake.
"These recommendations are based on current knowledge and should be considered subject to revision," Dr. Frieden said.
The efficacy of propranolol as a treatment for infantile hemangiomas is well documented, but its mechanism of action is not yet fully understood. "We don’t know why it works," she said.
Current hypotheses suggest that propranolol may decrease renin production, inhibit angiogenesis via vascular endothelial growth factor, or induce of apoptosis in microvascular endothelial cells.
A recent systematic review of 41 studies involving 1,264 patients who received beta blockers for infantile hemangiomas found that 28% of patients received prior medical therapy, most commonly oral prednisone. The review, which was reported during a poster session at the 2012 meeting of the Society for Pediatric Dermatology, found that propranolol was initiated at a mean age of 6.6 months with a mean dose of 2.1 mg/kg per day for a mean duration of 6.4 months.
The mean response rate was 98%, with a range between 82% and 100%. "Response measurements varied, but response rates were comparable irrespective of the anatomic site where the hemangioma was located," Dr. Frieden said.
Rebound growth occurred in 17% of cases and the adverse event rate ranged from 3% to 5%, most commonly sleep changes and acrocyanosis. Serious adverse events were rare.
Dr. Frieden disclosed that she has consulted for Pierre Fabre, which is developing propranolol as a treatment for infantile hemangiomas. SDEF and this news organization are owned by Frontline Medical Communications.
Inpatient hospitalization is recommended for infants with hemangiomas who are undergoing treatment with propanolol if they are younger than 8 weeks of gestational age, have inadequate social support, or have a comorbid condition affecting the cardiovascular or respiratory system, according to new consensus guidelines on the use of propranolol.
Outpatient initiation with monitoring can be considered for infants older than 8 weeks of age who have adequate social support and who do not have significant comorbidities, noted Dr. Ilona J. Frieden, who presented an overview of the soon-to-be published guidelines at the Women’s and Pediatric Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Dr. Frieden was part of a multispecialty consensus group of experts who met in December 2011 to draft the recommendations on when to admit patients for hospitalization and which patients should be considered for outpatient therapy.
The guidelines also emphasize that all patients who receive propranolol should be monitored with heart rate and blood pressure measurements at baseline and at 1 and 2 hours after receiving the initial dose.
"Clinicians should repeat these measurements with dose increases greater than 0.5 mg/kg per day, including at least one set of measurements after the target dose has been achieved," said Dr. Frieden, professor of dermatology and pediatrics at the University of California, San Francisco. "If heart rate and blood pressure are abnormal, the child should be monitored until the vital signs normalize."
According to Dr. Frieden, the guidelines do not recommend routine glucose testing. "The risk of hypoglycemia is age dependent and begins after 8 hours of fasting in children 0-2 years of age," she said. The guidelines recommend that infants younger than 6 weeks of age be fed every 4 hours, those 6 weeks to 4 months of age every 5 hours, and those older than 4 months every 6-8 hours. They also state that propranolol should be discontinued during intercurrent illness, especially in the setting of restricted oral intake.
"These recommendations are based on current knowledge and should be considered subject to revision," Dr. Frieden said.
The efficacy of propranolol as a treatment for infantile hemangiomas is well documented, but its mechanism of action is not yet fully understood. "We don’t know why it works," she said.
Current hypotheses suggest that propranolol may decrease renin production, inhibit angiogenesis via vascular endothelial growth factor, or induce of apoptosis in microvascular endothelial cells.
A recent systematic review of 41 studies involving 1,264 patients who received beta blockers for infantile hemangiomas found that 28% of patients received prior medical therapy, most commonly oral prednisone. The review, which was reported during a poster session at the 2012 meeting of the Society for Pediatric Dermatology, found that propranolol was initiated at a mean age of 6.6 months with a mean dose of 2.1 mg/kg per day for a mean duration of 6.4 months.
The mean response rate was 98%, with a range between 82% and 100%. "Response measurements varied, but response rates were comparable irrespective of the anatomic site where the hemangioma was located," Dr. Frieden said.
Rebound growth occurred in 17% of cases and the adverse event rate ranged from 3% to 5%, most commonly sleep changes and acrocyanosis. Serious adverse events were rare.
Dr. Frieden disclosed that she has consulted for Pierre Fabre, which is developing propranolol as a treatment for infantile hemangiomas. SDEF and this news organization are owned by Frontline Medical Communications.
Inpatient hospitalization is recommended for infants with hemangiomas who are undergoing treatment with propanolol if they are younger than 8 weeks of gestational age, have inadequate social support, or have a comorbid condition affecting the cardiovascular or respiratory system, according to new consensus guidelines on the use of propranolol.
Outpatient initiation with monitoring can be considered for infants older than 8 weeks of age who have adequate social support and who do not have significant comorbidities, noted Dr. Ilona J. Frieden, who presented an overview of the soon-to-be published guidelines at the Women’s and Pediatric Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
Dr. Frieden was part of a multispecialty consensus group of experts who met in December 2011 to draft the recommendations on when to admit patients for hospitalization and which patients should be considered for outpatient therapy.
The guidelines also emphasize that all patients who receive propranolol should be monitored with heart rate and blood pressure measurements at baseline and at 1 and 2 hours after receiving the initial dose.
"Clinicians should repeat these measurements with dose increases greater than 0.5 mg/kg per day, including at least one set of measurements after the target dose has been achieved," said Dr. Frieden, professor of dermatology and pediatrics at the University of California, San Francisco. "If heart rate and blood pressure are abnormal, the child should be monitored until the vital signs normalize."
According to Dr. Frieden, the guidelines do not recommend routine glucose testing. "The risk of hypoglycemia is age dependent and begins after 8 hours of fasting in children 0-2 years of age," she said. The guidelines recommend that infants younger than 6 weeks of age be fed every 4 hours, those 6 weeks to 4 months of age every 5 hours, and those older than 4 months every 6-8 hours. They also state that propranolol should be discontinued during intercurrent illness, especially in the setting of restricted oral intake.
"These recommendations are based on current knowledge and should be considered subject to revision," Dr. Frieden said.
The efficacy of propranolol as a treatment for infantile hemangiomas is well documented, but its mechanism of action is not yet fully understood. "We don’t know why it works," she said.
Current hypotheses suggest that propranolol may decrease renin production, inhibit angiogenesis via vascular endothelial growth factor, or induce of apoptosis in microvascular endothelial cells.
A recent systematic review of 41 studies involving 1,264 patients who received beta blockers for infantile hemangiomas found that 28% of patients received prior medical therapy, most commonly oral prednisone. The review, which was reported during a poster session at the 2012 meeting of the Society for Pediatric Dermatology, found that propranolol was initiated at a mean age of 6.6 months with a mean dose of 2.1 mg/kg per day for a mean duration of 6.4 months.
The mean response rate was 98%, with a range between 82% and 100%. "Response measurements varied, but response rates were comparable irrespective of the anatomic site where the hemangioma was located," Dr. Frieden said.
Rebound growth occurred in 17% of cases and the adverse event rate ranged from 3% to 5%, most commonly sleep changes and acrocyanosis. Serious adverse events were rare.
Dr. Frieden disclosed that she has consulted for Pierre Fabre, which is developing propranolol as a treatment for infantile hemangiomas. SDEF and this news organization are owned by Frontline Medical Communications.
EXPERT ANALYSIS FROM THE SDEF WOMEN'S & PEDIATRIC DERMATOLOGY SEMINAR