User login
Management of Colorectal Cancer in Older Adults
Introduction
Colorectal cancer (CRC) is the fourth most common cancer in the United States and has a high prevalence among the older population.1 In 2017, there were an estimated 135,430 new cases of CRC and 50,260 deaths due to CRC. It is the second leading cause of cancer death in the United States, and the death rate for patients with CRC increases with age (Figure).2
Although elderly persons are more frequently diagnosed with CRC, they are underrepresented in clinical trials. This may be due in part to stringent eligibility criteria in prospective randomized controlled trials that exclude older patients with certain comorbidities and decreased functional status. Hutchins and colleagues compared the proportion of persons aged 65 years and older enrolled in Southwest Oncology Group (SWOG) clinical trials and the proportion of persons in this age group in the US population with the same cancer diagnoses.5 They found that while 72% of the US population with CRC were aged ≥ 65 years, persons in this age group comprised only 40% of patients enrolled in SWOG trials. An update on this study performed after Medicare policy changed in 2000 to include coverage of costs incurred due to clinical trials showed an upward trend in the accrual of older patients in SWOG trials, from 25% during the period 1993–1996 to 38% during the period 2001–2003; however, the percentage of older patients with CRC on clinical trials overall remained stable from 1993 to 2003.6
The underrepresentation of older adults with CRC in clinical trials presents oncologists with a challenging task when practicing evidence-based medicine in this patient population. Analysis of a large claims database demonstrated that the use of multi-agent chemotherapy for the treatment of metastatic CRC in older adults increased over time, while the use of single-agent 5-fluorouracil (5-FU) decreased.7 However, the adoption of combination therapy with irinotecan or oxaliplatin in older adults lagged behind the initial adoption of these agents in younger patients. This data demonstrates that as the field of medical oncology evolves, providers are becoming more comfortable treating older patients with multiple medical problems using standard approved regimens.
Geriatric Assessment
Before treating older patients with cancer, it is necessary to define the patient’s physiological age, ideally through a multidisciplinary team evaluation.
The Eastern Cooperative Oncology Group performance status (ECOG PS) and Karnofsky Performance Status (KPS) are crude measures of functional status.12 Generally, elderly patients with good ECOG PS or KPS scores are considered fit enough to receive standard therapy similar to their younger counterparts. Evaluation of functional status using these performance scores is often suboptimal, resulting in patients with a normal or adequate performance status score who may still experience poor outcomes, including decreased survival and inability to tolerate treatment. A study that explored parameters among older patients that predict for increased risk of chemotherapy-related toxicities found that physician-rated KPS score did not accurately predict the risk for adverse events.13 Therefore, a CGA represents a better way to evaluate functional status and other domains.
Functional status can also be evaluated by self-reported tools such as activities of daily living, which refer to basic self-care, and instrumental activities of daily living (IADLs), which are essential for independent living in the community.14,15 Mobility, gait, and balance can also be measured using the “Timed Get Up and Go” test and gait speed. Klepin et al found that faster gait speed was associated with overall survival (OS) in patients with metastatic cancer.16
Cognitive function is an important component of the geriatric assessment in older patients with cancer, as dementia is a prognostic factor for survival in the overall geriatric population. In a retrospective review, patients with dementia were less likely to have a biopsy-proven diagnosis and were twice as likely to have their CRC diagnosed postmortem.17 In addition, establishing that the patient has intact cognitive function prior to initiating treatment is essential to ensure that the patient can comply with treatment and understands when to report adverse effects. Nutritional status is an important portion of the geriatric assessment because malnutrition is associated with increased mortality and decreased tolerance for chemotherapy.18–20 Evaluating the patient’s psychosocial support is crucial as well because older patients are at greater risk of social isolation and depression.21 While the incidence of depression is lower in older adults with cancer than in younger adults with cancer, clinically significant depression is still noted in 3% to 25% of elderly cancer patients.22 Other critical components of the CGA are review of the patient’s comorbidities and medications to avoid complications of polypharmacy.
Both the Cancer and Aging Research Group (CARG) and Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) toxicity tools are valuable tools, as they predict chemotherapy tolerance in elderly patients.13,23 These tools can help guide discussions between oncologists and patients as well as the formulation of an appropriate treatment plan.24 Although toxicity tools can help to determine which patients are at risk for severe toxicity secondary to treatment, these tools do not replace the CGA. A prospective cohort study that evaluated the impact of CGA on tolerance to chemotherapy in older patients with cancer compared patients aged ≥ 70 years at the start of their treatment with chemotherapy (± radiation therapy) using geriatrician-delivered CGA versus standard care given by oncology.8 Patients who received geriatrician-guided CGA interventions tolerated chemotherapy better and completed treatments as planned (odds ratio 4.14 [95% confidence interval {CI} 1.50 to 11.42], P = 0.006) with fewer treatment modifications.
Unfortunately, the CGA is time-consuming to administer and difficult to incorporate into a busy oncology practice. Therefore, other screening models are used to identify patients who may benefit from a full CGA. The International Society of Geriatric Oncology performed a systematic review of screening tools used to identify older cancer patients in need of geriatric assessment and found that the 3 most studied screening tools are the G8, the Vulnerable Elders Survey-13 (VES-13), and the Flemish version of the Triage Risk Screening Tool.25 Another study found that the G8 was more sensitive than the VES-13 (76.5% versus 68.7%, P = 0.0046), whereas the VES-13 was more specific than the G8 (74.3% versus 64.4%, P < 0.0001).26 In addition to providing guidance to initiate a full geriatric assessment, these screening tools may assist in decision making for older cancer patients, especially those with advanced disease.
Surgery
Early-Stage Disease
When possible, surgical resection of colorectal tumors is the primary treatment in both the curative setting and to avoid complications, such as obstruction or perforation.27 Multiple studies have shown that fit elderly patients benefit from curative surgery similarly to their younger counterparts.27–29 With the growing population of persons aged 65 years or older, surgeons are becoming more comfortable with operating on the elderly.4 However, a large systematic review of 28 independent studies with a total of 34,194 patients showed that older patients were less likely to undergo curative surgery.30 Eligibility for surgery should not be determined by age alone, but rather should be based on a full assessment of the patient’s health, including comorbidities, functional status, nutrition, cognition, social support, and psychological status. The impact of age on short-term outcomes after colorectal surgery in terms of 30-day postoperative morbidity and mortality rates was explored in a study that divided patients into 2 groups: those aged ≥ 80 years (mean age 85) and those aged < 80 years (mean age 55.3).31 There were no statistical differences in 30-day postoperative morbidity and mortality rates between the 2 groups, and preexisting comorbidities and urgent nature of surgery were important predictors of colorectal surgery outcomes in the older adults, results that have been seen in several other studies.28,30 When possible, laparoscopic surgery is preferred as it is associated with less intraoperative blood loss, less postoperative pain, reduced postoperative ileus, a shorter hospital stay, and fewer cardiovascular and pulmonary complications.32 The Preoperative Assessment of Cancer in the Elderly (PACE), which combines surgical risk assessment tools with CGA tools, can assist surgeons in determining candidacy for surgery and help decrease unequal access to surgery in the geriatric population.33
Metastasectomy
A large international multicenter cohort study explored the outcomes of patients aged ≥ 70 years who underwent liver resection of colorectal metastases. The study investigatorsfound that neoadjuvant chemotherapy was used less frequently and less extensive surgery was performed in elderly patients than in younger patients.34 Sixty-day postoperative mortality was slightly higher (3.8% versus 1.6%, P < 0.001) and 3-year OS was slightly lower (57.1% versus 60.2%, P < 0.001) in the elderly group as compared to their younger counterparts, but overall the outcomes after liver surgery were similar. Therefore, the management of liver metastases in oligometastatic disease in elderly patients fit for surgery should be the same as that offered to younger patients. Since outcomes are comparable, older patients should be offered neoadjuvant chemotherapy, as several studies have shown similar response rates and OS in younger and older patients.35,36
Rectal Cancer
The standard of care for locally advanced rectal cancer is combined modality treatment with radiation and chemotherapy followed by total mesorectal excision. However, given conflicting data regarding the ability of elderly patients to tolerate neoadjuvant 5-FU-based chemotherapy and radiation, elderly patients are treated with trimodality therapy less often than their younger counterparts.37,38 A systematic review of 22 randomized trials involving 8507 patients with rectal cancer showed that adjuvant radiation therapy could reduce the risk of local recurrence and death from rectal cancer in patients of all ages.39 However, the risk of noncancer-related death was increased in the older population. The Stockholm II trial showed similar benefits of preoperative radiation overall, but this benefit did not extend to patients older than 68 years because of an increased risk of morbidity and mortality.40 In older patients, mortality from noncancer causes within the first 6 months after surgery was higher in the group that received perioperative radiation than in the group that did not receive radiation. Elderly patients (age > 68 years) accounted for most of the mortality, which was predominantly due to cardiovascular disease.
A retrospective study of 36 patients aged ≥ 70 years with rectal cancer evaluated the toxicity and feasibility of neoadjuvant 5-FU combined with pelvic radiation for treating locally advanced rectal cancer. Patients were classified as healthy and “fit” or “vulnerable” based on the presence of comorbidities.41 This study demonstrated that tolerability and response to neoadjuvant chemotherapy and radiation as well as ability to undergo surgery were similar in “vulnerable” patients and “fit” patients. Conversely, Margalit and colleagues studied the rate of treatment deviations in elderly patients with rectal cancer treated with combined modality therapy and found that most patients required early termination of treatment, treatment interruptions, or dose reductions.42 While trimodality treatment is the standard of care in rectal cancer, there is conflicting data from retrospective studies regarding the tolerability and feasibility of this approach. It is important to proceed with caution but to still consider fit older patients with locally advanced rectal cancer for neoadjuvant chemotherapy and radiation followed by surgery.
In patients who have a complete response (CR) to neoadjuvant chemoradiation, watchful waiting rather than proceeding to surgery may be a reasonable strategy, especially in older patients. A systematic review of 867 patients with locally advanced rectal cancer showed no statistically significant difference in OS between patients who were observed with watchful waiting and those who underwent surgery.43 The International Watch and Wait Database includes 679 patients who were managed with a watch-and-wait regimen because they had a clinical CR after chemoradiation. An outcomes analysis of these patients showed that 25% had local regrowth, with 3-year OS of 91% overall and 87% in patients with local regrowth.44 In most patients (84%), regrowth of the tumor occurred within the first 2 years of follow up.
In frail older adults, for whom longer courses of treatment are not feasible or chemotherapy is contraindicated, short-course radiation therapy can be considered either in the neoadjuvant setting or alone for palliation.45 A randomized trial of short-course radiation versus long-course chemoradiation in patients with T3 rectal cancer found that the difference in 3-year local recurrence rates was not statistically significant.46
Chemotherapy
An expected natural decline in function occurs with age, but given the great variability that exists between patients, it is important to focus on physiologic age rather than chronologic age to determine ability to receive and tolerate anticancer treatment. Decreases in renal and hepatic function, cognitive impairment, changes in gastrointestinal motility, decrements in cardiac and bone marrow reserves, as well as comorbidities and polypharmacy affect a patient’s ability to tolerate chemotherapy.47,48 Toxicity tools such as CARG and CRASH can help to predict severity of toxicity with chemotherapy.13,23 The information provided by these tools can help guide conversations between the oncologist and patient regarding treatment plans.
Adjuvant Chemotherapy for Early-Stage Disease
Stage II Disease
Defining treatment guidelines for older patients with stage II colon cancer is difficult due to lack of data that shows benefit in this population. The QUASAR (Quick and Simple and Reliable) group’s prospective study of adjuvant single-agent 5-FU in stage II colon cancer patients showed an absolute improvement in survival of 3.6% when 5-FU was given after surgery (95% CI 1.0 to 6.0).49 The subgroup analysis of patients aged ≥ 70 years showed a limited benefit of adjuvant 5-FU (hazard ratio [HR] 1.13 [95% CI 0.74 to 1.75]). Given the limited benefit, adjuvant 5-FU for elderly patients with stage II colon cancer should be used judiciously as patients may have competing causes of morbidity or mortality.
The use of oxaliplatin-based therapy in the adjuvant setting for stage II disease was evaluated in a subgroup analysis of the MOSAIC study (Multicenter International Study of Oxaliplatin/5-FU/Leucovorin in the Adjuvant Treatment of Colon Cancer).50 Adjuvant oxaliplatin-based treatment may be offered to patients with stage II colon cancer that carries high-risk features (poorly differentiated histology, lymphovascular invasion, bowel obstruction and/or perforation, < 12 lymph nodes sampled, perineural invasion, or indeterminate or positive margins) due to a trend toward improved disease-free survival (DFS) at 5 years. Patients in this group who received adjuvant FOLFOX (leucovorin, oxaliplatin, 5-FU) versus 5-FU/leucovorin had a DFS of 82.3% versus 74.6%, respectively (HR 0.72 [95% CI 0.50 to 1.02]), a difference that was not statistically significant. A subgroup analysis of 315 patients aged 70 to 75 years with stage II colon cancer enrolled in the MOSAIC study found no statistically significant DFS or OS benefit with the addition of oxaliplatin to 5-FU/leucovorin.51 Therefore, use of this platinum/fluoropyrimidine combination for adjuvant therapy for high-risk stage II disease in older patients remains controversial given its associated risks and the lack of definitive data demonstrating a benefit in this patient group. Decisions regarding this therapy should be made through a shared discussion with patients about its risks and benefits.
Microsatellite status is an important biomarker in the evaluation of stage II CRC. Microsatellite stability is a marker of a functioning DNA mismatch repair system. In patients with colon cancer, tumor microsatellite stability is classified based on the percentage of abnormal microsatellite regions.52 Several studies have shown that patients with tumors that display high microsatellite instability (MSI-H) have an improved prognosis over patients with microsatellite stable tumors.53,54 While patients with stage II MSI-H colon cancer have better outcomes, MSI is associated with a reduced response to treatment with fluoropyrimidines, as demonstrated in a systematic review that found that patients with tumors with MSI obtained no benefit from adjuvant 5-FU (HR 1.24 [95% CI 0.72 to 2.14]).55 Aparicio and colleagues reported an increased prevalence of MSI-H tumors with increasing age.56 Therefore, mismatch repair phenotype should be considered when making adjuvant chemotherapy decisions in the older adult with colon cancer, as it may affect the decision to recommend single-agent 5-FU treatment.
Stage III Disease
The use of single-agent 5-FU for stage III resected CRC has been evaluated in multiple studies. Sargent et al performed a pooled analysis of 3351 patients from 7 randomized phase 3 trials comparing surgery and adjuvant 5-FU-based chemotherapy versus surgery alone in stage II or III colon cancer patients.57 Adjuvant chemotherapy was associated with improvement in both OS and time to tumor recurrence (HR 0.76 and 0.68, respectively). The 5-year OS was 71% for those who received adjuvant treatment and 64% for those who were treated with surgery alone. The benefit of adjuvant treatment was independent of age, and there was no difference in toxicity across age groups, except for 1 study which showed increased rates of leukopenia in the elderly. The oral fluoropyrimidine capecitabine was shown to be an effective alternative to 5-FU plus leucovorin as adjuvant treatment for those with resected stage III colon cancer.58 However, in the subgroup analysis of DFS in the intention-to-treat group, the improvement in DFS was not statistically significant in those aged ≥ 70 years. This study justified the phase 3 Xeloda in Adjuvant Colon Cancer Therapy (X-ACT) trial, which compared capecitabine and 5-FU/leucovorin as adjuvant therapy in patients with resected stage III colon cancer.59 The X-ACT trial showed no significant effect of age on DFS or OS.
The addition of oxaliplatin to 5-FU in the adjuvant setting for stage III tumors has been studied and debated in the elderly population in multiple trials. The MOSAIC trial investigated FOLFOX versus 5-FU/leucovorin in the adjuvant setting.50 The addition of oxaliplatin was associated with a DFS and OS benefit, with a 20% reduction in risk of colon cancer recurrence and 16% reduction in risk of death in all patients. The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-07 trial then studied 2409 patients with stage II or III colon cancer treated with weekly bolus 5-FU/leucovorin with or without oxaliplatin.60 In this study, OS was significantly improved with the addition of oxaliplatin in patients younger than 70 years, but OS at 5 years was 4.7% worse for patients aged ≥ 70 years treated with weekly 5-FU/leucovorin and oxaliplatin compared with those treated with weekly 5-FU/leucovorin (71.6% versus 76.3%, respectively). In contrast, the XELOXA trial (NO16968), which randomly assigned stage III colon cancer patients to capecitabine and oxaliplatin (XELOX) or bolus 5-FU/leucovorin (standard of care at study start), showed an efficacy benefit, albeit not statistically significant, in patients aged ≥ 70 years (HR 0.87 [95% CI 0.63 to 1.18]).61–63
The Adjuvant Colon Cancer Endpoints (ACCENT) database included 7 randomized trials totaling 14,528 patients with stage II or III colon cancer treated with adjuvant 5-FU with or without oxaliplatin or irinotecan.64 Subgroup analysis of patients aged ≥ 70 years (n = 2575) showed no benefit with an oxaliplatin-based regimen in DFS (HR 0.94 [95% CI 0.78 to 1.13]) or OS (HR 1.04 [95% CI, 0.85 to 1.27]). Based on these studies and the increased toxicity with oxaliplatin, oxaliplatin-based adjuvant chemotherapy is utilized less often than single-agent 5-FU in geriatric patients with early-stage colon cancer.65 Conversely, a recent pooled analysis of individual patient data from 4 randomized trials (NSABP C-08, XELOXA, X-ACT, and AVANT) showed improved DFS and OS with adjuvant XELOX or FOLFOX over single-agent 5-FU in patients aged ≥ 70 years (DFS HR 0.77 [95% CI 0.62 to 0.95], P = 0.014; OS HR 0.78 [95% CI 0.61 to 0.99], P = 0.045).66 This analysis also showed that grade 3 and 4 adverse events related to oxaliplatin were similar across age groups.
These data come from post-hoc analyses, and there is no prospective data to steer decision making in elderly patients with early-stage CRC (Table).
It is well established that patients with stage III colon cancer benefit from oxaliplatin-based adjuvant chemotherapy after curative surgical resection.68 However, older patients are less likely to be referred to oncology as compared with their younger counterparts, due to the conflicting data regarding the benefit of this approach in older adults. Studies have shown that when the referral is placed, the geriatric population is less likely to receive chemotherapy.69 Sanoff et al analyzed 4 data sets (SEER-Medicare, National Comprehensive Cancer Network, New York State Cancer Registry, and Cancer Care Outcomes Research and Surveillance Consortium) to assess the benefit of adjuvant chemotherapy for resected stage III CRC among patients aged ≥ 75 years. Their analysis showed that only 40% of patients evaluated received adjuvant chemotherapy for stage III CRC after surgical resection.70
Summary
Prospective data to guide the treatment of older patients with early-stage CRC in the adjuvant setting is lacking. For fit older patients with stage II disease, limited benefit will be derived from single-agent 5-FU. For those with stage III CRC, the benefit and toxicities of fluoropyrimidines as adjuvant therapy appear to be similar regardless of age. The addition of oxaliplatin to fluoropyrimidines in patients aged ≥ 70 years has not been proven to improve DFS or OS and could result in an incremental toxicity profile. Therefore, treatment plans must be individualized, and decisions should be made through an informed discussion evaluating the overall risk/benefit ratio of each approach.
Metastatic Disease
Palliative Chemotherapy
Approximately 20% of patients with CRC are diagnosed with metastatic disease at presentation, and 35% to 40% develop metastatic disease following surgery and adjuvant therapy.2 The mainstay of treatment in this population is systemic therapy in the form of chemotherapy with or without biologic agents. In this setting, several prospective studies specific to older adults have been completed, providing more evidence-based guidance to oncologists who see these patients. Folprecht et al retrospectively reviewed data from 22 clinical trials evaluating 5-FU-based palliative chemotherapy in 3825 patients with metastatic CRC, including 629 patients aged ≥ 70 years.71 OS in elderly patients (10.8 months [95% CI 9.7 to 11.8]) was equivalent to that in younger patients (11.3 months [95% CI 10.9 to 11.7], P = 0.31). Similarly, relative risk and progression-free survival (PFS) were comparable irrespective of age.
Standard of care for most patients with metastatic colon cancer consists of 5-FU/leucovorin in combination with either oxaliplatin (FOLFOX) or irinotecan (FOLFIRI) with a monoclonal antibody.72 A retrospective pooled analysis of patients with metastatic CRC compared the safety and efficacy of FOLFOX4 in patients aged < 70 years versus those aged ≥ 70 years.73 While age ≥ 70 years was associated with an increased rate of grade ≥ 3 hematologic toxicity, it was not associated with increased rates of severe neurologic events, diarrhea, nausea, vomiting, infection, 60-day mortality, or overall incidence of grade ≥ 3 toxicity. The benefit of treatment was consistent across both age groups; therefore, age alone should not exclude an otherwise healthy individual from receiving FOLFOX.
These post-hoc analyses show that fit older patients who were candidates for trial participation tolerated these treatments well; however, these treatments may be more challenging for less fit older adults. The UK Medical Research Council FOCUS2 (Fluorouracil, Oxaliplatin, CPT11 [irinotecan]: Use and Sequencing) study was a prospective phase 3 trial that included 459 patients with metastatic CRC who were deemed too frail or not fit enough for standard-dose chemotherapy by their oncologists.74 In this group, 43% of patients were older than 75 years and 13% were older than 80 years. Patients were randomly assigned to receive infusional 5-FU with levofolinate; oxaliplatin and 5-FU; capecitabine; or oxaliplatin and capecitabine; all regimens were initiated with an empiric 20% dose reduction. The addition of oxaliplatin suggested some improvement in PFS, but this was not significant (5.8 months versus 4.5 months, HR 0.84 [95% CI 0.69 to 1.01], P = 0.07). Oxaliplatin was not associated with increased grade 3 or 4 toxicities. Capecitabine is often viewed as less toxic because it is taken by mouth, but this study found that replacement of 5-FU with capecitabine did not improve quality of life. Grade 3 or 4 toxicities were seen more frequently in those receiving capecitabine than in those receiving 5-FU (40% versus 30%, P = 0.03) in this older and frailer group of patients. As the patients on this study were frail and treatment dose was reduced, this data may not apply to fit older adults who are candidates for standard therapy.
When managing an older patient with metastatic CRC, it is important to tailor therapy based on goals of care, toxicity of proposed treatment, other comorbidities, and the patient’s functional status. One approach to minimizing toxicity in the older population is the stop-and-go strategy. The OPTIMOX1 study showed that stopping oxaliplatin after 6 cycles of FOLFOX7 and continuing maintenance therapy with infusional 5-FU/leucovorin alone for 12 cycles prior to reintroducing FOLFOX7 achieved efficacy similar to continuous FOLFOX4 with decreased toxicity.75 Figer et al studied an exploratory cohort of 37 patients aged 76 to 80 years who were included in the OPTIMOX1 study.76 The overall relative risk, median PFS, and median OS did not differ between the older patients in this cohort and younger patients studied in the original study. Older patients did experience more neutropenia, neurotoxicity, and overall grade 3 to 4 toxicity, but there were no toxic deaths in patients older than 75 years. The approach of giving treatment breaks, as in OPTIMOX2, may also provide patients with better quality of life, but perhaps at the expense of cancer-related survival.77
The combination of irinotecan and 5-FU has also been studied as treatment for patients with metastatic CRC. A pooled analysis of 2691 patients aged ≥ 70 years with metastatic CRC across 4 phase 3 randomized trials investigating irinotecan and 5-FU demonstrated that irinotecan-containing chemotherapy provided similar benefits to both older and younger patients with similar risk of toxicity.78 A phase 2 trial studying FOLFIRI as first-line treatment in older metastatic CRC patients showed this to be a safe and active regimen with manageable toxicity.79 Another randomized phase 3 trial for older patients compared 5-FU/leucovorin with or without irinotecan for first-line treatment of metastatic CRC (FFCD 2001-02).80 The study accrued 282 patients aged ≥ 75 years (median age 80 years), and found that the addition of irinotecan to infusional 5-FU–based chemotherapy did not significantly increase either PFS or OS. Aparicio et al performed a substudy of baseline geriatric evaluation prior to treatment in the FFCD 2001-02 study and assessed the value of geriatric parameters for predicting outcomes (objective response rate [ORR], PFS, and OS).81 Multivariate analysis showed that none of the geriatric parameters were predictive of ORR or PFS but that normal IADL was associated with better OS. This combination may still be appropriate for some older patients with metastatic disease, while single- agent 5-FU may be more appropriate in frail patients.
Biologic Agents
VEGF Inhibitors
Targeted biologic agents have been studied in the treatment of metastatic CRC. Bevacizumab is a recombinant, humanized monoclonal antibody against vascular endothelial growth factor (VEGF) that is approved in the first-line setting for treatment of metastatic CRC. A pooled analysis examined 439 patients 65 years of age and older with metastatic CRC who received bevacizumab plus chemotherapy versus placebo plus chemotherapy.82 In this analysis, the addition of bevacizumab was associated with an improvement in OS (19.3 months versus 14.3 months, HR 0.7 [95% CI 0.55 to 0.90], P = 0.006) and in PFS (9.2 months versus 6.2 months, HR 0.52 [95% CI 0.40 to 0.67], P < 0.0001). Known adverse events associated with bevacizumab were seen in the bevacizumab plus chemotherapy group but not at increased rates in the older population compared to their younger counterparts. Conversely, another pooled analysis found that while there was a PFS and OS benefit in older patients receiving bevacizumab, there was an increased incidence of thrombotic events in patients older than 65 years.83 The BEAT (Bevacizumab Expanded Access Trial) and BRiTE (Bevacizumab Regimens Investigation of Treatment Effects) studies showed similar clinical outcomes across all age groups.84,85 While older patients experienced more arterial thromboembolic events with the addition of bevacizumab, other factors such as ECOG PS, prior anticoagulation, and history of arterial disease were more predictive of these adverse events than age.
The randomized phase 3 AVEX study explored the efficacy and tolerability of capecitabine plus bevacizumab versus capecitabine alone in 280 frail patients aged ≥ 70 years.86 PFS in the capecitabine/bevacizumab arm was 9.1 months versus 5.1 months in the capecitabine alone arm. While the OS difference was not statistically significant, patients in the capecitabine/bevacizumab arm had an OS of 20.7 months versus 16.8 months in the capecitabine alone group. As reported in prior studies, patients in the capecitabine/bevacizumab arm had increased rates of toxic events (40%) compared with those who received capecitabine alone (22%), with reports of hypertension, hand-foot syndrome, bleeding, and thrombotic events. More recently, the phase 2 PRODIGE 20 trial studied the addition of bevacizumab to chemotherapy (5-FU, FOLFOX, or FOLFIRI) based on physician choice in untreated metastatic CRC patients aged ≥ 75 years (median age 80 years).87 They found that the addition of bevacizumab to standard of care chemotherapy was both safe and effective. The adverse events seen with bevacizumab, such as hypertension and thrombotic events, were consistent with prior studies.
A newer antiangiogenic agent, ziv-aflibercept, has been approved for the second-line treatment of metastatic CRC. The VELOUR trial demonstrated that the addition of ziv-aflibercept to FOLFIRI benefited patients across all age groups compared with FOLFIRI plus placebo in patients who had failed prior oxaliplatin-based chemotherapy.88,89 Ramucirumab is a human IgG-1 monoclonal antibody approved in second-line treatment in combination with FOLFIRI. A subgroup analysis of the RAISE study showed that the survival benefit was similar in patients aged ≥ 65 years versus those < 65 years.90 Based on the above data, the use of a VEGF inhibitor in combination with chemotherapy should be considered in older patients with metastatic CRC. Furthermore, based on the conflicting data regarding the benefit of FOLFOX/FOLFIRI over single-agent 5-FU discussed above, the combination of capecitabine plus bevacizumab may be considered a front-line treatment option in older patients based on the AVEX study.
EGFR Inhibitors
Cetuximab and panitumumab are anti-epidermal growth factor receptor (EGFR) antibodies approved for the treatment of RAS wild-type metastatic CRC. Data regarding the use of EGFR inhibitors in the geriatric population is scarce and the data that does exist is conflicting.91,92 The PRIME study demonstrated that panitumumab plus FOLFOX had a PFS benefit compared to FOLFOX alone in KRAS wild-type metastatic CRC patients.92 While the study met its primary endpoint, the benefit did not translate to patients aged ≥ 65 years in subgroup analysis. Conversely, a retrospective study of the efficacy and safety of cetuximab in elderly patients with heavily pretreated metastatic CRC found similar efficacy in older and younger patients as well as no increased adverse events in the older population.91 A phase 2 trial investigating cetuximab as single-agent first-line treatment of metastatic CRC in fit older patients found cetuximab to be safe with moderate activity in this population, but did not support the use of cetuximab as first-line single-agent treatment in fit geriatric patients who may be candidates for combination therapy.93 Our group studied the patterns of use and tolerance of anti-EGFR antibodies in 117 older adults with metastatic CRC with a median age of 73 years.94 The study showed that older age at the time of treatment was associated with administration of anti-EGFR antibody as monotherapy rather than in combination with chemotherapy (P = 0.0009). We found no association between age and presence of grade 3 or higher toxicity. In addition, the toxicity profile seen in older patients was similar to what has been demonstrated in prior studies involving a younger patient population. Given the discordance seen between studies, additional prospective trials are needed to elucidate the efficacy and safety of EGFR inhibitors in the geriatric population.
Other Agents
Two newer agents approved in the treatment of metastatic CRC are regorafenib, a multikinase inhibitor, and trifluridine/tipiracil (TFD/TPI), a nucleoside analog combined with an inhibitor of thymidine phosphorylase. The phase 3 CORRECT trial studied regorafenib as monotherapy in previously treated metastatic CRC and found an OS benefit of 1.4 months and minimal PFS benefit.95 Van Cutsem et al performed a subgroup analysis by age and found similar OS benefit in patients < 65 years of age and ≥ 65 years.96 The most frequent adverse events grade 3 or higher were hand-foot syndrome, fatigue, diarrhea, hypertension, and desquamation/rash, which were seen at similar rates in both age groups. More recently, the phase 2 Regorafenib Dose Optimization Study (ReDOS) found that weekly dose escalation of regorafenib from 80 mg to 160 mg daily over 3 weeks was superior to the standard 160 mg daily dosing in patients with metastatic CRC.97 The dose escalation group had a longer median OS, although this difference was not statistically significant, as well as a more favorable toxicity profile. Therefore, this new dosing strategy may be a reasonable option for older patients with pretreated metastatic CRC. A study of TFD/TPI versus placebo in refractory metastatic CRC found an OS benefit of 7.1 months versus 5.3 months.98 In subgroup analyses, the OS benefit extended to both patients < 65 years and ≥ 65 years. Given the sparse data on these newer agents in the geriatric population and the modest benefit they provide to those with refractory metastatic CRC, more data is needed to determine their utility in elderly patients. The decision to use these agents in the older patients warrants a thorough discussion with the patient regarding risks, benefit, and treatment goals.
Immunotherapy
Between 3.5% and 6.5% of stage IV colorectal cancers are MSI-H and have deficient mismatch repair (dMMR).99–101 A recent phase 2 trial studied the use of pembrolizumab, an IgG4 monoclonal antibody against PD-1 (programmed cell death-1), in heavily pretreated patients with dMMR metastatic CRC, MMR-proficient (pMMR) metastatic CRC, and noncolorectal dMMR metastatic cancer.102 Patients with dMMR metastatic CRC had a 50% ORR and 89% disease control rate (DCR), as compared with an ORR of 0% and DCR of 16% in patients with pMMR metastatic CRC. There was also an OS and PFS benefit seen in the dMMR CRC group as compared with the pMMR CRC group. Another phase 2 study, CheckMate 142, studied the anti-PD-1 monoclonal antibody nivolumab with or without ipilimumab (a monoclonal antibody against cytotoxic T-lymphocyte antigen 4) in patients with dMMR and pMMR metastatic CRC.103 In the interim analysis, nivolumab was found to provide both disease control and durable response in patients with dMMR metastatic CRC.
While these studies led to the FDA approval of pembrolizumab and nivolumab for management of previously treated MSI-H or dMMR metastatic CRC, data on the use of immunotherapy in older adults is scarce. Immunosenescence, or the gradual deterioration of the immune system that comes with aging, may impact the efficacy of immune checkpoint inhibitors (ICI) in older patients with advanced cancer.104 There is conflicting data on the efficacy of PD-1 and programmed death ligand-1) PD-L1 inhibitors in older patients across different cancers. A meta-analysis of immunotherapy in older adults with a variety of malignancies showed overall efficacy comparable to that seen in adults younger than 65 years.105 However, another review found ICIs to be less effective in older patients with head and neck, non-small cell lung cancer, and renal cell carcinoma compared with their younger counterparts.104 Regarding the toxicity profile of ICIs in the elderly, similar rates of grade 3 or higher adverse events in patients younger than 65 years and older than 65 years have been reported.106 However, patients aged ≥ 70 years had increased rates of grade 3 to 5 adverse events as compared to patients younger than 65 years (71.7% versus 58.4%, respectively). Given the scant data on ICIs in older patients with MSI-H or dMMR metastatic CRC, more clinical trials inclusive of this population are needed in order to determine the efficacy and safety of immunotherapy.
Palliative Care
The incorporation of palliative care early following the diagnosis of cancer has been shown to improve quality of life, decrease depression, and help with symptom management.107 The triggers for geriatric patients to initiate palliative care may be different from those of younger patients, as older patients may have different goals of care.108 Older patients will often choose quality over quantity of life when making treatment decisions.109 The ideal medical treatment for the frail patient with colorectal cancer would focus on treating disease while providing palliative measures to help support the patient and improve quality of life. It is paramount that patients maintain functional independence as loss of independence is recognized as a major threat to an older patient’s quality of life.110 The optimal way to achieve these goals is through the efforts of a multidisciplinary care team including not only physicians and nurses, but also social workers, nutritionists, physical therapists, and family who can provide support for the patient’s psychosocial, cognitive, and medical needs.111 Although cancer and noncancer–related death occur more frequently in the geriatric population, data to guide a specific palliative care approach to the elderly population is lacking.108
Conclusion
Colorectal cancer is a disease of older adults with a median age at diagnosis of 67 years.1 With the aging population, oncologists will be faced with treating increasing numbers of older patients, and must adjust their practice to accommodate this population of patients. Treating geriatric patients is challenging given the lack of available data to guide the treatment approach. Although several prospective elderly-specific studies have been conducted evaluating treatments for metastatic CRC, most treatment decisions are made based on the available retrospective studies and pooled analyses. Oncologists must carefully consider and evaluate each patient based on physiologic age rather than chronologic age.112 Overall, older patients should be given the opportunity to receive standard of care treatments in the appropriate setting. The decision to modify treatment plans should be made after a thorough evaluation by a multidisciplinary team and a discussion with the patient regarding their goals and the risks and benefits of the treatment. Geriatric assessment tools can help the care team identify patients with various geriatric syndromes that may not be detected on routine oncology evaluation. This type of evaluation is time consuming and is rarely done in a busy oncology practice. Ongoing studies are aiming to develop a method to incorporate geriatric assessments into the care of older adults.Additional prospective trials targeting older, more frail patients are essential to improve upon our knowledge so we can provide best care for this growing elderly population.
1. National Cancer Institute. SEER cancer stat facts: colorectal cancer. http://seer.cancer.gov/statfacts/html/colorect.html. Accessed March 1, 2018.
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:7–30.
3. Kochanek KD, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief 2017:1-8.
4. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States, current population reports, P25-1140. Washington, DC: U.S. Census Bureau; 2014.
5. Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med 1999;341:2061–7.
6. Unger JM, Coltman CA Jr, Crowley JJ, et al. Impact of the year 2000 Medicare policy change on older patient enrollment to cancer clinical trials. J Clin Oncol 2006;24:141–4.
7. Vijayvergia N, Li T, Wong YN, et al. Chemotherapy use and adoption of new agents is affected by age and comorbidities in patients with metastatic colorectal cancer. Cancer 2016;122:3191–8.
8. Kalsi T, Babic-Illman G, Ross PJ, et al. The impact of comprehensive geriatric assessment interventions on tolerance to chemotherapy in older people. Br J Cancer 2015;112:1435–44.
9. National Comprehensive Cancer Network. Older adult oncology (Version 2.2017). Accessed March 1, 2018,
10. Balducci L. Frailty: a common pathway in aging and cancer. Interdiscip Top Gerontol 2013;38:61–72.
11. Baijal P, Periyakoil V. Understanding frailty in cancer patients. Cancer J 2014;20:358–66.
12. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–55.
13. Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 2011;29:3457–65.
14. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86.
15. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist 1970;10:20–30.
16. Klepin HD, Geiger AM, Tooze JA, et al. Physical performance and subsequent disability and survival in older adults with malignancy: results from the health, aging and body composition study. J Am Geriatr Soc 2010;58:76–82.
17. Gupta SK, Lamont EB. Patterns of presentation, diagnosis, and treatment in older patients with colon cancer and comorbid dementia. J Am Geriatr Soc 2004;52:1681–7.
18. Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 1980;69:491–7.
19. Aaldriks AA, van der Geest LG, Giltay EJ, et al. Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 2013;4:218–26.
20. Martucci RB, Barbosa MV, D’Almeida CA, et al. Undernutrition as independent predictor of early mortality in elderly cancer patients. Nutrition 2017;34:65–70.
21. Naeim A, Aapro M, Subbarao R, Balducci L. Supportive care considerations for older adults with cancer. J Clin Oncol 2014;32:2627–34.
22. Kua J. The prevalence of psychological and psychiatric sequelae of cancer in the elderly - how much do we know? Ann Acad Med Singapore 2005;34:250–6.
23. Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012;118:3377–86.
24. Kim J, Hurria A. Determining chemotherapy tolerance in older patients with cancer. J Natl Compr Canc Netw 2013;11:1494-502.
25. Decoster L, Van Puyvelde K, Mohile S, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations. Ann Oncol 2015;26:288–300.
26. Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PLoS One 2014; 9:e115060.
27. Gurevitch AJ, Davidovitch B, Kashtan H. Outcome of right colectomy for cancer in octogenarians. J Gastrointest Surg 2009;13:100–4.
28. Schiffmann L, Ozcan S, Schwarz F, et al. Colorectal cancer in the elderly: surgical treatment and long-term survival. Int J Colorectal Dis 2008;23:601–10.
29. Ong ES, Alassas M, Dunn KB, Rajput A. Colorectal cancer surgery in the elderly: acceptable morbidity? Am J Surg 2008;195:344–8.
30. Surgery for colorectal cancer in elderly patients: a systematic review. Colorectal Cancer Collaborative Group. Lancet 2000;356:968–74.
31. Shalaby M, Di Lorenzo N, Franceschilli L, et al. Outcome of colorectal surgery in elderly populations. Ann Coloproctol 2016;32:139–43.
32. Frasson M, Braga M, Vignali A, et al. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 2008;51:296–300.
33. PACE participants, Audisio RA, Pope D, et al. Shall we operate? Preoperative assessment in elderly cancer patients (PACE) can help. A SIOG surgical task force prospective study. Crit Rev Oncol Hematol 2008;65:156–63.
34. Adam R, Frilling A, Elias D, et al. Liver resection of colorectal metastases in elderly patients. Br J Surg 2010;97:366–76.
35. de Liguori Carino N, van Leeuwen BL, Ghaneh P, et al. Liver resection for colorectal liver metastases in older patients. Crit Rev Oncol Hematol 2008;67:273–8.
36. Tamandl D, Gruenberger B, Herberger B, et al. Surgery after neoadjuvant chemotherapy for colorectal liver metastases is safe and feasible in elderly patients. J Surg Oncol 2009;100:364–71.
37. Shahir MA, Lemmens VE, van de Poll-Franse LV, et al. Elderly patients with rectal cancer have a higher risk of treatment-related complications and a poorer prognosis than younger patients: a population-based study. Eur J Cancer 2006;42:3015–21.
38. Chang GJ, Skibber JM, Feig BW, Rodriguez-Bigas M. Are we undertreating rectal cancer in the elderly? An epidemiologic study. Ann Surg 2007;246:215–21.
39. Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 2001;358:1291–304.
40. Martling A, Holm T, Johansson H, et al, Stockholm Colorectal Cancer Study Group. The Stockholm II trial on preoperative radiotherapy in rectal carcinoma: long-term follow-up of a population-based study. Cancer 2001;92:896–902.
41. Pasetto LM, Friso ML, Pucciarelli S, et al. Rectal cancer neoadjuvant treatment in elderly patients. Anticancer Res 2006;26:3913–23.
42. Margalit DN, Mamon HJ, Ancukiewicz M, et al. Tolerability of combined modality therapy for rectal cancer in elderly patients aged 75 years and older. Int J Radiat Oncol Biol Phys 2011;81:e735–41.
43. Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2017;2:501–13.
44. van der Valk M. The International Watch & Wait database (IWWD) for rectal cancer: An update. J Clin Oncol 2017;35 suppl:521.
45. Donato V, Valeriani M, Zurlo A. Short course radiation therapy for elderly cancer patients. Evidences from the literature review. Crit Rev Oncol Hematol 2003;45:305–11.
46. Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 2012;30:3827–33.
47. McCleary NJ, Dotan E, Browner I. Refining the chemotherapy approach for older patients with colon cancer. J Clin Oncol 2014;32:2570–80.
48. Millan M, Merino S, Caro A, et al. Treatment of colorectal cancer in the elderly. World J Gastrointest Oncol 2015;7:204–20.
49. Quasar Collaborative Group, Gray R, Barnwell J, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370:2020–9.
50. Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009;27:3109–16.
51. Tournigand C, Andre T, Bonnetain F, et al. Adjuvant therapy with fluorouracil and oxaliplatin in stage II and elderly patients (between ages 70 and 75 years) with colon cancer: subgroup analyses of the Multicenter International Study of Oxaliplatin, Fluorouracil, and Leucovorin in the Adjuvant Treatment of Colon Cancer trial. J Clin Oncol 2012;30:3353–60.
52. Winder T, Lenz HJ. Molecular predictive and prognostic markers in colon cancer. Cancer Treat Rev 2010;36:550–6.
53. Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
54. Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
55. Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
56. Aparicio T, Schischmanoff O, Poupardin C, et al. Deficient mismatch repair phenotype is a prognostic factor for colorectal cancer in elderly patients. Dig Liver Dis 2013;45:245–50.
57. Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients. N Engl J Med 2001;345:1091–7.
58. Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
59. Twelves C, Scheithauer W, McKendrick J, et al. Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol 2012;23:1190–7.
60. Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 2011;29:3768–74.
61. Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
62. Haller DG, Cassidy J, Tabernero J, et al. Efficacy findings from a randomized phase III trial of capecitabine plus oxaliplatin versus bolus 5-FU/LV for stage III colon cancer (NO16968): impact of age on disease-free survival (DFS) [abstract]. J Clin Oncol 2010;28:3521.
63. Schmoll HJ, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
64. McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
65. Kahn KL, Adams JL, Weeks JC, et al. Adjuvant chemotherapy use and adverse events among older patients with stage III colon cancer. JAMA 2010;303:1037–45.
66. Haller DG, O’Connell MJ, Cartwright TH, et al. Impact of age and medical comorbidity on adjuvant treatment outcomes for stage III colon cancer: a pooled analysis of individual patient data from four randomized, controlled trials. Ann Oncol 2015;26:715-24.
67. Aparicio T, Francois E, Cristol-Dalstein L, et al. PRODIGE 34-FFCD 1402-ADAGE: Adjuvant chemotherapy in elderly patients with resected stage III colon cancer: A randomized phase 3 trial. Dig Liver Dis 2016;48:206–7.
68. Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
69. Mahoney T, Kuo YH, Topilow A, Davis JM. Stage III colon cancers: why adjuvant chemotherapy is not offered to elderly patients. Arch Surg 2000;135:182–5.
70. Sanoff HK, Carpenter WR, Sturmer T, et al. Effect of adjuvant chemotherapy on survival of patients with stage III colon cancer diagnosed after age 75 years. J Clin Oncol 2012;30:2624–34.
71. Folprecht G, Cunningham D, Ross P, et al. Efficacy of 5-fluorouracil-based chemotherapy in elderly patients with metastatic colorectal cancer: a pooled analysis of clinical trials. Ann Oncol 2004;15:1330–8.
72. Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, ESMO Guidelines Working Group. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25 Suppl 3:iii1–9.
73. Goldberg RM, Tabah-Fisch I, Bleiberg H, et al. Pooled analysis of safety and efficacy of oxaliplatin plus fluorouracil/leucovorin administered bimonthly in elderly patients with colorectal cancer. J Clin Oncol 2006;24:4085–91.
74. Seymour MT, Thompson LC, Wasan HS, et al. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): an open-label, randomised factorial trial. Lancet 2011;377:1749–59.
75. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer--a GERCOR study. J Clin Oncol 2006;24:394–400.
76. Figer A, Perez-Staub N, Carola E, et al. FOLFOX in patients aged between 76 and 80 years with metastatic colorectal cancer: an exploratory cohort of the OPTIMOX1 study. Cancer 2007;110:2666–71.
77. Chibaudel B, Maindrault-Goebel F, Lledo G, et al. Can chemotherapy be discontinued in unresectable metastatic colorectal cancer? The GERCOR OPTIMOX2 Study. J Clin Oncol 2009;27:5727–33.
78. Folprecht G, Seymour MT, Saltz L, et al. Irinotecan/fluorouracil combination in first-line therapy of older and younger patients with metastatic colorectal cancer: combined analysis of 2,691 patients in randomized controlled trials. J Clin Oncol 2008;26:1443–51.
79. Souglakos J, Pallis A, Kakolyris S, et al. Combination of irinotecan (CPT-11) plus 5-fluorouracil and leucovorin (FOLFIRI regimen) as first line treatment for elderly patients with metastatic colorectal cancer: a phase II trial. Oncology 2005;69:384–90.
80. Aparicio T, Lavau-Denes S, Phelip JM, et al. Randomized phase III trial in elderly patients comparing LV5FU2 with or without irinotecan for first-line treatment of metastatic colorectal cancer (FFCD 2001-02). Ann Oncol 2016;27:121–7.
81. Aparicio T, Gargot D, Teillet L, et al. Geriatric factors analyses from FFCD 2001-02 phase III study of first-line chemotherapy for elderly metastatic colorectal cancer patients. Eur J Cancer 2017;74:98–108.
82. Kabbinavar FF, Hurwitz HI, Yi J, et al. Addition of bevacizumab to fluorouracil-based first-line treatment of metastatic colorectal cancer: pooled analysis of cohorts of older patients from two randomized clinical trials. J Clin Oncol 2009;27:199–205.
83. Cassidy J, Saltz LB, Giantonio BJ, et al. Effect of bevacizumab in older patients with metastatic colorectal cancer: pooled analysis of four randomized studies. J Cancer Res Clin Oncol 2010;136:737–43.
84. Van Cutsem E, Rivera F, Berry S, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol 2009;20:1842–7.
85. Kozloff MF, Berlin J, Flynn PJ, et al. Clinical outcomes in elderly patients with metastatic colorectal cancer receiving bevacizumab and chemotherapy: results from the BRiTE observational cohort study. Oncology 2010;78:329–39.
86. Cunningham D, Lang I, Marcuello E, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol 2013;14:1077–85.
87. Aparicio T, Bouche O, Taieb J, et al. Bevacizumab+chemotherapy versus chemotherapy alone in elderly patients with untreated metastatic colorectal cancer: a randomized phase II trial-PRODIGE 20 study results. Ann Oncol 2018;29:133–8.
88. Van Cutsem E, Tabernero J, Lakomy R, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol 2012;30:3499–506.
89. Ruff P, Van Cutsem E, Lakomy R, et al. Observed benefit and safety of aflibercept in elderly patients with metastatic colorectal cancer: An age-based analysis from the randomized placebo-controlled phase III VELOUR trial. J Geriatr Oncol 2018;9:32–9.
90. Obermannova R, Van Cutsem E, Yoshino T, et al. Subgroup analysis in RAISE: a randomized, double-blind phase III study of irinotecan, folinic acid, and 5-fluorouracil (FOLFIRI) plus ramucirumab or placebo in patients with metastatic colorectal carcinoma progression. Ann Oncol 2016;27:2082–90.
91. Bouchahda M, Macarulla T, Spano JP, et al. Cetuximab efficacy and safety in a retrospective cohort of elderly patients with heavily pretreated metastatic colorectal cancer. Crit Rev Oncol Hematol 2008;67:255-62.
92. Douillard JY, Siena S, Cassidy J, et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol 2014;25:1346–55.
93. Sastre J, Gravalos C, Rivera F, et al. First-line cetuximab plus capecitabine in elderly patients with advanced colorectal cancer: clinical outcome and subgroup analysis according to KRAS status from a Spanish TTD Group Study. Oncologist 2012;17:339–45.
94. Dotan E, Devarajan K, D’Silva AJ, et al. Patterns of use and tolerance of anti-epidermal growth factor receptor antibodies in older adults with metastatic colorectal cancer. Clin Colorectal Cancer 2014;13:192–8.
95. Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381:303–12.
96. Van Cutsem E, Sobrero A, Siena S, et al. Regorafenib (REG) in progressive metastatic colorectal cancer (mCRC): Analysis of age subgroups in the phase III CORRECT trial [abstract]. J Clin Oncol 2013;31(15 suppl):3636-3636.
97. Bekaii-Saab TS, Ou FS, Anderson DM, et al. Regorafenib dose optimization study (ReDOS): Randomized phase II trial to evaluate dosing strategies for regorafenib in refractory metastatic colorectal cancer (mCRC): an ACCRU Network study [abstract]. J Clin Oncol 2018;36(4 suppl):611-611.
98. Mayer RJ, Van Cutsem E, Falcone A, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med 2015;372:1909–19.
99. Koopman M, Kortman GA, Mekenkamp L, et al. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br J Cancer 2009;100:266–73.
100. Venderbosch S, Nagtegaal ID, Maughan TS, et al. Mismatch repair status and BRAF mutation status in metastatic colorectal cancer patients: a pooled analysis of the CAIRO, CAIRO2, COIN, and FOCUS studies. Clin Cancer Res 2014;20:5322–30.
101. Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
102. Le DT, Uram JN, Wang H, et al. PD-1 Blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;372:2509–20.
103. Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017;18:1182–91.
104. Daste A, Domblides C, Gross-Goupil M, et al. Immune checkpoint inhibitors and elderly people: A review. Eur J Cancer 2017;82:155–66.
105. Elias R, Giobbie-Hurder A, McCleary NJ, et al. Efficacy of PD-1 & PD-L1 inhibitors in older adults: a meta-analysis. J Immunother Cancer 2018;6:26.
106. Singh H, Kim G, Maher VE, et al. FDA subset analysis of the safety of nivolumab in elderly patients with advanced cancers [abstract]. J Clin Oncol 2016;34(15 suppl):10010-10010.
107. Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol 2017;35:834–41.
108. Brighi N, Balducci L, Biasco G. Cancer in the elderly: is it time for palliative care in geriatric oncology? J Geriatr Oncol 2014;5:197–203.
109. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer 2008;113:3459–66.
110. Bagshaw SM, Stelfox HT, Johnson JA, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43:973–82.
111. Lynch MP, Marcone D, Kagan SH. Developing a multidisciplinary geriatric oncology program in a community cancer center. Clin J Oncol Nurs 2007;11:929–33.
112. Sheridan J, Walsh P, Kevans D, et al. Determinants of short- and long-term survival from colorectal cancer in very elderly patients. J Geriatr Oncol 2014;5:376–83.
Introduction
Colorectal cancer (CRC) is the fourth most common cancer in the United States and has a high prevalence among the older population.1 In 2017, there were an estimated 135,430 new cases of CRC and 50,260 deaths due to CRC. It is the second leading cause of cancer death in the United States, and the death rate for patients with CRC increases with age (Figure).2
Although elderly persons are more frequently diagnosed with CRC, they are underrepresented in clinical trials. This may be due in part to stringent eligibility criteria in prospective randomized controlled trials that exclude older patients with certain comorbidities and decreased functional status. Hutchins and colleagues compared the proportion of persons aged 65 years and older enrolled in Southwest Oncology Group (SWOG) clinical trials and the proportion of persons in this age group in the US population with the same cancer diagnoses.5 They found that while 72% of the US population with CRC were aged ≥ 65 years, persons in this age group comprised only 40% of patients enrolled in SWOG trials. An update on this study performed after Medicare policy changed in 2000 to include coverage of costs incurred due to clinical trials showed an upward trend in the accrual of older patients in SWOG trials, from 25% during the period 1993–1996 to 38% during the period 2001–2003; however, the percentage of older patients with CRC on clinical trials overall remained stable from 1993 to 2003.6
The underrepresentation of older adults with CRC in clinical trials presents oncologists with a challenging task when practicing evidence-based medicine in this patient population. Analysis of a large claims database demonstrated that the use of multi-agent chemotherapy for the treatment of metastatic CRC in older adults increased over time, while the use of single-agent 5-fluorouracil (5-FU) decreased.7 However, the adoption of combination therapy with irinotecan or oxaliplatin in older adults lagged behind the initial adoption of these agents in younger patients. This data demonstrates that as the field of medical oncology evolves, providers are becoming more comfortable treating older patients with multiple medical problems using standard approved regimens.
Geriatric Assessment
Before treating older patients with cancer, it is necessary to define the patient’s physiological age, ideally through a multidisciplinary team evaluation.
The Eastern Cooperative Oncology Group performance status (ECOG PS) and Karnofsky Performance Status (KPS) are crude measures of functional status.12 Generally, elderly patients with good ECOG PS or KPS scores are considered fit enough to receive standard therapy similar to their younger counterparts. Evaluation of functional status using these performance scores is often suboptimal, resulting in patients with a normal or adequate performance status score who may still experience poor outcomes, including decreased survival and inability to tolerate treatment. A study that explored parameters among older patients that predict for increased risk of chemotherapy-related toxicities found that physician-rated KPS score did not accurately predict the risk for adverse events.13 Therefore, a CGA represents a better way to evaluate functional status and other domains.
Functional status can also be evaluated by self-reported tools such as activities of daily living, which refer to basic self-care, and instrumental activities of daily living (IADLs), which are essential for independent living in the community.14,15 Mobility, gait, and balance can also be measured using the “Timed Get Up and Go” test and gait speed. Klepin et al found that faster gait speed was associated with overall survival (OS) in patients with metastatic cancer.16
Cognitive function is an important component of the geriatric assessment in older patients with cancer, as dementia is a prognostic factor for survival in the overall geriatric population. In a retrospective review, patients with dementia were less likely to have a biopsy-proven diagnosis and were twice as likely to have their CRC diagnosed postmortem.17 In addition, establishing that the patient has intact cognitive function prior to initiating treatment is essential to ensure that the patient can comply with treatment and understands when to report adverse effects. Nutritional status is an important portion of the geriatric assessment because malnutrition is associated with increased mortality and decreased tolerance for chemotherapy.18–20 Evaluating the patient’s psychosocial support is crucial as well because older patients are at greater risk of social isolation and depression.21 While the incidence of depression is lower in older adults with cancer than in younger adults with cancer, clinically significant depression is still noted in 3% to 25% of elderly cancer patients.22 Other critical components of the CGA are review of the patient’s comorbidities and medications to avoid complications of polypharmacy.
Both the Cancer and Aging Research Group (CARG) and Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) toxicity tools are valuable tools, as they predict chemotherapy tolerance in elderly patients.13,23 These tools can help guide discussions between oncologists and patients as well as the formulation of an appropriate treatment plan.24 Although toxicity tools can help to determine which patients are at risk for severe toxicity secondary to treatment, these tools do not replace the CGA. A prospective cohort study that evaluated the impact of CGA on tolerance to chemotherapy in older patients with cancer compared patients aged ≥ 70 years at the start of their treatment with chemotherapy (± radiation therapy) using geriatrician-delivered CGA versus standard care given by oncology.8 Patients who received geriatrician-guided CGA interventions tolerated chemotherapy better and completed treatments as planned (odds ratio 4.14 [95% confidence interval {CI} 1.50 to 11.42], P = 0.006) with fewer treatment modifications.
Unfortunately, the CGA is time-consuming to administer and difficult to incorporate into a busy oncology practice. Therefore, other screening models are used to identify patients who may benefit from a full CGA. The International Society of Geriatric Oncology performed a systematic review of screening tools used to identify older cancer patients in need of geriatric assessment and found that the 3 most studied screening tools are the G8, the Vulnerable Elders Survey-13 (VES-13), and the Flemish version of the Triage Risk Screening Tool.25 Another study found that the G8 was more sensitive than the VES-13 (76.5% versus 68.7%, P = 0.0046), whereas the VES-13 was more specific than the G8 (74.3% versus 64.4%, P < 0.0001).26 In addition to providing guidance to initiate a full geriatric assessment, these screening tools may assist in decision making for older cancer patients, especially those with advanced disease.
Surgery
Early-Stage Disease
When possible, surgical resection of colorectal tumors is the primary treatment in both the curative setting and to avoid complications, such as obstruction or perforation.27 Multiple studies have shown that fit elderly patients benefit from curative surgery similarly to their younger counterparts.27–29 With the growing population of persons aged 65 years or older, surgeons are becoming more comfortable with operating on the elderly.4 However, a large systematic review of 28 independent studies with a total of 34,194 patients showed that older patients were less likely to undergo curative surgery.30 Eligibility for surgery should not be determined by age alone, but rather should be based on a full assessment of the patient’s health, including comorbidities, functional status, nutrition, cognition, social support, and psychological status. The impact of age on short-term outcomes after colorectal surgery in terms of 30-day postoperative morbidity and mortality rates was explored in a study that divided patients into 2 groups: those aged ≥ 80 years (mean age 85) and those aged < 80 years (mean age 55.3).31 There were no statistical differences in 30-day postoperative morbidity and mortality rates between the 2 groups, and preexisting comorbidities and urgent nature of surgery were important predictors of colorectal surgery outcomes in the older adults, results that have been seen in several other studies.28,30 When possible, laparoscopic surgery is preferred as it is associated with less intraoperative blood loss, less postoperative pain, reduced postoperative ileus, a shorter hospital stay, and fewer cardiovascular and pulmonary complications.32 The Preoperative Assessment of Cancer in the Elderly (PACE), which combines surgical risk assessment tools with CGA tools, can assist surgeons in determining candidacy for surgery and help decrease unequal access to surgery in the geriatric population.33
Metastasectomy
A large international multicenter cohort study explored the outcomes of patients aged ≥ 70 years who underwent liver resection of colorectal metastases. The study investigatorsfound that neoadjuvant chemotherapy was used less frequently and less extensive surgery was performed in elderly patients than in younger patients.34 Sixty-day postoperative mortality was slightly higher (3.8% versus 1.6%, P < 0.001) and 3-year OS was slightly lower (57.1% versus 60.2%, P < 0.001) in the elderly group as compared to their younger counterparts, but overall the outcomes after liver surgery were similar. Therefore, the management of liver metastases in oligometastatic disease in elderly patients fit for surgery should be the same as that offered to younger patients. Since outcomes are comparable, older patients should be offered neoadjuvant chemotherapy, as several studies have shown similar response rates and OS in younger and older patients.35,36
Rectal Cancer
The standard of care for locally advanced rectal cancer is combined modality treatment with radiation and chemotherapy followed by total mesorectal excision. However, given conflicting data regarding the ability of elderly patients to tolerate neoadjuvant 5-FU-based chemotherapy and radiation, elderly patients are treated with trimodality therapy less often than their younger counterparts.37,38 A systematic review of 22 randomized trials involving 8507 patients with rectal cancer showed that adjuvant radiation therapy could reduce the risk of local recurrence and death from rectal cancer in patients of all ages.39 However, the risk of noncancer-related death was increased in the older population. The Stockholm II trial showed similar benefits of preoperative radiation overall, but this benefit did not extend to patients older than 68 years because of an increased risk of morbidity and mortality.40 In older patients, mortality from noncancer causes within the first 6 months after surgery was higher in the group that received perioperative radiation than in the group that did not receive radiation. Elderly patients (age > 68 years) accounted for most of the mortality, which was predominantly due to cardiovascular disease.
A retrospective study of 36 patients aged ≥ 70 years with rectal cancer evaluated the toxicity and feasibility of neoadjuvant 5-FU combined with pelvic radiation for treating locally advanced rectal cancer. Patients were classified as healthy and “fit” or “vulnerable” based on the presence of comorbidities.41 This study demonstrated that tolerability and response to neoadjuvant chemotherapy and radiation as well as ability to undergo surgery were similar in “vulnerable” patients and “fit” patients. Conversely, Margalit and colleagues studied the rate of treatment deviations in elderly patients with rectal cancer treated with combined modality therapy and found that most patients required early termination of treatment, treatment interruptions, or dose reductions.42 While trimodality treatment is the standard of care in rectal cancer, there is conflicting data from retrospective studies regarding the tolerability and feasibility of this approach. It is important to proceed with caution but to still consider fit older patients with locally advanced rectal cancer for neoadjuvant chemotherapy and radiation followed by surgery.
In patients who have a complete response (CR) to neoadjuvant chemoradiation, watchful waiting rather than proceeding to surgery may be a reasonable strategy, especially in older patients. A systematic review of 867 patients with locally advanced rectal cancer showed no statistically significant difference in OS between patients who were observed with watchful waiting and those who underwent surgery.43 The International Watch and Wait Database includes 679 patients who were managed with a watch-and-wait regimen because they had a clinical CR after chemoradiation. An outcomes analysis of these patients showed that 25% had local regrowth, with 3-year OS of 91% overall and 87% in patients with local regrowth.44 In most patients (84%), regrowth of the tumor occurred within the first 2 years of follow up.
In frail older adults, for whom longer courses of treatment are not feasible or chemotherapy is contraindicated, short-course radiation therapy can be considered either in the neoadjuvant setting or alone for palliation.45 A randomized trial of short-course radiation versus long-course chemoradiation in patients with T3 rectal cancer found that the difference in 3-year local recurrence rates was not statistically significant.46
Chemotherapy
An expected natural decline in function occurs with age, but given the great variability that exists between patients, it is important to focus on physiologic age rather than chronologic age to determine ability to receive and tolerate anticancer treatment. Decreases in renal and hepatic function, cognitive impairment, changes in gastrointestinal motility, decrements in cardiac and bone marrow reserves, as well as comorbidities and polypharmacy affect a patient’s ability to tolerate chemotherapy.47,48 Toxicity tools such as CARG and CRASH can help to predict severity of toxicity with chemotherapy.13,23 The information provided by these tools can help guide conversations between the oncologist and patient regarding treatment plans.
Adjuvant Chemotherapy for Early-Stage Disease
Stage II Disease
Defining treatment guidelines for older patients with stage II colon cancer is difficult due to lack of data that shows benefit in this population. The QUASAR (Quick and Simple and Reliable) group’s prospective study of adjuvant single-agent 5-FU in stage II colon cancer patients showed an absolute improvement in survival of 3.6% when 5-FU was given after surgery (95% CI 1.0 to 6.0).49 The subgroup analysis of patients aged ≥ 70 years showed a limited benefit of adjuvant 5-FU (hazard ratio [HR] 1.13 [95% CI 0.74 to 1.75]). Given the limited benefit, adjuvant 5-FU for elderly patients with stage II colon cancer should be used judiciously as patients may have competing causes of morbidity or mortality.
The use of oxaliplatin-based therapy in the adjuvant setting for stage II disease was evaluated in a subgroup analysis of the MOSAIC study (Multicenter International Study of Oxaliplatin/5-FU/Leucovorin in the Adjuvant Treatment of Colon Cancer).50 Adjuvant oxaliplatin-based treatment may be offered to patients with stage II colon cancer that carries high-risk features (poorly differentiated histology, lymphovascular invasion, bowel obstruction and/or perforation, < 12 lymph nodes sampled, perineural invasion, or indeterminate or positive margins) due to a trend toward improved disease-free survival (DFS) at 5 years. Patients in this group who received adjuvant FOLFOX (leucovorin, oxaliplatin, 5-FU) versus 5-FU/leucovorin had a DFS of 82.3% versus 74.6%, respectively (HR 0.72 [95% CI 0.50 to 1.02]), a difference that was not statistically significant. A subgroup analysis of 315 patients aged 70 to 75 years with stage II colon cancer enrolled in the MOSAIC study found no statistically significant DFS or OS benefit with the addition of oxaliplatin to 5-FU/leucovorin.51 Therefore, use of this platinum/fluoropyrimidine combination for adjuvant therapy for high-risk stage II disease in older patients remains controversial given its associated risks and the lack of definitive data demonstrating a benefit in this patient group. Decisions regarding this therapy should be made through a shared discussion with patients about its risks and benefits.
Microsatellite status is an important biomarker in the evaluation of stage II CRC. Microsatellite stability is a marker of a functioning DNA mismatch repair system. In patients with colon cancer, tumor microsatellite stability is classified based on the percentage of abnormal microsatellite regions.52 Several studies have shown that patients with tumors that display high microsatellite instability (MSI-H) have an improved prognosis over patients with microsatellite stable tumors.53,54 While patients with stage II MSI-H colon cancer have better outcomes, MSI is associated with a reduced response to treatment with fluoropyrimidines, as demonstrated in a systematic review that found that patients with tumors with MSI obtained no benefit from adjuvant 5-FU (HR 1.24 [95% CI 0.72 to 2.14]).55 Aparicio and colleagues reported an increased prevalence of MSI-H tumors with increasing age.56 Therefore, mismatch repair phenotype should be considered when making adjuvant chemotherapy decisions in the older adult with colon cancer, as it may affect the decision to recommend single-agent 5-FU treatment.
Stage III Disease
The use of single-agent 5-FU for stage III resected CRC has been evaluated in multiple studies. Sargent et al performed a pooled analysis of 3351 patients from 7 randomized phase 3 trials comparing surgery and adjuvant 5-FU-based chemotherapy versus surgery alone in stage II or III colon cancer patients.57 Adjuvant chemotherapy was associated with improvement in both OS and time to tumor recurrence (HR 0.76 and 0.68, respectively). The 5-year OS was 71% for those who received adjuvant treatment and 64% for those who were treated with surgery alone. The benefit of adjuvant treatment was independent of age, and there was no difference in toxicity across age groups, except for 1 study which showed increased rates of leukopenia in the elderly. The oral fluoropyrimidine capecitabine was shown to be an effective alternative to 5-FU plus leucovorin as adjuvant treatment for those with resected stage III colon cancer.58 However, in the subgroup analysis of DFS in the intention-to-treat group, the improvement in DFS was not statistically significant in those aged ≥ 70 years. This study justified the phase 3 Xeloda in Adjuvant Colon Cancer Therapy (X-ACT) trial, which compared capecitabine and 5-FU/leucovorin as adjuvant therapy in patients with resected stage III colon cancer.59 The X-ACT trial showed no significant effect of age on DFS or OS.
The addition of oxaliplatin to 5-FU in the adjuvant setting for stage III tumors has been studied and debated in the elderly population in multiple trials. The MOSAIC trial investigated FOLFOX versus 5-FU/leucovorin in the adjuvant setting.50 The addition of oxaliplatin was associated with a DFS and OS benefit, with a 20% reduction in risk of colon cancer recurrence and 16% reduction in risk of death in all patients. The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-07 trial then studied 2409 patients with stage II or III colon cancer treated with weekly bolus 5-FU/leucovorin with or without oxaliplatin.60 In this study, OS was significantly improved with the addition of oxaliplatin in patients younger than 70 years, but OS at 5 years was 4.7% worse for patients aged ≥ 70 years treated with weekly 5-FU/leucovorin and oxaliplatin compared with those treated with weekly 5-FU/leucovorin (71.6% versus 76.3%, respectively). In contrast, the XELOXA trial (NO16968), which randomly assigned stage III colon cancer patients to capecitabine and oxaliplatin (XELOX) or bolus 5-FU/leucovorin (standard of care at study start), showed an efficacy benefit, albeit not statistically significant, in patients aged ≥ 70 years (HR 0.87 [95% CI 0.63 to 1.18]).61–63
The Adjuvant Colon Cancer Endpoints (ACCENT) database included 7 randomized trials totaling 14,528 patients with stage II or III colon cancer treated with adjuvant 5-FU with or without oxaliplatin or irinotecan.64 Subgroup analysis of patients aged ≥ 70 years (n = 2575) showed no benefit with an oxaliplatin-based regimen in DFS (HR 0.94 [95% CI 0.78 to 1.13]) or OS (HR 1.04 [95% CI, 0.85 to 1.27]). Based on these studies and the increased toxicity with oxaliplatin, oxaliplatin-based adjuvant chemotherapy is utilized less often than single-agent 5-FU in geriatric patients with early-stage colon cancer.65 Conversely, a recent pooled analysis of individual patient data from 4 randomized trials (NSABP C-08, XELOXA, X-ACT, and AVANT) showed improved DFS and OS with adjuvant XELOX or FOLFOX over single-agent 5-FU in patients aged ≥ 70 years (DFS HR 0.77 [95% CI 0.62 to 0.95], P = 0.014; OS HR 0.78 [95% CI 0.61 to 0.99], P = 0.045).66 This analysis also showed that grade 3 and 4 adverse events related to oxaliplatin were similar across age groups.
These data come from post-hoc analyses, and there is no prospective data to steer decision making in elderly patients with early-stage CRC (Table).
It is well established that patients with stage III colon cancer benefit from oxaliplatin-based adjuvant chemotherapy after curative surgical resection.68 However, older patients are less likely to be referred to oncology as compared with their younger counterparts, due to the conflicting data regarding the benefit of this approach in older adults. Studies have shown that when the referral is placed, the geriatric population is less likely to receive chemotherapy.69 Sanoff et al analyzed 4 data sets (SEER-Medicare, National Comprehensive Cancer Network, New York State Cancer Registry, and Cancer Care Outcomes Research and Surveillance Consortium) to assess the benefit of adjuvant chemotherapy for resected stage III CRC among patients aged ≥ 75 years. Their analysis showed that only 40% of patients evaluated received adjuvant chemotherapy for stage III CRC after surgical resection.70
Summary
Prospective data to guide the treatment of older patients with early-stage CRC in the adjuvant setting is lacking. For fit older patients with stage II disease, limited benefit will be derived from single-agent 5-FU. For those with stage III CRC, the benefit and toxicities of fluoropyrimidines as adjuvant therapy appear to be similar regardless of age. The addition of oxaliplatin to fluoropyrimidines in patients aged ≥ 70 years has not been proven to improve DFS or OS and could result in an incremental toxicity profile. Therefore, treatment plans must be individualized, and decisions should be made through an informed discussion evaluating the overall risk/benefit ratio of each approach.
Metastatic Disease
Palliative Chemotherapy
Approximately 20% of patients with CRC are diagnosed with metastatic disease at presentation, and 35% to 40% develop metastatic disease following surgery and adjuvant therapy.2 The mainstay of treatment in this population is systemic therapy in the form of chemotherapy with or without biologic agents. In this setting, several prospective studies specific to older adults have been completed, providing more evidence-based guidance to oncologists who see these patients. Folprecht et al retrospectively reviewed data from 22 clinical trials evaluating 5-FU-based palliative chemotherapy in 3825 patients with metastatic CRC, including 629 patients aged ≥ 70 years.71 OS in elderly patients (10.8 months [95% CI 9.7 to 11.8]) was equivalent to that in younger patients (11.3 months [95% CI 10.9 to 11.7], P = 0.31). Similarly, relative risk and progression-free survival (PFS) were comparable irrespective of age.
Standard of care for most patients with metastatic colon cancer consists of 5-FU/leucovorin in combination with either oxaliplatin (FOLFOX) or irinotecan (FOLFIRI) with a monoclonal antibody.72 A retrospective pooled analysis of patients with metastatic CRC compared the safety and efficacy of FOLFOX4 in patients aged < 70 years versus those aged ≥ 70 years.73 While age ≥ 70 years was associated with an increased rate of grade ≥ 3 hematologic toxicity, it was not associated with increased rates of severe neurologic events, diarrhea, nausea, vomiting, infection, 60-day mortality, or overall incidence of grade ≥ 3 toxicity. The benefit of treatment was consistent across both age groups; therefore, age alone should not exclude an otherwise healthy individual from receiving FOLFOX.
These post-hoc analyses show that fit older patients who were candidates for trial participation tolerated these treatments well; however, these treatments may be more challenging for less fit older adults. The UK Medical Research Council FOCUS2 (Fluorouracil, Oxaliplatin, CPT11 [irinotecan]: Use and Sequencing) study was a prospective phase 3 trial that included 459 patients with metastatic CRC who were deemed too frail or not fit enough for standard-dose chemotherapy by their oncologists.74 In this group, 43% of patients were older than 75 years and 13% were older than 80 years. Patients were randomly assigned to receive infusional 5-FU with levofolinate; oxaliplatin and 5-FU; capecitabine; or oxaliplatin and capecitabine; all regimens were initiated with an empiric 20% dose reduction. The addition of oxaliplatin suggested some improvement in PFS, but this was not significant (5.8 months versus 4.5 months, HR 0.84 [95% CI 0.69 to 1.01], P = 0.07). Oxaliplatin was not associated with increased grade 3 or 4 toxicities. Capecitabine is often viewed as less toxic because it is taken by mouth, but this study found that replacement of 5-FU with capecitabine did not improve quality of life. Grade 3 or 4 toxicities were seen more frequently in those receiving capecitabine than in those receiving 5-FU (40% versus 30%, P = 0.03) in this older and frailer group of patients. As the patients on this study were frail and treatment dose was reduced, this data may not apply to fit older adults who are candidates for standard therapy.
When managing an older patient with metastatic CRC, it is important to tailor therapy based on goals of care, toxicity of proposed treatment, other comorbidities, and the patient’s functional status. One approach to minimizing toxicity in the older population is the stop-and-go strategy. The OPTIMOX1 study showed that stopping oxaliplatin after 6 cycles of FOLFOX7 and continuing maintenance therapy with infusional 5-FU/leucovorin alone for 12 cycles prior to reintroducing FOLFOX7 achieved efficacy similar to continuous FOLFOX4 with decreased toxicity.75 Figer et al studied an exploratory cohort of 37 patients aged 76 to 80 years who were included in the OPTIMOX1 study.76 The overall relative risk, median PFS, and median OS did not differ between the older patients in this cohort and younger patients studied in the original study. Older patients did experience more neutropenia, neurotoxicity, and overall grade 3 to 4 toxicity, but there were no toxic deaths in patients older than 75 years. The approach of giving treatment breaks, as in OPTIMOX2, may also provide patients with better quality of life, but perhaps at the expense of cancer-related survival.77
The combination of irinotecan and 5-FU has also been studied as treatment for patients with metastatic CRC. A pooled analysis of 2691 patients aged ≥ 70 years with metastatic CRC across 4 phase 3 randomized trials investigating irinotecan and 5-FU demonstrated that irinotecan-containing chemotherapy provided similar benefits to both older and younger patients with similar risk of toxicity.78 A phase 2 trial studying FOLFIRI as first-line treatment in older metastatic CRC patients showed this to be a safe and active regimen with manageable toxicity.79 Another randomized phase 3 trial for older patients compared 5-FU/leucovorin with or without irinotecan for first-line treatment of metastatic CRC (FFCD 2001-02).80 The study accrued 282 patients aged ≥ 75 years (median age 80 years), and found that the addition of irinotecan to infusional 5-FU–based chemotherapy did not significantly increase either PFS or OS. Aparicio et al performed a substudy of baseline geriatric evaluation prior to treatment in the FFCD 2001-02 study and assessed the value of geriatric parameters for predicting outcomes (objective response rate [ORR], PFS, and OS).81 Multivariate analysis showed that none of the geriatric parameters were predictive of ORR or PFS but that normal IADL was associated with better OS. This combination may still be appropriate for some older patients with metastatic disease, while single- agent 5-FU may be more appropriate in frail patients.
Biologic Agents
VEGF Inhibitors
Targeted biologic agents have been studied in the treatment of metastatic CRC. Bevacizumab is a recombinant, humanized monoclonal antibody against vascular endothelial growth factor (VEGF) that is approved in the first-line setting for treatment of metastatic CRC. A pooled analysis examined 439 patients 65 years of age and older with metastatic CRC who received bevacizumab plus chemotherapy versus placebo plus chemotherapy.82 In this analysis, the addition of bevacizumab was associated with an improvement in OS (19.3 months versus 14.3 months, HR 0.7 [95% CI 0.55 to 0.90], P = 0.006) and in PFS (9.2 months versus 6.2 months, HR 0.52 [95% CI 0.40 to 0.67], P < 0.0001). Known adverse events associated with bevacizumab were seen in the bevacizumab plus chemotherapy group but not at increased rates in the older population compared to their younger counterparts. Conversely, another pooled analysis found that while there was a PFS and OS benefit in older patients receiving bevacizumab, there was an increased incidence of thrombotic events in patients older than 65 years.83 The BEAT (Bevacizumab Expanded Access Trial) and BRiTE (Bevacizumab Regimens Investigation of Treatment Effects) studies showed similar clinical outcomes across all age groups.84,85 While older patients experienced more arterial thromboembolic events with the addition of bevacizumab, other factors such as ECOG PS, prior anticoagulation, and history of arterial disease were more predictive of these adverse events than age.
The randomized phase 3 AVEX study explored the efficacy and tolerability of capecitabine plus bevacizumab versus capecitabine alone in 280 frail patients aged ≥ 70 years.86 PFS in the capecitabine/bevacizumab arm was 9.1 months versus 5.1 months in the capecitabine alone arm. While the OS difference was not statistically significant, patients in the capecitabine/bevacizumab arm had an OS of 20.7 months versus 16.8 months in the capecitabine alone group. As reported in prior studies, patients in the capecitabine/bevacizumab arm had increased rates of toxic events (40%) compared with those who received capecitabine alone (22%), with reports of hypertension, hand-foot syndrome, bleeding, and thrombotic events. More recently, the phase 2 PRODIGE 20 trial studied the addition of bevacizumab to chemotherapy (5-FU, FOLFOX, or FOLFIRI) based on physician choice in untreated metastatic CRC patients aged ≥ 75 years (median age 80 years).87 They found that the addition of bevacizumab to standard of care chemotherapy was both safe and effective. The adverse events seen with bevacizumab, such as hypertension and thrombotic events, were consistent with prior studies.
A newer antiangiogenic agent, ziv-aflibercept, has been approved for the second-line treatment of metastatic CRC. The VELOUR trial demonstrated that the addition of ziv-aflibercept to FOLFIRI benefited patients across all age groups compared with FOLFIRI plus placebo in patients who had failed prior oxaliplatin-based chemotherapy.88,89 Ramucirumab is a human IgG-1 monoclonal antibody approved in second-line treatment in combination with FOLFIRI. A subgroup analysis of the RAISE study showed that the survival benefit was similar in patients aged ≥ 65 years versus those < 65 years.90 Based on the above data, the use of a VEGF inhibitor in combination with chemotherapy should be considered in older patients with metastatic CRC. Furthermore, based on the conflicting data regarding the benefit of FOLFOX/FOLFIRI over single-agent 5-FU discussed above, the combination of capecitabine plus bevacizumab may be considered a front-line treatment option in older patients based on the AVEX study.
EGFR Inhibitors
Cetuximab and panitumumab are anti-epidermal growth factor receptor (EGFR) antibodies approved for the treatment of RAS wild-type metastatic CRC. Data regarding the use of EGFR inhibitors in the geriatric population is scarce and the data that does exist is conflicting.91,92 The PRIME study demonstrated that panitumumab plus FOLFOX had a PFS benefit compared to FOLFOX alone in KRAS wild-type metastatic CRC patients.92 While the study met its primary endpoint, the benefit did not translate to patients aged ≥ 65 years in subgroup analysis. Conversely, a retrospective study of the efficacy and safety of cetuximab in elderly patients with heavily pretreated metastatic CRC found similar efficacy in older and younger patients as well as no increased adverse events in the older population.91 A phase 2 trial investigating cetuximab as single-agent first-line treatment of metastatic CRC in fit older patients found cetuximab to be safe with moderate activity in this population, but did not support the use of cetuximab as first-line single-agent treatment in fit geriatric patients who may be candidates for combination therapy.93 Our group studied the patterns of use and tolerance of anti-EGFR antibodies in 117 older adults with metastatic CRC with a median age of 73 years.94 The study showed that older age at the time of treatment was associated with administration of anti-EGFR antibody as monotherapy rather than in combination with chemotherapy (P = 0.0009). We found no association between age and presence of grade 3 or higher toxicity. In addition, the toxicity profile seen in older patients was similar to what has been demonstrated in prior studies involving a younger patient population. Given the discordance seen between studies, additional prospective trials are needed to elucidate the efficacy and safety of EGFR inhibitors in the geriatric population.
Other Agents
Two newer agents approved in the treatment of metastatic CRC are regorafenib, a multikinase inhibitor, and trifluridine/tipiracil (TFD/TPI), a nucleoside analog combined with an inhibitor of thymidine phosphorylase. The phase 3 CORRECT trial studied regorafenib as monotherapy in previously treated metastatic CRC and found an OS benefit of 1.4 months and minimal PFS benefit.95 Van Cutsem et al performed a subgroup analysis by age and found similar OS benefit in patients < 65 years of age and ≥ 65 years.96 The most frequent adverse events grade 3 or higher were hand-foot syndrome, fatigue, diarrhea, hypertension, and desquamation/rash, which were seen at similar rates in both age groups. More recently, the phase 2 Regorafenib Dose Optimization Study (ReDOS) found that weekly dose escalation of regorafenib from 80 mg to 160 mg daily over 3 weeks was superior to the standard 160 mg daily dosing in patients with metastatic CRC.97 The dose escalation group had a longer median OS, although this difference was not statistically significant, as well as a more favorable toxicity profile. Therefore, this new dosing strategy may be a reasonable option for older patients with pretreated metastatic CRC. A study of TFD/TPI versus placebo in refractory metastatic CRC found an OS benefit of 7.1 months versus 5.3 months.98 In subgroup analyses, the OS benefit extended to both patients < 65 years and ≥ 65 years. Given the sparse data on these newer agents in the geriatric population and the modest benefit they provide to those with refractory metastatic CRC, more data is needed to determine their utility in elderly patients. The decision to use these agents in the older patients warrants a thorough discussion with the patient regarding risks, benefit, and treatment goals.
Immunotherapy
Between 3.5% and 6.5% of stage IV colorectal cancers are MSI-H and have deficient mismatch repair (dMMR).99–101 A recent phase 2 trial studied the use of pembrolizumab, an IgG4 monoclonal antibody against PD-1 (programmed cell death-1), in heavily pretreated patients with dMMR metastatic CRC, MMR-proficient (pMMR) metastatic CRC, and noncolorectal dMMR metastatic cancer.102 Patients with dMMR metastatic CRC had a 50% ORR and 89% disease control rate (DCR), as compared with an ORR of 0% and DCR of 16% in patients with pMMR metastatic CRC. There was also an OS and PFS benefit seen in the dMMR CRC group as compared with the pMMR CRC group. Another phase 2 study, CheckMate 142, studied the anti-PD-1 monoclonal antibody nivolumab with or without ipilimumab (a monoclonal antibody against cytotoxic T-lymphocyte antigen 4) in patients with dMMR and pMMR metastatic CRC.103 In the interim analysis, nivolumab was found to provide both disease control and durable response in patients with dMMR metastatic CRC.
While these studies led to the FDA approval of pembrolizumab and nivolumab for management of previously treated MSI-H or dMMR metastatic CRC, data on the use of immunotherapy in older adults is scarce. Immunosenescence, or the gradual deterioration of the immune system that comes with aging, may impact the efficacy of immune checkpoint inhibitors (ICI) in older patients with advanced cancer.104 There is conflicting data on the efficacy of PD-1 and programmed death ligand-1) PD-L1 inhibitors in older patients across different cancers. A meta-analysis of immunotherapy in older adults with a variety of malignancies showed overall efficacy comparable to that seen in adults younger than 65 years.105 However, another review found ICIs to be less effective in older patients with head and neck, non-small cell lung cancer, and renal cell carcinoma compared with their younger counterparts.104 Regarding the toxicity profile of ICIs in the elderly, similar rates of grade 3 or higher adverse events in patients younger than 65 years and older than 65 years have been reported.106 However, patients aged ≥ 70 years had increased rates of grade 3 to 5 adverse events as compared to patients younger than 65 years (71.7% versus 58.4%, respectively). Given the scant data on ICIs in older patients with MSI-H or dMMR metastatic CRC, more clinical trials inclusive of this population are needed in order to determine the efficacy and safety of immunotherapy.
Palliative Care
The incorporation of palliative care early following the diagnosis of cancer has been shown to improve quality of life, decrease depression, and help with symptom management.107 The triggers for geriatric patients to initiate palliative care may be different from those of younger patients, as older patients may have different goals of care.108 Older patients will often choose quality over quantity of life when making treatment decisions.109 The ideal medical treatment for the frail patient with colorectal cancer would focus on treating disease while providing palliative measures to help support the patient and improve quality of life. It is paramount that patients maintain functional independence as loss of independence is recognized as a major threat to an older patient’s quality of life.110 The optimal way to achieve these goals is through the efforts of a multidisciplinary care team including not only physicians and nurses, but also social workers, nutritionists, physical therapists, and family who can provide support for the patient’s psychosocial, cognitive, and medical needs.111 Although cancer and noncancer–related death occur more frequently in the geriatric population, data to guide a specific palliative care approach to the elderly population is lacking.108
Conclusion
Colorectal cancer is a disease of older adults with a median age at diagnosis of 67 years.1 With the aging population, oncologists will be faced with treating increasing numbers of older patients, and must adjust their practice to accommodate this population of patients. Treating geriatric patients is challenging given the lack of available data to guide the treatment approach. Although several prospective elderly-specific studies have been conducted evaluating treatments for metastatic CRC, most treatment decisions are made based on the available retrospective studies and pooled analyses. Oncologists must carefully consider and evaluate each patient based on physiologic age rather than chronologic age.112 Overall, older patients should be given the opportunity to receive standard of care treatments in the appropriate setting. The decision to modify treatment plans should be made after a thorough evaluation by a multidisciplinary team and a discussion with the patient regarding their goals and the risks and benefits of the treatment. Geriatric assessment tools can help the care team identify patients with various geriatric syndromes that may not be detected on routine oncology evaluation. This type of evaluation is time consuming and is rarely done in a busy oncology practice. Ongoing studies are aiming to develop a method to incorporate geriatric assessments into the care of older adults.Additional prospective trials targeting older, more frail patients are essential to improve upon our knowledge so we can provide best care for this growing elderly population.
Introduction
Colorectal cancer (CRC) is the fourth most common cancer in the United States and has a high prevalence among the older population.1 In 2017, there were an estimated 135,430 new cases of CRC and 50,260 deaths due to CRC. It is the second leading cause of cancer death in the United States, and the death rate for patients with CRC increases with age (Figure).2
Although elderly persons are more frequently diagnosed with CRC, they are underrepresented in clinical trials. This may be due in part to stringent eligibility criteria in prospective randomized controlled trials that exclude older patients with certain comorbidities and decreased functional status. Hutchins and colleagues compared the proportion of persons aged 65 years and older enrolled in Southwest Oncology Group (SWOG) clinical trials and the proportion of persons in this age group in the US population with the same cancer diagnoses.5 They found that while 72% of the US population with CRC were aged ≥ 65 years, persons in this age group comprised only 40% of patients enrolled in SWOG trials. An update on this study performed after Medicare policy changed in 2000 to include coverage of costs incurred due to clinical trials showed an upward trend in the accrual of older patients in SWOG trials, from 25% during the period 1993–1996 to 38% during the period 2001–2003; however, the percentage of older patients with CRC on clinical trials overall remained stable from 1993 to 2003.6
The underrepresentation of older adults with CRC in clinical trials presents oncologists with a challenging task when practicing evidence-based medicine in this patient population. Analysis of a large claims database demonstrated that the use of multi-agent chemotherapy for the treatment of metastatic CRC in older adults increased over time, while the use of single-agent 5-fluorouracil (5-FU) decreased.7 However, the adoption of combination therapy with irinotecan or oxaliplatin in older adults lagged behind the initial adoption of these agents in younger patients. This data demonstrates that as the field of medical oncology evolves, providers are becoming more comfortable treating older patients with multiple medical problems using standard approved regimens.
Geriatric Assessment
Before treating older patients with cancer, it is necessary to define the patient’s physiological age, ideally through a multidisciplinary team evaluation.
The Eastern Cooperative Oncology Group performance status (ECOG PS) and Karnofsky Performance Status (KPS) are crude measures of functional status.12 Generally, elderly patients with good ECOG PS or KPS scores are considered fit enough to receive standard therapy similar to their younger counterparts. Evaluation of functional status using these performance scores is often suboptimal, resulting in patients with a normal or adequate performance status score who may still experience poor outcomes, including decreased survival and inability to tolerate treatment. A study that explored parameters among older patients that predict for increased risk of chemotherapy-related toxicities found that physician-rated KPS score did not accurately predict the risk for adverse events.13 Therefore, a CGA represents a better way to evaluate functional status and other domains.
Functional status can also be evaluated by self-reported tools such as activities of daily living, which refer to basic self-care, and instrumental activities of daily living (IADLs), which are essential for independent living in the community.14,15 Mobility, gait, and balance can also be measured using the “Timed Get Up and Go” test and gait speed. Klepin et al found that faster gait speed was associated with overall survival (OS) in patients with metastatic cancer.16
Cognitive function is an important component of the geriatric assessment in older patients with cancer, as dementia is a prognostic factor for survival in the overall geriatric population. In a retrospective review, patients with dementia were less likely to have a biopsy-proven diagnosis and were twice as likely to have their CRC diagnosed postmortem.17 In addition, establishing that the patient has intact cognitive function prior to initiating treatment is essential to ensure that the patient can comply with treatment and understands when to report adverse effects. Nutritional status is an important portion of the geriatric assessment because malnutrition is associated with increased mortality and decreased tolerance for chemotherapy.18–20 Evaluating the patient’s psychosocial support is crucial as well because older patients are at greater risk of social isolation and depression.21 While the incidence of depression is lower in older adults with cancer than in younger adults with cancer, clinically significant depression is still noted in 3% to 25% of elderly cancer patients.22 Other critical components of the CGA are review of the patient’s comorbidities and medications to avoid complications of polypharmacy.
Both the Cancer and Aging Research Group (CARG) and Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) toxicity tools are valuable tools, as they predict chemotherapy tolerance in elderly patients.13,23 These tools can help guide discussions between oncologists and patients as well as the formulation of an appropriate treatment plan.24 Although toxicity tools can help to determine which patients are at risk for severe toxicity secondary to treatment, these tools do not replace the CGA. A prospective cohort study that evaluated the impact of CGA on tolerance to chemotherapy in older patients with cancer compared patients aged ≥ 70 years at the start of their treatment with chemotherapy (± radiation therapy) using geriatrician-delivered CGA versus standard care given by oncology.8 Patients who received geriatrician-guided CGA interventions tolerated chemotherapy better and completed treatments as planned (odds ratio 4.14 [95% confidence interval {CI} 1.50 to 11.42], P = 0.006) with fewer treatment modifications.
Unfortunately, the CGA is time-consuming to administer and difficult to incorporate into a busy oncology practice. Therefore, other screening models are used to identify patients who may benefit from a full CGA. The International Society of Geriatric Oncology performed a systematic review of screening tools used to identify older cancer patients in need of geriatric assessment and found that the 3 most studied screening tools are the G8, the Vulnerable Elders Survey-13 (VES-13), and the Flemish version of the Triage Risk Screening Tool.25 Another study found that the G8 was more sensitive than the VES-13 (76.5% versus 68.7%, P = 0.0046), whereas the VES-13 was more specific than the G8 (74.3% versus 64.4%, P < 0.0001).26 In addition to providing guidance to initiate a full geriatric assessment, these screening tools may assist in decision making for older cancer patients, especially those with advanced disease.
Surgery
Early-Stage Disease
When possible, surgical resection of colorectal tumors is the primary treatment in both the curative setting and to avoid complications, such as obstruction or perforation.27 Multiple studies have shown that fit elderly patients benefit from curative surgery similarly to their younger counterparts.27–29 With the growing population of persons aged 65 years or older, surgeons are becoming more comfortable with operating on the elderly.4 However, a large systematic review of 28 independent studies with a total of 34,194 patients showed that older patients were less likely to undergo curative surgery.30 Eligibility for surgery should not be determined by age alone, but rather should be based on a full assessment of the patient’s health, including comorbidities, functional status, nutrition, cognition, social support, and psychological status. The impact of age on short-term outcomes after colorectal surgery in terms of 30-day postoperative morbidity and mortality rates was explored in a study that divided patients into 2 groups: those aged ≥ 80 years (mean age 85) and those aged < 80 years (mean age 55.3).31 There were no statistical differences in 30-day postoperative morbidity and mortality rates between the 2 groups, and preexisting comorbidities and urgent nature of surgery were important predictors of colorectal surgery outcomes in the older adults, results that have been seen in several other studies.28,30 When possible, laparoscopic surgery is preferred as it is associated with less intraoperative blood loss, less postoperative pain, reduced postoperative ileus, a shorter hospital stay, and fewer cardiovascular and pulmonary complications.32 The Preoperative Assessment of Cancer in the Elderly (PACE), which combines surgical risk assessment tools with CGA tools, can assist surgeons in determining candidacy for surgery and help decrease unequal access to surgery in the geriatric population.33
Metastasectomy
A large international multicenter cohort study explored the outcomes of patients aged ≥ 70 years who underwent liver resection of colorectal metastases. The study investigatorsfound that neoadjuvant chemotherapy was used less frequently and less extensive surgery was performed in elderly patients than in younger patients.34 Sixty-day postoperative mortality was slightly higher (3.8% versus 1.6%, P < 0.001) and 3-year OS was slightly lower (57.1% versus 60.2%, P < 0.001) in the elderly group as compared to their younger counterparts, but overall the outcomes after liver surgery were similar. Therefore, the management of liver metastases in oligometastatic disease in elderly patients fit for surgery should be the same as that offered to younger patients. Since outcomes are comparable, older patients should be offered neoadjuvant chemotherapy, as several studies have shown similar response rates and OS in younger and older patients.35,36
Rectal Cancer
The standard of care for locally advanced rectal cancer is combined modality treatment with radiation and chemotherapy followed by total mesorectal excision. However, given conflicting data regarding the ability of elderly patients to tolerate neoadjuvant 5-FU-based chemotherapy and radiation, elderly patients are treated with trimodality therapy less often than their younger counterparts.37,38 A systematic review of 22 randomized trials involving 8507 patients with rectal cancer showed that adjuvant radiation therapy could reduce the risk of local recurrence and death from rectal cancer in patients of all ages.39 However, the risk of noncancer-related death was increased in the older population. The Stockholm II trial showed similar benefits of preoperative radiation overall, but this benefit did not extend to patients older than 68 years because of an increased risk of morbidity and mortality.40 In older patients, mortality from noncancer causes within the first 6 months after surgery was higher in the group that received perioperative radiation than in the group that did not receive radiation. Elderly patients (age > 68 years) accounted for most of the mortality, which was predominantly due to cardiovascular disease.
A retrospective study of 36 patients aged ≥ 70 years with rectal cancer evaluated the toxicity and feasibility of neoadjuvant 5-FU combined with pelvic radiation for treating locally advanced rectal cancer. Patients were classified as healthy and “fit” or “vulnerable” based on the presence of comorbidities.41 This study demonstrated that tolerability and response to neoadjuvant chemotherapy and radiation as well as ability to undergo surgery were similar in “vulnerable” patients and “fit” patients. Conversely, Margalit and colleagues studied the rate of treatment deviations in elderly patients with rectal cancer treated with combined modality therapy and found that most patients required early termination of treatment, treatment interruptions, or dose reductions.42 While trimodality treatment is the standard of care in rectal cancer, there is conflicting data from retrospective studies regarding the tolerability and feasibility of this approach. It is important to proceed with caution but to still consider fit older patients with locally advanced rectal cancer for neoadjuvant chemotherapy and radiation followed by surgery.
In patients who have a complete response (CR) to neoadjuvant chemoradiation, watchful waiting rather than proceeding to surgery may be a reasonable strategy, especially in older patients. A systematic review of 867 patients with locally advanced rectal cancer showed no statistically significant difference in OS between patients who were observed with watchful waiting and those who underwent surgery.43 The International Watch and Wait Database includes 679 patients who were managed with a watch-and-wait regimen because they had a clinical CR after chemoradiation. An outcomes analysis of these patients showed that 25% had local regrowth, with 3-year OS of 91% overall and 87% in patients with local regrowth.44 In most patients (84%), regrowth of the tumor occurred within the first 2 years of follow up.
In frail older adults, for whom longer courses of treatment are not feasible or chemotherapy is contraindicated, short-course radiation therapy can be considered either in the neoadjuvant setting or alone for palliation.45 A randomized trial of short-course radiation versus long-course chemoradiation in patients with T3 rectal cancer found that the difference in 3-year local recurrence rates was not statistically significant.46
Chemotherapy
An expected natural decline in function occurs with age, but given the great variability that exists between patients, it is important to focus on physiologic age rather than chronologic age to determine ability to receive and tolerate anticancer treatment. Decreases in renal and hepatic function, cognitive impairment, changes in gastrointestinal motility, decrements in cardiac and bone marrow reserves, as well as comorbidities and polypharmacy affect a patient’s ability to tolerate chemotherapy.47,48 Toxicity tools such as CARG and CRASH can help to predict severity of toxicity with chemotherapy.13,23 The information provided by these tools can help guide conversations between the oncologist and patient regarding treatment plans.
Adjuvant Chemotherapy for Early-Stage Disease
Stage II Disease
Defining treatment guidelines for older patients with stage II colon cancer is difficult due to lack of data that shows benefit in this population. The QUASAR (Quick and Simple and Reliable) group’s prospective study of adjuvant single-agent 5-FU in stage II colon cancer patients showed an absolute improvement in survival of 3.6% when 5-FU was given after surgery (95% CI 1.0 to 6.0).49 The subgroup analysis of patients aged ≥ 70 years showed a limited benefit of adjuvant 5-FU (hazard ratio [HR] 1.13 [95% CI 0.74 to 1.75]). Given the limited benefit, adjuvant 5-FU for elderly patients with stage II colon cancer should be used judiciously as patients may have competing causes of morbidity or mortality.
The use of oxaliplatin-based therapy in the adjuvant setting for stage II disease was evaluated in a subgroup analysis of the MOSAIC study (Multicenter International Study of Oxaliplatin/5-FU/Leucovorin in the Adjuvant Treatment of Colon Cancer).50 Adjuvant oxaliplatin-based treatment may be offered to patients with stage II colon cancer that carries high-risk features (poorly differentiated histology, lymphovascular invasion, bowel obstruction and/or perforation, < 12 lymph nodes sampled, perineural invasion, or indeterminate or positive margins) due to a trend toward improved disease-free survival (DFS) at 5 years. Patients in this group who received adjuvant FOLFOX (leucovorin, oxaliplatin, 5-FU) versus 5-FU/leucovorin had a DFS of 82.3% versus 74.6%, respectively (HR 0.72 [95% CI 0.50 to 1.02]), a difference that was not statistically significant. A subgroup analysis of 315 patients aged 70 to 75 years with stage II colon cancer enrolled in the MOSAIC study found no statistically significant DFS or OS benefit with the addition of oxaliplatin to 5-FU/leucovorin.51 Therefore, use of this platinum/fluoropyrimidine combination for adjuvant therapy for high-risk stage II disease in older patients remains controversial given its associated risks and the lack of definitive data demonstrating a benefit in this patient group. Decisions regarding this therapy should be made through a shared discussion with patients about its risks and benefits.
Microsatellite status is an important biomarker in the evaluation of stage II CRC. Microsatellite stability is a marker of a functioning DNA mismatch repair system. In patients with colon cancer, tumor microsatellite stability is classified based on the percentage of abnormal microsatellite regions.52 Several studies have shown that patients with tumors that display high microsatellite instability (MSI-H) have an improved prognosis over patients with microsatellite stable tumors.53,54 While patients with stage II MSI-H colon cancer have better outcomes, MSI is associated with a reduced response to treatment with fluoropyrimidines, as demonstrated in a systematic review that found that patients with tumors with MSI obtained no benefit from adjuvant 5-FU (HR 1.24 [95% CI 0.72 to 2.14]).55 Aparicio and colleagues reported an increased prevalence of MSI-H tumors with increasing age.56 Therefore, mismatch repair phenotype should be considered when making adjuvant chemotherapy decisions in the older adult with colon cancer, as it may affect the decision to recommend single-agent 5-FU treatment.
Stage III Disease
The use of single-agent 5-FU for stage III resected CRC has been evaluated in multiple studies. Sargent et al performed a pooled analysis of 3351 patients from 7 randomized phase 3 trials comparing surgery and adjuvant 5-FU-based chemotherapy versus surgery alone in stage II or III colon cancer patients.57 Adjuvant chemotherapy was associated with improvement in both OS and time to tumor recurrence (HR 0.76 and 0.68, respectively). The 5-year OS was 71% for those who received adjuvant treatment and 64% for those who were treated with surgery alone. The benefit of adjuvant treatment was independent of age, and there was no difference in toxicity across age groups, except for 1 study which showed increased rates of leukopenia in the elderly. The oral fluoropyrimidine capecitabine was shown to be an effective alternative to 5-FU plus leucovorin as adjuvant treatment for those with resected stage III colon cancer.58 However, in the subgroup analysis of DFS in the intention-to-treat group, the improvement in DFS was not statistically significant in those aged ≥ 70 years. This study justified the phase 3 Xeloda in Adjuvant Colon Cancer Therapy (X-ACT) trial, which compared capecitabine and 5-FU/leucovorin as adjuvant therapy in patients with resected stage III colon cancer.59 The X-ACT trial showed no significant effect of age on DFS or OS.
The addition of oxaliplatin to 5-FU in the adjuvant setting for stage III tumors has been studied and debated in the elderly population in multiple trials. The MOSAIC trial investigated FOLFOX versus 5-FU/leucovorin in the adjuvant setting.50 The addition of oxaliplatin was associated with a DFS and OS benefit, with a 20% reduction in risk of colon cancer recurrence and 16% reduction in risk of death in all patients. The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-07 trial then studied 2409 patients with stage II or III colon cancer treated with weekly bolus 5-FU/leucovorin with or without oxaliplatin.60 In this study, OS was significantly improved with the addition of oxaliplatin in patients younger than 70 years, but OS at 5 years was 4.7% worse for patients aged ≥ 70 years treated with weekly 5-FU/leucovorin and oxaliplatin compared with those treated with weekly 5-FU/leucovorin (71.6% versus 76.3%, respectively). In contrast, the XELOXA trial (NO16968), which randomly assigned stage III colon cancer patients to capecitabine and oxaliplatin (XELOX) or bolus 5-FU/leucovorin (standard of care at study start), showed an efficacy benefit, albeit not statistically significant, in patients aged ≥ 70 years (HR 0.87 [95% CI 0.63 to 1.18]).61–63
The Adjuvant Colon Cancer Endpoints (ACCENT) database included 7 randomized trials totaling 14,528 patients with stage II or III colon cancer treated with adjuvant 5-FU with or without oxaliplatin or irinotecan.64 Subgroup analysis of patients aged ≥ 70 years (n = 2575) showed no benefit with an oxaliplatin-based regimen in DFS (HR 0.94 [95% CI 0.78 to 1.13]) or OS (HR 1.04 [95% CI, 0.85 to 1.27]). Based on these studies and the increased toxicity with oxaliplatin, oxaliplatin-based adjuvant chemotherapy is utilized less often than single-agent 5-FU in geriatric patients with early-stage colon cancer.65 Conversely, a recent pooled analysis of individual patient data from 4 randomized trials (NSABP C-08, XELOXA, X-ACT, and AVANT) showed improved DFS and OS with adjuvant XELOX or FOLFOX over single-agent 5-FU in patients aged ≥ 70 years (DFS HR 0.77 [95% CI 0.62 to 0.95], P = 0.014; OS HR 0.78 [95% CI 0.61 to 0.99], P = 0.045).66 This analysis also showed that grade 3 and 4 adverse events related to oxaliplatin were similar across age groups.
These data come from post-hoc analyses, and there is no prospective data to steer decision making in elderly patients with early-stage CRC (Table).
It is well established that patients with stage III colon cancer benefit from oxaliplatin-based adjuvant chemotherapy after curative surgical resection.68 However, older patients are less likely to be referred to oncology as compared with their younger counterparts, due to the conflicting data regarding the benefit of this approach in older adults. Studies have shown that when the referral is placed, the geriatric population is less likely to receive chemotherapy.69 Sanoff et al analyzed 4 data sets (SEER-Medicare, National Comprehensive Cancer Network, New York State Cancer Registry, and Cancer Care Outcomes Research and Surveillance Consortium) to assess the benefit of adjuvant chemotherapy for resected stage III CRC among patients aged ≥ 75 years. Their analysis showed that only 40% of patients evaluated received adjuvant chemotherapy for stage III CRC after surgical resection.70
Summary
Prospective data to guide the treatment of older patients with early-stage CRC in the adjuvant setting is lacking. For fit older patients with stage II disease, limited benefit will be derived from single-agent 5-FU. For those with stage III CRC, the benefit and toxicities of fluoropyrimidines as adjuvant therapy appear to be similar regardless of age. The addition of oxaliplatin to fluoropyrimidines in patients aged ≥ 70 years has not been proven to improve DFS or OS and could result in an incremental toxicity profile. Therefore, treatment plans must be individualized, and decisions should be made through an informed discussion evaluating the overall risk/benefit ratio of each approach.
Metastatic Disease
Palliative Chemotherapy
Approximately 20% of patients with CRC are diagnosed with metastatic disease at presentation, and 35% to 40% develop metastatic disease following surgery and adjuvant therapy.2 The mainstay of treatment in this population is systemic therapy in the form of chemotherapy with or without biologic agents. In this setting, several prospective studies specific to older adults have been completed, providing more evidence-based guidance to oncologists who see these patients. Folprecht et al retrospectively reviewed data from 22 clinical trials evaluating 5-FU-based palliative chemotherapy in 3825 patients with metastatic CRC, including 629 patients aged ≥ 70 years.71 OS in elderly patients (10.8 months [95% CI 9.7 to 11.8]) was equivalent to that in younger patients (11.3 months [95% CI 10.9 to 11.7], P = 0.31). Similarly, relative risk and progression-free survival (PFS) were comparable irrespective of age.
Standard of care for most patients with metastatic colon cancer consists of 5-FU/leucovorin in combination with either oxaliplatin (FOLFOX) or irinotecan (FOLFIRI) with a monoclonal antibody.72 A retrospective pooled analysis of patients with metastatic CRC compared the safety and efficacy of FOLFOX4 in patients aged < 70 years versus those aged ≥ 70 years.73 While age ≥ 70 years was associated with an increased rate of grade ≥ 3 hematologic toxicity, it was not associated with increased rates of severe neurologic events, diarrhea, nausea, vomiting, infection, 60-day mortality, or overall incidence of grade ≥ 3 toxicity. The benefit of treatment was consistent across both age groups; therefore, age alone should not exclude an otherwise healthy individual from receiving FOLFOX.
These post-hoc analyses show that fit older patients who were candidates for trial participation tolerated these treatments well; however, these treatments may be more challenging for less fit older adults. The UK Medical Research Council FOCUS2 (Fluorouracil, Oxaliplatin, CPT11 [irinotecan]: Use and Sequencing) study was a prospective phase 3 trial that included 459 patients with metastatic CRC who were deemed too frail or not fit enough for standard-dose chemotherapy by their oncologists.74 In this group, 43% of patients were older than 75 years and 13% were older than 80 years. Patients were randomly assigned to receive infusional 5-FU with levofolinate; oxaliplatin and 5-FU; capecitabine; or oxaliplatin and capecitabine; all regimens were initiated with an empiric 20% dose reduction. The addition of oxaliplatin suggested some improvement in PFS, but this was not significant (5.8 months versus 4.5 months, HR 0.84 [95% CI 0.69 to 1.01], P = 0.07). Oxaliplatin was not associated with increased grade 3 or 4 toxicities. Capecitabine is often viewed as less toxic because it is taken by mouth, but this study found that replacement of 5-FU with capecitabine did not improve quality of life. Grade 3 or 4 toxicities were seen more frequently in those receiving capecitabine than in those receiving 5-FU (40% versus 30%, P = 0.03) in this older and frailer group of patients. As the patients on this study were frail and treatment dose was reduced, this data may not apply to fit older adults who are candidates for standard therapy.
When managing an older patient with metastatic CRC, it is important to tailor therapy based on goals of care, toxicity of proposed treatment, other comorbidities, and the patient’s functional status. One approach to minimizing toxicity in the older population is the stop-and-go strategy. The OPTIMOX1 study showed that stopping oxaliplatin after 6 cycles of FOLFOX7 and continuing maintenance therapy with infusional 5-FU/leucovorin alone for 12 cycles prior to reintroducing FOLFOX7 achieved efficacy similar to continuous FOLFOX4 with decreased toxicity.75 Figer et al studied an exploratory cohort of 37 patients aged 76 to 80 years who were included in the OPTIMOX1 study.76 The overall relative risk, median PFS, and median OS did not differ between the older patients in this cohort and younger patients studied in the original study. Older patients did experience more neutropenia, neurotoxicity, and overall grade 3 to 4 toxicity, but there were no toxic deaths in patients older than 75 years. The approach of giving treatment breaks, as in OPTIMOX2, may also provide patients with better quality of life, but perhaps at the expense of cancer-related survival.77
The combination of irinotecan and 5-FU has also been studied as treatment for patients with metastatic CRC. A pooled analysis of 2691 patients aged ≥ 70 years with metastatic CRC across 4 phase 3 randomized trials investigating irinotecan and 5-FU demonstrated that irinotecan-containing chemotherapy provided similar benefits to both older and younger patients with similar risk of toxicity.78 A phase 2 trial studying FOLFIRI as first-line treatment in older metastatic CRC patients showed this to be a safe and active regimen with manageable toxicity.79 Another randomized phase 3 trial for older patients compared 5-FU/leucovorin with or without irinotecan for first-line treatment of metastatic CRC (FFCD 2001-02).80 The study accrued 282 patients aged ≥ 75 years (median age 80 years), and found that the addition of irinotecan to infusional 5-FU–based chemotherapy did not significantly increase either PFS or OS. Aparicio et al performed a substudy of baseline geriatric evaluation prior to treatment in the FFCD 2001-02 study and assessed the value of geriatric parameters for predicting outcomes (objective response rate [ORR], PFS, and OS).81 Multivariate analysis showed that none of the geriatric parameters were predictive of ORR or PFS but that normal IADL was associated with better OS. This combination may still be appropriate for some older patients with metastatic disease, while single- agent 5-FU may be more appropriate in frail patients.
Biologic Agents
VEGF Inhibitors
Targeted biologic agents have been studied in the treatment of metastatic CRC. Bevacizumab is a recombinant, humanized monoclonal antibody against vascular endothelial growth factor (VEGF) that is approved in the first-line setting for treatment of metastatic CRC. A pooled analysis examined 439 patients 65 years of age and older with metastatic CRC who received bevacizumab plus chemotherapy versus placebo plus chemotherapy.82 In this analysis, the addition of bevacizumab was associated with an improvement in OS (19.3 months versus 14.3 months, HR 0.7 [95% CI 0.55 to 0.90], P = 0.006) and in PFS (9.2 months versus 6.2 months, HR 0.52 [95% CI 0.40 to 0.67], P < 0.0001). Known adverse events associated with bevacizumab were seen in the bevacizumab plus chemotherapy group but not at increased rates in the older population compared to their younger counterparts. Conversely, another pooled analysis found that while there was a PFS and OS benefit in older patients receiving bevacizumab, there was an increased incidence of thrombotic events in patients older than 65 years.83 The BEAT (Bevacizumab Expanded Access Trial) and BRiTE (Bevacizumab Regimens Investigation of Treatment Effects) studies showed similar clinical outcomes across all age groups.84,85 While older patients experienced more arterial thromboembolic events with the addition of bevacizumab, other factors such as ECOG PS, prior anticoagulation, and history of arterial disease were more predictive of these adverse events than age.
The randomized phase 3 AVEX study explored the efficacy and tolerability of capecitabine plus bevacizumab versus capecitabine alone in 280 frail patients aged ≥ 70 years.86 PFS in the capecitabine/bevacizumab arm was 9.1 months versus 5.1 months in the capecitabine alone arm. While the OS difference was not statistically significant, patients in the capecitabine/bevacizumab arm had an OS of 20.7 months versus 16.8 months in the capecitabine alone group. As reported in prior studies, patients in the capecitabine/bevacizumab arm had increased rates of toxic events (40%) compared with those who received capecitabine alone (22%), with reports of hypertension, hand-foot syndrome, bleeding, and thrombotic events. More recently, the phase 2 PRODIGE 20 trial studied the addition of bevacizumab to chemotherapy (5-FU, FOLFOX, or FOLFIRI) based on physician choice in untreated metastatic CRC patients aged ≥ 75 years (median age 80 years).87 They found that the addition of bevacizumab to standard of care chemotherapy was both safe and effective. The adverse events seen with bevacizumab, such as hypertension and thrombotic events, were consistent with prior studies.
A newer antiangiogenic agent, ziv-aflibercept, has been approved for the second-line treatment of metastatic CRC. The VELOUR trial demonstrated that the addition of ziv-aflibercept to FOLFIRI benefited patients across all age groups compared with FOLFIRI plus placebo in patients who had failed prior oxaliplatin-based chemotherapy.88,89 Ramucirumab is a human IgG-1 monoclonal antibody approved in second-line treatment in combination with FOLFIRI. A subgroup analysis of the RAISE study showed that the survival benefit was similar in patients aged ≥ 65 years versus those < 65 years.90 Based on the above data, the use of a VEGF inhibitor in combination with chemotherapy should be considered in older patients with metastatic CRC. Furthermore, based on the conflicting data regarding the benefit of FOLFOX/FOLFIRI over single-agent 5-FU discussed above, the combination of capecitabine plus bevacizumab may be considered a front-line treatment option in older patients based on the AVEX study.
EGFR Inhibitors
Cetuximab and panitumumab are anti-epidermal growth factor receptor (EGFR) antibodies approved for the treatment of RAS wild-type metastatic CRC. Data regarding the use of EGFR inhibitors in the geriatric population is scarce and the data that does exist is conflicting.91,92 The PRIME study demonstrated that panitumumab plus FOLFOX had a PFS benefit compared to FOLFOX alone in KRAS wild-type metastatic CRC patients.92 While the study met its primary endpoint, the benefit did not translate to patients aged ≥ 65 years in subgroup analysis. Conversely, a retrospective study of the efficacy and safety of cetuximab in elderly patients with heavily pretreated metastatic CRC found similar efficacy in older and younger patients as well as no increased adverse events in the older population.91 A phase 2 trial investigating cetuximab as single-agent first-line treatment of metastatic CRC in fit older patients found cetuximab to be safe with moderate activity in this population, but did not support the use of cetuximab as first-line single-agent treatment in fit geriatric patients who may be candidates for combination therapy.93 Our group studied the patterns of use and tolerance of anti-EGFR antibodies in 117 older adults with metastatic CRC with a median age of 73 years.94 The study showed that older age at the time of treatment was associated with administration of anti-EGFR antibody as monotherapy rather than in combination with chemotherapy (P = 0.0009). We found no association between age and presence of grade 3 or higher toxicity. In addition, the toxicity profile seen in older patients was similar to what has been demonstrated in prior studies involving a younger patient population. Given the discordance seen between studies, additional prospective trials are needed to elucidate the efficacy and safety of EGFR inhibitors in the geriatric population.
Other Agents
Two newer agents approved in the treatment of metastatic CRC are regorafenib, a multikinase inhibitor, and trifluridine/tipiracil (TFD/TPI), a nucleoside analog combined with an inhibitor of thymidine phosphorylase. The phase 3 CORRECT trial studied regorafenib as monotherapy in previously treated metastatic CRC and found an OS benefit of 1.4 months and minimal PFS benefit.95 Van Cutsem et al performed a subgroup analysis by age and found similar OS benefit in patients < 65 years of age and ≥ 65 years.96 The most frequent adverse events grade 3 or higher were hand-foot syndrome, fatigue, diarrhea, hypertension, and desquamation/rash, which were seen at similar rates in both age groups. More recently, the phase 2 Regorafenib Dose Optimization Study (ReDOS) found that weekly dose escalation of regorafenib from 80 mg to 160 mg daily over 3 weeks was superior to the standard 160 mg daily dosing in patients with metastatic CRC.97 The dose escalation group had a longer median OS, although this difference was not statistically significant, as well as a more favorable toxicity profile. Therefore, this new dosing strategy may be a reasonable option for older patients with pretreated metastatic CRC. A study of TFD/TPI versus placebo in refractory metastatic CRC found an OS benefit of 7.1 months versus 5.3 months.98 In subgroup analyses, the OS benefit extended to both patients < 65 years and ≥ 65 years. Given the sparse data on these newer agents in the geriatric population and the modest benefit they provide to those with refractory metastatic CRC, more data is needed to determine their utility in elderly patients. The decision to use these agents in the older patients warrants a thorough discussion with the patient regarding risks, benefit, and treatment goals.
Immunotherapy
Between 3.5% and 6.5% of stage IV colorectal cancers are MSI-H and have deficient mismatch repair (dMMR).99–101 A recent phase 2 trial studied the use of pembrolizumab, an IgG4 monoclonal antibody against PD-1 (programmed cell death-1), in heavily pretreated patients with dMMR metastatic CRC, MMR-proficient (pMMR) metastatic CRC, and noncolorectal dMMR metastatic cancer.102 Patients with dMMR metastatic CRC had a 50% ORR and 89% disease control rate (DCR), as compared with an ORR of 0% and DCR of 16% in patients with pMMR metastatic CRC. There was also an OS and PFS benefit seen in the dMMR CRC group as compared with the pMMR CRC group. Another phase 2 study, CheckMate 142, studied the anti-PD-1 monoclonal antibody nivolumab with or without ipilimumab (a monoclonal antibody against cytotoxic T-lymphocyte antigen 4) in patients with dMMR and pMMR metastatic CRC.103 In the interim analysis, nivolumab was found to provide both disease control and durable response in patients with dMMR metastatic CRC.
While these studies led to the FDA approval of pembrolizumab and nivolumab for management of previously treated MSI-H or dMMR metastatic CRC, data on the use of immunotherapy in older adults is scarce. Immunosenescence, or the gradual deterioration of the immune system that comes with aging, may impact the efficacy of immune checkpoint inhibitors (ICI) in older patients with advanced cancer.104 There is conflicting data on the efficacy of PD-1 and programmed death ligand-1) PD-L1 inhibitors in older patients across different cancers. A meta-analysis of immunotherapy in older adults with a variety of malignancies showed overall efficacy comparable to that seen in adults younger than 65 years.105 However, another review found ICIs to be less effective in older patients with head and neck, non-small cell lung cancer, and renal cell carcinoma compared with their younger counterparts.104 Regarding the toxicity profile of ICIs in the elderly, similar rates of grade 3 or higher adverse events in patients younger than 65 years and older than 65 years have been reported.106 However, patients aged ≥ 70 years had increased rates of grade 3 to 5 adverse events as compared to patients younger than 65 years (71.7% versus 58.4%, respectively). Given the scant data on ICIs in older patients with MSI-H or dMMR metastatic CRC, more clinical trials inclusive of this population are needed in order to determine the efficacy and safety of immunotherapy.
Palliative Care
The incorporation of palliative care early following the diagnosis of cancer has been shown to improve quality of life, decrease depression, and help with symptom management.107 The triggers for geriatric patients to initiate palliative care may be different from those of younger patients, as older patients may have different goals of care.108 Older patients will often choose quality over quantity of life when making treatment decisions.109 The ideal medical treatment for the frail patient with colorectal cancer would focus on treating disease while providing palliative measures to help support the patient and improve quality of life. It is paramount that patients maintain functional independence as loss of independence is recognized as a major threat to an older patient’s quality of life.110 The optimal way to achieve these goals is through the efforts of a multidisciplinary care team including not only physicians and nurses, but also social workers, nutritionists, physical therapists, and family who can provide support for the patient’s psychosocial, cognitive, and medical needs.111 Although cancer and noncancer–related death occur more frequently in the geriatric population, data to guide a specific palliative care approach to the elderly population is lacking.108
Conclusion
Colorectal cancer is a disease of older adults with a median age at diagnosis of 67 years.1 With the aging population, oncologists will be faced with treating increasing numbers of older patients, and must adjust their practice to accommodate this population of patients. Treating geriatric patients is challenging given the lack of available data to guide the treatment approach. Although several prospective elderly-specific studies have been conducted evaluating treatments for metastatic CRC, most treatment decisions are made based on the available retrospective studies and pooled analyses. Oncologists must carefully consider and evaluate each patient based on physiologic age rather than chronologic age.112 Overall, older patients should be given the opportunity to receive standard of care treatments in the appropriate setting. The decision to modify treatment plans should be made after a thorough evaluation by a multidisciplinary team and a discussion with the patient regarding their goals and the risks and benefits of the treatment. Geriatric assessment tools can help the care team identify patients with various geriatric syndromes that may not be detected on routine oncology evaluation. This type of evaluation is time consuming and is rarely done in a busy oncology practice. Ongoing studies are aiming to develop a method to incorporate geriatric assessments into the care of older adults.Additional prospective trials targeting older, more frail patients are essential to improve upon our knowledge so we can provide best care for this growing elderly population.
1. National Cancer Institute. SEER cancer stat facts: colorectal cancer. http://seer.cancer.gov/statfacts/html/colorect.html. Accessed March 1, 2018.
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:7–30.
3. Kochanek KD, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief 2017:1-8.
4. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States, current population reports, P25-1140. Washington, DC: U.S. Census Bureau; 2014.
5. Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med 1999;341:2061–7.
6. Unger JM, Coltman CA Jr, Crowley JJ, et al. Impact of the year 2000 Medicare policy change on older patient enrollment to cancer clinical trials. J Clin Oncol 2006;24:141–4.
7. Vijayvergia N, Li T, Wong YN, et al. Chemotherapy use and adoption of new agents is affected by age and comorbidities in patients with metastatic colorectal cancer. Cancer 2016;122:3191–8.
8. Kalsi T, Babic-Illman G, Ross PJ, et al. The impact of comprehensive geriatric assessment interventions on tolerance to chemotherapy in older people. Br J Cancer 2015;112:1435–44.
9. National Comprehensive Cancer Network. Older adult oncology (Version 2.2017). Accessed March 1, 2018,
10. Balducci L. Frailty: a common pathway in aging and cancer. Interdiscip Top Gerontol 2013;38:61–72.
11. Baijal P, Periyakoil V. Understanding frailty in cancer patients. Cancer J 2014;20:358–66.
12. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–55.
13. Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 2011;29:3457–65.
14. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86.
15. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist 1970;10:20–30.
16. Klepin HD, Geiger AM, Tooze JA, et al. Physical performance and subsequent disability and survival in older adults with malignancy: results from the health, aging and body composition study. J Am Geriatr Soc 2010;58:76–82.
17. Gupta SK, Lamont EB. Patterns of presentation, diagnosis, and treatment in older patients with colon cancer and comorbid dementia. J Am Geriatr Soc 2004;52:1681–7.
18. Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 1980;69:491–7.
19. Aaldriks AA, van der Geest LG, Giltay EJ, et al. Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 2013;4:218–26.
20. Martucci RB, Barbosa MV, D’Almeida CA, et al. Undernutrition as independent predictor of early mortality in elderly cancer patients. Nutrition 2017;34:65–70.
21. Naeim A, Aapro M, Subbarao R, Balducci L. Supportive care considerations for older adults with cancer. J Clin Oncol 2014;32:2627–34.
22. Kua J. The prevalence of psychological and psychiatric sequelae of cancer in the elderly - how much do we know? Ann Acad Med Singapore 2005;34:250–6.
23. Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012;118:3377–86.
24. Kim J, Hurria A. Determining chemotherapy tolerance in older patients with cancer. J Natl Compr Canc Netw 2013;11:1494-502.
25. Decoster L, Van Puyvelde K, Mohile S, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations. Ann Oncol 2015;26:288–300.
26. Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PLoS One 2014; 9:e115060.
27. Gurevitch AJ, Davidovitch B, Kashtan H. Outcome of right colectomy for cancer in octogenarians. J Gastrointest Surg 2009;13:100–4.
28. Schiffmann L, Ozcan S, Schwarz F, et al. Colorectal cancer in the elderly: surgical treatment and long-term survival. Int J Colorectal Dis 2008;23:601–10.
29. Ong ES, Alassas M, Dunn KB, Rajput A. Colorectal cancer surgery in the elderly: acceptable morbidity? Am J Surg 2008;195:344–8.
30. Surgery for colorectal cancer in elderly patients: a systematic review. Colorectal Cancer Collaborative Group. Lancet 2000;356:968–74.
31. Shalaby M, Di Lorenzo N, Franceschilli L, et al. Outcome of colorectal surgery in elderly populations. Ann Coloproctol 2016;32:139–43.
32. Frasson M, Braga M, Vignali A, et al. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 2008;51:296–300.
33. PACE participants, Audisio RA, Pope D, et al. Shall we operate? Preoperative assessment in elderly cancer patients (PACE) can help. A SIOG surgical task force prospective study. Crit Rev Oncol Hematol 2008;65:156–63.
34. Adam R, Frilling A, Elias D, et al. Liver resection of colorectal metastases in elderly patients. Br J Surg 2010;97:366–76.
35. de Liguori Carino N, van Leeuwen BL, Ghaneh P, et al. Liver resection for colorectal liver metastases in older patients. Crit Rev Oncol Hematol 2008;67:273–8.
36. Tamandl D, Gruenberger B, Herberger B, et al. Surgery after neoadjuvant chemotherapy for colorectal liver metastases is safe and feasible in elderly patients. J Surg Oncol 2009;100:364–71.
37. Shahir MA, Lemmens VE, van de Poll-Franse LV, et al. Elderly patients with rectal cancer have a higher risk of treatment-related complications and a poorer prognosis than younger patients: a population-based study. Eur J Cancer 2006;42:3015–21.
38. Chang GJ, Skibber JM, Feig BW, Rodriguez-Bigas M. Are we undertreating rectal cancer in the elderly? An epidemiologic study. Ann Surg 2007;246:215–21.
39. Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 2001;358:1291–304.
40. Martling A, Holm T, Johansson H, et al, Stockholm Colorectal Cancer Study Group. The Stockholm II trial on preoperative radiotherapy in rectal carcinoma: long-term follow-up of a population-based study. Cancer 2001;92:896–902.
41. Pasetto LM, Friso ML, Pucciarelli S, et al. Rectal cancer neoadjuvant treatment in elderly patients. Anticancer Res 2006;26:3913–23.
42. Margalit DN, Mamon HJ, Ancukiewicz M, et al. Tolerability of combined modality therapy for rectal cancer in elderly patients aged 75 years and older. Int J Radiat Oncol Biol Phys 2011;81:e735–41.
43. Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2017;2:501–13.
44. van der Valk M. The International Watch & Wait database (IWWD) for rectal cancer: An update. J Clin Oncol 2017;35 suppl:521.
45. Donato V, Valeriani M, Zurlo A. Short course radiation therapy for elderly cancer patients. Evidences from the literature review. Crit Rev Oncol Hematol 2003;45:305–11.
46. Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 2012;30:3827–33.
47. McCleary NJ, Dotan E, Browner I. Refining the chemotherapy approach for older patients with colon cancer. J Clin Oncol 2014;32:2570–80.
48. Millan M, Merino S, Caro A, et al. Treatment of colorectal cancer in the elderly. World J Gastrointest Oncol 2015;7:204–20.
49. Quasar Collaborative Group, Gray R, Barnwell J, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370:2020–9.
50. Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009;27:3109–16.
51. Tournigand C, Andre T, Bonnetain F, et al. Adjuvant therapy with fluorouracil and oxaliplatin in stage II and elderly patients (between ages 70 and 75 years) with colon cancer: subgroup analyses of the Multicenter International Study of Oxaliplatin, Fluorouracil, and Leucovorin in the Adjuvant Treatment of Colon Cancer trial. J Clin Oncol 2012;30:3353–60.
52. Winder T, Lenz HJ. Molecular predictive and prognostic markers in colon cancer. Cancer Treat Rev 2010;36:550–6.
53. Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
54. Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
55. Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
56. Aparicio T, Schischmanoff O, Poupardin C, et al. Deficient mismatch repair phenotype is a prognostic factor for colorectal cancer in elderly patients. Dig Liver Dis 2013;45:245–50.
57. Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients. N Engl J Med 2001;345:1091–7.
58. Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
59. Twelves C, Scheithauer W, McKendrick J, et al. Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol 2012;23:1190–7.
60. Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 2011;29:3768–74.
61. Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
62. Haller DG, Cassidy J, Tabernero J, et al. Efficacy findings from a randomized phase III trial of capecitabine plus oxaliplatin versus bolus 5-FU/LV for stage III colon cancer (NO16968): impact of age on disease-free survival (DFS) [abstract]. J Clin Oncol 2010;28:3521.
63. Schmoll HJ, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
64. McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
65. Kahn KL, Adams JL, Weeks JC, et al. Adjuvant chemotherapy use and adverse events among older patients with stage III colon cancer. JAMA 2010;303:1037–45.
66. Haller DG, O’Connell MJ, Cartwright TH, et al. Impact of age and medical comorbidity on adjuvant treatment outcomes for stage III colon cancer: a pooled analysis of individual patient data from four randomized, controlled trials. Ann Oncol 2015;26:715-24.
67. Aparicio T, Francois E, Cristol-Dalstein L, et al. PRODIGE 34-FFCD 1402-ADAGE: Adjuvant chemotherapy in elderly patients with resected stage III colon cancer: A randomized phase 3 trial. Dig Liver Dis 2016;48:206–7.
68. Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
69. Mahoney T, Kuo YH, Topilow A, Davis JM. Stage III colon cancers: why adjuvant chemotherapy is not offered to elderly patients. Arch Surg 2000;135:182–5.
70. Sanoff HK, Carpenter WR, Sturmer T, et al. Effect of adjuvant chemotherapy on survival of patients with stage III colon cancer diagnosed after age 75 years. J Clin Oncol 2012;30:2624–34.
71. Folprecht G, Cunningham D, Ross P, et al. Efficacy of 5-fluorouracil-based chemotherapy in elderly patients with metastatic colorectal cancer: a pooled analysis of clinical trials. Ann Oncol 2004;15:1330–8.
72. Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, ESMO Guidelines Working Group. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25 Suppl 3:iii1–9.
73. Goldberg RM, Tabah-Fisch I, Bleiberg H, et al. Pooled analysis of safety and efficacy of oxaliplatin plus fluorouracil/leucovorin administered bimonthly in elderly patients with colorectal cancer. J Clin Oncol 2006;24:4085–91.
74. Seymour MT, Thompson LC, Wasan HS, et al. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): an open-label, randomised factorial trial. Lancet 2011;377:1749–59.
75. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer--a GERCOR study. J Clin Oncol 2006;24:394–400.
76. Figer A, Perez-Staub N, Carola E, et al. FOLFOX in patients aged between 76 and 80 years with metastatic colorectal cancer: an exploratory cohort of the OPTIMOX1 study. Cancer 2007;110:2666–71.
77. Chibaudel B, Maindrault-Goebel F, Lledo G, et al. Can chemotherapy be discontinued in unresectable metastatic colorectal cancer? The GERCOR OPTIMOX2 Study. J Clin Oncol 2009;27:5727–33.
78. Folprecht G, Seymour MT, Saltz L, et al. Irinotecan/fluorouracil combination in first-line therapy of older and younger patients with metastatic colorectal cancer: combined analysis of 2,691 patients in randomized controlled trials. J Clin Oncol 2008;26:1443–51.
79. Souglakos J, Pallis A, Kakolyris S, et al. Combination of irinotecan (CPT-11) plus 5-fluorouracil and leucovorin (FOLFIRI regimen) as first line treatment for elderly patients with metastatic colorectal cancer: a phase II trial. Oncology 2005;69:384–90.
80. Aparicio T, Lavau-Denes S, Phelip JM, et al. Randomized phase III trial in elderly patients comparing LV5FU2 with or without irinotecan for first-line treatment of metastatic colorectal cancer (FFCD 2001-02). Ann Oncol 2016;27:121–7.
81. Aparicio T, Gargot D, Teillet L, et al. Geriatric factors analyses from FFCD 2001-02 phase III study of first-line chemotherapy for elderly metastatic colorectal cancer patients. Eur J Cancer 2017;74:98–108.
82. Kabbinavar FF, Hurwitz HI, Yi J, et al. Addition of bevacizumab to fluorouracil-based first-line treatment of metastatic colorectal cancer: pooled analysis of cohorts of older patients from two randomized clinical trials. J Clin Oncol 2009;27:199–205.
83. Cassidy J, Saltz LB, Giantonio BJ, et al. Effect of bevacizumab in older patients with metastatic colorectal cancer: pooled analysis of four randomized studies. J Cancer Res Clin Oncol 2010;136:737–43.
84. Van Cutsem E, Rivera F, Berry S, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol 2009;20:1842–7.
85. Kozloff MF, Berlin J, Flynn PJ, et al. Clinical outcomes in elderly patients with metastatic colorectal cancer receiving bevacizumab and chemotherapy: results from the BRiTE observational cohort study. Oncology 2010;78:329–39.
86. Cunningham D, Lang I, Marcuello E, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol 2013;14:1077–85.
87. Aparicio T, Bouche O, Taieb J, et al. Bevacizumab+chemotherapy versus chemotherapy alone in elderly patients with untreated metastatic colorectal cancer: a randomized phase II trial-PRODIGE 20 study results. Ann Oncol 2018;29:133–8.
88. Van Cutsem E, Tabernero J, Lakomy R, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol 2012;30:3499–506.
89. Ruff P, Van Cutsem E, Lakomy R, et al. Observed benefit and safety of aflibercept in elderly patients with metastatic colorectal cancer: An age-based analysis from the randomized placebo-controlled phase III VELOUR trial. J Geriatr Oncol 2018;9:32–9.
90. Obermannova R, Van Cutsem E, Yoshino T, et al. Subgroup analysis in RAISE: a randomized, double-blind phase III study of irinotecan, folinic acid, and 5-fluorouracil (FOLFIRI) plus ramucirumab or placebo in patients with metastatic colorectal carcinoma progression. Ann Oncol 2016;27:2082–90.
91. Bouchahda M, Macarulla T, Spano JP, et al. Cetuximab efficacy and safety in a retrospective cohort of elderly patients with heavily pretreated metastatic colorectal cancer. Crit Rev Oncol Hematol 2008;67:255-62.
92. Douillard JY, Siena S, Cassidy J, et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol 2014;25:1346–55.
93. Sastre J, Gravalos C, Rivera F, et al. First-line cetuximab plus capecitabine in elderly patients with advanced colorectal cancer: clinical outcome and subgroup analysis according to KRAS status from a Spanish TTD Group Study. Oncologist 2012;17:339–45.
94. Dotan E, Devarajan K, D’Silva AJ, et al. Patterns of use and tolerance of anti-epidermal growth factor receptor antibodies in older adults with metastatic colorectal cancer. Clin Colorectal Cancer 2014;13:192–8.
95. Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381:303–12.
96. Van Cutsem E, Sobrero A, Siena S, et al. Regorafenib (REG) in progressive metastatic colorectal cancer (mCRC): Analysis of age subgroups in the phase III CORRECT trial [abstract]. J Clin Oncol 2013;31(15 suppl):3636-3636.
97. Bekaii-Saab TS, Ou FS, Anderson DM, et al. Regorafenib dose optimization study (ReDOS): Randomized phase II trial to evaluate dosing strategies for regorafenib in refractory metastatic colorectal cancer (mCRC): an ACCRU Network study [abstract]. J Clin Oncol 2018;36(4 suppl):611-611.
98. Mayer RJ, Van Cutsem E, Falcone A, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med 2015;372:1909–19.
99. Koopman M, Kortman GA, Mekenkamp L, et al. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br J Cancer 2009;100:266–73.
100. Venderbosch S, Nagtegaal ID, Maughan TS, et al. Mismatch repair status and BRAF mutation status in metastatic colorectal cancer patients: a pooled analysis of the CAIRO, CAIRO2, COIN, and FOCUS studies. Clin Cancer Res 2014;20:5322–30.
101. Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
102. Le DT, Uram JN, Wang H, et al. PD-1 Blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;372:2509–20.
103. Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017;18:1182–91.
104. Daste A, Domblides C, Gross-Goupil M, et al. Immune checkpoint inhibitors and elderly people: A review. Eur J Cancer 2017;82:155–66.
105. Elias R, Giobbie-Hurder A, McCleary NJ, et al. Efficacy of PD-1 & PD-L1 inhibitors in older adults: a meta-analysis. J Immunother Cancer 2018;6:26.
106. Singh H, Kim G, Maher VE, et al. FDA subset analysis of the safety of nivolumab in elderly patients with advanced cancers [abstract]. J Clin Oncol 2016;34(15 suppl):10010-10010.
107. Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol 2017;35:834–41.
108. Brighi N, Balducci L, Biasco G. Cancer in the elderly: is it time for palliative care in geriatric oncology? J Geriatr Oncol 2014;5:197–203.
109. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer 2008;113:3459–66.
110. Bagshaw SM, Stelfox HT, Johnson JA, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43:973–82.
111. Lynch MP, Marcone D, Kagan SH. Developing a multidisciplinary geriatric oncology program in a community cancer center. Clin J Oncol Nurs 2007;11:929–33.
112. Sheridan J, Walsh P, Kevans D, et al. Determinants of short- and long-term survival from colorectal cancer in very elderly patients. J Geriatr Oncol 2014;5:376–83.
1. National Cancer Institute. SEER cancer stat facts: colorectal cancer. http://seer.cancer.gov/statfacts/html/colorect.html. Accessed March 1, 2018.
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:7–30.
3. Kochanek KD, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. NCHS Data Brief 2017:1-8.
4. Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States, current population reports, P25-1140. Washington, DC: U.S. Census Bureau; 2014.
5. Hutchins LF, Unger JM, Crowley JJ, et al. Underrepresentation of patients 65 years of age or older in cancer-treatment trials. N Engl J Med 1999;341:2061–7.
6. Unger JM, Coltman CA Jr, Crowley JJ, et al. Impact of the year 2000 Medicare policy change on older patient enrollment to cancer clinical trials. J Clin Oncol 2006;24:141–4.
7. Vijayvergia N, Li T, Wong YN, et al. Chemotherapy use and adoption of new agents is affected by age and comorbidities in patients with metastatic colorectal cancer. Cancer 2016;122:3191–8.
8. Kalsi T, Babic-Illman G, Ross PJ, et al. The impact of comprehensive geriatric assessment interventions on tolerance to chemotherapy in older people. Br J Cancer 2015;112:1435–44.
9. National Comprehensive Cancer Network. Older adult oncology (Version 2.2017). Accessed March 1, 2018,
10. Balducci L. Frailty: a common pathway in aging and cancer. Interdiscip Top Gerontol 2013;38:61–72.
11. Baijal P, Periyakoil V. Understanding frailty in cancer patients. Cancer J 2014;20:358–66.
12. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–55.
13. Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 2011;29:3457–65.
14. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969;9:179–86.
15. Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist 1970;10:20–30.
16. Klepin HD, Geiger AM, Tooze JA, et al. Physical performance and subsequent disability and survival in older adults with malignancy: results from the health, aging and body composition study. J Am Geriatr Soc 2010;58:76–82.
17. Gupta SK, Lamont EB. Patterns of presentation, diagnosis, and treatment in older patients with colon cancer and comorbid dementia. J Am Geriatr Soc 2004;52:1681–7.
18. Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 1980;69:491–7.
19. Aaldriks AA, van der Geest LG, Giltay EJ, et al. Frailty and malnutrition predictive of mortality risk in older patients with advanced colorectal cancer receiving chemotherapy. J Geriatr Oncol 2013;4:218–26.
20. Martucci RB, Barbosa MV, D’Almeida CA, et al. Undernutrition as independent predictor of early mortality in elderly cancer patients. Nutrition 2017;34:65–70.
21. Naeim A, Aapro M, Subbarao R, Balducci L. Supportive care considerations for older adults with cancer. J Clin Oncol 2014;32:2627–34.
22. Kua J. The prevalence of psychological and psychiatric sequelae of cancer in the elderly - how much do we know? Ann Acad Med Singapore 2005;34:250–6.
23. Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012;118:3377–86.
24. Kim J, Hurria A. Determining chemotherapy tolerance in older patients with cancer. J Natl Compr Canc Netw 2013;11:1494-502.
25. Decoster L, Van Puyvelde K, Mohile S, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations. Ann Oncol 2015;26:288–300.
26. Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PLoS One 2014; 9:e115060.
27. Gurevitch AJ, Davidovitch B, Kashtan H. Outcome of right colectomy for cancer in octogenarians. J Gastrointest Surg 2009;13:100–4.
28. Schiffmann L, Ozcan S, Schwarz F, et al. Colorectal cancer in the elderly: surgical treatment and long-term survival. Int J Colorectal Dis 2008;23:601–10.
29. Ong ES, Alassas M, Dunn KB, Rajput A. Colorectal cancer surgery in the elderly: acceptable morbidity? Am J Surg 2008;195:344–8.
30. Surgery for colorectal cancer in elderly patients: a systematic review. Colorectal Cancer Collaborative Group. Lancet 2000;356:968–74.
31. Shalaby M, Di Lorenzo N, Franceschilli L, et al. Outcome of colorectal surgery in elderly populations. Ann Coloproctol 2016;32:139–43.
32. Frasson M, Braga M, Vignali A, et al. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 2008;51:296–300.
33. PACE participants, Audisio RA, Pope D, et al. Shall we operate? Preoperative assessment in elderly cancer patients (PACE) can help. A SIOG surgical task force prospective study. Crit Rev Oncol Hematol 2008;65:156–63.
34. Adam R, Frilling A, Elias D, et al. Liver resection of colorectal metastases in elderly patients. Br J Surg 2010;97:366–76.
35. de Liguori Carino N, van Leeuwen BL, Ghaneh P, et al. Liver resection for colorectal liver metastases in older patients. Crit Rev Oncol Hematol 2008;67:273–8.
36. Tamandl D, Gruenberger B, Herberger B, et al. Surgery after neoadjuvant chemotherapy for colorectal liver metastases is safe and feasible in elderly patients. J Surg Oncol 2009;100:364–71.
37. Shahir MA, Lemmens VE, van de Poll-Franse LV, et al. Elderly patients with rectal cancer have a higher risk of treatment-related complications and a poorer prognosis than younger patients: a population-based study. Eur J Cancer 2006;42:3015–21.
38. Chang GJ, Skibber JM, Feig BW, Rodriguez-Bigas M. Are we undertreating rectal cancer in the elderly? An epidemiologic study. Ann Surg 2007;246:215–21.
39. Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 2001;358:1291–304.
40. Martling A, Holm T, Johansson H, et al, Stockholm Colorectal Cancer Study Group. The Stockholm II trial on preoperative radiotherapy in rectal carcinoma: long-term follow-up of a population-based study. Cancer 2001;92:896–902.
41. Pasetto LM, Friso ML, Pucciarelli S, et al. Rectal cancer neoadjuvant treatment in elderly patients. Anticancer Res 2006;26:3913–23.
42. Margalit DN, Mamon HJ, Ancukiewicz M, et al. Tolerability of combined modality therapy for rectal cancer in elderly patients aged 75 years and older. Int J Radiat Oncol Biol Phys 2011;81:e735–41.
43. Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2017;2:501–13.
44. van der Valk M. The International Watch & Wait database (IWWD) for rectal cancer: An update. J Clin Oncol 2017;35 suppl:521.
45. Donato V, Valeriani M, Zurlo A. Short course radiation therapy for elderly cancer patients. Evidences from the literature review. Crit Rev Oncol Hematol 2003;45:305–11.
46. Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 2012;30:3827–33.
47. McCleary NJ, Dotan E, Browner I. Refining the chemotherapy approach for older patients with colon cancer. J Clin Oncol 2014;32:2570–80.
48. Millan M, Merino S, Caro A, et al. Treatment of colorectal cancer in the elderly. World J Gastrointest Oncol 2015;7:204–20.
49. Quasar Collaborative Group, Gray R, Barnwell J, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370:2020–9.
50. Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 2009;27:3109–16.
51. Tournigand C, Andre T, Bonnetain F, et al. Adjuvant therapy with fluorouracil and oxaliplatin in stage II and elderly patients (between ages 70 and 75 years) with colon cancer: subgroup analyses of the Multicenter International Study of Oxaliplatin, Fluorouracil, and Leucovorin in the Adjuvant Treatment of Colon Cancer trial. J Clin Oncol 2012;30:3353–60.
52. Winder T, Lenz HJ. Molecular predictive and prognostic markers in colon cancer. Cancer Treat Rev 2010;36:550–6.
53. Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
54. Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
55. Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
56. Aparicio T, Schischmanoff O, Poupardin C, et al. Deficient mismatch repair phenotype is a prognostic factor for colorectal cancer in elderly patients. Dig Liver Dis 2013;45:245–50.
57. Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients. N Engl J Med 2001;345:1091–7.
58. Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
59. Twelves C, Scheithauer W, McKendrick J, et al. Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol 2012;23:1190–7.
60. Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 2011;29:3768–74.
61. Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
62. Haller DG, Cassidy J, Tabernero J, et al. Efficacy findings from a randomized phase III trial of capecitabine plus oxaliplatin versus bolus 5-FU/LV for stage III colon cancer (NO16968): impact of age on disease-free survival (DFS) [abstract]. J Clin Oncol 2010;28:3521.
63. Schmoll HJ, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
64. McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
65. Kahn KL, Adams JL, Weeks JC, et al. Adjuvant chemotherapy use and adverse events among older patients with stage III colon cancer. JAMA 2010;303:1037–45.
66. Haller DG, O’Connell MJ, Cartwright TH, et al. Impact of age and medical comorbidity on adjuvant treatment outcomes for stage III colon cancer: a pooled analysis of individual patient data from four randomized, controlled trials. Ann Oncol 2015;26:715-24.
67. Aparicio T, Francois E, Cristol-Dalstein L, et al. PRODIGE 34-FFCD 1402-ADAGE: Adjuvant chemotherapy in elderly patients with resected stage III colon cancer: A randomized phase 3 trial. Dig Liver Dis 2016;48:206–7.
68. Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
69. Mahoney T, Kuo YH, Topilow A, Davis JM. Stage III colon cancers: why adjuvant chemotherapy is not offered to elderly patients. Arch Surg 2000;135:182–5.
70. Sanoff HK, Carpenter WR, Sturmer T, et al. Effect of adjuvant chemotherapy on survival of patients with stage III colon cancer diagnosed after age 75 years. J Clin Oncol 2012;30:2624–34.
71. Folprecht G, Cunningham D, Ross P, et al. Efficacy of 5-fluorouracil-based chemotherapy in elderly patients with metastatic colorectal cancer: a pooled analysis of clinical trials. Ann Oncol 2004;15:1330–8.
72. Van Cutsem E, Cervantes A, Nordlinger B, Arnold D, ESMO Guidelines Working Group. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25 Suppl 3:iii1–9.
73. Goldberg RM, Tabah-Fisch I, Bleiberg H, et al. Pooled analysis of safety and efficacy of oxaliplatin plus fluorouracil/leucovorin administered bimonthly in elderly patients with colorectal cancer. J Clin Oncol 2006;24:4085–91.
74. Seymour MT, Thompson LC, Wasan HS, et al. Chemotherapy options in elderly and frail patients with metastatic colorectal cancer (MRC FOCUS2): an open-label, randomised factorial trial. Lancet 2011;377:1749–59.
75. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer--a GERCOR study. J Clin Oncol 2006;24:394–400.
76. Figer A, Perez-Staub N, Carola E, et al. FOLFOX in patients aged between 76 and 80 years with metastatic colorectal cancer: an exploratory cohort of the OPTIMOX1 study. Cancer 2007;110:2666–71.
77. Chibaudel B, Maindrault-Goebel F, Lledo G, et al. Can chemotherapy be discontinued in unresectable metastatic colorectal cancer? The GERCOR OPTIMOX2 Study. J Clin Oncol 2009;27:5727–33.
78. Folprecht G, Seymour MT, Saltz L, et al. Irinotecan/fluorouracil combination in first-line therapy of older and younger patients with metastatic colorectal cancer: combined analysis of 2,691 patients in randomized controlled trials. J Clin Oncol 2008;26:1443–51.
79. Souglakos J, Pallis A, Kakolyris S, et al. Combination of irinotecan (CPT-11) plus 5-fluorouracil and leucovorin (FOLFIRI regimen) as first line treatment for elderly patients with metastatic colorectal cancer: a phase II trial. Oncology 2005;69:384–90.
80. Aparicio T, Lavau-Denes S, Phelip JM, et al. Randomized phase III trial in elderly patients comparing LV5FU2 with or without irinotecan for first-line treatment of metastatic colorectal cancer (FFCD 2001-02). Ann Oncol 2016;27:121–7.
81. Aparicio T, Gargot D, Teillet L, et al. Geriatric factors analyses from FFCD 2001-02 phase III study of first-line chemotherapy for elderly metastatic colorectal cancer patients. Eur J Cancer 2017;74:98–108.
82. Kabbinavar FF, Hurwitz HI, Yi J, et al. Addition of bevacizumab to fluorouracil-based first-line treatment of metastatic colorectal cancer: pooled analysis of cohorts of older patients from two randomized clinical trials. J Clin Oncol 2009;27:199–205.
83. Cassidy J, Saltz LB, Giantonio BJ, et al. Effect of bevacizumab in older patients with metastatic colorectal cancer: pooled analysis of four randomized studies. J Cancer Res Clin Oncol 2010;136:737–43.
84. Van Cutsem E, Rivera F, Berry S, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol 2009;20:1842–7.
85. Kozloff MF, Berlin J, Flynn PJ, et al. Clinical outcomes in elderly patients with metastatic colorectal cancer receiving bevacizumab and chemotherapy: results from the BRiTE observational cohort study. Oncology 2010;78:329–39.
86. Cunningham D, Lang I, Marcuello E, et al. Bevacizumab plus capecitabine versus capecitabine alone in elderly patients with previously untreated metastatic colorectal cancer (AVEX): an open-label, randomised phase 3 trial. Lancet Oncol 2013;14:1077–85.
87. Aparicio T, Bouche O, Taieb J, et al. Bevacizumab+chemotherapy versus chemotherapy alone in elderly patients with untreated metastatic colorectal cancer: a randomized phase II trial-PRODIGE 20 study results. Ann Oncol 2018;29:133–8.
88. Van Cutsem E, Tabernero J, Lakomy R, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol 2012;30:3499–506.
89. Ruff P, Van Cutsem E, Lakomy R, et al. Observed benefit and safety of aflibercept in elderly patients with metastatic colorectal cancer: An age-based analysis from the randomized placebo-controlled phase III VELOUR trial. J Geriatr Oncol 2018;9:32–9.
90. Obermannova R, Van Cutsem E, Yoshino T, et al. Subgroup analysis in RAISE: a randomized, double-blind phase III study of irinotecan, folinic acid, and 5-fluorouracil (FOLFIRI) plus ramucirumab or placebo in patients with metastatic colorectal carcinoma progression. Ann Oncol 2016;27:2082–90.
91. Bouchahda M, Macarulla T, Spano JP, et al. Cetuximab efficacy and safety in a retrospective cohort of elderly patients with heavily pretreated metastatic colorectal cancer. Crit Rev Oncol Hematol 2008;67:255-62.
92. Douillard JY, Siena S, Cassidy J, et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol 2014;25:1346–55.
93. Sastre J, Gravalos C, Rivera F, et al. First-line cetuximab plus capecitabine in elderly patients with advanced colorectal cancer: clinical outcome and subgroup analysis according to KRAS status from a Spanish TTD Group Study. Oncologist 2012;17:339–45.
94. Dotan E, Devarajan K, D’Silva AJ, et al. Patterns of use and tolerance of anti-epidermal growth factor receptor antibodies in older adults with metastatic colorectal cancer. Clin Colorectal Cancer 2014;13:192–8.
95. Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381:303–12.
96. Van Cutsem E, Sobrero A, Siena S, et al. Regorafenib (REG) in progressive metastatic colorectal cancer (mCRC): Analysis of age subgroups in the phase III CORRECT trial [abstract]. J Clin Oncol 2013;31(15 suppl):3636-3636.
97. Bekaii-Saab TS, Ou FS, Anderson DM, et al. Regorafenib dose optimization study (ReDOS): Randomized phase II trial to evaluate dosing strategies for regorafenib in refractory metastatic colorectal cancer (mCRC): an ACCRU Network study [abstract]. J Clin Oncol 2018;36(4 suppl):611-611.
98. Mayer RJ, Van Cutsem E, Falcone A, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med 2015;372:1909–19.
99. Koopman M, Kortman GA, Mekenkamp L, et al. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br J Cancer 2009;100:266–73.
100. Venderbosch S, Nagtegaal ID, Maughan TS, et al. Mismatch repair status and BRAF mutation status in metastatic colorectal cancer patients: a pooled analysis of the CAIRO, CAIRO2, COIN, and FOCUS studies. Clin Cancer Res 2014;20:5322–30.
101. Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
102. Le DT, Uram JN, Wang H, et al. PD-1 Blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015;372:2509–20.
103. Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017;18:1182–91.
104. Daste A, Domblides C, Gross-Goupil M, et al. Immune checkpoint inhibitors and elderly people: A review. Eur J Cancer 2017;82:155–66.
105. Elias R, Giobbie-Hurder A, McCleary NJ, et al. Efficacy of PD-1 & PD-L1 inhibitors in older adults: a meta-analysis. J Immunother Cancer 2018;6:26.
106. Singh H, Kim G, Maher VE, et al. FDA subset analysis of the safety of nivolumab in elderly patients with advanced cancers [abstract]. J Clin Oncol 2016;34(15 suppl):10010-10010.
107. Temel JS, Greer JA, El-Jawahri A, et al. Effects of early integrated palliative care in patients with lung and GI cancer: a randomized clinical trial. J Clin Oncol 2017;35:834–41.
108. Brighi N, Balducci L, Biasco G. Cancer in the elderly: is it time for palliative care in geriatric oncology? J Geriatr Oncol 2014;5:197–203.
109. Meropol NJ, Egleston BL, Buzaglo JS, et al. Cancer patient preferences for quality and length of life. Cancer 2008;113:3459–66.
110. Bagshaw SM, Stelfox HT, Johnson JA, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43:973–82.
111. Lynch MP, Marcone D, Kagan SH. Developing a multidisciplinary geriatric oncology program in a community cancer center. Clin J Oncol Nurs 2007;11:929–33.
112. Sheridan J, Walsh P, Kevans D, et al. Determinants of short- and long-term survival from colorectal cancer in very elderly patients. J Geriatr Oncol 2014;5:376–83.
Adjuvant Chemotherapy in the Treatment of Colon Cancer
INTRODUCTION
Colorectal cancer (CRC) is one of the most prevalent malignancies and is the fourth most common cancer in the United States, with an estimated 133,490 new cases diagnosed in 2016. Of these, approximately 95,520 are located in the colon and 39,970 are in the rectum.1 CRC is the third leading cause of cancer death in women and the second leading cause of cancer death in men, with an estimated 49,190 total deaths in 2016.2 The incidence appears to be increasing,3 especially in patients younger than 55 years of age;4 the reason for this increase remains uncertain.
A number of risk factors for the development of CRC have been identified. Numerous hered-itary CRC syndromes have been described, including familial adenomatous polyposis,5 hereditary non-polyposis colorectal cancer (HNPCC) or Lynch syndrome,6 and MUTYH-associated polyposis.7,8 A family history of CRC doubles the risk of developing CRC,9 and current guidelines support lowering the age of screening in individuals with a family history of CRC to 10 years younger than the age of diagnosis of the family member or 40 years of age, whichever is lower.10 Patients with a personal history of adenomatous polyps are at increased risk for developing CRC, as are patients with a personal history of CRC, with a relative risk ranging from 3 to 6.11 Ulcerative colitis and Crohn’s disease are associated with the development of CRC and also influence screening, though evidence suggests good control of these diseases may mitigate risk.12 Finally, modifiable risk factors for the development of CRC include high red meat consumption,13 diets low in fiber,14 obesity,13 smoking, alcohol use,15 and physical inactivity16; lifestyle modification targeting these factors has been shown to decrease rates of CRC.17 The majority of colon cancers present with clinical symptoms, often with rectal bleeding, abdominal pain, change in bowel habits, or obstructive symptoms. More rarely, these tumors are detected during screening colonoscopy, in which case they tend to be at an early stage.
SURGICAL MANAGEMENT
A critical goal in the resection of early-stage colon cancer is attaining R0 resection. Patients who achieve R0 resection as compared to R1 (microscopic residual tumor) and R2 (macroscopic residual tumor)18 have significantly improved long-term overall survival.19 Traditionally, open resection of the involved colonic segment was employed, with end-end anastomosis of the uninvolved free margins. Laparoscopic resection for early-stage disease has been utilized in attempts to decrease morbidity of open procedures, with similar outcomes and node sampling.20 Laparoscopic resection appears to provide similar outcomes even in locally advanced disease.21 Right-sided lesions are treated with right colectomy and primary ileocolic anastomosis.22 For patients presenting with obstructing masses, the Hartmann procedure is the most commonly performed operation. This involves creation of an ostomy with subtotal colectomy and subsequent ostomy reversal in a 2- or 3-stage protocol.23 Patients with locally advanced disease and invasion into surrounding structures require multivisceral resection, which involves resection en bloc with secondarily involved organs.24 Intestinal perforation presents a unique challenge and is associated with surgical complications, infection, and lower overall survival (OS) and 5-year disease-free survival (DFS). Complete mesocolic excision is a newer technique that has been performed with reports of better oncologic outcome at some centers; however, this approach is not currently considered standard of care.25
STAGING
According to a report by the National Cancer Institute, the estimated 5-year relative survival rates for localized colon cancer (lymph node negative), regional (lymph node positive) disease, and distant (metastatic) disease are 89.9%, 71.3%, and 13.9%, respectively.1 However, efforts have been made to further classify patients into distinct categories to allow fine-tuning of prognostication. In the current system, staging of colon cancer utilizes the American Joint Committee on Cancer tumor/node/metastasis (TNM) system.20 Clinical and pathologic features include depth of invasion, local invasion of other organs, nodal involvement, and presence of distant metastasis (Table 1). Studies completed prior to the adoption of the TNM system used the Dukes criteria, which divided colon cancer into A, B, and C, corresponding to TNM stage I, stage IIA–IIC, and stage IIIA-IIIC. This classification is rarely used in more contemporary studies.
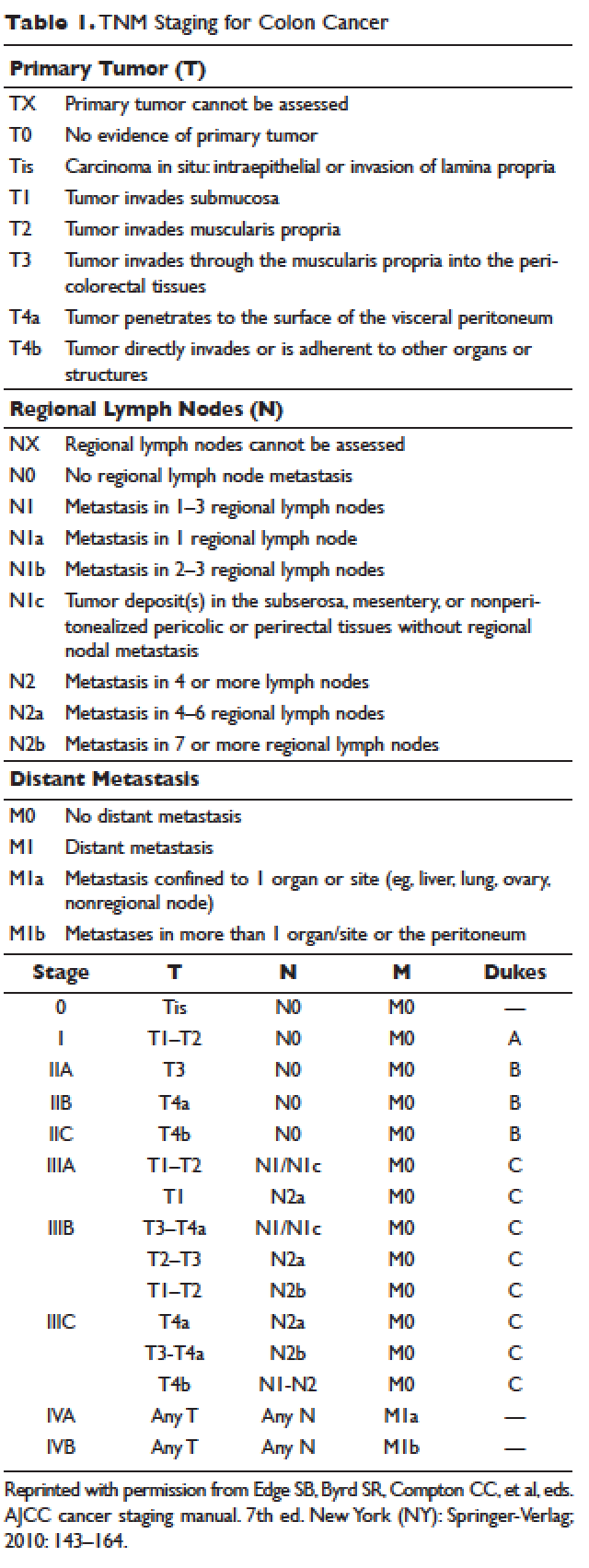
APPROACH TO ADJUVANT CHEMOTHERAPY
Adjuvant chemotherapy seeks to eliminate micrometastatic disease present following curative surgical resection. When stage 0 cancer is discovered incidentally during colonoscopy, endoscopic resection alone is the management of choice, as presence of micrometastatic disease is exceedingly unlikely.26 Stage I–III CRCs are treated with surgical resection withcurative intent. The 5-year survival rate for stage I and early-stage II CRC is estimated at 97% with surgery alone.27,28 The survival rate drops to about 60% for high-risk stage II tumors (T4aN0), and down to 50% or less for stage II-T4N0 or stage III cancers. Adjuvant chemotherapy is generally recommended to further decrease the rates of distant recurrence in certain cases of stage II and in all stage III tumors.
DETERMINATION OF BENEFIT FROM CHEMOTHERAPY: PROGNOSTIC MARKERS
Prior to administration of adjuvant chemotherapy, a clinical evaluation by the medical oncologist to determine appropriateness and safety of treatment is paramount. Poor performance status and comorbid conditions may indicate risk for excessive toxicity and minimal benefit from chemotherapy. CRC commonly presents in older individuals, with the median age at diagnosis of 69 years for men and 73 years for women.29 In this patient population, comorbidities such as cardiovascular disease, diabetes, and renal dysfunction are more prevalent.30 Decisions regarding adjuvant chemotherapy in this patient population have to take into consideration the fact that older patients may experience higher rates of toxicity with chemotherapy, including gastrointestinal toxicities and marrow suppression.31 Though some reports indicate patients older than 70 years derive similar benefit from adjuvant chemotherapy,32,33 a large pooled analysis of the ACCENT database, which included 7 adjuvant therapy trials and 14,528 patients, suggested limited benefit from the addition of oxaliplatin to fluorouracil in elderly patients.32 Other factors that weigh on the decision include stage, pathology, and presence of high-risk features. A common concern in the postoperative setting is delaying initiation of chemotherapy to allow adequate wound healing; however, evidence suggests that delays longer than 8 weeks leads to worse overall survival, with hazard ratios (HR) ranging from 1.4 to 1.7.34,35 Thus, the start of adjuvant therapy should ideally be within this time frame.
HIGH-RISK FEATURES
Multiple factors have been found to predict worse outcome and are classified as high-risk features (Table 2). Histologically, high-grade or poorly differentiated tumors are associated with higher recurrence rate and worse outcome.36 Certain histological subtypes, including mucinous and signet-ring, both appear to have more aggressive biology.37 Presence of microscopic invasion into surrounding blood vessels (vascular invasion) and nerves (perineural invasion) is associated with lower survival.38 Penetration of the cancer through the visceral peritoneum (T4a) or into surrounding structures (T4b) is associated with lower survival.36 During surgical resection, multiple lymph nodes are removed along with the primary tumor to evaluate for metastasis to the regional nodes. Multiple analyses have demonstrated that removal and pathologic assessment of fewer than 12 lymph nodes is associated with high risk of missing a positive node, and is thus equated with high risk.39–41 In addition, extension of tumor beyond the capsules of any single lymph node, termed extracapsular extension, is associated with an increased risk of all-cause mortality.42 Tumor deposits, or focal aggregates of adenocarcinoma in the pericolic fat that are not contiguous with the primary tumor and are not associated with lymph nodes, are currently classified as lymph nodes as N1c in the current TNM staging system. Presence of these deposits has been found to predict poor outcome stage for stage.43 Obstruction and/or perforation secondary to the tumor are also considered high-risk features that predict poor outcome.

SIDEDNESS
As reported at the 2016 American Society of Clinical Oncology annual meeting, tumor location predicts outcome in the metastatic setting. A report by Venook and colleagues based on a post-hoc analysis found that in the metastatic setting, location of the tumor primary in the left side is associated with longer OS (33.3 months) when compared to the right side of the colon (19.4 months).44 A retrospective analysis of multiple databases presented by Schrag and colleagues similarly reported inferior outcomes in patients with stage III and IV disease who had right-sided primary tumors.45 However, the prognostic implications for stage II disease remain uncertain.
BIOMARKERS
Given the controversy regarding adjuvant therapy of patients with stage II colon cancer, multiple biomarkers have been evaluated as possible predictive markers that can assist in this decision. The mismatch repair (MMR) system is a complex cellular enzymatic mechanism that identifies and corrects DNA errors during cell division and prevents mutagenesis.46 The familial cancer syndrome HNPCC is linked to alteration in a variety of MMR genes, leading to deficient mismatch repair (dMMR), also termed microsatellite instability-high (MSI-high).47,48 Epigenetic modification can also lead to silencing of the same implicated genes and accounts for 15% to 20% of sporadic colorectal cancer.49 These epigenetic modifications lead to hypermethylation of the promotor region of MLH1 in 70% of cases.50 The 4 MMR genes most commonly tested are MLH-1, MSH2, MSH6, and PMS2. Testing can be performed by immunohistochemistry or polymerase chain reaction.51 Across tumor histology and stage, MSI status is prognostic. Patients with MSI-high tumors have been shown to have improved prognosis and longer OS both in stage II and III disease52–54 and in the metastatic setting.55 However, despite this survival benefit, there is conflicting data as to whether patients with stage II, MSI-high colon cancer may benefit less from adjuvant chemotherapy. One early retrospective study compared outcomes of 70 patients with stage II and III disease and dMMR to those of 387 patients with stage II and III disease and proficient mismatch repair (pMMR). Adjuvant fluorouracil with leucovorin improved DFS for patients with pMMR (HR 0.67) but not for those with dMMR (HR 1.10). In addition, for patients with stage II disease and dMMR, the HR for OS was inferior at 2.95.56 Data collected from randomized clinical trials using fluorouracil-based adjuvant chemotherapy were analyzed in an attempt to predict benefit based on MSI status. Benefit was only seen in pMMR patients, with a HR of 0.72; this was not seen in the dMMR patients.57 Subsequent studies have had different findings and did not demonstrate a detrimental effect of fluorouracil in dMMR.58,59 For stage III patients, MSI status does not appear to affect benefit from chemotherapy, as analysis of data from the NSABP C-07 trial (Table 3) demonstrated benefit of FOLFOX (leucovorin, fluorouracil, oxaliplatin) in patients with dMMR status and stage III disease.59
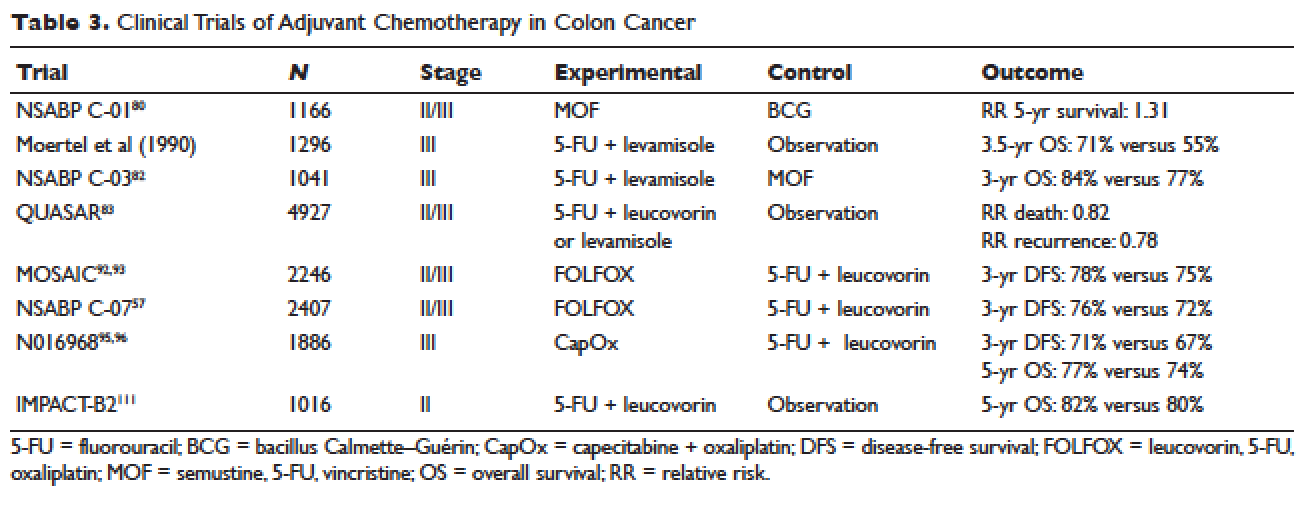
Another genetic abnormality identified in colon cancers is chromosome 18q loss of heterozygosity (LOH). The presence of 18q LOH appears to be inversely associated with MSI-high status. Some reports have linked presence of 18q with worse outcome,60 but others question this, arguing the finding may simply be related to MSI status.61,62 This biomarker has not been established as a clear prognostic marker that can aid clinical decisions.
Most recently, expression of caudal-type homeobox transcription factor 2 (CDX2) has been reported as a novel prognostic and predictive tool. A 2015 report linked lack of expression of CDX2 to worse outcome; in this study, 5-year DFS was 41% in patients with CDX2-negative tumors versus 74% in the CDX2-positive tumors, with a HR of disease recurrence of 2.73 for CDX2-negative tumors.63 Similar numbers were observed in patients with stage II disease, with 5-year OS of 40% in patients with CDX2-negative tumors versus 70% in those with CDX2-positive tumors. Treatment of CDX2-negative patients with adjuvant chemotherapy improved outcomes: 5-year DFS in the stage II subgroup was 91% with chemotherapy versus 56% without, and in the stage III subgroup, 74% with chemotherapy versus 37% without. The authors concluded that patients with stage II and III colon cancer that is CDX2-negative may benefit from adjuvant chemotherapy. Importantly, CDX2-negativity is a rare event, occurring in only 6.9% of evaluable tumors.
RISK ASSESSMENT TOOLS
Several risk assessment tools have been developed in an attempt to aid clinical decision making regarding adjuvant chemotherapy for patients with stage II colon cancer. The Oncotype DX Colon Assay analyses a 12-gene signature in the pathologic sample and was developed with the goal to improve prognostication and aid in treatment decision making. The test utilizes reverse transcription-PCR on RNA extracted from the tumor.64 After evaluating 12 genes, a recurrence score is generated that predicts the risk of disease recurrence. This score was validated using data from 3 large clinical trials.65–67 Unlike the Oncotype Dx score used in breast cancer, the test in colon cancer has not been found to predict the benefit from chemotherapy and has not been incorporated widely into clinical practice.
Adjuvant! Online (available at www.adjuvantonline.com) is a web-based tool that combines clinical and histological features to estimate outcome. Calculations are based on US SEER tumor registry-reported outcomes.68 A second web-based tool, Numeracy (available at www.mayoclinic.com/calcs), was developed by the Mayo Clinic using pooled data from 7 randomized clinical trials including 3341 patients.68 Both tools seek to predict absolute benefit for patients treated with fluorouracil, though data suggests Adjuvant! Online may be more reliable in its predictive ability.69 Adjuvant! Online has also been validated in an Asian population70 and patients older than 70 years.71
MUTATIONAL ANALYSIS
Multiple mutations in proto-oncogenes have been found in colon cancer cells. One such proto-oncogene is BRAF, which encodes a serine-threonine kinase in the rapidly accelerated fibrosarcoma (RAF). Mutations in BRAF have been found in 5% to 10% of colon cancers and are associated with right-sided tumors.72 As a prognostic marker, some studies have associated BRAF mutations with worse prognosis, including shorter time to relapse and shorter OS.73,74 Two other proto-oncogenes are Kristen rat sarcoma viral oncogene homolog (KRAS) and neuroblastoma rat sarcoma viral oncogene homolog (NRAS), both of which encode proteins downstream of epidermal growth factor receptor (EGFR). KRAS and NRAS mutations have been shown to be predictive in the metastatic setting where they predict resistance to the EGFR inhibitors cetuximab and panitumumab.75,76 The effect of KRAS and NRAS mutations on outcome in stage II and III colon cancer is uncertain. Some studies suggest worse outcome in KRAS-mutated cancers,77 while others failed to demonstrate this finding.73
CASE PRESENTATION 1
A 53-year-old man with no past medical history presents to the emergency department with early satiety and generalized abdominal pain. Laboratory evaluation shows a microcytic anemia with normal white blood cell count, platelet count, renal function, and liver function tests. Computed tomography (CT) scan of the abdomen and pelvis show a 4-cm mass in the transverse colon without obstruction and without abnormality in the liver. CT scan of the chest does not demonstrate pathologic lymphadenopathy or other findings. He undergoes robotic laparoscopic transverse colon resection and appendectomy. Pathology confirms a 3.5-cm focus of adenocarcinoma of the colon with invasion through the muscularis propria and 5 of 27 regional lymph nodes positive for adenocarcinoma and uninvolved proximal, distal, and radial margins. He is given a stage of IIIB pT3 pN2a M0 and referred to medical oncology for further management, where 6 months of adjuvant FOLFOX chemotherapy is recommended.
ADJUVANT CHEMOTHERAPY IN STAGE III COLON CANCER
Postoperative adjuvant chemotherapy is the standard of care for patients with stage III disease. In the 1960s, infusional fluorouracil was first used to treat inoperable colon cancer.78,79 After encouraging results, the agent was used both intraluminally and intravenously as an adjuvant therapy for patients undergoing resection with curative intent; however, only modest benefits were described.80,81 The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-01 trial (Table 3) was the first study to demonstrate a benefit from adjuvant chemotherapy in colon cancer. This study randomly assigned patients with stage II and III colon cancer to surgery alone, postoperative chemotherapy with fluorouracil, semustine, and vincristine (MOF), or postoperative bacillus Calmette-Guérin (BCG). DFS and OS were significantly improved with MOF chemotherapy.82 In 1990, a landmark study reported on outcomes after treatment of 1296 patients with stage III colon cancer with adjuvant fluorouracil and levamisole for 12 months. The combination was associated with a 41% reduction in risk of cancer recurrence and a 33% reduction in risk of death.83 The NSABP C-03 trial (Table 3) compared MOF to the combination of fluorouracil and leucovorin and demonstrated improved 3-year DFS (69% versus 73%) and 3-year OS (77% versus 84%) in patients with stage III disease.84 Building on these outcomes, the QUASAR study (Table 3) compared fluorouracil in combination with one of levamisole, low-dose leucovorin, or high-dose leucovorin. The study enrolled 4927 patients and found worse outcomes with fluorouracil plus levamisole and no difference in low-doseversus high-dose leucovorin.85 Levamisole fell out of use after associations with development of multifocal leukoencephalopathy,86 and was later shown to have inferior outcomes versus leucovorin when combined with fluorouracil.87,88 Intravenous fluorouracil has shown similar benefit when administered by bolus or infusion,89 although continuous infusion has been associated with lower incidence of severe toxicity.90 The efficacy of the oral fluoropyrimidine capecitabine has been shown to be equivalent to that of fluorouracil.91
Fluorouracil-based treatment remained the standard of care until the introduction of oxaliplatin in the mid-1990s. After encouraging results in the metastatic setting,92,93 the agent was moved to the adjuvant setting. The MOSAIC trial (Table 3) randomly assigned patients with stage II and III colon cancer to fluorouracil with leucovorin (FULV) versus FOLFOX given once every 2 weeks for 12 cycles. Analysis with respect to stage III patients showed a clear survival benefit, with a 10-year OS of 67.1% with FOLFOX chemotherapy versus 59% with fluorouracil and leucovorin.94,95 The NSABP C-07 (Table 3) trial used a similar trial design but employed bolus fluorouracil. More than 2400 patients with stage II and III colon cancer were randomly assigned to bolus FULV or bolus fluorouracil, leucovorin, and oxaliplatin (FLOX). The addition of oxaliplatin significantly improved outcomes, with 4-year DFS of 67% versus 71.8% for FULV and FLOX, respectively, and a HR of death of 0.80 with FLOX.59,96 The multicenter N016968 trial (Table 3) randomly assigned 1886 patients with stage III colon cancer to adjuvant capecitabine plus oxaliplatin (XELOX) or bolus fluorouracil plus leucovorin (FU/FA). The 3-year DFS was 70.9% versus 66.5% with XELOX and FU/FA, respectively, and 5-year OS was 77.6% versus 74.2%, respectively.97,98
In the metastatic setting, additional agents have shown efficacy, including irinotecan,99,100 bevacizumab,101,102 cetuximab,103,104 and regorafenib.105 This observation led to testing of these agents in earlier stage disease. The CALGB 89803 trial compared fluorouracil, leucovorin, and irinotecan to fluorouracil with leucovorin alone. No benefit in 5-year DFS or OS was seen.106 Similarly, infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) was not found to improve 5-year DFS as compared to fluorouracil with leucovorin alone in the PETACC-3 trial.107 The NSABP C-08 trial considered the addition of bevacizumab to FOLFOX. When compared to FOLFOX alone, the combination of bevacizumab to FOLFOX had similar 3-year DFS (77.9% versus 75.1%) and 5-year OS (82.5% versus 80.7%).108 This finding was confirmed in the Avant trial.109 The addition of cetuximab to FOLFOX was equally disappointing, as shown in the N0147 trial110 and PETACC-8 trial.111 Data on regorafenib in the adjuvant setting for stage III colon cancer is lacking; however, 2 ongoing clinical trials, NCT02425683 and NCT02664077, are each studying the use of regorafenib following completion of FOLFOX for patients with stage III disease.
Thus, after multiple trials comparing various regimens and despite attempts to improve outcomes by the addition of a third agent, the standard of care per National Comprehensive Cancer Network (NCCN) guidelines for management of stage III colon cancer remains 12 cycles of FOLFOX chemotherapy. Therapy should be initiated within 8 weeks of surgery. Data are emerging to support a short duration of therapy for patients with low-risk stage III tumors, as shown in an abstract presented at the 2017 American Society of Clinical Oncology annual meeting. The IDEA trial was a pooled analysis of 6 randomized clinical trials across multiple countries, all of which evaluated 3 versus 6 months of FOLFOX or capecitabine and oxaliplatin in the treatment of stage III colon cancer. The analysis was designed to test non-inferiority of 3 months of therapy as compared to 6 months. The analysis included 6088 patients across 244 centers in 6 countries. The overall analysis failed to establish noninferiority. The 3-year DFS rate was 74.6% for 3 months and 75.5% for 6 months, with a DFS HR of 1.07 and a confidence interval that did not meet the prespecified endpoint. Subgroup analysis suggested noninferiority for lower stage disease (T1–3 or N1) but not for higher stage disease (T4 or N2). Given the high rates of neuropathy with 6 months of oxaliplatin, these results suggest that 3 months of adjuvant therapy can be considered for patients with T1–3 or N1 disease in an attempt to limit toxicity.112
CASE PRESENTATION 2
A 57-year-old woman presents to the emergency department with fever and abdominal pain. CT of the abdomen and pelvis demonstrates a left-sided colonic mass with surrounding fat stranding and pelvic abscess. She is taken emergently for left hemicolectomy, cholecystectomy, and evacuation of pelvic abscess. Pathology reveals a 5-cm adenocarcinoma with invasion through the visceral peritoneum; 0/22 lymph nodes are involved. She is given a diagnosis of stage IIC and referred to medical oncology for further management. Due to her young age and presence of high-risk features, she is recommended adjuvant therapy with FOLFOX for 6 months.
ADJUVANT CHEMOTHERAPY IN STAGE II COLON CANCER
Because of excellent outcomes with surgical resection alone for stage II cancers, the use of adjuvant chemotherapy for patients with stage II disease is controversial. Limited prospective data is available to guide adjuvant treatment decisions for stage II patients. The QUASAR trial, which compared observation to adjuvant fluorouracil and leucovorin in patients with early-stage colon cancer, included 2963 patients with stage II disease and found a relative risk (RR) of death or recurrence of 0.82 and 0.78, respectively. Importantly, the absolute benefit of therapy was less than 5%.113 The IMPACT-B2 trial (Table 3) combined data from 5 separate trials and analyzed 1016 patients with stage II colon cancer who received fluorouracil with leucovorin or observation. Event-free survival was 0.86 versus 0.83 and 5-year OS was 82% versus 80%, suggesting no benefit.114 The benefit of addition of oxaliplatin to fluorouracil in stage II disease appears to be less than the benefit of adding this agent in the treatment of stage III CRC. As noted above, the MOSAIC trial randomly assigned patients with stage II and III colon cancer to receive adjuvant fluorouracil and leucovorin with or without oxaliplatin for 12 cycles. After a median follow-up of 9.5 years, 10-year OS rates for patients with stage II disease were 78.4% versus 79.5%. For patients with high-risk stage II disease (defined as T4, bowel perforation, or fewer than 10 lymph nodes examined), 10-year OS was 71.7% and 75.4% respectively, but these differences were not statistically significant.94
Because of conflicting data as to the benefit of adding oxaliplatin in stage II disease, oxaliplatin is not recommended for standard-risk stage II patients. The use of oxaliplatin in high-risk stage II tumors should be weighed carefully given the toxicity risk. Oxaliplatin is recognized to cause sensory neuropathy in many patients, which can become painful and debilitating.115 Two types of neuropathy are associated with oxaliplatin: acute and chronic. Acute neuropathy manifests most often as cold-induced paresthesias in the fingers and toes and is quite common, affecting up to 90% of patients. These symptoms are self-limited and resolve usually within 1 week of each treatment.116 Some patients, with reports ranging from 10% to 79%, develop chronic neuropathy that persists for 1 year or more and causes significant decrements in quality of life.117 Patients older than age 70 may be at greater risk for oxaliplatin-induced neuropathy, which would increase risk of falls in this population.118 In addition to neuropathy, oxaliplatin is associated with hypersensitivity reactions that can be severe and even fatal.119 In a single institution series, the incidence of severe reactions was 2%.120 Desensitization following hypersensitivity reactions is possible but requires a time-intensive protocol.121
Based on the inconclusive efficacy findings and due to concerns over toxicity, each decision must be individualized to fit patient characteristics and preferences. In general, for patients with stage II disease without high-risk features, an individualized discussion should be held as to the risks and benefits of single-agent fluorouracil, and this treatment should be offered in cases where the patient or provider would like to be aggressive. Patients with stage II cancer who have 1 or more high-risk features are often recommended adjuvant chemotherapy. Whether treatment with fluorouracil plus leucovorin or FOLFOX is preferred remains uncertain, and thus the risks and the potential gains of oxaliplatin must be discussed with the individual patient. MMR status can also influence the treatment recommendation for patients with stage II disease. In general, patients with standard-risk stage II tumors that are pMMR are offered MMR with leucovorin or oral capecitabine for 12 cycles. FOLFOX is considered for patients with MSI-high disease and those with multiple high-risk features.
MONITORING AFTER THERAPY
After completion of adjuvant chemotherapy, patients enter a period of survivorship. Patients are seen in clinic for symptom and laboratory monitoring of the complete blood count, liver function tests, and carcinoembryonic antigen (CEA). NCCN guidelines support history and physical examination with CEA testing every 3 to 6 months for the first 2 years, then every 6 months for the next 3 years, after which many patients continue to be seen annually. CT imaging of the chest, abdomen, and pelvis for monitoring of disease recurrence is recommended every 6 to 12 months for a total of 5 years. New elevations in CEA or liver function tests should prompt early imaging. Colonoscopy should be performed 1 year after completion of therapy; however, if no preoperative colonoscopy was performed, this should be done 3 to 6 months after completion. Colonoscopy is then repeated in 3 years and then every 5 years unless advanced adenomas are present.122
SUMMARY
The addition of chemotherapy to surgical management of colon cancer has lowered the rate of disease recurrence and improved long-term survival. Adjuvant FOLFOX for 12 cycles is the standard of care for patients with stage III colon cancer and for patients with stage II disease with certain high-risk features. Use of adjuvant chemotherapy in stage II disease without high-risk features is controversial, and treatment decisions should be individualized. Biologic markers such as MSI and CDX2 status as well as patient-related factors including age, overall health, and personal preferences can inform treatment decisions. If chemotherapy is recommended in this setting, it would be with single-agent fluorouracil in an infusional or oral formulation, unless the tumor has the MSI-high feature. Following completion of adjuvant therapy, patients should be followed with clinical evaluation, laboratory testing, and imaging for a total of 5 years as per recommended guidelines.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67(1):7–30.
- United States Cancer Statistics. 1999–2013 incidence and mortality web-based report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2016. www.cdc.gov/uscs. Accessed June 12, 2017.
- Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc 2014;89:216–24.
- Jemal A, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst 2017;109(8).
- Boursi B, Sella T, Liberman E, et al. The APC p.I1307K polymorphism is a significant risk factor for CRC in average risk Ashkenazi Jews. Eur J Cancer 2013;49:3680–5.
- Parry S, Win AK, Parry B, et al. Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 2011;60: 950–7.
- van Puijenbroek M, Nielsen M, Tops CM, et al. Identification of patients with (atypical) MUTYH-associated polyposis by KRAS2 c.34G > T prescreening followed by MUTYH hotspot analysis in formalin-fixed paraffin-embedded tissue. Clin Cancer Res 2008;14:139–42.
- Aretz S, Uhlhaas S, Goergens H, et al. MUTYH-associated polyposis: 70 of 71 patients with biallelic mutations present with an attenuated or atypical phenotype. Int J Cancer 2006;119:807–14.
- Tuohy TM, Rowe KG, Mineau GP, et al. Risk of colorectal cancer and adenomas in the families of patients with adenomas: a population-based study in Utah. Cancer 2014;120:35–42.
- Choi Y, Sateia HF, Peairs KS, Stewart RW. Screening for colorectal cancer. Semin Oncol 2017; 44:34–44.
- Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med 1992;326:658–62.
- Rutter MD. Surveillance programmes for neoplasia in colitis. J Gastroenterol 2011;46 Suppl 1:1–5.
- Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am 2002;31:925–43.
- Michels KB, Fuchs GS, Giovannucci E, et al. Fiber intake and incidence of colorectal cancer among 76,947 women and 47,279 men. Cancer Epidemiol Biomarkers Prev 2005;14:842–9.
- Omata F, Brown WR, Tokuda Y, et al. Modifiable risk factors for colorectal neoplasms and hyperplastic polyps. Intern Med 2009;48:123–8.
- Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer 2010;46:2593–604.
- Aleksandrova K, Pischon T, Jenab M, et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med 2014;12:168.
- Hermanek P, Wittekind C. The pathologist and the residual tumor (R) classification. Pathol Res Pract 1994;190:115–23.
- Lehnert T, Methner M, Pollok A, et al. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg 2002;235:217–25.
- Feinberg AE, et al. Oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis. Dis Colon Rectum 2017;60:116–125.
- Vignali A, et al. Laparoscopic treatment of advanced colonic cancer: a case-matched control with open surgery. Colorectal Dis 2013;15:944–8.
- Gainant A. Emergency management of acute colonic cancer obstruction. J Visc Surg 2012;149: e3–e10.
- Rosenman LD. Hartmann’s operation. Am J Surg 1994;168:283–4.
- Lee-Kong S, Lisle D. Surgical management of complicated colon cancer. Clin Colon Rectal Surg 2015;28:228–33.
- Bertelsen CA. Complete mesocolic excision an assessment of feasibility and outcome. Dan Med J 2017;64(2).
- Wolff WI SH. Definitive treatment of “malignant” polyps of the colon. Ann Surg 1975;182:516–25.
- Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–9.
- Gunderson LL, Jessup JM, Sarjent DJ, et al. Revised tumor and node categorization for rectal cancer based on surveillance, epidemiology, and end results and rectal pooled analysis outcomes. J Clin Oncol 2010;28:256–63.
- Noone AM, Cronin KA, Altekruse SF, et al. Cancer incidence and survival trends by subtype using data from the Surveillance Epidemiology and End Results Program, 1992-2013. Cancer Epidemiol Biomarkers Prev 2017;26:632–41.
- Alves A, Panis Y, Mathieu P, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg 2005;140:278–83.
- Popescu RA, Norman A, Ross PJ, et al, Adjuvant or palliative chemotherapy for colorectal cancer in patients 70 years or older. J Clin Oncol 1999;17:2412–8.
- McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
- Tominaga T, Nonaka T, Sumida Y, et al. Effectiveness of adjuvant chemotherapy for elderly patients with lymph node-positive colorectal cancer. World J Surg Oncol 2016;14:197.
- Bos AC, van Erning FN, van Gestel YR, et al. Timing of adjuvant chemotherapy and its relation to survival among patients with stage III colon cancer. Eur J Cancer 2015;51:2553–61.
- Peixoto RD, Kumar A, Speers C, et al. Effect of delay in adjuvant oxaliplatin-based chemotherapy for stage III colon cancer. Clin Colorectal Cancer 2015;14:25–30.
- Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:979–94.
- Lieu CH, Lambert LA, Wolff RA, et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol 2012;23:652–8.
- Krasna MJ, Flancbaum L, Cody RP, et al. Vascular and neural invasion in colorectal carcinoma. Incidence and prognostic significance. Cancer 1988;61:1018–23.
- Cianchi F, Palomba A, Boddi V, et al. Lymph node recovery from colorectal tumor specimens: recommendation for a minimum number of lymph nodes to be examined. World J Surg 2002;26:384–9.
- Yoshimatsu K, et al. How many lymph nodes should be examined in Dukes’ B colorectal cancer? Determination on the basis of cumulative survival rate. Hepatogastroenterology 2005;52:1703–6.
- Caplin S, Cerottini JP, Bosman FT, et al. For patients with Dukes’ B (TNM Stage II) colorectal carcinoma, examination of six or fewer lymph nodes is related to poor prognosis. Cancer 1998;83:666–72.
- Veronese N, Nottegar A, Pea A, et al. Prognostic impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol 2016;27:42–8.
- Li J, Yang S, Hu J, et al. Tumor deposits counted as positive lymph nodes in TNM staging for advanced colorectal cancer: a retrospective multicenter study. Oncotarget 2016;7:18269–79.
- Venook A, Niedzwiecki D, Innocenti Fet al. Impact of primary (1º) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol 2016;34 no. 15 suppl. Abstract 3504.
- Schrag D, Brooks G, Meyerhardt JA ,et al. The relationship between primary tumor sidedness and prognosis in colorectal cancer. J Clin Oncol 2016;34 no. 15 suppl. Abstract 3505.
- Larrea AA, Lujan SA, Kunkel TA. SnapShot: DNA mismatch repair. Cell 2010;141:730 e1.
- Jass JR. Pathology of hereditary nonpolyposis colorectal cancer. Ann N Y Acad Sci 2000;910:62–73.
- Lynch HT, Smyrk T. Hereditary nonpolyposis colorectal cancer (Lynch syndrome). An updated review. Cancer 1996;78:1149–67.
- Aaltonen LA, Peltomäki P, Leach FS, et al. Clues to the pathogenesis of familial colorectal cancer. Science 1993;260:812–6.
- Chen W, Swanson BJ, Frankel WL. Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn Pathol 2017;12:24.
- Bupathi M, Wu C. Biomarkers for immune therapy in colorectal cancer: mismatch-repair deficiency and others. J Gastrointest Oncol 2016;7:713–20.
- Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
- Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
- Ogino S, Kuchiba A, Qian ZR, et al. Prognostic significance and molecular associations of 18q loss of heterozygosity: a cohort study of microsatellite stable colorectal cancers. J Clin Oncol 2009; 27:4591–8.
- Kim ST, Lee J, Park SH, et al. The effect of DNA mismatch repair (MMR) status on oxaliplatin-based first-line chemotherapy as in recurrent or metastatic colon cancer. Med Oncol 2010;27:1277–85.
- Sargent DJ, Monges G, Thibodeau SN, et al. Therapy in colon cancer. J Clin Oncol 2010;28:4664.
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
- Hutchins G, Southward K, Handley K, et al. Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 2011;29:1261–270.
- Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses J Clin Oncol 2011;29:3768–74.
- Chang SC, Lin JK, Lin TC, Liang WY. Loss of heterozygosity: an independent prognostic factor of colorectal cancer. World J Gastroenterol 2005;11:778–84.
- Bertagnolli MM, Niedzwiecki D, Compton CC, et al. Microsatellite instability predicts improved response to adjuvant therapy with irinotecan, fluorouracil, and leucovorin in stage III colon cancer: Cancer and Leukemia Group B Protocol 89803. J Clin Oncol 2009;27:1814–21.
- Bertagnolli MM, Redston M, Compton CC, et al. Microsatellite instability and loss of heterozygosity at chromosomal location 18q: prospective evaluation of biomarkers for stages II and III colon cancer--a study of CALGB 9581 and 89803. J Clin Oncol 2011;29:3153–62.
- Dalerba P, et al. CDX2 as a prognostic biomarker in stage II and stage III colon cancer. N Engl J Med 2016;374: 211–22.
- Clark-Langone KM, Wu JY, Sangli C, et al. Biomarker discovery for colon cancer using a 761 gene RT-PCR assay. BMC Genomics 2007;8:279.
- Gray RG, Quirke P, Handley K, et al. Validation study of a quantitative multigene reverse transcriptase-polymerase chain reaction assay for assessment of recurrence risk in patients with stage II colon cancer. J Clin Oncol 2011;29:4611–9.
- Niedzwiecki D, Bertagnolli MM, Warren RS, et al. Documenting the natural history of patients with resected stage II adenocarcinoma of the colon after random assignment to adjuvant treatment with edrecolomab or observation: results from CALGB 9581. J Clin Oncol 2011;29:3146–52.
- Yothers G, O’Connell MJ, Lee M, et al. Validation of the 12-gene colon cancer recurrence score in NSABP C-07 as a predictor of recurrence in patients with stage II and III colon cancer treated with fluorouracil and leucovorin (FU/LV) and FU/LV plus oxaliplatin. J Clin Oncol 2013;31:4512–9.
- Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
- Gill S, Loprinzi C, Kennecke H, et al. Prognostic web-based models for stage II and III colon cancer: A population and clinical trials-based validation of numeracy and adjuvant! online. Cancer 2011;117:4155–65.
- Jung M, Kim GW, Jung I, et al. Application of the Western-based adjuvant online model to Korean colon cancer patients; a single institution experience. BMC Cancer 2012;12:471.
- Papamichael D, Renfro LA, Matthaiou C, et al. Validity of Adjuvant! Online in older patients with stage III colon cancer based on 2967 patients from the ACCENT database. J Geriatr Oncol 2016;7:422–9.
- Tran B, Kopetz S, Tie J, et al. Impact of BRAF mutation and microsatellite instability on the pattern of metastatic spread and prognosis in metastatic colorectal cancer. Cancer 2011;117:4623–32.
- Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol 2010;28:466–74.
- Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
- Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res 2007;67:2643–8.
- Therkildsen C, Bergmann TK, Henrichsen-Schnack T, et al. The predictive value of KRAS, NRAS, BRAF, PIK3CA and PTEN for anti-EGFR treatment in metastatic colorectal cancer: A systematic review and meta-analysis. Acta Oncol 2014;53:852–64.
- Taieb J, Le Malicot K, Shi Q, et al. Prognostic value of BRAF and KRAS mutations in MSI and MSS stage III colon cancer. J Natl Cancer Inst 2017;109(5).
- Palumbo LT, Sharpe WS, Henry JS. Cancer of the colon and rectum; analysis of 300 cases. Am J Surg 1965;109:439–44.
- Sharp GS, Benefiel WW. 5-Fluorouracil in the treatment of inoperable carcinoma of the colon and rectum. Cancer Chemother Rep 1962;20:97–101.
- Lawrence W Jr, Terz JJ, Horsley JS 3rd, et al. Chemotherapy as an adjuvant to surgery for colorectal cancer. Ann Surg 1975;181:616–23.
- Grage TD, et al. Adjuvant chemotherapy with 5-fluorouracil after surgical resection of colorectal carcinoma (COG protocol 7041). A preliminary report. Am J Surg 1977;133:59–66.
- Wolmark N, Fisher B, Rockette H, et al. Postoperative adjuvant chemotherapy or BCG for colon cancer: results from NSABP protocol C-01. J Natl Cancer Inst 1988;80:30–6.
- Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med 1990;322:352–8.
- Wolmark N, Rockette H, Fisher B, et al. The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol 1993;11:1879–87.
- Comparison of fluorouracil with additional levamisole, higher-dose folinic acid, or both, as adjuvant chemotherapy for colorectal cancer: a randomised trial. QUASAR Collaborative Group. Lancet 2000;355(9215):1588–96.
- Chen TC, Hinton DR, Leichman L, et al. Multifocal inflammatory leukoencephalopathy associated with levamisole and 5-fluorouracil: case report. Neurosurgery 1994;35:1138-42.
- Porschen R, Bermann A, Löffler T, et al. Fluorouracil plus leucovorin as effective adjuvant chemotherapy in curatively resected stage III colon cancer: results of the trial adjCCA-01. J Clin Oncol 2001;19:1787–94.
- Arkenau HT, Bermann A, Rettig K, et al. 5-Fluorouracil plus leucovorin is an effective adjuvant chemotherapy in curatively resected stage III colon cancer: long-term follow-up results of the adjCCA-01 trial. Ann Oncol 2003;14:395–9.
- Weinerman B, Shah A, Fields A, et al. Systemic infusion versus bolus chemotherapy with 5-fluorouracil in measurable metastatic colorectal cancer. Am J Clin Oncol 1992;15:518–23.
- Poplin EA, Benedetti JK, Estes NC, et al. Phase III Southwest Oncology Group 9415/Intergroup 0153 randomized trial of fluorouracil, leucovorin, and levamisole versus fluorouracil continuous infusion and levamisole for adjuvant treatment of stage III and high-risk stage II colon cancer. J Clin Oncol 2005;23:1819–25.
- Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
- de Gramont A, Vignoud J, Tournigand C, et al. Oxaliplatin with high-dose leucovorin and 5-fluorouracil 48-hour continuous infusion in pretreated metastatic colorectal cancer. Eur J Cancer 1997;33:214–9.
- Diaz-Rubio E, Sastre J, Zaniboni A, et al. Oxaliplatin as single agent in previously untreated colorectal carcinoma patients: a phase II multicentric study. Ann Oncol 1998;9:105–8.
- André T, de Gramont A, Vernerey D, et al. Adjuvant fluorouracil, leucovorin, and oxaliplatin in Stage II to III Colon Cancer: Updated 10-Year Survival and Outcomes According to BRAF mutation and mismatch repair status of the MOSAIC Study. J Clin Oncol 2015;33:4176–87.
- Andre T, Boni C, Mounedji-Boudiaf L, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004;350:2343–51.
- Kuebler JP, Wieand HS, O’Connell MJ, et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol 2007;25:2198–204.
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
- Schmoll HJ, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
- Colucci G, Gebbia V, Paoletti G, et al. Phase III randomized trial of FOLFIRI versus FOLFOX4 in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico Dell’Italia Meridionale. J Clin Oncol 2005;23:4866–75.
- Tournigand C, André T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 2004;22:229–37.
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 2004;350:2335–42.
- Saltz LB, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 2008;26:2013–9.
- Cremolini C, Loupakis F, Ruzzo A, et al. Predictors of benefit in colorectal cancer treated with cetuximab: are we getting “Lost in TranslationAL”? J Clin Oncol 2010;28:e173–4.
- Sorich MJ, Wiese MD, Rowland D, et al. Extended RAS mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann Oncol 2015;26:13–21.
- Grothey A, van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381(9863):303–12.
- Saltz LB, Niedzwiecki D, Hollis D, et al. Irinotecan fluorouracil plus leucovorin is not superior to fluorouracil plus leucovorin alone as adjuvant treatment for stage III colon cancer: results of CALGB 89803. J Clin Oncol 2007;25:3456–61.
- Van Cutsem E, et al. Randomized phase III trial comparing biweekly infusional fluorouracil/leucovorin alone or with irinotecan in the adjuvant treatment of stage III colon cancer: PETACC-3. J Clin Oncol 2009;27:3117–25.
- Allegra CJ, et al. Bevacizumab in stage II-III colon cancer: 5-year update of the National Surgical Adjuvant Breast and Bowel Project C-08 trial. J Clin Oncol 2013;31:359–64.
- de Gramont A, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012;13:1225–33.
- Alberts SR, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA 2012;307:1383–93.
- Taieb J, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:862–73.
- Shi Q, Sobrero AF, Shields AF, et al. Prospective pooled analysis of six phase III trials investigating duration of adjuvant (adjuvant) oxaliplatin-based therapy (3 vs 6 months) for patients (pts) with stage III colon cancer (CC): The IDEA (International Duration Evaluation of Adjuvant chemotherapy) collaboration. In: Proceedings from the American Society of Clinical Oncology; June 1–5, 2017; Chicago. Abstract LBA1.
- Quasar Collaborative Group; Gray R, Barnwell J, McConkey C, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370(9604):2020–9.
- Efficacy of adjuvant fluorouracil and folinic acid in B2 colon cancer. International Multicentre Pooled Analysis of B2 Colon Cancer Trials (IMPACT B2) Investigators. J Clin Oncol 1999;17:1356–63.
- Kidwell KM, et al. Long-term neurotoxicity effects of oxaliplatin added to fluorouracil and leucovorin as adjuvant therapy for colon cancer: results from National Surgical Adjuvant Breast and Bowel Project trials C-07 and LTS-01. Cancer 2012;118:5614–22.
- Beijers AJ, Mols F, Vreugdenhil G. A systematic review on chronic oxaliplatin-induced peripheral neuropathy and the relation with oxaliplatin administration. Support Care Cancer 2014;22:1999–2007.
- Mols F, Beijers T, Lemmens V, et al. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 2013;31:2699–707.
- Raphael MJ, Fischer HD, Fung K, et al. Neurotoxicity outcomes in a population-based cohort of elderly patients treated with adjuvant oxaliplatin for colorectal cancer. Clin Colorectal Cancer 2017 March 24.
- Toki MI, Saif MW, Syrigos KN. Hypersensitivity reactions associated with oxaliplatin and their clinical management. Expert Opin Drug Saf 2014;13:1545–54.
- Siu SW, Chan RT, Au GK. Hypersensitivity reactions to oxaliplatin: experience in a single institute. Ann Oncol 2006;17:259–61.
- Wong JT, Ling M, Patil S, et al. Oxaliplatin hypersensitivity: evaluation, implications of skin testing, and desensitization. J Allergy Clin Immunol Pract 2014;2:40–5.
- Benson AB 3rd, Venook AP, Cederquist L, et al. NCCN Guidelines Colon Cancer Version 2.2017. www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed May 8, 2017.
- Wolmark N, Rockette H, Mamounas E, et al. Clinical trial to assess the relative efficacy of fluorouracil and leucovorin, fluorouracil and levamisole, and fluorouracil, leucovorin, and levamisole in patients with Dukes’ B and C carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project C-04. J Clin Oncol 1999;17:3553–9.
INTRODUCTION
Colorectal cancer (CRC) is one of the most prevalent malignancies and is the fourth most common cancer in the United States, with an estimated 133,490 new cases diagnosed in 2016. Of these, approximately 95,520 are located in the colon and 39,970 are in the rectum.1 CRC is the third leading cause of cancer death in women and the second leading cause of cancer death in men, with an estimated 49,190 total deaths in 2016.2 The incidence appears to be increasing,3 especially in patients younger than 55 years of age;4 the reason for this increase remains uncertain.
A number of risk factors for the development of CRC have been identified. Numerous hered-itary CRC syndromes have been described, including familial adenomatous polyposis,5 hereditary non-polyposis colorectal cancer (HNPCC) or Lynch syndrome,6 and MUTYH-associated polyposis.7,8 A family history of CRC doubles the risk of developing CRC,9 and current guidelines support lowering the age of screening in individuals with a family history of CRC to 10 years younger than the age of diagnosis of the family member or 40 years of age, whichever is lower.10 Patients with a personal history of adenomatous polyps are at increased risk for developing CRC, as are patients with a personal history of CRC, with a relative risk ranging from 3 to 6.11 Ulcerative colitis and Crohn’s disease are associated with the development of CRC and also influence screening, though evidence suggests good control of these diseases may mitigate risk.12 Finally, modifiable risk factors for the development of CRC include high red meat consumption,13 diets low in fiber,14 obesity,13 smoking, alcohol use,15 and physical inactivity16; lifestyle modification targeting these factors has been shown to decrease rates of CRC.17 The majority of colon cancers present with clinical symptoms, often with rectal bleeding, abdominal pain, change in bowel habits, or obstructive symptoms. More rarely, these tumors are detected during screening colonoscopy, in which case they tend to be at an early stage.
SURGICAL MANAGEMENT
A critical goal in the resection of early-stage colon cancer is attaining R0 resection. Patients who achieve R0 resection as compared to R1 (microscopic residual tumor) and R2 (macroscopic residual tumor)18 have significantly improved long-term overall survival.19 Traditionally, open resection of the involved colonic segment was employed, with end-end anastomosis of the uninvolved free margins. Laparoscopic resection for early-stage disease has been utilized in attempts to decrease morbidity of open procedures, with similar outcomes and node sampling.20 Laparoscopic resection appears to provide similar outcomes even in locally advanced disease.21 Right-sided lesions are treated with right colectomy and primary ileocolic anastomosis.22 For patients presenting with obstructing masses, the Hartmann procedure is the most commonly performed operation. This involves creation of an ostomy with subtotal colectomy and subsequent ostomy reversal in a 2- or 3-stage protocol.23 Patients with locally advanced disease and invasion into surrounding structures require multivisceral resection, which involves resection en bloc with secondarily involved organs.24 Intestinal perforation presents a unique challenge and is associated with surgical complications, infection, and lower overall survival (OS) and 5-year disease-free survival (DFS). Complete mesocolic excision is a newer technique that has been performed with reports of better oncologic outcome at some centers; however, this approach is not currently considered standard of care.25
STAGING
According to a report by the National Cancer Institute, the estimated 5-year relative survival rates for localized colon cancer (lymph node negative), regional (lymph node positive) disease, and distant (metastatic) disease are 89.9%, 71.3%, and 13.9%, respectively.1 However, efforts have been made to further classify patients into distinct categories to allow fine-tuning of prognostication. In the current system, staging of colon cancer utilizes the American Joint Committee on Cancer tumor/node/metastasis (TNM) system.20 Clinical and pathologic features include depth of invasion, local invasion of other organs, nodal involvement, and presence of distant metastasis (Table 1). Studies completed prior to the adoption of the TNM system used the Dukes criteria, which divided colon cancer into A, B, and C, corresponding to TNM stage I, stage IIA–IIC, and stage IIIA-IIIC. This classification is rarely used in more contemporary studies.
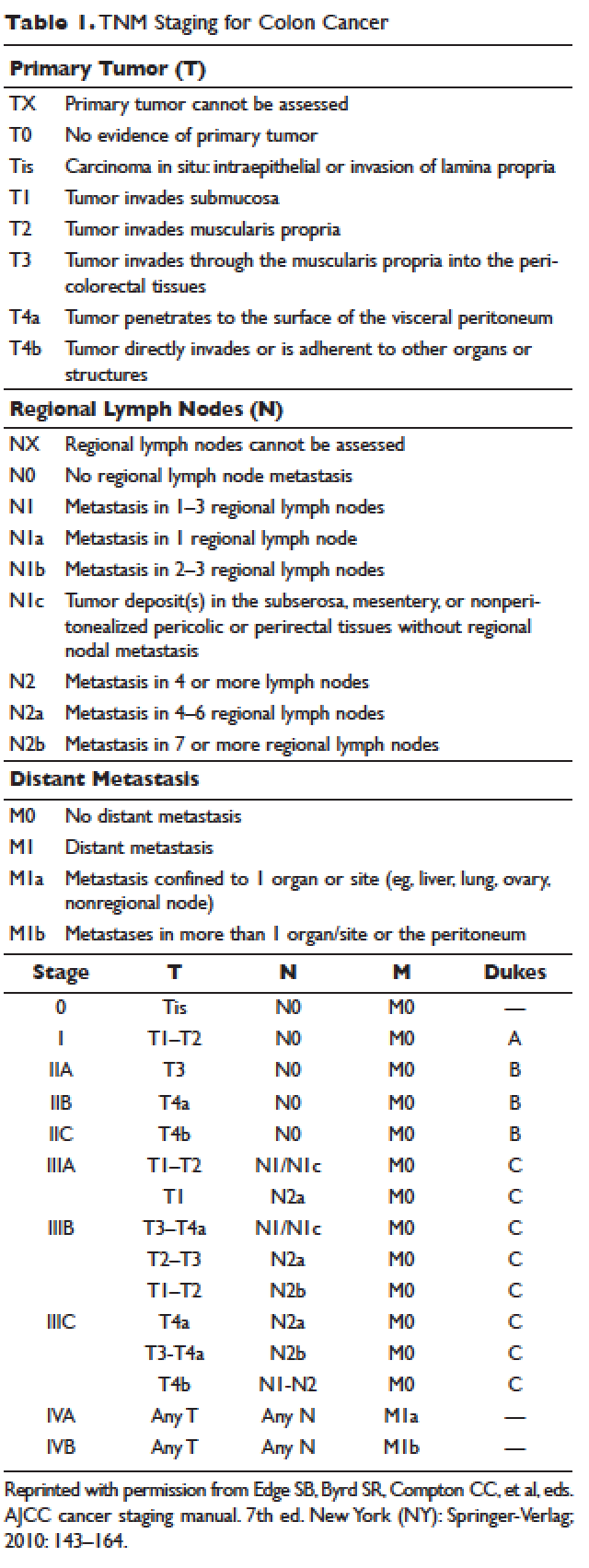
APPROACH TO ADJUVANT CHEMOTHERAPY
Adjuvant chemotherapy seeks to eliminate micrometastatic disease present following curative surgical resection. When stage 0 cancer is discovered incidentally during colonoscopy, endoscopic resection alone is the management of choice, as presence of micrometastatic disease is exceedingly unlikely.26 Stage I–III CRCs are treated with surgical resection withcurative intent. The 5-year survival rate for stage I and early-stage II CRC is estimated at 97% with surgery alone.27,28 The survival rate drops to about 60% for high-risk stage II tumors (T4aN0), and down to 50% or less for stage II-T4N0 or stage III cancers. Adjuvant chemotherapy is generally recommended to further decrease the rates of distant recurrence in certain cases of stage II and in all stage III tumors.
DETERMINATION OF BENEFIT FROM CHEMOTHERAPY: PROGNOSTIC MARKERS
Prior to administration of adjuvant chemotherapy, a clinical evaluation by the medical oncologist to determine appropriateness and safety of treatment is paramount. Poor performance status and comorbid conditions may indicate risk for excessive toxicity and minimal benefit from chemotherapy. CRC commonly presents in older individuals, with the median age at diagnosis of 69 years for men and 73 years for women.29 In this patient population, comorbidities such as cardiovascular disease, diabetes, and renal dysfunction are more prevalent.30 Decisions regarding adjuvant chemotherapy in this patient population have to take into consideration the fact that older patients may experience higher rates of toxicity with chemotherapy, including gastrointestinal toxicities and marrow suppression.31 Though some reports indicate patients older than 70 years derive similar benefit from adjuvant chemotherapy,32,33 a large pooled analysis of the ACCENT database, which included 7 adjuvant therapy trials and 14,528 patients, suggested limited benefit from the addition of oxaliplatin to fluorouracil in elderly patients.32 Other factors that weigh on the decision include stage, pathology, and presence of high-risk features. A common concern in the postoperative setting is delaying initiation of chemotherapy to allow adequate wound healing; however, evidence suggests that delays longer than 8 weeks leads to worse overall survival, with hazard ratios (HR) ranging from 1.4 to 1.7.34,35 Thus, the start of adjuvant therapy should ideally be within this time frame.
HIGH-RISK FEATURES
Multiple factors have been found to predict worse outcome and are classified as high-risk features (Table 2). Histologically, high-grade or poorly differentiated tumors are associated with higher recurrence rate and worse outcome.36 Certain histological subtypes, including mucinous and signet-ring, both appear to have more aggressive biology.37 Presence of microscopic invasion into surrounding blood vessels (vascular invasion) and nerves (perineural invasion) is associated with lower survival.38 Penetration of the cancer through the visceral peritoneum (T4a) or into surrounding structures (T4b) is associated with lower survival.36 During surgical resection, multiple lymph nodes are removed along with the primary tumor to evaluate for metastasis to the regional nodes. Multiple analyses have demonstrated that removal and pathologic assessment of fewer than 12 lymph nodes is associated with high risk of missing a positive node, and is thus equated with high risk.39–41 In addition, extension of tumor beyond the capsules of any single lymph node, termed extracapsular extension, is associated with an increased risk of all-cause mortality.42 Tumor deposits, or focal aggregates of adenocarcinoma in the pericolic fat that are not contiguous with the primary tumor and are not associated with lymph nodes, are currently classified as lymph nodes as N1c in the current TNM staging system. Presence of these deposits has been found to predict poor outcome stage for stage.43 Obstruction and/or perforation secondary to the tumor are also considered high-risk features that predict poor outcome.

SIDEDNESS
As reported at the 2016 American Society of Clinical Oncology annual meeting, tumor location predicts outcome in the metastatic setting. A report by Venook and colleagues based on a post-hoc analysis found that in the metastatic setting, location of the tumor primary in the left side is associated with longer OS (33.3 months) when compared to the right side of the colon (19.4 months).44 A retrospective analysis of multiple databases presented by Schrag and colleagues similarly reported inferior outcomes in patients with stage III and IV disease who had right-sided primary tumors.45 However, the prognostic implications for stage II disease remain uncertain.
BIOMARKERS
Given the controversy regarding adjuvant therapy of patients with stage II colon cancer, multiple biomarkers have been evaluated as possible predictive markers that can assist in this decision. The mismatch repair (MMR) system is a complex cellular enzymatic mechanism that identifies and corrects DNA errors during cell division and prevents mutagenesis.46 The familial cancer syndrome HNPCC is linked to alteration in a variety of MMR genes, leading to deficient mismatch repair (dMMR), also termed microsatellite instability-high (MSI-high).47,48 Epigenetic modification can also lead to silencing of the same implicated genes and accounts for 15% to 20% of sporadic colorectal cancer.49 These epigenetic modifications lead to hypermethylation of the promotor region of MLH1 in 70% of cases.50 The 4 MMR genes most commonly tested are MLH-1, MSH2, MSH6, and PMS2. Testing can be performed by immunohistochemistry or polymerase chain reaction.51 Across tumor histology and stage, MSI status is prognostic. Patients with MSI-high tumors have been shown to have improved prognosis and longer OS both in stage II and III disease52–54 and in the metastatic setting.55 However, despite this survival benefit, there is conflicting data as to whether patients with stage II, MSI-high colon cancer may benefit less from adjuvant chemotherapy. One early retrospective study compared outcomes of 70 patients with stage II and III disease and dMMR to those of 387 patients with stage II and III disease and proficient mismatch repair (pMMR). Adjuvant fluorouracil with leucovorin improved DFS for patients with pMMR (HR 0.67) but not for those with dMMR (HR 1.10). In addition, for patients with stage II disease and dMMR, the HR for OS was inferior at 2.95.56 Data collected from randomized clinical trials using fluorouracil-based adjuvant chemotherapy were analyzed in an attempt to predict benefit based on MSI status. Benefit was only seen in pMMR patients, with a HR of 0.72; this was not seen in the dMMR patients.57 Subsequent studies have had different findings and did not demonstrate a detrimental effect of fluorouracil in dMMR.58,59 For stage III patients, MSI status does not appear to affect benefit from chemotherapy, as analysis of data from the NSABP C-07 trial (Table 3) demonstrated benefit of FOLFOX (leucovorin, fluorouracil, oxaliplatin) in patients with dMMR status and stage III disease.59
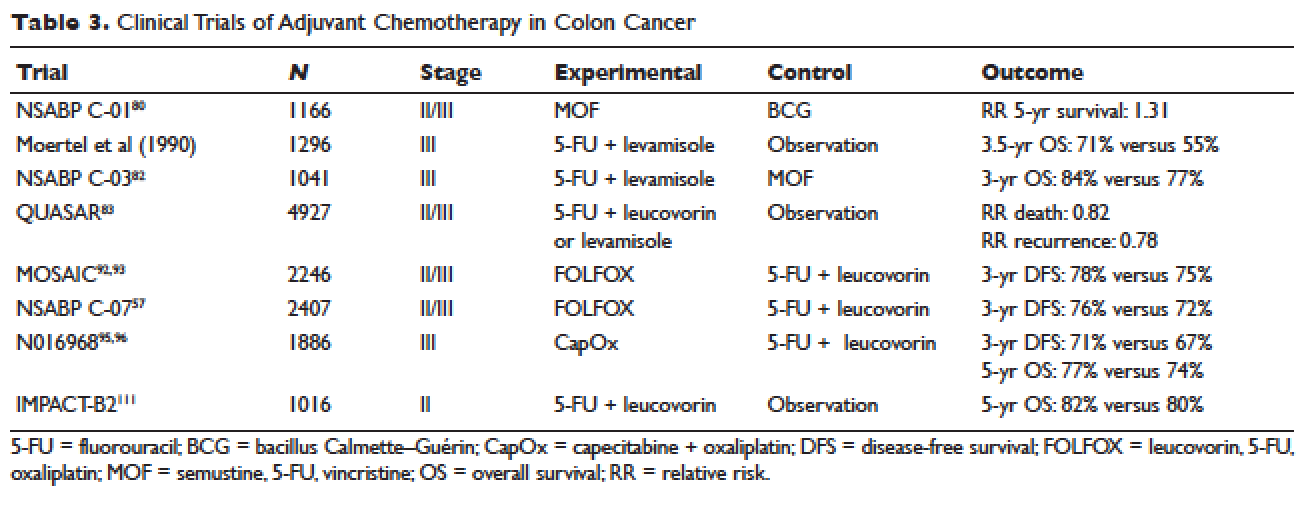
Another genetic abnormality identified in colon cancers is chromosome 18q loss of heterozygosity (LOH). The presence of 18q LOH appears to be inversely associated with MSI-high status. Some reports have linked presence of 18q with worse outcome,60 but others question this, arguing the finding may simply be related to MSI status.61,62 This biomarker has not been established as a clear prognostic marker that can aid clinical decisions.
Most recently, expression of caudal-type homeobox transcription factor 2 (CDX2) has been reported as a novel prognostic and predictive tool. A 2015 report linked lack of expression of CDX2 to worse outcome; in this study, 5-year DFS was 41% in patients with CDX2-negative tumors versus 74% in the CDX2-positive tumors, with a HR of disease recurrence of 2.73 for CDX2-negative tumors.63 Similar numbers were observed in patients with stage II disease, with 5-year OS of 40% in patients with CDX2-negative tumors versus 70% in those with CDX2-positive tumors. Treatment of CDX2-negative patients with adjuvant chemotherapy improved outcomes: 5-year DFS in the stage II subgroup was 91% with chemotherapy versus 56% without, and in the stage III subgroup, 74% with chemotherapy versus 37% without. The authors concluded that patients with stage II and III colon cancer that is CDX2-negative may benefit from adjuvant chemotherapy. Importantly, CDX2-negativity is a rare event, occurring in only 6.9% of evaluable tumors.
RISK ASSESSMENT TOOLS
Several risk assessment tools have been developed in an attempt to aid clinical decision making regarding adjuvant chemotherapy for patients with stage II colon cancer. The Oncotype DX Colon Assay analyses a 12-gene signature in the pathologic sample and was developed with the goal to improve prognostication and aid in treatment decision making. The test utilizes reverse transcription-PCR on RNA extracted from the tumor.64 After evaluating 12 genes, a recurrence score is generated that predicts the risk of disease recurrence. This score was validated using data from 3 large clinical trials.65–67 Unlike the Oncotype Dx score used in breast cancer, the test in colon cancer has not been found to predict the benefit from chemotherapy and has not been incorporated widely into clinical practice.
Adjuvant! Online (available at www.adjuvantonline.com) is a web-based tool that combines clinical and histological features to estimate outcome. Calculations are based on US SEER tumor registry-reported outcomes.68 A second web-based tool, Numeracy (available at www.mayoclinic.com/calcs), was developed by the Mayo Clinic using pooled data from 7 randomized clinical trials including 3341 patients.68 Both tools seek to predict absolute benefit for patients treated with fluorouracil, though data suggests Adjuvant! Online may be more reliable in its predictive ability.69 Adjuvant! Online has also been validated in an Asian population70 and patients older than 70 years.71
MUTATIONAL ANALYSIS
Multiple mutations in proto-oncogenes have been found in colon cancer cells. One such proto-oncogene is BRAF, which encodes a serine-threonine kinase in the rapidly accelerated fibrosarcoma (RAF). Mutations in BRAF have been found in 5% to 10% of colon cancers and are associated with right-sided tumors.72 As a prognostic marker, some studies have associated BRAF mutations with worse prognosis, including shorter time to relapse and shorter OS.73,74 Two other proto-oncogenes are Kristen rat sarcoma viral oncogene homolog (KRAS) and neuroblastoma rat sarcoma viral oncogene homolog (NRAS), both of which encode proteins downstream of epidermal growth factor receptor (EGFR). KRAS and NRAS mutations have been shown to be predictive in the metastatic setting where they predict resistance to the EGFR inhibitors cetuximab and panitumumab.75,76 The effect of KRAS and NRAS mutations on outcome in stage II and III colon cancer is uncertain. Some studies suggest worse outcome in KRAS-mutated cancers,77 while others failed to demonstrate this finding.73
CASE PRESENTATION 1
A 53-year-old man with no past medical history presents to the emergency department with early satiety and generalized abdominal pain. Laboratory evaluation shows a microcytic anemia with normal white blood cell count, platelet count, renal function, and liver function tests. Computed tomography (CT) scan of the abdomen and pelvis show a 4-cm mass in the transverse colon without obstruction and without abnormality in the liver. CT scan of the chest does not demonstrate pathologic lymphadenopathy or other findings. He undergoes robotic laparoscopic transverse colon resection and appendectomy. Pathology confirms a 3.5-cm focus of adenocarcinoma of the colon with invasion through the muscularis propria and 5 of 27 regional lymph nodes positive for adenocarcinoma and uninvolved proximal, distal, and radial margins. He is given a stage of IIIB pT3 pN2a M0 and referred to medical oncology for further management, where 6 months of adjuvant FOLFOX chemotherapy is recommended.
ADJUVANT CHEMOTHERAPY IN STAGE III COLON CANCER
Postoperative adjuvant chemotherapy is the standard of care for patients with stage III disease. In the 1960s, infusional fluorouracil was first used to treat inoperable colon cancer.78,79 After encouraging results, the agent was used both intraluminally and intravenously as an adjuvant therapy for patients undergoing resection with curative intent; however, only modest benefits were described.80,81 The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-01 trial (Table 3) was the first study to demonstrate a benefit from adjuvant chemotherapy in colon cancer. This study randomly assigned patients with stage II and III colon cancer to surgery alone, postoperative chemotherapy with fluorouracil, semustine, and vincristine (MOF), or postoperative bacillus Calmette-Guérin (BCG). DFS and OS were significantly improved with MOF chemotherapy.82 In 1990, a landmark study reported on outcomes after treatment of 1296 patients with stage III colon cancer with adjuvant fluorouracil and levamisole for 12 months. The combination was associated with a 41% reduction in risk of cancer recurrence and a 33% reduction in risk of death.83 The NSABP C-03 trial (Table 3) compared MOF to the combination of fluorouracil and leucovorin and demonstrated improved 3-year DFS (69% versus 73%) and 3-year OS (77% versus 84%) in patients with stage III disease.84 Building on these outcomes, the QUASAR study (Table 3) compared fluorouracil in combination with one of levamisole, low-dose leucovorin, or high-dose leucovorin. The study enrolled 4927 patients and found worse outcomes with fluorouracil plus levamisole and no difference in low-doseversus high-dose leucovorin.85 Levamisole fell out of use after associations with development of multifocal leukoencephalopathy,86 and was later shown to have inferior outcomes versus leucovorin when combined with fluorouracil.87,88 Intravenous fluorouracil has shown similar benefit when administered by bolus or infusion,89 although continuous infusion has been associated with lower incidence of severe toxicity.90 The efficacy of the oral fluoropyrimidine capecitabine has been shown to be equivalent to that of fluorouracil.91
Fluorouracil-based treatment remained the standard of care until the introduction of oxaliplatin in the mid-1990s. After encouraging results in the metastatic setting,92,93 the agent was moved to the adjuvant setting. The MOSAIC trial (Table 3) randomly assigned patients with stage II and III colon cancer to fluorouracil with leucovorin (FULV) versus FOLFOX given once every 2 weeks for 12 cycles. Analysis with respect to stage III patients showed a clear survival benefit, with a 10-year OS of 67.1% with FOLFOX chemotherapy versus 59% with fluorouracil and leucovorin.94,95 The NSABP C-07 (Table 3) trial used a similar trial design but employed bolus fluorouracil. More than 2400 patients with stage II and III colon cancer were randomly assigned to bolus FULV or bolus fluorouracil, leucovorin, and oxaliplatin (FLOX). The addition of oxaliplatin significantly improved outcomes, with 4-year DFS of 67% versus 71.8% for FULV and FLOX, respectively, and a HR of death of 0.80 with FLOX.59,96 The multicenter N016968 trial (Table 3) randomly assigned 1886 patients with stage III colon cancer to adjuvant capecitabine plus oxaliplatin (XELOX) or bolus fluorouracil plus leucovorin (FU/FA). The 3-year DFS was 70.9% versus 66.5% with XELOX and FU/FA, respectively, and 5-year OS was 77.6% versus 74.2%, respectively.97,98
In the metastatic setting, additional agents have shown efficacy, including irinotecan,99,100 bevacizumab,101,102 cetuximab,103,104 and regorafenib.105 This observation led to testing of these agents in earlier stage disease. The CALGB 89803 trial compared fluorouracil, leucovorin, and irinotecan to fluorouracil with leucovorin alone. No benefit in 5-year DFS or OS was seen.106 Similarly, infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) was not found to improve 5-year DFS as compared to fluorouracil with leucovorin alone in the PETACC-3 trial.107 The NSABP C-08 trial considered the addition of bevacizumab to FOLFOX. When compared to FOLFOX alone, the combination of bevacizumab to FOLFOX had similar 3-year DFS (77.9% versus 75.1%) and 5-year OS (82.5% versus 80.7%).108 This finding was confirmed in the Avant trial.109 The addition of cetuximab to FOLFOX was equally disappointing, as shown in the N0147 trial110 and PETACC-8 trial.111 Data on regorafenib in the adjuvant setting for stage III colon cancer is lacking; however, 2 ongoing clinical trials, NCT02425683 and NCT02664077, are each studying the use of regorafenib following completion of FOLFOX for patients with stage III disease.
Thus, after multiple trials comparing various regimens and despite attempts to improve outcomes by the addition of a third agent, the standard of care per National Comprehensive Cancer Network (NCCN) guidelines for management of stage III colon cancer remains 12 cycles of FOLFOX chemotherapy. Therapy should be initiated within 8 weeks of surgery. Data are emerging to support a short duration of therapy for patients with low-risk stage III tumors, as shown in an abstract presented at the 2017 American Society of Clinical Oncology annual meeting. The IDEA trial was a pooled analysis of 6 randomized clinical trials across multiple countries, all of which evaluated 3 versus 6 months of FOLFOX or capecitabine and oxaliplatin in the treatment of stage III colon cancer. The analysis was designed to test non-inferiority of 3 months of therapy as compared to 6 months. The analysis included 6088 patients across 244 centers in 6 countries. The overall analysis failed to establish noninferiority. The 3-year DFS rate was 74.6% for 3 months and 75.5% for 6 months, with a DFS HR of 1.07 and a confidence interval that did not meet the prespecified endpoint. Subgroup analysis suggested noninferiority for lower stage disease (T1–3 or N1) but not for higher stage disease (T4 or N2). Given the high rates of neuropathy with 6 months of oxaliplatin, these results suggest that 3 months of adjuvant therapy can be considered for patients with T1–3 or N1 disease in an attempt to limit toxicity.112
CASE PRESENTATION 2
A 57-year-old woman presents to the emergency department with fever and abdominal pain. CT of the abdomen and pelvis demonstrates a left-sided colonic mass with surrounding fat stranding and pelvic abscess. She is taken emergently for left hemicolectomy, cholecystectomy, and evacuation of pelvic abscess. Pathology reveals a 5-cm adenocarcinoma with invasion through the visceral peritoneum; 0/22 lymph nodes are involved. She is given a diagnosis of stage IIC and referred to medical oncology for further management. Due to her young age and presence of high-risk features, she is recommended adjuvant therapy with FOLFOX for 6 months.
ADJUVANT CHEMOTHERAPY IN STAGE II COLON CANCER
Because of excellent outcomes with surgical resection alone for stage II cancers, the use of adjuvant chemotherapy for patients with stage II disease is controversial. Limited prospective data is available to guide adjuvant treatment decisions for stage II patients. The QUASAR trial, which compared observation to adjuvant fluorouracil and leucovorin in patients with early-stage colon cancer, included 2963 patients with stage II disease and found a relative risk (RR) of death or recurrence of 0.82 and 0.78, respectively. Importantly, the absolute benefit of therapy was less than 5%.113 The IMPACT-B2 trial (Table 3) combined data from 5 separate trials and analyzed 1016 patients with stage II colon cancer who received fluorouracil with leucovorin or observation. Event-free survival was 0.86 versus 0.83 and 5-year OS was 82% versus 80%, suggesting no benefit.114 The benefit of addition of oxaliplatin to fluorouracil in stage II disease appears to be less than the benefit of adding this agent in the treatment of stage III CRC. As noted above, the MOSAIC trial randomly assigned patients with stage II and III colon cancer to receive adjuvant fluorouracil and leucovorin with or without oxaliplatin for 12 cycles. After a median follow-up of 9.5 years, 10-year OS rates for patients with stage II disease were 78.4% versus 79.5%. For patients with high-risk stage II disease (defined as T4, bowel perforation, or fewer than 10 lymph nodes examined), 10-year OS was 71.7% and 75.4% respectively, but these differences were not statistically significant.94
Because of conflicting data as to the benefit of adding oxaliplatin in stage II disease, oxaliplatin is not recommended for standard-risk stage II patients. The use of oxaliplatin in high-risk stage II tumors should be weighed carefully given the toxicity risk. Oxaliplatin is recognized to cause sensory neuropathy in many patients, which can become painful and debilitating.115 Two types of neuropathy are associated with oxaliplatin: acute and chronic. Acute neuropathy manifests most often as cold-induced paresthesias in the fingers and toes and is quite common, affecting up to 90% of patients. These symptoms are self-limited and resolve usually within 1 week of each treatment.116 Some patients, with reports ranging from 10% to 79%, develop chronic neuropathy that persists for 1 year or more and causes significant decrements in quality of life.117 Patients older than age 70 may be at greater risk for oxaliplatin-induced neuropathy, which would increase risk of falls in this population.118 In addition to neuropathy, oxaliplatin is associated with hypersensitivity reactions that can be severe and even fatal.119 In a single institution series, the incidence of severe reactions was 2%.120 Desensitization following hypersensitivity reactions is possible but requires a time-intensive protocol.121
Based on the inconclusive efficacy findings and due to concerns over toxicity, each decision must be individualized to fit patient characteristics and preferences. In general, for patients with stage II disease without high-risk features, an individualized discussion should be held as to the risks and benefits of single-agent fluorouracil, and this treatment should be offered in cases where the patient or provider would like to be aggressive. Patients with stage II cancer who have 1 or more high-risk features are often recommended adjuvant chemotherapy. Whether treatment with fluorouracil plus leucovorin or FOLFOX is preferred remains uncertain, and thus the risks and the potential gains of oxaliplatin must be discussed with the individual patient. MMR status can also influence the treatment recommendation for patients with stage II disease. In general, patients with standard-risk stage II tumors that are pMMR are offered MMR with leucovorin or oral capecitabine for 12 cycles. FOLFOX is considered for patients with MSI-high disease and those with multiple high-risk features.
MONITORING AFTER THERAPY
After completion of adjuvant chemotherapy, patients enter a period of survivorship. Patients are seen in clinic for symptom and laboratory monitoring of the complete blood count, liver function tests, and carcinoembryonic antigen (CEA). NCCN guidelines support history and physical examination with CEA testing every 3 to 6 months for the first 2 years, then every 6 months for the next 3 years, after which many patients continue to be seen annually. CT imaging of the chest, abdomen, and pelvis for monitoring of disease recurrence is recommended every 6 to 12 months for a total of 5 years. New elevations in CEA or liver function tests should prompt early imaging. Colonoscopy should be performed 1 year after completion of therapy; however, if no preoperative colonoscopy was performed, this should be done 3 to 6 months after completion. Colonoscopy is then repeated in 3 years and then every 5 years unless advanced adenomas are present.122
SUMMARY
The addition of chemotherapy to surgical management of colon cancer has lowered the rate of disease recurrence and improved long-term survival. Adjuvant FOLFOX for 12 cycles is the standard of care for patients with stage III colon cancer and for patients with stage II disease with certain high-risk features. Use of adjuvant chemotherapy in stage II disease without high-risk features is controversial, and treatment decisions should be individualized. Biologic markers such as MSI and CDX2 status as well as patient-related factors including age, overall health, and personal preferences can inform treatment decisions. If chemotherapy is recommended in this setting, it would be with single-agent fluorouracil in an infusional or oral formulation, unless the tumor has the MSI-high feature. Following completion of adjuvant therapy, patients should be followed with clinical evaluation, laboratory testing, and imaging for a total of 5 years as per recommended guidelines.
INTRODUCTION
Colorectal cancer (CRC) is one of the most prevalent malignancies and is the fourth most common cancer in the United States, with an estimated 133,490 new cases diagnosed in 2016. Of these, approximately 95,520 are located in the colon and 39,970 are in the rectum.1 CRC is the third leading cause of cancer death in women and the second leading cause of cancer death in men, with an estimated 49,190 total deaths in 2016.2 The incidence appears to be increasing,3 especially in patients younger than 55 years of age;4 the reason for this increase remains uncertain.
A number of risk factors for the development of CRC have been identified. Numerous hered-itary CRC syndromes have been described, including familial adenomatous polyposis,5 hereditary non-polyposis colorectal cancer (HNPCC) or Lynch syndrome,6 and MUTYH-associated polyposis.7,8 A family history of CRC doubles the risk of developing CRC,9 and current guidelines support lowering the age of screening in individuals with a family history of CRC to 10 years younger than the age of diagnosis of the family member or 40 years of age, whichever is lower.10 Patients with a personal history of adenomatous polyps are at increased risk for developing CRC, as are patients with a personal history of CRC, with a relative risk ranging from 3 to 6.11 Ulcerative colitis and Crohn’s disease are associated with the development of CRC and also influence screening, though evidence suggests good control of these diseases may mitigate risk.12 Finally, modifiable risk factors for the development of CRC include high red meat consumption,13 diets low in fiber,14 obesity,13 smoking, alcohol use,15 and physical inactivity16; lifestyle modification targeting these factors has been shown to decrease rates of CRC.17 The majority of colon cancers present with clinical symptoms, often with rectal bleeding, abdominal pain, change in bowel habits, or obstructive symptoms. More rarely, these tumors are detected during screening colonoscopy, in which case they tend to be at an early stage.
SURGICAL MANAGEMENT
A critical goal in the resection of early-stage colon cancer is attaining R0 resection. Patients who achieve R0 resection as compared to R1 (microscopic residual tumor) and R2 (macroscopic residual tumor)18 have significantly improved long-term overall survival.19 Traditionally, open resection of the involved colonic segment was employed, with end-end anastomosis of the uninvolved free margins. Laparoscopic resection for early-stage disease has been utilized in attempts to decrease morbidity of open procedures, with similar outcomes and node sampling.20 Laparoscopic resection appears to provide similar outcomes even in locally advanced disease.21 Right-sided lesions are treated with right colectomy and primary ileocolic anastomosis.22 For patients presenting with obstructing masses, the Hartmann procedure is the most commonly performed operation. This involves creation of an ostomy with subtotal colectomy and subsequent ostomy reversal in a 2- or 3-stage protocol.23 Patients with locally advanced disease and invasion into surrounding structures require multivisceral resection, which involves resection en bloc with secondarily involved organs.24 Intestinal perforation presents a unique challenge and is associated with surgical complications, infection, and lower overall survival (OS) and 5-year disease-free survival (DFS). Complete mesocolic excision is a newer technique that has been performed with reports of better oncologic outcome at some centers; however, this approach is not currently considered standard of care.25
STAGING
According to a report by the National Cancer Institute, the estimated 5-year relative survival rates for localized colon cancer (lymph node negative), regional (lymph node positive) disease, and distant (metastatic) disease are 89.9%, 71.3%, and 13.9%, respectively.1 However, efforts have been made to further classify patients into distinct categories to allow fine-tuning of prognostication. In the current system, staging of colon cancer utilizes the American Joint Committee on Cancer tumor/node/metastasis (TNM) system.20 Clinical and pathologic features include depth of invasion, local invasion of other organs, nodal involvement, and presence of distant metastasis (Table 1). Studies completed prior to the adoption of the TNM system used the Dukes criteria, which divided colon cancer into A, B, and C, corresponding to TNM stage I, stage IIA–IIC, and stage IIIA-IIIC. This classification is rarely used in more contemporary studies.
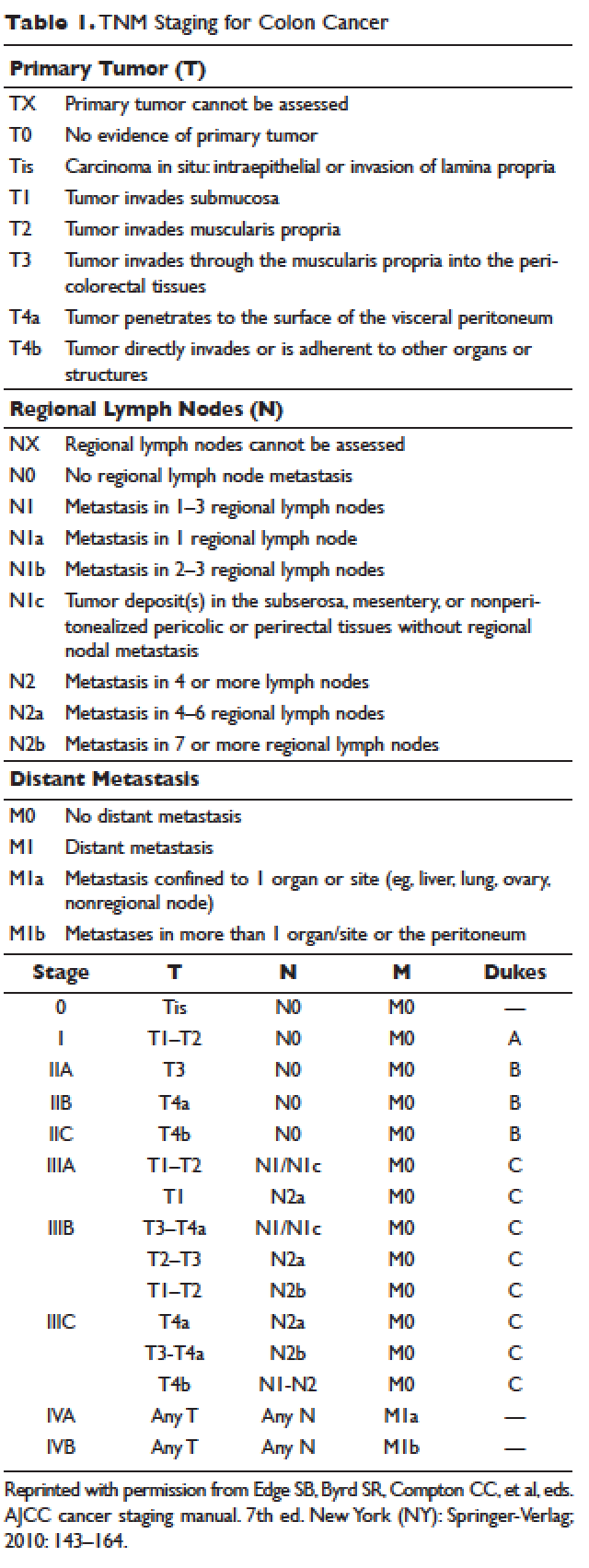
APPROACH TO ADJUVANT CHEMOTHERAPY
Adjuvant chemotherapy seeks to eliminate micrometastatic disease present following curative surgical resection. When stage 0 cancer is discovered incidentally during colonoscopy, endoscopic resection alone is the management of choice, as presence of micrometastatic disease is exceedingly unlikely.26 Stage I–III CRCs are treated with surgical resection withcurative intent. The 5-year survival rate for stage I and early-stage II CRC is estimated at 97% with surgery alone.27,28 The survival rate drops to about 60% for high-risk stage II tumors (T4aN0), and down to 50% or less for stage II-T4N0 or stage III cancers. Adjuvant chemotherapy is generally recommended to further decrease the rates of distant recurrence in certain cases of stage II and in all stage III tumors.
DETERMINATION OF BENEFIT FROM CHEMOTHERAPY: PROGNOSTIC MARKERS
Prior to administration of adjuvant chemotherapy, a clinical evaluation by the medical oncologist to determine appropriateness and safety of treatment is paramount. Poor performance status and comorbid conditions may indicate risk for excessive toxicity and minimal benefit from chemotherapy. CRC commonly presents in older individuals, with the median age at diagnosis of 69 years for men and 73 years for women.29 In this patient population, comorbidities such as cardiovascular disease, diabetes, and renal dysfunction are more prevalent.30 Decisions regarding adjuvant chemotherapy in this patient population have to take into consideration the fact that older patients may experience higher rates of toxicity with chemotherapy, including gastrointestinal toxicities and marrow suppression.31 Though some reports indicate patients older than 70 years derive similar benefit from adjuvant chemotherapy,32,33 a large pooled analysis of the ACCENT database, which included 7 adjuvant therapy trials and 14,528 patients, suggested limited benefit from the addition of oxaliplatin to fluorouracil in elderly patients.32 Other factors that weigh on the decision include stage, pathology, and presence of high-risk features. A common concern in the postoperative setting is delaying initiation of chemotherapy to allow adequate wound healing; however, evidence suggests that delays longer than 8 weeks leads to worse overall survival, with hazard ratios (HR) ranging from 1.4 to 1.7.34,35 Thus, the start of adjuvant therapy should ideally be within this time frame.
HIGH-RISK FEATURES
Multiple factors have been found to predict worse outcome and are classified as high-risk features (Table 2). Histologically, high-grade or poorly differentiated tumors are associated with higher recurrence rate and worse outcome.36 Certain histological subtypes, including mucinous and signet-ring, both appear to have more aggressive biology.37 Presence of microscopic invasion into surrounding blood vessels (vascular invasion) and nerves (perineural invasion) is associated with lower survival.38 Penetration of the cancer through the visceral peritoneum (T4a) or into surrounding structures (T4b) is associated with lower survival.36 During surgical resection, multiple lymph nodes are removed along with the primary tumor to evaluate for metastasis to the regional nodes. Multiple analyses have demonstrated that removal and pathologic assessment of fewer than 12 lymph nodes is associated with high risk of missing a positive node, and is thus equated with high risk.39–41 In addition, extension of tumor beyond the capsules of any single lymph node, termed extracapsular extension, is associated with an increased risk of all-cause mortality.42 Tumor deposits, or focal aggregates of adenocarcinoma in the pericolic fat that are not contiguous with the primary tumor and are not associated with lymph nodes, are currently classified as lymph nodes as N1c in the current TNM staging system. Presence of these deposits has been found to predict poor outcome stage for stage.43 Obstruction and/or perforation secondary to the tumor are also considered high-risk features that predict poor outcome.

SIDEDNESS
As reported at the 2016 American Society of Clinical Oncology annual meeting, tumor location predicts outcome in the metastatic setting. A report by Venook and colleagues based on a post-hoc analysis found that in the metastatic setting, location of the tumor primary in the left side is associated with longer OS (33.3 months) when compared to the right side of the colon (19.4 months).44 A retrospective analysis of multiple databases presented by Schrag and colleagues similarly reported inferior outcomes in patients with stage III and IV disease who had right-sided primary tumors.45 However, the prognostic implications for stage II disease remain uncertain.
BIOMARKERS
Given the controversy regarding adjuvant therapy of patients with stage II colon cancer, multiple biomarkers have been evaluated as possible predictive markers that can assist in this decision. The mismatch repair (MMR) system is a complex cellular enzymatic mechanism that identifies and corrects DNA errors during cell division and prevents mutagenesis.46 The familial cancer syndrome HNPCC is linked to alteration in a variety of MMR genes, leading to deficient mismatch repair (dMMR), also termed microsatellite instability-high (MSI-high).47,48 Epigenetic modification can also lead to silencing of the same implicated genes and accounts for 15% to 20% of sporadic colorectal cancer.49 These epigenetic modifications lead to hypermethylation of the promotor region of MLH1 in 70% of cases.50 The 4 MMR genes most commonly tested are MLH-1, MSH2, MSH6, and PMS2. Testing can be performed by immunohistochemistry or polymerase chain reaction.51 Across tumor histology and stage, MSI status is prognostic. Patients with MSI-high tumors have been shown to have improved prognosis and longer OS both in stage II and III disease52–54 and in the metastatic setting.55 However, despite this survival benefit, there is conflicting data as to whether patients with stage II, MSI-high colon cancer may benefit less from adjuvant chemotherapy. One early retrospective study compared outcomes of 70 patients with stage II and III disease and dMMR to those of 387 patients with stage II and III disease and proficient mismatch repair (pMMR). Adjuvant fluorouracil with leucovorin improved DFS for patients with pMMR (HR 0.67) but not for those with dMMR (HR 1.10). In addition, for patients with stage II disease and dMMR, the HR for OS was inferior at 2.95.56 Data collected from randomized clinical trials using fluorouracil-based adjuvant chemotherapy were analyzed in an attempt to predict benefit based on MSI status. Benefit was only seen in pMMR patients, with a HR of 0.72; this was not seen in the dMMR patients.57 Subsequent studies have had different findings and did not demonstrate a detrimental effect of fluorouracil in dMMR.58,59 For stage III patients, MSI status does not appear to affect benefit from chemotherapy, as analysis of data from the NSABP C-07 trial (Table 3) demonstrated benefit of FOLFOX (leucovorin, fluorouracil, oxaliplatin) in patients with dMMR status and stage III disease.59
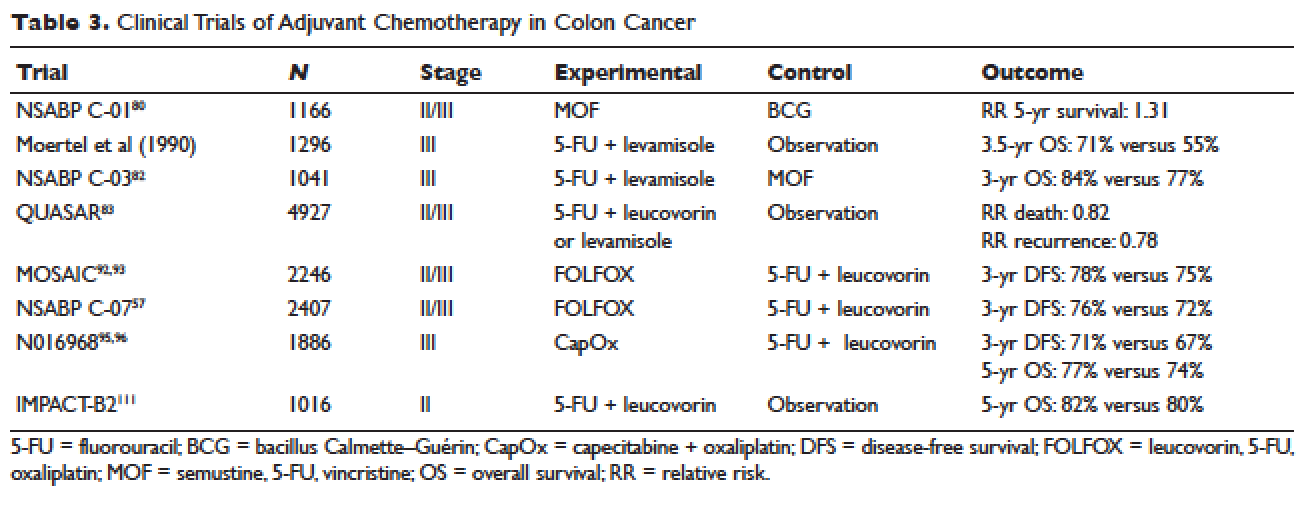
Another genetic abnormality identified in colon cancers is chromosome 18q loss of heterozygosity (LOH). The presence of 18q LOH appears to be inversely associated with MSI-high status. Some reports have linked presence of 18q with worse outcome,60 but others question this, arguing the finding may simply be related to MSI status.61,62 This biomarker has not been established as a clear prognostic marker that can aid clinical decisions.
Most recently, expression of caudal-type homeobox transcription factor 2 (CDX2) has been reported as a novel prognostic and predictive tool. A 2015 report linked lack of expression of CDX2 to worse outcome; in this study, 5-year DFS was 41% in patients with CDX2-negative tumors versus 74% in the CDX2-positive tumors, with a HR of disease recurrence of 2.73 for CDX2-negative tumors.63 Similar numbers were observed in patients with stage II disease, with 5-year OS of 40% in patients with CDX2-negative tumors versus 70% in those with CDX2-positive tumors. Treatment of CDX2-negative patients with adjuvant chemotherapy improved outcomes: 5-year DFS in the stage II subgroup was 91% with chemotherapy versus 56% without, and in the stage III subgroup, 74% with chemotherapy versus 37% without. The authors concluded that patients with stage II and III colon cancer that is CDX2-negative may benefit from adjuvant chemotherapy. Importantly, CDX2-negativity is a rare event, occurring in only 6.9% of evaluable tumors.
RISK ASSESSMENT TOOLS
Several risk assessment tools have been developed in an attempt to aid clinical decision making regarding adjuvant chemotherapy for patients with stage II colon cancer. The Oncotype DX Colon Assay analyses a 12-gene signature in the pathologic sample and was developed with the goal to improve prognostication and aid in treatment decision making. The test utilizes reverse transcription-PCR on RNA extracted from the tumor.64 After evaluating 12 genes, a recurrence score is generated that predicts the risk of disease recurrence. This score was validated using data from 3 large clinical trials.65–67 Unlike the Oncotype Dx score used in breast cancer, the test in colon cancer has not been found to predict the benefit from chemotherapy and has not been incorporated widely into clinical practice.
Adjuvant! Online (available at www.adjuvantonline.com) is a web-based tool that combines clinical and histological features to estimate outcome. Calculations are based on US SEER tumor registry-reported outcomes.68 A second web-based tool, Numeracy (available at www.mayoclinic.com/calcs), was developed by the Mayo Clinic using pooled data from 7 randomized clinical trials including 3341 patients.68 Both tools seek to predict absolute benefit for patients treated with fluorouracil, though data suggests Adjuvant! Online may be more reliable in its predictive ability.69 Adjuvant! Online has also been validated in an Asian population70 and patients older than 70 years.71
MUTATIONAL ANALYSIS
Multiple mutations in proto-oncogenes have been found in colon cancer cells. One such proto-oncogene is BRAF, which encodes a serine-threonine kinase in the rapidly accelerated fibrosarcoma (RAF). Mutations in BRAF have been found in 5% to 10% of colon cancers and are associated with right-sided tumors.72 As a prognostic marker, some studies have associated BRAF mutations with worse prognosis, including shorter time to relapse and shorter OS.73,74 Two other proto-oncogenes are Kristen rat sarcoma viral oncogene homolog (KRAS) and neuroblastoma rat sarcoma viral oncogene homolog (NRAS), both of which encode proteins downstream of epidermal growth factor receptor (EGFR). KRAS and NRAS mutations have been shown to be predictive in the metastatic setting where they predict resistance to the EGFR inhibitors cetuximab and panitumumab.75,76 The effect of KRAS and NRAS mutations on outcome in stage II and III colon cancer is uncertain. Some studies suggest worse outcome in KRAS-mutated cancers,77 while others failed to demonstrate this finding.73
CASE PRESENTATION 1
A 53-year-old man with no past medical history presents to the emergency department with early satiety and generalized abdominal pain. Laboratory evaluation shows a microcytic anemia with normal white blood cell count, platelet count, renal function, and liver function tests. Computed tomography (CT) scan of the abdomen and pelvis show a 4-cm mass in the transverse colon without obstruction and without abnormality in the liver. CT scan of the chest does not demonstrate pathologic lymphadenopathy or other findings. He undergoes robotic laparoscopic transverse colon resection and appendectomy. Pathology confirms a 3.5-cm focus of adenocarcinoma of the colon with invasion through the muscularis propria and 5 of 27 regional lymph nodes positive for adenocarcinoma and uninvolved proximal, distal, and radial margins. He is given a stage of IIIB pT3 pN2a M0 and referred to medical oncology for further management, where 6 months of adjuvant FOLFOX chemotherapy is recommended.
ADJUVANT CHEMOTHERAPY IN STAGE III COLON CANCER
Postoperative adjuvant chemotherapy is the standard of care for patients with stage III disease. In the 1960s, infusional fluorouracil was first used to treat inoperable colon cancer.78,79 After encouraging results, the agent was used both intraluminally and intravenously as an adjuvant therapy for patients undergoing resection with curative intent; however, only modest benefits were described.80,81 The National Surgical Adjuvant Breast and Bowel Project (NSABP) C-01 trial (Table 3) was the first study to demonstrate a benefit from adjuvant chemotherapy in colon cancer. This study randomly assigned patients with stage II and III colon cancer to surgery alone, postoperative chemotherapy with fluorouracil, semustine, and vincristine (MOF), or postoperative bacillus Calmette-Guérin (BCG). DFS and OS were significantly improved with MOF chemotherapy.82 In 1990, a landmark study reported on outcomes after treatment of 1296 patients with stage III colon cancer with adjuvant fluorouracil and levamisole for 12 months. The combination was associated with a 41% reduction in risk of cancer recurrence and a 33% reduction in risk of death.83 The NSABP C-03 trial (Table 3) compared MOF to the combination of fluorouracil and leucovorin and demonstrated improved 3-year DFS (69% versus 73%) and 3-year OS (77% versus 84%) in patients with stage III disease.84 Building on these outcomes, the QUASAR study (Table 3) compared fluorouracil in combination with one of levamisole, low-dose leucovorin, or high-dose leucovorin. The study enrolled 4927 patients and found worse outcomes with fluorouracil plus levamisole and no difference in low-doseversus high-dose leucovorin.85 Levamisole fell out of use after associations with development of multifocal leukoencephalopathy,86 and was later shown to have inferior outcomes versus leucovorin when combined with fluorouracil.87,88 Intravenous fluorouracil has shown similar benefit when administered by bolus or infusion,89 although continuous infusion has been associated with lower incidence of severe toxicity.90 The efficacy of the oral fluoropyrimidine capecitabine has been shown to be equivalent to that of fluorouracil.91
Fluorouracil-based treatment remained the standard of care until the introduction of oxaliplatin in the mid-1990s. After encouraging results in the metastatic setting,92,93 the agent was moved to the adjuvant setting. The MOSAIC trial (Table 3) randomly assigned patients with stage II and III colon cancer to fluorouracil with leucovorin (FULV) versus FOLFOX given once every 2 weeks for 12 cycles. Analysis with respect to stage III patients showed a clear survival benefit, with a 10-year OS of 67.1% with FOLFOX chemotherapy versus 59% with fluorouracil and leucovorin.94,95 The NSABP C-07 (Table 3) trial used a similar trial design but employed bolus fluorouracil. More than 2400 patients with stage II and III colon cancer were randomly assigned to bolus FULV or bolus fluorouracil, leucovorin, and oxaliplatin (FLOX). The addition of oxaliplatin significantly improved outcomes, with 4-year DFS of 67% versus 71.8% for FULV and FLOX, respectively, and a HR of death of 0.80 with FLOX.59,96 The multicenter N016968 trial (Table 3) randomly assigned 1886 patients with stage III colon cancer to adjuvant capecitabine plus oxaliplatin (XELOX) or bolus fluorouracil plus leucovorin (FU/FA). The 3-year DFS was 70.9% versus 66.5% with XELOX and FU/FA, respectively, and 5-year OS was 77.6% versus 74.2%, respectively.97,98
In the metastatic setting, additional agents have shown efficacy, including irinotecan,99,100 bevacizumab,101,102 cetuximab,103,104 and regorafenib.105 This observation led to testing of these agents in earlier stage disease. The CALGB 89803 trial compared fluorouracil, leucovorin, and irinotecan to fluorouracil with leucovorin alone. No benefit in 5-year DFS or OS was seen.106 Similarly, infusional fluorouracil, leucovorin, and irinotecan (FOLFIRI) was not found to improve 5-year DFS as compared to fluorouracil with leucovorin alone in the PETACC-3 trial.107 The NSABP C-08 trial considered the addition of bevacizumab to FOLFOX. When compared to FOLFOX alone, the combination of bevacizumab to FOLFOX had similar 3-year DFS (77.9% versus 75.1%) and 5-year OS (82.5% versus 80.7%).108 This finding was confirmed in the Avant trial.109 The addition of cetuximab to FOLFOX was equally disappointing, as shown in the N0147 trial110 and PETACC-8 trial.111 Data on regorafenib in the adjuvant setting for stage III colon cancer is lacking; however, 2 ongoing clinical trials, NCT02425683 and NCT02664077, are each studying the use of regorafenib following completion of FOLFOX for patients with stage III disease.
Thus, after multiple trials comparing various regimens and despite attempts to improve outcomes by the addition of a third agent, the standard of care per National Comprehensive Cancer Network (NCCN) guidelines for management of stage III colon cancer remains 12 cycles of FOLFOX chemotherapy. Therapy should be initiated within 8 weeks of surgery. Data are emerging to support a short duration of therapy for patients with low-risk stage III tumors, as shown in an abstract presented at the 2017 American Society of Clinical Oncology annual meeting. The IDEA trial was a pooled analysis of 6 randomized clinical trials across multiple countries, all of which evaluated 3 versus 6 months of FOLFOX or capecitabine and oxaliplatin in the treatment of stage III colon cancer. The analysis was designed to test non-inferiority of 3 months of therapy as compared to 6 months. The analysis included 6088 patients across 244 centers in 6 countries. The overall analysis failed to establish noninferiority. The 3-year DFS rate was 74.6% for 3 months and 75.5% for 6 months, with a DFS HR of 1.07 and a confidence interval that did not meet the prespecified endpoint. Subgroup analysis suggested noninferiority for lower stage disease (T1–3 or N1) but not for higher stage disease (T4 or N2). Given the high rates of neuropathy with 6 months of oxaliplatin, these results suggest that 3 months of adjuvant therapy can be considered for patients with T1–3 or N1 disease in an attempt to limit toxicity.112
CASE PRESENTATION 2
A 57-year-old woman presents to the emergency department with fever and abdominal pain. CT of the abdomen and pelvis demonstrates a left-sided colonic mass with surrounding fat stranding and pelvic abscess. She is taken emergently for left hemicolectomy, cholecystectomy, and evacuation of pelvic abscess. Pathology reveals a 5-cm adenocarcinoma with invasion through the visceral peritoneum; 0/22 lymph nodes are involved. She is given a diagnosis of stage IIC and referred to medical oncology for further management. Due to her young age and presence of high-risk features, she is recommended adjuvant therapy with FOLFOX for 6 months.
ADJUVANT CHEMOTHERAPY IN STAGE II COLON CANCER
Because of excellent outcomes with surgical resection alone for stage II cancers, the use of adjuvant chemotherapy for patients with stage II disease is controversial. Limited prospective data is available to guide adjuvant treatment decisions for stage II patients. The QUASAR trial, which compared observation to adjuvant fluorouracil and leucovorin in patients with early-stage colon cancer, included 2963 patients with stage II disease and found a relative risk (RR) of death or recurrence of 0.82 and 0.78, respectively. Importantly, the absolute benefit of therapy was less than 5%.113 The IMPACT-B2 trial (Table 3) combined data from 5 separate trials and analyzed 1016 patients with stage II colon cancer who received fluorouracil with leucovorin or observation. Event-free survival was 0.86 versus 0.83 and 5-year OS was 82% versus 80%, suggesting no benefit.114 The benefit of addition of oxaliplatin to fluorouracil in stage II disease appears to be less than the benefit of adding this agent in the treatment of stage III CRC. As noted above, the MOSAIC trial randomly assigned patients with stage II and III colon cancer to receive adjuvant fluorouracil and leucovorin with or without oxaliplatin for 12 cycles. After a median follow-up of 9.5 years, 10-year OS rates for patients with stage II disease were 78.4% versus 79.5%. For patients with high-risk stage II disease (defined as T4, bowel perforation, or fewer than 10 lymph nodes examined), 10-year OS was 71.7% and 75.4% respectively, but these differences were not statistically significant.94
Because of conflicting data as to the benefit of adding oxaliplatin in stage II disease, oxaliplatin is not recommended for standard-risk stage II patients. The use of oxaliplatin in high-risk stage II tumors should be weighed carefully given the toxicity risk. Oxaliplatin is recognized to cause sensory neuropathy in many patients, which can become painful and debilitating.115 Two types of neuropathy are associated with oxaliplatin: acute and chronic. Acute neuropathy manifests most often as cold-induced paresthesias in the fingers and toes and is quite common, affecting up to 90% of patients. These symptoms are self-limited and resolve usually within 1 week of each treatment.116 Some patients, with reports ranging from 10% to 79%, develop chronic neuropathy that persists for 1 year or more and causes significant decrements in quality of life.117 Patients older than age 70 may be at greater risk for oxaliplatin-induced neuropathy, which would increase risk of falls in this population.118 In addition to neuropathy, oxaliplatin is associated with hypersensitivity reactions that can be severe and even fatal.119 In a single institution series, the incidence of severe reactions was 2%.120 Desensitization following hypersensitivity reactions is possible but requires a time-intensive protocol.121
Based on the inconclusive efficacy findings and due to concerns over toxicity, each decision must be individualized to fit patient characteristics and preferences. In general, for patients with stage II disease without high-risk features, an individualized discussion should be held as to the risks and benefits of single-agent fluorouracil, and this treatment should be offered in cases where the patient or provider would like to be aggressive. Patients with stage II cancer who have 1 or more high-risk features are often recommended adjuvant chemotherapy. Whether treatment with fluorouracil plus leucovorin or FOLFOX is preferred remains uncertain, and thus the risks and the potential gains of oxaliplatin must be discussed with the individual patient. MMR status can also influence the treatment recommendation for patients with stage II disease. In general, patients with standard-risk stage II tumors that are pMMR are offered MMR with leucovorin or oral capecitabine for 12 cycles. FOLFOX is considered for patients with MSI-high disease and those with multiple high-risk features.
MONITORING AFTER THERAPY
After completion of adjuvant chemotherapy, patients enter a period of survivorship. Patients are seen in clinic for symptom and laboratory monitoring of the complete blood count, liver function tests, and carcinoembryonic antigen (CEA). NCCN guidelines support history and physical examination with CEA testing every 3 to 6 months for the first 2 years, then every 6 months for the next 3 years, after which many patients continue to be seen annually. CT imaging of the chest, abdomen, and pelvis for monitoring of disease recurrence is recommended every 6 to 12 months for a total of 5 years. New elevations in CEA or liver function tests should prompt early imaging. Colonoscopy should be performed 1 year after completion of therapy; however, if no preoperative colonoscopy was performed, this should be done 3 to 6 months after completion. Colonoscopy is then repeated in 3 years and then every 5 years unless advanced adenomas are present.122
SUMMARY
The addition of chemotherapy to surgical management of colon cancer has lowered the rate of disease recurrence and improved long-term survival. Adjuvant FOLFOX for 12 cycles is the standard of care for patients with stage III colon cancer and for patients with stage II disease with certain high-risk features. Use of adjuvant chemotherapy in stage II disease without high-risk features is controversial, and treatment decisions should be individualized. Biologic markers such as MSI and CDX2 status as well as patient-related factors including age, overall health, and personal preferences can inform treatment decisions. If chemotherapy is recommended in this setting, it would be with single-agent fluorouracil in an infusional or oral formulation, unless the tumor has the MSI-high feature. Following completion of adjuvant therapy, patients should be followed with clinical evaluation, laboratory testing, and imaging for a total of 5 years as per recommended guidelines.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67(1):7–30.
- United States Cancer Statistics. 1999–2013 incidence and mortality web-based report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2016. www.cdc.gov/uscs. Accessed June 12, 2017.
- Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc 2014;89:216–24.
- Jemal A, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst 2017;109(8).
- Boursi B, Sella T, Liberman E, et al. The APC p.I1307K polymorphism is a significant risk factor for CRC in average risk Ashkenazi Jews. Eur J Cancer 2013;49:3680–5.
- Parry S, Win AK, Parry B, et al. Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 2011;60: 950–7.
- van Puijenbroek M, Nielsen M, Tops CM, et al. Identification of patients with (atypical) MUTYH-associated polyposis by KRAS2 c.34G > T prescreening followed by MUTYH hotspot analysis in formalin-fixed paraffin-embedded tissue. Clin Cancer Res 2008;14:139–42.
- Aretz S, Uhlhaas S, Goergens H, et al. MUTYH-associated polyposis: 70 of 71 patients with biallelic mutations present with an attenuated or atypical phenotype. Int J Cancer 2006;119:807–14.
- Tuohy TM, Rowe KG, Mineau GP, et al. Risk of colorectal cancer and adenomas in the families of patients with adenomas: a population-based study in Utah. Cancer 2014;120:35–42.
- Choi Y, Sateia HF, Peairs KS, Stewart RW. Screening for colorectal cancer. Semin Oncol 2017; 44:34–44.
- Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med 1992;326:658–62.
- Rutter MD. Surveillance programmes for neoplasia in colitis. J Gastroenterol 2011;46 Suppl 1:1–5.
- Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am 2002;31:925–43.
- Michels KB, Fuchs GS, Giovannucci E, et al. Fiber intake and incidence of colorectal cancer among 76,947 women and 47,279 men. Cancer Epidemiol Biomarkers Prev 2005;14:842–9.
- Omata F, Brown WR, Tokuda Y, et al. Modifiable risk factors for colorectal neoplasms and hyperplastic polyps. Intern Med 2009;48:123–8.
- Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer 2010;46:2593–604.
- Aleksandrova K, Pischon T, Jenab M, et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med 2014;12:168.
- Hermanek P, Wittekind C. The pathologist and the residual tumor (R) classification. Pathol Res Pract 1994;190:115–23.
- Lehnert T, Methner M, Pollok A, et al. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg 2002;235:217–25.
- Feinberg AE, et al. Oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis. Dis Colon Rectum 2017;60:116–125.
- Vignali A, et al. Laparoscopic treatment of advanced colonic cancer: a case-matched control with open surgery. Colorectal Dis 2013;15:944–8.
- Gainant A. Emergency management of acute colonic cancer obstruction. J Visc Surg 2012;149: e3–e10.
- Rosenman LD. Hartmann’s operation. Am J Surg 1994;168:283–4.
- Lee-Kong S, Lisle D. Surgical management of complicated colon cancer. Clin Colon Rectal Surg 2015;28:228–33.
- Bertelsen CA. Complete mesocolic excision an assessment of feasibility and outcome. Dan Med J 2017;64(2).
- Wolff WI SH. Definitive treatment of “malignant” polyps of the colon. Ann Surg 1975;182:516–25.
- Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–9.
- Gunderson LL, Jessup JM, Sarjent DJ, et al. Revised tumor and node categorization for rectal cancer based on surveillance, epidemiology, and end results and rectal pooled analysis outcomes. J Clin Oncol 2010;28:256–63.
- Noone AM, Cronin KA, Altekruse SF, et al. Cancer incidence and survival trends by subtype using data from the Surveillance Epidemiology and End Results Program, 1992-2013. Cancer Epidemiol Biomarkers Prev 2017;26:632–41.
- Alves A, Panis Y, Mathieu P, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg 2005;140:278–83.
- Popescu RA, Norman A, Ross PJ, et al, Adjuvant or palliative chemotherapy for colorectal cancer in patients 70 years or older. J Clin Oncol 1999;17:2412–8.
- McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
- Tominaga T, Nonaka T, Sumida Y, et al. Effectiveness of adjuvant chemotherapy for elderly patients with lymph node-positive colorectal cancer. World J Surg Oncol 2016;14:197.
- Bos AC, van Erning FN, van Gestel YR, et al. Timing of adjuvant chemotherapy and its relation to survival among patients with stage III colon cancer. Eur J Cancer 2015;51:2553–61.
- Peixoto RD, Kumar A, Speers C, et al. Effect of delay in adjuvant oxaliplatin-based chemotherapy for stage III colon cancer. Clin Colorectal Cancer 2015;14:25–30.
- Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:979–94.
- Lieu CH, Lambert LA, Wolff RA, et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol 2012;23:652–8.
- Krasna MJ, Flancbaum L, Cody RP, et al. Vascular and neural invasion in colorectal carcinoma. Incidence and prognostic significance. Cancer 1988;61:1018–23.
- Cianchi F, Palomba A, Boddi V, et al. Lymph node recovery from colorectal tumor specimens: recommendation for a minimum number of lymph nodes to be examined. World J Surg 2002;26:384–9.
- Yoshimatsu K, et al. How many lymph nodes should be examined in Dukes’ B colorectal cancer? Determination on the basis of cumulative survival rate. Hepatogastroenterology 2005;52:1703–6.
- Caplin S, Cerottini JP, Bosman FT, et al. For patients with Dukes’ B (TNM Stage II) colorectal carcinoma, examination of six or fewer lymph nodes is related to poor prognosis. Cancer 1998;83:666–72.
- Veronese N, Nottegar A, Pea A, et al. Prognostic impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol 2016;27:42–8.
- Li J, Yang S, Hu J, et al. Tumor deposits counted as positive lymph nodes in TNM staging for advanced colorectal cancer: a retrospective multicenter study. Oncotarget 2016;7:18269–79.
- Venook A, Niedzwiecki D, Innocenti Fet al. Impact of primary (1º) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol 2016;34 no. 15 suppl. Abstract 3504.
- Schrag D, Brooks G, Meyerhardt JA ,et al. The relationship between primary tumor sidedness and prognosis in colorectal cancer. J Clin Oncol 2016;34 no. 15 suppl. Abstract 3505.
- Larrea AA, Lujan SA, Kunkel TA. SnapShot: DNA mismatch repair. Cell 2010;141:730 e1.
- Jass JR. Pathology of hereditary nonpolyposis colorectal cancer. Ann N Y Acad Sci 2000;910:62–73.
- Lynch HT, Smyrk T. Hereditary nonpolyposis colorectal cancer (Lynch syndrome). An updated review. Cancer 1996;78:1149–67.
- Aaltonen LA, Peltomäki P, Leach FS, et al. Clues to the pathogenesis of familial colorectal cancer. Science 1993;260:812–6.
- Chen W, Swanson BJ, Frankel WL. Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn Pathol 2017;12:24.
- Bupathi M, Wu C. Biomarkers for immune therapy in colorectal cancer: mismatch-repair deficiency and others. J Gastrointest Oncol 2016;7:713–20.
- Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
- Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
- Ogino S, Kuchiba A, Qian ZR, et al. Prognostic significance and molecular associations of 18q loss of heterozygosity: a cohort study of microsatellite stable colorectal cancers. J Clin Oncol 2009; 27:4591–8.
- Kim ST, Lee J, Park SH, et al. The effect of DNA mismatch repair (MMR) status on oxaliplatin-based first-line chemotherapy as in recurrent or metastatic colon cancer. Med Oncol 2010;27:1277–85.
- Sargent DJ, Monges G, Thibodeau SN, et al. Therapy in colon cancer. J Clin Oncol 2010;28:4664.
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
- Hutchins G, Southward K, Handley K, et al. Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 2011;29:1261–270.
- Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses J Clin Oncol 2011;29:3768–74.
- Chang SC, Lin JK, Lin TC, Liang WY. Loss of heterozygosity: an independent prognostic factor of colorectal cancer. World J Gastroenterol 2005;11:778–84.
- Bertagnolli MM, Niedzwiecki D, Compton CC, et al. Microsatellite instability predicts improved response to adjuvant therapy with irinotecan, fluorouracil, and leucovorin in stage III colon cancer: Cancer and Leukemia Group B Protocol 89803. J Clin Oncol 2009;27:1814–21.
- Bertagnolli MM, Redston M, Compton CC, et al. Microsatellite instability and loss of heterozygosity at chromosomal location 18q: prospective evaluation of biomarkers for stages II and III colon cancer--a study of CALGB 9581 and 89803. J Clin Oncol 2011;29:3153–62.
- Dalerba P, et al. CDX2 as a prognostic biomarker in stage II and stage III colon cancer. N Engl J Med 2016;374: 211–22.
- Clark-Langone KM, Wu JY, Sangli C, et al. Biomarker discovery for colon cancer using a 761 gene RT-PCR assay. BMC Genomics 2007;8:279.
- Gray RG, Quirke P, Handley K, et al. Validation study of a quantitative multigene reverse transcriptase-polymerase chain reaction assay for assessment of recurrence risk in patients with stage II colon cancer. J Clin Oncol 2011;29:4611–9.
- Niedzwiecki D, Bertagnolli MM, Warren RS, et al. Documenting the natural history of patients with resected stage II adenocarcinoma of the colon after random assignment to adjuvant treatment with edrecolomab or observation: results from CALGB 9581. J Clin Oncol 2011;29:3146–52.
- Yothers G, O’Connell MJ, Lee M, et al. Validation of the 12-gene colon cancer recurrence score in NSABP C-07 as a predictor of recurrence in patients with stage II and III colon cancer treated with fluorouracil and leucovorin (FU/LV) and FU/LV plus oxaliplatin. J Clin Oncol 2013;31:4512–9.
- Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
- Gill S, Loprinzi C, Kennecke H, et al. Prognostic web-based models for stage II and III colon cancer: A population and clinical trials-based validation of numeracy and adjuvant! online. Cancer 2011;117:4155–65.
- Jung M, Kim GW, Jung I, et al. Application of the Western-based adjuvant online model to Korean colon cancer patients; a single institution experience. BMC Cancer 2012;12:471.
- Papamichael D, Renfro LA, Matthaiou C, et al. Validity of Adjuvant! Online in older patients with stage III colon cancer based on 2967 patients from the ACCENT database. J Geriatr Oncol 2016;7:422–9.
- Tran B, Kopetz S, Tie J, et al. Impact of BRAF mutation and microsatellite instability on the pattern of metastatic spread and prognosis in metastatic colorectal cancer. Cancer 2011;117:4623–32.
- Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol 2010;28:466–74.
- Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
- Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res 2007;67:2643–8.
- Therkildsen C, Bergmann TK, Henrichsen-Schnack T, et al. The predictive value of KRAS, NRAS, BRAF, PIK3CA and PTEN for anti-EGFR treatment in metastatic colorectal cancer: A systematic review and meta-analysis. Acta Oncol 2014;53:852–64.
- Taieb J, Le Malicot K, Shi Q, et al. Prognostic value of BRAF and KRAS mutations in MSI and MSS stage III colon cancer. J Natl Cancer Inst 2017;109(5).
- Palumbo LT, Sharpe WS, Henry JS. Cancer of the colon and rectum; analysis of 300 cases. Am J Surg 1965;109:439–44.
- Sharp GS, Benefiel WW. 5-Fluorouracil in the treatment of inoperable carcinoma of the colon and rectum. Cancer Chemother Rep 1962;20:97–101.
- Lawrence W Jr, Terz JJ, Horsley JS 3rd, et al. Chemotherapy as an adjuvant to surgery for colorectal cancer. Ann Surg 1975;181:616–23.
- Grage TD, et al. Adjuvant chemotherapy with 5-fluorouracil after surgical resection of colorectal carcinoma (COG protocol 7041). A preliminary report. Am J Surg 1977;133:59–66.
- Wolmark N, Fisher B, Rockette H, et al. Postoperative adjuvant chemotherapy or BCG for colon cancer: results from NSABP protocol C-01. J Natl Cancer Inst 1988;80:30–6.
- Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med 1990;322:352–8.
- Wolmark N, Rockette H, Fisher B, et al. The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol 1993;11:1879–87.
- Comparison of fluorouracil with additional levamisole, higher-dose folinic acid, or both, as adjuvant chemotherapy for colorectal cancer: a randomised trial. QUASAR Collaborative Group. Lancet 2000;355(9215):1588–96.
- Chen TC, Hinton DR, Leichman L, et al. Multifocal inflammatory leukoencephalopathy associated with levamisole and 5-fluorouracil: case report. Neurosurgery 1994;35:1138-42.
- Porschen R, Bermann A, Löffler T, et al. Fluorouracil plus leucovorin as effective adjuvant chemotherapy in curatively resected stage III colon cancer: results of the trial adjCCA-01. J Clin Oncol 2001;19:1787–94.
- Arkenau HT, Bermann A, Rettig K, et al. 5-Fluorouracil plus leucovorin is an effective adjuvant chemotherapy in curatively resected stage III colon cancer: long-term follow-up results of the adjCCA-01 trial. Ann Oncol 2003;14:395–9.
- Weinerman B, Shah A, Fields A, et al. Systemic infusion versus bolus chemotherapy with 5-fluorouracil in measurable metastatic colorectal cancer. Am J Clin Oncol 1992;15:518–23.
- Poplin EA, Benedetti JK, Estes NC, et al. Phase III Southwest Oncology Group 9415/Intergroup 0153 randomized trial of fluorouracil, leucovorin, and levamisole versus fluorouracil continuous infusion and levamisole for adjuvant treatment of stage III and high-risk stage II colon cancer. J Clin Oncol 2005;23:1819–25.
- Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
- de Gramont A, Vignoud J, Tournigand C, et al. Oxaliplatin with high-dose leucovorin and 5-fluorouracil 48-hour continuous infusion in pretreated metastatic colorectal cancer. Eur J Cancer 1997;33:214–9.
- Diaz-Rubio E, Sastre J, Zaniboni A, et al. Oxaliplatin as single agent in previously untreated colorectal carcinoma patients: a phase II multicentric study. Ann Oncol 1998;9:105–8.
- André T, de Gramont A, Vernerey D, et al. Adjuvant fluorouracil, leucovorin, and oxaliplatin in Stage II to III Colon Cancer: Updated 10-Year Survival and Outcomes According to BRAF mutation and mismatch repair status of the MOSAIC Study. J Clin Oncol 2015;33:4176–87.
- Andre T, Boni C, Mounedji-Boudiaf L, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004;350:2343–51.
- Kuebler JP, Wieand HS, O’Connell MJ, et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol 2007;25:2198–204.
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
- Schmoll HJ, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
- Colucci G, Gebbia V, Paoletti G, et al. Phase III randomized trial of FOLFIRI versus FOLFOX4 in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico Dell’Italia Meridionale. J Clin Oncol 2005;23:4866–75.
- Tournigand C, André T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 2004;22:229–37.
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 2004;350:2335–42.
- Saltz LB, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 2008;26:2013–9.
- Cremolini C, Loupakis F, Ruzzo A, et al. Predictors of benefit in colorectal cancer treated with cetuximab: are we getting “Lost in TranslationAL”? J Clin Oncol 2010;28:e173–4.
- Sorich MJ, Wiese MD, Rowland D, et al. Extended RAS mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann Oncol 2015;26:13–21.
- Grothey A, van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381(9863):303–12.
- Saltz LB, Niedzwiecki D, Hollis D, et al. Irinotecan fluorouracil plus leucovorin is not superior to fluorouracil plus leucovorin alone as adjuvant treatment for stage III colon cancer: results of CALGB 89803. J Clin Oncol 2007;25:3456–61.
- Van Cutsem E, et al. Randomized phase III trial comparing biweekly infusional fluorouracil/leucovorin alone or with irinotecan in the adjuvant treatment of stage III colon cancer: PETACC-3. J Clin Oncol 2009;27:3117–25.
- Allegra CJ, et al. Bevacizumab in stage II-III colon cancer: 5-year update of the National Surgical Adjuvant Breast and Bowel Project C-08 trial. J Clin Oncol 2013;31:359–64.
- de Gramont A, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012;13:1225–33.
- Alberts SR, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA 2012;307:1383–93.
- Taieb J, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:862–73.
- Shi Q, Sobrero AF, Shields AF, et al. Prospective pooled analysis of six phase III trials investigating duration of adjuvant (adjuvant) oxaliplatin-based therapy (3 vs 6 months) for patients (pts) with stage III colon cancer (CC): The IDEA (International Duration Evaluation of Adjuvant chemotherapy) collaboration. In: Proceedings from the American Society of Clinical Oncology; June 1–5, 2017; Chicago. Abstract LBA1.
- Quasar Collaborative Group; Gray R, Barnwell J, McConkey C, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370(9604):2020–9.
- Efficacy of adjuvant fluorouracil and folinic acid in B2 colon cancer. International Multicentre Pooled Analysis of B2 Colon Cancer Trials (IMPACT B2) Investigators. J Clin Oncol 1999;17:1356–63.
- Kidwell KM, et al. Long-term neurotoxicity effects of oxaliplatin added to fluorouracil and leucovorin as adjuvant therapy for colon cancer: results from National Surgical Adjuvant Breast and Bowel Project trials C-07 and LTS-01. Cancer 2012;118:5614–22.
- Beijers AJ, Mols F, Vreugdenhil G. A systematic review on chronic oxaliplatin-induced peripheral neuropathy and the relation with oxaliplatin administration. Support Care Cancer 2014;22:1999–2007.
- Mols F, Beijers T, Lemmens V, et al. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 2013;31:2699–707.
- Raphael MJ, Fischer HD, Fung K, et al. Neurotoxicity outcomes in a population-based cohort of elderly patients treated with adjuvant oxaliplatin for colorectal cancer. Clin Colorectal Cancer 2017 March 24.
- Toki MI, Saif MW, Syrigos KN. Hypersensitivity reactions associated with oxaliplatin and their clinical management. Expert Opin Drug Saf 2014;13:1545–54.
- Siu SW, Chan RT, Au GK. Hypersensitivity reactions to oxaliplatin: experience in a single institute. Ann Oncol 2006;17:259–61.
- Wong JT, Ling M, Patil S, et al. Oxaliplatin hypersensitivity: evaluation, implications of skin testing, and desensitization. J Allergy Clin Immunol Pract 2014;2:40–5.
- Benson AB 3rd, Venook AP, Cederquist L, et al. NCCN Guidelines Colon Cancer Version 2.2017. www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed May 8, 2017.
- Wolmark N, Rockette H, Mamounas E, et al. Clinical trial to assess the relative efficacy of fluorouracil and leucovorin, fluorouracil and levamisole, and fluorouracil, leucovorin, and levamisole in patients with Dukes’ B and C carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project C-04. J Clin Oncol 1999;17:3553–9.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67(1):7–30.
- United States Cancer Statistics. 1999–2013 incidence and mortality web-based report. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2016. www.cdc.gov/uscs. Accessed June 12, 2017.
- Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc 2014;89:216–24.
- Jemal A, Fedewa SA, Anderson WF, et al. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst 2017;109(8).
- Boursi B, Sella T, Liberman E, et al. The APC p.I1307K polymorphism is a significant risk factor for CRC in average risk Ashkenazi Jews. Eur J Cancer 2013;49:3680–5.
- Parry S, Win AK, Parry B, et al. Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 2011;60: 950–7.
- van Puijenbroek M, Nielsen M, Tops CM, et al. Identification of patients with (atypical) MUTYH-associated polyposis by KRAS2 c.34G > T prescreening followed by MUTYH hotspot analysis in formalin-fixed paraffin-embedded tissue. Clin Cancer Res 2008;14:139–42.
- Aretz S, Uhlhaas S, Goergens H, et al. MUTYH-associated polyposis: 70 of 71 patients with biallelic mutations present with an attenuated or atypical phenotype. Int J Cancer 2006;119:807–14.
- Tuohy TM, Rowe KG, Mineau GP, et al. Risk of colorectal cancer and adenomas in the families of patients with adenomas: a population-based study in Utah. Cancer 2014;120:35–42.
- Choi Y, Sateia HF, Peairs KS, Stewart RW. Screening for colorectal cancer. Semin Oncol 2017; 44:34–44.
- Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med 1992;326:658–62.
- Rutter MD. Surveillance programmes for neoplasia in colitis. J Gastroenterol 2011;46 Suppl 1:1–5.
- Giovannucci E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am 2002;31:925–43.
- Michels KB, Fuchs GS, Giovannucci E, et al. Fiber intake and incidence of colorectal cancer among 76,947 women and 47,279 men. Cancer Epidemiol Biomarkers Prev 2005;14:842–9.
- Omata F, Brown WR, Tokuda Y, et al. Modifiable risk factors for colorectal neoplasms and hyperplastic polyps. Intern Med 2009;48:123–8.
- Friedenreich CM, Neilson HK, Lynch BM. State of the epidemiological evidence on physical activity and cancer prevention. Eur J Cancer 2010;46:2593–604.
- Aleksandrova K, Pischon T, Jenab M, et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med 2014;12:168.
- Hermanek P, Wittekind C. The pathologist and the residual tumor (R) classification. Pathol Res Pract 1994;190:115–23.
- Lehnert T, Methner M, Pollok A, et al. Multivisceral resection for locally advanced primary colon and rectal cancer: an analysis of prognostic factors in 201 patients. Ann Surg 2002;235:217–25.
- Feinberg AE, et al. Oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis. Dis Colon Rectum 2017;60:116–125.
- Vignali A, et al. Laparoscopic treatment of advanced colonic cancer: a case-matched control with open surgery. Colorectal Dis 2013;15:944–8.
- Gainant A. Emergency management of acute colonic cancer obstruction. J Visc Surg 2012;149: e3–e10.
- Rosenman LD. Hartmann’s operation. Am J Surg 1994;168:283–4.
- Lee-Kong S, Lisle D. Surgical management of complicated colon cancer. Clin Colon Rectal Surg 2015;28:228–33.
- Bertelsen CA. Complete mesocolic excision an assessment of feasibility and outcome. Dan Med J 2017;64(2).
- Wolff WI SH. Definitive treatment of “malignant” polyps of the colon. Ann Surg 1975;182:516–25.
- Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–9.
- Gunderson LL, Jessup JM, Sarjent DJ, et al. Revised tumor and node categorization for rectal cancer based on surveillance, epidemiology, and end results and rectal pooled analysis outcomes. J Clin Oncol 2010;28:256–63.
- Noone AM, Cronin KA, Altekruse SF, et al. Cancer incidence and survival trends by subtype using data from the Surveillance Epidemiology and End Results Program, 1992-2013. Cancer Epidemiol Biomarkers Prev 2017;26:632–41.
- Alves A, Panis Y, Mathieu P, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg 2005;140:278–83.
- Popescu RA, Norman A, Ross PJ, et al, Adjuvant or palliative chemotherapy for colorectal cancer in patients 70 years or older. J Clin Oncol 1999;17:2412–8.
- McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600–6.
- Tominaga T, Nonaka T, Sumida Y, et al. Effectiveness of adjuvant chemotherapy for elderly patients with lymph node-positive colorectal cancer. World J Surg Oncol 2016;14:197.
- Bos AC, van Erning FN, van Gestel YR, et al. Timing of adjuvant chemotherapy and its relation to survival among patients with stage III colon cancer. Eur J Cancer 2015;51:2553–61.
- Peixoto RD, Kumar A, Speers C, et al. Effect of delay in adjuvant oxaliplatin-based chemotherapy for stage III colon cancer. Clin Colorectal Cancer 2015;14:25–30.
- Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:979–94.
- Lieu CH, Lambert LA, Wolff RA, et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol 2012;23:652–8.
- Krasna MJ, Flancbaum L, Cody RP, et al. Vascular and neural invasion in colorectal carcinoma. Incidence and prognostic significance. Cancer 1988;61:1018–23.
- Cianchi F, Palomba A, Boddi V, et al. Lymph node recovery from colorectal tumor specimens: recommendation for a minimum number of lymph nodes to be examined. World J Surg 2002;26:384–9.
- Yoshimatsu K, et al. How many lymph nodes should be examined in Dukes’ B colorectal cancer? Determination on the basis of cumulative survival rate. Hepatogastroenterology 2005;52:1703–6.
- Caplin S, Cerottini JP, Bosman FT, et al. For patients with Dukes’ B (TNM Stage II) colorectal carcinoma, examination of six or fewer lymph nodes is related to poor prognosis. Cancer 1998;83:666–72.
- Veronese N, Nottegar A, Pea A, et al. Prognostic impact and implications of extracapsular lymph node involvement in colorectal cancer: a systematic review with meta-analysis. Ann Oncol 2016;27:42–8.
- Li J, Yang S, Hu J, et al. Tumor deposits counted as positive lymph nodes in TNM staging for advanced colorectal cancer: a retrospective multicenter study. Oncotarget 2016;7:18269–79.
- Venook A, Niedzwiecki D, Innocenti Fet al. Impact of primary (1º) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). J Clin Oncol 2016;34 no. 15 suppl. Abstract 3504.
- Schrag D, Brooks G, Meyerhardt JA ,et al. The relationship between primary tumor sidedness and prognosis in colorectal cancer. J Clin Oncol 2016;34 no. 15 suppl. Abstract 3505.
- Larrea AA, Lujan SA, Kunkel TA. SnapShot: DNA mismatch repair. Cell 2010;141:730 e1.
- Jass JR. Pathology of hereditary nonpolyposis colorectal cancer. Ann N Y Acad Sci 2000;910:62–73.
- Lynch HT, Smyrk T. Hereditary nonpolyposis colorectal cancer (Lynch syndrome). An updated review. Cancer 1996;78:1149–67.
- Aaltonen LA, Peltomäki P, Leach FS, et al. Clues to the pathogenesis of familial colorectal cancer. Science 1993;260:812–6.
- Chen W, Swanson BJ, Frankel WL. Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn Pathol 2017;12:24.
- Bupathi M, Wu C. Biomarkers for immune therapy in colorectal cancer: mismatch-repair deficiency and others. J Gastrointest Oncol 2016;7:713–20.
- Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609–18.
- Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77.
- Ogino S, Kuchiba A, Qian ZR, et al. Prognostic significance and molecular associations of 18q loss of heterozygosity: a cohort study of microsatellite stable colorectal cancers. J Clin Oncol 2009; 27:4591–8.
- Kim ST, Lee J, Park SH, et al. The effect of DNA mismatch repair (MMR) status on oxaliplatin-based first-line chemotherapy as in recurrent or metastatic colon cancer. Med Oncol 2010;27:1277–85.
- Sargent DJ, Monges G, Thibodeau SN, et al. Therapy in colon cancer. J Clin Oncol 2010;28:4664.
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247–57.
- Hutchins G, Southward K, Handley K, et al. Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol 2011;29:1261–270.
- Yothers G, O’Connell MJ, Allegra CJ, et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses J Clin Oncol 2011;29:3768–74.
- Chang SC, Lin JK, Lin TC, Liang WY. Loss of heterozygosity: an independent prognostic factor of colorectal cancer. World J Gastroenterol 2005;11:778–84.
- Bertagnolli MM, Niedzwiecki D, Compton CC, et al. Microsatellite instability predicts improved response to adjuvant therapy with irinotecan, fluorouracil, and leucovorin in stage III colon cancer: Cancer and Leukemia Group B Protocol 89803. J Clin Oncol 2009;27:1814–21.
- Bertagnolli MM, Redston M, Compton CC, et al. Microsatellite instability and loss of heterozygosity at chromosomal location 18q: prospective evaluation of biomarkers for stages II and III colon cancer--a study of CALGB 9581 and 89803. J Clin Oncol 2011;29:3153–62.
- Dalerba P, et al. CDX2 as a prognostic biomarker in stage II and stage III colon cancer. N Engl J Med 2016;374: 211–22.
- Clark-Langone KM, Wu JY, Sangli C, et al. Biomarker discovery for colon cancer using a 761 gene RT-PCR assay. BMC Genomics 2007;8:279.
- Gray RG, Quirke P, Handley K, et al. Validation study of a quantitative multigene reverse transcriptase-polymerase chain reaction assay for assessment of recurrence risk in patients with stage II colon cancer. J Clin Oncol 2011;29:4611–9.
- Niedzwiecki D, Bertagnolli MM, Warren RS, et al. Documenting the natural history of patients with resected stage II adenocarcinoma of the colon after random assignment to adjuvant treatment with edrecolomab or observation: results from CALGB 9581. J Clin Oncol 2011;29:3146–52.
- Yothers G, O’Connell MJ, Lee M, et al. Validation of the 12-gene colon cancer recurrence score in NSABP C-07 as a predictor of recurrence in patients with stage II and III colon cancer treated with fluorouracil and leucovorin (FU/LV) and FU/LV plus oxaliplatin. J Clin Oncol 2013;31:4512–9.
- Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797–806.
- Gill S, Loprinzi C, Kennecke H, et al. Prognostic web-based models for stage II and III colon cancer: A population and clinical trials-based validation of numeracy and adjuvant! online. Cancer 2011;117:4155–65.
- Jung M, Kim GW, Jung I, et al. Application of the Western-based adjuvant online model to Korean colon cancer patients; a single institution experience. BMC Cancer 2012;12:471.
- Papamichael D, Renfro LA, Matthaiou C, et al. Validity of Adjuvant! Online in older patients with stage III colon cancer based on 2967 patients from the ACCENT database. J Geriatr Oncol 2016;7:422–9.
- Tran B, Kopetz S, Tie J, et al. Impact of BRAF mutation and microsatellite instability on the pattern of metastatic spread and prognosis in metastatic colorectal cancer. Cancer 2011;117:4623–32.
- Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol 2010;28:466–74.
- Lochhead P, Kuchiba A, Imamura Y, et al. Microsatellite instability and BRAF mutation testing in colorectal cancer prognostication. J Natl Cancer Inst 2013;105:1151–6.
- Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F, et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res 2007;67:2643–8.
- Therkildsen C, Bergmann TK, Henrichsen-Schnack T, et al. The predictive value of KRAS, NRAS, BRAF, PIK3CA and PTEN for anti-EGFR treatment in metastatic colorectal cancer: A systematic review and meta-analysis. Acta Oncol 2014;53:852–64.
- Taieb J, Le Malicot K, Shi Q, et al. Prognostic value of BRAF and KRAS mutations in MSI and MSS stage III colon cancer. J Natl Cancer Inst 2017;109(5).
- Palumbo LT, Sharpe WS, Henry JS. Cancer of the colon and rectum; analysis of 300 cases. Am J Surg 1965;109:439–44.
- Sharp GS, Benefiel WW. 5-Fluorouracil in the treatment of inoperable carcinoma of the colon and rectum. Cancer Chemother Rep 1962;20:97–101.
- Lawrence W Jr, Terz JJ, Horsley JS 3rd, et al. Chemotherapy as an adjuvant to surgery for colorectal cancer. Ann Surg 1975;181:616–23.
- Grage TD, et al. Adjuvant chemotherapy with 5-fluorouracil after surgical resection of colorectal carcinoma (COG protocol 7041). A preliminary report. Am J Surg 1977;133:59–66.
- Wolmark N, Fisher B, Rockette H, et al. Postoperative adjuvant chemotherapy or BCG for colon cancer: results from NSABP protocol C-01. J Natl Cancer Inst 1988;80:30–6.
- Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med 1990;322:352–8.
- Wolmark N, Rockette H, Fisher B, et al. The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. J Clin Oncol 1993;11:1879–87.
- Comparison of fluorouracil with additional levamisole, higher-dose folinic acid, or both, as adjuvant chemotherapy for colorectal cancer: a randomised trial. QUASAR Collaborative Group. Lancet 2000;355(9215):1588–96.
- Chen TC, Hinton DR, Leichman L, et al. Multifocal inflammatory leukoencephalopathy associated with levamisole and 5-fluorouracil: case report. Neurosurgery 1994;35:1138-42.
- Porschen R, Bermann A, Löffler T, et al. Fluorouracil plus leucovorin as effective adjuvant chemotherapy in curatively resected stage III colon cancer: results of the trial adjCCA-01. J Clin Oncol 2001;19:1787–94.
- Arkenau HT, Bermann A, Rettig K, et al. 5-Fluorouracil plus leucovorin is an effective adjuvant chemotherapy in curatively resected stage III colon cancer: long-term follow-up results of the adjCCA-01 trial. Ann Oncol 2003;14:395–9.
- Weinerman B, Shah A, Fields A, et al. Systemic infusion versus bolus chemotherapy with 5-fluorouracil in measurable metastatic colorectal cancer. Am J Clin Oncol 1992;15:518–23.
- Poplin EA, Benedetti JK, Estes NC, et al. Phase III Southwest Oncology Group 9415/Intergroup 0153 randomized trial of fluorouracil, leucovorin, and levamisole versus fluorouracil continuous infusion and levamisole for adjuvant treatment of stage III and high-risk stage II colon cancer. J Clin Oncol 2005;23:1819–25.
- Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 2005;352:2696–704.
- de Gramont A, Vignoud J, Tournigand C, et al. Oxaliplatin with high-dose leucovorin and 5-fluorouracil 48-hour continuous infusion in pretreated metastatic colorectal cancer. Eur J Cancer 1997;33:214–9.
- Diaz-Rubio E, Sastre J, Zaniboni A, et al. Oxaliplatin as single agent in previously untreated colorectal carcinoma patients: a phase II multicentric study. Ann Oncol 1998;9:105–8.
- André T, de Gramont A, Vernerey D, et al. Adjuvant fluorouracil, leucovorin, and oxaliplatin in Stage II to III Colon Cancer: Updated 10-Year Survival and Outcomes According to BRAF mutation and mismatch repair status of the MOSAIC Study. J Clin Oncol 2015;33:4176–87.
- Andre T, Boni C, Mounedji-Boudiaf L, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004;350:2343–51.
- Kuebler JP, Wieand HS, O’Connell MJ, et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol 2007;25:2198–204.
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465–71.
- Schmoll HJ, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol 2015;33:3733–40.
- Colucci G, Gebbia V, Paoletti G, et al. Phase III randomized trial of FOLFIRI versus FOLFOX4 in the treatment of advanced colorectal cancer: a multicenter study of the Gruppo Oncologico Dell’Italia Meridionale. J Clin Oncol 2005;23:4866–75.
- Tournigand C, André T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 2004;22:229–37.
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 2004;350:2335–42.
- Saltz LB, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 2008;26:2013–9.
- Cremolini C, Loupakis F, Ruzzo A, et al. Predictors of benefit in colorectal cancer treated with cetuximab: are we getting “Lost in TranslationAL”? J Clin Oncol 2010;28:e173–4.
- Sorich MJ, Wiese MD, Rowland D, et al. Extended RAS mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann Oncol 2015;26:13–21.
- Grothey A, van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381(9863):303–12.
- Saltz LB, Niedzwiecki D, Hollis D, et al. Irinotecan fluorouracil plus leucovorin is not superior to fluorouracil plus leucovorin alone as adjuvant treatment for stage III colon cancer: results of CALGB 89803. J Clin Oncol 2007;25:3456–61.
- Van Cutsem E, et al. Randomized phase III trial comparing biweekly infusional fluorouracil/leucovorin alone or with irinotecan in the adjuvant treatment of stage III colon cancer: PETACC-3. J Clin Oncol 2009;27:3117–25.
- Allegra CJ, et al. Bevacizumab in stage II-III colon cancer: 5-year update of the National Surgical Adjuvant Breast and Bowel Project C-08 trial. J Clin Oncol 2013;31:359–64.
- de Gramont A, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012;13:1225–33.
- Alberts SR, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA 2012;307:1383–93.
- Taieb J, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:862–73.
- Shi Q, Sobrero AF, Shields AF, et al. Prospective pooled analysis of six phase III trials investigating duration of adjuvant (adjuvant) oxaliplatin-based therapy (3 vs 6 months) for patients (pts) with stage III colon cancer (CC): The IDEA (International Duration Evaluation of Adjuvant chemotherapy) collaboration. In: Proceedings from the American Society of Clinical Oncology; June 1–5, 2017; Chicago. Abstract LBA1.
- Quasar Collaborative Group; Gray R, Barnwell J, McConkey C, et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007;370(9604):2020–9.
- Efficacy of adjuvant fluorouracil and folinic acid in B2 colon cancer. International Multicentre Pooled Analysis of B2 Colon Cancer Trials (IMPACT B2) Investigators. J Clin Oncol 1999;17:1356–63.
- Kidwell KM, et al. Long-term neurotoxicity effects of oxaliplatin added to fluorouracil and leucovorin as adjuvant therapy for colon cancer: results from National Surgical Adjuvant Breast and Bowel Project trials C-07 and LTS-01. Cancer 2012;118:5614–22.
- Beijers AJ, Mols F, Vreugdenhil G. A systematic review on chronic oxaliplatin-induced peripheral neuropathy and the relation with oxaliplatin administration. Support Care Cancer 2014;22:1999–2007.
- Mols F, Beijers T, Lemmens V, et al. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol 2013;31:2699–707.
- Raphael MJ, Fischer HD, Fung K, et al. Neurotoxicity outcomes in a population-based cohort of elderly patients treated with adjuvant oxaliplatin for colorectal cancer. Clin Colorectal Cancer 2017 March 24.
- Toki MI, Saif MW, Syrigos KN. Hypersensitivity reactions associated with oxaliplatin and their clinical management. Expert Opin Drug Saf 2014;13:1545–54.
- Siu SW, Chan RT, Au GK. Hypersensitivity reactions to oxaliplatin: experience in a single institute. Ann Oncol 2006;17:259–61.
- Wong JT, Ling M, Patil S, et al. Oxaliplatin hypersensitivity: evaluation, implications of skin testing, and desensitization. J Allergy Clin Immunol Pract 2014;2:40–5.
- Benson AB 3rd, Venook AP, Cederquist L, et al. NCCN Guidelines Colon Cancer Version 2.2017. www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed May 8, 2017.
- Wolmark N, Rockette H, Mamounas E, et al. Clinical trial to assess the relative efficacy of fluorouracil and leucovorin, fluorouracil and levamisole, and fluorouracil, leucovorin, and levamisole in patients with Dukes’ B and C carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project C-04. J Clin Oncol 1999;17:3553–9.