User login
Potential new alternative in CML when TKI therapy fails

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—ABL001, an allosteric inhibitor of BCR-ABL1, has shown early evidence of single-agent activity in a multicenter, first-in-human, first-in-class trial of heavily treated patients with chronic myeloid leukemia (CML) that is resistant to or intolerant of prior tyrosine kinase inhibitors (TKIs), even at the lowest dose evaluated.
ABL001 and classical TKIs exhibit complementary mutation profiles, with ABL001 showing activity against TKI resistance mutations.
When combined with nilotinib in a mouse model of CML, ABL001 prevented the emergence of resistant disease even after treatment was discontinued.
“This produces a new therapeutic concept—that of allosteric inhibition,” said Oliver G. Ottmann, MD, of Cardiff University in the UK.
The ABL001 binding site is located in a region remote from the kinase domain and has the potential to combine with TKIs for greater pharmacologic control of BCR-ABL1.
“This obviously has the opportunity both for combining different treatments and for overcoming resistance to one or the other,” Dr Ottmann added.
Based on preliminary pharmacokinetic data and preclinical evidence, investigators proceeded to evaluate ABL001 in a phase 1 dose-escalation and dose-expansion study.
Their primary objective was to determine the maximum tolerated dose (MTD) in humans and the recommended dose for expansion (RDE). Secondary objectives were to evaluate the safety, tolerability, preliminary anti-CML activity, and pharmacokinetic and pharmacodynamic profile.
Dr Ottmann presented the findings during the 2015 ASH Annual Meeting as abstract 138.*
Study design
Patients received ABL001 orally as a single agent twice a day (BID) continuously until disease progression, unacceptable toxicity, consent withdrawal, or death.
The dose-escalation schema followed a Bayesian logistic regression model based on dose-limiting toxicities during cycle 1. Doses ranged from 10 mg to 200 mg BID.
A subsequent dose-expansion phase was planned to augment the data generated in the dose-escalation phase and to include patients with Ph-positive acute lymphoblastic leukemia resistant or intolerant to prior TKI therapy.
Dr Ottmann noted that there were 2 protocol amendments. The first amendment was made to include a once-daily (QD) dosing of ABL001 at 120 mg and 200 mg. The second amendment was made to evaluate the combination of 40 mg of ABL001 BID with nilotinib at 300 mg BID.
Inclusion/exclusion criteria
Patients had to be at least 18 years old with CML in chronic or accelerated phase. They had to have failed at least 2 prior TKIs or be intolerant of TKIs. Their performance status had to be 0–2.
Patients were excluded from the trial if they had an absolute neutrophil count less than 500/mm3, a platelet count less than 50,000/mm3, bilirubin level more than 1.5 x the upper limit of normal (ULN) or more than 3.0 x ULN in patients with Gilberts syndrome.
Their aspartate aminotransferase or alanine aminotransferase could not be above 3 x ULN, and creatinine could not be above 1.5 x ULN.
Patients were also excluded if they needed treatment with strong inhibitors or inducers of CYP3A4 or its substrates with narrow therapeutic index.
Patient demographics
Fifty-nine patients were enrolled on the trial at the time of the presentation and they had “typical” characteristics of patients at this stage, Dr Ottmann said.
Their median age was 56 (range, 23–78). Almost two-thirds (61%) were male and 39% female.
All but 1 patient had an ECOG performance status of 0, and patients had a median of 3.5 (range, 2–5) prior lines of therapy. Twenty-four patients (41%) had 2 prior TKIs, and 35 (59%) had 3 or more TKIs. Forty-five patients (76%) were resistant and 14 (24%) were intolerant to their prior TKI.
All but 1 patient had chronic phase CML, 18 (31%) were TKD nonmutated, 14 (24%) were mutated, and 17 (46%) were not evaluable.
Patient disposition
Of the 43 patients in the monotherapy BID cohort, 1 was treated at the 10 mg dose level, 5 at the 20 mg level, 12 at the 40 mg level, 12 at the 80 mg level, 8 at the 150 mg level, and 5 at the 200 mg level. They had a median duration of drug exposure ranging from 25 weeks to 67 weeks.
Of the 11 patients in the monotherapy QD group, 5 were treated at the 120 mg dose level and 6 at the 200 mg level. Their drug exposure was a median of 26 weeks for those receiving 120 mg and 9.8 weeks for those receiving the 200 mg dose.
And the 5 patients in the ABL001-plus-nilotinib group had a median of 6.3 weeks of drug exposure.
“We had a remarkably low rate of discontinuation to date,” Dr Ottmann pointed out.
Ten patients discontinued therapy, all in the monotherapy BID group, 1 at 10 mg, 2 at 40 mg, 2 at 80 mg, 3 at 150 mg, and 2 at 200 mg.
Seven patients discontinued for adverse events. Two patients withdrew consent, and 1 patient in the 40 mg group had disease progression, which is “quite remarkable in a phase 1,” Dr Ottmann said.
Pharmacokinetic profile
ABL001 is rapidly absorbed in a median of 2 to 3 hours, and there is a dose-proportional increase in exposure following single and repeated dosing.
The drug has an approximately 2-fold or lower accumulation on repeated dosing and a short elimination half-life of 5 to 6 hours.
Safety
“We have excellent tolerability,” Dr Ottmann said, with a small number of grade 3/4 adverse events (AEs).
Grade 3/4 AEs considered to be drug-related were mostly associated with hematologic suppression. Four patients (7%) had thrombocytopenia, 4 (7%) neutropenia, 3 (5%) anemia, 4 (7%) lipase increase, and 1 (2%) hypercholesterolemia.
AEs of all grades suspected of being related to the study drug and occurring in 5% or more of patients included thrombocytopenia (19%), neutropenia (15%), anemia (10%), nausea/vomiting/diarrhea (29%), arthralgia/myalgia (20%), rash (17%), fatigue (15%), lipase increase (14%), headache (14%), pruritus (10%), dry skin (7%), hypophosphatemia (7%), and acute pancreatitis (5%).
“The pancreatitis was reversible upon interruption or discontinuation of the drug,” Dr Ottmann explained.
There were 5 dose-limiting toxicities. Two patients had grade 3 lipase elevation in the 40 mg BID and 200 mg QD cohorts. One patient had grade 2 myalgia/arthralgia at 80 mg BID, 1 patient had a grade 3 acute coronary event at 150 mg BID, and 1 patient had a grade 3 bronchospasm at 200 mg BID.
No deaths occurred on the study, and the dose escalation is still ongoing.
Response
Twenty-nine patients with 3 months or more of follow-up were evaluable for response.
Twelve patients, who at baseline had hematologic relapse, achieved complete hematologic response within 2 months, and 8 who had cytogenetic relapse at baseline achieved a complete cytogenetic response within 3 to 6 months.
Of the 29 patients who had molecular relapse at baseline, 10 (34.5%) achieved a molecular response within 6 months, 7 (24.1%) had 1 log or more reduction in BCR-ABL1, 9 (31.0%) had less than a log reduction, and 3 (10.3%) had no reduction.
“The obvious question from the preclinical data,” Dr Ottmann said, “is do the mutations respond?”
And ABL001 has shown clinical activity across TKI-resistant mutations, such as V299L, F317L, and Y253H.
“So to conclude,” he said, “we have a new class, a new therapeutic category of drug, ABL001, which is quite well tolerated in extremely heavily treated patients with CML. We do consider this a promising approach.”
The trial was sponsored by Novartis. ![]()
*Data in the abstract differ from the presentation.

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—ABL001, an allosteric inhibitor of BCR-ABL1, has shown early evidence of single-agent activity in a multicenter, first-in-human, first-in-class trial of heavily treated patients with chronic myeloid leukemia (CML) that is resistant to or intolerant of prior tyrosine kinase inhibitors (TKIs), even at the lowest dose evaluated.
ABL001 and classical TKIs exhibit complementary mutation profiles, with ABL001 showing activity against TKI resistance mutations.
When combined with nilotinib in a mouse model of CML, ABL001 prevented the emergence of resistant disease even after treatment was discontinued.
“This produces a new therapeutic concept—that of allosteric inhibition,” said Oliver G. Ottmann, MD, of Cardiff University in the UK.
The ABL001 binding site is located in a region remote from the kinase domain and has the potential to combine with TKIs for greater pharmacologic control of BCR-ABL1.
“This obviously has the opportunity both for combining different treatments and for overcoming resistance to one or the other,” Dr Ottmann added.
Based on preliminary pharmacokinetic data and preclinical evidence, investigators proceeded to evaluate ABL001 in a phase 1 dose-escalation and dose-expansion study.
Their primary objective was to determine the maximum tolerated dose (MTD) in humans and the recommended dose for expansion (RDE). Secondary objectives were to evaluate the safety, tolerability, preliminary anti-CML activity, and pharmacokinetic and pharmacodynamic profile.
Dr Ottmann presented the findings during the 2015 ASH Annual Meeting as abstract 138.*
Study design
Patients received ABL001 orally as a single agent twice a day (BID) continuously until disease progression, unacceptable toxicity, consent withdrawal, or death.
The dose-escalation schema followed a Bayesian logistic regression model based on dose-limiting toxicities during cycle 1. Doses ranged from 10 mg to 200 mg BID.
A subsequent dose-expansion phase was planned to augment the data generated in the dose-escalation phase and to include patients with Ph-positive acute lymphoblastic leukemia resistant or intolerant to prior TKI therapy.
Dr Ottmann noted that there were 2 protocol amendments. The first amendment was made to include a once-daily (QD) dosing of ABL001 at 120 mg and 200 mg. The second amendment was made to evaluate the combination of 40 mg of ABL001 BID with nilotinib at 300 mg BID.
Inclusion/exclusion criteria
Patients had to be at least 18 years old with CML in chronic or accelerated phase. They had to have failed at least 2 prior TKIs or be intolerant of TKIs. Their performance status had to be 0–2.
Patients were excluded from the trial if they had an absolute neutrophil count less than 500/mm3, a platelet count less than 50,000/mm3, bilirubin level more than 1.5 x the upper limit of normal (ULN) or more than 3.0 x ULN in patients with Gilberts syndrome.
Their aspartate aminotransferase or alanine aminotransferase could not be above 3 x ULN, and creatinine could not be above 1.5 x ULN.
Patients were also excluded if they needed treatment with strong inhibitors or inducers of CYP3A4 or its substrates with narrow therapeutic index.
Patient demographics
Fifty-nine patients were enrolled on the trial at the time of the presentation and they had “typical” characteristics of patients at this stage, Dr Ottmann said.
Their median age was 56 (range, 23–78). Almost two-thirds (61%) were male and 39% female.
All but 1 patient had an ECOG performance status of 0, and patients had a median of 3.5 (range, 2–5) prior lines of therapy. Twenty-four patients (41%) had 2 prior TKIs, and 35 (59%) had 3 or more TKIs. Forty-five patients (76%) were resistant and 14 (24%) were intolerant to their prior TKI.
All but 1 patient had chronic phase CML, 18 (31%) were TKD nonmutated, 14 (24%) were mutated, and 17 (46%) were not evaluable.
Patient disposition
Of the 43 patients in the monotherapy BID cohort, 1 was treated at the 10 mg dose level, 5 at the 20 mg level, 12 at the 40 mg level, 12 at the 80 mg level, 8 at the 150 mg level, and 5 at the 200 mg level. They had a median duration of drug exposure ranging from 25 weeks to 67 weeks.
Of the 11 patients in the monotherapy QD group, 5 were treated at the 120 mg dose level and 6 at the 200 mg level. Their drug exposure was a median of 26 weeks for those receiving 120 mg and 9.8 weeks for those receiving the 200 mg dose.
And the 5 patients in the ABL001-plus-nilotinib group had a median of 6.3 weeks of drug exposure.
“We had a remarkably low rate of discontinuation to date,” Dr Ottmann pointed out.
Ten patients discontinued therapy, all in the monotherapy BID group, 1 at 10 mg, 2 at 40 mg, 2 at 80 mg, 3 at 150 mg, and 2 at 200 mg.
Seven patients discontinued for adverse events. Two patients withdrew consent, and 1 patient in the 40 mg group had disease progression, which is “quite remarkable in a phase 1,” Dr Ottmann said.
Pharmacokinetic profile
ABL001 is rapidly absorbed in a median of 2 to 3 hours, and there is a dose-proportional increase in exposure following single and repeated dosing.
The drug has an approximately 2-fold or lower accumulation on repeated dosing and a short elimination half-life of 5 to 6 hours.
Safety
“We have excellent tolerability,” Dr Ottmann said, with a small number of grade 3/4 adverse events (AEs).
Grade 3/4 AEs considered to be drug-related were mostly associated with hematologic suppression. Four patients (7%) had thrombocytopenia, 4 (7%) neutropenia, 3 (5%) anemia, 4 (7%) lipase increase, and 1 (2%) hypercholesterolemia.
AEs of all grades suspected of being related to the study drug and occurring in 5% or more of patients included thrombocytopenia (19%), neutropenia (15%), anemia (10%), nausea/vomiting/diarrhea (29%), arthralgia/myalgia (20%), rash (17%), fatigue (15%), lipase increase (14%), headache (14%), pruritus (10%), dry skin (7%), hypophosphatemia (7%), and acute pancreatitis (5%).
“The pancreatitis was reversible upon interruption or discontinuation of the drug,” Dr Ottmann explained.
There were 5 dose-limiting toxicities. Two patients had grade 3 lipase elevation in the 40 mg BID and 200 mg QD cohorts. One patient had grade 2 myalgia/arthralgia at 80 mg BID, 1 patient had a grade 3 acute coronary event at 150 mg BID, and 1 patient had a grade 3 bronchospasm at 200 mg BID.
No deaths occurred on the study, and the dose escalation is still ongoing.
Response
Twenty-nine patients with 3 months or more of follow-up were evaluable for response.
Twelve patients, who at baseline had hematologic relapse, achieved complete hematologic response within 2 months, and 8 who had cytogenetic relapse at baseline achieved a complete cytogenetic response within 3 to 6 months.
Of the 29 patients who had molecular relapse at baseline, 10 (34.5%) achieved a molecular response within 6 months, 7 (24.1%) had 1 log or more reduction in BCR-ABL1, 9 (31.0%) had less than a log reduction, and 3 (10.3%) had no reduction.
“The obvious question from the preclinical data,” Dr Ottmann said, “is do the mutations respond?”
And ABL001 has shown clinical activity across TKI-resistant mutations, such as V299L, F317L, and Y253H.
“So to conclude,” he said, “we have a new class, a new therapeutic category of drug, ABL001, which is quite well tolerated in extremely heavily treated patients with CML. We do consider this a promising approach.”
The trial was sponsored by Novartis. ![]()
*Data in the abstract differ from the presentation.

ASH Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—ABL001, an allosteric inhibitor of BCR-ABL1, has shown early evidence of single-agent activity in a multicenter, first-in-human, first-in-class trial of heavily treated patients with chronic myeloid leukemia (CML) that is resistant to or intolerant of prior tyrosine kinase inhibitors (TKIs), even at the lowest dose evaluated.
ABL001 and classical TKIs exhibit complementary mutation profiles, with ABL001 showing activity against TKI resistance mutations.
When combined with nilotinib in a mouse model of CML, ABL001 prevented the emergence of resistant disease even after treatment was discontinued.
“This produces a new therapeutic concept—that of allosteric inhibition,” said Oliver G. Ottmann, MD, of Cardiff University in the UK.
The ABL001 binding site is located in a region remote from the kinase domain and has the potential to combine with TKIs for greater pharmacologic control of BCR-ABL1.
“This obviously has the opportunity both for combining different treatments and for overcoming resistance to one or the other,” Dr Ottmann added.
Based on preliminary pharmacokinetic data and preclinical evidence, investigators proceeded to evaluate ABL001 in a phase 1 dose-escalation and dose-expansion study.
Their primary objective was to determine the maximum tolerated dose (MTD) in humans and the recommended dose for expansion (RDE). Secondary objectives were to evaluate the safety, tolerability, preliminary anti-CML activity, and pharmacokinetic and pharmacodynamic profile.
Dr Ottmann presented the findings during the 2015 ASH Annual Meeting as abstract 138.*
Study design
Patients received ABL001 orally as a single agent twice a day (BID) continuously until disease progression, unacceptable toxicity, consent withdrawal, or death.
The dose-escalation schema followed a Bayesian logistic regression model based on dose-limiting toxicities during cycle 1. Doses ranged from 10 mg to 200 mg BID.
A subsequent dose-expansion phase was planned to augment the data generated in the dose-escalation phase and to include patients with Ph-positive acute lymphoblastic leukemia resistant or intolerant to prior TKI therapy.
Dr Ottmann noted that there were 2 protocol amendments. The first amendment was made to include a once-daily (QD) dosing of ABL001 at 120 mg and 200 mg. The second amendment was made to evaluate the combination of 40 mg of ABL001 BID with nilotinib at 300 mg BID.
Inclusion/exclusion criteria
Patients had to be at least 18 years old with CML in chronic or accelerated phase. They had to have failed at least 2 prior TKIs or be intolerant of TKIs. Their performance status had to be 0–2.
Patients were excluded from the trial if they had an absolute neutrophil count less than 500/mm3, a platelet count less than 50,000/mm3, bilirubin level more than 1.5 x the upper limit of normal (ULN) or more than 3.0 x ULN in patients with Gilberts syndrome.
Their aspartate aminotransferase or alanine aminotransferase could not be above 3 x ULN, and creatinine could not be above 1.5 x ULN.
Patients were also excluded if they needed treatment with strong inhibitors or inducers of CYP3A4 or its substrates with narrow therapeutic index.
Patient demographics
Fifty-nine patients were enrolled on the trial at the time of the presentation and they had “typical” characteristics of patients at this stage, Dr Ottmann said.
Their median age was 56 (range, 23–78). Almost two-thirds (61%) were male and 39% female.
All but 1 patient had an ECOG performance status of 0, and patients had a median of 3.5 (range, 2–5) prior lines of therapy. Twenty-four patients (41%) had 2 prior TKIs, and 35 (59%) had 3 or more TKIs. Forty-five patients (76%) were resistant and 14 (24%) were intolerant to their prior TKI.
All but 1 patient had chronic phase CML, 18 (31%) were TKD nonmutated, 14 (24%) were mutated, and 17 (46%) were not evaluable.
Patient disposition
Of the 43 patients in the monotherapy BID cohort, 1 was treated at the 10 mg dose level, 5 at the 20 mg level, 12 at the 40 mg level, 12 at the 80 mg level, 8 at the 150 mg level, and 5 at the 200 mg level. They had a median duration of drug exposure ranging from 25 weeks to 67 weeks.
Of the 11 patients in the monotherapy QD group, 5 were treated at the 120 mg dose level and 6 at the 200 mg level. Their drug exposure was a median of 26 weeks for those receiving 120 mg and 9.8 weeks for those receiving the 200 mg dose.
And the 5 patients in the ABL001-plus-nilotinib group had a median of 6.3 weeks of drug exposure.
“We had a remarkably low rate of discontinuation to date,” Dr Ottmann pointed out.
Ten patients discontinued therapy, all in the monotherapy BID group, 1 at 10 mg, 2 at 40 mg, 2 at 80 mg, 3 at 150 mg, and 2 at 200 mg.
Seven patients discontinued for adverse events. Two patients withdrew consent, and 1 patient in the 40 mg group had disease progression, which is “quite remarkable in a phase 1,” Dr Ottmann said.
Pharmacokinetic profile
ABL001 is rapidly absorbed in a median of 2 to 3 hours, and there is a dose-proportional increase in exposure following single and repeated dosing.
The drug has an approximately 2-fold or lower accumulation on repeated dosing and a short elimination half-life of 5 to 6 hours.
Safety
“We have excellent tolerability,” Dr Ottmann said, with a small number of grade 3/4 adverse events (AEs).
Grade 3/4 AEs considered to be drug-related were mostly associated with hematologic suppression. Four patients (7%) had thrombocytopenia, 4 (7%) neutropenia, 3 (5%) anemia, 4 (7%) lipase increase, and 1 (2%) hypercholesterolemia.
AEs of all grades suspected of being related to the study drug and occurring in 5% or more of patients included thrombocytopenia (19%), neutropenia (15%), anemia (10%), nausea/vomiting/diarrhea (29%), arthralgia/myalgia (20%), rash (17%), fatigue (15%), lipase increase (14%), headache (14%), pruritus (10%), dry skin (7%), hypophosphatemia (7%), and acute pancreatitis (5%).
“The pancreatitis was reversible upon interruption or discontinuation of the drug,” Dr Ottmann explained.
There were 5 dose-limiting toxicities. Two patients had grade 3 lipase elevation in the 40 mg BID and 200 mg QD cohorts. One patient had grade 2 myalgia/arthralgia at 80 mg BID, 1 patient had a grade 3 acute coronary event at 150 mg BID, and 1 patient had a grade 3 bronchospasm at 200 mg BID.
No deaths occurred on the study, and the dose escalation is still ongoing.
Response
Twenty-nine patients with 3 months or more of follow-up were evaluable for response.
Twelve patients, who at baseline had hematologic relapse, achieved complete hematologic response within 2 months, and 8 who had cytogenetic relapse at baseline achieved a complete cytogenetic response within 3 to 6 months.
Of the 29 patients who had molecular relapse at baseline, 10 (34.5%) achieved a molecular response within 6 months, 7 (24.1%) had 1 log or more reduction in BCR-ABL1, 9 (31.0%) had less than a log reduction, and 3 (10.3%) had no reduction.
“The obvious question from the preclinical data,” Dr Ottmann said, “is do the mutations respond?”
And ABL001 has shown clinical activity across TKI-resistant mutations, such as V299L, F317L, and Y253H.
“So to conclude,” he said, “we have a new class, a new therapeutic category of drug, ABL001, which is quite well tolerated in extremely heavily treated patients with CML. We do consider this a promising approach.”
The trial was sponsored by Novartis. ![]()
*Data in the abstract differ from the presentation.
Osteoarticular pain affects CML patients stopping TKI

Photo courtesy of ASH
ORLANDO, FL—Cases of musculoskeletal pain have been reported after patients stop taking tyrosine kinase inhibitors (TKIs) for chronic myeloid leukemia (CML).
TKI discontinuation trials—notably, the STOP imatinib (STIM) trials and EURO-SKI trial—have been conducted to assess the feasibility of maintaining molecular remission once patients discontinue a TKI.
However, none of the studies collected low-grade events before or after patients discontinued TKI therapy.
So investigators collected data from the STIM2 study and EUROSKI trial and recorded all events from the time of TKI discontinuation.
They discovered that about 23% of patients who stopped TKI therapy experienced a withdrawal syndrome (WS) consisting largely of musculoskeletal pain, regardless of the TKI they were taking.
Philippe Rousselot, MD, PhD, of University of Versailles St-Quentin-en-Yvelines, Versailles, France, discussed this finding at the 2015 ASH Annual Meeting as abstract 137.*
Dr Rousselot noted that investigators first reported the TKI WS in 2014 in CML patients enrolled on the EURO-SKI trial who were discontinuing imatinib (Richter et al, JCO 2014).
A team of French investigators undertook the current observational study to estimate the prevalence of the WS and to identify clinical factors associated with it.
They collected, prospectively, the adverse events from all 428 French patients who were enrolled in the STIM2 (n=204) and EURO-SKI (n=224) trials. And they compared patients who stopped taking TKIs and had a painful WS to those who stopped TKIs and did not have a painful syndrome.
Patient characteristics
Patient characteristics were well balanced between the STIM2 and EURO-SKI groups, with the exception of the median time on TKI before discontinuation. In the STIM2 group, patients were a median of 77.4 months on TKI therapy. In the EURO-SKI group, the median time on a TKI was 100.4 months (P<0.001).
In all, there were 208 male and 220 female patients included. They were a median age of 64 (range, 53–73) and 63 (range, 53–70) years in the STIM2 and EURO-SKI groups, respectively.
Sokal scores were also comparable between the cohorts, with most patients falling in the low and intermediate ranges.
Prevalence and characteristics of WS
Overall, 326 patients (76.2%) were without WS and 102 (23.8%) had WS. In the STIM2 cohort, 193 patients (86.2%) were without WS and 31 (13.8%) had WS. In the EURO-SKI cohort, 133 patients (65.2%) were without WS and 71 (34.8%) had WS.
“And these differences [between cohorts] are significant,” Dr Rousselot pointed out.
Investigators analyzed clinical characteristics of WS in 40 patients and determined that the median time from TKI discontinuation to WS was 21 days, and the median duration of WS was 7 months (range, 3–30).
Pain was located in the shoulder and spine for 67% of the patients and elsewhere in 33%. About two-thirds of patients (62.5%) experienced grade 1–2 pain, and 37.5% experienced grade 3–4 pain.
Nineteen patients resumed TKI therapy, “because of loss of MMR [major molecular response] or loss of clinical response,” Dr Rousselot said.
And the pain disappeared in 52.6% of them when they resumed TKI therapy. The median duration of TKI therapy before WS pain disappeared was 3 weeks.
Risk factors for WS
Investigators determined that CML duration, time on a TKI, and previous history of osteoarticular symptoms were risk factors for WS.
Patients without WS had CML for a shorter time—a mean of 8.7 ± 3.1 months, compared to 9.7 ± 3.8 for those with WS (P=0.02).
Patients without WS were also on a TKI for a shorter time—a median of 81.2 months (range, 61.2–108.0), compared to 97.3 months (range, 73.7–122.9) for those with WS (P<0.001).
Patients with a previous history of osteoarticular symptoms were more likely to experience WS—22.9%, compared to 9.8% without a previous history (P=0.002).
Most patients were receiving imatinib—323 without WS and 100 with WS. The 1 patient receiving dasatinib had no WS. And of the 4 patients receiving nilotinib, 2 had WS and 2 didn’t.
And so the type of TKI therapy—dasatinib, imatinib, or nilotinib—was not significant (P=0.42).
Investigators performed a multivariate analysis adjusted for gender, CML duration, and Sokal score, and 2 risk factors emerged: previous history of osteoarticular symptoms (relative risk: 2.08) and time on TKI (relative risk: 2.23).
Discussion
Dr Rousselot compared the Richter trial (Richter et al, JCO 2014) to the current study and noted that the Richter trial, with an enrollment of 50 patients, had a WS prevalence of 30%. But the current trial had a prevalence of 24%.
The difference in WS may be due to time on TKI, Dr Rousselot said, as patients in the Richter trial were on TKI treatment for a longer period of time.
“The time of onset is the same [in both trials],” Dr Rousselot said, as are the TKI used, location of pain, and duration of pain.
“So what we can say is [with] shorter TKI treatment . . . , we have a higher risk of molecular relapse but a lower risk of withdrawal syndrome.”
And with longer TKI treatment, the converse appears to be true. It reduces the risk of molecular relapse but raises the risk of withdrawal syndrome. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Cases of musculoskeletal pain have been reported after patients stop taking tyrosine kinase inhibitors (TKIs) for chronic myeloid leukemia (CML).
TKI discontinuation trials—notably, the STOP imatinib (STIM) trials and EURO-SKI trial—have been conducted to assess the feasibility of maintaining molecular remission once patients discontinue a TKI.
However, none of the studies collected low-grade events before or after patients discontinued TKI therapy.
So investigators collected data from the STIM2 study and EUROSKI trial and recorded all events from the time of TKI discontinuation.
They discovered that about 23% of patients who stopped TKI therapy experienced a withdrawal syndrome (WS) consisting largely of musculoskeletal pain, regardless of the TKI they were taking.
Philippe Rousselot, MD, PhD, of University of Versailles St-Quentin-en-Yvelines, Versailles, France, discussed this finding at the 2015 ASH Annual Meeting as abstract 137.*
Dr Rousselot noted that investigators first reported the TKI WS in 2014 in CML patients enrolled on the EURO-SKI trial who were discontinuing imatinib (Richter et al, JCO 2014).
A team of French investigators undertook the current observational study to estimate the prevalence of the WS and to identify clinical factors associated with it.
They collected, prospectively, the adverse events from all 428 French patients who were enrolled in the STIM2 (n=204) and EURO-SKI (n=224) trials. And they compared patients who stopped taking TKIs and had a painful WS to those who stopped TKIs and did not have a painful syndrome.
Patient characteristics
Patient characteristics were well balanced between the STIM2 and EURO-SKI groups, with the exception of the median time on TKI before discontinuation. In the STIM2 group, patients were a median of 77.4 months on TKI therapy. In the EURO-SKI group, the median time on a TKI was 100.4 months (P<0.001).
In all, there were 208 male and 220 female patients included. They were a median age of 64 (range, 53–73) and 63 (range, 53–70) years in the STIM2 and EURO-SKI groups, respectively.
Sokal scores were also comparable between the cohorts, with most patients falling in the low and intermediate ranges.
Prevalence and characteristics of WS
Overall, 326 patients (76.2%) were without WS and 102 (23.8%) had WS. In the STIM2 cohort, 193 patients (86.2%) were without WS and 31 (13.8%) had WS. In the EURO-SKI cohort, 133 patients (65.2%) were without WS and 71 (34.8%) had WS.
“And these differences [between cohorts] are significant,” Dr Rousselot pointed out.
Investigators analyzed clinical characteristics of WS in 40 patients and determined that the median time from TKI discontinuation to WS was 21 days, and the median duration of WS was 7 months (range, 3–30).
Pain was located in the shoulder and spine for 67% of the patients and elsewhere in 33%. About two-thirds of patients (62.5%) experienced grade 1–2 pain, and 37.5% experienced grade 3–4 pain.
Nineteen patients resumed TKI therapy, “because of loss of MMR [major molecular response] or loss of clinical response,” Dr Rousselot said.
And the pain disappeared in 52.6% of them when they resumed TKI therapy. The median duration of TKI therapy before WS pain disappeared was 3 weeks.
Risk factors for WS
Investigators determined that CML duration, time on a TKI, and previous history of osteoarticular symptoms were risk factors for WS.
Patients without WS had CML for a shorter time—a mean of 8.7 ± 3.1 months, compared to 9.7 ± 3.8 for those with WS (P=0.02).
Patients without WS were also on a TKI for a shorter time—a median of 81.2 months (range, 61.2–108.0), compared to 97.3 months (range, 73.7–122.9) for those with WS (P<0.001).
Patients with a previous history of osteoarticular symptoms were more likely to experience WS—22.9%, compared to 9.8% without a previous history (P=0.002).
Most patients were receiving imatinib—323 without WS and 100 with WS. The 1 patient receiving dasatinib had no WS. And of the 4 patients receiving nilotinib, 2 had WS and 2 didn’t.
And so the type of TKI therapy—dasatinib, imatinib, or nilotinib—was not significant (P=0.42).
Investigators performed a multivariate analysis adjusted for gender, CML duration, and Sokal score, and 2 risk factors emerged: previous history of osteoarticular symptoms (relative risk: 2.08) and time on TKI (relative risk: 2.23).
Discussion
Dr Rousselot compared the Richter trial (Richter et al, JCO 2014) to the current study and noted that the Richter trial, with an enrollment of 50 patients, had a WS prevalence of 30%. But the current trial had a prevalence of 24%.
The difference in WS may be due to time on TKI, Dr Rousselot said, as patients in the Richter trial were on TKI treatment for a longer period of time.
“The time of onset is the same [in both trials],” Dr Rousselot said, as are the TKI used, location of pain, and duration of pain.
“So what we can say is [with] shorter TKI treatment . . . , we have a higher risk of molecular relapse but a lower risk of withdrawal syndrome.”
And with longer TKI treatment, the converse appears to be true. It reduces the risk of molecular relapse but raises the risk of withdrawal syndrome. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Cases of musculoskeletal pain have been reported after patients stop taking tyrosine kinase inhibitors (TKIs) for chronic myeloid leukemia (CML).
TKI discontinuation trials—notably, the STOP imatinib (STIM) trials and EURO-SKI trial—have been conducted to assess the feasibility of maintaining molecular remission once patients discontinue a TKI.
However, none of the studies collected low-grade events before or after patients discontinued TKI therapy.
So investigators collected data from the STIM2 study and EUROSKI trial and recorded all events from the time of TKI discontinuation.
They discovered that about 23% of patients who stopped TKI therapy experienced a withdrawal syndrome (WS) consisting largely of musculoskeletal pain, regardless of the TKI they were taking.
Philippe Rousselot, MD, PhD, of University of Versailles St-Quentin-en-Yvelines, Versailles, France, discussed this finding at the 2015 ASH Annual Meeting as abstract 137.*
Dr Rousselot noted that investigators first reported the TKI WS in 2014 in CML patients enrolled on the EURO-SKI trial who were discontinuing imatinib (Richter et al, JCO 2014).
A team of French investigators undertook the current observational study to estimate the prevalence of the WS and to identify clinical factors associated with it.
They collected, prospectively, the adverse events from all 428 French patients who were enrolled in the STIM2 (n=204) and EURO-SKI (n=224) trials. And they compared patients who stopped taking TKIs and had a painful WS to those who stopped TKIs and did not have a painful syndrome.
Patient characteristics
Patient characteristics were well balanced between the STIM2 and EURO-SKI groups, with the exception of the median time on TKI before discontinuation. In the STIM2 group, patients were a median of 77.4 months on TKI therapy. In the EURO-SKI group, the median time on a TKI was 100.4 months (P<0.001).
In all, there were 208 male and 220 female patients included. They were a median age of 64 (range, 53–73) and 63 (range, 53–70) years in the STIM2 and EURO-SKI groups, respectively.
Sokal scores were also comparable between the cohorts, with most patients falling in the low and intermediate ranges.
Prevalence and characteristics of WS
Overall, 326 patients (76.2%) were without WS and 102 (23.8%) had WS. In the STIM2 cohort, 193 patients (86.2%) were without WS and 31 (13.8%) had WS. In the EURO-SKI cohort, 133 patients (65.2%) were without WS and 71 (34.8%) had WS.
“And these differences [between cohorts] are significant,” Dr Rousselot pointed out.
Investigators analyzed clinical characteristics of WS in 40 patients and determined that the median time from TKI discontinuation to WS was 21 days, and the median duration of WS was 7 months (range, 3–30).
Pain was located in the shoulder and spine for 67% of the patients and elsewhere in 33%. About two-thirds of patients (62.5%) experienced grade 1–2 pain, and 37.5% experienced grade 3–4 pain.
Nineteen patients resumed TKI therapy, “because of loss of MMR [major molecular response] or loss of clinical response,” Dr Rousselot said.
And the pain disappeared in 52.6% of them when they resumed TKI therapy. The median duration of TKI therapy before WS pain disappeared was 3 weeks.
Risk factors for WS
Investigators determined that CML duration, time on a TKI, and previous history of osteoarticular symptoms were risk factors for WS.
Patients without WS had CML for a shorter time—a mean of 8.7 ± 3.1 months, compared to 9.7 ± 3.8 for those with WS (P=0.02).
Patients without WS were also on a TKI for a shorter time—a median of 81.2 months (range, 61.2–108.0), compared to 97.3 months (range, 73.7–122.9) for those with WS (P<0.001).
Patients with a previous history of osteoarticular symptoms were more likely to experience WS—22.9%, compared to 9.8% without a previous history (P=0.002).
Most patients were receiving imatinib—323 without WS and 100 with WS. The 1 patient receiving dasatinib had no WS. And of the 4 patients receiving nilotinib, 2 had WS and 2 didn’t.
And so the type of TKI therapy—dasatinib, imatinib, or nilotinib—was not significant (P=0.42).
Investigators performed a multivariate analysis adjusted for gender, CML duration, and Sokal score, and 2 risk factors emerged: previous history of osteoarticular symptoms (relative risk: 2.08) and time on TKI (relative risk: 2.23).
Discussion
Dr Rousselot compared the Richter trial (Richter et al, JCO 2014) to the current study and noted that the Richter trial, with an enrollment of 50 patients, had a WS prevalence of 30%. But the current trial had a prevalence of 24%.
The difference in WS may be due to time on TKI, Dr Rousselot said, as patients in the Richter trial were on TKI treatment for a longer period of time.
“The time of onset is the same [in both trials],” Dr Rousselot said, as are the TKI used, location of pain, and duration of pain.
“So what we can say is [with] shorter TKI treatment . . . , we have a higher risk of molecular relapse but a lower risk of withdrawal syndrome.”
And with longer TKI treatment, the converse appears to be true. It reduces the risk of molecular relapse but raises the risk of withdrawal syndrome. ![]()
*Data in the abstract differ from the presentation.
Venetoclax produces deep responses in ultra-high-risk CLL

Photo courtesy of ASH
ORLANDO, FL—The pivotal phase 2 study of venetoclax monotherapy in patients with relapsed/refractory 17p-deleted chronic lymphocytic leukemia (CLL) has achieved unprecedented deep responses, according to investigators.
More than 10% of patients had a complete response (CR), complete response with incomplete blood count recovery (CRi), or near partial response (nPR), as confirmed by an independent review committee (IRC).
And more than 20% of responders became negative for minimal residual disease (MRD).
Venetoclax is an orally bioavailable, selective BCL-2 inhibitor that directly induces apoptosis in CLL cells independent of p53.
The US Food and Drug Administration granted venetoclax breakthrough therapy designation for relapsed/refractory CLL earlier this year.
“Patients with a 17p deletion in CLL have very poor prognosis,” said Stephan Stilgenbauer, MD, of University of Ulm in Germany, “and limited treatment options.”
The median progression-free survival (PFS) with frontline chemoimmunotherapy in this population is less than 12 months.
The first-in-human study of venetoclax, which was recently published in NEJM, showed a 79% overall response rate (ORR) in relapsed/refractory CLL patients.
Dr Stilgenbauer presented the pivotal phase 2 results at the 2015 ASH Annual Meeting as LBA-6.
Study overview
The primary objective of the trial was ORR by independent review committee. The secondary endpoints were CR/PR rates, time to first response, duration of response, PFS, overall survival (OS), and safety.
Investigators also included the exploratory endpoint of MRD as determined by flow cytometry with a sensitivity of less than 10-4.
Patients had to have an ECOG score of 2 or less, an absolute neutrophil count of 1000/μL or greater, a platelet count of 40,000/mm3 or higher, and a hemoglobin count of at least 8 g/dL. They also had to have a creatinine clearance of 50 mL/min or more.
“With regard to performance status, blood counts, and creatinine clearance,” Dr Stilgenbauer said, “inclusion criteria were relatively liberal, allowing patients with comorbidity on the trial.”
Patients were excluded if they had prior allogeneic stem cell transplantation, Richter’s transformation, uncontrolled autoimmune cytopenia, other malignancy, or major organ dysfunction.
Trial design
Patients received an oral dose of venetoclax once daily continuously until disease progression or discontinuation for another reason.
Because tumor lysis syndrome (TLS) was a concern, investigators devised a step-wise weekly ramp-up with risk-based prophylaxis to mitigate TLS.
Patients started on a dose of 20 mg on day 1. If they did not experience any electrolyte abnormalities, they received a 50 mg daily dose for the rest of the first week, escalating to 100 mg, 200 mg, and to the target dose of 400 mg daily on subsequent weeks. Patients continued on 400 mg daily for the remainder of the study.
The investigators assessed response using iwCLL 2008 criteria with monthly physical exams and blood counts, CT scans to confirm clinical response at week 36, and a bone marrow biopsy to confirm CR.
Patient population and disposition
Investigators enrolled 107 patients with a median age of 67 (range, 37–85). Seventy (65%) were male.
Patients had a median of 2 prior therapies (range, 1–10): 54 (50%) had prior bendamustine and 38 (70%) were refractory to it; 78 (73%) had prior fludarabine and 34 (44%) were refractory to it; and 90 (84%) had a prior CD20 monoclonal antibody.
About half (52%) were ECOG grade 1, 53% had 1 or more nodes 5 cm or larger, and 51% had absolute lymphocyte (ALC) levels 25 x 109/L or higher.
Eighty-two percent of patients were in the medium and high TLS risk categories, slightly less than half were Rai stage III or IV, and 81% were IGHV unmutated.
As of the data lock on April 30, 2015, patients remained a median of 12.1 months on study (range, 0.03–21.5). Seventy are still active on venetoclax, and 37 discontinued the treatment.
Eleven patients discontinued due to Richter’s transformation, 11 due to CLL progression, and 9 due to adverse events. Three patients proceeded to stem cell transplant, 2 withdrew consent, and 1 was noncompliant.
Eighteen patients died, 14 due to disease progression.
Response
Eighty-five patients responded, for an ORR of 79.4% by IRC. Eight patients (7.5%) achieved a CR or CRi, 3 (2.8%) had an nPR, and 74 (69.2%) had a PR. Twenty-two patients (20.6%) had no response.
Twenty-five of 48 patients had no evidence of CLL in their bone marrow by immunohistochemistry, and 18 of 45 patients assessed were MRD-negative in the peripheral blood.
Reduction in lymphocytosis “was quite a universal phenomenon across this trial,” Dr Stilgenbauer said. Only 4 patients of 87 with baseline lymphocytosis failed to reduce their lymphocyte count to below 4 x 109/L, the usual threshold for a CR. And the median time to normalization was 22 days (range, 2–122).
Eighty-nine of 96 patients had 50% or more reduction in their nodal size in a median of 2.7 months (range, 0.7–8.4).
The median time to first response was 0.8 months (range, 0.1–8.1), and the median time to CR/CRi was 8.2 months (range, 3.0–16.3).
“And this number still appears to evolve over the duration of the trial,” Dr Stilgenbauer said.
The median duration of response has not yet been reached. But investigators estimated that of the 85 responders, 84.7% would maintain their response at 12 months, 100% of patients in the CR/CRi and nPR groups would maintain their response, and 94.4% of patients who were MRD-negative would maintain their response.
The median PFS and OS have not been reached. The PFS estimate for 12 months was 72.0%, and the OS estimate was 86.7%.
Adverse events
Treatment-emergent adverse events of any grade occurred in 96% of patients. The most frequent were neutropenia (43%), diarrhea (29%), nausea (29%), anemia (27%), fatigue (22%), pyrexia (20%), thrombocytopenia (19%), hyperphosphatemia (16%), vomiting (15%), and upper respiratory tract infection (15%).
The most frequent grade 3/4 adverse events were neutropenia (40%), anemia (18%), and thrombocytopenia (15%).
Dr Stilgenbauer pointed out that 22.4% of patients had neutropenia at baseline. Neutropenia was managed with dose interruption or reduction, G-CSF, and/or antibiotics.
Infections occurred in 72% of patients, with 20% of patients experiencing grade 3 or higher.
“The types of infections were the usual expected ones,” Dr Stilgenbauer said.
Laboratory TLS occurred in 5 patients exclusively during the ramp-up period. Two required a dose interruption of 1 day each. There were no clinical TLS events.
Serious adverse events occurred in 55% of patients, the most common being pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
The investigators concluded that venetoclax offers a favorable risk-benefit profile. The risk of TLS can be effectively mitigated with no clinical TLS, and the incidence of neutropenia and infection are similar to frontline chemoimmunotherapy.
“Venetoclax may provide an attractive treatment option for 17p-deleted CLL as monotherapy or as a component of novel combination strategies,” Dr Stilgenbauer said.
AbbVie and Genentech, collaborators in the development of venetoclax, provided financial support for the study design, study conduct, analysis, data interpretation, writing, and review. ![]()

Photo courtesy of ASH
ORLANDO, FL—The pivotal phase 2 study of venetoclax monotherapy in patients with relapsed/refractory 17p-deleted chronic lymphocytic leukemia (CLL) has achieved unprecedented deep responses, according to investigators.
More than 10% of patients had a complete response (CR), complete response with incomplete blood count recovery (CRi), or near partial response (nPR), as confirmed by an independent review committee (IRC).
And more than 20% of responders became negative for minimal residual disease (MRD).
Venetoclax is an orally bioavailable, selective BCL-2 inhibitor that directly induces apoptosis in CLL cells independent of p53.
The US Food and Drug Administration granted venetoclax breakthrough therapy designation for relapsed/refractory CLL earlier this year.
“Patients with a 17p deletion in CLL have very poor prognosis,” said Stephan Stilgenbauer, MD, of University of Ulm in Germany, “and limited treatment options.”
The median progression-free survival (PFS) with frontline chemoimmunotherapy in this population is less than 12 months.
The first-in-human study of venetoclax, which was recently published in NEJM, showed a 79% overall response rate (ORR) in relapsed/refractory CLL patients.
Dr Stilgenbauer presented the pivotal phase 2 results at the 2015 ASH Annual Meeting as LBA-6.
Study overview
The primary objective of the trial was ORR by independent review committee. The secondary endpoints were CR/PR rates, time to first response, duration of response, PFS, overall survival (OS), and safety.
Investigators also included the exploratory endpoint of MRD as determined by flow cytometry with a sensitivity of less than 10-4.
Patients had to have an ECOG score of 2 or less, an absolute neutrophil count of 1000/μL or greater, a platelet count of 40,000/mm3 or higher, and a hemoglobin count of at least 8 g/dL. They also had to have a creatinine clearance of 50 mL/min or more.
“With regard to performance status, blood counts, and creatinine clearance,” Dr Stilgenbauer said, “inclusion criteria were relatively liberal, allowing patients with comorbidity on the trial.”
Patients were excluded if they had prior allogeneic stem cell transplantation, Richter’s transformation, uncontrolled autoimmune cytopenia, other malignancy, or major organ dysfunction.
Trial design
Patients received an oral dose of venetoclax once daily continuously until disease progression or discontinuation for another reason.
Because tumor lysis syndrome (TLS) was a concern, investigators devised a step-wise weekly ramp-up with risk-based prophylaxis to mitigate TLS.
Patients started on a dose of 20 mg on day 1. If they did not experience any electrolyte abnormalities, they received a 50 mg daily dose for the rest of the first week, escalating to 100 mg, 200 mg, and to the target dose of 400 mg daily on subsequent weeks. Patients continued on 400 mg daily for the remainder of the study.
The investigators assessed response using iwCLL 2008 criteria with monthly physical exams and blood counts, CT scans to confirm clinical response at week 36, and a bone marrow biopsy to confirm CR.
Patient population and disposition
Investigators enrolled 107 patients with a median age of 67 (range, 37–85). Seventy (65%) were male.
Patients had a median of 2 prior therapies (range, 1–10): 54 (50%) had prior bendamustine and 38 (70%) were refractory to it; 78 (73%) had prior fludarabine and 34 (44%) were refractory to it; and 90 (84%) had a prior CD20 monoclonal antibody.
About half (52%) were ECOG grade 1, 53% had 1 or more nodes 5 cm or larger, and 51% had absolute lymphocyte (ALC) levels 25 x 109/L or higher.
Eighty-two percent of patients were in the medium and high TLS risk categories, slightly less than half were Rai stage III or IV, and 81% were IGHV unmutated.
As of the data lock on April 30, 2015, patients remained a median of 12.1 months on study (range, 0.03–21.5). Seventy are still active on venetoclax, and 37 discontinued the treatment.
Eleven patients discontinued due to Richter’s transformation, 11 due to CLL progression, and 9 due to adverse events. Three patients proceeded to stem cell transplant, 2 withdrew consent, and 1 was noncompliant.
Eighteen patients died, 14 due to disease progression.
Response
Eighty-five patients responded, for an ORR of 79.4% by IRC. Eight patients (7.5%) achieved a CR or CRi, 3 (2.8%) had an nPR, and 74 (69.2%) had a PR. Twenty-two patients (20.6%) had no response.
Twenty-five of 48 patients had no evidence of CLL in their bone marrow by immunohistochemistry, and 18 of 45 patients assessed were MRD-negative in the peripheral blood.
Reduction in lymphocytosis “was quite a universal phenomenon across this trial,” Dr Stilgenbauer said. Only 4 patients of 87 with baseline lymphocytosis failed to reduce their lymphocyte count to below 4 x 109/L, the usual threshold for a CR. And the median time to normalization was 22 days (range, 2–122).
Eighty-nine of 96 patients had 50% or more reduction in their nodal size in a median of 2.7 months (range, 0.7–8.4).
The median time to first response was 0.8 months (range, 0.1–8.1), and the median time to CR/CRi was 8.2 months (range, 3.0–16.3).
“And this number still appears to evolve over the duration of the trial,” Dr Stilgenbauer said.
The median duration of response has not yet been reached. But investigators estimated that of the 85 responders, 84.7% would maintain their response at 12 months, 100% of patients in the CR/CRi and nPR groups would maintain their response, and 94.4% of patients who were MRD-negative would maintain their response.
The median PFS and OS have not been reached. The PFS estimate for 12 months was 72.0%, and the OS estimate was 86.7%.
Adverse events
Treatment-emergent adverse events of any grade occurred in 96% of patients. The most frequent were neutropenia (43%), diarrhea (29%), nausea (29%), anemia (27%), fatigue (22%), pyrexia (20%), thrombocytopenia (19%), hyperphosphatemia (16%), vomiting (15%), and upper respiratory tract infection (15%).
The most frequent grade 3/4 adverse events were neutropenia (40%), anemia (18%), and thrombocytopenia (15%).
Dr Stilgenbauer pointed out that 22.4% of patients had neutropenia at baseline. Neutropenia was managed with dose interruption or reduction, G-CSF, and/or antibiotics.
Infections occurred in 72% of patients, with 20% of patients experiencing grade 3 or higher.
“The types of infections were the usual expected ones,” Dr Stilgenbauer said.
Laboratory TLS occurred in 5 patients exclusively during the ramp-up period. Two required a dose interruption of 1 day each. There were no clinical TLS events.
Serious adverse events occurred in 55% of patients, the most common being pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
The investigators concluded that venetoclax offers a favorable risk-benefit profile. The risk of TLS can be effectively mitigated with no clinical TLS, and the incidence of neutropenia and infection are similar to frontline chemoimmunotherapy.
“Venetoclax may provide an attractive treatment option for 17p-deleted CLL as monotherapy or as a component of novel combination strategies,” Dr Stilgenbauer said.
AbbVie and Genentech, collaborators in the development of venetoclax, provided financial support for the study design, study conduct, analysis, data interpretation, writing, and review. ![]()

Photo courtesy of ASH
ORLANDO, FL—The pivotal phase 2 study of venetoclax monotherapy in patients with relapsed/refractory 17p-deleted chronic lymphocytic leukemia (CLL) has achieved unprecedented deep responses, according to investigators.
More than 10% of patients had a complete response (CR), complete response with incomplete blood count recovery (CRi), or near partial response (nPR), as confirmed by an independent review committee (IRC).
And more than 20% of responders became negative for minimal residual disease (MRD).
Venetoclax is an orally bioavailable, selective BCL-2 inhibitor that directly induces apoptosis in CLL cells independent of p53.
The US Food and Drug Administration granted venetoclax breakthrough therapy designation for relapsed/refractory CLL earlier this year.
“Patients with a 17p deletion in CLL have very poor prognosis,” said Stephan Stilgenbauer, MD, of University of Ulm in Germany, “and limited treatment options.”
The median progression-free survival (PFS) with frontline chemoimmunotherapy in this population is less than 12 months.
The first-in-human study of venetoclax, which was recently published in NEJM, showed a 79% overall response rate (ORR) in relapsed/refractory CLL patients.
Dr Stilgenbauer presented the pivotal phase 2 results at the 2015 ASH Annual Meeting as LBA-6.
Study overview
The primary objective of the trial was ORR by independent review committee. The secondary endpoints were CR/PR rates, time to first response, duration of response, PFS, overall survival (OS), and safety.
Investigators also included the exploratory endpoint of MRD as determined by flow cytometry with a sensitivity of less than 10-4.
Patients had to have an ECOG score of 2 or less, an absolute neutrophil count of 1000/μL or greater, a platelet count of 40,000/mm3 or higher, and a hemoglobin count of at least 8 g/dL. They also had to have a creatinine clearance of 50 mL/min or more.
“With regard to performance status, blood counts, and creatinine clearance,” Dr Stilgenbauer said, “inclusion criteria were relatively liberal, allowing patients with comorbidity on the trial.”
Patients were excluded if they had prior allogeneic stem cell transplantation, Richter’s transformation, uncontrolled autoimmune cytopenia, other malignancy, or major organ dysfunction.
Trial design
Patients received an oral dose of venetoclax once daily continuously until disease progression or discontinuation for another reason.
Because tumor lysis syndrome (TLS) was a concern, investigators devised a step-wise weekly ramp-up with risk-based prophylaxis to mitigate TLS.
Patients started on a dose of 20 mg on day 1. If they did not experience any electrolyte abnormalities, they received a 50 mg daily dose for the rest of the first week, escalating to 100 mg, 200 mg, and to the target dose of 400 mg daily on subsequent weeks. Patients continued on 400 mg daily for the remainder of the study.
The investigators assessed response using iwCLL 2008 criteria with monthly physical exams and blood counts, CT scans to confirm clinical response at week 36, and a bone marrow biopsy to confirm CR.
Patient population and disposition
Investigators enrolled 107 patients with a median age of 67 (range, 37–85). Seventy (65%) were male.
Patients had a median of 2 prior therapies (range, 1–10): 54 (50%) had prior bendamustine and 38 (70%) were refractory to it; 78 (73%) had prior fludarabine and 34 (44%) were refractory to it; and 90 (84%) had a prior CD20 monoclonal antibody.
About half (52%) were ECOG grade 1, 53% had 1 or more nodes 5 cm or larger, and 51% had absolute lymphocyte (ALC) levels 25 x 109/L or higher.
Eighty-two percent of patients were in the medium and high TLS risk categories, slightly less than half were Rai stage III or IV, and 81% were IGHV unmutated.
As of the data lock on April 30, 2015, patients remained a median of 12.1 months on study (range, 0.03–21.5). Seventy are still active on venetoclax, and 37 discontinued the treatment.
Eleven patients discontinued due to Richter’s transformation, 11 due to CLL progression, and 9 due to adverse events. Three patients proceeded to stem cell transplant, 2 withdrew consent, and 1 was noncompliant.
Eighteen patients died, 14 due to disease progression.
Response
Eighty-five patients responded, for an ORR of 79.4% by IRC. Eight patients (7.5%) achieved a CR or CRi, 3 (2.8%) had an nPR, and 74 (69.2%) had a PR. Twenty-two patients (20.6%) had no response.
Twenty-five of 48 patients had no evidence of CLL in their bone marrow by immunohistochemistry, and 18 of 45 patients assessed were MRD-negative in the peripheral blood.
Reduction in lymphocytosis “was quite a universal phenomenon across this trial,” Dr Stilgenbauer said. Only 4 patients of 87 with baseline lymphocytosis failed to reduce their lymphocyte count to below 4 x 109/L, the usual threshold for a CR. And the median time to normalization was 22 days (range, 2–122).
Eighty-nine of 96 patients had 50% or more reduction in their nodal size in a median of 2.7 months (range, 0.7–8.4).
The median time to first response was 0.8 months (range, 0.1–8.1), and the median time to CR/CRi was 8.2 months (range, 3.0–16.3).
“And this number still appears to evolve over the duration of the trial,” Dr Stilgenbauer said.
The median duration of response has not yet been reached. But investigators estimated that of the 85 responders, 84.7% would maintain their response at 12 months, 100% of patients in the CR/CRi and nPR groups would maintain their response, and 94.4% of patients who were MRD-negative would maintain their response.
The median PFS and OS have not been reached. The PFS estimate for 12 months was 72.0%, and the OS estimate was 86.7%.
Adverse events
Treatment-emergent adverse events of any grade occurred in 96% of patients. The most frequent were neutropenia (43%), diarrhea (29%), nausea (29%), anemia (27%), fatigue (22%), pyrexia (20%), thrombocytopenia (19%), hyperphosphatemia (16%), vomiting (15%), and upper respiratory tract infection (15%).
The most frequent grade 3/4 adverse events were neutropenia (40%), anemia (18%), and thrombocytopenia (15%).
Dr Stilgenbauer pointed out that 22.4% of patients had neutropenia at baseline. Neutropenia was managed with dose interruption or reduction, G-CSF, and/or antibiotics.
Infections occurred in 72% of patients, with 20% of patients experiencing grade 3 or higher.
“The types of infections were the usual expected ones,” Dr Stilgenbauer said.
Laboratory TLS occurred in 5 patients exclusively during the ramp-up period. Two required a dose interruption of 1 day each. There were no clinical TLS events.
Serious adverse events occurred in 55% of patients, the most common being pyrexia (7%), autoimmune hemolytic anemia (7%), pneumonia (6%), and febrile neutropenia (5%).
The investigators concluded that venetoclax offers a favorable risk-benefit profile. The risk of TLS can be effectively mitigated with no clinical TLS, and the incidence of neutropenia and infection are similar to frontline chemoimmunotherapy.
“Venetoclax may provide an attractive treatment option for 17p-deleted CLL as monotherapy or as a component of novel combination strategies,” Dr Stilgenbauer said.
AbbVie and Genentech, collaborators in the development of venetoclax, provided financial support for the study design, study conduct, analysis, data interpretation, writing, and review. ![]()
SAA patients benefit from upfront eltrombopag combo

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.

Photo courtesy of ASH
ORLANDO, FL—Investigators are pursuing an upfront approval for eltrombopag in combination with immunosuppressive therapy for the treatment of severe aplastic anemia (SAA).
Based on eltrombopag’s single-agent activity in refractory SAA, they hypothesized that its addition to standard immunosuppressive therapy of horse antithymocyte globulin (hATG) and cyclosporine (CsA) in the first-line setting could improve patient outcome.
And, in a phase 2 trial, it did.
“The addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” said Danielle
Townsley, MD, who presented the data at the 2015 ASH Annual Meeting.
Dr Townsley, of the National Heart, Lung, and Blood Institute, National Institutes of Health, in Bethesda, Maryland, presented the findings as abstract LBA-2.*
The US Food and Drug Administration approved eltrombopag to treat refractory SAA in November 2014, and the European Commission approved it in 2015.
Investigators believed eltrombopag in the upfront, treatment-naïve setting could yield higher overall response rates (ORRs) than the 60% to 70% achieved with standard immunosuppressives worldwide.
“[It was] logical to consider treating patients early at the start of their disease,” Dr Townsley said.
So she and her colleagues conducted an investigator-initiated, phase 2, single-center trial of eltrombopag combined with immunosuppressive agents for first-line treatment of SAA.
Study design and patient population
Patients had to have confirmed treatment-naïve SAA, be a minimum of 2 years old, and weigh more than 12 kg. They were excluded if they had prior immunosuppressive therapy with ATG, alemtuzumab, or cyclophosphamide. They were also excluded if they had liver cirrhosis, AST/ALT more than 5 times normal, or Fanconi anemia.
Primary endpoints of the study were complete response (CR) at 6 months and toxicity. Secondary endpoints included ORR and partial response (PR) rate, survival, clonal evolution, and relapse.
Investigators defined CR as having an absolute neutrophil count (ANC) of 1000/μL or higher, a hemoglobin level of 10 g/dL or higher, and a platelet count of 100,000/μL or higher. They defined PR as blood counts no longer meeting criteria for SAA or CR.
All 92 patients received standard hATG (on days 1 to 4) and CsA (for 6 months). Patients in cohort 1 (n=30) also received eltrombopag at 150 mg daily, starting on day 14 for 6 months.
Patients in cohort 2 (n=31) received eltrombopag at 150 mg daily, starting on day 14 for 3 months. And the 31 patients in cohort 3 started 150 mg of daily eltrombopag simultaneously with the immunosuppressants and continued to receive the drug for 6 months.
Investigators assessed response at 3 and 6 months and planned to follow patients for at least 5 years.
Patients in all cohorts were a median of 32 years (range, 3–82), with 21% being younger than 18. About half were male, 66% had less than 1% of a paroxysmal nocturnal hemoglobinuria clone, 37% had a median neutrophil count less than 200/μL, a median reticulocyte count of 20,000/μL (range, 1600–60,400/μL), and a median platelet count of 9000/μL (range, 0–37,000/μL).
Results
At 3 months, the ORR for the entire population was 81%, and the CR rate was 28%. The ORR was 77% in cohorts 1 and 2 and 92% in cohort 3. The CR rate was 17%, 26%, and 44% in cohorts 1, 2, and 3, respectively.
At 6 months, the ORR for the entire population was 86%, and the CR rate was 37%. The ORR was 80%, 87%, and 95% in cohorts 1, 2, and 3, respectively. And the CR rate was 33%, 26%, and 60%, respectively.
Compared to historic rates for patients on hATG and CsA alone, “the addition of eltrombopag resulted in over 20% higher overall response rates and complete response rates for both 3 and 6 months,” Dr Townsley said.
“And for cohort 3, when eltrombopag is given on day 1, the rate of response in evaluable patients to date appears even higher, with 95% overall response rate at 6 months, of which 60% are complete.”
Dr Townsley also noted that, compared to historical experience, neutrophil recovery was more robust in responding patients treated with eltrombopag. Patients on eltrombopag had a mean ANC of 2253/μL, compared with an ANC of 1716/μL for the historic comparator.
“And likewise, more robust platelet recovery was observed with eltrombopag,” Dr Townsley said, with the eltrombopag-treated patients achieving a mean count of 115,262/μL, compared to a mean of 84,303/μL for the historic group.
She added that, among all eltrombopag-treated patients, the median time to neutrophil recovery was 29 days for an ANC greater than 200/μL and 47 days for an ANC greater than 500/μL. In cohort 3—in which eltrombopag was initiated on day 1—those endpoints were achieved in a median of 8 days and 38 days, respectively.
Patients became transfusion-independent for red cells in a median of 42 days and for platelets in a median of 32 days.
Eltrombopag-treated patients had a 99% overall survival at a median follow-up of 18 months (range 1 – 42) when censored for stem cell transplant. When not censored for transplant, their overall survival was 97%.
Adverse events
“The addition of eltrombopag to ATG and cyclosporine was, overall, well tolerated,” Dr Townsley said. “Few grade 3 to 4 events were attributed to eltrombopag.”
Severe cutaneous reactions in 2 patients caused eltrombopag to be stopped, and 10% of patients had grade 2–3 transaminase and bilirubin elevations.
Bone marrow biopsies revealed no increased fibrosis.
One patient with thymoma died while on study due to encephalopathy. And 2 deaths occurred after hematopoietic stem cell transplant, one with relapsed acute myeloid leukemia and the other from relapsed aplastic anemia.
Clonal evolution occurred in 7 patients, 2 who had achieved CR and evolved in 3 and 30 months. Neither patient had bone marrow dysplasia. One patient’s cytogenetics normalized, and the other had stable disease.
“In our protocol, we define any new cytogenetic abnormality as clonal evolution—we have always done this,” Dr Townsley said.
Of the other 5 patients who evolved, 1 achieved a CR and relapsed, 1 achieved a PR and relapsed, 2 achieved a PR, and 1 had no response. Three of these patients had stem cell transplants, 1 had stable disease, and 1 died of acute myeloid leukemia after stem cell transplant.
The investigators concluded that eltrombopag increases complete and overall hematologic response rates in treatment-naïve SAA patients. Immediate introduction of eltrombopag with immunosuppressant therapy may be optimal, and CR does not appear to prevent clonal evolution.
Investigators are currently in the process of conducting a long-term, serial genomic analysis. The study is open for accrual to an extension cohort.
Eltrombopag is marketed as Promacta in the US and Revolade in most countries outside the US.
Dr Townsley disclosed drug and research funding from GlaxoSmithKline and Novartis, developers of eltrombopag. ![]()
*Data in the abstract differ from the presentation.
Regimen with intensified PEG-ASP feasible in young adults with ALL
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—Results of a DFCI ALL Consortium trial have shown that adults with acute lymphoblastic leukemia (ALL) can be successfully and safely treated with a pediatric regimen using intensified pegylated asparaginase (PEG-ASP).
Investigators recently reported that young adults treated with native E coli asparaginase as part of their regimen had improved 4-year disease-free survival and overall survival (OS) rates.
Now, the team has shown it is possible to use PEG-ASP to improve young adult outcomes as well.
The investigators also described the toxicities with PEG-ASP and compared them to the prior DFCI ALL Consortium trial with native E coli asparaginase.
“[Wendy] Stock, years ago, analyzed young adult patients 16 to 20 based on whether or not they were treated on Children’s Cancer Group trials or CALGB trials,” said Daniel J. DeAngelo, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And what she reported was that there was a dramatic improvement in the disease- and event-free survival . . . . And since that publication and presentation at ASH several years ago, there’ve been a large number of us who’ve tried to adapt pediatric trials or pediatric-inspired trials for the treatment of young adults with acute lymphoblastic leukemia.”
The PEG-ASP DFCI ALL trial is one such effort. Dr DeAngelo discussed the results of this trial at the 2015 ASH Annual Meeting (abstract 80).
Patient population
Investigators enrolled 110 patients on the trial.
Patients had to be between 18 and 50 years of age, with untreated ALL and no history of secondary ALL. Patients with Burkitt’s lymphoma were excluded.
The patients’ median age was 32 (range, 18–50), 62% were male, 80% were white, and 85% were non-Hispanic. Eleven percent had central nervous system (CNS) status 2 or 3 prior to the initiation of chemotherapy.
Most (87%) had a performance status of 0 or 1, 82% had the B-cell and 18% the T-cell phenotype, 19% were Ph-positive, 6% had an MLL translocation (11q23), and 18% had other translocations.
Study design
Induction chemotherapy consisted of doxorubicin, prednisone, vincristine, PEG-ASP, and intrathecal therapy.
The first consolidation consisted of high-dose methotrexate followed by a BFM-like intensification and high-dose cytarabine, etoposide, and dexamethasone.
CNS prophylaxis included intrathecal chemotherapy and cranial irradiation.
The second consolidation consisted of eight 3-week courses of doxorubicin, vincristine, dexamethasone, 6-mercaptopurine, and 30 weeks of PEG-ASP.
The PEG-ASP was initially dosed at the pediatric level of 2500 IU/m2 every 2 weeks.
“But due to some toxicity concerns in this treatment strategy—with specific emphasis on liver function abnormalities with hyperbilirubinemia, elevations of AST/ALT—we decided to amend the protocol and decrease the PEG dose from 2500 to 2000 and increase the interval from every 2 weeks to every 3 weeks,” Dr DeAngelo said.
Therefore, during this 30-week course, patients received 10 doses of PEG ASP as opposed to 15.
“We also went back and swapped out the PEG asparaginase during induction and reinserted native E coli to really ascertain comparative properties,” he said.
Maintenance therapy consisted of 3-week courses of vincristine, dexamethasone, methotrexate, and 6-mercaptopurine for 2 years from achievement of complete remission (CR).
During PEG-ASP therapy, patients received anticoagulation prophylaxis, preferably with low-molecular-weight heparin, as long as patients had a platelet count greater than 30,000/μL.
Results
Of the 110 patients enrolled, 65 received the higher dose of asparaginase, and 45 received the amended lower dose.
Ninety-one patients (89%) achieved a CR, 57 of whom received the higher dose of asparaginase and 34 the lower dose.
There were 2 induction deaths, both in the higher-dose group.
Twenty-one patients went on to transplant in CR1, 15 in the higher-dose group and 6 in the lower-dose group.
Twenty-three patients relapsed, 17 in the higher-dose group and 6 in the lower-dose group. Two of the relapses were CNS only.
Three patients died in remission, 2 in the higher-dose asparaginase group and 1 in the lower. And 3 patients died after stem cell transplant in CR, 2 in the higher-dose group and 1 in the lower.
At a median follow-up of 42.2 months, the 3-year disease-free survival for the entire cohort was 73%, and overall survival was 75%.
Subset analyses
The investigators performed subgroup analyses and came up with some “interesting observations,” Dr DeAngelo said.
Younger patients, ages 18 to 19 and 20 to 29, had a better OS than the older patients. The OS for younger patients is in the 80% to 85% range, “which is significantly better than the other patients in the 30 to 40 or 40 to 50 age groups,” Dr DeAngelo said.
Patients with T-cell ALL had a better OS than those with B-cell ALL and Ph-positive ALL, who had the worst OS of approximately 50%. The vast majority of Ph-negative patients were transplanted, and all received imatinib in addition to chemotherapy.
“[Patients with the T-cell phenotype] seemed to do particularly well on this strategy, which is something we showed in the last study as well, with an overall survival of 80%, compared to 70% for the B-cell Philadelphia-negative [patients],” Dr DeAngelo said.
He and his colleagues also found an association between OS and body mass index (BMI).
Obese or morbidly obese patients with a BMI of 30 or over had an OS of around 40%, while underweight or normal-weight patients had an OS of almost 90%, a “profound overall survival in the less-than-obese patients,” Dr DeAngelo said.
“And I think one of the things that is bringing down the curves is the obese,” he added, “which is a concern as the body mass index of the American population increases.”
Another discovery was that patients with minimal residual disease (MRD) of less than 10-4 had better OS than those with a high MRD level.
After a single dose of PEG ASP during induction on day 4, asparagine was depleted for a median of 3 weeks. With a single dose of E coli asparaginase, on the other hand, asparagine is depleted for about a week.
Asparaginase levels during consolidation were “extraordinarily elevated” with the 2500 dose level of PEG-ASP compared to the lower dose level. Toxicity was much more manageable, however, as the dose was reduced, Dr DeAngelo said. And asparagine was still depleted throughout the 30 weeks, as per protocol.
Toxicity
The higher asparaginase dose group “surprisingly, had a very low rate of clinical pancreatitis,” Dr DeAngelo said.
At the higher asparaginase dose—2500 IU/m2 every 2 weeks—66 patients experienced grade 3-5 adverse events: 30 (46%) febrile neutropenia, 1 (1%) pancreatitis, 19 (29%) AST, 34 (52%) ALT, 24 (36%) bilirubin, 19 (29%) thrombosis, 2 (3%) CNS hemorrhage, 3 (4%) hypersensitivity, and 4 (6%) osteonecrosis.
After the protocol amendment, “we saw a marked reduction in hyperbilirubinemia,” Dr DeAngelo said.
Grade 3–4 hyperbilirubinemia decreased from 36% to 7%, grade 3–4 ALT elevation decreased from 52% to 29%, and the rate of thrombosis decreased from 29% to 16%.
“Whether the latter decrease [thrombosis] was reflective of the decreased dose of asparaginase or the addition of anticoagulation, I can’t determine,” Dr DeAngelo said, “but it seemed to reflect other studies.”
The investigators concluded that a dose-intensified pediatric regimen in adults is feasible, with an acceptable toxicity profile.
The team said this approach may translate to better survival for adults with ALL, with the exception of older adults and patients with a high BMI. PEG-ASP has increased toxicity in these patients.
The investigators recommend addressing the challenges that remain—psychosocial issues, practice patterns, and biology—with a unified approach and more cooperative group trials in young adults. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—Results of a DFCI ALL Consortium trial have shown that adults with acute lymphoblastic leukemia (ALL) can be successfully and safely treated with a pediatric regimen using intensified pegylated asparaginase (PEG-ASP).
Investigators recently reported that young adults treated with native E coli asparaginase as part of their regimen had improved 4-year disease-free survival and overall survival (OS) rates.
Now, the team has shown it is possible to use PEG-ASP to improve young adult outcomes as well.
The investigators also described the toxicities with PEG-ASP and compared them to the prior DFCI ALL Consortium trial with native E coli asparaginase.
“[Wendy] Stock, years ago, analyzed young adult patients 16 to 20 based on whether or not they were treated on Children’s Cancer Group trials or CALGB trials,” said Daniel J. DeAngelo, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And what she reported was that there was a dramatic improvement in the disease- and event-free survival . . . . And since that publication and presentation at ASH several years ago, there’ve been a large number of us who’ve tried to adapt pediatric trials or pediatric-inspired trials for the treatment of young adults with acute lymphoblastic leukemia.”
The PEG-ASP DFCI ALL trial is one such effort. Dr DeAngelo discussed the results of this trial at the 2015 ASH Annual Meeting (abstract 80).
Patient population
Investigators enrolled 110 patients on the trial.
Patients had to be between 18 and 50 years of age, with untreated ALL and no history of secondary ALL. Patients with Burkitt’s lymphoma were excluded.
The patients’ median age was 32 (range, 18–50), 62% were male, 80% were white, and 85% were non-Hispanic. Eleven percent had central nervous system (CNS) status 2 or 3 prior to the initiation of chemotherapy.
Most (87%) had a performance status of 0 or 1, 82% had the B-cell and 18% the T-cell phenotype, 19% were Ph-positive, 6% had an MLL translocation (11q23), and 18% had other translocations.
Study design
Induction chemotherapy consisted of doxorubicin, prednisone, vincristine, PEG-ASP, and intrathecal therapy.
The first consolidation consisted of high-dose methotrexate followed by a BFM-like intensification and high-dose cytarabine, etoposide, and dexamethasone.
CNS prophylaxis included intrathecal chemotherapy and cranial irradiation.
The second consolidation consisted of eight 3-week courses of doxorubicin, vincristine, dexamethasone, 6-mercaptopurine, and 30 weeks of PEG-ASP.
The PEG-ASP was initially dosed at the pediatric level of 2500 IU/m2 every 2 weeks.
“But due to some toxicity concerns in this treatment strategy—with specific emphasis on liver function abnormalities with hyperbilirubinemia, elevations of AST/ALT—we decided to amend the protocol and decrease the PEG dose from 2500 to 2000 and increase the interval from every 2 weeks to every 3 weeks,” Dr DeAngelo said.
Therefore, during this 30-week course, patients received 10 doses of PEG ASP as opposed to 15.
“We also went back and swapped out the PEG asparaginase during induction and reinserted native E coli to really ascertain comparative properties,” he said.
Maintenance therapy consisted of 3-week courses of vincristine, dexamethasone, methotrexate, and 6-mercaptopurine for 2 years from achievement of complete remission (CR).
During PEG-ASP therapy, patients received anticoagulation prophylaxis, preferably with low-molecular-weight heparin, as long as patients had a platelet count greater than 30,000/μL.
Results
Of the 110 patients enrolled, 65 received the higher dose of asparaginase, and 45 received the amended lower dose.
Ninety-one patients (89%) achieved a CR, 57 of whom received the higher dose of asparaginase and 34 the lower dose.
There were 2 induction deaths, both in the higher-dose group.
Twenty-one patients went on to transplant in CR1, 15 in the higher-dose group and 6 in the lower-dose group.
Twenty-three patients relapsed, 17 in the higher-dose group and 6 in the lower-dose group. Two of the relapses were CNS only.
Three patients died in remission, 2 in the higher-dose asparaginase group and 1 in the lower. And 3 patients died after stem cell transplant in CR, 2 in the higher-dose group and 1 in the lower.
At a median follow-up of 42.2 months, the 3-year disease-free survival for the entire cohort was 73%, and overall survival was 75%.
Subset analyses
The investigators performed subgroup analyses and came up with some “interesting observations,” Dr DeAngelo said.
Younger patients, ages 18 to 19 and 20 to 29, had a better OS than the older patients. The OS for younger patients is in the 80% to 85% range, “which is significantly better than the other patients in the 30 to 40 or 40 to 50 age groups,” Dr DeAngelo said.
Patients with T-cell ALL had a better OS than those with B-cell ALL and Ph-positive ALL, who had the worst OS of approximately 50%. The vast majority of Ph-negative patients were transplanted, and all received imatinib in addition to chemotherapy.
“[Patients with the T-cell phenotype] seemed to do particularly well on this strategy, which is something we showed in the last study as well, with an overall survival of 80%, compared to 70% for the B-cell Philadelphia-negative [patients],” Dr DeAngelo said.
He and his colleagues also found an association between OS and body mass index (BMI).
Obese or morbidly obese patients with a BMI of 30 or over had an OS of around 40%, while underweight or normal-weight patients had an OS of almost 90%, a “profound overall survival in the less-than-obese patients,” Dr DeAngelo said.
“And I think one of the things that is bringing down the curves is the obese,” he added, “which is a concern as the body mass index of the American population increases.”
Another discovery was that patients with minimal residual disease (MRD) of less than 10-4 had better OS than those with a high MRD level.
After a single dose of PEG ASP during induction on day 4, asparagine was depleted for a median of 3 weeks. With a single dose of E coli asparaginase, on the other hand, asparagine is depleted for about a week.
Asparaginase levels during consolidation were “extraordinarily elevated” with the 2500 dose level of PEG-ASP compared to the lower dose level. Toxicity was much more manageable, however, as the dose was reduced, Dr DeAngelo said. And asparagine was still depleted throughout the 30 weeks, as per protocol.
Toxicity
The higher asparaginase dose group “surprisingly, had a very low rate of clinical pancreatitis,” Dr DeAngelo said.
At the higher asparaginase dose—2500 IU/m2 every 2 weeks—66 patients experienced grade 3-5 adverse events: 30 (46%) febrile neutropenia, 1 (1%) pancreatitis, 19 (29%) AST, 34 (52%) ALT, 24 (36%) bilirubin, 19 (29%) thrombosis, 2 (3%) CNS hemorrhage, 3 (4%) hypersensitivity, and 4 (6%) osteonecrosis.
After the protocol amendment, “we saw a marked reduction in hyperbilirubinemia,” Dr DeAngelo said.
Grade 3–4 hyperbilirubinemia decreased from 36% to 7%, grade 3–4 ALT elevation decreased from 52% to 29%, and the rate of thrombosis decreased from 29% to 16%.
“Whether the latter decrease [thrombosis] was reflective of the decreased dose of asparaginase or the addition of anticoagulation, I can’t determine,” Dr DeAngelo said, “but it seemed to reflect other studies.”
The investigators concluded that a dose-intensified pediatric regimen in adults is feasible, with an acceptable toxicity profile.
The team said this approach may translate to better survival for adults with ALL, with the exception of older adults and patients with a high BMI. PEG-ASP has increased toxicity in these patients.
The investigators recommend addressing the challenges that remain—psychosocial issues, practice patterns, and biology—with a unified approach and more cooperative group trials in young adults. ![]()
Annual Meeting
Photo courtesy of ASH
ORLANDO, FL—Results of a DFCI ALL Consortium trial have shown that adults with acute lymphoblastic leukemia (ALL) can be successfully and safely treated with a pediatric regimen using intensified pegylated asparaginase (PEG-ASP).
Investigators recently reported that young adults treated with native E coli asparaginase as part of their regimen had improved 4-year disease-free survival and overall survival (OS) rates.
Now, the team has shown it is possible to use PEG-ASP to improve young adult outcomes as well.
The investigators also described the toxicities with PEG-ASP and compared them to the prior DFCI ALL Consortium trial with native E coli asparaginase.
“[Wendy] Stock, years ago, analyzed young adult patients 16 to 20 based on whether or not they were treated on Children’s Cancer Group trials or CALGB trials,” said Daniel J. DeAngelo, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And what she reported was that there was a dramatic improvement in the disease- and event-free survival . . . . And since that publication and presentation at ASH several years ago, there’ve been a large number of us who’ve tried to adapt pediatric trials or pediatric-inspired trials for the treatment of young adults with acute lymphoblastic leukemia.”
The PEG-ASP DFCI ALL trial is one such effort. Dr DeAngelo discussed the results of this trial at the 2015 ASH Annual Meeting (abstract 80).
Patient population
Investigators enrolled 110 patients on the trial.
Patients had to be between 18 and 50 years of age, with untreated ALL and no history of secondary ALL. Patients with Burkitt’s lymphoma were excluded.
The patients’ median age was 32 (range, 18–50), 62% were male, 80% were white, and 85% were non-Hispanic. Eleven percent had central nervous system (CNS) status 2 or 3 prior to the initiation of chemotherapy.
Most (87%) had a performance status of 0 or 1, 82% had the B-cell and 18% the T-cell phenotype, 19% were Ph-positive, 6% had an MLL translocation (11q23), and 18% had other translocations.
Study design
Induction chemotherapy consisted of doxorubicin, prednisone, vincristine, PEG-ASP, and intrathecal therapy.
The first consolidation consisted of high-dose methotrexate followed by a BFM-like intensification and high-dose cytarabine, etoposide, and dexamethasone.
CNS prophylaxis included intrathecal chemotherapy and cranial irradiation.
The second consolidation consisted of eight 3-week courses of doxorubicin, vincristine, dexamethasone, 6-mercaptopurine, and 30 weeks of PEG-ASP.
The PEG-ASP was initially dosed at the pediatric level of 2500 IU/m2 every 2 weeks.
“But due to some toxicity concerns in this treatment strategy—with specific emphasis on liver function abnormalities with hyperbilirubinemia, elevations of AST/ALT—we decided to amend the protocol and decrease the PEG dose from 2500 to 2000 and increase the interval from every 2 weeks to every 3 weeks,” Dr DeAngelo said.
Therefore, during this 30-week course, patients received 10 doses of PEG ASP as opposed to 15.
“We also went back and swapped out the PEG asparaginase during induction and reinserted native E coli to really ascertain comparative properties,” he said.
Maintenance therapy consisted of 3-week courses of vincristine, dexamethasone, methotrexate, and 6-mercaptopurine for 2 years from achievement of complete remission (CR).
During PEG-ASP therapy, patients received anticoagulation prophylaxis, preferably with low-molecular-weight heparin, as long as patients had a platelet count greater than 30,000/μL.
Results
Of the 110 patients enrolled, 65 received the higher dose of asparaginase, and 45 received the amended lower dose.
Ninety-one patients (89%) achieved a CR, 57 of whom received the higher dose of asparaginase and 34 the lower dose.
There were 2 induction deaths, both in the higher-dose group.
Twenty-one patients went on to transplant in CR1, 15 in the higher-dose group and 6 in the lower-dose group.
Twenty-three patients relapsed, 17 in the higher-dose group and 6 in the lower-dose group. Two of the relapses were CNS only.
Three patients died in remission, 2 in the higher-dose asparaginase group and 1 in the lower. And 3 patients died after stem cell transplant in CR, 2 in the higher-dose group and 1 in the lower.
At a median follow-up of 42.2 months, the 3-year disease-free survival for the entire cohort was 73%, and overall survival was 75%.
Subset analyses
The investigators performed subgroup analyses and came up with some “interesting observations,” Dr DeAngelo said.
Younger patients, ages 18 to 19 and 20 to 29, had a better OS than the older patients. The OS for younger patients is in the 80% to 85% range, “which is significantly better than the other patients in the 30 to 40 or 40 to 50 age groups,” Dr DeAngelo said.
Patients with T-cell ALL had a better OS than those with B-cell ALL and Ph-positive ALL, who had the worst OS of approximately 50%. The vast majority of Ph-negative patients were transplanted, and all received imatinib in addition to chemotherapy.
“[Patients with the T-cell phenotype] seemed to do particularly well on this strategy, which is something we showed in the last study as well, with an overall survival of 80%, compared to 70% for the B-cell Philadelphia-negative [patients],” Dr DeAngelo said.
He and his colleagues also found an association between OS and body mass index (BMI).
Obese or morbidly obese patients with a BMI of 30 or over had an OS of around 40%, while underweight or normal-weight patients had an OS of almost 90%, a “profound overall survival in the less-than-obese patients,” Dr DeAngelo said.
“And I think one of the things that is bringing down the curves is the obese,” he added, “which is a concern as the body mass index of the American population increases.”
Another discovery was that patients with minimal residual disease (MRD) of less than 10-4 had better OS than those with a high MRD level.
After a single dose of PEG ASP during induction on day 4, asparagine was depleted for a median of 3 weeks. With a single dose of E coli asparaginase, on the other hand, asparagine is depleted for about a week.
Asparaginase levels during consolidation were “extraordinarily elevated” with the 2500 dose level of PEG-ASP compared to the lower dose level. Toxicity was much more manageable, however, as the dose was reduced, Dr DeAngelo said. And asparagine was still depleted throughout the 30 weeks, as per protocol.
Toxicity
The higher asparaginase dose group “surprisingly, had a very low rate of clinical pancreatitis,” Dr DeAngelo said.
At the higher asparaginase dose—2500 IU/m2 every 2 weeks—66 patients experienced grade 3-5 adverse events: 30 (46%) febrile neutropenia, 1 (1%) pancreatitis, 19 (29%) AST, 34 (52%) ALT, 24 (36%) bilirubin, 19 (29%) thrombosis, 2 (3%) CNS hemorrhage, 3 (4%) hypersensitivity, and 4 (6%) osteonecrosis.
After the protocol amendment, “we saw a marked reduction in hyperbilirubinemia,” Dr DeAngelo said.
Grade 3–4 hyperbilirubinemia decreased from 36% to 7%, grade 3–4 ALT elevation decreased from 52% to 29%, and the rate of thrombosis decreased from 29% to 16%.
“Whether the latter decrease [thrombosis] was reflective of the decreased dose of asparaginase or the addition of anticoagulation, I can’t determine,” Dr DeAngelo said, “but it seemed to reflect other studies.”
The investigators concluded that a dose-intensified pediatric regimen in adults is feasible, with an acceptable toxicity profile.
The team said this approach may translate to better survival for adults with ALL, with the exception of older adults and patients with a high BMI. PEG-ASP has increased toxicity in these patients.
The investigators recommend addressing the challenges that remain—psychosocial issues, practice patterns, and biology—with a unified approach and more cooperative group trials in young adults. ![]()
Surprising finding in upfront use of idelalisib monotherapy

Photo courtesy of ASH
ORLANDO, FL—Investigators have observed early fulminant hepatotoxicity in a subset of primarily younger chronic lymphocytic leukemia (CLL) patients treated with idelalisib monotherapy in the frontline setting.
In a phase 2 study of idelalisib plus ofatumumab, 52% of the 24 patients enrolled experienced grade 3 or higher hepatotoxicity shortly after idelalisib was started.
The investigators say this may occur because a proportion of regulatory T cells in the peripheral blood decreases while patients are on idelalisib. The team believes this early hepatotoxicity is immune-mediated.
Benjamin Lampson, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, described these surprising findings at the 2015 ASH Annual Meeting as abstract 497.*
Study design and patient demographics
Patients received 150 mg of idelalisib twice daily as monotherapy on days 1 through 56. They then received combination therapy with idelalisib plus ofatumumab for 8 weekly infusions, followed by 4 monthly infusions through day 225, and then idelalisib monotherapy indefinitely.
The primary endpoint of overall response rate was assessed 2 months after the completion of combination therapy.
“This dosing strategy is slightly different than what has been previously used in trials combining these particular drugs,” Dr Lampson said. “Specifically, previously reported trials started these agents simultaneously without a lead-in period of monotherapy.”
The investigators monitored the patients weekly for toxicities during the 2-month monotherapy lead-in period.
Three-quarters of the patients are male. Their median age is 67.4 years (range, 57.6–84.9), 54% have unmutated IgHV, 17% have deletion 17p or TP53 mutation, 4% have deletion 11q, and 54% have deletion 13q.
The patients received no prior therapies.
Results
The trial is currently ongoing.
The 24 patients enrolled as of early November have been on therapy a median of 7.7 months, for a median follow-up time of 14.7 months.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr Lampson said.
In the first 2 months of therapy, 52% of patients developed transaminitis, and 13% developed colitis or diarrhea, all grade 3 or higher. Thirteen percent developed pneumonitis of any grade.
Younger age is a risk factor for early hepatotoxicity, Dr Lampson said, with a significance of P=0.02. All subjects age 65 or younger (n=7) required systemic steroids to treat their toxicities.
Hepatotoxicity developed in a median of 28 days, he said, “and the hepatotoxicity is typically occurring before the first dose of ofatumumab is administered at week 8, suggesting that idelalisib alone is the cause of the hepatotoxicity.”
Dr Lampson noted that toxicities resolved rapidly with steroids.
“I do want to point out that all subjects evaluable for a response have had a response,” he added. “Additionally, in all subjects where treatment has been discontinued, the discontinuation was due to adverse events rather than disease progression.”
Twelve patients with grade 2 or higher transaminitis were re-challenged with idelalisib after holding the drug for toxicity.
Five patients were re-challenged while off steroids, and 4 developed recurrent transaminitis within 4 days. Seven patients were re-challenged while on steroids, and 2 developed recurrent transaminitis within 4 days.
“In general, our experience has been, if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject can eventually be taken off steroids,” Dr Lampson said.
Comparison with earlier studies
The investigators compared the frequency of toxicity in their trial to earlier studies of idelalisib (Brown, Blood 2014; Coutre, EHA 2015, abstr P588; O’Brien, Blood 2015).
They found that grade 3 or higher transaminitis (52%) and any grade pneumonitis (13%) were higher in their trial than in the 3 other trials.
Colitis/diarrhea was about the same in 2 of the 3 other trials. But in the paper by O’Brien et al, 42% of patients experienced grade 3 or greater colitis/diarrhea.
The lower rate of colitis in the present trial may be due to the shorter follow-up, Dr Lampson said, as colitis is a late adverse event.
The O’Brien trial was also an upfront study, so patients had no prior therapies. The investigators observed that toxicities appeared to be more common in less heavily pretreated patients.
“As the median number of prior therapies decreases,” Dr Lampson said, “the frequency of adverse events increases.”
He noted that, in the O’Brien trial, idelalisib was started simultaneously with the other drugs, perhaps accounting for its somewhat lower rate (21%) of grade 3 or higher transaminitis.
Additionally, the patient population in the O’Brien trial was older than the population in the current trial, which could account for the higher rate of transaminitis, as younger age is a risk factor.
Decrease in regulatory T cells
Investigators noted a decrease in regulatory T cells while patients were on therapy. Eleven of 15 patients (73%) with matched samples had a significant (P<0.05) decrease in the percentage of T cells over time.
This, they say, could provide a possible explanation for the development of early hepatotoxicity.
The trial is investigator-initiated and funded by Gilead Sciences. ![]()
*Data in the presentation differs from the abstract.

Photo courtesy of ASH
ORLANDO, FL—Investigators have observed early fulminant hepatotoxicity in a subset of primarily younger chronic lymphocytic leukemia (CLL) patients treated with idelalisib monotherapy in the frontline setting.
In a phase 2 study of idelalisib plus ofatumumab, 52% of the 24 patients enrolled experienced grade 3 or higher hepatotoxicity shortly after idelalisib was started.
The investigators say this may occur because a proportion of regulatory T cells in the peripheral blood decreases while patients are on idelalisib. The team believes this early hepatotoxicity is immune-mediated.
Benjamin Lampson, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, described these surprising findings at the 2015 ASH Annual Meeting as abstract 497.*
Study design and patient demographics
Patients received 150 mg of idelalisib twice daily as monotherapy on days 1 through 56. They then received combination therapy with idelalisib plus ofatumumab for 8 weekly infusions, followed by 4 monthly infusions through day 225, and then idelalisib monotherapy indefinitely.
The primary endpoint of overall response rate was assessed 2 months after the completion of combination therapy.
“This dosing strategy is slightly different than what has been previously used in trials combining these particular drugs,” Dr Lampson said. “Specifically, previously reported trials started these agents simultaneously without a lead-in period of monotherapy.”
The investigators monitored the patients weekly for toxicities during the 2-month monotherapy lead-in period.
Three-quarters of the patients are male. Their median age is 67.4 years (range, 57.6–84.9), 54% have unmutated IgHV, 17% have deletion 17p or TP53 mutation, 4% have deletion 11q, and 54% have deletion 13q.
The patients received no prior therapies.
Results
The trial is currently ongoing.
The 24 patients enrolled as of early November have been on therapy a median of 7.7 months, for a median follow-up time of 14.7 months.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr Lampson said.
In the first 2 months of therapy, 52% of patients developed transaminitis, and 13% developed colitis or diarrhea, all grade 3 or higher. Thirteen percent developed pneumonitis of any grade.
Younger age is a risk factor for early hepatotoxicity, Dr Lampson said, with a significance of P=0.02. All subjects age 65 or younger (n=7) required systemic steroids to treat their toxicities.
Hepatotoxicity developed in a median of 28 days, he said, “and the hepatotoxicity is typically occurring before the first dose of ofatumumab is administered at week 8, suggesting that idelalisib alone is the cause of the hepatotoxicity.”
Dr Lampson noted that toxicities resolved rapidly with steroids.
“I do want to point out that all subjects evaluable for a response have had a response,” he added. “Additionally, in all subjects where treatment has been discontinued, the discontinuation was due to adverse events rather than disease progression.”
Twelve patients with grade 2 or higher transaminitis were re-challenged with idelalisib after holding the drug for toxicity.
Five patients were re-challenged while off steroids, and 4 developed recurrent transaminitis within 4 days. Seven patients were re-challenged while on steroids, and 2 developed recurrent transaminitis within 4 days.
“In general, our experience has been, if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject can eventually be taken off steroids,” Dr Lampson said.
Comparison with earlier studies
The investigators compared the frequency of toxicity in their trial to earlier studies of idelalisib (Brown, Blood 2014; Coutre, EHA 2015, abstr P588; O’Brien, Blood 2015).
They found that grade 3 or higher transaminitis (52%) and any grade pneumonitis (13%) were higher in their trial than in the 3 other trials.
Colitis/diarrhea was about the same in 2 of the 3 other trials. But in the paper by O’Brien et al, 42% of patients experienced grade 3 or greater colitis/diarrhea.
The lower rate of colitis in the present trial may be due to the shorter follow-up, Dr Lampson said, as colitis is a late adverse event.
The O’Brien trial was also an upfront study, so patients had no prior therapies. The investigators observed that toxicities appeared to be more common in less heavily pretreated patients.
“As the median number of prior therapies decreases,” Dr Lampson said, “the frequency of adverse events increases.”
He noted that, in the O’Brien trial, idelalisib was started simultaneously with the other drugs, perhaps accounting for its somewhat lower rate (21%) of grade 3 or higher transaminitis.
Additionally, the patient population in the O’Brien trial was older than the population in the current trial, which could account for the higher rate of transaminitis, as younger age is a risk factor.
Decrease in regulatory T cells
Investigators noted a decrease in regulatory T cells while patients were on therapy. Eleven of 15 patients (73%) with matched samples had a significant (P<0.05) decrease in the percentage of T cells over time.
This, they say, could provide a possible explanation for the development of early hepatotoxicity.
The trial is investigator-initiated and funded by Gilead Sciences. ![]()
*Data in the presentation differs from the abstract.

Photo courtesy of ASH
ORLANDO, FL—Investigators have observed early fulminant hepatotoxicity in a subset of primarily younger chronic lymphocytic leukemia (CLL) patients treated with idelalisib monotherapy in the frontline setting.
In a phase 2 study of idelalisib plus ofatumumab, 52% of the 24 patients enrolled experienced grade 3 or higher hepatotoxicity shortly after idelalisib was started.
The investigators say this may occur because a proportion of regulatory T cells in the peripheral blood decreases while patients are on idelalisib. The team believes this early hepatotoxicity is immune-mediated.
Benjamin Lampson, MD, PhD, of the Dana-Farber Cancer Institute in Boston, Massachusetts, described these surprising findings at the 2015 ASH Annual Meeting as abstract 497.*
Study design and patient demographics
Patients received 150 mg of idelalisib twice daily as monotherapy on days 1 through 56. They then received combination therapy with idelalisib plus ofatumumab for 8 weekly infusions, followed by 4 monthly infusions through day 225, and then idelalisib monotherapy indefinitely.
The primary endpoint of overall response rate was assessed 2 months after the completion of combination therapy.
“This dosing strategy is slightly different than what has been previously used in trials combining these particular drugs,” Dr Lampson said. “Specifically, previously reported trials started these agents simultaneously without a lead-in period of monotherapy.”
The investigators monitored the patients weekly for toxicities during the 2-month monotherapy lead-in period.
Three-quarters of the patients are male. Their median age is 67.4 years (range, 57.6–84.9), 54% have unmutated IgHV, 17% have deletion 17p or TP53 mutation, 4% have deletion 11q, and 54% have deletion 13q.
The patients received no prior therapies.
Results
The trial is currently ongoing.
The 24 patients enrolled as of early November have been on therapy a median of 7.7 months, for a median follow-up time of 14.7 months.
“What we began to notice after enrolling just a few subjects on the trial was that severe hepatotoxicity was occurring shortly after initiating idelalisib,” Dr Lampson said.
In the first 2 months of therapy, 52% of patients developed transaminitis, and 13% developed colitis or diarrhea, all grade 3 or higher. Thirteen percent developed pneumonitis of any grade.
Younger age is a risk factor for early hepatotoxicity, Dr Lampson said, with a significance of P=0.02. All subjects age 65 or younger (n=7) required systemic steroids to treat their toxicities.
Hepatotoxicity developed in a median of 28 days, he said, “and the hepatotoxicity is typically occurring before the first dose of ofatumumab is administered at week 8, suggesting that idelalisib alone is the cause of the hepatotoxicity.”
Dr Lampson noted that toxicities resolved rapidly with steroids.
“I do want to point out that all subjects evaluable for a response have had a response,” he added. “Additionally, in all subjects where treatment has been discontinued, the discontinuation was due to adverse events rather than disease progression.”
Twelve patients with grade 2 or higher transaminitis were re-challenged with idelalisib after holding the drug for toxicity.
Five patients were re-challenged while off steroids, and 4 developed recurrent transaminitis within 4 days. Seven patients were re-challenged while on steroids, and 2 developed recurrent transaminitis within 4 days.
“In general, our experience has been, if idelalisib is resumed while the subject remains on steroids, the drug is more likely to be tolerated and the subject can eventually be taken off steroids,” Dr Lampson said.
Comparison with earlier studies
The investigators compared the frequency of toxicity in their trial to earlier studies of idelalisib (Brown, Blood 2014; Coutre, EHA 2015, abstr P588; O’Brien, Blood 2015).
They found that grade 3 or higher transaminitis (52%) and any grade pneumonitis (13%) were higher in their trial than in the 3 other trials.
Colitis/diarrhea was about the same in 2 of the 3 other trials. But in the paper by O’Brien et al, 42% of patients experienced grade 3 or greater colitis/diarrhea.
The lower rate of colitis in the present trial may be due to the shorter follow-up, Dr Lampson said, as colitis is a late adverse event.
The O’Brien trial was also an upfront study, so patients had no prior therapies. The investigators observed that toxicities appeared to be more common in less heavily pretreated patients.
“As the median number of prior therapies decreases,” Dr Lampson said, “the frequency of adverse events increases.”
He noted that, in the O’Brien trial, idelalisib was started simultaneously with the other drugs, perhaps accounting for its somewhat lower rate (21%) of grade 3 or higher transaminitis.
Additionally, the patient population in the O’Brien trial was older than the population in the current trial, which could account for the higher rate of transaminitis, as younger age is a risk factor.
Decrease in regulatory T cells
Investigators noted a decrease in regulatory T cells while patients were on therapy. Eleven of 15 patients (73%) with matched samples had a significant (P<0.05) decrease in the percentage of T cells over time.
This, they say, could provide a possible explanation for the development of early hepatotoxicity.
The trial is investigator-initiated and funded by Gilead Sciences. ![]()
*Data in the presentation differs from the abstract.
Group recommends adding rituximab to ALL therapy

Photo courtesy of ASH
ORLANDO, FL—Investigators from the Group for Research on Adult Lymphoblastic Leukemia (GRAALL) recommend integrating rituximab into the treatment of adult patients with acute lymphoblastic leukemia (ALL) based on results of the GRAALL-R 2005 study.
Patients who received rituximab as part of their therapy had a median event-free survival (EFS) at 2 years of 65%, compared to 52% for patients who did not receive rituximab. After censoring for stem cell transplant in first complete remission, the benefit was even greater.
Sébastien Maury, MD, PhD, of Hȏpital Hénri Mondor in Creteil, France, presented the results during the plenary session of the 2015 ASH Annual Meeting as abstract 1.
Dr Maury said GRAALL-R 2005 is the first phase 3, randomized study to evaluate the role of rituximab in the treatment of B-cell precursor (BCP) ALL.
Only one previous study, he said, suggested a potential benefit of adding rituximab compared to historic controls of chemotherapy alone.
He explained that, because the CD20 antigen is expressed at diagnosis in 30% to 40% of patients with BCP-ALL, investigators undertook to evaluate whether adding the anti-CD20 monoclonal antibody rituximab to the ALL treatment regimen could be beneficial for newly diagnosed Ph-negative BCP-ALL patients.
Study design & population
Investigators randomized 105 patients to receive the pediatric-inspired GRAALL protocol plus rituximab and 104 patients to the same regimen without rituximab.
Patients had to have 20% or more CD20-positive leukemic blasts.
Patients in the rituximab arm received 375 mg/m2 during induction on days 1 and 7, during salvage reinduction (if needed) on days 1 and 7, during consolidation blocks (6 infusions), during late intensification on days 1 and 7, and during the first year of maintenance (6 infusions), for a total of 16 to 18 infusions.
“In this trial, allogeneic transplantation was offered in first remission to high-risk patients who were those patients with at least one of these baseline or response-related criteria,” Dr Maury said.
Investigators defined high-risk at baseline as having a white blood cell count of 30 x 109/L or higher, CNS involvement, CD10-negative disease, or unfavorable cytogenetics.
And response-related criteria for high-risk disease included poor peripheral blast clearance after the 1-week steroid pre-phase, poor bone marrow blast clearance after the first week of chemotherapy, or no hematologic complete response after the first induction course.
Patient characteristics were well balanced between the arms, with a median age for the entire group of 40.2 years. Rituximab-treated patients had 61% CD20-positive blasts, and the no-rituximab arm had 69%.
More patients in the rituximab arm had a better ECOG performance status, although the difference was not significant. Thirteen percent were assessed as being grade 2 or higher in the rituximab arm, compared with 18% in the no-rituximab arm (P=0.06).
“The proportion of high-risk patients was comparable in both arms,” Dr Maury said, “representing around two-thirds of the study population.”
In the rituximab arm, 70% were considered high-risk, compared with 64% in the no-rituximab arm (P=0.46).
“However, despite this,” he said, “a significantly higher proportion of patients received allo transplant at first remission in the rituximab arm, 34% versus 20%. And since this was not explained by a different proportion of high-risk patients, this was probably due to differences in donor availability.”
Dr Maury noted that compliance to treatment was “quite good.”
Efficacy
The median follow-up was 30 months, and the primary endpoint was EFS.
The EFS rate for rituximab-treated patients at 2 years was 65%, compared with 52% for the non-rituximab patients (hazard ratio=0.66, P=0.038).
EFS was also significantly better with rituximab when patients were censored at allogeneic transplant, with a hazard ratio of 0.59 and a significance of 0.021.
However, there were no significant differences in early complete response rates, minimal residual disease (MRD) after induction, and MRD after consolidation.
“[O]nly 40% of patients could be centrally analyzed [for MRD],” Dr Maury explained, “which may be the reason why we could not detect any impact of rituximab on MRD.”
The cumulative incidence of relapse at 2 years was 18% in the rituximab arm and 32% in the no-rituximab arm (hazard ratio=0.52, P=0.017). And after censoring for stem cell transplant in first complete remission, the hazard ratio was 0.49 in favor of rituximab (P=0.018).
Overall survival (OS) was not significantly different between the arms. Rituximab-treated patients had an OS rate of 71%, compared with 64% in the no-rituximab arm (P=0.095).
“However, this difference became significant when censoring patients at time of allo-transplant,” Dr Maury said.
There was a 12% cumulative incidence of death in first complete remission at 2 years in each arm.
Investigators performed multivariate analysis and found that treatment with rituximab (P=0.020), age (P=0.022), white blood cell count of 30 x 109/L or higher (P=0.005), and CNS involvement all significantly impacted EFS.
When they introduced stem cell transplant in first remission as a covariable, the same factors remained significant. Allogeneic stem cell transplant in first remission did not make a significant difference on EFS (P=0.62).
Safety
One hundred twenty-four patients reported 246 severe adverse events, the most frequent of which was infection—71 in the rituximab arm and 55 in the no-rituximab arm, a difference that was not significant (P=0.16).
Severe allergic events were significantly different between the arms, with 2 severe allergic events reported in the rituximab arm and 14 in the no-rituximab arm (P=0.002). Of these 16 events, all but one were due to asparaginase.
“We believe that this may reflect the protective effect of rituximab that might inhibit B-cell protection of antibodies against asparaginase,” Dr Maury said, although the investigators did not actually measure the antibodies.
Severe lab abnormalities, neurologic and pulmonary events, coagulopathy, cardiologic and gastrointestinal events were not significantly different between the arms.
Dr Maury emphasized that the addition of rituximab to standard intensive chemotherapy is well tolerated, significantly improves EFS, and prolongs OS in patients not receiving allogeneic transplant in first remission.
While the optimal dose schedule of rituximab still remains to be determined, the GRAALL investigators believe that “the addition of rituximab should be the new standard of care for these patients,” Dr Maury declared. ![]()

Photo courtesy of ASH
ORLANDO, FL—Investigators from the Group for Research on Adult Lymphoblastic Leukemia (GRAALL) recommend integrating rituximab into the treatment of adult patients with acute lymphoblastic leukemia (ALL) based on results of the GRAALL-R 2005 study.
Patients who received rituximab as part of their therapy had a median event-free survival (EFS) at 2 years of 65%, compared to 52% for patients who did not receive rituximab. After censoring for stem cell transplant in first complete remission, the benefit was even greater.
Sébastien Maury, MD, PhD, of Hȏpital Hénri Mondor in Creteil, France, presented the results during the plenary session of the 2015 ASH Annual Meeting as abstract 1.
Dr Maury said GRAALL-R 2005 is the first phase 3, randomized study to evaluate the role of rituximab in the treatment of B-cell precursor (BCP) ALL.
Only one previous study, he said, suggested a potential benefit of adding rituximab compared to historic controls of chemotherapy alone.
He explained that, because the CD20 antigen is expressed at diagnosis in 30% to 40% of patients with BCP-ALL, investigators undertook to evaluate whether adding the anti-CD20 monoclonal antibody rituximab to the ALL treatment regimen could be beneficial for newly diagnosed Ph-negative BCP-ALL patients.
Study design & population
Investigators randomized 105 patients to receive the pediatric-inspired GRAALL protocol plus rituximab and 104 patients to the same regimen without rituximab.
Patients had to have 20% or more CD20-positive leukemic blasts.
Patients in the rituximab arm received 375 mg/m2 during induction on days 1 and 7, during salvage reinduction (if needed) on days 1 and 7, during consolidation blocks (6 infusions), during late intensification on days 1 and 7, and during the first year of maintenance (6 infusions), for a total of 16 to 18 infusions.
“In this trial, allogeneic transplantation was offered in first remission to high-risk patients who were those patients with at least one of these baseline or response-related criteria,” Dr Maury said.
Investigators defined high-risk at baseline as having a white blood cell count of 30 x 109/L or higher, CNS involvement, CD10-negative disease, or unfavorable cytogenetics.
And response-related criteria for high-risk disease included poor peripheral blast clearance after the 1-week steroid pre-phase, poor bone marrow blast clearance after the first week of chemotherapy, or no hematologic complete response after the first induction course.
Patient characteristics were well balanced between the arms, with a median age for the entire group of 40.2 years. Rituximab-treated patients had 61% CD20-positive blasts, and the no-rituximab arm had 69%.
More patients in the rituximab arm had a better ECOG performance status, although the difference was not significant. Thirteen percent were assessed as being grade 2 or higher in the rituximab arm, compared with 18% in the no-rituximab arm (P=0.06).
“The proportion of high-risk patients was comparable in both arms,” Dr Maury said, “representing around two-thirds of the study population.”
In the rituximab arm, 70% were considered high-risk, compared with 64% in the no-rituximab arm (P=0.46).
“However, despite this,” he said, “a significantly higher proportion of patients received allo transplant at first remission in the rituximab arm, 34% versus 20%. And since this was not explained by a different proportion of high-risk patients, this was probably due to differences in donor availability.”
Dr Maury noted that compliance to treatment was “quite good.”
Efficacy
The median follow-up was 30 months, and the primary endpoint was EFS.
The EFS rate for rituximab-treated patients at 2 years was 65%, compared with 52% for the non-rituximab patients (hazard ratio=0.66, P=0.038).
EFS was also significantly better with rituximab when patients were censored at allogeneic transplant, with a hazard ratio of 0.59 and a significance of 0.021.
However, there were no significant differences in early complete response rates, minimal residual disease (MRD) after induction, and MRD after consolidation.
“[O]nly 40% of patients could be centrally analyzed [for MRD],” Dr Maury explained, “which may be the reason why we could not detect any impact of rituximab on MRD.”
The cumulative incidence of relapse at 2 years was 18% in the rituximab arm and 32% in the no-rituximab arm (hazard ratio=0.52, P=0.017). And after censoring for stem cell transplant in first complete remission, the hazard ratio was 0.49 in favor of rituximab (P=0.018).
Overall survival (OS) was not significantly different between the arms. Rituximab-treated patients had an OS rate of 71%, compared with 64% in the no-rituximab arm (P=0.095).
“However, this difference became significant when censoring patients at time of allo-transplant,” Dr Maury said.
There was a 12% cumulative incidence of death in first complete remission at 2 years in each arm.
Investigators performed multivariate analysis and found that treatment with rituximab (P=0.020), age (P=0.022), white blood cell count of 30 x 109/L or higher (P=0.005), and CNS involvement all significantly impacted EFS.
When they introduced stem cell transplant in first remission as a covariable, the same factors remained significant. Allogeneic stem cell transplant in first remission did not make a significant difference on EFS (P=0.62).
Safety
One hundred twenty-four patients reported 246 severe adverse events, the most frequent of which was infection—71 in the rituximab arm and 55 in the no-rituximab arm, a difference that was not significant (P=0.16).
Severe allergic events were significantly different between the arms, with 2 severe allergic events reported in the rituximab arm and 14 in the no-rituximab arm (P=0.002). Of these 16 events, all but one were due to asparaginase.
“We believe that this may reflect the protective effect of rituximab that might inhibit B-cell protection of antibodies against asparaginase,” Dr Maury said, although the investigators did not actually measure the antibodies.
Severe lab abnormalities, neurologic and pulmonary events, coagulopathy, cardiologic and gastrointestinal events were not significantly different between the arms.
Dr Maury emphasized that the addition of rituximab to standard intensive chemotherapy is well tolerated, significantly improves EFS, and prolongs OS in patients not receiving allogeneic transplant in first remission.
While the optimal dose schedule of rituximab still remains to be determined, the GRAALL investigators believe that “the addition of rituximab should be the new standard of care for these patients,” Dr Maury declared. ![]()

Photo courtesy of ASH
ORLANDO, FL—Investigators from the Group for Research on Adult Lymphoblastic Leukemia (GRAALL) recommend integrating rituximab into the treatment of adult patients with acute lymphoblastic leukemia (ALL) based on results of the GRAALL-R 2005 study.
Patients who received rituximab as part of their therapy had a median event-free survival (EFS) at 2 years of 65%, compared to 52% for patients who did not receive rituximab. After censoring for stem cell transplant in first complete remission, the benefit was even greater.
Sébastien Maury, MD, PhD, of Hȏpital Hénri Mondor in Creteil, France, presented the results during the plenary session of the 2015 ASH Annual Meeting as abstract 1.
Dr Maury said GRAALL-R 2005 is the first phase 3, randomized study to evaluate the role of rituximab in the treatment of B-cell precursor (BCP) ALL.
Only one previous study, he said, suggested a potential benefit of adding rituximab compared to historic controls of chemotherapy alone.
He explained that, because the CD20 antigen is expressed at diagnosis in 30% to 40% of patients with BCP-ALL, investigators undertook to evaluate whether adding the anti-CD20 monoclonal antibody rituximab to the ALL treatment regimen could be beneficial for newly diagnosed Ph-negative BCP-ALL patients.
Study design & population
Investigators randomized 105 patients to receive the pediatric-inspired GRAALL protocol plus rituximab and 104 patients to the same regimen without rituximab.
Patients had to have 20% or more CD20-positive leukemic blasts.
Patients in the rituximab arm received 375 mg/m2 during induction on days 1 and 7, during salvage reinduction (if needed) on days 1 and 7, during consolidation blocks (6 infusions), during late intensification on days 1 and 7, and during the first year of maintenance (6 infusions), for a total of 16 to 18 infusions.
“In this trial, allogeneic transplantation was offered in first remission to high-risk patients who were those patients with at least one of these baseline or response-related criteria,” Dr Maury said.
Investigators defined high-risk at baseline as having a white blood cell count of 30 x 109/L or higher, CNS involvement, CD10-negative disease, or unfavorable cytogenetics.
And response-related criteria for high-risk disease included poor peripheral blast clearance after the 1-week steroid pre-phase, poor bone marrow blast clearance after the first week of chemotherapy, or no hematologic complete response after the first induction course.
Patient characteristics were well balanced between the arms, with a median age for the entire group of 40.2 years. Rituximab-treated patients had 61% CD20-positive blasts, and the no-rituximab arm had 69%.
More patients in the rituximab arm had a better ECOG performance status, although the difference was not significant. Thirteen percent were assessed as being grade 2 or higher in the rituximab arm, compared with 18% in the no-rituximab arm (P=0.06).
“The proportion of high-risk patients was comparable in both arms,” Dr Maury said, “representing around two-thirds of the study population.”
In the rituximab arm, 70% were considered high-risk, compared with 64% in the no-rituximab arm (P=0.46).
“However, despite this,” he said, “a significantly higher proportion of patients received allo transplant at first remission in the rituximab arm, 34% versus 20%. And since this was not explained by a different proportion of high-risk patients, this was probably due to differences in donor availability.”
Dr Maury noted that compliance to treatment was “quite good.”
Efficacy
The median follow-up was 30 months, and the primary endpoint was EFS.
The EFS rate for rituximab-treated patients at 2 years was 65%, compared with 52% for the non-rituximab patients (hazard ratio=0.66, P=0.038).
EFS was also significantly better with rituximab when patients were censored at allogeneic transplant, with a hazard ratio of 0.59 and a significance of 0.021.
However, there were no significant differences in early complete response rates, minimal residual disease (MRD) after induction, and MRD after consolidation.
“[O]nly 40% of patients could be centrally analyzed [for MRD],” Dr Maury explained, “which may be the reason why we could not detect any impact of rituximab on MRD.”
The cumulative incidence of relapse at 2 years was 18% in the rituximab arm and 32% in the no-rituximab arm (hazard ratio=0.52, P=0.017). And after censoring for stem cell transplant in first complete remission, the hazard ratio was 0.49 in favor of rituximab (P=0.018).
Overall survival (OS) was not significantly different between the arms. Rituximab-treated patients had an OS rate of 71%, compared with 64% in the no-rituximab arm (P=0.095).
“However, this difference became significant when censoring patients at time of allo-transplant,” Dr Maury said.
There was a 12% cumulative incidence of death in first complete remission at 2 years in each arm.
Investigators performed multivariate analysis and found that treatment with rituximab (P=0.020), age (P=0.022), white blood cell count of 30 x 109/L or higher (P=0.005), and CNS involvement all significantly impacted EFS.
When they introduced stem cell transplant in first remission as a covariable, the same factors remained significant. Allogeneic stem cell transplant in first remission did not make a significant difference on EFS (P=0.62).
Safety
One hundred twenty-four patients reported 246 severe adverse events, the most frequent of which was infection—71 in the rituximab arm and 55 in the no-rituximab arm, a difference that was not significant (P=0.16).
Severe allergic events were significantly different between the arms, with 2 severe allergic events reported in the rituximab arm and 14 in the no-rituximab arm (P=0.002). Of these 16 events, all but one were due to asparaginase.
“We believe that this may reflect the protective effect of rituximab that might inhibit B-cell protection of antibodies against asparaginase,” Dr Maury said, although the investigators did not actually measure the antibodies.
Severe lab abnormalities, neurologic and pulmonary events, coagulopathy, cardiologic and gastrointestinal events were not significantly different between the arms.
Dr Maury emphasized that the addition of rituximab to standard intensive chemotherapy is well tolerated, significantly improves EFS, and prolongs OS in patients not receiving allogeneic transplant in first remission.
While the optimal dose schedule of rituximab still remains to be determined, the GRAALL investigators believe that “the addition of rituximab should be the new standard of care for these patients,” Dr Maury declared.
RATIFY trial results available after almost 10 years in the making

Photo courtesy of ASH
ORLANDO, FL—After almost 10 years, during which time no new drug for acute myeloid leukemia (AML) has been approved, results of the RATIFY trial are available.
In this trial, investigators evaluated midostaurin in combination with chemotherapy for younger patients with FLT3-mutated AML.
Patients who received midostaurin in their regimen instead of placebo experienced significantly longer overall survival (OS) and event-free survival (EFS).
“The primary endpoint of the trial was overall survival—which was very important—uncensored for transplant,” said Richard Stone, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“This is very much a ‘real-world’ trial. We just took patients from the start and saw how they did until the end.”
Dr Stone presented results from the trial during the plenary session of the 2015 ASH Annual Meeting (abstract 6*).
Midostaurin (PKC412), developed as a VEGF and protein kinase C inhibitor, is a known FLT3 inhibitor that specifically inhibits the growth of leukemic cell lines.
As a multi-kinase inhibitor, its potency against FLT3 may be limited, but it is active against both ITD and TKD mutations. Because AML is polyclonal at diagnosis, a multi-targeted inhibitor may have an advantage in newly diagnosed AML.
As a single agent, Dr Stone explained, midostaurin produced few remissions in advanced, mutant AML. But when combined with chemotherapy in a phase 1B study in newly diagnosed patients, it produced encouraging results.
So members of the Alliance for Clinical Trials in Oncology, formerly CALGB, and many other cooperative groups around the world—the AMLSG, CETLAM, ECOG, EORTC, GIMEMA, NCIC, OSHO, PETHEMA, SAL, and SWOG—conducted a phase 3, randomized, double-blind trial of induction and consolidation with or without midostaurin in patients younger than 60 with newly diagnosed FLT3-mutated AML.
The primary endpoint was OS, and secondary endpoints were OS censored and uncensored at the time of transplant, complete remission (CR) rates, EFS, disease-free survival (DFS), and adverse events.
Mark Levis, MD, of Johns Hopkins Sidney Kimmel Comprehensive Cancer Center in Baltimore, Maryland, who introduced the plenary presentation, suggested that OS may not be the best primary endpoint for an AML trial, given the long time it takes to complete a trial like this.
He pointed out that, “while we waited for RATIFY to accrue and mature, our approach to the disease changed.” Allogeneic transplant is now often the favored consolidation.
Eligibility criteria
Patients aged 18 to 60 with normal end-organ function and documented AML were eligible to enroll. Patients could not have had acute promyelocytic leukemia.
Their FLT3 mutation had to be centrally determined prior to enrollment by 1 of 9 academic labs around the world, and results had to be obtainable within 48 hours of sample collection.
Patients could receive up to 5 days of hydroxyurea prior to the start of treatment while awaiting the results of the mutation analysis.
Trial design
Investigators randomized patients to induction of daunorubicin and cytarabine with either midostaurin or placebo.
Daunorubicin was administered at 60 mg/m2 by intravenous push on days 1-3, cytarabine at 200 mg/m2 per day on days 1-7, and midostaurin at 50 mg orally twice a day on days 8-21.
A second cycle of induction was given based on day 21 bone marrow biopsy.
When patients achieved CR, they went on to consolidation with high-dose cytarabine (3 g/m2 over 3 hours every 12 hours on days 1, 3, and 5) and either midostaurin at the same induction dose or placebo.
After up to 4 doses of consolidation, patients went on to maintenance therapy for 12 months. This consisted of placebo or midostaurin at the same dose twice daily on days 1-28.
Patient population
The investigators screened 3279 patients younger than 60 years with newly diagnosed AML and found 27% (n=887) to be FLT3-positive.
They randomized 717 patients—81% of the FLT3-positive patients—to either the midostaurin arm (n=360) or the placebo arm (n=357). These 717 patients were evaluable for the intent-to-treat analysis.
The median age was 47.1 (range, 19.0–59.8) in the midostaurin arm and 48.6 (range, 18.0–60.9) in the placebo arm. There were significantly more males in the midostaurin arm (48.1%) than in the placebo arm (40.6%, P=0.045).
And the arms were almost identical for FLT3 stratification. In the midostaurin group, 22.5% had FLT3 TKD (no ITD), 47.5% had an ITD allelic ratio (+/- FLT3 TKD) less than 0.7, and 30.0% had a ratio of 0.7 or more.
In the placebo arm, 22.7% had FLT3 TKD, and 47.6% and 29.7% had ITD allelic ratios less than and greater than 0.7, respectively.
Safety
Rash/desquamation was the only significant difference in grade 3-4 non-hematologic events between the arms, with 13% in the midostaurin arm and 8% in the placebo arm (P=0.02).
Other grade 3-4 non-hematologic events occurring in 10% of patients or more included, in the midostaurin and placebo arms, respectively: febrile neutropenia (81%, 82%), infection (40%, 38%), diarrhea (15%, 16%), hypokalemia (13%, 17%), pain (13%, 13%), other infection (12%, 12%), ALT/SGPT (12%, 9%), and fatigue (9%, 11%).
There were 18 deaths (5%) in the midostaurin arm and 19 (5.3%) in the placebo arm during induction and consolidation treatment.
Efficacy
OS was superior for patients randomized to midostaurin. The median survival was 74.7 months (range, 31.7-not estimable) in the midostaurin arm and 25.6 months (range,18.6-42.9) in the placebo arm (P=0.0076).
Overall, there were 357 deaths, 171 and 186 in the midostaurin and placebo arms, respectively.
The 5-year survival rate was 50.9% for midostaurin and 43.9% for placebo.
EFS was also superior for patients randomized to midostaurin (P=0.0032), at a median of 8.0 months for midostaurin and 3.6 months for placebo. The 5-year EFS was 27.5% for midostaurin and 19.3% for placebo.
The CR rates by day 60 were not significantly different between the arms, at 59% and 53% for midostaurin and placebo, respectively. And the median time to CR was the same in each group, at 35 days.
The survival benefit, both overall and event-free, was consistent regardless of whether the patients were FLT3-ITD high, low, or FLT3-TKD.
The OS and EFS benefits were also consistent in censored and uncensored analyses, despite the high stem cell transplant rate. Four hundred eight patients (57%) received a transplant, 212 in the midostaurin arm and 196 in the placebo arm.
“The trial was positive whether you censored the patients at transplant or you kept following them for the whole time,” Dr Stone said.
He concluded that this type of international collaborative AML study based on genotype at diagnosis is feasible to do. But it took “a lot of collaboration, a lot of cooperation, a lot of persistence, because the trial took a long time to conceive of, conduct, and analyze.”
*Data in the presentation differ from the abstract.

Photo courtesy of ASH
ORLANDO, FL—After almost 10 years, during which time no new drug for acute myeloid leukemia (AML) has been approved, results of the RATIFY trial are available.
In this trial, investigators evaluated midostaurin in combination with chemotherapy for younger patients with FLT3-mutated AML.
Patients who received midostaurin in their regimen instead of placebo experienced significantly longer overall survival (OS) and event-free survival (EFS).
“The primary endpoint of the trial was overall survival—which was very important—uncensored for transplant,” said Richard Stone, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“This is very much a ‘real-world’ trial. We just took patients from the start and saw how they did until the end.”
Dr Stone presented results from the trial during the plenary session of the 2015 ASH Annual Meeting (abstract 6*).
Midostaurin (PKC412), developed as a VEGF and protein kinase C inhibitor, is a known FLT3 inhibitor that specifically inhibits the growth of leukemic cell lines.
As a multi-kinase inhibitor, its potency against FLT3 may be limited, but it is active against both ITD and TKD mutations. Because AML is polyclonal at diagnosis, a multi-targeted inhibitor may have an advantage in newly diagnosed AML.
As a single agent, Dr Stone explained, midostaurin produced few remissions in advanced, mutant AML. But when combined with chemotherapy in a phase 1B study in newly diagnosed patients, it produced encouraging results.
So members of the Alliance for Clinical Trials in Oncology, formerly CALGB, and many other cooperative groups around the world—the AMLSG, CETLAM, ECOG, EORTC, GIMEMA, NCIC, OSHO, PETHEMA, SAL, and SWOG—conducted a phase 3, randomized, double-blind trial of induction and consolidation with or without midostaurin in patients younger than 60 with newly diagnosed FLT3-mutated AML.
The primary endpoint was OS, and secondary endpoints were OS censored and uncensored at the time of transplant, complete remission (CR) rates, EFS, disease-free survival (DFS), and adverse events.
Mark Levis, MD, of Johns Hopkins Sidney Kimmel Comprehensive Cancer Center in Baltimore, Maryland, who introduced the plenary presentation, suggested that OS may not be the best primary endpoint for an AML trial, given the long time it takes to complete a trial like this.
He pointed out that, “while we waited for RATIFY to accrue and mature, our approach to the disease changed.” Allogeneic transplant is now often the favored consolidation.
Eligibility criteria
Patients aged 18 to 60 with normal end-organ function and documented AML were eligible to enroll. Patients could not have had acute promyelocytic leukemia.
Their FLT3 mutation had to be centrally determined prior to enrollment by 1 of 9 academic labs around the world, and results had to be obtainable within 48 hours of sample collection.
Patients could receive up to 5 days of hydroxyurea prior to the start of treatment while awaiting the results of the mutation analysis.
Trial design
Investigators randomized patients to induction of daunorubicin and cytarabine with either midostaurin or placebo.
Daunorubicin was administered at 60 mg/m2 by intravenous push on days 1-3, cytarabine at 200 mg/m2 per day on days 1-7, and midostaurin at 50 mg orally twice a day on days 8-21.
A second cycle of induction was given based on day 21 bone marrow biopsy.
When patients achieved CR, they went on to consolidation with high-dose cytarabine (3 g/m2 over 3 hours every 12 hours on days 1, 3, and 5) and either midostaurin at the same induction dose or placebo.
After up to 4 doses of consolidation, patients went on to maintenance therapy for 12 months. This consisted of placebo or midostaurin at the same dose twice daily on days 1-28.
Patient population
The investigators screened 3279 patients younger than 60 years with newly diagnosed AML and found 27% (n=887) to be FLT3-positive.
They randomized 717 patients—81% of the FLT3-positive patients—to either the midostaurin arm (n=360) or the placebo arm (n=357). These 717 patients were evaluable for the intent-to-treat analysis.
The median age was 47.1 (range, 19.0–59.8) in the midostaurin arm and 48.6 (range, 18.0–60.9) in the placebo arm. There were significantly more males in the midostaurin arm (48.1%) than in the placebo arm (40.6%, P=0.045).
And the arms were almost identical for FLT3 stratification. In the midostaurin group, 22.5% had FLT3 TKD (no ITD), 47.5% had an ITD allelic ratio (+/- FLT3 TKD) less than 0.7, and 30.0% had a ratio of 0.7 or more.
In the placebo arm, 22.7% had FLT3 TKD, and 47.6% and 29.7% had ITD allelic ratios less than and greater than 0.7, respectively.
Safety
Rash/desquamation was the only significant difference in grade 3-4 non-hematologic events between the arms, with 13% in the midostaurin arm and 8% in the placebo arm (P=0.02).
Other grade 3-4 non-hematologic events occurring in 10% of patients or more included, in the midostaurin and placebo arms, respectively: febrile neutropenia (81%, 82%), infection (40%, 38%), diarrhea (15%, 16%), hypokalemia (13%, 17%), pain (13%, 13%), other infection (12%, 12%), ALT/SGPT (12%, 9%), and fatigue (9%, 11%).
There were 18 deaths (5%) in the midostaurin arm and 19 (5.3%) in the placebo arm during induction and consolidation treatment.
Efficacy
OS was superior for patients randomized to midostaurin. The median survival was 74.7 months (range, 31.7-not estimable) in the midostaurin arm and 25.6 months (range,18.6-42.9) in the placebo arm (P=0.0076).
Overall, there were 357 deaths, 171 and 186 in the midostaurin and placebo arms, respectively.
The 5-year survival rate was 50.9% for midostaurin and 43.9% for placebo.
EFS was also superior for patients randomized to midostaurin (P=0.0032), at a median of 8.0 months for midostaurin and 3.6 months for placebo. The 5-year EFS was 27.5% for midostaurin and 19.3% for placebo.
The CR rates by day 60 were not significantly different between the arms, at 59% and 53% for midostaurin and placebo, respectively. And the median time to CR was the same in each group, at 35 days.
The survival benefit, both overall and event-free, was consistent regardless of whether the patients were FLT3-ITD high, low, or FLT3-TKD.
The OS and EFS benefits were also consistent in censored and uncensored analyses, despite the high stem cell transplant rate. Four hundred eight patients (57%) received a transplant, 212 in the midostaurin arm and 196 in the placebo arm.
“The trial was positive whether you censored the patients at transplant or you kept following them for the whole time,” Dr Stone said.
He concluded that this type of international collaborative AML study based on genotype at diagnosis is feasible to do. But it took “a lot of collaboration, a lot of cooperation, a lot of persistence, because the trial took a long time to conceive of, conduct, and analyze.”
*Data in the presentation differ from the abstract.

Photo courtesy of ASH
ORLANDO, FL—After almost 10 years, during which time no new drug for acute myeloid leukemia (AML) has been approved, results of the RATIFY trial are available.
In this trial, investigators evaluated midostaurin in combination with chemotherapy for younger patients with FLT3-mutated AML.
Patients who received midostaurin in their regimen instead of placebo experienced significantly longer overall survival (OS) and event-free survival (EFS).
“The primary endpoint of the trial was overall survival—which was very important—uncensored for transplant,” said Richard Stone, MD, of Dana-Farber Cancer Institute in Boston, Massachusetts.
“This is very much a ‘real-world’ trial. We just took patients from the start and saw how they did until the end.”
Dr Stone presented results from the trial during the plenary session of the 2015 ASH Annual Meeting (abstract 6*).
Midostaurin (PKC412), developed as a VEGF and protein kinase C inhibitor, is a known FLT3 inhibitor that specifically inhibits the growth of leukemic cell lines.
As a multi-kinase inhibitor, its potency against FLT3 may be limited, but it is active against both ITD and TKD mutations. Because AML is polyclonal at diagnosis, a multi-targeted inhibitor may have an advantage in newly diagnosed AML.
As a single agent, Dr Stone explained, midostaurin produced few remissions in advanced, mutant AML. But when combined with chemotherapy in a phase 1B study in newly diagnosed patients, it produced encouraging results.
So members of the Alliance for Clinical Trials in Oncology, formerly CALGB, and many other cooperative groups around the world—the AMLSG, CETLAM, ECOG, EORTC, GIMEMA, NCIC, OSHO, PETHEMA, SAL, and SWOG—conducted a phase 3, randomized, double-blind trial of induction and consolidation with or without midostaurin in patients younger than 60 with newly diagnosed FLT3-mutated AML.
The primary endpoint was OS, and secondary endpoints were OS censored and uncensored at the time of transplant, complete remission (CR) rates, EFS, disease-free survival (DFS), and adverse events.
Mark Levis, MD, of Johns Hopkins Sidney Kimmel Comprehensive Cancer Center in Baltimore, Maryland, who introduced the plenary presentation, suggested that OS may not be the best primary endpoint for an AML trial, given the long time it takes to complete a trial like this.
He pointed out that, “while we waited for RATIFY to accrue and mature, our approach to the disease changed.” Allogeneic transplant is now often the favored consolidation.
Eligibility criteria
Patients aged 18 to 60 with normal end-organ function and documented AML were eligible to enroll. Patients could not have had acute promyelocytic leukemia.
Their FLT3 mutation had to be centrally determined prior to enrollment by 1 of 9 academic labs around the world, and results had to be obtainable within 48 hours of sample collection.
Patients could receive up to 5 days of hydroxyurea prior to the start of treatment while awaiting the results of the mutation analysis.
Trial design
Investigators randomized patients to induction of daunorubicin and cytarabine with either midostaurin or placebo.
Daunorubicin was administered at 60 mg/m2 by intravenous push on days 1-3, cytarabine at 200 mg/m2 per day on days 1-7, and midostaurin at 50 mg orally twice a day on days 8-21.
A second cycle of induction was given based on day 21 bone marrow biopsy.
When patients achieved CR, they went on to consolidation with high-dose cytarabine (3 g/m2 over 3 hours every 12 hours on days 1, 3, and 5) and either midostaurin at the same induction dose or placebo.
After up to 4 doses of consolidation, patients went on to maintenance therapy for 12 months. This consisted of placebo or midostaurin at the same dose twice daily on days 1-28.
Patient population
The investigators screened 3279 patients younger than 60 years with newly diagnosed AML and found 27% (n=887) to be FLT3-positive.
They randomized 717 patients—81% of the FLT3-positive patients—to either the midostaurin arm (n=360) or the placebo arm (n=357). These 717 patients were evaluable for the intent-to-treat analysis.
The median age was 47.1 (range, 19.0–59.8) in the midostaurin arm and 48.6 (range, 18.0–60.9) in the placebo arm. There were significantly more males in the midostaurin arm (48.1%) than in the placebo arm (40.6%, P=0.045).
And the arms were almost identical for FLT3 stratification. In the midostaurin group, 22.5% had FLT3 TKD (no ITD), 47.5% had an ITD allelic ratio (+/- FLT3 TKD) less than 0.7, and 30.0% had a ratio of 0.7 or more.
In the placebo arm, 22.7% had FLT3 TKD, and 47.6% and 29.7% had ITD allelic ratios less than and greater than 0.7, respectively.
Safety
Rash/desquamation was the only significant difference in grade 3-4 non-hematologic events between the arms, with 13% in the midostaurin arm and 8% in the placebo arm (P=0.02).
Other grade 3-4 non-hematologic events occurring in 10% of patients or more included, in the midostaurin and placebo arms, respectively: febrile neutropenia (81%, 82%), infection (40%, 38%), diarrhea (15%, 16%), hypokalemia (13%, 17%), pain (13%, 13%), other infection (12%, 12%), ALT/SGPT (12%, 9%), and fatigue (9%, 11%).
There were 18 deaths (5%) in the midostaurin arm and 19 (5.3%) in the placebo arm during induction and consolidation treatment.
Efficacy
OS was superior for patients randomized to midostaurin. The median survival was 74.7 months (range, 31.7-not estimable) in the midostaurin arm and 25.6 months (range,18.6-42.9) in the placebo arm (P=0.0076).
Overall, there were 357 deaths, 171 and 186 in the midostaurin and placebo arms, respectively.
The 5-year survival rate was 50.9% for midostaurin and 43.9% for placebo.
EFS was also superior for patients randomized to midostaurin (P=0.0032), at a median of 8.0 months for midostaurin and 3.6 months for placebo. The 5-year EFS was 27.5% for midostaurin and 19.3% for placebo.
The CR rates by day 60 were not significantly different between the arms, at 59% and 53% for midostaurin and placebo, respectively. And the median time to CR was the same in each group, at 35 days.
The survival benefit, both overall and event-free, was consistent regardless of whether the patients were FLT3-ITD high, low, or FLT3-TKD.
The OS and EFS benefits were also consistent in censored and uncensored analyses, despite the high stem cell transplant rate. Four hundred eight patients (57%) received a transplant, 212 in the midostaurin arm and 196 in the placebo arm.
“The trial was positive whether you censored the patients at transplant or you kept following them for the whole time,” Dr Stone said.
He concluded that this type of international collaborative AML study based on genotype at diagnosis is feasible to do. But it took “a lot of collaboration, a lot of cooperation, a lot of persistence, because the trial took a long time to conceive of, conduct, and analyze.”
*Data in the presentation differ from the abstract.
ALL patients over-report their 6MP compliance, researchers say

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added.

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added.

Photo courtesy of ASH
ORLANDO, FL—A study comparing subjective versus objective reporting of treatment compliance in patients with acute lymphoblastic leukemia (ALL) has shown that about a fourth of patients over-report how compliant they are with taking 6-mercaptopurine (6MP) as part of their maintenance therapy.
An earlier analysis of the Children’s Oncology Group (COG) AALL03N1 compliance study showed that adherence rates of less than 95% were associated with a 3.7-fold increased risk of relapse.
And about 40% of patients were non-adherent. Yet patients indicate they are taking their medication when questioned.
“We ask our patients if they are taking their meds,” said Wendy Landier, PhD, “and they tell us they are.”
“Even in this cohort who were being closely monitored and knew that they were being closely monitored electronically and were asked to self-report, we found over-reporting.”
Dr Landier, of the University of Alabama at Birmingham, reported these findings comparing self-reported adherence with electronic monitoring of 6MP intake at the 2015 ASH Annual Meeting (abstract 82).
The investigators collected data over 6 months from 416 ALL patients who were 21 years at diagnosis or younger and were receiving 6MP as part of their maintenance therapy.
Investigators measured subjective self-reporting by a patient questionnaire, which included patient demographic information in addition to the number of days the patient took 6MP over the past month.
For the objective medication event-monitoring system (MEMS), patients received a 6MP bottle that was fitted with a TrackCapTM. The cap had a microprocessor chip that recorded the date and time of each bottle opening.
Investigators downloaded the data at the end of the study. They then compared the MEMS with the self-reported data.
The investigators classified perfect reporters as those whose self-report corresponded to their MEMS.
They classified over-reporters as those whose self-report was greater than their MEMS data for 5 days or more and 50% of the months.
The rest they classified as others.
Patients were a median age of 6.0 years, and 277 (66.6%) were male. Parents completed the survey for patients younger than 12.
Two hundred forty-two patients (60.9%) had fathers whose education was less than some college, 159 (38.4%) had NCI high-risk disease, and 168 (40.4%) were non-adherent to 6MP as determined by earlier analysis of the COG AALL03N1 study.
Thirty-six percent were non-Hispanic white, 37% were Hispanic, 14% Asian, and 13% African American.
The investigators monitored the patients’ 6MP intake for a total of 1344 patient-months at 87 COG sites.
And the correlation between subjective and objective reporting was moderate, Dr Landier said, with the correlation ranging from 0.36 to 0.58.
Twelve percent of the patients were perfect reporters, with no difference between the reporting methods.
Twenty-four percent over-reported their intake, 1% under-reported their intake, and 64% were other.
The investigators analyzed variables associated with over-reporting and found that age 12 years or older (P=0.02), being Hispanic (P=0.02), Asian (P=0.02), or African American (P<0.001), paternal education less than college (P=0.02), and being classified as 6MP non-adherent (P<0.001) were all significant.
“Over-reporting of 6MP ingestion is common,” Dr Landier said, with 88% of patients or parents over-reporting the number of days 6MP was taken.
“What we’ve learned from this study is that we cannot rely on patients’ self-report in the clinic,” she said. “What we found is that only 12% of our patients are perfect, so to speak, and that the others mainly over-estimate, and I don’t believe intentionally.”
“[W]e need to have a better way of identifying which patients are at risk for over-reporting their intake, whether they’re aware of it or not,” she added.
Breast cancer drug may also work in MCL, myeloma
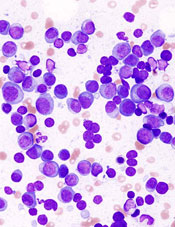
showing multiple myeloma
NEW YORK—Targeting the cell cycle with cyclin-dependent kinase (CDK) inhibitors may be an effective strategy to treat lymphoma and myeloma, according to a presentation at Lymphoma & Myeloma 2015.
Palbociclib, an inhibitor of CDK4 and CDK6, received accelerated approval from the US Food and Drug Administration to treat advanced breast cancer.
Now, it is showing promise in mantle cell lymphoma (MCL) and multiple myeloma (MM) as well.
CDK family members are important regulators of cell-cycle progression. Dysregulation of CDK4 and CDK6 is one of the most common genomic aberrations in human cancer, including myeloma, lymphoma, leukemia, breast cancer, metastatic lung adenocarcinoma, and glioblastoma.
MCL, which accounts for 6% of non-Hodgkin lymphomas, has an overall poor prognosis, with most patients eventually becoming resistant to drugs. MCL expresses cyclin D1 as a consequence of the t(11;14) translocation and overexpresses CDK4.
“So this is a perfect disease for the development of targeting CDK4,” said Selina Chen-Kiang, PhD, of Weill Cornell Medical College in New York, New York, who presented this information at the meeting.
CDK4 and CDK6 signaling occur at the beginning of the cell cycle and bring the cell from the resting state into early G2.
“If we could control that,” Dr Chen-Kiang explained, “we reasoned that we could control the DNA replication and cell division” and increase tumor-specific cell death.
Palbociclib (PD0332991; Ibrance), an orally bioavailable, selective CDK4/CDK6 inhibitor, induces early G1 arrest. It is reversible and low in toxicity, according to Dr Chen-Kiang.
Currently, it’s being tested in phase 1 trials in MCL with ibrutinib and in MM with lenalidomide-dexamethasone. Phase 1 trials have also been completed at Cornell with palbociclib as a single agent in MCL, with bortezomib in MCL, and with bortezomib-dexamethasone in MM.
Palbociclib in MCL
Investigators conducted a phase 1, single-agent study of palbociclib to determine whether it could be tolerated in humans.
“CDK4/CDK6 is expressed in every cell,” Dr Chen-Kiang noted, “and you are targeting 2 proteins that are needed for every cell.”
Seventeen patients received 125 mg of palbociclib per day for 21 of 28 days.
“And surprisingly,” Dr Chen-Kiang said, “it’s very well tolerated.”
The most common adverse events were neutropenia, fatigue, and diarrhea.
“And even more surprising,” she added “is that we actually had a complete response (CR) [and] 2 partial responses, in addition to 5 stable diseases.”
The investigators hypothesized that blocking the cell cycle in G1 creates an imbalance in gene expression.
They then conducted a trial of palbociclib plus bortezomib in 17 patients with recurrent MCL. Patients received palbociclib on days 1–12 and low-dose bortezomib on days 8, 11, 15, and 18.
The palbociclib dose ranged from 75 mg to 125 mg, and the bortezomib dose ranged from 1.0 mg/m2 to 1.3 mg/m2.
Eleven patients experienced a reduction in tumor volume, the majority at the 125-mg dose.
Using whole-exome and whole-transcriptome sequencing of serial biopsies, investigators determined that CDK4/CDK6 inhibition induces early G1 arrest in MCL cells in both responders and non-responders initially.
This may occur because the cell cycle is perfectly controlled, and there’s no mutation in CDK4 in any of the patients.
Investigators attempted to identify genes that could differentiate sensitivity from resistance to CDK4 targeting. They found that a very small number of genes display opposite regulation in prolonged early G1 arrest in responding versus non-responding patients.
These genes are involved in metabolism and redox homeostasis and include a gene called PIK3IP1, an inhibitor of PI3 kinase.
In earlier analyses, the investigators had discovered a relapse-specific C481S mutation at the ibrutinib binding site of Bruton’s tyrosine kinase (BTK) in MCL cells. The mutation occurred at progression following a durable response to ibrutinib.
The mutation is absent, however, in patients with transient ibrutinib responses or in primary resistance.
The team observed that early cell-cycle arrest by CDK4 inhibition reprograms MCL cells for killing by ibrutinib. This occurs through inhibition of BTK and AKT (protein kinase B).
So the investigators undertook to study palbociclib in combination with ibrutinib, “with extraordinary results,” Dr Chen-Kiang said.
The trial is ongoing and, at the moment, has a 60% CR rate with durable responses.
“We’re very happy with this,” Dr Chen-Kiang said.
Palbociclib in MM
In addition to the phase 1/2 study of palbociclib with bortezomib and dexamethasone, investigators are also pursuing palbociclib in combination with lenalidomide and dexamethasone, which Dr Chen-Kiang briefly elaborated upon.
Lenalidomide rarely produces a complete remission on its own, she explained, so the team decided to study palbociclib in combination with immunomodulatory drugs in MM (NCT02030483).
The strategy is to prime the cell cycle with palbociclib and then use lenalidomide and dexamethasone to increase efficacy.
Twenty patients have received this combination thus far, and investigators found that palbociclib enhances the activity of lenalidomide in the killing of primary bone marrow myeloma cells.
Lenalidomide reduces the MEIS2/CRBN ratio in these cells. The drug changes the ratio, reduces the blocker, and allows the CRBN to work.
“The whole principle here is to control the gene coupling to the cell cycle and induce imbalance in gene expression,” Dr Chen-Kiang said. “And this weakens the tumor cells.”
Two-thirds of the samples respond to palboclib, she said, and those patients go on to be treated with lenalidomide or pomalidomide.
One third will not respond, but their in vivo clinical response and the ex vivo responders’ purified cells mimic one another.
“Now, this is very exciting to us,” she said.
The combination study with lenalidomide and dexamethasone is currently underway.
Palbociclib is being developed by Pfizer.
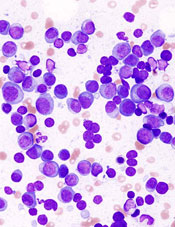
showing multiple myeloma
NEW YORK—Targeting the cell cycle with cyclin-dependent kinase (CDK) inhibitors may be an effective strategy to treat lymphoma and myeloma, according to a presentation at Lymphoma & Myeloma 2015.
Palbociclib, an inhibitor of CDK4 and CDK6, received accelerated approval from the US Food and Drug Administration to treat advanced breast cancer.
Now, it is showing promise in mantle cell lymphoma (MCL) and multiple myeloma (MM) as well.
CDK family members are important regulators of cell-cycle progression. Dysregulation of CDK4 and CDK6 is one of the most common genomic aberrations in human cancer, including myeloma, lymphoma, leukemia, breast cancer, metastatic lung adenocarcinoma, and glioblastoma.
MCL, which accounts for 6% of non-Hodgkin lymphomas, has an overall poor prognosis, with most patients eventually becoming resistant to drugs. MCL expresses cyclin D1 as a consequence of the t(11;14) translocation and overexpresses CDK4.
“So this is a perfect disease for the development of targeting CDK4,” said Selina Chen-Kiang, PhD, of Weill Cornell Medical College in New York, New York, who presented this information at the meeting.
CDK4 and CDK6 signaling occur at the beginning of the cell cycle and bring the cell from the resting state into early G2.
“If we could control that,” Dr Chen-Kiang explained, “we reasoned that we could control the DNA replication and cell division” and increase tumor-specific cell death.
Palbociclib (PD0332991; Ibrance), an orally bioavailable, selective CDK4/CDK6 inhibitor, induces early G1 arrest. It is reversible and low in toxicity, according to Dr Chen-Kiang.
Currently, it’s being tested in phase 1 trials in MCL with ibrutinib and in MM with lenalidomide-dexamethasone. Phase 1 trials have also been completed at Cornell with palbociclib as a single agent in MCL, with bortezomib in MCL, and with bortezomib-dexamethasone in MM.
Palbociclib in MCL
Investigators conducted a phase 1, single-agent study of palbociclib to determine whether it could be tolerated in humans.
“CDK4/CDK6 is expressed in every cell,” Dr Chen-Kiang noted, “and you are targeting 2 proteins that are needed for every cell.”
Seventeen patients received 125 mg of palbociclib per day for 21 of 28 days.
“And surprisingly,” Dr Chen-Kiang said, “it’s very well tolerated.”
The most common adverse events were neutropenia, fatigue, and diarrhea.
“And even more surprising,” she added “is that we actually had a complete response (CR) [and] 2 partial responses, in addition to 5 stable diseases.”
The investigators hypothesized that blocking the cell cycle in G1 creates an imbalance in gene expression.
They then conducted a trial of palbociclib plus bortezomib in 17 patients with recurrent MCL. Patients received palbociclib on days 1–12 and low-dose bortezomib on days 8, 11, 15, and 18.
The palbociclib dose ranged from 75 mg to 125 mg, and the bortezomib dose ranged from 1.0 mg/m2 to 1.3 mg/m2.
Eleven patients experienced a reduction in tumor volume, the majority at the 125-mg dose.
Using whole-exome and whole-transcriptome sequencing of serial biopsies, investigators determined that CDK4/CDK6 inhibition induces early G1 arrest in MCL cells in both responders and non-responders initially.
This may occur because the cell cycle is perfectly controlled, and there’s no mutation in CDK4 in any of the patients.
Investigators attempted to identify genes that could differentiate sensitivity from resistance to CDK4 targeting. They found that a very small number of genes display opposite regulation in prolonged early G1 arrest in responding versus non-responding patients.
These genes are involved in metabolism and redox homeostasis and include a gene called PIK3IP1, an inhibitor of PI3 kinase.
In earlier analyses, the investigators had discovered a relapse-specific C481S mutation at the ibrutinib binding site of Bruton’s tyrosine kinase (BTK) in MCL cells. The mutation occurred at progression following a durable response to ibrutinib.
The mutation is absent, however, in patients with transient ibrutinib responses or in primary resistance.
The team observed that early cell-cycle arrest by CDK4 inhibition reprograms MCL cells for killing by ibrutinib. This occurs through inhibition of BTK and AKT (protein kinase B).
So the investigators undertook to study palbociclib in combination with ibrutinib, “with extraordinary results,” Dr Chen-Kiang said.
The trial is ongoing and, at the moment, has a 60% CR rate with durable responses.
“We’re very happy with this,” Dr Chen-Kiang said.
Palbociclib in MM
In addition to the phase 1/2 study of palbociclib with bortezomib and dexamethasone, investigators are also pursuing palbociclib in combination with lenalidomide and dexamethasone, which Dr Chen-Kiang briefly elaborated upon.
Lenalidomide rarely produces a complete remission on its own, she explained, so the team decided to study palbociclib in combination with immunomodulatory drugs in MM (NCT02030483).
The strategy is to prime the cell cycle with palbociclib and then use lenalidomide and dexamethasone to increase efficacy.
Twenty patients have received this combination thus far, and investigators found that palbociclib enhances the activity of lenalidomide in the killing of primary bone marrow myeloma cells.
Lenalidomide reduces the MEIS2/CRBN ratio in these cells. The drug changes the ratio, reduces the blocker, and allows the CRBN to work.
“The whole principle here is to control the gene coupling to the cell cycle and induce imbalance in gene expression,” Dr Chen-Kiang said. “And this weakens the tumor cells.”
Two-thirds of the samples respond to palboclib, she said, and those patients go on to be treated with lenalidomide or pomalidomide.
One third will not respond, but their in vivo clinical response and the ex vivo responders’ purified cells mimic one another.
“Now, this is very exciting to us,” she said.
The combination study with lenalidomide and dexamethasone is currently underway.
Palbociclib is being developed by Pfizer.
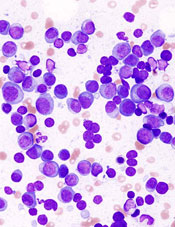
showing multiple myeloma
NEW YORK—Targeting the cell cycle with cyclin-dependent kinase (CDK) inhibitors may be an effective strategy to treat lymphoma and myeloma, according to a presentation at Lymphoma & Myeloma 2015.
Palbociclib, an inhibitor of CDK4 and CDK6, received accelerated approval from the US Food and Drug Administration to treat advanced breast cancer.
Now, it is showing promise in mantle cell lymphoma (MCL) and multiple myeloma (MM) as well.
CDK family members are important regulators of cell-cycle progression. Dysregulation of CDK4 and CDK6 is one of the most common genomic aberrations in human cancer, including myeloma, lymphoma, leukemia, breast cancer, metastatic lung adenocarcinoma, and glioblastoma.
MCL, which accounts for 6% of non-Hodgkin lymphomas, has an overall poor prognosis, with most patients eventually becoming resistant to drugs. MCL expresses cyclin D1 as a consequence of the t(11;14) translocation and overexpresses CDK4.
“So this is a perfect disease for the development of targeting CDK4,” said Selina Chen-Kiang, PhD, of Weill Cornell Medical College in New York, New York, who presented this information at the meeting.
CDK4 and CDK6 signaling occur at the beginning of the cell cycle and bring the cell from the resting state into early G2.
“If we could control that,” Dr Chen-Kiang explained, “we reasoned that we could control the DNA replication and cell division” and increase tumor-specific cell death.
Palbociclib (PD0332991; Ibrance), an orally bioavailable, selective CDK4/CDK6 inhibitor, induces early G1 arrest. It is reversible and low in toxicity, according to Dr Chen-Kiang.
Currently, it’s being tested in phase 1 trials in MCL with ibrutinib and in MM with lenalidomide-dexamethasone. Phase 1 trials have also been completed at Cornell with palbociclib as a single agent in MCL, with bortezomib in MCL, and with bortezomib-dexamethasone in MM.
Palbociclib in MCL
Investigators conducted a phase 1, single-agent study of palbociclib to determine whether it could be tolerated in humans.
“CDK4/CDK6 is expressed in every cell,” Dr Chen-Kiang noted, “and you are targeting 2 proteins that are needed for every cell.”
Seventeen patients received 125 mg of palbociclib per day for 21 of 28 days.
“And surprisingly,” Dr Chen-Kiang said, “it’s very well tolerated.”
The most common adverse events were neutropenia, fatigue, and diarrhea.
“And even more surprising,” she added “is that we actually had a complete response (CR) [and] 2 partial responses, in addition to 5 stable diseases.”
The investigators hypothesized that blocking the cell cycle in G1 creates an imbalance in gene expression.
They then conducted a trial of palbociclib plus bortezomib in 17 patients with recurrent MCL. Patients received palbociclib on days 1–12 and low-dose bortezomib on days 8, 11, 15, and 18.
The palbociclib dose ranged from 75 mg to 125 mg, and the bortezomib dose ranged from 1.0 mg/m2 to 1.3 mg/m2.
Eleven patients experienced a reduction in tumor volume, the majority at the 125-mg dose.
Using whole-exome and whole-transcriptome sequencing of serial biopsies, investigators determined that CDK4/CDK6 inhibition induces early G1 arrest in MCL cells in both responders and non-responders initially.
This may occur because the cell cycle is perfectly controlled, and there’s no mutation in CDK4 in any of the patients.
Investigators attempted to identify genes that could differentiate sensitivity from resistance to CDK4 targeting. They found that a very small number of genes display opposite regulation in prolonged early G1 arrest in responding versus non-responding patients.
These genes are involved in metabolism and redox homeostasis and include a gene called PIK3IP1, an inhibitor of PI3 kinase.
In earlier analyses, the investigators had discovered a relapse-specific C481S mutation at the ibrutinib binding site of Bruton’s tyrosine kinase (BTK) in MCL cells. The mutation occurred at progression following a durable response to ibrutinib.
The mutation is absent, however, in patients with transient ibrutinib responses or in primary resistance.
The team observed that early cell-cycle arrest by CDK4 inhibition reprograms MCL cells for killing by ibrutinib. This occurs through inhibition of BTK and AKT (protein kinase B).
So the investigators undertook to study palbociclib in combination with ibrutinib, “with extraordinary results,” Dr Chen-Kiang said.
The trial is ongoing and, at the moment, has a 60% CR rate with durable responses.
“We’re very happy with this,” Dr Chen-Kiang said.
Palbociclib in MM
In addition to the phase 1/2 study of palbociclib with bortezomib and dexamethasone, investigators are also pursuing palbociclib in combination with lenalidomide and dexamethasone, which Dr Chen-Kiang briefly elaborated upon.
Lenalidomide rarely produces a complete remission on its own, she explained, so the team decided to study palbociclib in combination with immunomodulatory drugs in MM (NCT02030483).
The strategy is to prime the cell cycle with palbociclib and then use lenalidomide and dexamethasone to increase efficacy.
Twenty patients have received this combination thus far, and investigators found that palbociclib enhances the activity of lenalidomide in the killing of primary bone marrow myeloma cells.
Lenalidomide reduces the MEIS2/CRBN ratio in these cells. The drug changes the ratio, reduces the blocker, and allows the CRBN to work.
“The whole principle here is to control the gene coupling to the cell cycle and induce imbalance in gene expression,” Dr Chen-Kiang said. “And this weakens the tumor cells.”
Two-thirds of the samples respond to palboclib, she said, and those patients go on to be treated with lenalidomide or pomalidomide.
One third will not respond, but their in vivo clinical response and the ex vivo responders’ purified cells mimic one another.
“Now, this is very exciting to us,” she said.
The combination study with lenalidomide and dexamethasone is currently underway.
Palbociclib is being developed by Pfizer.