User login
Latissimus Dorsi and Teres Major Injuries in Major League Baseball Pitchers: A Systematic Review
Upper extremity injuries are very common in pitchers in amateur and professional baseball. The vast majority involving labral or rotator cuff pathology.1-3 While uncommon, injuries to the latissimus dorsi (LD) (Figure) and teres major (TM) have been reported in Major League Baseball (MLB) pitchers.4 Jobe and colleagues5 demonstrated the role of the LD during the various phases of pitching. The LD is most active during the acceleration phase and remains active during the deceleration phase and follow-through.6 Anatomically, the TM lies posterior to the LD separated by bursal tissue. The tendon fibers converge and unite along their lower borders, leading to a synergistic mechanism of action.
Due to the rarity of LD and TM injuries, literature on the pathology and appropriate treatments for these injuries is limited. The goal of this review is to present the current literature on professional baseball players who have undergone either nonsurgical treatment or surgery for LD and TM strains and/or avulsion injuries. This review will ultimately assist clinicians when deciding on the optimal treatment method for professional baseball players.
Methods
We performed an extensive Medline database search with the following search algorithm: ([latissimus OR latissimus dorsi OR teres major] AND baseball). The search returned 20 citations. Inclusion criteria consisted of clinical studies that focused on professional baseball pitchers with TM and/or LD injuries that underwent either conservative nonsurgical treatment or surgical repair. There was no exclusion based on the type of injury present, such as avulsion vs strain. Any study with amateur athletes or athletes from other sports such as handball or rugby were excluded. Due to the limited amount of data available, the majority of included studies were case reports and case series.
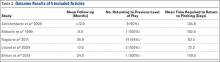
Based on these parameters, 5 articles met criteria for inclusion. Of the 5 included studies, 3 were case reports and 2 were case series. From the eligible articles, the following information was obtained: publication year, sample size, mean age, mean follow-up duration, type of treatment (conservative vs surgical), ability to return to original level of play, time required to return to original form, and complications (Tables 1, 2).
Results
Nonoperative Management
Four of the 5 included studies implemented only conservative therapy for their patients.4,7-9 The average duration these patients were followed for during treatment and rehabilitation was 26.3 months. Malcolm and colleagues7 followed patients for 8 months, the shortest length among the 4 conservative studies in this review. Leland and colleagues8 followed patients for 17 months, and Nagda and colleagues9 had the longest length of observation of 36 months (range 12 to 82 months).Schickendantz and colleagues4 followed patients for >12 months, but the exact duration was not specified. In order to calculate the average duration of observation, each patient was assigned a duration of 12 months.
Of the 30 patients included in this review, 29 were treated conservatively. All of the included studies consisted of male patients. The mean age was 26.8 years (range 22 to 28.1 years). Of the 29 injuries treated conservatively, there were 2 LD tendon avulsions, 4 TM tendon avulsions, 1 LD and TM tendon avulsion, 7 LD intramuscular strains, 9 TM intramuscular strains, and 6 LD and TM intramuscular strains.
Treatment Protocol
The various treatment and rehabilitation programs used for the conservative patient population all followed a similar pathway. After initial injury, a rest period focused on stretching was implemented. Patients were started on steroid or anti-inflammatory medications, cryotherapy, or other therapeutic modalities. Once pain-free and full range of motion was achieved, patients began the strength and throwing components of the rehabilitation program. Reoccurrence of symptoms would halt the throwing component of the rehabilitation program until symptoms improved. Patients were progressed through a return-to-throw program and once they could throw off the mound and achieve their preinjury velocity, strength, and range of motion, they were cleared to return to competitive pitching.
In the senior author’s (MSS) practice, all throwers are managed with the same nonoperative protocol.4 Initial treatment consists of short periods of rest and symptom control via the application of cryotherapy, among other modalities. Restoration of preinjury range of motion is achieved with active-assisted stretching exercises. As range of motion begins approaching pre-injury levels, strength training is initiated with isometric strengthening of the LD and TM progressing to resistance exercises. Exercising the abdominal core, strengthening the lower body, and cardiovascular conditioning are focal points of the rehabilitation period. Once patients regain preinjury shoulder strength and range of motion without pain, they begin a throwing program that consists of 4 weeks of long toss followed by 2 weeks of throwing from the pitching mound. After completion of the throwing program, the patient is allowed to return to competitive pitching. For patients who did not suffer season-ending injury, the average time required to return to play was 99.8 days (range 72.3 to 182.6 days).
Complications and Reinjury
The patients in Leland and colleagues8 and Malcolm and colleagues7 did not suffer any complications or reinjuries. In Schickendantz and colleagues4, all but 3 of the 10 patients were able to return to full speed pitching by 3 months. The other 3 required 4, 6, and 10 months. The patient that required 10 months tore both his LD and TM and the patient that required 6 months tore his TM and was never able to regain his pre-injury throwing velocity. None of the TM tears had a recurrence, while 1 LD tear had a recurrence of injury 6 months after returning to competitive pitching. This patient was successfully treated with 6 weeks of conservative rest and rehabilitation.
In Nagda and colleagues9, 2 athletes suffered injury recurrence. One athlete with a LD strain suffered 2 subsequent LD strains, 4 months and 1 year after initial injury. The other athlete with a LD avulsion suffered a subsequent TM avulsion 13 months after initial injury. One pitcher who had an LD and TM strain suffered a superior labrum anterior and posterior (SLAP) tear and was never able to return to his prior level of play.
Surgical Treatment
Only 1 of the 5 included studies utilized surgical repair for their patient.10 The single patient suffered an avulsion injury of the distal LD tendon and its insertion on the humerus. The LD tendon was retracted approximately 5 cm from the distal humeral insertion. The TM was not involved. Eight days post-injury, the patient underwent surgical repair.11 Postoperatively, the patient started passive range of motion after 2 weeks and active range of motion after 6 weeks. He started throwing at 12 weeks and returned to play at 30 weeks after he had returned to his preinjury form in regards to muscle strength, pitch control, and velocity. The patient was able to resume pitching at a high level in MLB.
Discussion
Overhand throwing athletes, especially professional baseball players, have to constantly deal with a variety of shoulder injuries.12,13 Currently, there is minimal literature on isolated TM and LD injuries. As a result, there is still debate about the optimal treatment method for these injuries, especially in athletes who compete at the highest level. In order to treat isolated injuries of these muscles, it is important to understand their anatomic relationship, as these 2 muscles are intimately associated. The LD originates from the thoracolumbar spine and inserts on the proximal humerus between the pectoralis<hl name="2"/> major and TM tendons. The TM originates from the scapula and, similar to the LD, inserts on the proximal humerus. In an anatomic study, the TM tendon inserted into the LD tendon before its humeral insertion in the majority of cadavers.14,15
The LD is responsible for extension, adduction, and internal rotation of the humerus. The TM, while not as extensively studied, is believed to also contribute to extension, adduction, and internal rotation of the humerus.16 As Jobe and colleagues5 demonstrated, the LD is vital during the acceleration phase of pitching. While they were unable to make any conclusions about the role of the TM during the pitching cycle, it is reasonable to hypothesize that these 2 muscles work together. While it is thought that these 2 muscles work as a unit, it is significant to note that a professional pitcher can sustain an isolated injury to the TM without injury to the LD, and vice versa. This questions whether these 2 muscles work more independently than once thought. One hypothesis is that the physical size of the LD provides protection from injuries that the smaller TM cannot overcome. This is a potential area of further research.
The most common findings in patients with TM injuries include swelling, bruising, tenderness of the proximal arm, and limitations of shoulder range of motion in abduction, flexion, and external rotation. There is also weakness when resistance is applied against internal rotation and extension. Similar to the TM, common findings in patients with LD injuries include pain in the posterior shoulder, bruising, and weakness when resistance is applied against internal rotation of the shoulder. Pitchers are often able to pinpoint the occurrence of their acute pain during a specific time in the game. They commonly experience a pulling sensation and sometimes even feel a “pop” in their shoulder followed by an acute onset of pain and stiffness in the posterior aspect of the axilla. These injuries seem to be associated with the pitcher throwing a “breaking ball,” a pitch that requires greater shoulder rotation since it changes trajectory while traveling towards home plate. Despite the clear role of the LD and hypothesized role of the TM in the pitching sequence, there has been limited research on the optimal treatment of isolated injuries of these muscles in MLB pitchers. The majority of studies in this review opted for conservative treatment for both LD and TM injuries. The only study that presented a surgical option was for a LD avulsion injury.
Athletes undergoing either conservative or surgical treatment required a significant period of recovery and rehabilitation before they were able to compete at the professional level. In Leland and colleagues8, it took about 10 to 12 weeks of rehabilitation for both pitchers to return to pitching against competition. In Schickendantz and colleagues4, barring any complications or injury recurrence, it took patients 12 weeks to return to their preinjury level. In Malcolm and colleagues7, magnetic resonance imaging after 8 weeks showed marked recovery, and shortly after the pitcher was able to return to the pitching rotation. In Nagda and colleagues9, the time lost to injury ranged from 7 weeks to an entire season. Of the 9 pitchers who were lost for the season, 6 had avulsion injuries. The other 3 consisted of an LD strain, TM strain, and LD plus TM strain.9 In this study, it seems that avulsion injuries had a more significant impact on patient recovery. On average, it took 35.6 days after injury for players to begin throwing. In contrast, it took an average of 65.5 days after an avulsion injury for players to begin throwing. Ellman and colleagues10 included the only surgically repaired injury, and it was for an avulsion of the LD tendon. In the surgical case, it took slightly longer for the pitcher to return to preinjury form. It took him 12 to 16 weeks to begin light throwing and his full return to pitching took about 20 to 30 weeks. Since muscle strains and tendon avulsions are significantly different injuries in regards to the type of soft tissue damage and healing potential, they may require different treatment strategies. An avulsion injury may require more aggressive intervention, whereas a strain may only require conservative rehabilitation. Ultimately, there does not seem to be a significant benefit of one treatment option compared to the other. The majority of conservatively managed pitchers were able to return to previous form in a reasonable time frame. While each rehabilitation protocol was slightly different, multiple studies advocated for rehab programs that centered around the following goals: slowly progressing pitchers to light throwing once their pain resolved, followed by long throwing, then throwing off of the mound, and finally returning to competitive pitching. It is important to discuss with patients that rehabilitation generally takes 12 to 16 weeks before they are able to fully return to pitching against competition and that rest should immediately follow any recurrence of pain or stiffness. Once those symptoms resolve, patients may continue the rehabilitation protocol.
As with any form of treatment, there are risks involved. This holds true for both conservative and nonconservative therapy for LD and TM injuries. One risk of nonoperative treatment of an LD avulsion is the development of strength deficits in the muscle.17 While this deficit may go unnoticed in a recreational athlete, it may be more pronounced in a professional athlete, especially since the LD of a professional baseball pitcher is more active on electromyography during the acceleration phase of the pitching cycle compared to a recreational athlete.18 Another risk of conservative treatment of an LD avulsion is jeopardizing the potential for future surgery. As a result, some advocate for early surgical intervention of an acute LD avulsion.19,20 Others, however, recommend conservative management with subsequent surgical intervention if conservative measures fail. One caveat is that surgical intervention to restore the original anatomy may become difficult after a certain period of time due to the buildup of scar tissue. Surgical intervention also has associated risks, such as nerve injury, infection, vascular damage, persistent pain, and the buildup of large amounts of scar tissue. It is important to discuss these risks with patients when deciding on a treatment option.
LD and TM avulsion and tears typically present after an acute event in throwing athletes. There are a number of case reports published that demonstrate successful outcomes with both nonoperative management21 and operative repair of LD injuries in non-throwing athletes such as competitive water skiers,22,23 steer wrestlers,24 professional wrestlers,25 and recreational rock climbers.26 The 5 studies included in this review were the first ones to present LD and TM injuries in MLB pitchers. They discussed the outcomes of mainly conservative and surgical management of LD and TM avulsion and tears. Unfortunately, there remains a limited number of cases on the treatment of these injuries in highly competitive throwing athletes. Further research is required to elucidate the advantages and disadvantages of operative vs nonoperative treatment. The goal of this review is to provide clinicians with a concise summary of the current literature so that they may offer some evidence to their patients when discussing appropriate treatment plans.
1. Conway JE, Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001;32(3):443-456.
2. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
3. Cerynik DL, Ewald TJ, Sastry A, Amin NH, Liao JG, Tom JA. Outcomes of isolated glenoid labral injuries in professional baseball pitchers. Clin J Sport Med. 2008;18(3):255-258
4. Schickendantz MS, Kaar SG, Meister K, Lund P, Beverley L. Latissimus dorsi and teres major tears in professional baseball pitchers: a case series. Am J Sports Med. 2009;37(10):2016-2020.
5. Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12(3):218-220.
6. Glousman R, Jobe F, Tibone J, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70(2):220-226.
7. Malcolm PN, Reinus WR, London SL. Magnetic resonance imaging appearance of teres major tendon injury in a baseball pitcher. Am J Sports Med. 1999;27(1):98-100.
8. Leland JM, Ciccotti MG, Cohen SB, Zoga AC, Frederick RJ. Teres major injuries in two professional baseball pitchers. J Shoulder Elbow Surg. 2009;18(6):e1-e5.
9. Nagda SH, Cohen SB, Noonan TJ, Raasch WG, Ciccotti MG, Yocum LA. Management and outcomes of latissimus dorsi and teres major injuries in professional baseball pitchers. Am J Sports Med. 2011;39(10):2181-2186.
10. Ellman MB, Yanke A, Juhan T, et al. Open repair of an acute latissimus tendon avulsion in a Major League Baseball pitcher. J Shoulder Elbow Surg. 2013;22(7):e19-e23.
11. Ellman MB, Yanke A, Juhan T, et al. Open repair of retracted latissimus dorsi tendon avulsion. Am J Orthop. 2013;42(6):280-285.
12. Altchek DW, Dines DM. Shoulder injuries in the throwing athlete. J Am Acad Orthop Surg. 1995;3(3):159-165.
13. Limpisvasti O, ElAttrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg. 2007;15(3):139-147.
14. Beck PA, Hoffer MM. Latissimus dorsi and teres major tendons: separate or conjoint tendons? J Pediatr Orthop. 1989;9(3):308-309.
15. Morelli M, Nagamori J, Gilbart M, Miniaci A. Latissimus dorsi tendon transfer for massive irreparable cuff tears: an anatomic study. J Shoulder Elbow Surg. 2008;17(1):139-143.
16. Broome HL, Basmajian JV. The function of the teres major muscle: an electromyographic study. Anat Rec. 1971;170(3):309-310.
17. Brumback RJ, McBride MS, Ortolani NC. Functional evaluation of the shoulder after transfer of the vascularized latissimus dorsi muscle. J Bone Joint Surg Am. 1992;74(3):377-382.
18. Gowan ID, Jobe FW, Tibone JE, Perry J, Moynes DR. A comparative electromyographic analysis of the shoulder during pitching. Professional versus amateur pitchers. Am J Sports Med. 1987;15(6):586-590.
19. Park JY, Lhee SH, Keum JS. Rupture of latissimus dorsi muscle in a tennis player. Orthopedics. 2008;31(10).
20. Gregory JM, Harwood DP, Sherman SL, Romeo AA. Surgical repair of a subacute latissimus dorsi tendon rupture. Tech Shoulder Elbow Surg. 2011;12(4):77-79.
21. Butterwick DJ, Mohtadi NG, Meeuwisse WH, Frizzell JB. Rupture of latissimus dorsi in an athlete. Clin J Sport Med. 2003;13(3):189-191.
22. Henry JC, Scerpella TA. Acute traumatic tear of the latissimus dorsi tendon from its insertion. A case report. Am J Sports Med. 2000;28(4):577-579.
23. Lim JK, Tilford ME, Hamersly SF, Sallay PI. Surgical repair of an acute latissimus dorsi tendon avulsion using suture anchors through a single incision. Am J Sports Med. 2006;34(8):1351-1355.
24. Hiemstra LA, Butterwick D, Cooke M, Walker RE. Surgical management of latissimus dorsi rupture in a steer wrestler. Clin J Sport Med. 2007;17(4):316-318.
25. Hapa O, Wijdicks CA, LaPrade RF, Braman JP. Out of the ring and into a sling: acute latissimus dorsi avulsion in a professional wrestler: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1146-1150.
26. Livesey J, Brownson P, Wallace WA. Traumatic latissimus dorsi tendon rupture. J Shoulder Elbow Surg. 2002;11(6):642-644.
Upper extremity injuries are very common in pitchers in amateur and professional baseball. The vast majority involving labral or rotator cuff pathology.1-3 While uncommon, injuries to the latissimus dorsi (LD) (Figure) and teres major (TM) have been reported in Major League Baseball (MLB) pitchers.4 Jobe and colleagues5 demonstrated the role of the LD during the various phases of pitching. The LD is most active during the acceleration phase and remains active during the deceleration phase and follow-through.6 Anatomically, the TM lies posterior to the LD separated by bursal tissue. The tendon fibers converge and unite along their lower borders, leading to a synergistic mechanism of action.
Due to the rarity of LD and TM injuries, literature on the pathology and appropriate treatments for these injuries is limited. The goal of this review is to present the current literature on professional baseball players who have undergone either nonsurgical treatment or surgery for LD and TM strains and/or avulsion injuries. This review will ultimately assist clinicians when deciding on the optimal treatment method for professional baseball players.
Methods
We performed an extensive Medline database search with the following search algorithm: ([latissimus OR latissimus dorsi OR teres major] AND baseball). The search returned 20 citations. Inclusion criteria consisted of clinical studies that focused on professional baseball pitchers with TM and/or LD injuries that underwent either conservative nonsurgical treatment or surgical repair. There was no exclusion based on the type of injury present, such as avulsion vs strain. Any study with amateur athletes or athletes from other sports such as handball or rugby were excluded. Due to the limited amount of data available, the majority of included studies were case reports and case series.
Based on these parameters, 5 articles met criteria for inclusion. Of the 5 included studies, 3 were case reports and 2 were case series. From the eligible articles, the following information was obtained: publication year, sample size, mean age, mean follow-up duration, type of treatment (conservative vs surgical), ability to return to original level of play, time required to return to original form, and complications (Tables 1, 2).
Results
Nonoperative Management
Four of the 5 included studies implemented only conservative therapy for their patients.4,7-9 The average duration these patients were followed for during treatment and rehabilitation was 26.3 months. Malcolm and colleagues7 followed patients for 8 months, the shortest length among the 4 conservative studies in this review. Leland and colleagues8 followed patients for 17 months, and Nagda and colleagues9 had the longest length of observation of 36 months (range 12 to 82 months).Schickendantz and colleagues4 followed patients for >12 months, but the exact duration was not specified. In order to calculate the average duration of observation, each patient was assigned a duration of 12 months.
Of the 30 patients included in this review, 29 were treated conservatively. All of the included studies consisted of male patients. The mean age was 26.8 years (range 22 to 28.1 years). Of the 29 injuries treated conservatively, there were 2 LD tendon avulsions, 4 TM tendon avulsions, 1 LD and TM tendon avulsion, 7 LD intramuscular strains, 9 TM intramuscular strains, and 6 LD and TM intramuscular strains.
Treatment Protocol
The various treatment and rehabilitation programs used for the conservative patient population all followed a similar pathway. After initial injury, a rest period focused on stretching was implemented. Patients were started on steroid or anti-inflammatory medications, cryotherapy, or other therapeutic modalities. Once pain-free and full range of motion was achieved, patients began the strength and throwing components of the rehabilitation program. Reoccurrence of symptoms would halt the throwing component of the rehabilitation program until symptoms improved. Patients were progressed through a return-to-throw program and once they could throw off the mound and achieve their preinjury velocity, strength, and range of motion, they were cleared to return to competitive pitching.
In the senior author’s (MSS) practice, all throwers are managed with the same nonoperative protocol.4 Initial treatment consists of short periods of rest and symptom control via the application of cryotherapy, among other modalities. Restoration of preinjury range of motion is achieved with active-assisted stretching exercises. As range of motion begins approaching pre-injury levels, strength training is initiated with isometric strengthening of the LD and TM progressing to resistance exercises. Exercising the abdominal core, strengthening the lower body, and cardiovascular conditioning are focal points of the rehabilitation period. Once patients regain preinjury shoulder strength and range of motion without pain, they begin a throwing program that consists of 4 weeks of long toss followed by 2 weeks of throwing from the pitching mound. After completion of the throwing program, the patient is allowed to return to competitive pitching. For patients who did not suffer season-ending injury, the average time required to return to play was 99.8 days (range 72.3 to 182.6 days).
Complications and Reinjury
The patients in Leland and colleagues8 and Malcolm and colleagues7 did not suffer any complications or reinjuries. In Schickendantz and colleagues4, all but 3 of the 10 patients were able to return to full speed pitching by 3 months. The other 3 required 4, 6, and 10 months. The patient that required 10 months tore both his LD and TM and the patient that required 6 months tore his TM and was never able to regain his pre-injury throwing velocity. None of the TM tears had a recurrence, while 1 LD tear had a recurrence of injury 6 months after returning to competitive pitching. This patient was successfully treated with 6 weeks of conservative rest and rehabilitation.
In Nagda and colleagues9, 2 athletes suffered injury recurrence. One athlete with a LD strain suffered 2 subsequent LD strains, 4 months and 1 year after initial injury. The other athlete with a LD avulsion suffered a subsequent TM avulsion 13 months after initial injury. One pitcher who had an LD and TM strain suffered a superior labrum anterior and posterior (SLAP) tear and was never able to return to his prior level of play.
Surgical Treatment
Only 1 of the 5 included studies utilized surgical repair for their patient.10 The single patient suffered an avulsion injury of the distal LD tendon and its insertion on the humerus. The LD tendon was retracted approximately 5 cm from the distal humeral insertion. The TM was not involved. Eight days post-injury, the patient underwent surgical repair.11 Postoperatively, the patient started passive range of motion after 2 weeks and active range of motion after 6 weeks. He started throwing at 12 weeks and returned to play at 30 weeks after he had returned to his preinjury form in regards to muscle strength, pitch control, and velocity. The patient was able to resume pitching at a high level in MLB.
Discussion
Overhand throwing athletes, especially professional baseball players, have to constantly deal with a variety of shoulder injuries.12,13 Currently, there is minimal literature on isolated TM and LD injuries. As a result, there is still debate about the optimal treatment method for these injuries, especially in athletes who compete at the highest level. In order to treat isolated injuries of these muscles, it is important to understand their anatomic relationship, as these 2 muscles are intimately associated. The LD originates from the thoracolumbar spine and inserts on the proximal humerus between the pectoralis<hl name="2"/> major and TM tendons. The TM originates from the scapula and, similar to the LD, inserts on the proximal humerus. In an anatomic study, the TM tendon inserted into the LD tendon before its humeral insertion in the majority of cadavers.14,15
The LD is responsible for extension, adduction, and internal rotation of the humerus. The TM, while not as extensively studied, is believed to also contribute to extension, adduction, and internal rotation of the humerus.16 As Jobe and colleagues5 demonstrated, the LD is vital during the acceleration phase of pitching. While they were unable to make any conclusions about the role of the TM during the pitching cycle, it is reasonable to hypothesize that these 2 muscles work together. While it is thought that these 2 muscles work as a unit, it is significant to note that a professional pitcher can sustain an isolated injury to the TM without injury to the LD, and vice versa. This questions whether these 2 muscles work more independently than once thought. One hypothesis is that the physical size of the LD provides protection from injuries that the smaller TM cannot overcome. This is a potential area of further research.
The most common findings in patients with TM injuries include swelling, bruising, tenderness of the proximal arm, and limitations of shoulder range of motion in abduction, flexion, and external rotation. There is also weakness when resistance is applied against internal rotation and extension. Similar to the TM, common findings in patients with LD injuries include pain in the posterior shoulder, bruising, and weakness when resistance is applied against internal rotation of the shoulder. Pitchers are often able to pinpoint the occurrence of their acute pain during a specific time in the game. They commonly experience a pulling sensation and sometimes even feel a “pop” in their shoulder followed by an acute onset of pain and stiffness in the posterior aspect of the axilla. These injuries seem to be associated with the pitcher throwing a “breaking ball,” a pitch that requires greater shoulder rotation since it changes trajectory while traveling towards home plate. Despite the clear role of the LD and hypothesized role of the TM in the pitching sequence, there has been limited research on the optimal treatment of isolated injuries of these muscles in MLB pitchers. The majority of studies in this review opted for conservative treatment for both LD and TM injuries. The only study that presented a surgical option was for a LD avulsion injury.
Athletes undergoing either conservative or surgical treatment required a significant period of recovery and rehabilitation before they were able to compete at the professional level. In Leland and colleagues8, it took about 10 to 12 weeks of rehabilitation for both pitchers to return to pitching against competition. In Schickendantz and colleagues4, barring any complications or injury recurrence, it took patients 12 weeks to return to their preinjury level. In Malcolm and colleagues7, magnetic resonance imaging after 8 weeks showed marked recovery, and shortly after the pitcher was able to return to the pitching rotation. In Nagda and colleagues9, the time lost to injury ranged from 7 weeks to an entire season. Of the 9 pitchers who were lost for the season, 6 had avulsion injuries. The other 3 consisted of an LD strain, TM strain, and LD plus TM strain.9 In this study, it seems that avulsion injuries had a more significant impact on patient recovery. On average, it took 35.6 days after injury for players to begin throwing. In contrast, it took an average of 65.5 days after an avulsion injury for players to begin throwing. Ellman and colleagues10 included the only surgically repaired injury, and it was for an avulsion of the LD tendon. In the surgical case, it took slightly longer for the pitcher to return to preinjury form. It took him 12 to 16 weeks to begin light throwing and his full return to pitching took about 20 to 30 weeks. Since muscle strains and tendon avulsions are significantly different injuries in regards to the type of soft tissue damage and healing potential, they may require different treatment strategies. An avulsion injury may require more aggressive intervention, whereas a strain may only require conservative rehabilitation. Ultimately, there does not seem to be a significant benefit of one treatment option compared to the other. The majority of conservatively managed pitchers were able to return to previous form in a reasonable time frame. While each rehabilitation protocol was slightly different, multiple studies advocated for rehab programs that centered around the following goals: slowly progressing pitchers to light throwing once their pain resolved, followed by long throwing, then throwing off of the mound, and finally returning to competitive pitching. It is important to discuss with patients that rehabilitation generally takes 12 to 16 weeks before they are able to fully return to pitching against competition and that rest should immediately follow any recurrence of pain or stiffness. Once those symptoms resolve, patients may continue the rehabilitation protocol.
As with any form of treatment, there are risks involved. This holds true for both conservative and nonconservative therapy for LD and TM injuries. One risk of nonoperative treatment of an LD avulsion is the development of strength deficits in the muscle.17 While this deficit may go unnoticed in a recreational athlete, it may be more pronounced in a professional athlete, especially since the LD of a professional baseball pitcher is more active on electromyography during the acceleration phase of the pitching cycle compared to a recreational athlete.18 Another risk of conservative treatment of an LD avulsion is jeopardizing the potential for future surgery. As a result, some advocate for early surgical intervention of an acute LD avulsion.19,20 Others, however, recommend conservative management with subsequent surgical intervention if conservative measures fail. One caveat is that surgical intervention to restore the original anatomy may become difficult after a certain period of time due to the buildup of scar tissue. Surgical intervention also has associated risks, such as nerve injury, infection, vascular damage, persistent pain, and the buildup of large amounts of scar tissue. It is important to discuss these risks with patients when deciding on a treatment option.
LD and TM avulsion and tears typically present after an acute event in throwing athletes. There are a number of case reports published that demonstrate successful outcomes with both nonoperative management21 and operative repair of LD injuries in non-throwing athletes such as competitive water skiers,22,23 steer wrestlers,24 professional wrestlers,25 and recreational rock climbers.26 The 5 studies included in this review were the first ones to present LD and TM injuries in MLB pitchers. They discussed the outcomes of mainly conservative and surgical management of LD and TM avulsion and tears. Unfortunately, there remains a limited number of cases on the treatment of these injuries in highly competitive throwing athletes. Further research is required to elucidate the advantages and disadvantages of operative vs nonoperative treatment. The goal of this review is to provide clinicians with a concise summary of the current literature so that they may offer some evidence to their patients when discussing appropriate treatment plans.
Upper extremity injuries are very common in pitchers in amateur and professional baseball. The vast majority involving labral or rotator cuff pathology.1-3 While uncommon, injuries to the latissimus dorsi (LD) (Figure) and teres major (TM) have been reported in Major League Baseball (MLB) pitchers.4 Jobe and colleagues5 demonstrated the role of the LD during the various phases of pitching. The LD is most active during the acceleration phase and remains active during the deceleration phase and follow-through.6 Anatomically, the TM lies posterior to the LD separated by bursal tissue. The tendon fibers converge and unite along their lower borders, leading to a synergistic mechanism of action.
Due to the rarity of LD and TM injuries, literature on the pathology and appropriate treatments for these injuries is limited. The goal of this review is to present the current literature on professional baseball players who have undergone either nonsurgical treatment or surgery for LD and TM strains and/or avulsion injuries. This review will ultimately assist clinicians when deciding on the optimal treatment method for professional baseball players.
Methods
We performed an extensive Medline database search with the following search algorithm: ([latissimus OR latissimus dorsi OR teres major] AND baseball). The search returned 20 citations. Inclusion criteria consisted of clinical studies that focused on professional baseball pitchers with TM and/or LD injuries that underwent either conservative nonsurgical treatment or surgical repair. There was no exclusion based on the type of injury present, such as avulsion vs strain. Any study with amateur athletes or athletes from other sports such as handball or rugby were excluded. Due to the limited amount of data available, the majority of included studies were case reports and case series.
Based on these parameters, 5 articles met criteria for inclusion. Of the 5 included studies, 3 were case reports and 2 were case series. From the eligible articles, the following information was obtained: publication year, sample size, mean age, mean follow-up duration, type of treatment (conservative vs surgical), ability to return to original level of play, time required to return to original form, and complications (Tables 1, 2).
Results
Nonoperative Management
Four of the 5 included studies implemented only conservative therapy for their patients.4,7-9 The average duration these patients were followed for during treatment and rehabilitation was 26.3 months. Malcolm and colleagues7 followed patients for 8 months, the shortest length among the 4 conservative studies in this review. Leland and colleagues8 followed patients for 17 months, and Nagda and colleagues9 had the longest length of observation of 36 months (range 12 to 82 months).Schickendantz and colleagues4 followed patients for >12 months, but the exact duration was not specified. In order to calculate the average duration of observation, each patient was assigned a duration of 12 months.
Of the 30 patients included in this review, 29 were treated conservatively. All of the included studies consisted of male patients. The mean age was 26.8 years (range 22 to 28.1 years). Of the 29 injuries treated conservatively, there were 2 LD tendon avulsions, 4 TM tendon avulsions, 1 LD and TM tendon avulsion, 7 LD intramuscular strains, 9 TM intramuscular strains, and 6 LD and TM intramuscular strains.
Treatment Protocol
The various treatment and rehabilitation programs used for the conservative patient population all followed a similar pathway. After initial injury, a rest period focused on stretching was implemented. Patients were started on steroid or anti-inflammatory medications, cryotherapy, or other therapeutic modalities. Once pain-free and full range of motion was achieved, patients began the strength and throwing components of the rehabilitation program. Reoccurrence of symptoms would halt the throwing component of the rehabilitation program until symptoms improved. Patients were progressed through a return-to-throw program and once they could throw off the mound and achieve their preinjury velocity, strength, and range of motion, they were cleared to return to competitive pitching.
In the senior author’s (MSS) practice, all throwers are managed with the same nonoperative protocol.4 Initial treatment consists of short periods of rest and symptom control via the application of cryotherapy, among other modalities. Restoration of preinjury range of motion is achieved with active-assisted stretching exercises. As range of motion begins approaching pre-injury levels, strength training is initiated with isometric strengthening of the LD and TM progressing to resistance exercises. Exercising the abdominal core, strengthening the lower body, and cardiovascular conditioning are focal points of the rehabilitation period. Once patients regain preinjury shoulder strength and range of motion without pain, they begin a throwing program that consists of 4 weeks of long toss followed by 2 weeks of throwing from the pitching mound. After completion of the throwing program, the patient is allowed to return to competitive pitching. For patients who did not suffer season-ending injury, the average time required to return to play was 99.8 days (range 72.3 to 182.6 days).
Complications and Reinjury
The patients in Leland and colleagues8 and Malcolm and colleagues7 did not suffer any complications or reinjuries. In Schickendantz and colleagues4, all but 3 of the 10 patients were able to return to full speed pitching by 3 months. The other 3 required 4, 6, and 10 months. The patient that required 10 months tore both his LD and TM and the patient that required 6 months tore his TM and was never able to regain his pre-injury throwing velocity. None of the TM tears had a recurrence, while 1 LD tear had a recurrence of injury 6 months after returning to competitive pitching. This patient was successfully treated with 6 weeks of conservative rest and rehabilitation.
In Nagda and colleagues9, 2 athletes suffered injury recurrence. One athlete with a LD strain suffered 2 subsequent LD strains, 4 months and 1 year after initial injury. The other athlete with a LD avulsion suffered a subsequent TM avulsion 13 months after initial injury. One pitcher who had an LD and TM strain suffered a superior labrum anterior and posterior (SLAP) tear and was never able to return to his prior level of play.
Surgical Treatment
Only 1 of the 5 included studies utilized surgical repair for their patient.10 The single patient suffered an avulsion injury of the distal LD tendon and its insertion on the humerus. The LD tendon was retracted approximately 5 cm from the distal humeral insertion. The TM was not involved. Eight days post-injury, the patient underwent surgical repair.11 Postoperatively, the patient started passive range of motion after 2 weeks and active range of motion after 6 weeks. He started throwing at 12 weeks and returned to play at 30 weeks after he had returned to his preinjury form in regards to muscle strength, pitch control, and velocity. The patient was able to resume pitching at a high level in MLB.
Discussion
Overhand throwing athletes, especially professional baseball players, have to constantly deal with a variety of shoulder injuries.12,13 Currently, there is minimal literature on isolated TM and LD injuries. As a result, there is still debate about the optimal treatment method for these injuries, especially in athletes who compete at the highest level. In order to treat isolated injuries of these muscles, it is important to understand their anatomic relationship, as these 2 muscles are intimately associated. The LD originates from the thoracolumbar spine and inserts on the proximal humerus between the pectoralis<hl name="2"/> major and TM tendons. The TM originates from the scapula and, similar to the LD, inserts on the proximal humerus. In an anatomic study, the TM tendon inserted into the LD tendon before its humeral insertion in the majority of cadavers.14,15
The LD is responsible for extension, adduction, and internal rotation of the humerus. The TM, while not as extensively studied, is believed to also contribute to extension, adduction, and internal rotation of the humerus.16 As Jobe and colleagues5 demonstrated, the LD is vital during the acceleration phase of pitching. While they were unable to make any conclusions about the role of the TM during the pitching cycle, it is reasonable to hypothesize that these 2 muscles work together. While it is thought that these 2 muscles work as a unit, it is significant to note that a professional pitcher can sustain an isolated injury to the TM without injury to the LD, and vice versa. This questions whether these 2 muscles work more independently than once thought. One hypothesis is that the physical size of the LD provides protection from injuries that the smaller TM cannot overcome. This is a potential area of further research.
The most common findings in patients with TM injuries include swelling, bruising, tenderness of the proximal arm, and limitations of shoulder range of motion in abduction, flexion, and external rotation. There is also weakness when resistance is applied against internal rotation and extension. Similar to the TM, common findings in patients with LD injuries include pain in the posterior shoulder, bruising, and weakness when resistance is applied against internal rotation of the shoulder. Pitchers are often able to pinpoint the occurrence of their acute pain during a specific time in the game. They commonly experience a pulling sensation and sometimes even feel a “pop” in their shoulder followed by an acute onset of pain and stiffness in the posterior aspect of the axilla. These injuries seem to be associated with the pitcher throwing a “breaking ball,” a pitch that requires greater shoulder rotation since it changes trajectory while traveling towards home plate. Despite the clear role of the LD and hypothesized role of the TM in the pitching sequence, there has been limited research on the optimal treatment of isolated injuries of these muscles in MLB pitchers. The majority of studies in this review opted for conservative treatment for both LD and TM injuries. The only study that presented a surgical option was for a LD avulsion injury.
Athletes undergoing either conservative or surgical treatment required a significant period of recovery and rehabilitation before they were able to compete at the professional level. In Leland and colleagues8, it took about 10 to 12 weeks of rehabilitation for both pitchers to return to pitching against competition. In Schickendantz and colleagues4, barring any complications or injury recurrence, it took patients 12 weeks to return to their preinjury level. In Malcolm and colleagues7, magnetic resonance imaging after 8 weeks showed marked recovery, and shortly after the pitcher was able to return to the pitching rotation. In Nagda and colleagues9, the time lost to injury ranged from 7 weeks to an entire season. Of the 9 pitchers who were lost for the season, 6 had avulsion injuries. The other 3 consisted of an LD strain, TM strain, and LD plus TM strain.9 In this study, it seems that avulsion injuries had a more significant impact on patient recovery. On average, it took 35.6 days after injury for players to begin throwing. In contrast, it took an average of 65.5 days after an avulsion injury for players to begin throwing. Ellman and colleagues10 included the only surgically repaired injury, and it was for an avulsion of the LD tendon. In the surgical case, it took slightly longer for the pitcher to return to preinjury form. It took him 12 to 16 weeks to begin light throwing and his full return to pitching took about 20 to 30 weeks. Since muscle strains and tendon avulsions are significantly different injuries in regards to the type of soft tissue damage and healing potential, they may require different treatment strategies. An avulsion injury may require more aggressive intervention, whereas a strain may only require conservative rehabilitation. Ultimately, there does not seem to be a significant benefit of one treatment option compared to the other. The majority of conservatively managed pitchers were able to return to previous form in a reasonable time frame. While each rehabilitation protocol was slightly different, multiple studies advocated for rehab programs that centered around the following goals: slowly progressing pitchers to light throwing once their pain resolved, followed by long throwing, then throwing off of the mound, and finally returning to competitive pitching. It is important to discuss with patients that rehabilitation generally takes 12 to 16 weeks before they are able to fully return to pitching against competition and that rest should immediately follow any recurrence of pain or stiffness. Once those symptoms resolve, patients may continue the rehabilitation protocol.
As with any form of treatment, there are risks involved. This holds true for both conservative and nonconservative therapy for LD and TM injuries. One risk of nonoperative treatment of an LD avulsion is the development of strength deficits in the muscle.17 While this deficit may go unnoticed in a recreational athlete, it may be more pronounced in a professional athlete, especially since the LD of a professional baseball pitcher is more active on electromyography during the acceleration phase of the pitching cycle compared to a recreational athlete.18 Another risk of conservative treatment of an LD avulsion is jeopardizing the potential for future surgery. As a result, some advocate for early surgical intervention of an acute LD avulsion.19,20 Others, however, recommend conservative management with subsequent surgical intervention if conservative measures fail. One caveat is that surgical intervention to restore the original anatomy may become difficult after a certain period of time due to the buildup of scar tissue. Surgical intervention also has associated risks, such as nerve injury, infection, vascular damage, persistent pain, and the buildup of large amounts of scar tissue. It is important to discuss these risks with patients when deciding on a treatment option.
LD and TM avulsion and tears typically present after an acute event in throwing athletes. There are a number of case reports published that demonstrate successful outcomes with both nonoperative management21 and operative repair of LD injuries in non-throwing athletes such as competitive water skiers,22,23 steer wrestlers,24 professional wrestlers,25 and recreational rock climbers.26 The 5 studies included in this review were the first ones to present LD and TM injuries in MLB pitchers. They discussed the outcomes of mainly conservative and surgical management of LD and TM avulsion and tears. Unfortunately, there remains a limited number of cases on the treatment of these injuries in highly competitive throwing athletes. Further research is required to elucidate the advantages and disadvantages of operative vs nonoperative treatment. The goal of this review is to provide clinicians with a concise summary of the current literature so that they may offer some evidence to their patients when discussing appropriate treatment plans.
1. Conway JE, Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001;32(3):443-456.
2. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
3. Cerynik DL, Ewald TJ, Sastry A, Amin NH, Liao JG, Tom JA. Outcomes of isolated glenoid labral injuries in professional baseball pitchers. Clin J Sport Med. 2008;18(3):255-258
4. Schickendantz MS, Kaar SG, Meister K, Lund P, Beverley L. Latissimus dorsi and teres major tears in professional baseball pitchers: a case series. Am J Sports Med. 2009;37(10):2016-2020.
5. Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12(3):218-220.
6. Glousman R, Jobe F, Tibone J, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70(2):220-226.
7. Malcolm PN, Reinus WR, London SL. Magnetic resonance imaging appearance of teres major tendon injury in a baseball pitcher. Am J Sports Med. 1999;27(1):98-100.
8. Leland JM, Ciccotti MG, Cohen SB, Zoga AC, Frederick RJ. Teres major injuries in two professional baseball pitchers. J Shoulder Elbow Surg. 2009;18(6):e1-e5.
9. Nagda SH, Cohen SB, Noonan TJ, Raasch WG, Ciccotti MG, Yocum LA. Management and outcomes of latissimus dorsi and teres major injuries in professional baseball pitchers. Am J Sports Med. 2011;39(10):2181-2186.
10. Ellman MB, Yanke A, Juhan T, et al. Open repair of an acute latissimus tendon avulsion in a Major League Baseball pitcher. J Shoulder Elbow Surg. 2013;22(7):e19-e23.
11. Ellman MB, Yanke A, Juhan T, et al. Open repair of retracted latissimus dorsi tendon avulsion. Am J Orthop. 2013;42(6):280-285.
12. Altchek DW, Dines DM. Shoulder injuries in the throwing athlete. J Am Acad Orthop Surg. 1995;3(3):159-165.
13. Limpisvasti O, ElAttrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg. 2007;15(3):139-147.
14. Beck PA, Hoffer MM. Latissimus dorsi and teres major tendons: separate or conjoint tendons? J Pediatr Orthop. 1989;9(3):308-309.
15. Morelli M, Nagamori J, Gilbart M, Miniaci A. Latissimus dorsi tendon transfer for massive irreparable cuff tears: an anatomic study. J Shoulder Elbow Surg. 2008;17(1):139-143.
16. Broome HL, Basmajian JV. The function of the teres major muscle: an electromyographic study. Anat Rec. 1971;170(3):309-310.
17. Brumback RJ, McBride MS, Ortolani NC. Functional evaluation of the shoulder after transfer of the vascularized latissimus dorsi muscle. J Bone Joint Surg Am. 1992;74(3):377-382.
18. Gowan ID, Jobe FW, Tibone JE, Perry J, Moynes DR. A comparative electromyographic analysis of the shoulder during pitching. Professional versus amateur pitchers. Am J Sports Med. 1987;15(6):586-590.
19. Park JY, Lhee SH, Keum JS. Rupture of latissimus dorsi muscle in a tennis player. Orthopedics. 2008;31(10).
20. Gregory JM, Harwood DP, Sherman SL, Romeo AA. Surgical repair of a subacute latissimus dorsi tendon rupture. Tech Shoulder Elbow Surg. 2011;12(4):77-79.
21. Butterwick DJ, Mohtadi NG, Meeuwisse WH, Frizzell JB. Rupture of latissimus dorsi in an athlete. Clin J Sport Med. 2003;13(3):189-191.
22. Henry JC, Scerpella TA. Acute traumatic tear of the latissimus dorsi tendon from its insertion. A case report. Am J Sports Med. 2000;28(4):577-579.
23. Lim JK, Tilford ME, Hamersly SF, Sallay PI. Surgical repair of an acute latissimus dorsi tendon avulsion using suture anchors through a single incision. Am J Sports Med. 2006;34(8):1351-1355.
24. Hiemstra LA, Butterwick D, Cooke M, Walker RE. Surgical management of latissimus dorsi rupture in a steer wrestler. Clin J Sport Med. 2007;17(4):316-318.
25. Hapa O, Wijdicks CA, LaPrade RF, Braman JP. Out of the ring and into a sling: acute latissimus dorsi avulsion in a professional wrestler: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1146-1150.
26. Livesey J, Brownson P, Wallace WA. Traumatic latissimus dorsi tendon rupture. J Shoulder Elbow Surg. 2002;11(6):642-644.
1. Conway JE, Arthroscopic repair of partial-thickness rotator cuff tears and SLAP lesions in professional baseball players. Orthop Clin North Am. 2001;32(3):443-456.
2. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
3. Cerynik DL, Ewald TJ, Sastry A, Amin NH, Liao JG, Tom JA. Outcomes of isolated glenoid labral injuries in professional baseball pitchers. Clin J Sport Med. 2008;18(3):255-258
4. Schickendantz MS, Kaar SG, Meister K, Lund P, Beverley L. Latissimus dorsi and teres major tears in professional baseball pitchers: a case series. Am J Sports Med. 2009;37(10):2016-2020.
5. Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching. A second report. Am J Sports Med. 1984;12(3):218-220.
6. Glousman R, Jobe F, Tibone J, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70(2):220-226.
7. Malcolm PN, Reinus WR, London SL. Magnetic resonance imaging appearance of teres major tendon injury in a baseball pitcher. Am J Sports Med. 1999;27(1):98-100.
8. Leland JM, Ciccotti MG, Cohen SB, Zoga AC, Frederick RJ. Teres major injuries in two professional baseball pitchers. J Shoulder Elbow Surg. 2009;18(6):e1-e5.
9. Nagda SH, Cohen SB, Noonan TJ, Raasch WG, Ciccotti MG, Yocum LA. Management and outcomes of latissimus dorsi and teres major injuries in professional baseball pitchers. Am J Sports Med. 2011;39(10):2181-2186.
10. Ellman MB, Yanke A, Juhan T, et al. Open repair of an acute latissimus tendon avulsion in a Major League Baseball pitcher. J Shoulder Elbow Surg. 2013;22(7):e19-e23.
11. Ellman MB, Yanke A, Juhan T, et al. Open repair of retracted latissimus dorsi tendon avulsion. Am J Orthop. 2013;42(6):280-285.
12. Altchek DW, Dines DM. Shoulder injuries in the throwing athlete. J Am Acad Orthop Surg. 1995;3(3):159-165.
13. Limpisvasti O, ElAttrache NS, Jobe FW. Understanding shoulder and elbow injuries in baseball. J Am Acad Orthop Surg. 2007;15(3):139-147.
14. Beck PA, Hoffer MM. Latissimus dorsi and teres major tendons: separate or conjoint tendons? J Pediatr Orthop. 1989;9(3):308-309.
15. Morelli M, Nagamori J, Gilbart M, Miniaci A. Latissimus dorsi tendon transfer for massive irreparable cuff tears: an anatomic study. J Shoulder Elbow Surg. 2008;17(1):139-143.
16. Broome HL, Basmajian JV. The function of the teres major muscle: an electromyographic study. Anat Rec. 1971;170(3):309-310.
17. Brumback RJ, McBride MS, Ortolani NC. Functional evaluation of the shoulder after transfer of the vascularized latissimus dorsi muscle. J Bone Joint Surg Am. 1992;74(3):377-382.
18. Gowan ID, Jobe FW, Tibone JE, Perry J, Moynes DR. A comparative electromyographic analysis of the shoulder during pitching. Professional versus amateur pitchers. Am J Sports Med. 1987;15(6):586-590.
19. Park JY, Lhee SH, Keum JS. Rupture of latissimus dorsi muscle in a tennis player. Orthopedics. 2008;31(10).
20. Gregory JM, Harwood DP, Sherman SL, Romeo AA. Surgical repair of a subacute latissimus dorsi tendon rupture. Tech Shoulder Elbow Surg. 2011;12(4):77-79.
21. Butterwick DJ, Mohtadi NG, Meeuwisse WH, Frizzell JB. Rupture of latissimus dorsi in an athlete. Clin J Sport Med. 2003;13(3):189-191.
22. Henry JC, Scerpella TA. Acute traumatic tear of the latissimus dorsi tendon from its insertion. A case report. Am J Sports Med. 2000;28(4):577-579.
23. Lim JK, Tilford ME, Hamersly SF, Sallay PI. Surgical repair of an acute latissimus dorsi tendon avulsion using suture anchors through a single incision. Am J Sports Med. 2006;34(8):1351-1355.
24. Hiemstra LA, Butterwick D, Cooke M, Walker RE. Surgical management of latissimus dorsi rupture in a steer wrestler. Clin J Sport Med. 2007;17(4):316-318.
25. Hapa O, Wijdicks CA, LaPrade RF, Braman JP. Out of the ring and into a sling: acute latissimus dorsi avulsion in a professional wrestler: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1146-1150.
26. Livesey J, Brownson P, Wallace WA. Traumatic latissimus dorsi tendon rupture. J Shoulder Elbow Surg. 2002;11(6):642-644.