User login
Implementation of an Automated Phone Call Distribution System in an Inpatient Pharmacy Setting
Pharmacy call centers have been successfully implemented in outpatient and specialty pharmacy settings.1 A centralized pharmacy call center gives patients immediate access to a pharmacist who can view their health records to answer specific questions or fulfill medication renewal requests.2-4 Little literature exists to describe its use in an inpatient setting.
Inpatient pharmacies receive numerous calls from health care professionals and patients. Challenges related to phone calls in the inpatient pharmacy setting may include interruptions, distractions, low accountability, poor efficiency, lack of optimal resources, and staffing.5 An unequal distribution and lack of accountability may exist when answering phone calls for the inpatient pharmacy team, which may contribute to long hold times and call abandonment rates. Phone calls also may be directed inefficiently between clinical pharmacists (CPs) and pharmacy technicians. Team member time related to answering phone calls may not be captured or measured.
The Edward Hines, Jr. Veterans Affairs Hospital (EHJVAH) in Illinois offers primary, extended, and specialty care and is a tertiary care referral center. The facility operates 483 beds and serves 6 community-based outpatient clinics.
Implementation
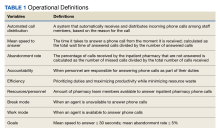
A new inpatient pharmacy service phone line extension was implemented. Data used to report quality metrics were obtained from the Global Navigator (GNAV), an information system that records calls, tracks the performance of agents, and coordinates personnel scheduling. The effectiveness of the ACD system was evaluated by quality metric goals of mean speed to answer ≤ 30 seconds and mean abandonment rate ≤ 5%. This project was determined to be quality improvement and was not reviewed by the EHJVAH Institutional Review Board.
The ACD system was set up in December 2020. After a 1-month implementation period, metrics were reported to the inpatient pharmacy team and leadership. By January 2021, EHJVAH fully implemented an ACD phone system operated by inpatient pharmacy technicians and CPs. EHJVAH inpatient pharmacy includes CPs who practice without a scope of practice and board-certified pharmacy technicians in 3 shifts. The CPs and pharmacy technicians work in the central pharmacy (the main pharmacy and inpatient pharmacy vault) or are decentralized with responsibility for answering phone calls and making deliveries (pharmacy technicians).
The pharmacy leadership team decided to implement 1 phone line with 2 ACD splits. The first split was directed to pharmacy technicians and the second to CPs. The intention was to streamline calls to be directed to proper team members within the inpatient pharmacy. The CP line also was designed to back up the pharmacy technician line. These calls were equally distributed among staff based on a standard algorithm. The pharmacy greeting stated, “Thank you for contacting the inpatient pharmacy at Hines VA Hospital. For missing doses, unit stock requests, or to speak with a pharmacy technician, please press 1. For clinical questions, order verification, or to speak with a pharmacist, please press 2.” Each inpatient pharmacy team member had a unique system login.
Fourteen ACD phone stations were established in the main pharmacy and in decentralized locations for order verification. The stations were distributed across the pharmacy service to optimize workload, space, and resources.
Training and Communication
Before implementing the inpatient pharmacy ACD phone system, the CPs and pharmacy technicians received mandatory ACD training. After the training, pharmacy team members were required to sign off on the training document to indicate that they had completed the course. The pharmacy team was trained on the importance of staffing the phones continuously. As a 24-hour pharmacy service in the acute care setting, any call may be critical for patient care.
A hospital-wide memorandum was distributed via email to all unit managers and hospital staff to educate them on the new ACD phone system, which included a new phone line extension for the inpatient pharmacy. Additionally, the inpatient pharmacy team was trained on the proper way of communicating the ACD phone system process with the hospital staff. The inpatient pharmacy team was notified that there would be an educational period to explain the queue process to hospital staff. Occasionally, hospital staff believed they were speaking to an automated system and hung up before their call was answered. The inpatient pharmacy team was instructed to notify the hospital staff to stay on the line since their call would be answered in the order it was received. Once the inpatient pharmacy team received proper training and felt comfortable with the phone system, it was set up and integrated into the workflow.
Postimplementation Evaluation
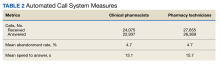
Inpatient pharmacy ACD phone system data were collected for 2021. To evaluate the effectiveness of an ACD system, the pharmacy leadership team set up the following metrics and goals for inpatient CPs and inpatient pharmacy technicians for monthly call volume/abandonment rate, mean speed to answer, mean call volume by shift, and the mean abandonment rate by shift.
Inpatient pharmacy technicians answered 27,655 calls with a mean call abandonment rate of 4.7%. and a mean 15.6 seconds to answer.
Discussion
Since implementing the inpatient pharmacy ACD phone system in January 2021, there have been successes and challenges. The implementation increased accountability and efficiency when answering pharmacy phone calls. An ACD uses an algorithm that ensures equitable distribution of phone calls between CPs and pharmacy technicians. Through this algorithm, the pharmacy team is held more accountable when answering incoming calls. Distributing phone calls equally allows for optimization and balances the workload. The ACD phone system also improved efficiency when answering incoming calls. By incorporating splits when a patient or health care professional calls, ACD routes the question to the appropriate staff member. As a result, CPs spend less time answering questions meant for pharmacy technicians and instead can answer clinical or order verification questions more efficiently.
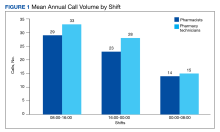
ACD data also allow pharmacy leadership to assess staffing needs, depending on the call volume. Based on ACD data, the busiest time of day was 8:00 AM to 4:00 PM. Based on this information, pharmacy leadership plans to staff more appropriately to have more pharmacy technicians working during the first shift to attend to phone calls.
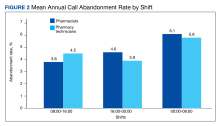
The mean call abandonment rate was 4.7% for both CPs and pharmacy technicians, which met the ≤ 5% goal. The highest call abandonment rate was from midnight to 8
Pharmacy technicians handled a higher total call volume, which may be attributed to more phone calls related to missing doses or unit stock requests compared with clinical questions or order verifications. This information may be beneficial to identify opportunities to improve pharmacy operations.
The main challenges encountered in the ACD implementation process were hardware installation and communication with hospital staff about the changes in the inpatient pharmacy phone system. To implement the new inpatient pharmacy ACD phone system, previous telephones and hardware were removed and replaced. Initially, hardware and installation delays made it difficult for the ACD phone system to operate efficiently in the early months of its implementation. The inpatient pharmacy team depends on the telecommunications system and computers for their daily activities. Delays and issues with the hardware and ACD phone system made it more difficult to provide patient care.
Communication is a continuous challenge to ensure that hospital staff are notified of the new inpatient pharmacy ACD phone number. Over time, the understanding and use of the new ACD phone system have increased dramatically, but there are still opportunities to capture any misdirected calls. Informal feedback was obtained at pharmacy huddles and 1-on-1 discussions with pharmacy staff, and the opinions were mixed. Members of the pharmacy staff expressed that the ACD phone system set up an effective way to triage phone calls. Another positive comment was that the system created a means of accountability for pharmacy phone calls. Critical feedback included challenges with triaging phone calls to appropriate pharmacists, because calls are assigned based on an algorithm, whereas clinical coverage is determined by designated unit daily assignments.
Limitations
There are potential limitations to this quality improvement project. This phone system may not apply to all inpatient hospital pharmacy settings. Potential limitations for implementation at other institutions may include but are not limited to, differing pharmacy practice models (centralized vs decentralized), implementation costs, and internal resources.
Future Goals
To improve the quality of service provided to patients and other hospital staff, the pharmacy leadership team can use the data to ensure that inpatient pharmacy technician resources are being used effectively during times of day with the greatest number of incoming ACD calls. The ACD phone system helps determine whether current resources are being used most efficiently and if they are not, can help identify areas of improvement.
The pharmacy leadership team plans on using reports for pharmacy team members to monitor performance. Reports on individual agent activity capture workload; this may be used as a performance-related metric for future performance plans.
Conclusions
The inpatient pharmacy ACD phone system at EHJVAH is a promising application of available technology. The implementation of the ACD system improved accountability, efficiency, work distribution, and the allocation of resources in the inpatient pharmacy service. The ACD phone system has yielded positive performance metrics including mean speed to answer ≤ 30 seconds and abandonment rate ≤ 5% over 12 months after implementation. With time, users of the inpatient pharmacy ACD phone system will become more comfortable with the technology, thus further improving the patient health care quality.
1. Rim MH, Thomas KC, Chandramouli J, Barrus SA, Nickman NA. Implementation and quality assessment of a pharmacy services call center for outpatient pharmacies and specialty pharmacy services in an academic health system. Am J Health Syst Pharm. 2018;75(10):633-641. doi:10.2146/ajhp170319
2. Patterson BJ, Doucette WR, Urmie JM, McDonough RP. Exploring relationships among pharmacy service use, patronage motives, and patient satisfaction. J Am Pharm Assoc (2003). 2013;53(4):382-389. doi:10.1331/JAPhA.2013.12100
3. Walker DM, Sieck CJ, Menser T, Huerta TR, Scheck McAlearney A. Information technology to support patient engagement: where do we stand and where can we go?. J Am Med Inform Assoc. 2017;24(6):1088-1094. doi:10.1093/jamia/ocx043
4. Menichetti J, Libreri C, Lozza E, Graffigna G. Giving patients a starring role in their own care: a bibliometric analysis of the on-going literature debate. Health Expect. 2016;19(3):516-526. doi:10.1111/hex.12299
5. Raimbault M, Guérin A, Caron É, Lebel D, Bussières J-F. Identifying and reducing distractions and interruptions in a pharmacy department. Am J Health Syst Pharm. 2013;70(3):186-190. doi:10.2146/ajhp120344
Pharmacy call centers have been successfully implemented in outpatient and specialty pharmacy settings.1 A centralized pharmacy call center gives patients immediate access to a pharmacist who can view their health records to answer specific questions or fulfill medication renewal requests.2-4 Little literature exists to describe its use in an inpatient setting.
Inpatient pharmacies receive numerous calls from health care professionals and patients. Challenges related to phone calls in the inpatient pharmacy setting may include interruptions, distractions, low accountability, poor efficiency, lack of optimal resources, and staffing.5 An unequal distribution and lack of accountability may exist when answering phone calls for the inpatient pharmacy team, which may contribute to long hold times and call abandonment rates. Phone calls also may be directed inefficiently between clinical pharmacists (CPs) and pharmacy technicians. Team member time related to answering phone calls may not be captured or measured.
The Edward Hines, Jr. Veterans Affairs Hospital (EHJVAH) in Illinois offers primary, extended, and specialty care and is a tertiary care referral center. The facility operates 483 beds and serves 6 community-based outpatient clinics.
Implementation
A new inpatient pharmacy service phone line extension was implemented. Data used to report quality metrics were obtained from the Global Navigator (GNAV), an information system that records calls, tracks the performance of agents, and coordinates personnel scheduling. The effectiveness of the ACD system was evaluated by quality metric goals of mean speed to answer ≤ 30 seconds and mean abandonment rate ≤ 5%. This project was determined to be quality improvement and was not reviewed by the EHJVAH Institutional Review Board.
The ACD system was set up in December 2020. After a 1-month implementation period, metrics were reported to the inpatient pharmacy team and leadership. By January 2021, EHJVAH fully implemented an ACD phone system operated by inpatient pharmacy technicians and CPs. EHJVAH inpatient pharmacy includes CPs who practice without a scope of practice and board-certified pharmacy technicians in 3 shifts. The CPs and pharmacy technicians work in the central pharmacy (the main pharmacy and inpatient pharmacy vault) or are decentralized with responsibility for answering phone calls and making deliveries (pharmacy technicians).
The pharmacy leadership team decided to implement 1 phone line with 2 ACD splits. The first split was directed to pharmacy technicians and the second to CPs. The intention was to streamline calls to be directed to proper team members within the inpatient pharmacy. The CP line also was designed to back up the pharmacy technician line. These calls were equally distributed among staff based on a standard algorithm. The pharmacy greeting stated, “Thank you for contacting the inpatient pharmacy at Hines VA Hospital. For missing doses, unit stock requests, or to speak with a pharmacy technician, please press 1. For clinical questions, order verification, or to speak with a pharmacist, please press 2.” Each inpatient pharmacy team member had a unique system login.
Fourteen ACD phone stations were established in the main pharmacy and in decentralized locations for order verification. The stations were distributed across the pharmacy service to optimize workload, space, and resources.
Training and Communication
Before implementing the inpatient pharmacy ACD phone system, the CPs and pharmacy technicians received mandatory ACD training. After the training, pharmacy team members were required to sign off on the training document to indicate that they had completed the course. The pharmacy team was trained on the importance of staffing the phones continuously. As a 24-hour pharmacy service in the acute care setting, any call may be critical for patient care.
A hospital-wide memorandum was distributed via email to all unit managers and hospital staff to educate them on the new ACD phone system, which included a new phone line extension for the inpatient pharmacy. Additionally, the inpatient pharmacy team was trained on the proper way of communicating the ACD phone system process with the hospital staff. The inpatient pharmacy team was notified that there would be an educational period to explain the queue process to hospital staff. Occasionally, hospital staff believed they were speaking to an automated system and hung up before their call was answered. The inpatient pharmacy team was instructed to notify the hospital staff to stay on the line since their call would be answered in the order it was received. Once the inpatient pharmacy team received proper training and felt comfortable with the phone system, it was set up and integrated into the workflow.
Postimplementation Evaluation
Inpatient pharmacy ACD phone system data were collected for 2021. To evaluate the effectiveness of an ACD system, the pharmacy leadership team set up the following metrics and goals for inpatient CPs and inpatient pharmacy technicians for monthly call volume/abandonment rate, mean speed to answer, mean call volume by shift, and the mean abandonment rate by shift.
Inpatient pharmacy technicians answered 27,655 calls with a mean call abandonment rate of 4.7%. and a mean 15.6 seconds to answer.
Discussion
Since implementing the inpatient pharmacy ACD phone system in January 2021, there have been successes and challenges. The implementation increased accountability and efficiency when answering pharmacy phone calls. An ACD uses an algorithm that ensures equitable distribution of phone calls between CPs and pharmacy technicians. Through this algorithm, the pharmacy team is held more accountable when answering incoming calls. Distributing phone calls equally allows for optimization and balances the workload. The ACD phone system also improved efficiency when answering incoming calls. By incorporating splits when a patient or health care professional calls, ACD routes the question to the appropriate staff member. As a result, CPs spend less time answering questions meant for pharmacy technicians and instead can answer clinical or order verification questions more efficiently.
ACD data also allow pharmacy leadership to assess staffing needs, depending on the call volume. Based on ACD data, the busiest time of day was 8:00 AM to 4:00 PM. Based on this information, pharmacy leadership plans to staff more appropriately to have more pharmacy technicians working during the first shift to attend to phone calls.
The mean call abandonment rate was 4.7% for both CPs and pharmacy technicians, which met the ≤ 5% goal. The highest call abandonment rate was from midnight to 8
Pharmacy technicians handled a higher total call volume, which may be attributed to more phone calls related to missing doses or unit stock requests compared with clinical questions or order verifications. This information may be beneficial to identify opportunities to improve pharmacy operations.
The main challenges encountered in the ACD implementation process were hardware installation and communication with hospital staff about the changes in the inpatient pharmacy phone system. To implement the new inpatient pharmacy ACD phone system, previous telephones and hardware were removed and replaced. Initially, hardware and installation delays made it difficult for the ACD phone system to operate efficiently in the early months of its implementation. The inpatient pharmacy team depends on the telecommunications system and computers for their daily activities. Delays and issues with the hardware and ACD phone system made it more difficult to provide patient care.
Communication is a continuous challenge to ensure that hospital staff are notified of the new inpatient pharmacy ACD phone number. Over time, the understanding and use of the new ACD phone system have increased dramatically, but there are still opportunities to capture any misdirected calls. Informal feedback was obtained at pharmacy huddles and 1-on-1 discussions with pharmacy staff, and the opinions were mixed. Members of the pharmacy staff expressed that the ACD phone system set up an effective way to triage phone calls. Another positive comment was that the system created a means of accountability for pharmacy phone calls. Critical feedback included challenges with triaging phone calls to appropriate pharmacists, because calls are assigned based on an algorithm, whereas clinical coverage is determined by designated unit daily assignments.
Limitations
There are potential limitations to this quality improvement project. This phone system may not apply to all inpatient hospital pharmacy settings. Potential limitations for implementation at other institutions may include but are not limited to, differing pharmacy practice models (centralized vs decentralized), implementation costs, and internal resources.
Future Goals
To improve the quality of service provided to patients and other hospital staff, the pharmacy leadership team can use the data to ensure that inpatient pharmacy technician resources are being used effectively during times of day with the greatest number of incoming ACD calls. The ACD phone system helps determine whether current resources are being used most efficiently and if they are not, can help identify areas of improvement.
The pharmacy leadership team plans on using reports for pharmacy team members to monitor performance. Reports on individual agent activity capture workload; this may be used as a performance-related metric for future performance plans.
Conclusions
The inpatient pharmacy ACD phone system at EHJVAH is a promising application of available technology. The implementation of the ACD system improved accountability, efficiency, work distribution, and the allocation of resources in the inpatient pharmacy service. The ACD phone system has yielded positive performance metrics including mean speed to answer ≤ 30 seconds and abandonment rate ≤ 5% over 12 months after implementation. With time, users of the inpatient pharmacy ACD phone system will become more comfortable with the technology, thus further improving the patient health care quality.
Pharmacy call centers have been successfully implemented in outpatient and specialty pharmacy settings.1 A centralized pharmacy call center gives patients immediate access to a pharmacist who can view their health records to answer specific questions or fulfill medication renewal requests.2-4 Little literature exists to describe its use in an inpatient setting.
Inpatient pharmacies receive numerous calls from health care professionals and patients. Challenges related to phone calls in the inpatient pharmacy setting may include interruptions, distractions, low accountability, poor efficiency, lack of optimal resources, and staffing.5 An unequal distribution and lack of accountability may exist when answering phone calls for the inpatient pharmacy team, which may contribute to long hold times and call abandonment rates. Phone calls also may be directed inefficiently between clinical pharmacists (CPs) and pharmacy technicians. Team member time related to answering phone calls may not be captured or measured.
The Edward Hines, Jr. Veterans Affairs Hospital (EHJVAH) in Illinois offers primary, extended, and specialty care and is a tertiary care referral center. The facility operates 483 beds and serves 6 community-based outpatient clinics.
Implementation
A new inpatient pharmacy service phone line extension was implemented. Data used to report quality metrics were obtained from the Global Navigator (GNAV), an information system that records calls, tracks the performance of agents, and coordinates personnel scheduling. The effectiveness of the ACD system was evaluated by quality metric goals of mean speed to answer ≤ 30 seconds and mean abandonment rate ≤ 5%. This project was determined to be quality improvement and was not reviewed by the EHJVAH Institutional Review Board.
The ACD system was set up in December 2020. After a 1-month implementation period, metrics were reported to the inpatient pharmacy team and leadership. By January 2021, EHJVAH fully implemented an ACD phone system operated by inpatient pharmacy technicians and CPs. EHJVAH inpatient pharmacy includes CPs who practice without a scope of practice and board-certified pharmacy technicians in 3 shifts. The CPs and pharmacy technicians work in the central pharmacy (the main pharmacy and inpatient pharmacy vault) or are decentralized with responsibility for answering phone calls and making deliveries (pharmacy technicians).
The pharmacy leadership team decided to implement 1 phone line with 2 ACD splits. The first split was directed to pharmacy technicians and the second to CPs. The intention was to streamline calls to be directed to proper team members within the inpatient pharmacy. The CP line also was designed to back up the pharmacy technician line. These calls were equally distributed among staff based on a standard algorithm. The pharmacy greeting stated, “Thank you for contacting the inpatient pharmacy at Hines VA Hospital. For missing doses, unit stock requests, or to speak with a pharmacy technician, please press 1. For clinical questions, order verification, or to speak with a pharmacist, please press 2.” Each inpatient pharmacy team member had a unique system login.
Fourteen ACD phone stations were established in the main pharmacy and in decentralized locations for order verification. The stations were distributed across the pharmacy service to optimize workload, space, and resources.
Training and Communication
Before implementing the inpatient pharmacy ACD phone system, the CPs and pharmacy technicians received mandatory ACD training. After the training, pharmacy team members were required to sign off on the training document to indicate that they had completed the course. The pharmacy team was trained on the importance of staffing the phones continuously. As a 24-hour pharmacy service in the acute care setting, any call may be critical for patient care.
A hospital-wide memorandum was distributed via email to all unit managers and hospital staff to educate them on the new ACD phone system, which included a new phone line extension for the inpatient pharmacy. Additionally, the inpatient pharmacy team was trained on the proper way of communicating the ACD phone system process with the hospital staff. The inpatient pharmacy team was notified that there would be an educational period to explain the queue process to hospital staff. Occasionally, hospital staff believed they were speaking to an automated system and hung up before their call was answered. The inpatient pharmacy team was instructed to notify the hospital staff to stay on the line since their call would be answered in the order it was received. Once the inpatient pharmacy team received proper training and felt comfortable with the phone system, it was set up and integrated into the workflow.
Postimplementation Evaluation
Inpatient pharmacy ACD phone system data were collected for 2021. To evaluate the effectiveness of an ACD system, the pharmacy leadership team set up the following metrics and goals for inpatient CPs and inpatient pharmacy technicians for monthly call volume/abandonment rate, mean speed to answer, mean call volume by shift, and the mean abandonment rate by shift.
Inpatient pharmacy technicians answered 27,655 calls with a mean call abandonment rate of 4.7%. and a mean 15.6 seconds to answer.
Discussion
Since implementing the inpatient pharmacy ACD phone system in January 2021, there have been successes and challenges. The implementation increased accountability and efficiency when answering pharmacy phone calls. An ACD uses an algorithm that ensures equitable distribution of phone calls between CPs and pharmacy technicians. Through this algorithm, the pharmacy team is held more accountable when answering incoming calls. Distributing phone calls equally allows for optimization and balances the workload. The ACD phone system also improved efficiency when answering incoming calls. By incorporating splits when a patient or health care professional calls, ACD routes the question to the appropriate staff member. As a result, CPs spend less time answering questions meant for pharmacy technicians and instead can answer clinical or order verification questions more efficiently.
ACD data also allow pharmacy leadership to assess staffing needs, depending on the call volume. Based on ACD data, the busiest time of day was 8:00 AM to 4:00 PM. Based on this information, pharmacy leadership plans to staff more appropriately to have more pharmacy technicians working during the first shift to attend to phone calls.
The mean call abandonment rate was 4.7% for both CPs and pharmacy technicians, which met the ≤ 5% goal. The highest call abandonment rate was from midnight to 8
Pharmacy technicians handled a higher total call volume, which may be attributed to more phone calls related to missing doses or unit stock requests compared with clinical questions or order verifications. This information may be beneficial to identify opportunities to improve pharmacy operations.
The main challenges encountered in the ACD implementation process were hardware installation and communication with hospital staff about the changes in the inpatient pharmacy phone system. To implement the new inpatient pharmacy ACD phone system, previous telephones and hardware were removed and replaced. Initially, hardware and installation delays made it difficult for the ACD phone system to operate efficiently in the early months of its implementation. The inpatient pharmacy team depends on the telecommunications system and computers for their daily activities. Delays and issues with the hardware and ACD phone system made it more difficult to provide patient care.
Communication is a continuous challenge to ensure that hospital staff are notified of the new inpatient pharmacy ACD phone number. Over time, the understanding and use of the new ACD phone system have increased dramatically, but there are still opportunities to capture any misdirected calls. Informal feedback was obtained at pharmacy huddles and 1-on-1 discussions with pharmacy staff, and the opinions were mixed. Members of the pharmacy staff expressed that the ACD phone system set up an effective way to triage phone calls. Another positive comment was that the system created a means of accountability for pharmacy phone calls. Critical feedback included challenges with triaging phone calls to appropriate pharmacists, because calls are assigned based on an algorithm, whereas clinical coverage is determined by designated unit daily assignments.
Limitations
There are potential limitations to this quality improvement project. This phone system may not apply to all inpatient hospital pharmacy settings. Potential limitations for implementation at other institutions may include but are not limited to, differing pharmacy practice models (centralized vs decentralized), implementation costs, and internal resources.
Future Goals
To improve the quality of service provided to patients and other hospital staff, the pharmacy leadership team can use the data to ensure that inpatient pharmacy technician resources are being used effectively during times of day with the greatest number of incoming ACD calls. The ACD phone system helps determine whether current resources are being used most efficiently and if they are not, can help identify areas of improvement.
The pharmacy leadership team plans on using reports for pharmacy team members to monitor performance. Reports on individual agent activity capture workload; this may be used as a performance-related metric for future performance plans.
Conclusions
The inpatient pharmacy ACD phone system at EHJVAH is a promising application of available technology. The implementation of the ACD system improved accountability, efficiency, work distribution, and the allocation of resources in the inpatient pharmacy service. The ACD phone system has yielded positive performance metrics including mean speed to answer ≤ 30 seconds and abandonment rate ≤ 5% over 12 months after implementation. With time, users of the inpatient pharmacy ACD phone system will become more comfortable with the technology, thus further improving the patient health care quality.
1. Rim MH, Thomas KC, Chandramouli J, Barrus SA, Nickman NA. Implementation and quality assessment of a pharmacy services call center for outpatient pharmacies and specialty pharmacy services in an academic health system. Am J Health Syst Pharm. 2018;75(10):633-641. doi:10.2146/ajhp170319
2. Patterson BJ, Doucette WR, Urmie JM, McDonough RP. Exploring relationships among pharmacy service use, patronage motives, and patient satisfaction. J Am Pharm Assoc (2003). 2013;53(4):382-389. doi:10.1331/JAPhA.2013.12100
3. Walker DM, Sieck CJ, Menser T, Huerta TR, Scheck McAlearney A. Information technology to support patient engagement: where do we stand and where can we go?. J Am Med Inform Assoc. 2017;24(6):1088-1094. doi:10.1093/jamia/ocx043
4. Menichetti J, Libreri C, Lozza E, Graffigna G. Giving patients a starring role in their own care: a bibliometric analysis of the on-going literature debate. Health Expect. 2016;19(3):516-526. doi:10.1111/hex.12299
5. Raimbault M, Guérin A, Caron É, Lebel D, Bussières J-F. Identifying and reducing distractions and interruptions in a pharmacy department. Am J Health Syst Pharm. 2013;70(3):186-190. doi:10.2146/ajhp120344
1. Rim MH, Thomas KC, Chandramouli J, Barrus SA, Nickman NA. Implementation and quality assessment of a pharmacy services call center for outpatient pharmacies and specialty pharmacy services in an academic health system. Am J Health Syst Pharm. 2018;75(10):633-641. doi:10.2146/ajhp170319
2. Patterson BJ, Doucette WR, Urmie JM, McDonough RP. Exploring relationships among pharmacy service use, patronage motives, and patient satisfaction. J Am Pharm Assoc (2003). 2013;53(4):382-389. doi:10.1331/JAPhA.2013.12100
3. Walker DM, Sieck CJ, Menser T, Huerta TR, Scheck McAlearney A. Information technology to support patient engagement: where do we stand and where can we go?. J Am Med Inform Assoc. 2017;24(6):1088-1094. doi:10.1093/jamia/ocx043
4. Menichetti J, Libreri C, Lozza E, Graffigna G. Giving patients a starring role in their own care: a bibliometric analysis of the on-going literature debate. Health Expect. 2016;19(3):516-526. doi:10.1111/hex.12299
5. Raimbault M, Guérin A, Caron É, Lebel D, Bussières J-F. Identifying and reducing distractions and interruptions in a pharmacy department. Am J Health Syst Pharm. 2013;70(3):186-190. doi:10.2146/ajhp120344