User login
Adult foot fractures: A guide
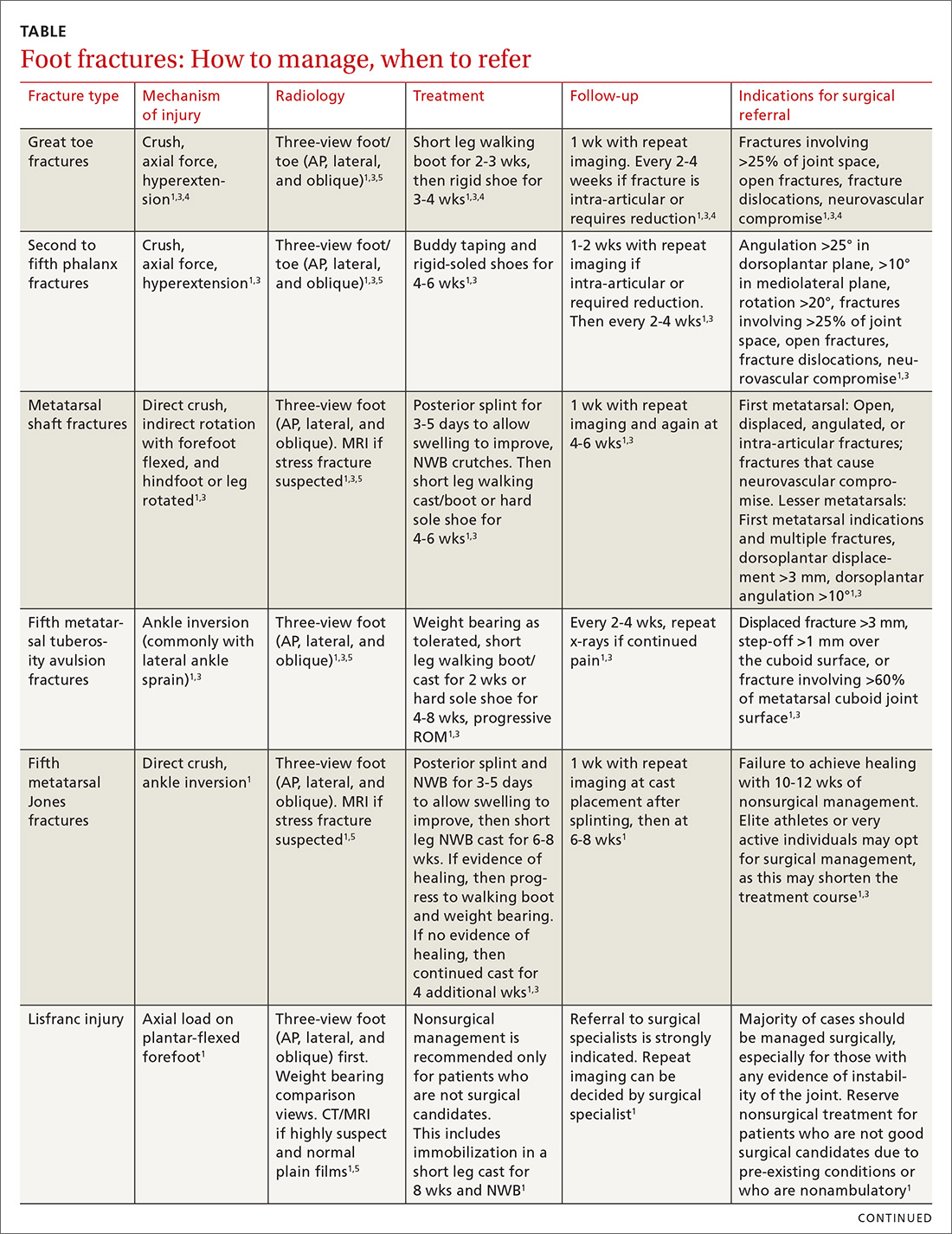
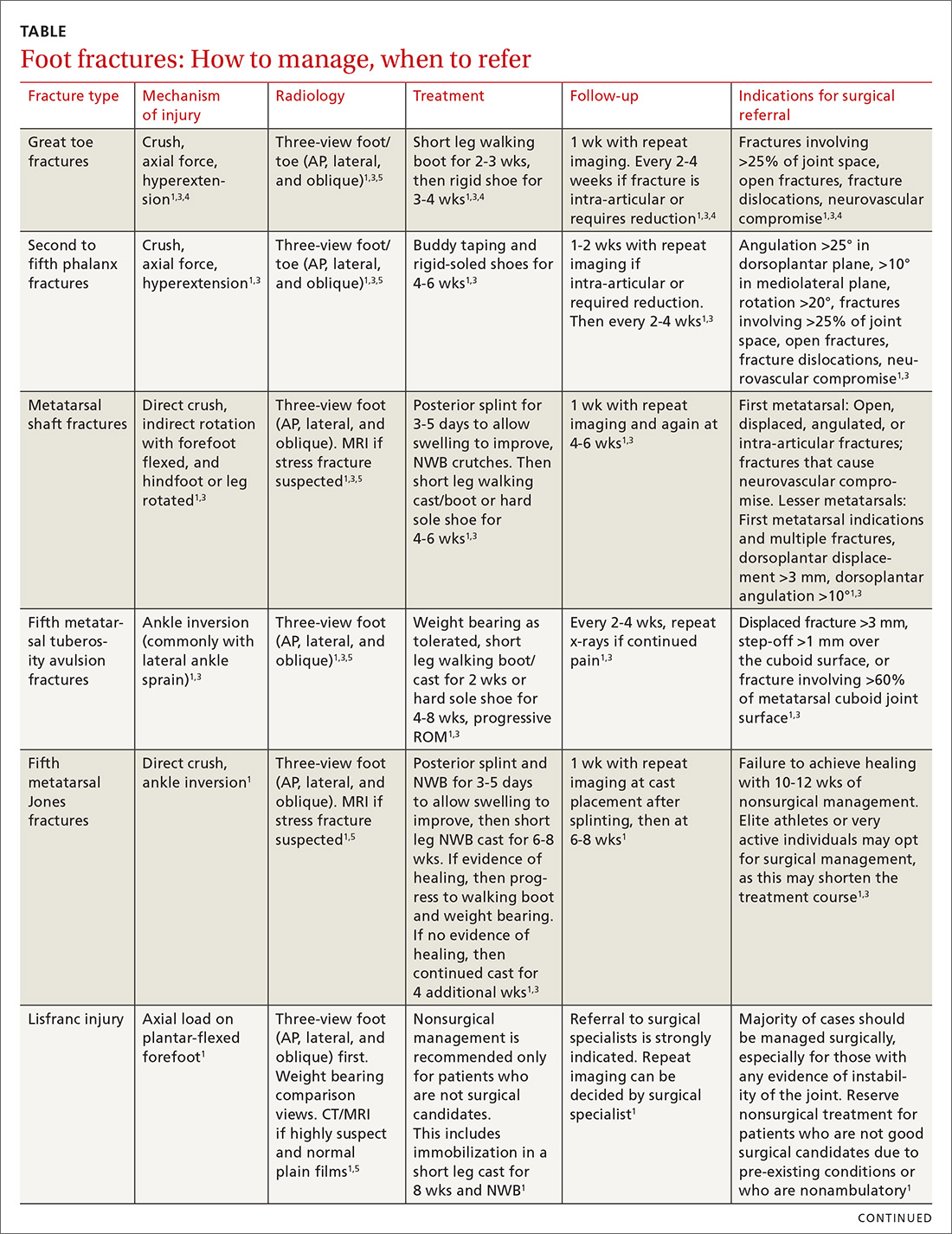
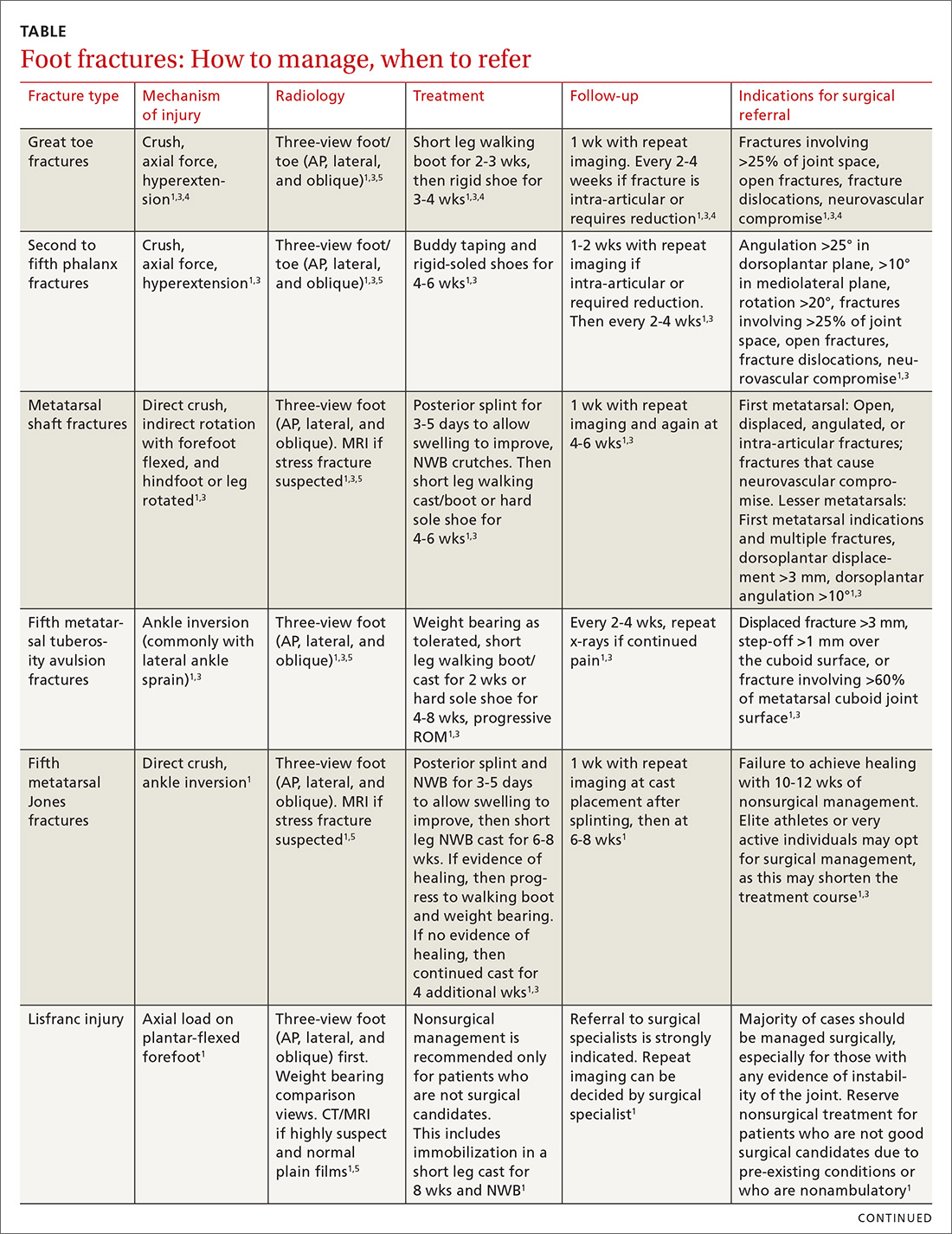
The evaluation and management of acute musculoskeletal conditions are frequently handled by primary care providers.1 It’s estimated that up to 14% of orthopedic complaints encountered by family physicians involve fractures,2 and approximately 15% of these are foot fractures.2 Diagnosis requires radiographic evaluation, but ultrasound is proving useful, too. This article reviews the diagnosis and management of adult foot fractures, with an emphasis on when advanced imaging and referral are indicated (TABLE1,3-10).
Phalanx fractures: The most common foot fractures
Phalanx fractures typically occur by crush injury, hyperextension, or direct axial force (eg, stubbing the toe).3 Patients with phalanx fractures typically present with pain at or near the site of injury, edema, ecchymosis, and erythema. Throbbing pain is characteristic, and dependent position may worsen the pain.1 Emergently evaluate any fracture causing tenting of the skin, protrusion from the skin, or neurovascular compromise, and attempt realignment to regain neurovascular function.

Most patients with phalanx fractures have point tenderness over the site of the fracture; however, this may also occur with contusions. Placing a gentle loading force along the long axis of the bone distal to the injury may help you differentiate between a contusion and a fracture.4 Pain observed with axial loading of the bone during examination points to a fracture rather than a contusion.
Differential diagnosis
Obtain imaging, including anterior-posterior (AP), lateral, and oblique views at a minimum, for all patients in whom you suspect fractures.5 Multiple fractures of the phalanges are common; therefore, always thoroughly examine the phalanges adjacent to the injured one.
Sesamoid bone fractures are uncommon but do occur and are usually due to direct injury from jumping or landing. The most common sesamoid to be injured is the medial sesamoid of the great toe, although the lateral sesamoid can also be injured. Bipartite sesamoids can occur and may confuse the examiner due to their similar appearance on x-rays to a sesamoid fracture.1 These normal variants often appear smooth and are commonly bilateral as opposed to the jagged or abrupt edges of a fracture. Stress fractures occur as well and are typically due to overuse-type injuries.
Other causes of pain similar to that experienced with phalanx fractures include soft tissue injuries to adjacent ligaments, tendons, and muscles. To help discern the cause of pain, evaluate nail beds for subungual hematomas, indicating injury to the nail bed causing bleeding and pressure under the nail. Obvious deformities of the toes or metatarsal-phalangeal joints signal the possibility of a fracture-dislocation. First metatarsophalangeal (MTP) sprain (“turf toe,” a condition common in athletes who hyperextend the toe, such as when pushing off from hard surfaces like turf) and gout can also present with acute pain in the first phalanx.
Treatment
Due to the role of the great toe in weight bearing and balance, great toe fractures are sometimes managed differently than fractures in Toes 2 through 5. Proper alignment and healing from a fracture in the first toe are critical to prevent future pain and other sequelae. Refer for orthopedic evaluation great toe fractures with displacement, angulation, rotational deformity, neurovascular compromise, >25% involvement of the joint space, or obvious dislocation.1 If referral is not indicated, treat great toe fractures with a short leg walking cast/boot for 2 to 3 weeks followed by buddy taping and use of a hard-soled shoe for 3 to 4 weeks.1
Continue to: With regard to the lesser toes...
With regard to the lesser toes, refer patients with fracture-dislocations, displaced intra-articular fractures, and fractures that do not reduce easily. Nondisplaced fractures of the lesser toes do not require surgical referral.1 These can be treated with splinting (buddy taping) and use of rigid-sole shoes for 4 to 6 weeks. Treatment duration depends largely on patient compliance; generally, continue treatment until point tenderness resolves.1
Treatment of sesamoid fractures consists of resting the affected foot with a walking boot, hard-soled shoe, or “donut” pad under the sesamoid bone to help distribute weight on the foot when standing. Length of treatment is approximately 6 to 8 weeks for most fractures.1 Consider surgical referral if nonoperative management is unsuccessful.
Metatarsal fractures: Look for malalignment
Metatarsal fractures account for 5% of all foot fractures encountered in primary care.2 These fractures typically occur as a result of falls, direct trauma, or rotational injuries (eg, ankle and foot sprains).1 In athletes, the most common cause of these fractures is high rotational force. Patients typically present with pain over the injury site, swelling, bruising, and pain with weight bearing.
As part of your exam, look for malalignment, rotational deformities, and evidence of open fracture. Palpation at the site of the fracture may increase the pain; however, as is true with phalanx fractures, contusions may also cause significant tenderness upon palpation. Also assess range of motion—with special attention to signs of malrotation—and evaluate the adjacent metatarsals, as multiple bones, ligaments, or both are often involved.1
Fifth metatarsal fractures are the most common in adults, likely because of decreased cortical thickness as compared with the other metatarsals.3,11 In addition, multiple soft tissue attachments connect at the proximal aspect of the fifth metatarsal. Classification of these types of metatarsal fractures is based on anatomic location.3 Jones fractures are one type of fracture at the proximal aspect of the fifth metatarsal that occur at the metaphyseal-diaphyseal junction specifically (FIGURE 1). Because this area receives its blood supply from small terminal vessels, fractures here have a high risk of non-union and, thus, should be top of mind in any patient with tenderness at the base of the fifth metatarsal.

Continue to: MRI/ultrasound in addition to plain films?
MRI/ultrasound in addition to plain films?
Use the Ottawa Ankle and Foot Rules to determine the need for foot radiographs in the acute setting.12 If indicated, imaging should include AP, lateral, and oblique views of the foot.5 Consider magnetic resonance imaging (MRI) if you suspect a stress fracture, which typically presents as an overuse injury in athletes.
Ultrasound may be effective for identifying metatarsal fractures, as well.13 Ultrasound can be used to visualize fractures of the long metatarsal bones and identify displacement, angulation, and step-offs. Although its use in the United States has been limited for this purpose, studies in other countries are showing that it yields results comparable to plain films in the emergency department setting for diagnosis and initial management of these fractures.13
Differential diagnosis
Multiple other diagnoses present similarly to metatarsal fractures including: ligamentous/tendon/soft tissue injuries, interdigital neuroma, sesamoid fractures, and Lisfranc ligament injury (which we'll discuss in a bit). Stress fractures of the metatarsal, most commonly seen in the second metatarsal, are insidious in nature and are common with repetitive movement such as that made by gymnasts, dancers, and track athletes.14 Metatarsalgia, which causes pain at the ball of the foot, is a condition that can stem from a myriad of causes including a low or high arch, biomechanics, and previous injury.
Treatment
Nondisplaced, minimally displaced (<3 mm), and minimally angulated (<10° dorsal/plantar angulation) fractures of any metatarsal shaft may be managed conservatively with a hard-soled shoe or walking boot with weight bearing as tolerated for 4 to 6 weeks.1 Most stress fractures (excluding fifth metatarsal stress fractures) may be treated similarly. Surgical referral is indicated for patients with any open fracture, first metatarsal fractures with displacement, central metatarsal fractures with >10° deformity, >3 mm of translation, multiple fractures, or fifth metatarsal stress fracture.1
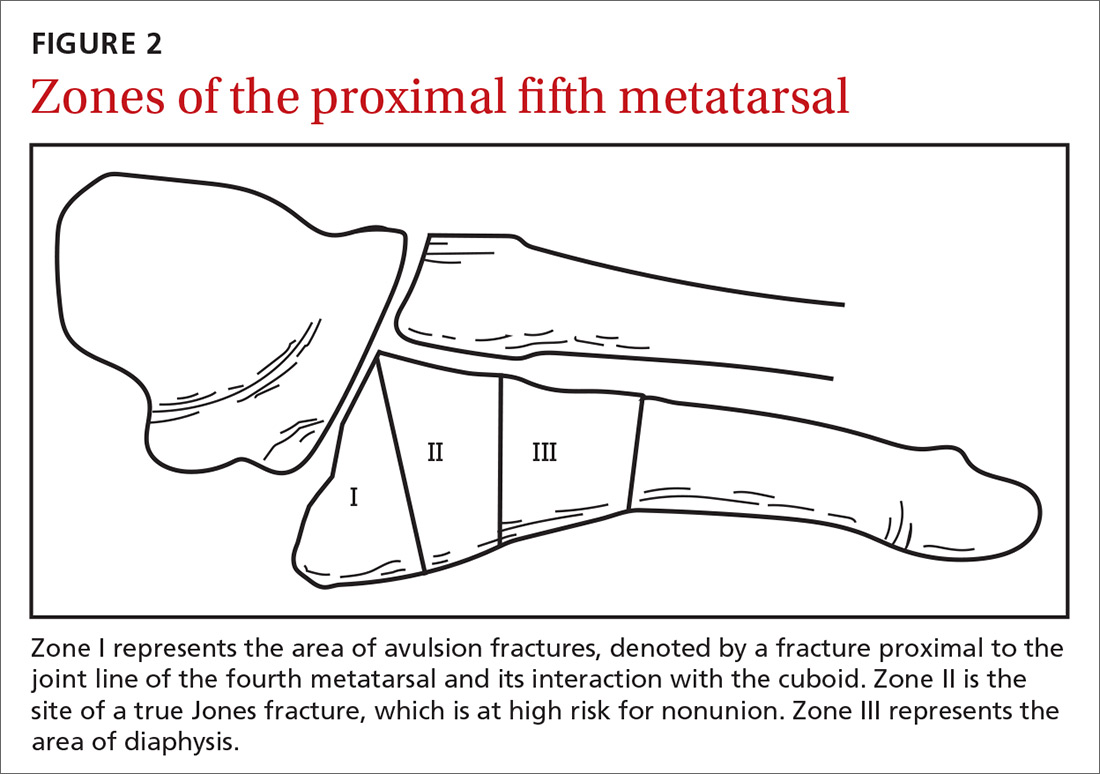
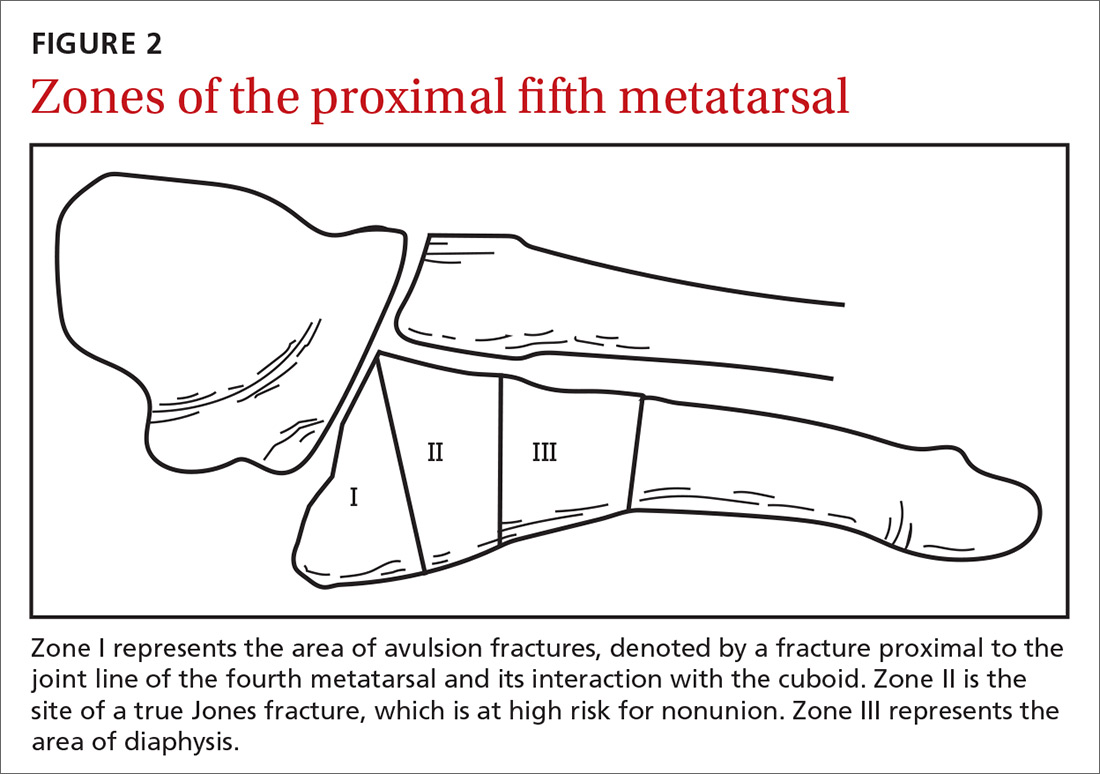
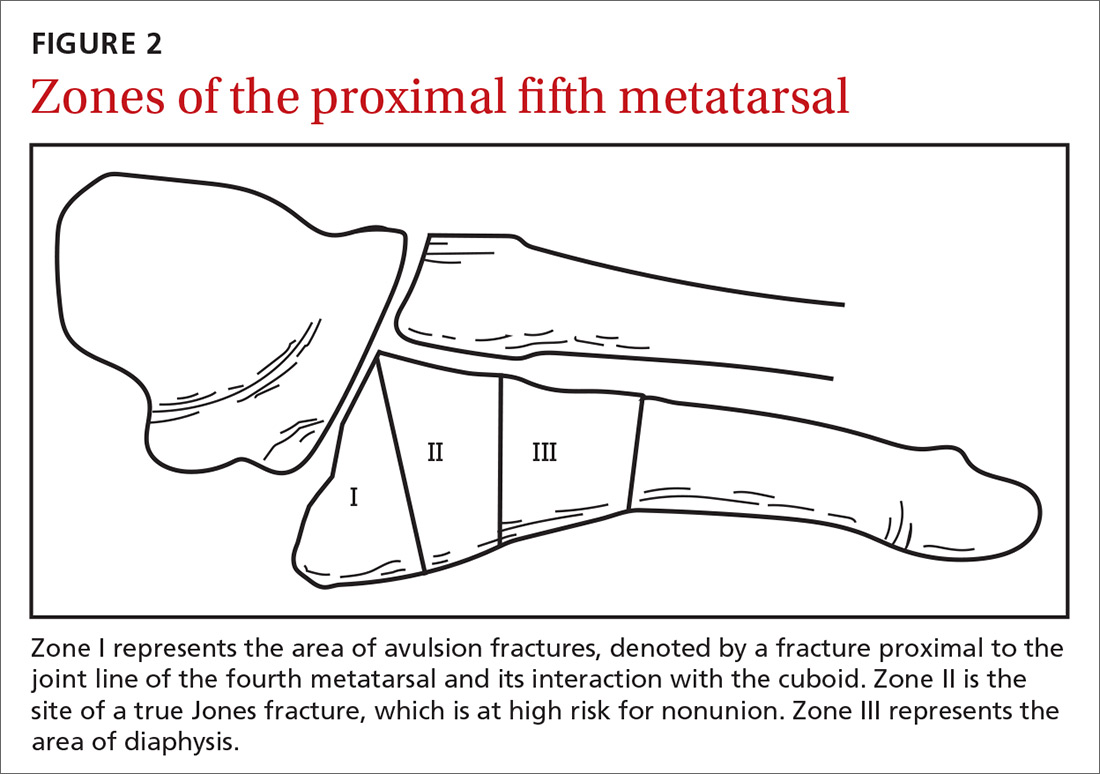
Base of fifth metatarsal tuberosity avulsion fractures can be managed nonoperatively with protected weight bearing in a boot or cast for 2 weeks or hard sole shoe for 4 to 8 weeks if the fracture is at the proximal tubercle (see Zone I, FIGURE 2). Jones fractures (Zone II, FIGURE 2) or fractures of the proximal diaphysis (Zone III, FIGURE 2) of the fifth metatarsal may also be managed nonoperatively in patients who are not competitive athletes. This can be done with a non-weight bearing (NWB) short leg cast for 6 to 8 weeks at a minimum.4 If the patient is an athlete who wishes to resume competition, surgical referral is indicated, as the risk of nonunion is high with these fractures.15
Continue to: Stress fractures and stress reactions...
Stress fractures and stress reactions (early evidence of bone edema seen on MRI, indicating progression to stress fracture) of the proximal fifth metatarsal should be managed with strict activity modifications and a NWB short leg cast for 6 to 8 weeks, given the high risk of nonunion.
Midfoot fractures: The cuboid, cuneiforms, and navicular bone
Although fractures are less common in the midfoot, the midfoot serves an important role in weight bearing and stabilization. In addition, along with the metatarsal bones, the midfoot is critical to proper alignment and articulation.
Cuboid and cuneiform fractures
Cuboid fractures may occur with high-velocity trauma, foot inversion with external rotation of the tibia, a direct blow, or axial load on a plantar-flexed heel. Pain with weight bearing or with walking on toes is usually present. Cuneiform fractures are less common and rarely occur in isolation.6 Mechanisms of injury for cuneiform fractures include direct impact, axial loading on a dorsiflexed or plantar-flexed foot with rotational force, and severe rotation of the midfoot section in a fixed foot. Pain is usually localized to the dorsal or dorsomedial aspect of the foot.
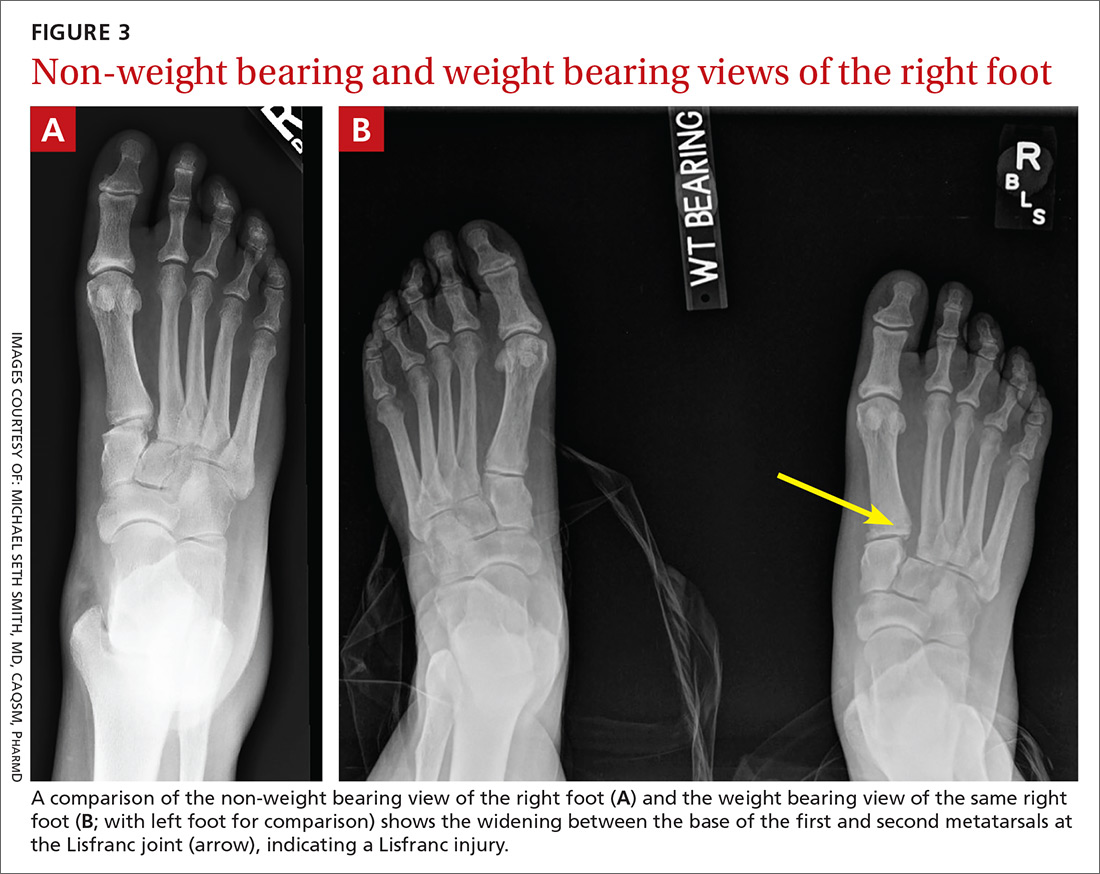
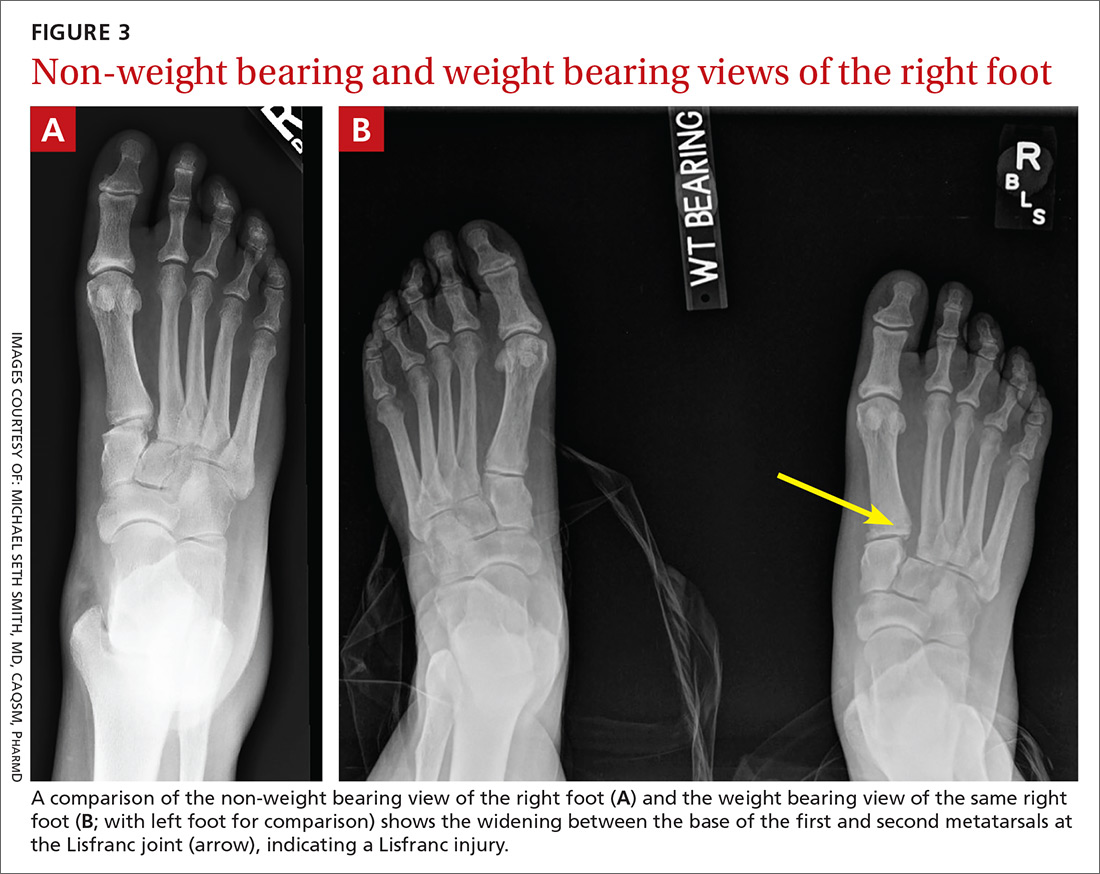
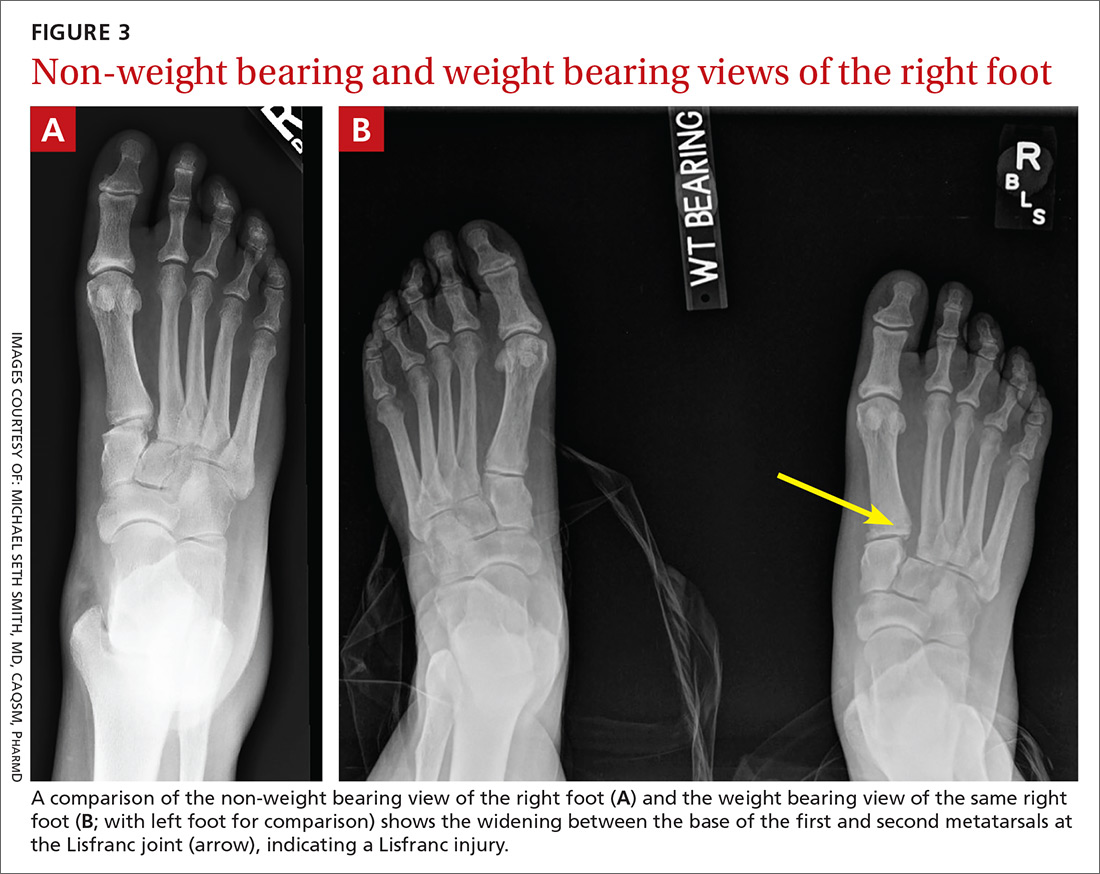
With these 2 midfoot injuries, the exam should include palpation of the cuboid, navicular, and cuneiform bones and careful inspection of the Lisfranc joint, as this can be injured in midfoot fractures.7 Obtain AP, lateral, and oblique views of the foot,5 and strongly consider bilateral weight-bearing films to evaluate for tarsometatarsal (TMT) joint complex injuries (typically Lisfranc joint complex injuries), given their association with midfoot fractures1 (FIGURE 3).
If the fracture is at or near the TMT joint complex, obtain a CT scan or MRI regardless of plain film findings to evaluate the Lisfranc joint complex. Because the Lisfranc joint is particularly important in midfoot stability, untreated injuries can lead to impaired gait or chronic foot pain and deformity. Early identification and surgical referral for these injuries is crucial.
Continue to: Navicular fractures
Navicular fractures
Navicular fractures are typically caused by a twisting mechanism with forced plantar flexion or forced dorsiflexion of the midfoot. They present with severe pain over the dorsal or dorsomedial foot, particularly while bearing weight. Tenderness to palpation over the navicular bone generally warrants imaging studies to rule out fracture, as undiagnosed fractures can lead to severe long-term disability. Use Ottawa Ankle and Foot Rules12 in the acute setting to determine the need for radiographs. If imaging is indicated, obtain AP, lateral, and oblique views.
Tuberosity fractures may be seen on the AP view, while dorsal avulsions, talonavicular joint disruptions, and naviculo-cuneiform joint injuries are better seen on lateral views.16 Patients, particularly cross-country and track athletes, presenting with insidious onset of pain over the navicular bone should be evaluated for stress fracture using MRI, even in the presence of normal radiographs.
Differential diagnosis. Suspect Lisfranc joint complex injuries in any patient with mid-foot pain or fracture. The transverse arch of the foot is reliant upon the articulation of the second metatarsal with all 5 neighboring bones. The Lisfranc ligament is the strongest of 3 supporting ligaments to anchor the TMT joint complex. Other causes of mid-foot pain include soft tissue injury, contusion, and tendinopathy. In addition, other conditions that may cause pain in this area include cuboid syndrome, peroneal tendinopathy, Jones fracture, stress fracture, anterior calcaneal fracture, and sinus tarsi syndrome.
Treatment. Nondisplaced fractures of the cuboid or cuneiform may be treated with a short leg walking cast/boot for 6 weeks followed by the use of a shoe with a thin, rigid, longitudinal arch support for an additional 6 weeks.1 Fractures requiring referral for surgical evaluation include fractures that are open and fractures with vascular or neurological compromise. Also refer comminuted fractures and those that present with >2 mm step-off. Lastly, midfoot fractures that involve the Lisfranc joint should be immobilized and referred for orthopedic evaluation with instructions to the patient to avoid weight bearing until orthopedic evaluation.8
Avulsion fractures of the navicular bone may be managed nonoperatively with a short leg walking cast/boot if there is <20% involvement of the talonavicular surface. Simple nondisplaced body fractures may also be managed conservatively with immobilization and protected weight bearing for 6 to 8 weeks.15 Refer for surgical evaluation avulsion fractures that are intra-articular or dorsal involving 20% or more of the talonavicular surface and tuberosity fractures, given their risk of nonunion.9 All navicular body fractures that are not longitudinal in nature should also be referred for surgical evaluation. Navicular stress fractures that do not extend into the plantar cortex may be managed conservatively with a minimum of 6 weeks of a short leg cast and strict NWB with close follow-up.17
Continue to: Calcaneal fractures
Calcaneal fractures
Calcaneal fractures typically occur from severe axial load or fall from a height. Weight bearing is usually limited and secondary to significant pain. Tenderness to palpation over the calcaneus or with squeezing of the heel will produce pain on exam. Initial x-rays should include a lateral and axial view of the calcaneus. Additional imaging, including a CT scan, may be indicated for further evaluation to determine the extent of the fracture or to determine if a fracture is present despite normal x-rays.10
Acute compartment syndrome occurs in 10% of calcaneal fractures and must be considered in patients with calcaneal fractures from severe trauma.18 Tendon injuries of the ankle, hindfoot, and midfoot may present similarly but can be ruled out with clinical exam and appropriate imaging.
Treatment
Avulsion fractures that do not involve more than 25% of the calcaneocuboid joint and nondisplaced calcaneal fractures may be managed conservatively by instructing patients to wear a NWB short leg cast/boot for 4 to 6 weeks.1 Refer for surgical evaluation patients with calcaneal fracture fragments >1 cm, displacement >3 mm, open fractures, joint involvement >25%, and those whose symptoms fail to resolve with conservative management. Stress fractures can be managed conservatively with cessation of aggravating activities and immobilization in a walking boot until symptoms resolve, which typically takes 4 to 6 weeks.1
CORRESPONDENCE
Michael Seth Smith, MD, CAQSM, PharmD, 3450 Hull Road, Gainesville, FL 32611; [email protected]
1. Eiff MP, Hatch RL, et al. Fracture Management for Primary Care. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
2. Hatch RL, Rosenbaum Cl. Fracture care by family physicians. A review of 295 cases. J Fam Pract. 1994;38:238-244.
3. Bica D, Sprouse RA, Armen J. Diagnosis and management of common foot fractures. Am Fam Physician. 2016;93:183-191.
4. Hatch RL, Hacking S. Evaluation and management of toe fractures. Am Fam Physician. 2003;68:2413-2418.
5. Snider RK. Essentials of Musculoskeletal Care. 2nd ed. Rosemont, IL: American Orthopedic Surgeons; 2001.
6. Guler F, Baz AB, Turan A, et al. Isolated medial cuneiform fractures: report of two cases and review of the literature. Foot Ankle Spec. 2011;4:306-309.
7. Borrelli J, De S, Van Pelt M. Fracture of the cuboid. J Am Acad Orthop Surg. 2012;20:472.
8. Pinney SJ, Sangeorzan BJ. Fractures of the tarsal bones. Orthop Clin North Am. 2001:32:21-33.
9. Rosenbaum AJ, Uhl R, DiPreta JA. Acute fractures of the tarsal navicular. Orthopedics. 2014;37:541-546.
10. Sanders RW, Clare MP. Calcaneous fractures. In: Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:2064.
11. Singer G, Cichocki M, Schalamon J, et al. A study of metatarsal fractures in children. J Bone Joint Surg Am. 2008;90:772-776.
12. Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384-390.
13. Ekinci S, Polat O, Günalp M, et al. The accuracy of ultrasound evaluation in foot and ankle trauma. Am J Emerg Med. 2013;31:1551-1555.
14. Welck MJ, Hayes T, Pastides P, et al. Stress fractures of the foot and ankle. Injury. 2017;48:1722-1726.
15. Hatch RL, Alsobrook JA, Clugston JR. Diagnosis and management of metatarsal fractures. Am Fam Physician. 2007;76:817-826.
16. Schildhauer TA, Coulibaly MO, Hoffman MF. Fractures and dislocations of the midfoot and forefoot. In: Rockwood and Green’s Fractures in Adults. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:2690.
17. Mayer SW, Joyner PW, Almekinders LC, et al. Stress fractures of the foot and ankle in athletes. Sports Health. 2014;6:481-491.
18. Kalsi R, Dempsey A, Bunney EB. Compartment syndrome of the foot after calcaneal fracture. J Emerg Med. 2012;43:e101-106.
The evaluation and management of acute musculoskeletal conditions are frequently handled by primary care providers.1 It’s estimated that up to 14% of orthopedic complaints encountered by family physicians involve fractures,2 and approximately 15% of these are foot fractures.2 Diagnosis requires radiographic evaluation, but ultrasound is proving useful, too. This article reviews the diagnosis and management of adult foot fractures, with an emphasis on when advanced imaging and referral are indicated (TABLE1,3-10).
Phalanx fractures: The most common foot fractures
Phalanx fractures typically occur by crush injury, hyperextension, or direct axial force (eg, stubbing the toe).3 Patients with phalanx fractures typically present with pain at or near the site of injury, edema, ecchymosis, and erythema. Throbbing pain is characteristic, and dependent position may worsen the pain.1 Emergently evaluate any fracture causing tenting of the skin, protrusion from the skin, or neurovascular compromise, and attempt realignment to regain neurovascular function.

Most patients with phalanx fractures have point tenderness over the site of the fracture; however, this may also occur with contusions. Placing a gentle loading force along the long axis of the bone distal to the injury may help you differentiate between a contusion and a fracture.4 Pain observed with axial loading of the bone during examination points to a fracture rather than a contusion.
Differential diagnosis
Obtain imaging, including anterior-posterior (AP), lateral, and oblique views at a minimum, for all patients in whom you suspect fractures.5 Multiple fractures of the phalanges are common; therefore, always thoroughly examine the phalanges adjacent to the injured one.
Sesamoid bone fractures are uncommon but do occur and are usually due to direct injury from jumping or landing. The most common sesamoid to be injured is the medial sesamoid of the great toe, although the lateral sesamoid can also be injured. Bipartite sesamoids can occur and may confuse the examiner due to their similar appearance on x-rays to a sesamoid fracture.1 These normal variants often appear smooth and are commonly bilateral as opposed to the jagged or abrupt edges of a fracture. Stress fractures occur as well and are typically due to overuse-type injuries.
Other causes of pain similar to that experienced with phalanx fractures include soft tissue injuries to adjacent ligaments, tendons, and muscles. To help discern the cause of pain, evaluate nail beds for subungual hematomas, indicating injury to the nail bed causing bleeding and pressure under the nail. Obvious deformities of the toes or metatarsal-phalangeal joints signal the possibility of a fracture-dislocation. First metatarsophalangeal (MTP) sprain (“turf toe,” a condition common in athletes who hyperextend the toe, such as when pushing off from hard surfaces like turf) and gout can also present with acute pain in the first phalanx.
Treatment
Due to the role of the great toe in weight bearing and balance, great toe fractures are sometimes managed differently than fractures in Toes 2 through 5. Proper alignment and healing from a fracture in the first toe are critical to prevent future pain and other sequelae. Refer for orthopedic evaluation great toe fractures with displacement, angulation, rotational deformity, neurovascular compromise, >25% involvement of the joint space, or obvious dislocation.1 If referral is not indicated, treat great toe fractures with a short leg walking cast/boot for 2 to 3 weeks followed by buddy taping and use of a hard-soled shoe for 3 to 4 weeks.1
Continue to: With regard to the lesser toes...
With regard to the lesser toes, refer patients with fracture-dislocations, displaced intra-articular fractures, and fractures that do not reduce easily. Nondisplaced fractures of the lesser toes do not require surgical referral.1 These can be treated with splinting (buddy taping) and use of rigid-sole shoes for 4 to 6 weeks. Treatment duration depends largely on patient compliance; generally, continue treatment until point tenderness resolves.1
Treatment of sesamoid fractures consists of resting the affected foot with a walking boot, hard-soled shoe, or “donut” pad under the sesamoid bone to help distribute weight on the foot when standing. Length of treatment is approximately 6 to 8 weeks for most fractures.1 Consider surgical referral if nonoperative management is unsuccessful.
Metatarsal fractures: Look for malalignment
Metatarsal fractures account for 5% of all foot fractures encountered in primary care.2 These fractures typically occur as a result of falls, direct trauma, or rotational injuries (eg, ankle and foot sprains).1 In athletes, the most common cause of these fractures is high rotational force. Patients typically present with pain over the injury site, swelling, bruising, and pain with weight bearing.
As part of your exam, look for malalignment, rotational deformities, and evidence of open fracture. Palpation at the site of the fracture may increase the pain; however, as is true with phalanx fractures, contusions may also cause significant tenderness upon palpation. Also assess range of motion—with special attention to signs of malrotation—and evaluate the adjacent metatarsals, as multiple bones, ligaments, or both are often involved.1
Fifth metatarsal fractures are the most common in adults, likely because of decreased cortical thickness as compared with the other metatarsals.3,11 In addition, multiple soft tissue attachments connect at the proximal aspect of the fifth metatarsal. Classification of these types of metatarsal fractures is based on anatomic location.3 Jones fractures are one type of fracture at the proximal aspect of the fifth metatarsal that occur at the metaphyseal-diaphyseal junction specifically (FIGURE 1). Because this area receives its blood supply from small terminal vessels, fractures here have a high risk of non-union and, thus, should be top of mind in any patient with tenderness at the base of the fifth metatarsal.

Continue to: MRI/ultrasound in addition to plain films?
MRI/ultrasound in addition to plain films?
Use the Ottawa Ankle and Foot Rules to determine the need for foot radiographs in the acute setting.12 If indicated, imaging should include AP, lateral, and oblique views of the foot.5 Consider magnetic resonance imaging (MRI) if you suspect a stress fracture, which typically presents as an overuse injury in athletes.
Ultrasound may be effective for identifying metatarsal fractures, as well.13 Ultrasound can be used to visualize fractures of the long metatarsal bones and identify displacement, angulation, and step-offs. Although its use in the United States has been limited for this purpose, studies in other countries are showing that it yields results comparable to plain films in the emergency department setting for diagnosis and initial management of these fractures.13
Differential diagnosis
Multiple other diagnoses present similarly to metatarsal fractures including: ligamentous/tendon/soft tissue injuries, interdigital neuroma, sesamoid fractures, and Lisfranc ligament injury (which we'll discuss in a bit). Stress fractures of the metatarsal, most commonly seen in the second metatarsal, are insidious in nature and are common with repetitive movement such as that made by gymnasts, dancers, and track athletes.14 Metatarsalgia, which causes pain at the ball of the foot, is a condition that can stem from a myriad of causes including a low or high arch, biomechanics, and previous injury.
Treatment
Nondisplaced, minimally displaced (<3 mm), and minimally angulated (<10° dorsal/plantar angulation) fractures of any metatarsal shaft may be managed conservatively with a hard-soled shoe or walking boot with weight bearing as tolerated for 4 to 6 weeks.1 Most stress fractures (excluding fifth metatarsal stress fractures) may be treated similarly. Surgical referral is indicated for patients with any open fracture, first metatarsal fractures with displacement, central metatarsal fractures with >10° deformity, >3 mm of translation, multiple fractures, or fifth metatarsal stress fracture.1
Base of fifth metatarsal tuberosity avulsion fractures can be managed nonoperatively with protected weight bearing in a boot or cast for 2 weeks or hard sole shoe for 4 to 8 weeks if the fracture is at the proximal tubercle (see Zone I, FIGURE 2). Jones fractures (Zone II, FIGURE 2) or fractures of the proximal diaphysis (Zone III, FIGURE 2) of the fifth metatarsal may also be managed nonoperatively in patients who are not competitive athletes. This can be done with a non-weight bearing (NWB) short leg cast for 6 to 8 weeks at a minimum.4 If the patient is an athlete who wishes to resume competition, surgical referral is indicated, as the risk of nonunion is high with these fractures.15
Continue to: Stress fractures and stress reactions...
Stress fractures and stress reactions (early evidence of bone edema seen on MRI, indicating progression to stress fracture) of the proximal fifth metatarsal should be managed with strict activity modifications and a NWB short leg cast for 6 to 8 weeks, given the high risk of nonunion.
Midfoot fractures: The cuboid, cuneiforms, and navicular bone
Although fractures are less common in the midfoot, the midfoot serves an important role in weight bearing and stabilization. In addition, along with the metatarsal bones, the midfoot is critical to proper alignment and articulation.
Cuboid and cuneiform fractures
Cuboid fractures may occur with high-velocity trauma, foot inversion with external rotation of the tibia, a direct blow, or axial load on a plantar-flexed heel. Pain with weight bearing or with walking on toes is usually present. Cuneiform fractures are less common and rarely occur in isolation.6 Mechanisms of injury for cuneiform fractures include direct impact, axial loading on a dorsiflexed or plantar-flexed foot with rotational force, and severe rotation of the midfoot section in a fixed foot. Pain is usually localized to the dorsal or dorsomedial aspect of the foot.
With these 2 midfoot injuries, the exam should include palpation of the cuboid, navicular, and cuneiform bones and careful inspection of the Lisfranc joint, as this can be injured in midfoot fractures.7 Obtain AP, lateral, and oblique views of the foot,5 and strongly consider bilateral weight-bearing films to evaluate for tarsometatarsal (TMT) joint complex injuries (typically Lisfranc joint complex injuries), given their association with midfoot fractures1 (FIGURE 3).
If the fracture is at or near the TMT joint complex, obtain a CT scan or MRI regardless of plain film findings to evaluate the Lisfranc joint complex. Because the Lisfranc joint is particularly important in midfoot stability, untreated injuries can lead to impaired gait or chronic foot pain and deformity. Early identification and surgical referral for these injuries is crucial.
Continue to: Navicular fractures
Navicular fractures
Navicular fractures are typically caused by a twisting mechanism with forced plantar flexion or forced dorsiflexion of the midfoot. They present with severe pain over the dorsal or dorsomedial foot, particularly while bearing weight. Tenderness to palpation over the navicular bone generally warrants imaging studies to rule out fracture, as undiagnosed fractures can lead to severe long-term disability. Use Ottawa Ankle and Foot Rules12 in the acute setting to determine the need for radiographs. If imaging is indicated, obtain AP, lateral, and oblique views.
Tuberosity fractures may be seen on the AP view, while dorsal avulsions, talonavicular joint disruptions, and naviculo-cuneiform joint injuries are better seen on lateral views.16 Patients, particularly cross-country and track athletes, presenting with insidious onset of pain over the navicular bone should be evaluated for stress fracture using MRI, even in the presence of normal radiographs.
Differential diagnosis. Suspect Lisfranc joint complex injuries in any patient with mid-foot pain or fracture. The transverse arch of the foot is reliant upon the articulation of the second metatarsal with all 5 neighboring bones. The Lisfranc ligament is the strongest of 3 supporting ligaments to anchor the TMT joint complex. Other causes of mid-foot pain include soft tissue injury, contusion, and tendinopathy. In addition, other conditions that may cause pain in this area include cuboid syndrome, peroneal tendinopathy, Jones fracture, stress fracture, anterior calcaneal fracture, and sinus tarsi syndrome.
Treatment. Nondisplaced fractures of the cuboid or cuneiform may be treated with a short leg walking cast/boot for 6 weeks followed by the use of a shoe with a thin, rigid, longitudinal arch support for an additional 6 weeks.1 Fractures requiring referral for surgical evaluation include fractures that are open and fractures with vascular or neurological compromise. Also refer comminuted fractures and those that present with >2 mm step-off. Lastly, midfoot fractures that involve the Lisfranc joint should be immobilized and referred for orthopedic evaluation with instructions to the patient to avoid weight bearing until orthopedic evaluation.8
Avulsion fractures of the navicular bone may be managed nonoperatively with a short leg walking cast/boot if there is <20% involvement of the talonavicular surface. Simple nondisplaced body fractures may also be managed conservatively with immobilization and protected weight bearing for 6 to 8 weeks.15 Refer for surgical evaluation avulsion fractures that are intra-articular or dorsal involving 20% or more of the talonavicular surface and tuberosity fractures, given their risk of nonunion.9 All navicular body fractures that are not longitudinal in nature should also be referred for surgical evaluation. Navicular stress fractures that do not extend into the plantar cortex may be managed conservatively with a minimum of 6 weeks of a short leg cast and strict NWB with close follow-up.17
Continue to: Calcaneal fractures
Calcaneal fractures
Calcaneal fractures typically occur from severe axial load or fall from a height. Weight bearing is usually limited and secondary to significant pain. Tenderness to palpation over the calcaneus or with squeezing of the heel will produce pain on exam. Initial x-rays should include a lateral and axial view of the calcaneus. Additional imaging, including a CT scan, may be indicated for further evaluation to determine the extent of the fracture or to determine if a fracture is present despite normal x-rays.10
Acute compartment syndrome occurs in 10% of calcaneal fractures and must be considered in patients with calcaneal fractures from severe trauma.18 Tendon injuries of the ankle, hindfoot, and midfoot may present similarly but can be ruled out with clinical exam and appropriate imaging.
Treatment
Avulsion fractures that do not involve more than 25% of the calcaneocuboid joint and nondisplaced calcaneal fractures may be managed conservatively by instructing patients to wear a NWB short leg cast/boot for 4 to 6 weeks.1 Refer for surgical evaluation patients with calcaneal fracture fragments >1 cm, displacement >3 mm, open fractures, joint involvement >25%, and those whose symptoms fail to resolve with conservative management. Stress fractures can be managed conservatively with cessation of aggravating activities and immobilization in a walking boot until symptoms resolve, which typically takes 4 to 6 weeks.1
CORRESPONDENCE
Michael Seth Smith, MD, CAQSM, PharmD, 3450 Hull Road, Gainesville, FL 32611; [email protected]
The evaluation and management of acute musculoskeletal conditions are frequently handled by primary care providers.1 It’s estimated that up to 14% of orthopedic complaints encountered by family physicians involve fractures,2 and approximately 15% of these are foot fractures.2 Diagnosis requires radiographic evaluation, but ultrasound is proving useful, too. This article reviews the diagnosis and management of adult foot fractures, with an emphasis on when advanced imaging and referral are indicated (TABLE1,3-10).
Phalanx fractures: The most common foot fractures
Phalanx fractures typically occur by crush injury, hyperextension, or direct axial force (eg, stubbing the toe).3 Patients with phalanx fractures typically present with pain at or near the site of injury, edema, ecchymosis, and erythema. Throbbing pain is characteristic, and dependent position may worsen the pain.1 Emergently evaluate any fracture causing tenting of the skin, protrusion from the skin, or neurovascular compromise, and attempt realignment to regain neurovascular function.

Most patients with phalanx fractures have point tenderness over the site of the fracture; however, this may also occur with contusions. Placing a gentle loading force along the long axis of the bone distal to the injury may help you differentiate between a contusion and a fracture.4 Pain observed with axial loading of the bone during examination points to a fracture rather than a contusion.
Differential diagnosis
Obtain imaging, including anterior-posterior (AP), lateral, and oblique views at a minimum, for all patients in whom you suspect fractures.5 Multiple fractures of the phalanges are common; therefore, always thoroughly examine the phalanges adjacent to the injured one.
Sesamoid bone fractures are uncommon but do occur and are usually due to direct injury from jumping or landing. The most common sesamoid to be injured is the medial sesamoid of the great toe, although the lateral sesamoid can also be injured. Bipartite sesamoids can occur and may confuse the examiner due to their similar appearance on x-rays to a sesamoid fracture.1 These normal variants often appear smooth and are commonly bilateral as opposed to the jagged or abrupt edges of a fracture. Stress fractures occur as well and are typically due to overuse-type injuries.
Other causes of pain similar to that experienced with phalanx fractures include soft tissue injuries to adjacent ligaments, tendons, and muscles. To help discern the cause of pain, evaluate nail beds for subungual hematomas, indicating injury to the nail bed causing bleeding and pressure under the nail. Obvious deformities of the toes or metatarsal-phalangeal joints signal the possibility of a fracture-dislocation. First metatarsophalangeal (MTP) sprain (“turf toe,” a condition common in athletes who hyperextend the toe, such as when pushing off from hard surfaces like turf) and gout can also present with acute pain in the first phalanx.
Treatment
Due to the role of the great toe in weight bearing and balance, great toe fractures are sometimes managed differently than fractures in Toes 2 through 5. Proper alignment and healing from a fracture in the first toe are critical to prevent future pain and other sequelae. Refer for orthopedic evaluation great toe fractures with displacement, angulation, rotational deformity, neurovascular compromise, >25% involvement of the joint space, or obvious dislocation.1 If referral is not indicated, treat great toe fractures with a short leg walking cast/boot for 2 to 3 weeks followed by buddy taping and use of a hard-soled shoe for 3 to 4 weeks.1
Continue to: With regard to the lesser toes...
With regard to the lesser toes, refer patients with fracture-dislocations, displaced intra-articular fractures, and fractures that do not reduce easily. Nondisplaced fractures of the lesser toes do not require surgical referral.1 These can be treated with splinting (buddy taping) and use of rigid-sole shoes for 4 to 6 weeks. Treatment duration depends largely on patient compliance; generally, continue treatment until point tenderness resolves.1
Treatment of sesamoid fractures consists of resting the affected foot with a walking boot, hard-soled shoe, or “donut” pad under the sesamoid bone to help distribute weight on the foot when standing. Length of treatment is approximately 6 to 8 weeks for most fractures.1 Consider surgical referral if nonoperative management is unsuccessful.
Metatarsal fractures: Look for malalignment
Metatarsal fractures account for 5% of all foot fractures encountered in primary care.2 These fractures typically occur as a result of falls, direct trauma, or rotational injuries (eg, ankle and foot sprains).1 In athletes, the most common cause of these fractures is high rotational force. Patients typically present with pain over the injury site, swelling, bruising, and pain with weight bearing.
As part of your exam, look for malalignment, rotational deformities, and evidence of open fracture. Palpation at the site of the fracture may increase the pain; however, as is true with phalanx fractures, contusions may also cause significant tenderness upon palpation. Also assess range of motion—with special attention to signs of malrotation—and evaluate the adjacent metatarsals, as multiple bones, ligaments, or both are often involved.1
Fifth metatarsal fractures are the most common in adults, likely because of decreased cortical thickness as compared with the other metatarsals.3,11 In addition, multiple soft tissue attachments connect at the proximal aspect of the fifth metatarsal. Classification of these types of metatarsal fractures is based on anatomic location.3 Jones fractures are one type of fracture at the proximal aspect of the fifth metatarsal that occur at the metaphyseal-diaphyseal junction specifically (FIGURE 1). Because this area receives its blood supply from small terminal vessels, fractures here have a high risk of non-union and, thus, should be top of mind in any patient with tenderness at the base of the fifth metatarsal.

Continue to: MRI/ultrasound in addition to plain films?
MRI/ultrasound in addition to plain films?
Use the Ottawa Ankle and Foot Rules to determine the need for foot radiographs in the acute setting.12 If indicated, imaging should include AP, lateral, and oblique views of the foot.5 Consider magnetic resonance imaging (MRI) if you suspect a stress fracture, which typically presents as an overuse injury in athletes.
Ultrasound may be effective for identifying metatarsal fractures, as well.13 Ultrasound can be used to visualize fractures of the long metatarsal bones and identify displacement, angulation, and step-offs. Although its use in the United States has been limited for this purpose, studies in other countries are showing that it yields results comparable to plain films in the emergency department setting for diagnosis and initial management of these fractures.13
Differential diagnosis
Multiple other diagnoses present similarly to metatarsal fractures including: ligamentous/tendon/soft tissue injuries, interdigital neuroma, sesamoid fractures, and Lisfranc ligament injury (which we'll discuss in a bit). Stress fractures of the metatarsal, most commonly seen in the second metatarsal, are insidious in nature and are common with repetitive movement such as that made by gymnasts, dancers, and track athletes.14 Metatarsalgia, which causes pain at the ball of the foot, is a condition that can stem from a myriad of causes including a low or high arch, biomechanics, and previous injury.
Treatment
Nondisplaced, minimally displaced (<3 mm), and minimally angulated (<10° dorsal/plantar angulation) fractures of any metatarsal shaft may be managed conservatively with a hard-soled shoe or walking boot with weight bearing as tolerated for 4 to 6 weeks.1 Most stress fractures (excluding fifth metatarsal stress fractures) may be treated similarly. Surgical referral is indicated for patients with any open fracture, first metatarsal fractures with displacement, central metatarsal fractures with >10° deformity, >3 mm of translation, multiple fractures, or fifth metatarsal stress fracture.1
Base of fifth metatarsal tuberosity avulsion fractures can be managed nonoperatively with protected weight bearing in a boot or cast for 2 weeks or hard sole shoe for 4 to 8 weeks if the fracture is at the proximal tubercle (see Zone I, FIGURE 2). Jones fractures (Zone II, FIGURE 2) or fractures of the proximal diaphysis (Zone III, FIGURE 2) of the fifth metatarsal may also be managed nonoperatively in patients who are not competitive athletes. This can be done with a non-weight bearing (NWB) short leg cast for 6 to 8 weeks at a minimum.4 If the patient is an athlete who wishes to resume competition, surgical referral is indicated, as the risk of nonunion is high with these fractures.15
Continue to: Stress fractures and stress reactions...
Stress fractures and stress reactions (early evidence of bone edema seen on MRI, indicating progression to stress fracture) of the proximal fifth metatarsal should be managed with strict activity modifications and a NWB short leg cast for 6 to 8 weeks, given the high risk of nonunion.
Midfoot fractures: The cuboid, cuneiforms, and navicular bone
Although fractures are less common in the midfoot, the midfoot serves an important role in weight bearing and stabilization. In addition, along with the metatarsal bones, the midfoot is critical to proper alignment and articulation.
Cuboid and cuneiform fractures
Cuboid fractures may occur with high-velocity trauma, foot inversion with external rotation of the tibia, a direct blow, or axial load on a plantar-flexed heel. Pain with weight bearing or with walking on toes is usually present. Cuneiform fractures are less common and rarely occur in isolation.6 Mechanisms of injury for cuneiform fractures include direct impact, axial loading on a dorsiflexed or plantar-flexed foot with rotational force, and severe rotation of the midfoot section in a fixed foot. Pain is usually localized to the dorsal or dorsomedial aspect of the foot.
With these 2 midfoot injuries, the exam should include palpation of the cuboid, navicular, and cuneiform bones and careful inspection of the Lisfranc joint, as this can be injured in midfoot fractures.7 Obtain AP, lateral, and oblique views of the foot,5 and strongly consider bilateral weight-bearing films to evaluate for tarsometatarsal (TMT) joint complex injuries (typically Lisfranc joint complex injuries), given their association with midfoot fractures1 (FIGURE 3).
If the fracture is at or near the TMT joint complex, obtain a CT scan or MRI regardless of plain film findings to evaluate the Lisfranc joint complex. Because the Lisfranc joint is particularly important in midfoot stability, untreated injuries can lead to impaired gait or chronic foot pain and deformity. Early identification and surgical referral for these injuries is crucial.
Continue to: Navicular fractures
Navicular fractures
Navicular fractures are typically caused by a twisting mechanism with forced plantar flexion or forced dorsiflexion of the midfoot. They present with severe pain over the dorsal or dorsomedial foot, particularly while bearing weight. Tenderness to palpation over the navicular bone generally warrants imaging studies to rule out fracture, as undiagnosed fractures can lead to severe long-term disability. Use Ottawa Ankle and Foot Rules12 in the acute setting to determine the need for radiographs. If imaging is indicated, obtain AP, lateral, and oblique views.
Tuberosity fractures may be seen on the AP view, while dorsal avulsions, talonavicular joint disruptions, and naviculo-cuneiform joint injuries are better seen on lateral views.16 Patients, particularly cross-country and track athletes, presenting with insidious onset of pain over the navicular bone should be evaluated for stress fracture using MRI, even in the presence of normal radiographs.
Differential diagnosis. Suspect Lisfranc joint complex injuries in any patient with mid-foot pain or fracture. The transverse arch of the foot is reliant upon the articulation of the second metatarsal with all 5 neighboring bones. The Lisfranc ligament is the strongest of 3 supporting ligaments to anchor the TMT joint complex. Other causes of mid-foot pain include soft tissue injury, contusion, and tendinopathy. In addition, other conditions that may cause pain in this area include cuboid syndrome, peroneal tendinopathy, Jones fracture, stress fracture, anterior calcaneal fracture, and sinus tarsi syndrome.
Treatment. Nondisplaced fractures of the cuboid or cuneiform may be treated with a short leg walking cast/boot for 6 weeks followed by the use of a shoe with a thin, rigid, longitudinal arch support for an additional 6 weeks.1 Fractures requiring referral for surgical evaluation include fractures that are open and fractures with vascular or neurological compromise. Also refer comminuted fractures and those that present with >2 mm step-off. Lastly, midfoot fractures that involve the Lisfranc joint should be immobilized and referred for orthopedic evaluation with instructions to the patient to avoid weight bearing until orthopedic evaluation.8
Avulsion fractures of the navicular bone may be managed nonoperatively with a short leg walking cast/boot if there is <20% involvement of the talonavicular surface. Simple nondisplaced body fractures may also be managed conservatively with immobilization and protected weight bearing for 6 to 8 weeks.15 Refer for surgical evaluation avulsion fractures that are intra-articular or dorsal involving 20% or more of the talonavicular surface and tuberosity fractures, given their risk of nonunion.9 All navicular body fractures that are not longitudinal in nature should also be referred for surgical evaluation. Navicular stress fractures that do not extend into the plantar cortex may be managed conservatively with a minimum of 6 weeks of a short leg cast and strict NWB with close follow-up.17
Continue to: Calcaneal fractures
Calcaneal fractures
Calcaneal fractures typically occur from severe axial load or fall from a height. Weight bearing is usually limited and secondary to significant pain. Tenderness to palpation over the calcaneus or with squeezing of the heel will produce pain on exam. Initial x-rays should include a lateral and axial view of the calcaneus. Additional imaging, including a CT scan, may be indicated for further evaluation to determine the extent of the fracture or to determine if a fracture is present despite normal x-rays.10
Acute compartment syndrome occurs in 10% of calcaneal fractures and must be considered in patients with calcaneal fractures from severe trauma.18 Tendon injuries of the ankle, hindfoot, and midfoot may present similarly but can be ruled out with clinical exam and appropriate imaging.
Treatment
Avulsion fractures that do not involve more than 25% of the calcaneocuboid joint and nondisplaced calcaneal fractures may be managed conservatively by instructing patients to wear a NWB short leg cast/boot for 4 to 6 weeks.1 Refer for surgical evaluation patients with calcaneal fracture fragments >1 cm, displacement >3 mm, open fractures, joint involvement >25%, and those whose symptoms fail to resolve with conservative management. Stress fractures can be managed conservatively with cessation of aggravating activities and immobilization in a walking boot until symptoms resolve, which typically takes 4 to 6 weeks.1
CORRESPONDENCE
Michael Seth Smith, MD, CAQSM, PharmD, 3450 Hull Road, Gainesville, FL 32611; [email protected]
1. Eiff MP, Hatch RL, et al. Fracture Management for Primary Care. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
2. Hatch RL, Rosenbaum Cl. Fracture care by family physicians. A review of 295 cases. J Fam Pract. 1994;38:238-244.
3. Bica D, Sprouse RA, Armen J. Diagnosis and management of common foot fractures. Am Fam Physician. 2016;93:183-191.
4. Hatch RL, Hacking S. Evaluation and management of toe fractures. Am Fam Physician. 2003;68:2413-2418.
5. Snider RK. Essentials of Musculoskeletal Care. 2nd ed. Rosemont, IL: American Orthopedic Surgeons; 2001.
6. Guler F, Baz AB, Turan A, et al. Isolated medial cuneiform fractures: report of two cases and review of the literature. Foot Ankle Spec. 2011;4:306-309.
7. Borrelli J, De S, Van Pelt M. Fracture of the cuboid. J Am Acad Orthop Surg. 2012;20:472.
8. Pinney SJ, Sangeorzan BJ. Fractures of the tarsal bones. Orthop Clin North Am. 2001:32:21-33.
9. Rosenbaum AJ, Uhl R, DiPreta JA. Acute fractures of the tarsal navicular. Orthopedics. 2014;37:541-546.
10. Sanders RW, Clare MP. Calcaneous fractures. In: Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:2064.
11. Singer G, Cichocki M, Schalamon J, et al. A study of metatarsal fractures in children. J Bone Joint Surg Am. 2008;90:772-776.
12. Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384-390.
13. Ekinci S, Polat O, Günalp M, et al. The accuracy of ultrasound evaluation in foot and ankle trauma. Am J Emerg Med. 2013;31:1551-1555.
14. Welck MJ, Hayes T, Pastides P, et al. Stress fractures of the foot and ankle. Injury. 2017;48:1722-1726.
15. Hatch RL, Alsobrook JA, Clugston JR. Diagnosis and management of metatarsal fractures. Am Fam Physician. 2007;76:817-826.
16. Schildhauer TA, Coulibaly MO, Hoffman MF. Fractures and dislocations of the midfoot and forefoot. In: Rockwood and Green’s Fractures in Adults. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:2690.
17. Mayer SW, Joyner PW, Almekinders LC, et al. Stress fractures of the foot and ankle in athletes. Sports Health. 2014;6:481-491.
18. Kalsi R, Dempsey A, Bunney EB. Compartment syndrome of the foot after calcaneal fracture. J Emerg Med. 2012;43:e101-106.
1. Eiff MP, Hatch RL, et al. Fracture Management for Primary Care. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
2. Hatch RL, Rosenbaum Cl. Fracture care by family physicians. A review of 295 cases. J Fam Pract. 1994;38:238-244.
3. Bica D, Sprouse RA, Armen J. Diagnosis and management of common foot fractures. Am Fam Physician. 2016;93:183-191.
4. Hatch RL, Hacking S. Evaluation and management of toe fractures. Am Fam Physician. 2003;68:2413-2418.
5. Snider RK. Essentials of Musculoskeletal Care. 2nd ed. Rosemont, IL: American Orthopedic Surgeons; 2001.
6. Guler F, Baz AB, Turan A, et al. Isolated medial cuneiform fractures: report of two cases and review of the literature. Foot Ankle Spec. 2011;4:306-309.
7. Borrelli J, De S, Van Pelt M. Fracture of the cuboid. J Am Acad Orthop Surg. 2012;20:472.
8. Pinney SJ, Sangeorzan BJ. Fractures of the tarsal bones. Orthop Clin North Am. 2001:32:21-33.
9. Rosenbaum AJ, Uhl R, DiPreta JA. Acute fractures of the tarsal navicular. Orthopedics. 2014;37:541-546.
10. Sanders RW, Clare MP. Calcaneous fractures. In: Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:2064.
11. Singer G, Cichocki M, Schalamon J, et al. A study of metatarsal fractures in children. J Bone Joint Surg Am. 2008;90:772-776.
12. Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384-390.
13. Ekinci S, Polat O, Günalp M, et al. The accuracy of ultrasound evaluation in foot and ankle trauma. Am J Emerg Med. 2013;31:1551-1555.
14. Welck MJ, Hayes T, Pastides P, et al. Stress fractures of the foot and ankle. Injury. 2017;48:1722-1726.
15. Hatch RL, Alsobrook JA, Clugston JR. Diagnosis and management of metatarsal fractures. Am Fam Physician. 2007;76:817-826.
16. Schildhauer TA, Coulibaly MO, Hoffman MF. Fractures and dislocations of the midfoot and forefoot. In: Rockwood and Green’s Fractures in Adults. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015:2690.
17. Mayer SW, Joyner PW, Almekinders LC, et al. Stress fractures of the foot and ankle in athletes. Sports Health. 2014;6:481-491.
18. Kalsi R, Dempsey A, Bunney EB. Compartment syndrome of the foot after calcaneal fracture. J Emerg Med. 2012;43:e101-106.
PRACTICE RECOMMENDATIONS
› Manage most fractures of the proximal fifth metatarsal metaphyseal-diaphyseal junction (Jones fracture) conservatively with appropriate treatment and close follow-up; refer for early surgical evaluation only those patients who are highly active and who are interested in a faster return to activity. B
› Use the Ottawa Ankle and Foot Rules to determine whether x-rays are needed in a patient with foot pain and a suspected fracture. A
› Start with weight-bearing x-rays and then consider computed tomography or magnetic resonance imaging for complete evaluation of suspected injury to the Lisfranc joint. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
