User login
What can we expect from nonoperative treatment options for shoulder pain?
- First-line treatment for shoulder pain and stage 1 impingement may include nonsteroidal anti-inflammatory drugs (NSAIDs) (B) or corticosteroid injection (A).
- Stage II or III Impingement (rotator cuff tears) are best treated initially with physical therapy (supervised or home exercise program) or corticosteroid injection.
- Steroid injections added to NSAID treatment probably confer no extra benefit.
- High pain levels during the day and associated neck pain may predict a longer recovery period.
Most shoulder pain responds best to NSAIDs or subacromial corticosteroid injections followed by a home exercise program or formal physical therapy exercises. Accumulating evidence is making it clearer what works and what doesn’t for specific diagnoses.
Time to healing varies greatly among persons with shoulder pain, and specific prognostic indicators may help you and your patients know what to expect.
Quick diagnostic review
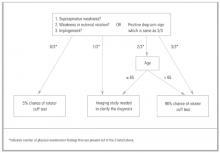
Consider the patient’s age, history of trauma, details of injury, and previous shoulder problems. Observe the patient’s general movements, assess range of motion, and use provocative testing to form a differential diagnosis ( Figure 1 ).
If the diagnosis is unclear, arrange for imaging studies ( Table 1 ). A more thorough review for diagnosing shoulder pain may be found in the article “Approach to the patient with shoulder pain” (J Fam Pract 2002; 7:605–611). The conditions causing shoulder pain (in order of frequency, as seen by primary care physicians) are subacromial impingement syndrome (SIS), adhesive capsulitis, acute bursitis, calcific tendinitis, glenohumeral arthrosis, biceps tendinitis, and labral tear.1,2
TABLE 1
Value of imaging tests for shoulder injuries
| Test | LOE | Sn | Sp | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial41 | 2b | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete41 | 1a | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall42-44 | 2b | 89–96 | 49–100 | 1.9–>25 | 0.08 | 58 | 94 |
| Impingement 42 | 2b | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears* 45,46 | 1b | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete41 | 1b | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete47 | 1b | 95 | — | — | — | — | — |
| Overall47 | 1b | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 80 | — | — | — | — | — |
| Complete47,4848 | 1b | 90–100 | 85 | 6.7 | >25 | — | — |
| Overall47 | 1b | 86 | 91–98 | 9.6–>25 | 0.14–0.15 | 96 | 73–93 |
| *MRI arthrography. | |||||||
| LOE, level of evidence (SORT); Sn, sensitivity; Sp, specificity; LR, likelihood ratio; PV, predictive value; MRI, magnetic resonance imaging; CT, computed tomography. | |||||||
FIGURE 1
Evaluating shoulder pain for possible rotator cuff tear
Subacromial impingement syndrome
This condition was first described by Neer, who estimated it leads to 95% of rotator cuff tears.3
Impingement occurs from repetitive overhead activities, acute trauma, or instability of the glenohumeral joint (subtle or overt). Current theory holds that degeneration of the rotator cuff tendons or inflammation of the subacromial bursa—caused by irritation against the coracoacromial arch—can progress to degeneration and a complete rotator cuff tear. So-called rotator cuff tendinitis is better described as a tendinopathy with mucoid degeneration of the tendon. SIS stage I involves edema and hemorrhage, as would be seen with rotator cuff tendinopathy or bursitis.
Progressive feedback loop of subacromial impingement syndrome. Acute bursitis involves the subacromial bursa and typically is secondary to subacromial impingement. As underlying tendinopathy, instability, or heterotrophic bone irritates the bursa, it will become inflamed and irritated. Inflammation exacerbates the impingement and that in turn causes worsening of the bursitis.
Stage II and III impingement syndrome. SIS stage II is a progression to fibrosis and partial tear of the rotator cuff. Stage III is a full-thickness tear of the rotator cuff. These stages of SIS are seen predominantly in patients over the age of 40 years, and they become more common with increasing age. The tear—partial or complete— usually occurs in the supraspinatus tendon. Tears of other rotator cuff muscles are less common.
Magnetic resonance imaging (MRI), with or without arthrography, is used in clinical practice and in research to diagnose rotator cuff tears. Growing evidence indicates that ultrasound is a less expensive and equally effective way to diagnose stage II or III impingement. In the United States, however, the option of ultrasound is limited by scarce availability and inadequate operator skill.
The subacromial injection test is useful in clinical practice. Local anesthetic is injected into the subacromial space. Persisting loss of strength despite pain relief is a positive sign of impairment of the rotator cuff.
MRI or ultrasound must be done in conjunction with history taking and physical examination. As the age of a person increases, the amount of asymptomatic rotator cuff tendon injury will also increase. The incidence of rotator cuff tears has been found to be between 50% to 60% in cadavers of deceased elderly. Thirty percent were found to be stage III impingement; 20% to 30% were partial stage II impingement.4
Adhesive capsulitis
Also known as frozen shoulder, adhesive capsulitis may begin with any inflammatory condition, but it is most commonly idiopathic. It characteristically progresses through 3 stages.
The hallmark of adhesive capsulitis is a progressive lack of range of motion with both passive and active movement.
The first stage involves progressive pain and decreased range of motion as the capsule scars.
The second stage involves maturation of capsule scaring, resulting in decreased pain and increased restriction of movement.
The third stage is resolution of the condition, leading to a gradual increase in range of motion.
Full range of motion may or may not return, and the time to resolution is typically 1 to 2 years. Adhesive capsulitis is most common in older persons, especially women in the fourth and fifth decades.5
Comparing nonoperative treatments
Nonoperative treatment modalities include protection, relative rest, and ice (PRI); anti-inflammatory medications; physical therapy (supervised or home exercise program); acupuncture; and steroid injection.
Operative treatments, depending on the particular disorder, include rotator cuff repair, subacromial decompression, capsular tightening, or manipulation under anesthesia.
The efficacy of nonoperative treatments for shoulder pain is not well known. Studies of treatment modalities have been numerous but generally of poor quality due to a lack of uniformity in how shoulder disorders are defined and in the variability of outcome measures used. Several recent systematic reviews have tried to identify which interventions are efficacious ( Table 2 ).6-11
Overall, NSAIDs and subacromial steroid injections are effective in the short-term treatment of shoulder pain.26-28 However, only nonselective NSAIDs have been studied. Evidence is insufficient to recommend use of cyclooxygenase-2 (COX-2) medications for shoulder pain.
Steroid injections may not confer extra benefit when added to NSAIDs, but they appear superior to NSAIDs in improving shoulder abduction. This is particularly true for the painful stiff shoulder, as seen with impingement or rotator cuff disease.26,28
Two recent randomized control trials showed corticosteroid injections to be superior to physical therapy for treatment of shoulder complaints.12,13
Shoulder instability may be treated nonoperatively at first with PRI, NSAIDs, and strengthening and proprioceptive exercises for the rotator cuff. If 3 to 6 months of nonoperative treatment fails, the patient should be referred for surgical evaluation, especially in cases of full-thickness rotator cuff tears.14
TABLE 2
Nonoperative treatment options for shoulder pain
| Treatment | Comment | SOR |
|---|---|---|
| NSAIDs |
| C |
| Physical therapy |
| B |
| Ultrasound |
| A |
| Steroid injection |
| B |
| Acupuncture |
| C |
| SOR, strength of recommendation (SORT); NSAIDs, nonsteroidal anti-inflammatory drugs. | ||
Treatment of specific shoulder disorders
Subacromial impingement syndrome stage I
A recommendation (SOR: B) can be made for the use of NSAIDs in the treatment of stage I impingement ( Table 3 ). This is based on level 2 evidence that NSAIDs are beneficial for rotator cuff tendinopathy and bicipital tendinitis, compared with placebo in a 1 to 2 week follow-up.15,17 No specific NSAID has proved better than another.18,19
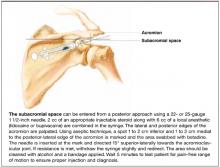
Steroid injection ( Figure 2 ) is beneficial for the acute treatment of SIS I reflected by improvement in pain (SOR: A).20-23 This is particularly evident during the first 1 to 2 weeks following injections.38 At 4 to 6 weeks, there appears to be no difference in the efficacy of steroid injection compared with NSAIDs,24,25 but they are both better than placebo.43
Physical therapy, specifically rotator cuff strengthening and range of motion, is as beneficial as surgery for SIS I at 6 month and 21/2-year follow-up, and both were better than placebo (SOR: B).26,27
TABLE 3
Treatments for SIS I impingement (rotator cuff tendinitis/tendinosis)
| Treatment | Comment | LOE |
|---|---|---|
| NSAIDs |
| 1c |
| NSAIDs vs steroid injection |
| 1a |
| Subacromial steroid injection |
| 1b |
| Surgery |
| 2a |
FIGURE 2
Steroid injection in the subacromial space
SIS stages II and III
There is very good evidence (SOR: B) regarding the efficacy of nonoperative treatment of SIS II and III, based on level 2 cohort studies that suggest nonoperative care leads to improvements in patient satisfaction, pain, and daily activities.28,29 Similar outcomes are reported for patients undergoing physical therapy alone.30,31 Weiss reported that corticosteroid injections for stage III/full-thickness rotator cuff tears resulted in an 86% improvement as measured by return to previous activities and less or no pain with motion ( Table 4 ).32
The most constant outcome measure was report of a reduction in pain. Younger patients or those with higher functional demands will likely consider surgical repair if nonoperative measures fail, particularly for full-thickness tears.
TABLE 4
Nonoperative treatments for SIS III (full-thickness rotator cuff tears)
| Treatment | Comment | SOR |
|---|---|---|
| Physical therapy |
| B |
| Subacromial injection |
| B |
| Multiple nonoperativetherapies |
| B |
Adhesive capsulitis
There is no consistent evidence that treatment of any one form reduces the pain or improves range of motion in frozen shoulders. Various treatments that have been tried include, though are not limited to, steroid injection, NSAIDs, and physical therapy.33-37 Studies on treatment efficacy are complicated by inherent discrepancy between patient and observer opinions of limitations in this condition, with objective range of motion findings often not being consistent with patient reported limitations.38
Indicators of quicker or slower recovery
Studies of prognosis following treatment have been difficult to assess due the heterogeneity of the underlying conditions and variability of treatments. A follow-up questionnaire in one instance found no difference between treatment groups. Complaints of pain or impaired mobility 2 to 3 years after treatment were similar among patients treated with steroid injection and physical therapy and with physical therapy alone.30 Overall, 76% of respondents were symptom free at 2 to 3 years.
Two prospective studies confirm that speed of recovery is slow, with complete recovery 23% at 1 month, 21% to 51% at 6 months, 59% at 1 year, and 69% at 18 months.39,40
Prognostic indicators of quicker recovery were preceding overuse or slight trauma and early presentation to the physician.58 Protracted recovery occurred more often with high pain levels during the day or associated neck pain.58 These results suggest that patients with subacromial impingement stage I respond better to nonoperative treatment than those patients with underlying degenerative changes or referred pain from the neck.
Finally, specialty surgical referral may be necessary in cases of failed nonoperative therapy or persistent diagnostic and therapeutic challenges.
Corresponding author
Thomas H. Trojian, MD, 99 Woodland Street, Hartford, CT 06105. E-mail: [email protected].
1. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-964.
2. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-642.
3. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
4. Dalton SE. The conservative management of rotator cuff disorders. Br J Rheumatol 1994;33:663-667.
5. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia, Pa: W.B. Saunders; 1994.
6. Green S, Buchbinder R, Glazier R, Forbes A. Interventions for shoulder pain (Cochrane Review). In: The Cochrane Library, Issue 1, 2001. Oxdord: Update Software.
7. Van der Hiejden GJ, Van der Windt DA, Kleijnen J, et al. Steroid injections for shoulder disorders: a systematic review of randomized clinical trials. Br J Gen Pract 1996;46:309-316.
8. Van der Windt DA, Van der Heijden GJ, Scholten RJ, et al. The efficacy of non-steroidal anti-inflammatory drugs (NSAIDs) for shoulder complaints. A systematic review. J Clin Epidemiol 1995;48:691-704.
9. Van der Heijden GJ, Van der Windt DA, De Winter AF. Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomized clinical trials. BMJ 1997;15:25-30.
10. Van der Windt DA, Van der Heijden GJ, Van den Berg GJ, et al. Ultrasound therapy for musculoskeletal disorders: a systematic review. Pain 1999;81:257-271.
11. Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain 2000;86:119-132.
12. Winters JC, Sobel JS, Groenier KH, et al. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomized, single blind study. BMJ 1997;314:1320-1325.
13. Van der Windt DA, Koes BW, Deville W, et al. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomized trial. BMJ 1998;317:1292-1296.
14. Mantone JK, Burkhead WZ, Noonan J. Nonoperative treatment of rotator cuff tears. Orthop Clin North Am 2000;31:295-311.
15. Lopez JM. Treatment of acute tendinitis and bursitis with fentiazac. A double blind comparison with placebo. Clin Ther 1982;5:79-84.
16. Zuinen C. Diclofenac/misprostol vs diclofenac/placebo in treating acute episodes of tendinitis/bursitis of the shoulder. Drugs 1993;45 Suppl 1:17-23.
17. Ginsberg F, Famaey JP. A double-blind comparison of slow-release and standard tablet formulations of fentiazac in the treatment of patients with tendinitis and bursitis. Curr Med Res Opin 1985;9:42-448.
18. Wober W. Comparative efficacy and safety of nimesulide and diclofenac in patients with acute shoulder, and a meta-analysis of controlled studies with nimesulide. Rheum 1999;38(Suppl 1):33-38.
19. Wober W, Rahlfs VW, Buchl N, et al. Comparative efficacy and safety of the non-steroidal anti-inflammatory drugs nimesulide and diclofenac in patients with acute subdeltoid bursitis and bicipital tendinitis. Int J Clin Pract 1998;52:169-175.
20. Valtonen E. Double acting betamethasone (celestone chronodose) in the treatment of supraspinatus tendinitis: A comparison of subacromial and gluteal single injections with placebo. J Int Men Res 1978;6:463-467.
21. Blair B, Rokito A, Cuomo F, Jarolem K, Zuckerman J. Efficacy of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am 1996;78:1685-1689.
22. Withrington R, Girgis F, Seifert M. A placebo-controlled trial of steroid injections in the treatment of supraspinatus tendinitis. Scand J Rheumatol 1985M;14:76-78.
23. Vecchio PC, Hazleman BL, King RH. A double-blind trial comparing subacromial methylprednisolone and ligno-caine in acute rotator cuff tendinitis. Br J Rheumatol 1993;32:743-745.
24. White R, Paull D, Fleming K. Rotator cuff tendinitis: comparison of subacromial injection of a long acting corticosteroid vs oral indomethacin therapy. J Rheumatol 1986;13:608-613.
25. Adebajo A, Nash P, Hazleman B. A Prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50mg TDS in patients with rotator cuff tendinitis. J Rheumatol 1990;17:1207-1210.
26. Brox JI, Staff PH, Ljunggren AE, Revik JI. Arthroscopic Surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ 1993;307:899-903
27. Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prosprective, randomized, controlled study in 125 patients with a 2 1/2 year follow up. J Shoulder Elbow Surg 1999;8:102-111.
28. Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop 1993;294:103-110.
29. Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop 1992;275:165-173.
30. Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop 1995;321:178-188.
31. Goldberg BA, Nowinski RJ, Matsen FA. Outcome of non-operative management of full thickness rotator cuff tears. Clin Orthop 2001;382:99-107.
32. Weiss JJ. Intra-articular steroids in the treatment of rota-tor cuff tear: reappraisal by arthrography. Arch Phys Med Rehabil 1981;62:555-557.
33. De Jong BA, Dahmen R, Hogeweg JA, Marti RK. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehab 1998;12:211-215.
34. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clonical study with an evaluation of three treatment regimens. Ann Rheum Dis 1984;43:353-360.
35. Thumb N, Kolarz G, Scherak O, Mayrhofer F. The efficacy and safety of Fentiazac and Diclofenac sodium in peri-arthritis of the shoulder: a multi-center, double-blind comparison. J Int Med Res 1987;15:327-334.
36. Rhind V, Downie WW, Bird HA, Wright V, Engler C. Naproxen and indomethacin in periarthritis of the shoulder. Rheumatol Rehabil 1982;21:51-53.
37. Lee PN, Lee M, Haq AM, Longton EB, Wright V. Periarthritis of the shoulder. Ann Rheum Dis 1974;33:116-119.
38. Hazleman BL. The painful stiff shoulder. Rheumatol Rehabil 1972;11:413-421.
39. Croft P, Pope D, Silman A. The clinical course of shoulder pain: prospective cohort study in primary care. BMJ 1996;313:601-602.
40. Van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996;46:519-523.
41. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
42. Burk DL, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. Am J Roentgenol 1989;153:87-92.
43. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-45.
44. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-139.
45. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-498.
46. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with en-enhanced MR imaging of the shoulder. Radiology 1996;200:519-524.
47. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator cuff tear. Findings at ultrasound, double contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-394.
48. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
49. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-146.
- First-line treatment for shoulder pain and stage 1 impingement may include nonsteroidal anti-inflammatory drugs (NSAIDs) (B) or corticosteroid injection (A).
- Stage II or III Impingement (rotator cuff tears) are best treated initially with physical therapy (supervised or home exercise program) or corticosteroid injection.
- Steroid injections added to NSAID treatment probably confer no extra benefit.
- High pain levels during the day and associated neck pain may predict a longer recovery period.
Most shoulder pain responds best to NSAIDs or subacromial corticosteroid injections followed by a home exercise program or formal physical therapy exercises. Accumulating evidence is making it clearer what works and what doesn’t for specific diagnoses.
Time to healing varies greatly among persons with shoulder pain, and specific prognostic indicators may help you and your patients know what to expect.
Quick diagnostic review
Consider the patient’s age, history of trauma, details of injury, and previous shoulder problems. Observe the patient’s general movements, assess range of motion, and use provocative testing to form a differential diagnosis ( Figure 1 ).
If the diagnosis is unclear, arrange for imaging studies ( Table 1 ). A more thorough review for diagnosing shoulder pain may be found in the article “Approach to the patient with shoulder pain” (J Fam Pract 2002; 7:605–611). The conditions causing shoulder pain (in order of frequency, as seen by primary care physicians) are subacromial impingement syndrome (SIS), adhesive capsulitis, acute bursitis, calcific tendinitis, glenohumeral arthrosis, biceps tendinitis, and labral tear.1,2
TABLE 1
Value of imaging tests for shoulder injuries
| Test | LOE | Sn | Sp | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial41 | 2b | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete41 | 1a | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall42-44 | 2b | 89–96 | 49–100 | 1.9–>25 | 0.08 | 58 | 94 |
| Impingement 42 | 2b | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears* 45,46 | 1b | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete41 | 1b | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete47 | 1b | 95 | — | — | — | — | — |
| Overall47 | 1b | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 80 | — | — | — | — | — |
| Complete47,4848 | 1b | 90–100 | 85 | 6.7 | >25 | — | — |
| Overall47 | 1b | 86 | 91–98 | 9.6–>25 | 0.14–0.15 | 96 | 73–93 |
| *MRI arthrography. | |||||||
| LOE, level of evidence (SORT); Sn, sensitivity; Sp, specificity; LR, likelihood ratio; PV, predictive value; MRI, magnetic resonance imaging; CT, computed tomography. | |||||||
FIGURE 1
Evaluating shoulder pain for possible rotator cuff tear
Subacromial impingement syndrome
This condition was first described by Neer, who estimated it leads to 95% of rotator cuff tears.3
Impingement occurs from repetitive overhead activities, acute trauma, or instability of the glenohumeral joint (subtle or overt). Current theory holds that degeneration of the rotator cuff tendons or inflammation of the subacromial bursa—caused by irritation against the coracoacromial arch—can progress to degeneration and a complete rotator cuff tear. So-called rotator cuff tendinitis is better described as a tendinopathy with mucoid degeneration of the tendon. SIS stage I involves edema and hemorrhage, as would be seen with rotator cuff tendinopathy or bursitis.
Progressive feedback loop of subacromial impingement syndrome. Acute bursitis involves the subacromial bursa and typically is secondary to subacromial impingement. As underlying tendinopathy, instability, or heterotrophic bone irritates the bursa, it will become inflamed and irritated. Inflammation exacerbates the impingement and that in turn causes worsening of the bursitis.
Stage II and III impingement syndrome. SIS stage II is a progression to fibrosis and partial tear of the rotator cuff. Stage III is a full-thickness tear of the rotator cuff. These stages of SIS are seen predominantly in patients over the age of 40 years, and they become more common with increasing age. The tear—partial or complete— usually occurs in the supraspinatus tendon. Tears of other rotator cuff muscles are less common.
Magnetic resonance imaging (MRI), with or without arthrography, is used in clinical practice and in research to diagnose rotator cuff tears. Growing evidence indicates that ultrasound is a less expensive and equally effective way to diagnose stage II or III impingement. In the United States, however, the option of ultrasound is limited by scarce availability and inadequate operator skill.
The subacromial injection test is useful in clinical practice. Local anesthetic is injected into the subacromial space. Persisting loss of strength despite pain relief is a positive sign of impairment of the rotator cuff.
MRI or ultrasound must be done in conjunction with history taking and physical examination. As the age of a person increases, the amount of asymptomatic rotator cuff tendon injury will also increase. The incidence of rotator cuff tears has been found to be between 50% to 60% in cadavers of deceased elderly. Thirty percent were found to be stage III impingement; 20% to 30% were partial stage II impingement.4
Adhesive capsulitis
Also known as frozen shoulder, adhesive capsulitis may begin with any inflammatory condition, but it is most commonly idiopathic. It characteristically progresses through 3 stages.
The hallmark of adhesive capsulitis is a progressive lack of range of motion with both passive and active movement.
The first stage involves progressive pain and decreased range of motion as the capsule scars.
The second stage involves maturation of capsule scaring, resulting in decreased pain and increased restriction of movement.
The third stage is resolution of the condition, leading to a gradual increase in range of motion.
Full range of motion may or may not return, and the time to resolution is typically 1 to 2 years. Adhesive capsulitis is most common in older persons, especially women in the fourth and fifth decades.5
Comparing nonoperative treatments
Nonoperative treatment modalities include protection, relative rest, and ice (PRI); anti-inflammatory medications; physical therapy (supervised or home exercise program); acupuncture; and steroid injection.
Operative treatments, depending on the particular disorder, include rotator cuff repair, subacromial decompression, capsular tightening, or manipulation under anesthesia.
The efficacy of nonoperative treatments for shoulder pain is not well known. Studies of treatment modalities have been numerous but generally of poor quality due to a lack of uniformity in how shoulder disorders are defined and in the variability of outcome measures used. Several recent systematic reviews have tried to identify which interventions are efficacious ( Table 2 ).6-11
Overall, NSAIDs and subacromial steroid injections are effective in the short-term treatment of shoulder pain.26-28 However, only nonselective NSAIDs have been studied. Evidence is insufficient to recommend use of cyclooxygenase-2 (COX-2) medications for shoulder pain.
Steroid injections may not confer extra benefit when added to NSAIDs, but they appear superior to NSAIDs in improving shoulder abduction. This is particularly true for the painful stiff shoulder, as seen with impingement or rotator cuff disease.26,28
Two recent randomized control trials showed corticosteroid injections to be superior to physical therapy for treatment of shoulder complaints.12,13
Shoulder instability may be treated nonoperatively at first with PRI, NSAIDs, and strengthening and proprioceptive exercises for the rotator cuff. If 3 to 6 months of nonoperative treatment fails, the patient should be referred for surgical evaluation, especially in cases of full-thickness rotator cuff tears.14
TABLE 2
Nonoperative treatment options for shoulder pain
| Treatment | Comment | SOR |
|---|---|---|
| NSAIDs |
| C |
| Physical therapy |
| B |
| Ultrasound |
| A |
| Steroid injection |
| B |
| Acupuncture |
| C |
| SOR, strength of recommendation (SORT); NSAIDs, nonsteroidal anti-inflammatory drugs. | ||
Treatment of specific shoulder disorders
Subacromial impingement syndrome stage I
A recommendation (SOR: B) can be made for the use of NSAIDs in the treatment of stage I impingement ( Table 3 ). This is based on level 2 evidence that NSAIDs are beneficial for rotator cuff tendinopathy and bicipital tendinitis, compared with placebo in a 1 to 2 week follow-up.15,17 No specific NSAID has proved better than another.18,19
Steroid injection ( Figure 2 ) is beneficial for the acute treatment of SIS I reflected by improvement in pain (SOR: A).20-23 This is particularly evident during the first 1 to 2 weeks following injections.38 At 4 to 6 weeks, there appears to be no difference in the efficacy of steroid injection compared with NSAIDs,24,25 but they are both better than placebo.43
Physical therapy, specifically rotator cuff strengthening and range of motion, is as beneficial as surgery for SIS I at 6 month and 21/2-year follow-up, and both were better than placebo (SOR: B).26,27
TABLE 3
Treatments for SIS I impingement (rotator cuff tendinitis/tendinosis)
| Treatment | Comment | LOE |
|---|---|---|
| NSAIDs |
| 1c |
| NSAIDs vs steroid injection |
| 1a |
| Subacromial steroid injection |
| 1b |
| Surgery |
| 2a |
FIGURE 2
Steroid injection in the subacromial space
SIS stages II and III
There is very good evidence (SOR: B) regarding the efficacy of nonoperative treatment of SIS II and III, based on level 2 cohort studies that suggest nonoperative care leads to improvements in patient satisfaction, pain, and daily activities.28,29 Similar outcomes are reported for patients undergoing physical therapy alone.30,31 Weiss reported that corticosteroid injections for stage III/full-thickness rotator cuff tears resulted in an 86% improvement as measured by return to previous activities and less or no pain with motion ( Table 4 ).32
The most constant outcome measure was report of a reduction in pain. Younger patients or those with higher functional demands will likely consider surgical repair if nonoperative measures fail, particularly for full-thickness tears.
TABLE 4
Nonoperative treatments for SIS III (full-thickness rotator cuff tears)
| Treatment | Comment | SOR |
|---|---|---|
| Physical therapy |
| B |
| Subacromial injection |
| B |
| Multiple nonoperativetherapies |
| B |
Adhesive capsulitis
There is no consistent evidence that treatment of any one form reduces the pain or improves range of motion in frozen shoulders. Various treatments that have been tried include, though are not limited to, steroid injection, NSAIDs, and physical therapy.33-37 Studies on treatment efficacy are complicated by inherent discrepancy between patient and observer opinions of limitations in this condition, with objective range of motion findings often not being consistent with patient reported limitations.38
Indicators of quicker or slower recovery
Studies of prognosis following treatment have been difficult to assess due the heterogeneity of the underlying conditions and variability of treatments. A follow-up questionnaire in one instance found no difference between treatment groups. Complaints of pain or impaired mobility 2 to 3 years after treatment were similar among patients treated with steroid injection and physical therapy and with physical therapy alone.30 Overall, 76% of respondents were symptom free at 2 to 3 years.
Two prospective studies confirm that speed of recovery is slow, with complete recovery 23% at 1 month, 21% to 51% at 6 months, 59% at 1 year, and 69% at 18 months.39,40
Prognostic indicators of quicker recovery were preceding overuse or slight trauma and early presentation to the physician.58 Protracted recovery occurred more often with high pain levels during the day or associated neck pain.58 These results suggest that patients with subacromial impingement stage I respond better to nonoperative treatment than those patients with underlying degenerative changes or referred pain from the neck.
Finally, specialty surgical referral may be necessary in cases of failed nonoperative therapy or persistent diagnostic and therapeutic challenges.
Corresponding author
Thomas H. Trojian, MD, 99 Woodland Street, Hartford, CT 06105. E-mail: [email protected].
- First-line treatment for shoulder pain and stage 1 impingement may include nonsteroidal anti-inflammatory drugs (NSAIDs) (B) or corticosteroid injection (A).
- Stage II or III Impingement (rotator cuff tears) are best treated initially with physical therapy (supervised or home exercise program) or corticosteroid injection.
- Steroid injections added to NSAID treatment probably confer no extra benefit.
- High pain levels during the day and associated neck pain may predict a longer recovery period.
Most shoulder pain responds best to NSAIDs or subacromial corticosteroid injections followed by a home exercise program or formal physical therapy exercises. Accumulating evidence is making it clearer what works and what doesn’t for specific diagnoses.
Time to healing varies greatly among persons with shoulder pain, and specific prognostic indicators may help you and your patients know what to expect.
Quick diagnostic review
Consider the patient’s age, history of trauma, details of injury, and previous shoulder problems. Observe the patient’s general movements, assess range of motion, and use provocative testing to form a differential diagnosis ( Figure 1 ).
If the diagnosis is unclear, arrange for imaging studies ( Table 1 ). A more thorough review for diagnosing shoulder pain may be found in the article “Approach to the patient with shoulder pain” (J Fam Pract 2002; 7:605–611). The conditions causing shoulder pain (in order of frequency, as seen by primary care physicians) are subacromial impingement syndrome (SIS), adhesive capsulitis, acute bursitis, calcific tendinitis, glenohumeral arthrosis, biceps tendinitis, and labral tear.1,2
TABLE 1
Value of imaging tests for shoulder injuries
| Test | LOE | Sn | Sp | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial41 | 2b | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete41 | 1a | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall42-44 | 2b | 89–96 | 49–100 | 1.9–>25 | 0.08 | 58 | 94 |
| Impingement 42 | 2b | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears* 45,46 | 1b | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete41 | 1b | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 70 | — | — | — | — | — |
| Complete47 | 1b | 95 | — | — | — | — | — |
| Overall47 | 1b | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial47 | 1b | 80 | — | — | — | — | — |
| Complete47,4848 | 1b | 90–100 | 85 | 6.7 | >25 | — | — |
| Overall47 | 1b | 86 | 91–98 | 9.6–>25 | 0.14–0.15 | 96 | 73–93 |
| *MRI arthrography. | |||||||
| LOE, level of evidence (SORT); Sn, sensitivity; Sp, specificity; LR, likelihood ratio; PV, predictive value; MRI, magnetic resonance imaging; CT, computed tomography. | |||||||
FIGURE 1
Evaluating shoulder pain for possible rotator cuff tear
Subacromial impingement syndrome
This condition was first described by Neer, who estimated it leads to 95% of rotator cuff tears.3
Impingement occurs from repetitive overhead activities, acute trauma, or instability of the glenohumeral joint (subtle or overt). Current theory holds that degeneration of the rotator cuff tendons or inflammation of the subacromial bursa—caused by irritation against the coracoacromial arch—can progress to degeneration and a complete rotator cuff tear. So-called rotator cuff tendinitis is better described as a tendinopathy with mucoid degeneration of the tendon. SIS stage I involves edema and hemorrhage, as would be seen with rotator cuff tendinopathy or bursitis.
Progressive feedback loop of subacromial impingement syndrome. Acute bursitis involves the subacromial bursa and typically is secondary to subacromial impingement. As underlying tendinopathy, instability, or heterotrophic bone irritates the bursa, it will become inflamed and irritated. Inflammation exacerbates the impingement and that in turn causes worsening of the bursitis.
Stage II and III impingement syndrome. SIS stage II is a progression to fibrosis and partial tear of the rotator cuff. Stage III is a full-thickness tear of the rotator cuff. These stages of SIS are seen predominantly in patients over the age of 40 years, and they become more common with increasing age. The tear—partial or complete— usually occurs in the supraspinatus tendon. Tears of other rotator cuff muscles are less common.
Magnetic resonance imaging (MRI), with or without arthrography, is used in clinical practice and in research to diagnose rotator cuff tears. Growing evidence indicates that ultrasound is a less expensive and equally effective way to diagnose stage II or III impingement. In the United States, however, the option of ultrasound is limited by scarce availability and inadequate operator skill.
The subacromial injection test is useful in clinical practice. Local anesthetic is injected into the subacromial space. Persisting loss of strength despite pain relief is a positive sign of impairment of the rotator cuff.
MRI or ultrasound must be done in conjunction with history taking and physical examination. As the age of a person increases, the amount of asymptomatic rotator cuff tendon injury will also increase. The incidence of rotator cuff tears has been found to be between 50% to 60% in cadavers of deceased elderly. Thirty percent were found to be stage III impingement; 20% to 30% were partial stage II impingement.4
Adhesive capsulitis
Also known as frozen shoulder, adhesive capsulitis may begin with any inflammatory condition, but it is most commonly idiopathic. It characteristically progresses through 3 stages.
The hallmark of adhesive capsulitis is a progressive lack of range of motion with both passive and active movement.
The first stage involves progressive pain and decreased range of motion as the capsule scars.
The second stage involves maturation of capsule scaring, resulting in decreased pain and increased restriction of movement.
The third stage is resolution of the condition, leading to a gradual increase in range of motion.
Full range of motion may or may not return, and the time to resolution is typically 1 to 2 years. Adhesive capsulitis is most common in older persons, especially women in the fourth and fifth decades.5
Comparing nonoperative treatments
Nonoperative treatment modalities include protection, relative rest, and ice (PRI); anti-inflammatory medications; physical therapy (supervised or home exercise program); acupuncture; and steroid injection.
Operative treatments, depending on the particular disorder, include rotator cuff repair, subacromial decompression, capsular tightening, or manipulation under anesthesia.
The efficacy of nonoperative treatments for shoulder pain is not well known. Studies of treatment modalities have been numerous but generally of poor quality due to a lack of uniformity in how shoulder disorders are defined and in the variability of outcome measures used. Several recent systematic reviews have tried to identify which interventions are efficacious ( Table 2 ).6-11
Overall, NSAIDs and subacromial steroid injections are effective in the short-term treatment of shoulder pain.26-28 However, only nonselective NSAIDs have been studied. Evidence is insufficient to recommend use of cyclooxygenase-2 (COX-2) medications for shoulder pain.
Steroid injections may not confer extra benefit when added to NSAIDs, but they appear superior to NSAIDs in improving shoulder abduction. This is particularly true for the painful stiff shoulder, as seen with impingement or rotator cuff disease.26,28
Two recent randomized control trials showed corticosteroid injections to be superior to physical therapy for treatment of shoulder complaints.12,13
Shoulder instability may be treated nonoperatively at first with PRI, NSAIDs, and strengthening and proprioceptive exercises for the rotator cuff. If 3 to 6 months of nonoperative treatment fails, the patient should be referred for surgical evaluation, especially in cases of full-thickness rotator cuff tears.14
TABLE 2
Nonoperative treatment options for shoulder pain
| Treatment | Comment | SOR |
|---|---|---|
| NSAIDs |
| C |
| Physical therapy |
| B |
| Ultrasound |
| A |
| Steroid injection |
| B |
| Acupuncture |
| C |
| SOR, strength of recommendation (SORT); NSAIDs, nonsteroidal anti-inflammatory drugs. | ||
Treatment of specific shoulder disorders
Subacromial impingement syndrome stage I
A recommendation (SOR: B) can be made for the use of NSAIDs in the treatment of stage I impingement ( Table 3 ). This is based on level 2 evidence that NSAIDs are beneficial for rotator cuff tendinopathy and bicipital tendinitis, compared with placebo in a 1 to 2 week follow-up.15,17 No specific NSAID has proved better than another.18,19
Steroid injection ( Figure 2 ) is beneficial for the acute treatment of SIS I reflected by improvement in pain (SOR: A).20-23 This is particularly evident during the first 1 to 2 weeks following injections.38 At 4 to 6 weeks, there appears to be no difference in the efficacy of steroid injection compared with NSAIDs,24,25 but they are both better than placebo.43
Physical therapy, specifically rotator cuff strengthening and range of motion, is as beneficial as surgery for SIS I at 6 month and 21/2-year follow-up, and both were better than placebo (SOR: B).26,27
TABLE 3
Treatments for SIS I impingement (rotator cuff tendinitis/tendinosis)
| Treatment | Comment | LOE |
|---|---|---|
| NSAIDs |
| 1c |
| NSAIDs vs steroid injection |
| 1a |
| Subacromial steroid injection |
| 1b |
| Surgery |
| 2a |
FIGURE 2
Steroid injection in the subacromial space
SIS stages II and III
There is very good evidence (SOR: B) regarding the efficacy of nonoperative treatment of SIS II and III, based on level 2 cohort studies that suggest nonoperative care leads to improvements in patient satisfaction, pain, and daily activities.28,29 Similar outcomes are reported for patients undergoing physical therapy alone.30,31 Weiss reported that corticosteroid injections for stage III/full-thickness rotator cuff tears resulted in an 86% improvement as measured by return to previous activities and less or no pain with motion ( Table 4 ).32
The most constant outcome measure was report of a reduction in pain. Younger patients or those with higher functional demands will likely consider surgical repair if nonoperative measures fail, particularly for full-thickness tears.
TABLE 4
Nonoperative treatments for SIS III (full-thickness rotator cuff tears)
| Treatment | Comment | SOR |
|---|---|---|
| Physical therapy |
| B |
| Subacromial injection |
| B |
| Multiple nonoperativetherapies |
| B |
Adhesive capsulitis
There is no consistent evidence that treatment of any one form reduces the pain or improves range of motion in frozen shoulders. Various treatments that have been tried include, though are not limited to, steroid injection, NSAIDs, and physical therapy.33-37 Studies on treatment efficacy are complicated by inherent discrepancy between patient and observer opinions of limitations in this condition, with objective range of motion findings often not being consistent with patient reported limitations.38
Indicators of quicker or slower recovery
Studies of prognosis following treatment have been difficult to assess due the heterogeneity of the underlying conditions and variability of treatments. A follow-up questionnaire in one instance found no difference between treatment groups. Complaints of pain or impaired mobility 2 to 3 years after treatment were similar among patients treated with steroid injection and physical therapy and with physical therapy alone.30 Overall, 76% of respondents were symptom free at 2 to 3 years.
Two prospective studies confirm that speed of recovery is slow, with complete recovery 23% at 1 month, 21% to 51% at 6 months, 59% at 1 year, and 69% at 18 months.39,40
Prognostic indicators of quicker recovery were preceding overuse or slight trauma and early presentation to the physician.58 Protracted recovery occurred more often with high pain levels during the day or associated neck pain.58 These results suggest that patients with subacromial impingement stage I respond better to nonoperative treatment than those patients with underlying degenerative changes or referred pain from the neck.
Finally, specialty surgical referral may be necessary in cases of failed nonoperative therapy or persistent diagnostic and therapeutic challenges.
Corresponding author
Thomas H. Trojian, MD, 99 Woodland Street, Hartford, CT 06105. E-mail: [email protected].
1. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-964.
2. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-642.
3. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
4. Dalton SE. The conservative management of rotator cuff disorders. Br J Rheumatol 1994;33:663-667.
5. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia, Pa: W.B. Saunders; 1994.
6. Green S, Buchbinder R, Glazier R, Forbes A. Interventions for shoulder pain (Cochrane Review). In: The Cochrane Library, Issue 1, 2001. Oxdord: Update Software.
7. Van der Hiejden GJ, Van der Windt DA, Kleijnen J, et al. Steroid injections for shoulder disorders: a systematic review of randomized clinical trials. Br J Gen Pract 1996;46:309-316.
8. Van der Windt DA, Van der Heijden GJ, Scholten RJ, et al. The efficacy of non-steroidal anti-inflammatory drugs (NSAIDs) for shoulder complaints. A systematic review. J Clin Epidemiol 1995;48:691-704.
9. Van der Heijden GJ, Van der Windt DA, De Winter AF. Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomized clinical trials. BMJ 1997;15:25-30.
10. Van der Windt DA, Van der Heijden GJ, Van den Berg GJ, et al. Ultrasound therapy for musculoskeletal disorders: a systematic review. Pain 1999;81:257-271.
11. Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain 2000;86:119-132.
12. Winters JC, Sobel JS, Groenier KH, et al. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomized, single blind study. BMJ 1997;314:1320-1325.
13. Van der Windt DA, Koes BW, Deville W, et al. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomized trial. BMJ 1998;317:1292-1296.
14. Mantone JK, Burkhead WZ, Noonan J. Nonoperative treatment of rotator cuff tears. Orthop Clin North Am 2000;31:295-311.
15. Lopez JM. Treatment of acute tendinitis and bursitis with fentiazac. A double blind comparison with placebo. Clin Ther 1982;5:79-84.
16. Zuinen C. Diclofenac/misprostol vs diclofenac/placebo in treating acute episodes of tendinitis/bursitis of the shoulder. Drugs 1993;45 Suppl 1:17-23.
17. Ginsberg F, Famaey JP. A double-blind comparison of slow-release and standard tablet formulations of fentiazac in the treatment of patients with tendinitis and bursitis. Curr Med Res Opin 1985;9:42-448.
18. Wober W. Comparative efficacy and safety of nimesulide and diclofenac in patients with acute shoulder, and a meta-analysis of controlled studies with nimesulide. Rheum 1999;38(Suppl 1):33-38.
19. Wober W, Rahlfs VW, Buchl N, et al. Comparative efficacy and safety of the non-steroidal anti-inflammatory drugs nimesulide and diclofenac in patients with acute subdeltoid bursitis and bicipital tendinitis. Int J Clin Pract 1998;52:169-175.
20. Valtonen E. Double acting betamethasone (celestone chronodose) in the treatment of supraspinatus tendinitis: A comparison of subacromial and gluteal single injections with placebo. J Int Men Res 1978;6:463-467.
21. Blair B, Rokito A, Cuomo F, Jarolem K, Zuckerman J. Efficacy of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am 1996;78:1685-1689.
22. Withrington R, Girgis F, Seifert M. A placebo-controlled trial of steroid injections in the treatment of supraspinatus tendinitis. Scand J Rheumatol 1985M;14:76-78.
23. Vecchio PC, Hazleman BL, King RH. A double-blind trial comparing subacromial methylprednisolone and ligno-caine in acute rotator cuff tendinitis. Br J Rheumatol 1993;32:743-745.
24. White R, Paull D, Fleming K. Rotator cuff tendinitis: comparison of subacromial injection of a long acting corticosteroid vs oral indomethacin therapy. J Rheumatol 1986;13:608-613.
25. Adebajo A, Nash P, Hazleman B. A Prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50mg TDS in patients with rotator cuff tendinitis. J Rheumatol 1990;17:1207-1210.
26. Brox JI, Staff PH, Ljunggren AE, Revik JI. Arthroscopic Surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ 1993;307:899-903
27. Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prosprective, randomized, controlled study in 125 patients with a 2 1/2 year follow up. J Shoulder Elbow Surg 1999;8:102-111.
28. Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop 1993;294:103-110.
29. Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop 1992;275:165-173.
30. Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop 1995;321:178-188.
31. Goldberg BA, Nowinski RJ, Matsen FA. Outcome of non-operative management of full thickness rotator cuff tears. Clin Orthop 2001;382:99-107.
32. Weiss JJ. Intra-articular steroids in the treatment of rota-tor cuff tear: reappraisal by arthrography. Arch Phys Med Rehabil 1981;62:555-557.
33. De Jong BA, Dahmen R, Hogeweg JA, Marti RK. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehab 1998;12:211-215.
34. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clonical study with an evaluation of three treatment regimens. Ann Rheum Dis 1984;43:353-360.
35. Thumb N, Kolarz G, Scherak O, Mayrhofer F. The efficacy and safety of Fentiazac and Diclofenac sodium in peri-arthritis of the shoulder: a multi-center, double-blind comparison. J Int Med Res 1987;15:327-334.
36. Rhind V, Downie WW, Bird HA, Wright V, Engler C. Naproxen and indomethacin in periarthritis of the shoulder. Rheumatol Rehabil 1982;21:51-53.
37. Lee PN, Lee M, Haq AM, Longton EB, Wright V. Periarthritis of the shoulder. Ann Rheum Dis 1974;33:116-119.
38. Hazleman BL. The painful stiff shoulder. Rheumatol Rehabil 1972;11:413-421.
39. Croft P, Pope D, Silman A. The clinical course of shoulder pain: prospective cohort study in primary care. BMJ 1996;313:601-602.
40. Van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996;46:519-523.
41. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
42. Burk DL, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. Am J Roentgenol 1989;153:87-92.
43. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-45.
44. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-139.
45. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-498.
46. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with en-enhanced MR imaging of the shoulder. Radiology 1996;200:519-524.
47. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator cuff tear. Findings at ultrasound, double contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-394.
48. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
49. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-146.
1. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-964.
2. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-642.
3. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
4. Dalton SE. The conservative management of rotator cuff disorders. Br J Rheumatol 1994;33:663-667.
5. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia, Pa: W.B. Saunders; 1994.
6. Green S, Buchbinder R, Glazier R, Forbes A. Interventions for shoulder pain (Cochrane Review). In: The Cochrane Library, Issue 1, 2001. Oxdord: Update Software.
7. Van der Hiejden GJ, Van der Windt DA, Kleijnen J, et al. Steroid injections for shoulder disorders: a systematic review of randomized clinical trials. Br J Gen Pract 1996;46:309-316.
8. Van der Windt DA, Van der Heijden GJ, Scholten RJ, et al. The efficacy of non-steroidal anti-inflammatory drugs (NSAIDs) for shoulder complaints. A systematic review. J Clin Epidemiol 1995;48:691-704.
9. Van der Heijden GJ, Van der Windt DA, De Winter AF. Physiotherapy for patients with soft tissue shoulder disorders: a systematic review of randomized clinical trials. BMJ 1997;15:25-30.
10. Van der Windt DA, Van der Heijden GJ, Van den Berg GJ, et al. Ultrasound therapy for musculoskeletal disorders: a systematic review. Pain 1999;81:257-271.
11. Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain 2000;86:119-132.
12. Winters JC, Sobel JS, Groenier KH, et al. Comparison of physiotherapy, manipulation, and corticosteroid injection for treating shoulder complaints in general practice: randomized, single blind study. BMJ 1997;314:1320-1325.
13. Van der Windt DA, Koes BW, Deville W, et al. Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care: randomized trial. BMJ 1998;317:1292-1296.
14. Mantone JK, Burkhead WZ, Noonan J. Nonoperative treatment of rotator cuff tears. Orthop Clin North Am 2000;31:295-311.
15. Lopez JM. Treatment of acute tendinitis and bursitis with fentiazac. A double blind comparison with placebo. Clin Ther 1982;5:79-84.
16. Zuinen C. Diclofenac/misprostol vs diclofenac/placebo in treating acute episodes of tendinitis/bursitis of the shoulder. Drugs 1993;45 Suppl 1:17-23.
17. Ginsberg F, Famaey JP. A double-blind comparison of slow-release and standard tablet formulations of fentiazac in the treatment of patients with tendinitis and bursitis. Curr Med Res Opin 1985;9:42-448.
18. Wober W. Comparative efficacy and safety of nimesulide and diclofenac in patients with acute shoulder, and a meta-analysis of controlled studies with nimesulide. Rheum 1999;38(Suppl 1):33-38.
19. Wober W, Rahlfs VW, Buchl N, et al. Comparative efficacy and safety of the non-steroidal anti-inflammatory drugs nimesulide and diclofenac in patients with acute subdeltoid bursitis and bicipital tendinitis. Int J Clin Pract 1998;52:169-175.
20. Valtonen E. Double acting betamethasone (celestone chronodose) in the treatment of supraspinatus tendinitis: A comparison of subacromial and gluteal single injections with placebo. J Int Men Res 1978;6:463-467.
21. Blair B, Rokito A, Cuomo F, Jarolem K, Zuckerman J. Efficacy of corticosteroids for subacromial impingement syndrome. J Bone Joint Surg Am 1996;78:1685-1689.
22. Withrington R, Girgis F, Seifert M. A placebo-controlled trial of steroid injections in the treatment of supraspinatus tendinitis. Scand J Rheumatol 1985M;14:76-78.
23. Vecchio PC, Hazleman BL, King RH. A double-blind trial comparing subacromial methylprednisolone and ligno-caine in acute rotator cuff tendinitis. Br J Rheumatol 1993;32:743-745.
24. White R, Paull D, Fleming K. Rotator cuff tendinitis: comparison of subacromial injection of a long acting corticosteroid vs oral indomethacin therapy. J Rheumatol 1986;13:608-613.
25. Adebajo A, Nash P, Hazleman B. A Prospective double blind dummy placebo controlled study comparing triamcinolone hexacetonide injection with oral diclofenac 50mg TDS in patients with rotator cuff tendinitis. J Rheumatol 1990;17:1207-1210.
26. Brox JI, Staff PH, Ljunggren AE, Revik JI. Arthroscopic Surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ 1993;307:899-903
27. Brox JI, Gjengedal E, Uppheim G, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prosprective, randomized, controlled study in 125 patients with a 2 1/2 year follow up. J Shoulder Elbow Surg 1999;8:102-111.
28. Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop 1993;294:103-110.
29. Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop 1992;275:165-173.
30. Hawkins RH, Dunlop R. Nonoperative treatment of rotator cuff tears. Clin Orthop 1995;321:178-188.
31. Goldberg BA, Nowinski RJ, Matsen FA. Outcome of non-operative management of full thickness rotator cuff tears. Clin Orthop 2001;382:99-107.
32. Weiss JJ. Intra-articular steroids in the treatment of rota-tor cuff tear: reappraisal by arthrography. Arch Phys Med Rehabil 1981;62:555-557.
33. De Jong BA, Dahmen R, Hogeweg JA, Marti RK. Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehab 1998;12:211-215.
34. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clonical study with an evaluation of three treatment regimens. Ann Rheum Dis 1984;43:353-360.
35. Thumb N, Kolarz G, Scherak O, Mayrhofer F. The efficacy and safety of Fentiazac and Diclofenac sodium in peri-arthritis of the shoulder: a multi-center, double-blind comparison. J Int Med Res 1987;15:327-334.
36. Rhind V, Downie WW, Bird HA, Wright V, Engler C. Naproxen and indomethacin in periarthritis of the shoulder. Rheumatol Rehabil 1982;21:51-53.
37. Lee PN, Lee M, Haq AM, Longton EB, Wright V. Periarthritis of the shoulder. Ann Rheum Dis 1974;33:116-119.
38. Hazleman BL. The painful stiff shoulder. Rheumatol Rehabil 1972;11:413-421.
39. Croft P, Pope D, Silman A. The clinical course of shoulder pain: prospective cohort study in primary care. BMJ 1996;313:601-602.
40. Van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996;46:519-523.
41. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
42. Burk DL, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. Am J Roentgenol 1989;153:87-92.
43. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-45.
44. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-139.
45. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-498.
46. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with en-enhanced MR imaging of the shoulder. Radiology 1996;200:519-524.
47. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator cuff tear. Findings at ultrasound, double contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-394.
48. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
49. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-146.
Evaluation of shoulder pain
- Shoulder pain is a common complaint seen in primary care.
- Subacromial impingement syndrome and rotator cuff tears are the most common disorders encountered.
- The history and physical examination are keys to most shoulder pain diagnoses, particularly when used in combination.
- Imaging studies are indicated for failed conservative therapy, severe shoulder pathology, or unclear diagnosis.
Shoulder pain is a common problem that can pose difficult diagnostic and therapeutic challenges for the family physician. It is the third most common musculoskeletal complaint in the general population, and accounts for 5% of all general practitioner musculoskeletal consults.1,2 The incidence of shoulder pain is 6.6 to 25 cases per 1000 patients, with a peak incidence in the fourth through sixth decades.3-6 Shoulder pain is second only to knee pain for referrals to orthopedic surgery or primary care sports medicine clinics.7,8 Furthermore, 8% to 13% of athletic injuries involve the shoulder and account for up to 3.9% of new emergency department visits.9,10
Differential diagnosis
The challenge for the physician evaluating shoulder pain is the myriad of etiologies and the potential for multiple disorders. Compounding the challenge is a lack of uniformity in the literature regarding diagnostic classification.11 As Table 1 shows, the age of the patient will help focus the differential diagnosis. Patients younger than 30 years old tend to have biomechanical or mild inflammatory etiologies for their pain such as atraumatic instability, tendinosis, and arthropathies. Less than 1% of shoulder injuries in persons younger than 30 years are complete rotator cuff tears, which occur in 35% of patients older than 45 years with shoulder pain.12,13
The rotator cuff is the most commonly affected structure in the shoulder, and subacromial impingement syndrome is the leading cause of rotator cuff injury.4,12,14-16 Neer14 described 3 stages of shoulder impingement that he estimated lead to 95% of rotator cuff tears. Impingement can be caused by repetitive overhead activities, acute trauma, or subtle instability (atraumatic instability). The current theory is that inflammation of the rotator cuff tendons and/or bursa, caused by irritation against the coracoacromial arch, can progress to a complete rotator cuff tear over time.
Referred sources of shoulder pain should be included in the differential diagnosis of shoulder pain. Potential sources include cervical spondylolysis, cervical arthritis, cervical disc disease, myocardial ischemia, reflex sympathetic dystrophy, diaphragmatic irritation, thoracic outlet syndrome, and gallbladder disease.
TABLE 1
Differential diagnosis of shoulder pain
| Diagnosis | Primary care setting4-15(%) | Age (y) of presentation, Mean (SD)14 |
|---|---|---|
| Subacromial impingement syndrome | 48–72 | |
| Stage I (edema and hemorrhage) | 16 | 23 (7) |
| Stage II (cuff fibrosis and partial tear) | 42 | 41 (11) |
| Stage III (full-thickness tear) | 15 | 62 (12) |
| Adhesive capsulitis | 16–22 | 53 (10) |
| Acute bursitis | 17 | |
| Calcific tendonitis | 6 | |
| Myofascial pain syndrome | 5 | |
| Glenohumeral joint arthrosis | 2.5 | 64 (10) |
| Thoracic outlet syndrome | 2 | |
| Biceps tendonitis | 0.8 |
Using the history and physical examination
As noted above, the likelihood of specific conditions such as a complete rotator cuff tear varies with the setting, age of the patient, and specialty of the physi-cian.4,13,17,18 It is important to keep this pretest probability in mind while interpreting the history and physical examination. For example, a positive empty can test in a 50-year-old patient almost certainly represents a rotator cuff tear, whereas many younger patients with this finding will not have a tear. Moreover, certain components of the history and physical examination are more indicative of disorders while others are better at ruling them out. This concept is represented by the positive and negative likelihood ratios listed in Table 2.
The clinical evaluation begins with identification of the chief complaint and a thorough history. Common complaints include pain, weakness, stiffness, instability, locking, catching, and deformity.26 Determining the duration of symptoms and mechanism of injury will narrow the differential diagnosis. If trauma occurred, the mechanism can determine radiological needs. Aggravating and alleviating factors should be reviewed, including work, recreation, sports, or hobbies. Night pain when lying on the affected side and a history of trauma in a patient older than 65 years both suggest a rotator cuff tear, but no individual symptom is definitive for the diagnosis (Table 2).19 Pain with overhead work may indicate impingement syndrome, especially if the patient is symptomatic through the arc of 60 to 120 degrees.
The physical examination should include observation, palpation, range of motion (ROM), and provocative testing. Observation requires adequate exposure of the shoulders bilaterally to identify any gross deformities or abnormalities, including muscle atrophy, acromioclavicular joint disparity, or evidence of trauma. Muscle atrophy of either the supraspinatus or infraspinatus muscles is moderately predictive of rotator cuff tears in the elderly population, with a positive predictive value of 81%. However, this sign is not useful if absent, with a negative predictive value of only 43%.19 No studies have assessed the role of palpation in the evaluation of shoulder pain. Nevertheless, the role of palpation in discerning acromioclavicular joint pathology from shoulder and neck makes it a useful part of the examination.
The shoulder’s ROM should be evaluated both actively and passively. The shoulder is a mobile joint with a complexity of movements. These include flexion to 180 degrees, extension to 40 degrees, abduction to 120 degrees with palms down and 180 degrees with palms up, internal rotation to 55 degrees, and external rotation to 45 degrees with arms at the side. Although determining abduction ROM is consistent among examiners,27 interrater reliability is poor for assessment of external rotation ROM. Lack of full ROM that is equally limited with both passive and active examination is found in arthropathies and adhesive capsulitis.
Pain between 60 and 120 degrees of abduction “the painful arc”) is associated with subacromial impingement, whereas pain after 120 degrees is an indication of acromioclavicular joint origin. However, Calis and coworkers17 found that the presence of subacromial impingement has a positive likelihood ratio of only 1.7.
After assessing the ROM, the next steps are to evaluate the rotator cuff and biceps tendon, perform impingement testing, check for instability, and finally assess the acromioclavicular joint. The tests are listed in Table 2 in our preferred order of examination and represent the tests best supported by the evidence; the results are based on a literature search of Medline, PubMed, DARE, and Sports Discuss. The technique of each examination maneuver has been published elsewhere and is not described in detail here. Figure 1 through 4 illustrate several common examination maneuvers described below. A Web site that demonstrates the physical examination more thoroughly can be found at http://www.nismat.org/orthocor/exam/shoulder.html#Evaluation.
TABLE 2
Use of history and physical examination to diagnose shoulder pain
| History or maneuver | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| Rotator cuff tear | |||||||
| History of trauma19 | 2B | 36 | 73 | 1.3 | 0.88 | 72 | 37 |
| Night pain19 | 2B | 88 | 20 | 1.1 | 0.6 | 70 | 43 |
| Painful arc17 | 2B | 33 | 81 | 1.7 | 0.83 | 81 | 33 |
| Empty can test18,20,21 | 1B | 84–89 | 50–58 | 1.7–2 | 0.22–0.28 | 36–98 | 22–93 |
| Drop sign21 | 1B | 21 | 100 | >25 | 0.79 | 100 | 32 |
| Lift off test (for subscapularis tears)21 | 1B | 62 | 100 | >25 | 0.38 | 100 | 69 |
| Impingement | |||||||
| Hawkin’s test20,22 | 1B | 87–89 | 60 | 2.2 | 0.18 | 71 | 83 |
| Instability | |||||||
| Relocation test23 | 2B | 57 | 100 | >25 | 0.43 | 100 | 73 |
| Augmented apprehension23 | 2B | 68 | 100 | >25 | 0.32 | 100 | 78 |
| Labral tear | |||||||
| Crank test24 | 2B | 91 | 93 | 13 | 0.10 | 94 | 90 |
| Active compression test25 | 1B | 100 | 99 | >25 | 0.01 | 95 | 100 |
| Acromioclavicular joint | |||||||
| Active compression test25 | 1B | 100 | 97 | >25 | 0.01 | 89 | 100 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| LR+ = positive likelihood ratio; LR− = negative likelihood ratio; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Figure 1
The empty can test
Rotator cuff tests
The drop arm test assesses the integrity of the rotator cuff, predominantly the supraspinatus muscle. The empty can test (Figure 1) isolates the supraspinatus against resistance. The lift off test (Figure 2) assesses the subscapularis integrity.
Figure 2
The lift off test
Impingement syndrome
Hawkin’s sign (Figure 3) is a test for evidence of impingement by re-creation of its symptoms.
Figures 3A & 3B
Hawkin’s sign
Glenohumeral joint stability
The augmented anterior apprehension test evaluates anterior shoulder instability. The relocation test, which helps confirm anterior instability, is carried out immediately after a positive anterior apprehension test.
Labral tears
The crank test is used to identify chronic labral injury, whereas the active compression test25 (Figure 4) indicates labral injury if pain is deep in the shoulder.
Figure 4
The active compression test
Acromioclavicular joint
The active compression test25 (Figure 4) indicates acromioclavicular joint inflammation, arthritis, or injury if pain is localized to the top of the shoulder.
Diagnostic tests
Imaging studies used in the evaluation of shoulder pain include plain radiographs, arthrography, computed tomography (CT), ultrasound (US), and magnetic resonance imaging (MRI). Often no imaging is required, or plain radiographs are the sole imaging study needed. Soft tissue injuries are best identified by MRI or US, whereas bony pathology is seen best with plain radiographs or CT. Indications for imaging include severe injury, uncontrolled pain, failure of conservative therapy, return to play considerations, and examiner discretion. Table 3 outlines the accuracy of imaging modalities organized by diagnosis.
TABLE 3
Imaging tests to diagnose shoulder pain
| Diagnostic test | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial28 | 2B | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete15 | 1B | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall16,29,30 | 2B | 89–96 | 49–100 | 1.9 to >25 | 0.08 | 58 | 94 |
| Impingement28 | 2B | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears31-32 | 1B | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete15 | 1A | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete33 | 1B | 95 | — | — | — | — | — |
| Overall33 | 1B | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 80 | — | — | — | — | — |
| Complete33 | 1B | 90 | — | — | — | — | — |
| Overall33,34 | 1B | 86 | 91 | 9.6 | 0.15 | 96 | 73 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| CT, computed tomography; LR+ = positive likelihood ratio; LR− = negative likelihood ratio; MRI, magnetic resonance imaging; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Plain radiographs
Plain radiographs are the first step in diagnostic imaging. They can reveal fractures, dislocation, subluxation, bony lesions, outlet obstruction, acromioclavicular joint pathology, and arthritic changes. No definitive clinical studies on the needs of radiographs have been done. Plain radiographs should be taken when ROM is lost, especially when there is abduction of less than 90 degrees, severe pain, and after trauma. Our preferred x-rays include a glenohumeral anteroposterior (AP) view, a supraspinatus outlet view, and an axillary view. Anteroposterior views with internal and external rotation are added in cases of trauma to help rule out fracture. Positive acromioclavicular joint tests (crossover or palpation) should be followed by acromioclavicular joint radiographs because a shoulder series does not give a clear view of this joint. Additional views of the neck as well as a chest x-ray or abdominal imaging should be considered if a referred source of shoulder pain remains a possibility.
Arthrography
Arthrography was the diagnostic test of choice before MRI. It is specific for rotator cuff tears but lacks sensitivity15 because it cannot detect partial-thickness or associated soft tissue injuries of the shoulder. Arthrography still has a role in evaluating adhesive capsulitis by demonstrating decreased intracapsular volume.26 The test can be therapeutic if the capsule is dilated during the procedure. Additionally, patients with claustrophobia may be good candidates for arthrography if a full-thickness tear is suspected and MRI is not possible.
Computed tomography
Computed tomography may be used to evaluate bony lesions, including glenoid rim fractures, humoral fractures, and acromioclavicular joint disease. Computed tomography arthrograms may have a role in assessing labral tears and full-thickness rotator cuff tears.35 The use of CT arthrography has fallen into disfavor compared with MRI because of the risks associated with contrast exposure and poor sensitivity for partial-thickness rotator cuff tears or associated soft tissue injury.
Ultrasound
Ultrasound has been used in the evaluation of rotator cuff tears with varying degrees of sensitivity and specificity.12,29,34 This inconsistency may be related to variation in operator skill. Advantages of US include relatively low cost, speed, and noninvasiveness.
Magnetic resonance imaging
Magnetic resonance imaging has become the gold standard for diagnostic imaging of the shoulder related to soft tissue injury. The advantages include its noninvasive nature, lack of contrast exposure, nonionizing radiation, high degree of resolution, and the ability to evaluate multiple potential pathologic processes.36 Magnetic resonance imaging is the preferred test for evaluating impingement syndrome and rotator cuff pathology. A normal MRI greatly reduces the chances of a rotator cuff tear, with a negative likelihood ratio of 0.08.16,29,30 Magnetic resonance imaging is also useful in the evaluation of avascular necrosis, biceps tendon disorders, inflammatory processes, and tumors.13 The diagnosis of labral lesions can be challenging given the relatively low sensitivity and negative predictive value noted in several trials.16,28,31 Finally, it is important to note that up to one third of all asymptomatic patients and more than half of those older than 60 years demonstrate asymptomatic rotator cuff tears on MRI.37
Approach to the patient
A general approach to the patient with shoulder pain is summarized in Figure 5. Pre- and posttest probabilities are included to give an understanding of how tests may help diagnose or rule out a complete rotator cuff tear. A recent prospective study combining multiple examination maneuvers demonstrated that a combination of 3 physical examination findings (supraspinatus weakness, weakness in external rotation, and impingement) along with the patient’s age can often diagnose or rule out a rotator cuff tear.38 This group of tests did not distinguish full versus partial thickness tears. This approach is summarized in Figure 6.
Figure 5
Basic approach to assess for complete rotator cuff tear
Figure 6
Alternative approach to a suspected rotator cuff tear
1. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649-55.
2. Peters D, Davies P, Pietroni P. Musculoskeletal clinic in general practice: study of one year’s referrals. Br J Gen Pract 1994;44:25-9.
3. Croft P. Soft-tissue rheumatism. In: Sillman AJ, Hochberg MC, Eds. Epidemiology of the Rheumatic Disease. Oxford, England: Oxford University Press; 1993;375-421.
4. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-64.
5. Bjelle A. Epidemiology of shoulder problems. Baillieres Clin Rheumatol 1989;3:437-51.
6. Lamberts H, Brouwer HJ, Mohrs J. Reason for Encounter-, Episode-and Process-Oriented Standard Output From Transition Project. Part I. Amsterdam: Department of General Practice/Family Medicine. University of Amsterdam; 1991.
7. Glockner SM. Shoulder pain: a diagnostic dilemma. Am Fam Physician 1995;51:1677-87-1690-2.
8. Butcher JD. Patient profile, referral sources, and consultant utilization in a primary care sports medicine clinic. J Fam Pract 1996;43:556-60.
9. Hill JA. Epidemiological perspective on shoulder injuries. Clin Sports Med 1983;2:241-6.
10. Watters DA, Brooks S, Elton RA, Little K. Sports injuries in an accident and emergency department. Arch Emerg Med 1984;1:105-11.
11. Croft P. Measuring up to shoulder pain. Ann Rheum Dis 1998;57:65-6.
12. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
13. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia: W.B. Saunders; 1994.
14. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
15. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-42.
16. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-5.
17. Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis 2000;59:44-7.
18. Itoi E, Kido T, Samo A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med 1999;27:65-8.
19. Litaker D, Pioro M, El Bilbeisi H, Brems J. Returning to the bedside: using the history and physical exam to identify rotator cuff tears. J Am Geriatr Soc 2000;48:1633-7.
20. Leroux JL, Thomas E, Bonnel F, Blotman F. Diagnostic value of clinical tests for shoulder impingement syndrome. Rev Rhum Engl Ed 1995;62:423-8.
21. Hertel R, Ballmer RT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 1996;5:307-13.
22. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg 2000;9:299-301.
23. Speer KP, Hannafin JA, Altchek DW, Warren RF. An evaluation of shoulder relocation test. Am J Sports Med 1994;22:177-83.
24. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of a new physical examination in predicting glenoid labral tears. Am J Sports Med 1996;24:721-5.
25. O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med 1998;26:610-3.
26. Howard T, O’Connor FG. The injured shoulder: primary care assessment. Arch Fam Med 1997;6:376-84.
27. Croft P, Pope D, Boswell R, Rigby A, Silman A. Observer variability in measuring elevation and external rotation of the shoulder. Primary Care Rheumatology Society Shoulder Study Group. Br J Rheumatol 1994;3 3:942-6.
28. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
29. Burk DL, Jr, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. AJR Am J Roentgenol 1989;153:87-92.
30. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-9.
31. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-8.
32. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology 1996;200:519-24.
33. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator-cuff tear. Findings at ultrasound, double-contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-94.
34. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-6.
35. Wilson AJ, Totty WG, Murphy WA, Hardy DC. Shoulder joint: arthrographic CT and long term follow-up, with surgical correlation. Radiology 1989;173:329-33.
36. Meyer SJ, Dalinka MK. Magnetic resonance imaging of the shoulder. Orthop Clin North Am 1990;21:497-513.
37. Sher JS, Uribe JW, Posada A, Murphy B, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77-A:10-5.
38. Murrell G, Walton J. Diagnosis of rotator cuff tears. Lancet 2001;357:769-70.
- Shoulder pain is a common complaint seen in primary care.
- Subacromial impingement syndrome and rotator cuff tears are the most common disorders encountered.
- The history and physical examination are keys to most shoulder pain diagnoses, particularly when used in combination.
- Imaging studies are indicated for failed conservative therapy, severe shoulder pathology, or unclear diagnosis.
Shoulder pain is a common problem that can pose difficult diagnostic and therapeutic challenges for the family physician. It is the third most common musculoskeletal complaint in the general population, and accounts for 5% of all general practitioner musculoskeletal consults.1,2 The incidence of shoulder pain is 6.6 to 25 cases per 1000 patients, with a peak incidence in the fourth through sixth decades.3-6 Shoulder pain is second only to knee pain for referrals to orthopedic surgery or primary care sports medicine clinics.7,8 Furthermore, 8% to 13% of athletic injuries involve the shoulder and account for up to 3.9% of new emergency department visits.9,10
Differential diagnosis
The challenge for the physician evaluating shoulder pain is the myriad of etiologies and the potential for multiple disorders. Compounding the challenge is a lack of uniformity in the literature regarding diagnostic classification.11 As Table 1 shows, the age of the patient will help focus the differential diagnosis. Patients younger than 30 years old tend to have biomechanical or mild inflammatory etiologies for their pain such as atraumatic instability, tendinosis, and arthropathies. Less than 1% of shoulder injuries in persons younger than 30 years are complete rotator cuff tears, which occur in 35% of patients older than 45 years with shoulder pain.12,13
The rotator cuff is the most commonly affected structure in the shoulder, and subacromial impingement syndrome is the leading cause of rotator cuff injury.4,12,14-16 Neer14 described 3 stages of shoulder impingement that he estimated lead to 95% of rotator cuff tears. Impingement can be caused by repetitive overhead activities, acute trauma, or subtle instability (atraumatic instability). The current theory is that inflammation of the rotator cuff tendons and/or bursa, caused by irritation against the coracoacromial arch, can progress to a complete rotator cuff tear over time.
Referred sources of shoulder pain should be included in the differential diagnosis of shoulder pain. Potential sources include cervical spondylolysis, cervical arthritis, cervical disc disease, myocardial ischemia, reflex sympathetic dystrophy, diaphragmatic irritation, thoracic outlet syndrome, and gallbladder disease.
TABLE 1
Differential diagnosis of shoulder pain
| Diagnosis | Primary care setting4-15(%) | Age (y) of presentation, Mean (SD)14 |
|---|---|---|
| Subacromial impingement syndrome | 48–72 | |
| Stage I (edema and hemorrhage) | 16 | 23 (7) |
| Stage II (cuff fibrosis and partial tear) | 42 | 41 (11) |
| Stage III (full-thickness tear) | 15 | 62 (12) |
| Adhesive capsulitis | 16–22 | 53 (10) |
| Acute bursitis | 17 | |
| Calcific tendonitis | 6 | |
| Myofascial pain syndrome | 5 | |
| Glenohumeral joint arthrosis | 2.5 | 64 (10) |
| Thoracic outlet syndrome | 2 | |
| Biceps tendonitis | 0.8 |
Using the history and physical examination
As noted above, the likelihood of specific conditions such as a complete rotator cuff tear varies with the setting, age of the patient, and specialty of the physi-cian.4,13,17,18 It is important to keep this pretest probability in mind while interpreting the history and physical examination. For example, a positive empty can test in a 50-year-old patient almost certainly represents a rotator cuff tear, whereas many younger patients with this finding will not have a tear. Moreover, certain components of the history and physical examination are more indicative of disorders while others are better at ruling them out. This concept is represented by the positive and negative likelihood ratios listed in Table 2.
The clinical evaluation begins with identification of the chief complaint and a thorough history. Common complaints include pain, weakness, stiffness, instability, locking, catching, and deformity.26 Determining the duration of symptoms and mechanism of injury will narrow the differential diagnosis. If trauma occurred, the mechanism can determine radiological needs. Aggravating and alleviating factors should be reviewed, including work, recreation, sports, or hobbies. Night pain when lying on the affected side and a history of trauma in a patient older than 65 years both suggest a rotator cuff tear, but no individual symptom is definitive for the diagnosis (Table 2).19 Pain with overhead work may indicate impingement syndrome, especially if the patient is symptomatic through the arc of 60 to 120 degrees.
The physical examination should include observation, palpation, range of motion (ROM), and provocative testing. Observation requires adequate exposure of the shoulders bilaterally to identify any gross deformities or abnormalities, including muscle atrophy, acromioclavicular joint disparity, or evidence of trauma. Muscle atrophy of either the supraspinatus or infraspinatus muscles is moderately predictive of rotator cuff tears in the elderly population, with a positive predictive value of 81%. However, this sign is not useful if absent, with a negative predictive value of only 43%.19 No studies have assessed the role of palpation in the evaluation of shoulder pain. Nevertheless, the role of palpation in discerning acromioclavicular joint pathology from shoulder and neck makes it a useful part of the examination.
The shoulder’s ROM should be evaluated both actively and passively. The shoulder is a mobile joint with a complexity of movements. These include flexion to 180 degrees, extension to 40 degrees, abduction to 120 degrees with palms down and 180 degrees with palms up, internal rotation to 55 degrees, and external rotation to 45 degrees with arms at the side. Although determining abduction ROM is consistent among examiners,27 interrater reliability is poor for assessment of external rotation ROM. Lack of full ROM that is equally limited with both passive and active examination is found in arthropathies and adhesive capsulitis.
Pain between 60 and 120 degrees of abduction “the painful arc”) is associated with subacromial impingement, whereas pain after 120 degrees is an indication of acromioclavicular joint origin. However, Calis and coworkers17 found that the presence of subacromial impingement has a positive likelihood ratio of only 1.7.
After assessing the ROM, the next steps are to evaluate the rotator cuff and biceps tendon, perform impingement testing, check for instability, and finally assess the acromioclavicular joint. The tests are listed in Table 2 in our preferred order of examination and represent the tests best supported by the evidence; the results are based on a literature search of Medline, PubMed, DARE, and Sports Discuss. The technique of each examination maneuver has been published elsewhere and is not described in detail here. Figure 1 through 4 illustrate several common examination maneuvers described below. A Web site that demonstrates the physical examination more thoroughly can be found at http://www.nismat.org/orthocor/exam/shoulder.html#Evaluation.
TABLE 2
Use of history and physical examination to diagnose shoulder pain
| History or maneuver | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| Rotator cuff tear | |||||||
| History of trauma19 | 2B | 36 | 73 | 1.3 | 0.88 | 72 | 37 |
| Night pain19 | 2B | 88 | 20 | 1.1 | 0.6 | 70 | 43 |
| Painful arc17 | 2B | 33 | 81 | 1.7 | 0.83 | 81 | 33 |
| Empty can test18,20,21 | 1B | 84–89 | 50–58 | 1.7–2 | 0.22–0.28 | 36–98 | 22–93 |
| Drop sign21 | 1B | 21 | 100 | >25 | 0.79 | 100 | 32 |
| Lift off test (for subscapularis tears)21 | 1B | 62 | 100 | >25 | 0.38 | 100 | 69 |
| Impingement | |||||||
| Hawkin’s test20,22 | 1B | 87–89 | 60 | 2.2 | 0.18 | 71 | 83 |
| Instability | |||||||
| Relocation test23 | 2B | 57 | 100 | >25 | 0.43 | 100 | 73 |
| Augmented apprehension23 | 2B | 68 | 100 | >25 | 0.32 | 100 | 78 |
| Labral tear | |||||||
| Crank test24 | 2B | 91 | 93 | 13 | 0.10 | 94 | 90 |
| Active compression test25 | 1B | 100 | 99 | >25 | 0.01 | 95 | 100 |
| Acromioclavicular joint | |||||||
| Active compression test25 | 1B | 100 | 97 | >25 | 0.01 | 89 | 100 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| LR+ = positive likelihood ratio; LR− = negative likelihood ratio; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Figure 1
The empty can test
Rotator cuff tests
The drop arm test assesses the integrity of the rotator cuff, predominantly the supraspinatus muscle. The empty can test (Figure 1) isolates the supraspinatus against resistance. The lift off test (Figure 2) assesses the subscapularis integrity.
Figure 2
The lift off test
Impingement syndrome
Hawkin’s sign (Figure 3) is a test for evidence of impingement by re-creation of its symptoms.
Figures 3A & 3B
Hawkin’s sign
Glenohumeral joint stability
The augmented anterior apprehension test evaluates anterior shoulder instability. The relocation test, which helps confirm anterior instability, is carried out immediately after a positive anterior apprehension test.
Labral tears
The crank test is used to identify chronic labral injury, whereas the active compression test25 (Figure 4) indicates labral injury if pain is deep in the shoulder.
Figure 4
The active compression test
Acromioclavicular joint
The active compression test25 (Figure 4) indicates acromioclavicular joint inflammation, arthritis, or injury if pain is localized to the top of the shoulder.
Diagnostic tests
Imaging studies used in the evaluation of shoulder pain include plain radiographs, arthrography, computed tomography (CT), ultrasound (US), and magnetic resonance imaging (MRI). Often no imaging is required, or plain radiographs are the sole imaging study needed. Soft tissue injuries are best identified by MRI or US, whereas bony pathology is seen best with plain radiographs or CT. Indications for imaging include severe injury, uncontrolled pain, failure of conservative therapy, return to play considerations, and examiner discretion. Table 3 outlines the accuracy of imaging modalities organized by diagnosis.
TABLE 3
Imaging tests to diagnose shoulder pain
| Diagnostic test | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial28 | 2B | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete15 | 1B | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall16,29,30 | 2B | 89–96 | 49–100 | 1.9 to >25 | 0.08 | 58 | 94 |
| Impingement28 | 2B | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears31-32 | 1B | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete15 | 1A | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete33 | 1B | 95 | — | — | — | — | — |
| Overall33 | 1B | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 80 | — | — | — | — | — |
| Complete33 | 1B | 90 | — | — | — | — | — |
| Overall33,34 | 1B | 86 | 91 | 9.6 | 0.15 | 96 | 73 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| CT, computed tomography; LR+ = positive likelihood ratio; LR− = negative likelihood ratio; MRI, magnetic resonance imaging; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Plain radiographs
Plain radiographs are the first step in diagnostic imaging. They can reveal fractures, dislocation, subluxation, bony lesions, outlet obstruction, acromioclavicular joint pathology, and arthritic changes. No definitive clinical studies on the needs of radiographs have been done. Plain radiographs should be taken when ROM is lost, especially when there is abduction of less than 90 degrees, severe pain, and after trauma. Our preferred x-rays include a glenohumeral anteroposterior (AP) view, a supraspinatus outlet view, and an axillary view. Anteroposterior views with internal and external rotation are added in cases of trauma to help rule out fracture. Positive acromioclavicular joint tests (crossover or palpation) should be followed by acromioclavicular joint radiographs because a shoulder series does not give a clear view of this joint. Additional views of the neck as well as a chest x-ray or abdominal imaging should be considered if a referred source of shoulder pain remains a possibility.
Arthrography
Arthrography was the diagnostic test of choice before MRI. It is specific for rotator cuff tears but lacks sensitivity15 because it cannot detect partial-thickness or associated soft tissue injuries of the shoulder. Arthrography still has a role in evaluating adhesive capsulitis by demonstrating decreased intracapsular volume.26 The test can be therapeutic if the capsule is dilated during the procedure. Additionally, patients with claustrophobia may be good candidates for arthrography if a full-thickness tear is suspected and MRI is not possible.
Computed tomography
Computed tomography may be used to evaluate bony lesions, including glenoid rim fractures, humoral fractures, and acromioclavicular joint disease. Computed tomography arthrograms may have a role in assessing labral tears and full-thickness rotator cuff tears.35 The use of CT arthrography has fallen into disfavor compared with MRI because of the risks associated with contrast exposure and poor sensitivity for partial-thickness rotator cuff tears or associated soft tissue injury.
Ultrasound
Ultrasound has been used in the evaluation of rotator cuff tears with varying degrees of sensitivity and specificity.12,29,34 This inconsistency may be related to variation in operator skill. Advantages of US include relatively low cost, speed, and noninvasiveness.
Magnetic resonance imaging
Magnetic resonance imaging has become the gold standard for diagnostic imaging of the shoulder related to soft tissue injury. The advantages include its noninvasive nature, lack of contrast exposure, nonionizing radiation, high degree of resolution, and the ability to evaluate multiple potential pathologic processes.36 Magnetic resonance imaging is the preferred test for evaluating impingement syndrome and rotator cuff pathology. A normal MRI greatly reduces the chances of a rotator cuff tear, with a negative likelihood ratio of 0.08.16,29,30 Magnetic resonance imaging is also useful in the evaluation of avascular necrosis, biceps tendon disorders, inflammatory processes, and tumors.13 The diagnosis of labral lesions can be challenging given the relatively low sensitivity and negative predictive value noted in several trials.16,28,31 Finally, it is important to note that up to one third of all asymptomatic patients and more than half of those older than 60 years demonstrate asymptomatic rotator cuff tears on MRI.37
Approach to the patient
A general approach to the patient with shoulder pain is summarized in Figure 5. Pre- and posttest probabilities are included to give an understanding of how tests may help diagnose or rule out a complete rotator cuff tear. A recent prospective study combining multiple examination maneuvers demonstrated that a combination of 3 physical examination findings (supraspinatus weakness, weakness in external rotation, and impingement) along with the patient’s age can often diagnose or rule out a rotator cuff tear.38 This group of tests did not distinguish full versus partial thickness tears. This approach is summarized in Figure 6.
Figure 5
Basic approach to assess for complete rotator cuff tear
Figure 6
Alternative approach to a suspected rotator cuff tear
- Shoulder pain is a common complaint seen in primary care.
- Subacromial impingement syndrome and rotator cuff tears are the most common disorders encountered.
- The history and physical examination are keys to most shoulder pain diagnoses, particularly when used in combination.
- Imaging studies are indicated for failed conservative therapy, severe shoulder pathology, or unclear diagnosis.
Shoulder pain is a common problem that can pose difficult diagnostic and therapeutic challenges for the family physician. It is the third most common musculoskeletal complaint in the general population, and accounts for 5% of all general practitioner musculoskeletal consults.1,2 The incidence of shoulder pain is 6.6 to 25 cases per 1000 patients, with a peak incidence in the fourth through sixth decades.3-6 Shoulder pain is second only to knee pain for referrals to orthopedic surgery or primary care sports medicine clinics.7,8 Furthermore, 8% to 13% of athletic injuries involve the shoulder and account for up to 3.9% of new emergency department visits.9,10
Differential diagnosis
The challenge for the physician evaluating shoulder pain is the myriad of etiologies and the potential for multiple disorders. Compounding the challenge is a lack of uniformity in the literature regarding diagnostic classification.11 As Table 1 shows, the age of the patient will help focus the differential diagnosis. Patients younger than 30 years old tend to have biomechanical or mild inflammatory etiologies for their pain such as atraumatic instability, tendinosis, and arthropathies. Less than 1% of shoulder injuries in persons younger than 30 years are complete rotator cuff tears, which occur in 35% of patients older than 45 years with shoulder pain.12,13
The rotator cuff is the most commonly affected structure in the shoulder, and subacromial impingement syndrome is the leading cause of rotator cuff injury.4,12,14-16 Neer14 described 3 stages of shoulder impingement that he estimated lead to 95% of rotator cuff tears. Impingement can be caused by repetitive overhead activities, acute trauma, or subtle instability (atraumatic instability). The current theory is that inflammation of the rotator cuff tendons and/or bursa, caused by irritation against the coracoacromial arch, can progress to a complete rotator cuff tear over time.
Referred sources of shoulder pain should be included in the differential diagnosis of shoulder pain. Potential sources include cervical spondylolysis, cervical arthritis, cervical disc disease, myocardial ischemia, reflex sympathetic dystrophy, diaphragmatic irritation, thoracic outlet syndrome, and gallbladder disease.
TABLE 1
Differential diagnosis of shoulder pain
| Diagnosis | Primary care setting4-15(%) | Age (y) of presentation, Mean (SD)14 |
|---|---|---|
| Subacromial impingement syndrome | 48–72 | |
| Stage I (edema and hemorrhage) | 16 | 23 (7) |
| Stage II (cuff fibrosis and partial tear) | 42 | 41 (11) |
| Stage III (full-thickness tear) | 15 | 62 (12) |
| Adhesive capsulitis | 16–22 | 53 (10) |
| Acute bursitis | 17 | |
| Calcific tendonitis | 6 | |
| Myofascial pain syndrome | 5 | |
| Glenohumeral joint arthrosis | 2.5 | 64 (10) |
| Thoracic outlet syndrome | 2 | |
| Biceps tendonitis | 0.8 |
Using the history and physical examination
As noted above, the likelihood of specific conditions such as a complete rotator cuff tear varies with the setting, age of the patient, and specialty of the physi-cian.4,13,17,18 It is important to keep this pretest probability in mind while interpreting the history and physical examination. For example, a positive empty can test in a 50-year-old patient almost certainly represents a rotator cuff tear, whereas many younger patients with this finding will not have a tear. Moreover, certain components of the history and physical examination are more indicative of disorders while others are better at ruling them out. This concept is represented by the positive and negative likelihood ratios listed in Table 2.
The clinical evaluation begins with identification of the chief complaint and a thorough history. Common complaints include pain, weakness, stiffness, instability, locking, catching, and deformity.26 Determining the duration of symptoms and mechanism of injury will narrow the differential diagnosis. If trauma occurred, the mechanism can determine radiological needs. Aggravating and alleviating factors should be reviewed, including work, recreation, sports, or hobbies. Night pain when lying on the affected side and a history of trauma in a patient older than 65 years both suggest a rotator cuff tear, but no individual symptom is definitive for the diagnosis (Table 2).19 Pain with overhead work may indicate impingement syndrome, especially if the patient is symptomatic through the arc of 60 to 120 degrees.
The physical examination should include observation, palpation, range of motion (ROM), and provocative testing. Observation requires adequate exposure of the shoulders bilaterally to identify any gross deformities or abnormalities, including muscle atrophy, acromioclavicular joint disparity, or evidence of trauma. Muscle atrophy of either the supraspinatus or infraspinatus muscles is moderately predictive of rotator cuff tears in the elderly population, with a positive predictive value of 81%. However, this sign is not useful if absent, with a negative predictive value of only 43%.19 No studies have assessed the role of palpation in the evaluation of shoulder pain. Nevertheless, the role of palpation in discerning acromioclavicular joint pathology from shoulder and neck makes it a useful part of the examination.
The shoulder’s ROM should be evaluated both actively and passively. The shoulder is a mobile joint with a complexity of movements. These include flexion to 180 degrees, extension to 40 degrees, abduction to 120 degrees with palms down and 180 degrees with palms up, internal rotation to 55 degrees, and external rotation to 45 degrees with arms at the side. Although determining abduction ROM is consistent among examiners,27 interrater reliability is poor for assessment of external rotation ROM. Lack of full ROM that is equally limited with both passive and active examination is found in arthropathies and adhesive capsulitis.
Pain between 60 and 120 degrees of abduction “the painful arc”) is associated with subacromial impingement, whereas pain after 120 degrees is an indication of acromioclavicular joint origin. However, Calis and coworkers17 found that the presence of subacromial impingement has a positive likelihood ratio of only 1.7.
After assessing the ROM, the next steps are to evaluate the rotator cuff and biceps tendon, perform impingement testing, check for instability, and finally assess the acromioclavicular joint. The tests are listed in Table 2 in our preferred order of examination and represent the tests best supported by the evidence; the results are based on a literature search of Medline, PubMed, DARE, and Sports Discuss. The technique of each examination maneuver has been published elsewhere and is not described in detail here. Figure 1 through 4 illustrate several common examination maneuvers described below. A Web site that demonstrates the physical examination more thoroughly can be found at http://www.nismat.org/orthocor/exam/shoulder.html#Evaluation.
TABLE 2
Use of history and physical examination to diagnose shoulder pain
| History or maneuver | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| Rotator cuff tear | |||||||
| History of trauma19 | 2B | 36 | 73 | 1.3 | 0.88 | 72 | 37 |
| Night pain19 | 2B | 88 | 20 | 1.1 | 0.6 | 70 | 43 |
| Painful arc17 | 2B | 33 | 81 | 1.7 | 0.83 | 81 | 33 |
| Empty can test18,20,21 | 1B | 84–89 | 50–58 | 1.7–2 | 0.22–0.28 | 36–98 | 22–93 |
| Drop sign21 | 1B | 21 | 100 | >25 | 0.79 | 100 | 32 |
| Lift off test (for subscapularis tears)21 | 1B | 62 | 100 | >25 | 0.38 | 100 | 69 |
| Impingement | |||||||
| Hawkin’s test20,22 | 1B | 87–89 | 60 | 2.2 | 0.18 | 71 | 83 |
| Instability | |||||||
| Relocation test23 | 2B | 57 | 100 | >25 | 0.43 | 100 | 73 |
| Augmented apprehension23 | 2B | 68 | 100 | >25 | 0.32 | 100 | 78 |
| Labral tear | |||||||
| Crank test24 | 2B | 91 | 93 | 13 | 0.10 | 94 | 90 |
| Active compression test25 | 1B | 100 | 99 | >25 | 0.01 | 95 | 100 |
| Acromioclavicular joint | |||||||
| Active compression test25 | 1B | 100 | 97 | >25 | 0.01 | 89 | 100 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| LR+ = positive likelihood ratio; LR− = negative likelihood ratio; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Figure 1
The empty can test
Rotator cuff tests
The drop arm test assesses the integrity of the rotator cuff, predominantly the supraspinatus muscle. The empty can test (Figure 1) isolates the supraspinatus against resistance. The lift off test (Figure 2) assesses the subscapularis integrity.
Figure 2
The lift off test
Impingement syndrome
Hawkin’s sign (Figure 3) is a test for evidence of impingement by re-creation of its symptoms.
Figures 3A & 3B
Hawkin’s sign
Glenohumeral joint stability
The augmented anterior apprehension test evaluates anterior shoulder instability. The relocation test, which helps confirm anterior instability, is carried out immediately after a positive anterior apprehension test.
Labral tears
The crank test is used to identify chronic labral injury, whereas the active compression test25 (Figure 4) indicates labral injury if pain is deep in the shoulder.
Figure 4
The active compression test
Acromioclavicular joint
The active compression test25 (Figure 4) indicates acromioclavicular joint inflammation, arthritis, or injury if pain is localized to the top of the shoulder.
Diagnostic tests
Imaging studies used in the evaluation of shoulder pain include plain radiographs, arthrography, computed tomography (CT), ultrasound (US), and magnetic resonance imaging (MRI). Often no imaging is required, or plain radiographs are the sole imaging study needed. Soft tissue injuries are best identified by MRI or US, whereas bony pathology is seen best with plain radiographs or CT. Indications for imaging include severe injury, uncontrolled pain, failure of conservative therapy, return to play considerations, and examiner discretion. Table 3 outlines the accuracy of imaging modalities organized by diagnosis.
TABLE 3
Imaging tests to diagnose shoulder pain
| Diagnostic test | Study quality (1A–5)* | Sensitivity | Specificity | LR+ | LR− | PV+ | PV− |
|---|---|---|---|---|---|---|---|
| MRI | |||||||
| Rotator cuff tears | |||||||
| Partial28 | 2B | 82 | 85 | 5.5 | 0.21 | 82 | 85 |
| Complete15 | 1B | 81 | 78 | 3.7 | 0.24 | — | — |
| Overall16,29,30 | 2B | 89–96 | 49–100 | 1.9 to >25 | 0.08 | 58 | 94 |
| Impingement28 | 2B | 93 | 87 | 7.2 | 0.08 | 93 | 87 |
| Labral tears31-32 | 1B | 75–89 | 97–100 | >25 | 0.11–0.25 | 100 | 41 |
| Plain arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete15 | 1A | 50 | 96 | 13 | 0.52 | — | — |
| CT arthrogram | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 70 | — | — | — | — | — |
| Complete33 | 1B | 95 | — | — | — | — | — |
| Overall33 | 1B | 86 | 98 | >25 | 0.14 | 96 | 93 |
| Ultrasound | |||||||
| Rotator cuff tears | |||||||
| Partial33 | 1B | 80 | — | — | — | — | — |
| Complete33 | 1B | 90 | — | — | — | — | — |
| Overall33,34 | 1B | 86 | 91 | 9.6 | 0.15 | 96 | 73 |
| *Based on the guidelines for evidence quality outlined by the Center for Evidence-Based Medicine (http://163.1.96.10/docs/levels.html). | |||||||
| CT, computed tomography; LR+ = positive likelihood ratio; LR− = negative likelihood ratio; MRI, magnetic resonance imaging; PV+ = positive predictive value; PV− = negative predictive value. | |||||||
Plain radiographs
Plain radiographs are the first step in diagnostic imaging. They can reveal fractures, dislocation, subluxation, bony lesions, outlet obstruction, acromioclavicular joint pathology, and arthritic changes. No definitive clinical studies on the needs of radiographs have been done. Plain radiographs should be taken when ROM is lost, especially when there is abduction of less than 90 degrees, severe pain, and after trauma. Our preferred x-rays include a glenohumeral anteroposterior (AP) view, a supraspinatus outlet view, and an axillary view. Anteroposterior views with internal and external rotation are added in cases of trauma to help rule out fracture. Positive acromioclavicular joint tests (crossover or palpation) should be followed by acromioclavicular joint radiographs because a shoulder series does not give a clear view of this joint. Additional views of the neck as well as a chest x-ray or abdominal imaging should be considered if a referred source of shoulder pain remains a possibility.
Arthrography
Arthrography was the diagnostic test of choice before MRI. It is specific for rotator cuff tears but lacks sensitivity15 because it cannot detect partial-thickness or associated soft tissue injuries of the shoulder. Arthrography still has a role in evaluating adhesive capsulitis by demonstrating decreased intracapsular volume.26 The test can be therapeutic if the capsule is dilated during the procedure. Additionally, patients with claustrophobia may be good candidates for arthrography if a full-thickness tear is suspected and MRI is not possible.
Computed tomography
Computed tomography may be used to evaluate bony lesions, including glenoid rim fractures, humoral fractures, and acromioclavicular joint disease. Computed tomography arthrograms may have a role in assessing labral tears and full-thickness rotator cuff tears.35 The use of CT arthrography has fallen into disfavor compared with MRI because of the risks associated with contrast exposure and poor sensitivity for partial-thickness rotator cuff tears or associated soft tissue injury.
Ultrasound
Ultrasound has been used in the evaluation of rotator cuff tears with varying degrees of sensitivity and specificity.12,29,34 This inconsistency may be related to variation in operator skill. Advantages of US include relatively low cost, speed, and noninvasiveness.
Magnetic resonance imaging
Magnetic resonance imaging has become the gold standard for diagnostic imaging of the shoulder related to soft tissue injury. The advantages include its noninvasive nature, lack of contrast exposure, nonionizing radiation, high degree of resolution, and the ability to evaluate multiple potential pathologic processes.36 Magnetic resonance imaging is the preferred test for evaluating impingement syndrome and rotator cuff pathology. A normal MRI greatly reduces the chances of a rotator cuff tear, with a negative likelihood ratio of 0.08.16,29,30 Magnetic resonance imaging is also useful in the evaluation of avascular necrosis, biceps tendon disorders, inflammatory processes, and tumors.13 The diagnosis of labral lesions can be challenging given the relatively low sensitivity and negative predictive value noted in several trials.16,28,31 Finally, it is important to note that up to one third of all asymptomatic patients and more than half of those older than 60 years demonstrate asymptomatic rotator cuff tears on MRI.37
Approach to the patient
A general approach to the patient with shoulder pain is summarized in Figure 5. Pre- and posttest probabilities are included to give an understanding of how tests may help diagnose or rule out a complete rotator cuff tear. A recent prospective study combining multiple examination maneuvers demonstrated that a combination of 3 physical examination findings (supraspinatus weakness, weakness in external rotation, and impingement) along with the patient’s age can often diagnose or rule out a rotator cuff tear.38 This group of tests did not distinguish full versus partial thickness tears. This approach is summarized in Figure 6.
Figure 5
Basic approach to assess for complete rotator cuff tear
Figure 6
Alternative approach to a suspected rotator cuff tear
1. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649-55.
2. Peters D, Davies P, Pietroni P. Musculoskeletal clinic in general practice: study of one year’s referrals. Br J Gen Pract 1994;44:25-9.
3. Croft P. Soft-tissue rheumatism. In: Sillman AJ, Hochberg MC, Eds. Epidemiology of the Rheumatic Disease. Oxford, England: Oxford University Press; 1993;375-421.
4. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-64.
5. Bjelle A. Epidemiology of shoulder problems. Baillieres Clin Rheumatol 1989;3:437-51.
6. Lamberts H, Brouwer HJ, Mohrs J. Reason for Encounter-, Episode-and Process-Oriented Standard Output From Transition Project. Part I. Amsterdam: Department of General Practice/Family Medicine. University of Amsterdam; 1991.
7. Glockner SM. Shoulder pain: a diagnostic dilemma. Am Fam Physician 1995;51:1677-87-1690-2.
8. Butcher JD. Patient profile, referral sources, and consultant utilization in a primary care sports medicine clinic. J Fam Pract 1996;43:556-60.
9. Hill JA. Epidemiological perspective on shoulder injuries. Clin Sports Med 1983;2:241-6.
10. Watters DA, Brooks S, Elton RA, Little K. Sports injuries in an accident and emergency department. Arch Emerg Med 1984;1:105-11.
11. Croft P. Measuring up to shoulder pain. Ann Rheum Dis 1998;57:65-6.
12. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
13. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia: W.B. Saunders; 1994.
14. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
15. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-42.
16. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-5.
17. Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis 2000;59:44-7.
18. Itoi E, Kido T, Samo A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med 1999;27:65-8.
19. Litaker D, Pioro M, El Bilbeisi H, Brems J. Returning to the bedside: using the history and physical exam to identify rotator cuff tears. J Am Geriatr Soc 2000;48:1633-7.
20. Leroux JL, Thomas E, Bonnel F, Blotman F. Diagnostic value of clinical tests for shoulder impingement syndrome. Rev Rhum Engl Ed 1995;62:423-8.
21. Hertel R, Ballmer RT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 1996;5:307-13.
22. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg 2000;9:299-301.
23. Speer KP, Hannafin JA, Altchek DW, Warren RF. An evaluation of shoulder relocation test. Am J Sports Med 1994;22:177-83.
24. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of a new physical examination in predicting glenoid labral tears. Am J Sports Med 1996;24:721-5.
25. O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med 1998;26:610-3.
26. Howard T, O’Connor FG. The injured shoulder: primary care assessment. Arch Fam Med 1997;6:376-84.
27. Croft P, Pope D, Boswell R, Rigby A, Silman A. Observer variability in measuring elevation and external rotation of the shoulder. Primary Care Rheumatology Society Shoulder Study Group. Br J Rheumatol 1994;3 3:942-6.
28. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
29. Burk DL, Jr, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. AJR Am J Roentgenol 1989;153:87-92.
30. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-9.
31. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-8.
32. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology 1996;200:519-24.
33. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator-cuff tear. Findings at ultrasound, double-contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-94.
34. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-6.
35. Wilson AJ, Totty WG, Murphy WA, Hardy DC. Shoulder joint: arthrographic CT and long term follow-up, with surgical correlation. Radiology 1989;173:329-33.
36. Meyer SJ, Dalinka MK. Magnetic resonance imaging of the shoulder. Orthop Clin North Am 1990;21:497-513.
37. Sher JS, Uribe JW, Posada A, Murphy B, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77-A:10-5.
38. Murrell G, Walton J. Diagnosis of rotator cuff tears. Lancet 2001;357:769-70.
1. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;57:649-55.
2. Peters D, Davies P, Pietroni P. Musculoskeletal clinic in general practice: study of one year’s referrals. Br J Gen Pract 1994;44:25-9.
3. Croft P. Soft-tissue rheumatism. In: Sillman AJ, Hochberg MC, Eds. Epidemiology of the Rheumatic Disease. Oxford, England: Oxford University Press; 1993;375-421.
4. Van der Windt DA, Koes BW, De Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959-64.
5. Bjelle A. Epidemiology of shoulder problems. Baillieres Clin Rheumatol 1989;3:437-51.
6. Lamberts H, Brouwer HJ, Mohrs J. Reason for Encounter-, Episode-and Process-Oriented Standard Output From Transition Project. Part I. Amsterdam: Department of General Practice/Family Medicine. University of Amsterdam; 1991.
7. Glockner SM. Shoulder pain: a diagnostic dilemma. Am Fam Physician 1995;51:1677-87-1690-2.
8. Butcher JD. Patient profile, referral sources, and consultant utilization in a primary care sports medicine clinic. J Fam Pract 1996;43:556-60.
9. Hill JA. Epidemiological perspective on shoulder injuries. Clin Sports Med 1983;2:241-6.
10. Watters DA, Brooks S, Elton RA, Little K. Sports injuries in an accident and emergency department. Arch Emerg Med 1984;1:105-11.
11. Croft P. Measuring up to shoulder pain. Ann Rheum Dis 1998;57:65-6.
12. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am 2000;82:498-504.
13. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Practical Evaluation and Management of the Shoulder. Philadelphia: W.B. Saunders; 1994.
14. Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41-50.
15. Blanchard TK, Bearcroft PW, Constant CR, Griffin DR, Dixon AK. Diagnostic and therapeutic impact of MRI and arthrography in the investigation of full-thickness rotator cuff tears. Eur Radiol 1999;9:638-42.
16. Torstensen ET, Hollinshead RM. Comparison of magnetic resonance imaging and arthroscopy in the evaluation of shoulder pathology. J Shoulder Elbow Surg 1999;8:42-5.
17. Calis M, Akgun K, Birtane M, Karacan I, Calis H, Tuzun F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis 2000;59:44-7.
18. Itoi E, Kido T, Samo A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med 1999;27:65-8.
19. Litaker D, Pioro M, El Bilbeisi H, Brems J. Returning to the bedside: using the history and physical exam to identify rotator cuff tears. J Am Geriatr Soc 2000;48:1633-7.
20. Leroux JL, Thomas E, Bonnel F, Blotman F. Diagnostic value of clinical tests for shoulder impingement syndrome. Rev Rhum Engl Ed 1995;62:423-8.
21. Hertel R, Ballmer RT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg 1996;5:307-13.
22. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg 2000;9:299-301.
23. Speer KP, Hannafin JA, Altchek DW, Warren RF. An evaluation of shoulder relocation test. Am J Sports Med 1994;22:177-83.
24. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of a new physical examination in predicting glenoid labral tears. Am J Sports Med 1996;24:721-5.
25. O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med 1998;26:610-3.
26. Howard T, O’Connor FG. The injured shoulder: primary care assessment. Arch Fam Med 1997;6:376-84.
27. Croft P, Pope D, Boswell R, Rigby A, Silman A. Observer variability in measuring elevation and external rotation of the shoulder. Primary Care Rheumatology Society Shoulder Study Group. Br J Rheumatol 1994;3 3:942-6.
28. Iannotti JP, Zlatkin MB, Esterhai JL, Kressel HY, Dalinka MK, Spindler KP. Magnetic resonance imaging of the shoulder. Sensitivity, specificity, and predictive value. J Bone Joint Surg 1991;73:17-29.
29. Burk DL, Jr, Karasick D, Kurtz AB, et al. Rotator cuff tears: prospective comparison of MR imaging with arthrography, sonography, and surgery. AJR Am J Roentgenol 1989;153:87-92.
30. Yeu K, Jiang CC, Shih TT. Correlation between MRI and operative findings of the rotator cuff tear. J Formos Med Assoc 1994;93:134-9.
31. Green MR, Christensen KP. Magnetic resonance imaging of the glenoid labrum in anterior shoulder instability. Am J Sports Med 1994;22:493-8.
32. Gusmer PB, Potter HG, Schaltz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology 1996;200:519-24.
33. Farin PU, Kaukanen E, Jaroma H, Vaatainen U, Miettinen H, Soimakallio S. Site and size of rotator-cuff tear. Findings at ultrasound, double-contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol 1996;31:387-94.
34. Van Moppes FI, Veldkam O, Roorda J. Role of shoulder ultrasonography in the evaluation of the painful shoulder. Eur J Radiol 1995;19:142-6.
35. Wilson AJ, Totty WG, Murphy WA, Hardy DC. Shoulder joint: arthrographic CT and long term follow-up, with surgical correlation. Radiology 1989;173:329-33.
36. Meyer SJ, Dalinka MK. Magnetic resonance imaging of the shoulder. Orthop Clin North Am 1990;21:497-513.
37. Sher JS, Uribe JW, Posada A, Murphy B, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995;77-A:10-5.
38. Murrell G, Walton J. Diagnosis of rotator cuff tears. Lancet 2001;357:769-70.