User login
Team creates tool to assess frailty in MM
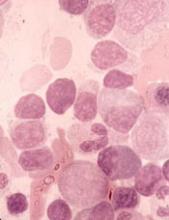
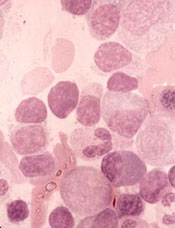
Researchers say they have developed a frailty index that can predict overall survival (OS) in patients newly diagnosed with multiple myeloma (MM).
An increasing frailty index score was significantly associated with an increased risk of death in these patients, and frailty retained a significant association with OS even after the researchers controlled for patients’ chronological age.
“Our goal was to create a tool that could be widely applied using data sources at hand and that helps doctors provide better informed treatment recommendations for their patients,” said Tanya S. Wildes, MD, of the Washington University School of Medicine in St Louis, Missouri.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health.”
Dr Wildes and her colleagues reported these results in JCO Clinical Cancer Informatics.
Creating the index
The researchers began this study with data from 2,692,361 patients without cancer who were older than 66 years of age. The data were collected from the Medicare Health Outcomes Survey (MHOS), which is used to annually collect self-reported symptoms, functional status, and health-related quality of life data from Medicare beneficiaries enrolled in Medicare Advantage plans.
The researchers used the MHOS data to create a deficit accumulation frailty index made up of a 25-item scale and scoring system. The index includes criteria in 5 categories for scoring frailty:
- Activities of daily living (eg, difficulty dressing or eating)
- Chronic health conditions
- Functioning (eg, difficulty walking or climbing several sets of stairs)
- General health
- Mental health.
Patients whose scores exceed a certain threshold on the scale are classified as frail.
Applying the index
The researchers applied their frailty index to 305 patients with newly diagnosed MM. Data from these patients were obtained from the Surveillance, Epidemiology, and End Results (SEER)-MHOS linked database. In this dataset, data from MHOS are linked to demographics, tumor characteristics, and survival for individuals with a cancer diagnosis who reside in the coverage area of the 14 registries participating in the SEER-MHOS linkage.
The researchers compared findings in the MM patients to findings in the patients without cancer.
In the non-cancer patients, the median age was 74, and the mean frailty score was 0.23. In the MM patients, the median age was 76, and the mean frailty score was 0.28.
Chronological age was weakly correlated with a higher frailty score in MM patients. However, for non-cancer patients, an increase in chronological age was strongly correlated with a higher frailty score.
Among non-cancer patients, each 10% increase in frailty score was associated with a 40% increased risk for death (adjusted hazard ratio, 1.397; P<0.001).
Among MM patients, each 10% increase in frailty score was associated with a 16% increased risk of death (adjusted hazard ratio, 1.159; P<0.001).
The median OS was 33 months for the entire MM cohort, 26.8 months for frail MM patients, and 43.7 months for non-frail MM patients (P=0.015 for the frail to non-frail comparison).
“These findings underscore the need to place more consideration on biological age versus chronological age in multiple myeloma, recognizing that frailty is dynamic and encompasses many factors beyond the disease itself,” Dr Wildes said.
“Ultimately, the hope is that this tool will help us to better personalize care based on a fuller picture of our patients’ health so that we are not under-treating an older adult who can tolerate a more intense therapy or over-treating one who’s going to be vulnerable to the toxicities of therapy.”
Limitations and next steps
The researchers believe there are several options for optimizing the data in the frailty index, including turning it into a computerized program and examining patients who are not newly diagnosed and have subsequent relapses, disease burden, and treatment toxicities.
This study is limited in the fact that researchers only assessed OS and not progression-free survival, chemotherapy toxicity, or hospitalization rates.
Additionally, the MM data was derived from patients enrolled in the Medicare Advantage program, which may have contributed to selecting participants who are, overall, lower-risk due to the way the program incentivizes lower-cost enrollees.
Researchers say they have developed a frailty index that can predict overall survival (OS) in patients newly diagnosed with multiple myeloma (MM).
An increasing frailty index score was significantly associated with an increased risk of death in these patients, and frailty retained a significant association with OS even after the researchers controlled for patients’ chronological age.
“Our goal was to create a tool that could be widely applied using data sources at hand and that helps doctors provide better informed treatment recommendations for their patients,” said Tanya S. Wildes, MD, of the Washington University School of Medicine in St Louis, Missouri.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health.”
Dr Wildes and her colleagues reported these results in JCO Clinical Cancer Informatics.
Creating the index
The researchers began this study with data from 2,692,361 patients without cancer who were older than 66 years of age. The data were collected from the Medicare Health Outcomes Survey (MHOS), which is used to annually collect self-reported symptoms, functional status, and health-related quality of life data from Medicare beneficiaries enrolled in Medicare Advantage plans.
The researchers used the MHOS data to create a deficit accumulation frailty index made up of a 25-item scale and scoring system. The index includes criteria in 5 categories for scoring frailty:
- Activities of daily living (eg, difficulty dressing or eating)
- Chronic health conditions
- Functioning (eg, difficulty walking or climbing several sets of stairs)
- General health
- Mental health.
Patients whose scores exceed a certain threshold on the scale are classified as frail.
Applying the index
The researchers applied their frailty index to 305 patients with newly diagnosed MM. Data from these patients were obtained from the Surveillance, Epidemiology, and End Results (SEER)-MHOS linked database. In this dataset, data from MHOS are linked to demographics, tumor characteristics, and survival for individuals with a cancer diagnosis who reside in the coverage area of the 14 registries participating in the SEER-MHOS linkage.
The researchers compared findings in the MM patients to findings in the patients without cancer.
In the non-cancer patients, the median age was 74, and the mean frailty score was 0.23. In the MM patients, the median age was 76, and the mean frailty score was 0.28.
Chronological age was weakly correlated with a higher frailty score in MM patients. However, for non-cancer patients, an increase in chronological age was strongly correlated with a higher frailty score.
Among non-cancer patients, each 10% increase in frailty score was associated with a 40% increased risk for death (adjusted hazard ratio, 1.397; P<0.001).
Among MM patients, each 10% increase in frailty score was associated with a 16% increased risk of death (adjusted hazard ratio, 1.159; P<0.001).
The median OS was 33 months for the entire MM cohort, 26.8 months for frail MM patients, and 43.7 months for non-frail MM patients (P=0.015 for the frail to non-frail comparison).
“These findings underscore the need to place more consideration on biological age versus chronological age in multiple myeloma, recognizing that frailty is dynamic and encompasses many factors beyond the disease itself,” Dr Wildes said.
“Ultimately, the hope is that this tool will help us to better personalize care based on a fuller picture of our patients’ health so that we are not under-treating an older adult who can tolerate a more intense therapy or over-treating one who’s going to be vulnerable to the toxicities of therapy.”
Limitations and next steps
The researchers believe there are several options for optimizing the data in the frailty index, including turning it into a computerized program and examining patients who are not newly diagnosed and have subsequent relapses, disease burden, and treatment toxicities.
This study is limited in the fact that researchers only assessed OS and not progression-free survival, chemotherapy toxicity, or hospitalization rates.
Additionally, the MM data was derived from patients enrolled in the Medicare Advantage program, which may have contributed to selecting participants who are, overall, lower-risk due to the way the program incentivizes lower-cost enrollees.
Researchers say they have developed a frailty index that can predict overall survival (OS) in patients newly diagnosed with multiple myeloma (MM).
An increasing frailty index score was significantly associated with an increased risk of death in these patients, and frailty retained a significant association with OS even after the researchers controlled for patients’ chronological age.
“Our goal was to create a tool that could be widely applied using data sources at hand and that helps doctors provide better informed treatment recommendations for their patients,” said Tanya S. Wildes, MD, of the Washington University School of Medicine in St Louis, Missouri.
“Our results demonstrate that, for patients with multiple myeloma, chronological age alone is not a good measure for assessing overall health.”
Dr Wildes and her colleagues reported these results in JCO Clinical Cancer Informatics.
Creating the index
The researchers began this study with data from 2,692,361 patients without cancer who were older than 66 years of age. The data were collected from the Medicare Health Outcomes Survey (MHOS), which is used to annually collect self-reported symptoms, functional status, and health-related quality of life data from Medicare beneficiaries enrolled in Medicare Advantage plans.
The researchers used the MHOS data to create a deficit accumulation frailty index made up of a 25-item scale and scoring system. The index includes criteria in 5 categories for scoring frailty:
- Activities of daily living (eg, difficulty dressing or eating)
- Chronic health conditions
- Functioning (eg, difficulty walking or climbing several sets of stairs)
- General health
- Mental health.
Patients whose scores exceed a certain threshold on the scale are classified as frail.
Applying the index
The researchers applied their frailty index to 305 patients with newly diagnosed MM. Data from these patients were obtained from the Surveillance, Epidemiology, and End Results (SEER)-MHOS linked database. In this dataset, data from MHOS are linked to demographics, tumor characteristics, and survival for individuals with a cancer diagnosis who reside in the coverage area of the 14 registries participating in the SEER-MHOS linkage.
The researchers compared findings in the MM patients to findings in the patients without cancer.
In the non-cancer patients, the median age was 74, and the mean frailty score was 0.23. In the MM patients, the median age was 76, and the mean frailty score was 0.28.
Chronological age was weakly correlated with a higher frailty score in MM patients. However, for non-cancer patients, an increase in chronological age was strongly correlated with a higher frailty score.
Among non-cancer patients, each 10% increase in frailty score was associated with a 40% increased risk for death (adjusted hazard ratio, 1.397; P<0.001).
Among MM patients, each 10% increase in frailty score was associated with a 16% increased risk of death (adjusted hazard ratio, 1.159; P<0.001).
The median OS was 33 months for the entire MM cohort, 26.8 months for frail MM patients, and 43.7 months for non-frail MM patients (P=0.015 for the frail to non-frail comparison).
“These findings underscore the need to place more consideration on biological age versus chronological age in multiple myeloma, recognizing that frailty is dynamic and encompasses many factors beyond the disease itself,” Dr Wildes said.
“Ultimately, the hope is that this tool will help us to better personalize care based on a fuller picture of our patients’ health so that we are not under-treating an older adult who can tolerate a more intense therapy or over-treating one who’s going to be vulnerable to the toxicities of therapy.”
Limitations and next steps
The researchers believe there are several options for optimizing the data in the frailty index, including turning it into a computerized program and examining patients who are not newly diagnosed and have subsequent relapses, disease burden, and treatment toxicities.
This study is limited in the fact that researchers only assessed OS and not progression-free survival, chemotherapy toxicity, or hospitalization rates.
Additionally, the MM data was derived from patients enrolled in the Medicare Advantage program, which may have contributed to selecting participants who are, overall, lower-risk due to the way the program incentivizes lower-cost enrollees.
Plasma transfusion during air transport can reduce mortality
Receiving a plasma transfusion during emergency air transport can improve survival for trauma patients, according to a study published in NEJM.
Trauma patients with severe bleeding had a significant decrease in 30-day mortality when they received a plasma transfusion while being airlifted to a hospital.
Transfusion-related reactions and allergic reactions were more common among plasma recipients than patients who only received standard care.
However, this difference was not significant, and most of these reactions were considered minor.
“These results have the power to significantly alter trauma resuscitation, and their importance to the trauma community cannot be overstated,” said study author Jason Sperry, MD, of the University of Pittsburgh School of Medicine in Pennsylvania.
“This is the first trial in a quarter century to have the potential to alter prehospital care so considerably.”
Patients and intervention
This trial, known as PAMPer (Prehospital Air Medical Plasma), was a phase 3, randomized study enrolling 501 trauma patients at risk of hemorrhagic shock.
Most patients were male (72.7%), and most had suffered blunt trauma (82.4%). About half of patients (51.1%) had prehospital intubation, and more than a third (34.7%) received a prehospital transfusion of red blood cells.
Air medical bases participating in this study were randomized to administer plasma or standard care to eligible patients for 1-month intervals. When the air transport teams were in their plasma interval, they’d begin administering 2 units of thawed plasma to a patient as soon as trial eligibility was confirmed.
If the 2 units were completed during the flight, the team would revert to standard care. If the transfusions weren’t completed, the plasma would continue to be administered when the patient arrived at the trauma center.
The teams administered the assigned treatment 99% of the time (496/501).
In the plasma group, there were 205 patients (89.1%) who received 2 units of plasma, 21 (9.1%) who received 1 unit, and 4 patients (1.7%) who did not receive plasma due to logistical challenges.
In 84.4% of the patients, the plasma infusion was completed during air transport. The remaining patients completed their plasma transfusions at the trauma center.
There was 1 patient (0.4%) in the standard-care group who received plasma before transport began.
Primary outcome
The study’s primary outcome was 30-day mortality. Ninety-six percent of patients (n=481) had data for this outcome—220 patients in the plasma group and 261 in the standard-care group.
Thirty-day mortality was significantly lower in the plasma group than the standard-care group—23.2% and 33.0%, respectively (P=0.03).
In an adjusted analysis, the administration of prehospital plasma was associated with a 39% lower risk for 30-day mortality than standard care (adjusted odds ratio, 0.61; P=0.02).
Secondary outcomes
Initially, there were significant differences between the plasma (n=230) and standard-care groups (n=271) when it came to:
- Mortality at 24 hours—13.9% and 22.1%, respectively (P=0.02)
- In-hospital mortality—22.2% and 32.5%, respectively (P=0.01)
- Median volume of blood components transfused in the first 24 hours—3 and 4 units, respectively (P=0.02)
- Median volume of red cells transfused in the first 24 hours—3 and 4 units, respectively (P=0.03).
- Median prothrombin-time ratio at first blood sampling—1.2 and 1.3, respectively (P<0.001).
When the researchers adjusted P values for multiple comparisons, the between-group difference in prothrombin-time ratio remained significant (P<0.001).
However, the differences in 24-hour mortality (P=0.55), in-hospital mortality (P=0.33), blood components transfused (P=0.41), and red cells transfused (P=0.69) did not retain significance.
Likewise, there were no significant between-group differences (in adjusted or unadjusted analyses) when it came to multi-organ failure, acute lung injury/acute respiratory distress syndrome, nosocomial infections, or allergic/transfusion-related reactions.
There were 10 adverse events (AEs) considered related to the trial regimen. In the standard-care group, the 4 AEs were sepsis (a serious AE), adult respiratory distress syndrome (a serious AE), fever, and pain.
In the plasma group, the 6 AEs were 2 allergic reactions, 1 case of anaphylaxis, 1 case of hypotension, 1 case of urticaria, and 1 transfusion-related reaction (a serious AE).
Receiving a plasma transfusion during emergency air transport can improve survival for trauma patients, according to a study published in NEJM.
Trauma patients with severe bleeding had a significant decrease in 30-day mortality when they received a plasma transfusion while being airlifted to a hospital.
Transfusion-related reactions and allergic reactions were more common among plasma recipients than patients who only received standard care.
However, this difference was not significant, and most of these reactions were considered minor.
“These results have the power to significantly alter trauma resuscitation, and their importance to the trauma community cannot be overstated,” said study author Jason Sperry, MD, of the University of Pittsburgh School of Medicine in Pennsylvania.
“This is the first trial in a quarter century to have the potential to alter prehospital care so considerably.”
Patients and intervention
This trial, known as PAMPer (Prehospital Air Medical Plasma), was a phase 3, randomized study enrolling 501 trauma patients at risk of hemorrhagic shock.
Most patients were male (72.7%), and most had suffered blunt trauma (82.4%). About half of patients (51.1%) had prehospital intubation, and more than a third (34.7%) received a prehospital transfusion of red blood cells.
Air medical bases participating in this study were randomized to administer plasma or standard care to eligible patients for 1-month intervals. When the air transport teams were in their plasma interval, they’d begin administering 2 units of thawed plasma to a patient as soon as trial eligibility was confirmed.
If the 2 units were completed during the flight, the team would revert to standard care. If the transfusions weren’t completed, the plasma would continue to be administered when the patient arrived at the trauma center.
The teams administered the assigned treatment 99% of the time (496/501).
In the plasma group, there were 205 patients (89.1%) who received 2 units of plasma, 21 (9.1%) who received 1 unit, and 4 patients (1.7%) who did not receive plasma due to logistical challenges.
In 84.4% of the patients, the plasma infusion was completed during air transport. The remaining patients completed their plasma transfusions at the trauma center.
There was 1 patient (0.4%) in the standard-care group who received plasma before transport began.
Primary outcome
The study’s primary outcome was 30-day mortality. Ninety-six percent of patients (n=481) had data for this outcome—220 patients in the plasma group and 261 in the standard-care group.
Thirty-day mortality was significantly lower in the plasma group than the standard-care group—23.2% and 33.0%, respectively (P=0.03).
In an adjusted analysis, the administration of prehospital plasma was associated with a 39% lower risk for 30-day mortality than standard care (adjusted odds ratio, 0.61; P=0.02).
Secondary outcomes
Initially, there were significant differences between the plasma (n=230) and standard-care groups (n=271) when it came to:
- Mortality at 24 hours—13.9% and 22.1%, respectively (P=0.02)
- In-hospital mortality—22.2% and 32.5%, respectively (P=0.01)
- Median volume of blood components transfused in the first 24 hours—3 and 4 units, respectively (P=0.02)
- Median volume of red cells transfused in the first 24 hours—3 and 4 units, respectively (P=0.03).
- Median prothrombin-time ratio at first blood sampling—1.2 and 1.3, respectively (P<0.001).
When the researchers adjusted P values for multiple comparisons, the between-group difference in prothrombin-time ratio remained significant (P<0.001).
However, the differences in 24-hour mortality (P=0.55), in-hospital mortality (P=0.33), blood components transfused (P=0.41), and red cells transfused (P=0.69) did not retain significance.
Likewise, there were no significant between-group differences (in adjusted or unadjusted analyses) when it came to multi-organ failure, acute lung injury/acute respiratory distress syndrome, nosocomial infections, or allergic/transfusion-related reactions.
There were 10 adverse events (AEs) considered related to the trial regimen. In the standard-care group, the 4 AEs were sepsis (a serious AE), adult respiratory distress syndrome (a serious AE), fever, and pain.
In the plasma group, the 6 AEs were 2 allergic reactions, 1 case of anaphylaxis, 1 case of hypotension, 1 case of urticaria, and 1 transfusion-related reaction (a serious AE).
Receiving a plasma transfusion during emergency air transport can improve survival for trauma patients, according to a study published in NEJM.
Trauma patients with severe bleeding had a significant decrease in 30-day mortality when they received a plasma transfusion while being airlifted to a hospital.
Transfusion-related reactions and allergic reactions were more common among plasma recipients than patients who only received standard care.
However, this difference was not significant, and most of these reactions were considered minor.
“These results have the power to significantly alter trauma resuscitation, and their importance to the trauma community cannot be overstated,” said study author Jason Sperry, MD, of the University of Pittsburgh School of Medicine in Pennsylvania.
“This is the first trial in a quarter century to have the potential to alter prehospital care so considerably.”
Patients and intervention
This trial, known as PAMPer (Prehospital Air Medical Plasma), was a phase 3, randomized study enrolling 501 trauma patients at risk of hemorrhagic shock.
Most patients were male (72.7%), and most had suffered blunt trauma (82.4%). About half of patients (51.1%) had prehospital intubation, and more than a third (34.7%) received a prehospital transfusion of red blood cells.
Air medical bases participating in this study were randomized to administer plasma or standard care to eligible patients for 1-month intervals. When the air transport teams were in their plasma interval, they’d begin administering 2 units of thawed plasma to a patient as soon as trial eligibility was confirmed.
If the 2 units were completed during the flight, the team would revert to standard care. If the transfusions weren’t completed, the plasma would continue to be administered when the patient arrived at the trauma center.
The teams administered the assigned treatment 99% of the time (496/501).
In the plasma group, there were 205 patients (89.1%) who received 2 units of plasma, 21 (9.1%) who received 1 unit, and 4 patients (1.7%) who did not receive plasma due to logistical challenges.
In 84.4% of the patients, the plasma infusion was completed during air transport. The remaining patients completed their plasma transfusions at the trauma center.
There was 1 patient (0.4%) in the standard-care group who received plasma before transport began.
Primary outcome
The study’s primary outcome was 30-day mortality. Ninety-six percent of patients (n=481) had data for this outcome—220 patients in the plasma group and 261 in the standard-care group.
Thirty-day mortality was significantly lower in the plasma group than the standard-care group—23.2% and 33.0%, respectively (P=0.03).
In an adjusted analysis, the administration of prehospital plasma was associated with a 39% lower risk for 30-day mortality than standard care (adjusted odds ratio, 0.61; P=0.02).
Secondary outcomes
Initially, there were significant differences between the plasma (n=230) and standard-care groups (n=271) when it came to:
- Mortality at 24 hours—13.9% and 22.1%, respectively (P=0.02)
- In-hospital mortality—22.2% and 32.5%, respectively (P=0.01)
- Median volume of blood components transfused in the first 24 hours—3 and 4 units, respectively (P=0.02)
- Median volume of red cells transfused in the first 24 hours—3 and 4 units, respectively (P=0.03).
- Median prothrombin-time ratio at first blood sampling—1.2 and 1.3, respectively (P<0.001).
When the researchers adjusted P values for multiple comparisons, the between-group difference in prothrombin-time ratio remained significant (P<0.001).
However, the differences in 24-hour mortality (P=0.55), in-hospital mortality (P=0.33), blood components transfused (P=0.41), and red cells transfused (P=0.69) did not retain significance.
Likewise, there were no significant between-group differences (in adjusted or unadjusted analyses) when it came to multi-organ failure, acute lung injury/acute respiratory distress syndrome, nosocomial infections, or allergic/transfusion-related reactions.
There were 10 adverse events (AEs) considered related to the trial regimen. In the standard-care group, the 4 AEs were sepsis (a serious AE), adult respiratory distress syndrome (a serious AE), fever, and pain.
In the plasma group, the 6 AEs were 2 allergic reactions, 1 case of anaphylaxis, 1 case of hypotension, 1 case of urticaria, and 1 transfusion-related reaction (a serious AE).
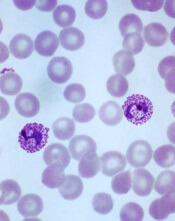
Drug receives fast track designation for WM
The US Food and Drug Administration (FDA) has granted fast track designation to zanubrutinib for the treatment of Waldenström’s macroglobulinemia (WM).
Zanubrutinib (BGB-3111) is a BTK inhibitor being developed by BeiGene to treat various B-cell malignancies.
BeiGene is preparing to submit to the FDA, in the first half of 2019, a new drug application seeking accelerated approval of zanubrutinib for patients with WM.
The application will be supported by results from a phase 1 study. Results from this trial were presented at the 14th International Conference on Malignant Lymphoma (14-ICML) last year.
Researchers are also evaluating zanubrutinib in phase 2 (NCT03332173) and phase 3 (NCT03053440) trials of WM patients. In the phase 3 trial, researchers are comparing zanubrutinib to the BTK inhibitor ibrutinib.
Phase 1 results
As of March 31, 2017, 48 WM patients were enrolled in the phase 1 study. Thirty-eight patients had relapsed/refractory disease, and 10 patients were treatment-naïve.
There was a dose-escalation phase and a dose-expansion phase. The dose-expansion phase included doses of 160 mg twice a day or 320 mg once a day.
The most common (>10%) adverse events, (AEs) of any attribution were petechiae/purpura/contusion (35%), upper respiratory tract infection (31%), constipation (25%), diarrhea (19%), epistaxis (19%), nausea (17%), cough (15%), anemia (15%), headache (15%), neutropenia (13%), and rash (13%).
Most of these events were grade 1 or 2 in severity. The exceptions were grade 3/4 anemia and neutropenia (8% each) as well as grade 3/4 diarrhea and headache (2% each).
Five serious AEs were considered possibly related to zanubrutinib—1 case each of hemothorax, atrial fibrillation, colitis, febrile neutropenia, and headache. Three AEs led to treatment discontinuation—1 case each of bronchiectasis, prostate adenocarcinoma, and adenocarcinoma of pylorus.
At the time of the data cutoff, 42 patients were evaluable for response. At a median follow-up of 12.3 months (range, 4.4 to 30.5 months), the overall response rate was 90% (38/42).
The major response rate was 76% (32/42), with very good partial responses in 43% (18/42) of patients and partial responses in 33% (14/42) of patients. There were no complete responses and 2 cases of disease progression.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to zanubrutinib for the treatment of Waldenström’s macroglobulinemia (WM).
Zanubrutinib (BGB-3111) is a BTK inhibitor being developed by BeiGene to treat various B-cell malignancies.
BeiGene is preparing to submit to the FDA, in the first half of 2019, a new drug application seeking accelerated approval of zanubrutinib for patients with WM.
The application will be supported by results from a phase 1 study. Results from this trial were presented at the 14th International Conference on Malignant Lymphoma (14-ICML) last year.
Researchers are also evaluating zanubrutinib in phase 2 (NCT03332173) and phase 3 (NCT03053440) trials of WM patients. In the phase 3 trial, researchers are comparing zanubrutinib to the BTK inhibitor ibrutinib.
Phase 1 results
As of March 31, 2017, 48 WM patients were enrolled in the phase 1 study. Thirty-eight patients had relapsed/refractory disease, and 10 patients were treatment-naïve.
There was a dose-escalation phase and a dose-expansion phase. The dose-expansion phase included doses of 160 mg twice a day or 320 mg once a day.
The most common (>10%) adverse events, (AEs) of any attribution were petechiae/purpura/contusion (35%), upper respiratory tract infection (31%), constipation (25%), diarrhea (19%), epistaxis (19%), nausea (17%), cough (15%), anemia (15%), headache (15%), neutropenia (13%), and rash (13%).
Most of these events were grade 1 or 2 in severity. The exceptions were grade 3/4 anemia and neutropenia (8% each) as well as grade 3/4 diarrhea and headache (2% each).
Five serious AEs were considered possibly related to zanubrutinib—1 case each of hemothorax, atrial fibrillation, colitis, febrile neutropenia, and headache. Three AEs led to treatment discontinuation—1 case each of bronchiectasis, prostate adenocarcinoma, and adenocarcinoma of pylorus.
At the time of the data cutoff, 42 patients were evaluable for response. At a median follow-up of 12.3 months (range, 4.4 to 30.5 months), the overall response rate was 90% (38/42).
The major response rate was 76% (32/42), with very good partial responses in 43% (18/42) of patients and partial responses in 33% (14/42) of patients. There were no complete responses and 2 cases of disease progression.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to zanubrutinib for the treatment of Waldenström’s macroglobulinemia (WM).
Zanubrutinib (BGB-3111) is a BTK inhibitor being developed by BeiGene to treat various B-cell malignancies.
BeiGene is preparing to submit to the FDA, in the first half of 2019, a new drug application seeking accelerated approval of zanubrutinib for patients with WM.
The application will be supported by results from a phase 1 study. Results from this trial were presented at the 14th International Conference on Malignant Lymphoma (14-ICML) last year.
Researchers are also evaluating zanubrutinib in phase 2 (NCT03332173) and phase 3 (NCT03053440) trials of WM patients. In the phase 3 trial, researchers are comparing zanubrutinib to the BTK inhibitor ibrutinib.
Phase 1 results
As of March 31, 2017, 48 WM patients were enrolled in the phase 1 study. Thirty-eight patients had relapsed/refractory disease, and 10 patients were treatment-naïve.
There was a dose-escalation phase and a dose-expansion phase. The dose-expansion phase included doses of 160 mg twice a day or 320 mg once a day.
The most common (>10%) adverse events, (AEs) of any attribution were petechiae/purpura/contusion (35%), upper respiratory tract infection (31%), constipation (25%), diarrhea (19%), epistaxis (19%), nausea (17%), cough (15%), anemia (15%), headache (15%), neutropenia (13%), and rash (13%).
Most of these events were grade 1 or 2 in severity. The exceptions were grade 3/4 anemia and neutropenia (8% each) as well as grade 3/4 diarrhea and headache (2% each).
Five serious AEs were considered possibly related to zanubrutinib—1 case each of hemothorax, atrial fibrillation, colitis, febrile neutropenia, and headache. Three AEs led to treatment discontinuation—1 case each of bronchiectasis, prostate adenocarcinoma, and adenocarcinoma of pylorus.
At the time of the data cutoff, 42 patients were evaluable for response. At a median follow-up of 12.3 months (range, 4.4 to 30.5 months), the overall response rate was 90% (38/42).
The major response rate was 76% (32/42), with very good partial responses in 43% (18/42) of patients and partial responses in 33% (14/42) of patients. There were no complete responses and 2 cases of disease progression.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
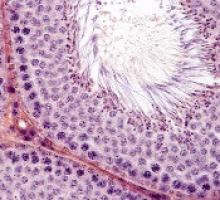
Treatments, disease affect spermatogonia in boys
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Alkylating agents, hydroxyurea (HU), and certain non-malignant diseases can significantly deplete spermatogonial cell counts in young boys, according to research published in Human Reproduction.
Boys who received alkylating agents to treat cancer had significantly lower spermatogonial cell counts than control subjects or boys with malignant/nonmalignant diseases treated with non-alkylating agents.
Five of 6 SCD patients treated with HU had a totally depleted spermatogonial pool, and the remaining patient had a low spermatogonial cell count.
Five boys with non-malignant diseases who were not exposed to chemotherapy had significantly lower spermatogonial cell counts than controls.
“Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated,” said study author Cecilia Petersen, MD, PhD, of Karolinska Institutet and University Hospital in Stockholm, Sweden.
“This needs to be communicated to physicians as well as patients and their parents or carers. However, until sperm that are able to fertilize eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
Dr Petersen and her colleagues also noted that preserving testicular tissue may not be a viable option for boys who have low spermatogonial cell counts prior to treatment.
Patients and controls
For this study, the researchers analyzed testicular tissue from 32 boys facing treatments that carried a high risk of infertility—testicular irradiation, chemotherapy, or radiotherapy in advance of stem cell transplant.
Twenty boys had the tissue taken after initial chemotherapy, and 12 had it taken before starting any treatment.1
Eight patients had received chemotherapy with non-alkylating agents, 6 (all with malignancies) had received alkylating agents, and 6 (all with SCD) had received HU.
Diseases included acute lymphoblastic leukemia (n=6), SCD (n=6), acute myeloid leukemia (n=3), thalassemia major (n=3), neuroblastoma (n=2), juvenile myelomonocytic leukemia (n=2), myelodysplastic syndromes (n=2), primary immunodeficiency (n=2), Wilms tumor (n=1), adrenoleukodystrophy (n=1), hepatoblastoma (n=1), primitive neuroectodermal tumor (n=1), severe aplastic anemia (n=1), and Fanconi anemia (n=1).
The researchers compared samples from these 32 patients to 14 healthy testicular tissue samples stored in the biobank at the Karolinska University Hospital.
For both sample types, the team counted the number of spermatogonial cells found in a cross-section of seminiferous tubules.
“We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained study author Jan-Bernd Stukenborg, PhD, of Karolinska Institutet and University Hospital.
Impact of treatment
There was no significant difference in the mean quantity of spermatogonia per transverse tubular cross-section (S/T) between patients exposed to non-alkylating agents (1.7 ± 1.0, n=8) and biobank controls (4.1 ± 4.6, n=14).
However, samples from patients who received alkylating agents had a significantly lower mean S/T value (0.2 ± 0.3, n=6) than samples from patients treated with non-alkylating agents (P=0.003) and biobank controls (P<0.001).
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to 0 in patients treated with alkylating agents,” Dr Stukenborg said.
Samples from the SCD patients also had a significantly lower mean S/T value (0.3 ± 0.6, n=6) than biobank controls (P=0.003).
Dr Stukenborg noted that the germ cell pool was totally depleted in 5 of the boys with SCD, and the pool was “very low” in the sixth SCD patient.
“This was not seen in patients who had not started treatment or were treated with non-alkylating agents or in the biobank tissues,” Dr Stukenborg said.2
He and his colleagues noted that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but high doses of alkylating agents and radiotherapy to the testicles are strongly associated with permanent or long-term infertility.
“The first group of boys who received bone marrow transplants are now reaching their thirties,” said study author Kirsi Jahnukainen, MD, PhD, of Helsinki University Central Hospital in Finland.
“Recent data suggest they may have a high chance of their sperm production recovering, even if they received high-dose alkylating therapies, so long as they had no testicular irradiation.”
Impact of disease
The researchers also found evidence to suggest that, for some boys, their disease may have affected spermatogonial cell counts before any treatment began.
Five patients with non-malignant disease who had not been exposed to chemotherapy (3 with thalassemia major, 1 with Fanconi anemia, and 1 with primary immunodeficiency) had a significantly lower mean S/T value (0.4 ± 0.5) than controls (P=0.006).
“Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age,” Dr Jahnukainen said.
“This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers noted that a limitation of this study was that biobank samples had no detailed information regarding previous medical treatments and testicular volumes.
1. Testicular tissue is taken from patients under general anesthesia. The surgeon removes approximately 20% of the tissue from the testicular capsule in one of the testicles. For this study, a third of the tissue was taken to the Karolinska Institutet for analysis.
2. A recent meta-analysis showed that normal testicular tissue samples of newborns contain approximately 2.5 germ cells per tubular cross-section. This number decreases to approximately 1.2 within the first 3 years of age, followed by an increase up to 2.6 germ cells per tubular cross-section at 6 to 7 years, reaching a plateau until the age of 11. At the onset of puberty, an increase of up to 7 spermatogonia per tubular cross-section could be observed.
Fitness trackers help monitor cancer patients
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
A small study suggests fitness trackers can be used to assess the quality of life and daily functioning of cancer patients during treatment.
Results indicated that objective data collected from these wearable activity monitors can supplement current assessments of health status and physical function.
This is important because current assessments are limited by their subjectivity and potential for bias, according to Gillian Gresham, PhD, of Cedars-Sinai Medical Center in Los Angeles, California.
Dr Gresham and her colleagues conducted this study and reported the results in npj Digital Medicine.
“One of the challenges in treating patients with advanced cancer is obtaining ongoing, timely, objective data about their physical status during therapy,” said study author Andrew Hendifar, MD, of Cedars-Sinai.
“After all, patients typically spend most of their time at home or work, not in a clinic, and their health statuses change from day to day.”
With this in mind, the researchers studied 37 patients undergoing treatment for advanced cancer at Cedars-Sinai.
The patients wore wrist-mounted fitness trackers throughout the study except when showering or swimming. These devices log the wearer’s step counts, stairs climbed, calories, heart rate, and sleep.
Sets of activity data were collected for 3 consecutive visits during treatment. After the final clinical visit, patients were followed for 6 months to gather additional clinical and survival outcomes.
The researchers compared data from the trackers with patients’ assessments of their own symptoms, including pain, fatigue, and sleep quality, as collected from a National Institutes of Health questionnaire.
These data sets were also compared with Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) scores.
Results
Patients had a median age of 62 (range, 34-81), about 54% were male, and most (73%) had pancreatic cancer. On average, the patients walked 3700 steps (1.7 miles) per day, climbed 3 flights of stairs per day, and slept 8 hours per night.
The researchers found that activity metrics correlated with ECOG-PS and KPS scores. As scores increased, daily steps and flights of stairs decreased.
The team said the largest correlation coefficients (r) were observed between average steps and increasing ECOG-PS (r=0.63, P<0.01) and KPS (r=0.69, P<0.01) scores.
Patient-reported outcomes also correlated with activity metrics. Average steps were significantly (P<0.05 for all) associated with physical functioning (r=0.57), pain (r=—0.46), and fatigue (r=—0.53). There were significant associations for distance walked and stairs climbed as well.
Finally, the researchers observed an association between activity and grade 3/4 adverse events, hospitalizations, and survival.
An increase of 1000 steps per day, on average, was associated with significantly lower odds of hospitalization (odds ratio: 0.21, 95% CI 0.56, 0.79) and grade 3/4 adverse events (odds ratio: 0.34, 95% CI 0.13, 0.94) as well as increased survival (hazard ratio: 0.48, 95% CI 0.28, 0.83).
“Data gathered through advancements in technology has the potential to help physicians measure the impact of a particular treatment on a patient’s daily functioning,” Dr Gresham said. “Furthermore, continuous activity monitoring may help predict and monitor treatment complications and allow for more timely and appropriate interventions.”
As a next step, the researchers plan to study long-term use of activity monitors in a larger, more diverse group of advanced cancer patients and correlate that data with clinical and self-reported outcomes.
“Our hope is that findings from future studies with wearable activity monitors could lead to development of individualized treatment and exercise plans that may result in increased treatment tolerability and improved survival outcomes for patients,” Dr Hendifar said.
NIH aims to improve access to cloud computing
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
The National Institutes of Health (NIH) is attempting to improve biomedical researchers’ access to cloud computing.
With its new STRIDES* initiative, the NIH intends to establish partnerships with commercial cloud service providers (CSPs) to reduce economic and technological barriers to accessing and computing on large biomedical data sets.
The CSPs will work with the NIH and its funded researchers to develop and test new ways to make large data sets and associated computational tools available to wider audiences.
The NIH’s initial efforts with the STRIDES initiative will focus on making NIH high-value data sets more accessible through the cloud, leveraging partnerships with CSPs to take advantage of data-related innovations such as machine learning and artificial intelligence, and experimenting with new ways to optimize technology-intensive research.
The goals of the STRIDES initiative are to:
- Support researchers’ transition to conducting biomedical research using commercial cloud technologies through cost-effective storage and computing arrangements with CSPs
- Provide NIH researchers access to and training on new and emerging cloud-based tools and services
- Facilitate researchers’ access to and use of high-value NIH research data that are currently stored on, or will be moved into, cloud environments
- Enable the formation of an interconnected ecosystem that breaks down silos related to generating, analyzing, and sharing research data.
The NIH has already partnered with Google Cloud for the STRIDES initiative, but the agency hopes to create partnerships with other CSPs as well.
“NIH is in a unique position to bring together academic and innovation industry partners to create a biomedical data ecosystem that maximizes the use of NIH-supported biomedical research data for the greatest benefit to human health,” said NIH Principal Deputy Director Lawrence A. Tabak, DDS, PhD.
The NIH says its agreement with Google Cloud creates a cost-efficient framework for NIH researchers, as well as researchers receiving NIH support, to make use of Google Cloud’s storage, computing, and machine learning technologies.
The partnership will also enable the creation of training programs for researchers at NIH-funded institutions on how to use the Google Cloud platform. And the partnership will involve collaboration with NIH’s Data Commons Pilot—a group of projects testing new tools and methods for working with and sharing data in the cloud.
“Through our partnership with NIH, we are bringing the power of data and the cloud to the biomedical research community globally,” said Gregory Moore, MD, PhD, vice-president of healthcare at Google Cloud.
“Together, we are making it easier for scientists and physicians to access and garner insights from NIH-funded data sets with appropriate privacy protections, which will ultimately accelerate biomedical research progress toward finding treatments and cures for the most devastating diseases of our time.”
A central tenet of STRIDES is that data made available through these partnerships will incorporate standards endorsed by the biomedical research community to make data findable, accessible, interoperable, and reusable.
*Science and Technology Research Infrastructure for Discovery, Experimentation, and Sustainability
Drug approved for radical cure of P vivax malaria
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
The US Food and Drug Administration (FDA) has approved tafenoquine (Krintafel) for the radical cure of Plasmodium vivax malaria.
Tafenoquine is a single-dose medicine that is now approved to prevent relapse of P vivax malaria in patients age 16 and older who are receiving appropriate antimalarial therapy for acute P vivax infection.
Tafenoquine is the first new treatment approved for P vivax malaria in more than 60 years.
Tafenoquine is an 8-aminoquinoline derivative with activity against all stages of the P vivax lifecycle, including hypnozoites. The product was first synthesized by scientists at the Walter Reed Army Institute of Research in 1978.
GSK began developing tafenoquine as a potential medicine for malaria more than 20 years ago. In 2008, GSK entered into a collaboration with Medicines for Malaria Venture to develop tafenoquine as an anti-relapse medicine for patients infected with P vivax.
The primary evidence for the clinical efficacy and safety of the 300 mg, single dose of tafenoquine was provided by a pair of phase 3 studies—DETECTIVE (NCT01376167, TAF112582) and GATHER (NCT02216123, TAF116564).
Results from these studies were presented at the 6th International Conference on Plasmodium vivax Research (ICPVR) in 2017 (abstract 63245 and abstract 63246).
DETECTIVE trial
In this double-blind, double-dummy study, researchers evaluated the efficacy, safety, and tolerability of tafenoquine. The trial included 522 patients with P vivax malaria who were randomized to receive one of the following:
- A single dose (1 day) of tafenoquine (300 mg)
- A 14-day course of primaquine (15 mg)
- Placebo.
All patients also received a 3-day course of chloroquine to treat the acute blood stage of the infection.
A significantly greater proportion of patients remained relapse-free over the 6-month follow-up period if they were treated with tafenoquine rather than placebo—60% and 26%, respectively—with an odds ratio for risk of relapse of 0.24 (P<0.001).
Likewise, a significantly greater proportion of patients were relapse-free when treated with primaquine rather than placebo—64% and 26%, respectively—with an odds ratio of 0.20 (P<0.001).
The frequency of adverse events (AEs) was 63% for the tafenoquine group, 59% for the primaquine group, and 65% for the placebo group. The frequency of serious AEs was 8%, 3%, and 5%, respectively.
GATHER trial
This study enrolled 251 patients, ages 16 and older, with microscopy-confirmed parasitemia.
Researchers compared how a single dose of tafenoquine (300 mg) and a 14-day course of primaquine (15 mg) affected hemoglobin levels in these patients. All patients also received a standard 3-day course of chloroquine.
The incidence of decline in hemoglobin (the primary endpoint) was similar between the 2 treatment groups—2.4% in the tafenoquine arm and 1.2% in the primaquine arm. The difference in proportion was 1.23% (95% CI, -4.16%, 4.98%).
None of the patients in this study required a blood transfusion.
The frequency of AEs was 72% for the tafenoquine group and 75% for the primaquine group. The frequency of serious AEs was 4% and 1%, respectively.
Team finds potential therapeutic targets for T-ALL
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
Researchers have found the NOTCH1 pathway “hijacks” heat shock transcription factor 1 (HSF1) signaling in T-cell acute lymphoblastic leukemia (T-ALL).
Therefore, blocking one or more genes in the HSF1 pathway could represent a new approach to treating T-ALL.
An experimental drug, PU-H71, is already in development against one of these targets, heat shock protein 90 (HSP90).
The researchers found that PU-H71 was active against T-ALL in vitro and in vivo.
The team recounted these findings in Nature Medicine.
“Our study shows how the NOTCH1 pathway hijacks the heat shock transcription factor 1 pathway to promote tumor growth,” said study author Iannis Aifantis, PhD, of NYU School of Medicine in New York, New York.
“The cancer cells are sending into overdrive a system that helps healthy cells respond to stress.”
Dr Aifantis and his colleagues found that HSF1 is involved in the pathogenesis of T-ALL. When they knocked down HSF1 in T-ALL cell lines, the researchers observed an increase in apoptosis, defective proteostasis, and a decrease in the growth of leukemic cells.
Similarly, HSF1 was deemed necessary for disease progression in mouse models of T-ALL. When the researchers deleted HSF1, mice experienced “striking” reductions in leukemic burden and “dramatic” improvements in survival. However, HSF1 deletion did not affect normal hematopoiesis.
Dr Aifantis and his colleagues also showed that NOTCH1 regulates the epichaperome in T-ALL. The team said previous studies have shown that, in the presence of oncogenic stress, heat shock proteins participate in a network nucleated by HSP90 and HSP70 chaperones—the epichaperome.
The researchers found that an intact epichaperome was critical for T-ALL by showing that pharmacologic inhibition of HSP90 and HSP70 significantly hindered the growth of human T-ALL in vitro. The team also found the HSP90 inhibitor PU-H71 reduced leukemic burden and extended survival in a NOTCH1-inducible T-ALL mouse model.
Then, the researchers found NOTCH1 levels could predict response to HSP90 inhibition in vitro. T-ALL patient samples expressing high levels of nuclear NOTCH1 and high levels of epichaperome were significantly more sensitive to treatment with PU-H71.
PU-H71 is already in early clinical trials of patients with breast cancer. If further testing proves successful, PU-H71 could be quickly adapted for trials in T-ALL patients, according to Dr Aifantis.
In the meantime, he and his colleagues plan to evaluate the effects of another 8 proteins produced by genes active in the HSF1 pathway to see if any show promising anticancer activity in T-ALL.
GPS receives fast track designation for MM
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted fast track designation to the cancer vaccine galinpepimut-S (GPS) for the treatment of multiple myeloma (MM).
GPS consists of 4 modified peptide chains that induce an innate immune response (CD4+/CD8+ T cells) against the Wilms’ tumor 1 (WT1) antigen.
GPS is administered in combination with an adjuvant and an immune modulator to improve the immune response to the target.
GPS has been tested in a phase 2 trial of patients with MM. Results from this trial were presented at the 44th Annual Meeting of the EBMT in March.
Phase 2 trial
The study enrolled 19 MM patients. Fifteen of them had high-risk cytogenetics at diagnosis, and 18 were at least minimal residual disease-positive after autologous stem cell transplant (ASCT).
Patients began receiving GPS within 22 days of ASCT. Initially, they received 6 doses (administered subcutaneously with the oil emulsifier montanide) every 2 weeks. Injection sites were pre-stimulated with granulocyte-macrophage colony-stimulating factor (70 μg) on days -2 (± 1 day) and 0 of each GPS vaccination.
The patients underwent assessment 2 to 4 weeks after the 6th GPS dose. Then, they received 6 additional monthly doses of GPS in conjunction with lenalidomide maintenance (10 mg daily), starting on day 100 post-ASCT. Patients were assessed 2 to 4 weeks after the 12th GPS dose.
The researchers found that GPS stimulated time-dependent CD4+ or CD8+ T-cell immune responses specific for all 4 WT1 peptides within GPS, 2 of which are heteroclitic.
Immune responses were confirmed in up to 91% of patients, with multivalent immune responses in up to 64% of patients. Three-quarters of patients had multifunctional cross-epitope T-cell reactivity to antigenic epitopes against which the hosts were not specifically immunized, in a pattern akin to epitope spreading.
In patients who received all 12 doses of GPS (n=12), there was a “strong” association between clinical benefit—defined as complete response (CR) or very good partial response (VGPR)—and frequency of CD4/CD8 immune responses.
Of those patients who had achieved CR/VGPR upon completion of GPS treatment, 100% (n=11) had CD4 immune responses, and 81.8% (n=9) had CD8 immune responses.
The median progression-free survival was 23.6 months, and the median overall survival was not reached. At 18 months, the rate of progression-free survival was 62%, and the rate of overall survival was 88%.
About fast track designation
The FDA’s fast track development program is designed to expedite clinical development and submission of applications for products with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the product’s development plan and written communications about issues such as trial design and use of biomarkers.
Products that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met. Such products may also be eligible for rolling review, which allows a developer to submit individual sections of a product’s application for review as they are ready, rather than waiting until all sections are complete.
FDA approves drug for IDH1-mutated AML
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.
The US Food and Drug Administration (FDA) has granted full approval for the isocitrate dehydrogenase-1 (IDH1) inhibitor ivosidenib (Tibsovo®).
The drug is approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) who have an IDH1 mutation, as detected by an FDA-approved test.
Ivosidenib was approved concurrently with the RealTime IDH1 Assay, a companion diagnostic that can detect IDH1 mutation.
The FDA granted approval of ivosidenib to Agios Pharmaceuticals, Inc., and approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA’s approval of ivosidenib was based on data from a single-arm, phase 1 study. Agios received fast track, priority review, and orphan drug designations for ivosidenib.
Safety risks
Ivosidenib must be dispensed with a patient medication guide that describes important information about the drug’s uses and risks.
The prescribing information for ivosidenib includes a Boxed Warning noting that patients treated with ivosidenib have experienced symptoms of differentiation syndrome, which can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, or hepatic, renal, or multi-organ dysfunction.
At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor them closely until symptoms subside.
Ivosidenib also poses a risk of life-threatening QT prolongation and Guillain-Barré syndrome, so patients should be monitored for these adverse events (AEs) as well.
Phase 1 trial
Results from the phase 1 trial of ivosidenib were presented at the 2018 ASCO Annual Meeting and published simultaneously in NEJM. The following data were pulled from the drug’s prescribing information.
Efficacy results were available for 174 adults with relapsed/refractory AML and an IDH1 mutation identified or confirmed by the Abbott RealTime™ IDH1 assay. The patients received ivosidenib at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplant.
The patients had a median age of 67 (range, 18 to 87) and had received a median of 2 prior therapies (range, 1 to 6). Sixty-three percent were refractory to previous therapy, and 33% had secondary AML.
The study’s primary endpoint was the combined rate of complete remission (CR) rate and CR with partial hematologic improvement (CRh).
The CR+CRh rate was 32.8% (57/174), the CR rate was 24.7% (43/174), and the CRh rate was 8% (14/174).
The median duration of CR+CRh was 8.2 months (95% CI 5.6, 12). The median time to best response of CR or CRh was 2.0 months (range, 0.9 to 5.6 months).
Twelve percent of patients (21/174) went on to transplant.
The researchers evaluated the safety of ivosidenib in 179 patients treated with a dose of 500 mg daily. The median duration of exposure to ivosidenib was 3.9 months (range, 0.1 to 39.5 months).
Nineteen percent of patients (34/179) experienced differentiation syndrome. Seventy-nine percent of these patients (27/34) recovered after treatment or ivosidenib dose interruption.
The most frequent serious AEs (>5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolongation (7%). There was one case of progressive multifocal leukoencephalopathy.
The most common AEs leading to dose interruption were QT prolongation (7%), differentiation syndrome (3%), leukocytosis (3%), and dyspnea (3%). AEs leading to a dose reduction included QT prolongation (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%).
AEs leading to permanent discontinuation of ivosidenib included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increase (1%).
For additional data and more details on ivosidenib, see the full prescribing information or visit Tibsovo.com.