User login
Conflicts of interest among FDA advisers
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
An investigative report has unearthed potential conflicts of interest among physicians who serve on advisory panels for the US Food and Drug Administration (FDA).
The investigation revealed that some FDA advisers are receiving significant post-hoc payments from the makers of drugs they reviewed.
The investigation also uncovered relationships between advisers and drug companies that predate drug reviews.
Journalist Charles Piller and his colleagues conducted this investigation and detailed the results in Science.
The report includes data—from the federal Open Payments website—on 107 physicians who voted on FDA advisory committees between 2013 and 2016.
Forty of these advisers received more than $10,000 in post-hoc earnings or research support from the makers of drugs they reviewed or from competing drug companies.
Twenty-six advisers received more than $100,000, and 7 advisers received more than $1 million.
The 17 top earners received more than $300,000 each. For these advisers, 94% of their earnings came from the makers of drugs they previously reviewed or from those companies’ competitors.
The data also show that some advisers received funds from drug companies concurrent with or in the year before their advisory service.
Of the 17 top-earning advisers, 11 received financial support from competing companies on one or more of the drugs they reviewed. Five advisers also received support from the makers of one or more of the drugs reviewed.
The FDA did not disclose this information to the public or issue waivers for these potential conflicts. The FDA can issue a waiver to allow the participation of an adviser with an active conflict or one that ended in the year before a vote, as long as the adviser in question can provide expertise that cannot be provided by someone else.
It is possible that the FDA dismissed the aforementioned financial ties that predated drug reviews, deciding these relationships were not conflicts and did not require a waiver. However, it is also possible that the FDA did not know about these potential conflicts.
Piller and his colleagues were unable to determine what the FDA knew, as the agency refused to release disclosure documents, discuss individual advisers, or explain what steps, if any, the FDA takes to validate advisers’ disclosures.
ESMO, ASCO seek improved cancer services
The European Society for Medical Oncology (ESMO) and the American Society of Clinical Oncology (ASCO) have called for renewed political commitment to improve cancer services and reduce cancer deaths.
ASCO and ESMO issued a joint statement in which they asked heads of state and health ministers to attend the United Nations Civil Society Hearing on Non-communicable Diseases (NCDs) in September and reconfirm their commitment to “pass legislation and invest in actions that will reduce the burden of NCDs, including cancer.”
Specifically, ESMO and ASCO said governments should:
- Implement the 2017 World Health Assembly Cancer Resolution
- Develop and strengthen educational programs that provide lifestyle recommendations to reduce cancer risk (eg, prevent tobacco use, encourage healthy weight control, etc.)
- Develop efficient and cost-effective primary prevention measures (eg, Helicobacter pylori eradication)
- Ensure timely access to screening, early stage diagnosis, and treatment for all stages of cancer
- Strengthen health systems so they can provide cancer services to all who need them
- Provide essential secondary healthcare services that ensure an adequate number of well-trained oncology professionals who have access to necessary resources
- Aim to reduce premature mortality by 25% by 2025 and by 33% by 2030 across all NCDs.
“Recent UN and WHO reports1,2,3,4 note that, unless countries significantly scale-up their actions and investments, they will not meet agreed targets to reduce deaths from non-communicable diseases,” said ESMO President Josep Tabernero, MD, PhD.
“We are concerned that governments may find it easier to achieve their targets by reducing deaths from only some NCDs, leaving cancer patients behind. We believe there are cost-effective ways to improve cancer care and stand ready to assist countries in doing this by providing our expertise in cancer management to support implementation of the 2017 World Health Assembly Cancer Resolution.”
“We urge member states to consider our joint call and amendments to strengthen the political declaration to be approved during the UN high-level meeting on 27 September and thus change the future outlook for cancer patients worldwide.”
1. United Nations Report by the Secretary General, Document A_72_662, 21 December 2017: http://www.who.int/ncds/governance/high-level-commission/A_72_662.pdf
2. World Health Assembly Report by the WHO Director General, Document WHA 71.2, 26 May 2018: http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_R2-en.pdf
3. WHO Independent High-Level Commission on NCDs Report, Time to Deliver, 1 June 2018: http://apps.who.int/iris/bitstream/handle/10665/272710/9789241514163-eng.pdf?ua=1
4. WHO Report Saving Lives, Spending Less, 21 May 2018: http://apps.who.int/iris/bitstream/handle/10665/272534/WHO-NMH-NVI-18.8-eng.pdf
The European Society for Medical Oncology (ESMO) and the American Society of Clinical Oncology (ASCO) have called for renewed political commitment to improve cancer services and reduce cancer deaths.
ASCO and ESMO issued a joint statement in which they asked heads of state and health ministers to attend the United Nations Civil Society Hearing on Non-communicable Diseases (NCDs) in September and reconfirm their commitment to “pass legislation and invest in actions that will reduce the burden of NCDs, including cancer.”
Specifically, ESMO and ASCO said governments should:
- Implement the 2017 World Health Assembly Cancer Resolution
- Develop and strengthen educational programs that provide lifestyle recommendations to reduce cancer risk (eg, prevent tobacco use, encourage healthy weight control, etc.)
- Develop efficient and cost-effective primary prevention measures (eg, Helicobacter pylori eradication)
- Ensure timely access to screening, early stage diagnosis, and treatment for all stages of cancer
- Strengthen health systems so they can provide cancer services to all who need them
- Provide essential secondary healthcare services that ensure an adequate number of well-trained oncology professionals who have access to necessary resources
- Aim to reduce premature mortality by 25% by 2025 and by 33% by 2030 across all NCDs.
“Recent UN and WHO reports1,2,3,4 note that, unless countries significantly scale-up their actions and investments, they will not meet agreed targets to reduce deaths from non-communicable diseases,” said ESMO President Josep Tabernero, MD, PhD.
“We are concerned that governments may find it easier to achieve their targets by reducing deaths from only some NCDs, leaving cancer patients behind. We believe there are cost-effective ways to improve cancer care and stand ready to assist countries in doing this by providing our expertise in cancer management to support implementation of the 2017 World Health Assembly Cancer Resolution.”
“We urge member states to consider our joint call and amendments to strengthen the political declaration to be approved during the UN high-level meeting on 27 September and thus change the future outlook for cancer patients worldwide.”
1. United Nations Report by the Secretary General, Document A_72_662, 21 December 2017: http://www.who.int/ncds/governance/high-level-commission/A_72_662.pdf
2. World Health Assembly Report by the WHO Director General, Document WHA 71.2, 26 May 2018: http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_R2-en.pdf
3. WHO Independent High-Level Commission on NCDs Report, Time to Deliver, 1 June 2018: http://apps.who.int/iris/bitstream/handle/10665/272710/9789241514163-eng.pdf?ua=1
4. WHO Report Saving Lives, Spending Less, 21 May 2018: http://apps.who.int/iris/bitstream/handle/10665/272534/WHO-NMH-NVI-18.8-eng.pdf
The European Society for Medical Oncology (ESMO) and the American Society of Clinical Oncology (ASCO) have called for renewed political commitment to improve cancer services and reduce cancer deaths.
ASCO and ESMO issued a joint statement in which they asked heads of state and health ministers to attend the United Nations Civil Society Hearing on Non-communicable Diseases (NCDs) in September and reconfirm their commitment to “pass legislation and invest in actions that will reduce the burden of NCDs, including cancer.”
Specifically, ESMO and ASCO said governments should:
- Implement the 2017 World Health Assembly Cancer Resolution
- Develop and strengthen educational programs that provide lifestyle recommendations to reduce cancer risk (eg, prevent tobacco use, encourage healthy weight control, etc.)
- Develop efficient and cost-effective primary prevention measures (eg, Helicobacter pylori eradication)
- Ensure timely access to screening, early stage diagnosis, and treatment for all stages of cancer
- Strengthen health systems so they can provide cancer services to all who need them
- Provide essential secondary healthcare services that ensure an adequate number of well-trained oncology professionals who have access to necessary resources
- Aim to reduce premature mortality by 25% by 2025 and by 33% by 2030 across all NCDs.
“Recent UN and WHO reports1,2,3,4 note that, unless countries significantly scale-up their actions and investments, they will not meet agreed targets to reduce deaths from non-communicable diseases,” said ESMO President Josep Tabernero, MD, PhD.
“We are concerned that governments may find it easier to achieve their targets by reducing deaths from only some NCDs, leaving cancer patients behind. We believe there are cost-effective ways to improve cancer care and stand ready to assist countries in doing this by providing our expertise in cancer management to support implementation of the 2017 World Health Assembly Cancer Resolution.”
“We urge member states to consider our joint call and amendments to strengthen the political declaration to be approved during the UN high-level meeting on 27 September and thus change the future outlook for cancer patients worldwide.”
1. United Nations Report by the Secretary General, Document A_72_662, 21 December 2017: http://www.who.int/ncds/governance/high-level-commission/A_72_662.pdf
2. World Health Assembly Report by the WHO Director General, Document WHA 71.2, 26 May 2018: http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_R2-en.pdf
3. WHO Independent High-Level Commission on NCDs Report, Time to Deliver, 1 June 2018: http://apps.who.int/iris/bitstream/handle/10665/272710/9789241514163-eng.pdf?ua=1
4. WHO Report Saving Lives, Spending Less, 21 May 2018: http://apps.who.int/iris/bitstream/handle/10665/272534/WHO-NMH-NVI-18.8-eng.pdf
FDA revises guidance on screening blood for Zika
The US Food and Drug Administration (FDA) has released a revised guidance on testing donated blood and blood components for Zika virus.
The revised guidance states that it is no longer necessary to screen every donation individually.
Pooled donations can be tested for Zika virus in most cases, although, in areas where there is an increased risk of mosquito-borne transmission of Zika, donations should be tested individually.
The FDA said the revised guidance is a result of careful consideration of all available scientific evidence, including consultation with other public health agencies, and following the recommendations of the December 2017 meeting of the Blood Products Advisory Committee.
“When Zika virus first emerged, the unknown course of the epidemic and the observed severe effects from the disease indicated that individual donor testing was needed to ensure the continued safety of the blood supply,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Now, given the significant decrease in cases of Zika virus infection in the US and its territories, we are moving away from testing each individual donation to testing pooled donations. This is usually more cost-effective and less burdensome for blood establishments. However, the FDA will continue to monitor the situation closely, and as appropriate, reconsider what measures are needed to maintain the safety of the blood supply.”
The FDA’s revised guidance replaces the August 2016 guidance, which recommended universal nucleic acid testing of individual units of blood donated in US states and territories.
The revised guidance explains that, to comply with applicable testing regulations, blood establishments must continue to test all donated whole blood and blood components for Zika virus using a nucleic acid test.
However, in many cases, pooled testing of donations using an FDA-licensed screening test is a sufficient method for complying with these regulations. If there is an increased risk of local mosquito-borne transmission of Zika virus in a specific area, donations should be tested individually.
As an alternative to pooled or individual testing, blood establishments can use an FDA-approved pathogen-reduction device for plasma and certain platelet products.
The FDA said these recommendations will continue to ensure the safety of the US blood supply by reducing the risk of Zika virus transmission while also reducing the burden of testing for blood establishments.
The US Food and Drug Administration (FDA) has released a revised guidance on testing donated blood and blood components for Zika virus.
The revised guidance states that it is no longer necessary to screen every donation individually.
Pooled donations can be tested for Zika virus in most cases, although, in areas where there is an increased risk of mosquito-borne transmission of Zika, donations should be tested individually.
The FDA said the revised guidance is a result of careful consideration of all available scientific evidence, including consultation with other public health agencies, and following the recommendations of the December 2017 meeting of the Blood Products Advisory Committee.
“When Zika virus first emerged, the unknown course of the epidemic and the observed severe effects from the disease indicated that individual donor testing was needed to ensure the continued safety of the blood supply,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Now, given the significant decrease in cases of Zika virus infection in the US and its territories, we are moving away from testing each individual donation to testing pooled donations. This is usually more cost-effective and less burdensome for blood establishments. However, the FDA will continue to monitor the situation closely, and as appropriate, reconsider what measures are needed to maintain the safety of the blood supply.”
The FDA’s revised guidance replaces the August 2016 guidance, which recommended universal nucleic acid testing of individual units of blood donated in US states and territories.
The revised guidance explains that, to comply with applicable testing regulations, blood establishments must continue to test all donated whole blood and blood components for Zika virus using a nucleic acid test.
However, in many cases, pooled testing of donations using an FDA-licensed screening test is a sufficient method for complying with these regulations. If there is an increased risk of local mosquito-borne transmission of Zika virus in a specific area, donations should be tested individually.
As an alternative to pooled or individual testing, blood establishments can use an FDA-approved pathogen-reduction device for plasma and certain platelet products.
The FDA said these recommendations will continue to ensure the safety of the US blood supply by reducing the risk of Zika virus transmission while also reducing the burden of testing for blood establishments.
The US Food and Drug Administration (FDA) has released a revised guidance on testing donated blood and blood components for Zika virus.
The revised guidance states that it is no longer necessary to screen every donation individually.
Pooled donations can be tested for Zika virus in most cases, although, in areas where there is an increased risk of mosquito-borne transmission of Zika, donations should be tested individually.
The FDA said the revised guidance is a result of careful consideration of all available scientific evidence, including consultation with other public health agencies, and following the recommendations of the December 2017 meeting of the Blood Products Advisory Committee.
“When Zika virus first emerged, the unknown course of the epidemic and the observed severe effects from the disease indicated that individual donor testing was needed to ensure the continued safety of the blood supply,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research.
“Now, given the significant decrease in cases of Zika virus infection in the US and its territories, we are moving away from testing each individual donation to testing pooled donations. This is usually more cost-effective and less burdensome for blood establishments. However, the FDA will continue to monitor the situation closely, and as appropriate, reconsider what measures are needed to maintain the safety of the blood supply.”
The FDA’s revised guidance replaces the August 2016 guidance, which recommended universal nucleic acid testing of individual units of blood donated in US states and territories.
The revised guidance explains that, to comply with applicable testing regulations, blood establishments must continue to test all donated whole blood and blood components for Zika virus using a nucleic acid test.
However, in many cases, pooled testing of donations using an FDA-licensed screening test is a sufficient method for complying with these regulations. If there is an increased risk of local mosquito-borne transmission of Zika virus in a specific area, donations should be tested individually.
As an alternative to pooled or individual testing, blood establishments can use an FDA-approved pathogen-reduction device for plasma and certain platelet products.
The FDA said these recommendations will continue to ensure the safety of the US blood supply by reducing the risk of Zika virus transmission while also reducing the burden of testing for blood establishments.
EC approves new use, formulation of dasatinib
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
Drug proves active in resistant MM
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
Lower risk of bleeding with apixaban
Real-world data suggest that apixaban poses a lower risk of bleeding than warfarin, but patients who receive lower doses of apixaban have an increased risk of all-cause mortality.
Compared to warfarin, apixaban was associated with a decreased risk of major bleeding, intracranial bleeding, and gastrointestinal bleeding in certain patients.
Dabigatran and rivaroxaban were associated with a decreased risk of intracranial bleeding for certain patients, compared to warfarin.
However, patients who received rivaroxaban or lower doses of apixaban had an increased risk of all-cause mortality, compared to patients who received warfarin.
Yana Vinogradova, PhD, of University of Nottingham in the UK, and her colleagues reported these results in The BMJ.
The researchers set out to investigate the risks and benefits associated with apixaban, dabigatran, and rivaroxaban compared with warfarin in patients with and without atrial fibrillation (AF).
Using data from 2 large UK primary care databases, the researchers identified 196,061 patients who started or restarted anticoagulants (after more than a 12-month gap) between 2011 and 2016.
There were 132,231 patients taking warfarin, 7744 on dabigatran, 37,863 on rivaroxaban, and 18,223 on apixaban.
Slightly more than half of patients (53%, n=103,270) were diagnosed with AF, and 47% (n=92,791) were prescribed anticoagulants for other conditions.
When compared to warfarin in patients with AF, apixaban was associated with a decreased risk of:
- Major bleeding—adjusted hazard ratio [aHR]=0.66
- Intracranial bleeding—aHR=0.40.
In patients without AF, apixaban was associated with a decreased risk of:
- Major bleeding—aHR=0.60
- Any gastrointestinal bleeding—aHR=0.55
- Upper gastrointestinal bleeding—aHR=0.55.
In patients with AF, dabigatran was associated with a decreased risk of intracranial bleeding—aHR=0.45—compared to warfarin.
In patients without AF, rivaroxaban was associated with a decreased risk of intracranial bleeding—aHR=0.54—compared to warfarin.
Compared to patients taking warfarin, there was an increased risk of all-cause mortality for patients:
- With AF taking rivaroxaban—aHR=1.19
- Without AF taking rivaroxaban— aHR=1.51
- With AF taking lower doses of apixaban—aHR=1.27
- Without AF taking lower doses of apixaban—aHR=1.34.
The researchers said the increased risk of all-cause mortality in these patients may reflect the fact that patients taking warfarin are monitored more closely, or it may be related to underlying conditions.
The team did point out that this is an observational study, so no firm conclusions can be drawn about cause and effect. They also outlined some limitations, such as possible misclassification due to patients not taking their medication.
Nevertheless, the researchers concluded that “the risk of major bleeding is lower in apixaban users, regardless of the reason for prescribing, appearing to show apixaban to be the safest drug.”
Real-world data suggest that apixaban poses a lower risk of bleeding than warfarin, but patients who receive lower doses of apixaban have an increased risk of all-cause mortality.
Compared to warfarin, apixaban was associated with a decreased risk of major bleeding, intracranial bleeding, and gastrointestinal bleeding in certain patients.
Dabigatran and rivaroxaban were associated with a decreased risk of intracranial bleeding for certain patients, compared to warfarin.
However, patients who received rivaroxaban or lower doses of apixaban had an increased risk of all-cause mortality, compared to patients who received warfarin.
Yana Vinogradova, PhD, of University of Nottingham in the UK, and her colleagues reported these results in The BMJ.
The researchers set out to investigate the risks and benefits associated with apixaban, dabigatran, and rivaroxaban compared with warfarin in patients with and without atrial fibrillation (AF).
Using data from 2 large UK primary care databases, the researchers identified 196,061 patients who started or restarted anticoagulants (after more than a 12-month gap) between 2011 and 2016.
There were 132,231 patients taking warfarin, 7744 on dabigatran, 37,863 on rivaroxaban, and 18,223 on apixaban.
Slightly more than half of patients (53%, n=103,270) were diagnosed with AF, and 47% (n=92,791) were prescribed anticoagulants for other conditions.
When compared to warfarin in patients with AF, apixaban was associated with a decreased risk of:
- Major bleeding—adjusted hazard ratio [aHR]=0.66
- Intracranial bleeding—aHR=0.40.
In patients without AF, apixaban was associated with a decreased risk of:
- Major bleeding—aHR=0.60
- Any gastrointestinal bleeding—aHR=0.55
- Upper gastrointestinal bleeding—aHR=0.55.
In patients with AF, dabigatran was associated with a decreased risk of intracranial bleeding—aHR=0.45—compared to warfarin.
In patients without AF, rivaroxaban was associated with a decreased risk of intracranial bleeding—aHR=0.54—compared to warfarin.
Compared to patients taking warfarin, there was an increased risk of all-cause mortality for patients:
- With AF taking rivaroxaban—aHR=1.19
- Without AF taking rivaroxaban— aHR=1.51
- With AF taking lower doses of apixaban—aHR=1.27
- Without AF taking lower doses of apixaban—aHR=1.34.
The researchers said the increased risk of all-cause mortality in these patients may reflect the fact that patients taking warfarin are monitored more closely, or it may be related to underlying conditions.
The team did point out that this is an observational study, so no firm conclusions can be drawn about cause and effect. They also outlined some limitations, such as possible misclassification due to patients not taking their medication.
Nevertheless, the researchers concluded that “the risk of major bleeding is lower in apixaban users, regardless of the reason for prescribing, appearing to show apixaban to be the safest drug.”
Real-world data suggest that apixaban poses a lower risk of bleeding than warfarin, but patients who receive lower doses of apixaban have an increased risk of all-cause mortality.
Compared to warfarin, apixaban was associated with a decreased risk of major bleeding, intracranial bleeding, and gastrointestinal bleeding in certain patients.
Dabigatran and rivaroxaban were associated with a decreased risk of intracranial bleeding for certain patients, compared to warfarin.
However, patients who received rivaroxaban or lower doses of apixaban had an increased risk of all-cause mortality, compared to patients who received warfarin.
Yana Vinogradova, PhD, of University of Nottingham in the UK, and her colleagues reported these results in The BMJ.
The researchers set out to investigate the risks and benefits associated with apixaban, dabigatran, and rivaroxaban compared with warfarin in patients with and without atrial fibrillation (AF).
Using data from 2 large UK primary care databases, the researchers identified 196,061 patients who started or restarted anticoagulants (after more than a 12-month gap) between 2011 and 2016.
There were 132,231 patients taking warfarin, 7744 on dabigatran, 37,863 on rivaroxaban, and 18,223 on apixaban.
Slightly more than half of patients (53%, n=103,270) were diagnosed with AF, and 47% (n=92,791) were prescribed anticoagulants for other conditions.
When compared to warfarin in patients with AF, apixaban was associated with a decreased risk of:
- Major bleeding—adjusted hazard ratio [aHR]=0.66
- Intracranial bleeding—aHR=0.40.
In patients without AF, apixaban was associated with a decreased risk of:
- Major bleeding—aHR=0.60
- Any gastrointestinal bleeding—aHR=0.55
- Upper gastrointestinal bleeding—aHR=0.55.
In patients with AF, dabigatran was associated with a decreased risk of intracranial bleeding—aHR=0.45—compared to warfarin.
In patients without AF, rivaroxaban was associated with a decreased risk of intracranial bleeding—aHR=0.54—compared to warfarin.
Compared to patients taking warfarin, there was an increased risk of all-cause mortality for patients:
- With AF taking rivaroxaban—aHR=1.19
- Without AF taking rivaroxaban— aHR=1.51
- With AF taking lower doses of apixaban—aHR=1.27
- Without AF taking lower doses of apixaban—aHR=1.34.
The researchers said the increased risk of all-cause mortality in these patients may reflect the fact that patients taking warfarin are monitored more closely, or it may be related to underlying conditions.
The team did point out that this is an observational study, so no firm conclusions can be drawn about cause and effect. They also outlined some limitations, such as possible misclassification due to patients not taking their medication.
Nevertheless, the researchers concluded that “the risk of major bleeding is lower in apixaban users, regardless of the reason for prescribing, appearing to show apixaban to be the safest drug.”
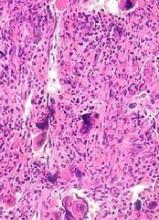
JAK inhibition linked to B-cell lymphoma
New research indicates that JAK inhibitors may increase the risk of lymphoma in patients with myelofibrosis (MF).
The patients studied had a 15- to 25-fold higher risk of developing B-cell lymphoma if they received treatment with JAK inhibitors.
The researchers speculate that screening MF patients for a pre-existing B-cell clone before starting JAK inhibitor therapy may help prevent lymphoma development.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, and his colleagues conducted this research and reported the findings in Blood.
“[W]e started noticing sporadic cases of lymphomas developing in patients being treated for myeloproliferative neoplasms and wanted to know if this phenomenon was connected to treatment,” Dr Gisslinger said.
Therefore, he and his colleagues assessed 626 patients receiving treatment for myeloproliferative neoplasms (MPNs) at the Medical University of Vienna.
The incidence of B-cell lymphoma was 5.8% (4/69) in patients treated with JAK inhibitors and 0.36% (2/557) in patients who did not receive JAK inhibitors. That amounts to a 16-fold increased risk of lymphoma in patients receiving JAK inhibitors.
When the researchers analyzed only patients with primary MF (n=216), the increased risk of B-cell lymphoma was even greater. The incidence of lymphoma was 9.68% (3/31) in patients treated with JAK inhibitors and 0.54% (1/185) in patients who did not receive JAK inhibitors.
That corresponds to a 19-fold increased risk of B-cell lymphoma in primary MF patients treated with JAK inhibitors. When the researchers adjusted for age, there was a 21-fold greater risk. When they adjusted for sex, the risk was 25 times higher.
In a second cohort of 929 MPN patients, the incidence of B-cell lymphoma was 3.51% (2/57) in patients who received JAK inhibitors and 0.23% (2/872) in patients who did not. This corresponds to a 15-fold increased risk of lymphoma in the JAK inhibitor recipients.
Lymphoma cases
In all, there were 6 patients who developed lymphoma after JAK inhibitor treatment. Five developed diffuse large B-cell lymphoma, and 1 had high-grade B-cell lymphoma not otherwise specified.
Four of the patients had primary MF, 1 had post-polycythemia vera MF, and 1 had post-essential thrombocythemia (ET) MF. Five patients had a JAK2V617F mutation, and 1 (the post-ET MF patient) had a CALR mutation.
All 6 patients had received treatment with ruxolitinib. One patient also received fedratinib.
B-cell clone
The researchers studied bone marrow samples from 54 of the 69 patients treated with JAK inhibitors in the first cohort. The team found a pre-existing B-cell clone in 3 of the 4 patients who developed lymphoma. Further investigation suggested this was the clone that later transformed into lymphoma.
The researchers also found an association between JAK inhibition and an increased frequency of aggressive B-cell lymphomas in mouse models.
“By replicating this link between this B-cell clone and aggressive lymphoma, we hope to speed the discovery of an alternative therapy for myelofibrosis,” said study author Veronica Sexl, MD, of the University of Veterinary Medicine in Vienna. “These findings are going to be valuable in clinical care.”
“We determined that patients with this pre-existing B-cell clone in their bone marrow are most at risk for developing aggressive lymphoma,” added study author Ulrich Jäger, MD, of the Medical University of Vienna.
“We also know that up to 16% of people with myelofibrosis have immunoglobulin gene rearrangements like this B-cell clone. Therefore, our findings suggest that all patients with myelofibrosis should be tested for such gene rearrangements before prescribing JAK inhibitors to treat their disease.”
New research indicates that JAK inhibitors may increase the risk of lymphoma in patients with myelofibrosis (MF).
The patients studied had a 15- to 25-fold higher risk of developing B-cell lymphoma if they received treatment with JAK inhibitors.
The researchers speculate that screening MF patients for a pre-existing B-cell clone before starting JAK inhibitor therapy may help prevent lymphoma development.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, and his colleagues conducted this research and reported the findings in Blood.
“[W]e started noticing sporadic cases of lymphomas developing in patients being treated for myeloproliferative neoplasms and wanted to know if this phenomenon was connected to treatment,” Dr Gisslinger said.
Therefore, he and his colleagues assessed 626 patients receiving treatment for myeloproliferative neoplasms (MPNs) at the Medical University of Vienna.
The incidence of B-cell lymphoma was 5.8% (4/69) in patients treated with JAK inhibitors and 0.36% (2/557) in patients who did not receive JAK inhibitors. That amounts to a 16-fold increased risk of lymphoma in patients receiving JAK inhibitors.
When the researchers analyzed only patients with primary MF (n=216), the increased risk of B-cell lymphoma was even greater. The incidence of lymphoma was 9.68% (3/31) in patients treated with JAK inhibitors and 0.54% (1/185) in patients who did not receive JAK inhibitors.
That corresponds to a 19-fold increased risk of B-cell lymphoma in primary MF patients treated with JAK inhibitors. When the researchers adjusted for age, there was a 21-fold greater risk. When they adjusted for sex, the risk was 25 times higher.
In a second cohort of 929 MPN patients, the incidence of B-cell lymphoma was 3.51% (2/57) in patients who received JAK inhibitors and 0.23% (2/872) in patients who did not. This corresponds to a 15-fold increased risk of lymphoma in the JAK inhibitor recipients.
Lymphoma cases
In all, there were 6 patients who developed lymphoma after JAK inhibitor treatment. Five developed diffuse large B-cell lymphoma, and 1 had high-grade B-cell lymphoma not otherwise specified.
Four of the patients had primary MF, 1 had post-polycythemia vera MF, and 1 had post-essential thrombocythemia (ET) MF. Five patients had a JAK2V617F mutation, and 1 (the post-ET MF patient) had a CALR mutation.
All 6 patients had received treatment with ruxolitinib. One patient also received fedratinib.
B-cell clone
The researchers studied bone marrow samples from 54 of the 69 patients treated with JAK inhibitors in the first cohort. The team found a pre-existing B-cell clone in 3 of the 4 patients who developed lymphoma. Further investigation suggested this was the clone that later transformed into lymphoma.
The researchers also found an association between JAK inhibition and an increased frequency of aggressive B-cell lymphomas in mouse models.
“By replicating this link between this B-cell clone and aggressive lymphoma, we hope to speed the discovery of an alternative therapy for myelofibrosis,” said study author Veronica Sexl, MD, of the University of Veterinary Medicine in Vienna. “These findings are going to be valuable in clinical care.”
“We determined that patients with this pre-existing B-cell clone in their bone marrow are most at risk for developing aggressive lymphoma,” added study author Ulrich Jäger, MD, of the Medical University of Vienna.
“We also know that up to 16% of people with myelofibrosis have immunoglobulin gene rearrangements like this B-cell clone. Therefore, our findings suggest that all patients with myelofibrosis should be tested for such gene rearrangements before prescribing JAK inhibitors to treat their disease.”
New research indicates that JAK inhibitors may increase the risk of lymphoma in patients with myelofibrosis (MF).
The patients studied had a 15- to 25-fold higher risk of developing B-cell lymphoma if they received treatment with JAK inhibitors.
The researchers speculate that screening MF patients for a pre-existing B-cell clone before starting JAK inhibitor therapy may help prevent lymphoma development.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, and his colleagues conducted this research and reported the findings in Blood.
“[W]e started noticing sporadic cases of lymphomas developing in patients being treated for myeloproliferative neoplasms and wanted to know if this phenomenon was connected to treatment,” Dr Gisslinger said.
Therefore, he and his colleagues assessed 626 patients receiving treatment for myeloproliferative neoplasms (MPNs) at the Medical University of Vienna.
The incidence of B-cell lymphoma was 5.8% (4/69) in patients treated with JAK inhibitors and 0.36% (2/557) in patients who did not receive JAK inhibitors. That amounts to a 16-fold increased risk of lymphoma in patients receiving JAK inhibitors.
When the researchers analyzed only patients with primary MF (n=216), the increased risk of B-cell lymphoma was even greater. The incidence of lymphoma was 9.68% (3/31) in patients treated with JAK inhibitors and 0.54% (1/185) in patients who did not receive JAK inhibitors.
That corresponds to a 19-fold increased risk of B-cell lymphoma in primary MF patients treated with JAK inhibitors. When the researchers adjusted for age, there was a 21-fold greater risk. When they adjusted for sex, the risk was 25 times higher.
In a second cohort of 929 MPN patients, the incidence of B-cell lymphoma was 3.51% (2/57) in patients who received JAK inhibitors and 0.23% (2/872) in patients who did not. This corresponds to a 15-fold increased risk of lymphoma in the JAK inhibitor recipients.
Lymphoma cases
In all, there were 6 patients who developed lymphoma after JAK inhibitor treatment. Five developed diffuse large B-cell lymphoma, and 1 had high-grade B-cell lymphoma not otherwise specified.
Four of the patients had primary MF, 1 had post-polycythemia vera MF, and 1 had post-essential thrombocythemia (ET) MF. Five patients had a JAK2V617F mutation, and 1 (the post-ET MF patient) had a CALR mutation.
All 6 patients had received treatment with ruxolitinib. One patient also received fedratinib.
B-cell clone
The researchers studied bone marrow samples from 54 of the 69 patients treated with JAK inhibitors in the first cohort. The team found a pre-existing B-cell clone in 3 of the 4 patients who developed lymphoma. Further investigation suggested this was the clone that later transformed into lymphoma.
The researchers also found an association between JAK inhibition and an increased frequency of aggressive B-cell lymphomas in mouse models.
“By replicating this link between this B-cell clone and aggressive lymphoma, we hope to speed the discovery of an alternative therapy for myelofibrosis,” said study author Veronica Sexl, MD, of the University of Veterinary Medicine in Vienna. “These findings are going to be valuable in clinical care.”
“We determined that patients with this pre-existing B-cell clone in their bone marrow are most at risk for developing aggressive lymphoma,” added study author Ulrich Jäger, MD, of the Medical University of Vienna.
“We also know that up to 16% of people with myelofibrosis have immunoglobulin gene rearrangements like this B-cell clone. Therefore, our findings suggest that all patients with myelofibrosis should be tested for such gene rearrangements before prescribing JAK inhibitors to treat their disease.”
Cell therapy receives RMAT designation
The US Food and Drug Administration (FDA) has granted regenerative medicine advanced therapy (RMAT) designation for romyelocel-L, a myeloid progenitor cell therapy that doesn’t require HLA matching.
Romyelocel-L (CLT-008) is being developed as prophylaxis for serious bacterial and fungal infections in patients with de novo acute myeloid leukemia (AML) who develop neutropenia while receiving induction chemotherapy.
The FDA grants RMAT designation to therapies intended to treat serious or life-threatening conditions if there is preliminary clinical evidence that the therapies could address unmet medical needs.
RMAT designation provides similar advantages as breakthrough therapy designation, including early interactions with the FDA to discuss potential ways to accelerate the development of a therapy toward regulatory approval.
The FDA granted romyelocel-L RMAT designation based on a randomized, phase 2 trial of newly diagnosed AML patients who received induction consisting of cytarabine and an anthracycline.
Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 7043).
The trial enrolled 163 AML patients and randomized them, on the first day of induction, to receive:
- Daily granulocyte colony-stimulating factor (G-CSF) starting on day 14 (n=84)
- Romyelocel-L (7.5 x 106cells/kg) on day 9 plus daily G-CSF starting on day 14 (n=79).
Patients received G-CSF until neutrophil recovery to at least 500/µL.
Baseline characteristics were well balanced between the treatment arms.
There were 120 evaluable patients—59 in the romyelocel-L arm and 61 in the control arm.
The study’s primary endpoint was days in a febrile episode (DFE). The mean DFE from day 9 to 28 was 6.46 days in the romyelocel-L arm and 6.86 days in the control arm (P=0.350). The mean DFE for days 15 to 28 was 2.36 and 3.90, respectively (P=0.020).
The incidence of microbiologically or clinically diagnosed infection from day 9 to 28 was 35.6% in the romyelocel-L arm and 47.5% in the control arm, a decrease of 25% (P=0.089).
From day 15 to 28 the incidence of infection was 6.8% in the romyelocel-L arm and 27.9% in the control arm, a decrease of 76% (P=0.002).
There were no infectious deaths in the romyelocel-L arm but 2 deaths attributed to pneumonia in the control arm.
The mean hospital stay was 25.5 days in the romyelocel-L arm and 28.7 days in the control arm (P=0.002).
The proportion of patients with serious adverse events (AEs) was 14% in the romyelocel-L arm and 18% in the control arm. The proportion of patients with infectious serious AEs was 50% and 77%, respectively.
The most frequent treatment-emergent AEs (in the romyelocel-L and control arms, respectively) were febrile neutropenia (31.4% and 31%), diarrhea (25.7% and 32.4%), hypokalemia (31.4% and 25.4%), hypophosphatemia (21.4% and 23.9%), and pyrexia (22.9% and 22.5%).
There were no cases of graft-versus-host disease.
The US Food and Drug Administration (FDA) has granted regenerative medicine advanced therapy (RMAT) designation for romyelocel-L, a myeloid progenitor cell therapy that doesn’t require HLA matching.
Romyelocel-L (CLT-008) is being developed as prophylaxis for serious bacterial and fungal infections in patients with de novo acute myeloid leukemia (AML) who develop neutropenia while receiving induction chemotherapy.
The FDA grants RMAT designation to therapies intended to treat serious or life-threatening conditions if there is preliminary clinical evidence that the therapies could address unmet medical needs.
RMAT designation provides similar advantages as breakthrough therapy designation, including early interactions with the FDA to discuss potential ways to accelerate the development of a therapy toward regulatory approval.
The FDA granted romyelocel-L RMAT designation based on a randomized, phase 2 trial of newly diagnosed AML patients who received induction consisting of cytarabine and an anthracycline.
Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 7043).
The trial enrolled 163 AML patients and randomized them, on the first day of induction, to receive:
- Daily granulocyte colony-stimulating factor (G-CSF) starting on day 14 (n=84)
- Romyelocel-L (7.5 x 106cells/kg) on day 9 plus daily G-CSF starting on day 14 (n=79).
Patients received G-CSF until neutrophil recovery to at least 500/µL.
Baseline characteristics were well balanced between the treatment arms.
There were 120 evaluable patients—59 in the romyelocel-L arm and 61 in the control arm.
The study’s primary endpoint was days in a febrile episode (DFE). The mean DFE from day 9 to 28 was 6.46 days in the romyelocel-L arm and 6.86 days in the control arm (P=0.350). The mean DFE for days 15 to 28 was 2.36 and 3.90, respectively (P=0.020).
The incidence of microbiologically or clinically diagnosed infection from day 9 to 28 was 35.6% in the romyelocel-L arm and 47.5% in the control arm, a decrease of 25% (P=0.089).
From day 15 to 28 the incidence of infection was 6.8% in the romyelocel-L arm and 27.9% in the control arm, a decrease of 76% (P=0.002).
There were no infectious deaths in the romyelocel-L arm but 2 deaths attributed to pneumonia in the control arm.
The mean hospital stay was 25.5 days in the romyelocel-L arm and 28.7 days in the control arm (P=0.002).
The proportion of patients with serious adverse events (AEs) was 14% in the romyelocel-L arm and 18% in the control arm. The proportion of patients with infectious serious AEs was 50% and 77%, respectively.
The most frequent treatment-emergent AEs (in the romyelocel-L and control arms, respectively) were febrile neutropenia (31.4% and 31%), diarrhea (25.7% and 32.4%), hypokalemia (31.4% and 25.4%), hypophosphatemia (21.4% and 23.9%), and pyrexia (22.9% and 22.5%).
There were no cases of graft-versus-host disease.
The US Food and Drug Administration (FDA) has granted regenerative medicine advanced therapy (RMAT) designation for romyelocel-L, a myeloid progenitor cell therapy that doesn’t require HLA matching.
Romyelocel-L (CLT-008) is being developed as prophylaxis for serious bacterial and fungal infections in patients with de novo acute myeloid leukemia (AML) who develop neutropenia while receiving induction chemotherapy.
The FDA grants RMAT designation to therapies intended to treat serious or life-threatening conditions if there is preliminary clinical evidence that the therapies could address unmet medical needs.
RMAT designation provides similar advantages as breakthrough therapy designation, including early interactions with the FDA to discuss potential ways to accelerate the development of a therapy toward regulatory approval.
The FDA granted romyelocel-L RMAT designation based on a randomized, phase 2 trial of newly diagnosed AML patients who received induction consisting of cytarabine and an anthracycline.
Results from this trial were presented at the 2018 ASCO Annual Meeting (abstract 7043).
The trial enrolled 163 AML patients and randomized them, on the first day of induction, to receive:
- Daily granulocyte colony-stimulating factor (G-CSF) starting on day 14 (n=84)
- Romyelocel-L (7.5 x 106cells/kg) on day 9 plus daily G-CSF starting on day 14 (n=79).
Patients received G-CSF until neutrophil recovery to at least 500/µL.
Baseline characteristics were well balanced between the treatment arms.
There were 120 evaluable patients—59 in the romyelocel-L arm and 61 in the control arm.
The study’s primary endpoint was days in a febrile episode (DFE). The mean DFE from day 9 to 28 was 6.46 days in the romyelocel-L arm and 6.86 days in the control arm (P=0.350). The mean DFE for days 15 to 28 was 2.36 and 3.90, respectively (P=0.020).
The incidence of microbiologically or clinically diagnosed infection from day 9 to 28 was 35.6% in the romyelocel-L arm and 47.5% in the control arm, a decrease of 25% (P=0.089).
From day 15 to 28 the incidence of infection was 6.8% in the romyelocel-L arm and 27.9% in the control arm, a decrease of 76% (P=0.002).
There were no infectious deaths in the romyelocel-L arm but 2 deaths attributed to pneumonia in the control arm.
The mean hospital stay was 25.5 days in the romyelocel-L arm and 28.7 days in the control arm (P=0.002).
The proportion of patients with serious adverse events (AEs) was 14% in the romyelocel-L arm and 18% in the control arm. The proportion of patients with infectious serious AEs was 50% and 77%, respectively.
The most frequent treatment-emergent AEs (in the romyelocel-L and control arms, respectively) were febrile neutropenia (31.4% and 31%), diarrhea (25.7% and 32.4%), hypokalemia (31.4% and 25.4%), hypophosphatemia (21.4% and 23.9%), and pyrexia (22.9% and 22.5%).
There were no cases of graft-versus-host disease.
CHMP recommends rVWF for VWD
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The CHMP is recommending vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of vonicog alfa is supported by a pair of phase 3 trials.
Non-surgical setting
Results from a phase 3 trial of vonicog alfa in a non-surgical setting were published in Blood in 2015.
The study included 49 patients with VWD who received vonicog alfa with or without recombinant factor VIII (FVIII).
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (n=192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events (AEs) considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious AEs—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
Surgical setting
Results from the phase 3 trial in a surgical setting were presented at the WFH 2018 World Congress.
The trial enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
The study’s primary endpoint was met. Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The CHMP is recommending vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of vonicog alfa is supported by a pair of phase 3 trials.
Non-surgical setting
Results from a phase 3 trial of vonicog alfa in a non-surgical setting were published in Blood in 2015.
The study included 49 patients with VWD who received vonicog alfa with or without recombinant factor VIII (FVIII).
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (n=192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events (AEs) considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious AEs—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
Surgical setting
Results from the phase 3 trial in a surgical setting were presented at the WFH 2018 World Congress.
The trial enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
The study’s primary endpoint was met. Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for vonicog alfa (Veyvondi), a recombinant von Willebrand factor (rVWF) product.
The CHMP is recommending vonicog alfa for the treatment of bleeding events and treatment/prevention of surgical bleeding in adults (age 18 and older) with von Willebrand disease (VWD) when desmopressin treatment alone is ineffective or not indicated.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of vonicog alfa is supported by a pair of phase 3 trials.
Non-surgical setting
Results from a phase 3 trial of vonicog alfa in a non-surgical setting were published in Blood in 2015.
The study included 49 patients with VWD who received vonicog alfa with or without recombinant factor VIII (FVIII).
All participants had successful treatment of bleeding episodes. Most (96.9%) treated bleeds (n=192 bleeds in 22 patients) were given an “excellent” efficacy rating (as good as or better than expected).
Most bleeds (81.8%) were resolved with a single infusion of vonicog alfa, and the treatment had a mean half-life of 21.9 hours.
There were 8 adverse events (AEs) considered related to vonicog alfa, and 2 were serious. One patient experienced 2 simultaneous serious AEs—chest discomfort and increased heart rate—but these were resolved.
There were no thrombotic events in this trial, no treatment-related binding or neutralizing antibodies against VWF, and no neutralizing antibodies against FVIII.
Surgical setting
Results from the phase 3 trial in a surgical setting were presented at the WFH 2018 World Congress.
The trial enrolled 15 adults with severe VWD who were undergoing elective surgical procedures (10 of them major procedures).
Patients received vonicog alfa at 40 to 60 IU per kg of body weight 12 to 24 hours before surgery. Within 3 hours of surgery, each patient’s FVIII level (FVIII:C) was assessed, with a target of 30 IU/dL for minor surgeries and 60 IU/dL for major surgeries.
Within an hour of surgery, patients received a dose of vonicog alfa, with or without recombinant factor VIII, depending on the target FVIII:C levels at the 3-hour assessment.
Ten patients received rVWF alone, 12 did not receive any preoperative FVIII, and 2 did not receive rVWF postoperatively.
The study’s primary endpoint was met. Vonicog alfa demonstrated overall hemostatic efficacy, as assessed 24 hours after the last perioperative infusion or the completion of the study visit, whichever occurred earlier.
Intra- and post-operative hemostasis was rated as “excellent” (as good as or better than expected) in 60% of patients and “good” (probably as good as expected) in 40% of patients.
One patient developed deep vein thrombosis 3 days after undergoing hip replacement surgery.
One patient tested positive for binding antibodies to VWF. None of the patients developed binding antibodies against potential impurities such as rFurin, CHO-protein, or mouse IgG.
CHMP supports authorization of drug for AML
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for CPX-351 (Vyxeos™), a liposomal formulation that delivers a fixed ratio (1:5) of daunorubicin and cytarabine.
The CHMP is recommending approval of CPX-351 (44 mg/100 mg) for the treatment of adults with newly diagnosed, therapy-related acute myeloid leukemia or AML with myelodysplasia-related changes.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for CPX-351 is supported by data from 5 studies, including a phase 3 study.
Data from the phase 3 study were presented at the 2016 ASCO Annual Meeting and are available in the US prescribing information for CPX-351. (The following data are taken from the prescribing information.)
This trial enrolled 309 patients, ages 60 to 75, with newly diagnosed, therapy-related AML or AML with myelodysplasia-related changes.
They received CPX-351 (n=153) or cytarabine and daunorubicin (7+3; n=156).
The complete response rate was 38% in the CPX-351 arm and 26% in the 7+3 arm (P=0.036).
The rate of hematopoietic stem cell transplant was 34% in the CPX-351 arm and 25% in the 7+3 arm.
The median overall survival was 9.6 months in the CPX-351 arm and 5.9 months in the 7+3 arm (P=0.005).
All-cause 30-day mortality was 6% in the CPX-351 arm and 11% in the 7+3 arm. Sixty-day mortality was 14% and 21%, respectively.
Six percent of patients in both arms had a fatal adverse event (AE) on treatment or within 30 days of therapy that was not in the setting of progressive disease.
The rate of AEs that led to discontinuation was 18% in the CPX-351 arm and 13% in the 7+3 arm. AEs leading to discontinuation in the CPX-351 arm included prolonged cytopenias, infection, cardiotoxicity, respiratory failure, hemorrhage, renal insufficiency, colitis, and generalized medical deterioration.
The most common AEs (incidence ≥ 25%) in the CPX-351 arm were hemorrhagic events, febrile neutropenia, rash, edema, nausea, mucositis, diarrhea, constipation, musculoskeletal pain, fatigue, abdominal pain, dyspnea, headache, cough, decreased appetite, arrhythmia, pneumonia, bacteremia, chills, sleep disorders, and vomiting.
The most common serious AEs (incidence ≥ 5%) in the CPX-351 arm were dyspnea, myocardial toxicity, sepsis, pneumonia, febrile neutropenia, bacteremia, and hemorrhage.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for CPX-351 (Vyxeos™), a liposomal formulation that delivers a fixed ratio (1:5) of daunorubicin and cytarabine.
The CHMP is recommending approval of CPX-351 (44 mg/100 mg) for the treatment of adults with newly diagnosed, therapy-related acute myeloid leukemia or AML with myelodysplasia-related changes.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for CPX-351 is supported by data from 5 studies, including a phase 3 study.
Data from the phase 3 study were presented at the 2016 ASCO Annual Meeting and are available in the US prescribing information for CPX-351. (The following data are taken from the prescribing information.)
This trial enrolled 309 patients, ages 60 to 75, with newly diagnosed, therapy-related AML or AML with myelodysplasia-related changes.
They received CPX-351 (n=153) or cytarabine and daunorubicin (7+3; n=156).
The complete response rate was 38% in the CPX-351 arm and 26% in the 7+3 arm (P=0.036).
The rate of hematopoietic stem cell transplant was 34% in the CPX-351 arm and 25% in the 7+3 arm.
The median overall survival was 9.6 months in the CPX-351 arm and 5.9 months in the 7+3 arm (P=0.005).
All-cause 30-day mortality was 6% in the CPX-351 arm and 11% in the 7+3 arm. Sixty-day mortality was 14% and 21%, respectively.
Six percent of patients in both arms had a fatal adverse event (AE) on treatment or within 30 days of therapy that was not in the setting of progressive disease.
The rate of AEs that led to discontinuation was 18% in the CPX-351 arm and 13% in the 7+3 arm. AEs leading to discontinuation in the CPX-351 arm included prolonged cytopenias, infection, cardiotoxicity, respiratory failure, hemorrhage, renal insufficiency, colitis, and generalized medical deterioration.
The most common AEs (incidence ≥ 25%) in the CPX-351 arm were hemorrhagic events, febrile neutropenia, rash, edema, nausea, mucositis, diarrhea, constipation, musculoskeletal pain, fatigue, abdominal pain, dyspnea, headache, cough, decreased appetite, arrhythmia, pneumonia, bacteremia, chills, sleep disorders, and vomiting.
The most common serious AEs (incidence ≥ 5%) in the CPX-351 arm were dyspnea, myocardial toxicity, sepsis, pneumonia, febrile neutropenia, bacteremia, and hemorrhage.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended marketing authorization for CPX-351 (Vyxeos™), a liposomal formulation that delivers a fixed ratio (1:5) of daunorubicin and cytarabine.
The CHMP is recommending approval of CPX-351 (44 mg/100 mg) for the treatment of adults with newly diagnosed, therapy-related acute myeloid leukemia or AML with myelodysplasia-related changes.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for CPX-351 is supported by data from 5 studies, including a phase 3 study.
Data from the phase 3 study were presented at the 2016 ASCO Annual Meeting and are available in the US prescribing information for CPX-351. (The following data are taken from the prescribing information.)
This trial enrolled 309 patients, ages 60 to 75, with newly diagnosed, therapy-related AML or AML with myelodysplasia-related changes.
They received CPX-351 (n=153) or cytarabine and daunorubicin (7+3; n=156).
The complete response rate was 38% in the CPX-351 arm and 26% in the 7+3 arm (P=0.036).
The rate of hematopoietic stem cell transplant was 34% in the CPX-351 arm and 25% in the 7+3 arm.
The median overall survival was 9.6 months in the CPX-351 arm and 5.9 months in the 7+3 arm (P=0.005).
All-cause 30-day mortality was 6% in the CPX-351 arm and 11% in the 7+3 arm. Sixty-day mortality was 14% and 21%, respectively.
Six percent of patients in both arms had a fatal adverse event (AE) on treatment or within 30 days of therapy that was not in the setting of progressive disease.
The rate of AEs that led to discontinuation was 18% in the CPX-351 arm and 13% in the 7+3 arm. AEs leading to discontinuation in the CPX-351 arm included prolonged cytopenias, infection, cardiotoxicity, respiratory failure, hemorrhage, renal insufficiency, colitis, and generalized medical deterioration.
The most common AEs (incidence ≥ 25%) in the CPX-351 arm were hemorrhagic events, febrile neutropenia, rash, edema, nausea, mucositis, diarrhea, constipation, musculoskeletal pain, fatigue, abdominal pain, dyspnea, headache, cough, decreased appetite, arrhythmia, pneumonia, bacteremia, chills, sleep disorders, and vomiting.
The most common serious AEs (incidence ≥ 5%) in the CPX-351 arm were dyspnea, myocardial toxicity, sepsis, pneumonia, febrile neutropenia, bacteremia, and hemorrhage.