User login
Cost of imatinib still high despite generic options, team says
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
The availability of generic imatinib has had limited effects on costs of the drug, according to research published in Health Affairs.
Data suggest the cost of Gleevec in the US has more than doubled since the drug was approved in 2001, and the introduction of generic imatinib has reduced costs only slightly.
Two years after generic imatinib hit the market, a month’s supply of Gleevec cost about $9000, and the cost for generic imatinib was about $8000.
“Patients and providers have all looked forward to generic entry, expecting major price reductions,” said study author Stacie Dusetzina, PhD, of Vanderbilt University School of Medicine in Nashville, Tennessee.
“Unfortunately, we don’t see prices drop as quickly and as low as we would hope when generics are available.”
For this study, Dr Dusetzina and a colleague analyzed data from the MarketScan Commercial Research Database. The database contained records of 139,233 prescription fills for imatinib, which were made by 7201 patients from May 2001 through September 2017.
The researchers noted that Gleevec was priced at nearly $4000 for a 1-month (400 mg) supply when it came on the market in 2001. That price escalated to nearly $10,000 by 2015 before a generic competitor entered the market.
However, prices for Gleevec and generic imatinib remained high 2 years later. In 2017, a month’s supply of Gleevec cost about $9000, and the cost of generic imatinib was about $8000.
The researchers said the Gleevec case demonstrates several potential barriers to effective generic price competition, including shifts in prescribing toward more expensive brand-name treatments and smaller-than-expected price reductions.
Twenty-four percent of imatinib (Gleevec) prescriptions claims were for “dispense as written,” according to the researchers. This suggests that patients or providers specifically wanted to stay on the brand-name drug instead of switching to the generic.
“The more than doubling of the drug price over time and the lack of price reductions observed with nearly 2 years of generic drug competition is concerning,” Dr Dusetzina said.
“It begs the question whether we can rely on generic entry as a primary approach to address drug pricing for high-priced specialty medications. We need robust competition to move prices in this space.”
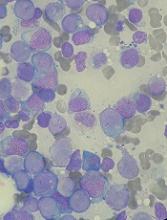
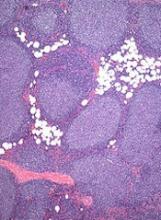
Y chromosome gene protects against AML
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
Researchers have discovered the first leukemia-protective gene that is specific to the Y chromosome, according to an article published in Nature Genetics.
The researchers were investigating how loss of the X-chromosome gene UTX hastens the development of acute myeloid leukemia (AML).
However, they found that UTY, a related gene on the Y chromosome, protected male mice lacking UTX from developing AML.
The researchers then found that, in AML and other cancers, loss of UTX is accompanied by loss of UTY.
“This is the first Y chromosome-specific gene that protects against AML,” said study author Malgorzata Gozdecka, PhD, of the Wellcome Sanger Institute in Hinxton, UK.
“Previously, it had been suggested that the only function of the Y chromosome is in creating male sexual characteristics, but our results indicate that the Y chromosome could also protect against AML and other cancers.”
For this work, Dr Gozdecka and her colleagues studied the UTX gene in human cells and mice.
In addition to their discovery that UTY acts as a tumor suppressor gene, the researchers uncovered a new mechanism for how loss of UTX leads to AML.
They discovered that UTX acts as a common scaffold, bringing together a large number of regulatory proteins that control access to DNA and gene expression, a function that can also be carried out by UTY.
Specifically, the team said UTX suppresses AML by repressing oncogenic ETS and upregulating tumor-suppressive GATA programs. And loss of UTX leads to “altered patterns of gene expression that induce and maintain” AML.
“Treatments for AML have not changed in decades, and there is a large unmet need for new therapies,” said study author George Vassiliou, PhD, of the Wellcome Sanger Institute.
“This study helps us understand the development of AML and gives us clues for developing new drug targets to disrupt leukemia-causing processes. We hope this study will enable new lines of research for the development of previously unforeseen treatments and improve the lives of patients with AML.”
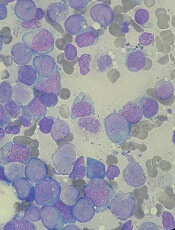
How ruxolitinib reduces thrombosis in MPNs
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
Preclinical research helps explain how the JAK1/2 inhibitor ruxolitinib can reduce thrombosis in patients with myeloproliferative neoplasms (MPNs).
Experiments revealed a link between JAK2V617F and the formation of neutrophil extracellular traps (NETs), which have been implicated in thrombosis.
Researchers found that ruxolitinib reduced NET formation and decreased thrombosis in JAK2-mutant mice.
Benjamin L. Ebert, MD, PhD, of Brigham and Women’s Hospital in Boston, Massachusetts, and his colleagues reported these findings in Science Translational Medicine.
The researchers noted that patients with MPNs have an increased risk of thrombosis, and previous research linked thrombosis to the formation of NETs. NETs are structures that help trap pathogens but may also promote autoimmune responses and excessive blood clotting.
With the current study, Dr Ebert and his colleagues examined whether NET formation could promote thrombosis in patients with MPNs.
The team found that neutrophils from MPN patients were more likely to form NETs than neutrophils from healthy individuals. However, incubating neutrophils with ruxolitinib reduced NET formation.
The researchers also found that mice with JAK2V617F were more likely to form NETs and develop thrombosis when compared to wild-type mice. However, treatment with ruxolitinib reduced rates of thrombosis and prevented NET formation in the mice.
The researchers noted that expression of PAD4, a protein required for NET formation, is increased in JAK2V617F-expressing neutrophils. And the team found that PAD4 is required for JAK2V617F-driven NET formation and thrombosis in mouse models of MPNs.
Lastly, the researchers looked at data from 10,893 human subjects. None of these subjects had MPNs, but some had JAK2V617F.
Subjects who were JAK2V617F-positive had a significantly higher risk of thrombotic events than subjects without the mutation (P=0.0003).
Taken together, these findings suggest that JAK2 inhibition can reduce NET formation and ameliorate thrombosis in patients with MPNs or the JAK2V617F mutation.
The researchers noted that, in the phase 3 RESPONSE trial, patients with polycythemia vera had a lower rate of thromboembolic events if they received ruxolitinib rather than standard therapy.
FDA approves antidote for factor Xa inhibitors
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
The US Food and Drug Administration (FDA) has granted accelerated approval for andexanet alfa (Andexxa®), the first antidote for the reversal of factor Xa inhibitors.
Andexanet alfa is approved for use in patients treated with rivaroxaban or apixaban when reversal of anticoagulation is needed due to life-threatening or uncontrolled bleeding.
Andexanet alfa was granted accelerated approval for this indication based on the drug’s anti-factor Xa activity in healthy volunteers.
Continued FDA approval of andexanet alfa may be contingent upon post-marketing study results to demonstrate an improvement in hemostasis in patients taking rivaroxaban or apixaban who require reversal of anticoagulation.
The post-marketing requirement is a trial in which patients will be randomized to receive either andexanet alfa or usual care. This study is scheduled to start in 2019, with results expected to be available in 2023.
Portola Pharmaceuticals, Inc., said it expects to launch andexanet alfa in early June. This drug will be produced using the generation 1 manufacturing process.
A broader commercial launch of andexanet alfa is anticipated in early 2019, dependent upon FDA approval of the generation 2 manufacturing process.
Supporting trials
The FDA’s approval of andexanet alfa is supported by data from a pair of phase 3 studies—ANNEXA-R and ANNEXA-A.
These trials were designed to evaluate the safety and efficacy of andexanet alfa in reversing the anticoagulant activity of rivaroxaban and apixaban in healthy volunteers.
Results from both studies were published in NEJM in 2015.
The FDA also assessed interim data from the ongoing ANNEXA-4 study as part of the review and approval of andexanet alfa.
In ANNEXA-4, researchers are evaluating andexanet alfa in patients experiencing major bleeding while taking factor Xa inhibitors.
Interim results from this trial were presented at the American College of Cardiology’s 67th Annual Scientific Session & Expo in March.
About andexanet alfa
Andexanet alfa is a modified human factor Xa molecule that acts as a decoy to target and sequester both oral and injectable factor Xa inhibitors in the blood. Once bound, the factor Xa inhibitors are unable to bind to and inhibit native factor Xa, thus potentially allowing for the restoration of normal hemostatic processes.
Portola Pharmaceuticals first submitted the biologics license application (BLA) for andexanet alfa in December 2015. The FDA had already granted andexanet alfa orphan drug designation earlier in 2015 and breakthrough therapy designation in 2013.
With its first BLA submission, Portola was seeking approval for andexanet alfa as a reversal agent for patients anticoagulated with an oral or injectable factor Xa inhibitor—apixaban, rivaroxaban, edoxaban, or enoxaparin—who experience serious uncontrolled or life-threatening bleeding or who require urgent or emergency surgery.
In August 2016, the FDA issued a complete response letter explaining why the agency could not approve andexanet alfa for this indication.
The FDA requested additional information related to manufacturing of the drug and asked Portola for additional data to support the inclusion of edoxaban and enoxaparin on andexanet alfa’s label. This was because the ANNEXA-A and ANNEXA-R trials only included subjects who received apixaban or rivaroxaban.
In August 2017, Portola resubmitted the BLA for andexanet alfa. This time, the company sought approval of the drug only for patients on apixaban or rivaroxaban who are experiencing uncontrolled or life-threatening bleeding.
For additional information on andexanet alfa, visit https://www.andexxa.com/.
Drug granted fast track designations for FL, DLBCL
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
The US Food and Drug Administration (FDA) has granted 2 fast track designations to 5F9, an anti-CD47 antibody.
The designations are for 5F9 as a treatment for relapsed or refractory diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma (FL).
Data supporting the fast track designations were derived from a phase 1b/2 trial of 5F9 in combination with rituximab in patients with relapsed or refractory B-cell non-Hodgkin lymphoma, including DLBCL and FL.
Forty Seven, Inc., the company developing 5F9, expects to announce initial safety and efficacy data from the phase 1b portion of the trial in the second quarter of 2018.
About fast track designation
The FDA’s fast track drug development program is designed to expedite clinical development and submission of applications for drugs with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss the drug’s development plan and written communications about issues such as trial design and use of biomarkers.
Drugs that receive fast track designation may be eligible for accelerated approval and priority review if relevant criteria are met.
Fast track drugs may also be eligible for rolling review, which allows a developer to submit individual sections of a drug’s application for review as they are ready, rather than waiting until all sections are complete.
‘Essential’ genes could be targeted to treat malaria
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
More than 2000 genes are “essential” for the malaria parasite Plasmodium falciparum, according to research published in Science.
Researchers identified 2680 genes that appear necessary for growth and survival during P falciparum’s asexual blood stage.
The researchers therefore believe these genes could be viable therapeutic targets for P falciparum malaria.
“Malaria parasites are extremely technically difficult to manipulate and sequence, and, until this study, only a few of P falciparum’s essential genes had been determined,” said study author Iraad Bronner, of the Wellcome Sanger Institute in Hinxton, UK.
“Our technological advances enabled us to identify all the essential genes in P falciparum—the first time this has been possible for a human malaria parasite.”
To determine which genes P falciparum needs to survive and thrive, the researchers disrupted the parasite’s genes.
The team used piggyBac-transposon insertional mutagenesis to inactivate genes at random and then used DNA sequencing technology to identify which genes were affected.
The researchers made more than 38,000 mutations, then looked for genes that hadn’t been changed, implying they were essential for P falciparum to survive and grow.
This revealed 2680 non-mutable genes, about 1000 of which are conserved in all Plasmodium species and have unknown functions.
“What our team has done is develop a way to analyze every gene in this parasite’s genome,” said study author John H. Adams, PhD, of the University of South Florida in Tampa.
“Using our genetic analysis tools, we’re able to determine the relative importance of each gene for parasite survival. This understanding will help guide future drug development efforts targeting those essential genes.”
The researchers noted that the proteasome pathway had a “high ratio of essential to dispensable genes,” and recent research has linked this pathway to resistance to artemisinin combination therapy.
“We need new drug targets against malaria now more than ever, since our current antimalarial drugs are failing,” said study author Julian C. Rayner, PhD, of Wellcome Sanger Institute.
“This is the first large-scale genetic study in the major human malaria parasite P falciparum and gives a list of 2680 essential genes that researchers can prioritize as promising possible drug targets. We hope this functional genomics approach will help to speed up the pipeline to develop new treatments for this devastating disease.”
Study shows increased risk of VTE among earthquake evacuees
New research has revealed a link between earthquake evacuation and venous thromboembolism (VTE).
The study showed that people who spent the night in their cars after the Kumamoto earthquakes had an increased risk of VTE.
Researchers have therefore called for education about the risk of VTE among people who remain seated and immobile in vehicles for prolonged periods.
“Preventive awareness activities by professional medical teams, supported by education in the media about the risk of VTEs after spending the night in a vehicle, and raising awareness of evacuation centers could lead to a reduced number of victims of VTE,” said Seiji Hokimoto, MD, PhD, of Kumamoto University in Kumamoto, Japan.
Dr Hokimoto and colleagues made this point in a letter published in the Canadian Journal of Cardiology.
The researchers studied the aftermath of the Kumamoto earthquakes that occurred in April 2016.
The team noted that a high number of aftershocks at night prompted many people to evacuate their homes. Although some individuals reached a public evacuation shelter, many were forced to stay in their vehicles overnight.
To assess the impact of remaining seated in cars for extended periods of time, the researchers gathered data from 21 local medical institutions.
They found that 51 patients were hospitalized for VTE after the earthquakes, including 35 who developed pulmonary embolism (PE).
Most of the patients who developed VTE had spent the night in a vehicle (82.4%, n=42).
The researchers found that VTE patients who spent the night in a vehicle were significantly younger than patients who did not, with mean ages of 64.6 ± 13.3 and 79.8 ± 12.1, respectively (P=0.001).
The mean time to onset of VTE after the earthquakes was significantly shorter in patients who spent the night in a vehicle—7.3 ± 5.3 days vs 20.1 ± 25.6 days (P=0.003).
And the incidence of PE was significantly higher in patients who spent the night in a vehicle—83% vs 33% (P=0.001).
“This is a dramatic example of the risks inherent in spending prolonged periods immobilized in a cramped position,” said Stanley Nattel, MD, editor-in-chief of the Canadian Journal of Cardiology.
“It is an important reminder of a public health point and reinforces the need to get up and walk around regularly when on an airplane or when forced to stay in a car for a long time.”
New research has revealed a link between earthquake evacuation and venous thromboembolism (VTE).
The study showed that people who spent the night in their cars after the Kumamoto earthquakes had an increased risk of VTE.
Researchers have therefore called for education about the risk of VTE among people who remain seated and immobile in vehicles for prolonged periods.
“Preventive awareness activities by professional medical teams, supported by education in the media about the risk of VTEs after spending the night in a vehicle, and raising awareness of evacuation centers could lead to a reduced number of victims of VTE,” said Seiji Hokimoto, MD, PhD, of Kumamoto University in Kumamoto, Japan.
Dr Hokimoto and colleagues made this point in a letter published in the Canadian Journal of Cardiology.
The researchers studied the aftermath of the Kumamoto earthquakes that occurred in April 2016.
The team noted that a high number of aftershocks at night prompted many people to evacuate their homes. Although some individuals reached a public evacuation shelter, many were forced to stay in their vehicles overnight.
To assess the impact of remaining seated in cars for extended periods of time, the researchers gathered data from 21 local medical institutions.
They found that 51 patients were hospitalized for VTE after the earthquakes, including 35 who developed pulmonary embolism (PE).
Most of the patients who developed VTE had spent the night in a vehicle (82.4%, n=42).
The researchers found that VTE patients who spent the night in a vehicle were significantly younger than patients who did not, with mean ages of 64.6 ± 13.3 and 79.8 ± 12.1, respectively (P=0.001).
The mean time to onset of VTE after the earthquakes was significantly shorter in patients who spent the night in a vehicle—7.3 ± 5.3 days vs 20.1 ± 25.6 days (P=0.003).
And the incidence of PE was significantly higher in patients who spent the night in a vehicle—83% vs 33% (P=0.001).
“This is a dramatic example of the risks inherent in spending prolonged periods immobilized in a cramped position,” said Stanley Nattel, MD, editor-in-chief of the Canadian Journal of Cardiology.
“It is an important reminder of a public health point and reinforces the need to get up and walk around regularly when on an airplane or when forced to stay in a car for a long time.”
New research has revealed a link between earthquake evacuation and venous thromboembolism (VTE).
The study showed that people who spent the night in their cars after the Kumamoto earthquakes had an increased risk of VTE.
Researchers have therefore called for education about the risk of VTE among people who remain seated and immobile in vehicles for prolonged periods.
“Preventive awareness activities by professional medical teams, supported by education in the media about the risk of VTEs after spending the night in a vehicle, and raising awareness of evacuation centers could lead to a reduced number of victims of VTE,” said Seiji Hokimoto, MD, PhD, of Kumamoto University in Kumamoto, Japan.
Dr Hokimoto and colleagues made this point in a letter published in the Canadian Journal of Cardiology.
The researchers studied the aftermath of the Kumamoto earthquakes that occurred in April 2016.
The team noted that a high number of aftershocks at night prompted many people to evacuate their homes. Although some individuals reached a public evacuation shelter, many were forced to stay in their vehicles overnight.
To assess the impact of remaining seated in cars for extended periods of time, the researchers gathered data from 21 local medical institutions.
They found that 51 patients were hospitalized for VTE after the earthquakes, including 35 who developed pulmonary embolism (PE).
Most of the patients who developed VTE had spent the night in a vehicle (82.4%, n=42).
The researchers found that VTE patients who spent the night in a vehicle were significantly younger than patients who did not, with mean ages of 64.6 ± 13.3 and 79.8 ± 12.1, respectively (P=0.001).
The mean time to onset of VTE after the earthquakes was significantly shorter in patients who spent the night in a vehicle—7.3 ± 5.3 days vs 20.1 ± 25.6 days (P=0.003).
And the incidence of PE was significantly higher in patients who spent the night in a vehicle—83% vs 33% (P=0.001).
“This is a dramatic example of the risks inherent in spending prolonged periods immobilized in a cramped position,” said Stanley Nattel, MD, editor-in-chief of the Canadian Journal of Cardiology.
“It is an important reminder of a public health point and reinforces the need to get up and walk around regularly when on an airplane or when forced to stay in a car for a long time.”
Blood type linked to death risk after trauma
Having type O blood is associated with high death rates in severe trauma patients, according to a study published in Critical Care.
Researchers found that severe trauma patients with type O blood had a death rate of 28%, compared to a rate of 11% in patients with other blood types.
“Loss of blood is the leading cause of death in patients with severe trauma, but studies on the association between different blood types and the risk of trauma death have been scarce,” said study author Wataru Takayama, of Tokyo Medical and Dental University Hospital of Medicine in Japan.
“We wanted to test the hypothesis that trauma survival is affected by differences in blood types.”
To do this, the researchers evaluated the medical records of 901 patients with severe trauma who had been transported to either of 2 tertiary emergency critical care medical centers in Japan from 2013 to 2016.
Most patients had type O (n=284, 32%) or type A blood (n=285, 32%), followed by type B (n=209, 23%) and type AB (n=123, 13%).
The mortality rate was significantly higher in patients with type O blood than in patients with the other blood types—28% and 11%, respectively (P<0.001).
In a multivariate analysis, mortality was significantly higher for patients with type O blood. The adjusted odds ratio was 2.86 (P<0.001).
Patients with type O blood have been shown to have lower levels of von Willebrand factor than patients with other blood types. The researchers suggested that a lower level of von Willebrand factor is a possible explanation for the higher death rate in trauma patients with blood type O.
“Our results also raise questions about how emergency transfusion of O type red blood cells to a severe trauma patient could affect homeostasis . . . and if this is different from other blood types,” Dr Takayama said.
“Further research is necessary to investigate the results of our study and develop the best treatment strategy for severe trauma patients.”
In particular, further research is needed to determine if the findings from this study apply to other ethnic groups, as all the patients in this study were Japanese.
In addition, the researchers didn’t evaluate the impact of the individual blood types A, AB, or B on severe trauma death rates. They only compared type O to non-O blood types, which may have diluted the effect of individual blood types on patient survival.
Having type O blood is associated with high death rates in severe trauma patients, according to a study published in Critical Care.
Researchers found that severe trauma patients with type O blood had a death rate of 28%, compared to a rate of 11% in patients with other blood types.
“Loss of blood is the leading cause of death in patients with severe trauma, but studies on the association between different blood types and the risk of trauma death have been scarce,” said study author Wataru Takayama, of Tokyo Medical and Dental University Hospital of Medicine in Japan.
“We wanted to test the hypothesis that trauma survival is affected by differences in blood types.”
To do this, the researchers evaluated the medical records of 901 patients with severe trauma who had been transported to either of 2 tertiary emergency critical care medical centers in Japan from 2013 to 2016.
Most patients had type O (n=284, 32%) or type A blood (n=285, 32%), followed by type B (n=209, 23%) and type AB (n=123, 13%).
The mortality rate was significantly higher in patients with type O blood than in patients with the other blood types—28% and 11%, respectively (P<0.001).
In a multivariate analysis, mortality was significantly higher for patients with type O blood. The adjusted odds ratio was 2.86 (P<0.001).
Patients with type O blood have been shown to have lower levels of von Willebrand factor than patients with other blood types. The researchers suggested that a lower level of von Willebrand factor is a possible explanation for the higher death rate in trauma patients with blood type O.
“Our results also raise questions about how emergency transfusion of O type red blood cells to a severe trauma patient could affect homeostasis . . . and if this is different from other blood types,” Dr Takayama said.
“Further research is necessary to investigate the results of our study and develop the best treatment strategy for severe trauma patients.”
In particular, further research is needed to determine if the findings from this study apply to other ethnic groups, as all the patients in this study were Japanese.
In addition, the researchers didn’t evaluate the impact of the individual blood types A, AB, or B on severe trauma death rates. They only compared type O to non-O blood types, which may have diluted the effect of individual blood types on patient survival.
Having type O blood is associated with high death rates in severe trauma patients, according to a study published in Critical Care.
Researchers found that severe trauma patients with type O blood had a death rate of 28%, compared to a rate of 11% in patients with other blood types.
“Loss of blood is the leading cause of death in patients with severe trauma, but studies on the association between different blood types and the risk of trauma death have been scarce,” said study author Wataru Takayama, of Tokyo Medical and Dental University Hospital of Medicine in Japan.
“We wanted to test the hypothesis that trauma survival is affected by differences in blood types.”
To do this, the researchers evaluated the medical records of 901 patients with severe trauma who had been transported to either of 2 tertiary emergency critical care medical centers in Japan from 2013 to 2016.
Most patients had type O (n=284, 32%) or type A blood (n=285, 32%), followed by type B (n=209, 23%) and type AB (n=123, 13%).
The mortality rate was significantly higher in patients with type O blood than in patients with the other blood types—28% and 11%, respectively (P<0.001).
In a multivariate analysis, mortality was significantly higher for patients with type O blood. The adjusted odds ratio was 2.86 (P<0.001).
Patients with type O blood have been shown to have lower levels of von Willebrand factor than patients with other blood types. The researchers suggested that a lower level of von Willebrand factor is a possible explanation for the higher death rate in trauma patients with blood type O.
“Our results also raise questions about how emergency transfusion of O type red blood cells to a severe trauma patient could affect homeostasis . . . and if this is different from other blood types,” Dr Takayama said.
“Further research is necessary to investigate the results of our study and develop the best treatment strategy for severe trauma patients.”
In particular, further research is needed to determine if the findings from this study apply to other ethnic groups, as all the patients in this study were Japanese.
In addition, the researchers didn’t evaluate the impact of the individual blood types A, AB, or B on severe trauma death rates. They only compared type O to non-O blood types, which may have diluted the effect of individual blood types on patient survival.
Single injection could treat hemophilia B long-term
Cell therapy could produce lasting effects in hemophilia B, according to a group of researchers.
They genetically modified induced pluripotent cells (iPSCs) derived from patients with hemophilia B and converted those iPSCs into hepatocyte-like cells (HLCs).
When transplanted into mouse models of hemophilia B, the HLCs remained functional for months, increasing levels of factor IX (FIX) and clotting efficiency.
However, the HLCs were substantially less effective than cryopreserved human hepatocytes (hHeps), which were able to correct clotting defects in mice long-term.
“The appeal of a cell-based approach is that you minimize the number of treatments that a patient needs,” explained Suvasini Ramaswamy, PhD, of The Boston Consulting Group in Massachusetts.
“Rather than constant injections, you can do this in one shot.”
Dr Ramaswamy and her colleagues described their results with this approach in Cell Reports. Study authors include employees of Shire Therapeutics, Vertex Pharmaceuticals, and Thermo Fisher Scientific.
The researchers first developed a quadruple knockout mouse model of hemophilia B that allows for the engraftment and expansion of hHeps. The team crossed transgenic FIX-/--deficient mice with Rag2-/- IL2rg -/- Fah-/- mice to create this model.
The researchers transplanted cryopreserved hHeps into the mice and observed a sustained increase in circulating levels of human albumin, human FIX, and clusters of FIX- or Fah-positive cells in the liver.
The team said the hHeps were able to restore clotting function to wild-type levels in the mice—at least 10-fold higher than levels needed for a significant improvement in hemophilia B.
The hHeps remained functional for up to a year, and the researchers believe the cells could persist even longer. The team noted that there was no difference in the efficacy of hHeps from different donors or vendors.
The researchers then tested the cell therapy they developed using iPSCs. They collected blood samples from 2 patients with severe hemophilia B, reprogrammed peripheral blood-derived mononuclear cells into iPSCs, and used CRISPR/Cas9 to repair the mutations in each patient’s FIX gene.
The team coaxed those repaired cells into HLCs and tested the HLCs in the mouse model of hemophilia B. The HLCs were transplanted through the spleen so the cells were distributed uniformly in the liver.
The researchers said the HLCs were present and functional in the liver for up to a year, but they were less effective than hHeps. Mice that received HLCs experienced “modest” increases in clotting efficiency, from less than 10% to about 25% of wild-type activity.
The researchers believe this work demonstrates the value of combining stem cell reprogramming and gene-modifying approaches to treat genetic diseases. However, more work is needed to optimize this approach for hemophilia B.
Cell therapy could produce lasting effects in hemophilia B, according to a group of researchers.
They genetically modified induced pluripotent cells (iPSCs) derived from patients with hemophilia B and converted those iPSCs into hepatocyte-like cells (HLCs).
When transplanted into mouse models of hemophilia B, the HLCs remained functional for months, increasing levels of factor IX (FIX) and clotting efficiency.
However, the HLCs were substantially less effective than cryopreserved human hepatocytes (hHeps), which were able to correct clotting defects in mice long-term.
“The appeal of a cell-based approach is that you minimize the number of treatments that a patient needs,” explained Suvasini Ramaswamy, PhD, of The Boston Consulting Group in Massachusetts.
“Rather than constant injections, you can do this in one shot.”
Dr Ramaswamy and her colleagues described their results with this approach in Cell Reports. Study authors include employees of Shire Therapeutics, Vertex Pharmaceuticals, and Thermo Fisher Scientific.
The researchers first developed a quadruple knockout mouse model of hemophilia B that allows for the engraftment and expansion of hHeps. The team crossed transgenic FIX-/--deficient mice with Rag2-/- IL2rg -/- Fah-/- mice to create this model.
The researchers transplanted cryopreserved hHeps into the mice and observed a sustained increase in circulating levels of human albumin, human FIX, and clusters of FIX- or Fah-positive cells in the liver.
The team said the hHeps were able to restore clotting function to wild-type levels in the mice—at least 10-fold higher than levels needed for a significant improvement in hemophilia B.
The hHeps remained functional for up to a year, and the researchers believe the cells could persist even longer. The team noted that there was no difference in the efficacy of hHeps from different donors or vendors.
The researchers then tested the cell therapy they developed using iPSCs. They collected blood samples from 2 patients with severe hemophilia B, reprogrammed peripheral blood-derived mononuclear cells into iPSCs, and used CRISPR/Cas9 to repair the mutations in each patient’s FIX gene.
The team coaxed those repaired cells into HLCs and tested the HLCs in the mouse model of hemophilia B. The HLCs were transplanted through the spleen so the cells were distributed uniformly in the liver.
The researchers said the HLCs were present and functional in the liver for up to a year, but they were less effective than hHeps. Mice that received HLCs experienced “modest” increases in clotting efficiency, from less than 10% to about 25% of wild-type activity.
The researchers believe this work demonstrates the value of combining stem cell reprogramming and gene-modifying approaches to treat genetic diseases. However, more work is needed to optimize this approach for hemophilia B.
Cell therapy could produce lasting effects in hemophilia B, according to a group of researchers.
They genetically modified induced pluripotent cells (iPSCs) derived from patients with hemophilia B and converted those iPSCs into hepatocyte-like cells (HLCs).
When transplanted into mouse models of hemophilia B, the HLCs remained functional for months, increasing levels of factor IX (FIX) and clotting efficiency.
However, the HLCs were substantially less effective than cryopreserved human hepatocytes (hHeps), which were able to correct clotting defects in mice long-term.
“The appeal of a cell-based approach is that you minimize the number of treatments that a patient needs,” explained Suvasini Ramaswamy, PhD, of The Boston Consulting Group in Massachusetts.
“Rather than constant injections, you can do this in one shot.”
Dr Ramaswamy and her colleagues described their results with this approach in Cell Reports. Study authors include employees of Shire Therapeutics, Vertex Pharmaceuticals, and Thermo Fisher Scientific.
The researchers first developed a quadruple knockout mouse model of hemophilia B that allows for the engraftment and expansion of hHeps. The team crossed transgenic FIX-/--deficient mice with Rag2-/- IL2rg -/- Fah-/- mice to create this model.
The researchers transplanted cryopreserved hHeps into the mice and observed a sustained increase in circulating levels of human albumin, human FIX, and clusters of FIX- or Fah-positive cells in the liver.
The team said the hHeps were able to restore clotting function to wild-type levels in the mice—at least 10-fold higher than levels needed for a significant improvement in hemophilia B.
The hHeps remained functional for up to a year, and the researchers believe the cells could persist even longer. The team noted that there was no difference in the efficacy of hHeps from different donors or vendors.
The researchers then tested the cell therapy they developed using iPSCs. They collected blood samples from 2 patients with severe hemophilia B, reprogrammed peripheral blood-derived mononuclear cells into iPSCs, and used CRISPR/Cas9 to repair the mutations in each patient’s FIX gene.
The team coaxed those repaired cells into HLCs and tested the HLCs in the mouse model of hemophilia B. The HLCs were transplanted through the spleen so the cells were distributed uniformly in the liver.
The researchers said the HLCs were present and functional in the liver for up to a year, but they were less effective than hHeps. Mice that received HLCs experienced “modest” increases in clotting efficiency, from less than 10% to about 25% of wild-type activity.
The researchers believe this work demonstrates the value of combining stem cell reprogramming and gene-modifying approaches to treat genetic diseases. However, more work is needed to optimize this approach for hemophilia B.
FDA issues CRL for proposed biosimilar rituximab
The US Food and Drug Administration (FDA) has issued a complete response letter (CRL) saying the agency cannot approve Sandoz’s proposed biosimilar rituximab.
Sandoz submitted the biologics licensing application for the product, known as GP2013, in September 2017.
The company was seeking approval for GP2013 to treat follicular lymphoma (FL), diffuse large B-cell lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
The drug already has approval for these indications in Europe. The European Commission approved GP2013 (Rixathon) in June 2017.
As for US approval, Sandoz said it is evaluating the content of the FDA’s CRL and “remains committed to further discussions with FDA in order to bring this important medicine to US patients as soon as possible.”
The company said it “stands behind the robust body of evidence included in the regulatory submission” for GP2013.
Part of this evidence is the ASSIST-FL trial, in which researchers compared GP2013 to the reference product, Roche’s MabThera. Results from this trial were published in The Lancet Haematology and presented at ESMO 2017 Congress.
This phase 3 trial included adults with previously untreated, advanced stage FL. Patients received 8 cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% (271/311) in the GP2013 arm and 88% in the rituximab arm (274/313). Complete response rates were 15% (n=46) and 13% (n=42), respectively.
Rates of adverse events (AEs) were 93% in the GP2013 arm and 91% in the rituximab arm. Rates of serious AEs were 23% and 20%, respectively. The rate of discontinuation due to AEs was 7% in both arms.
The most common AE was neutropenia, which occurred in 26% of patients in the GP2013 arm and 30% of those in the rituximab arm in the combination phase. Rates of neutropenia in the maintenance phase were 10% and 6%, respectively.
The US Food and Drug Administration (FDA) has issued a complete response letter (CRL) saying the agency cannot approve Sandoz’s proposed biosimilar rituximab.
Sandoz submitted the biologics licensing application for the product, known as GP2013, in September 2017.
The company was seeking approval for GP2013 to treat follicular lymphoma (FL), diffuse large B-cell lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
The drug already has approval for these indications in Europe. The European Commission approved GP2013 (Rixathon) in June 2017.
As for US approval, Sandoz said it is evaluating the content of the FDA’s CRL and “remains committed to further discussions with FDA in order to bring this important medicine to US patients as soon as possible.”
The company said it “stands behind the robust body of evidence included in the regulatory submission” for GP2013.
Part of this evidence is the ASSIST-FL trial, in which researchers compared GP2013 to the reference product, Roche’s MabThera. Results from this trial were published in The Lancet Haematology and presented at ESMO 2017 Congress.
This phase 3 trial included adults with previously untreated, advanced stage FL. Patients received 8 cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% (271/311) in the GP2013 arm and 88% in the rituximab arm (274/313). Complete response rates were 15% (n=46) and 13% (n=42), respectively.
Rates of adverse events (AEs) were 93% in the GP2013 arm and 91% in the rituximab arm. Rates of serious AEs were 23% and 20%, respectively. The rate of discontinuation due to AEs was 7% in both arms.
The most common AE was neutropenia, which occurred in 26% of patients in the GP2013 arm and 30% of those in the rituximab arm in the combination phase. Rates of neutropenia in the maintenance phase were 10% and 6%, respectively.
The US Food and Drug Administration (FDA) has issued a complete response letter (CRL) saying the agency cannot approve Sandoz’s proposed biosimilar rituximab.
Sandoz submitted the biologics licensing application for the product, known as GP2013, in September 2017.
The company was seeking approval for GP2013 to treat follicular lymphoma (FL), diffuse large B-cell lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, and microscopic polyangiitis.
The drug already has approval for these indications in Europe. The European Commission approved GP2013 (Rixathon) in June 2017.
As for US approval, Sandoz said it is evaluating the content of the FDA’s CRL and “remains committed to further discussions with FDA in order to bring this important medicine to US patients as soon as possible.”
The company said it “stands behind the robust body of evidence included in the regulatory submission” for GP2013.
Part of this evidence is the ASSIST-FL trial, in which researchers compared GP2013 to the reference product, Roche’s MabThera. Results from this trial were published in The Lancet Haematology and presented at ESMO 2017 Congress.
This phase 3 trial included adults with previously untreated, advanced stage FL. Patients received 8 cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% (271/311) in the GP2013 arm and 88% in the rituximab arm (274/313). Complete response rates were 15% (n=46) and 13% (n=42), respectively.
Rates of adverse events (AEs) were 93% in the GP2013 arm and 91% in the rituximab arm. Rates of serious AEs were 23% and 20%, respectively. The rate of discontinuation due to AEs was 7% in both arms.
The most common AE was neutropenia, which occurred in 26% of patients in the GP2013 arm and 30% of those in the rituximab arm in the combination phase. Rates of neutropenia in the maintenance phase were 10% and 6%, respectively.