User login
Team recommends changes to trial guidelines
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
Researchers have recommended changes to international guidelines used in the development of clinical trials.
The group’s goal is to improve the use of patient-reported outcomes (PROs)—feedback from patients about how the clinical trial has affected their overall health and quality of life.
“Patient-reported outcome data from clinical trials can provide valuable evidence to inform shared-decision making, pharmaceutical labeling claims, clinical guidelines, and health policy,” said Melanie Calvert, PhD, of the University of Birmingham in Edgbaston, Birmingham, England.
“However, clinical trial protocols often lack important information regarding the collection of quality of life and symptom data. Working in collaboration with international stakeholders, we have developed consensus-based, PRO-specific protocol guidance to help ensure high-quality data to inform patient-centered care.”
Dr Calvert and her colleagues published the guidance in JAMA.
The guidance is known as the SPIRIT-PRO Extension. The SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) statement, which was published in 2013, was intended to improve trial protocols by providing evidence-based recommendations for the minimum set of items to be addressed.
To add a PRO component to SPIRIT, Dr Calvert and her colleagues conducted a systematic review of existing PRO-specific protocol guidance. A taskforce used this data to compile a list of potential PRO-specific protocol items.
The review revealed 162 PRO-specific protocol recommendations, and the task force reduced this to 56. After 138 international stakeholders and 99 Delphi panelists weighed in, the final recommendations were agreed upon by 29 participants at a consensus meeting.
The final recommendations include 11 extensions and 5 elaborations to the SPIRIT checklist. The recommendations focus on PRO-specific issues relating to objectives, eligibility criteria, data collection, monitoring, and other aspects of trials.
“While this guidance has been developed for trials where PROs are a primary or key secondary outcome, we are actively encouraging protocol writers to consider use of this guidance in all trials or clinical research studies where PROs are collected,” Dr Calvert said.
“The guidance does not aim to be prescriptive, but instead to encourage and facilitate careful planning of PRO components of trials and thereby improve PRO trial design, which we hope will help staff and patients understand the rationale for PRO assessment, improve PRO data completeness and quality, facilitate high-quality analysis and reporting, and ultimately improve the quality of the global PRO evidence base.” ![]()
FDA expands approved use of ferumoxytol injection
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for ferumoxytol injection (Feraheme®).
The drug is now approved to treat adults with iron deficiency anemia (IDA) who cannot tolerate or have had an unsatisfactory response to oral iron.
Ferumoxytol injection was previously approved by the FDA to treat IDA in adults with chronic kidney disease.
“Iron deficiency anemia is a serious and under-treated health condition which negatively impacts quality of life for millions of people, many of whom do not benefit from or cannot tolerate oral iron therapy,” said Michael Auerbach, MD, of Georgetown University School of Medicine in Washington, DC.
“Physicians now have a new option for patients who meet the broader ferumoxytol injection indication that can be administered in 15 minutes, providing a gram of iron in 2 doses as few as 3 days apart.”
The expanded approval for ferumoxytol injection was supported by a trio of phase 3 trials. All 3 trials included IDA patients who could not tolerate or had an unsatisfactory response to oral iron.
In the first trial (NCT01114139), researchers compared ferumoxytol injection to placebo.
The second trial (NCT01114204) was a comparison of ferumoxytol injection and iron sucrose.
In the third trial (NCT02694978), researchers compared ferumoxytol injection to ferric carboxymaltose injection (Injectafer®).
Details on these trials are included in the prescribing information for ferumoxytol injection, which is available at www.feraheme.com.
The prescribing information includes a boxed warning detailing the risk of fatal and serious hypersensitivity reactions, including anaphylaxis, in patients receiving ferumoxytol injection.
Ferumoxytol injection is a product of AMAG Pharmaceuticals, Inc.
The company has a patient access support program called AMAG Assist™. Uninsured or underinsured patients who need help paying for their ferumoxytol injection prescription can call 844-635-2624 to see if they qualify for help. ![]()
Analysis reveals potential MM risk variants
Researchers have used high-risk pedigrees (HRPs) to identify gene variants that may cause multiple myeloma (MM).
The team’s analysis revealed shared genomic segments harboring genes with potential MM risk variants.
These single nucleotide variants (SNVs) are in USP45, a gene involved in DNA repair, and ARID1A, a gene in the SWI/SNF chromatin remodeling complex.
Nicola Camp, PhD, of the University of Utah School of Medicine in Salt Lake City, and her colleagues reported these findings in PLOS Genetics.
The researchers developed a new method to analyze HRPs (large, multi-generational families with more affected members than would be expected by chance) to identify shared regions of the genome that likely harbor MM risk variants.
The team applied the method using pedigrees from 11 Utah families at risk of MM as well as whole-exome sequencing of shared genomic segments in 1063 patients with MM or monoclonal gammopathy of undetermined significance (MGUS) and 964 control subjects.
The analysis revealed 2 regions that may contribute to MM. One was a 1.8 Mb segment at 6q16 with SNVs in USP45, and the other was a 1.2 Mb segment at 1p36.11 with SNVs in ARID1A.
One of the SNVs in USP45 was a stop gain—p.Gln691*—which was shared by 3 siblings, 1 with MM and 2 with MGUS. The other was a missense SNV—p.Gln621Glu—which was shared by 2 of 4 siblings in a family, 1 with MM and 1 with MGUS.
One of the missense SNVs in ARID1A—rs752026201, p. Ser90Gly—was shared by 3 MM cases. The other missense SNV—rs140664170, p.Met890Val—was shared by 2 cousins with MM.
The researchers believe these findings show that HRPs can be effective for identifying risk variants in complex diseases.
“We are very encouraged by the new method,” Dr Camp said. “It certainly plays to the strengths of the large Utah pedigrees, revitalizing the family design for complex diseases. As we did in this study, the focused regions can be further investigated in smaller families to find genes and specific mutations. The method can be used for any complex disease.”
“We are already pursuing large pedigrees in several other domains, including other cancers, psychiatric disorders, birth defects, and pre-term birth phenotypes, with several more genome-wide significant regions found. We’re excited about the potential.” ![]()
Researchers have used high-risk pedigrees (HRPs) to identify gene variants that may cause multiple myeloma (MM).
The team’s analysis revealed shared genomic segments harboring genes with potential MM risk variants.
These single nucleotide variants (SNVs) are in USP45, a gene involved in DNA repair, and ARID1A, a gene in the SWI/SNF chromatin remodeling complex.
Nicola Camp, PhD, of the University of Utah School of Medicine in Salt Lake City, and her colleagues reported these findings in PLOS Genetics.
The researchers developed a new method to analyze HRPs (large, multi-generational families with more affected members than would be expected by chance) to identify shared regions of the genome that likely harbor MM risk variants.
The team applied the method using pedigrees from 11 Utah families at risk of MM as well as whole-exome sequencing of shared genomic segments in 1063 patients with MM or monoclonal gammopathy of undetermined significance (MGUS) and 964 control subjects.
The analysis revealed 2 regions that may contribute to MM. One was a 1.8 Mb segment at 6q16 with SNVs in USP45, and the other was a 1.2 Mb segment at 1p36.11 with SNVs in ARID1A.
One of the SNVs in USP45 was a stop gain—p.Gln691*—which was shared by 3 siblings, 1 with MM and 2 with MGUS. The other was a missense SNV—p.Gln621Glu—which was shared by 2 of 4 siblings in a family, 1 with MM and 1 with MGUS.
One of the missense SNVs in ARID1A—rs752026201, p. Ser90Gly—was shared by 3 MM cases. The other missense SNV—rs140664170, p.Met890Val—was shared by 2 cousins with MM.
The researchers believe these findings show that HRPs can be effective for identifying risk variants in complex diseases.
“We are very encouraged by the new method,” Dr Camp said. “It certainly plays to the strengths of the large Utah pedigrees, revitalizing the family design for complex diseases. As we did in this study, the focused regions can be further investigated in smaller families to find genes and specific mutations. The method can be used for any complex disease.”
“We are already pursuing large pedigrees in several other domains, including other cancers, psychiatric disorders, birth defects, and pre-term birth phenotypes, with several more genome-wide significant regions found. We’re excited about the potential.” ![]()
Researchers have used high-risk pedigrees (HRPs) to identify gene variants that may cause multiple myeloma (MM).
The team’s analysis revealed shared genomic segments harboring genes with potential MM risk variants.
These single nucleotide variants (SNVs) are in USP45, a gene involved in DNA repair, and ARID1A, a gene in the SWI/SNF chromatin remodeling complex.
Nicola Camp, PhD, of the University of Utah School of Medicine in Salt Lake City, and her colleagues reported these findings in PLOS Genetics.
The researchers developed a new method to analyze HRPs (large, multi-generational families with more affected members than would be expected by chance) to identify shared regions of the genome that likely harbor MM risk variants.
The team applied the method using pedigrees from 11 Utah families at risk of MM as well as whole-exome sequencing of shared genomic segments in 1063 patients with MM or monoclonal gammopathy of undetermined significance (MGUS) and 964 control subjects.
The analysis revealed 2 regions that may contribute to MM. One was a 1.8 Mb segment at 6q16 with SNVs in USP45, and the other was a 1.2 Mb segment at 1p36.11 with SNVs in ARID1A.
One of the SNVs in USP45 was a stop gain—p.Gln691*—which was shared by 3 siblings, 1 with MM and 2 with MGUS. The other was a missense SNV—p.Gln621Glu—which was shared by 2 of 4 siblings in a family, 1 with MM and 1 with MGUS.
One of the missense SNVs in ARID1A—rs752026201, p. Ser90Gly—was shared by 3 MM cases. The other missense SNV—rs140664170, p.Met890Val—was shared by 2 cousins with MM.
The researchers believe these findings show that HRPs can be effective for identifying risk variants in complex diseases.
“We are very encouraged by the new method,” Dr Camp said. “It certainly plays to the strengths of the large Utah pedigrees, revitalizing the family design for complex diseases. As we did in this study, the focused regions can be further investigated in smaller families to find genes and specific mutations. The method can be used for any complex disease.”
“We are already pursuing large pedigrees in several other domains, including other cancers, psychiatric disorders, birth defects, and pre-term birth phenotypes, with several more genome-wide significant regions found. We’re excited about the potential.” ![]()
FDA investigating VTEs related to ECP
The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

The US Food and Drug Administration (FDA) says it is evaluating reports of venous thromboembolism (VTE) in patients treated with the CELLEX Photopheresis System by Therakos, Inc.
This extracorporeal photopheresis (ECP) device system is FDA-approved for use in patients with cutaneous T-cell lymphoma (CTCL).
The system is used to perform ultraviolet-A irradiation of a patient’s own leukocyte-enriched blood that is then used as palliative treatment for skin manifestations of CTCL that are unresponsive to other forms of treatment.
The CELLEX Photopheresis System is also used to treat graft-vs-host disease (GVHD) that is resistant to standard immunosuppressive therapy and acute cardiac allograft rejection that is resistant to standard immunosuppressive therapy.
The CELLEX Photopheresis System uses methoxsalen as a photosensitizing agent and heparin as an anticoagulant.
Since 2012, the FDA has received 7 reports of pulmonary embolism (PE) and 2 reports of deep vein thrombosis (DVT) occurring during or soon after treatment with the CELLEX Photopheresis System.
Two of the patients who developed a PE died, although it’s not clear whether PE was the cause of death.
Four of the 7 PEs occurred in patients undergoing treatment for GVHD, including the 2 patients who died. Both DVTs occurred in patients undergoing treatment for GVHD as well.
The FDA is recommending that healthcare providers inform patients, clinical staff, and technicians that PE and DVT can occur during or after an ECP procedure.
The agency also recommends that healthcare providers consult device labeling regarding anticoagulation and use clinical judgment in adjusting a patient’s heparin dosage.
Finally, providers should report VTEs related to ECP procedures to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program.
If possible, reports should include the following:
- The indication for ECP therapy
- Comorbidities that may predispose a patient to increased coagulation and history of DVT or PE
- The anticoagulation regimen used
- The number of ECP sessions the patient underwent prior to VTE onset, including the date of the first treatment session, frequency of treatment sessions, and timing of the final treatment
- Timing of the VTE in relation to the most recent treatment session
- Interventions required to manage the VTE.

Socioeconomic deprivation tied to survival in ALL
Socioeconomic deprivation may decrease survival in adults with acute lymphoblastic leukemia (ALL), according to research published in BMC Cancer.
Researchers found that ALL patients living in more deprived areas of England had a 16% to 21% greater risk of dying than patients living in the least deprived areas.
The researchers also observed a 33% higher risk of mortality in patients who were treated at hospitals that manage few ALL patients.
“The findings are likely to have significant implications for the organization of NHS [National Health Service] services for the treatment of adults with this rare but serious condition,” said study author Ravi Maheswaran, MD, of the University of Sheffield in Sheffield, UK.
To conduct this study, Dr Maheswaran and Nick Morley, MBBS, of Royal Hallamshire Hospital in Sheffield, analyzed anonymized NHS data on hospital admissions.
The researchers identified 2921 adults (age 18 and older) who were diagnosed with ALL from 2001 to 2012 and assessed follow-up data on survival rates up to 2013.
There were 1870 deaths during follow-up, and the 5-year survival rate was 32%.
As expected, survival decreased with age but increased over time. The mortality hazard ratio (HR) was 1.38 for patients ages 30 to 39, 3.72 for patients ages 60 to 69, and 9.02 for patients age 80 and older.
The HR was 0.98 for patients diagnosed from 2005 to 2008 and 0.70 for patients diagnosed from 2009 to 2012, compared to 1.00 for patients diagnosed from 2001 to 2004.
Patients living in areas of socioeconomic deprivation had a greater risk of death, but it did not seem to matter whether the patients lived in rural or urban areas.
The mortality HR was 1.16 for patients living in the most deprived areas and 1.21 for patients in intermediate areas (with the least deprived areas as the reference, 1.00). The HR was 1.00 for both rural and urban areas.
The risk of death was higher for patients treated at hospitals with low volumes of adults with ALL. The mortality HR was 1.33 for low-volume hospitals, which were defined as hospitals with 15 or fewer ALL patients admitted over a 3-year time period for which data were available.
“These results, although concerning, are from a single study, and further work is needed to confirm our findings,” Dr Maheswaran said.
“If the association between high deprivation and poorer survival is confirmed, more investigation will be needed to understand why adults with this type of leukemia living in deprived areas have poorer survival and what can be done to address this inequality.”
“Confirmation that hospitals treating few patients with this rare condition have worse outcomes would mean that the NHS should seriously consider if treatment services for adults with acute lymphoblastic leukemia should mainly be provided by specialist centers in order to improve survival.” ![]()
Socioeconomic deprivation may decrease survival in adults with acute lymphoblastic leukemia (ALL), according to research published in BMC Cancer.
Researchers found that ALL patients living in more deprived areas of England had a 16% to 21% greater risk of dying than patients living in the least deprived areas.
The researchers also observed a 33% higher risk of mortality in patients who were treated at hospitals that manage few ALL patients.
“The findings are likely to have significant implications for the organization of NHS [National Health Service] services for the treatment of adults with this rare but serious condition,” said study author Ravi Maheswaran, MD, of the University of Sheffield in Sheffield, UK.
To conduct this study, Dr Maheswaran and Nick Morley, MBBS, of Royal Hallamshire Hospital in Sheffield, analyzed anonymized NHS data on hospital admissions.
The researchers identified 2921 adults (age 18 and older) who were diagnosed with ALL from 2001 to 2012 and assessed follow-up data on survival rates up to 2013.
There were 1870 deaths during follow-up, and the 5-year survival rate was 32%.
As expected, survival decreased with age but increased over time. The mortality hazard ratio (HR) was 1.38 for patients ages 30 to 39, 3.72 for patients ages 60 to 69, and 9.02 for patients age 80 and older.
The HR was 0.98 for patients diagnosed from 2005 to 2008 and 0.70 for patients diagnosed from 2009 to 2012, compared to 1.00 for patients diagnosed from 2001 to 2004.
Patients living in areas of socioeconomic deprivation had a greater risk of death, but it did not seem to matter whether the patients lived in rural or urban areas.
The mortality HR was 1.16 for patients living in the most deprived areas and 1.21 for patients in intermediate areas (with the least deprived areas as the reference, 1.00). The HR was 1.00 for both rural and urban areas.
The risk of death was higher for patients treated at hospitals with low volumes of adults with ALL. The mortality HR was 1.33 for low-volume hospitals, which were defined as hospitals with 15 or fewer ALL patients admitted over a 3-year time period for which data were available.
“These results, although concerning, are from a single study, and further work is needed to confirm our findings,” Dr Maheswaran said.
“If the association between high deprivation and poorer survival is confirmed, more investigation will be needed to understand why adults with this type of leukemia living in deprived areas have poorer survival and what can be done to address this inequality.”
“Confirmation that hospitals treating few patients with this rare condition have worse outcomes would mean that the NHS should seriously consider if treatment services for adults with acute lymphoblastic leukemia should mainly be provided by specialist centers in order to improve survival.” ![]()
Socioeconomic deprivation may decrease survival in adults with acute lymphoblastic leukemia (ALL), according to research published in BMC Cancer.
Researchers found that ALL patients living in more deprived areas of England had a 16% to 21% greater risk of dying than patients living in the least deprived areas.
The researchers also observed a 33% higher risk of mortality in patients who were treated at hospitals that manage few ALL patients.
“The findings are likely to have significant implications for the organization of NHS [National Health Service] services for the treatment of adults with this rare but serious condition,” said study author Ravi Maheswaran, MD, of the University of Sheffield in Sheffield, UK.
To conduct this study, Dr Maheswaran and Nick Morley, MBBS, of Royal Hallamshire Hospital in Sheffield, analyzed anonymized NHS data on hospital admissions.
The researchers identified 2921 adults (age 18 and older) who were diagnosed with ALL from 2001 to 2012 and assessed follow-up data on survival rates up to 2013.
There were 1870 deaths during follow-up, and the 5-year survival rate was 32%.
As expected, survival decreased with age but increased over time. The mortality hazard ratio (HR) was 1.38 for patients ages 30 to 39, 3.72 for patients ages 60 to 69, and 9.02 for patients age 80 and older.
The HR was 0.98 for patients diagnosed from 2005 to 2008 and 0.70 for patients diagnosed from 2009 to 2012, compared to 1.00 for patients diagnosed from 2001 to 2004.
Patients living in areas of socioeconomic deprivation had a greater risk of death, but it did not seem to matter whether the patients lived in rural or urban areas.
The mortality HR was 1.16 for patients living in the most deprived areas and 1.21 for patients in intermediate areas (with the least deprived areas as the reference, 1.00). The HR was 1.00 for both rural and urban areas.
The risk of death was higher for patients treated at hospitals with low volumes of adults with ALL. The mortality HR was 1.33 for low-volume hospitals, which were defined as hospitals with 15 or fewer ALL patients admitted over a 3-year time period for which data were available.
“These results, although concerning, are from a single study, and further work is needed to confirm our findings,” Dr Maheswaran said.
“If the association between high deprivation and poorer survival is confirmed, more investigation will be needed to understand why adults with this type of leukemia living in deprived areas have poorer survival and what can be done to address this inequality.”
“Confirmation that hospitals treating few patients with this rare condition have worse outcomes would mean that the NHS should seriously consider if treatment services for adults with acute lymphoblastic leukemia should mainly be provided by specialist centers in order to improve survival.” ![]()
In situ vaccination eradicates lymphoma, other cancers
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
Experiments in mice have shown that injecting immune-stimulating agents directly into a tumor can help the immune system eradicate tumors in other areas of the body.
The approach worked for several cancers, including lymphomas.
The researchers believe the local application of the agents could serve as a rapid and relatively inexpensive cancer therapy that is unlikely to cause the adverse effects often seen with more widespread immune stimulation.
“Our approach uses a one-time application of very small amounts of two agents to stimulate the immune cells only within the tumor itself,” said Ronald Levy, MD, of Stanford University Medical Center in California.
“In the mice, we saw amazing, body-wide effects, including the elimination of tumors all over the animal. This approach bypasses the need to identify tumor-specific immune targets and doesn’t require wholesale activation of the immune system or customization of a patient’s immune cells.”
Dr Levy and his colleagues described this approach in Science Translational Medicine.
The method involves reactivating cancer-specific T cells by injecting microgram amounts of two agents directly into the tumor site.
One of the agents is an unmethylated CG–enriched oligodeoxynucleotide (CpG)—a Toll-like receptor 9 (TLR9) ligand. It works with nearby immune cells to amplify the expression of OX40 on the surface of T cells.
The other agent is an antibody that binds to OX40. It activates the T cells to lead the charge against the cancer cells.
Because the agents are injected directly into the tumor, only T cells that have infiltrated it are activated. In effect, these T cells are “prescreened” by the body to recognize only cancer-specific proteins.
Some of these tumor-specific, activated T cells then leave the original tumor to find and destroy other identical tumors throughout the body.
The researchers found this approach worked well in mice with A20 B-cell lymphoma tumors transplanted in two sites on their bodies.
Injecting one tumor site with the agents caused regression of the untreated tumor as well as the treated one. In this way, 87 of 90 mice were cured.
Although lymphoma recurred in 3 of the mice, the tumors again regressed after a second treatment with CpG and anti-OX40.
The researchers saw similar results in mice with melanoma as well as breast and colon cancer.
Mice genetically engineered to spontaneously develop breast cancers in all 10 of their mammary pads also responded to the treatment. Treating the first tumor that arose often prevented the occurrence of future tumors and significantly increased the animals’ life span, the researchers found.
Finally, the team explored the specificity of the T cells by transplanting two types of tumors into mice.
They transplanted A20 lymphoma cells in two locations and a colon cancer cell line in a third location. Treatment of one of the lymphoma sites caused the regression of both lymphoma tumors but did not affect the colon cancer cells.
“This is a very targeted approach,” Dr Levy said. “Only the tumor that shares the protein targets displayed by the treated site is affected. We’re attacking specific targets without having to identify exactly what proteins the T cells are recognizing.”
Dr Levy and his colleagues have launched a clinical trial (NCT03410901) to test this treatment approach. The researchers hope to determine the adverse effects and optimal dose of the TLR9 agonist SD-101, the anti-OX40 antibody BMS 986178, and radiation therapy in patients with low-grade B-cell non-Hodgkin lymphomas.
If the trial is successful, Dr Levy believes the treatment could be useful for many tumor types.
“I don’t think there’s a limit to the type of tumor we could potentially treat,” he said, “as long as it has been infiltrated by the immune system.” ![]()
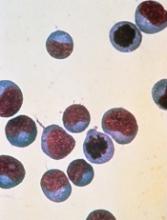
Combo could treat double-hit lymphoma
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.” ![]()
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.” ![]()
Existing drugs could be combined to treat double-hit lymphoma (DHL), according to preclinical research published in Science Translational Medicine.
The drugs are tigecycline, an antibiotic, and venetoclax, a BCL2 inhibitor.
Researchers observed promising activity with these drugs in combination, both in cell lines and mouse models of DHL.
The team therefore believes the drugs could be repurposed to treat DHL, which currently has a dismal prognosis.
Study author Micol Ravà, PhD, of the European Institute of Oncology in Milan, Italy, and her colleagues noted that DHL is driven by the abnormal activation of MYC and BCL2. However, selective BCL2 inhibitors like venetoclax have failed to halt disease progression in DHL patients.
Seeking a way to sensitize DHL to BCL2 inhibitors, the researchers turned to tigecycline, which interferes with mitochondria to trigger a MYC-dependent cell death pathway.
The team found that tigecycline and venetoclax demonstrated synergy in 5 DHL cell lines. The drugs were synergistic in 3 cell lines—Karpas-422, SU-DHL-6, and DOHH-2—in which neither drug alone showed significant pro-apoptotic activity.
In 2 other cell lines—SU-DHL-4 and OCI-LY8—venetoclax was active when given alone, but its activity was enhanced by the addition of tigecycline.
In mouse models of DHL (using the human cell lines SU-DHL-6, DOHH-2, and OCI-LY8), each of the drugs alone were able to slow tumor progression somewhat.
However, combination tigecycline and venetoclax exhibited “strong antitumoral activity,” according to the researchers. In fact, the combination caused full disease regression in all 8 SU-DHL-6 mice and 3 of 9 OCI-LY8 mice.
Dr Ravà and her colleagues also found the combination produced “rapid and marked tumor regression” in mice with a patient-derived xenograft.
The researchers observed no toxicity when tigecycline and venetoclax were given at low doses. However, mice receiving more aggressive treatment had some inflammation in the liver and spleen. And some mice treated with high doses of tigecycline and venetoclax died within 1 week of treatment initiation.
Finally, Dr Ravà and her colleagues found that tigecycline and venetoclax each synergized with rituximab. The team therefore concluded that tigecycline and venetoclax “have the potential to reinforce rituximab-containing therapies in the clinic.”
Interim trial results may be misleading
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice.
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice.
Interim results from randomized trials may be misleading at times, according to research published in JAMA.
Researchers compared interim and final publications on randomized trials and found that, 21% of the time, results changed significantly.
“Changes between interim and final publication matter because clinicians and the public could have been misled about whether an intervention was beneficial, harmful, or ineffective,” said study author Lisa Schwartz, MD, of Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire.
She and her colleagues searched PubMed for randomized trials from 2006 to 2015 with “interim,” “not mature,” or “immature” in the title or abstract.
To identify final publications, they searched PubMed, ClinicalTrials.gov, and Web of Science through 2016. The team emailed authors of interim reports when no final publication was identified.
For interim and final publications reporting the same efficacy and or safety outcome, the researchers compared trial characteristics and prominence. They also categorized abstract conclusions (not different, beneficial, or harmful) and compared changes between interim and final publications.
Findings
Interim results were reported in 613 of 1267 screened publications.
Of those publications, 72% reported on trials stopped early (for benefit, harm, futility, or other problems). The remaining 171 ongoing trials (mostly in oncology, surgery, or cardiology) reported interim efficacy or safety results.
Forty-one percent of the publications stated that the interim analysis was specified in the protocol, but half provided no reason for the interim publication.
Final results were published for 98 of the 160 trials (61%) that were more than 1 year beyond the completion date.
The researchers compared 73 interim and final publications reporting the same efficacy or safety outcome. And they found that interim and final publications had similar prominence.
In most cases (79%), the abstract conclusions did not change from the interim publication to the final publication. However, for 21% of trials, there were significant changes.
For 4 trials, the conclusions changed from “no difference” between randomized to treatments to the study treatment being “beneficial.” In 3 trials, the conclusions changed from “not different” to “harmful or possibly harmful.”
In 6 trials, the conclusions changed from “beneficial” to “not different.” One trial changed from “beneficial” to “harmful,” and another changed from “inconclusive” to “noninferior.”
Dr Schwartz and her colleagues concluded that while most interim and final publications reached similar conclusions, frequent non-publication of final results can lead to confusion or unfounded assumptions with true treatment effects remaining unknown.
To safeguard against any such confusion, the researchers recommended routinely adding the word “interim” in the title and justifying the reason in the publication. (Many interim publications reported analyses without any justification.)
“Most importantly, journals, authors, and funders should commit to making final results accessible by linking interim publications to final reports whenever available,” said study author Steven Woloshin, MD, of Dartmouth Institute for Health Policy and Clinical Practice.
CAR T-cell therapy produces durable CRs in ALL
Updated results from the phase 2 ELIANA study have shown that tisagenlecleucel can produce durable complete responses (CRs) in children and young adults with relapsed/refractory acute lymphoblastic leukemia (ALL).
Sixty percent of patients who received the chimeric antigen receptor (CAR) T-cell therapy achieved a CR, and 21% had a CR with incomplete hematologic recovery (CRi).
The median duration of CR/CRi was not reached at a median follow-up of 13.1 months.
The most common treatment-related adverse event (AE) was cytokine release syndrome (CRS), occurring in 77% of patients.
Researchers reported these results in NEJM. The study was sponsored by Novartis.
“This expanded, global study of CAR T-cell therapy gives us further evidence of how remarkable this treatment can be for our young patients in whom all other treatments failed,” said study author Shannon L. Maude, MD, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Our data show not only can we can achieve longer-term durable remissions and longer-term survival for our patients but that these personalized, cancer-fighting cells can remain in the body for months or even years, effectively doing their job.”
The trial included 75 patients who received tisagenlecleucel. At enrollment, the patients’ median age was 11 (range, 3 to 23).
Patients had received a median of 3 prior therapies (range, 1 to 8), and they had a median marrow blast percentage of 74% (range, 5 to 99).
All patients received a single infusion of tisagenlecleucel. Most (n=72) received lymphodepleting chemotherapy prior to the CAR T cells.
Results
The median duration of follow-up was 13.1 months.
The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CRi within 3 months. The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
The researchers said tisagenlecleucel persisted in the blood for as long as 20 months.
The relapse-free survival rate among patients with a CR/CRi was 80% at 6 months and 59% at 12 months.
Seventeen patients who had achieved a CR relapsed before receiving subsequent treatment. Three patients went on to subsequent therapy before relapse but ultimately relapsed.
Relapse was also reported in 2 patients who had been classified as non-responders because they did not maintain a response for at least 28 days.
Eight patients underwent allogeneic hematopoietic stem cell transplant while in remission, and all 8 were alive when the manuscript for this study was submitted. Four patients had not relapsed, and the other 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the overall survival rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. Grade 3/4 AEs occurred in 88% of patients. In 73% of patients, these AEs were thought to be related to treatment.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The median duration of CRS was 8 days (range, 1-36). Forty-seven patients were admitted to the intensive care unit to receive treatment for CRS, with a median stay of 7 days (range, 1-34).
“One of our more challenging questions—‘Can we manage the serious side effects of CAR T-cell therapy?’—was asked and answered in this global study,” said author Stephan A. Grupp, MD, PhD, of Children’s Hospital of Philadelphia.
“Some of our patients get very sick, but we showed that most toxic effects can be short-lived and reversible, with the potential for our patients to achieve durable complete remissions. That’s a pretty amazing turnaround for the high-risk child who, up until now, had little chance of surviving.”
Updated results from the phase 2 ELIANA study have shown that tisagenlecleucel can produce durable complete responses (CRs) in children and young adults with relapsed/refractory acute lymphoblastic leukemia (ALL).
Sixty percent of patients who received the chimeric antigen receptor (CAR) T-cell therapy achieved a CR, and 21% had a CR with incomplete hematologic recovery (CRi).
The median duration of CR/CRi was not reached at a median follow-up of 13.1 months.
The most common treatment-related adverse event (AE) was cytokine release syndrome (CRS), occurring in 77% of patients.
Researchers reported these results in NEJM. The study was sponsored by Novartis.
“This expanded, global study of CAR T-cell therapy gives us further evidence of how remarkable this treatment can be for our young patients in whom all other treatments failed,” said study author Shannon L. Maude, MD, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Our data show not only can we can achieve longer-term durable remissions and longer-term survival for our patients but that these personalized, cancer-fighting cells can remain in the body for months or even years, effectively doing their job.”
The trial included 75 patients who received tisagenlecleucel. At enrollment, the patients’ median age was 11 (range, 3 to 23).
Patients had received a median of 3 prior therapies (range, 1 to 8), and they had a median marrow blast percentage of 74% (range, 5 to 99).
All patients received a single infusion of tisagenlecleucel. Most (n=72) received lymphodepleting chemotherapy prior to the CAR T cells.
Results
The median duration of follow-up was 13.1 months.
The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CRi within 3 months. The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
The researchers said tisagenlecleucel persisted in the blood for as long as 20 months.
The relapse-free survival rate among patients with a CR/CRi was 80% at 6 months and 59% at 12 months.
Seventeen patients who had achieved a CR relapsed before receiving subsequent treatment. Three patients went on to subsequent therapy before relapse but ultimately relapsed.
Relapse was also reported in 2 patients who had been classified as non-responders because they did not maintain a response for at least 28 days.
Eight patients underwent allogeneic hematopoietic stem cell transplant while in remission, and all 8 were alive when the manuscript for this study was submitted. Four patients had not relapsed, and the other 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the overall survival rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. Grade 3/4 AEs occurred in 88% of patients. In 73% of patients, these AEs were thought to be related to treatment.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The median duration of CRS was 8 days (range, 1-36). Forty-seven patients were admitted to the intensive care unit to receive treatment for CRS, with a median stay of 7 days (range, 1-34).
“One of our more challenging questions—‘Can we manage the serious side effects of CAR T-cell therapy?’—was asked and answered in this global study,” said author Stephan A. Grupp, MD, PhD, of Children’s Hospital of Philadelphia.
“Some of our patients get very sick, but we showed that most toxic effects can be short-lived and reversible, with the potential for our patients to achieve durable complete remissions. That’s a pretty amazing turnaround for the high-risk child who, up until now, had little chance of surviving.”
Updated results from the phase 2 ELIANA study have shown that tisagenlecleucel can produce durable complete responses (CRs) in children and young adults with relapsed/refractory acute lymphoblastic leukemia (ALL).
Sixty percent of patients who received the chimeric antigen receptor (CAR) T-cell therapy achieved a CR, and 21% had a CR with incomplete hematologic recovery (CRi).
The median duration of CR/CRi was not reached at a median follow-up of 13.1 months.
The most common treatment-related adverse event (AE) was cytokine release syndrome (CRS), occurring in 77% of patients.
Researchers reported these results in NEJM. The study was sponsored by Novartis.
“This expanded, global study of CAR T-cell therapy gives us further evidence of how remarkable this treatment can be for our young patients in whom all other treatments failed,” said study author Shannon L. Maude, MD, PhD, of Children’s Hospital of Philadelphia in Pennsylvania.
“Our data show not only can we can achieve longer-term durable remissions and longer-term survival for our patients but that these personalized, cancer-fighting cells can remain in the body for months or even years, effectively doing their job.”
The trial included 75 patients who received tisagenlecleucel. At enrollment, the patients’ median age was 11 (range, 3 to 23).
Patients had received a median of 3 prior therapies (range, 1 to 8), and they had a median marrow blast percentage of 74% (range, 5 to 99).
All patients received a single infusion of tisagenlecleucel. Most (n=72) received lymphodepleting chemotherapy prior to the CAR T cells.
Results
The median duration of follow-up was 13.1 months.
The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CRi within 3 months. The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
The researchers said tisagenlecleucel persisted in the blood for as long as 20 months.
The relapse-free survival rate among patients with a CR/CRi was 80% at 6 months and 59% at 12 months.
Seventeen patients who had achieved a CR relapsed before receiving subsequent treatment. Three patients went on to subsequent therapy before relapse but ultimately relapsed.
Relapse was also reported in 2 patients who had been classified as non-responders because they did not maintain a response for at least 28 days.
Eight patients underwent allogeneic hematopoietic stem cell transplant while in remission, and all 8 were alive when the manuscript for this study was submitted. Four patients had not relapsed, and the other 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the overall survival rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. Grade 3/4 AEs occurred in 88% of patients. In 73% of patients, these AEs were thought to be related to treatment.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The median duration of CRS was 8 days (range, 1-36). Forty-seven patients were admitted to the intensive care unit to receive treatment for CRS, with a median stay of 7 days (range, 1-34).
“One of our more challenging questions—‘Can we manage the serious side effects of CAR T-cell therapy?’—was asked and answered in this global study,” said author Stephan A. Grupp, MD, PhD, of Children’s Hospital of Philadelphia.
“Some of our patients get very sick, but we showed that most toxic effects can be short-lived and reversible, with the potential for our patients to achieve durable complete remissions. That’s a pretty amazing turnaround for the high-risk child who, up until now, had little chance of surviving.”
FDA places T-cell therapy on clinical hold
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501.
* Data in the abstract were updated in the oral presentation and reported on the company’s website.
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501.
* Data in the abstract were updated in the oral presentation and reported on the company’s website.
The US Food and Drug Administration (FDA) has placed BPX-501, a T-cell therapy being evaluated in patients who undergo haploidentical hematopoietic stem cell transplants (HSCTs), on clinical hold.
Three cases of encephalopathy possibly related to BPX-501 prompted the agency to impose the hold.
Bellicum Pharmaceuticals is the developer of BPX-501, and the company was conducting 4 trials in the US in children and adults with hematologic disorders.
The BPX-501 registration trial in Europe is not affected by the clinical hold.
BPX-501 is designed to fight infection, support engraftment, prevent disease relapse, and potentially stop graft-versus-host disease (GVHD) should it occur.
BPX-501 contains a safety switch, CaspaCIDe®, that can be activated with the administration of rimiducid to kill the toxic T cells in the event of GVHD.
The 3 cases of encephalopathy are complex, according to a company press release, and have confounding factors. These include prior failed transplants, prior history of immunodeficiency, concurrent infection, and administration of rimiducid in combination with other medications.
Encephalopathy had not emerged as an adverse event in 240 patients treated with the cell therapy, until now.
BPX-501 had produced encouraging results, according to trial data presented at EHA 2017 and ASH 2017 (abstract 211*).
In this trial, 112 pediatric patients were transfused with BPX-501 cells about 2 weeks after transplant. Patients had acute leukemia (n=53), primary immune deficiencies (n=26), erythroid disorders (n=17), Fanconi anemia (n=7), and other diseases (n=9).
Investigators reported that infused cells expanded and persisted, with peak expansion reached at 9 months after infusion. Investigators continued to detect BPX-501 cells after 2 years.
The European Commission granted BPX-501 orphan drug designation for the agent for treatment in HSCT, and for the activator agent rimiducid for the treatment of GVHD.
And the FDA had granted the agents orphan drug status as a combination replacement T-cell therapy for the treatment of immunodeficiency and GVHD after HSCT.
Bellicum says it is working with the FDA to evaluate the risk of encephalopathy in patients receiving BPX-501.
* Data in the abstract were updated in the oral presentation and reported on the company’s website.