User login
Young kids with SCA not receiving recommended prophylaxis
Many young children with sickle cell anemia (SCA) may not be taking the recommended antibiotics to prevent invasive pneumococcal disease (IPD), according to research published in Pediatrics.
Results of a previous study indicated that daily treatment with penicillin could reduce the risk of IPD by 84% in young children with SCA.
In the current study, only 18% of young SCA patients received daily penicillin or an equivalent antibiotic as IPD prophylaxis.
“Most children with sickle cell anemia are not getting the antibiotics they should be to adequately protect against potentially deadly infections,” said study author Sarah Reeves, PhD, of the University of Michigan Medical School in Ann Arbor.
“Long-standing recommendations say children with sickle cell anemia should take antibiotics daily for their first 5 years of life. It can be life-saving.”
For this study, Dr Reeves and her colleagues analyzed data on 2821 SCA patients, ages 3 months to 5 years, living in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The patients were continuously enrolled in the Medicaid program for at least 1 calendar year between 2005 and 2012. The researchers evaluated the receipt of antibiotics through the insurance claims for filled prescriptions.
The team found that, overall, 18% of patients received at least 300 days of antibiotics.
Sixteen percent of patients received at least 300 days of penicillin; 16% received at least 300 days of penicillin or erythromycin; 18% received at least 300 days of penicillin, erythromycin, or amoxicillin; and 22% received at least 300 days of any antibiotic to prevent Streptococcus pneumoniae.
On average, patients received 162 days of penicillin; 164 days of penicillin or erythromycin; 178 days of penicillin, erythromycin, or amoxicillin; and 193 days of any antibiotic to prevent S pneumoniae.
Multivariable analysis suggested that medical visits and a patient’s state of residence were associated with receiving at least 300 days of antibiotics.
The researchers said that each additional SCA-related outpatient visit and well-child visit was associated with incrementally increased odds of receiving at least 300 days of antibiotics. The odds ratio (OR) was 1.01 for SCA-related outpatient visits and 1.08 for well-child visits (P<0.05 for both).
Patients in Florida (OR=0.51, P<0.05), Louisiana (OR=0.57, P<0.05), Michigan (OR=0.60, P<0.05), and South Carolina (OR=0.62, P<0.05) had lower odds of receiving at least 300 days of antibiotics than patients in Illinois (OR=1.00) or Texas (OR=1.01).
The researchers did not investigate why children were not receiving recommended antibiotics, but Dr Reeves identified possible barriers to compliance. She noted that caregiver challenges include picking up prescriptions every 2 weeks from a pharmacy as well as remembering to administer an antibiotic to a young, healthy-appearing child twice a day.
“The types of challenges involved in making sure children get the recommended dose of antibiotics is exacerbated by the substantial burden of care already experienced by families to help control the symptoms of this disease,” Dr Reeves said.
She added that future studies should more deeply explore barriers preventing families from getting antibiotics and potential interventions to improve the rate of children receiving recommended prescriptions.
“Interventions to improve the receipt of antibiotics among children with sickle cell anemia should include enhanced collaboration between healthcare providers, pharmacists, and families,” Dr Reeves said.
“Doctors need to repeatedly discuss the importance of taking antibiotics with families of children with sickle cell anemia. Social factors that may impact receiving filled prescriptions should also be considered, such as the availability of transportation and time to travel to pharmacies to pick up the prescriptions.” ![]()
Many young children with sickle cell anemia (SCA) may not be taking the recommended antibiotics to prevent invasive pneumococcal disease (IPD), according to research published in Pediatrics.
Results of a previous study indicated that daily treatment with penicillin could reduce the risk of IPD by 84% in young children with SCA.
In the current study, only 18% of young SCA patients received daily penicillin or an equivalent antibiotic as IPD prophylaxis.
“Most children with sickle cell anemia are not getting the antibiotics they should be to adequately protect against potentially deadly infections,” said study author Sarah Reeves, PhD, of the University of Michigan Medical School in Ann Arbor.
“Long-standing recommendations say children with sickle cell anemia should take antibiotics daily for their first 5 years of life. It can be life-saving.”
For this study, Dr Reeves and her colleagues analyzed data on 2821 SCA patients, ages 3 months to 5 years, living in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The patients were continuously enrolled in the Medicaid program for at least 1 calendar year between 2005 and 2012. The researchers evaluated the receipt of antibiotics through the insurance claims for filled prescriptions.
The team found that, overall, 18% of patients received at least 300 days of antibiotics.
Sixteen percent of patients received at least 300 days of penicillin; 16% received at least 300 days of penicillin or erythromycin; 18% received at least 300 days of penicillin, erythromycin, or amoxicillin; and 22% received at least 300 days of any antibiotic to prevent Streptococcus pneumoniae.
On average, patients received 162 days of penicillin; 164 days of penicillin or erythromycin; 178 days of penicillin, erythromycin, or amoxicillin; and 193 days of any antibiotic to prevent S pneumoniae.
Multivariable analysis suggested that medical visits and a patient’s state of residence were associated with receiving at least 300 days of antibiotics.
The researchers said that each additional SCA-related outpatient visit and well-child visit was associated with incrementally increased odds of receiving at least 300 days of antibiotics. The odds ratio (OR) was 1.01 for SCA-related outpatient visits and 1.08 for well-child visits (P<0.05 for both).
Patients in Florida (OR=0.51, P<0.05), Louisiana (OR=0.57, P<0.05), Michigan (OR=0.60, P<0.05), and South Carolina (OR=0.62, P<0.05) had lower odds of receiving at least 300 days of antibiotics than patients in Illinois (OR=1.00) or Texas (OR=1.01).
The researchers did not investigate why children were not receiving recommended antibiotics, but Dr Reeves identified possible barriers to compliance. She noted that caregiver challenges include picking up prescriptions every 2 weeks from a pharmacy as well as remembering to administer an antibiotic to a young, healthy-appearing child twice a day.
“The types of challenges involved in making sure children get the recommended dose of antibiotics is exacerbated by the substantial burden of care already experienced by families to help control the symptoms of this disease,” Dr Reeves said.
She added that future studies should more deeply explore barriers preventing families from getting antibiotics and potential interventions to improve the rate of children receiving recommended prescriptions.
“Interventions to improve the receipt of antibiotics among children with sickle cell anemia should include enhanced collaboration between healthcare providers, pharmacists, and families,” Dr Reeves said.
“Doctors need to repeatedly discuss the importance of taking antibiotics with families of children with sickle cell anemia. Social factors that may impact receiving filled prescriptions should also be considered, such as the availability of transportation and time to travel to pharmacies to pick up the prescriptions.” ![]()
Many young children with sickle cell anemia (SCA) may not be taking the recommended antibiotics to prevent invasive pneumococcal disease (IPD), according to research published in Pediatrics.
Results of a previous study indicated that daily treatment with penicillin could reduce the risk of IPD by 84% in young children with SCA.
In the current study, only 18% of young SCA patients received daily penicillin or an equivalent antibiotic as IPD prophylaxis.
“Most children with sickle cell anemia are not getting the antibiotics they should be to adequately protect against potentially deadly infections,” said study author Sarah Reeves, PhD, of the University of Michigan Medical School in Ann Arbor.
“Long-standing recommendations say children with sickle cell anemia should take antibiotics daily for their first 5 years of life. It can be life-saving.”
For this study, Dr Reeves and her colleagues analyzed data on 2821 SCA patients, ages 3 months to 5 years, living in Florida, Illinois, Louisiana, Michigan, South Carolina, and Texas.
The patients were continuously enrolled in the Medicaid program for at least 1 calendar year between 2005 and 2012. The researchers evaluated the receipt of antibiotics through the insurance claims for filled prescriptions.
The team found that, overall, 18% of patients received at least 300 days of antibiotics.
Sixteen percent of patients received at least 300 days of penicillin; 16% received at least 300 days of penicillin or erythromycin; 18% received at least 300 days of penicillin, erythromycin, or amoxicillin; and 22% received at least 300 days of any antibiotic to prevent Streptococcus pneumoniae.
On average, patients received 162 days of penicillin; 164 days of penicillin or erythromycin; 178 days of penicillin, erythromycin, or amoxicillin; and 193 days of any antibiotic to prevent S pneumoniae.
Multivariable analysis suggested that medical visits and a patient’s state of residence were associated with receiving at least 300 days of antibiotics.
The researchers said that each additional SCA-related outpatient visit and well-child visit was associated with incrementally increased odds of receiving at least 300 days of antibiotics. The odds ratio (OR) was 1.01 for SCA-related outpatient visits and 1.08 for well-child visits (P<0.05 for both).
Patients in Florida (OR=0.51, P<0.05), Louisiana (OR=0.57, P<0.05), Michigan (OR=0.60, P<0.05), and South Carolina (OR=0.62, P<0.05) had lower odds of receiving at least 300 days of antibiotics than patients in Illinois (OR=1.00) or Texas (OR=1.01).
The researchers did not investigate why children were not receiving recommended antibiotics, but Dr Reeves identified possible barriers to compliance. She noted that caregiver challenges include picking up prescriptions every 2 weeks from a pharmacy as well as remembering to administer an antibiotic to a young, healthy-appearing child twice a day.
“The types of challenges involved in making sure children get the recommended dose of antibiotics is exacerbated by the substantial burden of care already experienced by families to help control the symptoms of this disease,” Dr Reeves said.
She added that future studies should more deeply explore barriers preventing families from getting antibiotics and potential interventions to improve the rate of children receiving recommended prescriptions.
“Interventions to improve the receipt of antibiotics among children with sickle cell anemia should include enhanced collaboration between healthcare providers, pharmacists, and families,” Dr Reeves said.
“Doctors need to repeatedly discuss the importance of taking antibiotics with families of children with sickle cell anemia. Social factors that may impact receiving filled prescriptions should also be considered, such as the availability of transportation and time to travel to pharmacies to pick up the prescriptions.” ![]()
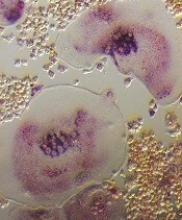
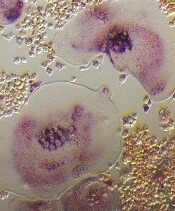
JAK2 inhibition could reduce risk of GVHD
Preclinical research suggests that targeting JAK2 can reduce the risk of graft-versus-host disease (GVHD) in transplant recipients.
Researchers found that genetic ablation of JAK2 on donor T cells or inhibition of JAK2 via treatment with pacritinib reduced GVHD in mice without compromising graft-versus-leukemia (GVL) activity.
“An effort to identify selective immune suppression whereby GVHD is reduced and the antitumor activity of the graft is preserved is key to improving the success of blood and marrow transplantation,” said Brian C. Betts, MD, of Moffitt Cancer Center in Tampa, Florida.
Dr Betts and his colleagues conducted this research and recounted their findings in PNAS.
In experiments with mice, the researchers found that donor T cells with JAK2 deletion were less likely than wild-type donor T cells to induce GVHD. However, JAK2 deletion did not impair the GVL effect.
Mice that received JAK2−/− T cells had longer survival, higher body weights, and less GVHD than control mice.
The researchers said targeting JAK2 may reduce GVHD, in part, by limiting Th1 differentiation and the migratory capacity of alloreactive T cells. However, targeting JAK2 promotes beneficial regulatory-T-cell and Th2 differentiation as well.
The researchers also tested the effects of JAK2 inhibition with pacritinib. Mice received allografts and were treated with pacritinib or vehicle control for 3 weeks.
As before, JAK2 inhibition reduced acute GVHD mortality while preserving the GVL effect.
The team also discovered that pacritinib could protect mice from tissue graft rejection, suggesting the drug could be used to prevent kidney or liver transplant rejection.
Now, the researchers are working on a phase 1/2 trial designed to determine if pacritinib and standard immune suppression can prevent acute GVHD after hematopoietic stem cell transplant (NCT02891603). ![]()
Preclinical research suggests that targeting JAK2 can reduce the risk of graft-versus-host disease (GVHD) in transplant recipients.
Researchers found that genetic ablation of JAK2 on donor T cells or inhibition of JAK2 via treatment with pacritinib reduced GVHD in mice without compromising graft-versus-leukemia (GVL) activity.
“An effort to identify selective immune suppression whereby GVHD is reduced and the antitumor activity of the graft is preserved is key to improving the success of blood and marrow transplantation,” said Brian C. Betts, MD, of Moffitt Cancer Center in Tampa, Florida.
Dr Betts and his colleagues conducted this research and recounted their findings in PNAS.
In experiments with mice, the researchers found that donor T cells with JAK2 deletion were less likely than wild-type donor T cells to induce GVHD. However, JAK2 deletion did not impair the GVL effect.
Mice that received JAK2−/− T cells had longer survival, higher body weights, and less GVHD than control mice.
The researchers said targeting JAK2 may reduce GVHD, in part, by limiting Th1 differentiation and the migratory capacity of alloreactive T cells. However, targeting JAK2 promotes beneficial regulatory-T-cell and Th2 differentiation as well.
The researchers also tested the effects of JAK2 inhibition with pacritinib. Mice received allografts and were treated with pacritinib or vehicle control for 3 weeks.
As before, JAK2 inhibition reduced acute GVHD mortality while preserving the GVL effect.
The team also discovered that pacritinib could protect mice from tissue graft rejection, suggesting the drug could be used to prevent kidney or liver transplant rejection.
Now, the researchers are working on a phase 1/2 trial designed to determine if pacritinib and standard immune suppression can prevent acute GVHD after hematopoietic stem cell transplant (NCT02891603). ![]()
Preclinical research suggests that targeting JAK2 can reduce the risk of graft-versus-host disease (GVHD) in transplant recipients.
Researchers found that genetic ablation of JAK2 on donor T cells or inhibition of JAK2 via treatment with pacritinib reduced GVHD in mice without compromising graft-versus-leukemia (GVL) activity.
“An effort to identify selective immune suppression whereby GVHD is reduced and the antitumor activity of the graft is preserved is key to improving the success of blood and marrow transplantation,” said Brian C. Betts, MD, of Moffitt Cancer Center in Tampa, Florida.
Dr Betts and his colleagues conducted this research and recounted their findings in PNAS.
In experiments with mice, the researchers found that donor T cells with JAK2 deletion were less likely than wild-type donor T cells to induce GVHD. However, JAK2 deletion did not impair the GVL effect.
Mice that received JAK2−/− T cells had longer survival, higher body weights, and less GVHD than control mice.
The researchers said targeting JAK2 may reduce GVHD, in part, by limiting Th1 differentiation and the migratory capacity of alloreactive T cells. However, targeting JAK2 promotes beneficial regulatory-T-cell and Th2 differentiation as well.
The researchers also tested the effects of JAK2 inhibition with pacritinib. Mice received allografts and were treated with pacritinib or vehicle control for 3 weeks.
As before, JAK2 inhibition reduced acute GVHD mortality while preserving the GVL effect.
The team also discovered that pacritinib could protect mice from tissue graft rejection, suggesting the drug could be used to prevent kidney or liver transplant rejection.
Now, the researchers are working on a phase 1/2 trial designed to determine if pacritinib and standard immune suppression can prevent acute GVHD after hematopoietic stem cell transplant (NCT02891603). ![]()
Child’s cancer diagnosis can affect mother’s income long-term
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
A study conducted in Sweden revealed that social benefits can ease financial burdens for parents of children recently diagnosed with cancer.
However, the study also showed that mothers experienced persistently lower income after benefits diminished.
Ayako Hiyoshi, PhD, of Örebro University in Örebro, Sweden, and her colleagues detailed these findings in Cancer.
The researchers gathered information from Swedish national registers and examined the trajectories of parents’ income from different sources.
Parents of children with cancer diagnosed between 2004 and 2009 were identified and matched with parents of children without cancer (reference parents).
In total, 20,091 families were followed from the year before cancer diagnosis to a maximum of 8 years.
The researchers noted that, around the time of a child’s cancer diagnosis, total income (from all sources) was, on average, higher in mothers of children with cancer than in reference mothers.
The ratio of mean total income for mothers of children with cancer, compared to reference mothers, was 1.032 at 1 year prior to the child’s diagnosis and 1.064 the year of diagnosis.
For fathers of children with cancer, total income was slightly lower than reference fathers’ income. The ratios were 0.987 at 1 year prior to diagnosis and 0.995 the year of diagnosis.
The researchers also noted that parents’ income from work was at its lowest around the time of a child’s cancer diagnosis but increased with time.
At cancer diagnosis, the ratio of mean income from work was 0.642 for mothers and 0.858 for fathers. One year later, the ratios were 0.786 and 0.956, respectively. At 3 years, the ratios were 0.876 and 0.986, respectively. At 6 years, the ratios were 0.856 and 1.058, respectively.
The researchers pointed out that sickness and childcare-related benefits, which compensated for income loss, were greater for parents of children with cancer than for reference parents. However, social benefits diminished over time.
One year prior to cancer diagnosis, the ratio of sickness benefits was 3.495 for mothers and 5.213 for fathers. The year of diagnosis, the ratios were 4.785 and 5.795, respectively. At 3 years, the ratios were 1.404 and 1.339, respectively. And at 6 years, the ratios were 0.931 and 1.421, respectively.
One year prior to cancer diagnosis, the ratio of childcare-related benefits was 2.830 for mothers and 3.514 for fathers. The year of diagnosis, the ratios were 4.553 and 4.930, respectively. At 3 years, the ratios were 2.225 and 1.948, respectively. And at 6 years, the ratios were 1.272 and 1.095, respectively.
The decline of social benefits over time meant that cancer mothers’ total income became lower than that of reference mothers, and this difference persisted over the period studied. This was not the case for cancer fathers, however.
The ratio of income from all sources for cancer mothers compared to reference mothers was 1.064 the year of diagnosis, 0.985 at 2 years, 0.966 at 4 years, and 0.934 at 6 years.
The ratio of income from all sources for cancer fathers compared to reference fathers was 0.995 the year of diagnosis, 0.993 at 2 years, 0.998 at 4 years, and 1.029 at 6 years.
“A significant and unexpected finding was that, although income from employment stayed lower for several years for mothers, total income was higher for mothers of children with cancer around the time of the child’s cancer diagnosis when the compensation from social benefits were included,” Dr Hiyoshi said.
“The persistently lower income from employment for mothers of children with cancer compared with mothers of cancer-free children implies potential long-term consequences for the mothers of children with cancer, including their career and future pension in old age.” ![]()
Product increases FIX levels in hemophilia B
MADRID—The recombinant factor IX (FIX) product CB 2679d/ISU304 can increase FIX levels in patients with severe hemophilia B, according to a phase 1/2 trial.
Results showed a continuous linear increase in FIX activity levels following daily subcutaneous (SQ) dosing of CB 2679d for 6 days.
Adverse events were mild to moderate, and none of the patients have developed inhibitors to CB 2679d or FIX.
Howard Levy, MB ChB, PhD, chief medical officer of Catalyst Biosciences, Inc., presented these results at the 11th Annual Congress of The European Association for Haemophilia and Allied Disorders (EAHAD).
The research was sponsored by Catalyst Biosciences, Inc.
This phase 1/2 trial was divided into 5 cohorts.
In cohort 1, researchers compared single doses of intravenous (IV) CB 2679d and IV BeneFIX (recombinant FIX). CB 2679d proved 22 times more potent than BeneFIX. The products’ half-lives were 27.0 hours and 21.0 hours, respectively.
In cohorts 2 and 3, researchers compared single, ascending doses of IV CB 2679d to SQ CB 2679d. The bioavailability of SQ CB 2679d was 18.5%, and the half-life was 98.7 hours.
Cohort 4 was dropped, as it was another comparison of IV and SQ CB 2679d, which was considered unnecessary.
Cohort 5 included 5 patients who received daily doses of SQ CB 2679d. For 6 days, patients received CB 2679d at a dose of 140 IU/kg SQ.
The patients’ FIX activity levels increased from a median of <1% at baseline to a median of 15.7% (interquartile range, 14.9% to 16.6%) after all 6 doses.
The increase in FIX activity levels after the daily dosing was linear, indicating that continued SQ dosing may increase FIX activity further.
The median half-life was 63.2 hours (interquartile range, 60.2 to 64 hours), with the result that activity levels were still at 4% to 6.4% five days after the last dose.
No inhibitors to CB 2679d or FIX were observed in any of the cohorts in this trial.
In cohort 5, adverse events included pain, erythema, redness, and bruising after injections. Bruising occurred only with initial injections, and the severity of pain, erythema, and redness decreased over time (from moderate to mild).
“Existing IV therapies have FIX trough levels that can drop as low as 1% to 3% before repeat dosing,” Dr Levey said. “Daily subcutaneous dosing of CB 2679d has the potential to minimize the variability in FIX activity levels observed between IV doses and maintain individuals in the mild or even normal hemophilia range. This study demonstrates that, even after just 6 days of treatment, CB 2679d compares favorably to currently approved therapies for hemophilia B, all of which are infused IV.” ![]()
MADRID—The recombinant factor IX (FIX) product CB 2679d/ISU304 can increase FIX levels in patients with severe hemophilia B, according to a phase 1/2 trial.
Results showed a continuous linear increase in FIX activity levels following daily subcutaneous (SQ) dosing of CB 2679d for 6 days.
Adverse events were mild to moderate, and none of the patients have developed inhibitors to CB 2679d or FIX.
Howard Levy, MB ChB, PhD, chief medical officer of Catalyst Biosciences, Inc., presented these results at the 11th Annual Congress of The European Association for Haemophilia and Allied Disorders (EAHAD).
The research was sponsored by Catalyst Biosciences, Inc.
This phase 1/2 trial was divided into 5 cohorts.
In cohort 1, researchers compared single doses of intravenous (IV) CB 2679d and IV BeneFIX (recombinant FIX). CB 2679d proved 22 times more potent than BeneFIX. The products’ half-lives were 27.0 hours and 21.0 hours, respectively.
In cohorts 2 and 3, researchers compared single, ascending doses of IV CB 2679d to SQ CB 2679d. The bioavailability of SQ CB 2679d was 18.5%, and the half-life was 98.7 hours.
Cohort 4 was dropped, as it was another comparison of IV and SQ CB 2679d, which was considered unnecessary.
Cohort 5 included 5 patients who received daily doses of SQ CB 2679d. For 6 days, patients received CB 2679d at a dose of 140 IU/kg SQ.
The patients’ FIX activity levels increased from a median of <1% at baseline to a median of 15.7% (interquartile range, 14.9% to 16.6%) after all 6 doses.
The increase in FIX activity levels after the daily dosing was linear, indicating that continued SQ dosing may increase FIX activity further.
The median half-life was 63.2 hours (interquartile range, 60.2 to 64 hours), with the result that activity levels were still at 4% to 6.4% five days after the last dose.
No inhibitors to CB 2679d or FIX were observed in any of the cohorts in this trial.
In cohort 5, adverse events included pain, erythema, redness, and bruising after injections. Bruising occurred only with initial injections, and the severity of pain, erythema, and redness decreased over time (from moderate to mild).
“Existing IV therapies have FIX trough levels that can drop as low as 1% to 3% before repeat dosing,” Dr Levey said. “Daily subcutaneous dosing of CB 2679d has the potential to minimize the variability in FIX activity levels observed between IV doses and maintain individuals in the mild or even normal hemophilia range. This study demonstrates that, even after just 6 days of treatment, CB 2679d compares favorably to currently approved therapies for hemophilia B, all of which are infused IV.” ![]()
MADRID—The recombinant factor IX (FIX) product CB 2679d/ISU304 can increase FIX levels in patients with severe hemophilia B, according to a phase 1/2 trial.
Results showed a continuous linear increase in FIX activity levels following daily subcutaneous (SQ) dosing of CB 2679d for 6 days.
Adverse events were mild to moderate, and none of the patients have developed inhibitors to CB 2679d or FIX.
Howard Levy, MB ChB, PhD, chief medical officer of Catalyst Biosciences, Inc., presented these results at the 11th Annual Congress of The European Association for Haemophilia and Allied Disorders (EAHAD).
The research was sponsored by Catalyst Biosciences, Inc.
This phase 1/2 trial was divided into 5 cohorts.
In cohort 1, researchers compared single doses of intravenous (IV) CB 2679d and IV BeneFIX (recombinant FIX). CB 2679d proved 22 times more potent than BeneFIX. The products’ half-lives were 27.0 hours and 21.0 hours, respectively.
In cohorts 2 and 3, researchers compared single, ascending doses of IV CB 2679d to SQ CB 2679d. The bioavailability of SQ CB 2679d was 18.5%, and the half-life was 98.7 hours.
Cohort 4 was dropped, as it was another comparison of IV and SQ CB 2679d, which was considered unnecessary.
Cohort 5 included 5 patients who received daily doses of SQ CB 2679d. For 6 days, patients received CB 2679d at a dose of 140 IU/kg SQ.
The patients’ FIX activity levels increased from a median of <1% at baseline to a median of 15.7% (interquartile range, 14.9% to 16.6%) after all 6 doses.
The increase in FIX activity levels after the daily dosing was linear, indicating that continued SQ dosing may increase FIX activity further.
The median half-life was 63.2 hours (interquartile range, 60.2 to 64 hours), with the result that activity levels were still at 4% to 6.4% five days after the last dose.
No inhibitors to CB 2679d or FIX were observed in any of the cohorts in this trial.
In cohort 5, adverse events included pain, erythema, redness, and bruising after injections. Bruising occurred only with initial injections, and the severity of pain, erythema, and redness decreased over time (from moderate to mild).
“Existing IV therapies have FIX trough levels that can drop as low as 1% to 3% before repeat dosing,” Dr Levey said. “Daily subcutaneous dosing of CB 2679d has the potential to minimize the variability in FIX activity levels observed between IV doses and maintain individuals in the mild or even normal hemophilia range. This study demonstrates that, even after just 6 days of treatment, CB 2679d compares favorably to currently approved therapies for hemophilia B, all of which are infused IV.” ![]()
Agent can decrease GI toxicity in MM patients
Results of a case-control study suggest a cytoprotective agent can reduce treatment-related gastrointestinal (GI) toxicity in patients with multiple myeloma (MM).
Use of this agent, amifostine, was associated with significantly lower rates of grade 2 or higher oral mucositis, nausea, vomiting, and diarrhea.
Additionally, amifostine did not appear to compromise the anti-myeloma activity of treatment, which consisted of high-dose melphalan (HDM) and autologous hematopoietic stem cell transplant (auto-HSCT).
Ehsan Malek, MD, of Case Western Reserve University in Cleveland, Ohio, and his colleagues reported these findings in Leukemia & Lymphoma.
The researchers compared HDM plus auto-HSCT, with or without pre-treatment amifostine, in previously treated MM patients.
There were 107 patients who received amifostine and 114 who did not. The 107 patients received amifostine at 740 mg/m2, given as a bolus infusion at 24 hours and 15 minutes before HDM.
Baseline characteristics were largely similar in the amifostine and control groups. However, more patients in the amifostine group received a tandem HSCT (17 vs 0), and more patients in the control group had an ECOG performance status of 0 (64.3% vs 43%).
Patients in the amifostine group had a longer median time from diagnosis to first HSCT—10 months (range, 4-39) vs 7 months (range, 1-95).
A majority of patients in both groups were in partial response or better at baseline. However, more patients in the control group had stable disease (6.2% vs 1%) or progressive disease (8% vs 0%).
Results
For all-grade GI toxicities, there was largely no significant difference between the amifostine and control groups. However, patients in the amifostine group had significantly lower rates of grade 2 or higher GI toxicities.
Rates of all-grade GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—53.3% vs 64.0%, P=0.104
- Nausea—90.7% vs 95.6%, P=0.143
- Vomiting—65.4% vs 75.4%, P=0.102
- Diarrhea—93.5% vs 84.2%,P=0.030.
Rates of grade 2 or higher GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—27.1% vs 47.4%, P=0.002
- Nausea—31.8% vs 86.0%, P<0.0001
- Vomiting—18.7% vs 52.6%, P<0.0001
- Diarrhea—56.1% vs 73.7%, P=0.006.
The researchers said amifostine was well tolerated and produced no significant adverse effects.
They also said amifostine had “no discernable effect” on engraftment, progression-free survival, or overall survival.
The median time to neutrophil engraftment was 11 days (range, 9-16) in the control group and 10 days (range, 6-21) in the amifostine group (P=0.011). The median time to platelet engraftment was 18 days (range, 0-26) and 19 days (range, 8-71), respectively (P<0.21).
The median progression-free survival was 40 months in the amifostine group and 32 months in the control group (P=0.012). The median overall survival was 70 months and 67 months, respectively (P=0.84). ![]()
Results of a case-control study suggest a cytoprotective agent can reduce treatment-related gastrointestinal (GI) toxicity in patients with multiple myeloma (MM).
Use of this agent, amifostine, was associated with significantly lower rates of grade 2 or higher oral mucositis, nausea, vomiting, and diarrhea.
Additionally, amifostine did not appear to compromise the anti-myeloma activity of treatment, which consisted of high-dose melphalan (HDM) and autologous hematopoietic stem cell transplant (auto-HSCT).
Ehsan Malek, MD, of Case Western Reserve University in Cleveland, Ohio, and his colleagues reported these findings in Leukemia & Lymphoma.
The researchers compared HDM plus auto-HSCT, with or without pre-treatment amifostine, in previously treated MM patients.
There were 107 patients who received amifostine and 114 who did not. The 107 patients received amifostine at 740 mg/m2, given as a bolus infusion at 24 hours and 15 minutes before HDM.
Baseline characteristics were largely similar in the amifostine and control groups. However, more patients in the amifostine group received a tandem HSCT (17 vs 0), and more patients in the control group had an ECOG performance status of 0 (64.3% vs 43%).
Patients in the amifostine group had a longer median time from diagnosis to first HSCT—10 months (range, 4-39) vs 7 months (range, 1-95).
A majority of patients in both groups were in partial response or better at baseline. However, more patients in the control group had stable disease (6.2% vs 1%) or progressive disease (8% vs 0%).
Results
For all-grade GI toxicities, there was largely no significant difference between the amifostine and control groups. However, patients in the amifostine group had significantly lower rates of grade 2 or higher GI toxicities.
Rates of all-grade GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—53.3% vs 64.0%, P=0.104
- Nausea—90.7% vs 95.6%, P=0.143
- Vomiting—65.4% vs 75.4%, P=0.102
- Diarrhea—93.5% vs 84.2%,P=0.030.
Rates of grade 2 or higher GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—27.1% vs 47.4%, P=0.002
- Nausea—31.8% vs 86.0%, P<0.0001
- Vomiting—18.7% vs 52.6%, P<0.0001
- Diarrhea—56.1% vs 73.7%, P=0.006.
The researchers said amifostine was well tolerated and produced no significant adverse effects.
They also said amifostine had “no discernable effect” on engraftment, progression-free survival, or overall survival.
The median time to neutrophil engraftment was 11 days (range, 9-16) in the control group and 10 days (range, 6-21) in the amifostine group (P=0.011). The median time to platelet engraftment was 18 days (range, 0-26) and 19 days (range, 8-71), respectively (P<0.21).
The median progression-free survival was 40 months in the amifostine group and 32 months in the control group (P=0.012). The median overall survival was 70 months and 67 months, respectively (P=0.84). ![]()
Results of a case-control study suggest a cytoprotective agent can reduce treatment-related gastrointestinal (GI) toxicity in patients with multiple myeloma (MM).
Use of this agent, amifostine, was associated with significantly lower rates of grade 2 or higher oral mucositis, nausea, vomiting, and diarrhea.
Additionally, amifostine did not appear to compromise the anti-myeloma activity of treatment, which consisted of high-dose melphalan (HDM) and autologous hematopoietic stem cell transplant (auto-HSCT).
Ehsan Malek, MD, of Case Western Reserve University in Cleveland, Ohio, and his colleagues reported these findings in Leukemia & Lymphoma.
The researchers compared HDM plus auto-HSCT, with or without pre-treatment amifostine, in previously treated MM patients.
There were 107 patients who received amifostine and 114 who did not. The 107 patients received amifostine at 740 mg/m2, given as a bolus infusion at 24 hours and 15 minutes before HDM.
Baseline characteristics were largely similar in the amifostine and control groups. However, more patients in the amifostine group received a tandem HSCT (17 vs 0), and more patients in the control group had an ECOG performance status of 0 (64.3% vs 43%).
Patients in the amifostine group had a longer median time from diagnosis to first HSCT—10 months (range, 4-39) vs 7 months (range, 1-95).
A majority of patients in both groups were in partial response or better at baseline. However, more patients in the control group had stable disease (6.2% vs 1%) or progressive disease (8% vs 0%).
Results
For all-grade GI toxicities, there was largely no significant difference between the amifostine and control groups. However, patients in the amifostine group had significantly lower rates of grade 2 or higher GI toxicities.
Rates of all-grade GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—53.3% vs 64.0%, P=0.104
- Nausea—90.7% vs 95.6%, P=0.143
- Vomiting—65.4% vs 75.4%, P=0.102
- Diarrhea—93.5% vs 84.2%,P=0.030.
Rates of grade 2 or higher GI toxicities in the amifostine and control groups, respectively, were:
- Oral mucositis—27.1% vs 47.4%, P=0.002
- Nausea—31.8% vs 86.0%, P<0.0001
- Vomiting—18.7% vs 52.6%, P<0.0001
- Diarrhea—56.1% vs 73.7%, P=0.006.
The researchers said amifostine was well tolerated and produced no significant adverse effects.
They also said amifostine had “no discernable effect” on engraftment, progression-free survival, or overall survival.
The median time to neutrophil engraftment was 11 days (range, 9-16) in the control group and 10 days (range, 6-21) in the amifostine group (P=0.011). The median time to platelet engraftment was 18 days (range, 0-26) and 19 days (range, 8-71), respectively (P<0.21).
The median progression-free survival was 40 months in the amifostine group and 32 months in the control group (P=0.012). The median overall survival was 70 months and 67 months, respectively (P=0.84). ![]()
Drugs appear comparable for delaying SREs in MM
In a phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying skeletal-related events (SREs) in patients with multiple myeloma (MM).
The median time to first on-study SRE was 23 months in the denosumab arm and 24 months in the zoledronic acid arm.
There were fewer renal adverse events (AEs) but more hypocalcemia AEs in the denosumab arm.
“Until recently, treatment options for the prevention of skeletal-related events in multiple myeloma were limited to bisphosphonates, which are cleared through the kidneys and can be associated with increased renal impairment,” said Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston.
“Denosumab, which is not cleared through the kidneys, provides a new treatment option for the prevention of skeletal-related events in patients with multiple myeloma.”
Dr Raje and her colleagues conducted this phase 3 trial of denosumab and reported the results in The Lancet Oncology. The trial was sponsored by Amgen, the company developing denosumab.
Denosumab is the first fully human monoclonal antibody that binds to and neutralizes RANK ligand—a protein essential for the formation, function, and survival of osteoclasts—thereby inhibiting osteoclast-mediated bone destruction.
In this trial, researchers compared denosumab to zoledronic acid for the prevention of SREs in adults with newly diagnosed MM and bone disease.
The team randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859). All patients also received investigators’ choice of first-line MM therapy.
Skeletal surveys using conventional radiography were obtained every 12 to 24 weeks per protocol. The primary endpoint of the study was non-inferiority of denosumab to zoledronic acid for time to first on-study SRE (pathologic fracture, radiation to bone, surgery to bone, or spinal cord compression).
The primary endpoint was met. The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio [HR]=0.98; 95% confidence interval [CI]: 0.85-1.14; P non-inferiority=0.010).
Approximately 60% of all first SREs occurred within the first 3 months, and 81% occurred within the first 6 months.
Overall survival, a secondary endpoint, was similar between the denosumab and zoledronic acid arms (HR=0.90; 95% CI: 0.70-1.16; P=0.41).
There were fewer renal treatment-emergent AEs in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively. There were more hypocalcemia AEs in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
The incidence of osteonecrosis of the jaw was 4% in the denosumab arm and 3% in the zoledronic acid arm.
The most common grade 3 or higher treatment-emergent AEs (in the denosumab and zoledronic acid arms, respectively) were neutropenia (15% in both arms), thrombocytopenia (14% and 12%), anemia (12% and 10%), febrile neutropenia (11% and 10%), and pneumonia (8% in both arms).
The most common serious AE was pneumonia (8% in both arms).
Treatment-emergent AEs led to study drug discontinuation in 13% of patients in the denosumab arm and 12% in the zoledronic acid arm.
One patient in the zoledronic acid arm died of cardiac arrest that was deemed treatment-related. No other deaths were considered treatment-related. ![]()
In a phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying skeletal-related events (SREs) in patients with multiple myeloma (MM).
The median time to first on-study SRE was 23 months in the denosumab arm and 24 months in the zoledronic acid arm.
There were fewer renal adverse events (AEs) but more hypocalcemia AEs in the denosumab arm.
“Until recently, treatment options for the prevention of skeletal-related events in multiple myeloma were limited to bisphosphonates, which are cleared through the kidneys and can be associated with increased renal impairment,” said Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston.
“Denosumab, which is not cleared through the kidneys, provides a new treatment option for the prevention of skeletal-related events in patients with multiple myeloma.”
Dr Raje and her colleagues conducted this phase 3 trial of denosumab and reported the results in The Lancet Oncology. The trial was sponsored by Amgen, the company developing denosumab.
Denosumab is the first fully human monoclonal antibody that binds to and neutralizes RANK ligand—a protein essential for the formation, function, and survival of osteoclasts—thereby inhibiting osteoclast-mediated bone destruction.
In this trial, researchers compared denosumab to zoledronic acid for the prevention of SREs in adults with newly diagnosed MM and bone disease.
The team randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859). All patients also received investigators’ choice of first-line MM therapy.
Skeletal surveys using conventional radiography were obtained every 12 to 24 weeks per protocol. The primary endpoint of the study was non-inferiority of denosumab to zoledronic acid for time to first on-study SRE (pathologic fracture, radiation to bone, surgery to bone, or spinal cord compression).
The primary endpoint was met. The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio [HR]=0.98; 95% confidence interval [CI]: 0.85-1.14; P non-inferiority=0.010).
Approximately 60% of all first SREs occurred within the first 3 months, and 81% occurred within the first 6 months.
Overall survival, a secondary endpoint, was similar between the denosumab and zoledronic acid arms (HR=0.90; 95% CI: 0.70-1.16; P=0.41).
There were fewer renal treatment-emergent AEs in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively. There were more hypocalcemia AEs in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
The incidence of osteonecrosis of the jaw was 4% in the denosumab arm and 3% in the zoledronic acid arm.
The most common grade 3 or higher treatment-emergent AEs (in the denosumab and zoledronic acid arms, respectively) were neutropenia (15% in both arms), thrombocytopenia (14% and 12%), anemia (12% and 10%), febrile neutropenia (11% and 10%), and pneumonia (8% in both arms).
The most common serious AE was pneumonia (8% in both arms).
Treatment-emergent AEs led to study drug discontinuation in 13% of patients in the denosumab arm and 12% in the zoledronic acid arm.
One patient in the zoledronic acid arm died of cardiac arrest that was deemed treatment-related. No other deaths were considered treatment-related. ![]()
In a phase 3 trial, denosumab proved non-inferior to zoledronic acid for delaying skeletal-related events (SREs) in patients with multiple myeloma (MM).
The median time to first on-study SRE was 23 months in the denosumab arm and 24 months in the zoledronic acid arm.
There were fewer renal adverse events (AEs) but more hypocalcemia AEs in the denosumab arm.
“Until recently, treatment options for the prevention of skeletal-related events in multiple myeloma were limited to bisphosphonates, which are cleared through the kidneys and can be associated with increased renal impairment,” said Noopur Raje, MD, of Massachusetts General Hospital Cancer Center in Boston.
“Denosumab, which is not cleared through the kidneys, provides a new treatment option for the prevention of skeletal-related events in patients with multiple myeloma.”
Dr Raje and her colleagues conducted this phase 3 trial of denosumab and reported the results in The Lancet Oncology. The trial was sponsored by Amgen, the company developing denosumab.
Denosumab is the first fully human monoclonal antibody that binds to and neutralizes RANK ligand—a protein essential for the formation, function, and survival of osteoclasts—thereby inhibiting osteoclast-mediated bone destruction.
In this trial, researchers compared denosumab to zoledronic acid for the prevention of SREs in adults with newly diagnosed MM and bone disease.
The team randomized 1718 patients to receive subcutaneous denosumab at 120 mg and intravenous placebo every 4 weeks (n=859) or intravenous zoledronic acid at 4 mg (adjusted for renal function at baseline) and subcutaneous placebo every 4 weeks (n=859). All patients also received investigators’ choice of first-line MM therapy.
Skeletal surveys using conventional radiography were obtained every 12 to 24 weeks per protocol. The primary endpoint of the study was non-inferiority of denosumab to zoledronic acid for time to first on-study SRE (pathologic fracture, radiation to bone, surgery to bone, or spinal cord compression).
The primary endpoint was met. The median time to first on-study SRE was 22.8 months for patients in the denosumab arm and 24 months for those in the zoledronic acid arm (hazard ratio [HR]=0.98; 95% confidence interval [CI]: 0.85-1.14; P non-inferiority=0.010).
Approximately 60% of all first SREs occurred within the first 3 months, and 81% occurred within the first 6 months.
Overall survival, a secondary endpoint, was similar between the denosumab and zoledronic acid arms (HR=0.90; 95% CI: 0.70-1.16; P=0.41).
There were fewer renal treatment-emergent AEs in the denosumab arm than the zoledronic acid arm—10% and 17%, respectively. There were more hypocalcemia AEs in the denosumab arm than the zoledronic acid arm—17% and 12%, respectively.
The incidence of osteonecrosis of the jaw was 4% in the denosumab arm and 3% in the zoledronic acid arm.
The most common grade 3 or higher treatment-emergent AEs (in the denosumab and zoledronic acid arms, respectively) were neutropenia (15% in both arms), thrombocytopenia (14% and 12%), anemia (12% and 10%), febrile neutropenia (11% and 10%), and pneumonia (8% in both arms).
The most common serious AE was pneumonia (8% in both arms).
Treatment-emergent AEs led to study drug discontinuation in 13% of patients in the denosumab arm and 12% in the zoledronic acid arm.
One patient in the zoledronic acid arm died of cardiac arrest that was deemed treatment-related. No other deaths were considered treatment-related. ![]()
Factor IX product launched in US
The recombinant, GlycoPEGylated coagulation factor IX product Rebinyn® is now available in the US for the treatment of patients with hemophilia B.
Last May, Rebinyn was approved by the US Food and Drug Administration for on-demand treatment and control of bleeding episodes as well as perioperative management of bleeding in adults and children with hemophilia B.
The product is not approved for routine prophylaxis or immune tolerance induction in hemophilia B patients.
The full prescribing information is available at www.Rebinyn.com.
Rebinyn is also approved for use in the European Union, where it is known as nonacog beta pegol or by the brand name Refixia.
There, the product is approved for use as prophylaxis, for on-demand treatment of bleeding, and for control of bleeding related to surgical procedures in adolescents (older than 12 years of age) and adults with hemophilia B.
Trial results
The US and European approvals of nonacog beta pegol (N9-GP) were based on results from the paradigm™ clinical trials. Results from the paradigm 4 trial were published in Thrombosis Research in May 2016.
Paradigm 4 was an extension trial enrolling patients who had participated in the phase 3 trials paradigm 2 and paradigm 3.
In paradigm 2, researchers assessed N9-GP as treatment and prophylaxis in previously treated patients with hemophilia B. In paradigm 3, researchers assessed N9-GP in hemophilia B patients undergoing surgical procedures.
Paradigm 4 included 71 patients (ages 13 to 70) who continued to receive N9-GP as on-demand treatment (40 IU/kg for mild/moderate bleeds and 80 IU/kg for severe bleeds) or prophylaxis (10 IU/kg or 40 IU/kg once-weekly). Sixty-five patients completed treatment.
Safety
None of the patients developed factor IX inhibitors. Two patients had transient binding antibodies to N9-GP, but there was no sign that these antibodies had an inhibitory effect.
Four patients developed anti-CHO antibodies, but only 2 of these patients were still positive for these antibodies at the end of the trial.
There were a total of 155 adverse events. However, only 4 of these (in 3 patients) were considered possibly or probably related to N9-GP.
These events consisted of an injection site rash in 1 patient, 2 overdoses in 1 patient, and neutropenia in 1 patient. The rash and neutropenia resolved, and the patient who overdosed recovered without complications.
Efficacy
The researchers said the success rate for the treatment of reported bleeds was 94.6%. Most bleeds (87.9%) were resolved with a single injection of N9-GP, but 9.2% required 2 injections, and 2.9% required 3 or 4 injections.
The median annualized bleeding rate for patients on prophylaxis was 1.05 (interquartile range [IQR], 0.00–2.20) overall. It was 1.36 (IQR, 0.00-2.23) for the 10 IU/kg arm and 1.00 (IQR, 0.00-2.03) for the 40 IU/kg arm.
There were 14 patients on prophylaxis who underwent 23 minor surgical procedures.
The hemostatic response was considered “excellent” (better than expected/predicted for the procedure in question) in 19 procedures and “good” (as expected) in 2 procedures. In the remaining 2 procedures, hemostatic responses were not determined. ![]()
The recombinant, GlycoPEGylated coagulation factor IX product Rebinyn® is now available in the US for the treatment of patients with hemophilia B.
Last May, Rebinyn was approved by the US Food and Drug Administration for on-demand treatment and control of bleeding episodes as well as perioperative management of bleeding in adults and children with hemophilia B.
The product is not approved for routine prophylaxis or immune tolerance induction in hemophilia B patients.
The full prescribing information is available at www.Rebinyn.com.
Rebinyn is also approved for use in the European Union, where it is known as nonacog beta pegol or by the brand name Refixia.
There, the product is approved for use as prophylaxis, for on-demand treatment of bleeding, and for control of bleeding related to surgical procedures in adolescents (older than 12 years of age) and adults with hemophilia B.
Trial results
The US and European approvals of nonacog beta pegol (N9-GP) were based on results from the paradigm™ clinical trials. Results from the paradigm 4 trial were published in Thrombosis Research in May 2016.
Paradigm 4 was an extension trial enrolling patients who had participated in the phase 3 trials paradigm 2 and paradigm 3.
In paradigm 2, researchers assessed N9-GP as treatment and prophylaxis in previously treated patients with hemophilia B. In paradigm 3, researchers assessed N9-GP in hemophilia B patients undergoing surgical procedures.
Paradigm 4 included 71 patients (ages 13 to 70) who continued to receive N9-GP as on-demand treatment (40 IU/kg for mild/moderate bleeds and 80 IU/kg for severe bleeds) or prophylaxis (10 IU/kg or 40 IU/kg once-weekly). Sixty-five patients completed treatment.
Safety
None of the patients developed factor IX inhibitors. Two patients had transient binding antibodies to N9-GP, but there was no sign that these antibodies had an inhibitory effect.
Four patients developed anti-CHO antibodies, but only 2 of these patients were still positive for these antibodies at the end of the trial.
There were a total of 155 adverse events. However, only 4 of these (in 3 patients) were considered possibly or probably related to N9-GP.
These events consisted of an injection site rash in 1 patient, 2 overdoses in 1 patient, and neutropenia in 1 patient. The rash and neutropenia resolved, and the patient who overdosed recovered without complications.
Efficacy
The researchers said the success rate for the treatment of reported bleeds was 94.6%. Most bleeds (87.9%) were resolved with a single injection of N9-GP, but 9.2% required 2 injections, and 2.9% required 3 or 4 injections.
The median annualized bleeding rate for patients on prophylaxis was 1.05 (interquartile range [IQR], 0.00–2.20) overall. It was 1.36 (IQR, 0.00-2.23) for the 10 IU/kg arm and 1.00 (IQR, 0.00-2.03) for the 40 IU/kg arm.
There were 14 patients on prophylaxis who underwent 23 minor surgical procedures.
The hemostatic response was considered “excellent” (better than expected/predicted for the procedure in question) in 19 procedures and “good” (as expected) in 2 procedures. In the remaining 2 procedures, hemostatic responses were not determined. ![]()
The recombinant, GlycoPEGylated coagulation factor IX product Rebinyn® is now available in the US for the treatment of patients with hemophilia B.
Last May, Rebinyn was approved by the US Food and Drug Administration for on-demand treatment and control of bleeding episodes as well as perioperative management of bleeding in adults and children with hemophilia B.
The product is not approved for routine prophylaxis or immune tolerance induction in hemophilia B patients.
The full prescribing information is available at www.Rebinyn.com.
Rebinyn is also approved for use in the European Union, where it is known as nonacog beta pegol or by the brand name Refixia.
There, the product is approved for use as prophylaxis, for on-demand treatment of bleeding, and for control of bleeding related to surgical procedures in adolescents (older than 12 years of age) and adults with hemophilia B.
Trial results
The US and European approvals of nonacog beta pegol (N9-GP) were based on results from the paradigm™ clinical trials. Results from the paradigm 4 trial were published in Thrombosis Research in May 2016.
Paradigm 4 was an extension trial enrolling patients who had participated in the phase 3 trials paradigm 2 and paradigm 3.
In paradigm 2, researchers assessed N9-GP as treatment and prophylaxis in previously treated patients with hemophilia B. In paradigm 3, researchers assessed N9-GP in hemophilia B patients undergoing surgical procedures.
Paradigm 4 included 71 patients (ages 13 to 70) who continued to receive N9-GP as on-demand treatment (40 IU/kg for mild/moderate bleeds and 80 IU/kg for severe bleeds) or prophylaxis (10 IU/kg or 40 IU/kg once-weekly). Sixty-five patients completed treatment.
Safety
None of the patients developed factor IX inhibitors. Two patients had transient binding antibodies to N9-GP, but there was no sign that these antibodies had an inhibitory effect.
Four patients developed anti-CHO antibodies, but only 2 of these patients were still positive for these antibodies at the end of the trial.
There were a total of 155 adverse events. However, only 4 of these (in 3 patients) were considered possibly or probably related to N9-GP.
These events consisted of an injection site rash in 1 patient, 2 overdoses in 1 patient, and neutropenia in 1 patient. The rash and neutropenia resolved, and the patient who overdosed recovered without complications.
Efficacy
The researchers said the success rate for the treatment of reported bleeds was 94.6%. Most bleeds (87.9%) were resolved with a single injection of N9-GP, but 9.2% required 2 injections, and 2.9% required 3 or 4 injections.
The median annualized bleeding rate for patients on prophylaxis was 1.05 (interquartile range [IQR], 0.00–2.20) overall. It was 1.36 (IQR, 0.00-2.23) for the 10 IU/kg arm and 1.00 (IQR, 0.00-2.03) for the 40 IU/kg arm.
There were 14 patients on prophylaxis who underwent 23 minor surgical procedures.
The hemostatic response was considered “excellent” (better than expected/predicted for the procedure in question) in 19 procedures and “good” (as expected) in 2 procedures. In the remaining 2 procedures, hemostatic responses were not determined.
Assay identifies actionable mutations in lymphoid malignancies
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.”
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.”
Researchers say hybrid capture sequencing is an accurate and sensitive method for identifying actionable gene mutations in lymphoid malignancies.
This method revealed potentially actionable mutations in 91% of patients studied, who had diffuse large B-cell lymphoma (DLBCL), follicular lymphoma (FL), or chronic lymphocytic leukemia (CLL).
The researchers therefore believe hybrid capture sequencing will bring the benefits of precision diagnosis and individualized therapy to patients with lymphoid malignancies.
“To realize the benefits of the most recent progress in cancer genomics, clinical implementation of precision medicine approaches is needed in the form of novel biomarker assays,” said study author Christian Steidl, MD, of the University of British Columbia in Vancouver, Canada.
“Fully implemented targeted sequencing-based assays in routine diagnostic pathology laboratories are currently lacking in lymphoid cancer care. Our findings demonstrate the feasibility and outline the clinical utility of integrating a lymphoma-specific pipeline into personalized cancer care.”
Dr Steidl and his colleagues reported these findings in The Journal of Molecular Diagnostics.
The researchers first compared capture hybridization and amplicon sequencing using samples from 8 patients with lymphoma. Fresh-frozen and formalin-fixed, paraffin-embedded tumor samples were sequenced using a panel of 20 lymphoma-specific genes.
The team found that capture hybridization provided “deep, more uniform coverage” and yielded “higher sensitivity for variant calling” than amplicon sequencing.
The researchers then developed a targeted sequencing pipeline using a 32-gene panel. The panel was developed with input from a group of 6 specialists who kept updating it based on the latest available information.
“This allows for continuous integration of additional gene features as our knowledge base improves,” Dr Steidl noted.
He and his colleagues then applied the hybrid capture sequencing assay and 32-gene panel to tissues from 219 patients—114 with FL, 76 with DLBCL, and 29 with CLL—who were treated in British Columbia between 2013 and 2016.
Results revealed at least one actionable mutation in 91% of the tumors. And the assay uncovered subtype-specific mutational profiles that were highly similar to published mutational profiles for FL, DLBCL, and CLL.
Furthermore, the assay had 93% concordance with whole-genome sequencing.
“Our developed assay harnesses the power of modern sequencing for clinical diagnostics purposes and potentially better deployment of novel treatments in lymphoid cancers,” Dr Steidl said. “We believe our study will help establish evidence-based approaches to decision making in lymphoid cancer care.”
“The next steps are to implement sequencing-based biomarker assays, such as reported in our study, in accredited pathology laboratories. Toward the goal of biomarker-driven clinical decision making, testing of potentially predictive biomarker assays is needed alongside clinical trials investigating novel cancer therapeutics.”
Azacitidine now available in China
Azacitidine for injection (Vidaza®) is now available in China.
The nucleoside metabolic inhibitor was approved in China to treat patients with intermediate-2/high-risk myelodysplastic syndromes (MDS), acute myeloid leukemia (AML) with 20% to 30% bone marrow blasts, and chronic myelomonocytic leukemia (CMML).
Azacitidine for injection is marketed in China by BeiGene Ltd. under an exclusive license from Celgene Corporation.
“Vidaza is the only approved hypomethylating agent shown to prolong survival for patients with MDS and the first new treatment for MDS patients approved in China since 2009,” said John V. Oyler, founder, chief executive officer, and chairman of BeiGene.
“We are excited to announce that the first prescription was made in January 2018. From now on, Chinese patients can benefit from Vidaza in hospitals around China.”
Azacitidine was evaluated in a global phase 3 trial of patients with intermediate-2- and high-risk MDS, CMML, or AML (AZA-001). Results from this trial were published in The Lancet Oncology in 2009.
Patients were randomized to receive azacitidine plus best supportive care (BSC, n=179) or conventional care regimens plus BSC (105 to BSC alone, 49 to low-dose cytarabine, and 25 to chemotherapy with cytarabine and anthracycline).
Azacitidine was given subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days every 28 days until disease progression, relapse after response, or unacceptable toxicity.
The median overall survival was 24.5 months with azacitidine, compared to 15 months for patients treated with conventional care regimens.
There was a higher hematologic response rate in the azacitidine arm than the conventional care arm—29% and 12%, respectively.
In the azacitidine group, 45% of patients who were dependent on red blood cell transfusions at baseline became transfusion independent, compared with 11% in the conventional care group.
Forty-six percent of patients in the azacitidine arm and 63% in the conventional care arm died.
Grade 3/4 hematologic toxicity (in the azacitidine and conventional care arms, respectively) included neutropenia (91% and 76%), thrombocytopenia (85% and 80%), and anemia (57% and 68%).
Azacitidine for injection (Vidaza®) is now available in China.
The nucleoside metabolic inhibitor was approved in China to treat patients with intermediate-2/high-risk myelodysplastic syndromes (MDS), acute myeloid leukemia (AML) with 20% to 30% bone marrow blasts, and chronic myelomonocytic leukemia (CMML).
Azacitidine for injection is marketed in China by BeiGene Ltd. under an exclusive license from Celgene Corporation.
“Vidaza is the only approved hypomethylating agent shown to prolong survival for patients with MDS and the first new treatment for MDS patients approved in China since 2009,” said John V. Oyler, founder, chief executive officer, and chairman of BeiGene.
“We are excited to announce that the first prescription was made in January 2018. From now on, Chinese patients can benefit from Vidaza in hospitals around China.”
Azacitidine was evaluated in a global phase 3 trial of patients with intermediate-2- and high-risk MDS, CMML, or AML (AZA-001). Results from this trial were published in The Lancet Oncology in 2009.
Patients were randomized to receive azacitidine plus best supportive care (BSC, n=179) or conventional care regimens plus BSC (105 to BSC alone, 49 to low-dose cytarabine, and 25 to chemotherapy with cytarabine and anthracycline).
Azacitidine was given subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days every 28 days until disease progression, relapse after response, or unacceptable toxicity.
The median overall survival was 24.5 months with azacitidine, compared to 15 months for patients treated with conventional care regimens.
There was a higher hematologic response rate in the azacitidine arm than the conventional care arm—29% and 12%, respectively.
In the azacitidine group, 45% of patients who were dependent on red blood cell transfusions at baseline became transfusion independent, compared with 11% in the conventional care group.
Forty-six percent of patients in the azacitidine arm and 63% in the conventional care arm died.
Grade 3/4 hematologic toxicity (in the azacitidine and conventional care arms, respectively) included neutropenia (91% and 76%), thrombocytopenia (85% and 80%), and anemia (57% and 68%).
Azacitidine for injection (Vidaza®) is now available in China.
The nucleoside metabolic inhibitor was approved in China to treat patients with intermediate-2/high-risk myelodysplastic syndromes (MDS), acute myeloid leukemia (AML) with 20% to 30% bone marrow blasts, and chronic myelomonocytic leukemia (CMML).
Azacitidine for injection is marketed in China by BeiGene Ltd. under an exclusive license from Celgene Corporation.
“Vidaza is the only approved hypomethylating agent shown to prolong survival for patients with MDS and the first new treatment for MDS patients approved in China since 2009,” said John V. Oyler, founder, chief executive officer, and chairman of BeiGene.
“We are excited to announce that the first prescription was made in January 2018. From now on, Chinese patients can benefit from Vidaza in hospitals around China.”
Azacitidine was evaluated in a global phase 3 trial of patients with intermediate-2- and high-risk MDS, CMML, or AML (AZA-001). Results from this trial were published in The Lancet Oncology in 2009.
Patients were randomized to receive azacitidine plus best supportive care (BSC, n=179) or conventional care regimens plus BSC (105 to BSC alone, 49 to low-dose cytarabine, and 25 to chemotherapy with cytarabine and anthracycline).
Azacitidine was given subcutaneously at a dose of 75 mg/m2 daily for 7 consecutive days every 28 days until disease progression, relapse after response, or unacceptable toxicity.
The median overall survival was 24.5 months with azacitidine, compared to 15 months for patients treated with conventional care regimens.
There was a higher hematologic response rate in the azacitidine arm than the conventional care arm—29% and 12%, respectively.
In the azacitidine group, 45% of patients who were dependent on red blood cell transfusions at baseline became transfusion independent, compared with 11% in the conventional care group.
Forty-six percent of patients in the azacitidine arm and 63% in the conventional care arm died.
Grade 3/4 hematologic toxicity (in the azacitidine and conventional care arms, respectively) included neutropenia (91% and 76%), thrombocytopenia (85% and 80%), and anemia (57% and 68%).
Disease burden impacts survival, toxicity after CAR T-cell therapy
Adults with relapsed or refractory acute lymphoblastic leukemia (ALL) have better outcomes if they have a low disease burden when receiving chimeric antigen receptor (CAR) T-cell therapy, according to research published in NEJM.
The final analysis of a phase 1 trial showed that patients with a low disease burden at baseline had superior event-free survival (EFS) and overall survival (OS) after therapy, compared to patients with a high disease burden.
Patients with a low disease burden also had a lower rate of cytokine release syndrome (CRS) and neurotoxic events.
“This is the longest follow-up study of people with ALL treated with CAR therapy,” said study author Jae Park, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“With the long follow-up, we were able to demonstrate, for the first time, that patients with a lower disease burden benefited the most from CAR therapy, with significantly improved survival and reduced toxicity.”
The study included 53 adults with ALL who had a median age of 44 (range, 23-74).
They were heavily pretreated, with 68% receiving CAR T-cell therapy as a third or later salvage treatment. Thirty-six percent of patients had received an allogeneic transplant, and 23% had primary refractory disease.
In this trial, patients received a single infusion of 19-28z CAR T cells after conditioning chemotherapy. The maximum follow-up time was 5.5 years, with a median follow-up of 29 months.
In all, 83% of patients achieved a complete response. The median EFS was 6.1 months, and the median OS was 12.9 months.
The median EFS was significantly longer for patients with a low disease burden (<5% bone marrow blasts) compared to a high disease burden (≥5% bone marrow blasts or extramedullary disease)—10.6 months and 5.6 months, respectively (P=0.01).
The same was true for the median OS, which was 20.1 months in patients with a low disease burden and 12.4 months in those with a high disease burden (P=0.02).
For the entire study population, the rate of CRS was 85%, and 26% of patients had severe CRS. One patient died of severe CRS and multi-organ failure before the researchers began modifying the dose of CAR T cells according to the pretreatment disease burden.
Severe CRS occurred in 41% of patients with a high disease burden and 5% of those with a low disease burden.
In the entire study population, 2% of patients had grade 2 neurotoxic effects, 36% had grade 3, 6% had grade 4, and none had grade 5. The rate of severe neurotoxicity was 42%.
Neurotoxic effects occurred in 59% of patients with a high disease burden and 14% of those with a low disease burden.
“Among all of the clinical and disease factors we examined, pretreatment disease burden was the strongest predictor of long-term outcome after CAR therapy,” Dr Park said. “Our data supports the incorporation of CAR therapy in an earlier treatment setting in ALL, when the disease volume is small, so as to achieve the greatest long-term efficacy and lowest toxicity.”
This work was supported by Juno Therapeutics, the National Institutes of Health, the Carson Family Charitable Trust, the Emerald Foundation, the Mr. and Mrs. Goodwyn Commonwealth Fund, the Terry Fox Run for Cancer Research organized by the Canadian Association of New York, Kate’s Team, William Laurence and Blanche Hughes Foundation, the Center for Experimental Therapeutics at Memorial Sloan Kettering, and the Lake Road Foundation.
Adults with relapsed or refractory acute lymphoblastic leukemia (ALL) have better outcomes if they have a low disease burden when receiving chimeric antigen receptor (CAR) T-cell therapy, according to research published in NEJM.
The final analysis of a phase 1 trial showed that patients with a low disease burden at baseline had superior event-free survival (EFS) and overall survival (OS) after therapy, compared to patients with a high disease burden.
Patients with a low disease burden also had a lower rate of cytokine release syndrome (CRS) and neurotoxic events.
“This is the longest follow-up study of people with ALL treated with CAR therapy,” said study author Jae Park, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“With the long follow-up, we were able to demonstrate, for the first time, that patients with a lower disease burden benefited the most from CAR therapy, with significantly improved survival and reduced toxicity.”
The study included 53 adults with ALL who had a median age of 44 (range, 23-74).
They were heavily pretreated, with 68% receiving CAR T-cell therapy as a third or later salvage treatment. Thirty-six percent of patients had received an allogeneic transplant, and 23% had primary refractory disease.
In this trial, patients received a single infusion of 19-28z CAR T cells after conditioning chemotherapy. The maximum follow-up time was 5.5 years, with a median follow-up of 29 months.
In all, 83% of patients achieved a complete response. The median EFS was 6.1 months, and the median OS was 12.9 months.
The median EFS was significantly longer for patients with a low disease burden (<5% bone marrow blasts) compared to a high disease burden (≥5% bone marrow blasts or extramedullary disease)—10.6 months and 5.6 months, respectively (P=0.01).
The same was true for the median OS, which was 20.1 months in patients with a low disease burden and 12.4 months in those with a high disease burden (P=0.02).
For the entire study population, the rate of CRS was 85%, and 26% of patients had severe CRS. One patient died of severe CRS and multi-organ failure before the researchers began modifying the dose of CAR T cells according to the pretreatment disease burden.
Severe CRS occurred in 41% of patients with a high disease burden and 5% of those with a low disease burden.
In the entire study population, 2% of patients had grade 2 neurotoxic effects, 36% had grade 3, 6% had grade 4, and none had grade 5. The rate of severe neurotoxicity was 42%.
Neurotoxic effects occurred in 59% of patients with a high disease burden and 14% of those with a low disease burden.
“Among all of the clinical and disease factors we examined, pretreatment disease burden was the strongest predictor of long-term outcome after CAR therapy,” Dr Park said. “Our data supports the incorporation of CAR therapy in an earlier treatment setting in ALL, when the disease volume is small, so as to achieve the greatest long-term efficacy and lowest toxicity.”
This work was supported by Juno Therapeutics, the National Institutes of Health, the Carson Family Charitable Trust, the Emerald Foundation, the Mr. and Mrs. Goodwyn Commonwealth Fund, the Terry Fox Run for Cancer Research organized by the Canadian Association of New York, Kate’s Team, William Laurence and Blanche Hughes Foundation, the Center for Experimental Therapeutics at Memorial Sloan Kettering, and the Lake Road Foundation.
Adults with relapsed or refractory acute lymphoblastic leukemia (ALL) have better outcomes if they have a low disease burden when receiving chimeric antigen receptor (CAR) T-cell therapy, according to research published in NEJM.
The final analysis of a phase 1 trial showed that patients with a low disease burden at baseline had superior event-free survival (EFS) and overall survival (OS) after therapy, compared to patients with a high disease burden.
Patients with a low disease burden also had a lower rate of cytokine release syndrome (CRS) and neurotoxic events.
“This is the longest follow-up study of people with ALL treated with CAR therapy,” said study author Jae Park, MD, of Memorial Sloan Kettering Cancer Center in New York, New York.
“With the long follow-up, we were able to demonstrate, for the first time, that patients with a lower disease burden benefited the most from CAR therapy, with significantly improved survival and reduced toxicity.”
The study included 53 adults with ALL who had a median age of 44 (range, 23-74).
They were heavily pretreated, with 68% receiving CAR T-cell therapy as a third or later salvage treatment. Thirty-six percent of patients had received an allogeneic transplant, and 23% had primary refractory disease.
In this trial, patients received a single infusion of 19-28z CAR T cells after conditioning chemotherapy. The maximum follow-up time was 5.5 years, with a median follow-up of 29 months.
In all, 83% of patients achieved a complete response. The median EFS was 6.1 months, and the median OS was 12.9 months.
The median EFS was significantly longer for patients with a low disease burden (<5% bone marrow blasts) compared to a high disease burden (≥5% bone marrow blasts or extramedullary disease)—10.6 months and 5.6 months, respectively (P=0.01).
The same was true for the median OS, which was 20.1 months in patients with a low disease burden and 12.4 months in those with a high disease burden (P=0.02).
For the entire study population, the rate of CRS was 85%, and 26% of patients had severe CRS. One patient died of severe CRS and multi-organ failure before the researchers began modifying the dose of CAR T cells according to the pretreatment disease burden.
Severe CRS occurred in 41% of patients with a high disease burden and 5% of those with a low disease burden.
In the entire study population, 2% of patients had grade 2 neurotoxic effects, 36% had grade 3, 6% had grade 4, and none had grade 5. The rate of severe neurotoxicity was 42%.
Neurotoxic effects occurred in 59% of patients with a high disease burden and 14% of those with a low disease burden.
“Among all of the clinical and disease factors we examined, pretreatment disease burden was the strongest predictor of long-term outcome after CAR therapy,” Dr Park said. “Our data supports the incorporation of CAR therapy in an earlier treatment setting in ALL, when the disease volume is small, so as to achieve the greatest long-term efficacy and lowest toxicity.”
This work was supported by Juno Therapeutics, the National Institutes of Health, the Carson Family Charitable Trust, the Emerald Foundation, the Mr. and Mrs. Goodwyn Commonwealth Fund, the Terry Fox Run for Cancer Research organized by the Canadian Association of New York, Kate’s Team, William Laurence and Blanche Hughes Foundation, the Center for Experimental Therapeutics at Memorial Sloan Kettering, and the Lake Road Foundation.