User login
Status Epilepticus in the Emergency Department, Part 2: Treatment
In part 1 of this 2-part review, the authors detailed proper diagnosis of seizures in the ED setting. In this concluding article, they focus on appropriate management and treatment options for patients with seizure.
Status epilepticus is defined as continuous seizure activity for greater than 5 minutes, or repeated episodes of seizures without resolution of the postictal period. When the clinician arrives at the patient’s bedside or the emergency medical technician arrives at the scene in the prehospital setting, the patient may be minutes into seizure activity. If the seizure does not immediately resolve, the provider should treat as if status is imminent, if not ongoing. Regardless of setting, if the patient is discovered to be seizing, treatment should be initiated.
It is important to distinguish between provoked and unprovoked seizures, since successful management may require treating an underlying etiology. Although there are as many types of status epilepticus as there are types of seizures, the focus of this review is on generalized convulsive status epilepticus (GCSE).
As a GCSE continues, the overt seizure activity may become subtle—essentially a transformation of generalized status to a state with minimal or no motor movements. Whether or not there is an absence of, or minimal, movement, GCSE still represents a medical emergency, since the excessive neuronal activity causes neuronal injury. An electroencephalogram (EEG) may be required to detect transformed GCSE, which should be suspected if the patient does not exhibit improved mental status within 20 to 30 minutes of convulsive seizure cessation, or if neuromuscular paralysis for intubation has occurred.
Initial Management
Initial management of seizure patients is consistent with the care of any critical patient in the ED. Assessment of the airway and airway management with endotracheal intubation may be necessary for patients who are apneic or at risk for aspiration, or in whom more conservative management is inadequate.
While placing a patient in the left lateral decubitus position may mitigate aspiration risk, since vomiting is common in a postictal state, moving a convulsing patient may be challenging.1 Patients should be placed on cardiac monitoring with pulse oximetry if feasible. Intravenous (IV) access should be established if possible, though intramuscular (IM) or other alternative routes for benzodiazepines may be used if obtaining IV access will result in a delay in treatment.2
Oxygen should be administered via nonrebreather or bag-valve-mask to patients with apnea to prevent both systemic and cerebral hypoxia.3Since cardiac dysrhythmias with cerebral hypoxia may cause seizure-like activity, it is imperative to check the patient’s pulses, blood pressure, and to maintain cardiac monitoring during convulsive episodes.4 The patient’s glucose levels should be checked upon arrival to determine if the seizure is due to metabolic disturbance, which is an easily reversible cause of seizure. If glucose point-of-care testing is not available, it is reasonable to treat empirically for hypoglycemia.
Emergent Initial Therapy: First-Line Agents
Benzodiazepines
Benzodiazepines are the mainstay of emergent treatment for status epilepticus. The choice of benzodiazepine may be dependent on the clinical setting and availability of IV access or other resources. In the United States, diazepam, lorazepam, and midazolam are the common formulations used for abortive emergent initial therapy.
Diazepam. One of the advantages of diazepam is that it is has the advantage of being water soluble at room temperature, which allows rectal rescue kits for home treatment. Although diazepam is efficacious for status epilepticus, variable pharmacokinetics leading to repeat dosing and further sedation make other benzodiazepines safer.
Lorazepam. Generally accepted as the preferred IV formulation for seizure, lorazepam requires refrigeration and has a short shelf life, making its use challenging in the prehospital setting. When administered via the IV route, lorazepam works as rapidly as diazepam in treating seizures but with a longer duration of effectiveness, resulting in a decreased need to re-dose or administer an alternative antiepileptic drug (AED).5
Midazolam. Newer studies suggest that buccal, intranasal, and IM midazolam may be superior to buccal, intranasal, and IM diazepam in treating GCSE.6 The Rapid Anticonvulsant Medication Prior to Arrival Trial demonstrated IM midazolam to be at least as efficacious as IV lorazepam in the prehospital setting for treating GCSE.2
Efficacy, Route, and Dosing
A meta-analysis of all three benzodiazepines in pediatric patients with seizure showed midazolam to have the highest probability of aborting seizure activity, while lorazepam had the least likelihood of causing respiratory depression.7The authors concluded that IV lorazepam and non-IV midazolam were superior to IV and non-IV diazepam in the treatment of pediatric seizures.7
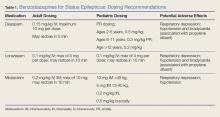
A recent retrospective study that analyzed benzodiazepine use in the emergency setting noted underdosing of benzodiazepines in the ED for nonprotocol-driven treatment of status epilepticus, resulting in the increased potential for adverse outcomes and intubations.8 Table 1 provides benzodiazepine dosing recommendations by route for adult and pediatric patients, along with potential adverse effects.
Adverse Effects
As noted previously, benzodiazepines can cause respiratory depression. Anecdotally, respiratory depression is often related to the rate at which the benzodiazepine is administered. For example, most treatment recommendations advise giving IV lorazepam over a 2-minute time period—not as an IV push.7
With respect to other adverse effects, it is important to note that IV formulations of diazepam and lorazepam contain propylene glycol as a diluent, which may lead to hypotension and bradycardia, especially when large volumes are infused over short periods of time.9
Second-Line Agents
While emergent initial therapy with benzodiazepines is well established, the preferred second-line agent, or urgent control therapy, continues to be a subject of controversy due to a lack of conclusive evidence for a superior agent.10 The Established Status Epilepticus Treatment Trial (ESETT) is currently conducting a head-to-head study to determine if any of the commonly used second-line agents (ie, fosphenytoin, levetiracetam, valproic acid) will prove to be more efficacious.11 Recently, the adult arm of the ESETT trial was halted due to futility.
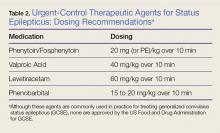
All patients without an identifiable secondary cause of GCSE (eg, hypoglycemia, hyponatremia, hypocalcemia) should be started on a second-line agent. Treatment with a second-line agent provides two benefits: First, patients who experience resolution of seizure activity may rapidly attain therapeutic levels of AEDs, which may be sustained through maintenance therapy; and second, the second-line treatment may abort refractory cases of status.12 Table 2 provides dosing recommendations for second-line agents.
Phenytoin and Fosphenytoin
Phenytoin and the newer prodrug fosphenytoin are a mainstay urgent-control therapy for emergency physicians (EPs) and neurologists alike. In one of the few head-to-head studies of AEDs,13 phenytoin did not perform as well as the other study agents (diazepam, lorazepam, and phenobarbital); however, generalizability from this study is limited. Fosphenytoin continues to be an efficacious choice for second-line treatment of AED.
Fosphenytoin, a water-soluble prodrug of phenytoin, is given preferentially over IV phenytoin due to its decreased risk of cardiovascular (CV) side effects and more rapid administration.14 Moreover, fosphenytoin is compatible with most IV fluids (eg, dextrose, lactated Ringer’s solution, normal saline [NS]), whereas phenytoin is only compatible with NS. For convenience, fosphenytoin is dosed in phenytoin equivalents (PE/kg)—eg, administration of 20 PE/kg over 10 minutes is a potential loading dose for fosphenytoin.
Valproic Acid
Valproic acid has become a favored second-line agent for many providers due to its relatively safe profile and rapid infusion time. Most studies have shown IV valproic acid is at least as effective as phenytoin, but data continue to be somewhat weak and most of the studies are uncontrolled.15
Hepatotoxicity is generally only associated with long-term use of valproic acid, but it remains reasonable to abstain from using this agent in patients with preexisting hepatic disease. Valproic acid toxicity can lead to somnolence, ataxia, seizures, and coma with marked hyperammonemia.16
Levetiracetam
Intravenous levetiracetam is becoming a more commonly used drug both for emergent initial treatment of seizure and as a maintenance therapy. While data on levetiracetam are limited, a few studies tout the efficacy and safety of IV loading to abort GCSE.
In observational studies, levetiracetam appears to have similar efficacy to other AEDs and may be more beneficial in early therapy.17 An ongoing current study, The Emergency Treatment With Levetiracetam or Phenytoin in Status Epilepticus trial, is examining a prospective cohort of pediatric patients comparing levetiracetam against phenytoin.18
Levetiracetam is generally considered safe. The most commonly reported side effects are dizziness, somnolence, nausea, and brief transaminitis.19 Levetiracetam has also been associated with neuropsychiatric exacerbations.20
Phenobarbital
Intravenous phenobarbital has been used as an urgent-control therapy for seizure with good efficacy, even in recent years.21 Despite this, phenobarbital may cause profound CV depression necessitating the use of vasopressors.22 Large-dose phenobarbital can be used to induce coma in patients, although this should not be attempted without the guidance of a neurologist. While phenobarbital can be used safely in certain circumstances, its use has fallen out of favor in the ED due to the availability of safer alternative options.
Refractory Status Epilepticus
If after receiving two AEDs, a patient continues to demonstrate seizure activity on physical examination or EEG, she or he is considered to have refractory status epilepticus, which is a medical emergency. Patients in refractory status epilepticus will likely require a continuous infusion of an AED as well as definitive airway management as a result of either seizure or continuous treatment. In rare cases, some patients will continue to seize despite continuous treatment. Such patients are considered to have super refractory status epilepticus, which is defined as continuing seizure activity despite treatment with general anesthetics for more than 24 hours. This condition is beyond the scope of traditional EP practice, who in this scenario would consult emergently with neurology or critical care services.
Propofol
Propofol, a sedative-hypnotic agent that activates both γ-aminobutyric acid and N-methyl-D-aspartate receptors, is commonly given to patients with refractory status epilepticus. While head-to-head reviews have not shown propofol to be superior to phenobarbital or midazolam in treating refractory seizure, it is a drug that is familiar to most EPs.23 Midazolam or propofol are typically given to patients in the ED who require intubation with sedation.
With respect to side effects, propofol can cause dose-limiting hypotension. In addition, propofol infusion syndrome leading to lactic acidosis and cardiac dysfunction in patients receiving long-term propofol infusion.24 One possible infusion dose is 0.5-1 mg/kg loading dose with a continuous infusion of 2 mg/kg/h IV.
High-Dose Midazolam
High-dose midazolam may be given as an alternative to propofol as some studies have shown its efficacy in treating refractory status epilepticus.25 Continuous low-dose infusions of midazolam (0.2 mg/kg/h) have been given to patients in the neurological intensive care unit (ICU); however, there are some data to support treating with a higher dose (≥0.4 mg/kg/h).25 In one single-center retrospective trial, post discharge all-cause mortality was lower in the cohort group that received the higher dose infusion (40% vs 62%).25 Although higher rates of hypotension were noted in the high-dose group, it did not appear to affect mortality.
Ketamine
Ketamine has become a valued anesthetic in emergency medicine, and EPs have become comfortable with its dosing and safety profile. While animal studies on ketamine are promising to treat status epilepticus, human data are limited and often extrapolated from retrospective ICU data. Many patients are placed on a ketamine infusion multiple days into status epilepticus, and for this reason, ketamine is not recommended as a second-line abortive drug in the ED.26
Alternative Treatments and Super Refractory GCSE
In cases of patients with seizure activity ongoing beyond conventional therapy, other methods have been attempted to cease seizure activity and achieve burst suppression on EEG. None of these treatments is in the purview of the EP and should only be undertaken by a neurologist.
Two pharmacologic agents that have some limited efficacy include lacosamide and topiramate. Isoflurane is the most commonly used inhaled anesthetic.27 Thiopental and pentobarbital are barbiturate anesthetics which are used in super refractory GCSE. Barbiturates have a desirable theoretical neuroprotective effect, but are limited by their CV depression at high doses.28 Vagus nerve stimulation, induced hypothermia, transcranial magnetic stimulation, and neurosurgical intervention have all been attempted with varying degrees of success in select patients.29
Eclampsia and Seizures During Pregnancy
Treating a pregnant patient with status epilepticus presents a unique challenge in the ED. The EP must weigh the importance of aborting seizure activity with the possibility of teratogenic effects. All AEDs must be used carefully, but valproic acid and phenytoin are potent teratogens and should be avoided in this patient population. Most evidence points to safety with exposure to benzodiazepines during pregnancy.30 Eclampsia must be considered in patients who may be pregnant or recently pregnant; magnesium should be used with or without the use of benzodiazepines in these patients.
Summary
The diagnosis and treatment of status epilepticus in the ED can be challenging. While there is a multitude of first-, second-, and third-line agents available to treat this condition, choosing the correct therapy for a patient can be daunting, and evidence of which treatment is superior can be lacking. However, the judicious use of benzodiazepines continues to be the primary treatment option. If status epilepticus persists, alternative agents and airway management may be necessary. The goal of treatment is to abort seizure-like activity observed on physician examination or EEG. It is important to remember that symptoms of status epilepticus can be subtle (eg, mild twitching, eye deviation), particularly when airway management is required since neuromuscular blockade can mask overt symptoms. Consultation with neurology and critical care colleagues should be initiated early; when such consultation is not available, the EP should consider patient transfer to an appropriate facility.
1. DeToledo JC, Lowe MR. Seizures, lateral decubitus, aspiration, and shoulder dislocation: time to change the guidelines? Neurology. 2001;56(3):290-291. doi:10.1212/wnl.56.3.290.
2. Silbergleit R, Lowenstein D, Durkalski V, et al; Neurological Emergency Treatment Trials (NETT) Investigators. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial): a double-blind randomized clinical trial of the efficacy of intramuscular midazolam versus intravenous lorazepam in the prehospital treatment of status epilepticus by paramedics. Epilepsia. 2011;52(Suppl 8):45-47. doi:10.1111/j.1528-1167.2011.03235.x.
3. Kreisman NR. Cerebral hypoxia during repetitive seizures. In: Somjen G, ed. Advances in Behavioral Biology: Mechanisms of Cerebral Hypoxia and Stroke. Vol 35. Boston, MA: Springer; 1988:139-149.
4. Van der Lende M, Surges R, Sander JW, Thijs RD. Cardiac arrhythmias during or after epileptic seizures. J Neurol Neurosurg Psychiatry. 2016;87(1):69-74. doi:10.1136/jnnp-2015-310559.
5. Appletan R, Sweeney A, Choonara I, Robson J, Molyneux E. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Dev Med Child Neurol. 1995;37(8):682-688. doi:10.1111/j.1469-8749.1995.tb15014.x.
6. McMullan J, Sasson C, Pancioli A, Silbergleit R. Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. Acad Emerg Med. 2010;17(6):575-582. doi:10.1111/j.1553-2712.2010.00751.x.
7. Zhao ZY, Wang HY, Wen B, Yang ZB, Feng K, Fan JC. A comparison of midazolam, lorazepam, and diazepam for the treatment of status epilepticus in children: a network meta-analysis. J Child Neurol. 2016;31(9):1093-1107. doi:10.1177/0883073816638757.
8. Braun J, Gau E, Revelle S, Byrne L, Kumar A. Impact of non-guideline-based treatment of status epilepticus. J Neurol Sci. 2017;382:126-130. doi:10.1016/j.jns.2017.09.031.
9. Pillai U, Hothi JC, Bhat ZY. Severe propylene glycol toxicity secondary to use of anti-epileptics. Am J Ther. 2014;21(4):e106-e109. doi:10.1097/MJT.0b013e31824c407d.
10. Berkowitz R, Koyfman A. What is the best first-line agent for benzodiazepine-resistant convulsive status epilepticus? Ann Emerg Med. 2014;64(6):656-657. doi:10.1016/j.annemergmed.2014.04.017.
11. Established Status Epilepticus Treatment Trial. U.S. National Library of Medicine. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT01960075. Accessed June 7, 2018.
12. O’Phelan KH, Miller CM. Emergency neurological life support: third edition, updates in the approach to early management of a neurological emergency. Neurocrit Care. 2017;27(Suppl 1):1-3. doi:10.1007/s12028-017-0448-x.
13. Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339(12):792-798. doi:10.1056/NEJM199809173391202.
14. Thomson A. Fosphenytoin for the treatment of status epilepticus: an evidence-based assessment of its clinical and economic outcomes. Core Evid. 2005;1(1):65-75. doi:10.2147/ce.s6408.
15. Kanner AM. Intravenous valproate for status epilepticus...an effective, yet still merely empirical alternative! 2008;8(3):66-67. doi:10.1111/j.1535-7511.2008.00240.x.
16. Mishra D, Jain R, Juneja M, Chakrabarty B. Valproate associated hyperammonemic encephalopathy. J Pediatr Neurol. 2015;9(1):93-95. doi:10.3233/jpn-2010-0437.
17. Aiguabella M, Falip M, Villanueva V, et al. Efficacy of intravenous levetiracetam as an add-on treatment in status epilepticus: a multicentric observational study. Seizure. 2011;20(1):60-64. doi:10.1016/j.seizure.2010.10.009.
18. Lyttle MD, Gamble C, Messahel S, et al; supported by Paediatric Emergency Research in the United Kingdom & Ireland (PERUKI). Emergency treatment with levetiracetam or phenytoin in status epilepticus in children—the EcLiPSE study: study protocol for a randomised controlled trial. Trials. 2017;18(1):283. doi:10.1186/s13063-017-2010-8.
19. Uges JW, van Huizen MD, Engelsman J, et al. Safety and pharmacokinetics of intravenous levetiracetam infusion as add-on in status epilepticus. Epilepsia. 2009;50(3):415-421. doi:10.1111/j.1528-1167.2008.01889.x.
20. Afazal U, Oostema JA, Smith B. Emergency department initiation of levetiracetam for seizure: a cohort study examining psychiatric risk assessment and counseling. Ann Emerg Med. 2013;62(4):S131. doi:10.1016/j.annemergmed.2013.07.194.
21. Muramoto E, Mizobuchi M, Sumi Y, et al. Efficacy of intravenous phenobarbital treatment for status epilepticus. Brain Nerve. 2013;65(8):983-987.
22. Wijdicks EFM. Status epilepticus. In: The Practice of Emergency and Critical Care Neurology. New York, NY: Oxford University Press; 2010:558-559.
23. Claassen J, Hirsch LJ, Emerson RG, Mayer SA. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43(2):146-153. doi:10.1046/j.1528-1157.2002.28501.x.
24. Choi YJ, Kim MC, Lim YJ, Yoon SZ, Yoon SM, Yoon HR. Propofol infusion associated metabolic acidosis in patients undergoing neurosurgical anesthesia: a retrospective study. J Korean Neurosurg Soc. 2014;56(2):135-140. doi:10.3340/jkns.2014.56.2.135.
25. Fernandez A, Lantigua H, Lesch C, et al. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2013;82(4): 359-365. doi:10.1212/wnl.0000000000000054.
26. Dorandeu F. Ketamine for the treatment of (super) refractory status epilepticus? Not quite yet. Expert Rev Neurother. 2017;17(5):419-421. doi:10.1080/14737175.2017.1288099.
27. Zeiler FA, Zeiler KJ, Teitelbaum J, Gillman LM, West M. Modern inhalational anesthetics for refractory status epilepticus. Can J Neurol Sci. 2015;42(2):106-115. doi:10.1017/cjn.2014.121.
28. Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134(10):2802-2818. doi:10.1093/brain/awr215.
29. Winkler PA. Surgical treatment of status epilepticus: a palliative approach. Epilepsia. 2013;54(Suppl 6):68-71. doi:10.1111/epi.12282.
30. Eros E, Czeizel AE, Rockenbauer M, Sorensen HT, Olsen J. A population-based case-control teratologic study of nitrazepam, medazepam, tofisopam, alprazolum and clonazepam treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):147-154. doi:10.1016/s0301-2115(01)00545-0.
In part 1 of this 2-part review, the authors detailed proper diagnosis of seizures in the ED setting. In this concluding article, they focus on appropriate management and treatment options for patients with seizure.
In part 1 of this 2-part review, the authors detailed proper diagnosis of seizures in the ED setting. In this concluding article, they focus on appropriate management and treatment options for patients with seizure.
Status epilepticus is defined as continuous seizure activity for greater than 5 minutes, or repeated episodes of seizures without resolution of the postictal period. When the clinician arrives at the patient’s bedside or the emergency medical technician arrives at the scene in the prehospital setting, the patient may be minutes into seizure activity. If the seizure does not immediately resolve, the provider should treat as if status is imminent, if not ongoing. Regardless of setting, if the patient is discovered to be seizing, treatment should be initiated.
It is important to distinguish between provoked and unprovoked seizures, since successful management may require treating an underlying etiology. Although there are as many types of status epilepticus as there are types of seizures, the focus of this review is on generalized convulsive status epilepticus (GCSE).
As a GCSE continues, the overt seizure activity may become subtle—essentially a transformation of generalized status to a state with minimal or no motor movements. Whether or not there is an absence of, or minimal, movement, GCSE still represents a medical emergency, since the excessive neuronal activity causes neuronal injury. An electroencephalogram (EEG) may be required to detect transformed GCSE, which should be suspected if the patient does not exhibit improved mental status within 20 to 30 minutes of convulsive seizure cessation, or if neuromuscular paralysis for intubation has occurred.
Initial Management
Initial management of seizure patients is consistent with the care of any critical patient in the ED. Assessment of the airway and airway management with endotracheal intubation may be necessary for patients who are apneic or at risk for aspiration, or in whom more conservative management is inadequate.
While placing a patient in the left lateral decubitus position may mitigate aspiration risk, since vomiting is common in a postictal state, moving a convulsing patient may be challenging.1 Patients should be placed on cardiac monitoring with pulse oximetry if feasible. Intravenous (IV) access should be established if possible, though intramuscular (IM) or other alternative routes for benzodiazepines may be used if obtaining IV access will result in a delay in treatment.2
Oxygen should be administered via nonrebreather or bag-valve-mask to patients with apnea to prevent both systemic and cerebral hypoxia.3Since cardiac dysrhythmias with cerebral hypoxia may cause seizure-like activity, it is imperative to check the patient’s pulses, blood pressure, and to maintain cardiac monitoring during convulsive episodes.4 The patient’s glucose levels should be checked upon arrival to determine if the seizure is due to metabolic disturbance, which is an easily reversible cause of seizure. If glucose point-of-care testing is not available, it is reasonable to treat empirically for hypoglycemia.
Emergent Initial Therapy: First-Line Agents
Benzodiazepines
Benzodiazepines are the mainstay of emergent treatment for status epilepticus. The choice of benzodiazepine may be dependent on the clinical setting and availability of IV access or other resources. In the United States, diazepam, lorazepam, and midazolam are the common formulations used for abortive emergent initial therapy.
Diazepam. One of the advantages of diazepam is that it is has the advantage of being water soluble at room temperature, which allows rectal rescue kits for home treatment. Although diazepam is efficacious for status epilepticus, variable pharmacokinetics leading to repeat dosing and further sedation make other benzodiazepines safer.
Lorazepam. Generally accepted as the preferred IV formulation for seizure, lorazepam requires refrigeration and has a short shelf life, making its use challenging in the prehospital setting. When administered via the IV route, lorazepam works as rapidly as diazepam in treating seizures but with a longer duration of effectiveness, resulting in a decreased need to re-dose or administer an alternative antiepileptic drug (AED).5
Midazolam. Newer studies suggest that buccal, intranasal, and IM midazolam may be superior to buccal, intranasal, and IM diazepam in treating GCSE.6 The Rapid Anticonvulsant Medication Prior to Arrival Trial demonstrated IM midazolam to be at least as efficacious as IV lorazepam in the prehospital setting for treating GCSE.2
Efficacy, Route, and Dosing
A meta-analysis of all three benzodiazepines in pediatric patients with seizure showed midazolam to have the highest probability of aborting seizure activity, while lorazepam had the least likelihood of causing respiratory depression.7The authors concluded that IV lorazepam and non-IV midazolam were superior to IV and non-IV diazepam in the treatment of pediatric seizures.7
A recent retrospective study that analyzed benzodiazepine use in the emergency setting noted underdosing of benzodiazepines in the ED for nonprotocol-driven treatment of status epilepticus, resulting in the increased potential for adverse outcomes and intubations.8 Table 1 provides benzodiazepine dosing recommendations by route for adult and pediatric patients, along with potential adverse effects.
Adverse Effects
As noted previously, benzodiazepines can cause respiratory depression. Anecdotally, respiratory depression is often related to the rate at which the benzodiazepine is administered. For example, most treatment recommendations advise giving IV lorazepam over a 2-minute time period—not as an IV push.7
With respect to other adverse effects, it is important to note that IV formulations of diazepam and lorazepam contain propylene glycol as a diluent, which may lead to hypotension and bradycardia, especially when large volumes are infused over short periods of time.9
Second-Line Agents
While emergent initial therapy with benzodiazepines is well established, the preferred second-line agent, or urgent control therapy, continues to be a subject of controversy due to a lack of conclusive evidence for a superior agent.10 The Established Status Epilepticus Treatment Trial (ESETT) is currently conducting a head-to-head study to determine if any of the commonly used second-line agents (ie, fosphenytoin, levetiracetam, valproic acid) will prove to be more efficacious.11 Recently, the adult arm of the ESETT trial was halted due to futility.
All patients without an identifiable secondary cause of GCSE (eg, hypoglycemia, hyponatremia, hypocalcemia) should be started on a second-line agent. Treatment with a second-line agent provides two benefits: First, patients who experience resolution of seizure activity may rapidly attain therapeutic levels of AEDs, which may be sustained through maintenance therapy; and second, the second-line treatment may abort refractory cases of status.12 Table 2 provides dosing recommendations for second-line agents.
Phenytoin and Fosphenytoin
Phenytoin and the newer prodrug fosphenytoin are a mainstay urgent-control therapy for emergency physicians (EPs) and neurologists alike. In one of the few head-to-head studies of AEDs,13 phenytoin did not perform as well as the other study agents (diazepam, lorazepam, and phenobarbital); however, generalizability from this study is limited. Fosphenytoin continues to be an efficacious choice for second-line treatment of AED.
Fosphenytoin, a water-soluble prodrug of phenytoin, is given preferentially over IV phenytoin due to its decreased risk of cardiovascular (CV) side effects and more rapid administration.14 Moreover, fosphenytoin is compatible with most IV fluids (eg, dextrose, lactated Ringer’s solution, normal saline [NS]), whereas phenytoin is only compatible with NS. For convenience, fosphenytoin is dosed in phenytoin equivalents (PE/kg)—eg, administration of 20 PE/kg over 10 minutes is a potential loading dose for fosphenytoin.
Valproic Acid
Valproic acid has become a favored second-line agent for many providers due to its relatively safe profile and rapid infusion time. Most studies have shown IV valproic acid is at least as effective as phenytoin, but data continue to be somewhat weak and most of the studies are uncontrolled.15
Hepatotoxicity is generally only associated with long-term use of valproic acid, but it remains reasonable to abstain from using this agent in patients with preexisting hepatic disease. Valproic acid toxicity can lead to somnolence, ataxia, seizures, and coma with marked hyperammonemia.16
Levetiracetam
Intravenous levetiracetam is becoming a more commonly used drug both for emergent initial treatment of seizure and as a maintenance therapy. While data on levetiracetam are limited, a few studies tout the efficacy and safety of IV loading to abort GCSE.
In observational studies, levetiracetam appears to have similar efficacy to other AEDs and may be more beneficial in early therapy.17 An ongoing current study, The Emergency Treatment With Levetiracetam or Phenytoin in Status Epilepticus trial, is examining a prospective cohort of pediatric patients comparing levetiracetam against phenytoin.18
Levetiracetam is generally considered safe. The most commonly reported side effects are dizziness, somnolence, nausea, and brief transaminitis.19 Levetiracetam has also been associated with neuropsychiatric exacerbations.20
Phenobarbital
Intravenous phenobarbital has been used as an urgent-control therapy for seizure with good efficacy, even in recent years.21 Despite this, phenobarbital may cause profound CV depression necessitating the use of vasopressors.22 Large-dose phenobarbital can be used to induce coma in patients, although this should not be attempted without the guidance of a neurologist. While phenobarbital can be used safely in certain circumstances, its use has fallen out of favor in the ED due to the availability of safer alternative options.
Refractory Status Epilepticus
If after receiving two AEDs, a patient continues to demonstrate seizure activity on physical examination or EEG, she or he is considered to have refractory status epilepticus, which is a medical emergency. Patients in refractory status epilepticus will likely require a continuous infusion of an AED as well as definitive airway management as a result of either seizure or continuous treatment. In rare cases, some patients will continue to seize despite continuous treatment. Such patients are considered to have super refractory status epilepticus, which is defined as continuing seizure activity despite treatment with general anesthetics for more than 24 hours. This condition is beyond the scope of traditional EP practice, who in this scenario would consult emergently with neurology or critical care services.
Propofol
Propofol, a sedative-hypnotic agent that activates both γ-aminobutyric acid and N-methyl-D-aspartate receptors, is commonly given to patients with refractory status epilepticus. While head-to-head reviews have not shown propofol to be superior to phenobarbital or midazolam in treating refractory seizure, it is a drug that is familiar to most EPs.23 Midazolam or propofol are typically given to patients in the ED who require intubation with sedation.
With respect to side effects, propofol can cause dose-limiting hypotension. In addition, propofol infusion syndrome leading to lactic acidosis and cardiac dysfunction in patients receiving long-term propofol infusion.24 One possible infusion dose is 0.5-1 mg/kg loading dose with a continuous infusion of 2 mg/kg/h IV.
High-Dose Midazolam
High-dose midazolam may be given as an alternative to propofol as some studies have shown its efficacy in treating refractory status epilepticus.25 Continuous low-dose infusions of midazolam (0.2 mg/kg/h) have been given to patients in the neurological intensive care unit (ICU); however, there are some data to support treating with a higher dose (≥0.4 mg/kg/h).25 In one single-center retrospective trial, post discharge all-cause mortality was lower in the cohort group that received the higher dose infusion (40% vs 62%).25 Although higher rates of hypotension were noted in the high-dose group, it did not appear to affect mortality.
Ketamine
Ketamine has become a valued anesthetic in emergency medicine, and EPs have become comfortable with its dosing and safety profile. While animal studies on ketamine are promising to treat status epilepticus, human data are limited and often extrapolated from retrospective ICU data. Many patients are placed on a ketamine infusion multiple days into status epilepticus, and for this reason, ketamine is not recommended as a second-line abortive drug in the ED.26
Alternative Treatments and Super Refractory GCSE
In cases of patients with seizure activity ongoing beyond conventional therapy, other methods have been attempted to cease seizure activity and achieve burst suppression on EEG. None of these treatments is in the purview of the EP and should only be undertaken by a neurologist.
Two pharmacologic agents that have some limited efficacy include lacosamide and topiramate. Isoflurane is the most commonly used inhaled anesthetic.27 Thiopental and pentobarbital are barbiturate anesthetics which are used in super refractory GCSE. Barbiturates have a desirable theoretical neuroprotective effect, but are limited by their CV depression at high doses.28 Vagus nerve stimulation, induced hypothermia, transcranial magnetic stimulation, and neurosurgical intervention have all been attempted with varying degrees of success in select patients.29
Eclampsia and Seizures During Pregnancy
Treating a pregnant patient with status epilepticus presents a unique challenge in the ED. The EP must weigh the importance of aborting seizure activity with the possibility of teratogenic effects. All AEDs must be used carefully, but valproic acid and phenytoin are potent teratogens and should be avoided in this patient population. Most evidence points to safety with exposure to benzodiazepines during pregnancy.30 Eclampsia must be considered in patients who may be pregnant or recently pregnant; magnesium should be used with or without the use of benzodiazepines in these patients.
Summary
The diagnosis and treatment of status epilepticus in the ED can be challenging. While there is a multitude of first-, second-, and third-line agents available to treat this condition, choosing the correct therapy for a patient can be daunting, and evidence of which treatment is superior can be lacking. However, the judicious use of benzodiazepines continues to be the primary treatment option. If status epilepticus persists, alternative agents and airway management may be necessary. The goal of treatment is to abort seizure-like activity observed on physician examination or EEG. It is important to remember that symptoms of status epilepticus can be subtle (eg, mild twitching, eye deviation), particularly when airway management is required since neuromuscular blockade can mask overt symptoms. Consultation with neurology and critical care colleagues should be initiated early; when such consultation is not available, the EP should consider patient transfer to an appropriate facility.
Status epilepticus is defined as continuous seizure activity for greater than 5 minutes, or repeated episodes of seizures without resolution of the postictal period. When the clinician arrives at the patient’s bedside or the emergency medical technician arrives at the scene in the prehospital setting, the patient may be minutes into seizure activity. If the seizure does not immediately resolve, the provider should treat as if status is imminent, if not ongoing. Regardless of setting, if the patient is discovered to be seizing, treatment should be initiated.
It is important to distinguish between provoked and unprovoked seizures, since successful management may require treating an underlying etiology. Although there are as many types of status epilepticus as there are types of seizures, the focus of this review is on generalized convulsive status epilepticus (GCSE).
As a GCSE continues, the overt seizure activity may become subtle—essentially a transformation of generalized status to a state with minimal or no motor movements. Whether or not there is an absence of, or minimal, movement, GCSE still represents a medical emergency, since the excessive neuronal activity causes neuronal injury. An electroencephalogram (EEG) may be required to detect transformed GCSE, which should be suspected if the patient does not exhibit improved mental status within 20 to 30 minutes of convulsive seizure cessation, or if neuromuscular paralysis for intubation has occurred.
Initial Management
Initial management of seizure patients is consistent with the care of any critical patient in the ED. Assessment of the airway and airway management with endotracheal intubation may be necessary for patients who are apneic or at risk for aspiration, or in whom more conservative management is inadequate.
While placing a patient in the left lateral decubitus position may mitigate aspiration risk, since vomiting is common in a postictal state, moving a convulsing patient may be challenging.1 Patients should be placed on cardiac monitoring with pulse oximetry if feasible. Intravenous (IV) access should be established if possible, though intramuscular (IM) or other alternative routes for benzodiazepines may be used if obtaining IV access will result in a delay in treatment.2
Oxygen should be administered via nonrebreather or bag-valve-mask to patients with apnea to prevent both systemic and cerebral hypoxia.3Since cardiac dysrhythmias with cerebral hypoxia may cause seizure-like activity, it is imperative to check the patient’s pulses, blood pressure, and to maintain cardiac monitoring during convulsive episodes.4 The patient’s glucose levels should be checked upon arrival to determine if the seizure is due to metabolic disturbance, which is an easily reversible cause of seizure. If glucose point-of-care testing is not available, it is reasonable to treat empirically for hypoglycemia.
Emergent Initial Therapy: First-Line Agents
Benzodiazepines
Benzodiazepines are the mainstay of emergent treatment for status epilepticus. The choice of benzodiazepine may be dependent on the clinical setting and availability of IV access or other resources. In the United States, diazepam, lorazepam, and midazolam are the common formulations used for abortive emergent initial therapy.
Diazepam. One of the advantages of diazepam is that it is has the advantage of being water soluble at room temperature, which allows rectal rescue kits for home treatment. Although diazepam is efficacious for status epilepticus, variable pharmacokinetics leading to repeat dosing and further sedation make other benzodiazepines safer.
Lorazepam. Generally accepted as the preferred IV formulation for seizure, lorazepam requires refrigeration and has a short shelf life, making its use challenging in the prehospital setting. When administered via the IV route, lorazepam works as rapidly as diazepam in treating seizures but with a longer duration of effectiveness, resulting in a decreased need to re-dose or administer an alternative antiepileptic drug (AED).5
Midazolam. Newer studies suggest that buccal, intranasal, and IM midazolam may be superior to buccal, intranasal, and IM diazepam in treating GCSE.6 The Rapid Anticonvulsant Medication Prior to Arrival Trial demonstrated IM midazolam to be at least as efficacious as IV lorazepam in the prehospital setting for treating GCSE.2
Efficacy, Route, and Dosing
A meta-analysis of all three benzodiazepines in pediatric patients with seizure showed midazolam to have the highest probability of aborting seizure activity, while lorazepam had the least likelihood of causing respiratory depression.7The authors concluded that IV lorazepam and non-IV midazolam were superior to IV and non-IV diazepam in the treatment of pediatric seizures.7
A recent retrospective study that analyzed benzodiazepine use in the emergency setting noted underdosing of benzodiazepines in the ED for nonprotocol-driven treatment of status epilepticus, resulting in the increased potential for adverse outcomes and intubations.8 Table 1 provides benzodiazepine dosing recommendations by route for adult and pediatric patients, along with potential adverse effects.
Adverse Effects
As noted previously, benzodiazepines can cause respiratory depression. Anecdotally, respiratory depression is often related to the rate at which the benzodiazepine is administered. For example, most treatment recommendations advise giving IV lorazepam over a 2-minute time period—not as an IV push.7
With respect to other adverse effects, it is important to note that IV formulations of diazepam and lorazepam contain propylene glycol as a diluent, which may lead to hypotension and bradycardia, especially when large volumes are infused over short periods of time.9
Second-Line Agents
While emergent initial therapy with benzodiazepines is well established, the preferred second-line agent, or urgent control therapy, continues to be a subject of controversy due to a lack of conclusive evidence for a superior agent.10 The Established Status Epilepticus Treatment Trial (ESETT) is currently conducting a head-to-head study to determine if any of the commonly used second-line agents (ie, fosphenytoin, levetiracetam, valproic acid) will prove to be more efficacious.11 Recently, the adult arm of the ESETT trial was halted due to futility.
All patients without an identifiable secondary cause of GCSE (eg, hypoglycemia, hyponatremia, hypocalcemia) should be started on a second-line agent. Treatment with a second-line agent provides two benefits: First, patients who experience resolution of seizure activity may rapidly attain therapeutic levels of AEDs, which may be sustained through maintenance therapy; and second, the second-line treatment may abort refractory cases of status.12 Table 2 provides dosing recommendations for second-line agents.
Phenytoin and Fosphenytoin
Phenytoin and the newer prodrug fosphenytoin are a mainstay urgent-control therapy for emergency physicians (EPs) and neurologists alike. In one of the few head-to-head studies of AEDs,13 phenytoin did not perform as well as the other study agents (diazepam, lorazepam, and phenobarbital); however, generalizability from this study is limited. Fosphenytoin continues to be an efficacious choice for second-line treatment of AED.
Fosphenytoin, a water-soluble prodrug of phenytoin, is given preferentially over IV phenytoin due to its decreased risk of cardiovascular (CV) side effects and more rapid administration.14 Moreover, fosphenytoin is compatible with most IV fluids (eg, dextrose, lactated Ringer’s solution, normal saline [NS]), whereas phenytoin is only compatible with NS. For convenience, fosphenytoin is dosed in phenytoin equivalents (PE/kg)—eg, administration of 20 PE/kg over 10 minutes is a potential loading dose for fosphenytoin.
Valproic Acid
Valproic acid has become a favored second-line agent for many providers due to its relatively safe profile and rapid infusion time. Most studies have shown IV valproic acid is at least as effective as phenytoin, but data continue to be somewhat weak and most of the studies are uncontrolled.15
Hepatotoxicity is generally only associated with long-term use of valproic acid, but it remains reasonable to abstain from using this agent in patients with preexisting hepatic disease. Valproic acid toxicity can lead to somnolence, ataxia, seizures, and coma with marked hyperammonemia.16
Levetiracetam
Intravenous levetiracetam is becoming a more commonly used drug both for emergent initial treatment of seizure and as a maintenance therapy. While data on levetiracetam are limited, a few studies tout the efficacy and safety of IV loading to abort GCSE.
In observational studies, levetiracetam appears to have similar efficacy to other AEDs and may be more beneficial in early therapy.17 An ongoing current study, The Emergency Treatment With Levetiracetam or Phenytoin in Status Epilepticus trial, is examining a prospective cohort of pediatric patients comparing levetiracetam against phenytoin.18
Levetiracetam is generally considered safe. The most commonly reported side effects are dizziness, somnolence, nausea, and brief transaminitis.19 Levetiracetam has also been associated with neuropsychiatric exacerbations.20
Phenobarbital
Intravenous phenobarbital has been used as an urgent-control therapy for seizure with good efficacy, even in recent years.21 Despite this, phenobarbital may cause profound CV depression necessitating the use of vasopressors.22 Large-dose phenobarbital can be used to induce coma in patients, although this should not be attempted without the guidance of a neurologist. While phenobarbital can be used safely in certain circumstances, its use has fallen out of favor in the ED due to the availability of safer alternative options.
Refractory Status Epilepticus
If after receiving two AEDs, a patient continues to demonstrate seizure activity on physical examination or EEG, she or he is considered to have refractory status epilepticus, which is a medical emergency. Patients in refractory status epilepticus will likely require a continuous infusion of an AED as well as definitive airway management as a result of either seizure or continuous treatment. In rare cases, some patients will continue to seize despite continuous treatment. Such patients are considered to have super refractory status epilepticus, which is defined as continuing seizure activity despite treatment with general anesthetics for more than 24 hours. This condition is beyond the scope of traditional EP practice, who in this scenario would consult emergently with neurology or critical care services.
Propofol
Propofol, a sedative-hypnotic agent that activates both γ-aminobutyric acid and N-methyl-D-aspartate receptors, is commonly given to patients with refractory status epilepticus. While head-to-head reviews have not shown propofol to be superior to phenobarbital or midazolam in treating refractory seizure, it is a drug that is familiar to most EPs.23 Midazolam or propofol are typically given to patients in the ED who require intubation with sedation.
With respect to side effects, propofol can cause dose-limiting hypotension. In addition, propofol infusion syndrome leading to lactic acidosis and cardiac dysfunction in patients receiving long-term propofol infusion.24 One possible infusion dose is 0.5-1 mg/kg loading dose with a continuous infusion of 2 mg/kg/h IV.
High-Dose Midazolam
High-dose midazolam may be given as an alternative to propofol as some studies have shown its efficacy in treating refractory status epilepticus.25 Continuous low-dose infusions of midazolam (0.2 mg/kg/h) have been given to patients in the neurological intensive care unit (ICU); however, there are some data to support treating with a higher dose (≥0.4 mg/kg/h).25 In one single-center retrospective trial, post discharge all-cause mortality was lower in the cohort group that received the higher dose infusion (40% vs 62%).25 Although higher rates of hypotension were noted in the high-dose group, it did not appear to affect mortality.
Ketamine
Ketamine has become a valued anesthetic in emergency medicine, and EPs have become comfortable with its dosing and safety profile. While animal studies on ketamine are promising to treat status epilepticus, human data are limited and often extrapolated from retrospective ICU data. Many patients are placed on a ketamine infusion multiple days into status epilepticus, and for this reason, ketamine is not recommended as a second-line abortive drug in the ED.26
Alternative Treatments and Super Refractory GCSE
In cases of patients with seizure activity ongoing beyond conventional therapy, other methods have been attempted to cease seizure activity and achieve burst suppression on EEG. None of these treatments is in the purview of the EP and should only be undertaken by a neurologist.
Two pharmacologic agents that have some limited efficacy include lacosamide and topiramate. Isoflurane is the most commonly used inhaled anesthetic.27 Thiopental and pentobarbital are barbiturate anesthetics which are used in super refractory GCSE. Barbiturates have a desirable theoretical neuroprotective effect, but are limited by their CV depression at high doses.28 Vagus nerve stimulation, induced hypothermia, transcranial magnetic stimulation, and neurosurgical intervention have all been attempted with varying degrees of success in select patients.29
Eclampsia and Seizures During Pregnancy
Treating a pregnant patient with status epilepticus presents a unique challenge in the ED. The EP must weigh the importance of aborting seizure activity with the possibility of teratogenic effects. All AEDs must be used carefully, but valproic acid and phenytoin are potent teratogens and should be avoided in this patient population. Most evidence points to safety with exposure to benzodiazepines during pregnancy.30 Eclampsia must be considered in patients who may be pregnant or recently pregnant; magnesium should be used with or without the use of benzodiazepines in these patients.
Summary
The diagnosis and treatment of status epilepticus in the ED can be challenging. While there is a multitude of first-, second-, and third-line agents available to treat this condition, choosing the correct therapy for a patient can be daunting, and evidence of which treatment is superior can be lacking. However, the judicious use of benzodiazepines continues to be the primary treatment option. If status epilepticus persists, alternative agents and airway management may be necessary. The goal of treatment is to abort seizure-like activity observed on physician examination or EEG. It is important to remember that symptoms of status epilepticus can be subtle (eg, mild twitching, eye deviation), particularly when airway management is required since neuromuscular blockade can mask overt symptoms. Consultation with neurology and critical care colleagues should be initiated early; when such consultation is not available, the EP should consider patient transfer to an appropriate facility.
1. DeToledo JC, Lowe MR. Seizures, lateral decubitus, aspiration, and shoulder dislocation: time to change the guidelines? Neurology. 2001;56(3):290-291. doi:10.1212/wnl.56.3.290.
2. Silbergleit R, Lowenstein D, Durkalski V, et al; Neurological Emergency Treatment Trials (NETT) Investigators. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial): a double-blind randomized clinical trial of the efficacy of intramuscular midazolam versus intravenous lorazepam in the prehospital treatment of status epilepticus by paramedics. Epilepsia. 2011;52(Suppl 8):45-47. doi:10.1111/j.1528-1167.2011.03235.x.
3. Kreisman NR. Cerebral hypoxia during repetitive seizures. In: Somjen G, ed. Advances in Behavioral Biology: Mechanisms of Cerebral Hypoxia and Stroke. Vol 35. Boston, MA: Springer; 1988:139-149.
4. Van der Lende M, Surges R, Sander JW, Thijs RD. Cardiac arrhythmias during or after epileptic seizures. J Neurol Neurosurg Psychiatry. 2016;87(1):69-74. doi:10.1136/jnnp-2015-310559.
5. Appletan R, Sweeney A, Choonara I, Robson J, Molyneux E. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Dev Med Child Neurol. 1995;37(8):682-688. doi:10.1111/j.1469-8749.1995.tb15014.x.
6. McMullan J, Sasson C, Pancioli A, Silbergleit R. Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. Acad Emerg Med. 2010;17(6):575-582. doi:10.1111/j.1553-2712.2010.00751.x.
7. Zhao ZY, Wang HY, Wen B, Yang ZB, Feng K, Fan JC. A comparison of midazolam, lorazepam, and diazepam for the treatment of status epilepticus in children: a network meta-analysis. J Child Neurol. 2016;31(9):1093-1107. doi:10.1177/0883073816638757.
8. Braun J, Gau E, Revelle S, Byrne L, Kumar A. Impact of non-guideline-based treatment of status epilepticus. J Neurol Sci. 2017;382:126-130. doi:10.1016/j.jns.2017.09.031.
9. Pillai U, Hothi JC, Bhat ZY. Severe propylene glycol toxicity secondary to use of anti-epileptics. Am J Ther. 2014;21(4):e106-e109. doi:10.1097/MJT.0b013e31824c407d.
10. Berkowitz R, Koyfman A. What is the best first-line agent for benzodiazepine-resistant convulsive status epilepticus? Ann Emerg Med. 2014;64(6):656-657. doi:10.1016/j.annemergmed.2014.04.017.
11. Established Status Epilepticus Treatment Trial. U.S. National Library of Medicine. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT01960075. Accessed June 7, 2018.
12. O’Phelan KH, Miller CM. Emergency neurological life support: third edition, updates in the approach to early management of a neurological emergency. Neurocrit Care. 2017;27(Suppl 1):1-3. doi:10.1007/s12028-017-0448-x.
13. Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339(12):792-798. doi:10.1056/NEJM199809173391202.
14. Thomson A. Fosphenytoin for the treatment of status epilepticus: an evidence-based assessment of its clinical and economic outcomes. Core Evid. 2005;1(1):65-75. doi:10.2147/ce.s6408.
15. Kanner AM. Intravenous valproate for status epilepticus...an effective, yet still merely empirical alternative! 2008;8(3):66-67. doi:10.1111/j.1535-7511.2008.00240.x.
16. Mishra D, Jain R, Juneja M, Chakrabarty B. Valproate associated hyperammonemic encephalopathy. J Pediatr Neurol. 2015;9(1):93-95. doi:10.3233/jpn-2010-0437.
17. Aiguabella M, Falip M, Villanueva V, et al. Efficacy of intravenous levetiracetam as an add-on treatment in status epilepticus: a multicentric observational study. Seizure. 2011;20(1):60-64. doi:10.1016/j.seizure.2010.10.009.
18. Lyttle MD, Gamble C, Messahel S, et al; supported by Paediatric Emergency Research in the United Kingdom & Ireland (PERUKI). Emergency treatment with levetiracetam or phenytoin in status epilepticus in children—the EcLiPSE study: study protocol for a randomised controlled trial. Trials. 2017;18(1):283. doi:10.1186/s13063-017-2010-8.
19. Uges JW, van Huizen MD, Engelsman J, et al. Safety and pharmacokinetics of intravenous levetiracetam infusion as add-on in status epilepticus. Epilepsia. 2009;50(3):415-421. doi:10.1111/j.1528-1167.2008.01889.x.
20. Afazal U, Oostema JA, Smith B. Emergency department initiation of levetiracetam for seizure: a cohort study examining psychiatric risk assessment and counseling. Ann Emerg Med. 2013;62(4):S131. doi:10.1016/j.annemergmed.2013.07.194.
21. Muramoto E, Mizobuchi M, Sumi Y, et al. Efficacy of intravenous phenobarbital treatment for status epilepticus. Brain Nerve. 2013;65(8):983-987.
22. Wijdicks EFM. Status epilepticus. In: The Practice of Emergency and Critical Care Neurology. New York, NY: Oxford University Press; 2010:558-559.
23. Claassen J, Hirsch LJ, Emerson RG, Mayer SA. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43(2):146-153. doi:10.1046/j.1528-1157.2002.28501.x.
24. Choi YJ, Kim MC, Lim YJ, Yoon SZ, Yoon SM, Yoon HR. Propofol infusion associated metabolic acidosis in patients undergoing neurosurgical anesthesia: a retrospective study. J Korean Neurosurg Soc. 2014;56(2):135-140. doi:10.3340/jkns.2014.56.2.135.
25. Fernandez A, Lantigua H, Lesch C, et al. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2013;82(4): 359-365. doi:10.1212/wnl.0000000000000054.
26. Dorandeu F. Ketamine for the treatment of (super) refractory status epilepticus? Not quite yet. Expert Rev Neurother. 2017;17(5):419-421. doi:10.1080/14737175.2017.1288099.
27. Zeiler FA, Zeiler KJ, Teitelbaum J, Gillman LM, West M. Modern inhalational anesthetics for refractory status epilepticus. Can J Neurol Sci. 2015;42(2):106-115. doi:10.1017/cjn.2014.121.
28. Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134(10):2802-2818. doi:10.1093/brain/awr215.
29. Winkler PA. Surgical treatment of status epilepticus: a palliative approach. Epilepsia. 2013;54(Suppl 6):68-71. doi:10.1111/epi.12282.
30. Eros E, Czeizel AE, Rockenbauer M, Sorensen HT, Olsen J. A population-based case-control teratologic study of nitrazepam, medazepam, tofisopam, alprazolum and clonazepam treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):147-154. doi:10.1016/s0301-2115(01)00545-0.
1. DeToledo JC, Lowe MR. Seizures, lateral decubitus, aspiration, and shoulder dislocation: time to change the guidelines? Neurology. 2001;56(3):290-291. doi:10.1212/wnl.56.3.290.
2. Silbergleit R, Lowenstein D, Durkalski V, et al; Neurological Emergency Treatment Trials (NETT) Investigators. RAMPART (Rapid Anticonvulsant Medication Prior to Arrival Trial): a double-blind randomized clinical trial of the efficacy of intramuscular midazolam versus intravenous lorazepam in the prehospital treatment of status epilepticus by paramedics. Epilepsia. 2011;52(Suppl 8):45-47. doi:10.1111/j.1528-1167.2011.03235.x.
3. Kreisman NR. Cerebral hypoxia during repetitive seizures. In: Somjen G, ed. Advances in Behavioral Biology: Mechanisms of Cerebral Hypoxia and Stroke. Vol 35. Boston, MA: Springer; 1988:139-149.
4. Van der Lende M, Surges R, Sander JW, Thijs RD. Cardiac arrhythmias during or after epileptic seizures. J Neurol Neurosurg Psychiatry. 2016;87(1):69-74. doi:10.1136/jnnp-2015-310559.
5. Appletan R, Sweeney A, Choonara I, Robson J, Molyneux E. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Dev Med Child Neurol. 1995;37(8):682-688. doi:10.1111/j.1469-8749.1995.tb15014.x.
6. McMullan J, Sasson C, Pancioli A, Silbergleit R. Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. Acad Emerg Med. 2010;17(6):575-582. doi:10.1111/j.1553-2712.2010.00751.x.
7. Zhao ZY, Wang HY, Wen B, Yang ZB, Feng K, Fan JC. A comparison of midazolam, lorazepam, and diazepam for the treatment of status epilepticus in children: a network meta-analysis. J Child Neurol. 2016;31(9):1093-1107. doi:10.1177/0883073816638757.
8. Braun J, Gau E, Revelle S, Byrne L, Kumar A. Impact of non-guideline-based treatment of status epilepticus. J Neurol Sci. 2017;382:126-130. doi:10.1016/j.jns.2017.09.031.
9. Pillai U, Hothi JC, Bhat ZY. Severe propylene glycol toxicity secondary to use of anti-epileptics. Am J Ther. 2014;21(4):e106-e109. doi:10.1097/MJT.0b013e31824c407d.
10. Berkowitz R, Koyfman A. What is the best first-line agent for benzodiazepine-resistant convulsive status epilepticus? Ann Emerg Med. 2014;64(6):656-657. doi:10.1016/j.annemergmed.2014.04.017.
11. Established Status Epilepticus Treatment Trial. U.S. National Library of Medicine. ClinicalTrials.gov Web site. https://clinicaltrials.gov/ct2/show/NCT01960075. Accessed June 7, 2018.
12. O’Phelan KH, Miller CM. Emergency neurological life support: third edition, updates in the approach to early management of a neurological emergency. Neurocrit Care. 2017;27(Suppl 1):1-3. doi:10.1007/s12028-017-0448-x.
13. Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339(12):792-798. doi:10.1056/NEJM199809173391202.
14. Thomson A. Fosphenytoin for the treatment of status epilepticus: an evidence-based assessment of its clinical and economic outcomes. Core Evid. 2005;1(1):65-75. doi:10.2147/ce.s6408.
15. Kanner AM. Intravenous valproate for status epilepticus...an effective, yet still merely empirical alternative! 2008;8(3):66-67. doi:10.1111/j.1535-7511.2008.00240.x.
16. Mishra D, Jain R, Juneja M, Chakrabarty B. Valproate associated hyperammonemic encephalopathy. J Pediatr Neurol. 2015;9(1):93-95. doi:10.3233/jpn-2010-0437.
17. Aiguabella M, Falip M, Villanueva V, et al. Efficacy of intravenous levetiracetam as an add-on treatment in status epilepticus: a multicentric observational study. Seizure. 2011;20(1):60-64. doi:10.1016/j.seizure.2010.10.009.
18. Lyttle MD, Gamble C, Messahel S, et al; supported by Paediatric Emergency Research in the United Kingdom & Ireland (PERUKI). Emergency treatment with levetiracetam or phenytoin in status epilepticus in children—the EcLiPSE study: study protocol for a randomised controlled trial. Trials. 2017;18(1):283. doi:10.1186/s13063-017-2010-8.
19. Uges JW, van Huizen MD, Engelsman J, et al. Safety and pharmacokinetics of intravenous levetiracetam infusion as add-on in status epilepticus. Epilepsia. 2009;50(3):415-421. doi:10.1111/j.1528-1167.2008.01889.x.
20. Afazal U, Oostema JA, Smith B. Emergency department initiation of levetiracetam for seizure: a cohort study examining psychiatric risk assessment and counseling. Ann Emerg Med. 2013;62(4):S131. doi:10.1016/j.annemergmed.2013.07.194.
21. Muramoto E, Mizobuchi M, Sumi Y, et al. Efficacy of intravenous phenobarbital treatment for status epilepticus. Brain Nerve. 2013;65(8):983-987.
22. Wijdicks EFM. Status epilepticus. In: The Practice of Emergency and Critical Care Neurology. New York, NY: Oxford University Press; 2010:558-559.
23. Claassen J, Hirsch LJ, Emerson RG, Mayer SA. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002;43(2):146-153. doi:10.1046/j.1528-1157.2002.28501.x.
24. Choi YJ, Kim MC, Lim YJ, Yoon SZ, Yoon SM, Yoon HR. Propofol infusion associated metabolic acidosis in patients undergoing neurosurgical anesthesia: a retrospective study. J Korean Neurosurg Soc. 2014;56(2):135-140. doi:10.3340/jkns.2014.56.2.135.
25. Fernandez A, Lantigua H, Lesch C, et al. High-dose midazolam infusion for refractory status epilepticus. Neurology. 2013;82(4): 359-365. doi:10.1212/wnl.0000000000000054.
26. Dorandeu F. Ketamine for the treatment of (super) refractory status epilepticus? Not quite yet. Expert Rev Neurother. 2017;17(5):419-421. doi:10.1080/14737175.2017.1288099.
27. Zeiler FA, Zeiler KJ, Teitelbaum J, Gillman LM, West M. Modern inhalational anesthetics for refractory status epilepticus. Can J Neurol Sci. 2015;42(2):106-115. doi:10.1017/cjn.2014.121.
28. Shorvon S, Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011;134(10):2802-2818. doi:10.1093/brain/awr215.
29. Winkler PA. Surgical treatment of status epilepticus: a palliative approach. Epilepsia. 2013;54(Suppl 6):68-71. doi:10.1111/epi.12282.
30. Eros E, Czeizel AE, Rockenbauer M, Sorensen HT, Olsen J. A population-based case-control teratologic study of nitrazepam, medazepam, tofisopam, alprazolum and clonazepam treatment during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):147-154. doi:10.1016/s0301-2115(01)00545-0.
Evaluation of Seizures and Seizure-like Activity in the Emergency Department: Part 1
Seizures are a common emergency presentation, accounting for approximately 1% of all ED visits.1 Presentations include patients with epilepsy, new-onset or first-time seizure (whether provoked or unprovoked), and other diagnostic entities that can mimic seizure but are not a true epileptic seizure. Even after a detailed and comprehensive evaluation, correctly determining the diagnosis can still be a challenge.2
Seizure Phases
The International League Against Epilepsy (ILAE) defines epileptic seizures as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain.”3 There are typically three phases of a seizure—the aural, ictal, and postictal states.
Aural Phase. Patients may or may not experience an aura prior to seizure onset. An aura can manifest as a sense of déjà vu or a rising sensation in the abdomen, abnormal taste or smell, or autonomic changes. These are not warning signs of a seizure but rather an early manifestation of a focal seizure before there has been enough electrical spread to cause cognitive or motor symptoms.
Ictal Phase. The second stage of seizure, the ictal phase, is the typical cognitive or motor manifestations of seizure activity. Seizures can last several seconds to minutes, but the majority has a duration of less than 1 minute.
Postictal Phase. The postictal period occurs after the active phase of seizure and is characterized by confusion, altered mental status, and somnolence. The postictal period can last from several minutes to hours and can result in suppression of function; including cognitive or motor deficits such as Todd’s paralysis wherein a patient experiences transient paralysis confined to one hemisphere.4
Etiology and Classification
Seizures can be subdivided based on two different categories: etiology or origin of abnormal electrical impulses within the brain. To categorize seizures based on etiology, the clinician must determine whether the seizure was brought on by an identifiable cause.
Provoked Seizure
Provoked seizures are also referred to as acute symptomatic seizures, because they present within 7 days of a systemic insult, whether it be secondary to an electrolyte abnormality (eg, hyponatremia, hypoglycemia, hypercalcemia), substance withdrawal (eg, alcohol, benzodiazepines), toxic ingestion, infection, central nervous system lesions, or head injury. The aforementioned does not represent a comprehensive list, but rather some of the more common etiologies of seizures.2,5
Unprovoked Seizure
An unprovoked seizure occurs without an identifiable acute precipitating insult. These types of seizures are generally more consistent with epilepsy or are due to a remote systemic insult greater than 7 days prior. Examples include patients who have a history of stroke, traumatic brain injury, or congenital brain malformation.2,5
Epilepsy is described as a seizure disorder where recurrent, usually unprovoked seizures occur. Determining the probable etiology of a seizure can be important when pursuing proper objective evaluation and work up, as we will discuss in this article.
Seizure Type
Seizures can also be classified as being generalized or focal, depending on the probable origin of the abnormal electrical discharges within the brain. This classification system is widely used and was developed by the ILAE.6
Generalized Seizures
Generalized seizures have bilateral cortical involvement at the onset of presentation and are associated with loss of consciousness. This is determined through electroencephalogram (EEG) monitoring because focal seizures, where the initiation of abnormal electrical discharges are located in one cortical hemisphere or localized area of the brain, may rapidly spread to both hemispheres and appear very similar to a primary generalized seizure.
Tonic-Clonic Seizures. The most colloquial type of generalized seizure is a tonic-clonic seizure. “Tonic” refers to the muscle stiffness or rigidity that occurs during this type of seizure, and “clonic” describes the rhythmic jerking of these muscles.
Nontonic-Clonic Seizures. Other types of generalized seizures include absence seizures (brief staring episodes or an arrest in behavior), atonic seizures (loss of muscle tone), and myoclonic seizures (brief, sudden muscular contractions).5
Focal Seizures
Focal seizures are diagnosed when the history, clinical presentation, and EEG findings support the localization of abnormal electrical neuronal discharges to one hemisphere of the brain. Loss of consciousness does not always occur during a focal seizure, and the ILAE recently updated the terminology in this regard to this distinction in 2017. Instead of classifying focal seizures as simple partial or complex partial in relation to the preservation of consciousness, the terminology has now changed to focal aware (no loss of consciousness) and focal impaired awareness (affected consciousness). Focal seizures can have not only motor manifestations, but may also present with sensory, autonomic, or psychic symptoms, depending on the anatomic location of the abnormal neuronal activity.5-6
Evaluation in the ED Setting
The classification of a seizure does not often change the ED management of seizures, but it is important to be able to recognize that seizures may present with different clinical appearances. It is also important to remember that not all seizure-like activity is due to epilepsy or abnormal neuronal discharges. There are several other conditions that can present with physical symptoms and characteristics similar to seizure, and are often misdiagnosed as seizures. The next section describes several of these seizure mimics and how to recognize or differentiate them from seizures through a careful history, physical examination, and laboratory evaluation; as one diagnostic tool, the EEG, is not routinely available to the emergency physician (EP).
Seizure Mimics
Syncope
Syncope is secondary to decreased cerebral perfusion, which results in brief loss of consciousness and postural tone, and often with brief convulsions. Myoclonic jerking lasting a few seconds can be seen in many syncopal episodes, and if present is termed convulsive syncope. Following any syncopal episode, patients generally return to their baseline mental status without a postictal period. A prodrome of pallor and sweating can be helpful clues to identify a syncopal episode. In addition, a patient’s eyes may remain open during the event.
There are several types of syncope: cardiac, orthostatic, or neurocardiogenic (vasovagal). History and physical examination can help distinguish syncope from seizure.
Cardiac Syncope. Cardiogenic causes of syncope may be seen in elderly patients who lack a prodrome prior to the event, chest pain may have been present, the event may occur with exercise, or there is evidence of underlying heart disease. An electrocardiogram (ECG) should be done to detect cardiac dysrhythmias. Orthostatic Syncope. Vital signs may be useful in assessing for an orthostatic cause of syncope (drop in systolic blood pressure [BP] by 20 mm Hg or more and drop in diastolic BP by 10 mm Hg or more within 3 minutes of standing), though orthostatic hypotension is common in the elderly.7-8 Dysautonomia as a cause of orthostatic hypotension may show a delayed drop in BP after standing 5 to 10 minutes, in contrast to hypovolemia which tends to be present with immediate standing.Neurocardiogenic Syncope. Neurocardiogenic syncope, a somewhat confusing term, is perhaps better described as a reflex syncope, or simple faint. Often this is referred to as “vasovagal” syncope. Typically, there are physical or psychological noxious stimuli prior to the brief loss of consciousness and postural tone. Pain or strong emotions are common triggers.
Convulsive Concussion
Another seizure mimic is convulsive concussion in which the patient exhibits nonepileptic movement following a closed head injury. It is hypothesized that these post-traumatic convulsions are due to transient functional abnormalities, rather than structural brain injury. In one study, 22 cases of concussive convulsions were identified in which tonic-clonic convulsions began within 2 seconds of impact, and lasted for up to 150 seconds. These patients generally have good outcomes and do not require antiepileptic treatment; they also do not need to abstain from sports or other physical activities.9-11
Movement Disorders
Certain movement disorders can appear similar to seizures with sustained muscle contractions, repetitive movements, dystonias, or even abnormal posturing. However, these abnormal movements are generally painful and there is often impairment of consciousness. They may be genetic in nature or secondary to a neurologic disease or medications such as neuroleptics or antipsychotics.
Psychogenic Nonepileptic Seizures
Psychogenic nonepileptic seizures (PNES) are defined as episodes of altered movements or sensations that appear similar to epileptic seizures, but have an underlying psychological etiology rather than abnormal neuronal discharges. Seventy percent of these patients have a psychiatric illness, such as depression, post-traumatic stress disorder, or personality disorders. Features that can help distinguish PNES from epileptic seizures include long duration, fluctuating symptoms, asynchronous or non-rhythmic movements, pelvic thrusting, side-to-side head or body movements, closed eyes, lack of tongue biting, memory recall, crying, or suppression by distraction. Laboratory testing provides little benefit, aside from a lactate level, which if elevated can suggest a possible epileptic etiology.12 These cases may require consultation with neurology and psychiatry or video-EEG monitoring to correctly diagnose.13-14
Other non-epileptic and possible seizure mimic diagnoses to be considered include stroke, transient ischemic attack, migraine headache, and sleep disorders.
Evaluation
When assessing a patient presenting with seizure-like activity or altered mental status, the clinician must keep a broad differential diagnosis. The first step is to evaluate the ABCs. Once that is completed, a blood glucose should be obtained, as it is a quick test and can determine whether hypoglycemia is the likely cause. Intravenous (IV) access should be obtained and routine labs ordered, including a complete blood count (CBC), a comprehensive metabolic profile (CMP), magnesium, urinalysis, ECG, and lactate. Other labs that may be of clinical utility in certain cases include anticonvulsant levels (in patients that are on these medications), toxicology screens, and cerebrospinal fluid studies, if indicated. It is important to note that anticonvulsant reference ranges are trough values, so levels that are drawn within a few hours of the last dose taken
Patient Disposition
The management and ultimate disposition of a patient with a seizure depends on the underlying cause, and whether the patient has neurologic deficits and/or is back to their baseline mental status. For patients presenting with a first-time seizure and have returned to baseline, the American College of Emergency Physicians’ (ACEP) clinical policy states that precipitating medical conditions should be identified and addressed accordingly if it is a provoked seizure.
If patients present with a first-time unprovoked seizure and do not have evidence of brain injury or neurologic disease (ie, persistent altered mental status or abnormal neurologic examination), then the EP does not need to initiate antiepileptic medications. If there is evidence of neurologic disease or brain injury in an unprovoked seizure, then the EP may either choose to initiate antiepileptic medications or choose to defer, pending consultation with neurology. This group of patients (first-time unprovoked seizure back to baseline) do not need to be admitted to the hospital under the premise that they have a negative workup, to include glucose, CT scan (if indicated), ECG, CBC, and CMP. They must also have normal vital signs, be advised regarding seizure precautions such as not to drive until further medical evaluation (with duration perhaps being set by state law), and have good social support. They will require close follow up for further evaluation and definitive diagnosis, which may include head imaging, if not already performed in the ED, and EEG.
Patients with a history of epilepsy can have recurrent seizures that are either provoked or unprovoked. If the seizure appears clinically similar to their previous seizures, then causes that could lower the seizure threshold should be investigated; including compliance with antiepileptic medications (obtain serum levels), infection (urinalysis and/or chest X-ray), sleep deprivation, electrolyte imbalances, or medications known to lower seizure threshold (eg, certain antibiotics such as fluoroquinolones, antidepressants such as bupropion and venlafaxine, and antipsychotics such as clozapine). These underlying causes should be treated accordingly. If a patient has been noncompliant with their medications, a loading dose can be given in the ED, although there are no definitive studies that either support or debunk this practice. If it is a true, unprovoked seizure and the patient is compliant with their antiepileptic medication, it is reasonable to discuss medication regimen changes with the patient’s neurologist.17A patient that presents with seizure-like activity and does not return back to their baseline mental status requires a more immediate and comprehensive evaluation. Persistent altered mental status has a vast differential diagnosis, and is outside the scope of this article, but if seizures were part of the clinical presentation, the possibility of non-convulsive epilepticus should be considered. These patients may require treatment with medications (usually IV benzodiazepines), admission to the hospital, neurology consultation, EEG, imaging (CT vs MRI), and +/- lumbar puncture depending on the clinical scenario.
Status epilepticus will be further discussed in part 2 of this review.
1. Pallin DJ, Goldstein JN, Moussally JS, Pelletier AJ, Green AR, Carmargo CA Jr. Seizure visits in the US emergency departments: epidemiology and potential disparities in care. Int J Emerg Med. 2008;1(2):97-105.
2. Huff JS, Melnick ER, Tomaszewski CA, Thiessen ME, Jagoda AS, Fesmire FM; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with seizures. Ann Emerg Med. 2014;63(4):437-447.e15. doi:10.1016/j.annemergmed.2014.01.018.
3. Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470-472.
4. Webb J, Long B, Koyfman A. An emergency medicine-focused review of seizure mimics. J Emerg Med. 2017;52(5):645-653. doi:10.1016/j.jemermed.2016.11.002.
5. Huff JS, Fountain NB. Pathophysiology and definitions of seizures and status epilepticus. Emerg Med Clin North Am. 2011;29(1):1-13. doi:10.1016/j.emc.2010.08.001.
6. Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):522-530. doi:10.1111/epi.13670.
7. Kanjwal K, Karabin B, Kanjwal Y, Grubb BP. Differentiation of convulsive syncope from epilepsy with an implantable loop recorder. Int J Med Sci. 2009;6(6):296-300.
8. Ozkara C, Metin B, Kucukoglu S. Convulsive syncope: a condition to be differentiated from epilepsy. Epileptic Disord. 2009;11(4):315-319. doi:10.1684/epd.2009.0281.
9. McCrory PR, Berkovic SF. Concussive convulsions. Incidence in sport and treatment recommendations. Sports Med. 1998;25(2);131-136.
10. Ellis MJ, Wennberg R. Convulsions in a 17-year-old boy after a head injury sustained while playing hockey. CMAJ. 2016;188(6):443-445. doi:10.1503/cmaj.150124.
11. McCrory PR, Bladin PF, Berkovic SF. Retrospective study of concussive convulsions in elite Australian rules and rugby league footballers: phenomenology, aetiology, and outcome. BMJ. 1997;314(7075):171-174.
12. Webb JL, Long B. Seizure mimics: pearls and pitfalls. emDocs Web site. http://www.emdocs.net/seizure-mimics-pearls-pitfalls/. Accessed May 15, 2018.
13. Chen DK, LaFrance WC Jr. Diagnosis and treatment of nonepileptic seizures. Continuum (Mineapp Minn). 2016;22(1):116-131. doi:10.1212/CON.0000000000000282.
14. O’Sullivan SS, Redwood RI, Hunt D, McMahon EM, O’Sullivan S. Recognition of psychogenic non-epileptic seizures: a curable neurophobia? J Neurol Neurosurg Psychiatry. 2013;84(2):228-231. doi:10.1136/jnnp-2012-303062.
15. Clinical policy for the initial approach to patients presenting with a chief complaint of seizure, who are not in status epilepticus. Ann Emerg Med. 1993;22(5):875-883.
16. Reassessment: neuroimaging in the emergency patient presenting with seizure (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;69(18):1772-1780.
17. Montouris GD, Jagoda AS. Management of breakthrough seizures in the emergency department: continuity of patient care. Curr Med Res Opin. 2007;23(7):1583-1592.
Seizures are a common emergency presentation, accounting for approximately 1% of all ED visits.1 Presentations include patients with epilepsy, new-onset or first-time seizure (whether provoked or unprovoked), and other diagnostic entities that can mimic seizure but are not a true epileptic seizure. Even after a detailed and comprehensive evaluation, correctly determining the diagnosis can still be a challenge.2
Seizure Phases
The International League Against Epilepsy (ILAE) defines epileptic seizures as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain.”3 There are typically three phases of a seizure—the aural, ictal, and postictal states.
Aural Phase. Patients may or may not experience an aura prior to seizure onset. An aura can manifest as a sense of déjà vu or a rising sensation in the abdomen, abnormal taste or smell, or autonomic changes. These are not warning signs of a seizure but rather an early manifestation of a focal seizure before there has been enough electrical spread to cause cognitive or motor symptoms.
Ictal Phase. The second stage of seizure, the ictal phase, is the typical cognitive or motor manifestations of seizure activity. Seizures can last several seconds to minutes, but the majority has a duration of less than 1 minute.
Postictal Phase. The postictal period occurs after the active phase of seizure and is characterized by confusion, altered mental status, and somnolence. The postictal period can last from several minutes to hours and can result in suppression of function; including cognitive or motor deficits such as Todd’s paralysis wherein a patient experiences transient paralysis confined to one hemisphere.4
Etiology and Classification
Seizures can be subdivided based on two different categories: etiology or origin of abnormal electrical impulses within the brain. To categorize seizures based on etiology, the clinician must determine whether the seizure was brought on by an identifiable cause.
Provoked Seizure
Provoked seizures are also referred to as acute symptomatic seizures, because they present within 7 days of a systemic insult, whether it be secondary to an electrolyte abnormality (eg, hyponatremia, hypoglycemia, hypercalcemia), substance withdrawal (eg, alcohol, benzodiazepines), toxic ingestion, infection, central nervous system lesions, or head injury. The aforementioned does not represent a comprehensive list, but rather some of the more common etiologies of seizures.2,5
Unprovoked Seizure
An unprovoked seizure occurs without an identifiable acute precipitating insult. These types of seizures are generally more consistent with epilepsy or are due to a remote systemic insult greater than 7 days prior. Examples include patients who have a history of stroke, traumatic brain injury, or congenital brain malformation.2,5
Epilepsy is described as a seizure disorder where recurrent, usually unprovoked seizures occur. Determining the probable etiology of a seizure can be important when pursuing proper objective evaluation and work up, as we will discuss in this article.
Seizure Type
Seizures can also be classified as being generalized or focal, depending on the probable origin of the abnormal electrical discharges within the brain. This classification system is widely used and was developed by the ILAE.6
Generalized Seizures
Generalized seizures have bilateral cortical involvement at the onset of presentation and are associated with loss of consciousness. This is determined through electroencephalogram (EEG) monitoring because focal seizures, where the initiation of abnormal electrical discharges are located in one cortical hemisphere or localized area of the brain, may rapidly spread to both hemispheres and appear very similar to a primary generalized seizure.
Tonic-Clonic Seizures. The most colloquial type of generalized seizure is a tonic-clonic seizure. “Tonic” refers to the muscle stiffness or rigidity that occurs during this type of seizure, and “clonic” describes the rhythmic jerking of these muscles.
Nontonic-Clonic Seizures. Other types of generalized seizures include absence seizures (brief staring episodes or an arrest in behavior), atonic seizures (loss of muscle tone), and myoclonic seizures (brief, sudden muscular contractions).5
Focal Seizures
Focal seizures are diagnosed when the history, clinical presentation, and EEG findings support the localization of abnormal electrical neuronal discharges to one hemisphere of the brain. Loss of consciousness does not always occur during a focal seizure, and the ILAE recently updated the terminology in this regard to this distinction in 2017. Instead of classifying focal seizures as simple partial or complex partial in relation to the preservation of consciousness, the terminology has now changed to focal aware (no loss of consciousness) and focal impaired awareness (affected consciousness). Focal seizures can have not only motor manifestations, but may also present with sensory, autonomic, or psychic symptoms, depending on the anatomic location of the abnormal neuronal activity.5-6
Evaluation in the ED Setting
The classification of a seizure does not often change the ED management of seizures, but it is important to be able to recognize that seizures may present with different clinical appearances. It is also important to remember that not all seizure-like activity is due to epilepsy or abnormal neuronal discharges. There are several other conditions that can present with physical symptoms and characteristics similar to seizure, and are often misdiagnosed as seizures. The next section describes several of these seizure mimics and how to recognize or differentiate them from seizures through a careful history, physical examination, and laboratory evaluation; as one diagnostic tool, the EEG, is not routinely available to the emergency physician (EP).
Seizure Mimics
Syncope
Syncope is secondary to decreased cerebral perfusion, which results in brief loss of consciousness and postural tone, and often with brief convulsions. Myoclonic jerking lasting a few seconds can be seen in many syncopal episodes, and if present is termed convulsive syncope. Following any syncopal episode, patients generally return to their baseline mental status without a postictal period. A prodrome of pallor and sweating can be helpful clues to identify a syncopal episode. In addition, a patient’s eyes may remain open during the event.
There are several types of syncope: cardiac, orthostatic, or neurocardiogenic (vasovagal). History and physical examination can help distinguish syncope from seizure.
Cardiac Syncope. Cardiogenic causes of syncope may be seen in elderly patients who lack a prodrome prior to the event, chest pain may have been present, the event may occur with exercise, or there is evidence of underlying heart disease. An electrocardiogram (ECG) should be done to detect cardiac dysrhythmias. Orthostatic Syncope. Vital signs may be useful in assessing for an orthostatic cause of syncope (drop in systolic blood pressure [BP] by 20 mm Hg or more and drop in diastolic BP by 10 mm Hg or more within 3 minutes of standing), though orthostatic hypotension is common in the elderly.7-8 Dysautonomia as a cause of orthostatic hypotension may show a delayed drop in BP after standing 5 to 10 minutes, in contrast to hypovolemia which tends to be present with immediate standing.Neurocardiogenic Syncope. Neurocardiogenic syncope, a somewhat confusing term, is perhaps better described as a reflex syncope, or simple faint. Often this is referred to as “vasovagal” syncope. Typically, there are physical or psychological noxious stimuli prior to the brief loss of consciousness and postural tone. Pain or strong emotions are common triggers.
Convulsive Concussion
Another seizure mimic is convulsive concussion in which the patient exhibits nonepileptic movement following a closed head injury. It is hypothesized that these post-traumatic convulsions are due to transient functional abnormalities, rather than structural brain injury. In one study, 22 cases of concussive convulsions were identified in which tonic-clonic convulsions began within 2 seconds of impact, and lasted for up to 150 seconds. These patients generally have good outcomes and do not require antiepileptic treatment; they also do not need to abstain from sports or other physical activities.9-11
Movement Disorders
Certain movement disorders can appear similar to seizures with sustained muscle contractions, repetitive movements, dystonias, or even abnormal posturing. However, these abnormal movements are generally painful and there is often impairment of consciousness. They may be genetic in nature or secondary to a neurologic disease or medications such as neuroleptics or antipsychotics.
Psychogenic Nonepileptic Seizures
Psychogenic nonepileptic seizures (PNES) are defined as episodes of altered movements or sensations that appear similar to epileptic seizures, but have an underlying psychological etiology rather than abnormal neuronal discharges. Seventy percent of these patients have a psychiatric illness, such as depression, post-traumatic stress disorder, or personality disorders. Features that can help distinguish PNES from epileptic seizures include long duration, fluctuating symptoms, asynchronous or non-rhythmic movements, pelvic thrusting, side-to-side head or body movements, closed eyes, lack of tongue biting, memory recall, crying, or suppression by distraction. Laboratory testing provides little benefit, aside from a lactate level, which if elevated can suggest a possible epileptic etiology.12 These cases may require consultation with neurology and psychiatry or video-EEG monitoring to correctly diagnose.13-14
Other non-epileptic and possible seizure mimic diagnoses to be considered include stroke, transient ischemic attack, migraine headache, and sleep disorders.
Evaluation
When assessing a patient presenting with seizure-like activity or altered mental status, the clinician must keep a broad differential diagnosis. The first step is to evaluate the ABCs. Once that is completed, a blood glucose should be obtained, as it is a quick test and can determine whether hypoglycemia is the likely cause. Intravenous (IV) access should be obtained and routine labs ordered, including a complete blood count (CBC), a comprehensive metabolic profile (CMP), magnesium, urinalysis, ECG, and lactate. Other labs that may be of clinical utility in certain cases include anticonvulsant levels (in patients that are on these medications), toxicology screens, and cerebrospinal fluid studies, if indicated. It is important to note that anticonvulsant reference ranges are trough values, so levels that are drawn within a few hours of the last dose taken
Patient Disposition
The management and ultimate disposition of a patient with a seizure depends on the underlying cause, and whether the patient has neurologic deficits and/or is back to their baseline mental status. For patients presenting with a first-time seizure and have returned to baseline, the American College of Emergency Physicians’ (ACEP) clinical policy states that precipitating medical conditions should be identified and addressed accordingly if it is a provoked seizure.
If patients present with a first-time unprovoked seizure and do not have evidence of brain injury or neurologic disease (ie, persistent altered mental status or abnormal neurologic examination), then the EP does not need to initiate antiepileptic medications. If there is evidence of neurologic disease or brain injury in an unprovoked seizure, then the EP may either choose to initiate antiepileptic medications or choose to defer, pending consultation with neurology. This group of patients (first-time unprovoked seizure back to baseline) do not need to be admitted to the hospital under the premise that they have a negative workup, to include glucose, CT scan (if indicated), ECG, CBC, and CMP. They must also have normal vital signs, be advised regarding seizure precautions such as not to drive until further medical evaluation (with duration perhaps being set by state law), and have good social support. They will require close follow up for further evaluation and definitive diagnosis, which may include head imaging, if not already performed in the ED, and EEG.
Patients with a history of epilepsy can have recurrent seizures that are either provoked or unprovoked. If the seizure appears clinically similar to their previous seizures, then causes that could lower the seizure threshold should be investigated; including compliance with antiepileptic medications (obtain serum levels), infection (urinalysis and/or chest X-ray), sleep deprivation, electrolyte imbalances, or medications known to lower seizure threshold (eg, certain antibiotics such as fluoroquinolones, antidepressants such as bupropion and venlafaxine, and antipsychotics such as clozapine). These underlying causes should be treated accordingly. If a patient has been noncompliant with their medications, a loading dose can be given in the ED, although there are no definitive studies that either support or debunk this practice. If it is a true, unprovoked seizure and the patient is compliant with their antiepileptic medication, it is reasonable to discuss medication regimen changes with the patient’s neurologist.17A patient that presents with seizure-like activity and does not return back to their baseline mental status requires a more immediate and comprehensive evaluation. Persistent altered mental status has a vast differential diagnosis, and is outside the scope of this article, but if seizures were part of the clinical presentation, the possibility of non-convulsive epilepticus should be considered. These patients may require treatment with medications (usually IV benzodiazepines), admission to the hospital, neurology consultation, EEG, imaging (CT vs MRI), and +/- lumbar puncture depending on the clinical scenario.
Status epilepticus will be further discussed in part 2 of this review.
Seizures are a common emergency presentation, accounting for approximately 1% of all ED visits.1 Presentations include patients with epilepsy, new-onset or first-time seizure (whether provoked or unprovoked), and other diagnostic entities that can mimic seizure but are not a true epileptic seizure. Even after a detailed and comprehensive evaluation, correctly determining the diagnosis can still be a challenge.2
Seizure Phases
The International League Against Epilepsy (ILAE) defines epileptic seizures as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain.”3 There are typically three phases of a seizure—the aural, ictal, and postictal states.
Aural Phase. Patients may or may not experience an aura prior to seizure onset. An aura can manifest as a sense of déjà vu or a rising sensation in the abdomen, abnormal taste or smell, or autonomic changes. These are not warning signs of a seizure but rather an early manifestation of a focal seizure before there has been enough electrical spread to cause cognitive or motor symptoms.
Ictal Phase. The second stage of seizure, the ictal phase, is the typical cognitive or motor manifestations of seizure activity. Seizures can last several seconds to minutes, but the majority has a duration of less than 1 minute.
Postictal Phase. The postictal period occurs after the active phase of seizure and is characterized by confusion, altered mental status, and somnolence. The postictal period can last from several minutes to hours and can result in suppression of function; including cognitive or motor deficits such as Todd’s paralysis wherein a patient experiences transient paralysis confined to one hemisphere.4
Etiology and Classification
Seizures can be subdivided based on two different categories: etiology or origin of abnormal electrical impulses within the brain. To categorize seizures based on etiology, the clinician must determine whether the seizure was brought on by an identifiable cause.
Provoked Seizure
Provoked seizures are also referred to as acute symptomatic seizures, because they present within 7 days of a systemic insult, whether it be secondary to an electrolyte abnormality (eg, hyponatremia, hypoglycemia, hypercalcemia), substance withdrawal (eg, alcohol, benzodiazepines), toxic ingestion, infection, central nervous system lesions, or head injury. The aforementioned does not represent a comprehensive list, but rather some of the more common etiologies of seizures.2,5
Unprovoked Seizure
An unprovoked seizure occurs without an identifiable acute precipitating insult. These types of seizures are generally more consistent with epilepsy or are due to a remote systemic insult greater than 7 days prior. Examples include patients who have a history of stroke, traumatic brain injury, or congenital brain malformation.2,5
Epilepsy is described as a seizure disorder where recurrent, usually unprovoked seizures occur. Determining the probable etiology of a seizure can be important when pursuing proper objective evaluation and work up, as we will discuss in this article.
Seizure Type
Seizures can also be classified as being generalized or focal, depending on the probable origin of the abnormal electrical discharges within the brain. This classification system is widely used and was developed by the ILAE.6
Generalized Seizures
Generalized seizures have bilateral cortical involvement at the onset of presentation and are associated with loss of consciousness. This is determined through electroencephalogram (EEG) monitoring because focal seizures, where the initiation of abnormal electrical discharges are located in one cortical hemisphere or localized area of the brain, may rapidly spread to both hemispheres and appear very similar to a primary generalized seizure.
Tonic-Clonic Seizures. The most colloquial type of generalized seizure is a tonic-clonic seizure. “Tonic” refers to the muscle stiffness or rigidity that occurs during this type of seizure, and “clonic” describes the rhythmic jerking of these muscles.
Nontonic-Clonic Seizures. Other types of generalized seizures include absence seizures (brief staring episodes or an arrest in behavior), atonic seizures (loss of muscle tone), and myoclonic seizures (brief, sudden muscular contractions).5
Focal Seizures
Focal seizures are diagnosed when the history, clinical presentation, and EEG findings support the localization of abnormal electrical neuronal discharges to one hemisphere of the brain. Loss of consciousness does not always occur during a focal seizure, and the ILAE recently updated the terminology in this regard to this distinction in 2017. Instead of classifying focal seizures as simple partial or complex partial in relation to the preservation of consciousness, the terminology has now changed to focal aware (no loss of consciousness) and focal impaired awareness (affected consciousness). Focal seizures can have not only motor manifestations, but may also present with sensory, autonomic, or psychic symptoms, depending on the anatomic location of the abnormal neuronal activity.5-6
Evaluation in the ED Setting
The classification of a seizure does not often change the ED management of seizures, but it is important to be able to recognize that seizures may present with different clinical appearances. It is also important to remember that not all seizure-like activity is due to epilepsy or abnormal neuronal discharges. There are several other conditions that can present with physical symptoms and characteristics similar to seizure, and are often misdiagnosed as seizures. The next section describes several of these seizure mimics and how to recognize or differentiate them from seizures through a careful history, physical examination, and laboratory evaluation; as one diagnostic tool, the EEG, is not routinely available to the emergency physician (EP).
Seizure Mimics
Syncope
Syncope is secondary to decreased cerebral perfusion, which results in brief loss of consciousness and postural tone, and often with brief convulsions. Myoclonic jerking lasting a few seconds can be seen in many syncopal episodes, and if present is termed convulsive syncope. Following any syncopal episode, patients generally return to their baseline mental status without a postictal period. A prodrome of pallor and sweating can be helpful clues to identify a syncopal episode. In addition, a patient’s eyes may remain open during the event.
There are several types of syncope: cardiac, orthostatic, or neurocardiogenic (vasovagal). History and physical examination can help distinguish syncope from seizure.
Cardiac Syncope. Cardiogenic causes of syncope may be seen in elderly patients who lack a prodrome prior to the event, chest pain may have been present, the event may occur with exercise, or there is evidence of underlying heart disease. An electrocardiogram (ECG) should be done to detect cardiac dysrhythmias. Orthostatic Syncope. Vital signs may be useful in assessing for an orthostatic cause of syncope (drop in systolic blood pressure [BP] by 20 mm Hg or more and drop in diastolic BP by 10 mm Hg or more within 3 minutes of standing), though orthostatic hypotension is common in the elderly.7-8 Dysautonomia as a cause of orthostatic hypotension may show a delayed drop in BP after standing 5 to 10 minutes, in contrast to hypovolemia which tends to be present with immediate standing.Neurocardiogenic Syncope. Neurocardiogenic syncope, a somewhat confusing term, is perhaps better described as a reflex syncope, or simple faint. Often this is referred to as “vasovagal” syncope. Typically, there are physical or psychological noxious stimuli prior to the brief loss of consciousness and postural tone. Pain or strong emotions are common triggers.
Convulsive Concussion
Another seizure mimic is convulsive concussion in which the patient exhibits nonepileptic movement following a closed head injury. It is hypothesized that these post-traumatic convulsions are due to transient functional abnormalities, rather than structural brain injury. In one study, 22 cases of concussive convulsions were identified in which tonic-clonic convulsions began within 2 seconds of impact, and lasted for up to 150 seconds. These patients generally have good outcomes and do not require antiepileptic treatment; they also do not need to abstain from sports or other physical activities.9-11
Movement Disorders
Certain movement disorders can appear similar to seizures with sustained muscle contractions, repetitive movements, dystonias, or even abnormal posturing. However, these abnormal movements are generally painful and there is often impairment of consciousness. They may be genetic in nature or secondary to a neurologic disease or medications such as neuroleptics or antipsychotics.
Psychogenic Nonepileptic Seizures
Psychogenic nonepileptic seizures (PNES) are defined as episodes of altered movements or sensations that appear similar to epileptic seizures, but have an underlying psychological etiology rather than abnormal neuronal discharges. Seventy percent of these patients have a psychiatric illness, such as depression, post-traumatic stress disorder, or personality disorders. Features that can help distinguish PNES from epileptic seizures include long duration, fluctuating symptoms, asynchronous or non-rhythmic movements, pelvic thrusting, side-to-side head or body movements, closed eyes, lack of tongue biting, memory recall, crying, or suppression by distraction. Laboratory testing provides little benefit, aside from a lactate level, which if elevated can suggest a possible epileptic etiology.12 These cases may require consultation with neurology and psychiatry or video-EEG monitoring to correctly diagnose.13-14
Other non-epileptic and possible seizure mimic diagnoses to be considered include stroke, transient ischemic attack, migraine headache, and sleep disorders.
Evaluation
When assessing a patient presenting with seizure-like activity or altered mental status, the clinician must keep a broad differential diagnosis. The first step is to evaluate the ABCs. Once that is completed, a blood glucose should be obtained, as it is a quick test and can determine whether hypoglycemia is the likely cause. Intravenous (IV) access should be obtained and routine labs ordered, including a complete blood count (CBC), a comprehensive metabolic profile (CMP), magnesium, urinalysis, ECG, and lactate. Other labs that may be of clinical utility in certain cases include anticonvulsant levels (in patients that are on these medications), toxicology screens, and cerebrospinal fluid studies, if indicated. It is important to note that anticonvulsant reference ranges are trough values, so levels that are drawn within a few hours of the last dose taken
Patient Disposition
The management and ultimate disposition of a patient with a seizure depends on the underlying cause, and whether the patient has neurologic deficits and/or is back to their baseline mental status. For patients presenting with a first-time seizure and have returned to baseline, the American College of Emergency Physicians’ (ACEP) clinical policy states that precipitating medical conditions should be identified and addressed accordingly if it is a provoked seizure.
If patients present with a first-time unprovoked seizure and do not have evidence of brain injury or neurologic disease (ie, persistent altered mental status or abnormal neurologic examination), then the EP does not need to initiate antiepileptic medications. If there is evidence of neurologic disease or brain injury in an unprovoked seizure, then the EP may either choose to initiate antiepileptic medications or choose to defer, pending consultation with neurology. This group of patients (first-time unprovoked seizure back to baseline) do not need to be admitted to the hospital under the premise that they have a negative workup, to include glucose, CT scan (if indicated), ECG, CBC, and CMP. They must also have normal vital signs, be advised regarding seizure precautions such as not to drive until further medical evaluation (with duration perhaps being set by state law), and have good social support. They will require close follow up for further evaluation and definitive diagnosis, which may include head imaging, if not already performed in the ED, and EEG.
Patients with a history of epilepsy can have recurrent seizures that are either provoked or unprovoked. If the seizure appears clinically similar to their previous seizures, then causes that could lower the seizure threshold should be investigated; including compliance with antiepileptic medications (obtain serum levels), infection (urinalysis and/or chest X-ray), sleep deprivation, electrolyte imbalances, or medications known to lower seizure threshold (eg, certain antibiotics such as fluoroquinolones, antidepressants such as bupropion and venlafaxine, and antipsychotics such as clozapine). These underlying causes should be treated accordingly. If a patient has been noncompliant with their medications, a loading dose can be given in the ED, although there are no definitive studies that either support or debunk this practice. If it is a true, unprovoked seizure and the patient is compliant with their antiepileptic medication, it is reasonable to discuss medication regimen changes with the patient’s neurologist.17A patient that presents with seizure-like activity and does not return back to their baseline mental status requires a more immediate and comprehensive evaluation. Persistent altered mental status has a vast differential diagnosis, and is outside the scope of this article, but if seizures were part of the clinical presentation, the possibility of non-convulsive epilepticus should be considered. These patients may require treatment with medications (usually IV benzodiazepines), admission to the hospital, neurology consultation, EEG, imaging (CT vs MRI), and +/- lumbar puncture depending on the clinical scenario.
Status epilepticus will be further discussed in part 2 of this review.
1. Pallin DJ, Goldstein JN, Moussally JS, Pelletier AJ, Green AR, Carmargo CA Jr. Seizure visits in the US emergency departments: epidemiology and potential disparities in care. Int J Emerg Med. 2008;1(2):97-105.
2. Huff JS, Melnick ER, Tomaszewski CA, Thiessen ME, Jagoda AS, Fesmire FM; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with seizures. Ann Emerg Med. 2014;63(4):437-447.e15. doi:10.1016/j.annemergmed.2014.01.018.
3. Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470-472.
4. Webb J, Long B, Koyfman A. An emergency medicine-focused review of seizure mimics. J Emerg Med. 2017;52(5):645-653. doi:10.1016/j.jemermed.2016.11.002.
5. Huff JS, Fountain NB. Pathophysiology and definitions of seizures and status epilepticus. Emerg Med Clin North Am. 2011;29(1):1-13. doi:10.1016/j.emc.2010.08.001.
6. Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):522-530. doi:10.1111/epi.13670.
7. Kanjwal K, Karabin B, Kanjwal Y, Grubb BP. Differentiation of convulsive syncope from epilepsy with an implantable loop recorder. Int J Med Sci. 2009;6(6):296-300.
8. Ozkara C, Metin B, Kucukoglu S. Convulsive syncope: a condition to be differentiated from epilepsy. Epileptic Disord. 2009;11(4):315-319. doi:10.1684/epd.2009.0281.
9. McCrory PR, Berkovic SF. Concussive convulsions. Incidence in sport and treatment recommendations. Sports Med. 1998;25(2);131-136.
10. Ellis MJ, Wennberg R. Convulsions in a 17-year-old boy after a head injury sustained while playing hockey. CMAJ. 2016;188(6):443-445. doi:10.1503/cmaj.150124.
11. McCrory PR, Bladin PF, Berkovic SF. Retrospective study of concussive convulsions in elite Australian rules and rugby league footballers: phenomenology, aetiology, and outcome. BMJ. 1997;314(7075):171-174.
12. Webb JL, Long B. Seizure mimics: pearls and pitfalls. emDocs Web site. http://www.emdocs.net/seizure-mimics-pearls-pitfalls/. Accessed May 15, 2018.
13. Chen DK, LaFrance WC Jr. Diagnosis and treatment of nonepileptic seizures. Continuum (Mineapp Minn). 2016;22(1):116-131. doi:10.1212/CON.0000000000000282.
14. O’Sullivan SS, Redwood RI, Hunt D, McMahon EM, O’Sullivan S. Recognition of psychogenic non-epileptic seizures: a curable neurophobia? J Neurol Neurosurg Psychiatry. 2013;84(2):228-231. doi:10.1136/jnnp-2012-303062.
15. Clinical policy for the initial approach to patients presenting with a chief complaint of seizure, who are not in status epilepticus. Ann Emerg Med. 1993;22(5):875-883.
16. Reassessment: neuroimaging in the emergency patient presenting with seizure (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;69(18):1772-1780.
17. Montouris GD, Jagoda AS. Management of breakthrough seizures in the emergency department: continuity of patient care. Curr Med Res Opin. 2007;23(7):1583-1592.
1. Pallin DJ, Goldstein JN, Moussally JS, Pelletier AJ, Green AR, Carmargo CA Jr. Seizure visits in the US emergency departments: epidemiology and potential disparities in care. Int J Emerg Med. 2008;1(2):97-105.
2. Huff JS, Melnick ER, Tomaszewski CA, Thiessen ME, Jagoda AS, Fesmire FM; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with seizures. Ann Emerg Med. 2014;63(4):437-447.e15. doi:10.1016/j.annemergmed.2014.01.018.
3. Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470-472.
4. Webb J, Long B, Koyfman A. An emergency medicine-focused review of seizure mimics. J Emerg Med. 2017;52(5):645-653. doi:10.1016/j.jemermed.2016.11.002.
5. Huff JS, Fountain NB. Pathophysiology and definitions of seizures and status epilepticus. Emerg Med Clin North Am. 2011;29(1):1-13. doi:10.1016/j.emc.2010.08.001.
6. Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):522-530. doi:10.1111/epi.13670.
7. Kanjwal K, Karabin B, Kanjwal Y, Grubb BP. Differentiation of convulsive syncope from epilepsy with an implantable loop recorder. Int J Med Sci. 2009;6(6):296-300.
8. Ozkara C, Metin B, Kucukoglu S. Convulsive syncope: a condition to be differentiated from epilepsy. Epileptic Disord. 2009;11(4):315-319. doi:10.1684/epd.2009.0281.
9. McCrory PR, Berkovic SF. Concussive convulsions. Incidence in sport and treatment recommendations. Sports Med. 1998;25(2);131-136.
10. Ellis MJ, Wennberg R. Convulsions in a 17-year-old boy after a head injury sustained while playing hockey. CMAJ. 2016;188(6):443-445. doi:10.1503/cmaj.150124.
11. McCrory PR, Bladin PF, Berkovic SF. Retrospective study of concussive convulsions in elite Australian rules and rugby league footballers: phenomenology, aetiology, and outcome. BMJ. 1997;314(7075):171-174.
12. Webb JL, Long B. Seizure mimics: pearls and pitfalls. emDocs Web site. http://www.emdocs.net/seizure-mimics-pearls-pitfalls/. Accessed May 15, 2018.
13. Chen DK, LaFrance WC Jr. Diagnosis and treatment of nonepileptic seizures. Continuum (Mineapp Minn). 2016;22(1):116-131. doi:10.1212/CON.0000000000000282.
14. O’Sullivan SS, Redwood RI, Hunt D, McMahon EM, O’Sullivan S. Recognition of psychogenic non-epileptic seizures: a curable neurophobia? J Neurol Neurosurg Psychiatry. 2013;84(2):228-231. doi:10.1136/jnnp-2012-303062.
15. Clinical policy for the initial approach to patients presenting with a chief complaint of seizure, who are not in status epilepticus. Ann Emerg Med. 1993;22(5):875-883.
16. Reassessment: neuroimaging in the emergency patient presenting with seizure (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;69(18):1772-1780.
17. Montouris GD, Jagoda AS. Management of breakthrough seizures in the emergency department: continuity of patient care. Curr Med Res Opin. 2007;23(7):1583-1592.