User login
Predictors of Recurrent Readmissions
Hospital readmissions are recognized as both a significant contributor to health care costs and a putative indicator of healthcare quality.1, 2 Older medical patients with chronic medical comorbidities are at particularly high risk for hospital readmission3 and attendant risks of hospitalization.4 Many intervention strategies have been used in trials to reduce readmissions in such patients. Single interventions such as case management,5 care coordination,6 and self‐management7 have been disappointing. There is emerging evidence to support complex, multidisciplinary interventions which include outreach and support in the early post‐hospital period, especially in heart failure patients,8 but also in medical patients with a range of conditions.9 However, such interventions are resource intensive and it remains uncertain which patients may benefit most from interventions.
Although there are many studies of risk factors for hospital admission and readmission, few studies have reported predictors of recurrent readmission.1012 Patients with 2 or more recent hospitalizations are readily identifiable and have a substantially increased risk of hospital readmission compared to patients with only 1 recent hospitalization.10, 11, 1315 These patients may have a unique risk factor profile, and may be a group which may particularly benefit from complex interventions,16 but no previous study has specifically examined risk factors in this high‐risk group.
Previous studies of readmission predictors have largely focussed on demographic and disease characteristics which are not amenable to intervention at individual level. The results of such studies may determine a population at increased risk, but do not inform an intervention strategy.14 Psychological and behavioral factors such as depression and anxiety, perceptions of health, and adherence patterns may also contribute to hospitalizations.17, 18 However, the role of these factors in repeated admissions of medical patients has been poorly studied.
The aim of this study was to describe the association of a wider range of biological, functional, and psychosocial variables with the risk of unplanned hospital readmission within 6 months in medical patients with 2 or more recent hospitalizations. There was a particular emphasis on risk factors which might be amenable to intervention.
Methods
Setting and Participants
The study was a prospective longitudinal cohort study. Participant enrolment was undertaken from February 2006 to February 2007. The study setting was the Internal Medicine Department of a tertiary teaching hospital in Brisbane, Australia. The Internal Medicine Department admits approximately 5000 inpatients per annum; more than 95% of these are unplanned admissions (general practitioner referral or self‐referral) via the Emergency Department. Acute and some subacute care are provided by 1 of 5 medical units, each staffed by 2 to 3 consultant general physicians, 2 medical residents (post‐graduate year 3‐4), 2 interns (post‐graduate year 1), and a consistent multidisciplinary team of allied health professionals and senior nursing staff. Descriptions of the inpatient case‐mix and model of care have been published previously.19
Participants were identified by 2 trained research nurses. Daily reports were generated from the hospital admission database to identify all consecutive patients admitted to any general medical unit who had already been hospitalized at the study hospital within the previous six months. The medical record was then screened for eligibility.
Patients were considered for inclusion if they were aged 50 years or older, based on clinical consensus that different factors may be relevant in younger patients, and the demonstrated validity of the selected tools in an older medical population. For logistic reasons, patients were ineligible if they lived outside the greater Brisbane area; came from residential care; had significant language or cognitive difficulties which would preclude participation in interviews; were admitted for end‐of‐life care; or were considered otherwise unsuitable for post‐hospital interviews (eg, no fixed address). Eligible patients were invited to participate in the study. Informed consent was obtained from all participants. The study was approved by the Royal Brisbane and Women's Hospitals and University of Queensland Human Research Ethics Committees.
Outcome and Variables
The primary outcome was 1 or more unplanned readmission to any ward at the study hospital within 6 months of the date of hospital discharge. Information about the frequency and duration of planned and unplanned hospital readmissions in the 6 months after discharge was obtained from the hospital admissions database. Planned readmissions included elective surgical or procedural admissions and scheduled day‐case admissions. Unplanned readmissions included all presentations through the emergency department, except for brief emergency department attendances where the participant was not formally admitted under a consultant.
Information was abstracted from the medical record at the time of discharge using a structured audit tool, including age, sex, primary diagnosis according to the treating clinical team, Charlson comorbidity score, number of medications at discharge, living situation at time of discharge, and the number of hospitalizations in the previous 12 months. Note was made of whether a discharge summary was completed and faxed to the general practitioner within 24 hours of discharge. Weight and height were measured by the research assistant to calculate the body mass index (BMI) which was categorized according to World Health Organization recommended cut‐offs.
Within 5 days of discharge from the index admission, the participant was contacted by telephone to schedule an interview at home within the next week. Posthospital interviews were undertaken using a structured interview tool composed of validated measures of the variables of interest, as described below. Interviews took 45 to 90 minutes to complete, and were performed by one of eight postgraduate clinical psychology students from the University of Queensland, who received training and regular supervision by a senior academic psychologist (NP).
Cognitive status was tested using the 3MS cognitive screening test, a sensitive test for early cognitive impairment.20 The Cambridge Contextual Reading Test (CCRT, short version) was used as a measure of literacy and verbal intelligence, as it may be robust in the presence of early cognitive decline21 Mood disturbances were evaluated using the Geriatric Depression Scale (GDS, short version)22 and the Geriatric Anxiety Inventory (GAI).23 The Social Support Questionnaire short form (SSQ6) was used to identify satisfaction with supports.24 Self‐rated health and income adequacy were rated using a 5 point Likert scale. Compliance with prescribed medication was assessed using the Medication Adherence Rating Scale (MARS) (R Horne, personal communication). Alcohol consumption was evaluated using the alcohol use disorders identification tool (AUDIT).25 Instrumental activities of daily living (IADL: using the telephone, using transport, shopping, housework, meal preparation, medication management, managing money) and basic activities of daily living (BADL: bathing, dressing, eating, mobility, transfers, grooming) were assessed using items from the Older Americans Resources and Services (OARS) questionnaire.26 Relevant permissions were obtained from the developers.
Analysis
Data were analyzed using SPSS 17.0. The distribution of each explanatory and confounding variable was examined and summarized using appropriate statistics (mean, median or proportion). Ordinal and some continuous variables were grouped into categories according to previously validated cut‐offs and clinical meaning. Logarithmic transformation was used in analyses of length of stay due to the highly skewed distribution. ADL and IADL function were grouped into independent in all activities, dependent in IADL function only, and dependent in basic ADL function. Bivariate analysis was undertaken using contingency tables and chi‐square testing for categorical variables and independent samples t‐test or equivalent nonparametric testing for continuous variables, to identify potential associations with the primary outcome.
Dealing with diagnosis posed particular difficulties because of the large number of disease categories. Other authors have restricted the sample to a limited number of diagnoses,27, 28 explored the impact of a limited number of diagnoses compared to all others,13 or grouped diagnoses in a pre‐specified or post hoc manner.3, 15 Considering previous studies and preliminary examination of the data (Table 3), we grouped diagnoses as chronic (heart failure, chronic lung disease, diabetes) vs. other for analysis purposes.
| Follow‐Up Data (n = 142) | No Follow‐Up Data (n = 48) | P | |
|---|---|---|---|
| |||
| Age, years, mean (SD) | 74.0 (10.9) | 76.8 (10.1) | 0.13 |
| Male, % | 52.8 | 56.3 | 0.68 |
| Admissions past 12 months, median (IQR) | 2 (1, 2.25) | 1 (1,2) | 0.38 |
| Comorbidity score, median (IQR) | 2 (1,4) | 2 (1,3) | 0.48 |
| Medications on discharge, mean (SD) | 8.8 (4.0) | 9.0 (4.5) | 0.86 |
| Length of stay, median (IQR) | 6.5 (4,11) | 7 (4,14) | 0.35 |
| Discharged to | 0.30 | ||
| Independent living alone | 38.7 | 47.9 | |
| Independent living with others | 54.2 | 50.0 | |
| Assisted living/residential care | 7.1 | 2.1 | |
| Community services on discharge, % | 42.3 | 56.3 | 0.16 |
| Number (%) with characteristic | % Readmitted | P | |
|---|---|---|---|
| |||
| Age (years) | 0.78 | ||
| <65 | 31 (22) | 39 | |
| 6584.9 | 92 (65) | 40 | |
| 85 or more | 19 (13) | 32 | |
| Male | 75 (53) | 40 | 0.74 |
| Admissions past 12 months | 0.78 | ||
| 1 | 67 (47) | 39 | |
| 2 | 40 (28) | 35 | |
| 3 or more | 35 (25) | 43 | |
| Body mass index | 0.02 | ||
| Underweight | 11 (8) | 72 | |
| Normal | 55 (39) | 27 | |
| Overweight | 43 (30) | 37 | |
| Obese | 32 (23) | 50 | |
| Chronic disease diagnosis | 27 (19) | 67 | 0.001 |
| Functional dependence | 0.16 | ||
| Independent | 27 (19) | 26 | |
| Dependent in IADLs | 48 (34) | 48 | |
| Dependent in BADLs | 66 (47) | 36 | |
| Comorbidity score | 0.15 | ||
| 0 | 19 (13) | 26 | |
| 12 | 62 (44) | 34 | |
| 3 or more | 61 (43) | 48 | |
| Summary sent within 24 hours | 117 (82) | 40 | 0.93 |
| Discharge supports | 0.60 | ||
| community | 72 (51) | 35 | |
| community with supports | 60 (42) | 43 | |
| residential care | 10 (7) | 40 | |
| Poor cognition (3MS 85)* | 80 (58) | 36 | 0.68 |
| Reduced literacy (CCRT<21) | 61 (48) | 41 | 0.55 |
| Depressive symptoms (GDS 5) | 72 (51) | 47 | 0.04 |
| Anxiety symptoms (GAI 9) | 45 (32) | 38 | 0.93 |
| Poor adherence (MARS <24) | 48 (34) | 35 | 0.56 |
| Hazardous drinking (AUDIT >6) | 18 (13) | 39 | 0.98 |
| English as second language | 19 (13) | 32 | 0.50 |
| Self‐rated health fair or poor | 102 (72) | 38 | 0.68 |
| Financial hardship | 46 (32) | 35 | 0.47 |
| Total | 142 | 39 | |
| Diagnosis | Number with diagnosis (%) | % readmitted |
|---|---|---|
| Heart failure | 13 (9) | 69 |
| Diabetes | 6 (4) | 67 |
| Chronic lung disease | 8 (6) | 63 |
| Cellulitis | 8 (6) | 63 |
| Syncope/arrhythmia | 11 (8) | 46 |
| Pneumonia | 10 (7) | 40 |
| Urinary infection | 15 (11) | 33 |
| Fall or fracture | 18 (13) | 33 |
| Gastrointestinal disease | 7 (5) | 29 |
| Ischemic heart disease | 11 (8) | 18 |
| Neurological disease | 7 (5) | 0 |
| Other | 28 (20) | 29 |
| Total | 142 (100) | 39 |
Potentially important variables were chosen based on bivariate analysis (P < 0.2) and previous literature. These variables were then entered into a multiple logistic regression model, and a significant association in the adjusted model was defined as P < 0.05. The performance of the final model was assessed by constructing a receiver operating curve. Given a 40% to 50% anticipated event rate, we estimated that 150 to 200 participants would provide power to include 7 to 10 variables of interest within the model.
Results
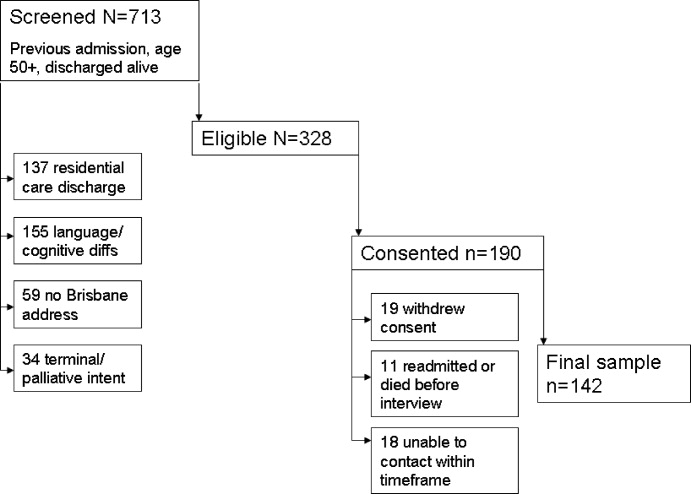
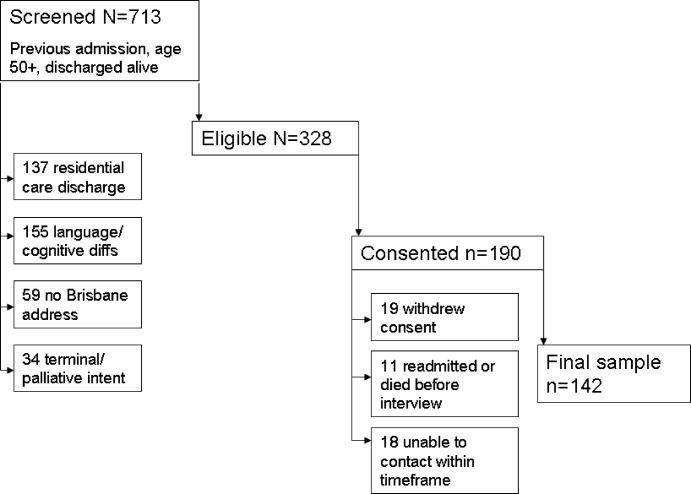
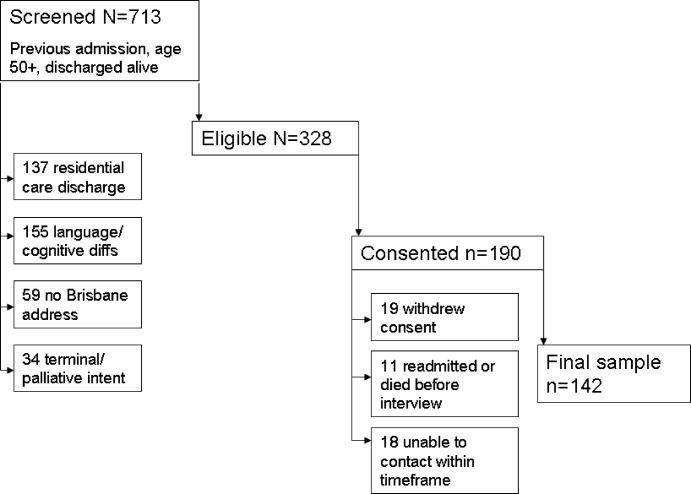
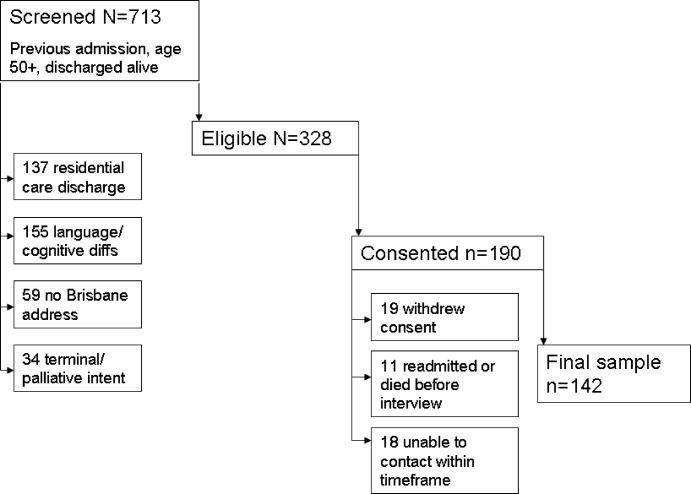
Active screening over 12 months identified 1194 new admissions with a documented hospitalization in the previous 6 months. Of these, 85 were discharged prior to clinical review, 227 were aged less than 50 years, 16 died in hospital, and 153 had been screened previously in the study, leaving 713 individual patients for eligibility screening. Screening identified 328 of 713 (46.0%) patients eligible to participate in the study, who were approached for consent. Of these eligible patients, 190 of 328 (57.9%) agreed to participate but 48 of 190 (25%) did not complete posthospital follow‐up, leaving a total of 142 participants. Patient eligibility, consent, and follow‐up are detailed in Figure 1.
Demographic and disease characteristics of the study participants are shown in Table 1. The 48 participants without follow‐up data appeared similar to those with full data, and 25 (52.1%) of these participants without follow‐up data had an unplanned admission within 6 months.
By 6 months, 55 of 142 participants with follow‐up data (38.7%) had had a total of 102 unplanned admissions to the study hospital. Of these, 42 of 55 (76%) were readmitted to internal medicine. Of the 55 participants with an unplanned readmission, 30 had only 1 unplanned readmission, 9 had 2, and 16 had 3 or more unplanned readmissions within 6 months of the index hospitalization.
During 6 month follow‐up of all 142 participants, there were also 97 planned (scheduled) admissions, 56 (58%) of which occurred in the group with an unplanned admission. Thus the 55 participants with an unplanned readmission accounted for a total of 1055 hospital bed‐days (mean 19.2 days per patient over 6 months follow‐up) while the 87 participants without an unplanned readmission used only 147 bed‐days (mean 1.7 days per patient over 6 months).
Bivariate analysis of the association of unplanned readmissions with the study variables is detailed in Table 2. BMI showed a nonlinear relationship with readmission, with a higher risk apparent at each end of the distribution. Depressive symptoms were also associated with a higher risk of readmission.
Age, sex, number of previous admissions, and discharge supports were not significantly different between the 2 groups. There was no difference in length of the index hospital stay: median length of stay was 6 days (interquartile range [IQR] 3‐14 days) in the readmitted group and 7 (IQR 4‐10 days) in the non‐readmitted group. There was a trend to higher mean number of medications in the readmitted group (9.4 vs. 8.8, P = 0.21).
The strongest predictor of readmission was the presence of a chronic disease diagnosis. Patterns of readmission for each primary clinical diagnosis are shown in Table 3. Chronic comorbidities including heart failure, chronic renal failure, and diabetes were associated with a higher risk of readmission (Table 4). Median comorbidity score was 3 (IQR 1‐5) in the readmitted group compared to 2 (IQR 1‐3) in the nonreadmitted group (P = 0.02).
| Co‐Morbidity | Number with Co‐Morbidity (%) | % Readmitted | P |
|---|---|---|---|
| Heart failure | 30 (21) | 57 | 0.02 |
| Chronic renal impairment | 22 (15) | 59 | 0.03 |
| Diabetes | 36 (25) | 53 | 0.05 |
| Chronic lung disease | 39 (27) | 49 | 0.13 |
| Peripheral vascular disease | 25 (18) | 44 | 0.55 |
| Cerebrovascular disease | 36 (25) | 44 | 0.42 |
| Ischemic heart disease | 57 (40) | 40 | 0.75 |
| Cancer | 23 (16) | 35 | 0.67 |
On the basis of these findings and the literature, a multivariate binary logistic regression model for unplanned admission within 6 months was fitted, including chronic disease diagnosis, comorbiditiy score, BMI, functional status, and GDS as explanatory variables, and adjusting for the potential confounders of age and length of stay (as a severity surrogate). The model is shown in Table 5, and demonstrates a significant association between readmission and chronic conditions, BMI, and depressive symptoms. The area under the receiving operating curve was 0.73.
| Odds Ratio (95% CI) | P Value | |
|---|---|---|
| ||
| Body mass index (reference 18.525) | ||
| Underweight (<18.5) | 12.7 (2.370.7) | 0.004 |
| Overweight (2530) | 1.9 (0.75.1) | 0.18 |
| Obese (>30) | 2.6 (0.97.3) | 0.07 |
| Depressive symptoms (GDS 5) | 3.0 (1.36.8) | 0.01 |
| Chronic disease diagnosis | 3.4 (1.39.3) | 0.02 |
| Co‐morbidity score | 1.3 (1.01.6) | 0.02 |
| Dependency (reference independent) | 0.32 | |
| IADL dependency only | 1.7 (0.55.4) | |
| BADL dependency | 0.9 (0.32.8) | |
| Age group (reference <65 years) | 0.94 | |
| 6584 | 1.1 (0.42.8) | |
| 85 or older | 0.9 (0.23.5) | |
| Log length of stay | 0.99 (0.961.01) | 0.43 |
Discussion
This study demonstrates a number of important findings. First, 39% of this group of participants went on to further unplanned hospital readmissions in the ensuing 6 months, demonstrating the high risk in this group with more than 1 recent hospital admission. However, within this group, the risk of readmission was not related to the frequency of admission within the previous year, consistent with several previous studies.29, 30 These finding suggest that 1 or more recent previous admissions identified at the time of a medical admission is an effective identifier of high risk patients. Subgroup analysis of a recent discharge intervention study in medical patients suggests that this high risk group may particularly benefit from such an intervention.16
Second, the study describes important predictors of readmission which may inform novel interventions. The BMI showed a significant nonlinear relationship with readmission, with an increased risk both above and below the normal weight range. Almost half the group was overweight or obese, with a 2‐fold risk compared to normal weight patients. While underweight was less prevalent, it carried a markedly increased probability of readmission. Limited previous studies support the association of nutritional status and unplanned readmission.31, 32 Malnutrition may be a marker of disease stage or severity, or may be associated with other unmeasured social determinants which increase readmission risk. However, malnutrition itself may reduce physiological resilience and predispose to higher health care needs. There are no published trials of posthospital nutritional intervention programs for reducing readmission rates in general medical patients.
The risk of readmission was also increased in participants with depressive symptoms, consistent with several previous studies.3336 This effect was independent of illness type and comorbidity. Depression is increasingly recognized as an important independent predictor of a range of important outcomes in older medical patients, including posthospital functional decline,37 institutionalization and mortality.36, 38 Posthospital decline and poor self‐management might contribute to higher rehospitalization. There is some evidence that effective treatment of psychological comorbidities in medically ill patients may reduce readmissions.18, 39
Both the number and type of chronic conditions appear to be predictors of readmission in this high risk group, where there was a high baseline prevalence of chronic diseases such as heart failure, diabetes, renal impairment, and chronic lung disease which have been associated with higher readmission rates in a number of previous studies.13, 15, 30, 40 Almost all participants had one or more significant comorbid conditions in addition to their presenting complaint; single disease‐focused chronic disease management programs may not be an optimal solution in this group. Consistent with this comorbidity burden, most participants were prescribed a large number of medications. In keeping with other studies,17 about one‐third of participants reported reduced medication adherence but this was not associated with a higher readmission risk.
Like most previous studies in medical patients,10, 11, 15, 29, 30, 35, 36, 40, 41 there was no evidence of increasing readmission rates with age. Functional status impairment was not a significant predictor of readmission, probably reflecting selection of a patient subgroup with a high prevalence of disability and chronic disease. Satisfaction with social support was generally high, and not associated with readmission. This may reflect the emphasis on discharge planning and postacute social and functional support already occurring in usual care.
Measures of cognition and literacy were not associated with readmission. However, these were the items with the most missing data (see Table 2), which may have reduced our ability to detect an association. The study design excluded patients with significant cognitive or communication deficits who were unable to participate in detailed assessments. Such stringent eligibility criteria may be seen as a weakness of this study, reducing the generalizability of the findings. However, the study deliberately sampled a population of older adults suitable for a multifacetted posthospital management program, in order to inform specific intervention targets, and the eligibility criteria reflect these practical considerations. Although some previous studies have found that cognitive impairment is a predictor of readmission,10, 12 others have found no association.29, 30, 36, 40, 41
The main study weaknesses are the small sample size (reflected in the wide confidence intervals [CIs] in the multivariate analysis), and the relatively high rate of drop‐outs (25% of enrolments) for whom detailed posthospital data could not be collected. This problem reflects the age and burden of illness in the population under study. Readmission data were collected for all participants, and a similar rate of readmission was observed in patients with missing data (52% vs. 39%, P = 0.11). The heterogeneous patients mix may have concealed some important associations within individual diagnoses or other patient subgroups. This heterogeneity reflects the reality of the selected high risk subgroup, and the study deliberately avoided a disease‐specific focus for generalizability.
Conclusions
This study confirms the high rate of hospital readmission in medical patients who have already had a previous inpatient admission in the past 6 months. It shifts the emphasis from nonmodifiable disease and demographic predictors to consideration of common, nondisease specific factors which might have a plausible causative relationship with readmission and may be amenable to specific interventions. The population sampled had a high prevalence of chronic disease, and often multiple diseases. Nutritional status and depressive symptoms are emerging as important modifiers of disease course and mortality in the setting of several chronic diseases; this study also supports their potential contribution to increased hospital resource consumption in a high‐risk group. Posthospital programs which specifically address these factors in the context of optimal medical management of underlying chronic diseases have the potential to reduce hospital readmissions.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,.Clinical and sociodemographic risk factors for reamdission of Medicare benficiaries.Health Care Financ Rev.1988;10(1):27–36.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118:219–223.
- ,,,,.A case manager intervention to reduce readmissions.Arch Intern Med.1995;154(15):1721–1729.
- ,,, et al.A transitional care service for elderly chronic disease patients at risk of readmission.Aust Health Rev.2004;28(3):275–284.
- ,,,,.Self‐management programmes by lay leaders for people with chronic conditions.Cochrane Database Syst Rev.2007(4):Art No.CD005108.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,, et al.Discharge planning from hospital to home.Cochrane Database Syst Rev.2010(Issue 1):Art No.CD000313.
- ,,, et al.Characteristics of geriatric patients related to early and late readmissions to hospital.Aging Clin Exp Res.1998;10:339–346.
- ,,, et al.Hospital readmission among older medical patietns in Hong Kong.J R Coll Physicians Lond.1999;33(2):153–156.
- ,,, et al.Early re‐hospitalization of elderly people discharged from a geriatric ward.Aging Clin Exp Res.2006;18(1):63–69.
- ,,,,.Readmission patterns in patients with chronic obstructive pulmonary disease, chronic heart failure and diabetes mellitus: an administrative dataset analysis.Intern Med J.2005;35:296–299.
- ,,,.Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients.BMJ.2006;333:327–330.
- ,,,.Predicting emergency readmission for patients discharged from the medical service of a teaching hospital.J Gen Intern Med.1987;2:400–405.
- ,,, et al.A reengineered hospital discharge program to decrease hospitalization.Ann Intern Med.2009;150:178–187.
- ,,.The role of medication noncompliance and adverse drug reactions in hospitalisations in the elderly.Arch Intern Med.1990;150:841–845.
- ,,, et al.UPBEAT: the impact of a psychogeriatric intervention in VA medical centers.Med Care.2001;39(5):500–512.
- ,,,.Controlled trial of multidisciplinary care teams for acutely ill medical inpatients: enhanced multidisciplinary care.Intern Med J.2006;36:558–563.
- ,.The modified mini‐mental state (3MS) examination.J Clin Psychiatry.1987;48:314–318.
- .Development of the Cambridge Contextual Reading Test for improving the examination of premorbid verbal intelligence in older persons with dementia.Br J Clin Psychol.1998;37:229–240.
- ,.Geriatric Depression Scale (GDS): recent evidence and development of a shorter version.Clinics in Gerontology.1986;5:165–172.
- ,,,,,.Development and validation of the Geriatric Anxiety Inventory.Int Psychogeriatr.2007;19(1):103–114.
- ,,.A brief measure of social support: practical and theoretical implications.J Soc Pers Relat.1987;4:497–510.
- ,,,,.Screening for problem drinking: comparison of the CAGE and AUDIT.J Gen Intern Med.1998;13(6):379–388.
- ,.OARS methodology: a decade of experience in geriatric assessment.J Am Geriatr Soc.1985;33:607–615.
- ,.Hospital readmissions among the elderly.J Am Geriatr Soc.1985;33:595–601.
- ,,,,,.Discharge destination and repeat hospitalizations.Med Care.1997;35:756–767.
- ,,, et al.Measuring frailty in the hospitalized elderly. Concept of functional homeostasis.Am J Phys Med Rehab.1998;77(3):252–257.
- ,.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6(5):389–393.
- .Risk factors for early hospital readmission in a select population of geriatric rehabilitation patients: the significance of functional status.J Am Geriatr Soc.1992;40:792–798.
- ,,,.Predicting early nonelective hospital readmission in nutritionally compromised older adults.Am J Clin Nutr.1997;65:1714–1720.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107(1):13–17.
- ,,,.Depression and activities of daily living predict rehospitalisation within 6 months of discharge from geriatric rehabilitation.Rehabil Psychol.2004;49(3):219–223.
- ,,,.Depressive symptoms and negative outcomes in older hospitalized patients.Arch Intern Med.2002;162:948–949.
- ,,,.Depressive symptoms as a predictor of 6‐month outcomes and services utilization in elderly medical inpatients.Arch Intern Med.2001;161:2609–2615.
- ,,,,.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126(6):417–425.
- ,,,.Diabetes, depression and death. A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT).Diabetes Care.2007;30(12):3005–3010.
- ,,.Clinical implications of a reduction in psychosocial distress in cardiac prognosis in patients participating in a psychosocial intervention programme.Psychosom Med.2001;63(2):257–266.
- ,,, et al.Predictors of immediate and 6‐month outcomes in hospitalized elderly patients.J Am Geriatr Soc.1988;36:775–783.
- ,,,,.Factors predictive of outcome on admission to an acute geriatric ward.Age Ageing.1999;28:429–432.
Hospital readmissions are recognized as both a significant contributor to health care costs and a putative indicator of healthcare quality.1, 2 Older medical patients with chronic medical comorbidities are at particularly high risk for hospital readmission3 and attendant risks of hospitalization.4 Many intervention strategies have been used in trials to reduce readmissions in such patients. Single interventions such as case management,5 care coordination,6 and self‐management7 have been disappointing. There is emerging evidence to support complex, multidisciplinary interventions which include outreach and support in the early post‐hospital period, especially in heart failure patients,8 but also in medical patients with a range of conditions.9 However, such interventions are resource intensive and it remains uncertain which patients may benefit most from interventions.
Although there are many studies of risk factors for hospital admission and readmission, few studies have reported predictors of recurrent readmission.1012 Patients with 2 or more recent hospitalizations are readily identifiable and have a substantially increased risk of hospital readmission compared to patients with only 1 recent hospitalization.10, 11, 1315 These patients may have a unique risk factor profile, and may be a group which may particularly benefit from complex interventions,16 but no previous study has specifically examined risk factors in this high‐risk group.
Previous studies of readmission predictors have largely focussed on demographic and disease characteristics which are not amenable to intervention at individual level. The results of such studies may determine a population at increased risk, but do not inform an intervention strategy.14 Psychological and behavioral factors such as depression and anxiety, perceptions of health, and adherence patterns may also contribute to hospitalizations.17, 18 However, the role of these factors in repeated admissions of medical patients has been poorly studied.
The aim of this study was to describe the association of a wider range of biological, functional, and psychosocial variables with the risk of unplanned hospital readmission within 6 months in medical patients with 2 or more recent hospitalizations. There was a particular emphasis on risk factors which might be amenable to intervention.
Methods
Setting and Participants
The study was a prospective longitudinal cohort study. Participant enrolment was undertaken from February 2006 to February 2007. The study setting was the Internal Medicine Department of a tertiary teaching hospital in Brisbane, Australia. The Internal Medicine Department admits approximately 5000 inpatients per annum; more than 95% of these are unplanned admissions (general practitioner referral or self‐referral) via the Emergency Department. Acute and some subacute care are provided by 1 of 5 medical units, each staffed by 2 to 3 consultant general physicians, 2 medical residents (post‐graduate year 3‐4), 2 interns (post‐graduate year 1), and a consistent multidisciplinary team of allied health professionals and senior nursing staff. Descriptions of the inpatient case‐mix and model of care have been published previously.19
Participants were identified by 2 trained research nurses. Daily reports were generated from the hospital admission database to identify all consecutive patients admitted to any general medical unit who had already been hospitalized at the study hospital within the previous six months. The medical record was then screened for eligibility.
Patients were considered for inclusion if they were aged 50 years or older, based on clinical consensus that different factors may be relevant in younger patients, and the demonstrated validity of the selected tools in an older medical population. For logistic reasons, patients were ineligible if they lived outside the greater Brisbane area; came from residential care; had significant language or cognitive difficulties which would preclude participation in interviews; were admitted for end‐of‐life care; or were considered otherwise unsuitable for post‐hospital interviews (eg, no fixed address). Eligible patients were invited to participate in the study. Informed consent was obtained from all participants. The study was approved by the Royal Brisbane and Women's Hospitals and University of Queensland Human Research Ethics Committees.
Outcome and Variables
The primary outcome was 1 or more unplanned readmission to any ward at the study hospital within 6 months of the date of hospital discharge. Information about the frequency and duration of planned and unplanned hospital readmissions in the 6 months after discharge was obtained from the hospital admissions database. Planned readmissions included elective surgical or procedural admissions and scheduled day‐case admissions. Unplanned readmissions included all presentations through the emergency department, except for brief emergency department attendances where the participant was not formally admitted under a consultant.
Information was abstracted from the medical record at the time of discharge using a structured audit tool, including age, sex, primary diagnosis according to the treating clinical team, Charlson comorbidity score, number of medications at discharge, living situation at time of discharge, and the number of hospitalizations in the previous 12 months. Note was made of whether a discharge summary was completed and faxed to the general practitioner within 24 hours of discharge. Weight and height were measured by the research assistant to calculate the body mass index (BMI) which was categorized according to World Health Organization recommended cut‐offs.
Within 5 days of discharge from the index admission, the participant was contacted by telephone to schedule an interview at home within the next week. Posthospital interviews were undertaken using a structured interview tool composed of validated measures of the variables of interest, as described below. Interviews took 45 to 90 minutes to complete, and were performed by one of eight postgraduate clinical psychology students from the University of Queensland, who received training and regular supervision by a senior academic psychologist (NP).
Cognitive status was tested using the 3MS cognitive screening test, a sensitive test for early cognitive impairment.20 The Cambridge Contextual Reading Test (CCRT, short version) was used as a measure of literacy and verbal intelligence, as it may be robust in the presence of early cognitive decline21 Mood disturbances were evaluated using the Geriatric Depression Scale (GDS, short version)22 and the Geriatric Anxiety Inventory (GAI).23 The Social Support Questionnaire short form (SSQ6) was used to identify satisfaction with supports.24 Self‐rated health and income adequacy were rated using a 5 point Likert scale. Compliance with prescribed medication was assessed using the Medication Adherence Rating Scale (MARS) (R Horne, personal communication). Alcohol consumption was evaluated using the alcohol use disorders identification tool (AUDIT).25 Instrumental activities of daily living (IADL: using the telephone, using transport, shopping, housework, meal preparation, medication management, managing money) and basic activities of daily living (BADL: bathing, dressing, eating, mobility, transfers, grooming) were assessed using items from the Older Americans Resources and Services (OARS) questionnaire.26 Relevant permissions were obtained from the developers.
Analysis
Data were analyzed using SPSS 17.0. The distribution of each explanatory and confounding variable was examined and summarized using appropriate statistics (mean, median or proportion). Ordinal and some continuous variables were grouped into categories according to previously validated cut‐offs and clinical meaning. Logarithmic transformation was used in analyses of length of stay due to the highly skewed distribution. ADL and IADL function were grouped into independent in all activities, dependent in IADL function only, and dependent in basic ADL function. Bivariate analysis was undertaken using contingency tables and chi‐square testing for categorical variables and independent samples t‐test or equivalent nonparametric testing for continuous variables, to identify potential associations with the primary outcome.
Dealing with diagnosis posed particular difficulties because of the large number of disease categories. Other authors have restricted the sample to a limited number of diagnoses,27, 28 explored the impact of a limited number of diagnoses compared to all others,13 or grouped diagnoses in a pre‐specified or post hoc manner.3, 15 Considering previous studies and preliminary examination of the data (Table 3), we grouped diagnoses as chronic (heart failure, chronic lung disease, diabetes) vs. other for analysis purposes.
| Follow‐Up Data (n = 142) | No Follow‐Up Data (n = 48) | P | |
|---|---|---|---|
| |||
| Age, years, mean (SD) | 74.0 (10.9) | 76.8 (10.1) | 0.13 |
| Male, % | 52.8 | 56.3 | 0.68 |
| Admissions past 12 months, median (IQR) | 2 (1, 2.25) | 1 (1,2) | 0.38 |
| Comorbidity score, median (IQR) | 2 (1,4) | 2 (1,3) | 0.48 |
| Medications on discharge, mean (SD) | 8.8 (4.0) | 9.0 (4.5) | 0.86 |
| Length of stay, median (IQR) | 6.5 (4,11) | 7 (4,14) | 0.35 |
| Discharged to | 0.30 | ||
| Independent living alone | 38.7 | 47.9 | |
| Independent living with others | 54.2 | 50.0 | |
| Assisted living/residential care | 7.1 | 2.1 | |
| Community services on discharge, % | 42.3 | 56.3 | 0.16 |
| Number (%) with characteristic | % Readmitted | P | |
|---|---|---|---|
| |||
| Age (years) | 0.78 | ||
| <65 | 31 (22) | 39 | |
| 6584.9 | 92 (65) | 40 | |
| 85 or more | 19 (13) | 32 | |
| Male | 75 (53) | 40 | 0.74 |
| Admissions past 12 months | 0.78 | ||
| 1 | 67 (47) | 39 | |
| 2 | 40 (28) | 35 | |
| 3 or more | 35 (25) | 43 | |
| Body mass index | 0.02 | ||
| Underweight | 11 (8) | 72 | |
| Normal | 55 (39) | 27 | |
| Overweight | 43 (30) | 37 | |
| Obese | 32 (23) | 50 | |
| Chronic disease diagnosis | 27 (19) | 67 | 0.001 |
| Functional dependence | 0.16 | ||
| Independent | 27 (19) | 26 | |
| Dependent in IADLs | 48 (34) | 48 | |
| Dependent in BADLs | 66 (47) | 36 | |
| Comorbidity score | 0.15 | ||
| 0 | 19 (13) | 26 | |
| 12 | 62 (44) | 34 | |
| 3 or more | 61 (43) | 48 | |
| Summary sent within 24 hours | 117 (82) | 40 | 0.93 |
| Discharge supports | 0.60 | ||
| community | 72 (51) | 35 | |
| community with supports | 60 (42) | 43 | |
| residential care | 10 (7) | 40 | |
| Poor cognition (3MS 85)* | 80 (58) | 36 | 0.68 |
| Reduced literacy (CCRT<21) | 61 (48) | 41 | 0.55 |
| Depressive symptoms (GDS 5) | 72 (51) | 47 | 0.04 |
| Anxiety symptoms (GAI 9) | 45 (32) | 38 | 0.93 |
| Poor adherence (MARS <24) | 48 (34) | 35 | 0.56 |
| Hazardous drinking (AUDIT >6) | 18 (13) | 39 | 0.98 |
| English as second language | 19 (13) | 32 | 0.50 |
| Self‐rated health fair or poor | 102 (72) | 38 | 0.68 |
| Financial hardship | 46 (32) | 35 | 0.47 |
| Total | 142 | 39 | |
| Diagnosis | Number with diagnosis (%) | % readmitted |
|---|---|---|
| Heart failure | 13 (9) | 69 |
| Diabetes | 6 (4) | 67 |
| Chronic lung disease | 8 (6) | 63 |
| Cellulitis | 8 (6) | 63 |
| Syncope/arrhythmia | 11 (8) | 46 |
| Pneumonia | 10 (7) | 40 |
| Urinary infection | 15 (11) | 33 |
| Fall or fracture | 18 (13) | 33 |
| Gastrointestinal disease | 7 (5) | 29 |
| Ischemic heart disease | 11 (8) | 18 |
| Neurological disease | 7 (5) | 0 |
| Other | 28 (20) | 29 |
| Total | 142 (100) | 39 |
Potentially important variables were chosen based on bivariate analysis (P < 0.2) and previous literature. These variables were then entered into a multiple logistic regression model, and a significant association in the adjusted model was defined as P < 0.05. The performance of the final model was assessed by constructing a receiver operating curve. Given a 40% to 50% anticipated event rate, we estimated that 150 to 200 participants would provide power to include 7 to 10 variables of interest within the model.
Results
Active screening over 12 months identified 1194 new admissions with a documented hospitalization in the previous 6 months. Of these, 85 were discharged prior to clinical review, 227 were aged less than 50 years, 16 died in hospital, and 153 had been screened previously in the study, leaving 713 individual patients for eligibility screening. Screening identified 328 of 713 (46.0%) patients eligible to participate in the study, who were approached for consent. Of these eligible patients, 190 of 328 (57.9%) agreed to participate but 48 of 190 (25%) did not complete posthospital follow‐up, leaving a total of 142 participants. Patient eligibility, consent, and follow‐up are detailed in Figure 1.
Demographic and disease characteristics of the study participants are shown in Table 1. The 48 participants without follow‐up data appeared similar to those with full data, and 25 (52.1%) of these participants without follow‐up data had an unplanned admission within 6 months.
By 6 months, 55 of 142 participants with follow‐up data (38.7%) had had a total of 102 unplanned admissions to the study hospital. Of these, 42 of 55 (76%) were readmitted to internal medicine. Of the 55 participants with an unplanned readmission, 30 had only 1 unplanned readmission, 9 had 2, and 16 had 3 or more unplanned readmissions within 6 months of the index hospitalization.
During 6 month follow‐up of all 142 participants, there were also 97 planned (scheduled) admissions, 56 (58%) of which occurred in the group with an unplanned admission. Thus the 55 participants with an unplanned readmission accounted for a total of 1055 hospital bed‐days (mean 19.2 days per patient over 6 months follow‐up) while the 87 participants without an unplanned readmission used only 147 bed‐days (mean 1.7 days per patient over 6 months).
Bivariate analysis of the association of unplanned readmissions with the study variables is detailed in Table 2. BMI showed a nonlinear relationship with readmission, with a higher risk apparent at each end of the distribution. Depressive symptoms were also associated with a higher risk of readmission.
Age, sex, number of previous admissions, and discharge supports were not significantly different between the 2 groups. There was no difference in length of the index hospital stay: median length of stay was 6 days (interquartile range [IQR] 3‐14 days) in the readmitted group and 7 (IQR 4‐10 days) in the non‐readmitted group. There was a trend to higher mean number of medications in the readmitted group (9.4 vs. 8.8, P = 0.21).
The strongest predictor of readmission was the presence of a chronic disease diagnosis. Patterns of readmission for each primary clinical diagnosis are shown in Table 3. Chronic comorbidities including heart failure, chronic renal failure, and diabetes were associated with a higher risk of readmission (Table 4). Median comorbidity score was 3 (IQR 1‐5) in the readmitted group compared to 2 (IQR 1‐3) in the nonreadmitted group (P = 0.02).
| Co‐Morbidity | Number with Co‐Morbidity (%) | % Readmitted | P |
|---|---|---|---|
| Heart failure | 30 (21) | 57 | 0.02 |
| Chronic renal impairment | 22 (15) | 59 | 0.03 |
| Diabetes | 36 (25) | 53 | 0.05 |
| Chronic lung disease | 39 (27) | 49 | 0.13 |
| Peripheral vascular disease | 25 (18) | 44 | 0.55 |
| Cerebrovascular disease | 36 (25) | 44 | 0.42 |
| Ischemic heart disease | 57 (40) | 40 | 0.75 |
| Cancer | 23 (16) | 35 | 0.67 |
On the basis of these findings and the literature, a multivariate binary logistic regression model for unplanned admission within 6 months was fitted, including chronic disease diagnosis, comorbiditiy score, BMI, functional status, and GDS as explanatory variables, and adjusting for the potential confounders of age and length of stay (as a severity surrogate). The model is shown in Table 5, and demonstrates a significant association between readmission and chronic conditions, BMI, and depressive symptoms. The area under the receiving operating curve was 0.73.
| Odds Ratio (95% CI) | P Value | |
|---|---|---|
| ||
| Body mass index (reference 18.525) | ||
| Underweight (<18.5) | 12.7 (2.370.7) | 0.004 |
| Overweight (2530) | 1.9 (0.75.1) | 0.18 |
| Obese (>30) | 2.6 (0.97.3) | 0.07 |
| Depressive symptoms (GDS 5) | 3.0 (1.36.8) | 0.01 |
| Chronic disease diagnosis | 3.4 (1.39.3) | 0.02 |
| Co‐morbidity score | 1.3 (1.01.6) | 0.02 |
| Dependency (reference independent) | 0.32 | |
| IADL dependency only | 1.7 (0.55.4) | |
| BADL dependency | 0.9 (0.32.8) | |
| Age group (reference <65 years) | 0.94 | |
| 6584 | 1.1 (0.42.8) | |
| 85 or older | 0.9 (0.23.5) | |
| Log length of stay | 0.99 (0.961.01) | 0.43 |
Discussion
This study demonstrates a number of important findings. First, 39% of this group of participants went on to further unplanned hospital readmissions in the ensuing 6 months, demonstrating the high risk in this group with more than 1 recent hospital admission. However, within this group, the risk of readmission was not related to the frequency of admission within the previous year, consistent with several previous studies.29, 30 These finding suggest that 1 or more recent previous admissions identified at the time of a medical admission is an effective identifier of high risk patients. Subgroup analysis of a recent discharge intervention study in medical patients suggests that this high risk group may particularly benefit from such an intervention.16
Second, the study describes important predictors of readmission which may inform novel interventions. The BMI showed a significant nonlinear relationship with readmission, with an increased risk both above and below the normal weight range. Almost half the group was overweight or obese, with a 2‐fold risk compared to normal weight patients. While underweight was less prevalent, it carried a markedly increased probability of readmission. Limited previous studies support the association of nutritional status and unplanned readmission.31, 32 Malnutrition may be a marker of disease stage or severity, or may be associated with other unmeasured social determinants which increase readmission risk. However, malnutrition itself may reduce physiological resilience and predispose to higher health care needs. There are no published trials of posthospital nutritional intervention programs for reducing readmission rates in general medical patients.
The risk of readmission was also increased in participants with depressive symptoms, consistent with several previous studies.3336 This effect was independent of illness type and comorbidity. Depression is increasingly recognized as an important independent predictor of a range of important outcomes in older medical patients, including posthospital functional decline,37 institutionalization and mortality.36, 38 Posthospital decline and poor self‐management might contribute to higher rehospitalization. There is some evidence that effective treatment of psychological comorbidities in medically ill patients may reduce readmissions.18, 39
Both the number and type of chronic conditions appear to be predictors of readmission in this high risk group, where there was a high baseline prevalence of chronic diseases such as heart failure, diabetes, renal impairment, and chronic lung disease which have been associated with higher readmission rates in a number of previous studies.13, 15, 30, 40 Almost all participants had one or more significant comorbid conditions in addition to their presenting complaint; single disease‐focused chronic disease management programs may not be an optimal solution in this group. Consistent with this comorbidity burden, most participants were prescribed a large number of medications. In keeping with other studies,17 about one‐third of participants reported reduced medication adherence but this was not associated with a higher readmission risk.
Like most previous studies in medical patients,10, 11, 15, 29, 30, 35, 36, 40, 41 there was no evidence of increasing readmission rates with age. Functional status impairment was not a significant predictor of readmission, probably reflecting selection of a patient subgroup with a high prevalence of disability and chronic disease. Satisfaction with social support was generally high, and not associated with readmission. This may reflect the emphasis on discharge planning and postacute social and functional support already occurring in usual care.
Measures of cognition and literacy were not associated with readmission. However, these were the items with the most missing data (see Table 2), which may have reduced our ability to detect an association. The study design excluded patients with significant cognitive or communication deficits who were unable to participate in detailed assessments. Such stringent eligibility criteria may be seen as a weakness of this study, reducing the generalizability of the findings. However, the study deliberately sampled a population of older adults suitable for a multifacetted posthospital management program, in order to inform specific intervention targets, and the eligibility criteria reflect these practical considerations. Although some previous studies have found that cognitive impairment is a predictor of readmission,10, 12 others have found no association.29, 30, 36, 40, 41
The main study weaknesses are the small sample size (reflected in the wide confidence intervals [CIs] in the multivariate analysis), and the relatively high rate of drop‐outs (25% of enrolments) for whom detailed posthospital data could not be collected. This problem reflects the age and burden of illness in the population under study. Readmission data were collected for all participants, and a similar rate of readmission was observed in patients with missing data (52% vs. 39%, P = 0.11). The heterogeneous patients mix may have concealed some important associations within individual diagnoses or other patient subgroups. This heterogeneity reflects the reality of the selected high risk subgroup, and the study deliberately avoided a disease‐specific focus for generalizability.
Conclusions
This study confirms the high rate of hospital readmission in medical patients who have already had a previous inpatient admission in the past 6 months. It shifts the emphasis from nonmodifiable disease and demographic predictors to consideration of common, nondisease specific factors which might have a plausible causative relationship with readmission and may be amenable to specific interventions. The population sampled had a high prevalence of chronic disease, and often multiple diseases. Nutritional status and depressive symptoms are emerging as important modifiers of disease course and mortality in the setting of several chronic diseases; this study also supports their potential contribution to increased hospital resource consumption in a high‐risk group. Posthospital programs which specifically address these factors in the context of optimal medical management of underlying chronic diseases have the potential to reduce hospital readmissions.
Hospital readmissions are recognized as both a significant contributor to health care costs and a putative indicator of healthcare quality.1, 2 Older medical patients with chronic medical comorbidities are at particularly high risk for hospital readmission3 and attendant risks of hospitalization.4 Many intervention strategies have been used in trials to reduce readmissions in such patients. Single interventions such as case management,5 care coordination,6 and self‐management7 have been disappointing. There is emerging evidence to support complex, multidisciplinary interventions which include outreach and support in the early post‐hospital period, especially in heart failure patients,8 but also in medical patients with a range of conditions.9 However, such interventions are resource intensive and it remains uncertain which patients may benefit most from interventions.
Although there are many studies of risk factors for hospital admission and readmission, few studies have reported predictors of recurrent readmission.1012 Patients with 2 or more recent hospitalizations are readily identifiable and have a substantially increased risk of hospital readmission compared to patients with only 1 recent hospitalization.10, 11, 1315 These patients may have a unique risk factor profile, and may be a group which may particularly benefit from complex interventions,16 but no previous study has specifically examined risk factors in this high‐risk group.
Previous studies of readmission predictors have largely focussed on demographic and disease characteristics which are not amenable to intervention at individual level. The results of such studies may determine a population at increased risk, but do not inform an intervention strategy.14 Psychological and behavioral factors such as depression and anxiety, perceptions of health, and adherence patterns may also contribute to hospitalizations.17, 18 However, the role of these factors in repeated admissions of medical patients has been poorly studied.
The aim of this study was to describe the association of a wider range of biological, functional, and psychosocial variables with the risk of unplanned hospital readmission within 6 months in medical patients with 2 or more recent hospitalizations. There was a particular emphasis on risk factors which might be amenable to intervention.
Methods
Setting and Participants
The study was a prospective longitudinal cohort study. Participant enrolment was undertaken from February 2006 to February 2007. The study setting was the Internal Medicine Department of a tertiary teaching hospital in Brisbane, Australia. The Internal Medicine Department admits approximately 5000 inpatients per annum; more than 95% of these are unplanned admissions (general practitioner referral or self‐referral) via the Emergency Department. Acute and some subacute care are provided by 1 of 5 medical units, each staffed by 2 to 3 consultant general physicians, 2 medical residents (post‐graduate year 3‐4), 2 interns (post‐graduate year 1), and a consistent multidisciplinary team of allied health professionals and senior nursing staff. Descriptions of the inpatient case‐mix and model of care have been published previously.19
Participants were identified by 2 trained research nurses. Daily reports were generated from the hospital admission database to identify all consecutive patients admitted to any general medical unit who had already been hospitalized at the study hospital within the previous six months. The medical record was then screened for eligibility.
Patients were considered for inclusion if they were aged 50 years or older, based on clinical consensus that different factors may be relevant in younger patients, and the demonstrated validity of the selected tools in an older medical population. For logistic reasons, patients were ineligible if they lived outside the greater Brisbane area; came from residential care; had significant language or cognitive difficulties which would preclude participation in interviews; were admitted for end‐of‐life care; or were considered otherwise unsuitable for post‐hospital interviews (eg, no fixed address). Eligible patients were invited to participate in the study. Informed consent was obtained from all participants. The study was approved by the Royal Brisbane and Women's Hospitals and University of Queensland Human Research Ethics Committees.
Outcome and Variables
The primary outcome was 1 or more unplanned readmission to any ward at the study hospital within 6 months of the date of hospital discharge. Information about the frequency and duration of planned and unplanned hospital readmissions in the 6 months after discharge was obtained from the hospital admissions database. Planned readmissions included elective surgical or procedural admissions and scheduled day‐case admissions. Unplanned readmissions included all presentations through the emergency department, except for brief emergency department attendances where the participant was not formally admitted under a consultant.
Information was abstracted from the medical record at the time of discharge using a structured audit tool, including age, sex, primary diagnosis according to the treating clinical team, Charlson comorbidity score, number of medications at discharge, living situation at time of discharge, and the number of hospitalizations in the previous 12 months. Note was made of whether a discharge summary was completed and faxed to the general practitioner within 24 hours of discharge. Weight and height were measured by the research assistant to calculate the body mass index (BMI) which was categorized according to World Health Organization recommended cut‐offs.
Within 5 days of discharge from the index admission, the participant was contacted by telephone to schedule an interview at home within the next week. Posthospital interviews were undertaken using a structured interview tool composed of validated measures of the variables of interest, as described below. Interviews took 45 to 90 minutes to complete, and were performed by one of eight postgraduate clinical psychology students from the University of Queensland, who received training and regular supervision by a senior academic psychologist (NP).
Cognitive status was tested using the 3MS cognitive screening test, a sensitive test for early cognitive impairment.20 The Cambridge Contextual Reading Test (CCRT, short version) was used as a measure of literacy and verbal intelligence, as it may be robust in the presence of early cognitive decline21 Mood disturbances were evaluated using the Geriatric Depression Scale (GDS, short version)22 and the Geriatric Anxiety Inventory (GAI).23 The Social Support Questionnaire short form (SSQ6) was used to identify satisfaction with supports.24 Self‐rated health and income adequacy were rated using a 5 point Likert scale. Compliance with prescribed medication was assessed using the Medication Adherence Rating Scale (MARS) (R Horne, personal communication). Alcohol consumption was evaluated using the alcohol use disorders identification tool (AUDIT).25 Instrumental activities of daily living (IADL: using the telephone, using transport, shopping, housework, meal preparation, medication management, managing money) and basic activities of daily living (BADL: bathing, dressing, eating, mobility, transfers, grooming) were assessed using items from the Older Americans Resources and Services (OARS) questionnaire.26 Relevant permissions were obtained from the developers.
Analysis
Data were analyzed using SPSS 17.0. The distribution of each explanatory and confounding variable was examined and summarized using appropriate statistics (mean, median or proportion). Ordinal and some continuous variables were grouped into categories according to previously validated cut‐offs and clinical meaning. Logarithmic transformation was used in analyses of length of stay due to the highly skewed distribution. ADL and IADL function were grouped into independent in all activities, dependent in IADL function only, and dependent in basic ADL function. Bivariate analysis was undertaken using contingency tables and chi‐square testing for categorical variables and independent samples t‐test or equivalent nonparametric testing for continuous variables, to identify potential associations with the primary outcome.
Dealing with diagnosis posed particular difficulties because of the large number of disease categories. Other authors have restricted the sample to a limited number of diagnoses,27, 28 explored the impact of a limited number of diagnoses compared to all others,13 or grouped diagnoses in a pre‐specified or post hoc manner.3, 15 Considering previous studies and preliminary examination of the data (Table 3), we grouped diagnoses as chronic (heart failure, chronic lung disease, diabetes) vs. other for analysis purposes.
| Follow‐Up Data (n = 142) | No Follow‐Up Data (n = 48) | P | |
|---|---|---|---|
| |||
| Age, years, mean (SD) | 74.0 (10.9) | 76.8 (10.1) | 0.13 |
| Male, % | 52.8 | 56.3 | 0.68 |
| Admissions past 12 months, median (IQR) | 2 (1, 2.25) | 1 (1,2) | 0.38 |
| Comorbidity score, median (IQR) | 2 (1,4) | 2 (1,3) | 0.48 |
| Medications on discharge, mean (SD) | 8.8 (4.0) | 9.0 (4.5) | 0.86 |
| Length of stay, median (IQR) | 6.5 (4,11) | 7 (4,14) | 0.35 |
| Discharged to | 0.30 | ||
| Independent living alone | 38.7 | 47.9 | |
| Independent living with others | 54.2 | 50.0 | |
| Assisted living/residential care | 7.1 | 2.1 | |
| Community services on discharge, % | 42.3 | 56.3 | 0.16 |
| Number (%) with characteristic | % Readmitted | P | |
|---|---|---|---|
| |||
| Age (years) | 0.78 | ||
| <65 | 31 (22) | 39 | |
| 6584.9 | 92 (65) | 40 | |
| 85 or more | 19 (13) | 32 | |
| Male | 75 (53) | 40 | 0.74 |
| Admissions past 12 months | 0.78 | ||
| 1 | 67 (47) | 39 | |
| 2 | 40 (28) | 35 | |
| 3 or more | 35 (25) | 43 | |
| Body mass index | 0.02 | ||
| Underweight | 11 (8) | 72 | |
| Normal | 55 (39) | 27 | |
| Overweight | 43 (30) | 37 | |
| Obese | 32 (23) | 50 | |
| Chronic disease diagnosis | 27 (19) | 67 | 0.001 |
| Functional dependence | 0.16 | ||
| Independent | 27 (19) | 26 | |
| Dependent in IADLs | 48 (34) | 48 | |
| Dependent in BADLs | 66 (47) | 36 | |
| Comorbidity score | 0.15 | ||
| 0 | 19 (13) | 26 | |
| 12 | 62 (44) | 34 | |
| 3 or more | 61 (43) | 48 | |
| Summary sent within 24 hours | 117 (82) | 40 | 0.93 |
| Discharge supports | 0.60 | ||
| community | 72 (51) | 35 | |
| community with supports | 60 (42) | 43 | |
| residential care | 10 (7) | 40 | |
| Poor cognition (3MS 85)* | 80 (58) | 36 | 0.68 |
| Reduced literacy (CCRT<21) | 61 (48) | 41 | 0.55 |
| Depressive symptoms (GDS 5) | 72 (51) | 47 | 0.04 |
| Anxiety symptoms (GAI 9) | 45 (32) | 38 | 0.93 |
| Poor adherence (MARS <24) | 48 (34) | 35 | 0.56 |
| Hazardous drinking (AUDIT >6) | 18 (13) | 39 | 0.98 |
| English as second language | 19 (13) | 32 | 0.50 |
| Self‐rated health fair or poor | 102 (72) | 38 | 0.68 |
| Financial hardship | 46 (32) | 35 | 0.47 |
| Total | 142 | 39 | |
| Diagnosis | Number with diagnosis (%) | % readmitted |
|---|---|---|
| Heart failure | 13 (9) | 69 |
| Diabetes | 6 (4) | 67 |
| Chronic lung disease | 8 (6) | 63 |
| Cellulitis | 8 (6) | 63 |
| Syncope/arrhythmia | 11 (8) | 46 |
| Pneumonia | 10 (7) | 40 |
| Urinary infection | 15 (11) | 33 |
| Fall or fracture | 18 (13) | 33 |
| Gastrointestinal disease | 7 (5) | 29 |
| Ischemic heart disease | 11 (8) | 18 |
| Neurological disease | 7 (5) | 0 |
| Other | 28 (20) | 29 |
| Total | 142 (100) | 39 |
Potentially important variables were chosen based on bivariate analysis (P < 0.2) and previous literature. These variables were then entered into a multiple logistic regression model, and a significant association in the adjusted model was defined as P < 0.05. The performance of the final model was assessed by constructing a receiver operating curve. Given a 40% to 50% anticipated event rate, we estimated that 150 to 200 participants would provide power to include 7 to 10 variables of interest within the model.
Results
Active screening over 12 months identified 1194 new admissions with a documented hospitalization in the previous 6 months. Of these, 85 were discharged prior to clinical review, 227 were aged less than 50 years, 16 died in hospital, and 153 had been screened previously in the study, leaving 713 individual patients for eligibility screening. Screening identified 328 of 713 (46.0%) patients eligible to participate in the study, who were approached for consent. Of these eligible patients, 190 of 328 (57.9%) agreed to participate but 48 of 190 (25%) did not complete posthospital follow‐up, leaving a total of 142 participants. Patient eligibility, consent, and follow‐up are detailed in Figure 1.
Demographic and disease characteristics of the study participants are shown in Table 1. The 48 participants without follow‐up data appeared similar to those with full data, and 25 (52.1%) of these participants without follow‐up data had an unplanned admission within 6 months.
By 6 months, 55 of 142 participants with follow‐up data (38.7%) had had a total of 102 unplanned admissions to the study hospital. Of these, 42 of 55 (76%) were readmitted to internal medicine. Of the 55 participants with an unplanned readmission, 30 had only 1 unplanned readmission, 9 had 2, and 16 had 3 or more unplanned readmissions within 6 months of the index hospitalization.
During 6 month follow‐up of all 142 participants, there were also 97 planned (scheduled) admissions, 56 (58%) of which occurred in the group with an unplanned admission. Thus the 55 participants with an unplanned readmission accounted for a total of 1055 hospital bed‐days (mean 19.2 days per patient over 6 months follow‐up) while the 87 participants without an unplanned readmission used only 147 bed‐days (mean 1.7 days per patient over 6 months).
Bivariate analysis of the association of unplanned readmissions with the study variables is detailed in Table 2. BMI showed a nonlinear relationship with readmission, with a higher risk apparent at each end of the distribution. Depressive symptoms were also associated with a higher risk of readmission.
Age, sex, number of previous admissions, and discharge supports were not significantly different between the 2 groups. There was no difference in length of the index hospital stay: median length of stay was 6 days (interquartile range [IQR] 3‐14 days) in the readmitted group and 7 (IQR 4‐10 days) in the non‐readmitted group. There was a trend to higher mean number of medications in the readmitted group (9.4 vs. 8.8, P = 0.21).
The strongest predictor of readmission was the presence of a chronic disease diagnosis. Patterns of readmission for each primary clinical diagnosis are shown in Table 3. Chronic comorbidities including heart failure, chronic renal failure, and diabetes were associated with a higher risk of readmission (Table 4). Median comorbidity score was 3 (IQR 1‐5) in the readmitted group compared to 2 (IQR 1‐3) in the nonreadmitted group (P = 0.02).
| Co‐Morbidity | Number with Co‐Morbidity (%) | % Readmitted | P |
|---|---|---|---|
| Heart failure | 30 (21) | 57 | 0.02 |
| Chronic renal impairment | 22 (15) | 59 | 0.03 |
| Diabetes | 36 (25) | 53 | 0.05 |
| Chronic lung disease | 39 (27) | 49 | 0.13 |
| Peripheral vascular disease | 25 (18) | 44 | 0.55 |
| Cerebrovascular disease | 36 (25) | 44 | 0.42 |
| Ischemic heart disease | 57 (40) | 40 | 0.75 |
| Cancer | 23 (16) | 35 | 0.67 |
On the basis of these findings and the literature, a multivariate binary logistic regression model for unplanned admission within 6 months was fitted, including chronic disease diagnosis, comorbiditiy score, BMI, functional status, and GDS as explanatory variables, and adjusting for the potential confounders of age and length of stay (as a severity surrogate). The model is shown in Table 5, and demonstrates a significant association between readmission and chronic conditions, BMI, and depressive symptoms. The area under the receiving operating curve was 0.73.
| Odds Ratio (95% CI) | P Value | |
|---|---|---|
| ||
| Body mass index (reference 18.525) | ||
| Underweight (<18.5) | 12.7 (2.370.7) | 0.004 |
| Overweight (2530) | 1.9 (0.75.1) | 0.18 |
| Obese (>30) | 2.6 (0.97.3) | 0.07 |
| Depressive symptoms (GDS 5) | 3.0 (1.36.8) | 0.01 |
| Chronic disease diagnosis | 3.4 (1.39.3) | 0.02 |
| Co‐morbidity score | 1.3 (1.01.6) | 0.02 |
| Dependency (reference independent) | 0.32 | |
| IADL dependency only | 1.7 (0.55.4) | |
| BADL dependency | 0.9 (0.32.8) | |
| Age group (reference <65 years) | 0.94 | |
| 6584 | 1.1 (0.42.8) | |
| 85 or older | 0.9 (0.23.5) | |
| Log length of stay | 0.99 (0.961.01) | 0.43 |
Discussion
This study demonstrates a number of important findings. First, 39% of this group of participants went on to further unplanned hospital readmissions in the ensuing 6 months, demonstrating the high risk in this group with more than 1 recent hospital admission. However, within this group, the risk of readmission was not related to the frequency of admission within the previous year, consistent with several previous studies.29, 30 These finding suggest that 1 or more recent previous admissions identified at the time of a medical admission is an effective identifier of high risk patients. Subgroup analysis of a recent discharge intervention study in medical patients suggests that this high risk group may particularly benefit from such an intervention.16
Second, the study describes important predictors of readmission which may inform novel interventions. The BMI showed a significant nonlinear relationship with readmission, with an increased risk both above and below the normal weight range. Almost half the group was overweight or obese, with a 2‐fold risk compared to normal weight patients. While underweight was less prevalent, it carried a markedly increased probability of readmission. Limited previous studies support the association of nutritional status and unplanned readmission.31, 32 Malnutrition may be a marker of disease stage or severity, or may be associated with other unmeasured social determinants which increase readmission risk. However, malnutrition itself may reduce physiological resilience and predispose to higher health care needs. There are no published trials of posthospital nutritional intervention programs for reducing readmission rates in general medical patients.
The risk of readmission was also increased in participants with depressive symptoms, consistent with several previous studies.3336 This effect was independent of illness type and comorbidity. Depression is increasingly recognized as an important independent predictor of a range of important outcomes in older medical patients, including posthospital functional decline,37 institutionalization and mortality.36, 38 Posthospital decline and poor self‐management might contribute to higher rehospitalization. There is some evidence that effective treatment of psychological comorbidities in medically ill patients may reduce readmissions.18, 39
Both the number and type of chronic conditions appear to be predictors of readmission in this high risk group, where there was a high baseline prevalence of chronic diseases such as heart failure, diabetes, renal impairment, and chronic lung disease which have been associated with higher readmission rates in a number of previous studies.13, 15, 30, 40 Almost all participants had one or more significant comorbid conditions in addition to their presenting complaint; single disease‐focused chronic disease management programs may not be an optimal solution in this group. Consistent with this comorbidity burden, most participants were prescribed a large number of medications. In keeping with other studies,17 about one‐third of participants reported reduced medication adherence but this was not associated with a higher readmission risk.
Like most previous studies in medical patients,10, 11, 15, 29, 30, 35, 36, 40, 41 there was no evidence of increasing readmission rates with age. Functional status impairment was not a significant predictor of readmission, probably reflecting selection of a patient subgroup with a high prevalence of disability and chronic disease. Satisfaction with social support was generally high, and not associated with readmission. This may reflect the emphasis on discharge planning and postacute social and functional support already occurring in usual care.
Measures of cognition and literacy were not associated with readmission. However, these were the items with the most missing data (see Table 2), which may have reduced our ability to detect an association. The study design excluded patients with significant cognitive or communication deficits who were unable to participate in detailed assessments. Such stringent eligibility criteria may be seen as a weakness of this study, reducing the generalizability of the findings. However, the study deliberately sampled a population of older adults suitable for a multifacetted posthospital management program, in order to inform specific intervention targets, and the eligibility criteria reflect these practical considerations. Although some previous studies have found that cognitive impairment is a predictor of readmission,10, 12 others have found no association.29, 30, 36, 40, 41
The main study weaknesses are the small sample size (reflected in the wide confidence intervals [CIs] in the multivariate analysis), and the relatively high rate of drop‐outs (25% of enrolments) for whom detailed posthospital data could not be collected. This problem reflects the age and burden of illness in the population under study. Readmission data were collected for all participants, and a similar rate of readmission was observed in patients with missing data (52% vs. 39%, P = 0.11). The heterogeneous patients mix may have concealed some important associations within individual diagnoses or other patient subgroups. This heterogeneity reflects the reality of the selected high risk subgroup, and the study deliberately avoided a disease‐specific focus for generalizability.
Conclusions
This study confirms the high rate of hospital readmission in medical patients who have already had a previous inpatient admission in the past 6 months. It shifts the emphasis from nonmodifiable disease and demographic predictors to consideration of common, nondisease specific factors which might have a plausible causative relationship with readmission and may be amenable to specific interventions. The population sampled had a high prevalence of chronic disease, and often multiple diseases. Nutritional status and depressive symptoms are emerging as important modifiers of disease course and mortality in the setting of several chronic diseases; this study also supports their potential contribution to increased hospital resource consumption in a high‐risk group. Posthospital programs which specifically address these factors in the context of optimal medical management of underlying chronic diseases have the potential to reduce hospital readmissions.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,.Clinical and sociodemographic risk factors for reamdission of Medicare benficiaries.Health Care Financ Rev.1988;10(1):27–36.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118:219–223.
- ,,,,.A case manager intervention to reduce readmissions.Arch Intern Med.1995;154(15):1721–1729.
- ,,, et al.A transitional care service for elderly chronic disease patients at risk of readmission.Aust Health Rev.2004;28(3):275–284.
- ,,,,.Self‐management programmes by lay leaders for people with chronic conditions.Cochrane Database Syst Rev.2007(4):Art No.CD005108.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,, et al.Discharge planning from hospital to home.Cochrane Database Syst Rev.2010(Issue 1):Art No.CD000313.
- ,,, et al.Characteristics of geriatric patients related to early and late readmissions to hospital.Aging Clin Exp Res.1998;10:339–346.
- ,,, et al.Hospital readmission among older medical patietns in Hong Kong.J R Coll Physicians Lond.1999;33(2):153–156.
- ,,, et al.Early re‐hospitalization of elderly people discharged from a geriatric ward.Aging Clin Exp Res.2006;18(1):63–69.
- ,,,,.Readmission patterns in patients with chronic obstructive pulmonary disease, chronic heart failure and diabetes mellitus: an administrative dataset analysis.Intern Med J.2005;35:296–299.
- ,,,.Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients.BMJ.2006;333:327–330.
- ,,,.Predicting emergency readmission for patients discharged from the medical service of a teaching hospital.J Gen Intern Med.1987;2:400–405.
- ,,, et al.A reengineered hospital discharge program to decrease hospitalization.Ann Intern Med.2009;150:178–187.
- ,,.The role of medication noncompliance and adverse drug reactions in hospitalisations in the elderly.Arch Intern Med.1990;150:841–845.
- ,,, et al.UPBEAT: the impact of a psychogeriatric intervention in VA medical centers.Med Care.2001;39(5):500–512.
- ,,,.Controlled trial of multidisciplinary care teams for acutely ill medical inpatients: enhanced multidisciplinary care.Intern Med J.2006;36:558–563.
- ,.The modified mini‐mental state (3MS) examination.J Clin Psychiatry.1987;48:314–318.
- .Development of the Cambridge Contextual Reading Test for improving the examination of premorbid verbal intelligence in older persons with dementia.Br J Clin Psychol.1998;37:229–240.
- ,.Geriatric Depression Scale (GDS): recent evidence and development of a shorter version.Clinics in Gerontology.1986;5:165–172.
- ,,,,,.Development and validation of the Geriatric Anxiety Inventory.Int Psychogeriatr.2007;19(1):103–114.
- ,,.A brief measure of social support: practical and theoretical implications.J Soc Pers Relat.1987;4:497–510.
- ,,,,.Screening for problem drinking: comparison of the CAGE and AUDIT.J Gen Intern Med.1998;13(6):379–388.
- ,.OARS methodology: a decade of experience in geriatric assessment.J Am Geriatr Soc.1985;33:607–615.
- ,.Hospital readmissions among the elderly.J Am Geriatr Soc.1985;33:595–601.
- ,,,,,.Discharge destination and repeat hospitalizations.Med Care.1997;35:756–767.
- ,,, et al.Measuring frailty in the hospitalized elderly. Concept of functional homeostasis.Am J Phys Med Rehab.1998;77(3):252–257.
- ,.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6(5):389–393.
- .Risk factors for early hospital readmission in a select population of geriatric rehabilitation patients: the significance of functional status.J Am Geriatr Soc.1992;40:792–798.
- ,,,.Predicting early nonelective hospital readmission in nutritionally compromised older adults.Am J Clin Nutr.1997;65:1714–1720.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107(1):13–17.
- ,,,.Depression and activities of daily living predict rehospitalisation within 6 months of discharge from geriatric rehabilitation.Rehabil Psychol.2004;49(3):219–223.
- ,,,.Depressive symptoms and negative outcomes in older hospitalized patients.Arch Intern Med.2002;162:948–949.
- ,,,.Depressive symptoms as a predictor of 6‐month outcomes and services utilization in elderly medical inpatients.Arch Intern Med.2001;161:2609–2615.
- ,,,,.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126(6):417–425.
- ,,,.Diabetes, depression and death. A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT).Diabetes Care.2007;30(12):3005–3010.
- ,,.Clinical implications of a reduction in psychosocial distress in cardiac prognosis in patients participating in a psychosocial intervention programme.Psychosom Med.2001;63(2):257–266.
- ,,, et al.Predictors of immediate and 6‐month outcomes in hospitalized elderly patients.J Am Geriatr Soc.1988;36:775–783.
- ,,,,.Factors predictive of outcome on admission to an acute geriatric ward.Age Ageing.1999;28:429–432.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,,,,.Hospital readmissions and quality of care.Med Care.1999;37(5):490–501.
- ,,.Clinical and sociodemographic risk factors for reamdission of Medicare benficiaries.Health Care Financ Rev.1988;10(1):27–36.
- .Hazards of hospitalization of the elderly.Ann Intern Med.1993;118:219–223.
- ,,,,.A case manager intervention to reduce readmissions.Arch Intern Med.1995;154(15):1721–1729.
- ,,, et al.A transitional care service for elderly chronic disease patients at risk of readmission.Aust Health Rev.2004;28(3):275–284.
- ,,,,.Self‐management programmes by lay leaders for people with chronic conditions.Cochrane Database Syst Rev.2007(4):Art No.CD005108.
- ,,,.The effectiveness of disease management programmes in reducing hospital re‐admission in older patients with heart failure: a systematic review and meta‐analysis of published reports.Eur Heart J.2004;25:1570–1595.
- ,,, et al.Discharge planning from hospital to home.Cochrane Database Syst Rev.2010(Issue 1):Art No.CD000313.
- ,,, et al.Characteristics of geriatric patients related to early and late readmissions to hospital.Aging Clin Exp Res.1998;10:339–346.
- ,,, et al.Hospital readmission among older medical patietns in Hong Kong.J R Coll Physicians Lond.1999;33(2):153–156.
- ,,, et al.Early re‐hospitalization of elderly people discharged from a geriatric ward.Aging Clin Exp Res.2006;18(1):63–69.
- ,,,,.Readmission patterns in patients with chronic obstructive pulmonary disease, chronic heart failure and diabetes mellitus: an administrative dataset analysis.Intern Med J.2005;35:296–299.
- ,,,.Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients.BMJ.2006;333:327–330.
- ,,,.Predicting emergency readmission for patients discharged from the medical service of a teaching hospital.J Gen Intern Med.1987;2:400–405.
- ,,, et al.A reengineered hospital discharge program to decrease hospitalization.Ann Intern Med.2009;150:178–187.
- ,,.The role of medication noncompliance and adverse drug reactions in hospitalisations in the elderly.Arch Intern Med.1990;150:841–845.
- ,,, et al.UPBEAT: the impact of a psychogeriatric intervention in VA medical centers.Med Care.2001;39(5):500–512.
- ,,,.Controlled trial of multidisciplinary care teams for acutely ill medical inpatients: enhanced multidisciplinary care.Intern Med J.2006;36:558–563.
- ,.The modified mini‐mental state (3MS) examination.J Clin Psychiatry.1987;48:314–318.
- .Development of the Cambridge Contextual Reading Test for improving the examination of premorbid verbal intelligence in older persons with dementia.Br J Clin Psychol.1998;37:229–240.
- ,.Geriatric Depression Scale (GDS): recent evidence and development of a shorter version.Clinics in Gerontology.1986;5:165–172.
- ,,,,,.Development and validation of the Geriatric Anxiety Inventory.Int Psychogeriatr.2007;19(1):103–114.
- ,,.A brief measure of social support: practical and theoretical implications.J Soc Pers Relat.1987;4:497–510.
- ,,,,.Screening for problem drinking: comparison of the CAGE and AUDIT.J Gen Intern Med.1998;13(6):379–388.
- ,.OARS methodology: a decade of experience in geriatric assessment.J Am Geriatr Soc.1985;33:607–615.
- ,.Hospital readmissions among the elderly.J Am Geriatr Soc.1985;33:595–601.
- ,,,,,.Discharge destination and repeat hospitalizations.Med Care.1997;35:756–767.
- ,,, et al.Measuring frailty in the hospitalized elderly. Concept of functional homeostasis.Am J Phys Med Rehab.1998;77(3):252–257.
- ,.Factors predicting readmission of older general medicine patients.J Gen Intern Med.1991;6(5):389–393.
- .Risk factors for early hospital readmission in a select population of geriatric rehabilitation patients: the significance of functional status.J Am Geriatr Soc.1992;40:792–798.
- ,,,.Predicting early nonelective hospital readmission in nutritionally compromised older adults.Am J Clin Nutr.1997;65:1714–1720.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107(1):13–17.
- ,,,.Depression and activities of daily living predict rehospitalisation within 6 months of discharge from geriatric rehabilitation.Rehabil Psychol.2004;49(3):219–223.
- ,,,.Depressive symptoms and negative outcomes in older hospitalized patients.Arch Intern Med.2002;162:948–949.
- ,,,.Depressive symptoms as a predictor of 6‐month outcomes and services utilization in elderly medical inpatients.Arch Intern Med.2001;161:2609–2615.
- ,,,,.Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons.Ann Intern Med.1997;126(6):417–425.
- ,,,.Diabetes, depression and death. A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT).Diabetes Care.2007;30(12):3005–3010.
- ,,.Clinical implications of a reduction in psychosocial distress in cardiac prognosis in patients participating in a psychosocial intervention programme.Psychosom Med.2001;63(2):257–266.
- ,,, et al.Predictors of immediate and 6‐month outcomes in hospitalized elderly patients.J Am Geriatr Soc.1988;36:775–783.
- ,,,,.Factors predictive of outcome on admission to an acute geriatric ward.Age Ageing.1999;28:429–432.
Copyright © 2010 Society of Hospital Medicine