User login
Pseudobulbar affect: When patients laugh or cry, but don’t know why
Pseudobulbar affect (PBA) is a disorder of affective expression that manifests as stereotyped and frequent outbursts of crying (not limited to lacrimation) or laughter. Symptoms are involuntary, uncontrolled, and exaggerated or incongruent with current mood. Episodes, lasting a few seconds to several minutes, may be unprovoked or occur in response to a mild stimulus, and patients typically display a normal affect between episodes.1 PBA is estimated to affect 1 to 2 million people in the United States, although some studies suggest as many as 7 million,1,2 depending on the evaluation method and threshold criteria used.3
Where to look for pseudobulbar affect
PBA has been most commonly described in 6 major neurologic disorders:
- Alzheimer’s disease
- amyotrophic lateral sclerosis (ALS)
- multiple sclerosis (MS)
- Parkinson’s disease
- stroke
- traumatic brain injury (TBI).
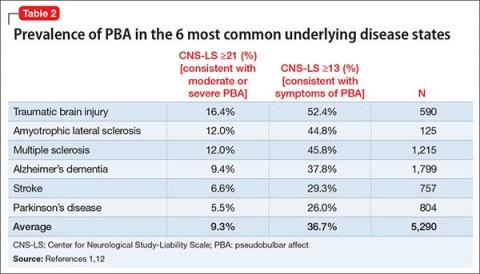
Of these disorders, most studies have found the highest PBA prevalence in patients with ALS and TBI, with lesser (although significant) prevalence in Parkinson’s disease (Table 2).1,12 These “big 6” diagnoses are not a comprehensive list, as many other disease states are associated with PBA (Table 3).12-14
2 Pathways: ‘Generator’ and ‘governor’
Despite the many and varied injuries and illnesses associated with PBA, Lauterbach et al10 noted patterns that suggest dysregulation of 2 distinct but interconnected brain pathways: an emotional pathway controlled by a separate volitional pathway. Lesions to the volitional pathway (or its associated feedback or processing circuits) are thought to cause PBA symptoms.
To borrow an analogy from engineering, the emotional pathway is the “generator” of affect, whereas the volitional pathway is the “governor” of affect. Thus, injury to the “governor” results in overspill, or overflow, of affect that usually would be suppressed.
The emotional pathway, which coordinates the motor aspect of reflex laughing or crying, originates at the frontotemporal cortex, relaying to the amygdala and hypothalamus, then projecting to the dorsal brainstem, which includes the midbrain-pontine periaqueductal gray (PAG), dorsal tegmentum, and related brainstem.
The volitional pathway, which regulates the emotional pathway, originates in the dorsal and lateral frontoparietal cortex, projects through the internal capsule and midbrain basis pedunculi, and continues on to the anteroventral basis pontis. The basis pontis then serves as an afferent relay center for cerebellar activity. Projections from the pons then regulate the emotional circuitry primarily at the level of the PAG.10
Lesions of the volitional pathway have been correlated with conditions of PBA, whereas direct activation of the emotional pathway tended to lead to emotional lability or the crying and laughing behaviors observed in dacrystic or gelastic epilepsy.10 The pivotal nature of the regulation occurring at the PAG has guided treatment options. Neurotransmitter receptors most closely associated with this region include glutamatergic N-methyl-
When to screen for PBA
Ask the right question. PBA as a disease state likely has been widely under-reported, under-recognized, and misdiagnosed (typically, as a primary mood disorder).9 Three factors underscore this problem:
- Patients do not specifically report symptoms of affective disturbance (perhaps because they lack a vocabulary to separate concepts of mood and affect)
- Physicians do not ask patients about separations of mood and affect
- Perhaps most importantly, PBA lacks a general awareness and understanding.
Co-occurring mood disorders also may thwart PBA detection. One study of PBA in Alzheimer’s dementia found that 53% of patients with symptoms consistent with PBA also had a distinct mood disorder.17 This suggests that a PBA-specific screening test is needed for accurate diagnosis.
A single question might best refine the likelihood that a patient has PBA: “Do you ever cry for no reason?” In primary psychiatric illness, crying typically is associated with a specific trigger (eg, depressed mood, despair, anxiety). A patient’s inability to identify a trigger for crying suggests the pathological separation of mood and affect—the core of PBA, and worthy of further investigation.
Clinical rating scales that correlate to disease severity appear to be the most effective in identifying PBA. The PRISM study, to date the largest clinic-based study of PBA symptoms, used the Center for Neurologic Study-Liability Scale (CNS-LS) to gauge the presence and severity of PBA symptoms.1 A 7-question, patient self-administered tool, the CNS-LS is graded on a 5-point Likert scale. A score ≥13 has high sensitivity and specificity for diagnosis of PBA, compared with physician diagnosis.
Another option, the 16-question Pathological Laughing and Crying Scale, is a clinician-administered screening tool. Again, a score ≥13 is consistent with symptoms required for a PBA diagnosis.
Treating PBA symptoms
Until recently, most pharmacotherapeutic interventions for PBA were based on off-label use of tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs). From 1980 to 2010, only 7 of 22 case reports or trials of TCAs or SSRIs for PBA were randomized, double-blind, and placebo-controlled. Five had 12 to 28 patients, and 2 had 106 and 128 patients, respectively. Only 1 controlled trial included a validated symptom severity scale, and none included a scale validated for PBA.18
In particular, imipramine and nortriptyline were studied for managing PBA in patients with stroke; amitriptyline, in patients with MS; and various SSRIs, in patients with stroke.11 Response of PBA symptoms to antidepressant therapy was greater in all placebo-controlled trials than response to placebo.18 As seen in pharmacotherapy of depression, the lower burden of adverse effects and overall better tolerability of SSRIs resulted in their preferred use over TCAs. In some cases, the side effects of TCAs can be leveraged for therapeutic gain. If insomnia is a problem, a nighttime dose of a TCA could ameliorate this. Similarly, if a patient has sialorrhea, the anticholinergic effect of a TCA may show some benefit.19
Dextromethorphan plus quinidine. Dextromethorphan has long been of interest for a variety of neurodegenerative diseases. Studies of its efficacy were largely unsuccessful, however, because rapid metabolism by cytochrome P450 (CYP) 2D6 prevented CNS penetration.20 Quinidine is an avid inhibitor of CYP2D6, even at very low dosages. Adding quinidine to dextromethorphan limits metabolism, allowing dextromethorphan to accumulate to a plasma concentration sufficient to penetrate the CNS.12 In 2010, the combination agent dextromethorphan hydrobromide (20 mg)/quinidine (10 mg) (DM/Q) became the first treatment to receive FDA approval for managing PBA.11
Mechanism of action. The exact mechanism of DM/Q in PBA remains unknown. Dextromethorphan is an agonist of sigma-1 receptors and a relatively specific noncompetitive antagonist of NMDA receptors. It also has been shown to modulate glutamate and serotonin neurotransmission and ion channel function.20 Sigma-1 receptors are concentrated in the brainstem and parts of the cerebellum that are thought to coordinate motor emotional responses. Agonism of sigma-1 receptors on glutamatergic neurons has been proposed to limit release of glutamate from the presynaptic neuron while also limiting downstream transmission of glutamatergic signal in postsynaptic neurons.
Clinical trials. Two large trials have demonstrated efficacy of DM/Q in PBA. STAR was a 12-week, double-blind, placebo-controlled trial with 326 patients diagnosed with ALS or MS who showed PBA symptoms (CNS-LS score ≥13). Compared with placebo, DM/Q use was associated with significantly reduced (P < .01) daily episodes of PBA at 2, 4, 8, and 12 weeks.20 The effect was rapid, with 30% fewer PBA episodes after the first week (P < .0167). At 12 weeks, 51% of patients on DM/Q had been symptom-free for at least 2 weeks.
The PRISM II study examined the efficacy of DM/Q in managing PBA in 102 individuals with dementia, 92 with stroke, and 67 with TBI. After 30 and 90 days, CNL-LS scores were significantly reduced (P < .001) compared with baseline scores.20
Prescribing information. Dextromethorphan—typically in the form of cough syrup—has been implicated as a substance of abuse. A placebo-controlled trial demonstrated that co-administering quinidine with dextromethorphan limits measures of positive reinforcement, such as euphoria and drug liking. This suggests that quinidine may be used to reduce abuse of dextromethorphan.20 As such, the abuse potential of DM/Q appears to be low.
The most common adverse effects reported with DM/Q are diarrhea, dizziness, and cough.12 Notably, patients who received DM/Q in the STAR trial were more likely to report dizziness than those receiving placebo (10.3% vs 5.5%), but patients receiving placebo were more likely to fall.21,22
Package labeling warns that DM/Q causes dose-dependent QTc prolongation.21 Quinidine can be associated with significant QTc prolongation when dosed at antiarrhythmic levels, although mean plasma concentrations found with the 10 mg of quinidine in the approved DM/Q formulation are 1% to 3% of those associated with typical dosages used in antiarrhythmic therapy. Electrophysiology studies of quinidine 10 mg dosed every 12 hours have demonstrated a mean QTc increase at steady state of 6.8 milliseconds, compared with 9.1 milliseconds for a reference control (moxifloxacin).12,21
Although this would seem to indicate a relatively low risk of clinically significant QTc prolongation at these ultra-low dosages of quinidine, it may be advisable to obtain an initial pre-dose and post-dose ECG and longitudinally monitor the QTc interval in patients with conditions that predispose to cardiac arrhythmias. Because quinidine inhibits CYP2D6, use caution when prescribing and monitoring other medications metabolized by this pathway.
Bottom Line
1. Brooks BR, Crumpacker D, Fellus J, et al. PRISM: a novel research tool to assess the prevalence of pseudobulbar affect symptoms across neurological conditions. PLoS One. 2013;8(8):e72232. doi: 10.1371/journal.pone.0072232.
2. Cruz MP. Nuedexta for the treatment of pseudobulbar affect: a condition of involuntary laughing and crying. P T. 2013;38(6):325-328.
3. Work SS, Colamonico JA, Bradley WG, et al. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586-601.
4. Arciniegas DB, Lauterbach EC, Anderson KE, et al. The differential diagnosis of pseudobulbar affect (PBA). Distinguishing PBA among disorders of mood and affect. Proceedings of a roundtable meeting. CNS Spectr. 2005;10(5):1-14; quiz 15-16.
5. Darwin C. The expression of the emotions in man and animals. London, United Kingdom: John Murray; 1872.
6. Oppenheim H, Siemerling E. Mitteilungen über Pseudobulbärparalyse und akute Bulbärparalyse. Berl Kli Woch. 1886;46.
7. Wilson SA. Original papers: some problems in neurology. J Neurol Psychopathol. 1924;4(16):299-333.
8. Poeck K, Risso M, Pilleri G. Contribution to the pathophysiology and clinical systematology of pathological laughing and crying [in German]. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr. 1963;204:181-198.
9. Cummings JL, Gilbart J, Andersen G. Pseudobulbar affect - a disabling but under-recognised consequence of neurological disease and brain injury. Eur Neurol Rev. 2013;8(2):74-81.
10. Lauterbach EC, Cummings JL, Kuppuswamy PS. Toward a more precise, clinically–informed pathophysiology of pathological laughing and crying. Neurosci Biobehav Rev. 2013;37(8):1893-1916.
11. Pioro EP. Review of dextromethorphan 20 mg/quinidine 10 mg (Nuedexta(®)) for pseudobulbar affect. Neurol Ther. 2014;3(1):15-28.
12. Schoedel KA, Morrow SA, Sellers EM. Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatr Dis Treat. 2014;10:1161-1174.
13. Li Z, Luo S, Ou J, et al. Persistent pseudobulbar affect secondary to acute disseminated encephalomyelitis. Socioaffect Neurosci Psychol. 2015;5:26210. doi: 10.3402/snp.v5.26210.
14. Pattee GL, Wymer JP, Lomen-Hoerth C, et al. An open-label multicenter study to assess the safety of dextromethorphan/quinidine in patients with pseudobulbar affect associated with a range of underlying neurological conditions. Curr Med Res Opin. 2014;30(11):2255-2265.
15. Strowd RE, Cartwright MS, Okun MS, et al. Pseudobulbar affect: prevalence and quality of life impact in movement disorders. J Neurol. 2010;257(8):1382-1387.
16. Colamonico J, Formella A, Bradley W. Pseudobulbar affect: burden of illness in the USA. Adv Ther. 2012;29(9):775-798.
17. Starkstein SE, Migliorelli R, Tesón A, et al. Prevalence and clinical correlates of pathological affective display in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1995;59(1):55-60.
18. Pioro EP. Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs. 2011;71(9):1193-1207.
19. Ahmed A, Simmons A. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483-489.
20. Yang LP, Deeks ED. Dextromethorphan/quinidine: a review of its use in adults with pseudobulbar affect. Drugs. 2015;75(1):83-90.
21. Nuedexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals, Inc.; 2015.
22. Pioro EP, Brooks BR, Cummings J, et al; Safety, Tolerability, and Efficacy trial of AVP-923 in PBA Investigators. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68(5):693-702.
Pseudobulbar affect (PBA) is a disorder of affective expression that manifests as stereotyped and frequent outbursts of crying (not limited to lacrimation) or laughter. Symptoms are involuntary, uncontrolled, and exaggerated or incongruent with current mood. Episodes, lasting a few seconds to several minutes, may be unprovoked or occur in response to a mild stimulus, and patients typically display a normal affect between episodes.1 PBA is estimated to affect 1 to 2 million people in the United States, although some studies suggest as many as 7 million,1,2 depending on the evaluation method and threshold criteria used.3
Where to look for pseudobulbar affect
PBA has been most commonly described in 6 major neurologic disorders:
- Alzheimer’s disease
- amyotrophic lateral sclerosis (ALS)
- multiple sclerosis (MS)
- Parkinson’s disease
- stroke
- traumatic brain injury (TBI).
Of these disorders, most studies have found the highest PBA prevalence in patients with ALS and TBI, with lesser (although significant) prevalence in Parkinson’s disease (Table 2).1,12 These “big 6” diagnoses are not a comprehensive list, as many other disease states are associated with PBA (Table 3).12-14
2 Pathways: ‘Generator’ and ‘governor’
Despite the many and varied injuries and illnesses associated with PBA, Lauterbach et al10 noted patterns that suggest dysregulation of 2 distinct but interconnected brain pathways: an emotional pathway controlled by a separate volitional pathway. Lesions to the volitional pathway (or its associated feedback or processing circuits) are thought to cause PBA symptoms.
To borrow an analogy from engineering, the emotional pathway is the “generator” of affect, whereas the volitional pathway is the “governor” of affect. Thus, injury to the “governor” results in overspill, or overflow, of affect that usually would be suppressed.
The emotional pathway, which coordinates the motor aspect of reflex laughing or crying, originates at the frontotemporal cortex, relaying to the amygdala and hypothalamus, then projecting to the dorsal brainstem, which includes the midbrain-pontine periaqueductal gray (PAG), dorsal tegmentum, and related brainstem.
The volitional pathway, which regulates the emotional pathway, originates in the dorsal and lateral frontoparietal cortex, projects through the internal capsule and midbrain basis pedunculi, and continues on to the anteroventral basis pontis. The basis pontis then serves as an afferent relay center for cerebellar activity. Projections from the pons then regulate the emotional circuitry primarily at the level of the PAG.10
Lesions of the volitional pathway have been correlated with conditions of PBA, whereas direct activation of the emotional pathway tended to lead to emotional lability or the crying and laughing behaviors observed in dacrystic or gelastic epilepsy.10 The pivotal nature of the regulation occurring at the PAG has guided treatment options. Neurotransmitter receptors most closely associated with this region include glutamatergic N-methyl-
When to screen for PBA
Ask the right question. PBA as a disease state likely has been widely under-reported, under-recognized, and misdiagnosed (typically, as a primary mood disorder).9 Three factors underscore this problem:
- Patients do not specifically report symptoms of affective disturbance (perhaps because they lack a vocabulary to separate concepts of mood and affect)
- Physicians do not ask patients about separations of mood and affect
- Perhaps most importantly, PBA lacks a general awareness and understanding.
Co-occurring mood disorders also may thwart PBA detection. One study of PBA in Alzheimer’s dementia found that 53% of patients with symptoms consistent with PBA also had a distinct mood disorder.17 This suggests that a PBA-specific screening test is needed for accurate diagnosis.
A single question might best refine the likelihood that a patient has PBA: “Do you ever cry for no reason?” In primary psychiatric illness, crying typically is associated with a specific trigger (eg, depressed mood, despair, anxiety). A patient’s inability to identify a trigger for crying suggests the pathological separation of mood and affect—the core of PBA, and worthy of further investigation.
Clinical rating scales that correlate to disease severity appear to be the most effective in identifying PBA. The PRISM study, to date the largest clinic-based study of PBA symptoms, used the Center for Neurologic Study-Liability Scale (CNS-LS) to gauge the presence and severity of PBA symptoms.1 A 7-question, patient self-administered tool, the CNS-LS is graded on a 5-point Likert scale. A score ≥13 has high sensitivity and specificity for diagnosis of PBA, compared with physician diagnosis.
Another option, the 16-question Pathological Laughing and Crying Scale, is a clinician-administered screening tool. Again, a score ≥13 is consistent with symptoms required for a PBA diagnosis.
Treating PBA symptoms
Until recently, most pharmacotherapeutic interventions for PBA were based on off-label use of tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs). From 1980 to 2010, only 7 of 22 case reports or trials of TCAs or SSRIs for PBA were randomized, double-blind, and placebo-controlled. Five had 12 to 28 patients, and 2 had 106 and 128 patients, respectively. Only 1 controlled trial included a validated symptom severity scale, and none included a scale validated for PBA.18
In particular, imipramine and nortriptyline were studied for managing PBA in patients with stroke; amitriptyline, in patients with MS; and various SSRIs, in patients with stroke.11 Response of PBA symptoms to antidepressant therapy was greater in all placebo-controlled trials than response to placebo.18 As seen in pharmacotherapy of depression, the lower burden of adverse effects and overall better tolerability of SSRIs resulted in their preferred use over TCAs. In some cases, the side effects of TCAs can be leveraged for therapeutic gain. If insomnia is a problem, a nighttime dose of a TCA could ameliorate this. Similarly, if a patient has sialorrhea, the anticholinergic effect of a TCA may show some benefit.19
Dextromethorphan plus quinidine. Dextromethorphan has long been of interest for a variety of neurodegenerative diseases. Studies of its efficacy were largely unsuccessful, however, because rapid metabolism by cytochrome P450 (CYP) 2D6 prevented CNS penetration.20 Quinidine is an avid inhibitor of CYP2D6, even at very low dosages. Adding quinidine to dextromethorphan limits metabolism, allowing dextromethorphan to accumulate to a plasma concentration sufficient to penetrate the CNS.12 In 2010, the combination agent dextromethorphan hydrobromide (20 mg)/quinidine (10 mg) (DM/Q) became the first treatment to receive FDA approval for managing PBA.11
Mechanism of action. The exact mechanism of DM/Q in PBA remains unknown. Dextromethorphan is an agonist of sigma-1 receptors and a relatively specific noncompetitive antagonist of NMDA receptors. It also has been shown to modulate glutamate and serotonin neurotransmission and ion channel function.20 Sigma-1 receptors are concentrated in the brainstem and parts of the cerebellum that are thought to coordinate motor emotional responses. Agonism of sigma-1 receptors on glutamatergic neurons has been proposed to limit release of glutamate from the presynaptic neuron while also limiting downstream transmission of glutamatergic signal in postsynaptic neurons.
Clinical trials. Two large trials have demonstrated efficacy of DM/Q in PBA. STAR was a 12-week, double-blind, placebo-controlled trial with 326 patients diagnosed with ALS or MS who showed PBA symptoms (CNS-LS score ≥13). Compared with placebo, DM/Q use was associated with significantly reduced (P < .01) daily episodes of PBA at 2, 4, 8, and 12 weeks.20 The effect was rapid, with 30% fewer PBA episodes after the first week (P < .0167). At 12 weeks, 51% of patients on DM/Q had been symptom-free for at least 2 weeks.
The PRISM II study examined the efficacy of DM/Q in managing PBA in 102 individuals with dementia, 92 with stroke, and 67 with TBI. After 30 and 90 days, CNL-LS scores were significantly reduced (P < .001) compared with baseline scores.20
Prescribing information. Dextromethorphan—typically in the form of cough syrup—has been implicated as a substance of abuse. A placebo-controlled trial demonstrated that co-administering quinidine with dextromethorphan limits measures of positive reinforcement, such as euphoria and drug liking. This suggests that quinidine may be used to reduce abuse of dextromethorphan.20 As such, the abuse potential of DM/Q appears to be low.
The most common adverse effects reported with DM/Q are diarrhea, dizziness, and cough.12 Notably, patients who received DM/Q in the STAR trial were more likely to report dizziness than those receiving placebo (10.3% vs 5.5%), but patients receiving placebo were more likely to fall.21,22
Package labeling warns that DM/Q causes dose-dependent QTc prolongation.21 Quinidine can be associated with significant QTc prolongation when dosed at antiarrhythmic levels, although mean plasma concentrations found with the 10 mg of quinidine in the approved DM/Q formulation are 1% to 3% of those associated with typical dosages used in antiarrhythmic therapy. Electrophysiology studies of quinidine 10 mg dosed every 12 hours have demonstrated a mean QTc increase at steady state of 6.8 milliseconds, compared with 9.1 milliseconds for a reference control (moxifloxacin).12,21
Although this would seem to indicate a relatively low risk of clinically significant QTc prolongation at these ultra-low dosages of quinidine, it may be advisable to obtain an initial pre-dose and post-dose ECG and longitudinally monitor the QTc interval in patients with conditions that predispose to cardiac arrhythmias. Because quinidine inhibits CYP2D6, use caution when prescribing and monitoring other medications metabolized by this pathway.
Bottom Line
Pseudobulbar affect (PBA) is a disorder of affective expression that manifests as stereotyped and frequent outbursts of crying (not limited to lacrimation) or laughter. Symptoms are involuntary, uncontrolled, and exaggerated or incongruent with current mood. Episodes, lasting a few seconds to several minutes, may be unprovoked or occur in response to a mild stimulus, and patients typically display a normal affect between episodes.1 PBA is estimated to affect 1 to 2 million people in the United States, although some studies suggest as many as 7 million,1,2 depending on the evaluation method and threshold criteria used.3
Where to look for pseudobulbar affect
PBA has been most commonly described in 6 major neurologic disorders:
- Alzheimer’s disease
- amyotrophic lateral sclerosis (ALS)
- multiple sclerosis (MS)
- Parkinson’s disease
- stroke
- traumatic brain injury (TBI).
Of these disorders, most studies have found the highest PBA prevalence in patients with ALS and TBI, with lesser (although significant) prevalence in Parkinson’s disease (Table 2).1,12 These “big 6” diagnoses are not a comprehensive list, as many other disease states are associated with PBA (Table 3).12-14
2 Pathways: ‘Generator’ and ‘governor’
Despite the many and varied injuries and illnesses associated with PBA, Lauterbach et al10 noted patterns that suggest dysregulation of 2 distinct but interconnected brain pathways: an emotional pathway controlled by a separate volitional pathway. Lesions to the volitional pathway (or its associated feedback or processing circuits) are thought to cause PBA symptoms.
To borrow an analogy from engineering, the emotional pathway is the “generator” of affect, whereas the volitional pathway is the “governor” of affect. Thus, injury to the “governor” results in overspill, or overflow, of affect that usually would be suppressed.
The emotional pathway, which coordinates the motor aspect of reflex laughing or crying, originates at the frontotemporal cortex, relaying to the amygdala and hypothalamus, then projecting to the dorsal brainstem, which includes the midbrain-pontine periaqueductal gray (PAG), dorsal tegmentum, and related brainstem.
The volitional pathway, which regulates the emotional pathway, originates in the dorsal and lateral frontoparietal cortex, projects through the internal capsule and midbrain basis pedunculi, and continues on to the anteroventral basis pontis. The basis pontis then serves as an afferent relay center for cerebellar activity. Projections from the pons then regulate the emotional circuitry primarily at the level of the PAG.10
Lesions of the volitional pathway have been correlated with conditions of PBA, whereas direct activation of the emotional pathway tended to lead to emotional lability or the crying and laughing behaviors observed in dacrystic or gelastic epilepsy.10 The pivotal nature of the regulation occurring at the PAG has guided treatment options. Neurotransmitter receptors most closely associated with this region include glutamatergic N-methyl-
When to screen for PBA
Ask the right question. PBA as a disease state likely has been widely under-reported, under-recognized, and misdiagnosed (typically, as a primary mood disorder).9 Three factors underscore this problem:
- Patients do not specifically report symptoms of affective disturbance (perhaps because they lack a vocabulary to separate concepts of mood and affect)
- Physicians do not ask patients about separations of mood and affect
- Perhaps most importantly, PBA lacks a general awareness and understanding.
Co-occurring mood disorders also may thwart PBA detection. One study of PBA in Alzheimer’s dementia found that 53% of patients with symptoms consistent with PBA also had a distinct mood disorder.17 This suggests that a PBA-specific screening test is needed for accurate diagnosis.
A single question might best refine the likelihood that a patient has PBA: “Do you ever cry for no reason?” In primary psychiatric illness, crying typically is associated with a specific trigger (eg, depressed mood, despair, anxiety). A patient’s inability to identify a trigger for crying suggests the pathological separation of mood and affect—the core of PBA, and worthy of further investigation.
Clinical rating scales that correlate to disease severity appear to be the most effective in identifying PBA. The PRISM study, to date the largest clinic-based study of PBA symptoms, used the Center for Neurologic Study-Liability Scale (CNS-LS) to gauge the presence and severity of PBA symptoms.1 A 7-question, patient self-administered tool, the CNS-LS is graded on a 5-point Likert scale. A score ≥13 has high sensitivity and specificity for diagnosis of PBA, compared with physician diagnosis.
Another option, the 16-question Pathological Laughing and Crying Scale, is a clinician-administered screening tool. Again, a score ≥13 is consistent with symptoms required for a PBA diagnosis.
Treating PBA symptoms
Until recently, most pharmacotherapeutic interventions for PBA were based on off-label use of tricyclic antidepressants (TCAs) or selective serotonin reuptake inhibitors (SSRIs). From 1980 to 2010, only 7 of 22 case reports or trials of TCAs or SSRIs for PBA were randomized, double-blind, and placebo-controlled. Five had 12 to 28 patients, and 2 had 106 and 128 patients, respectively. Only 1 controlled trial included a validated symptom severity scale, and none included a scale validated for PBA.18
In particular, imipramine and nortriptyline were studied for managing PBA in patients with stroke; amitriptyline, in patients with MS; and various SSRIs, in patients with stroke.11 Response of PBA symptoms to antidepressant therapy was greater in all placebo-controlled trials than response to placebo.18 As seen in pharmacotherapy of depression, the lower burden of adverse effects and overall better tolerability of SSRIs resulted in their preferred use over TCAs. In some cases, the side effects of TCAs can be leveraged for therapeutic gain. If insomnia is a problem, a nighttime dose of a TCA could ameliorate this. Similarly, if a patient has sialorrhea, the anticholinergic effect of a TCA may show some benefit.19
Dextromethorphan plus quinidine. Dextromethorphan has long been of interest for a variety of neurodegenerative diseases. Studies of its efficacy were largely unsuccessful, however, because rapid metabolism by cytochrome P450 (CYP) 2D6 prevented CNS penetration.20 Quinidine is an avid inhibitor of CYP2D6, even at very low dosages. Adding quinidine to dextromethorphan limits metabolism, allowing dextromethorphan to accumulate to a plasma concentration sufficient to penetrate the CNS.12 In 2010, the combination agent dextromethorphan hydrobromide (20 mg)/quinidine (10 mg) (DM/Q) became the first treatment to receive FDA approval for managing PBA.11
Mechanism of action. The exact mechanism of DM/Q in PBA remains unknown. Dextromethorphan is an agonist of sigma-1 receptors and a relatively specific noncompetitive antagonist of NMDA receptors. It also has been shown to modulate glutamate and serotonin neurotransmission and ion channel function.20 Sigma-1 receptors are concentrated in the brainstem and parts of the cerebellum that are thought to coordinate motor emotional responses. Agonism of sigma-1 receptors on glutamatergic neurons has been proposed to limit release of glutamate from the presynaptic neuron while also limiting downstream transmission of glutamatergic signal in postsynaptic neurons.
Clinical trials. Two large trials have demonstrated efficacy of DM/Q in PBA. STAR was a 12-week, double-blind, placebo-controlled trial with 326 patients diagnosed with ALS or MS who showed PBA symptoms (CNS-LS score ≥13). Compared with placebo, DM/Q use was associated with significantly reduced (P < .01) daily episodes of PBA at 2, 4, 8, and 12 weeks.20 The effect was rapid, with 30% fewer PBA episodes after the first week (P < .0167). At 12 weeks, 51% of patients on DM/Q had been symptom-free for at least 2 weeks.
The PRISM II study examined the efficacy of DM/Q in managing PBA in 102 individuals with dementia, 92 with stroke, and 67 with TBI. After 30 and 90 days, CNL-LS scores were significantly reduced (P < .001) compared with baseline scores.20
Prescribing information. Dextromethorphan—typically in the form of cough syrup—has been implicated as a substance of abuse. A placebo-controlled trial demonstrated that co-administering quinidine with dextromethorphan limits measures of positive reinforcement, such as euphoria and drug liking. This suggests that quinidine may be used to reduce abuse of dextromethorphan.20 As such, the abuse potential of DM/Q appears to be low.
The most common adverse effects reported with DM/Q are diarrhea, dizziness, and cough.12 Notably, patients who received DM/Q in the STAR trial were more likely to report dizziness than those receiving placebo (10.3% vs 5.5%), but patients receiving placebo were more likely to fall.21,22
Package labeling warns that DM/Q causes dose-dependent QTc prolongation.21 Quinidine can be associated with significant QTc prolongation when dosed at antiarrhythmic levels, although mean plasma concentrations found with the 10 mg of quinidine in the approved DM/Q formulation are 1% to 3% of those associated with typical dosages used in antiarrhythmic therapy. Electrophysiology studies of quinidine 10 mg dosed every 12 hours have demonstrated a mean QTc increase at steady state of 6.8 milliseconds, compared with 9.1 milliseconds for a reference control (moxifloxacin).12,21
Although this would seem to indicate a relatively low risk of clinically significant QTc prolongation at these ultra-low dosages of quinidine, it may be advisable to obtain an initial pre-dose and post-dose ECG and longitudinally monitor the QTc interval in patients with conditions that predispose to cardiac arrhythmias. Because quinidine inhibits CYP2D6, use caution when prescribing and monitoring other medications metabolized by this pathway.
Bottom Line
1. Brooks BR, Crumpacker D, Fellus J, et al. PRISM: a novel research tool to assess the prevalence of pseudobulbar affect symptoms across neurological conditions. PLoS One. 2013;8(8):e72232. doi: 10.1371/journal.pone.0072232.
2. Cruz MP. Nuedexta for the treatment of pseudobulbar affect: a condition of involuntary laughing and crying. P T. 2013;38(6):325-328.
3. Work SS, Colamonico JA, Bradley WG, et al. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586-601.
4. Arciniegas DB, Lauterbach EC, Anderson KE, et al. The differential diagnosis of pseudobulbar affect (PBA). Distinguishing PBA among disorders of mood and affect. Proceedings of a roundtable meeting. CNS Spectr. 2005;10(5):1-14; quiz 15-16.
5. Darwin C. The expression of the emotions in man and animals. London, United Kingdom: John Murray; 1872.
6. Oppenheim H, Siemerling E. Mitteilungen über Pseudobulbärparalyse und akute Bulbärparalyse. Berl Kli Woch. 1886;46.
7. Wilson SA. Original papers: some problems in neurology. J Neurol Psychopathol. 1924;4(16):299-333.
8. Poeck K, Risso M, Pilleri G. Contribution to the pathophysiology and clinical systematology of pathological laughing and crying [in German]. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr. 1963;204:181-198.
9. Cummings JL, Gilbart J, Andersen G. Pseudobulbar affect - a disabling but under-recognised consequence of neurological disease and brain injury. Eur Neurol Rev. 2013;8(2):74-81.
10. Lauterbach EC, Cummings JL, Kuppuswamy PS. Toward a more precise, clinically–informed pathophysiology of pathological laughing and crying. Neurosci Biobehav Rev. 2013;37(8):1893-1916.
11. Pioro EP. Review of dextromethorphan 20 mg/quinidine 10 mg (Nuedexta(®)) for pseudobulbar affect. Neurol Ther. 2014;3(1):15-28.
12. Schoedel KA, Morrow SA, Sellers EM. Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatr Dis Treat. 2014;10:1161-1174.
13. Li Z, Luo S, Ou J, et al. Persistent pseudobulbar affect secondary to acute disseminated encephalomyelitis. Socioaffect Neurosci Psychol. 2015;5:26210. doi: 10.3402/snp.v5.26210.
14. Pattee GL, Wymer JP, Lomen-Hoerth C, et al. An open-label multicenter study to assess the safety of dextromethorphan/quinidine in patients with pseudobulbar affect associated with a range of underlying neurological conditions. Curr Med Res Opin. 2014;30(11):2255-2265.
15. Strowd RE, Cartwright MS, Okun MS, et al. Pseudobulbar affect: prevalence and quality of life impact in movement disorders. J Neurol. 2010;257(8):1382-1387.
16. Colamonico J, Formella A, Bradley W. Pseudobulbar affect: burden of illness in the USA. Adv Ther. 2012;29(9):775-798.
17. Starkstein SE, Migliorelli R, Tesón A, et al. Prevalence and clinical correlates of pathological affective display in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1995;59(1):55-60.
18. Pioro EP. Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs. 2011;71(9):1193-1207.
19. Ahmed A, Simmons A. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483-489.
20. Yang LP, Deeks ED. Dextromethorphan/quinidine: a review of its use in adults with pseudobulbar affect. Drugs. 2015;75(1):83-90.
21. Nuedexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals, Inc.; 2015.
22. Pioro EP, Brooks BR, Cummings J, et al; Safety, Tolerability, and Efficacy trial of AVP-923 in PBA Investigators. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68(5):693-702.
1. Brooks BR, Crumpacker D, Fellus J, et al. PRISM: a novel research tool to assess the prevalence of pseudobulbar affect symptoms across neurological conditions. PLoS One. 2013;8(8):e72232. doi: 10.1371/journal.pone.0072232.
2. Cruz MP. Nuedexta for the treatment of pseudobulbar affect: a condition of involuntary laughing and crying. P T. 2013;38(6):325-328.
3. Work SS, Colamonico JA, Bradley WG, et al. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586-601.
4. Arciniegas DB, Lauterbach EC, Anderson KE, et al. The differential diagnosis of pseudobulbar affect (PBA). Distinguishing PBA among disorders of mood and affect. Proceedings of a roundtable meeting. CNS Spectr. 2005;10(5):1-14; quiz 15-16.
5. Darwin C. The expression of the emotions in man and animals. London, United Kingdom: John Murray; 1872.
6. Oppenheim H, Siemerling E. Mitteilungen über Pseudobulbärparalyse und akute Bulbärparalyse. Berl Kli Woch. 1886;46.
7. Wilson SA. Original papers: some problems in neurology. J Neurol Psychopathol. 1924;4(16):299-333.
8. Poeck K, Risso M, Pilleri G. Contribution to the pathophysiology and clinical systematology of pathological laughing and crying [in German]. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr. 1963;204:181-198.
9. Cummings JL, Gilbart J, Andersen G. Pseudobulbar affect - a disabling but under-recognised consequence of neurological disease and brain injury. Eur Neurol Rev. 2013;8(2):74-81.
10. Lauterbach EC, Cummings JL, Kuppuswamy PS. Toward a more precise, clinically–informed pathophysiology of pathological laughing and crying. Neurosci Biobehav Rev. 2013;37(8):1893-1916.
11. Pioro EP. Review of dextromethorphan 20 mg/quinidine 10 mg (Nuedexta(®)) for pseudobulbar affect. Neurol Ther. 2014;3(1):15-28.
12. Schoedel KA, Morrow SA, Sellers EM. Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatr Dis Treat. 2014;10:1161-1174.
13. Li Z, Luo S, Ou J, et al. Persistent pseudobulbar affect secondary to acute disseminated encephalomyelitis. Socioaffect Neurosci Psychol. 2015;5:26210. doi: 10.3402/snp.v5.26210.
14. Pattee GL, Wymer JP, Lomen-Hoerth C, et al. An open-label multicenter study to assess the safety of dextromethorphan/quinidine in patients with pseudobulbar affect associated with a range of underlying neurological conditions. Curr Med Res Opin. 2014;30(11):2255-2265.
15. Strowd RE, Cartwright MS, Okun MS, et al. Pseudobulbar affect: prevalence and quality of life impact in movement disorders. J Neurol. 2010;257(8):1382-1387.
16. Colamonico J, Formella A, Bradley W. Pseudobulbar affect: burden of illness in the USA. Adv Ther. 2012;29(9):775-798.
17. Starkstein SE, Migliorelli R, Tesón A, et al. Prevalence and clinical correlates of pathological affective display in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1995;59(1):55-60.
18. Pioro EP. Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs. 2011;71(9):1193-1207.
19. Ahmed A, Simmons A. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag. 2013;9:483-489.
20. Yang LP, Deeks ED. Dextromethorphan/quinidine: a review of its use in adults with pseudobulbar affect. Drugs. 2015;75(1):83-90.
21. Nuedexta [package insert]. Aliso Viejo, CA: Avanir Pharmaceuticals, Inc.; 2015.
22. Pioro EP, Brooks BR, Cummings J, et al; Safety, Tolerability, and Efficacy trial of AVP-923 in PBA Investigators. Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Ann Neurol. 2010;68(5):693-702.
Mnemonics in a mnutshell: 32 aids to psychiatric diagnosis
From SIG: E CAPS to CAGE and WWHHHHIMPS, mnemonics help practitioners and trainees recall important lists (such as criteria for depression, screening questions for alcoholism, or life-threatening causes of delirium, respectively). Mnemonics’ efficacy rests on the principle that grouped information is easier to remember than individual points of data.
Not everyone loves mnemonics, but recollecting diagnostic criteria is useful in clinical practice and research, on board examinations, and for insurance reimbursement. Thus, tools that assist in recalling diagnostic criteria have a role in psychiatric practice and teaching.
In this article, we present 32 mnemonics to help clinicians diagnose:
- affective disorders (Box 1)1,2
- anxiety disorders (Box 2)3-6
- medication adverse effects (Box 3)7,8
- personality disorders (Box 4)9-11
- addiction disorders (Box 5)12,13
- causes of delirium (Box 6).14
We also discuss how mnemonics improve one’s memory, based on the principles of learning theory.
How mnemonics work
A mnemonic—from the Greek word “mnemonikos” (“of memory”)—links new data with previously learned information. Mnemonics assist in learning by reducing the amount of information (“cognitive load”) that needs to be stored for long-term processing and retrieval.15
Memory, defined as the “persistence of learning in a state that can be revealed at a later time,”16 can be divided into 2 types:
- declarative (a conscious recollection of facts, such as remembering a relative’s birthday)
- procedural (skills-based learning, such as riding a bicycle).
Declarative memory has a conscious component and may be mediated by the medial temporal lobe and cortical association structures. Procedural memory has less of a conscious component; it may involve the basal ganglia, cerebellum, and a variety of cortical sensory-perceptive regions.17
| Depression SIG: E CAPS* Suicidal thoughts Interests decreased Guilt Energy decreased Concentration decreased Appetite disturbance (increased or decreased) Psychomotor changes (agitation or retardation) Sleep disturbance (increased or decreased) * Created by Carey Gross, MD | Dysthymia HE’S 2 SAD2 Hopelessness Energy loss or fatigue Self-esteem is low 2 years minimum of depressed mood most of the day, for more days than not Sleep is increased or decreased Appetite is increased or decreased Decision-making or concentration is impaired | Mania DIG FAST Distractibility Indiscretion Grandiosity Flight of ideas Activity increase Sleep deficit Talkativeness |
| Depression C GASP DIE1 Concentration decreased Guilt Appetite Sleep disturbance Psychomotor agitation or retardation Death or suicide (thoughts or acts of) Interests decreased Energy decreased | Hypomania TAD HIGH Talkative Attention deficit Decreased need for sleep High self-esteem/grandiosity Ideas that race Goal-directed activity increased High-risk activity | Mania DeTeR the HIGH* Distractibility Talkativeness Reckless behavior Hyposomnia Ideas that race Grandiosity Hypersexuality * Created by Carey Gross, MD |
Declarative memory can be subdivided into working memory and long-term memory.
With working memory, new items of information are held briefly so that encoding and eventual storage can take place.
Working memory guides decision-making and future planning and is intricately related to attention.18-21 Functional MRI and positron emission tomography as well as neurocognitive testing have shown that working memory tasks activate the prefrontal cortex and brain regions specific to language and visuospatial memory.
The hippocampus is thought to rapidly absorb new information, and this data is consolidated and permanently stored via the prefrontal cortex.22-26 Given the hippocampus’ limited storage capacity, new information (such as what you ate for breakfast 3 weeks ago) will disappear if it is not repeated regularly.17
Long-term memory, on the other hand, is encoded knowledge that is linked to facts learned in the past; it is consolidated in the brain and can be readily retrieved. Neuroimaging studies have demonstrated opposing patterns of activation in the hippocampus and prefrontal cortex, depending on whether the memory being recalled is:
- new (high hippocampal activity, low prefrontal cortex activity)
- old (low hippocampal activity, high prefrontal cortex activity).27
Mnemonics are thought to affect working memory by reducing the introduced cognitive load and increasing the efficiency of memory acquisition and encoding. They reduce cognitive load by grouping objects into a single verbal or visual cue that can be introduced into working memory. Learning is optimized when the load on working memory is minimized, enabling long-term memory to be facilitated.28
| Generalized anxiety disorder Worry WARTS3 Wound up Worn-out Absentminded Restless Touchy Sleepless | Posttraumatic stress disorder TRAUMA5 Traumatic event Re-experience Avoidance Unable to function Month or more of symptoms Arousal increased | Anxiety disorder due to a general medical condition Physical Diseases That Have Commonly Appeared Anxious: Pheochromocytoma Diabetes mellitus Temporal lobe epilepsy Hyperthyroidism Carcinoid Alcohol withdrawal Arrhythmias |
| Generalized anxiety disorder WATCHERS4 Worry Anxiety Tension in muscles Concentration difficulty Hyperarousal (or irritability) Energy loss Restlessness Sleep disturbance | Posttraumatic stress disorder DREAMS6 Disinterest in usual activities Re-experience Event preceding symptoms Avoidance Month or more of symptoms Sympathetic arousal |
| Antidepressant discontinuation syndrome FINISH7 Flu-like symptoms Insomnia Nausea Imbalance Sensory disturbances Hyperarousal (anxiety/agitation) | Neuroleptic malignant syndrome FEVER8 Fever Encephalopathy Vital sign instability Elevated WBC/CPK Rigidity WBC: white blood cell count CPK: creatine phosphokinase | Serotonin syndrome HARMED Hyperthermia Autonomic instability Rigidity Myoclonus Encephalopathy Diaphoresis |
Mnemonics may use rhyme, music, or visual cues to enhance memory. Most mnemonics used in medical practice and education are word-based, including:
- Acronyms—words, each letter of which stands for a particular piece of information to be recalled (such as RICE for treatment of a sprained joint: rest, ice, compression, elevation).
- Acrostics—sentences with the first letter of each word prompting the desired recollection (such as “To Zanzibar by motor car” for the branches of the facial nerve: temporal, zygomatic, buccal, mandibular, cervical).
- Alphabetical sequences (such as ABCDE of trauma assessment: airway, breathing, circulation, disability, exposure).29
An appropriate teaching tool?
Dozens of mnemonics addressing psychiatric diagnosis and treatment have been published, but relatively few are widely used. Psychiatric educators may resist teaching with mnemonics, believing they might erode a humanistic approach to patients by reducing psychopathology to “a laundry list” of symptoms and the art of psychiatric diagnosis to a “check-box” endeavor. Mnemonics that use humor may be rejected as irreverent or unprofessional.30 Publishing a novel mnemonic may be viewed with disdain by some as an “easy” way of padding a curriculum vitae.
| Paranoid personality disorder SUSPECT9 Spousal infidelity suspected Unforgiving (bears grudges) Suspicious Perceives attacks (and reacts quickly) Enemy or friend? (suspects associates and friends) Confiding in others is feared Threats perceived in benign events | Schizotypal personality disorder ME PECULIAR9 Magical thinking Experiences unusual perceptions Paranoid ideation Eccentric behavior or appearance Constricted or inappropriate affect Unusual thinking or speech Lacks close friends Ideas of reference Anxiety in social situations Rule out psychotic or pervasive developmental disorders | Borderline personality disorder IMPULSIVE10 Impulsive Moodiness Paranoia or dissociation under stress Unstable self-image Labile intense relationships Suicidal gestures Inappropriate anger Vulnerability to abandonment Emptiness (feelings of) | Histrionic personality disorder PRAISE ME9 Provocative or seductive behavior Relationships considered more intimate than they are Attention (need to be the center of) Influenced easily Style of speech (impressionistic, lacking detail) Emotions (rapidly shifting, shallow) Make up (physical appearance used to draw attention to self) Emotions exaggerated | Narcissistic personality disorder GRANDIOSE11 Grandiose Requires attention Arrogant Need to be special Dreams of success and power Interpersonally exploitative Others (unable to recognize feelings/needs of) Sense of entitlement Envious | Dependent personality disorder RELIANCE9 Reassurance required Expressing disagreement difficult Life responsibilities assumed by others Initiating projects difficult Alone (feels helpless and uncomfortable when alone) Nurturance (goes to excessive lengths to obtain) Companionship sought urgently when a relationship ends Exaggerated fears of being left to care for self |
| Schizoid personality disorder DISTANT9 Detached or flattened affect Indifferent to criticism or praise Sexual experiences of little interest Tasks done solitarily Absence of close friends Neither desires nor enjoys close relationships Takes pleasure in few activities | Antisocial personality disorder CORRUPT9 Cannot conform to law Obligations ignored Reckless disregard for safety Remorseless Underhanded (deceitful) Planning insufficient (impulsive) Temper (irritable and aggressive) | Borderline personality disorder DESPAIRER* Disturbance of identity Emotionally labile Suicidal behavior Paranoia or dissociation Abandonment (fear of) Impulsive Relationships unstable Emptiness (feelings of) Rage (inappropriate) * Created by Jason P. Caplan, MD | Histrionic personality disorder ACTRESSS* Appearance focused Center of attention Theatrical Relationships (believed to be more intimate than they are) Easily influenced Seductive behavior Shallow emotions Speech (impressionistic and vague) * Created by Jason P. Caplan, MD | Avoidant personality disorder CRINGES9 Criticism or rejection preoccupies thoughts in social situations Restraint in relationships due to fear of shame Inhibited in new relationships Needs to be sure of being liked before engaging socially Gets around occupational activities with need for interpersonal contact Embarrassment prevents new activity or taking risks Self viewed as unappealing or inferior | Obsessive-compulsive personality disorder SCRIMPER* Stubborn Cannot discard worthless objects Rule obsessed Inflexible Miserly Perfectionistic Excludes leisure due to devotion to work Reluctant to delegate to others * Created by Jason P. Caplan, MD |
Entire Web sites exist to share mnemonics for medical education (see Related Resources). Thus it is likely that trainees are using them with or without their teachers’ supervision. Psychiatric educators need to be aware of the mnemonics their trainees are using and to:
- screen these tools for factual errors (such as incomplete diagnostic criteria)
- remind trainees that although mnemonics are useful, psychiatrists should approach patients as individuals without the prejudice of a potentially pejorative label.
Our methodology
In preparing this article, we gathered numerous mnemonics (some published and some novel) designed to capture the learner’s attention and impart information pertinent to psychiatric diagnosis and treatment. Whenever possible, we credited each mnemonic to its creator, but—given the difficulty in confirming authorship of (what in many cases has become) oral history—we’ve listed some mnemonics without citation.
Our list is far from complete because we likely are unaware of many mnemonics, and we have excluded some that seemed obscure, unwieldy, or redundant. We have not excluded mnemonics that some may view as pejorative but merely report their existence. Including them does not mean that we endorse them.
This article lists 32 mnemonics related to psychiatric diagnosis. Thus, it seems odd that an informal survey of >60 residents at the Massachusetts General Hospital (MGH)/McLean Residency Training Program in Psychiatry revealed that most were aware of only 2 or 3 psychiatric mnemonics, typically:
- SIG: E CAPS (a tool to recall the criteria for depression)
- DIG FAST (a list of criteria for diagnosing mania)
- WWHHHHIMPS (a tool for recalling life-threatening causes of delirium).
Although this unscientific survey may be biased because faculty or trainees at MGH created the above 3 mnemonics, it nonetheless begs the question of what qualities make a mnemonic memorable.
Learning theory provides several clues. George Miller’s classic 1956 paper, “The magical number seven, plus or minus two: some limits on our capacity for processing information,” discussed the finding that 7 seems to be the upper limit of individual pieces of data that can be easily remembered.31 Research also has shown that recruiting the limbic system (potentially through the use of humor) aids in the recall of otherwise dry, cortical information.32,33
Intuitively, it would seem that nonrepeating letters would facilitate the recall of the linked data, allowing each letter to provide a distinct cue, without any clouding by redundancy. Of the 3 most popular psychiatric mnemonics, however, only DIG FAST fits the learning theory. It contains 7 letters, repeats no letters, and has the limbic cue of allowing the learner to imagine a person with mania digging furiously.
| Substance dependence ADDICTeD12 Activities are given up or reduced Dependence, physical: tolerance Dependence, physical: withdrawal Intrapersonal (Internal) consequences, physical or psychological Can’t cut down or control use Time-consuming Duration or amount of use is greater than intended | Substance abuse WILD12 Work, school, or home role obligation failures Interpersonal or social consequences Legal problems Dangerous use | Alcohol abuse CAGE13 Have you ever felt you should CUT DOWN your drinking? Have people ANNOYED you by criticizing your drinking? Have you ever felt bad or GUILTY about your drinking? Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover (EYE-OPENER)? |
SIG: E CAPS falls within the range of 7 plus or minus 2, includes a limbic cue (although often forgotten, it refers to the prescription of energy capsules for depression), but repeats the letter S.
WWHHHHIMPS, with 10 letters, exceeds the recommended range, repeats the W (appearing twice) and the H (appearing 4 times), and provides no clear limbic cue.
| Causes I WATCH DEATH Infection Withdrawal Acute metabolic Trauma CNS pathology Hypoxia Deficiencies Endocrinopathies Acute vascular Toxins or drugs Heavy metals | Life-threatening causes WWHHHHIMPS* Wernicke’s encephalopathy Withdrawal Hypertensive crisis Hypoperfusion/hypoxia of the brain Hypoglycemia Hyper/hypothermia Intracranial process/infection Metabolic/meningitis Poisons Status epilepticus * Created by Gary W. Small, MD | Deliriogenic medications ACUTE CHANGE IN MS14 Antibiotics Cardiac drugs Urinary incontinence drugs Theophylline Ethanol Corticosteroids H2 blockers Antiparkinsonian drugs Narcotics Geriatric psychiatric drugs ENT drugs Insomnia drugs NSAIDs Muscle relaxants Seizure medicines |
It may be that recruiting the limbic system provides the greatest likelihood of recall. Recruiting this system may add increased valence to a particular mnemonic for a specific individual, but this same limbic valence may limit its usefulness in a professional context.
- Free searchable database of medical mnemonics. www.medicalmnemonics.com.
- Robinson DJ. Mnemonics and more for psychiatry. Port Huron, MI: Rapid Psychler Press, 2001.
1. Abraham PF, Shirley ER. New mnemonic for depressive symptoms. Am J Psychiatry 2006;163(2):329-30.
2. Christman DS. “HE’S 2 SAD” detects dysthymic disorder. Current Psychiatry 2008;7(3):120.-
3. Coupland NJ. Worry WARTS have generalized anxiety disorder. Can J Psychiatry 2002;47(2):197.-
4. Berber MJ. WATCHERS: recognizing generalized anxiety disorder. J Clin Psychiatry 2000;61(6):447.-
5. Khouzam HR. A simple mnemonic for the diagnostic criteria for post-traumatic stress disorder. West J Med 2001;174(6):424.-
6. Short DD, Workman EA, Morse JH, Turner RL. Mnemonics for eight DSM-III-R disorders. Hosp Community Psychiatry 1992;43(6):642-4.
7. Berber MJ. FINISH: remembering the discontinuation syndrome. Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, and Hyperarousal (anxiety/agitation). J Clin Psychiatry 1998;59(5):255.-
8. Christensen RC. Identify neuroleptic malignant syndrome with FEVER. Current Psychiatry 2005;4(7):102.-
9. Pinkofsky HB. Mnemonics for DSM-IV personality disorders. Psychiatr Serv 1997;48(9):1197-8.
10. Senger HL. Borderline mnemonic. Am J Psychiatry 1997;154(9):1321.-
11. Kim SI, Swanson TA, Caplan JP, eds. Underground clinical vignettes step 2: psychiatry. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:130.
12. Bogenschutz MP, Quinn DK. Acronyms for substance use disorders. J Clin Psychiatry 2001;62(6):474-5.
13. Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252(14):1905-7.
14. Flaherty JH. Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter remedies: causes of confusion. Clin Geriatr Med 1998;14:101-27.
15. Sweller J. Cognitive load theory, learning difficulty, and instructional design. Learn Instr 1994;4:295-312.
16. Squire LR. Memory and brain. New York, NY: Oxford University Press; 1987.
17. DeLuca J, Lengenfelder J, Eslinger P. Memory and learning. In: Rizzo M, Eslinger P, eds. Principles and practice of behavioral neurology and neuropsychology. Philadelphia, PA: Saunders; 2004:251.
18. Dash PK, Moore AN, Kobori N, et al. Molecular activity underlying working memory. Learn Mem 2007;14:554-63.
19. Awh E, Vogel EK, Oh SH. Interactions between attention and working memory. Neuroscience 2006;139:201-8.
20. Knudson EI. Fundamental components of attention. Ann Rev Neurosci 2007;30:57-78.
21. Postle BR. Working memory as an emergent property of the mind and brain. Neuroscience 2006;139:23-36.
22. Fletcher PC, Henson RN. Frontal lobes and human memory: Insights from functional neuroimaging. Brain 2001;124:849-81.
23. Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Ann Rev Neurosci 2001;24:167-202.
24. Schumacher EH, Lauber E, Awh E, et al. PET evidence for a modal verbal working memory system. Neuroimage 1996;3:79-88.
25. Smith EE, Jonides J, Koeppe RA. Dissociating verbal and spatial working memory using PET. Cereb Cortex 1996;6:11-20.
26. Wager TD, Smith EE. Neuroimaging studies of working memory: a meta-analysis. Cogn Affect Behav Neurosci 2003;3(4):255-74.
27. Frankland PW, Bontempi B. The organization of recent and remote memories. Nat Rev Neurosci 2005;6:119-30.
28. Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci 1988;12(1):257-85.
29. Beitz JM. Unleashing the power of memory: the mighty mnemonic. Nurse Educ 1997;22(2):25-9.
30. Larson EW. Criticism of mnemonic device. Am J Psychiatry 1990;147(7):963-4.
31. Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev 1956;63:81-97.
32. Schmidt SR. Effects of humor on sentence memory. J Exp Psychol Learn Mem Cogn 1994;20(4):953-67.
33. Lippman LG, Dunn ML. Contextual connections within puns: effects on perceived humor and memory. J Gen Psychol 2000;127(2):185-97.
From SIG: E CAPS to CAGE and WWHHHHIMPS, mnemonics help practitioners and trainees recall important lists (such as criteria for depression, screening questions for alcoholism, or life-threatening causes of delirium, respectively). Mnemonics’ efficacy rests on the principle that grouped information is easier to remember than individual points of data.
Not everyone loves mnemonics, but recollecting diagnostic criteria is useful in clinical practice and research, on board examinations, and for insurance reimbursement. Thus, tools that assist in recalling diagnostic criteria have a role in psychiatric practice and teaching.
In this article, we present 32 mnemonics to help clinicians diagnose:
- affective disorders (Box 1)1,2
- anxiety disorders (Box 2)3-6
- medication adverse effects (Box 3)7,8
- personality disorders (Box 4)9-11
- addiction disorders (Box 5)12,13
- causes of delirium (Box 6).14
We also discuss how mnemonics improve one’s memory, based on the principles of learning theory.
How mnemonics work
A mnemonic—from the Greek word “mnemonikos” (“of memory”)—links new data with previously learned information. Mnemonics assist in learning by reducing the amount of information (“cognitive load”) that needs to be stored for long-term processing and retrieval.15
Memory, defined as the “persistence of learning in a state that can be revealed at a later time,”16 can be divided into 2 types:
- declarative (a conscious recollection of facts, such as remembering a relative’s birthday)
- procedural (skills-based learning, such as riding a bicycle).
Declarative memory has a conscious component and may be mediated by the medial temporal lobe and cortical association structures. Procedural memory has less of a conscious component; it may involve the basal ganglia, cerebellum, and a variety of cortical sensory-perceptive regions.17
| Depression SIG: E CAPS* Suicidal thoughts Interests decreased Guilt Energy decreased Concentration decreased Appetite disturbance (increased or decreased) Psychomotor changes (agitation or retardation) Sleep disturbance (increased or decreased) * Created by Carey Gross, MD | Dysthymia HE’S 2 SAD2 Hopelessness Energy loss or fatigue Self-esteem is low 2 years minimum of depressed mood most of the day, for more days than not Sleep is increased or decreased Appetite is increased or decreased Decision-making or concentration is impaired | Mania DIG FAST Distractibility Indiscretion Grandiosity Flight of ideas Activity increase Sleep deficit Talkativeness |
| Depression C GASP DIE1 Concentration decreased Guilt Appetite Sleep disturbance Psychomotor agitation or retardation Death or suicide (thoughts or acts of) Interests decreased Energy decreased | Hypomania TAD HIGH Talkative Attention deficit Decreased need for sleep High self-esteem/grandiosity Ideas that race Goal-directed activity increased High-risk activity | Mania DeTeR the HIGH* Distractibility Talkativeness Reckless behavior Hyposomnia Ideas that race Grandiosity Hypersexuality * Created by Carey Gross, MD |
Declarative memory can be subdivided into working memory and long-term memory.
With working memory, new items of information are held briefly so that encoding and eventual storage can take place.
Working memory guides decision-making and future planning and is intricately related to attention.18-21 Functional MRI and positron emission tomography as well as neurocognitive testing have shown that working memory tasks activate the prefrontal cortex and brain regions specific to language and visuospatial memory.
The hippocampus is thought to rapidly absorb new information, and this data is consolidated and permanently stored via the prefrontal cortex.22-26 Given the hippocampus’ limited storage capacity, new information (such as what you ate for breakfast 3 weeks ago) will disappear if it is not repeated regularly.17
Long-term memory, on the other hand, is encoded knowledge that is linked to facts learned in the past; it is consolidated in the brain and can be readily retrieved. Neuroimaging studies have demonstrated opposing patterns of activation in the hippocampus and prefrontal cortex, depending on whether the memory being recalled is:
- new (high hippocampal activity, low prefrontal cortex activity)
- old (low hippocampal activity, high prefrontal cortex activity).27
Mnemonics are thought to affect working memory by reducing the introduced cognitive load and increasing the efficiency of memory acquisition and encoding. They reduce cognitive load by grouping objects into a single verbal or visual cue that can be introduced into working memory. Learning is optimized when the load on working memory is minimized, enabling long-term memory to be facilitated.28
| Generalized anxiety disorder Worry WARTS3 Wound up Worn-out Absentminded Restless Touchy Sleepless | Posttraumatic stress disorder TRAUMA5 Traumatic event Re-experience Avoidance Unable to function Month or more of symptoms Arousal increased | Anxiety disorder due to a general medical condition Physical Diseases That Have Commonly Appeared Anxious: Pheochromocytoma Diabetes mellitus Temporal lobe epilepsy Hyperthyroidism Carcinoid Alcohol withdrawal Arrhythmias |
| Generalized anxiety disorder WATCHERS4 Worry Anxiety Tension in muscles Concentration difficulty Hyperarousal (or irritability) Energy loss Restlessness Sleep disturbance | Posttraumatic stress disorder DREAMS6 Disinterest in usual activities Re-experience Event preceding symptoms Avoidance Month or more of symptoms Sympathetic arousal |
| Antidepressant discontinuation syndrome FINISH7 Flu-like symptoms Insomnia Nausea Imbalance Sensory disturbances Hyperarousal (anxiety/agitation) | Neuroleptic malignant syndrome FEVER8 Fever Encephalopathy Vital sign instability Elevated WBC/CPK Rigidity WBC: white blood cell count CPK: creatine phosphokinase | Serotonin syndrome HARMED Hyperthermia Autonomic instability Rigidity Myoclonus Encephalopathy Diaphoresis |
Mnemonics may use rhyme, music, or visual cues to enhance memory. Most mnemonics used in medical practice and education are word-based, including:
- Acronyms—words, each letter of which stands for a particular piece of information to be recalled (such as RICE for treatment of a sprained joint: rest, ice, compression, elevation).
- Acrostics—sentences with the first letter of each word prompting the desired recollection (such as “To Zanzibar by motor car” for the branches of the facial nerve: temporal, zygomatic, buccal, mandibular, cervical).
- Alphabetical sequences (such as ABCDE of trauma assessment: airway, breathing, circulation, disability, exposure).29
An appropriate teaching tool?
Dozens of mnemonics addressing psychiatric diagnosis and treatment have been published, but relatively few are widely used. Psychiatric educators may resist teaching with mnemonics, believing they might erode a humanistic approach to patients by reducing psychopathology to “a laundry list” of symptoms and the art of psychiatric diagnosis to a “check-box” endeavor. Mnemonics that use humor may be rejected as irreverent or unprofessional.30 Publishing a novel mnemonic may be viewed with disdain by some as an “easy” way of padding a curriculum vitae.
| Paranoid personality disorder SUSPECT9 Spousal infidelity suspected Unforgiving (bears grudges) Suspicious Perceives attacks (and reacts quickly) Enemy or friend? (suspects associates and friends) Confiding in others is feared Threats perceived in benign events | Schizotypal personality disorder ME PECULIAR9 Magical thinking Experiences unusual perceptions Paranoid ideation Eccentric behavior or appearance Constricted or inappropriate affect Unusual thinking or speech Lacks close friends Ideas of reference Anxiety in social situations Rule out psychotic or pervasive developmental disorders | Borderline personality disorder IMPULSIVE10 Impulsive Moodiness Paranoia or dissociation under stress Unstable self-image Labile intense relationships Suicidal gestures Inappropriate anger Vulnerability to abandonment Emptiness (feelings of) | Histrionic personality disorder PRAISE ME9 Provocative or seductive behavior Relationships considered more intimate than they are Attention (need to be the center of) Influenced easily Style of speech (impressionistic, lacking detail) Emotions (rapidly shifting, shallow) Make up (physical appearance used to draw attention to self) Emotions exaggerated | Narcissistic personality disorder GRANDIOSE11 Grandiose Requires attention Arrogant Need to be special Dreams of success and power Interpersonally exploitative Others (unable to recognize feelings/needs of) Sense of entitlement Envious | Dependent personality disorder RELIANCE9 Reassurance required Expressing disagreement difficult Life responsibilities assumed by others Initiating projects difficult Alone (feels helpless and uncomfortable when alone) Nurturance (goes to excessive lengths to obtain) Companionship sought urgently when a relationship ends Exaggerated fears of being left to care for self |
| Schizoid personality disorder DISTANT9 Detached or flattened affect Indifferent to criticism or praise Sexual experiences of little interest Tasks done solitarily Absence of close friends Neither desires nor enjoys close relationships Takes pleasure in few activities | Antisocial personality disorder CORRUPT9 Cannot conform to law Obligations ignored Reckless disregard for safety Remorseless Underhanded (deceitful) Planning insufficient (impulsive) Temper (irritable and aggressive) | Borderline personality disorder DESPAIRER* Disturbance of identity Emotionally labile Suicidal behavior Paranoia or dissociation Abandonment (fear of) Impulsive Relationships unstable Emptiness (feelings of) Rage (inappropriate) * Created by Jason P. Caplan, MD | Histrionic personality disorder ACTRESSS* Appearance focused Center of attention Theatrical Relationships (believed to be more intimate than they are) Easily influenced Seductive behavior Shallow emotions Speech (impressionistic and vague) * Created by Jason P. Caplan, MD | Avoidant personality disorder CRINGES9 Criticism or rejection preoccupies thoughts in social situations Restraint in relationships due to fear of shame Inhibited in new relationships Needs to be sure of being liked before engaging socially Gets around occupational activities with need for interpersonal contact Embarrassment prevents new activity or taking risks Self viewed as unappealing or inferior | Obsessive-compulsive personality disorder SCRIMPER* Stubborn Cannot discard worthless objects Rule obsessed Inflexible Miserly Perfectionistic Excludes leisure due to devotion to work Reluctant to delegate to others * Created by Jason P. Caplan, MD |
Entire Web sites exist to share mnemonics for medical education (see Related Resources). Thus it is likely that trainees are using them with or without their teachers’ supervision. Psychiatric educators need to be aware of the mnemonics their trainees are using and to:
- screen these tools for factual errors (such as incomplete diagnostic criteria)
- remind trainees that although mnemonics are useful, psychiatrists should approach patients as individuals without the prejudice of a potentially pejorative label.
Our methodology
In preparing this article, we gathered numerous mnemonics (some published and some novel) designed to capture the learner’s attention and impart information pertinent to psychiatric diagnosis and treatment. Whenever possible, we credited each mnemonic to its creator, but—given the difficulty in confirming authorship of (what in many cases has become) oral history—we’ve listed some mnemonics without citation.
Our list is far from complete because we likely are unaware of many mnemonics, and we have excluded some that seemed obscure, unwieldy, or redundant. We have not excluded mnemonics that some may view as pejorative but merely report their existence. Including them does not mean that we endorse them.
This article lists 32 mnemonics related to psychiatric diagnosis. Thus, it seems odd that an informal survey of >60 residents at the Massachusetts General Hospital (MGH)/McLean Residency Training Program in Psychiatry revealed that most were aware of only 2 or 3 psychiatric mnemonics, typically:
- SIG: E CAPS (a tool to recall the criteria for depression)
- DIG FAST (a list of criteria for diagnosing mania)
- WWHHHHIMPS (a tool for recalling life-threatening causes of delirium).
Although this unscientific survey may be biased because faculty or trainees at MGH created the above 3 mnemonics, it nonetheless begs the question of what qualities make a mnemonic memorable.
Learning theory provides several clues. George Miller’s classic 1956 paper, “The magical number seven, plus or minus two: some limits on our capacity for processing information,” discussed the finding that 7 seems to be the upper limit of individual pieces of data that can be easily remembered.31 Research also has shown that recruiting the limbic system (potentially through the use of humor) aids in the recall of otherwise dry, cortical information.32,33
Intuitively, it would seem that nonrepeating letters would facilitate the recall of the linked data, allowing each letter to provide a distinct cue, without any clouding by redundancy. Of the 3 most popular psychiatric mnemonics, however, only DIG FAST fits the learning theory. It contains 7 letters, repeats no letters, and has the limbic cue of allowing the learner to imagine a person with mania digging furiously.
| Substance dependence ADDICTeD12 Activities are given up or reduced Dependence, physical: tolerance Dependence, physical: withdrawal Intrapersonal (Internal) consequences, physical or psychological Can’t cut down or control use Time-consuming Duration or amount of use is greater than intended | Substance abuse WILD12 Work, school, or home role obligation failures Interpersonal or social consequences Legal problems Dangerous use | Alcohol abuse CAGE13 Have you ever felt you should CUT DOWN your drinking? Have people ANNOYED you by criticizing your drinking? Have you ever felt bad or GUILTY about your drinking? Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover (EYE-OPENER)? |
SIG: E CAPS falls within the range of 7 plus or minus 2, includes a limbic cue (although often forgotten, it refers to the prescription of energy capsules for depression), but repeats the letter S.
WWHHHHIMPS, with 10 letters, exceeds the recommended range, repeats the W (appearing twice) and the H (appearing 4 times), and provides no clear limbic cue.
| Causes I WATCH DEATH Infection Withdrawal Acute metabolic Trauma CNS pathology Hypoxia Deficiencies Endocrinopathies Acute vascular Toxins or drugs Heavy metals | Life-threatening causes WWHHHHIMPS* Wernicke’s encephalopathy Withdrawal Hypertensive crisis Hypoperfusion/hypoxia of the brain Hypoglycemia Hyper/hypothermia Intracranial process/infection Metabolic/meningitis Poisons Status epilepticus * Created by Gary W. Small, MD | Deliriogenic medications ACUTE CHANGE IN MS14 Antibiotics Cardiac drugs Urinary incontinence drugs Theophylline Ethanol Corticosteroids H2 blockers Antiparkinsonian drugs Narcotics Geriatric psychiatric drugs ENT drugs Insomnia drugs NSAIDs Muscle relaxants Seizure medicines |
It may be that recruiting the limbic system provides the greatest likelihood of recall. Recruiting this system may add increased valence to a particular mnemonic for a specific individual, but this same limbic valence may limit its usefulness in a professional context.
- Free searchable database of medical mnemonics. www.medicalmnemonics.com.
- Robinson DJ. Mnemonics and more for psychiatry. Port Huron, MI: Rapid Psychler Press, 2001.
From SIG: E CAPS to CAGE and WWHHHHIMPS, mnemonics help practitioners and trainees recall important lists (such as criteria for depression, screening questions for alcoholism, or life-threatening causes of delirium, respectively). Mnemonics’ efficacy rests on the principle that grouped information is easier to remember than individual points of data.
Not everyone loves mnemonics, but recollecting diagnostic criteria is useful in clinical practice and research, on board examinations, and for insurance reimbursement. Thus, tools that assist in recalling diagnostic criteria have a role in psychiatric practice and teaching.
In this article, we present 32 mnemonics to help clinicians diagnose:
- affective disorders (Box 1)1,2
- anxiety disorders (Box 2)3-6
- medication adverse effects (Box 3)7,8
- personality disorders (Box 4)9-11
- addiction disorders (Box 5)12,13
- causes of delirium (Box 6).14
We also discuss how mnemonics improve one’s memory, based on the principles of learning theory.
How mnemonics work
A mnemonic—from the Greek word “mnemonikos” (“of memory”)—links new data with previously learned information. Mnemonics assist in learning by reducing the amount of information (“cognitive load”) that needs to be stored for long-term processing and retrieval.15
Memory, defined as the “persistence of learning in a state that can be revealed at a later time,”16 can be divided into 2 types:
- declarative (a conscious recollection of facts, such as remembering a relative’s birthday)
- procedural (skills-based learning, such as riding a bicycle).
Declarative memory has a conscious component and may be mediated by the medial temporal lobe and cortical association structures. Procedural memory has less of a conscious component; it may involve the basal ganglia, cerebellum, and a variety of cortical sensory-perceptive regions.17
| Depression SIG: E CAPS* Suicidal thoughts Interests decreased Guilt Energy decreased Concentration decreased Appetite disturbance (increased or decreased) Psychomotor changes (agitation or retardation) Sleep disturbance (increased or decreased) * Created by Carey Gross, MD | Dysthymia HE’S 2 SAD2 Hopelessness Energy loss or fatigue Self-esteem is low 2 years minimum of depressed mood most of the day, for more days than not Sleep is increased or decreased Appetite is increased or decreased Decision-making or concentration is impaired | Mania DIG FAST Distractibility Indiscretion Grandiosity Flight of ideas Activity increase Sleep deficit Talkativeness |
| Depression C GASP DIE1 Concentration decreased Guilt Appetite Sleep disturbance Psychomotor agitation or retardation Death or suicide (thoughts or acts of) Interests decreased Energy decreased | Hypomania TAD HIGH Talkative Attention deficit Decreased need for sleep High self-esteem/grandiosity Ideas that race Goal-directed activity increased High-risk activity | Mania DeTeR the HIGH* Distractibility Talkativeness Reckless behavior Hyposomnia Ideas that race Grandiosity Hypersexuality * Created by Carey Gross, MD |
Declarative memory can be subdivided into working memory and long-term memory.
With working memory, new items of information are held briefly so that encoding and eventual storage can take place.
Working memory guides decision-making and future planning and is intricately related to attention.18-21 Functional MRI and positron emission tomography as well as neurocognitive testing have shown that working memory tasks activate the prefrontal cortex and brain regions specific to language and visuospatial memory.
The hippocampus is thought to rapidly absorb new information, and this data is consolidated and permanently stored via the prefrontal cortex.22-26 Given the hippocampus’ limited storage capacity, new information (such as what you ate for breakfast 3 weeks ago) will disappear if it is not repeated regularly.17
Long-term memory, on the other hand, is encoded knowledge that is linked to facts learned in the past; it is consolidated in the brain and can be readily retrieved. Neuroimaging studies have demonstrated opposing patterns of activation in the hippocampus and prefrontal cortex, depending on whether the memory being recalled is:
- new (high hippocampal activity, low prefrontal cortex activity)
- old (low hippocampal activity, high prefrontal cortex activity).27
Mnemonics are thought to affect working memory by reducing the introduced cognitive load and increasing the efficiency of memory acquisition and encoding. They reduce cognitive load by grouping objects into a single verbal or visual cue that can be introduced into working memory. Learning is optimized when the load on working memory is minimized, enabling long-term memory to be facilitated.28
| Generalized anxiety disorder Worry WARTS3 Wound up Worn-out Absentminded Restless Touchy Sleepless | Posttraumatic stress disorder TRAUMA5 Traumatic event Re-experience Avoidance Unable to function Month or more of symptoms Arousal increased | Anxiety disorder due to a general medical condition Physical Diseases That Have Commonly Appeared Anxious: Pheochromocytoma Diabetes mellitus Temporal lobe epilepsy Hyperthyroidism Carcinoid Alcohol withdrawal Arrhythmias |
| Generalized anxiety disorder WATCHERS4 Worry Anxiety Tension in muscles Concentration difficulty Hyperarousal (or irritability) Energy loss Restlessness Sleep disturbance | Posttraumatic stress disorder DREAMS6 Disinterest in usual activities Re-experience Event preceding symptoms Avoidance Month or more of symptoms Sympathetic arousal |
| Antidepressant discontinuation syndrome FINISH7 Flu-like symptoms Insomnia Nausea Imbalance Sensory disturbances Hyperarousal (anxiety/agitation) | Neuroleptic malignant syndrome FEVER8 Fever Encephalopathy Vital sign instability Elevated WBC/CPK Rigidity WBC: white blood cell count CPK: creatine phosphokinase | Serotonin syndrome HARMED Hyperthermia Autonomic instability Rigidity Myoclonus Encephalopathy Diaphoresis |
Mnemonics may use rhyme, music, or visual cues to enhance memory. Most mnemonics used in medical practice and education are word-based, including:
- Acronyms—words, each letter of which stands for a particular piece of information to be recalled (such as RICE for treatment of a sprained joint: rest, ice, compression, elevation).
- Acrostics—sentences with the first letter of each word prompting the desired recollection (such as “To Zanzibar by motor car” for the branches of the facial nerve: temporal, zygomatic, buccal, mandibular, cervical).
- Alphabetical sequences (such as ABCDE of trauma assessment: airway, breathing, circulation, disability, exposure).29
An appropriate teaching tool?
Dozens of mnemonics addressing psychiatric diagnosis and treatment have been published, but relatively few are widely used. Psychiatric educators may resist teaching with mnemonics, believing they might erode a humanistic approach to patients by reducing psychopathology to “a laundry list” of symptoms and the art of psychiatric diagnosis to a “check-box” endeavor. Mnemonics that use humor may be rejected as irreverent or unprofessional.30 Publishing a novel mnemonic may be viewed with disdain by some as an “easy” way of padding a curriculum vitae.
| Paranoid personality disorder SUSPECT9 Spousal infidelity suspected Unforgiving (bears grudges) Suspicious Perceives attacks (and reacts quickly) Enemy or friend? (suspects associates and friends) Confiding in others is feared Threats perceived in benign events | Schizotypal personality disorder ME PECULIAR9 Magical thinking Experiences unusual perceptions Paranoid ideation Eccentric behavior or appearance Constricted or inappropriate affect Unusual thinking or speech Lacks close friends Ideas of reference Anxiety in social situations Rule out psychotic or pervasive developmental disorders | Borderline personality disorder IMPULSIVE10 Impulsive Moodiness Paranoia or dissociation under stress Unstable self-image Labile intense relationships Suicidal gestures Inappropriate anger Vulnerability to abandonment Emptiness (feelings of) | Histrionic personality disorder PRAISE ME9 Provocative or seductive behavior Relationships considered more intimate than they are Attention (need to be the center of) Influenced easily Style of speech (impressionistic, lacking detail) Emotions (rapidly shifting, shallow) Make up (physical appearance used to draw attention to self) Emotions exaggerated | Narcissistic personality disorder GRANDIOSE11 Grandiose Requires attention Arrogant Need to be special Dreams of success and power Interpersonally exploitative Others (unable to recognize feelings/needs of) Sense of entitlement Envious | Dependent personality disorder RELIANCE9 Reassurance required Expressing disagreement difficult Life responsibilities assumed by others Initiating projects difficult Alone (feels helpless and uncomfortable when alone) Nurturance (goes to excessive lengths to obtain) Companionship sought urgently when a relationship ends Exaggerated fears of being left to care for self |
| Schizoid personality disorder DISTANT9 Detached or flattened affect Indifferent to criticism or praise Sexual experiences of little interest Tasks done solitarily Absence of close friends Neither desires nor enjoys close relationships Takes pleasure in few activities | Antisocial personality disorder CORRUPT9 Cannot conform to law Obligations ignored Reckless disregard for safety Remorseless Underhanded (deceitful) Planning insufficient (impulsive) Temper (irritable and aggressive) | Borderline personality disorder DESPAIRER* Disturbance of identity Emotionally labile Suicidal behavior Paranoia or dissociation Abandonment (fear of) Impulsive Relationships unstable Emptiness (feelings of) Rage (inappropriate) * Created by Jason P. Caplan, MD | Histrionic personality disorder ACTRESSS* Appearance focused Center of attention Theatrical Relationships (believed to be more intimate than they are) Easily influenced Seductive behavior Shallow emotions Speech (impressionistic and vague) * Created by Jason P. Caplan, MD | Avoidant personality disorder CRINGES9 Criticism or rejection preoccupies thoughts in social situations Restraint in relationships due to fear of shame Inhibited in new relationships Needs to be sure of being liked before engaging socially Gets around occupational activities with need for interpersonal contact Embarrassment prevents new activity or taking risks Self viewed as unappealing or inferior | Obsessive-compulsive personality disorder SCRIMPER* Stubborn Cannot discard worthless objects Rule obsessed Inflexible Miserly Perfectionistic Excludes leisure due to devotion to work Reluctant to delegate to others * Created by Jason P. Caplan, MD |
Entire Web sites exist to share mnemonics for medical education (see Related Resources). Thus it is likely that trainees are using them with or without their teachers’ supervision. Psychiatric educators need to be aware of the mnemonics their trainees are using and to:
- screen these tools for factual errors (such as incomplete diagnostic criteria)
- remind trainees that although mnemonics are useful, psychiatrists should approach patients as individuals without the prejudice of a potentially pejorative label.
Our methodology
In preparing this article, we gathered numerous mnemonics (some published and some novel) designed to capture the learner’s attention and impart information pertinent to psychiatric diagnosis and treatment. Whenever possible, we credited each mnemonic to its creator, but—given the difficulty in confirming authorship of (what in many cases has become) oral history—we’ve listed some mnemonics without citation.
Our list is far from complete because we likely are unaware of many mnemonics, and we have excluded some that seemed obscure, unwieldy, or redundant. We have not excluded mnemonics that some may view as pejorative but merely report their existence. Including them does not mean that we endorse them.
This article lists 32 mnemonics related to psychiatric diagnosis. Thus, it seems odd that an informal survey of >60 residents at the Massachusetts General Hospital (MGH)/McLean Residency Training Program in Psychiatry revealed that most were aware of only 2 or 3 psychiatric mnemonics, typically:
- SIG: E CAPS (a tool to recall the criteria for depression)
- DIG FAST (a list of criteria for diagnosing mania)
- WWHHHHIMPS (a tool for recalling life-threatening causes of delirium).
Although this unscientific survey may be biased because faculty or trainees at MGH created the above 3 mnemonics, it nonetheless begs the question of what qualities make a mnemonic memorable.
Learning theory provides several clues. George Miller’s classic 1956 paper, “The magical number seven, plus or minus two: some limits on our capacity for processing information,” discussed the finding that 7 seems to be the upper limit of individual pieces of data that can be easily remembered.31 Research also has shown that recruiting the limbic system (potentially through the use of humor) aids in the recall of otherwise dry, cortical information.32,33
Intuitively, it would seem that nonrepeating letters would facilitate the recall of the linked data, allowing each letter to provide a distinct cue, without any clouding by redundancy. Of the 3 most popular psychiatric mnemonics, however, only DIG FAST fits the learning theory. It contains 7 letters, repeats no letters, and has the limbic cue of allowing the learner to imagine a person with mania digging furiously.
| Substance dependence ADDICTeD12 Activities are given up or reduced Dependence, physical: tolerance Dependence, physical: withdrawal Intrapersonal (Internal) consequences, physical or psychological Can’t cut down or control use Time-consuming Duration or amount of use is greater than intended | Substance abuse WILD12 Work, school, or home role obligation failures Interpersonal or social consequences Legal problems Dangerous use | Alcohol abuse CAGE13 Have you ever felt you should CUT DOWN your drinking? Have people ANNOYED you by criticizing your drinking? Have you ever felt bad or GUILTY about your drinking? Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover (EYE-OPENER)? |
SIG: E CAPS falls within the range of 7 plus or minus 2, includes a limbic cue (although often forgotten, it refers to the prescription of energy capsules for depression), but repeats the letter S.
WWHHHHIMPS, with 10 letters, exceeds the recommended range, repeats the W (appearing twice) and the H (appearing 4 times), and provides no clear limbic cue.
| Causes I WATCH DEATH Infection Withdrawal Acute metabolic Trauma CNS pathology Hypoxia Deficiencies Endocrinopathies Acute vascular Toxins or drugs Heavy metals | Life-threatening causes WWHHHHIMPS* Wernicke’s encephalopathy Withdrawal Hypertensive crisis Hypoperfusion/hypoxia of the brain Hypoglycemia Hyper/hypothermia Intracranial process/infection Metabolic/meningitis Poisons Status epilepticus * Created by Gary W. Small, MD | Deliriogenic medications ACUTE CHANGE IN MS14 Antibiotics Cardiac drugs Urinary incontinence drugs Theophylline Ethanol Corticosteroids H2 blockers Antiparkinsonian drugs Narcotics Geriatric psychiatric drugs ENT drugs Insomnia drugs NSAIDs Muscle relaxants Seizure medicines |
It may be that recruiting the limbic system provides the greatest likelihood of recall. Recruiting this system may add increased valence to a particular mnemonic for a specific individual, but this same limbic valence may limit its usefulness in a professional context.
- Free searchable database of medical mnemonics. www.medicalmnemonics.com.
- Robinson DJ. Mnemonics and more for psychiatry. Port Huron, MI: Rapid Psychler Press, 2001.
1. Abraham PF, Shirley ER. New mnemonic for depressive symptoms. Am J Psychiatry 2006;163(2):329-30.
2. Christman DS. “HE’S 2 SAD” detects dysthymic disorder. Current Psychiatry 2008;7(3):120.-
3. Coupland NJ. Worry WARTS have generalized anxiety disorder. Can J Psychiatry 2002;47(2):197.-
4. Berber MJ. WATCHERS: recognizing generalized anxiety disorder. J Clin Psychiatry 2000;61(6):447.-
5. Khouzam HR. A simple mnemonic for the diagnostic criteria for post-traumatic stress disorder. West J Med 2001;174(6):424.-
6. Short DD, Workman EA, Morse JH, Turner RL. Mnemonics for eight DSM-III-R disorders. Hosp Community Psychiatry 1992;43(6):642-4.
7. Berber MJ. FINISH: remembering the discontinuation syndrome. Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, and Hyperarousal (anxiety/agitation). J Clin Psychiatry 1998;59(5):255.-
8. Christensen RC. Identify neuroleptic malignant syndrome with FEVER. Current Psychiatry 2005;4(7):102.-
9. Pinkofsky HB. Mnemonics for DSM-IV personality disorders. Psychiatr Serv 1997;48(9):1197-8.
10. Senger HL. Borderline mnemonic. Am J Psychiatry 1997;154(9):1321.-
11. Kim SI, Swanson TA, Caplan JP, eds. Underground clinical vignettes step 2: psychiatry. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:130.
12. Bogenschutz MP, Quinn DK. Acronyms for substance use disorders. J Clin Psychiatry 2001;62(6):474-5.
13. Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252(14):1905-7.
14. Flaherty JH. Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter remedies: causes of confusion. Clin Geriatr Med 1998;14:101-27.
15. Sweller J. Cognitive load theory, learning difficulty, and instructional design. Learn Instr 1994;4:295-312.
16. Squire LR. Memory and brain. New York, NY: Oxford University Press; 1987.
17. DeLuca J, Lengenfelder J, Eslinger P. Memory and learning. In: Rizzo M, Eslinger P, eds. Principles and practice of behavioral neurology and neuropsychology. Philadelphia, PA: Saunders; 2004:251.
18. Dash PK, Moore AN, Kobori N, et al. Molecular activity underlying working memory. Learn Mem 2007;14:554-63.
19. Awh E, Vogel EK, Oh SH. Interactions between attention and working memory. Neuroscience 2006;139:201-8.
20. Knudson EI. Fundamental components of attention. Ann Rev Neurosci 2007;30:57-78.
21. Postle BR. Working memory as an emergent property of the mind and brain. Neuroscience 2006;139:23-36.
22. Fletcher PC, Henson RN. Frontal lobes and human memory: Insights from functional neuroimaging. Brain 2001;124:849-81.
23. Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Ann Rev Neurosci 2001;24:167-202.
24. Schumacher EH, Lauber E, Awh E, et al. PET evidence for a modal verbal working memory system. Neuroimage 1996;3:79-88.
25. Smith EE, Jonides J, Koeppe RA. Dissociating verbal and spatial working memory using PET. Cereb Cortex 1996;6:11-20.
26. Wager TD, Smith EE. Neuroimaging studies of working memory: a meta-analysis. Cogn Affect Behav Neurosci 2003;3(4):255-74.
27. Frankland PW, Bontempi B. The organization of recent and remote memories. Nat Rev Neurosci 2005;6:119-30.
28. Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci 1988;12(1):257-85.
29. Beitz JM. Unleashing the power of memory: the mighty mnemonic. Nurse Educ 1997;22(2):25-9.
30. Larson EW. Criticism of mnemonic device. Am J Psychiatry 1990;147(7):963-4.
31. Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev 1956;63:81-97.
32. Schmidt SR. Effects of humor on sentence memory. J Exp Psychol Learn Mem Cogn 1994;20(4):953-67.
33. Lippman LG, Dunn ML. Contextual connections within puns: effects on perceived humor and memory. J Gen Psychol 2000;127(2):185-97.
1. Abraham PF, Shirley ER. New mnemonic for depressive symptoms. Am J Psychiatry 2006;163(2):329-30.
2. Christman DS. “HE’S 2 SAD” detects dysthymic disorder. Current Psychiatry 2008;7(3):120.-
3. Coupland NJ. Worry WARTS have generalized anxiety disorder. Can J Psychiatry 2002;47(2):197.-
4. Berber MJ. WATCHERS: recognizing generalized anxiety disorder. J Clin Psychiatry 2000;61(6):447.-
5. Khouzam HR. A simple mnemonic for the diagnostic criteria for post-traumatic stress disorder. West J Med 2001;174(6):424.-
6. Short DD, Workman EA, Morse JH, Turner RL. Mnemonics for eight DSM-III-R disorders. Hosp Community Psychiatry 1992;43(6):642-4.
7. Berber MJ. FINISH: remembering the discontinuation syndrome. Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, and Hyperarousal (anxiety/agitation). J Clin Psychiatry 1998;59(5):255.-
8. Christensen RC. Identify neuroleptic malignant syndrome with FEVER. Current Psychiatry 2005;4(7):102.-
9. Pinkofsky HB. Mnemonics for DSM-IV personality disorders. Psychiatr Serv 1997;48(9):1197-8.
10. Senger HL. Borderline mnemonic. Am J Psychiatry 1997;154(9):1321.-
11. Kim SI, Swanson TA, Caplan JP, eds. Underground clinical vignettes step 2: psychiatry. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:130.
12. Bogenschutz MP, Quinn DK. Acronyms for substance use disorders. J Clin Psychiatry 2001;62(6):474-5.
13. Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA 1984;252(14):1905-7.
14. Flaherty JH. Psychotherapeutic agents in older adults. Commonly prescribed and over-the-counter remedies: causes of confusion. Clin Geriatr Med 1998;14:101-27.
15. Sweller J. Cognitive load theory, learning difficulty, and instructional design. Learn Instr 1994;4:295-312.
16. Squire LR. Memory and brain. New York, NY: Oxford University Press; 1987.
17. DeLuca J, Lengenfelder J, Eslinger P. Memory and learning. In: Rizzo M, Eslinger P, eds. Principles and practice of behavioral neurology and neuropsychology. Philadelphia, PA: Saunders; 2004:251.
18. Dash PK, Moore AN, Kobori N, et al. Molecular activity underlying working memory. Learn Mem 2007;14:554-63.
19. Awh E, Vogel EK, Oh SH. Interactions between attention and working memory. Neuroscience 2006;139:201-8.
20. Knudson EI. Fundamental components of attention. Ann Rev Neurosci 2007;30:57-78.
21. Postle BR. Working memory as an emergent property of the mind and brain. Neuroscience 2006;139:23-36.
22. Fletcher PC, Henson RN. Frontal lobes and human memory: Insights from functional neuroimaging. Brain 2001;124:849-81.
23. Miller EK, Cohen JD. An integrative theory of prefrontal cortex function. Ann Rev Neurosci 2001;24:167-202.
24. Schumacher EH, Lauber E, Awh E, et al. PET evidence for a modal verbal working memory system. Neuroimage 1996;3:79-88.
25. Smith EE, Jonides J, Koeppe RA. Dissociating verbal and spatial working memory using PET. Cereb Cortex 1996;6:11-20.
26. Wager TD, Smith EE. Neuroimaging studies of working memory: a meta-analysis. Cogn Affect Behav Neurosci 2003;3(4):255-74.
27. Frankland PW, Bontempi B. The organization of recent and remote memories. Nat Rev Neurosci 2005;6:119-30.
28. Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci 1988;12(1):257-85.
29. Beitz JM. Unleashing the power of memory: the mighty mnemonic. Nurse Educ 1997;22(2):25-9.
30. Larson EW. Criticism of mnemonic device. Am J Psychiatry 1990;147(7):963-4.
31. Miller GA. The magical number seven, plus or minus two: some limits on our capacity for processing information. Psychol Rev 1956;63:81-97.
32. Schmidt SR. Effects of humor on sentence memory. J Exp Psychol Learn Mem Cogn 1994;20(4):953-67.
33. Lippman LG, Dunn ML. Contextual connections within puns: effects on perceived humor and memory. J Gen Psychol 2000;127(2):185-97.