User login
Jennifer Smith is the editor of Oncology Practice, part of MDedge Hematology/Oncology. She was previously the editor of Hematology Times, an editor at Principal Investigators Association, and a reporter at The Oneida Daily Dispatch. She has a BS in journalism.
FDA approves subcutaneous trastuzumab for HER2-positive breast cancers
The Food and Drug Administration has approved a subcutaneous formulation of trastuzumab – trastuzumab and hyaluronidase-oysk (Herceptin Hylecta) – for the treatment of patients with HER2-overexpressing breast cancer.
Approval of the subcutaneous formulation is based on results from two clinical studies in HER2-positive early breast cancer – HannaH and SafeHER, the FDA said in a press release.
In the phase 3 HannaH study (NCT00950300), researchers compared neoadjuvant and adjuvant trastuzumab and hyaluronidase-oysk with intravenous trastuzumab, both in combination with chemotherapy. Trastuzumab and hyaluronidase-oysk proved noninferior to intravenous trastuzumab in this trial (Lancet Oncol. 2012 Sep;13[9]:869-78).
In the phase 3 SafeHER study (NCT01566721), the safety profile of trastuzumab and hyaluronidase-oysk was deemed consistent with the known safety profiles of intravenous trastuzumab and trastuzumab and hyaluronidase-oysk (Eur J Cancer. 2017 Sep;82:237-246).
The most common adverse reactions observed in patients receiving the subcutaneous formulation were fatigue, arthralgia, diarrhea, injection-site reaction, upper respiratory tract infection, rash, myalgia, nausea, headache, edema, flushing, pyrexia, cough, and pain in extremity, the FDA said.
Trastuzumab plus hyaluronidase-oysk was approved with a black box warning detailing the risk of cardiomyopathy, pulmonary toxicity, and embryo-fetal toxicity associated with the product.
The recommended dose is 600 mg/10,000 units (600 mg trastuzumab and 10,000 units hyaluronidase) administered subcutaneously over approximately 2-5 minutes once every 3 weeks.
Additional details can be found in the prescribing information.
The Food and Drug Administration has approved a subcutaneous formulation of trastuzumab – trastuzumab and hyaluronidase-oysk (Herceptin Hylecta) – for the treatment of patients with HER2-overexpressing breast cancer.
Approval of the subcutaneous formulation is based on results from two clinical studies in HER2-positive early breast cancer – HannaH and SafeHER, the FDA said in a press release.
In the phase 3 HannaH study (NCT00950300), researchers compared neoadjuvant and adjuvant trastuzumab and hyaluronidase-oysk with intravenous trastuzumab, both in combination with chemotherapy. Trastuzumab and hyaluronidase-oysk proved noninferior to intravenous trastuzumab in this trial (Lancet Oncol. 2012 Sep;13[9]:869-78).
In the phase 3 SafeHER study (NCT01566721), the safety profile of trastuzumab and hyaluronidase-oysk was deemed consistent with the known safety profiles of intravenous trastuzumab and trastuzumab and hyaluronidase-oysk (Eur J Cancer. 2017 Sep;82:237-246).
The most common adverse reactions observed in patients receiving the subcutaneous formulation were fatigue, arthralgia, diarrhea, injection-site reaction, upper respiratory tract infection, rash, myalgia, nausea, headache, edema, flushing, pyrexia, cough, and pain in extremity, the FDA said.
Trastuzumab plus hyaluronidase-oysk was approved with a black box warning detailing the risk of cardiomyopathy, pulmonary toxicity, and embryo-fetal toxicity associated with the product.
The recommended dose is 600 mg/10,000 units (600 mg trastuzumab and 10,000 units hyaluronidase) administered subcutaneously over approximately 2-5 minutes once every 3 weeks.
Additional details can be found in the prescribing information.
The Food and Drug Administration has approved a subcutaneous formulation of trastuzumab – trastuzumab and hyaluronidase-oysk (Herceptin Hylecta) – for the treatment of patients with HER2-overexpressing breast cancer.
Approval of the subcutaneous formulation is based on results from two clinical studies in HER2-positive early breast cancer – HannaH and SafeHER, the FDA said in a press release.
In the phase 3 HannaH study (NCT00950300), researchers compared neoadjuvant and adjuvant trastuzumab and hyaluronidase-oysk with intravenous trastuzumab, both in combination with chemotherapy. Trastuzumab and hyaluronidase-oysk proved noninferior to intravenous trastuzumab in this trial (Lancet Oncol. 2012 Sep;13[9]:869-78).
In the phase 3 SafeHER study (NCT01566721), the safety profile of trastuzumab and hyaluronidase-oysk was deemed consistent with the known safety profiles of intravenous trastuzumab and trastuzumab and hyaluronidase-oysk (Eur J Cancer. 2017 Sep;82:237-246).
The most common adverse reactions observed in patients receiving the subcutaneous formulation were fatigue, arthralgia, diarrhea, injection-site reaction, upper respiratory tract infection, rash, myalgia, nausea, headache, edema, flushing, pyrexia, cough, and pain in extremity, the FDA said.
Trastuzumab plus hyaluronidase-oysk was approved with a black box warning detailing the risk of cardiomyopathy, pulmonary toxicity, and embryo-fetal toxicity associated with the product.
The recommended dose is 600 mg/10,000 units (600 mg trastuzumab and 10,000 units hyaluronidase) administered subcutaneously over approximately 2-5 minutes once every 3 weeks.
Additional details can be found in the prescribing information.
Cancer researchers awarded for breakthroughs
The Royal Swedish Academy of Sciences has awarded the 2019 Sjöberg Prize to Dennis J. Slamon, MD, PhD, and Brian J. Druker, MD.
The pair received the prize, which is worth $1 million, “for their groundbreaking contributions to the clinical development of targeted therapy directed against genetic aberrations in cancer.”
Dr. Slamon, a professor at the University of California, Los Angeles, conducted research that led to the development of trastuzumab as a treatment for HER2-positive breast cancer.
Dr. Druker, a professor at Oregon Health and Science University in Portland, found that imatinib could treat chronic myeloid leukemia by inhibiting BCR-ABL.
Dr. Druker and Dr. Slamon both plan to use the prize money to identify new targets for cancer therapies.
In other news, Steven A. Rosenberg, MD, PhD, of the National Cancer Institute in Bethesda, Md., won the 2019 Szent-Györgyi Prize for Progress in Cancer Research.
Dr. Rosenberg won the $25,000 prize for his “pioneering role in the development of adoptive immunotherapy to treat cancer.”
Dr. Rosenberg is credited with conducting trials of interleukin-2 that led to its U.S. approval, identifying tumor-infiltrating lymphocytes in metastatic melanoma, showing that adoptive cell transfer can prompt tumor regression in advanced melanoma and breast cancer, and being the first person to use chimeric antigen receptor (CAR) T cells to treat aggressive lymphomas.
With his current work, Dr. Rosenberg is exploring the use of adoptive cell transfer in epithelial cancers.
Dr. Rosenberg also received the 2019 Dr. Nathan Davis Award for Outstanding Government Service. He is one of eight individuals who won the award this year.
The award is named after the founding father of the American Medical Association and is given to “elected and career officials in federal, state, or municipal service whose outstanding contributions have promoted the art and science of medicine and the betterment of public health.”
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
The Royal Swedish Academy of Sciences has awarded the 2019 Sjöberg Prize to Dennis J. Slamon, MD, PhD, and Brian J. Druker, MD.
The pair received the prize, which is worth $1 million, “for their groundbreaking contributions to the clinical development of targeted therapy directed against genetic aberrations in cancer.”
Dr. Slamon, a professor at the University of California, Los Angeles, conducted research that led to the development of trastuzumab as a treatment for HER2-positive breast cancer.
Dr. Druker, a professor at Oregon Health and Science University in Portland, found that imatinib could treat chronic myeloid leukemia by inhibiting BCR-ABL.
Dr. Druker and Dr. Slamon both plan to use the prize money to identify new targets for cancer therapies.
In other news, Steven A. Rosenberg, MD, PhD, of the National Cancer Institute in Bethesda, Md., won the 2019 Szent-Györgyi Prize for Progress in Cancer Research.
Dr. Rosenberg won the $25,000 prize for his “pioneering role in the development of adoptive immunotherapy to treat cancer.”
Dr. Rosenberg is credited with conducting trials of interleukin-2 that led to its U.S. approval, identifying tumor-infiltrating lymphocytes in metastatic melanoma, showing that adoptive cell transfer can prompt tumor regression in advanced melanoma and breast cancer, and being the first person to use chimeric antigen receptor (CAR) T cells to treat aggressive lymphomas.
With his current work, Dr. Rosenberg is exploring the use of adoptive cell transfer in epithelial cancers.
Dr. Rosenberg also received the 2019 Dr. Nathan Davis Award for Outstanding Government Service. He is one of eight individuals who won the award this year.
The award is named after the founding father of the American Medical Association and is given to “elected and career officials in federal, state, or municipal service whose outstanding contributions have promoted the art and science of medicine and the betterment of public health.”
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
The Royal Swedish Academy of Sciences has awarded the 2019 Sjöberg Prize to Dennis J. Slamon, MD, PhD, and Brian J. Druker, MD.
The pair received the prize, which is worth $1 million, “for their groundbreaking contributions to the clinical development of targeted therapy directed against genetic aberrations in cancer.”
Dr. Slamon, a professor at the University of California, Los Angeles, conducted research that led to the development of trastuzumab as a treatment for HER2-positive breast cancer.
Dr. Druker, a professor at Oregon Health and Science University in Portland, found that imatinib could treat chronic myeloid leukemia by inhibiting BCR-ABL.
Dr. Druker and Dr. Slamon both plan to use the prize money to identify new targets for cancer therapies.
In other news, Steven A. Rosenberg, MD, PhD, of the National Cancer Institute in Bethesda, Md., won the 2019 Szent-Györgyi Prize for Progress in Cancer Research.
Dr. Rosenberg won the $25,000 prize for his “pioneering role in the development of adoptive immunotherapy to treat cancer.”
Dr. Rosenberg is credited with conducting trials of interleukin-2 that led to its U.S. approval, identifying tumor-infiltrating lymphocytes in metastatic melanoma, showing that adoptive cell transfer can prompt tumor regression in advanced melanoma and breast cancer, and being the first person to use chimeric antigen receptor (CAR) T cells to treat aggressive lymphomas.
With his current work, Dr. Rosenberg is exploring the use of adoptive cell transfer in epithelial cancers.
Dr. Rosenberg also received the 2019 Dr. Nathan Davis Award for Outstanding Government Service. He is one of eight individuals who won the award this year.
The award is named after the founding father of the American Medical Association and is given to “elected and career officials in federal, state, or municipal service whose outstanding contributions have promoted the art and science of medicine and the betterment of public health.”
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
Similar results for once- or twice-weekly carfilzomib in MM
Patients with newly diagnosed multiple myeloma have similar outcomes whether they receive carfilzomib once or twice a week, according to a pooled analysis of trial data.
Researchers found no significant difference in safety, progression-free survival (PFS), or overall survival (OS) whether patients received carfilzomib at 70 mg/m2 once a week or 36 mg/m2 twice a week.
Sara Bringhen, MD, PhD, of University of Turin, Italy, and her colleagues conducted this analysis and detailed the results in Haematologica.
The researchers pooled data from a phase 1/2 trial (NCT01857115) and a phase 2 trial (NCT01346787), both enrolling transplant-ineligible patients with newly diagnosed multiple myeloma.
In both studies, induction consisted of nine 4-week cycles of carfilzomib (given once or twice weekly), cyclophosphamide (300 mg on days 1, 8, and 15), and dexamethasone (40 mg on days 1, 8, 15, and 22). After induction, patients received carfilzomib maintenance (at either dose) until progression or intolerable toxicity.
The pooled analysis included 121 patients: 63 who received carfilzomib at 70 mg/m2 once weekly and 58 who received carfilzomib at 36 mg/m2 twice weekly.
There were no significant differences in baseline characteristics between the dosing groups. For the entire cohort, the median age at diagnosis was 72 years (range, 55-86), and the median follow-up was 39 months.
A total of 119 patients started induction (63 in the once-weekly group and 56 in the twice-weekly group), and 90 patients received maintenance (47 and 43, respectively). Patients received maintenance for a median of 17 months in the once-weekly group and 20 months in the twice-weekly group (P = .17).
There was no significant difference between the groups with regard to PFS or OS, either from enrollment or the start of maintenance.
From enrollment, the median PFS was 35.7 months in the once-weekly group and 35.5 months in the twice-weekly group (hazard ratio [HR] = 1.39; P = .26). The 3-year OS was 70% and 72%, respectively (HR = 1.27; P = .5).
From the start of maintenance, the 3-year PFS was 47% in the once-weekly group and 51% in the twice-weekly group (HR = 1.04; P = .92). The 3-year OS was 72% and 73%, respectively (HR = 0.82; P = .71).
There were no significant between-group differences in the rates of grade 3-5 adverse events (AEs) or the need for carfilzomib dose reduction or discontinuation.
Grade 3-5 hematologic AEs occurred in 24% of patients in the once-weekly group and 30% of those in the twice-weekly group. Grade 3-5 nonhematologic AEs occurred in 38% and 41%, respectively.
Twenty-nine percent of patients in the once-weekly group required a reduction in carfilzomib dose, as did 30% of patients in the twice-weekly group. Common AEs leading to dose reduction were acute kidney injury, infections, and hypertension.
AEs leading to carfilzomib discontinuation occurred in 27% of patients in the once-weekly group and 30% of those in the twice-weekly group. Common AEs leading to discontinuation were cardiac injury, infections, and thromboembolism.
Both trials were sponsored by Stichting Hemato-Oncologie voor Volwassenen Nederland in collaboration with Fondazione Neoplasie Sangue ONLUS and supported by funding from Amgen (Onyx Pharmaceuticals). Dr. Bringhen reported relationships with Amgen and other companies. Coauthor Antonio Palumbo, MD, is an employee of Takeda, and other authors reported relationships with a range of companies.
SOURCE: Bringhen S et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.208272.
Patients with newly diagnosed multiple myeloma have similar outcomes whether they receive carfilzomib once or twice a week, according to a pooled analysis of trial data.
Researchers found no significant difference in safety, progression-free survival (PFS), or overall survival (OS) whether patients received carfilzomib at 70 mg/m2 once a week or 36 mg/m2 twice a week.
Sara Bringhen, MD, PhD, of University of Turin, Italy, and her colleagues conducted this analysis and detailed the results in Haematologica.
The researchers pooled data from a phase 1/2 trial (NCT01857115) and a phase 2 trial (NCT01346787), both enrolling transplant-ineligible patients with newly diagnosed multiple myeloma.
In both studies, induction consisted of nine 4-week cycles of carfilzomib (given once or twice weekly), cyclophosphamide (300 mg on days 1, 8, and 15), and dexamethasone (40 mg on days 1, 8, 15, and 22). After induction, patients received carfilzomib maintenance (at either dose) until progression or intolerable toxicity.
The pooled analysis included 121 patients: 63 who received carfilzomib at 70 mg/m2 once weekly and 58 who received carfilzomib at 36 mg/m2 twice weekly.
There were no significant differences in baseline characteristics between the dosing groups. For the entire cohort, the median age at diagnosis was 72 years (range, 55-86), and the median follow-up was 39 months.
A total of 119 patients started induction (63 in the once-weekly group and 56 in the twice-weekly group), and 90 patients received maintenance (47 and 43, respectively). Patients received maintenance for a median of 17 months in the once-weekly group and 20 months in the twice-weekly group (P = .17).
There was no significant difference between the groups with regard to PFS or OS, either from enrollment or the start of maintenance.
From enrollment, the median PFS was 35.7 months in the once-weekly group and 35.5 months in the twice-weekly group (hazard ratio [HR] = 1.39; P = .26). The 3-year OS was 70% and 72%, respectively (HR = 1.27; P = .5).
From the start of maintenance, the 3-year PFS was 47% in the once-weekly group and 51% in the twice-weekly group (HR = 1.04; P = .92). The 3-year OS was 72% and 73%, respectively (HR = 0.82; P = .71).
There were no significant between-group differences in the rates of grade 3-5 adverse events (AEs) or the need for carfilzomib dose reduction or discontinuation.
Grade 3-5 hematologic AEs occurred in 24% of patients in the once-weekly group and 30% of those in the twice-weekly group. Grade 3-5 nonhematologic AEs occurred in 38% and 41%, respectively.
Twenty-nine percent of patients in the once-weekly group required a reduction in carfilzomib dose, as did 30% of patients in the twice-weekly group. Common AEs leading to dose reduction were acute kidney injury, infections, and hypertension.
AEs leading to carfilzomib discontinuation occurred in 27% of patients in the once-weekly group and 30% of those in the twice-weekly group. Common AEs leading to discontinuation were cardiac injury, infections, and thromboembolism.
Both trials were sponsored by Stichting Hemato-Oncologie voor Volwassenen Nederland in collaboration with Fondazione Neoplasie Sangue ONLUS and supported by funding from Amgen (Onyx Pharmaceuticals). Dr. Bringhen reported relationships with Amgen and other companies. Coauthor Antonio Palumbo, MD, is an employee of Takeda, and other authors reported relationships with a range of companies.
SOURCE: Bringhen S et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.208272.
Patients with newly diagnosed multiple myeloma have similar outcomes whether they receive carfilzomib once or twice a week, according to a pooled analysis of trial data.
Researchers found no significant difference in safety, progression-free survival (PFS), or overall survival (OS) whether patients received carfilzomib at 70 mg/m2 once a week or 36 mg/m2 twice a week.
Sara Bringhen, MD, PhD, of University of Turin, Italy, and her colleagues conducted this analysis and detailed the results in Haematologica.
The researchers pooled data from a phase 1/2 trial (NCT01857115) and a phase 2 trial (NCT01346787), both enrolling transplant-ineligible patients with newly diagnosed multiple myeloma.
In both studies, induction consisted of nine 4-week cycles of carfilzomib (given once or twice weekly), cyclophosphamide (300 mg on days 1, 8, and 15), and dexamethasone (40 mg on days 1, 8, 15, and 22). After induction, patients received carfilzomib maintenance (at either dose) until progression or intolerable toxicity.
The pooled analysis included 121 patients: 63 who received carfilzomib at 70 mg/m2 once weekly and 58 who received carfilzomib at 36 mg/m2 twice weekly.
There were no significant differences in baseline characteristics between the dosing groups. For the entire cohort, the median age at diagnosis was 72 years (range, 55-86), and the median follow-up was 39 months.
A total of 119 patients started induction (63 in the once-weekly group and 56 in the twice-weekly group), and 90 patients received maintenance (47 and 43, respectively). Patients received maintenance for a median of 17 months in the once-weekly group and 20 months in the twice-weekly group (P = .17).
There was no significant difference between the groups with regard to PFS or OS, either from enrollment or the start of maintenance.
From enrollment, the median PFS was 35.7 months in the once-weekly group and 35.5 months in the twice-weekly group (hazard ratio [HR] = 1.39; P = .26). The 3-year OS was 70% and 72%, respectively (HR = 1.27; P = .5).
From the start of maintenance, the 3-year PFS was 47% in the once-weekly group and 51% in the twice-weekly group (HR = 1.04; P = .92). The 3-year OS was 72% and 73%, respectively (HR = 0.82; P = .71).
There were no significant between-group differences in the rates of grade 3-5 adverse events (AEs) or the need for carfilzomib dose reduction or discontinuation.
Grade 3-5 hematologic AEs occurred in 24% of patients in the once-weekly group and 30% of those in the twice-weekly group. Grade 3-5 nonhematologic AEs occurred in 38% and 41%, respectively.
Twenty-nine percent of patients in the once-weekly group required a reduction in carfilzomib dose, as did 30% of patients in the twice-weekly group. Common AEs leading to dose reduction were acute kidney injury, infections, and hypertension.
AEs leading to carfilzomib discontinuation occurred in 27% of patients in the once-weekly group and 30% of those in the twice-weekly group. Common AEs leading to discontinuation were cardiac injury, infections, and thromboembolism.
Both trials were sponsored by Stichting Hemato-Oncologie voor Volwassenen Nederland in collaboration with Fondazione Neoplasie Sangue ONLUS and supported by funding from Amgen (Onyx Pharmaceuticals). Dr. Bringhen reported relationships with Amgen and other companies. Coauthor Antonio Palumbo, MD, is an employee of Takeda, and other authors reported relationships with a range of companies.
SOURCE: Bringhen S et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.208272.
FROM HAEMATOLOGICA
Regimen shows promise as salvage for classical HL
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
A retrospective study suggests a four-drug regimen can be effective salvage therapy for patients with relapsed or refractory classical Hodgkin lymphoma.
The regimen – brentuximab vedotin plus ifosfamide, gemcitabine, and vinorelbine (BV-IGEV) – produced responses in 27 of 28 patients studied, allowing them to undergo autologous hematopoietic stem cell transplant (HSCT).
After HSCT, the estimated 2-year progression-free survival (PFS) was 87.1% and the overall survival (OS) was 73.5%.
Though this study was limited by its small population and retrospective nature, the results “warrant further investigation,” according to Khadega A. Abuelgasim, MD, of King Abdullah International Medical Research Center in Riyadh, Saudi Arabia, and colleagues.
The researchers reported the results in a letter to Bone Marrow Transplantation.
The study included 28 patients with classical Hodgkin lymphoma, 15 of them male. The patients’ median age at HSCT was 25 years (range, 15-49 years). Twenty patients (71%) had constitutional symptoms at diagnosis, and eight (29%) had bulky disease.
Twenty-three patients (82%) received doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline therapy, and four (14%) received ABVD followed by escalated bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone. One patient received a different frontline regimen.
The median time to relapse was 7.9 months (range, 1.9-133 months), and 12 patients (43%) were refractory to frontline treatment.
Half of patients (n = 14) received BV-IGEV as first salvage. The regimen was given as follows: ifosfamide at 2,000 mg/m2 on days 1-4, gemcitabine at 800 mg/m2 on days 1 and 4, vinorelbine at 20 mg/m2 on day 1, prednisolone at 100 mg on days 1-4, and BV at a dose of 1.8 mg/kg on day 1 of each 3-week IGEV course.
All patients received at least two cycles of BV-IGEV and were assessed for response after one or two cycles. The median follow-up was 17 months (range, 0-65 months).
Twenty patients (71%) had a complete metabolic response to BV-IGEV, seven (25%) had a partial metabolic response, and one patient (4%) had stable disease. The patient with stable disease went on to receive another salvage regimen and achieved a partial response to that regimen.
The most common adverse events during BV-IGEV treatment were grade 3-4 neutropenia (n = 27; 96%) and thrombocytopenia (n = 25; 89%). Febrile neutropenia was also common (n = 16; 57%), as were mucositis (n = 6; 21%) and diarrhea (n = 6; 21%). Six patients had a reduction in BV dose because of an adverse event.
All patients underwent autologous HSCT. They received carmustine, etoposide, cytarabine, and melphalan as conditioning beforehand, and 18 patients (64%) received consolidative BV after transplant.
PFS and OS were calculated from the date of stem cell infusion. The estimated 2-year PFS was 87.1%, and the estimated 2-year OS was 73.5%.
Patients who received BV-IGEV as first salvage fared better than those who received the regimen as second salvage. The PFS rates were 100% and 75%, respectively (P = .0078), and OS rates were 100% and 50%, respectively (P = .08).
Six patients relapsed after HSCT, and three died. Two patients died of progressive disease and one died of pulmonary infection.
These results suggest BV-IGEV can produce high response rates without compromising stem cell mobilization, but the combination should be investigated further, according to the researchers.
The researchers reported having no conflicts of interest.
SOURCE: Abuelgasim KA et al. Bone Marrow Transplant. 2019 Jan 30. doi: 10.1038/s41409-019-0454-z.
FROM BONE MARROW TRANSPLANTATION
FDA grants priority review to polatuzumab vedotin for DLBCL
With this BLA, Genentech is seeking approval for polatuzumab vedotin in combination with bendamustine and rituximab (BR) to treat patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency aims to take action on a priority review application within 6 months, rather than the standard 10 months.
The FDA is expected to make a decision on this BLA by Aug. 19, 2019.
The BLA is supported by a phase 1b/2 trial (NCT02257567) of patients with relapsed or refractory follicular lymphoma or DLBCL who received polatuzumab vedotin in combination with BR or obinutuzumab.
The trial’s phase 2 stage included 80 DLBCL patients who were randomized to receive BR or BR plus polatuzumab vedotin, according to Genentech.
The complete response rate was 40% in the polatuzumab vedotin arm and 18% in the BR arm. The median duration of response was 10.3 months and 4.1 months, respectively (hazard ratio [HR] = 0.44).
The median progression-free survival was 7.6 months in the polatuzumab vedotin arm and 2.0 months in the BR arm (HR = 0.34).
Among patients who were ineligible for a transplant, the median overall survival (an exploratory endpoint) was 12.4 months in the polatuzumab vedotin arm and 4.7 months in the BR arm (HR = 0.42).
Patients who received polatuzumab vedotin had higher rates of grade 3-4 cytopenias, compared with patients who received BR alone. Rates of infection and transfusion were similar between the arms.
With this BLA, Genentech is seeking approval for polatuzumab vedotin in combination with bendamustine and rituximab (BR) to treat patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency aims to take action on a priority review application within 6 months, rather than the standard 10 months.
The FDA is expected to make a decision on this BLA by Aug. 19, 2019.
The BLA is supported by a phase 1b/2 trial (NCT02257567) of patients with relapsed or refractory follicular lymphoma or DLBCL who received polatuzumab vedotin in combination with BR or obinutuzumab.
The trial’s phase 2 stage included 80 DLBCL patients who were randomized to receive BR or BR plus polatuzumab vedotin, according to Genentech.
The complete response rate was 40% in the polatuzumab vedotin arm and 18% in the BR arm. The median duration of response was 10.3 months and 4.1 months, respectively (hazard ratio [HR] = 0.44).
The median progression-free survival was 7.6 months in the polatuzumab vedotin arm and 2.0 months in the BR arm (HR = 0.34).
Among patients who were ineligible for a transplant, the median overall survival (an exploratory endpoint) was 12.4 months in the polatuzumab vedotin arm and 4.7 months in the BR arm (HR = 0.42).
Patients who received polatuzumab vedotin had higher rates of grade 3-4 cytopenias, compared with patients who received BR alone. Rates of infection and transfusion were similar between the arms.
With this BLA, Genentech is seeking approval for polatuzumab vedotin in combination with bendamustine and rituximab (BR) to treat patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL).
The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions. The agency aims to take action on a priority review application within 6 months, rather than the standard 10 months.
The FDA is expected to make a decision on this BLA by Aug. 19, 2019.
The BLA is supported by a phase 1b/2 trial (NCT02257567) of patients with relapsed or refractory follicular lymphoma or DLBCL who received polatuzumab vedotin in combination with BR or obinutuzumab.
The trial’s phase 2 stage included 80 DLBCL patients who were randomized to receive BR or BR plus polatuzumab vedotin, according to Genentech.
The complete response rate was 40% in the polatuzumab vedotin arm and 18% in the BR arm. The median duration of response was 10.3 months and 4.1 months, respectively (hazard ratio [HR] = 0.44).
The median progression-free survival was 7.6 months in the polatuzumab vedotin arm and 2.0 months in the BR arm (HR = 0.34).
Among patients who were ineligible for a transplant, the median overall survival (an exploratory endpoint) was 12.4 months in the polatuzumab vedotin arm and 4.7 months in the BR arm (HR = 0.42).
Patients who received polatuzumab vedotin had higher rates of grade 3-4 cytopenias, compared with patients who received BR alone. Rates of infection and transfusion were similar between the arms.
FDA approves turoctocog alfa pegol for hemophilia A
The agency approved turoctocog alfa pegol for use as routine prophylaxis to reduce the frequency of bleeding episodes, for on-demand treatment and control of bleeding episodes, and for perioperative management of bleeding in adults and children with hemophilia A.
Turoctocog alfa pegol will not be available in the United States before 2020, according to Novo Nordisk. The company cannot yet launch the product because of third-party intellectual property agreements.
The FDA’s approval of turoctocog alfa pegol was supported by results from the pathfinder 2 (NCT01480180), pathfinder 3 (NCT01489111), and pathfinder 5 (NCT01731600) trials.
The trials included children, adolescents, and adults with previously treated, severe hemophilia A and no history of inhibitors. Turoctocog alfa pegol was considered effective and well tolerated in these trials.
Pooled results from pathfinder 2 and pathfinder 5 were presented at the 2018 annual meeting of the American Society of Hematology (Blood. 2018:132:1177).
Results from pathfinder 3 were previously published in Haemophilia (2017. Sep;23[5]:689-96).
The agency approved turoctocog alfa pegol for use as routine prophylaxis to reduce the frequency of bleeding episodes, for on-demand treatment and control of bleeding episodes, and for perioperative management of bleeding in adults and children with hemophilia A.
Turoctocog alfa pegol will not be available in the United States before 2020, according to Novo Nordisk. The company cannot yet launch the product because of third-party intellectual property agreements.
The FDA’s approval of turoctocog alfa pegol was supported by results from the pathfinder 2 (NCT01480180), pathfinder 3 (NCT01489111), and pathfinder 5 (NCT01731600) trials.
The trials included children, adolescents, and adults with previously treated, severe hemophilia A and no history of inhibitors. Turoctocog alfa pegol was considered effective and well tolerated in these trials.
Pooled results from pathfinder 2 and pathfinder 5 were presented at the 2018 annual meeting of the American Society of Hematology (Blood. 2018:132:1177).
Results from pathfinder 3 were previously published in Haemophilia (2017. Sep;23[5]:689-96).
The agency approved turoctocog alfa pegol for use as routine prophylaxis to reduce the frequency of bleeding episodes, for on-demand treatment and control of bleeding episodes, and for perioperative management of bleeding in adults and children with hemophilia A.
Turoctocog alfa pegol will not be available in the United States before 2020, according to Novo Nordisk. The company cannot yet launch the product because of third-party intellectual property agreements.
The FDA’s approval of turoctocog alfa pegol was supported by results from the pathfinder 2 (NCT01480180), pathfinder 3 (NCT01489111), and pathfinder 5 (NCT01731600) trials.
The trials included children, adolescents, and adults with previously treated, severe hemophilia A and no history of inhibitors. Turoctocog alfa pegol was considered effective and well tolerated in these trials.
Pooled results from pathfinder 2 and pathfinder 5 were presented at the 2018 annual meeting of the American Society of Hematology (Blood. 2018:132:1177).
Results from pathfinder 3 were previously published in Haemophilia (2017. Sep;23[5]:689-96).
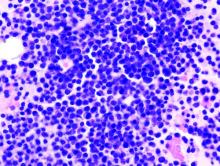
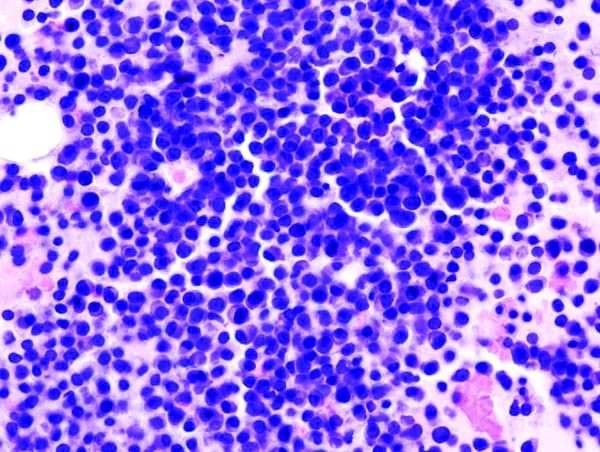
Researchers characterize new subtype of high-grade DLBCL
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
FROM THE JOURNAL OF CLINICAL ONCOLOGY
CAR T-cell therapies difficult to compare
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
FROM JOURNAL OF CLINICAL ONCOLOGY
EC approves BV plus AVD for Hodgkin lymphoma
The to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
This is the fifth approved indication for BV (adults with CD30+ HL at increased risk of relapse or progression after autologous stem cell transplant (ASCT); relapsed or refractory, CD30+ HL after ASCT or at least two prior therapies when ASCT or multi-agent chemotherapy is not an option; relapsed or refractory systemic anaplastic large-cell lymphoma; and CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
The EC’s approval of BV plus AVD is supported by the phase 3 ECHELON-1 trial (N Engl J Med. 2018;378:331-44).
ECHELON-1 included 1,334 patients with advanced HL who received BV plus AVD (n = 664) or doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD, n = 670) as frontline treatment.
The study's primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV plus AVD provided a significant improvement in modified PFS. The 2-year modified PFS rate was 82% in the BV-AVD arm and 77% in the ABVD arm (hazard ratio = 0.77; P = .04).
There was no significant difference between the treatment arms in response rates or overall survival.
The overall incidence of adverse events (AEs) was 99% in the BV-AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively. The incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV-AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a Takeda company) in collaboration with Seattle Genetics.
The to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
This is the fifth approved indication for BV (adults with CD30+ HL at increased risk of relapse or progression after autologous stem cell transplant (ASCT); relapsed or refractory, CD30+ HL after ASCT or at least two prior therapies when ASCT or multi-agent chemotherapy is not an option; relapsed or refractory systemic anaplastic large-cell lymphoma; and CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
The EC’s approval of BV plus AVD is supported by the phase 3 ECHELON-1 trial (N Engl J Med. 2018;378:331-44).
ECHELON-1 included 1,334 patients with advanced HL who received BV plus AVD (n = 664) or doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD, n = 670) as frontline treatment.
The study's primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV plus AVD provided a significant improvement in modified PFS. The 2-year modified PFS rate was 82% in the BV-AVD arm and 77% in the ABVD arm (hazard ratio = 0.77; P = .04).
There was no significant difference between the treatment arms in response rates or overall survival.
The overall incidence of adverse events (AEs) was 99% in the BV-AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively. The incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV-AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a Takeda company) in collaboration with Seattle Genetics.
The to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
This is the fifth approved indication for BV (adults with CD30+ HL at increased risk of relapse or progression after autologous stem cell transplant (ASCT); relapsed or refractory, CD30+ HL after ASCT or at least two prior therapies when ASCT or multi-agent chemotherapy is not an option; relapsed or refractory systemic anaplastic large-cell lymphoma; and CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
The EC’s approval of BV plus AVD is supported by the phase 3 ECHELON-1 trial (N Engl J Med. 2018;378:331-44).
ECHELON-1 included 1,334 patients with advanced HL who received BV plus AVD (n = 664) or doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD, n = 670) as frontline treatment.
The study's primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV plus AVD provided a significant improvement in modified PFS. The 2-year modified PFS rate was 82% in the BV-AVD arm and 77% in the ABVD arm (hazard ratio = 0.77; P = .04).
There was no significant difference between the treatment arms in response rates or overall survival.
The overall incidence of adverse events (AEs) was 99% in the BV-AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively. The incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV-AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a Takeda company) in collaboration with Seattle Genetics.
Few DLBCL patients benefit from nivolumab
Nivolumab may provide a benefit for a small group of patients with diffuse large B-cell lymphoma (DLBCL) who have failed a transplant or are ineligible for one, according to researchers.
Nivolumab produced a response in 10 of 121 DLBCL patients studied. Three patients achieved a complete response (CR) lasting 11 months or more.
Why this small group responded to nivolumab isn’t clear, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minn., and his colleagues.
Some responders did have 9p24.1 alterations, but others did not. None of the responders had tumor cells positive for programmed death–ligand 1 (PD-L1), and only one responder had detectable PD-L2 expression in malignant cells.
Dr. Ansell and his colleagues described these findings in the Journal of Clinical Oncology.
The researchers evaluated nivolumab in a phase 2 trial (NCT02038933) of patients with relapsed/refractory DLBCL. Of the 121 patients, 87 had failed autologous hematopoietic stem cell transplant (HSCT) and 34 were ineligible for autologous HSCT. The patients received nivolumab at 3 mg/kg every 2 weeks until disease progression, unacceptable toxicity, or study withdrawal.
HSCT failures
The patients who had failed HSCT had a median age of 62 years (range, 24-75 years). They had received a median of three prior systemic therapies (range, 1-11), and 28% were refractory to their most recent therapy.
About 40% of patients had germinal center B-cell–like (GCB) DLBCL, 32% had non-GCB disease, and data on disease subtype were missing for the rest of the group.
The patients received a median of four nivolumab doses (range, 1-44) and were followed for a median of 9 months (range, 0.1-25 months).
Nine patients (10%) achieved a response, and the median duration of response was 11 months. Responses occurred in patients with GCB and non-GCB DLBCL.
Three patients achieved a CR. Two of them were still on treatment and in CR at the data cutoff. Their responses had lasted 11 months and 14 months, respectively. The third complete responder did not progress on nivolumab but developed myelodysplastic syndrome, which was unrelated to the drug, and died.
Among all patients who had failed HSCT, the median progression-free survival was 1.9 months, and the median overall survival was 12.2 months.
Seven patients in this group were still receiving nivolumab at the data cutoff. Two of them were in CR, two had a partial response, and three had stable disease.
HSCT-ineligible group
The patients who were ineligible for HSCT had a median age of 68 years (range, 28-86 years). They had received a median of three prior systemic therapies (range, 1-7), and 59% were refractory to their most recent therapy.
About 56% of these patients had GCB DLBCL, 18% had non-GCB disease, and data on subtype were missing for the rest of the group.
The patients received a median of three nivolumab doses (range, 1-22) and were followed for a median of 6 months (range, 0.2-24 months). One patient (3%) achieved a partial response, which lasted 8.3 months.
The median progression-free survival in this group was 1.4 months, and the median overall survival was 5.8 months.
None of the patients in this group were still taking nivolumab at the data cutoff.
Biomarkers of response
Dr. Ansell and his colleagues were able to look for 9p24.1 alterations in archival tumor biopsy specimens from 74 patients. The team reported that 9p24.1 alterations were “infrequent,” but they were found in some responders.
Among the three complete responders, one patient had high-level 9p24.1 amplification, one had normal 9p24.1 copy number, and one did not have a biopsy available.
Among the seven patients who achieved a partial response, five had biopsy specimens. Three patients had low-level polysomy, one had copy gain, and one patient had normal 9p24.1.
None of the responders had PD-L1 expression in their tumor cells, but one complete responder had PD-L2–positive malignant cells.
Dr. Ansell and his colleagues wrote that the “biologic basis for response in the other two [complete responders] is unclear,” and the researchers were unable to assess associations between response and c-myc expression or double-hit lymphoma.
Safety
Of all 121 patients, 62% had a treatment-related adverse event (AE) and 24% had a grade 3/4–related AE.
The most common related AEs of any grade were nausea (17%), fatigue (17%), diarrhea (10%), neutropenia (7%), thrombocytopenia (6%), decreased appetite (6%), lipase increase (5%), rash (5%), and pyrexia (5%).
Four patients (3%) stopped taking nivolumab because of treatment-related AEs, including neutropenia, thrombocytopenia, diarrhea, pancreatitis, lipase increase, and psoriasiform dermatitis. There were no fatal treatment-related AEs.
This research was supported by Bristol-Myers Squibb and other groups. The study authors reported relationships with Bristol-Myers Squibb and other companies.
SOURCE: Ansell SM et al. J Clin Oncol. 2019 Jan 8. doi: 10.1200/JCO.18.00766.
Nivolumab may provide a benefit for a small group of patients with diffuse large B-cell lymphoma (DLBCL) who have failed a transplant or are ineligible for one, according to researchers.
Nivolumab produced a response in 10 of 121 DLBCL patients studied. Three patients achieved a complete response (CR) lasting 11 months or more.
Why this small group responded to nivolumab isn’t clear, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minn., and his colleagues.
Some responders did have 9p24.1 alterations, but others did not. None of the responders had tumor cells positive for programmed death–ligand 1 (PD-L1), and only one responder had detectable PD-L2 expression in malignant cells.
Dr. Ansell and his colleagues described these findings in the Journal of Clinical Oncology.
The researchers evaluated nivolumab in a phase 2 trial (NCT02038933) of patients with relapsed/refractory DLBCL. Of the 121 patients, 87 had failed autologous hematopoietic stem cell transplant (HSCT) and 34 were ineligible for autologous HSCT. The patients received nivolumab at 3 mg/kg every 2 weeks until disease progression, unacceptable toxicity, or study withdrawal.
HSCT failures
The patients who had failed HSCT had a median age of 62 years (range, 24-75 years). They had received a median of three prior systemic therapies (range, 1-11), and 28% were refractory to their most recent therapy.
About 40% of patients had germinal center B-cell–like (GCB) DLBCL, 32% had non-GCB disease, and data on disease subtype were missing for the rest of the group.
The patients received a median of four nivolumab doses (range, 1-44) and were followed for a median of 9 months (range, 0.1-25 months).
Nine patients (10%) achieved a response, and the median duration of response was 11 months. Responses occurred in patients with GCB and non-GCB DLBCL.
Three patients achieved a CR. Two of them were still on treatment and in CR at the data cutoff. Their responses had lasted 11 months and 14 months, respectively. The third complete responder did not progress on nivolumab but developed myelodysplastic syndrome, which was unrelated to the drug, and died.
Among all patients who had failed HSCT, the median progression-free survival was 1.9 months, and the median overall survival was 12.2 months.
Seven patients in this group were still receiving nivolumab at the data cutoff. Two of them were in CR, two had a partial response, and three had stable disease.
HSCT-ineligible group
The patients who were ineligible for HSCT had a median age of 68 years (range, 28-86 years). They had received a median of three prior systemic therapies (range, 1-7), and 59% were refractory to their most recent therapy.
About 56% of these patients had GCB DLBCL, 18% had non-GCB disease, and data on subtype were missing for the rest of the group.
The patients received a median of three nivolumab doses (range, 1-22) and were followed for a median of 6 months (range, 0.2-24 months). One patient (3%) achieved a partial response, which lasted 8.3 months.
The median progression-free survival in this group was 1.4 months, and the median overall survival was 5.8 months.
None of the patients in this group were still taking nivolumab at the data cutoff.
Biomarkers of response
Dr. Ansell and his colleagues were able to look for 9p24.1 alterations in archival tumor biopsy specimens from 74 patients. The team reported that 9p24.1 alterations were “infrequent,” but they were found in some responders.
Among the three complete responders, one patient had high-level 9p24.1 amplification, one had normal 9p24.1 copy number, and one did not have a biopsy available.
Among the seven patients who achieved a partial response, five had biopsy specimens. Three patients had low-level polysomy, one had copy gain, and one patient had normal 9p24.1.
None of the responders had PD-L1 expression in their tumor cells, but one complete responder had PD-L2–positive malignant cells.
Dr. Ansell and his colleagues wrote that the “biologic basis for response in the other two [complete responders] is unclear,” and the researchers were unable to assess associations between response and c-myc expression or double-hit lymphoma.
Safety
Of all 121 patients, 62% had a treatment-related adverse event (AE) and 24% had a grade 3/4–related AE.
The most common related AEs of any grade were nausea (17%), fatigue (17%), diarrhea (10%), neutropenia (7%), thrombocytopenia (6%), decreased appetite (6%), lipase increase (5%), rash (5%), and pyrexia (5%).
Four patients (3%) stopped taking nivolumab because of treatment-related AEs, including neutropenia, thrombocytopenia, diarrhea, pancreatitis, lipase increase, and psoriasiform dermatitis. There were no fatal treatment-related AEs.
This research was supported by Bristol-Myers Squibb and other groups. The study authors reported relationships with Bristol-Myers Squibb and other companies.
SOURCE: Ansell SM et al. J Clin Oncol. 2019 Jan 8. doi: 10.1200/JCO.18.00766.
Nivolumab may provide a benefit for a small group of patients with diffuse large B-cell lymphoma (DLBCL) who have failed a transplant or are ineligible for one, according to researchers.
Nivolumab produced a response in 10 of 121 DLBCL patients studied. Three patients achieved a complete response (CR) lasting 11 months or more.
Why this small group responded to nivolumab isn’t clear, according to Stephen M. Ansell, MD, PhD, of the Mayo Clinic in Rochester, Minn., and his colleagues.
Some responders did have 9p24.1 alterations, but others did not. None of the responders had tumor cells positive for programmed death–ligand 1 (PD-L1), and only one responder had detectable PD-L2 expression in malignant cells.
Dr. Ansell and his colleagues described these findings in the Journal of Clinical Oncology.
The researchers evaluated nivolumab in a phase 2 trial (NCT02038933) of patients with relapsed/refractory DLBCL. Of the 121 patients, 87 had failed autologous hematopoietic stem cell transplant (HSCT) and 34 were ineligible for autologous HSCT. The patients received nivolumab at 3 mg/kg every 2 weeks until disease progression, unacceptable toxicity, or study withdrawal.
HSCT failures
The patients who had failed HSCT had a median age of 62 years (range, 24-75 years). They had received a median of three prior systemic therapies (range, 1-11), and 28% were refractory to their most recent therapy.
About 40% of patients had germinal center B-cell–like (GCB) DLBCL, 32% had non-GCB disease, and data on disease subtype were missing for the rest of the group.
The patients received a median of four nivolumab doses (range, 1-44) and were followed for a median of 9 months (range, 0.1-25 months).
Nine patients (10%) achieved a response, and the median duration of response was 11 months. Responses occurred in patients with GCB and non-GCB DLBCL.
Three patients achieved a CR. Two of them were still on treatment and in CR at the data cutoff. Their responses had lasted 11 months and 14 months, respectively. The third complete responder did not progress on nivolumab but developed myelodysplastic syndrome, which was unrelated to the drug, and died.
Among all patients who had failed HSCT, the median progression-free survival was 1.9 months, and the median overall survival was 12.2 months.
Seven patients in this group were still receiving nivolumab at the data cutoff. Two of them were in CR, two had a partial response, and three had stable disease.
HSCT-ineligible group
The patients who were ineligible for HSCT had a median age of 68 years (range, 28-86 years). They had received a median of three prior systemic therapies (range, 1-7), and 59% were refractory to their most recent therapy.
About 56% of these patients had GCB DLBCL, 18% had non-GCB disease, and data on subtype were missing for the rest of the group.
The patients received a median of three nivolumab doses (range, 1-22) and were followed for a median of 6 months (range, 0.2-24 months). One patient (3%) achieved a partial response, which lasted 8.3 months.
The median progression-free survival in this group was 1.4 months, and the median overall survival was 5.8 months.
None of the patients in this group were still taking nivolumab at the data cutoff.
Biomarkers of response
Dr. Ansell and his colleagues were able to look for 9p24.1 alterations in archival tumor biopsy specimens from 74 patients. The team reported that 9p24.1 alterations were “infrequent,” but they were found in some responders.
Among the three complete responders, one patient had high-level 9p24.1 amplification, one had normal 9p24.1 copy number, and one did not have a biopsy available.
Among the seven patients who achieved a partial response, five had biopsy specimens. Three patients had low-level polysomy, one had copy gain, and one patient had normal 9p24.1.
None of the responders had PD-L1 expression in their tumor cells, but one complete responder had PD-L2–positive malignant cells.
Dr. Ansell and his colleagues wrote that the “biologic basis for response in the other two [complete responders] is unclear,” and the researchers were unable to assess associations between response and c-myc expression or double-hit lymphoma.
Safety
Of all 121 patients, 62% had a treatment-related adverse event (AE) and 24% had a grade 3/4–related AE.
The most common related AEs of any grade were nausea (17%), fatigue (17%), diarrhea (10%), neutropenia (7%), thrombocytopenia (6%), decreased appetite (6%), lipase increase (5%), rash (5%), and pyrexia (5%).
Four patients (3%) stopped taking nivolumab because of treatment-related AEs, including neutropenia, thrombocytopenia, diarrhea, pancreatitis, lipase increase, and psoriasiform dermatitis. There were no fatal treatment-related AEs.
This research was supported by Bristol-Myers Squibb and other groups. The study authors reported relationships with Bristol-Myers Squibb and other companies.
SOURCE: Ansell SM et al. J Clin Oncol. 2019 Jan 8. doi: 10.1200/JCO.18.00766.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point:
Major finding: Nivolumab produced a response in 10 of 121 patients, including three complete responses.
Study details: A phase 2 study of 121 patients with relapsed/refractory diffuse large B-cell lymphoma.
Disclosures: This research was supported by Bristol-Myers Squibb and other organizations. The study authors reported relationships with Bristol-Myers Squibb and other companies.
Source: Ansell SM et al. J Clin Oncol. 2019 Jan 8. doi: 10.1200/JCO.18.00766.