User login
Jennifer Smith is the editor of Oncology Practice, part of MDedge Hematology/Oncology. She was previously the editor of Hematology Times, an editor at Principal Investigators Association, and a reporter at The Oneida Daily Dispatch. She has a BS in journalism.
Brachytherapy proves beneficial regardless of treatment duration
, according to a retrospective study.
Researchers found that patients who received brachytherapy in addition to chemotherapy and external beam radiation therapy had better overall survival than patients who received chemoradiation alone.
Although the best overall survival was observed in patients who received brachytherapy within the recommended 8 weeks, patients who received brachytherapy outside that timeframe also had better overall survival than patients treated with chemoradiation alone.
Travis-Riley K. Korenaga, MD, of University of California, San Francisco, presented these findings at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
To examine the use of brachytherapy, Dr. Korenaga and his colleagues analyzed patients from the U.S. National Cancer Database who had stage II-IVA cervical cancer and were diagnosed between 2004 and 2015.
The researchers identified 18,592 patients who received at least 4,500 cGy of external beam radiation therapy and concurrent chemotherapy as their primary treatment. In this group, there were 17,150 patients who had data on brachytherapy use and time to treatment completion.
A majority of patients (n = 13,642) received brachytherapy, and roughly half of those (n = 6,871) received it within the recommended 8 weeks.
“This is a pretty low rate of adherence to standard of care; 36.9% of women receive brachytherapy and complete it within that 8-week timeframe,” Dr. Korenaga said. “And that 36.9% of women do have a superior overall survival that blows everything else out of the water.”
The median overall survival was:
- 113.7 months (95% confidence interval [CI], 103.3-121.3) in patients who received brachytherapy within 8 weeks
- 75.7 months (95% CI, 69.7-82.4) in those who received brachytherapy for more than 8 weeks
- 58.5 months (95% CI, 48.3-74.2) in patients who received only chemoradiation within 8 weeks
- 46.2 months (95% CI, 39.8-56.4) in those who received only chemoradiation for more than 8 weeks.
“Getting some type of brachytherapy, no matter whether it’s within 8 weeks or beyond 8 weeks, is still associated with an improved overall survival,” Dr. Korenaga noted.
He and his colleagues also identified factors that were significantly associated with a reduced likelihood of receiving brachytherapy within 8 weeks, including:
- Having stage III/IVA disease vs. stage II disease (P less than .0001)
- Being non-Hispanic black vs. non-Hispanic white (P less than .001)
- Having an annual income below $38,000 vs. $63,000 or higher (P less than .0001)
- Having public vs. private insurance (P less than .0001)
- Living 10 to 60 miles (P = .01) or more than 100 miles (P less than .001) from the treatment facility vs. less than 10 miles
- Being treated at a facility with a community cancer program (P = .02) or a comprehensive community cancer program (P less than .0001) vs. an academic research program.
Dr. Korenaga said these results highlight the fact that more work needs to be done to increase the use of brachytherapy in patients with locally advanced cervical cancer.
He and his colleagues have suggested a few measures that might help, including early referrals for brachytherapy, connecting patients with care navigators, and developing centers of excellence for brachytherapy.
Dr. Korenaga had no relevant financial disclosures.
SOURCE: Korenaga TRK et al. SGO 2019. Abstract 10.
, according to a retrospective study.
Researchers found that patients who received brachytherapy in addition to chemotherapy and external beam radiation therapy had better overall survival than patients who received chemoradiation alone.
Although the best overall survival was observed in patients who received brachytherapy within the recommended 8 weeks, patients who received brachytherapy outside that timeframe also had better overall survival than patients treated with chemoradiation alone.
Travis-Riley K. Korenaga, MD, of University of California, San Francisco, presented these findings at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
To examine the use of brachytherapy, Dr. Korenaga and his colleagues analyzed patients from the U.S. National Cancer Database who had stage II-IVA cervical cancer and were diagnosed between 2004 and 2015.
The researchers identified 18,592 patients who received at least 4,500 cGy of external beam radiation therapy and concurrent chemotherapy as their primary treatment. In this group, there were 17,150 patients who had data on brachytherapy use and time to treatment completion.
A majority of patients (n = 13,642) received brachytherapy, and roughly half of those (n = 6,871) received it within the recommended 8 weeks.
“This is a pretty low rate of adherence to standard of care; 36.9% of women receive brachytherapy and complete it within that 8-week timeframe,” Dr. Korenaga said. “And that 36.9% of women do have a superior overall survival that blows everything else out of the water.”
The median overall survival was:
- 113.7 months (95% confidence interval [CI], 103.3-121.3) in patients who received brachytherapy within 8 weeks
- 75.7 months (95% CI, 69.7-82.4) in those who received brachytherapy for more than 8 weeks
- 58.5 months (95% CI, 48.3-74.2) in patients who received only chemoradiation within 8 weeks
- 46.2 months (95% CI, 39.8-56.4) in those who received only chemoradiation for more than 8 weeks.
“Getting some type of brachytherapy, no matter whether it’s within 8 weeks or beyond 8 weeks, is still associated with an improved overall survival,” Dr. Korenaga noted.
He and his colleagues also identified factors that were significantly associated with a reduced likelihood of receiving brachytherapy within 8 weeks, including:
- Having stage III/IVA disease vs. stage II disease (P less than .0001)
- Being non-Hispanic black vs. non-Hispanic white (P less than .001)
- Having an annual income below $38,000 vs. $63,000 or higher (P less than .0001)
- Having public vs. private insurance (P less than .0001)
- Living 10 to 60 miles (P = .01) or more than 100 miles (P less than .001) from the treatment facility vs. less than 10 miles
- Being treated at a facility with a community cancer program (P = .02) or a comprehensive community cancer program (P less than .0001) vs. an academic research program.
Dr. Korenaga said these results highlight the fact that more work needs to be done to increase the use of brachytherapy in patients with locally advanced cervical cancer.
He and his colleagues have suggested a few measures that might help, including early referrals for brachytherapy, connecting patients with care navigators, and developing centers of excellence for brachytherapy.
Dr. Korenaga had no relevant financial disclosures.
SOURCE: Korenaga TRK et al. SGO 2019. Abstract 10.
, according to a retrospective study.
Researchers found that patients who received brachytherapy in addition to chemotherapy and external beam radiation therapy had better overall survival than patients who received chemoradiation alone.
Although the best overall survival was observed in patients who received brachytherapy within the recommended 8 weeks, patients who received brachytherapy outside that timeframe also had better overall survival than patients treated with chemoradiation alone.
Travis-Riley K. Korenaga, MD, of University of California, San Francisco, presented these findings at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
To examine the use of brachytherapy, Dr. Korenaga and his colleagues analyzed patients from the U.S. National Cancer Database who had stage II-IVA cervical cancer and were diagnosed between 2004 and 2015.
The researchers identified 18,592 patients who received at least 4,500 cGy of external beam radiation therapy and concurrent chemotherapy as their primary treatment. In this group, there were 17,150 patients who had data on brachytherapy use and time to treatment completion.
A majority of patients (n = 13,642) received brachytherapy, and roughly half of those (n = 6,871) received it within the recommended 8 weeks.
“This is a pretty low rate of adherence to standard of care; 36.9% of women receive brachytherapy and complete it within that 8-week timeframe,” Dr. Korenaga said. “And that 36.9% of women do have a superior overall survival that blows everything else out of the water.”
The median overall survival was:
- 113.7 months (95% confidence interval [CI], 103.3-121.3) in patients who received brachytherapy within 8 weeks
- 75.7 months (95% CI, 69.7-82.4) in those who received brachytherapy for more than 8 weeks
- 58.5 months (95% CI, 48.3-74.2) in patients who received only chemoradiation within 8 weeks
- 46.2 months (95% CI, 39.8-56.4) in those who received only chemoradiation for more than 8 weeks.
“Getting some type of brachytherapy, no matter whether it’s within 8 weeks or beyond 8 weeks, is still associated with an improved overall survival,” Dr. Korenaga noted.
He and his colleagues also identified factors that were significantly associated with a reduced likelihood of receiving brachytherapy within 8 weeks, including:
- Having stage III/IVA disease vs. stage II disease (P less than .0001)
- Being non-Hispanic black vs. non-Hispanic white (P less than .001)
- Having an annual income below $38,000 vs. $63,000 or higher (P less than .0001)
- Having public vs. private insurance (P less than .0001)
- Living 10 to 60 miles (P = .01) or more than 100 miles (P less than .001) from the treatment facility vs. less than 10 miles
- Being treated at a facility with a community cancer program (P = .02) or a comprehensive community cancer program (P less than .0001) vs. an academic research program.
Dr. Korenaga said these results highlight the fact that more work needs to be done to increase the use of brachytherapy in patients with locally advanced cervical cancer.
He and his colleagues have suggested a few measures that might help, including early referrals for brachytherapy, connecting patients with care navigators, and developing centers of excellence for brachytherapy.
Dr. Korenaga had no relevant financial disclosures.
SOURCE: Korenaga TRK et al. SGO 2019. Abstract 10.
REPORTING FROM SGO 2019
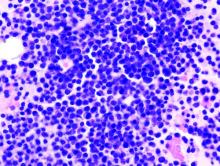
Oral triplet deemed effective in relapsed/refractory myeloma
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
An all-oral, three-drug regimen may be a treatment option for relapsed or refractory multiple myeloma, according to researchers.
The regimen – clarithromycin, pomalidomide, and dexamethasone (ClaPd) – produced an overall response rate (ORR) of 60% in a phase 2 trial of patients with relapsed/refractory multiple myeloma (RRMM). Response rates were similar whether patients were refractory to lenalidomide, bortezomib, or both drugs.
The most common adverse events (AEs) in this trial were hematologic toxicities.
Tomer M. Mark, MD, of the University of Colorado at Denver, Aurora, and his colleagues, reported these results in Blood Advances.
The trial (NCT01159574) included 120 patients with RRMM. They had a median age of 63 years (range, 42-87 years) and were a median of 4.6 years (range, 0.8-21.2 years) from diagnosis at baseline.
The patients had received a median of 5 (range, 3-15) prior lines of therapy. Most patients were refractory to lenalidomide (n = 101), bortezomib (n = 94), or both (n = 81).
The ClaPd regimen consisted of clarithromycin given at 500 mg twice daily, pomalidomide at 4 mg on days 1-21, and dexamethasone at 40 mg on days 1, 8, 15, and 22 of a 28-day cycle. The patients received ClaPd until intolerance or disease progression. In addition to ClaPd, patients received thromboprophylaxis (aspirin at 81 mg daily) and Pneumocystis jiroveci prophylaxis (trimethoprim-sulfamethoxazole or an alternative).
The toxicities were manageable, with low rates of nonhematologic and high-grade events, according to the researchers. The most common grade 3 or higher AEs were lymphopenia (60%), neutropenia (58%), leukopenia (34%), thrombocytopenia (31%), and anemia (28%).
Among all evaluable patients, the ORR was 60% (70/117). One patient had a complete response, 6 had a stringent complete response, 20 had a very good partial response, and 43 had a partial response.
ORRs were similar whether patients were refractory to bortezomib, lenalidomide, or both. The ORR was 58% (n = 59) among lenalidomide-refractory patients, 55% (n = 52) among bortezomib-refractory patients, and 54% (n = 44) among double-refractory patients.
For the entire cohort, the median progression-free survival was 7.7 months and the median overall survival was 19.2 months.
In a multivariate analysis, there were two factors significantly associated with inferior overall survival – having a revised International Staging System score greater than 1 (hazard ratio, 2.75; P = .044) and having at least 5% of CD138 cells positive for Ki67 on immunohistochemistry (hazard ratio, 1.84, P = .030).
“The ClaPd regimen demonstrated high rates of overall response and significant duration of disease control in a heavily pretreated RRMM population while maintaining a toxicity profile similar to Pom-dex [pomalidone-dexamethasone] alone,” Dr. Mark and his colleagues wrote. “The clinical efficacy advantage of adding clarithromycin to Pom-dex should be explored further in a phase 3 clinical trial.”
This research was supported by Celgene; the Myeloma Center at Weill Cornell Medicine, New York; and a grant from the National Institutes of Health. Dr. Mark reported relationships with Amgen, Takeda, Celgene, and Janssen. Other study authors reported relationships with Celgene, Takeda, and Onyx Pharmaceuticals.
SOURCE: Mark TM et al. Blood Adv. 2019 Feb 26;3(4):603-11.
FROM BLOOD ADVANCES
Guadecitabine may be option for certain MDS/AML patients
New research suggests guadecitabine may be an option for select patients with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) who have failed treatment with azacitidine.
In a phase 2 trial, eight of 56 patients with high-risk MDS or low-blast-count AML responded to guadecitabine after azacitidine failure. Patients were significantly more likely to respond if they had few or no somatic mutations.
Marie Sébert, MD, of Hôpital Saint Louis in Paris and her colleagues conducted this trial and reported the results in Haematologica.
The trial (NCT02197676) included 56 patients with the following disease types:
- Refractory anemia with excess blasts (RAEB) type 2 (n = 31; 55%).
- RAEB type 1 (n = 11; 20%).
- Low-blast-count AML (n = 11; 20%).
- Refractory cytopenias with multilineage dysplasia (RCMD; n = 2; 4%).
- Chronic myelomonocytic leukemia (n = 1; 2%).
The patients had a median age of 75 years (range, 70-79) at baseline, and 37 (66%) were men. Thirty-four patients (61%) had very-high-risk disease according to the revised International Prognostic Scoring System. Forty-nine patients (87.5%) had at least one somatic mutation. The most commonly mutated genes were ASXL1, RUNX1, TP53, U2AF1, and DNMT3A.
Most patients (n = 41, 73%) had relapsed after azacitidine, and 15 (27%) had primary resistance to the drug. Patients had received a median of 13 azacitidine cycles (range, 6-23).
The patients received guadecitabine subcutaneously at 60 mg/m2 on days 1-5 of a 28-day cycle. They were treated until progression, death, unacceptable toxicity, or no response after six to nine cycles. Patients received a median of three cycles (range, 0-27). One patient died of infection before receiving guadecitabine, but the remaining 55 patients received at least one cycle of treatment. Eighteen patients had a dose reduction.
Eight patients (14.3%) responded to guadecitabine. Two patients achieved a complete response (CR) – one who had RAEB-2 and one with AML. Two patients with RAEB-1 had marrow CRs. Two patients – one with RAEB-2 and one with AML – had marrow CRs with hematologic improvement. A patient with RCMD had hematologic improvement, and a patient with RAEB-2 had a partial response.
The researchers said mutation frequency was the only significant predictor of response. The response rate was significantly higher in patients who did not have somatic mutations (P = .036). The median number of mutations was one (range, zero to three) in responders and two (range, zero to six) in nonresponders (P = .035). None of the patients with TP53 mutations achieved a response.
The median duration of response was 11.5 months. The median overall survival was 17.9 months in responders and 7.1 months in the overall population.
In a multivariate analysis, the following factors were significantly associated with longer survival:
- Having low- to high-risk (vs. very-high-risk) disease (P = .03).
- Having experienced primary (vs. secondary) azacitidine failure (P = .01).
- Having a high rate of demethylation in blood during the first treatment cycle (P = .03).
There were 99 serious adverse events (AEs) reported in 44 patients. Most AEs were hematologic events, and the most common of these was myelosuppression (n = 88; 88%). The most common grade 3/4 nonhematologic AE was pulmonary toxicity (n = 7; 12.5%). Thirteen patients were hospitalized for febrile neutropenia for a median of 14 days.
The researchers said patients reported less pain and fewer secondary lesions with guadecitabine than they had with azacitidine.
This trial was sponsored by Groupe Francophone des Myelodysplasies in collaboration with Astex Pharmaceuticals. The researchers reported having no competing interests.
SOURCE: Sébert M et al. Haematologica. 2019 Feb 7. doi: 0.3324/haematol.2018.207118.
New research suggests guadecitabine may be an option for select patients with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) who have failed treatment with azacitidine.
In a phase 2 trial, eight of 56 patients with high-risk MDS or low-blast-count AML responded to guadecitabine after azacitidine failure. Patients were significantly more likely to respond if they had few or no somatic mutations.
Marie Sébert, MD, of Hôpital Saint Louis in Paris and her colleagues conducted this trial and reported the results in Haematologica.
The trial (NCT02197676) included 56 patients with the following disease types:
- Refractory anemia with excess blasts (RAEB) type 2 (n = 31; 55%).
- RAEB type 1 (n = 11; 20%).
- Low-blast-count AML (n = 11; 20%).
- Refractory cytopenias with multilineage dysplasia (RCMD; n = 2; 4%).
- Chronic myelomonocytic leukemia (n = 1; 2%).
The patients had a median age of 75 years (range, 70-79) at baseline, and 37 (66%) were men. Thirty-four patients (61%) had very-high-risk disease according to the revised International Prognostic Scoring System. Forty-nine patients (87.5%) had at least one somatic mutation. The most commonly mutated genes were ASXL1, RUNX1, TP53, U2AF1, and DNMT3A.
Most patients (n = 41, 73%) had relapsed after azacitidine, and 15 (27%) had primary resistance to the drug. Patients had received a median of 13 azacitidine cycles (range, 6-23).
The patients received guadecitabine subcutaneously at 60 mg/m2 on days 1-5 of a 28-day cycle. They were treated until progression, death, unacceptable toxicity, or no response after six to nine cycles. Patients received a median of three cycles (range, 0-27). One patient died of infection before receiving guadecitabine, but the remaining 55 patients received at least one cycle of treatment. Eighteen patients had a dose reduction.
Eight patients (14.3%) responded to guadecitabine. Two patients achieved a complete response (CR) – one who had RAEB-2 and one with AML. Two patients with RAEB-1 had marrow CRs. Two patients – one with RAEB-2 and one with AML – had marrow CRs with hematologic improvement. A patient with RCMD had hematologic improvement, and a patient with RAEB-2 had a partial response.
The researchers said mutation frequency was the only significant predictor of response. The response rate was significantly higher in patients who did not have somatic mutations (P = .036). The median number of mutations was one (range, zero to three) in responders and two (range, zero to six) in nonresponders (P = .035). None of the patients with TP53 mutations achieved a response.
The median duration of response was 11.5 months. The median overall survival was 17.9 months in responders and 7.1 months in the overall population.
In a multivariate analysis, the following factors were significantly associated with longer survival:
- Having low- to high-risk (vs. very-high-risk) disease (P = .03).
- Having experienced primary (vs. secondary) azacitidine failure (P = .01).
- Having a high rate of demethylation in blood during the first treatment cycle (P = .03).
There were 99 serious adverse events (AEs) reported in 44 patients. Most AEs were hematologic events, and the most common of these was myelosuppression (n = 88; 88%). The most common grade 3/4 nonhematologic AE was pulmonary toxicity (n = 7; 12.5%). Thirteen patients were hospitalized for febrile neutropenia for a median of 14 days.
The researchers said patients reported less pain and fewer secondary lesions with guadecitabine than they had with azacitidine.
This trial was sponsored by Groupe Francophone des Myelodysplasies in collaboration with Astex Pharmaceuticals. The researchers reported having no competing interests.
SOURCE: Sébert M et al. Haematologica. 2019 Feb 7. doi: 0.3324/haematol.2018.207118.
New research suggests guadecitabine may be an option for select patients with myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) who have failed treatment with azacitidine.
In a phase 2 trial, eight of 56 patients with high-risk MDS or low-blast-count AML responded to guadecitabine after azacitidine failure. Patients were significantly more likely to respond if they had few or no somatic mutations.
Marie Sébert, MD, of Hôpital Saint Louis in Paris and her colleagues conducted this trial and reported the results in Haematologica.
The trial (NCT02197676) included 56 patients with the following disease types:
- Refractory anemia with excess blasts (RAEB) type 2 (n = 31; 55%).
- RAEB type 1 (n = 11; 20%).
- Low-blast-count AML (n = 11; 20%).
- Refractory cytopenias with multilineage dysplasia (RCMD; n = 2; 4%).
- Chronic myelomonocytic leukemia (n = 1; 2%).
The patients had a median age of 75 years (range, 70-79) at baseline, and 37 (66%) were men. Thirty-four patients (61%) had very-high-risk disease according to the revised International Prognostic Scoring System. Forty-nine patients (87.5%) had at least one somatic mutation. The most commonly mutated genes were ASXL1, RUNX1, TP53, U2AF1, and DNMT3A.
Most patients (n = 41, 73%) had relapsed after azacitidine, and 15 (27%) had primary resistance to the drug. Patients had received a median of 13 azacitidine cycles (range, 6-23).
The patients received guadecitabine subcutaneously at 60 mg/m2 on days 1-5 of a 28-day cycle. They were treated until progression, death, unacceptable toxicity, or no response after six to nine cycles. Patients received a median of three cycles (range, 0-27). One patient died of infection before receiving guadecitabine, but the remaining 55 patients received at least one cycle of treatment. Eighteen patients had a dose reduction.
Eight patients (14.3%) responded to guadecitabine. Two patients achieved a complete response (CR) – one who had RAEB-2 and one with AML. Two patients with RAEB-1 had marrow CRs. Two patients – one with RAEB-2 and one with AML – had marrow CRs with hematologic improvement. A patient with RCMD had hematologic improvement, and a patient with RAEB-2 had a partial response.
The researchers said mutation frequency was the only significant predictor of response. The response rate was significantly higher in patients who did not have somatic mutations (P = .036). The median number of mutations was one (range, zero to three) in responders and two (range, zero to six) in nonresponders (P = .035). None of the patients with TP53 mutations achieved a response.
The median duration of response was 11.5 months. The median overall survival was 17.9 months in responders and 7.1 months in the overall population.
In a multivariate analysis, the following factors were significantly associated with longer survival:
- Having low- to high-risk (vs. very-high-risk) disease (P = .03).
- Having experienced primary (vs. secondary) azacitidine failure (P = .01).
- Having a high rate of demethylation in blood during the first treatment cycle (P = .03).
There were 99 serious adverse events (AEs) reported in 44 patients. Most AEs were hematologic events, and the most common of these was myelosuppression (n = 88; 88%). The most common grade 3/4 nonhematologic AE was pulmonary toxicity (n = 7; 12.5%). Thirteen patients were hospitalized for febrile neutropenia for a median of 14 days.
The researchers said patients reported less pain and fewer secondary lesions with guadecitabine than they had with azacitidine.
This trial was sponsored by Groupe Francophone des Myelodysplasies in collaboration with Astex Pharmaceuticals. The researchers reported having no competing interests.
SOURCE: Sébert M et al. Haematologica. 2019 Feb 7. doi: 0.3324/haematol.2018.207118.
REPORTING FROM HAEMATOLOGICA
Early career researchers win funding
John Krais, PhD, a researcher at Fox Chase Cancer Center in Philadelphia, has received a $75,000 grant from the Ovarian Cancer Research Alliance.
Dr. Krais received the 2-year grant to fund his investigation into DNA repair processes in BRCA1-mutant cancers, which will focus on the RNF168 protein.
Seven other early career researchers have joined the Parker Institute for Cancer Immunotherapy as part of the Parker Scholars, Parker Bridge Scholars, and Parker Fellows programs.
These researchers will receive a total of up to $3.1 million in funding to further their research on immunotherapies for cancers. Cécile Alanio, MD, PhD, a Parker Bridge Scholar at the University of Pennsylvania in Philadelphia, is researching the impact of infections on T cells in healthy patients with the goal of revealing new approaches to immunotherapy for cancer patients.
Kenneth Hu, PhD, a Parker Scholar at the University of California, San Francisco, plans to use single-cell profiling and microscopy to gain a better understanding of immune cells’ interactions in the tumor microenvironment.
Xihao (Sherlock) Hu, PhD, a Parker Scholar at the Dana-Farber Cancer Institute in Boston, plans to study the interactions between tumor antigens and tumor-infiltrating B cells.
Justin Eyquem, PhD, a Parker Fellow at the University of California, San Francisco, plans to use a genome-editing platform he developed to improve the function of chimeric antigen receptor (CAR) T cells in solid tumors.
Tijana Martinov, PhD, a Parker Scholar at Fred Hutchinson Cancer Research Center in Seattle, is seeking to produce T cells that can target multiple myeloma cells.
Sierra McDonald, a PhD candidate and Parker Scholar at the University of Pennsylvania, is investigating ways to improve responses to CAR T-cell therapy by studying the HMG-box family of proteins.
Roberta Zappasodi, PhD, of Memorial Sloan Kettering Cancer Center in New York, is transitioning from a Parker Scholar to a Parker Bridge Scholar. She previously characterized a population of immune-suppressive T cells. Now, she is working to determine how these cells can be used to improve the efficacy of checkpoint inhibition.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
John Krais, PhD, a researcher at Fox Chase Cancer Center in Philadelphia, has received a $75,000 grant from the Ovarian Cancer Research Alliance.
Dr. Krais received the 2-year grant to fund his investigation into DNA repair processes in BRCA1-mutant cancers, which will focus on the RNF168 protein.
Seven other early career researchers have joined the Parker Institute for Cancer Immunotherapy as part of the Parker Scholars, Parker Bridge Scholars, and Parker Fellows programs.
These researchers will receive a total of up to $3.1 million in funding to further their research on immunotherapies for cancers. Cécile Alanio, MD, PhD, a Parker Bridge Scholar at the University of Pennsylvania in Philadelphia, is researching the impact of infections on T cells in healthy patients with the goal of revealing new approaches to immunotherapy for cancer patients.
Kenneth Hu, PhD, a Parker Scholar at the University of California, San Francisco, plans to use single-cell profiling and microscopy to gain a better understanding of immune cells’ interactions in the tumor microenvironment.
Xihao (Sherlock) Hu, PhD, a Parker Scholar at the Dana-Farber Cancer Institute in Boston, plans to study the interactions between tumor antigens and tumor-infiltrating B cells.
Justin Eyquem, PhD, a Parker Fellow at the University of California, San Francisco, plans to use a genome-editing platform he developed to improve the function of chimeric antigen receptor (CAR) T cells in solid tumors.
Tijana Martinov, PhD, a Parker Scholar at Fred Hutchinson Cancer Research Center in Seattle, is seeking to produce T cells that can target multiple myeloma cells.
Sierra McDonald, a PhD candidate and Parker Scholar at the University of Pennsylvania, is investigating ways to improve responses to CAR T-cell therapy by studying the HMG-box family of proteins.
Roberta Zappasodi, PhD, of Memorial Sloan Kettering Cancer Center in New York, is transitioning from a Parker Scholar to a Parker Bridge Scholar. She previously characterized a population of immune-suppressive T cells. Now, she is working to determine how these cells can be used to improve the efficacy of checkpoint inhibition.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
John Krais, PhD, a researcher at Fox Chase Cancer Center in Philadelphia, has received a $75,000 grant from the Ovarian Cancer Research Alliance.
Dr. Krais received the 2-year grant to fund his investigation into DNA repair processes in BRCA1-mutant cancers, which will focus on the RNF168 protein.
Seven other early career researchers have joined the Parker Institute for Cancer Immunotherapy as part of the Parker Scholars, Parker Bridge Scholars, and Parker Fellows programs.
These researchers will receive a total of up to $3.1 million in funding to further their research on immunotherapies for cancers. Cécile Alanio, MD, PhD, a Parker Bridge Scholar at the University of Pennsylvania in Philadelphia, is researching the impact of infections on T cells in healthy patients with the goal of revealing new approaches to immunotherapy for cancer patients.
Kenneth Hu, PhD, a Parker Scholar at the University of California, San Francisco, plans to use single-cell profiling and microscopy to gain a better understanding of immune cells’ interactions in the tumor microenvironment.
Xihao (Sherlock) Hu, PhD, a Parker Scholar at the Dana-Farber Cancer Institute in Boston, plans to study the interactions between tumor antigens and tumor-infiltrating B cells.
Justin Eyquem, PhD, a Parker Fellow at the University of California, San Francisco, plans to use a genome-editing platform he developed to improve the function of chimeric antigen receptor (CAR) T cells in solid tumors.
Tijana Martinov, PhD, a Parker Scholar at Fred Hutchinson Cancer Research Center in Seattle, is seeking to produce T cells that can target multiple myeloma cells.
Sierra McDonald, a PhD candidate and Parker Scholar at the University of Pennsylvania, is investigating ways to improve responses to CAR T-cell therapy by studying the HMG-box family of proteins.
Roberta Zappasodi, PhD, of Memorial Sloan Kettering Cancer Center in New York, is transitioning from a Parker Scholar to a Parker Bridge Scholar. She previously characterized a population of immune-suppressive T cells. Now, she is working to determine how these cells can be used to improve the efficacy of checkpoint inhibition.
Movers in Medicine highlights career moves and personal achievements by hematologists and oncologists. Did you switch jobs, take on a new role, climb a mountain? Tell us all about it at [email protected], and you could be featured in Movers in Medicine.
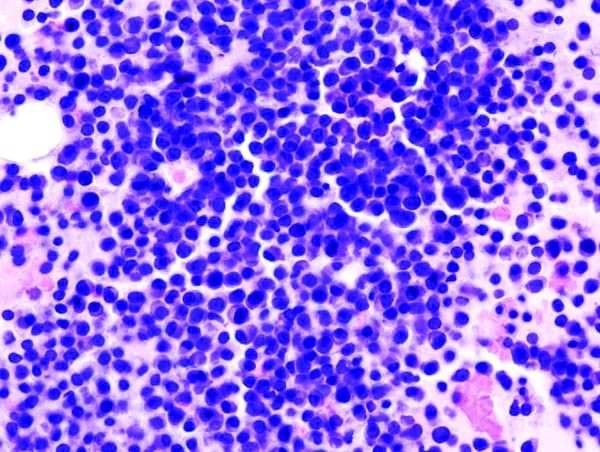
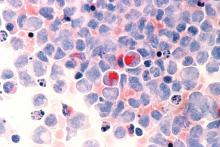
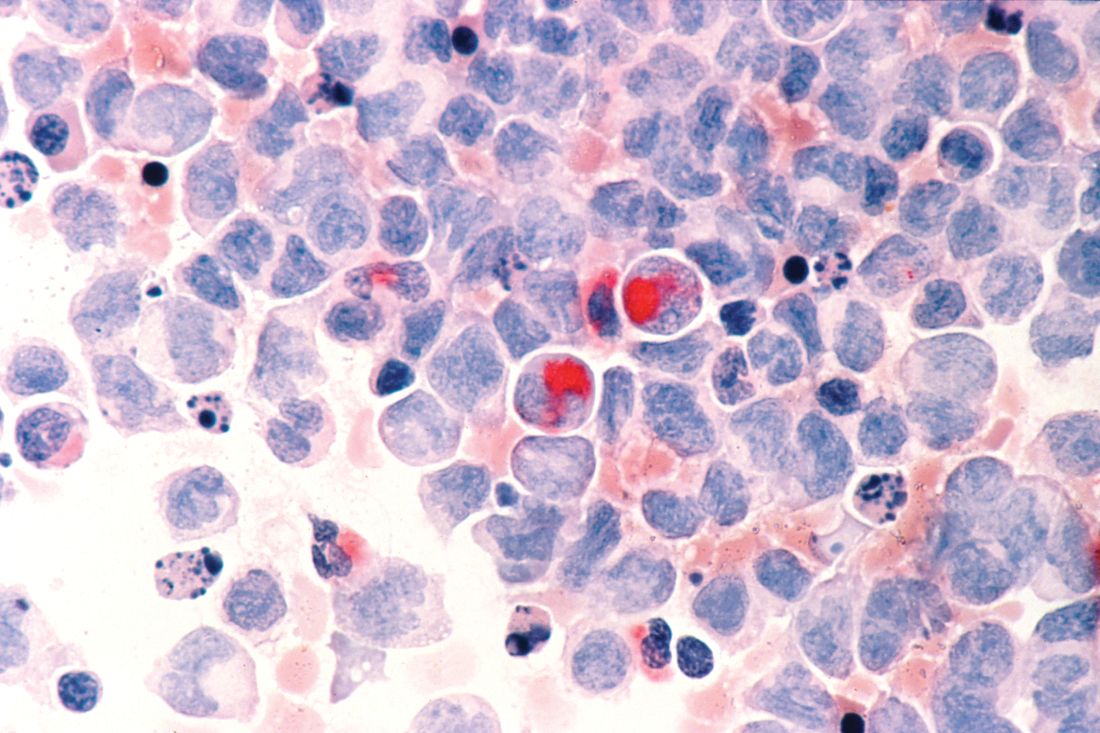
Analysis suggests ‘Burkitt-like lymphoma’ is a misnomer
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
They found that BLL-11q has a genomic and mutational profile more closely related to that of high grade B-cell lymphoma (HGBCL) or diffuse large B-cell lymphoma (DLBCL) than typical Burkitt lymphoma (BL).
The researchers also found that BLL-11q has clinical, morphologic, and phenotypic features that are “more consistent” with HGBCL or DLBCL than with typical BL.
“These observations support a reconsideration of the ‘Burkitt-like’ term for these tumors,” Blanca Gonzalez-Farre, MD, of Hospital Clínic de Barcelona, and her colleagues wrote in Haematologica.
To reach this conclusion, the researchers performed copy number analysis and sequencing of B-cell lymphoma-related genes in 11 cases of BLL-11q.
The copy number analysis revealed that seven BLL-11q cases had the typical 11q gain/loss pattern, two had an 11q terminal deletion, one had two gains and two losses, and one had an 11q23.3-q25 copy number neutral loss of heterozygosity in addition to gain.
The BLL-11q cases also had frequent gains of 5q21.3-q32 and losses of 6q12.1-q21. However, they lacked the 1q gains observed in MYC-positive BL and alterations typically observed in germinal center B-cell like (GCB) DLBCL, such as gains in 2p16.1 and 7p.
Targeted sequencing of the BLL-11q cases revealed mutations typically observed in germinal center-derived lymphomas, including mutations in BTG2, DDX3X, ETS1, EP300, GNA13, CREBBP, KMT2C, EZH2, ARID1A, KMT2D, HIST1H1D, HIST1H2BC, and TMEM30A.
However, the BLL-11q cases lacked mutations in ID3, TCF3, and CCND3, which are typically observed in BL.
“In addition to the genetic differences, our BLL-11q differed clinically, morphologically, and phenotypically from conventional BL and instead showed features more consistent with HGBCL or DLBCL,” the researchers wrote.
Specifically, the BLL-11q patients were all younger than 40 years, with a median age of 15. Most presented with localized lymphadenopathy. And all had favorable treatment outcomes, remaining alive and free of disease at a median follow-up of 30 months.
All cases had a germinal center phenotype. They did not have the typical cytological features of BL, but they did have a high proliferative index, and some cases had a starry sky pattern.
The researchers said the BLL-11q cases were better classified as HGBCL not otherwise specified (n = 8), DLBCL (n = 2), and atypical BL (n = 1).
Considering these findings together, the team concluded that a more appropriate name for BLL-11q might be “aggressive B-cell lymphoma with 11q aberration.”
This research was supported by Asociación Española Contra el Cáncer and other organizations, as well as the government of Catalonia.
SOURCE: Gonzalez-Farre B et al. Haematologica. 2019 Feb 7. doi: 10.3324/haematol.2018.207928.
REPORTING FROM HAEMATOLOGICA
KD025 produces durable responses in patients with cGVHD
HOUSTON – The according to a speaker at the Transplantation & Cellular Therapy Meetings.
In an ongoing phase 2 trial (NCT02841995), KD025 produced an overall response rate of 59%. Responses occurred in all affected organ systems, and 72% of responders experienced an improvement in Lee Symptom Scale (LSS) score.
The median duration of response was 28 weeks, but durability data are still maturing, according to Madan Jagasia, MBBS, of Vanderbilt University in Nashville, Tenn.
Dr. Jagasia and his colleagues evaluated KD025 in 54 adults who had persistent, active cGVHD after at least 2 months of steroid therapy. Sixty-seven percent of patients had received at least two prior lines of therapy, and 48% had involvement in four or more organs.
KD025 was given at three doses: 200 mg once daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg once daily (cohort 3). Patients also received glucocorticoid therapy, with or without calcineurin inhibitor therapy.
Cohort 1 included 17 patients who had a median age of 50 years (range, 20-63). They received KD025 for a median of 37 weeks, and six patients were still receiving KD025 at last follow-up.
Cohort 2 included 16 patients who had a median age of 55 years (range, 30-75). They received KD025 for a median of 33 weeks, and three patients were still receiving KD025 at last follow-up.
Cohort 3 included 21 patients who had a median age of 46 years (range, 25-75). They received KD025 for a median of 27 weeks, and 11 patients were still receiving KD025 at last follow-up.
The ORR was 59% (32/54) across the study, 65% (11/17) in cohort 1, 63% (10/16) in cohort 2, and 52% (11/21) in cohort 3. Three patients in cohort 3 didn’t reach the first response assessment, so the ORR in response-evaluable patients was 61% (11/18).
The ORR was 58% in patients who had received two or more prior lines of therapy, 55% in patients with severe cGVHD, and 62% in patients who had four or more organs involved.
“Responses were observed across all affected organ systems,” Dr. Jagasia said. “CRs [complete responses] were seen in all organs except the lung, and there were two partial responses observed in the lung.”
The median duration of response was 28 weeks. Eighty-two percent of responders in cohort 1, 50% of responders in cohort 2, and 36% of responders in cohort 3 had responses lasting 20 weeks or more.
“Keep in mind, the median duration of follow-up in cohort 3 is still short, and the durability data will continue to mature,” Dr. Jagasia said.
Most responders (72%) had at least a 7-point reduction in LSS score. Considering responders and nonresponders together, 65% of patients in cohort 1, 56% in cohort 2, and 52% in cohort 3 had an improvement in LSS score.
In all, 69% of patients stopped or reduced their use of steroids or other immunosuppressants. Seven patients completely discontinued steroids.
Forty-four percent of patients (n = 24) had a treatment-related adverse event (AE), but none of these AEs were considered serious. Four percent of patients (n = 2) had a related AE that led to treatment discontinuation, and 15% (n = 8) had grade 3/4 related AEs.
“The AEs were, overall, consistent with those expected in chronic graft-versus-host disease patients receiving corticosteroids,” Dr. Jagasia said. “Most important to note, there was no apparent increased risk of infection. Specifically, there was no CMV [cytomegalovirus] infection.”
The most common AEs were upper respiratory tract infection, fatigue, nausea, AST/ALT increase, and diarrhea. The most common grade 3/4 AEs were gamma-glutamyltransferase increase, hyperglycemia, anemia, and dyspnea.
There were three on-study deaths, all considered unrelated to KD025. One patient died of leukemia relapse, one died of lung infection, and one died of cardiac arrest.
Dr. Jagasia presented these results at the Transplantation & Cellular Therapy Meetings, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Jagasia reported relationships with Kadmon Holdings, Mallinckrodt, and Janssen. The trial was sponsored by Kadmon Holdings.
SOURCE: Jagasia M et al. TCT 2019, Abstract 36.
HOUSTON – The according to a speaker at the Transplantation & Cellular Therapy Meetings.
In an ongoing phase 2 trial (NCT02841995), KD025 produced an overall response rate of 59%. Responses occurred in all affected organ systems, and 72% of responders experienced an improvement in Lee Symptom Scale (LSS) score.
The median duration of response was 28 weeks, but durability data are still maturing, according to Madan Jagasia, MBBS, of Vanderbilt University in Nashville, Tenn.
Dr. Jagasia and his colleagues evaluated KD025 in 54 adults who had persistent, active cGVHD after at least 2 months of steroid therapy. Sixty-seven percent of patients had received at least two prior lines of therapy, and 48% had involvement in four or more organs.
KD025 was given at three doses: 200 mg once daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg once daily (cohort 3). Patients also received glucocorticoid therapy, with or without calcineurin inhibitor therapy.
Cohort 1 included 17 patients who had a median age of 50 years (range, 20-63). They received KD025 for a median of 37 weeks, and six patients were still receiving KD025 at last follow-up.
Cohort 2 included 16 patients who had a median age of 55 years (range, 30-75). They received KD025 for a median of 33 weeks, and three patients were still receiving KD025 at last follow-up.
Cohort 3 included 21 patients who had a median age of 46 years (range, 25-75). They received KD025 for a median of 27 weeks, and 11 patients were still receiving KD025 at last follow-up.
The ORR was 59% (32/54) across the study, 65% (11/17) in cohort 1, 63% (10/16) in cohort 2, and 52% (11/21) in cohort 3. Three patients in cohort 3 didn’t reach the first response assessment, so the ORR in response-evaluable patients was 61% (11/18).
The ORR was 58% in patients who had received two or more prior lines of therapy, 55% in patients with severe cGVHD, and 62% in patients who had four or more organs involved.
“Responses were observed across all affected organ systems,” Dr. Jagasia said. “CRs [complete responses] were seen in all organs except the lung, and there were two partial responses observed in the lung.”
The median duration of response was 28 weeks. Eighty-two percent of responders in cohort 1, 50% of responders in cohort 2, and 36% of responders in cohort 3 had responses lasting 20 weeks or more.
“Keep in mind, the median duration of follow-up in cohort 3 is still short, and the durability data will continue to mature,” Dr. Jagasia said.
Most responders (72%) had at least a 7-point reduction in LSS score. Considering responders and nonresponders together, 65% of patients in cohort 1, 56% in cohort 2, and 52% in cohort 3 had an improvement in LSS score.
In all, 69% of patients stopped or reduced their use of steroids or other immunosuppressants. Seven patients completely discontinued steroids.
Forty-four percent of patients (n = 24) had a treatment-related adverse event (AE), but none of these AEs were considered serious. Four percent of patients (n = 2) had a related AE that led to treatment discontinuation, and 15% (n = 8) had grade 3/4 related AEs.
“The AEs were, overall, consistent with those expected in chronic graft-versus-host disease patients receiving corticosteroids,” Dr. Jagasia said. “Most important to note, there was no apparent increased risk of infection. Specifically, there was no CMV [cytomegalovirus] infection.”
The most common AEs were upper respiratory tract infection, fatigue, nausea, AST/ALT increase, and diarrhea. The most common grade 3/4 AEs were gamma-glutamyltransferase increase, hyperglycemia, anemia, and dyspnea.
There were three on-study deaths, all considered unrelated to KD025. One patient died of leukemia relapse, one died of lung infection, and one died of cardiac arrest.
Dr. Jagasia presented these results at the Transplantation & Cellular Therapy Meetings, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Jagasia reported relationships with Kadmon Holdings, Mallinckrodt, and Janssen. The trial was sponsored by Kadmon Holdings.
SOURCE: Jagasia M et al. TCT 2019, Abstract 36.
HOUSTON – The according to a speaker at the Transplantation & Cellular Therapy Meetings.
In an ongoing phase 2 trial (NCT02841995), KD025 produced an overall response rate of 59%. Responses occurred in all affected organ systems, and 72% of responders experienced an improvement in Lee Symptom Scale (LSS) score.
The median duration of response was 28 weeks, but durability data are still maturing, according to Madan Jagasia, MBBS, of Vanderbilt University in Nashville, Tenn.
Dr. Jagasia and his colleagues evaluated KD025 in 54 adults who had persistent, active cGVHD after at least 2 months of steroid therapy. Sixty-seven percent of patients had received at least two prior lines of therapy, and 48% had involvement in four or more organs.
KD025 was given at three doses: 200 mg once daily (cohort 1), 200 mg twice daily (cohort 2), and 400 mg once daily (cohort 3). Patients also received glucocorticoid therapy, with or without calcineurin inhibitor therapy.
Cohort 1 included 17 patients who had a median age of 50 years (range, 20-63). They received KD025 for a median of 37 weeks, and six patients were still receiving KD025 at last follow-up.
Cohort 2 included 16 patients who had a median age of 55 years (range, 30-75). They received KD025 for a median of 33 weeks, and three patients were still receiving KD025 at last follow-up.
Cohort 3 included 21 patients who had a median age of 46 years (range, 25-75). They received KD025 for a median of 27 weeks, and 11 patients were still receiving KD025 at last follow-up.
The ORR was 59% (32/54) across the study, 65% (11/17) in cohort 1, 63% (10/16) in cohort 2, and 52% (11/21) in cohort 3. Three patients in cohort 3 didn’t reach the first response assessment, so the ORR in response-evaluable patients was 61% (11/18).
The ORR was 58% in patients who had received two or more prior lines of therapy, 55% in patients with severe cGVHD, and 62% in patients who had four or more organs involved.
“Responses were observed across all affected organ systems,” Dr. Jagasia said. “CRs [complete responses] were seen in all organs except the lung, and there were two partial responses observed in the lung.”
The median duration of response was 28 weeks. Eighty-two percent of responders in cohort 1, 50% of responders in cohort 2, and 36% of responders in cohort 3 had responses lasting 20 weeks or more.
“Keep in mind, the median duration of follow-up in cohort 3 is still short, and the durability data will continue to mature,” Dr. Jagasia said.
Most responders (72%) had at least a 7-point reduction in LSS score. Considering responders and nonresponders together, 65% of patients in cohort 1, 56% in cohort 2, and 52% in cohort 3 had an improvement in LSS score.
In all, 69% of patients stopped or reduced their use of steroids or other immunosuppressants. Seven patients completely discontinued steroids.
Forty-four percent of patients (n = 24) had a treatment-related adverse event (AE), but none of these AEs were considered serious. Four percent of patients (n = 2) had a related AE that led to treatment discontinuation, and 15% (n = 8) had grade 3/4 related AEs.
“The AEs were, overall, consistent with those expected in chronic graft-versus-host disease patients receiving corticosteroids,” Dr. Jagasia said. “Most important to note, there was no apparent increased risk of infection. Specifically, there was no CMV [cytomegalovirus] infection.”
The most common AEs were upper respiratory tract infection, fatigue, nausea, AST/ALT increase, and diarrhea. The most common grade 3/4 AEs were gamma-glutamyltransferase increase, hyperglycemia, anemia, and dyspnea.
There were three on-study deaths, all considered unrelated to KD025. One patient died of leukemia relapse, one died of lung infection, and one died of cardiac arrest.
Dr. Jagasia presented these results at the Transplantation & Cellular Therapy Meetings, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Jagasia reported relationships with Kadmon Holdings, Mallinckrodt, and Janssen. The trial was sponsored by Kadmon Holdings.
SOURCE: Jagasia M et al. TCT 2019, Abstract 36.
REPORTING FROM TCT 2019
Ixazomib targets treatment failure in chronic GVHD
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
HOUSTON –
Patients who received ixazomib in this trial had a lower rate of treatment failure – a composite endpoint of death, relapse, and need for additional systemic immunosuppressive therapy – than that of historical controls.
Joseph Pidala, MD, PhD, of Moffitt Cancer Center in Tampa, Fla., presented this finding at the Transplantation & Cellular Therapy Meetings.
The trial (NCT02513498) included 50 patients with a median age of 58 years (range, 44-65). Patients had acute leukemia (52%), lymphoma (18%), chronic leukemia (12%), myelodysplastic syndromes/myeloproliferative neoplasms (8%), and myeloma (4%).
Most patients (90%) received peripheral blood transplants, but 10% received bone marrow. Patients had matched unrelated donors (48%), matched related donors (44%), mismatched unrelated donors (6%), and mismatched related donors (2%).
Most patients (84%) had severe cGVHD, but 16% had moderate cGVHD. About half of patients (52%) had four or more organs involved, and 78% received three or more prior lines of systemic therapy for cGVHD. The median time from cGVHD onset to trial enrollment was 33.5 months.
“[I]t was an advanced population that was highly treatment experienced,” Dr. Pidala said.
Initially, patients received ixazomib at 4 mg on days 1, 8, and 15 of a 28-day cycle for up to six cycles. However, the protocol was amended to allow additional cycles for responders.
Fifty-two percent of patients (n = 26) completed at least six cycles of therapy. The remaining patients stopped treatment because of unresolved toxicity, treatment failure, withdrawal, noncompliance, and death.
“Seven patients, in total, did continue therapy beyond six cycles,” Dr. Pidala said. “Six of these had partial response at 6 months, and one had stable disease.”
The overall response rate at 6 months was 40%. All 20 responders had partial responses.
The 6-month treatment failure rate was significantly lower in this trial than in historical controls (Blood 2013 121:2340-6). The rates of treatment failure were 28% and 44%, respectively (P = .01).
Treatment failure was largely due to the need for additional treatment, Dr. Pidala noted. Relapse and nonrelapse mortality were “uncommon” in this trial.
The investigators did not find any patient, transplant, or cGVHD-related factors significantly associated with 6-month treatment failure.
The failure-free survival rate at 6 months was 72% in this trial and 56% in historical controls. The failure-free survival rate at 12 months was 57% and 45%, respectively.
Serious adverse events occurred in 38% of patients on this trial. Patients required ixazomib dose reductions due to thrombocytopenia, fatigue, diarrhea, and infection.
There were five deaths, and two of them were considered possibly related to ixazomib.
“This was driven by the proximity of the death events to the last dose of ixazomib, specifically, within 1 month,” Dr. Pidala said. “One of these death events was a case of respiratory failure. The other was a case of sudden, unexplained death.”
The meeting was held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Pidala reported having nothing to disclose. Other investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda. The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute.
SOURCE: Pidala J et al. TCT 2019, Abstract 35.
REPORTING FROM TCT 2019
Key clinical point: Ixazomib may reduce treatment failure in patients with advanced chronic graft-versus-host disease.
Major finding: The 6-month treatment failure rate was significantly lower in this trial than in historical controls – 28% and 44%, respectively (P = .01).
Study details: A phase 2 trial of 50 patients with hematologic malignancies.
Disclosures: The trial was sponsored by the Fred Hutchinson Cancer Research Center in collaboration with the National Cancer Institute. The investigators reported relationships with Pfizer, CSL Behring, Agios, Incyte, Genentech, and Takeda.
Source: Pidala J et al. TCT 2019, Abstract 35.
Post-HCT azithromycin doesn’t increase relapse risk, study suggests
HOUSTON — When given after transplant, azithromycin does not increase the risk of relapse in patients with moderate to severe chronic graft-versus-host disease (cGVHD) and bronchiolitis obliterans syndrome (BOS), according to a retrospective study.
A prior study, ALLOZITHRO (JAMA. 2017 Aug 8;318[6]:557-66), showed an increased risk of relapse and death in patients who received azithromycin as BOS prophylaxis prior to hematopoietic cell transplant (HCT).
That discovery prompted the Food and Drug Administration to release a safety communication warning prescribers about the risks associated with azithromycin as BOS prophylaxis. However, it wasn’t clear if the same risks exist when azithromycin is given for cGVHD management after HCT.
To gain some insight, Mark Shamoun, MD, of the University of Michigan, Ann Arbor, and his colleagues examined data on patients with moderate to severe cGVHD and BOS who received azithromycin after undergoing HCT to treat a hematologic malignancy.
Dr. Shamoun presented the group’s findings at the Transplantation & Cellular Therapy Meetings.
The researchers reviewed data on 239 patients enrolled in the University of Michigan’s HCT database from 2010 to 2017. The median age at baseline was 55 years (range, 4-72 years).
The patients received transplants to treat acute myeloid leukemia or myelodysplastic syndromes (n = 141), acute lymphoblastic leukemia (n = 40), lymphoma (n = 26), chronic leukemia (n = 24), multiple myeloma (n = 6), and myeloproliferative neoplasms (n = 2).
The patients had matched related donors (43%) or matched unrelated donors (57%). Most patients received peripheral blood transplants (84%), though some received bone marrow (14%) or cord blood (2%). All patients had moderate (38%) or severe (62%) cGVHD.
Patients were split into two cohorts. Patients in cohort A (n = 86) had BOS and received azithromycin for more than 14 days.
Patients in cohort B (n = 153) either did not receive azithromycin or received it for 14 days or less. Fewer than 5% of patients in cohort B had BOS.
Most other baseline characteristics were similar between the cohorts. However, severe cGVHD was more prevalent in cohort A than B — 78% and 51%, respectively.
In cohort A, the median time to the start of azithromycin was 15 months after HCT (range, 3-68 months). The median duration of azithromycin treatment was 26 months (range, 1-77 months).
Results
The 2-year relapse rate was significantly lower in patients who received azithromycin than in those who did not — 4% and 17%, respectively (P = .001).
There was a significant difference in relapse rate both from the time of HCT (P = .001) and from the start of azithromycin or cGVHD (P = .011).
There was no significant difference in overall survival between the cohorts, either from the time of HCT (P = .294) or from the start of azithromycin or cGVHD (P = .428).
Dr. Shamoun said these results suggest azithromycin does not increase the risk of relapse when it is used to manage cGVHD. However, this study is limited by its retrospective nature. In addition, most patients in cohort B did not have BOS, severe cGVHD was more common in cohort A, and the incidence of relapse was not calculated from the time of azithromycin initiation in both cohorts. Therefore, additional investigation is needed.
Dr. Shamoun presented these results at Transplantation & Cellular Therapy Meetings, which is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society, the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Shamoun reported no conflicts of interest.
SOURCE: Shamoun M et al. TCT 2019, Abstract 33.
HOUSTON — When given after transplant, azithromycin does not increase the risk of relapse in patients with moderate to severe chronic graft-versus-host disease (cGVHD) and bronchiolitis obliterans syndrome (BOS), according to a retrospective study.
A prior study, ALLOZITHRO (JAMA. 2017 Aug 8;318[6]:557-66), showed an increased risk of relapse and death in patients who received azithromycin as BOS prophylaxis prior to hematopoietic cell transplant (HCT).
That discovery prompted the Food and Drug Administration to release a safety communication warning prescribers about the risks associated with azithromycin as BOS prophylaxis. However, it wasn’t clear if the same risks exist when azithromycin is given for cGVHD management after HCT.
To gain some insight, Mark Shamoun, MD, of the University of Michigan, Ann Arbor, and his colleagues examined data on patients with moderate to severe cGVHD and BOS who received azithromycin after undergoing HCT to treat a hematologic malignancy.
Dr. Shamoun presented the group’s findings at the Transplantation & Cellular Therapy Meetings.
The researchers reviewed data on 239 patients enrolled in the University of Michigan’s HCT database from 2010 to 2017. The median age at baseline was 55 years (range, 4-72 years).
The patients received transplants to treat acute myeloid leukemia or myelodysplastic syndromes (n = 141), acute lymphoblastic leukemia (n = 40), lymphoma (n = 26), chronic leukemia (n = 24), multiple myeloma (n = 6), and myeloproliferative neoplasms (n = 2).
The patients had matched related donors (43%) or matched unrelated donors (57%). Most patients received peripheral blood transplants (84%), though some received bone marrow (14%) or cord blood (2%). All patients had moderate (38%) or severe (62%) cGVHD.
Patients were split into two cohorts. Patients in cohort A (n = 86) had BOS and received azithromycin for more than 14 days.
Patients in cohort B (n = 153) either did not receive azithromycin or received it for 14 days or less. Fewer than 5% of patients in cohort B had BOS.
Most other baseline characteristics were similar between the cohorts. However, severe cGVHD was more prevalent in cohort A than B — 78% and 51%, respectively.
In cohort A, the median time to the start of azithromycin was 15 months after HCT (range, 3-68 months). The median duration of azithromycin treatment was 26 months (range, 1-77 months).
Results
The 2-year relapse rate was significantly lower in patients who received azithromycin than in those who did not — 4% and 17%, respectively (P = .001).
There was a significant difference in relapse rate both from the time of HCT (P = .001) and from the start of azithromycin or cGVHD (P = .011).
There was no significant difference in overall survival between the cohorts, either from the time of HCT (P = .294) or from the start of azithromycin or cGVHD (P = .428).
Dr. Shamoun said these results suggest azithromycin does not increase the risk of relapse when it is used to manage cGVHD. However, this study is limited by its retrospective nature. In addition, most patients in cohort B did not have BOS, severe cGVHD was more common in cohort A, and the incidence of relapse was not calculated from the time of azithromycin initiation in both cohorts. Therefore, additional investigation is needed.
Dr. Shamoun presented these results at Transplantation & Cellular Therapy Meetings, which is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society, the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Shamoun reported no conflicts of interest.
SOURCE: Shamoun M et al. TCT 2019, Abstract 33.
HOUSTON — When given after transplant, azithromycin does not increase the risk of relapse in patients with moderate to severe chronic graft-versus-host disease (cGVHD) and bronchiolitis obliterans syndrome (BOS), according to a retrospective study.
A prior study, ALLOZITHRO (JAMA. 2017 Aug 8;318[6]:557-66), showed an increased risk of relapse and death in patients who received azithromycin as BOS prophylaxis prior to hematopoietic cell transplant (HCT).
That discovery prompted the Food and Drug Administration to release a safety communication warning prescribers about the risks associated with azithromycin as BOS prophylaxis. However, it wasn’t clear if the same risks exist when azithromycin is given for cGVHD management after HCT.
To gain some insight, Mark Shamoun, MD, of the University of Michigan, Ann Arbor, and his colleagues examined data on patients with moderate to severe cGVHD and BOS who received azithromycin after undergoing HCT to treat a hematologic malignancy.
Dr. Shamoun presented the group’s findings at the Transplantation & Cellular Therapy Meetings.
The researchers reviewed data on 239 patients enrolled in the University of Michigan’s HCT database from 2010 to 2017. The median age at baseline was 55 years (range, 4-72 years).
The patients received transplants to treat acute myeloid leukemia or myelodysplastic syndromes (n = 141), acute lymphoblastic leukemia (n = 40), lymphoma (n = 26), chronic leukemia (n = 24), multiple myeloma (n = 6), and myeloproliferative neoplasms (n = 2).
The patients had matched related donors (43%) or matched unrelated donors (57%). Most patients received peripheral blood transplants (84%), though some received bone marrow (14%) or cord blood (2%). All patients had moderate (38%) or severe (62%) cGVHD.
Patients were split into two cohorts. Patients in cohort A (n = 86) had BOS and received azithromycin for more than 14 days.
Patients in cohort B (n = 153) either did not receive azithromycin or received it for 14 days or less. Fewer than 5% of patients in cohort B had BOS.
Most other baseline characteristics were similar between the cohorts. However, severe cGVHD was more prevalent in cohort A than B — 78% and 51%, respectively.
In cohort A, the median time to the start of azithromycin was 15 months after HCT (range, 3-68 months). The median duration of azithromycin treatment was 26 months (range, 1-77 months).
Results
The 2-year relapse rate was significantly lower in patients who received azithromycin than in those who did not — 4% and 17%, respectively (P = .001).
There was a significant difference in relapse rate both from the time of HCT (P = .001) and from the start of azithromycin or cGVHD (P = .011).
There was no significant difference in overall survival between the cohorts, either from the time of HCT (P = .294) or from the start of azithromycin or cGVHD (P = .428).
Dr. Shamoun said these results suggest azithromycin does not increase the risk of relapse when it is used to manage cGVHD. However, this study is limited by its retrospective nature. In addition, most patients in cohort B did not have BOS, severe cGVHD was more common in cohort A, and the incidence of relapse was not calculated from the time of azithromycin initiation in both cohorts. Therefore, additional investigation is needed.
Dr. Shamoun presented these results at Transplantation & Cellular Therapy Meetings, which is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At the meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society, the American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Shamoun reported no conflicts of interest.
SOURCE: Shamoun M et al. TCT 2019, Abstract 33.
REPORTING FROM TCT 2019
Gene expression signature reveals high-grade GCB DLBCL
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
New research suggests a gene expression signature can distinguish high-grade diffuse large B-cell lymphomas (DLBCLs) from other germinal center B-cell–like (GCB) DLBCLs.
Researchers identified GCB DLBCL patients with this 104-gene signature who had a “distinct mutational landscape” and inferior treatment outcomes. David W. Scott, MBChB, PhD, of the British Columbia Cancer Research Centre in Vancouver, and his colleagues described these patients in the Journal of Clinical Oncology.
The findings were published alongside a related editorial and a similar study from another group.
Dr. Scott and his colleagues began their study by analyzing data from 157 patients with de novo GCB DLBCL. Twenty-five of these patients had double- or triple-hit high-grade B-cell lymphoma with BCL2 translocations (HGBL-DH/TH-BCL2).
The researchers identified 104 genes that were the “most significantly differentially expressed between HGBL-DH/TH-BCL2 and other GCB DLBCLs” to create their double-hit gene signature (DHITsig).
The signature divided the patients into two groups — 42 patients (27%) whose tumors were positive for the DHITsig and 115 (73%) whose tumors were negative. Notably, 22 of the 25 HGBL-DH/TH-BCL2 tumors were DHITsig-positive and 3 were negative.
The DHITsig was not associated with clinical variables such as tumor volume, but it was associated with prognosis. Treatment outcomes were inferior in patients who were DHITsig-positive.
The 5-year time to progression rate was 81% in patients who were DHITsig-negative and 57% in those who were positive (P less than .001). The 5-year overall survival rate was 81% and 60%, respectively (P = .001).
The researchers observed similar results in a validation cohort of 262 patients with GCB-DLBCL who received rituximab-based therapy. The 5-year overall survival rate was 76% in patients who were DHITsig-negative and 49% in those who were positive (P less than .001).
Dr. Scott and his colleagues also evaluated the DHITsig in a second validation cohort of 162 patients with GCB DLBCL.
In analyzing data from all three cohorts, the researchers found that mutations in MYC, BCL2, CREBBP, EZH2Y646, DDX3X, TP53, and KMT2D were more frequent in DHITsig-positive patients and mutations in TNFAIP3, KLHL6, NFKBIE, TET2, CD58, and STAT3 were more common in DHITsig-negative patients.
Additional analyses suggested the cell of origin for DHITsig-positive tumors comes from the intermediate zone or dark zone of the germinal center.
Finally, the researchers found they could use a “clinically relevant assay” to detect the DHITsig. They added a 30-gene module to the Lymph3Cx assay to create a NanoString-based assay called DLBCL90.
The team tested DLBCL90 in 171 GCB DLBCL patients. In this group, 26% of patients were DHITsig-positive, 64% were negative, and 10% were indeterminate. The prognostic significance of the signature was maintained with the assay results, according to the researchers.
Dr. Scott and his colleagues also wanted to validate the association between the DHITsig and HGBL-DH/TH-BCL2, so they tested the DLBCL90 assay in two additional groups of patients.
First, the assay was used in 88 patients who had transformed follicular lymphoma with DLBCL morphology. Eleven of the 25 DHITsig-positive tumors and 4 of the 13 DHITsig-indeterminate tumors were HGBL-DH/TH-BCL2. However, none of the 50 DHITsig-negative tumors were HGBL-DH/TH-BCL2.
The researchers then used the DLBCL90 assay on 26 HGBL tumors. Twenty-three of these were DHITsig-positive and 3 were indeterminate.
This research was supported by the Canadian Cancer Society Research Institute and other organizations. The researchers reported relationships with Seattle Genetics, Roche, Janssen, Celgene, and various other companies.
SOURCE: Scott DW et al. J Clin Oncol. 2019 Jan 20;37(3):190-201.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Priority review granted to lenalidomide for FL, MZL
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.
The Food and Drug Administration has granted priority review to a supplemental new drug application (sNDA) for lenalidomide (Revlimid).
Celgene is seeking approval for lenalidomide in combination with rituximab to treat patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL).
The FDA plans to make a decision on the sNDA by June 27, 2019.
The FDA aims to take action on a priority review application within 6 months of receiving it rather than the standard 10 months. The FDA grants priority review to applications for products that are expected to provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The sNDA for lenalidomide is supported by the phase 3 AUGMENT study (NCT01938001) in which researchers compared rituximab plus lenalidomide to rituximab plus placebo in patients with relapsed/refractory FL or MZL.
Results from AUGMENT were presented at the 2018 annual meeting of the American Society of Hematology (Blood 2018 Nov 29;132:445).
According to the ASH abstract, the trial included 358 patients who were randomized to receive rituximab plus lenalidomide (n = 178) or rituximab plus placebo (n = 180).
At a median follow-up of 28.3 months, the overall response rate was 78% in the lenalidomide arm and 53% in the placebo arm (P less than .0001). The complete response rate was 34% and 18%, respectively (P = .001).
The median progression-free survival was 39.4 months in the lenalidomide arm and 14.1 months in the placebo arm. Overall survival data were not mature, but there were 16 deaths reported in the lenalidomide arm and 26 deaths in the placebo arm.
Treatment-emergent adverse events that were more common in the lenalidomide arm than the placebo arm included infections, cutaneous reactions, constipation, thrombocytopenia, and tumor flare reaction.