User login
Colonoscopy Bowel Preparation Instructions
According to the CDC, colorectal cancer (CRC) is largely preventable but remains the second leading cancer killer for men and women in the U.S. Screening for polyps (detection of abnormal growths) and surveillance (based on prior bowel preparation quality, findings, and personal and family histories) are key elements for CRC prevention and survival.1 However, inadequate bowel preparation greatly reduces accuracy of its intended purpose: finding and removing precancerous polyps or lesions before they develop into a cancer, typically within a 10-year window. If preparation quality is not satisfactory, the ability of the endoscopist to meet national polyp detection rates is limited. These rates are currently 25% for men and 15% for women.2 Compounding poor preparation, many veterans avoid CRC screening due to anxiety, shame, and fear of what could be found.
Related: Do I Need a Colonoscopy?
About 60% of veterans presenting for colonoscopy have inadequate bowel preparation.3 Colonoscopy remains the gold standard for detection of colorectal pathology and is available to veterans without insurance preauthorization, eliminating a significant barrier to screening.1 Inadequate bowel preparation can result in missed polyps, cancelled procedures, and increased procedure time. Nonadherence to the liquid diet and high-volume, bowel-cleansing solution can lead to a repeated colonoscopy.
Two nurse practitioners (NPs) at the Philadelphia VAMC (PVAMC) gastroenterology (GE) section recognized that many veterans had poor bowel preparation in spite of preprocedure visits, written instructions, and no financial limitations. Repeated colonoscopies were impacting patient satisfaction, facility costs, and endoscopy staff morale. The NPs developed a study to examine bowel preparation outcomes after a group preprocedure class that provided comprehensive and multimedia education in comparison to standard mailed instructions. The study was approved by the Institutional Review Board. The hypothesis was that group patient education would result in better adherence to bowel preparation instructions than did mailed instructions and that better adherence would result in significantly improved colonoscopy outcomes.
Methods
This was a descriptive pilot study with a convenience sample of 200 veterans randomly selected between 2009 and 2011. The study measured 2 groups. The control group received only the mailed standard bowel preparation instructions, whereas the intervention group received the standard bowel preparation instructions and participated in a group intervention class. Eligible participants were aged 45 to 79 years and were enrolled as patients in a single center (PVAMC GE clinic).
Related: E-Consults in Gastroenterology: A Quality Improvement Project
After referral consults were initially selected for appropriate colonoscopy screening or surveillance, potential patient subjects were randomized into either the control or intervention groups by the coin toss method, followed by mailed letters inviting them to participate in the study. If subjects expressed interest, then consent was obtained. The colonoscopy procedure note was updated to reflect bowel preparation quality. All subjects were de-identified. There were about 8 endoscopists; all were board-certified gastroenterologists plus GE fellows who performed procedures at the time of the study. (Fellows rotated every 2 to 4 weeks in the GE clinic and were always accompanied by an attending gastroenterologist.)
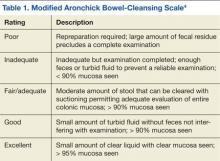
All the endoscopists were instructed in the grading system adapted from the modified Aronchick scale (Table 1).4 This scale measures the quality of bowel preparation for the entire colon: excellent (> 95% visualization of bowel mucosa); good (> 90% of mucosa was visible); fair (some semisolid stool could be suctioned out, but > 90% of mucosa was visible), and poor (semisolid stool cannot be suctioned out and < 90% of mucosa was seen). The modified Aronchick scale also has an inadequate rating, but this was not used in the study. For this study, bowel preparation that was excellent or good received a 1, a fair preparation received a 2, and poor preparation received a 3. The Pearson correlation for the modified Aronchick scale coefficients was 0.62 (P < .001). The value for the kappa statistic was 0.77 (P < .001).5
Results
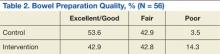
There were 77 men and 5 women enrolled in the study. The control group had 43 subjects, and the intervention group had 39 subjects. Only 28 subjects each from the control and intervention groups had the quality of bowel preparation rated by the endoscopists. In the control group, 53.6% were rated excellent or good, 42.9% were fair, and 3.5% were poor. In the intervention group, 42.9 % of preparations were excellent or good, 42.8% were fair, and 14.3% were poor (Table 2).
Preparation quality was not described in the procedure documentation for 34.9% and 28.2% of the subjects, respectively, for the control and intervention groups. There was no significant difference in no-show rates to procedures in either of the groups. Based on the data, a Fisher exact test for association was performed (P = .39), indicating there was no evidence of association between the intervention group and preparation quality.
The authors observed several recurrent themes during the group interventions. Fear of finding cancer and the perception of the procedure’s invasiveness were raised and addressed. Also misconceptions about CRC were debunked, such as the belief that a lack of bowel symptoms indicated no chance of having CRC or that only a family history indicated a risk factor. Patients discussed how much they learned about CRC, colon anatomy, and the importance of the bowel preparation. A multifaceted teaching approach was used to convey teaching points, such as flip charts, colonoscopy equipment, tours of procedure rooms, and visuals of various bowel preparation qualities. Throughout the educational intervention, humor, active listening, and reflection were woven into discussions to create a comfortable and relaxed learning environment.
Discussion and Limitations
The study results were unexpected. The authors had hypothesized that the group preprocedure educational intervention would have made a statistically significant difference in preparation quality, but it did not. In addition, the authors’ observations during the intervention led them to believe that the subjects had gained knowledge about how to correctly administer the bowel preparation.
Related: Do Age and Gender Matter in Colorectal Cancer?
A significant limitation of this pilot study was the difficulty in extrapolating meaningful data within the intervention group and between the intervention and control groups. After closely examining the raw data, the authors identified some key issues: There were only 28 subjects in each group who had bowel preparation quality described. This small sample size makes it difficult to draw meaningful conclusions. However, the education session in and of itself was clearly a positive experience for subjects, and the authors would recommend a future study with a larger sample size.
A prior power analysis would have helped this study determine a sufficient number of subjects that would be needed to determine whether the intervention had an effect. Furthermore, instead of tossing a coin to randomize the study groups, other types of randomization could have been used.
Other study limitations that came to light were:
- Variable preparation quality documentation by endoscopists;
- Limited availability of days to schedule group intervention classes;
- Some subjects did not attend the group session but still had the procedure done;
- The study invitation letter was long, and there were no financial incentives to participate;
- If pre- and postintervention testing had been conducted, effective and ineffective teaching strategies could have been identified; and
- The principal investigator also performed some of the procedures during the study, introducing potential bias.
Since the study, the authors have learned more about changes in national standards for bowel preparation administration and polyp surveillance. Preparation instructions need to be updated to reflect current recommendations for split-dose preparation administration in which the bowel preparation is taken in spaced doses, leading to better compliance and outcomes.6 Informally, patients and family have told staff that preparation instructions are difficult to understand. Following a Plan-Do-Study-Act cycle, feedback from patients should be obtained before revising and printing preparation instructions.7 This feedback could ensure that preparation instructions are written in patient-friendly, easily understood language.
Conclusion
Nursing professionals are likely to be effective in helping veterans achieve improved bowel preparation quality, because nurses have an established record as patient educators and advocates. Good bowel preparation quality is an important, achievable objective for veterans. As Mangnall reported, bowel preparation quality data are a strong nurse-sensitive quality measure that can be used to devise more effective interventions to obtain better bowel preparation results.8 As clinicians working on the frontline, nurses are well positioned to assess, intervene, and evaluate whether or not the modifications they have made to bowel preparation instructions are effective as they measure bowel preparation quality status post colonoscopy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. American Society of Gastrointestinal Endoscopy. Media backgrounder: Colorectal cancer screening. American Society of Gastrointestinal Endoscopy Website. http://www.asge.org/PressroomIndex .aspx?id=552. Updated August 2014. Accessed January 29, 2015.
2. Lee RH. Quality colonoscopy: A matter of time, technique or technology? World J Gastroenterol. 2013;19(10):1517-1522.
3. Health Services Research & Development. 1004—Impact of a novel patient educational booklet on colonoscopy preparation in veterans. US Department of Veterans Affairs Website. http://www.hsrd .research.va.gov/meetings/2009/print_abstract .cfm?recordid=541. Accessed January 29, 2015.
4. Gurudu SR, Ratuapli S, Heigh R, DiBaise J, Leighton J, Crowell M. Quality of bowel cleansing for afternoon colonoscopy is influenced by time of administration. Am J Gastroenterol. 2010;105(11):2318-2322.
5. Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59(4):482-486.
6. Cohen, LB. Split dosing of bowel preparation for colonoscopy: An analysis of its efficacy, safety and tolerability. Gastrointest Endosc. 2010;72(2):406-412.
7. Institute for Healthcare Improvement. How to improve: Model for improvement. Institute for Healthcare improvement; 2015. Institute for Healthcare Improvement Website. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed February 5, 2015.
8. Mangnall R. Good bowel cleaning vital for effective colonoscopy. Nurse N Z. 2012;18(16):17-19.
According to the CDC, colorectal cancer (CRC) is largely preventable but remains the second leading cancer killer for men and women in the U.S. Screening for polyps (detection of abnormal growths) and surveillance (based on prior bowel preparation quality, findings, and personal and family histories) are key elements for CRC prevention and survival.1 However, inadequate bowel preparation greatly reduces accuracy of its intended purpose: finding and removing precancerous polyps or lesions before they develop into a cancer, typically within a 10-year window. If preparation quality is not satisfactory, the ability of the endoscopist to meet national polyp detection rates is limited. These rates are currently 25% for men and 15% for women.2 Compounding poor preparation, many veterans avoid CRC screening due to anxiety, shame, and fear of what could be found.
Related: Do I Need a Colonoscopy?
About 60% of veterans presenting for colonoscopy have inadequate bowel preparation.3 Colonoscopy remains the gold standard for detection of colorectal pathology and is available to veterans without insurance preauthorization, eliminating a significant barrier to screening.1 Inadequate bowel preparation can result in missed polyps, cancelled procedures, and increased procedure time. Nonadherence to the liquid diet and high-volume, bowel-cleansing solution can lead to a repeated colonoscopy.
Two nurse practitioners (NPs) at the Philadelphia VAMC (PVAMC) gastroenterology (GE) section recognized that many veterans had poor bowel preparation in spite of preprocedure visits, written instructions, and no financial limitations. Repeated colonoscopies were impacting patient satisfaction, facility costs, and endoscopy staff morale. The NPs developed a study to examine bowel preparation outcomes after a group preprocedure class that provided comprehensive and multimedia education in comparison to standard mailed instructions. The study was approved by the Institutional Review Board. The hypothesis was that group patient education would result in better adherence to bowel preparation instructions than did mailed instructions and that better adherence would result in significantly improved colonoscopy outcomes.
Methods
This was a descriptive pilot study with a convenience sample of 200 veterans randomly selected between 2009 and 2011. The study measured 2 groups. The control group received only the mailed standard bowel preparation instructions, whereas the intervention group received the standard bowel preparation instructions and participated in a group intervention class. Eligible participants were aged 45 to 79 years and were enrolled as patients in a single center (PVAMC GE clinic).
Related: E-Consults in Gastroenterology: A Quality Improvement Project
After referral consults were initially selected for appropriate colonoscopy screening or surveillance, potential patient subjects were randomized into either the control or intervention groups by the coin toss method, followed by mailed letters inviting them to participate in the study. If subjects expressed interest, then consent was obtained. The colonoscopy procedure note was updated to reflect bowel preparation quality. All subjects were de-identified. There were about 8 endoscopists; all were board-certified gastroenterologists plus GE fellows who performed procedures at the time of the study. (Fellows rotated every 2 to 4 weeks in the GE clinic and were always accompanied by an attending gastroenterologist.)
All the endoscopists were instructed in the grading system adapted from the modified Aronchick scale (Table 1).4 This scale measures the quality of bowel preparation for the entire colon: excellent (> 95% visualization of bowel mucosa); good (> 90% of mucosa was visible); fair (some semisolid stool could be suctioned out, but > 90% of mucosa was visible), and poor (semisolid stool cannot be suctioned out and < 90% of mucosa was seen). The modified Aronchick scale also has an inadequate rating, but this was not used in the study. For this study, bowel preparation that was excellent or good received a 1, a fair preparation received a 2, and poor preparation received a 3. The Pearson correlation for the modified Aronchick scale coefficients was 0.62 (P < .001). The value for the kappa statistic was 0.77 (P < .001).5
Results
There were 77 men and 5 women enrolled in the study. The control group had 43 subjects, and the intervention group had 39 subjects. Only 28 subjects each from the control and intervention groups had the quality of bowel preparation rated by the endoscopists. In the control group, 53.6% were rated excellent or good, 42.9% were fair, and 3.5% were poor. In the intervention group, 42.9 % of preparations were excellent or good, 42.8% were fair, and 14.3% were poor (Table 2).
Preparation quality was not described in the procedure documentation for 34.9% and 28.2% of the subjects, respectively, for the control and intervention groups. There was no significant difference in no-show rates to procedures in either of the groups. Based on the data, a Fisher exact test for association was performed (P = .39), indicating there was no evidence of association between the intervention group and preparation quality.
The authors observed several recurrent themes during the group interventions. Fear of finding cancer and the perception of the procedure’s invasiveness were raised and addressed. Also misconceptions about CRC were debunked, such as the belief that a lack of bowel symptoms indicated no chance of having CRC or that only a family history indicated a risk factor. Patients discussed how much they learned about CRC, colon anatomy, and the importance of the bowel preparation. A multifaceted teaching approach was used to convey teaching points, such as flip charts, colonoscopy equipment, tours of procedure rooms, and visuals of various bowel preparation qualities. Throughout the educational intervention, humor, active listening, and reflection were woven into discussions to create a comfortable and relaxed learning environment.
Discussion and Limitations
The study results were unexpected. The authors had hypothesized that the group preprocedure educational intervention would have made a statistically significant difference in preparation quality, but it did not. In addition, the authors’ observations during the intervention led them to believe that the subjects had gained knowledge about how to correctly administer the bowel preparation.
Related: Do Age and Gender Matter in Colorectal Cancer?
A significant limitation of this pilot study was the difficulty in extrapolating meaningful data within the intervention group and between the intervention and control groups. After closely examining the raw data, the authors identified some key issues: There were only 28 subjects in each group who had bowel preparation quality described. This small sample size makes it difficult to draw meaningful conclusions. However, the education session in and of itself was clearly a positive experience for subjects, and the authors would recommend a future study with a larger sample size.
A prior power analysis would have helped this study determine a sufficient number of subjects that would be needed to determine whether the intervention had an effect. Furthermore, instead of tossing a coin to randomize the study groups, other types of randomization could have been used.
Other study limitations that came to light were:
- Variable preparation quality documentation by endoscopists;
- Limited availability of days to schedule group intervention classes;
- Some subjects did not attend the group session but still had the procedure done;
- The study invitation letter was long, and there were no financial incentives to participate;
- If pre- and postintervention testing had been conducted, effective and ineffective teaching strategies could have been identified; and
- The principal investigator also performed some of the procedures during the study, introducing potential bias.
Since the study, the authors have learned more about changes in national standards for bowel preparation administration and polyp surveillance. Preparation instructions need to be updated to reflect current recommendations for split-dose preparation administration in which the bowel preparation is taken in spaced doses, leading to better compliance and outcomes.6 Informally, patients and family have told staff that preparation instructions are difficult to understand. Following a Plan-Do-Study-Act cycle, feedback from patients should be obtained before revising and printing preparation instructions.7 This feedback could ensure that preparation instructions are written in patient-friendly, easily understood language.
Conclusion
Nursing professionals are likely to be effective in helping veterans achieve improved bowel preparation quality, because nurses have an established record as patient educators and advocates. Good bowel preparation quality is an important, achievable objective for veterans. As Mangnall reported, bowel preparation quality data are a strong nurse-sensitive quality measure that can be used to devise more effective interventions to obtain better bowel preparation results.8 As clinicians working on the frontline, nurses are well positioned to assess, intervene, and evaluate whether or not the modifications they have made to bowel preparation instructions are effective as they measure bowel preparation quality status post colonoscopy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
According to the CDC, colorectal cancer (CRC) is largely preventable but remains the second leading cancer killer for men and women in the U.S. Screening for polyps (detection of abnormal growths) and surveillance (based on prior bowel preparation quality, findings, and personal and family histories) are key elements for CRC prevention and survival.1 However, inadequate bowel preparation greatly reduces accuracy of its intended purpose: finding and removing precancerous polyps or lesions before they develop into a cancer, typically within a 10-year window. If preparation quality is not satisfactory, the ability of the endoscopist to meet national polyp detection rates is limited. These rates are currently 25% for men and 15% for women.2 Compounding poor preparation, many veterans avoid CRC screening due to anxiety, shame, and fear of what could be found.
Related: Do I Need a Colonoscopy?
About 60% of veterans presenting for colonoscopy have inadequate bowel preparation.3 Colonoscopy remains the gold standard for detection of colorectal pathology and is available to veterans without insurance preauthorization, eliminating a significant barrier to screening.1 Inadequate bowel preparation can result in missed polyps, cancelled procedures, and increased procedure time. Nonadherence to the liquid diet and high-volume, bowel-cleansing solution can lead to a repeated colonoscopy.
Two nurse practitioners (NPs) at the Philadelphia VAMC (PVAMC) gastroenterology (GE) section recognized that many veterans had poor bowel preparation in spite of preprocedure visits, written instructions, and no financial limitations. Repeated colonoscopies were impacting patient satisfaction, facility costs, and endoscopy staff morale. The NPs developed a study to examine bowel preparation outcomes after a group preprocedure class that provided comprehensive and multimedia education in comparison to standard mailed instructions. The study was approved by the Institutional Review Board. The hypothesis was that group patient education would result in better adherence to bowel preparation instructions than did mailed instructions and that better adherence would result in significantly improved colonoscopy outcomes.
Methods
This was a descriptive pilot study with a convenience sample of 200 veterans randomly selected between 2009 and 2011. The study measured 2 groups. The control group received only the mailed standard bowel preparation instructions, whereas the intervention group received the standard bowel preparation instructions and participated in a group intervention class. Eligible participants were aged 45 to 79 years and were enrolled as patients in a single center (PVAMC GE clinic).
Related: E-Consults in Gastroenterology: A Quality Improvement Project
After referral consults were initially selected for appropriate colonoscopy screening or surveillance, potential patient subjects were randomized into either the control or intervention groups by the coin toss method, followed by mailed letters inviting them to participate in the study. If subjects expressed interest, then consent was obtained. The colonoscopy procedure note was updated to reflect bowel preparation quality. All subjects were de-identified. There were about 8 endoscopists; all were board-certified gastroenterologists plus GE fellows who performed procedures at the time of the study. (Fellows rotated every 2 to 4 weeks in the GE clinic and were always accompanied by an attending gastroenterologist.)
All the endoscopists were instructed in the grading system adapted from the modified Aronchick scale (Table 1).4 This scale measures the quality of bowel preparation for the entire colon: excellent (> 95% visualization of bowel mucosa); good (> 90% of mucosa was visible); fair (some semisolid stool could be suctioned out, but > 90% of mucosa was visible), and poor (semisolid stool cannot be suctioned out and < 90% of mucosa was seen). The modified Aronchick scale also has an inadequate rating, but this was not used in the study. For this study, bowel preparation that was excellent or good received a 1, a fair preparation received a 2, and poor preparation received a 3. The Pearson correlation for the modified Aronchick scale coefficients was 0.62 (P < .001). The value for the kappa statistic was 0.77 (P < .001).5
Results
There were 77 men and 5 women enrolled in the study. The control group had 43 subjects, and the intervention group had 39 subjects. Only 28 subjects each from the control and intervention groups had the quality of bowel preparation rated by the endoscopists. In the control group, 53.6% were rated excellent or good, 42.9% were fair, and 3.5% were poor. In the intervention group, 42.9 % of preparations were excellent or good, 42.8% were fair, and 14.3% were poor (Table 2).
Preparation quality was not described in the procedure documentation for 34.9% and 28.2% of the subjects, respectively, for the control and intervention groups. There was no significant difference in no-show rates to procedures in either of the groups. Based on the data, a Fisher exact test for association was performed (P = .39), indicating there was no evidence of association between the intervention group and preparation quality.
The authors observed several recurrent themes during the group interventions. Fear of finding cancer and the perception of the procedure’s invasiveness were raised and addressed. Also misconceptions about CRC were debunked, such as the belief that a lack of bowel symptoms indicated no chance of having CRC or that only a family history indicated a risk factor. Patients discussed how much they learned about CRC, colon anatomy, and the importance of the bowel preparation. A multifaceted teaching approach was used to convey teaching points, such as flip charts, colonoscopy equipment, tours of procedure rooms, and visuals of various bowel preparation qualities. Throughout the educational intervention, humor, active listening, and reflection were woven into discussions to create a comfortable and relaxed learning environment.
Discussion and Limitations
The study results were unexpected. The authors had hypothesized that the group preprocedure educational intervention would have made a statistically significant difference in preparation quality, but it did not. In addition, the authors’ observations during the intervention led them to believe that the subjects had gained knowledge about how to correctly administer the bowel preparation.
Related: Do Age and Gender Matter in Colorectal Cancer?
A significant limitation of this pilot study was the difficulty in extrapolating meaningful data within the intervention group and between the intervention and control groups. After closely examining the raw data, the authors identified some key issues: There were only 28 subjects in each group who had bowel preparation quality described. This small sample size makes it difficult to draw meaningful conclusions. However, the education session in and of itself was clearly a positive experience for subjects, and the authors would recommend a future study with a larger sample size.
A prior power analysis would have helped this study determine a sufficient number of subjects that would be needed to determine whether the intervention had an effect. Furthermore, instead of tossing a coin to randomize the study groups, other types of randomization could have been used.
Other study limitations that came to light were:
- Variable preparation quality documentation by endoscopists;
- Limited availability of days to schedule group intervention classes;
- Some subjects did not attend the group session but still had the procedure done;
- The study invitation letter was long, and there were no financial incentives to participate;
- If pre- and postintervention testing had been conducted, effective and ineffective teaching strategies could have been identified; and
- The principal investigator also performed some of the procedures during the study, introducing potential bias.
Since the study, the authors have learned more about changes in national standards for bowel preparation administration and polyp surveillance. Preparation instructions need to be updated to reflect current recommendations for split-dose preparation administration in which the bowel preparation is taken in spaced doses, leading to better compliance and outcomes.6 Informally, patients and family have told staff that preparation instructions are difficult to understand. Following a Plan-Do-Study-Act cycle, feedback from patients should be obtained before revising and printing preparation instructions.7 This feedback could ensure that preparation instructions are written in patient-friendly, easily understood language.
Conclusion
Nursing professionals are likely to be effective in helping veterans achieve improved bowel preparation quality, because nurses have an established record as patient educators and advocates. Good bowel preparation quality is an important, achievable objective for veterans. As Mangnall reported, bowel preparation quality data are a strong nurse-sensitive quality measure that can be used to devise more effective interventions to obtain better bowel preparation results.8 As clinicians working on the frontline, nurses are well positioned to assess, intervene, and evaluate whether or not the modifications they have made to bowel preparation instructions are effective as they measure bowel preparation quality status post colonoscopy.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. American Society of Gastrointestinal Endoscopy. Media backgrounder: Colorectal cancer screening. American Society of Gastrointestinal Endoscopy Website. http://www.asge.org/PressroomIndex .aspx?id=552. Updated August 2014. Accessed January 29, 2015.
2. Lee RH. Quality colonoscopy: A matter of time, technique or technology? World J Gastroenterol. 2013;19(10):1517-1522.
3. Health Services Research & Development. 1004—Impact of a novel patient educational booklet on colonoscopy preparation in veterans. US Department of Veterans Affairs Website. http://www.hsrd .research.va.gov/meetings/2009/print_abstract .cfm?recordid=541. Accessed January 29, 2015.
4. Gurudu SR, Ratuapli S, Heigh R, DiBaise J, Leighton J, Crowell M. Quality of bowel cleansing for afternoon colonoscopy is influenced by time of administration. Am J Gastroenterol. 2010;105(11):2318-2322.
5. Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59(4):482-486.
6. Cohen, LB. Split dosing of bowel preparation for colonoscopy: An analysis of its efficacy, safety and tolerability. Gastrointest Endosc. 2010;72(2):406-412.
7. Institute for Healthcare Improvement. How to improve: Model for improvement. Institute for Healthcare improvement; 2015. Institute for Healthcare Improvement Website. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed February 5, 2015.
8. Mangnall R. Good bowel cleaning vital for effective colonoscopy. Nurse N Z. 2012;18(16):17-19.
1. American Society of Gastrointestinal Endoscopy. Media backgrounder: Colorectal cancer screening. American Society of Gastrointestinal Endoscopy Website. http://www.asge.org/PressroomIndex .aspx?id=552. Updated August 2014. Accessed January 29, 2015.
2. Lee RH. Quality colonoscopy: A matter of time, technique or technology? World J Gastroenterol. 2013;19(10):1517-1522.
3. Health Services Research & Development. 1004—Impact of a novel patient educational booklet on colonoscopy preparation in veterans. US Department of Veterans Affairs Website. http://www.hsrd .research.va.gov/meetings/2009/print_abstract .cfm?recordid=541. Accessed January 29, 2015.
4. Gurudu SR, Ratuapli S, Heigh R, DiBaise J, Leighton J, Crowell M. Quality of bowel cleansing for afternoon colonoscopy is influenced by time of administration. Am J Gastroenterol. 2010;105(11):2318-2322.
5. Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59(4):482-486.
6. Cohen, LB. Split dosing of bowel preparation for colonoscopy: An analysis of its efficacy, safety and tolerability. Gastrointest Endosc. 2010;72(2):406-412.
7. Institute for Healthcare Improvement. How to improve: Model for improvement. Institute for Healthcare improvement; 2015. Institute for Healthcare Improvement Website. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx. Accessed February 5, 2015.
8. Mangnall R. Good bowel cleaning vital for effective colonoscopy. Nurse N Z. 2012;18(16):17-19.