User login
Improving Admission Process Efficiency
Maintaining high‐quality patient care, optimizing patient safety, and providing adequate trainee supervision has been an area of debate in medical education recently, and many physicians remain concerned that excessive regulation and duty hour restrictions may prevent residents from obtaining sufficient experience and developing an appropriate sense of autonomy.[1, 2, 3, 4] However, pediatric hospital medicine (PHM) has seen dramatic increases in evening and nighttime in‐house attending coverage, and the trend is expected to continue.[5, 6] Whether it be for financial, educational, or patient‐centered reasons, increased in‐house attending coverage at an academic medical setting, almost by definition, increases direct resident supervision.[7]
Increased supervision may result in better educational outcomes,[8] but many forces, such as night float systems and electronic medical records (EMRs), pull residents away from the bedside, leaving them with fewer opportunities to make decisions and a reduced sense of personal responsibility and patient ownership. Experiential learning is of great value in medical training, and without this, residents may exit their training with less confidence and competence, only rarely having been able to make important medical decisions on their own.[9, 10]
Counter to the shift toward increased supervision, we recently amended our process for pediatric admissions to the PHM service by transitioning from mandatory to on‐demand attending input during the admissions process. We hypothesized that this would improve its efficiency by encouraging residents to develop an increased sense of patient ownership and would not significantly impact patient care.
METHODS
Setting
This cohort study was conducted at the Golisano Children's Hospital (GCH) at the University of Rochester in Rochester, New York. The pediatric residency program at this tertiary care center includes 48 pediatric residents and 21 medicinepediatric residents. The PHM division, comprised of 8 pediatric hospitalists, provides care to approximately one‐third of the children with medical illnesses admitted to GCH. During the daytime, PHM attendings provide in‐house supervision for 2 resident teams, each consisting of a senior resident and 2 interns. At night, PHM attendings take calls from home. Residents are encouraged to contact attendings, available by cell phone and pager, with questions or concerns regarding patient care. The institutional review board of the University of Rochester Medical Center approved this study and informed consent was waived.
Process Change
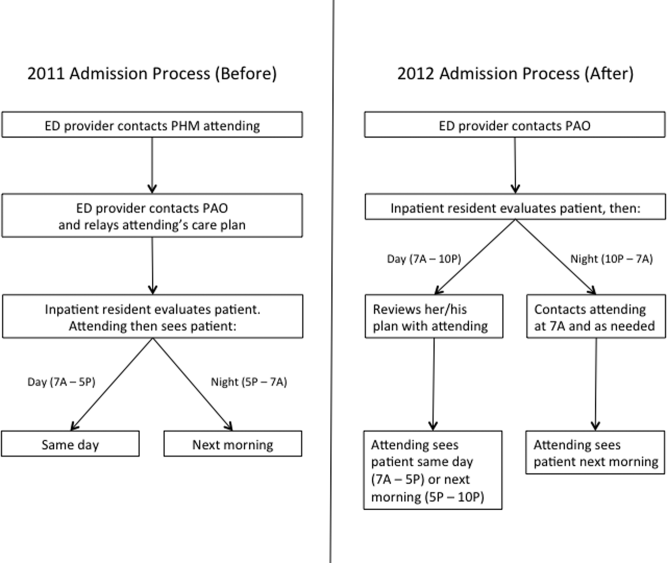
Prior to the change, a pediatric emergency department (ED) provider at GCH directly contacted the PHM attending for all admissions to the PHM service (Figure 1). If the PHM attending accepted the admission, the ED provider then notified the pediatric admitting officer (PAO), a third‐year pediatric or fourth‐year medicinepediatric resident, who either performed or delegated the admission duties (eg, history and physical exam, admission orders).
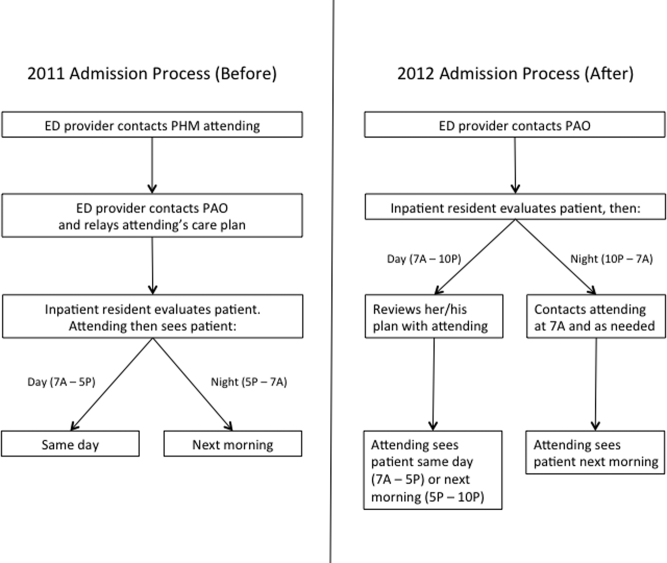
On June 18, 2012, a new process for pediatric admissions was implemented (Figure 1). The ED provider now called the PAO, and not the attending, to discuss an admission to the PHM service. The PAO was empowered to accept the patient on behalf of the PHM attending, and perform or delegate the admission duties. During daytime hours (7:00 am5:00 pm), the PAO was expected to alert the PHM attending of the admission to allow the attending to see the patient on the day of admission. The PHM attending discussed the case with the admitting resident after the resident had an opportunity to assess the patient and formulate a management plan. During evening hours (5:00 pm10:00 pm), the admitting resident was expected to contact the PHM attending on call after evaluating the patient and developing a plan. Overnight (10:00 pm7:00 am), the PAO was given discretion as to whether she/he needed to contact the PHM attending on call; the PHM service attending then saw the patient in the morning. Residents were strongly encouraged to call the PHM attending with any questions or concerns or if they did not feel an admission was appropriate to the PHM service.
Study Population
The study population included all patients <19 years of age admitted to the PHM service from the ED. The pre‐ and post‐intervention cohorts included patients admitted from July 1, 2011 to September 30, 2011 and July 1, 2012 to September 30, 2012, respectively. These dates were chosen because residents are least experienced in the summer months, and hence we would predict the greatest disparity during this time. Patients who were directly admitted via transport from an outside facility, office or from home, or who were transferred from another service within GCH were excluded. Patients were identified from administrative databases.
Data Collection
Date and time of admission, severity of illness (SOI) scores, and risk of mortality (ROM) scores were obtained from the administrative dataset. The EMR was then used to extract the following variables: gender; date and time of the ED provider's admission request and first inpatient resident order; date and time of patient discharge, defined as the time the after‐visit summary was finalized by an inpatient provider; and the number of rapid response team (RRT) activations within 24 hours of the first inpatient resident order. The order time difference was calculated by subtracting the date and time of the ED provider admission request from the first inpatient order. Cases in which the order time difference was negative were excluded from the order time analysis due to the possibility that some extenuating circumstance for these patients, not related to the admission process, caused the early inpatient order. Length of stay (LOS) was calculated as the difference between the date and time of ED admission request and date and time of patient discharge.
The first 24 hours of each admission were reviewed independently by 3 PHM attending investigators. Neither reviewer evaluated a chart for which he had cosigned the admission note. Charts were assessed to determine whether a reasonable standard of care (SOC) was provided by the inpatient resident during admission. For instances in which SOC was not felt to have been provided by the resident, the chart was reviewed by the second investigator. If there was disagreement between the 2 investigators, a third PHM attending was used to determine the majority opinion. Due to the nature of data collected, it was not possible to blind reviewers.
PHM attending investigators also assessed how often the inpatient resident's antibiotic choice was changed by the admitting PHM attending. This evaluation excluded topical antibiotics and antibiotics not related to the admitting diagnosis (eg, continuation of outpatient antibiotics for otitis media). A change in antibiotics was defined as a change in class or a change within classes, initiation, or discontinuation of an antibiotic by the attending. Switching the route of administration was considered a change if it was not done as part of the transition to discharge. Antibiotic choice was considered in agreement if a change was made by the PHM attending based on new patient information that was not available to the admitting inpatient resident if it could be reasonably concluded that the attending would have otherwise agreed with the original choice. If this determination could not be made, the antibiotic agreement was classified as unknown. Data regarding antibiotic agreement were analyzed in 2 ways. The first included all patients for which agreement could be determined. For this analysis, if a patient was not prescribed an antibiotic by the resident or attending, there was considered to have been antibiotic agreement. The second analysis included only the patients for whom an antibiotic was started by the inpatient resident or admitting attending.
Finally, RRT activations within the first 24 hours of admission in the 2012 cohort were evaluated to determine whether the RRT could have been prevented by the original admission process. This determination was made via majority opinion of 3 PHM attendings who each independently reviewed the cases.
Statistical Analysis
The distributions of continuous variables (eg, order time difference, LOS) and the ordinal variables (ROM and SOI) were compared using Wilcoxon rank sum tests. 2 tests or Fisher exact tests were used to assess the differences in categorical variables (eg, SOC, gender). All tests were 2‐sided, and the significance level was set at 0.05. Analyses were conducted using the SAS statistical package version 9.3 (SAS Institute Inc., Cary, NC) and SPSS version 21 (IBM/SPSS, Armonk, NY).
RESULTS
The initial search identified 532 admissions. Of these, 140 were excluded (72 were via route other than the ED, 44 were not admitted to PHM, 14 were outside the study period, and 10 did not meet age criteria). Therefore, 182 admissions in the 2011 cohort and 210 admissions in the 2012 cohort were included. For all patients in the 2012 cohort, the correct admission process was followed.
Demographic characteristics between cohorts were similar (Table 1). Data for ROM and SOI were available for 141 (78%) 2011 patients and for 169 (81%) 2012 patients. The distribution of patients over the study months differed between cohorts. Age, gender, ROM, and SOI were not significantly different.
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Male gender, n (%) | 107 (59) | 105 (50) | 0.082 |
| Median age, y (IQR) | 2 (010) | 2 (07) | 0.689 |
| Month admitted, n (%) | 0.002 | ||
| July | 60 (33) | 87 (41) | |
| August | 57 (31) | 81 (39) | |
| September | 65 (36) | 42 (20) | |
| Nighttime admission, n (%)* | 71 (39) | 90 (43) | 0.440 |
| Risk of mortality, n (%) | 0.910 | ||
| 1, lowest risk | 114 (81) | 138 (82) | |
| 2 | 22 (16) | 23 (14) | |
| 3 | 5 (4) | 6 (4) | |
| 4, highest risk | 0 (0) | 2 (1) | |
| Severity of illness, n (%) | 0.095 | ||
| 1, lowest severity | 60 (43) | 86 (51) | |
| 2 | 54 (38) | 62 (37) | |
| 3 | 25 (18) | 15 (9) | |
| 4, highest severity | 2 (1) | 6 (4) | |
The median difference in time from the ED provider admission request to the first inpatient resident order was roughly half as long in 2012 than in 2011 (123 vs 62 minutes, P<0.001) (Table 2). There were 12 cases in which the inpatient order came prior to the ED admission request in 2012 and 2 cases in 2011, and these were excluded from the order time difference analysis. LOS was not significantly different between groups (P=0.348). There were no differences in the frequency of antibiotic changes when all patients were considered or in the subgroup in whom antibiotics were prescribed by either the resident or attending. The number of cases for which the admitting resident's plan was deemed not to have met standard of care were few and not significantly different (P=1). None of these patients experienced harm as a result, and in all cases, SOC was determined to have been provided by the admitting PHM attending. The frequency of RRT calls within the first 24 hours of admission on PHM patients was not significantly different (P=0.114).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)a | 123 (70188) | 62 (30105) | <0.001 |
| Length of stay, h, median (IQR)b | 44 (3167) | 41 (2271) | 0.348 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 13/182 (7) | 18/210 (9) | 0.617 |
| Change by attending to resident's antibiotic choice in patients who received antibiotics, n (%) | 13/97 (13) | 18/96 (19) | 0.312 |
| Resident met standard of care, n (%) | 180/182 (99) | 207/210 (99) | 1 |
| RRT called within first 24 hours, n (%) | 2/182 (1) | 8/210 (4) | 0.114 |
When only patients admitted during the night in 2011 and 2012 were compared, results were consistent with the overall finding that there was a shorter time to inpatient admission order without a difference in other studied variables (Table 3).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)ab | 90 (40151) | 42 (1767) | 0.002 |
| Length of stay, h, median (IQR)b | 53 (3461) | 36 (1769) | 0.307 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 7/70 (10) | 7/88 (8) | 1 |
| Resident met standard of care, n (%) | 70/71 (99) | 88/90 (98) | 1 |
| RRT called within first 24 hours, n (%) | 2/71 (3) | 6/90 (7) | 0.468 |
DISCUSSION
The purpose of this study was to evaluate an admission process that removed an ineffective method of attending oversight and allowed residents an opportunity to develop patient care plans prior to attending input. The key change from the original process was removing the step in which the ED provider contacted the PHM attending for new admissions, thus eliminating mandatory inpatient attending input, removing an impediment to workflow, and empowering inpatient pediatric residents to assess new patients and develop management plans. Our data show a reduction in the time difference between the ED admission request and the inpatient resident's first order by more than an hour, indicating a more efficient admission process. Although one might expect that eliminating the act of a phone call would shorten this time by a few minutes, it cannot account for the extent of the difference we found. We postulate that an increased sense of accountability motivated inpatient residents to evaluate and begin management sooner, a topic that requires further exploration.
A more efficient admission process benefits emergency medicine residents and other ED providers as well. It is well documented that ED crowding is associated with decreased quality of care,[11, 12] and ED efficiency is receiving increased attention with newly reportable quality metrics such as Admit Decision Time to Emergency Department Departure Time for Admitted Patients.[13]
Our data do not attenuate the importance of hospitalists in patient care, as evidenced by the fact that PHM attendings continued to frequently amend the residents' antibiotic choicethe only variable we evaluated in terms of change in planand recognized several cases in which the residents' plan did not meet standard of care. Furthermore, attendings continued to be available by phone and pager for guidance and education when needed or requested by the residents. Instead, our data show that removing mandated attending input at the time of admission did not significantly impact major patient outcomes, which may partly be attributable to the general safety of the inpatient pediatric wards.[14, 15] In our study, a comprehensive analysis of patient harm was not possible given the variable list and infrequency with which SOC was not met or RRTs were called. Furthermore, our residency program continues to comply with national pediatric residency requirements for nighttime supervision.[7]
Our PHM division, which had previously allocated 2 hours of attending clinical time per call night, now averages <15 minutes. These data conflict with the current trend in PHM toward more, rather than less, direct attending oversight. Many PHM divisions have moved toward 24/7 in‐house coverage,[5] a situation that often results in shiftwork and multiple handoffs. Removing the in‐house attending overnight would allow for the rapidly growing PHM subspecialty to allocate hospitalists elsewhere depending on their scholarly needs, particularly as divisions seek to become increasingly involved in medical education, research, and hospital leadership.[16, 17] Although one might posit a financial benefit to having in‐house attendings determine the appropriateness of an admission overnight, we identified no case in which the insurance denied an admission.
Safety equivalence of an in‐house to on‐call attending is poorly studied in PHM. However, even in intensive care units, where the majority of morbidity and mortality occur, it is unclear that the presence of an attending, let alone mandating phone calls, positively impacts survival. One prospective trial failed to demonstrate a difference in patient outcomes in the critical care setting when comparing mandated attending in‐house involvement to optional attending availability by phone.[18] Furthermore, several studies have found no association with time of admission and mortality, implying there is no criticality specifically requiring nighttime coverage.[19, 20]
One adult study of nocturnists showed that residents felt they had more contact with attendings who were in‐house than attendings taking home calls.[21] However, when the residents were asked why they did not contact the attending, the only difference between at‐home and in‐house attendings was that for attendings available by phone, residents were less likely to know who to call and were hesitant to wake the attending.
This study had several limitations. First, we could not effectively blind reviewers; a salient point given that the reviewers benefited from the new system with a reduced nighttime workload. We attempted to minimize this bias by employing multiple independent evaluations followed by group consensus whenever possible. Second, even though we had 3 hospitalists independently review each 2012 RRT to determine whether it was preventable by the prior system, this task was prone to retrospective bias. Third, there was a significant difference in the month of admission between cohorts. Rather than biasing toward our observed time difference, the fact that more patients were admitted in July 2012the beginning of the academic yearmay have decreased our observed difference given that residents were less experienced. Forth, this study used certain measurable outcomes as proxies for quality of care and patient harm and was likely underpowered to truly detect a difference in some of the more infrequent variables. Furthermore, we did not evaluate other potential harms, such as cost. Fifth, we did not evaluate whether or not the new process changed ED provider behavior (ie, an ED provider may wait longer to request admission overnight given that the PHM attending is not mandated to provide input until the morning). Finally, although LOS was used as a balancing measure, it would likely have taken major events or omissions during the admission process to cause it to change significantly, and therefore the lack of statistical difference in this metric does not necessarily imply that more subtle aspects of care were the same between groups. We also chose not to include readmission rate for this reason, as any change could not conclusively be attributed to the new admission process.
CONCLUSION
Increasing resident autonomy by removing mandated input during PHM admissions makes the process more efficient and results in no significant changes to major patient outcomes. These data may be used by rapidly growing PHM divisions to redefine faculty clinical responsibilities, particularly at night.
ACKNOWLEDGMENTS
Disclosures: This project was supported by the University of Rochester CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors report no conflicts of interest.
- Accreditation Council for Graduate Medical Education Task Force on Quality Care and Professionalism. The ACGME 2011 duty hour standards: enhancing quality of care, supervision, and resident professional development. Accreditation Council for Graduate Medical Education, Chicago, IL; 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PDFs/jgme‐monograph[1].pdf. Last accessed on December 18, 2013.
- , , , , . Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systemic review. BMJ. 2011;342:d1580.
- , . ACGME 2011 duty‐hour guidelines: consequences expected by radiology residency directors and chief residents. J Am Coll Radiol. 2012;9(11):820–827.
- . Justifying patient risks associated with medical education. JAMA. 2007;298(9):1046–1048.
- , , , , , . Survey of academic pediatric hospitalist programs in the U.S.: organizational, administrative and financial factors. J Hosp Med. 2013;8(6):285–291.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. ACGME Approved: September 30, 2012; Effective: July 1, 2013. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Accessed September 17, 2013.
- , , , et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med. 2012;87(4):428–442.
- , . Twenty‐four‐hour intensivist staffing in teaching hospitals: tension between safety today and safety tomorrow. Chest. 2012;141(5):1315–1320.
- . Medical education on the brink: 62 years of front‐line observations and opinions. Tex Heart Inst J. 2012;39(3):322–329.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:6–7.
- , , , et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10.
- The Specifications Manual for National Hospital Inpatient Quality Measures. A Collaboration of the Centers for Medicare 128(1):72–78.
- , , , et al. Effect of a rapid response team on hospital‐wide mortality and code rates outside the ICU in a Children's Hospital. JAMA. 2007;298(19):2267–2274.
- Section on Hospital Medicine. Guiding principles for Pediatric Hospital Medicine programs. Pediatrics. 2013;132(4):782–786. SHM fact sheet: about hospital medicine. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Media_Kit42(5):120–126.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- , , , , , . Association between time of admission to the ICU and mortality: a systematic review and meta‐analysis. Chest. 2010;138(1):68–75.
- , , , . After‐hours admissions are not associated with increased risk‐adjusted mortality in pediatric intensive care. Intensive Care Med. 2008;34(1):148–151.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
Maintaining high‐quality patient care, optimizing patient safety, and providing adequate trainee supervision has been an area of debate in medical education recently, and many physicians remain concerned that excessive regulation and duty hour restrictions may prevent residents from obtaining sufficient experience and developing an appropriate sense of autonomy.[1, 2, 3, 4] However, pediatric hospital medicine (PHM) has seen dramatic increases in evening and nighttime in‐house attending coverage, and the trend is expected to continue.[5, 6] Whether it be for financial, educational, or patient‐centered reasons, increased in‐house attending coverage at an academic medical setting, almost by definition, increases direct resident supervision.[7]
Increased supervision may result in better educational outcomes,[8] but many forces, such as night float systems and electronic medical records (EMRs), pull residents away from the bedside, leaving them with fewer opportunities to make decisions and a reduced sense of personal responsibility and patient ownership. Experiential learning is of great value in medical training, and without this, residents may exit their training with less confidence and competence, only rarely having been able to make important medical decisions on their own.[9, 10]
Counter to the shift toward increased supervision, we recently amended our process for pediatric admissions to the PHM service by transitioning from mandatory to on‐demand attending input during the admissions process. We hypothesized that this would improve its efficiency by encouraging residents to develop an increased sense of patient ownership and would not significantly impact patient care.
METHODS
Setting
This cohort study was conducted at the Golisano Children's Hospital (GCH) at the University of Rochester in Rochester, New York. The pediatric residency program at this tertiary care center includes 48 pediatric residents and 21 medicinepediatric residents. The PHM division, comprised of 8 pediatric hospitalists, provides care to approximately one‐third of the children with medical illnesses admitted to GCH. During the daytime, PHM attendings provide in‐house supervision for 2 resident teams, each consisting of a senior resident and 2 interns. At night, PHM attendings take calls from home. Residents are encouraged to contact attendings, available by cell phone and pager, with questions or concerns regarding patient care. The institutional review board of the University of Rochester Medical Center approved this study and informed consent was waived.
Process Change
Prior to the change, a pediatric emergency department (ED) provider at GCH directly contacted the PHM attending for all admissions to the PHM service (Figure 1). If the PHM attending accepted the admission, the ED provider then notified the pediatric admitting officer (PAO), a third‐year pediatric or fourth‐year medicinepediatric resident, who either performed or delegated the admission duties (eg, history and physical exam, admission orders).
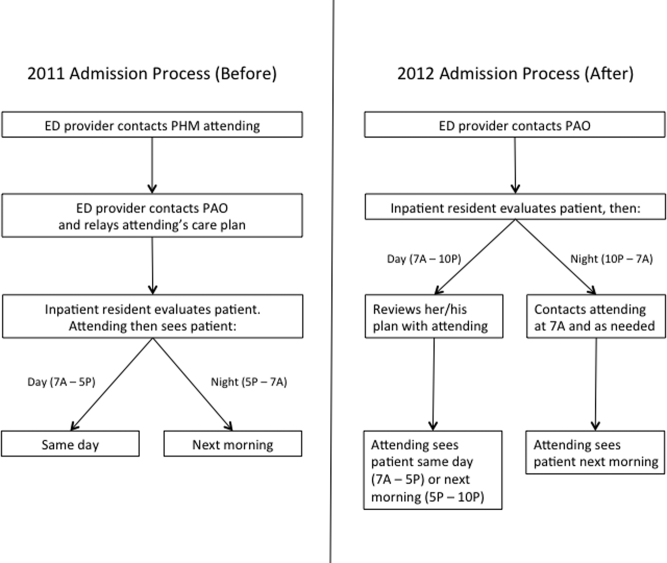
On June 18, 2012, a new process for pediatric admissions was implemented (Figure 1). The ED provider now called the PAO, and not the attending, to discuss an admission to the PHM service. The PAO was empowered to accept the patient on behalf of the PHM attending, and perform or delegate the admission duties. During daytime hours (7:00 am5:00 pm), the PAO was expected to alert the PHM attending of the admission to allow the attending to see the patient on the day of admission. The PHM attending discussed the case with the admitting resident after the resident had an opportunity to assess the patient and formulate a management plan. During evening hours (5:00 pm10:00 pm), the admitting resident was expected to contact the PHM attending on call after evaluating the patient and developing a plan. Overnight (10:00 pm7:00 am), the PAO was given discretion as to whether she/he needed to contact the PHM attending on call; the PHM service attending then saw the patient in the morning. Residents were strongly encouraged to call the PHM attending with any questions or concerns or if they did not feel an admission was appropriate to the PHM service.
Study Population
The study population included all patients <19 years of age admitted to the PHM service from the ED. The pre‐ and post‐intervention cohorts included patients admitted from July 1, 2011 to September 30, 2011 and July 1, 2012 to September 30, 2012, respectively. These dates were chosen because residents are least experienced in the summer months, and hence we would predict the greatest disparity during this time. Patients who were directly admitted via transport from an outside facility, office or from home, or who were transferred from another service within GCH were excluded. Patients were identified from administrative databases.
Data Collection
Date and time of admission, severity of illness (SOI) scores, and risk of mortality (ROM) scores were obtained from the administrative dataset. The EMR was then used to extract the following variables: gender; date and time of the ED provider's admission request and first inpatient resident order; date and time of patient discharge, defined as the time the after‐visit summary was finalized by an inpatient provider; and the number of rapid response team (RRT) activations within 24 hours of the first inpatient resident order. The order time difference was calculated by subtracting the date and time of the ED provider admission request from the first inpatient order. Cases in which the order time difference was negative were excluded from the order time analysis due to the possibility that some extenuating circumstance for these patients, not related to the admission process, caused the early inpatient order. Length of stay (LOS) was calculated as the difference between the date and time of ED admission request and date and time of patient discharge.
The first 24 hours of each admission were reviewed independently by 3 PHM attending investigators. Neither reviewer evaluated a chart for which he had cosigned the admission note. Charts were assessed to determine whether a reasonable standard of care (SOC) was provided by the inpatient resident during admission. For instances in which SOC was not felt to have been provided by the resident, the chart was reviewed by the second investigator. If there was disagreement between the 2 investigators, a third PHM attending was used to determine the majority opinion. Due to the nature of data collected, it was not possible to blind reviewers.
PHM attending investigators also assessed how often the inpatient resident's antibiotic choice was changed by the admitting PHM attending. This evaluation excluded topical antibiotics and antibiotics not related to the admitting diagnosis (eg, continuation of outpatient antibiotics for otitis media). A change in antibiotics was defined as a change in class or a change within classes, initiation, or discontinuation of an antibiotic by the attending. Switching the route of administration was considered a change if it was not done as part of the transition to discharge. Antibiotic choice was considered in agreement if a change was made by the PHM attending based on new patient information that was not available to the admitting inpatient resident if it could be reasonably concluded that the attending would have otherwise agreed with the original choice. If this determination could not be made, the antibiotic agreement was classified as unknown. Data regarding antibiotic agreement were analyzed in 2 ways. The first included all patients for which agreement could be determined. For this analysis, if a patient was not prescribed an antibiotic by the resident or attending, there was considered to have been antibiotic agreement. The second analysis included only the patients for whom an antibiotic was started by the inpatient resident or admitting attending.
Finally, RRT activations within the first 24 hours of admission in the 2012 cohort were evaluated to determine whether the RRT could have been prevented by the original admission process. This determination was made via majority opinion of 3 PHM attendings who each independently reviewed the cases.
Statistical Analysis
The distributions of continuous variables (eg, order time difference, LOS) and the ordinal variables (ROM and SOI) were compared using Wilcoxon rank sum tests. 2 tests or Fisher exact tests were used to assess the differences in categorical variables (eg, SOC, gender). All tests were 2‐sided, and the significance level was set at 0.05. Analyses were conducted using the SAS statistical package version 9.3 (SAS Institute Inc., Cary, NC) and SPSS version 21 (IBM/SPSS, Armonk, NY).
RESULTS
The initial search identified 532 admissions. Of these, 140 were excluded (72 were via route other than the ED, 44 were not admitted to PHM, 14 were outside the study period, and 10 did not meet age criteria). Therefore, 182 admissions in the 2011 cohort and 210 admissions in the 2012 cohort were included. For all patients in the 2012 cohort, the correct admission process was followed.
Demographic characteristics between cohorts were similar (Table 1). Data for ROM and SOI were available for 141 (78%) 2011 patients and for 169 (81%) 2012 patients. The distribution of patients over the study months differed between cohorts. Age, gender, ROM, and SOI were not significantly different.
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Male gender, n (%) | 107 (59) | 105 (50) | 0.082 |
| Median age, y (IQR) | 2 (010) | 2 (07) | 0.689 |
| Month admitted, n (%) | 0.002 | ||
| July | 60 (33) | 87 (41) | |
| August | 57 (31) | 81 (39) | |
| September | 65 (36) | 42 (20) | |
| Nighttime admission, n (%)* | 71 (39) | 90 (43) | 0.440 |
| Risk of mortality, n (%) | 0.910 | ||
| 1, lowest risk | 114 (81) | 138 (82) | |
| 2 | 22 (16) | 23 (14) | |
| 3 | 5 (4) | 6 (4) | |
| 4, highest risk | 0 (0) | 2 (1) | |
| Severity of illness, n (%) | 0.095 | ||
| 1, lowest severity | 60 (43) | 86 (51) | |
| 2 | 54 (38) | 62 (37) | |
| 3 | 25 (18) | 15 (9) | |
| 4, highest severity | 2 (1) | 6 (4) | |
The median difference in time from the ED provider admission request to the first inpatient resident order was roughly half as long in 2012 than in 2011 (123 vs 62 minutes, P<0.001) (Table 2). There were 12 cases in which the inpatient order came prior to the ED admission request in 2012 and 2 cases in 2011, and these were excluded from the order time difference analysis. LOS was not significantly different between groups (P=0.348). There were no differences in the frequency of antibiotic changes when all patients were considered or in the subgroup in whom antibiotics were prescribed by either the resident or attending. The number of cases for which the admitting resident's plan was deemed not to have met standard of care were few and not significantly different (P=1). None of these patients experienced harm as a result, and in all cases, SOC was determined to have been provided by the admitting PHM attending. The frequency of RRT calls within the first 24 hours of admission on PHM patients was not significantly different (P=0.114).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)a | 123 (70188) | 62 (30105) | <0.001 |
| Length of stay, h, median (IQR)b | 44 (3167) | 41 (2271) | 0.348 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 13/182 (7) | 18/210 (9) | 0.617 |
| Change by attending to resident's antibiotic choice in patients who received antibiotics, n (%) | 13/97 (13) | 18/96 (19) | 0.312 |
| Resident met standard of care, n (%) | 180/182 (99) | 207/210 (99) | 1 |
| RRT called within first 24 hours, n (%) | 2/182 (1) | 8/210 (4) | 0.114 |
When only patients admitted during the night in 2011 and 2012 were compared, results were consistent with the overall finding that there was a shorter time to inpatient admission order without a difference in other studied variables (Table 3).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)ab | 90 (40151) | 42 (1767) | 0.002 |
| Length of stay, h, median (IQR)b | 53 (3461) | 36 (1769) | 0.307 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 7/70 (10) | 7/88 (8) | 1 |
| Resident met standard of care, n (%) | 70/71 (99) | 88/90 (98) | 1 |
| RRT called within first 24 hours, n (%) | 2/71 (3) | 6/90 (7) | 0.468 |
DISCUSSION
The purpose of this study was to evaluate an admission process that removed an ineffective method of attending oversight and allowed residents an opportunity to develop patient care plans prior to attending input. The key change from the original process was removing the step in which the ED provider contacted the PHM attending for new admissions, thus eliminating mandatory inpatient attending input, removing an impediment to workflow, and empowering inpatient pediatric residents to assess new patients and develop management plans. Our data show a reduction in the time difference between the ED admission request and the inpatient resident's first order by more than an hour, indicating a more efficient admission process. Although one might expect that eliminating the act of a phone call would shorten this time by a few minutes, it cannot account for the extent of the difference we found. We postulate that an increased sense of accountability motivated inpatient residents to evaluate and begin management sooner, a topic that requires further exploration.
A more efficient admission process benefits emergency medicine residents and other ED providers as well. It is well documented that ED crowding is associated with decreased quality of care,[11, 12] and ED efficiency is receiving increased attention with newly reportable quality metrics such as Admit Decision Time to Emergency Department Departure Time for Admitted Patients.[13]
Our data do not attenuate the importance of hospitalists in patient care, as evidenced by the fact that PHM attendings continued to frequently amend the residents' antibiotic choicethe only variable we evaluated in terms of change in planand recognized several cases in which the residents' plan did not meet standard of care. Furthermore, attendings continued to be available by phone and pager for guidance and education when needed or requested by the residents. Instead, our data show that removing mandated attending input at the time of admission did not significantly impact major patient outcomes, which may partly be attributable to the general safety of the inpatient pediatric wards.[14, 15] In our study, a comprehensive analysis of patient harm was not possible given the variable list and infrequency with which SOC was not met or RRTs were called. Furthermore, our residency program continues to comply with national pediatric residency requirements for nighttime supervision.[7]
Our PHM division, which had previously allocated 2 hours of attending clinical time per call night, now averages <15 minutes. These data conflict with the current trend in PHM toward more, rather than less, direct attending oversight. Many PHM divisions have moved toward 24/7 in‐house coverage,[5] a situation that often results in shiftwork and multiple handoffs. Removing the in‐house attending overnight would allow for the rapidly growing PHM subspecialty to allocate hospitalists elsewhere depending on their scholarly needs, particularly as divisions seek to become increasingly involved in medical education, research, and hospital leadership.[16, 17] Although one might posit a financial benefit to having in‐house attendings determine the appropriateness of an admission overnight, we identified no case in which the insurance denied an admission.
Safety equivalence of an in‐house to on‐call attending is poorly studied in PHM. However, even in intensive care units, where the majority of morbidity and mortality occur, it is unclear that the presence of an attending, let alone mandating phone calls, positively impacts survival. One prospective trial failed to demonstrate a difference in patient outcomes in the critical care setting when comparing mandated attending in‐house involvement to optional attending availability by phone.[18] Furthermore, several studies have found no association with time of admission and mortality, implying there is no criticality specifically requiring nighttime coverage.[19, 20]
One adult study of nocturnists showed that residents felt they had more contact with attendings who were in‐house than attendings taking home calls.[21] However, when the residents were asked why they did not contact the attending, the only difference between at‐home and in‐house attendings was that for attendings available by phone, residents were less likely to know who to call and were hesitant to wake the attending.
This study had several limitations. First, we could not effectively blind reviewers; a salient point given that the reviewers benefited from the new system with a reduced nighttime workload. We attempted to minimize this bias by employing multiple independent evaluations followed by group consensus whenever possible. Second, even though we had 3 hospitalists independently review each 2012 RRT to determine whether it was preventable by the prior system, this task was prone to retrospective bias. Third, there was a significant difference in the month of admission between cohorts. Rather than biasing toward our observed time difference, the fact that more patients were admitted in July 2012the beginning of the academic yearmay have decreased our observed difference given that residents were less experienced. Forth, this study used certain measurable outcomes as proxies for quality of care and patient harm and was likely underpowered to truly detect a difference in some of the more infrequent variables. Furthermore, we did not evaluate other potential harms, such as cost. Fifth, we did not evaluate whether or not the new process changed ED provider behavior (ie, an ED provider may wait longer to request admission overnight given that the PHM attending is not mandated to provide input until the morning). Finally, although LOS was used as a balancing measure, it would likely have taken major events or omissions during the admission process to cause it to change significantly, and therefore the lack of statistical difference in this metric does not necessarily imply that more subtle aspects of care were the same between groups. We also chose not to include readmission rate for this reason, as any change could not conclusively be attributed to the new admission process.
CONCLUSION
Increasing resident autonomy by removing mandated input during PHM admissions makes the process more efficient and results in no significant changes to major patient outcomes. These data may be used by rapidly growing PHM divisions to redefine faculty clinical responsibilities, particularly at night.
ACKNOWLEDGMENTS
Disclosures: This project was supported by the University of Rochester CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors report no conflicts of interest.
Maintaining high‐quality patient care, optimizing patient safety, and providing adequate trainee supervision has been an area of debate in medical education recently, and many physicians remain concerned that excessive regulation and duty hour restrictions may prevent residents from obtaining sufficient experience and developing an appropriate sense of autonomy.[1, 2, 3, 4] However, pediatric hospital medicine (PHM) has seen dramatic increases in evening and nighttime in‐house attending coverage, and the trend is expected to continue.[5, 6] Whether it be for financial, educational, or patient‐centered reasons, increased in‐house attending coverage at an academic medical setting, almost by definition, increases direct resident supervision.[7]
Increased supervision may result in better educational outcomes,[8] but many forces, such as night float systems and electronic medical records (EMRs), pull residents away from the bedside, leaving them with fewer opportunities to make decisions and a reduced sense of personal responsibility and patient ownership. Experiential learning is of great value in medical training, and without this, residents may exit their training with less confidence and competence, only rarely having been able to make important medical decisions on their own.[9, 10]
Counter to the shift toward increased supervision, we recently amended our process for pediatric admissions to the PHM service by transitioning from mandatory to on‐demand attending input during the admissions process. We hypothesized that this would improve its efficiency by encouraging residents to develop an increased sense of patient ownership and would not significantly impact patient care.
METHODS
Setting
This cohort study was conducted at the Golisano Children's Hospital (GCH) at the University of Rochester in Rochester, New York. The pediatric residency program at this tertiary care center includes 48 pediatric residents and 21 medicinepediatric residents. The PHM division, comprised of 8 pediatric hospitalists, provides care to approximately one‐third of the children with medical illnesses admitted to GCH. During the daytime, PHM attendings provide in‐house supervision for 2 resident teams, each consisting of a senior resident and 2 interns. At night, PHM attendings take calls from home. Residents are encouraged to contact attendings, available by cell phone and pager, with questions or concerns regarding patient care. The institutional review board of the University of Rochester Medical Center approved this study and informed consent was waived.
Process Change
Prior to the change, a pediatric emergency department (ED) provider at GCH directly contacted the PHM attending for all admissions to the PHM service (Figure 1). If the PHM attending accepted the admission, the ED provider then notified the pediatric admitting officer (PAO), a third‐year pediatric or fourth‐year medicinepediatric resident, who either performed or delegated the admission duties (eg, history and physical exam, admission orders).
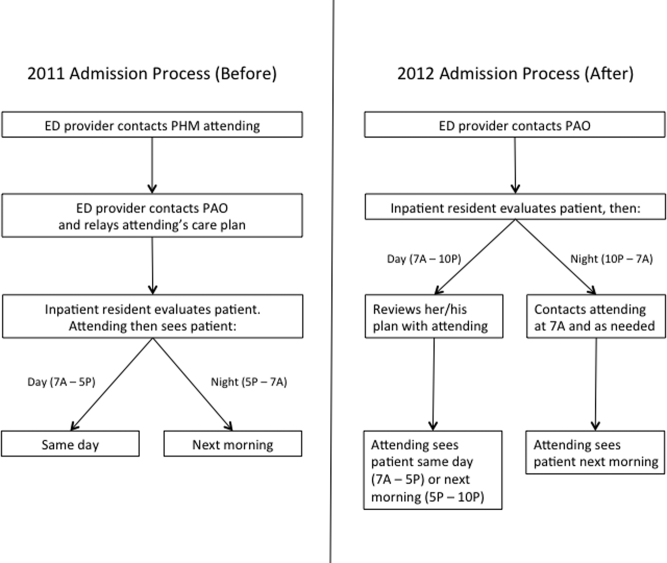
On June 18, 2012, a new process for pediatric admissions was implemented (Figure 1). The ED provider now called the PAO, and not the attending, to discuss an admission to the PHM service. The PAO was empowered to accept the patient on behalf of the PHM attending, and perform or delegate the admission duties. During daytime hours (7:00 am5:00 pm), the PAO was expected to alert the PHM attending of the admission to allow the attending to see the patient on the day of admission. The PHM attending discussed the case with the admitting resident after the resident had an opportunity to assess the patient and formulate a management plan. During evening hours (5:00 pm10:00 pm), the admitting resident was expected to contact the PHM attending on call after evaluating the patient and developing a plan. Overnight (10:00 pm7:00 am), the PAO was given discretion as to whether she/he needed to contact the PHM attending on call; the PHM service attending then saw the patient in the morning. Residents were strongly encouraged to call the PHM attending with any questions or concerns or if they did not feel an admission was appropriate to the PHM service.
Study Population
The study population included all patients <19 years of age admitted to the PHM service from the ED. The pre‐ and post‐intervention cohorts included patients admitted from July 1, 2011 to September 30, 2011 and July 1, 2012 to September 30, 2012, respectively. These dates were chosen because residents are least experienced in the summer months, and hence we would predict the greatest disparity during this time. Patients who were directly admitted via transport from an outside facility, office or from home, or who were transferred from another service within GCH were excluded. Patients were identified from administrative databases.
Data Collection
Date and time of admission, severity of illness (SOI) scores, and risk of mortality (ROM) scores were obtained from the administrative dataset. The EMR was then used to extract the following variables: gender; date and time of the ED provider's admission request and first inpatient resident order; date and time of patient discharge, defined as the time the after‐visit summary was finalized by an inpatient provider; and the number of rapid response team (RRT) activations within 24 hours of the first inpatient resident order. The order time difference was calculated by subtracting the date and time of the ED provider admission request from the first inpatient order. Cases in which the order time difference was negative were excluded from the order time analysis due to the possibility that some extenuating circumstance for these patients, not related to the admission process, caused the early inpatient order. Length of stay (LOS) was calculated as the difference between the date and time of ED admission request and date and time of patient discharge.
The first 24 hours of each admission were reviewed independently by 3 PHM attending investigators. Neither reviewer evaluated a chart for which he had cosigned the admission note. Charts were assessed to determine whether a reasonable standard of care (SOC) was provided by the inpatient resident during admission. For instances in which SOC was not felt to have been provided by the resident, the chart was reviewed by the second investigator. If there was disagreement between the 2 investigators, a third PHM attending was used to determine the majority opinion. Due to the nature of data collected, it was not possible to blind reviewers.
PHM attending investigators also assessed how often the inpatient resident's antibiotic choice was changed by the admitting PHM attending. This evaluation excluded topical antibiotics and antibiotics not related to the admitting diagnosis (eg, continuation of outpatient antibiotics for otitis media). A change in antibiotics was defined as a change in class or a change within classes, initiation, or discontinuation of an antibiotic by the attending. Switching the route of administration was considered a change if it was not done as part of the transition to discharge. Antibiotic choice was considered in agreement if a change was made by the PHM attending based on new patient information that was not available to the admitting inpatient resident if it could be reasonably concluded that the attending would have otherwise agreed with the original choice. If this determination could not be made, the antibiotic agreement was classified as unknown. Data regarding antibiotic agreement were analyzed in 2 ways. The first included all patients for which agreement could be determined. For this analysis, if a patient was not prescribed an antibiotic by the resident or attending, there was considered to have been antibiotic agreement. The second analysis included only the patients for whom an antibiotic was started by the inpatient resident or admitting attending.
Finally, RRT activations within the first 24 hours of admission in the 2012 cohort were evaluated to determine whether the RRT could have been prevented by the original admission process. This determination was made via majority opinion of 3 PHM attendings who each independently reviewed the cases.
Statistical Analysis
The distributions of continuous variables (eg, order time difference, LOS) and the ordinal variables (ROM and SOI) were compared using Wilcoxon rank sum tests. 2 tests or Fisher exact tests were used to assess the differences in categorical variables (eg, SOC, gender). All tests were 2‐sided, and the significance level was set at 0.05. Analyses were conducted using the SAS statistical package version 9.3 (SAS Institute Inc., Cary, NC) and SPSS version 21 (IBM/SPSS, Armonk, NY).
RESULTS
The initial search identified 532 admissions. Of these, 140 were excluded (72 were via route other than the ED, 44 were not admitted to PHM, 14 were outside the study period, and 10 did not meet age criteria). Therefore, 182 admissions in the 2011 cohort and 210 admissions in the 2012 cohort were included. For all patients in the 2012 cohort, the correct admission process was followed.
Demographic characteristics between cohorts were similar (Table 1). Data for ROM and SOI were available for 141 (78%) 2011 patients and for 169 (81%) 2012 patients. The distribution of patients over the study months differed between cohorts. Age, gender, ROM, and SOI were not significantly different.
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Male gender, n (%) | 107 (59) | 105 (50) | 0.082 |
| Median age, y (IQR) | 2 (010) | 2 (07) | 0.689 |
| Month admitted, n (%) | 0.002 | ||
| July | 60 (33) | 87 (41) | |
| August | 57 (31) | 81 (39) | |
| September | 65 (36) | 42 (20) | |
| Nighttime admission, n (%)* | 71 (39) | 90 (43) | 0.440 |
| Risk of mortality, n (%) | 0.910 | ||
| 1, lowest risk | 114 (81) | 138 (82) | |
| 2 | 22 (16) | 23 (14) | |
| 3 | 5 (4) | 6 (4) | |
| 4, highest risk | 0 (0) | 2 (1) | |
| Severity of illness, n (%) | 0.095 | ||
| 1, lowest severity | 60 (43) | 86 (51) | |
| 2 | 54 (38) | 62 (37) | |
| 3 | 25 (18) | 15 (9) | |
| 4, highest severity | 2 (1) | 6 (4) | |
The median difference in time from the ED provider admission request to the first inpatient resident order was roughly half as long in 2012 than in 2011 (123 vs 62 minutes, P<0.001) (Table 2). There were 12 cases in which the inpatient order came prior to the ED admission request in 2012 and 2 cases in 2011, and these were excluded from the order time difference analysis. LOS was not significantly different between groups (P=0.348). There were no differences in the frequency of antibiotic changes when all patients were considered or in the subgroup in whom antibiotics were prescribed by either the resident or attending. The number of cases for which the admitting resident's plan was deemed not to have met standard of care were few and not significantly different (P=1). None of these patients experienced harm as a result, and in all cases, SOC was determined to have been provided by the admitting PHM attending. The frequency of RRT calls within the first 24 hours of admission on PHM patients was not significantly different (P=0.114).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)a | 123 (70188) | 62 (30105) | <0.001 |
| Length of stay, h, median (IQR)b | 44 (3167) | 41 (2271) | 0.348 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 13/182 (7) | 18/210 (9) | 0.617 |
| Change by attending to resident's antibiotic choice in patients who received antibiotics, n (%) | 13/97 (13) | 18/96 (19) | 0.312 |
| Resident met standard of care, n (%) | 180/182 (99) | 207/210 (99) | 1 |
| RRT called within first 24 hours, n (%) | 2/182 (1) | 8/210 (4) | 0.114 |
When only patients admitted during the night in 2011 and 2012 were compared, results were consistent with the overall finding that there was a shorter time to inpatient admission order without a difference in other studied variables (Table 3).
| Variable | 2011 | 2012 | P Value |
|---|---|---|---|
| |||
| Time from admission decision to first inpatient order, min, median (IQR)ab | 90 (40151) | 42 (1767) | 0.002 |
| Length of stay, h, median (IQR)b | 53 (3461) | 36 (1769) | 0.307 |
| Change by attending to resident's antibiotic choice in all patients, n (%) | 7/70 (10) | 7/88 (8) | 1 |
| Resident met standard of care, n (%) | 70/71 (99) | 88/90 (98) | 1 |
| RRT called within first 24 hours, n (%) | 2/71 (3) | 6/90 (7) | 0.468 |
DISCUSSION
The purpose of this study was to evaluate an admission process that removed an ineffective method of attending oversight and allowed residents an opportunity to develop patient care plans prior to attending input. The key change from the original process was removing the step in which the ED provider contacted the PHM attending for new admissions, thus eliminating mandatory inpatient attending input, removing an impediment to workflow, and empowering inpatient pediatric residents to assess new patients and develop management plans. Our data show a reduction in the time difference between the ED admission request and the inpatient resident's first order by more than an hour, indicating a more efficient admission process. Although one might expect that eliminating the act of a phone call would shorten this time by a few minutes, it cannot account for the extent of the difference we found. We postulate that an increased sense of accountability motivated inpatient residents to evaluate and begin management sooner, a topic that requires further exploration.
A more efficient admission process benefits emergency medicine residents and other ED providers as well. It is well documented that ED crowding is associated with decreased quality of care,[11, 12] and ED efficiency is receiving increased attention with newly reportable quality metrics such as Admit Decision Time to Emergency Department Departure Time for Admitted Patients.[13]
Our data do not attenuate the importance of hospitalists in patient care, as evidenced by the fact that PHM attendings continued to frequently amend the residents' antibiotic choicethe only variable we evaluated in terms of change in planand recognized several cases in which the residents' plan did not meet standard of care. Furthermore, attendings continued to be available by phone and pager for guidance and education when needed or requested by the residents. Instead, our data show that removing mandated attending input at the time of admission did not significantly impact major patient outcomes, which may partly be attributable to the general safety of the inpatient pediatric wards.[14, 15] In our study, a comprehensive analysis of patient harm was not possible given the variable list and infrequency with which SOC was not met or RRTs were called. Furthermore, our residency program continues to comply with national pediatric residency requirements for nighttime supervision.[7]
Our PHM division, which had previously allocated 2 hours of attending clinical time per call night, now averages <15 minutes. These data conflict with the current trend in PHM toward more, rather than less, direct attending oversight. Many PHM divisions have moved toward 24/7 in‐house coverage,[5] a situation that often results in shiftwork and multiple handoffs. Removing the in‐house attending overnight would allow for the rapidly growing PHM subspecialty to allocate hospitalists elsewhere depending on their scholarly needs, particularly as divisions seek to become increasingly involved in medical education, research, and hospital leadership.[16, 17] Although one might posit a financial benefit to having in‐house attendings determine the appropriateness of an admission overnight, we identified no case in which the insurance denied an admission.
Safety equivalence of an in‐house to on‐call attending is poorly studied in PHM. However, even in intensive care units, where the majority of morbidity and mortality occur, it is unclear that the presence of an attending, let alone mandating phone calls, positively impacts survival. One prospective trial failed to demonstrate a difference in patient outcomes in the critical care setting when comparing mandated attending in‐house involvement to optional attending availability by phone.[18] Furthermore, several studies have found no association with time of admission and mortality, implying there is no criticality specifically requiring nighttime coverage.[19, 20]
One adult study of nocturnists showed that residents felt they had more contact with attendings who were in‐house than attendings taking home calls.[21] However, when the residents were asked why they did not contact the attending, the only difference between at‐home and in‐house attendings was that for attendings available by phone, residents were less likely to know who to call and were hesitant to wake the attending.
This study had several limitations. First, we could not effectively blind reviewers; a salient point given that the reviewers benefited from the new system with a reduced nighttime workload. We attempted to minimize this bias by employing multiple independent evaluations followed by group consensus whenever possible. Second, even though we had 3 hospitalists independently review each 2012 RRT to determine whether it was preventable by the prior system, this task was prone to retrospective bias. Third, there was a significant difference in the month of admission between cohorts. Rather than biasing toward our observed time difference, the fact that more patients were admitted in July 2012the beginning of the academic yearmay have decreased our observed difference given that residents were less experienced. Forth, this study used certain measurable outcomes as proxies for quality of care and patient harm and was likely underpowered to truly detect a difference in some of the more infrequent variables. Furthermore, we did not evaluate other potential harms, such as cost. Fifth, we did not evaluate whether or not the new process changed ED provider behavior (ie, an ED provider may wait longer to request admission overnight given that the PHM attending is not mandated to provide input until the morning). Finally, although LOS was used as a balancing measure, it would likely have taken major events or omissions during the admission process to cause it to change significantly, and therefore the lack of statistical difference in this metric does not necessarily imply that more subtle aspects of care were the same between groups. We also chose not to include readmission rate for this reason, as any change could not conclusively be attributed to the new admission process.
CONCLUSION
Increasing resident autonomy by removing mandated input during PHM admissions makes the process more efficient and results in no significant changes to major patient outcomes. These data may be used by rapidly growing PHM divisions to redefine faculty clinical responsibilities, particularly at night.
ACKNOWLEDGMENTS
Disclosures: This project was supported by the University of Rochester CTSA award number UL1 TR000042 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors report no conflicts of interest.
- Accreditation Council for Graduate Medical Education Task Force on Quality Care and Professionalism. The ACGME 2011 duty hour standards: enhancing quality of care, supervision, and resident professional development. Accreditation Council for Graduate Medical Education, Chicago, IL; 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PDFs/jgme‐monograph[1].pdf. Last accessed on December 18, 2013.
- , , , , . Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systemic review. BMJ. 2011;342:d1580.
- , . ACGME 2011 duty‐hour guidelines: consequences expected by radiology residency directors and chief residents. J Am Coll Radiol. 2012;9(11):820–827.
- . Justifying patient risks associated with medical education. JAMA. 2007;298(9):1046–1048.
- , , , , , . Survey of academic pediatric hospitalist programs in the U.S.: organizational, administrative and financial factors. J Hosp Med. 2013;8(6):285–291.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. ACGME Approved: September 30, 2012; Effective: July 1, 2013. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Accessed September 17, 2013.
- , , , et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med. 2012;87(4):428–442.
- , . Twenty‐four‐hour intensivist staffing in teaching hospitals: tension between safety today and safety tomorrow. Chest. 2012;141(5):1315–1320.
- . Medical education on the brink: 62 years of front‐line observations and opinions. Tex Heart Inst J. 2012;39(3):322–329.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:6–7.
- , , , et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10.
- The Specifications Manual for National Hospital Inpatient Quality Measures. A Collaboration of the Centers for Medicare 128(1):72–78.
- , , , et al. Effect of a rapid response team on hospital‐wide mortality and code rates outside the ICU in a Children's Hospital. JAMA. 2007;298(19):2267–2274.
- Section on Hospital Medicine. Guiding principles for Pediatric Hospital Medicine programs. Pediatrics. 2013;132(4):782–786. SHM fact sheet: about hospital medicine. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Media_Kit42(5):120–126.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- , , , , , . Association between time of admission to the ICU and mortality: a systematic review and meta‐analysis. Chest. 2010;138(1):68–75.
- , , , . After‐hours admissions are not associated with increased risk‐adjusted mortality in pediatric intensive care. Intensive Care Med. 2008;34(1):148–151.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
- Accreditation Council for Graduate Medical Education Task Force on Quality Care and Professionalism. The ACGME 2011 duty hour standards: enhancing quality of care, supervision, and resident professional development. Accreditation Council for Graduate Medical Education, Chicago, IL; 2011. Available at: http://www.acgme.org/acgmeweb/Portals/0/PDFs/jgme‐monograph[1].pdf. Last accessed on December 18, 2013.
- , , , , . Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systemic review. BMJ. 2011;342:d1580.
- , . ACGME 2011 duty‐hour guidelines: consequences expected by radiology residency directors and chief residents. J Am Coll Radiol. 2012;9(11):820–827.
- . Justifying patient risks associated with medical education. JAMA. 2007;298(9):1046–1048.
- , , , , , . Survey of academic pediatric hospitalist programs in the U.S.: organizational, administrative and financial factors. J Hosp Med. 2013;8(6):285–291.
- , , , . Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist. J Hosp Med. 2012;7(4):299–303.
- ACGME Program Requirements for Graduate Medical Education in Pediatrics. ACGME Approved: September 30, 2012; Effective: July 1, 2013. Available at: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/2013‐PR‐FAQ‐PIF/320_pediatrics_07012013.pdf. Accessed September 17, 2013.
- , , , et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med. 2012;87(4):428–442.
- , . Twenty‐four‐hour intensivist staffing in teaching hospitals: tension between safety today and safety tomorrow. Chest. 2012;141(5):1315–1320.
- . Medical education on the brink: 62 years of front‐line observations and opinions. Tex Heart Inst J. 2012;39(3):322–329.
- , . Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:6–7.
- , , , et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10.
- The Specifications Manual for National Hospital Inpatient Quality Measures. A Collaboration of the Centers for Medicare 128(1):72–78.
- , , , et al. Effect of a rapid response team on hospital‐wide mortality and code rates outside the ICU in a Children's Hospital. JAMA. 2007;298(19):2267–2274.
- Section on Hospital Medicine. Guiding principles for Pediatric Hospital Medicine programs. Pediatrics. 2013;132(4):782–786. SHM fact sheet: about hospital medicine. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Media_Kit42(5):120–126.
- , , , et al. A randomized trial of nighttime physician staffing in an intensive care unit. N Engl J Med. 2013;368(23):2201–2209.
- , , , , , . Association between time of admission to the ICU and mortality: a systematic review and meta‐analysis. Chest. 2010;138(1):68–75.
- , , , . After‐hours admissions are not associated with increased risk‐adjusted mortality in pediatric intensive care. Intensive Care Med. 2008;34(1):148–151.
- , , , , , . Effects of increased overnight supervision on resident education, decision‐making, and autonomy. J Hosp Med. 2012;7(8):606–610.
© 2013 Society of Hospital Medicine