User login
Geriatric Train‐The‐Trainer Program
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
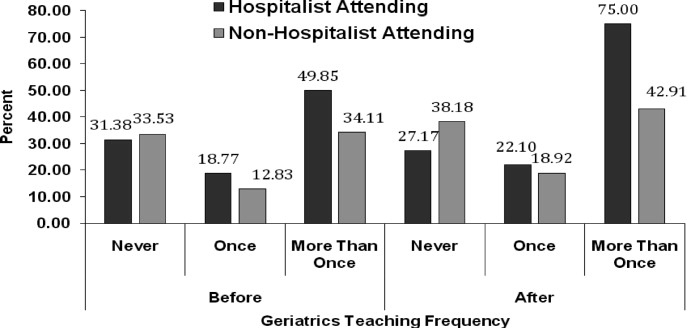
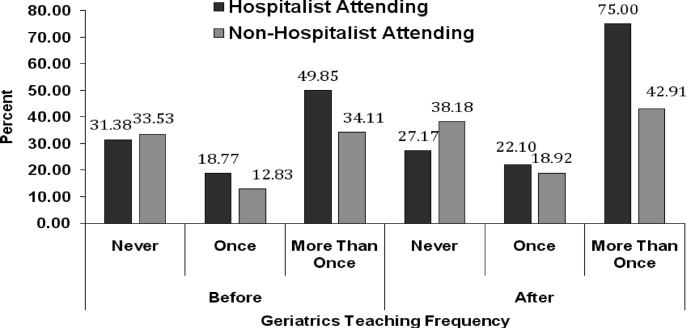
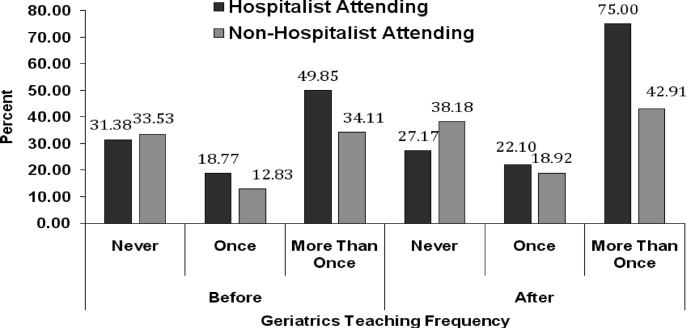
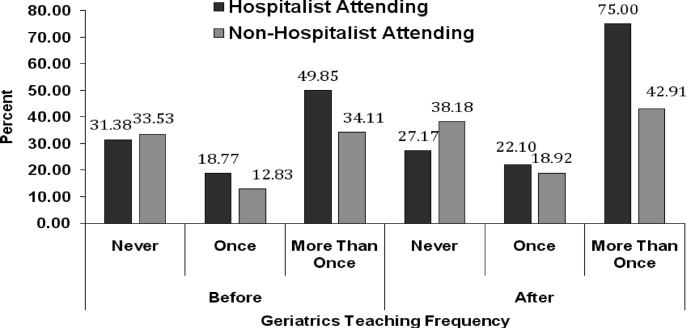
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
Nearly half of the hospital beds in the United States are occupied by the elderly,1 whose numbers are increasing.2 The odds of a hospitalized Medicare patient being cared for by a hospitalist are increasing by nearly 30% per year.3 Hospitalists require competence in geriatrics to serve their patients and to teach trainees. Train‐the‐Trainer (TTT) programs both educate health care providers and provide educational materials, information, and skills for teaching others.4 This model has been successfully used in geriatrics to impact knowledge, attitudes, and self‐efficacy among health care workers.46
A prominent example of a geriatrics TTT program is the University of Chicago Curriculum for the Hospitalized Aging Medical Patient (CHAMP),7 which requires 48 hours of instruction over 12 sessions. To create a less time‐intensive learning format for busy hospitalists, the University of Chicago developed Mini‐CHAMP, a streamlined 2‐day workshop with web‐based components for hospitalist clinicians, but not necessarily hospitalist educators.7
We created The Donald W. Reynolds Program for Advancing Geriatrics Education (PAGE) at the University of California, San Francisco (UCSF), in light of the time intensity of CHAMP, to integrate geriatric TTT sessions within preexisting hospitalist faculty meetings. This model is consistent with current practices in faculty development.8 This paper describes the evaluation of the PAGE Model, which sought answers to 3 research questions: (1) Does PAGE increase faculty confidence in teaching geriatrics?, (2) Does PAGE increase the frequency of hospitalist teaching geriatrics topics?, and (3) Does PAGE increase residents' practice of geriatrics skills?
Methods
The PAGE Model
The PAGE Model comprises 10 hour‐long monthly seminars held at UCSF from January through December 2008 to teach specific geriatrics principles and clinical skills relevant to providing competent care to a hospitalized older adult. The aims of the PAGE are to:
Give hospitalist physicians knowledge and skills to teach geriatric topics to trainees in a time‐limited environment
Provide exportable teaching modules on geriatric topics for inpatient teaching
Increase teaching about geriatrics received by internal medicine residents
Increase resident use of 15 specific geriatric skills
Create a collaborative environment between the Geriatrics and Hospital Medicine Divisions at UCSF
The PAGE Development Group, which included 2 hospitalists, 2 geriatricians, and an analyst funded by the Donald W. Reynolds Foundation, reviewed American Geriatrics Society core competencies,9 national guidelines and mandates,10, 11 and existing published geriatric curricula.7, 1214 In late 2007, an email‐based needs assessment listing 38 possible topics, drawn from the resources above, was emailed to the 31 hospitalists at UCSF. Each hospitalist identified, in no particular order, 5 topics considered most useful to improve his/her geriatric teaching skills, with write‐in space for additional topic suggestions. The needs assessment also queried what format of teaching tools would be most useful and efficient, such as PowerPoint slides or pocket cards, and interest in session coteaching.
The topics most commonly selected by the respondents (n = 14, response rate 45%) included: home/community resources (64%), delirium/dementia (57%), minimizing medication problems (50%), using prognostic indices to make decisions (43%), and general approach to older inpatients (43%). The Development Group identified less popular topics (falls, pressure ulcers, indwelling catheters/emncontinence) that were gaining significant national attention.15 Finally, a topic suggested by many hospitalists, pain management, was added. Each topic session was mapped to 1 or more of the 15 geriatrics skills in the CHAMP model7 for residents to acquire. The requested and selected topics were then modified to create distinct sessions grouped around a theme, shown in Table 1. For example home and community resources was addressed in the session on Framework on Transitions in Care.
| Topics | Geriatric Skills Addressed for Hospitalized Older Patients |
|---|---|
| |
| 1. Approach to the vulnerable older patient; assessing function; goals of care | Conduct functional status assessmentMobilize early to prevent deconditioning |
| 2. Minimizing medication problems | Reduce polypharmacy and use of high risk/low benefit drugs |
| 3. Framework for transitions in care (including home and community resources) | Develop a safe and appropriate discharge plan, involving communication with other team members, family members and primary care physicians |
| 4. Using prognostics to guide treatment decisions | Give bad news |
| Document advance directives and DNR orders | |
| Discuss hospice care | |
| 5. Falls & immobility | Identify risk factors of hospital falls, including conventional and unconventional types of restraints |
| 6. Delirium | Assess risk and prevent delirium |
| 7. Dementia & depression | Conduct cognitive assessmentScreen for depression |
| Routinely assess pain at bedside in persons with dementia | |
| 8. Pain assessment in the elderly | Routinely assess pain at bedside in persons with dementia |
| Manage pain using the WHO 3‐step ladder and opiate conversion table and manage side effects of opiates | |
| 9. Foley catheters and incontinence | Determine appropriateness for urinary catheter use, discontinuing when inappropriate |
| 10. Pressure ulcers and wound care | Routinely perform a complete skin exam |
Most respondents (86%) wanted teaching materials in a format suitable for attending rounds; 64% preferred teaching cases, 29% PowerPoint presentations, and 29% quality improvement resources. The Development Group, with approval of the Chief of Hospital Medicine, planned 10, 1‐hour monthly sessions during weekly hospitalist meetings to optimize participation. Nine hospitalists agreed to lead sessions with geriatricians; 1 session was co‐led by a hospitalist and urologist.
The Development Group encouraged session leaders to create case‐based PowerPoint teaching modules that could be used during attending rounds, highlighting teaching triggers or teachable moments that modify or reinforce skills.1618 A Development Group hospitalist/geriatrician team cotaught the first session, which modeled the structure and style recommended. A teaching team typically met at least once to define goals and outline their teaching hour; most met repeatedly to refine their presentations. An example of a 1 PAGE session can be found online.19
Evaluation
Evaluation involved data from hospitalist faculty trainees, hospitalist and geriatrician session leaders, and internal medicine residents. The institutional review board approved this study. Self‐report rating scales were used for data collection, which were reviewed by experts in medical education at UCSF and piloted on nonparticipant faculty, or had been previously used by the CHAMP study.7
Hospitalist Trainees' Program Perceptions and Self‐Efficacy
Hospitalist trainees (n = 36) completed paper questionnaires after each session to assess perceived likelihood to use the teaching tools that were presented (1: not at all likely, 5: highly likely), whether they would recommend the program to colleagues (1: do not recommend, 5: highly recommend), and the utility of the PAGE program (Was this experience useful? and Prior to the sessions, did you think it would be useful? 1: definitely not, 5: definitely yes). Change in trainees' perceived self‐efficacy20 to teach geriatrics skills was assessed at the end of the PAGE program, using a posttest and retrospective pretest format with a 12‐items (1: low, 5: high) that was used in the CHAMP study.7 This format was used to avoid response shift bias, or the program‐produced change in a participant's understanding of the construct being measured.21
Faculty Session Leaders' Program Perceptions
After PAGE completion, all faculty session leaders (n = 15) completed an online questionnaire assessing teaching satisfaction (Likert‐type 5‐point scales), experience with coteaching, and years of faculty teaching experience.
Medical Residents
To assess change in hospitalists' teaching about geriatrics and residents' practice of geriatric clinical skills, residents (n = 56; post‐graduate year (PGY)1 = 29, PGY2 = 27) who would not complete residency before the end of PAGE received an online questionnaire, modified from the CHAMP study,7 prior to and after the completion of PAGE. Respondents received monetary gift cards as incentives. Residents gave separate ratings for their inpatient teaching attendings who were hospitalists (80% of inpatient ward attendings) and nonhospitalists (20%, mostly generalists) regarding frequency over the past year of being taught each of 15 geriatric clinical skills. A 3‐point scale was used: (1) never, (2) once, and (3) more than once. Residents also reported the frequency of practicing those skills themselves, using a questionnaire from the CHAMP study,7 with a scale of (1) never to (5) always.
Analysis
Descriptive statistics were computed for all measures. Scale means were constructed from all individual items for the retrospective pretest and posttest measures. Wilcoxon matched‐pairs signed ranks‐tests were used to compare teaching differences between hospitalist and other attendings. For the unmatched pre‐post data on frequency of teaching, Wilcoxon‐Mann‐Whitney tests were used to determine significant differences in instruction, conducting separate tests for hospitalists and nonhospitalist attendings. Effect size22 was calculated using Cohen's d23 to determine the magnitude of increase in self‐efficacy to teach geriatrics; an effect size exceeding 0.8 is considered large. Statistics were performed using PASW Statistics 17.0 (SPSS Inc., Chicago, IL, USA).
Results
The hospitalist group grew from 31 to 36 members in June of 2008. On average, 14 hospitalists (M = 14.40, standard deviation [SD] = 2.41, range 1119) attended each session, with all hospitalists (n = 36) attending 1 session (M = 3.83, SD = 2.35, range 19). At each session, an average of 72% completed a post‐session evaluation form. Overall, faculty were likely to use the PAGE teaching tools (M = 4.61, SD = 0.53) and would recommend PAGE to other hospitalists (M = 4.63, SD = 0.51).
Thirteen hospitalist trainees of 36 (36%) completed a post‐PAGE online questionnaire. Respondents taught on faculty for an average of 5 years (mean (M) = 5.08, SD = 3.52). Faculty perceived self‐efficacy at teaching residents about geriatrics improved significantly with a large effect size (pretest M = 3.05, SD = .60; posttest M = 3.96, SD = .36, d = 1.52; P < 0.001). Session attendance was positively correlated with the increase in geriatrics teaching self‐efficacy (r = .62, P < 0.05), while teaching experience was not (r = 0.05, P = 0.88). Hospitalist trainees found the PAGE model more useful after participating (M = 4.62, SD = 0.65), than they had expected (M = 3.92, SD = 0.76; P < 0.05).
All session leaders (n = 15) completed the questionnaire after PAGE (9 hospitalists, 5 geriatricians, 1 urologist). Two‐thirds had 5 years on faculty; eight had no prior experience as a faculty development trainer. Over 80% indicated that they found their coteaching experience, enjoyable, useful and collaborative. Only 1 participant did not commit to interdisciplinary teaching again. Most hospitalist session leaders reported that coteaching with a geriatrician enhanced their knowledge; they were more likely to consult a geriatrician regarding patients. All but 2 session leaders felt that the model fostered a collaborative environment between their 2 divisions.
Of the 56 residents, 41% (16 PGY1, 7 PGY2) completed a pretest; 43% (15 PGY1, 9 PGY2) completed a posttest. Residents reported receiving inpatient teaching on geriatrics skills significantly more frequently from hospitalists vs. nonhospitalist attendings both before PAGE (hospitalists M = 2.18, SD = 0.37; nonhospitalists M = 2.00, SD = 0.53, P < 0.05), and after (hospitalists M = 2.39, SD = 0.46; nonhospitalists M = 2.05, SD = 0.57, P < 0.05; see Fig. 1). Although hospitalists taught more frequently about geriatrics than nonhospitalists before PAGE, our findings suggest that they increased their teaching by a greater magnitude than nonhospitalists (P < 0.01, P > 0.05, respectively). Residents reported increased geriatric skill practice after PAGE with a medium effect size (pretest M = 2.92, SD = 0.55, posttest M = 3.28, SD = 0.66, P = 0.052, d = 0.66). There was greater mean reported practice for all skills with the exception of hospice care, which already was being performed between often and very often before PAGE. The largest increases in skill practice were (descending order, most increased first): assessing polypharmacy, performing skin exams, prognostication, performing functional assessments and examining Foley catheter use.
Discussion
Our aging population and a shortage of geriatricians necessitates new, feasible models for geriatric training. Similar to the CHAMP model,7 PAGE had a favorable impact on faculty perceived behavioral change; after the PAGE sessions, faculty reported significantly greater self‐efficacy of teaching geriatrics. However, this study also examined the impact of the PAGE Model on 2 groups not previously reported in the literature: faculty session leaders and medicine residents.
To our knowledge, this is the first study about a hospitalist TTT program codeveloped with nonhospitalists aimed at teaching geriatrics skills to residents, though smaller scale programs for medical students exist.24 We believe codevelopment was important in our model for many reasons. First, using hospitalist peers and local geriatricians likely increased trust in the educational curricula and allowed for strong communication channels between instructors.25, 26 Second, coteaching allowed for hospitalist mentorship. Hospitalists acknowledged their coleaders as mentors and several hospitalists subsequently engaged in new geriatric projects. Third, coteaching was felt to enhance patient care and increase geriatrician consultations. Coteaching may have applicability to other hospitalist faculty development such as intensive care and palliative care, and hospitalist programs may benefit from creating faculty development programs internally with their colleagues, rather than using online resources.
Another important finding of this study is that training hospitalists to teach about geriatrics seems to result in an increase in both the geriatric teaching that residents receive and residents' practice of geriatric skills. This outcome has not been previously demonstrated with geriatric TTT activities.27 This trickle‐down effect to residents likely results from both the increased teaching efficacy of hospitalists after the PAGE Model and the exportable nature of the teaching tools.
Several continuing medical education best practices were used which we believe contributed to the success of PAGE. First, we conducted a needs assessment, which improves knowledge outcomes.28, 29 Second, sessions included cases, lectures, and discussions. Use of multiple educational techniques yields greater knowledge and behavioral change as compared to a single method, such as lecture alone.24, 25, 30, 31 Finally, sessions were sequenced over a year, rather than clustered in short, intensive activity. Sequenced, or learn‐work‐learn opportunities allow education to be translated to practice and reinforced.8, 27, 30, 32
We believe that the PAGE Model is transportable to other hospitalist programs due to its cost and flexible nature. In economically‐lean times, hospitalist divisions can create a program similar to the PAGE Model essentially at no cost, except for donated faculty preparation time. In contrast, CHAMP was expensive, costing nearly $72,000 for 12 faculty to participate in the 48‐hour curriculum,7, 33 and volunteering physicians were compensated for their time. Though Mini‐CHAMP is a streamlined 2‐day workshop that offers free online lectures and slide sets, there may be some benefit to producing a faculty development program internally, as we stated above, and PAGE included additional topics (urinary catheters and decubitus ulcers/wound care) not covered in mini‐CHAMP.
There were several limitations to this study. First, some outcomes of the PAGE Model were assessed by retrospective self‐report, which may allow for recall bias. Although self‐report may or may not correlate with actual behavior,34 faculty and resident perspectives of their teaching and learning experiences are themselves important. Furthermore, a retrospective presurvey allows for content of an educational program or intervention to be explained prior to a survey, so that participants first assess their new level of understanding or skill on the post test, then reflectively assess the level of understanding or skill they had prior to the workshop. This avoids response shift bias and can improve internal validity.21, 35
Second, the small numbers of session leaders, hospitalist trainees, and residents restricted statistical power to detect small effects. The fact that we found significant improvements enhances the likelihood that the differences observed were not due to chance.
Third, the low response rates from the hospitalist trainee post‐intervention questionnaire and the residents' questionnaires may affect the validity of our results. For the resident survey, the subjects were not matched, and we cannot state that an individual's geriatric skill practice changed due to PAGE, though the results suggest the residency program as a whole improved the frequency of geriatric skill practice.
Finally, the residents were required to report the frequency of teaching on and practice of geriatric skills practice over the prior year and accuracy of recall may be an issue. However, frequencies were queried both pre and post intervention and favorable change was noted. Furthermore, because the high end of the 3‐point teaching scale was limited to more than once, the true amount of teaching may have been underestimated if more than once actually represented high frequencies.
Future studies are needed to replicate these findings at other institutions to confirm generalizability. It would be beneficial to measure patient outcomes to determine whether increased teaching and skill practice benefits patients using measures such as reduction in catheter related urinary tract infections, falls, and inadequate pain management. Further investigations of cotaught faculty development programs between hospitalists and other specialists help emphasize why internally created TTT programs are of greater value than online resources.
Conclusions
This time‐sensitive adaptation of a hospitalist geriatric TTT program was successfully implemented at an academic medical center and suggests improved hospitalist faculty self‐efficacy at teaching geriatric skills, increased frequency of inpatient geriatric teaching by hospitalists and increased resident geriatric skill practice. Confidence to care for geriatric patients and a strong skill set to assess risks and manage them appropriately will equip hospitalists and trainees to provide care that reduces geriatric patients' in‐hospital morbidity and costs of care. As hospitalists increasingly care for older adults, the need for time‐efficient methods of teaching geriatrics will continue to grow. The PAGE Model, and other new models of geriatric training for hospitalists, demonstrates that we are beginning to address this urgent need.
Acknowledgements
The authors thank Joan Abrams, MA, MPA, and Patricia O'Sullivan, EdD, whose work was key to the success of this program and this manuscript. They also thank the Donald W. Reynolds Foundation for support of this project.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
- ,.2005 National Hospital Discharge Survey.Adv Data.2007;385:1–19.
- ,,,. In:U.S. Census Bureau, Current Population Reports, 65+ in the United States: 2005,Washington, D.C.:U.S. Government Printing Office;2005:23–209.
- ,,,.Growth in the care of older patients by hospitalists in the United States.N Engl J Med.2009;360(11):1102–1112.
- ,,,.Providing dementia outreach education to rural communities: lessons learned from a train‐the‐trainer program.J Appl Gerontol.2002;21:294–313.
- .Gerontologizing health care: a train‐the‐trainer program for nurses.Gerontol Geriatr Educ.1999;19:47–56.
- ,,.A statewide model detection and prevention program for geriatric alcoholism and alcohol abuse: increased knowledge among service providers.Community Ment Health J.2000;36:137–148.
- ,,, et al.The curriculum for the hospitalized aging medical patient program: a collaborative faculty development program for hospitalists, general internists, and geriatricians.J Hosp Med.2008;3(5):384–393.
- Reframing professional development through understanding authentic professional learning.Rev Educ Res.2009;79:702–739.
- The Education Committee Writing Group of the American Geriatrics Society.Core competencies for the care of older patients: recommendations of the American Geriatrics Society.Acad Med.2000;75:252–255.
- ,,, et al.American Geriatrics Society Task Force on the future of geriatric medicine.J Am Geriatr Soc.2005;53 (6 Suppl):S245–S256.
- Nadzam, Deborah. Preventing patient falls. Joint Commission Resources. Available at: http://www.jcrinc.com/Preventing‐Patient‐Falls. Accessed April2010.
- ,.Curricular recommendations for resident training in nursing home care. A collaborative effort of the Society of General Internal Medicine Task Force on Geriatric Medicine, the Society of Teachers of Family Medicine Geriatrics Task Force, the American Medical Directors Association, and the American Geriatrics Society Education Committee.J Am Geriatr Soc.1994;42:1200–1201.
- ,,,,.Curriculum recommendations for resident training in geriatrics interdisciplinary team care.J Am Geriatr Soc.1999;47:1145–1148.
- ,.ACGME requirements for geriatrics medicine curricula in medical specialties: Progress made and progress needed.Acad Med.2005;80:279–285.
- CMS Office of Public Affairs. CMS Improves Patient Safety for Medicare and Medicaid by Addressing Never Events, August 04, 2008. Available at: http://www.cms.gov/apps/media/press/factsheet.asp?Counter=322434(5):337–343.
- ,.The changing paradigm for continuing medical education: impact of information on the teachable moment.Bull Med Libr Assoc.1990;78(2):173–179.
- ,.Creating the teachable moment.J Nurs Educ.1998;37(6):278–280.
- Society of Hospital Medicine, BOOSTing Care Transitions Resource Room. Mazotti L, Johnston CB. Faculty development: Teaching triggers for transitional care. “A train‐the‐trainer model.” Available at: http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_CareTransitions/PDFs/Mazotti_UCSF_Transitions.PPT. Accessed April2010.
- .Self‐efficacy: The Exercise of Control.New York:W.H. Freeman and Company;1997.
- .Internal invalidity in pretest‐posttest self‐report evaluations and a re‐evaluation of retrospective pretests.Applied Psychological Measurement.1979;3:1–23.
- ,.A visitor's guide to effect sizes.Adv Health Sci Educ Theory Pract.2004;9:241–249.
- .Statistical Power Analyses for the Behavioral Sciences.2nd ed.Hillsdale, NJ:Lawrence Erlbaum Associates;1988.
- ,,,.Hazards of hospitalization: Hospitalists and geriatricians educating medical students about delirium and falls in geriatric patients.Gerontol Geriatr Educ.2008;28(4):94–104.
- ,,, et al.Continuing medical education, continuing professional development, and knowledge translation: Improving care of older patients by practicing physicians.J Am Geriatr Soc.2006:54(10):1610–1618.
- ,,, et al.Practicing physician education in geriatrics: Lessons learned from a train‐the‐trainer model.J Am Geriatr Soc.2007:55(8):1281–1286.
- ,.CHAMP trains champions: hospitalist‐educators develop new ways to teach care for older patients.J Hosp Med.2008;3(5):357–360.
- ,,,,,.Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes?JAMA.1999;282(9):867–874.
- ,.Association for the Study of Medical Education Booklet: The effectiveness of continuing professional development.Edinburgh, Scotland:Association for the Study of Medical Education;2000.
- ,,, et al.Effectiveness of continuing medical education.Evid Rep Technol Assess (Full Rep).2007;149:1–69.
- ,,, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes.Cochrane Database Syst Rev.2009;(2):CD003030.
- ,.Continuing medical education and the physician as learner: guide to the evidence.JAMA.2002;288(9):1057–1060.
- .Care of hospitalized older patients: opportunities for hospital‐based physicians.J Hosp Med.2006;1:42–47.
- ,.What we say and what we do: self‐reported teaching behavior versus performances in written simulations among medical school faculty.Acad Med.1992;67(8):522–527.
- ,.The retrospective pretest and the role of pretest information in evaluation studies.Psychol Rep.1992;70:699–704.
Copyright © 2010 Society of Hospital Medicine
Hospitalist Attendings: Systematic Review
Wachter and Goldman1 described the hospitalist model for inpatient care more than a decade ago. The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.2 This care delivery model has enjoyed exponential growth, with approximately 20,000 hospitalists in the United States, and an estimated 30,000 by the end of the decade.35 Currently, 29% of hospitals, including 55% with at least 200 beds, employ hospitalists to coordinate inpatient care.6 Data suggests that hospitalists promote cost containment and decrease length of stay without negatively affecting rates of death, readmission, or patient satisfaction.715
In academic settings, hospitalists also provide a substantial amount of teaching to trainees,1618 and the hospitalist model represents a fundamental change in inpatient education delivery. Traditional ward attendings typically consisted of a heterogeneous group of subspecialists, laboratory‐based clinician scientists, and general internists, many of whom attended and taught relatively infrequently. By virtue of focusing purely on inpatient care, hospitalists are more intimately involved with inpatient care systems, as well as teaching challenges (and opportunities) in the inpatient setting. The theoretical educational benefits of hospitalists include greater availability, more expertise in hospital medicine, and more emphasis on cost‐effective care.7, 18, 19 Concerns that trainees would have diminished autonomy and less exposure to subspecialist care have not been borne out.16, 20, 21
The purpose of this study was to examine the role of hospitalists on inpatient trainee education. We systematically reviewed the literature to determine the impact of hospitalists compared to nonhospitalist attendings on medical students' and residents' education.
MATERIALS AND METHODS
Data Sources
We searched the MEDLINE, Database of Reviews of Effectiveness (DARE), National Health Service (NHS) Economic Evaluation Database (EED), Health Technology Assessment (HTA), and Cochrane Collaboration databases for citations using the term hospitalist through November 2007, and updated the literature search through October 1, 2008. Additionally, we manually searched the bibliographies of relevant retrieved articles and national meeting abstracts from the SHM (2002‐2007), Society of General Internal Medicine (SGIM) (2001‐2007), and Pediatric Academic Societies (PAS) (2000‐2007). The authors of included meeting abstracts were contacted for additional information.
Data Selection
We included English‐language studies that reported the effects of hospitalist attending physicians on the knowledge, skills, or attitudes of medical students or residents in an inpatient setting, and compared these outcomes to a comparison group of trainees taught by nonhospitalist attending physicians. We excluded opinion articles, review articles, descriptions of curricula, surveys of program leaders, and evaluations of teaching without trainee assessments.
Data Extraction
We developed a standardized data extraction form based on the Best Evidence Medical Education (BEME) Collaboration protocol.22 The following information was extracted from each article: study design and measurement scale; attending and trainee information; study setting; response rate, if available; outcomes measuring attending physician's teaching ability; and outcomes assessing trainees' attitudes, knowledge, and skills. Open‐ended items solicited overall impression, concerns, new insights, and avenues for research not already captured in the data extraction form. A meta‐analysis was not performed due to varying measures for teacher assessments.
One investigator (P.N.) performed the literature search and a second investigator (K.E.H.) reviewed and confirmed the appropriateness of the articles retained and excluded based on review of the titles and abstracts. Next, 3 investigators (P.N., K.E.H., S.R.) confirmed that all the included articles met inclusion criteria. All 3 independently abstracted each article and coded the strength of findings and methodological quality based on: (1) response rate: (2) number of trainees and attendings; (3) control for additional education interventions; (4) explicit indication of random allocation of trainees to attendings; and (5) presence of a contemporaneous comparison group of nonhospitalist attendings. The level of behavioral impact by the 4‐level Kirkpatrick hierarchy was also recorded for each study to assess the strength of the intervention.23 The strength of data was rated for each study on a scale of 1 to 5, with 1 = no clear conclusions can be drawn; 2 = results ambiguous, but appears to be a trend; 3 = conclusions can probably be based on results; 4 = results are clear and very likely to be true; and 5 = results are unequivocal. Disagreements about search criteria, data extraction, and classification of study results were resolved by consensus.
RESULTS
Search Results
The database searches yielded 711 articles (Figure 1). Based on review of titles and abstracts, 32 articles were retrieved for full‐text review. During full‐text review, we eliminated 26 studies because they had no nonhospitalist control group,7, 16, 18, 2427 were opinion or review articles,19, 21, 2834 examined hospitalists' roles without trainee outcomes,17, 3540 surveyed program administration,41 or did not involve hospitalists.42, 43 Ultimately, 6 citations published between 2002 and 2007 met all inclusion criteria (Table 1).4449 The updated literature search through October 1, 2008 did not yield any additional relevant studies.
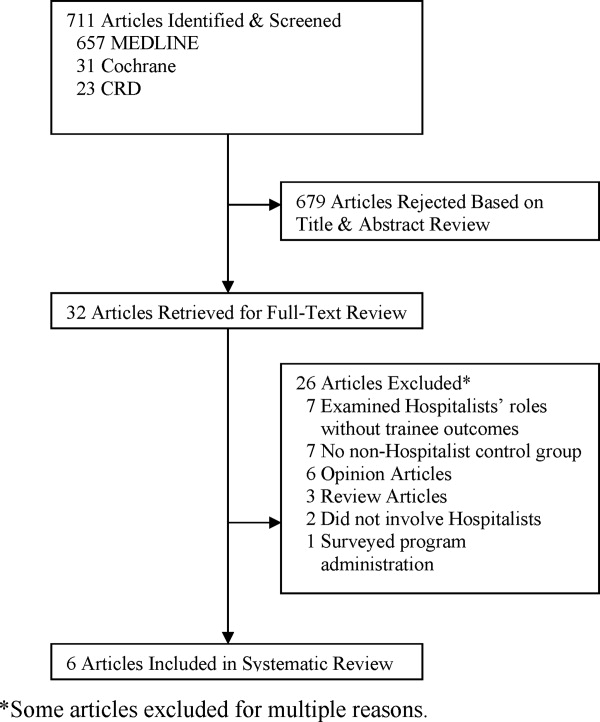
| Location, yearreference | Learners (n) | Number of Attendings | Attending Ward Responsibilities (weeks per year) | Attending Experience (mean years postgraduation) | Attending Gender (% female) | Survey Response Rate (%) | Data Strength |
|---|---|---|---|---|---|---|---|
| |||||||
| University of Chicago, 200244 | PGY‐unspecified (86) | 2‐4 hospitalists; unknown nonhospitalists | 12‐24 hospitalists; 4‐8 nonhospitalists | 58 | 2 | ||
| Children's Hospital, Boston, 200245 | PGY‐1, PGY‐3 (unknown) | 8 hospitalists; 75 nonhospitalists | 12‐16 hospitalists; 2‐4 nonhospitalists | 63 | 2 | ||
| Oregon Health & Sciences, 200446 | MS3 (138) | 6 hospitalists; 11 nonhospitalists | 22.8 hospitalists; 6.4 nonhospitalists | 4.2 hospitalists; 10.9 nonhospitalists | 2/6 (33%) hospitalists; 4/11 (36%) nonhospitalists | 72 | 3 |
| University of California, San Francisco, 200447 | MS3‐4, PGY1‐3 (917) | 17 hospitalists; 39 general internists; 13 subspecialists | 12 hospitalists; 3.24 nonhospitalists | 6/17 (35%) hospitalists; 17/52 (33%) nonhospitalists | 91 | 4 | |
| Grady Memorial, 200448 | MS3‐4, PGY1‐3 (unknown) | 12 hospitalists; 27 general internists; 51 subspecialists | 24 hospitalists; 6 nonhospitalists | 6.1 hospitalists; 9.7 general internists; 21.6 subspecialists | 6/12 (50%) hospitalists; 16/51 (31%) nonhospitalists | 81 | 3 |
| Penn State Children's Hospital, 200749 | MS3 (67) | 2 hospitalists; 8 nonhospitalists | 2 MDs covered 32 hospitalists; 8 MDs covered 28 nonhospitalists | 1/2 (50%) hospitalists; 2/8 (25%) nonhospitalists | 100 | 3 | |
| Multiple sites, 200550* | MS3 (294) | 54 | 2 | ||||
| California Pacific Medical Center, 200651* | PGY‐unspecified (unknown) | 1 | |||||
Examination of meeting abstracts yielded a total of 7,062 abstracts (Figure 2), of which 9 abstracts were retrieved for full‐text review. Two abstracts met inclusion criteria (Table 1).50, 51 Excluded meeting abstracts included published studies that were already abstracted as manuscripts,52, 53 had no nonhospitalist control group,54, 55 did not involve hospitalists,56 surveyed program administrators,57 or examined hospitalists' roles without trainee outcomes.58 Our communications with abstract authors did not yield any relevant additional information.
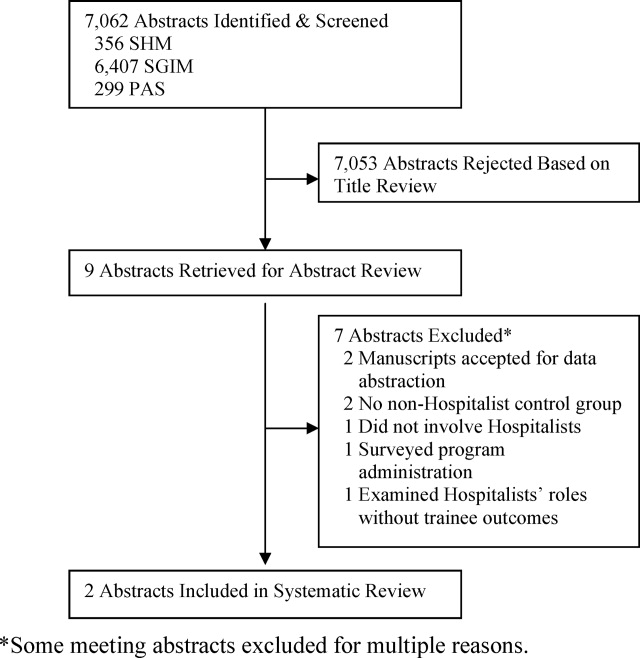
Study Settings, Designs, and Outcomes
Six of 8 included studies occurred in an internal medicine inpatient setting: 4 in university hospitals,44, 46, 47, 50 1 in a public safety‐net hospital,48 and 1 in a community teaching hospital.51 The remaining 2 studied the inpatient pediatric wards in university hospitals.45, 49
In 7 of 8 included studies, trainees were assigned to work with hospitalists or nonhospitalists according to the study site's standard method for allocating trainees to rotations; trainees were not allowed to choose their supervising attending. We considered these studies to be quasirandomized. The other study compared nonhospitalist attending evaluations the year prior to implementing hospitalists to hospitalist attending evaluations the year afterward.45
Studies measured trainee attitudes through routinely administered evaluations,46, 47, 49, 51 dedicated surveys,44, 48, 50 or both.45 One also qualitatively coded trainees' written responses to determine themes.48
Characteristics of Learners
Studies assessed only residents,44, 45, 51 only third‐year medical students,46, 49, 50 or residents and third‐year and fourth‐year medical students.47, 48 The amount of time trainees spent with each attending physician ranged from 2 to 4 weeks. One‐half of the studies reported the number of trainees responding to surveys in each attending group. Two studies had an equivalent number of trainees respond for each attending group,47, 49 while the other 2 had approximately twice as many trainees working with hospitalists respond.46, 50 No studies reported other characteristics of trainees assigned to the different attending groups.
Characteristics of Attendings
Hospitalists were described as attending between 12 and 32 weeks per year while nonhospitalists worked 2 to 12 weeks, except in 1 study where nonhospitalists worked 28 weeks (Table 1).49 Two studies separated nonhospitalists into general internists and subspecialists47, 48 but only 1 contrasted the weeks on service for the 2 groups of nonhospitalists.48 On average, hospitalists tended to be younger and have less experience than nonhospitalist attendings (Table 1). In those reporting attending gender, there was no significant difference between the 2 attending groups.
Methodological Quality
Because all of the included studies only evaluated trainee attitudes, they were all coded as Level 1 by the Kirkpatrick hierarchy for covering learners' views on the learning experience, its organization, presentation, content, teaching methods, and aspects of the instructional organization, materials, quality of instruction.23
The methodological quality of the studies varied. Seven studies used a contemporaneous control group, and 145 employed a noncontemporaneous comparison of hospitalists to nonhospitalists. Seven included studies reported the trainee response rate, which varied widely (from 54% to 100%) (Table 1). None of the studies reported whether any other educational interventions that could have biased study results were implemented during the study period. Of the 6 published studies, the strength of the data for 5 studies was rated as a 2 or 3 and for 1 the strength was rated a 4 (Table 1).
Trainee Evaluations Comparing Hospitalists to All Nonhospitalists
The most commonly evaluated attending measures included trainees' overall satisfaction with attendings (n = 8 studies),4451 trainees' ratings of teaching effectiveness (n = 5 studies),44, 46, 47, 49, 50 attending effectiveness of feedback delivery (n = 4 studies),4548 trainees' perceptions of attending knowledge (n = 3 studies),45, 47, 48 and attending involvement of trainees in patient care decisions (n = 3 studies) (Table 2).44, 45, 47 Several other outcomes were reported in 2 or fewer studies (Table 3). All studies reported nonnormally distributed evaluation ratings, with trainee ratings of all attending groups skewed toward high ratings.
| Number of Studies Evaluated | Hospitalists Better | Nonhospitalists Better | No Difference | |
|---|---|---|---|---|
| ||||
| Overall rating of attending | 8 | 44‐46, 47*, 48‐51 | 47 | |
| Teaching effectiveness | 5 | 44, 48‐50 | 46 | |
| Feedback delivery | 4 | 45, 47*, 48 | 47 | 46 |
| Involvement of trainees in patient care decisions | 3 | 45, 48 | 44 | |
| Quality of ward rounds | 2 | 44, 49 | ||
| Effectiveness as a role model | 2 | 45, 48 | ||
| Communication of rotation goals | 1 | 46 | ||
| Emphasizes evidence‐based care | 1 | 48 | ||
| Emphasizes cost‐effective care | 1 | 47 | ||
| Availability | 2 | 45 | 48 | |
| Perceived knowledge | 3 | 45, 48 | 47 | |
| Bedside teaching | 1 | 45 | ||
| Apparent interest in psychosocial aspects of care | 1 | 47* | 47 | |
| Reference Citation, Location, Year | Study Design | Major Findings | Data Strength |
|---|---|---|---|
| |||
| Chung et al.,44 University of Chicago, 2002 | Retrospective, quasirandomized with contemporaneous controls | % of Internal Medicine house staff very satisfied with Internal Medicine attendings (5‐point scale, 5 = very satisfied): End of month: hospitalist 58%, nonhospitalist 39%; end of year: hospitalists 76%, nonhospitalists 48%. Compared to residents who did not work with hospitalists, residents with experience with hospitalists had fewer concerns about loss of autonomy (8% vs. 41%, P = 0.02), and no difference in concerns about exposure to different faculty (41% vs. 60%, P = 0.08) | 2 |
| Landrigan et al.,45 Children's Hospital, Boston, 2002 | Retrospective, single group with historical control | Overall satisfaction with inpatient experience (4‐point scale, 4 = extremely satisfied): interns, 3.5 with hospitalists, 3.2 with nonhospitalists. PGY3, 3.5 with hospitalists, 3.5 with nonhospitalists. Rating of teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.7, nonhospitalists 4.4. PGY3s reported less ability to make decisions independently, less ability to supervise with hospitalist attendings, but differences did not meet statistical significance (P = 0.07). | 2 |
| Hunter et al.,46 Oregon Health & Sciences, 2004 | Retrospective, quasirandomized with contemporaneous controls | MS3 combined overall rating of attending during Internal Medicine clerkship (9‐point scale, 9 = outstanding): hospitalists 8.56, nonhospitalists 8.22. Combined rating was a composite of 7 parameters (communication of rotation goals, establishing learning climate, use of educational time, teaching style, evaluation and feedback, contribution to growth and development, and effectiveness as clinical teacher). | 3 |
| Hauer et al.,47 University of California, San Francisco, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 overall satisfaction with Internal Medicine attending (9‐point scale, 9 = excellent): hospitalists 8.3 (SD 0.9), nonhospitalist general internists 7.9 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.20 for comparison of hospitalists vs. subspecialists. Attending teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.8 (SD 0.6), general internists 4.5 (SD 0.8), specialists 4.5 (SD 1.1); P 0.001 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.03 for comparison of hospitalists vs. subspecialists. Attending knowledge (9‐point scale): hospitalists 8.2 (SD 1.1), nonhospitalists 7.9 (SD 1.2), subspecialists 8.1 (SD 1.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.10 for comparison of hospitalists vs. subspecialists. Attending valuation of trainee opinions (9‐point scale): hospitalists 8.3 (SD 0.9), nonhospitalist generalists 8.2 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.20 for comparison of hospitalists vs. nonhospitalist generalists; P = 0.60 for comparison of hospitalist vs. subspecialists. Provision of feedback (9‐point scale): hospitalists 7.9 (SD 1.6), nonhospitalist generalists 7.2 (SD 2.3), subspecialists 7.0 (SD 2.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.01 for comparison of hospitalists vs. subspecialists. | 4 |
| Kripalani et al.,48 Grady Memorial, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 satisfaction with Internal Medicine attending teaching effectiveness (25‐item McGill Clinical Tutor Evaluation, maximum score 150): hospitalists 134.5 (95% CI, 130.2‐138.8), general internists 135.0 (95% CI, 131.2‐138.8), specialists 126.3 (95% CI, 120.4‐132.1). | 3 |
| Geskey and Kees‐Folts,49 Penn State Children's Hospital, 2007 | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Pediatric attending teaching (4‐point scale, 4 = excellent), hospitalists 3.9, nonhospitalists 3.0. MS3s rated hospitalists higher than nonhospitalists in all 4 attending characteristics measured: teaching effectiveness, effectiveness as a pediatrician, student advocacy effectiveness, and overall. | 3 |
| Arora et al.,50 Multiple sites, 2005*, | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Internal Medicine clerkship (5‐point scale, 5 = very satisfied): hospitalists 4.5, nonhospitalists 4.3. Trends toward greater emphasis on education (P = 0.07) and higher quality attending rounds (P = 0.07) with hospitalists. Effects of hospitalists on resident perceptions of autonomy not reported. | 2 |
| Chintharajah and Aronowitz,51 California Pacific Medical Center, 2006* | Retrospective, with contemporaneous controls. Method of assignment to attending type not stated. | Internal Medicine house staff ratings of Internal Medicine attendings: Using a 9‐point scale in 1998‐2002, then 5‐point scale in 2003‐2005, Hospitalists were rated higher than nonhospitalists in all areas assessed in 1998‐2002, but were rated higher in only 3 areas in 2003‐2005 (accessibility, feedback, and teaching procedures.) Data not shown. | 1 |
Of the 8 studies comparing hospitalists to all nonhospitalists, trainees were statistically significantly more satisfied with hospitalists in all but 1 (Table 3).4451 Hospitalists' overall teaching effectiveness was rated significantly higher in 4 studies,44, 47, 49, 50 but 1 did not demonstrate a difference.46 Hospitalists were also rated higher at feedback delivery compared to all nonhospitalists, with 2 studies45, 47 and 1 abstract reporting hospitalists' superiority. One other study showed increased satisfaction with hospitalists' feedback only compared to subspecialists.48 Hospitalists were perceived as being more knowledgeable and allowing greater trainee involvement in patient care decisions, in 2 of 3 studies addressing each of these questions. In order to evaluate preconceived notions, 1 study demonstrated that residents who never worked with hospitalists were significantly more concerned about hospitalists negatively impacting their clinical autonomy than residents who had worked with hospitalists at least once.44
Hospitalists were rated as more available in 1 study45 with a trend toward more availability in another.47 Trainee satisfaction was higher with hospitalists on other measures including quality of ward rounds,44, 49 effectiveness as a role model,45, 48 communication of rotations' goals,46 emphasis on evidence‐based medicine,48 and emphasis on cost‐effective care.47 In 1 study, trainees were significantly more satisfied with the bedside teaching of nonhospitalists.45 In another, trainees felt that, compared to hospitalists, general internists seemed to be more interested in the psychosocial aspects of patients' care.48
Trainee Evaluations Comparing Hospitalists to Outpatient Generalists and Subspecialists
Of the studies that examined whether the type of nonhospitalist (general internist vs. subspecialist) impacted trainee ratings, 1 showed that trainees were equally satisfied with hospitalists and general internists but that general internists were rated higher than hospitalists for feedback delivery.48 Hospitalists were rated significantly higher than subspecialists overall and for feedback delivery.48 The other study that subclassified nonhospitalists into general internists and subspecialists showed that hospitalists were more highly rated than both general internists and subspecialists overall and for teaching effectiveness and feedback delivery.47
DISCUSSION
This systematic review of the literature describing hospitalists as educators shows that trainees are generally more satisfied with hospitalists than nonhospitalists on their inpatient rotations. Hospitalists were rated more highly than traditional ward attendings overall, and for teaching effectiveness44, 47, 49, 50 and feedback delivery.45, 47 Limited data (3 studies each) indicates that trainees perceive hospitalists as being at least as knowledgeable as traditional attendings, and encouraging similar levels of trainee involvement in patient care decisions. Trainees may be more satisfied with hospitalists than with general internists or subspecialists, although some comparisons have shown that general internists may be preferred. No studies have evaluated the impact of hospitalists on trainee outcomes beyond satisfaction, such as knowledge acquisition, rotation grades, or clinical performance.
Our review suggests that, with increased time spent on the wards, hospitalists exhibit attributes consistent with specialization in inpatient care.1, 14 Hospitalists were noted to emphasize cost‐effectiveness47 and evidence‐based medicine48 and to conduct higher‐quality ward rounds.44, 49 Hospitalists are uniquely qualified to teach about inpatient goals and processes such as decreasing length of stay in the hospital and cost‐effective care.1, 3, 7, 12, 15 Trainees see hospitalists as role models,45, 47 and the site‐defined nature of hospital medicine promotes trainees' access to hospitalist attendings. Such accessibility has been described as an independent attribute of excellent physician role models,59, 60, 62 Our findings from our methodologically rigorous systematic review of the literature extend the conclusions of a narrative review of the literature on hospitalists as educators that also identified favorable ratings of hospitalists, with some unresolved concerns about resident autonomy and the role of subspecialist teachers in hospitalist systems.63
Diminished trainee autonomy was an early concern about hospitalists in academic medical centers.16, 20, 21 In the earliest study we identified that assessed autonomy, trainees perceived similar amounts of autonomy with hospitalists compared to nonhospitalists.44 Interestingly, house staff in more experienced hospitalist models even described experiencing increased involvement in patient care when supervised by hospitalist attendings in both the pediatric and internal medicine settings.45, 47 Hospitalists might also generate more clinical diversity for house staff by reducing length of stay and thereby enhancing opportunities for learning with newly admitted patients.13, 14, 64
The studies that did not demonstrate increased satisfaction with hospitalists may be instructive as well. One negative study46 reported results from a program that instituted the hospitalist model in response to declining trainee satisfaction. With an emphasis on improving the educational experience, nonhospitalist physicians who were already rated highly as teachers were also selected to attend on the wards. Nonetheless, trainees still were more satisfied with hospitalists overall. One study showed that hospitalists were rated more highly than subspecialists when delivering feedback but less so than general internists.47 The authors suggest that their general internists may have been at a more optimum demographic by being a few more years out of training; such correlations of age and rank to evaluations have not been previously described.60, 61
The disadvantages of hospitalists in trainee education identified by this systematic review include the quality of bedside teaching in one study45 and interest in psychosocial aspects of care in another48 compared to general internists. The decline in satisfaction with bedside teaching is a concern but the comparison was noncontemporaneous and the authors explained that the team size increased and resulted in an overall decrease in time at the bedside.45 The concern that decreased patient length of stays may translate to less time spent with patients and less bedside teaching is not new.18 Although hospitalists have shown particular educational advantages, the balance of clinical efficiency and education remains challenging. Trainees' perception that hospitalists were less interested in the psychosocial aspects of care compared to general internists48 was also anticipated when inpatient attending models began to shift, because hospitalization may now be viewed by trainees as discontinuous from a patient's outpatient care and social situation.18 Nevertheless, hospitalists have been able to achieve such quality measures as decreased length of stay without decreasing patient satisfaction.10, 12
Our study has several limitations. First, all attendings were rated highly in all studies. These high ratings are commonly seen with educational evaluations,65 and this phenomenon creates a ceiling effect that limits variability within the group. Nevertheless, trainees rated hospitalists significantly higher than nonhospitalists overall in all of the included studies. The impact of these small but significant differences on trainees' learning and future clinical performance is unknown. Additionally, the distinction between hospitalists and nonhospitalists was not universal. Initially, it was proposed that academic hospitalists work as hospitalists 3 to 6 months each year.1 This definition is sustained through almost all included studies that reported attending time on the wards, with hospitalists working 3 to 7 months and nonhospitalists working less than 3 months, but observed variability does not permit a universal hospitalist definition. It is possible that publication bias influenced our findings toward positive ratings of hospitalists; we reviewed and included meeting abstracts to minimize this bias. We did not review family medicine meeting abstracts.
The included studies had some methodologic strengths, including quasirandom assignment of trainees and use of a contemporaneous control group in almost all studies. However, the overall methodologic strength was fair given limitations in response rates and reporting of cointerventions; we thus considered most studies to represent trends rather than definitive results. Finally, all of the studies meeting our inclusion criteria to date only evaluated trainees' attitudes and beliefs. Because knowledge and skills were not objectively assessed, it is unclear how increased trainee satisfaction translates to knowledge and skill acquisition on the wards. However, Miller's pyramid and its proposed modification, the Cambridge model, suggest that targeting attitudes precedes knowledge acquisition,66 and our study suggests the need for a research agenda examining the impact of hospitalists on trainees' future performance. Griffith et al.67 demonstrated an association between increased satisfaction with teaching and medical students' performance on clerkship examinations and the U.S. Medical Licensing Examination (USMLE) Step 2.
Overall, trainees were more satisfied with hospitalists' teaching and feedback delivery. Our literature search shows that, although there are a limited number of studies of varying level of quality that cannot be compared using meta‐analytic techniques, the currently available data suggests that hospitalists lead to improved learner satisfaction. More studies to delineate the differences between hospitalists and nonhospitalist general internists are needed. Continued exploration of the effects of attending age and rank on trainee learning may help determine whether this effect is reproducible, and what facets of attendings' teaching actually impact trainees' knowledge, skill acquisition, and behaviors. Since all studies only evaluated attitudes, studies analyzing knowledge and skills are required to more fully understand the educational outcomes of the hospitalist model.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_ Information130:343–349.
- Society of Hospital Medicine. Hospital Medicine Specialty Shows 20 Percent Growth. Available at: http://www.hospitalmedicine.org/AM/Template. cfm?Section=Press_Releases21:1079–1085.
- , , , .The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- , , , , .Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , , , , .Reorganizing an academic medical service. Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , .Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- , , , et al.Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system.Am J Med.2000;108:621–626.
- , , , et al.Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience.Ann Intern Med.1999;130:355–359.
- , , , .The impact of an inpatient physician program on quality, utilization, and satisfaction.Am J Manag Care.2000;6:549–555.
- , , .Decreased length of stay, costs and mortality in a randomized trial of academic hospitalists.J Gen Intern Med.2001;16:S208.
- , , , , , .Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137(11):859–865.
- , , , , , .Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357(25):2589–2600.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- , .The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- , .Implications of the hospitalist model for medical students' education.Acad Med.2001;76:324–330.
- , .Changing teaching for changing times: the effect of a hospitalist program on the education of students.Acad Med.2000;75:521.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- .Response to the effect of hospitalist systems on residency education: re‐incorporating medical subspecialists.Acad Med.2001;76:555–556.
- Best Evidence Medical Education (BEME) Collaboration, Dundee, UK. Home page. Available at: http://www.bemecollaboration.org. Accessed May2009.
- .Evaluation of Training. In: Craig R, Mittel I, eds.Training and Development Handbook.New York:McGraw‐Hill;1967:87–112.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , .Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114(6):1545–1549.
- .How pediatric hospitalist programs can affect graduate medical education.Pediatr Ann.2003;32(12):822–824.
- .A “hospitalist” rotation increases short‐term knowledge of fourth‐year medical students.South Med J.2002;95(3):374.
- .The hospitalist movement 10 years later: life as a Swiss army knife.MedGenMed.2006;8(3):30.
- , , , , .Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- .Hospitalists in medical education: coming to an academic medical center near you.J Natl Med Assoc.2006;98(9):1501–1504.
- , .Teaching residents to consider costs in medical decision making.Am J Bioeth.2006;6(4):33–34.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , .Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1–e7.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- , , , , .The spectrum of community‐based hospitalist practice: a call to tailor internal medicine residency training.Arch Intern Med.2007;167(7):727–728.
- , , , , .How to use the core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(suppl 1):57–67.
- , , , , .Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(suppl 1):48–56.
- , , .How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .Determining the professional attributes of a hospitalist: experience in one Australian metropolitan hospital.Intern Med J.2005;35(5):305–308.
- .The internal medicine clerkship: the view from the vantage point of one chair of medicine.Am J Med.1999;107(2):109–111.
- , , , , .The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- , , , et al.Learning opportunities for Australian prevocational hospital doctors: exposure, perceived quality and desired methods of learning.Med J Aust.2006;184(9):436–440.
- , , , , .Training the ideal hospital doctor: the specialist registrars' perspective.Med Educ.2001;35(10):957–966.
- , , , , , .Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112(7):597–601.
- , , , , , .Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- , , , .Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79(1):78–82.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , .Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- , , , et al. The effects of hospitalist teaching attendings on medical student satisfaction and career interest: results from the multicenter hospitalist study. Society of Hospital Medicine;2005 Annual Meeting Abstracts.
- , . Hospitalist teachers may lose their superiority over non‐hospitalist teachers in “mature” hospitalist systems. Society of General Internal Medicine;2006 Annual Meeting Abstracts.
- , , , . Medical student evaluation of the quality of hospitalist and non‐hospitalist teaching faculty on inpatient medicine rotations. Society of Hospital Medicine;2003 Annual Meeting Abstracts.
- , , , . Effects of hospitalist attendings on trainee satisfaction with rotations. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine and orthopedic residents' perception of education and satisfaction after the initiation of a non‐resident hospitalist service. Society of Hospital Medicine;2004 Annual Meeting Abstracts.
- , , , . Medical subinternship: student experience on a resident uncovered hospitalist service. Society of Hospital Medicine;2006 Annual Meeting Abstracts.
- , , , , . A randomized controlled trial to evaluate the effect of dedicated clinical teachers (or “Educationalists”) on the internal medicine clerkship experience. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine residency program goals drive the development of hospitalist programs at teaching hospitals. Society of Hospital Medicine;2002 Annual Meeting Abstracts.
- , . The role of the hospitalist in teaching. Society of General Internal Medicine;2003 Annual Meeting Abstracts.
- , , .Clinical tutor evaluation: a 5‐year study by students on an inpatient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–54.
- , , , , .Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1992.
- , , .Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- , , , .Attending rounds: a survey of physician attitudes.J Gen Intern Med.1990;5:229–233.
- , .Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75:430–435.
- , , , .Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- , , .Grade inflation in internal medicine clerkships: results of a national survey.Teach Learn Med.2000;12:112–116.
- , , , et al.The relationship between competence and performance: implications for assessing practice performance.Med Educ.2002;36(10):901–909.
- , , .Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances.Acad Med.2000;75(10 suppl):S62–S64.
Wachter and Goldman1 described the hospitalist model for inpatient care more than a decade ago. The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.2 This care delivery model has enjoyed exponential growth, with approximately 20,000 hospitalists in the United States, and an estimated 30,000 by the end of the decade.35 Currently, 29% of hospitals, including 55% with at least 200 beds, employ hospitalists to coordinate inpatient care.6 Data suggests that hospitalists promote cost containment and decrease length of stay without negatively affecting rates of death, readmission, or patient satisfaction.715
In academic settings, hospitalists also provide a substantial amount of teaching to trainees,1618 and the hospitalist model represents a fundamental change in inpatient education delivery. Traditional ward attendings typically consisted of a heterogeneous group of subspecialists, laboratory‐based clinician scientists, and general internists, many of whom attended and taught relatively infrequently. By virtue of focusing purely on inpatient care, hospitalists are more intimately involved with inpatient care systems, as well as teaching challenges (and opportunities) in the inpatient setting. The theoretical educational benefits of hospitalists include greater availability, more expertise in hospital medicine, and more emphasis on cost‐effective care.7, 18, 19 Concerns that trainees would have diminished autonomy and less exposure to subspecialist care have not been borne out.16, 20, 21
The purpose of this study was to examine the role of hospitalists on inpatient trainee education. We systematically reviewed the literature to determine the impact of hospitalists compared to nonhospitalist attendings on medical students' and residents' education.
MATERIALS AND METHODS
Data Sources
We searched the MEDLINE, Database of Reviews of Effectiveness (DARE), National Health Service (NHS) Economic Evaluation Database (EED), Health Technology Assessment (HTA), and Cochrane Collaboration databases for citations using the term hospitalist through November 2007, and updated the literature search through October 1, 2008. Additionally, we manually searched the bibliographies of relevant retrieved articles and national meeting abstracts from the SHM (2002‐2007), Society of General Internal Medicine (SGIM) (2001‐2007), and Pediatric Academic Societies (PAS) (2000‐2007). The authors of included meeting abstracts were contacted for additional information.
Data Selection
We included English‐language studies that reported the effects of hospitalist attending physicians on the knowledge, skills, or attitudes of medical students or residents in an inpatient setting, and compared these outcomes to a comparison group of trainees taught by nonhospitalist attending physicians. We excluded opinion articles, review articles, descriptions of curricula, surveys of program leaders, and evaluations of teaching without trainee assessments.
Data Extraction
We developed a standardized data extraction form based on the Best Evidence Medical Education (BEME) Collaboration protocol.22 The following information was extracted from each article: study design and measurement scale; attending and trainee information; study setting; response rate, if available; outcomes measuring attending physician's teaching ability; and outcomes assessing trainees' attitudes, knowledge, and skills. Open‐ended items solicited overall impression, concerns, new insights, and avenues for research not already captured in the data extraction form. A meta‐analysis was not performed due to varying measures for teacher assessments.
One investigator (P.N.) performed the literature search and a second investigator (K.E.H.) reviewed and confirmed the appropriateness of the articles retained and excluded based on review of the titles and abstracts. Next, 3 investigators (P.N., K.E.H., S.R.) confirmed that all the included articles met inclusion criteria. All 3 independently abstracted each article and coded the strength of findings and methodological quality based on: (1) response rate: (2) number of trainees and attendings; (3) control for additional education interventions; (4) explicit indication of random allocation of trainees to attendings; and (5) presence of a contemporaneous comparison group of nonhospitalist attendings. The level of behavioral impact by the 4‐level Kirkpatrick hierarchy was also recorded for each study to assess the strength of the intervention.23 The strength of data was rated for each study on a scale of 1 to 5, with 1 = no clear conclusions can be drawn; 2 = results ambiguous, but appears to be a trend; 3 = conclusions can probably be based on results; 4 = results are clear and very likely to be true; and 5 = results are unequivocal. Disagreements about search criteria, data extraction, and classification of study results were resolved by consensus.
RESULTS
Search Results
The database searches yielded 711 articles (Figure 1). Based on review of titles and abstracts, 32 articles were retrieved for full‐text review. During full‐text review, we eliminated 26 studies because they had no nonhospitalist control group,7, 16, 18, 2427 were opinion or review articles,19, 21, 2834 examined hospitalists' roles without trainee outcomes,17, 3540 surveyed program administration,41 or did not involve hospitalists.42, 43 Ultimately, 6 citations published between 2002 and 2007 met all inclusion criteria (Table 1).4449 The updated literature search through October 1, 2008 did not yield any additional relevant studies.
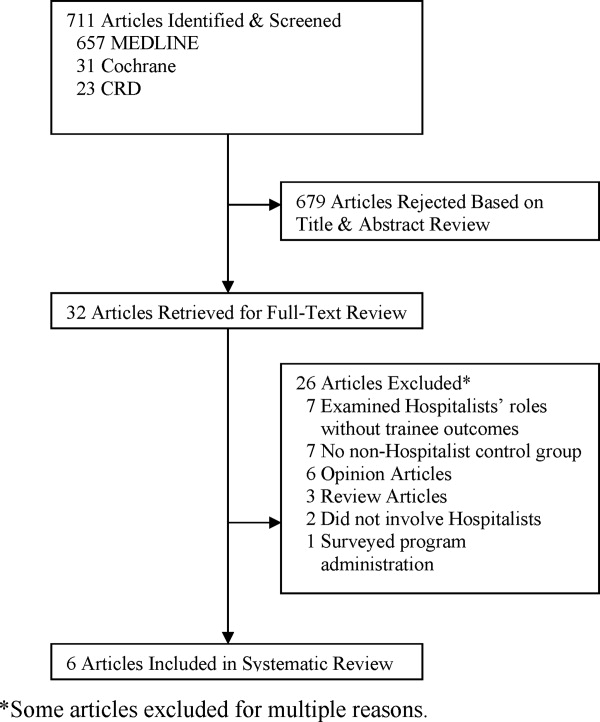
| Location, yearreference | Learners (n) | Number of Attendings | Attending Ward Responsibilities (weeks per year) | Attending Experience (mean years postgraduation) | Attending Gender (% female) | Survey Response Rate (%) | Data Strength |
|---|---|---|---|---|---|---|---|
| |||||||
| University of Chicago, 200244 | PGY‐unspecified (86) | 2‐4 hospitalists; unknown nonhospitalists | 12‐24 hospitalists; 4‐8 nonhospitalists | 58 | 2 | ||
| Children's Hospital, Boston, 200245 | PGY‐1, PGY‐3 (unknown) | 8 hospitalists; 75 nonhospitalists | 12‐16 hospitalists; 2‐4 nonhospitalists | 63 | 2 | ||
| Oregon Health & Sciences, 200446 | MS3 (138) | 6 hospitalists; 11 nonhospitalists | 22.8 hospitalists; 6.4 nonhospitalists | 4.2 hospitalists; 10.9 nonhospitalists | 2/6 (33%) hospitalists; 4/11 (36%) nonhospitalists | 72 | 3 |
| University of California, San Francisco, 200447 | MS3‐4, PGY1‐3 (917) | 17 hospitalists; 39 general internists; 13 subspecialists | 12 hospitalists; 3.24 nonhospitalists | 6/17 (35%) hospitalists; 17/52 (33%) nonhospitalists | 91 | 4 | |
| Grady Memorial, 200448 | MS3‐4, PGY1‐3 (unknown) | 12 hospitalists; 27 general internists; 51 subspecialists | 24 hospitalists; 6 nonhospitalists | 6.1 hospitalists; 9.7 general internists; 21.6 subspecialists | 6/12 (50%) hospitalists; 16/51 (31%) nonhospitalists | 81 | 3 |
| Penn State Children's Hospital, 200749 | MS3 (67) | 2 hospitalists; 8 nonhospitalists | 2 MDs covered 32 hospitalists; 8 MDs covered 28 nonhospitalists | 1/2 (50%) hospitalists; 2/8 (25%) nonhospitalists | 100 | 3 | |
| Multiple sites, 200550* | MS3 (294) | 54 | 2 | ||||
| California Pacific Medical Center, 200651* | PGY‐unspecified (unknown) | 1 | |||||
Examination of meeting abstracts yielded a total of 7,062 abstracts (Figure 2), of which 9 abstracts were retrieved for full‐text review. Two abstracts met inclusion criteria (Table 1).50, 51 Excluded meeting abstracts included published studies that were already abstracted as manuscripts,52, 53 had no nonhospitalist control group,54, 55 did not involve hospitalists,56 surveyed program administrators,57 or examined hospitalists' roles without trainee outcomes.58 Our communications with abstract authors did not yield any relevant additional information.
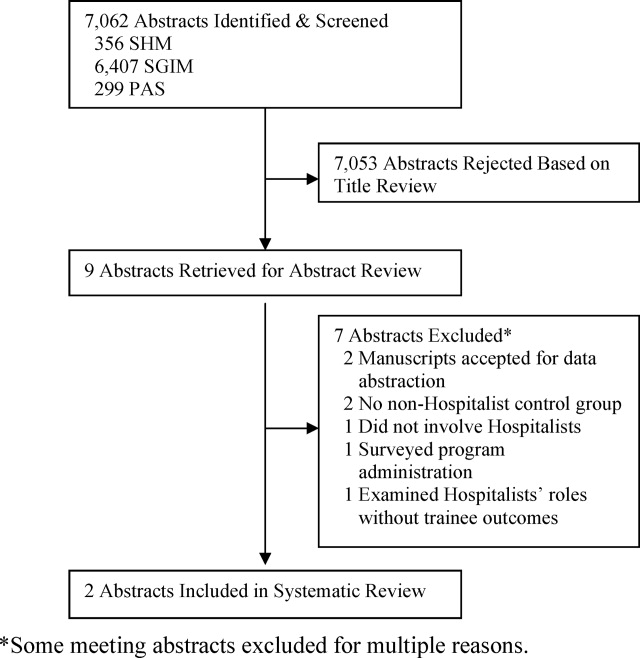
Study Settings, Designs, and Outcomes
Six of 8 included studies occurred in an internal medicine inpatient setting: 4 in university hospitals,44, 46, 47, 50 1 in a public safety‐net hospital,48 and 1 in a community teaching hospital.51 The remaining 2 studied the inpatient pediatric wards in university hospitals.45, 49
In 7 of 8 included studies, trainees were assigned to work with hospitalists or nonhospitalists according to the study site's standard method for allocating trainees to rotations; trainees were not allowed to choose their supervising attending. We considered these studies to be quasirandomized. The other study compared nonhospitalist attending evaluations the year prior to implementing hospitalists to hospitalist attending evaluations the year afterward.45
Studies measured trainee attitudes through routinely administered evaluations,46, 47, 49, 51 dedicated surveys,44, 48, 50 or both.45 One also qualitatively coded trainees' written responses to determine themes.48
Characteristics of Learners
Studies assessed only residents,44, 45, 51 only third‐year medical students,46, 49, 50 or residents and third‐year and fourth‐year medical students.47, 48 The amount of time trainees spent with each attending physician ranged from 2 to 4 weeks. One‐half of the studies reported the number of trainees responding to surveys in each attending group. Two studies had an equivalent number of trainees respond for each attending group,47, 49 while the other 2 had approximately twice as many trainees working with hospitalists respond.46, 50 No studies reported other characteristics of trainees assigned to the different attending groups.
Characteristics of Attendings
Hospitalists were described as attending between 12 and 32 weeks per year while nonhospitalists worked 2 to 12 weeks, except in 1 study where nonhospitalists worked 28 weeks (Table 1).49 Two studies separated nonhospitalists into general internists and subspecialists47, 48 but only 1 contrasted the weeks on service for the 2 groups of nonhospitalists.48 On average, hospitalists tended to be younger and have less experience than nonhospitalist attendings (Table 1). In those reporting attending gender, there was no significant difference between the 2 attending groups.
Methodological Quality
Because all of the included studies only evaluated trainee attitudes, they were all coded as Level 1 by the Kirkpatrick hierarchy for covering learners' views on the learning experience, its organization, presentation, content, teaching methods, and aspects of the instructional organization, materials, quality of instruction.23
The methodological quality of the studies varied. Seven studies used a contemporaneous control group, and 145 employed a noncontemporaneous comparison of hospitalists to nonhospitalists. Seven included studies reported the trainee response rate, which varied widely (from 54% to 100%) (Table 1). None of the studies reported whether any other educational interventions that could have biased study results were implemented during the study period. Of the 6 published studies, the strength of the data for 5 studies was rated as a 2 or 3 and for 1 the strength was rated a 4 (Table 1).
Trainee Evaluations Comparing Hospitalists to All Nonhospitalists
The most commonly evaluated attending measures included trainees' overall satisfaction with attendings (n = 8 studies),4451 trainees' ratings of teaching effectiveness (n = 5 studies),44, 46, 47, 49, 50 attending effectiveness of feedback delivery (n = 4 studies),4548 trainees' perceptions of attending knowledge (n = 3 studies),45, 47, 48 and attending involvement of trainees in patient care decisions (n = 3 studies) (Table 2).44, 45, 47 Several other outcomes were reported in 2 or fewer studies (Table 3). All studies reported nonnormally distributed evaluation ratings, with trainee ratings of all attending groups skewed toward high ratings.
| Number of Studies Evaluated | Hospitalists Better | Nonhospitalists Better | No Difference | |
|---|---|---|---|---|
| ||||
| Overall rating of attending | 8 | 44‐46, 47*, 48‐51 | 47 | |
| Teaching effectiveness | 5 | 44, 48‐50 | 46 | |
| Feedback delivery | 4 | 45, 47*, 48 | 47 | 46 |
| Involvement of trainees in patient care decisions | 3 | 45, 48 | 44 | |
| Quality of ward rounds | 2 | 44, 49 | ||
| Effectiveness as a role model | 2 | 45, 48 | ||
| Communication of rotation goals | 1 | 46 | ||
| Emphasizes evidence‐based care | 1 | 48 | ||
| Emphasizes cost‐effective care | 1 | 47 | ||
| Availability | 2 | 45 | 48 | |
| Perceived knowledge | 3 | 45, 48 | 47 | |
| Bedside teaching | 1 | 45 | ||
| Apparent interest in psychosocial aspects of care | 1 | 47* | 47 | |
| Reference Citation, Location, Year | Study Design | Major Findings | Data Strength |
|---|---|---|---|
| |||
| Chung et al.,44 University of Chicago, 2002 | Retrospective, quasirandomized with contemporaneous controls | % of Internal Medicine house staff very satisfied with Internal Medicine attendings (5‐point scale, 5 = very satisfied): End of month: hospitalist 58%, nonhospitalist 39%; end of year: hospitalists 76%, nonhospitalists 48%. Compared to residents who did not work with hospitalists, residents with experience with hospitalists had fewer concerns about loss of autonomy (8% vs. 41%, P = 0.02), and no difference in concerns about exposure to different faculty (41% vs. 60%, P = 0.08) | 2 |
| Landrigan et al.,45 Children's Hospital, Boston, 2002 | Retrospective, single group with historical control | Overall satisfaction with inpatient experience (4‐point scale, 4 = extremely satisfied): interns, 3.5 with hospitalists, 3.2 with nonhospitalists. PGY3, 3.5 with hospitalists, 3.5 with nonhospitalists. Rating of teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.7, nonhospitalists 4.4. PGY3s reported less ability to make decisions independently, less ability to supervise with hospitalist attendings, but differences did not meet statistical significance (P = 0.07). | 2 |
| Hunter et al.,46 Oregon Health & Sciences, 2004 | Retrospective, quasirandomized with contemporaneous controls | MS3 combined overall rating of attending during Internal Medicine clerkship (9‐point scale, 9 = outstanding): hospitalists 8.56, nonhospitalists 8.22. Combined rating was a composite of 7 parameters (communication of rotation goals, establishing learning climate, use of educational time, teaching style, evaluation and feedback, contribution to growth and development, and effectiveness as clinical teacher). | 3 |
| Hauer et al.,47 University of California, San Francisco, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 overall satisfaction with Internal Medicine attending (9‐point scale, 9 = excellent): hospitalists 8.3 (SD 0.9), nonhospitalist general internists 7.9 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.20 for comparison of hospitalists vs. subspecialists. Attending teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.8 (SD 0.6), general internists 4.5 (SD 0.8), specialists 4.5 (SD 1.1); P 0.001 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.03 for comparison of hospitalists vs. subspecialists. Attending knowledge (9‐point scale): hospitalists 8.2 (SD 1.1), nonhospitalists 7.9 (SD 1.2), subspecialists 8.1 (SD 1.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.10 for comparison of hospitalists vs. subspecialists. Attending valuation of trainee opinions (9‐point scale): hospitalists 8.3 (SD 0.9), nonhospitalist generalists 8.2 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.20 for comparison of hospitalists vs. nonhospitalist generalists; P = 0.60 for comparison of hospitalist vs. subspecialists. Provision of feedback (9‐point scale): hospitalists 7.9 (SD 1.6), nonhospitalist generalists 7.2 (SD 2.3), subspecialists 7.0 (SD 2.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.01 for comparison of hospitalists vs. subspecialists. | 4 |
| Kripalani et al.,48 Grady Memorial, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 satisfaction with Internal Medicine attending teaching effectiveness (25‐item McGill Clinical Tutor Evaluation, maximum score 150): hospitalists 134.5 (95% CI, 130.2‐138.8), general internists 135.0 (95% CI, 131.2‐138.8), specialists 126.3 (95% CI, 120.4‐132.1). | 3 |
| Geskey and Kees‐Folts,49 Penn State Children's Hospital, 2007 | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Pediatric attending teaching (4‐point scale, 4 = excellent), hospitalists 3.9, nonhospitalists 3.0. MS3s rated hospitalists higher than nonhospitalists in all 4 attending characteristics measured: teaching effectiveness, effectiveness as a pediatrician, student advocacy effectiveness, and overall. | 3 |
| Arora et al.,50 Multiple sites, 2005*, | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Internal Medicine clerkship (5‐point scale, 5 = very satisfied): hospitalists 4.5, nonhospitalists 4.3. Trends toward greater emphasis on education (P = 0.07) and higher quality attending rounds (P = 0.07) with hospitalists. Effects of hospitalists on resident perceptions of autonomy not reported. | 2 |
| Chintharajah and Aronowitz,51 California Pacific Medical Center, 2006* | Retrospective, with contemporaneous controls. Method of assignment to attending type not stated. | Internal Medicine house staff ratings of Internal Medicine attendings: Using a 9‐point scale in 1998‐2002, then 5‐point scale in 2003‐2005, Hospitalists were rated higher than nonhospitalists in all areas assessed in 1998‐2002, but were rated higher in only 3 areas in 2003‐2005 (accessibility, feedback, and teaching procedures.) Data not shown. | 1 |
Of the 8 studies comparing hospitalists to all nonhospitalists, trainees were statistically significantly more satisfied with hospitalists in all but 1 (Table 3).4451 Hospitalists' overall teaching effectiveness was rated significantly higher in 4 studies,44, 47, 49, 50 but 1 did not demonstrate a difference.46 Hospitalists were also rated higher at feedback delivery compared to all nonhospitalists, with 2 studies45, 47 and 1 abstract reporting hospitalists' superiority. One other study showed increased satisfaction with hospitalists' feedback only compared to subspecialists.48 Hospitalists were perceived as being more knowledgeable and allowing greater trainee involvement in patient care decisions, in 2 of 3 studies addressing each of these questions. In order to evaluate preconceived notions, 1 study demonstrated that residents who never worked with hospitalists were significantly more concerned about hospitalists negatively impacting their clinical autonomy than residents who had worked with hospitalists at least once.44
Hospitalists were rated as more available in 1 study45 with a trend toward more availability in another.47 Trainee satisfaction was higher with hospitalists on other measures including quality of ward rounds,44, 49 effectiveness as a role model,45, 48 communication of rotations' goals,46 emphasis on evidence‐based medicine,48 and emphasis on cost‐effective care.47 In 1 study, trainees were significantly more satisfied with the bedside teaching of nonhospitalists.45 In another, trainees felt that, compared to hospitalists, general internists seemed to be more interested in the psychosocial aspects of patients' care.48
Trainee Evaluations Comparing Hospitalists to Outpatient Generalists and Subspecialists
Of the studies that examined whether the type of nonhospitalist (general internist vs. subspecialist) impacted trainee ratings, 1 showed that trainees were equally satisfied with hospitalists and general internists but that general internists were rated higher than hospitalists for feedback delivery.48 Hospitalists were rated significantly higher than subspecialists overall and for feedback delivery.48 The other study that subclassified nonhospitalists into general internists and subspecialists showed that hospitalists were more highly rated than both general internists and subspecialists overall and for teaching effectiveness and feedback delivery.47
DISCUSSION
This systematic review of the literature describing hospitalists as educators shows that trainees are generally more satisfied with hospitalists than nonhospitalists on their inpatient rotations. Hospitalists were rated more highly than traditional ward attendings overall, and for teaching effectiveness44, 47, 49, 50 and feedback delivery.45, 47 Limited data (3 studies each) indicates that trainees perceive hospitalists as being at least as knowledgeable as traditional attendings, and encouraging similar levels of trainee involvement in patient care decisions. Trainees may be more satisfied with hospitalists than with general internists or subspecialists, although some comparisons have shown that general internists may be preferred. No studies have evaluated the impact of hospitalists on trainee outcomes beyond satisfaction, such as knowledge acquisition, rotation grades, or clinical performance.
Our review suggests that, with increased time spent on the wards, hospitalists exhibit attributes consistent with specialization in inpatient care.1, 14 Hospitalists were noted to emphasize cost‐effectiveness47 and evidence‐based medicine48 and to conduct higher‐quality ward rounds.44, 49 Hospitalists are uniquely qualified to teach about inpatient goals and processes such as decreasing length of stay in the hospital and cost‐effective care.1, 3, 7, 12, 15 Trainees see hospitalists as role models,45, 47 and the site‐defined nature of hospital medicine promotes trainees' access to hospitalist attendings. Such accessibility has been described as an independent attribute of excellent physician role models,59, 60, 62 Our findings from our methodologically rigorous systematic review of the literature extend the conclusions of a narrative review of the literature on hospitalists as educators that also identified favorable ratings of hospitalists, with some unresolved concerns about resident autonomy and the role of subspecialist teachers in hospitalist systems.63
Diminished trainee autonomy was an early concern about hospitalists in academic medical centers.16, 20, 21 In the earliest study we identified that assessed autonomy, trainees perceived similar amounts of autonomy with hospitalists compared to nonhospitalists.44 Interestingly, house staff in more experienced hospitalist models even described experiencing increased involvement in patient care when supervised by hospitalist attendings in both the pediatric and internal medicine settings.45, 47 Hospitalists might also generate more clinical diversity for house staff by reducing length of stay and thereby enhancing opportunities for learning with newly admitted patients.13, 14, 64
The studies that did not demonstrate increased satisfaction with hospitalists may be instructive as well. One negative study46 reported results from a program that instituted the hospitalist model in response to declining trainee satisfaction. With an emphasis on improving the educational experience, nonhospitalist physicians who were already rated highly as teachers were also selected to attend on the wards. Nonetheless, trainees still were more satisfied with hospitalists overall. One study showed that hospitalists were rated more highly than subspecialists when delivering feedback but less so than general internists.47 The authors suggest that their general internists may have been at a more optimum demographic by being a few more years out of training; such correlations of age and rank to evaluations have not been previously described.60, 61
The disadvantages of hospitalists in trainee education identified by this systematic review include the quality of bedside teaching in one study45 and interest in psychosocial aspects of care in another48 compared to general internists. The decline in satisfaction with bedside teaching is a concern but the comparison was noncontemporaneous and the authors explained that the team size increased and resulted in an overall decrease in time at the bedside.45 The concern that decreased patient length of stays may translate to less time spent with patients and less bedside teaching is not new.18 Although hospitalists have shown particular educational advantages, the balance of clinical efficiency and education remains challenging. Trainees' perception that hospitalists were less interested in the psychosocial aspects of care compared to general internists48 was also anticipated when inpatient attending models began to shift, because hospitalization may now be viewed by trainees as discontinuous from a patient's outpatient care and social situation.18 Nevertheless, hospitalists have been able to achieve such quality measures as decreased length of stay without decreasing patient satisfaction.10, 12
Our study has several limitations. First, all attendings were rated highly in all studies. These high ratings are commonly seen with educational evaluations,65 and this phenomenon creates a ceiling effect that limits variability within the group. Nevertheless, trainees rated hospitalists significantly higher than nonhospitalists overall in all of the included studies. The impact of these small but significant differences on trainees' learning and future clinical performance is unknown. Additionally, the distinction between hospitalists and nonhospitalists was not universal. Initially, it was proposed that academic hospitalists work as hospitalists 3 to 6 months each year.1 This definition is sustained through almost all included studies that reported attending time on the wards, with hospitalists working 3 to 7 months and nonhospitalists working less than 3 months, but observed variability does not permit a universal hospitalist definition. It is possible that publication bias influenced our findings toward positive ratings of hospitalists; we reviewed and included meeting abstracts to minimize this bias. We did not review family medicine meeting abstracts.
The included studies had some methodologic strengths, including quasirandom assignment of trainees and use of a contemporaneous control group in almost all studies. However, the overall methodologic strength was fair given limitations in response rates and reporting of cointerventions; we thus considered most studies to represent trends rather than definitive results. Finally, all of the studies meeting our inclusion criteria to date only evaluated trainees' attitudes and beliefs. Because knowledge and skills were not objectively assessed, it is unclear how increased trainee satisfaction translates to knowledge and skill acquisition on the wards. However, Miller's pyramid and its proposed modification, the Cambridge model, suggest that targeting attitudes precedes knowledge acquisition,66 and our study suggests the need for a research agenda examining the impact of hospitalists on trainees' future performance. Griffith et al.67 demonstrated an association between increased satisfaction with teaching and medical students' performance on clerkship examinations and the U.S. Medical Licensing Examination (USMLE) Step 2.
Overall, trainees were more satisfied with hospitalists' teaching and feedback delivery. Our literature search shows that, although there are a limited number of studies of varying level of quality that cannot be compared using meta‐analytic techniques, the currently available data suggests that hospitalists lead to improved learner satisfaction. More studies to delineate the differences between hospitalists and nonhospitalist general internists are needed. Continued exploration of the effects of attending age and rank on trainee learning may help determine whether this effect is reproducible, and what facets of attendings' teaching actually impact trainees' knowledge, skill acquisition, and behaviors. Since all studies only evaluated attitudes, studies analyzing knowledge and skills are required to more fully understand the educational outcomes of the hospitalist model.
Wachter and Goldman1 described the hospitalist model for inpatient care more than a decade ago. The Society of Hospital Medicine (SHM) defines hospitalists as physicians whose primary professional focus is the general medical care of hospitalized patients. Their activities include patient care, teaching, research, and leadership related to hospital medicine.2 This care delivery model has enjoyed exponential growth, with approximately 20,000 hospitalists in the United States, and an estimated 30,000 by the end of the decade.35 Currently, 29% of hospitals, including 55% with at least 200 beds, employ hospitalists to coordinate inpatient care.6 Data suggests that hospitalists promote cost containment and decrease length of stay without negatively affecting rates of death, readmission, or patient satisfaction.715
In academic settings, hospitalists also provide a substantial amount of teaching to trainees,1618 and the hospitalist model represents a fundamental change in inpatient education delivery. Traditional ward attendings typically consisted of a heterogeneous group of subspecialists, laboratory‐based clinician scientists, and general internists, many of whom attended and taught relatively infrequently. By virtue of focusing purely on inpatient care, hospitalists are more intimately involved with inpatient care systems, as well as teaching challenges (and opportunities) in the inpatient setting. The theoretical educational benefits of hospitalists include greater availability, more expertise in hospital medicine, and more emphasis on cost‐effective care.7, 18, 19 Concerns that trainees would have diminished autonomy and less exposure to subspecialist care have not been borne out.16, 20, 21
The purpose of this study was to examine the role of hospitalists on inpatient trainee education. We systematically reviewed the literature to determine the impact of hospitalists compared to nonhospitalist attendings on medical students' and residents' education.
MATERIALS AND METHODS
Data Sources
We searched the MEDLINE, Database of Reviews of Effectiveness (DARE), National Health Service (NHS) Economic Evaluation Database (EED), Health Technology Assessment (HTA), and Cochrane Collaboration databases for citations using the term hospitalist through November 2007, and updated the literature search through October 1, 2008. Additionally, we manually searched the bibliographies of relevant retrieved articles and national meeting abstracts from the SHM (2002‐2007), Society of General Internal Medicine (SGIM) (2001‐2007), and Pediatric Academic Societies (PAS) (2000‐2007). The authors of included meeting abstracts were contacted for additional information.
Data Selection
We included English‐language studies that reported the effects of hospitalist attending physicians on the knowledge, skills, or attitudes of medical students or residents in an inpatient setting, and compared these outcomes to a comparison group of trainees taught by nonhospitalist attending physicians. We excluded opinion articles, review articles, descriptions of curricula, surveys of program leaders, and evaluations of teaching without trainee assessments.
Data Extraction
We developed a standardized data extraction form based on the Best Evidence Medical Education (BEME) Collaboration protocol.22 The following information was extracted from each article: study design and measurement scale; attending and trainee information; study setting; response rate, if available; outcomes measuring attending physician's teaching ability; and outcomes assessing trainees' attitudes, knowledge, and skills. Open‐ended items solicited overall impression, concerns, new insights, and avenues for research not already captured in the data extraction form. A meta‐analysis was not performed due to varying measures for teacher assessments.
One investigator (P.N.) performed the literature search and a second investigator (K.E.H.) reviewed and confirmed the appropriateness of the articles retained and excluded based on review of the titles and abstracts. Next, 3 investigators (P.N., K.E.H., S.R.) confirmed that all the included articles met inclusion criteria. All 3 independently abstracted each article and coded the strength of findings and methodological quality based on: (1) response rate: (2) number of trainees and attendings; (3) control for additional education interventions; (4) explicit indication of random allocation of trainees to attendings; and (5) presence of a contemporaneous comparison group of nonhospitalist attendings. The level of behavioral impact by the 4‐level Kirkpatrick hierarchy was also recorded for each study to assess the strength of the intervention.23 The strength of data was rated for each study on a scale of 1 to 5, with 1 = no clear conclusions can be drawn; 2 = results ambiguous, but appears to be a trend; 3 = conclusions can probably be based on results; 4 = results are clear and very likely to be true; and 5 = results are unequivocal. Disagreements about search criteria, data extraction, and classification of study results were resolved by consensus.
RESULTS
Search Results
The database searches yielded 711 articles (Figure 1). Based on review of titles and abstracts, 32 articles were retrieved for full‐text review. During full‐text review, we eliminated 26 studies because they had no nonhospitalist control group,7, 16, 18, 2427 were opinion or review articles,19, 21, 2834 examined hospitalists' roles without trainee outcomes,17, 3540 surveyed program administration,41 or did not involve hospitalists.42, 43 Ultimately, 6 citations published between 2002 and 2007 met all inclusion criteria (Table 1).4449 The updated literature search through October 1, 2008 did not yield any additional relevant studies.
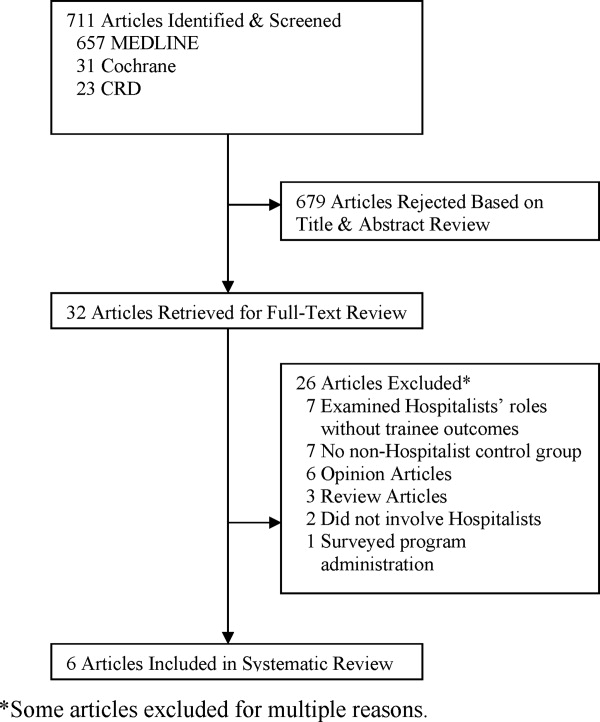
| Location, yearreference | Learners (n) | Number of Attendings | Attending Ward Responsibilities (weeks per year) | Attending Experience (mean years postgraduation) | Attending Gender (% female) | Survey Response Rate (%) | Data Strength |
|---|---|---|---|---|---|---|---|
| |||||||
| University of Chicago, 200244 | PGY‐unspecified (86) | 2‐4 hospitalists; unknown nonhospitalists | 12‐24 hospitalists; 4‐8 nonhospitalists | 58 | 2 | ||
| Children's Hospital, Boston, 200245 | PGY‐1, PGY‐3 (unknown) | 8 hospitalists; 75 nonhospitalists | 12‐16 hospitalists; 2‐4 nonhospitalists | 63 | 2 | ||
| Oregon Health & Sciences, 200446 | MS3 (138) | 6 hospitalists; 11 nonhospitalists | 22.8 hospitalists; 6.4 nonhospitalists | 4.2 hospitalists; 10.9 nonhospitalists | 2/6 (33%) hospitalists; 4/11 (36%) nonhospitalists | 72 | 3 |
| University of California, San Francisco, 200447 | MS3‐4, PGY1‐3 (917) | 17 hospitalists; 39 general internists; 13 subspecialists | 12 hospitalists; 3.24 nonhospitalists | 6/17 (35%) hospitalists; 17/52 (33%) nonhospitalists | 91 | 4 | |
| Grady Memorial, 200448 | MS3‐4, PGY1‐3 (unknown) | 12 hospitalists; 27 general internists; 51 subspecialists | 24 hospitalists; 6 nonhospitalists | 6.1 hospitalists; 9.7 general internists; 21.6 subspecialists | 6/12 (50%) hospitalists; 16/51 (31%) nonhospitalists | 81 | 3 |
| Penn State Children's Hospital, 200749 | MS3 (67) | 2 hospitalists; 8 nonhospitalists | 2 MDs covered 32 hospitalists; 8 MDs covered 28 nonhospitalists | 1/2 (50%) hospitalists; 2/8 (25%) nonhospitalists | 100 | 3 | |
| Multiple sites, 200550* | MS3 (294) | 54 | 2 | ||||
| California Pacific Medical Center, 200651* | PGY‐unspecified (unknown) | 1 | |||||
Examination of meeting abstracts yielded a total of 7,062 abstracts (Figure 2), of which 9 abstracts were retrieved for full‐text review. Two abstracts met inclusion criteria (Table 1).50, 51 Excluded meeting abstracts included published studies that were already abstracted as manuscripts,52, 53 had no nonhospitalist control group,54, 55 did not involve hospitalists,56 surveyed program administrators,57 or examined hospitalists' roles without trainee outcomes.58 Our communications with abstract authors did not yield any relevant additional information.
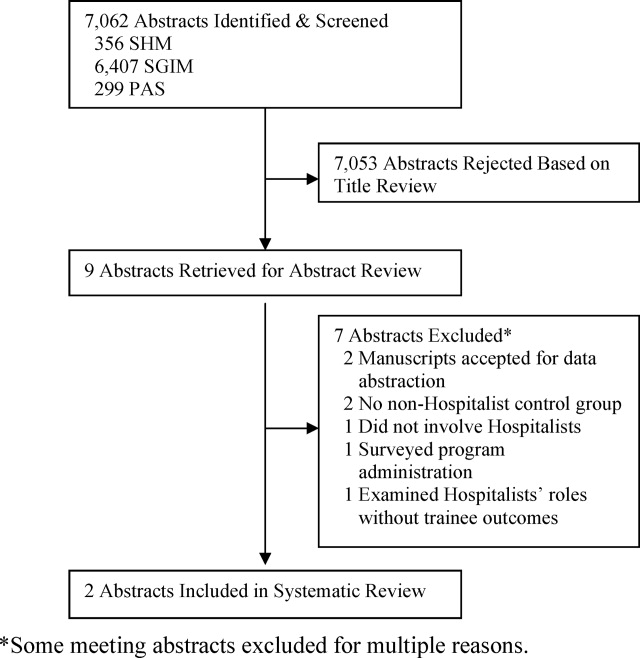
Study Settings, Designs, and Outcomes
Six of 8 included studies occurred in an internal medicine inpatient setting: 4 in university hospitals,44, 46, 47, 50 1 in a public safety‐net hospital,48 and 1 in a community teaching hospital.51 The remaining 2 studied the inpatient pediatric wards in university hospitals.45, 49
In 7 of 8 included studies, trainees were assigned to work with hospitalists or nonhospitalists according to the study site's standard method for allocating trainees to rotations; trainees were not allowed to choose their supervising attending. We considered these studies to be quasirandomized. The other study compared nonhospitalist attending evaluations the year prior to implementing hospitalists to hospitalist attending evaluations the year afterward.45
Studies measured trainee attitudes through routinely administered evaluations,46, 47, 49, 51 dedicated surveys,44, 48, 50 or both.45 One also qualitatively coded trainees' written responses to determine themes.48
Characteristics of Learners
Studies assessed only residents,44, 45, 51 only third‐year medical students,46, 49, 50 or residents and third‐year and fourth‐year medical students.47, 48 The amount of time trainees spent with each attending physician ranged from 2 to 4 weeks. One‐half of the studies reported the number of trainees responding to surveys in each attending group. Two studies had an equivalent number of trainees respond for each attending group,47, 49 while the other 2 had approximately twice as many trainees working with hospitalists respond.46, 50 No studies reported other characteristics of trainees assigned to the different attending groups.
Characteristics of Attendings
Hospitalists were described as attending between 12 and 32 weeks per year while nonhospitalists worked 2 to 12 weeks, except in 1 study where nonhospitalists worked 28 weeks (Table 1).49 Two studies separated nonhospitalists into general internists and subspecialists47, 48 but only 1 contrasted the weeks on service for the 2 groups of nonhospitalists.48 On average, hospitalists tended to be younger and have less experience than nonhospitalist attendings (Table 1). In those reporting attending gender, there was no significant difference between the 2 attending groups.
Methodological Quality
Because all of the included studies only evaluated trainee attitudes, they were all coded as Level 1 by the Kirkpatrick hierarchy for covering learners' views on the learning experience, its organization, presentation, content, teaching methods, and aspects of the instructional organization, materials, quality of instruction.23
The methodological quality of the studies varied. Seven studies used a contemporaneous control group, and 145 employed a noncontemporaneous comparison of hospitalists to nonhospitalists. Seven included studies reported the trainee response rate, which varied widely (from 54% to 100%) (Table 1). None of the studies reported whether any other educational interventions that could have biased study results were implemented during the study period. Of the 6 published studies, the strength of the data for 5 studies was rated as a 2 or 3 and for 1 the strength was rated a 4 (Table 1).
Trainee Evaluations Comparing Hospitalists to All Nonhospitalists
The most commonly evaluated attending measures included trainees' overall satisfaction with attendings (n = 8 studies),4451 trainees' ratings of teaching effectiveness (n = 5 studies),44, 46, 47, 49, 50 attending effectiveness of feedback delivery (n = 4 studies),4548 trainees' perceptions of attending knowledge (n = 3 studies),45, 47, 48 and attending involvement of trainees in patient care decisions (n = 3 studies) (Table 2).44, 45, 47 Several other outcomes were reported in 2 or fewer studies (Table 3). All studies reported nonnormally distributed evaluation ratings, with trainee ratings of all attending groups skewed toward high ratings.
| Number of Studies Evaluated | Hospitalists Better | Nonhospitalists Better | No Difference | |
|---|---|---|---|---|
| ||||
| Overall rating of attending | 8 | 44‐46, 47*, 48‐51 | 47 | |
| Teaching effectiveness | 5 | 44, 48‐50 | 46 | |
| Feedback delivery | 4 | 45, 47*, 48 | 47 | 46 |
| Involvement of trainees in patient care decisions | 3 | 45, 48 | 44 | |
| Quality of ward rounds | 2 | 44, 49 | ||
| Effectiveness as a role model | 2 | 45, 48 | ||
| Communication of rotation goals | 1 | 46 | ||
| Emphasizes evidence‐based care | 1 | 48 | ||
| Emphasizes cost‐effective care | 1 | 47 | ||
| Availability | 2 | 45 | 48 | |
| Perceived knowledge | 3 | 45, 48 | 47 | |
| Bedside teaching | 1 | 45 | ||
| Apparent interest in psychosocial aspects of care | 1 | 47* | 47 | |
| Reference Citation, Location, Year | Study Design | Major Findings | Data Strength |
|---|---|---|---|
| |||
| Chung et al.,44 University of Chicago, 2002 | Retrospective, quasirandomized with contemporaneous controls | % of Internal Medicine house staff very satisfied with Internal Medicine attendings (5‐point scale, 5 = very satisfied): End of month: hospitalist 58%, nonhospitalist 39%; end of year: hospitalists 76%, nonhospitalists 48%. Compared to residents who did not work with hospitalists, residents with experience with hospitalists had fewer concerns about loss of autonomy (8% vs. 41%, P = 0.02), and no difference in concerns about exposure to different faculty (41% vs. 60%, P = 0.08) | 2 |
| Landrigan et al.,45 Children's Hospital, Boston, 2002 | Retrospective, single group with historical control | Overall satisfaction with inpatient experience (4‐point scale, 4 = extremely satisfied): interns, 3.5 with hospitalists, 3.2 with nonhospitalists. PGY3, 3.5 with hospitalists, 3.5 with nonhospitalists. Rating of teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.7, nonhospitalists 4.4. PGY3s reported less ability to make decisions independently, less ability to supervise with hospitalist attendings, but differences did not meet statistical significance (P = 0.07). | 2 |
| Hunter et al.,46 Oregon Health & Sciences, 2004 | Retrospective, quasirandomized with contemporaneous controls | MS3 combined overall rating of attending during Internal Medicine clerkship (9‐point scale, 9 = outstanding): hospitalists 8.56, nonhospitalists 8.22. Combined rating was a composite of 7 parameters (communication of rotation goals, establishing learning climate, use of educational time, teaching style, evaluation and feedback, contribution to growth and development, and effectiveness as clinical teacher). | 3 |
| Hauer et al.,47 University of California, San Francisco, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 overall satisfaction with Internal Medicine attending (9‐point scale, 9 = excellent): hospitalists 8.3 (SD 0.9), nonhospitalist general internists 7.9 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.20 for comparison of hospitalists vs. subspecialists. Attending teaching effectiveness (5‐point scale, 5 = excellent): hospitalists 4.8 (SD 0.6), general internists 4.5 (SD 0.8), specialists 4.5 (SD 1.1); P 0.001 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.03 for comparison of hospitalists vs. subspecialists. Attending knowledge (9‐point scale): hospitalists 8.2 (SD 1.1), nonhospitalists 7.9 (SD 1.2), subspecialists 8.1 (SD 1.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.10 for comparison of hospitalists vs. subspecialists. Attending valuation of trainee opinions (9‐point scale): hospitalists 8.3 (SD 0.9), nonhospitalist generalists 8.2 (SD 1.3), subspecialists 8.1 (SD 1.7); P = 0.20 for comparison of hospitalists vs. nonhospitalist generalists; P = 0.60 for comparison of hospitalist vs. subspecialists. Provision of feedback (9‐point scale): hospitalists 7.9 (SD 1.6), nonhospitalist generalists 7.2 (SD 2.3), subspecialists 7.0 (SD 2.5); P 0.01 for comparison of hospitalists vs. nonhospitalist generalists, P = 0.01 for comparison of hospitalists vs. subspecialists. | 4 |
| Kripalani et al.,48 Grady Memorial, 2004 | Retrospective, quasirandomized with contemporaneous controls | Internal medicine house staff, MS4 and MS3 satisfaction with Internal Medicine attending teaching effectiveness (25‐item McGill Clinical Tutor Evaluation, maximum score 150): hospitalists 134.5 (95% CI, 130.2‐138.8), general internists 135.0 (95% CI, 131.2‐138.8), specialists 126.3 (95% CI, 120.4‐132.1). | 3 |
| Geskey and Kees‐Folts,49 Penn State Children's Hospital, 2007 | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Pediatric attending teaching (4‐point scale, 4 = excellent), hospitalists 3.9, nonhospitalists 3.0. MS3s rated hospitalists higher than nonhospitalists in all 4 attending characteristics measured: teaching effectiveness, effectiveness as a pediatrician, student advocacy effectiveness, and overall. | 3 |
| Arora et al.,50 Multiple sites, 2005*, | Retrospective, quasirandomized with contemporaneous controls | MS3 overall satisfaction with Internal Medicine clerkship (5‐point scale, 5 = very satisfied): hospitalists 4.5, nonhospitalists 4.3. Trends toward greater emphasis on education (P = 0.07) and higher quality attending rounds (P = 0.07) with hospitalists. Effects of hospitalists on resident perceptions of autonomy not reported. | 2 |
| Chintharajah and Aronowitz,51 California Pacific Medical Center, 2006* | Retrospective, with contemporaneous controls. Method of assignment to attending type not stated. | Internal Medicine house staff ratings of Internal Medicine attendings: Using a 9‐point scale in 1998‐2002, then 5‐point scale in 2003‐2005, Hospitalists were rated higher than nonhospitalists in all areas assessed in 1998‐2002, but were rated higher in only 3 areas in 2003‐2005 (accessibility, feedback, and teaching procedures.) Data not shown. | 1 |
Of the 8 studies comparing hospitalists to all nonhospitalists, trainees were statistically significantly more satisfied with hospitalists in all but 1 (Table 3).4451 Hospitalists' overall teaching effectiveness was rated significantly higher in 4 studies,44, 47, 49, 50 but 1 did not demonstrate a difference.46 Hospitalists were also rated higher at feedback delivery compared to all nonhospitalists, with 2 studies45, 47 and 1 abstract reporting hospitalists' superiority. One other study showed increased satisfaction with hospitalists' feedback only compared to subspecialists.48 Hospitalists were perceived as being more knowledgeable and allowing greater trainee involvement in patient care decisions, in 2 of 3 studies addressing each of these questions. In order to evaluate preconceived notions, 1 study demonstrated that residents who never worked with hospitalists were significantly more concerned about hospitalists negatively impacting their clinical autonomy than residents who had worked with hospitalists at least once.44
Hospitalists were rated as more available in 1 study45 with a trend toward more availability in another.47 Trainee satisfaction was higher with hospitalists on other measures including quality of ward rounds,44, 49 effectiveness as a role model,45, 48 communication of rotations' goals,46 emphasis on evidence‐based medicine,48 and emphasis on cost‐effective care.47 In 1 study, trainees were significantly more satisfied with the bedside teaching of nonhospitalists.45 In another, trainees felt that, compared to hospitalists, general internists seemed to be more interested in the psychosocial aspects of patients' care.48
Trainee Evaluations Comparing Hospitalists to Outpatient Generalists and Subspecialists
Of the studies that examined whether the type of nonhospitalist (general internist vs. subspecialist) impacted trainee ratings, 1 showed that trainees were equally satisfied with hospitalists and general internists but that general internists were rated higher than hospitalists for feedback delivery.48 Hospitalists were rated significantly higher than subspecialists overall and for feedback delivery.48 The other study that subclassified nonhospitalists into general internists and subspecialists showed that hospitalists were more highly rated than both general internists and subspecialists overall and for teaching effectiveness and feedback delivery.47
DISCUSSION
This systematic review of the literature describing hospitalists as educators shows that trainees are generally more satisfied with hospitalists than nonhospitalists on their inpatient rotations. Hospitalists were rated more highly than traditional ward attendings overall, and for teaching effectiveness44, 47, 49, 50 and feedback delivery.45, 47 Limited data (3 studies each) indicates that trainees perceive hospitalists as being at least as knowledgeable as traditional attendings, and encouraging similar levels of trainee involvement in patient care decisions. Trainees may be more satisfied with hospitalists than with general internists or subspecialists, although some comparisons have shown that general internists may be preferred. No studies have evaluated the impact of hospitalists on trainee outcomes beyond satisfaction, such as knowledge acquisition, rotation grades, or clinical performance.
Our review suggests that, with increased time spent on the wards, hospitalists exhibit attributes consistent with specialization in inpatient care.1, 14 Hospitalists were noted to emphasize cost‐effectiveness47 and evidence‐based medicine48 and to conduct higher‐quality ward rounds.44, 49 Hospitalists are uniquely qualified to teach about inpatient goals and processes such as decreasing length of stay in the hospital and cost‐effective care.1, 3, 7, 12, 15 Trainees see hospitalists as role models,45, 47 and the site‐defined nature of hospital medicine promotes trainees' access to hospitalist attendings. Such accessibility has been described as an independent attribute of excellent physician role models,59, 60, 62 Our findings from our methodologically rigorous systematic review of the literature extend the conclusions of a narrative review of the literature on hospitalists as educators that also identified favorable ratings of hospitalists, with some unresolved concerns about resident autonomy and the role of subspecialist teachers in hospitalist systems.63
Diminished trainee autonomy was an early concern about hospitalists in academic medical centers.16, 20, 21 In the earliest study we identified that assessed autonomy, trainees perceived similar amounts of autonomy with hospitalists compared to nonhospitalists.44 Interestingly, house staff in more experienced hospitalist models even described experiencing increased involvement in patient care when supervised by hospitalist attendings in both the pediatric and internal medicine settings.45, 47 Hospitalists might also generate more clinical diversity for house staff by reducing length of stay and thereby enhancing opportunities for learning with newly admitted patients.13, 14, 64
The studies that did not demonstrate increased satisfaction with hospitalists may be instructive as well. One negative study46 reported results from a program that instituted the hospitalist model in response to declining trainee satisfaction. With an emphasis on improving the educational experience, nonhospitalist physicians who were already rated highly as teachers were also selected to attend on the wards. Nonetheless, trainees still were more satisfied with hospitalists overall. One study showed that hospitalists were rated more highly than subspecialists when delivering feedback but less so than general internists.47 The authors suggest that their general internists may have been at a more optimum demographic by being a few more years out of training; such correlations of age and rank to evaluations have not been previously described.60, 61
The disadvantages of hospitalists in trainee education identified by this systematic review include the quality of bedside teaching in one study45 and interest in psychosocial aspects of care in another48 compared to general internists. The decline in satisfaction with bedside teaching is a concern but the comparison was noncontemporaneous and the authors explained that the team size increased and resulted in an overall decrease in time at the bedside.45 The concern that decreased patient length of stays may translate to less time spent with patients and less bedside teaching is not new.18 Although hospitalists have shown particular educational advantages, the balance of clinical efficiency and education remains challenging. Trainees' perception that hospitalists were less interested in the psychosocial aspects of care compared to general internists48 was also anticipated when inpatient attending models began to shift, because hospitalization may now be viewed by trainees as discontinuous from a patient's outpatient care and social situation.18 Nevertheless, hospitalists have been able to achieve such quality measures as decreased length of stay without decreasing patient satisfaction.10, 12
Our study has several limitations. First, all attendings were rated highly in all studies. These high ratings are commonly seen with educational evaluations,65 and this phenomenon creates a ceiling effect that limits variability within the group. Nevertheless, trainees rated hospitalists significantly higher than nonhospitalists overall in all of the included studies. The impact of these small but significant differences on trainees' learning and future clinical performance is unknown. Additionally, the distinction between hospitalists and nonhospitalists was not universal. Initially, it was proposed that academic hospitalists work as hospitalists 3 to 6 months each year.1 This definition is sustained through almost all included studies that reported attending time on the wards, with hospitalists working 3 to 7 months and nonhospitalists working less than 3 months, but observed variability does not permit a universal hospitalist definition. It is possible that publication bias influenced our findings toward positive ratings of hospitalists; we reviewed and included meeting abstracts to minimize this bias. We did not review family medicine meeting abstracts.
The included studies had some methodologic strengths, including quasirandom assignment of trainees and use of a contemporaneous control group in almost all studies. However, the overall methodologic strength was fair given limitations in response rates and reporting of cointerventions; we thus considered most studies to represent trends rather than definitive results. Finally, all of the studies meeting our inclusion criteria to date only evaluated trainees' attitudes and beliefs. Because knowledge and skills were not objectively assessed, it is unclear how increased trainee satisfaction translates to knowledge and skill acquisition on the wards. However, Miller's pyramid and its proposed modification, the Cambridge model, suggest that targeting attitudes precedes knowledge acquisition,66 and our study suggests the need for a research agenda examining the impact of hospitalists on trainees' future performance. Griffith et al.67 demonstrated an association between increased satisfaction with teaching and medical students' performance on clerkship examinations and the U.S. Medical Licensing Examination (USMLE) Step 2.
Overall, trainees were more satisfied with hospitalists' teaching and feedback delivery. Our literature search shows that, although there are a limited number of studies of varying level of quality that cannot be compared using meta‐analytic techniques, the currently available data suggests that hospitalists lead to improved learner satisfaction. More studies to delineate the differences between hospitalists and nonhospitalist general internists are needed. Continued exploration of the effects of attending age and rank on trainee learning may help determine whether this effect is reproducible, and what facets of attendings' teaching actually impact trainees' knowledge, skill acquisition, and behaviors. Since all studies only evaluated attitudes, studies analyzing knowledge and skills are required to more fully understand the educational outcomes of the hospitalist model.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_ Information130:343–349.
- Society of Hospital Medicine. Hospital Medicine Specialty Shows 20 Percent Growth. Available at: http://www.hospitalmedicine.org/AM/Template. cfm?Section=Press_Releases21:1079–1085.
- , , , .The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- , , , , .Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , , , , .Reorganizing an academic medical service. Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , .Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- , , , et al.Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system.Am J Med.2000;108:621–626.
- , , , et al.Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience.Ann Intern Med.1999;130:355–359.
- , , , .The impact of an inpatient physician program on quality, utilization, and satisfaction.Am J Manag Care.2000;6:549–555.
- , , .Decreased length of stay, costs and mortality in a randomized trial of academic hospitalists.J Gen Intern Med.2001;16:S208.
- , , , , , .Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137(11):859–865.
- , , , , , .Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357(25):2589–2600.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- , .The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- , .Implications of the hospitalist model for medical students' education.Acad Med.2001;76:324–330.
- , .Changing teaching for changing times: the effect of a hospitalist program on the education of students.Acad Med.2000;75:521.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- .Response to the effect of hospitalist systems on residency education: re‐incorporating medical subspecialists.Acad Med.2001;76:555–556.
- Best Evidence Medical Education (BEME) Collaboration, Dundee, UK. Home page. Available at: http://www.bemecollaboration.org. Accessed May2009.
- .Evaluation of Training. In: Craig R, Mittel I, eds.Training and Development Handbook.New York:McGraw‐Hill;1967:87–112.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , .Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114(6):1545–1549.
- .How pediatric hospitalist programs can affect graduate medical education.Pediatr Ann.2003;32(12):822–824.
- .A “hospitalist” rotation increases short‐term knowledge of fourth‐year medical students.South Med J.2002;95(3):374.
- .The hospitalist movement 10 years later: life as a Swiss army knife.MedGenMed.2006;8(3):30.
- , , , , .Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- .Hospitalists in medical education: coming to an academic medical center near you.J Natl Med Assoc.2006;98(9):1501–1504.
- , .Teaching residents to consider costs in medical decision making.Am J Bioeth.2006;6(4):33–34.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , .Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1–e7.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- , , , , .The spectrum of community‐based hospitalist practice: a call to tailor internal medicine residency training.Arch Intern Med.2007;167(7):727–728.
- , , , , .How to use the core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(suppl 1):57–67.
- , , , , .Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(suppl 1):48–56.
- , , .How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .Determining the professional attributes of a hospitalist: experience in one Australian metropolitan hospital.Intern Med J.2005;35(5):305–308.
- .The internal medicine clerkship: the view from the vantage point of one chair of medicine.Am J Med.1999;107(2):109–111.
- , , , , .The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- , , , et al.Learning opportunities for Australian prevocational hospital doctors: exposure, perceived quality and desired methods of learning.Med J Aust.2006;184(9):436–440.
- , , , , .Training the ideal hospital doctor: the specialist registrars' perspective.Med Educ.2001;35(10):957–966.
- , , , , , .Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112(7):597–601.
- , , , , , .Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- , , , .Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79(1):78–82.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , .Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- , , , et al. The effects of hospitalist teaching attendings on medical student satisfaction and career interest: results from the multicenter hospitalist study. Society of Hospital Medicine;2005 Annual Meeting Abstracts.
- , . Hospitalist teachers may lose their superiority over non‐hospitalist teachers in “mature” hospitalist systems. Society of General Internal Medicine;2006 Annual Meeting Abstracts.
- , , , . Medical student evaluation of the quality of hospitalist and non‐hospitalist teaching faculty on inpatient medicine rotations. Society of Hospital Medicine;2003 Annual Meeting Abstracts.
- , , , . Effects of hospitalist attendings on trainee satisfaction with rotations. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine and orthopedic residents' perception of education and satisfaction after the initiation of a non‐resident hospitalist service. Society of Hospital Medicine;2004 Annual Meeting Abstracts.
- , , , . Medical subinternship: student experience on a resident uncovered hospitalist service. Society of Hospital Medicine;2006 Annual Meeting Abstracts.
- , , , , . A randomized controlled trial to evaluate the effect of dedicated clinical teachers (or “Educationalists”) on the internal medicine clerkship experience. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine residency program goals drive the development of hospitalist programs at teaching hospitals. Society of Hospital Medicine;2002 Annual Meeting Abstracts.
- , . The role of the hospitalist in teaching. Society of General Internal Medicine;2003 Annual Meeting Abstracts.
- , , .Clinical tutor evaluation: a 5‐year study by students on an inpatient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–54.
- , , , , .Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1992.
- , , .Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- , , , .Attending rounds: a survey of physician attitudes.J Gen Intern Med.1990;5:229–233.
- , .Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75:430–435.
- , , , .Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- , , .Grade inflation in internal medicine clerkships: results of a national survey.Teach Learn Med.2000;12:112–116.
- , , , et al.The relationship between competence and performance: implications for assessing practice performance.Med Educ.2002;36(10):901–909.
- , , .Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances.Acad Med.2000;75(10 suppl):S62–S64.
- , .The emerging role of “hospitalists” in the American health care system.N Engl J Med.1996;335:514–517.
- Society of Hospital Medicine. Definition of a Hospitalist. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=General_ Information130:343–349.
- Society of Hospital Medicine. Hospital Medicine Specialty Shows 20 Percent Growth. Available at: http://www.hospitalmedicine.org/AM/Template. cfm?Section=Press_Releases21:1079–1085.
- , , , .The status of hospital medicine groups in the United States.J Hosp Med.2006;1:75–80.
- , , , , .Assessing the value of hospitalists to academic health centers: Brigham and Women's Hospital and Harvard Medical School.Am J Med.1999;106:134–137.
- , , , , .Reorganizing an academic medical service. Impact on cost, quality, patient satisfaction, and education.JAMA.1998;279:1560–1565.
- , .Implications of the hospitalist movement for academic departments of medicine: lessons from the UCSF experience.Am J Med.1999;106:127–133.
- , , , et al.Effects of hospitalists on cost, outcomes, and patient satisfaction in a rural health system.Am J Med.2000;108:621–626.
- , , , et al.Implementation of a hospitalist system in a large health maintenance organization: the Kaiser Permanente experience.Ann Intern Med.1999;130:355–359.
- , , , .The impact of an inpatient physician program on quality, utilization, and satisfaction.Am J Manag Care.2000;6:549–555.
- , , .Decreased length of stay, costs and mortality in a randomized trial of academic hospitalists.J Gen Intern Med.2001;16:S208.
- , , , , , .Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes.Ann Intern Med.2002;137(11):859–865.
- , , , , , .Outcomes of care by hospitalists, general internists, and family physicians.N Engl J Med.2007;357(25):2589–2600.
- .The impact of hospitalists on medical education and the academic health system.Ann Intern Med.1999;130:364–367.
- , .The role of hospitalists in medical education.Am J Med.1999;107:305–309.
- , .Implications of the hospitalist model for medical students' education.Acad Med.2001;76:324–330.
- , .Changing teaching for changing times: the effect of a hospitalist program on the education of students.Acad Med.2000;75:521.
- .Reflections: the hospitalist movement a decade later.J Hosp Med.2006;1(4):248–252.
- .Response to the effect of hospitalist systems on residency education: re‐incorporating medical subspecialists.Acad Med.2001;76:555–556.
- Best Evidence Medical Education (BEME) Collaboration, Dundee, UK. Home page. Available at: http://www.bemecollaboration.org. Accessed May2009.
- .Evaluation of Training. In: Craig R, Mittel I, eds.Training and Development Handbook.New York:McGraw‐Hill;1967:87–112.
- , , , et al.The positive impact of initiation of hospitalist clinician educators.J Gen Intern Med.2004;19(4):293–301.
- , , , .Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114(6):1545–1549.
- .How pediatric hospitalist programs can affect graduate medical education.Pediatr Ann.2003;32(12):822–824.
- .A “hospitalist” rotation increases short‐term knowledge of fourth‐year medical students.South Med J.2002;95(3):374.
- .The hospitalist movement 10 years later: life as a Swiss army knife.MedGenMed.2006;8(3):30.
- , , , , .Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- .Hospitalists in medical education: coming to an academic medical center near you.J Natl Med Assoc.2006;98(9):1501–1504.
- , .Teaching residents to consider costs in medical decision making.Am J Bioeth.2006;6(4):33–34.
- Association of Program Directors in Internal Medicine;, , , , .Redesigning residency education in internal medicine: a position paper from the Association of Program Directors in Internal Medicine.Ann Intern Med.2006;144(12):920–926.
- , , , .Hospital medicine fellowships: works in progress.Am J Med.2006;119(1):72.e1–e7.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- , , , , .The spectrum of community‐based hospitalist practice: a call to tailor internal medicine residency training.Arch Intern Med.2007;167(7):727–728.
- , , , , .How to use the core competencies in hospital medicine: a framework for curriculum development.J Hosp Med.2006;1(suppl 1):57–67.
- , , , , .Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(suppl 1):48–56.
- , , .How hospitalists spend their time: insights on efficiency and safety.J Hosp Med.2006;1(2):88–93.
- .Determining the professional attributes of a hospitalist: experience in one Australian metropolitan hospital.Intern Med J.2005;35(5):305–308.
- .The internal medicine clerkship: the view from the vantage point of one chair of medicine.Am J Med.1999;107(2):109–111.
- , , , , .The presence of hospitalists in medical education.Acad Med.2000;75(10 suppl):S34–S36.
- , , , et al.Learning opportunities for Australian prevocational hospital doctors: exposure, perceived quality and desired methods of learning.Med J Aust.2006;184(9):436–440.
- , , , , .Training the ideal hospital doctor: the specialist registrars' perspective.Med Educ.2001;35(10):957–966.
- , , , , , .Resident satisfaction on an academic hospitalist service: time to teach.Am J Med.2002;112(7):597–601.
- , , , , , .Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- , , , .Medical student evaluation of the quality of hospitalist and nonhospitalist teaching faculty on inpatient medicine rotations.Acad Med.2004;79(1):78–82.
- , , , , .Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations.Arch Intern Med.2004;164(17):1866–1871.
- , , , et al.Hospitalists as teachers.J Gen Intern Med.2004;19(1):8–15.
- , .Third‐year medical students' evaluation of hospitalist and nonhospitalist faculty during the inpatient portion of their pediatrics clerkships.J Hosp Med.2007;2(1):17–22.
- , , , et al. The effects of hospitalist teaching attendings on medical student satisfaction and career interest: results from the multicenter hospitalist study. Society of Hospital Medicine;2005 Annual Meeting Abstracts.
- , . Hospitalist teachers may lose their superiority over non‐hospitalist teachers in “mature” hospitalist systems. Society of General Internal Medicine;2006 Annual Meeting Abstracts.
- , , , . Medical student evaluation of the quality of hospitalist and non‐hospitalist teaching faculty on inpatient medicine rotations. Society of Hospital Medicine;2003 Annual Meeting Abstracts.
- , , , . Effects of hospitalist attendings on trainee satisfaction with rotations. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine and orthopedic residents' perception of education and satisfaction after the initiation of a non‐resident hospitalist service. Society of Hospital Medicine;2004 Annual Meeting Abstracts.
- , , , . Medical subinternship: student experience on a resident uncovered hospitalist service. Society of Hospital Medicine;2006 Annual Meeting Abstracts.
- , , , , . A randomized controlled trial to evaluate the effect of dedicated clinical teachers (or “Educationalists”) on the internal medicine clerkship experience. Society of General Internal Medicine;2002 Annual Meeting Abstracts.
- , , . Internal medicine residency program goals drive the development of hospitalist programs at teaching hospitals. Society of Hospital Medicine;2002 Annual Meeting Abstracts.
- , . The role of the hospitalist in teaching. Society of General Internal Medicine;2003 Annual Meeting Abstracts.
- , , .Clinical tutor evaluation: a 5‐year study by students on an inpatient service and residents in an ambulatory care clinic.Med Educ.1993;27:48–54.
- , , , , .Attributes of excellent attending‐physician role models.N Engl J Med.1998;339:1986–1992.
- , , .Factors affecting ratings of clinical teachers by medical students and residents.J Med Educ.1987;62:1–7.
- , , , .Attending rounds: a survey of physician attitudes.J Gen Intern Med.1990;5:229–233.
- , .Hospitalist educators: future of inpatient internal medicine training.Mt Sinai J Med.2008;75:430–435.
- , , , .Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117:1736–1744.
- , , .Grade inflation in internal medicine clerkships: results of a national survey.Teach Learn Med.2000;12:112–116.
- , , , et al.The relationship between competence and performance: implications for assessing practice performance.Med Educ.2002;36(10):901–909.
- , , .Six‐year documentation of the association between excellent clinical teaching and improved students' examination performances.Acad Med.2000;75(10 suppl):S62–S64.
Editorial
Older Americans comprise approximately half the patients on inpatient medical wards. There are too few geriatricians to care for these patients, and few geriatricians practice hospital medicine. Hospitalists often provide the majority of inpatient geriatric care, and at teaching hospitals, hospitalists also play a pivotal role in educating residents and students to provide high‐quality care for hospitalized geriatric patients. Thus, hospitalists will be the primary clinicians educating many trainees to care for older patients, and the hospitalists must be skilled in addressing the clinical syndromes that are common in these patients, including delirium, dementia, falls, and infection.1 Generalists and geriatricians have anticipated a shortfall in clinicians prepared to educate trainees about geriatrics and called for faculty development for generalists in geriatrics.2, 3
In this issue of the Journal of Hospital Medicine, Podrazik and colleagues present initial results from a major initiative to enhance the quality and quantity of geriatric inpatient education for residents and students.4 The Curriculum for the Hospitalized Aging Medical Patient (CHAMP) at the University of Chicago represents a multifaceted faculty development effort funded in part by the Donald W. Reynolds and John A. Hartford Foundations. In 12 half‐day sessions offered weekly, hospitalist and general internist faculty members learned about four thematic areasthe frail older person, hazards of hospitalization, end‐of‐life issues, and transitions of carewhile also receiving training in engaging and effective teaching strategies. At each session, participants drew on their own experiences attending on the wards to generate clinical examples and test new teaching strategies. CHAMP incorporates the attributes of best practices for integrating geriatrics education into internal medicine residency training: it promotes model care for older hospital patients, uses a train‐the‐trainer model, addresses care transitions, and promotes interdisciplinary teamwork.5
CHAMP achieved its initial goals. Faculty participants were satisfied and CHAMP substantially increased participants' confidence in practicing and teaching geriatric care. Faculty participants also gained confidence in their teaching abilities and presumably learned teaching strategies that could be applied to other topics in inpatient medicine. Faculty participants demonstrated modest improvements in their knowledge of geriatric issues and more positive attitudes about geriatrics at the end of the course than at the beginning. It is worth noting that the hospitalist and general internist ward attending physicians who participated in CHAMP were volunteers and may have started the process with greater interest in learning geriatric care than other attendings. Thus, it is unknown whether CHAMP might have greater or lesser effect on other faculty.
The CHAMP train‐the‐trainer model offers the potential to impact future practitioners. Findings of the CHAMP investigators are consistent with the literature on faculty development programs for educators, which shows that faculty development on teaching yields high participant satisfaction, knowledge gains, and improved self‐assessment of the ability to implement changes in teaching practice.6 The use in CHAMP of a diverse menu of teaching strategies and active learning techniques such as case‐based discussions and the Objective Structured Teaching Exercise in a small group of colleagues should promote learning and retention.
Is the CHAMP curriculum worth the cost? The program requires resources to pay for 48 hours for each faculty participant and for instructors with expertise in geriatrics and teaching skills. We estimate that the cost for 12 faculty participants would be roughly $72,000. We believe this investment will likely pay off in terms of enhancing faculty skills, improving faculty job satisfaction, promoting faculty retention in academic or other teaching positions, and improving care provided by trainees. For example, if CHAMP were to lead to the retention and promotion of even 2 faculty for just 1 year, it would save recruitment costs that would exceed the direct program costs, and other benefits of CHAMP would only further add value. However, analysis of the benefits of CHAMP will require more in‐depth evaluation data of its impact. The program leaders currently contact former participants around the time of ward attending to reinforce teaching concepts and encourage implementation of CHAMP materials, through a Commitment to Change contract. The ultimate downstream educational goal would be that these faculty learners retain and apply this newly acquired knowledge and skills in their clinical practice and teaching activities. Ideally, evidence would confirm that these benefits improve patient care. The long‐term evaluation plan for CHAMP incorporates important additional outcome measures including resident and student geriatric knowledge as well as patient satisfaction and clinical outcomes. We commend the authors for aiming to expand their evaluation plan over time and aspiring for sustained changes in teaching practice. The literature on the impact of hospitalists has similarly evolved from early descriptions of hospitalists and the logistics of developing a hospitalist program to sophisticated analyses of the impact of hospitalists on clinical outcomes such as length of stay and mortality.7, 8
The feasibility of disseminating CHAMP is an open question. The University of Chicago model employs a time‐intensive curriculum that engages participants in part by releasing them from clinical duties for a half day per week. Release time was funded through combined support from external funding sources and the Department of Medicine. This model addresses the major barrier to faculty development in geriatrics for general internists: lack of time.2, 9 The investment in intensive, longitudinal faculty development may generate higher returns than periodic short faculty workshop sessions that do not build in the time for role‐playing, practice, and reinforcement of key concepts. This type of intervention may also be more feasible when done in conjunction with one of the approximately 50 Health Resources and Services Administration (HRSA)supported Geriatrics Education Centers, which can fund teachers and infrastructure for faculty development.
How is this article useful for hospitalist educators? Many hospitalists at academic centers serve important teaching functions, and some will aspire to advance their educational efforts through more scholarly activities such as curriculum design. The CHAMP curriculum represents a successful model for hospitalists aiming to follow a rigorous approach to curriculum design relevant to inpatient medicine, and the extensive CHAMP materials are available online.10 It serves as a practical model that could be applied to other clinical topics related to hospital medicine. Hospitalists are effective and respected teachers for residents and students, and they develop unique expertise in the content and process of inpatient medicine.11 The authors followed the 6 steps of effective curriculum design: problem identification, targeted needs assessment, goals and objectives, education methods, implementation, and evaluation.12
The CHAMP curriculum typifies a set of materials that aligns well with the Society of Hospital Medicine (SHM) Core Competencies.13 As part of their needs assessment, the authors also surveyed hospitalists at a regional SHM meeting to determine the geriatrics topics for which they perceived greatest educational need. The Core Competencies chapters on the care of the elderly patient, delirium and dementia, hospital‐acquired infections, and palliative care highlight the common learning goals shared by hospital medicine and geriatrics. Both disciplines also emphasize the team‐based, multidisciplinary approach to care, particularly during care transitions, that is highlighted in the CHAMP curriculum.
More generally, the CHAMP curriculum can be used to teach and assess the Accreditation Council for Graduate Medical Education (ACGME) competencies, which must be assessed in all ACGME‐accredited residency programs.14 In an initial session on Teaching on Today's Wards, CHAMP participants brainstorm about how to incorporate both geriatrics content and the ACGME competencies into their post‐call rounds. The emphasis in CHAMP on the health care system and interdisciplinary care is evident in topics such as end‐of‐life care and transitions in care, and provides opportunity for assessment of residents' performance in the ACGME competency of systems‐based practice. The organization of the curriculum by ACGME competency makes it more applicable today than some prior geriatric curricula that emphasized similar themes but without the emphasis on demonstrating competency as an outcome.15
Hospitalists partnering with the Donald W. Reynolds and John A. Hartford Foundations and other external organizations may find funding opportunities for educational projects. For example, the Hartford Foundation has partnered with SHM since 2002 to support hospitalists' efforts to improve care for older adults. Products of this collaboration include a Geriatric Toolbox that contains assessment tools designed for use with geriatric patients.16 The tools assess a range of parameters including nutritional, functional, and mental status, and the website supplies guidelines on the advantages and disadvantages and appropriate use of each assessment tool. With support from the Hartford Foundation, hospitalists have also conducted several workshops at SHM meetings on improving assessment and care of geriatric patients and developed a discharge‐planning checklist for older adults.
As hospitalist programs gain traction in academic centers, hospitalists will increasingly serve as key geriatric content educators for trainees. The CHAMP curriculum offers a model of intensive faculty development for hospitalists and general internists that clinician educators find engaging and empowering. The partnerships of geriatricians and hospitalists, and of the SHM with national geriatrics organizations, have the potential for widespread benefits for both learners and elderly patients.
Older Americans comprise approximately half the patients on inpatient medical wards. There are too few geriatricians to care for these patients, and few geriatricians practice hospital medicine. Hospitalists often provide the majority of inpatient geriatric care, and at teaching hospitals, hospitalists also play a pivotal role in educating residents and students to provide high‐quality care for hospitalized geriatric patients. Thus, hospitalists will be the primary clinicians educating many trainees to care for older patients, and the hospitalists must be skilled in addressing the clinical syndromes that are common in these patients, including delirium, dementia, falls, and infection.1 Generalists and geriatricians have anticipated a shortfall in clinicians prepared to educate trainees about geriatrics and called for faculty development for generalists in geriatrics.2, 3
In this issue of the Journal of Hospital Medicine, Podrazik and colleagues present initial results from a major initiative to enhance the quality and quantity of geriatric inpatient education for residents and students.4 The Curriculum for the Hospitalized Aging Medical Patient (CHAMP) at the University of Chicago represents a multifaceted faculty development effort funded in part by the Donald W. Reynolds and John A. Hartford Foundations. In 12 half‐day sessions offered weekly, hospitalist and general internist faculty members learned about four thematic areasthe frail older person, hazards of hospitalization, end‐of‐life issues, and transitions of carewhile also receiving training in engaging and effective teaching strategies. At each session, participants drew on their own experiences attending on the wards to generate clinical examples and test new teaching strategies. CHAMP incorporates the attributes of best practices for integrating geriatrics education into internal medicine residency training: it promotes model care for older hospital patients, uses a train‐the‐trainer model, addresses care transitions, and promotes interdisciplinary teamwork.5
CHAMP achieved its initial goals. Faculty participants were satisfied and CHAMP substantially increased participants' confidence in practicing and teaching geriatric care. Faculty participants also gained confidence in their teaching abilities and presumably learned teaching strategies that could be applied to other topics in inpatient medicine. Faculty participants demonstrated modest improvements in their knowledge of geriatric issues and more positive attitudes about geriatrics at the end of the course than at the beginning. It is worth noting that the hospitalist and general internist ward attending physicians who participated in CHAMP were volunteers and may have started the process with greater interest in learning geriatric care than other attendings. Thus, it is unknown whether CHAMP might have greater or lesser effect on other faculty.
The CHAMP train‐the‐trainer model offers the potential to impact future practitioners. Findings of the CHAMP investigators are consistent with the literature on faculty development programs for educators, which shows that faculty development on teaching yields high participant satisfaction, knowledge gains, and improved self‐assessment of the ability to implement changes in teaching practice.6 The use in CHAMP of a diverse menu of teaching strategies and active learning techniques such as case‐based discussions and the Objective Structured Teaching Exercise in a small group of colleagues should promote learning and retention.
Is the CHAMP curriculum worth the cost? The program requires resources to pay for 48 hours for each faculty participant and for instructors with expertise in geriatrics and teaching skills. We estimate that the cost for 12 faculty participants would be roughly $72,000. We believe this investment will likely pay off in terms of enhancing faculty skills, improving faculty job satisfaction, promoting faculty retention in academic or other teaching positions, and improving care provided by trainees. For example, if CHAMP were to lead to the retention and promotion of even 2 faculty for just 1 year, it would save recruitment costs that would exceed the direct program costs, and other benefits of CHAMP would only further add value. However, analysis of the benefits of CHAMP will require more in‐depth evaluation data of its impact. The program leaders currently contact former participants around the time of ward attending to reinforce teaching concepts and encourage implementation of CHAMP materials, through a Commitment to Change contract. The ultimate downstream educational goal would be that these faculty learners retain and apply this newly acquired knowledge and skills in their clinical practice and teaching activities. Ideally, evidence would confirm that these benefits improve patient care. The long‐term evaluation plan for CHAMP incorporates important additional outcome measures including resident and student geriatric knowledge as well as patient satisfaction and clinical outcomes. We commend the authors for aiming to expand their evaluation plan over time and aspiring for sustained changes in teaching practice. The literature on the impact of hospitalists has similarly evolved from early descriptions of hospitalists and the logistics of developing a hospitalist program to sophisticated analyses of the impact of hospitalists on clinical outcomes such as length of stay and mortality.7, 8
The feasibility of disseminating CHAMP is an open question. The University of Chicago model employs a time‐intensive curriculum that engages participants in part by releasing them from clinical duties for a half day per week. Release time was funded through combined support from external funding sources and the Department of Medicine. This model addresses the major barrier to faculty development in geriatrics for general internists: lack of time.2, 9 The investment in intensive, longitudinal faculty development may generate higher returns than periodic short faculty workshop sessions that do not build in the time for role‐playing, practice, and reinforcement of key concepts. This type of intervention may also be more feasible when done in conjunction with one of the approximately 50 Health Resources and Services Administration (HRSA)supported Geriatrics Education Centers, which can fund teachers and infrastructure for faculty development.
How is this article useful for hospitalist educators? Many hospitalists at academic centers serve important teaching functions, and some will aspire to advance their educational efforts through more scholarly activities such as curriculum design. The CHAMP curriculum represents a successful model for hospitalists aiming to follow a rigorous approach to curriculum design relevant to inpatient medicine, and the extensive CHAMP materials are available online.10 It serves as a practical model that could be applied to other clinical topics related to hospital medicine. Hospitalists are effective and respected teachers for residents and students, and they develop unique expertise in the content and process of inpatient medicine.11 The authors followed the 6 steps of effective curriculum design: problem identification, targeted needs assessment, goals and objectives, education methods, implementation, and evaluation.12
The CHAMP curriculum typifies a set of materials that aligns well with the Society of Hospital Medicine (SHM) Core Competencies.13 As part of their needs assessment, the authors also surveyed hospitalists at a regional SHM meeting to determine the geriatrics topics for which they perceived greatest educational need. The Core Competencies chapters on the care of the elderly patient, delirium and dementia, hospital‐acquired infections, and palliative care highlight the common learning goals shared by hospital medicine and geriatrics. Both disciplines also emphasize the team‐based, multidisciplinary approach to care, particularly during care transitions, that is highlighted in the CHAMP curriculum.
More generally, the CHAMP curriculum can be used to teach and assess the Accreditation Council for Graduate Medical Education (ACGME) competencies, which must be assessed in all ACGME‐accredited residency programs.14 In an initial session on Teaching on Today's Wards, CHAMP participants brainstorm about how to incorporate both geriatrics content and the ACGME competencies into their post‐call rounds. The emphasis in CHAMP on the health care system and interdisciplinary care is evident in topics such as end‐of‐life care and transitions in care, and provides opportunity for assessment of residents' performance in the ACGME competency of systems‐based practice. The organization of the curriculum by ACGME competency makes it more applicable today than some prior geriatric curricula that emphasized similar themes but without the emphasis on demonstrating competency as an outcome.15
Hospitalists partnering with the Donald W. Reynolds and John A. Hartford Foundations and other external organizations may find funding opportunities for educational projects. For example, the Hartford Foundation has partnered with SHM since 2002 to support hospitalists' efforts to improve care for older adults. Products of this collaboration include a Geriatric Toolbox that contains assessment tools designed for use with geriatric patients.16 The tools assess a range of parameters including nutritional, functional, and mental status, and the website supplies guidelines on the advantages and disadvantages and appropriate use of each assessment tool. With support from the Hartford Foundation, hospitalists have also conducted several workshops at SHM meetings on improving assessment and care of geriatric patients and developed a discharge‐planning checklist for older adults.
As hospitalist programs gain traction in academic centers, hospitalists will increasingly serve as key geriatric content educators for trainees. The CHAMP curriculum offers a model of intensive faculty development for hospitalists and general internists that clinician educators find engaging and empowering. The partnerships of geriatricians and hospitalists, and of the SHM with national geriatrics organizations, have the potential for widespread benefits for both learners and elderly patients.
Older Americans comprise approximately half the patients on inpatient medical wards. There are too few geriatricians to care for these patients, and few geriatricians practice hospital medicine. Hospitalists often provide the majority of inpatient geriatric care, and at teaching hospitals, hospitalists also play a pivotal role in educating residents and students to provide high‐quality care for hospitalized geriatric patients. Thus, hospitalists will be the primary clinicians educating many trainees to care for older patients, and the hospitalists must be skilled in addressing the clinical syndromes that are common in these patients, including delirium, dementia, falls, and infection.1 Generalists and geriatricians have anticipated a shortfall in clinicians prepared to educate trainees about geriatrics and called for faculty development for generalists in geriatrics.2, 3
In this issue of the Journal of Hospital Medicine, Podrazik and colleagues present initial results from a major initiative to enhance the quality and quantity of geriatric inpatient education for residents and students.4 The Curriculum for the Hospitalized Aging Medical Patient (CHAMP) at the University of Chicago represents a multifaceted faculty development effort funded in part by the Donald W. Reynolds and John A. Hartford Foundations. In 12 half‐day sessions offered weekly, hospitalist and general internist faculty members learned about four thematic areasthe frail older person, hazards of hospitalization, end‐of‐life issues, and transitions of carewhile also receiving training in engaging and effective teaching strategies. At each session, participants drew on their own experiences attending on the wards to generate clinical examples and test new teaching strategies. CHAMP incorporates the attributes of best practices for integrating geriatrics education into internal medicine residency training: it promotes model care for older hospital patients, uses a train‐the‐trainer model, addresses care transitions, and promotes interdisciplinary teamwork.5
CHAMP achieved its initial goals. Faculty participants were satisfied and CHAMP substantially increased participants' confidence in practicing and teaching geriatric care. Faculty participants also gained confidence in their teaching abilities and presumably learned teaching strategies that could be applied to other topics in inpatient medicine. Faculty participants demonstrated modest improvements in their knowledge of geriatric issues and more positive attitudes about geriatrics at the end of the course than at the beginning. It is worth noting that the hospitalist and general internist ward attending physicians who participated in CHAMP were volunteers and may have started the process with greater interest in learning geriatric care than other attendings. Thus, it is unknown whether CHAMP might have greater or lesser effect on other faculty.
The CHAMP train‐the‐trainer model offers the potential to impact future practitioners. Findings of the CHAMP investigators are consistent with the literature on faculty development programs for educators, which shows that faculty development on teaching yields high participant satisfaction, knowledge gains, and improved self‐assessment of the ability to implement changes in teaching practice.6 The use in CHAMP of a diverse menu of teaching strategies and active learning techniques such as case‐based discussions and the Objective Structured Teaching Exercise in a small group of colleagues should promote learning and retention.
Is the CHAMP curriculum worth the cost? The program requires resources to pay for 48 hours for each faculty participant and for instructors with expertise in geriatrics and teaching skills. We estimate that the cost for 12 faculty participants would be roughly $72,000. We believe this investment will likely pay off in terms of enhancing faculty skills, improving faculty job satisfaction, promoting faculty retention in academic or other teaching positions, and improving care provided by trainees. For example, if CHAMP were to lead to the retention and promotion of even 2 faculty for just 1 year, it would save recruitment costs that would exceed the direct program costs, and other benefits of CHAMP would only further add value. However, analysis of the benefits of CHAMP will require more in‐depth evaluation data of its impact. The program leaders currently contact former participants around the time of ward attending to reinforce teaching concepts and encourage implementation of CHAMP materials, through a Commitment to Change contract. The ultimate downstream educational goal would be that these faculty learners retain and apply this newly acquired knowledge and skills in their clinical practice and teaching activities. Ideally, evidence would confirm that these benefits improve patient care. The long‐term evaluation plan for CHAMP incorporates important additional outcome measures including resident and student geriatric knowledge as well as patient satisfaction and clinical outcomes. We commend the authors for aiming to expand their evaluation plan over time and aspiring for sustained changes in teaching practice. The literature on the impact of hospitalists has similarly evolved from early descriptions of hospitalists and the logistics of developing a hospitalist program to sophisticated analyses of the impact of hospitalists on clinical outcomes such as length of stay and mortality.7, 8
The feasibility of disseminating CHAMP is an open question. The University of Chicago model employs a time‐intensive curriculum that engages participants in part by releasing them from clinical duties for a half day per week. Release time was funded through combined support from external funding sources and the Department of Medicine. This model addresses the major barrier to faculty development in geriatrics for general internists: lack of time.2, 9 The investment in intensive, longitudinal faculty development may generate higher returns than periodic short faculty workshop sessions that do not build in the time for role‐playing, practice, and reinforcement of key concepts. This type of intervention may also be more feasible when done in conjunction with one of the approximately 50 Health Resources and Services Administration (HRSA)supported Geriatrics Education Centers, which can fund teachers and infrastructure for faculty development.
How is this article useful for hospitalist educators? Many hospitalists at academic centers serve important teaching functions, and some will aspire to advance their educational efforts through more scholarly activities such as curriculum design. The CHAMP curriculum represents a successful model for hospitalists aiming to follow a rigorous approach to curriculum design relevant to inpatient medicine, and the extensive CHAMP materials are available online.10 It serves as a practical model that could be applied to other clinical topics related to hospital medicine. Hospitalists are effective and respected teachers for residents and students, and they develop unique expertise in the content and process of inpatient medicine.11 The authors followed the 6 steps of effective curriculum design: problem identification, targeted needs assessment, goals and objectives, education methods, implementation, and evaluation.12
The CHAMP curriculum typifies a set of materials that aligns well with the Society of Hospital Medicine (SHM) Core Competencies.13 As part of their needs assessment, the authors also surveyed hospitalists at a regional SHM meeting to determine the geriatrics topics for which they perceived greatest educational need. The Core Competencies chapters on the care of the elderly patient, delirium and dementia, hospital‐acquired infections, and palliative care highlight the common learning goals shared by hospital medicine and geriatrics. Both disciplines also emphasize the team‐based, multidisciplinary approach to care, particularly during care transitions, that is highlighted in the CHAMP curriculum.
More generally, the CHAMP curriculum can be used to teach and assess the Accreditation Council for Graduate Medical Education (ACGME) competencies, which must be assessed in all ACGME‐accredited residency programs.14 In an initial session on Teaching on Today's Wards, CHAMP participants brainstorm about how to incorporate both geriatrics content and the ACGME competencies into their post‐call rounds. The emphasis in CHAMP on the health care system and interdisciplinary care is evident in topics such as end‐of‐life care and transitions in care, and provides opportunity for assessment of residents' performance in the ACGME competency of systems‐based practice. The organization of the curriculum by ACGME competency makes it more applicable today than some prior geriatric curricula that emphasized similar themes but without the emphasis on demonstrating competency as an outcome.15
Hospitalists partnering with the Donald W. Reynolds and John A. Hartford Foundations and other external organizations may find funding opportunities for educational projects. For example, the Hartford Foundation has partnered with SHM since 2002 to support hospitalists' efforts to improve care for older adults. Products of this collaboration include a Geriatric Toolbox that contains assessment tools designed for use with geriatric patients.16 The tools assess a range of parameters including nutritional, functional, and mental status, and the website supplies guidelines on the advantages and disadvantages and appropriate use of each assessment tool. With support from the Hartford Foundation, hospitalists have also conducted several workshops at SHM meetings on improving assessment and care of geriatric patients and developed a discharge‐planning checklist for older adults.
As hospitalist programs gain traction in academic centers, hospitalists will increasingly serve as key geriatric content educators for trainees. The CHAMP curriculum offers a model of intensive faculty development for hospitalists and general internists that clinician educators find engaging and empowering. The partnerships of geriatricians and hospitalists, and of the SHM with national geriatrics organizations, have the potential for widespread benefits for both learners and elderly patients.
Postdischarge Follow‐Up Visits for Medical/Pharmacy Students
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
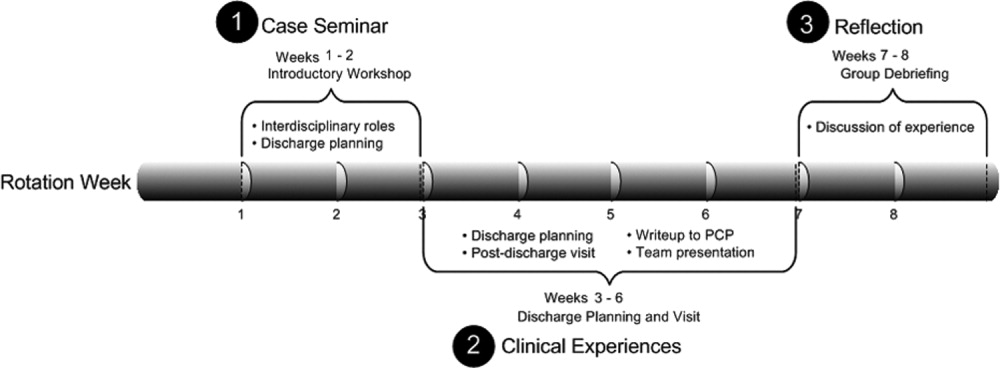
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
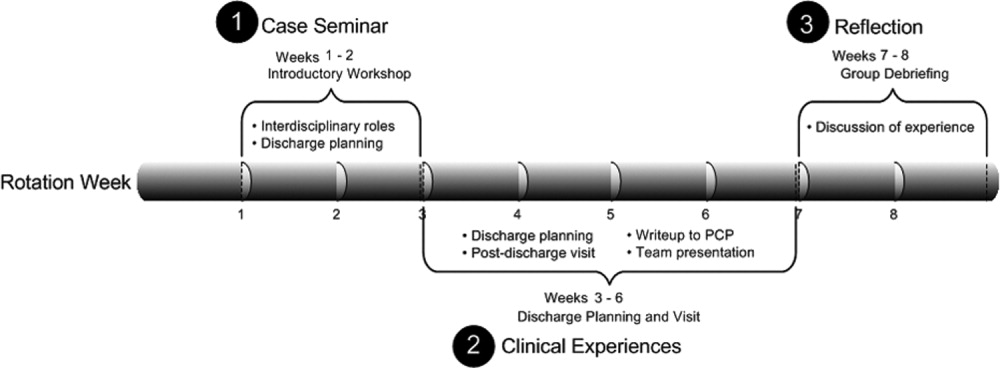
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
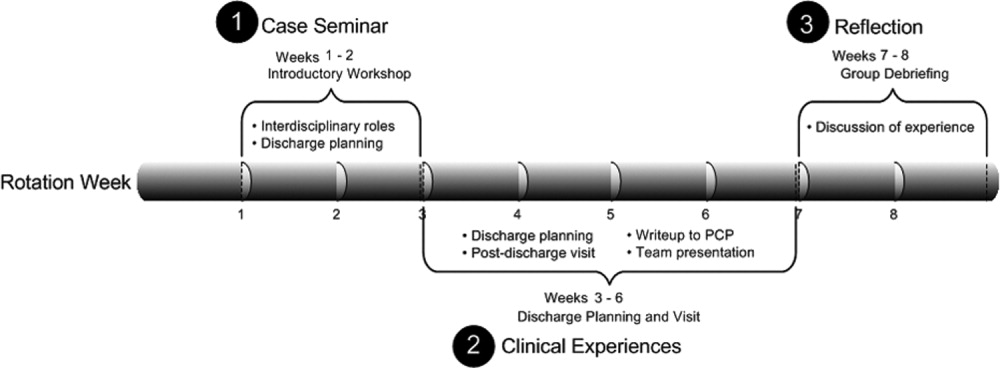
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
Copyright © 2008 Society of Hospital Medicine