User login
Cutaneous eruption on chest and back
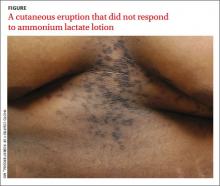
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
A 22-year-old African American man sought care at our clinic for an asymptomatic, “dirty-looking” rash on the epigastrium that had expanded and thickened over the previous 2 years. The rash hadn’t responded to scrubbing with soap and water, ammonium lactate lotion 12% BID, or over-the-counter moisturizing lotions.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Confluent and reticulated papillomatosis
This patient was given a diagnosis of confluent and reticulated papillomatosis (CRP) based on the clinical presentation.
Although this condition is uncommon,1 we see it at least once a month in our dermatology clinic. CRP is characterized by centrally confluent and peripherally reticulated scaly brown plaques and papules that are cosmetically disfiguring.1
CRP usually is asymptomatic2 and primarily affects young adults—especially teenagers.3 It occurs in both males and females3 and it commonly occurs on the trunk.1,2
CRP is believed to be a disorder of keratinization. Malassezia furfur may induce CRP’s hyperproliferative epidermal changes, but systemic treatment that eliminates this organism does not clear CRP.3
Differential diagnosis includes acanthosis nigricans
Acanthosis nigricans (AN) shares similar “dirty” brown, confluent textural plaques, as well as nonspecific acanthosis and papillomatosis on histopathologic examination. However, AN affects flexural areas, whereas CRP typically is found on the epigastrium, central chest, and central back.1,2
Tinea versicolor (TV) and CRP are both brown in color, and occur in a similar distribution on the central back and chest.4 However, in contrast to the fine perifollicular scaling seen in TV, CRP is associated with textural, confluent plaques. TV also can be distinguished by its pathognomonic “spaghetti and meatball” pattern of hyphae and spores on potassium hydroxide (KOH) preparation; KOH will be negative in patients with CRP. When a presumed case of TV does not respond to antifungal therapy, CRP should be considered.1
Making the diagnosis
A CRP diagnosis is made based on clinical presentation. The eruption usually begins as verrucous papules in the inframammary or epigastric region that enlarge to 4 to 5 mm in diameter and coalesce to form a confluent plaque with a peripheral reticulated pattern. CRP can extend over the back, chest, and abdomen to the neck, shoulders, and gluteal cleft. CRP does not affect the oral mucosa and rarely involves flexural areas.2 Although most cases are asymptomatic, mild pruritus may occur.1,2
A skin biopsy rarely is necessary for making a CRP diagnosis, but histopathologic findings include papillomatosis, hyperkeratosis, variable acanthosis, follicular plugging, and sparse dermal inflammation.1,3
Antibiotics usually clear this rash
Systemic antibiotics, most commonly minocycline 100 mg twice daily for 30 days or doxycycline 100 mg twice daily for 30 days, are safe and effective for CRP.1,5 Sometimes treatment is extended for as long as 6 months. Although CRP usually responds to minocycline or doxycycline, it is believed that this is the result of these drugs’ anti-inflammatory—rather than antibiotic—properties.1,2,5 Azithromycin is an effective alternative therapy.2,5
There is a high rate of recurrence of CRP in patients after systemic antibiotics are discontinued.2 Uniform responses to treatment and retreatment of flares have solidified the belief that antibiotics are an effective suppressive if not curative therapy, despite a lack of randomized controlled trials.5
Our patient was treated with minocycline 100 mg BID. After 1 month, the rash had improved by 70%. In 3 months it was completely clear and the treatment was discontinued.
CORRESPONDENCE
Robert T. Brodell, MD, Division of Dermatology, University of Mississippi Medical Center, 2500 North State Street, Jackson, MS 39216; [email protected]
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.
1. Davis MD, Weenig RH, Camilleri MJ. Confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome): a minocycline-responsive dermatosis without evidence for yeast in pathogenesis. A study of 39 patients and a proposal of diagnostic criteria. Br J Dermatol. 2006;154:287-293.
2. Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7: 305-313.
3. Tamraz H, Raffoul M, Kurban M, et al. Confluent and reticulated papillomatosis: clinical and histopathological study of 10 cases from Lebanon. J Eur Acad Dermatol Venereol. 2013;27:e119-e123.
4. Hudacek KD, Haque MS, Hochberg AL, et al. An unusual variant of confluent and reticulated papillomatosis masquerading as tinea versicolor. Arch Dermatol. 2012;148:505-508.
5. Jang HS, Oh CK, Cha JH, et al. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. J Am Acad Dermatol. 2001;44:652-655.