User login
A toddler with failure to thrive and impaired vision
A 2½-year-old boy came to the office for a routine check-up. His height and weight were below the fifth percentile and he was developmentally delayed. His parents noted that while he could walk unsupported, he could only say “mama” and “dada,” and had just recently started climbing stairs. His previous physician had diagnosed him with hypothyroidism, but he was not taking any medications.
The child’s birth history revealed that he was born to a 20-year-old G1P0 female via Cesarean section secondary to fetal distress at 42 weeks’ gestation. He subsequently spent 1 week in the neonatal intensive care unit due to hypoglycemia.
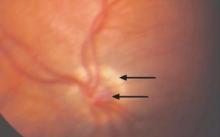
Following the office visit, the patient was admitted to the children’s hospital to investigate his failure to thrive and possible pituitary dysfunction. An ophthalmologic exam in the hospital showed that the patient was unable to follow objects, but did blink to bright light. Intermittent nystagmus was noted. A fundus exam revealed pale, hypoplastic optic nerves, bilaterally. Both nerves were also positive for the “double ring” sign (FIGURE 1).
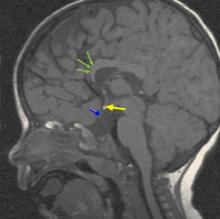
Magnetic resonance imaging (MRI) of the brain (FIGURE 2) revealed hypoplastic genu of the corpus callosum, cavum septum pellucidum, ectopic posterior pituitary, and small anterior pituitary. There was also enhancement of the inferior hypothalamus.
FIGURE 1
Hypoplastic left optic nerve
FIGURE 2
MRI of the brain
What is your diagnosis?
How would you manage the patient?
Diagnosis: Septo-optic dysplasia
Septo-optic dysplasia is a form of optic nerve hypoplasia, the most common congenital optic nerve anomaly, which results from a decreased number of ganglion cell axons.1,2 By definition the syndrome also includes the absence or dysplasia of the septum pellucidum. In many cases, there are other central nervous system abnormalities, such as thinning of the corpus callosum, pituitary malformation, and schizencephaly.3 Most cases of septo-optic dysplasia are diagnosed in infancy and childhood, and there is an equal gender distribution. While rare (6.3 cases per 100,000), septo-optic dysplasia is potentially fatal.1,4
The exact cause of septo-optic dysplasia is unknown; however, both genetic and environmental factors appear to play a role. It has been linked with a defect in the HESX1 gene, young maternal age, maternal insulin-dependent diabetes mellitus, and a variety of toxins.1,5
Poor vision and the “double ring” sign
Most patients present with visual disturbance secondary to optic nerve hypoplasia. Visual acuity may range from 20/20 to no light perception; however, the majority of patients have vision worse than 20/200.1,3 Severe congenital vision loss often leads to sensory nystagmus and strabismus, as well as absent fixation, visual inattentiveness, and an afferent pupillary defect.1,2,6
On examination of the fundus, you may see a “double ring” sign, the appearance of 2 borders around the optic nerve. This outer ring shows a visible sclera at the outer border of a normal-sized nerve and the inner represents the junction between the retinal pigment epithelium and the actual nerve border.1,2,3,7
From CNS abnormalities to pituitary and adrenal problems
While the absence of a septum pellucidum alone has been shown to be clinically insignificant, the presence of other central nervous system abnormalities—such as schizencephaly, cortical heterotopias, or periventricular leukomalacia—can lead to a variety of deficits.8,9 Three-fourths of patients present with seizures, mental retardation, focal neurological deficits, cerebral palsy, or cortical visual loss.1,9
In addition, 15% of patients have some level of pituitary hormone deficiency. Decreased growth hormone is most common, followed by lack of thyroid-stimulating hormone, corticotropic hormone, and vasopressin. Common presentations include failure to thrive, hypoglycemia, prolonged jaundice, thermoregulatory dysfunction, developmental delay, growth retardation, hypotension, recurrent infection, polydipsia, polyuria, and hyper-natremia.1,4,10
Sudden death has been reported in septo-optic dysplasia patients who exhibit hypocortisolism (adrenal insufficiency), diabetes insipidus, and thermo-regulatory dysfunction. Viral illness and other forms of stress are particularly problematic for these patients, as they are unable to mount an appropriate response and are overwhelmed by hypoglycemia, dehydration, shock, and high fevers.4 As a result, clinicians need to be watch for those infants and neonates who are vulnerable to this stress. Extra care should be taken if they require surgery.4,6
Differentiation from a broad swath of possibilities
Due to the variety of presentations, the differential diagnosis for septo-optic dysplasia is very large. It includes all causes of failure to thrive, pituitary dysfunction, neurodevelopmental delay, and congenital vision loss. However, it’s important to maintain a high suspicion for the condition when the combination of the common signs and symptoms are present.
In addition to a full history and physical with dilated fundus exam, one of the most valuable tools in the diagnosis and prognosis of a patient with septo-optic dysplasia is an MRI of the brain with and without contrast, including the pituitary gland. In addition to detecting severely hypoplastic optic nerves, an MRI may also reveal the condition of the septum pellucidum and corpus callosum, cerebral hemispheric abnormalities, and pituitary ectopia. The presence or absence of these findings can help predict the clinical course in relation to pituitary function and neurodevelopmental delay.9,11
Laboratory testing of the hypothalamic-pituitary axis is important, as well. Referrals to both an ophthalmologist and endocrinologist are also necessary.6
Management
In septo-optic dysplasia, the goals of treatment are to preserve the patient’s vision, normalize hormone levels, and assist with neurodevelopmental delays.
Ophthalmology
Patients should be followed closely by an ophthalmologist. That’s because a patient may have a component of delayed maturation of vision, which may improve as he develops. Also, those with unilateral or asymmetric vision loss must be monitored and treated for a resulting amblyopia. Patching of the unaffected eye can aid toward this end.1,7
Endocrinology
Those patients with documented hormonal insufficiency require supplementation. Any patient at risk for developing a deficiency should also be closely monitored so that a change in hormone levels can be quickly recognized and treated. This will help avoid such complications as impaired growth and development—or even death.1,4
Parent education
It’s very important to teach parents about the critical signs and symptoms of dangerous hormone insufficiencies. In patients with cortisol deficiency or diabetes insipidus, febrile illnesses or extreme dehydration require an immediate stress dose of injectable parenteral corticosteroids and hospitalization.3,4 Parents should also be told to monitor their child for the development of other hormone insufficiencies by paying close attention to his growth pattern.1
Outcome
Our patient had deficiencies of growth hormone, thyroid stimulating hormone, and corticotropic hormone. As a result, we started him on supplements, including somatropin, levothyroxine, and hydrocortisone sodium succinate.
Our patient was also diagnosed with oral aversion, so a gastric tube was placed to ensure adequate nutrition. His parents were instructed to follow-up with ophthalmology, neurology, and endocrinology, as well as his primary care physician.
Five months after discharge, the patient had gained 3 kg and adjustments were made to his hormone therapy.
CORRESPONDENCE
Madhu Agarwal, MD Loma Linda University Department of Ophthalmology, 11370 Anderson, Suite 1800, Loma Linda, CA 92354. [email protected]
1. Smith PM, Rismondo V. Diagnosing septo-optic dysplasia. Eyenet 2006;March:37-39.
2. Zeki SM, Hollman AS, Dutton GN. Neuroradiologic features of patients with optic nerve hypoplasia. J Ped Ophthalmol Strabis 1993;29:107-112.
3. Brodsky MC. Congenital optic disc anomalies. In: Yanoff: Ophthalmogy., 2nd ed. St Louis, Mo: Mosby, Inc; 2004:1255-1256.
4. Brodsky MC, Conte FA, Taylor D, et al. Sudden death in septo-optic dysplasia. Report of 5 cases. Arch Ophthalmol 1997;155:66-70.
5. Oliver SCN, Bennett JL. Genetic disorders and the optic nerve: a clinical survey. Ophthalmol Clin N Am 2004;17:435-445.
6. Siatkowski RM, Sanchez JC, Andrade R, Alvarez A. The clinical, neuroradiographic, and endocrinologic profile of patients with bilateral optic nerve hypoplasia. Ophthalmology 1997;104:493-496.
7. Levin AV. Congenital eye anomalies. Pediatric Clin N Am 2003;50:55-76.
8. Williams J, Brodsky MC, Griebel M, et al. Septo-optic dysplasia: The clinical insignificance of an absent septum pellucidum. Develop Med Child Neurol 1993;35:490-501.
9. Brodsky MC, Glasier CM. Optic nerve hypoplasia: Clinical significance of associated central nervous system abnormalities of magnetic resonance imaging. Arch Ophthalmol 1993;111:66-74.
10. Donahue SP, Lavina A, Najjar J. Infantile infection and diabetes insipidus in children with optic nerve hypoplasia. Br J Ophthalmol 2005;89:1275-1277.
11. Brodsky MC, Glasier CM, Pollock SC, et al. Optic nerve hypoplasia: Identification by magnetic resonance imaging. Arch Ophthalmol 1990;108:1562-1568.
A 2½-year-old boy came to the office for a routine check-up. His height and weight were below the fifth percentile and he was developmentally delayed. His parents noted that while he could walk unsupported, he could only say “mama” and “dada,” and had just recently started climbing stairs. His previous physician had diagnosed him with hypothyroidism, but he was not taking any medications.
The child’s birth history revealed that he was born to a 20-year-old G1P0 female via Cesarean section secondary to fetal distress at 42 weeks’ gestation. He subsequently spent 1 week in the neonatal intensive care unit due to hypoglycemia.
Following the office visit, the patient was admitted to the children’s hospital to investigate his failure to thrive and possible pituitary dysfunction. An ophthalmologic exam in the hospital showed that the patient was unable to follow objects, but did blink to bright light. Intermittent nystagmus was noted. A fundus exam revealed pale, hypoplastic optic nerves, bilaterally. Both nerves were also positive for the “double ring” sign (FIGURE 1).
Magnetic resonance imaging (MRI) of the brain (FIGURE 2) revealed hypoplastic genu of the corpus callosum, cavum septum pellucidum, ectopic posterior pituitary, and small anterior pituitary. There was also enhancement of the inferior hypothalamus.
FIGURE 1
Hypoplastic left optic nerve
FIGURE 2
MRI of the brain
What is your diagnosis?
How would you manage the patient?
Diagnosis: Septo-optic dysplasia
Septo-optic dysplasia is a form of optic nerve hypoplasia, the most common congenital optic nerve anomaly, which results from a decreased number of ganglion cell axons.1,2 By definition the syndrome also includes the absence or dysplasia of the septum pellucidum. In many cases, there are other central nervous system abnormalities, such as thinning of the corpus callosum, pituitary malformation, and schizencephaly.3 Most cases of septo-optic dysplasia are diagnosed in infancy and childhood, and there is an equal gender distribution. While rare (6.3 cases per 100,000), septo-optic dysplasia is potentially fatal.1,4
The exact cause of septo-optic dysplasia is unknown; however, both genetic and environmental factors appear to play a role. It has been linked with a defect in the HESX1 gene, young maternal age, maternal insulin-dependent diabetes mellitus, and a variety of toxins.1,5
Poor vision and the “double ring” sign
Most patients present with visual disturbance secondary to optic nerve hypoplasia. Visual acuity may range from 20/20 to no light perception; however, the majority of patients have vision worse than 20/200.1,3 Severe congenital vision loss often leads to sensory nystagmus and strabismus, as well as absent fixation, visual inattentiveness, and an afferent pupillary defect.1,2,6
On examination of the fundus, you may see a “double ring” sign, the appearance of 2 borders around the optic nerve. This outer ring shows a visible sclera at the outer border of a normal-sized nerve and the inner represents the junction between the retinal pigment epithelium and the actual nerve border.1,2,3,7
From CNS abnormalities to pituitary and adrenal problems
While the absence of a septum pellucidum alone has been shown to be clinically insignificant, the presence of other central nervous system abnormalities—such as schizencephaly, cortical heterotopias, or periventricular leukomalacia—can lead to a variety of deficits.8,9 Three-fourths of patients present with seizures, mental retardation, focal neurological deficits, cerebral palsy, or cortical visual loss.1,9
In addition, 15% of patients have some level of pituitary hormone deficiency. Decreased growth hormone is most common, followed by lack of thyroid-stimulating hormone, corticotropic hormone, and vasopressin. Common presentations include failure to thrive, hypoglycemia, prolonged jaundice, thermoregulatory dysfunction, developmental delay, growth retardation, hypotension, recurrent infection, polydipsia, polyuria, and hyper-natremia.1,4,10
Sudden death has been reported in septo-optic dysplasia patients who exhibit hypocortisolism (adrenal insufficiency), diabetes insipidus, and thermo-regulatory dysfunction. Viral illness and other forms of stress are particularly problematic for these patients, as they are unable to mount an appropriate response and are overwhelmed by hypoglycemia, dehydration, shock, and high fevers.4 As a result, clinicians need to be watch for those infants and neonates who are vulnerable to this stress. Extra care should be taken if they require surgery.4,6
Differentiation from a broad swath of possibilities
Due to the variety of presentations, the differential diagnosis for septo-optic dysplasia is very large. It includes all causes of failure to thrive, pituitary dysfunction, neurodevelopmental delay, and congenital vision loss. However, it’s important to maintain a high suspicion for the condition when the combination of the common signs and symptoms are present.
In addition to a full history and physical with dilated fundus exam, one of the most valuable tools in the diagnosis and prognosis of a patient with septo-optic dysplasia is an MRI of the brain with and without contrast, including the pituitary gland. In addition to detecting severely hypoplastic optic nerves, an MRI may also reveal the condition of the septum pellucidum and corpus callosum, cerebral hemispheric abnormalities, and pituitary ectopia. The presence or absence of these findings can help predict the clinical course in relation to pituitary function and neurodevelopmental delay.9,11
Laboratory testing of the hypothalamic-pituitary axis is important, as well. Referrals to both an ophthalmologist and endocrinologist are also necessary.6
Management
In septo-optic dysplasia, the goals of treatment are to preserve the patient’s vision, normalize hormone levels, and assist with neurodevelopmental delays.
Ophthalmology
Patients should be followed closely by an ophthalmologist. That’s because a patient may have a component of delayed maturation of vision, which may improve as he develops. Also, those with unilateral or asymmetric vision loss must be monitored and treated for a resulting amblyopia. Patching of the unaffected eye can aid toward this end.1,7
Endocrinology
Those patients with documented hormonal insufficiency require supplementation. Any patient at risk for developing a deficiency should also be closely monitored so that a change in hormone levels can be quickly recognized and treated. This will help avoid such complications as impaired growth and development—or even death.1,4
Parent education
It’s very important to teach parents about the critical signs and symptoms of dangerous hormone insufficiencies. In patients with cortisol deficiency or diabetes insipidus, febrile illnesses or extreme dehydration require an immediate stress dose of injectable parenteral corticosteroids and hospitalization.3,4 Parents should also be told to monitor their child for the development of other hormone insufficiencies by paying close attention to his growth pattern.1
Outcome
Our patient had deficiencies of growth hormone, thyroid stimulating hormone, and corticotropic hormone. As a result, we started him on supplements, including somatropin, levothyroxine, and hydrocortisone sodium succinate.
Our patient was also diagnosed with oral aversion, so a gastric tube was placed to ensure adequate nutrition. His parents were instructed to follow-up with ophthalmology, neurology, and endocrinology, as well as his primary care physician.
Five months after discharge, the patient had gained 3 kg and adjustments were made to his hormone therapy.
CORRESPONDENCE
Madhu Agarwal, MD Loma Linda University Department of Ophthalmology, 11370 Anderson, Suite 1800, Loma Linda, CA 92354. [email protected]
A 2½-year-old boy came to the office for a routine check-up. His height and weight were below the fifth percentile and he was developmentally delayed. His parents noted that while he could walk unsupported, he could only say “mama” and “dada,” and had just recently started climbing stairs. His previous physician had diagnosed him with hypothyroidism, but he was not taking any medications.
The child’s birth history revealed that he was born to a 20-year-old G1P0 female via Cesarean section secondary to fetal distress at 42 weeks’ gestation. He subsequently spent 1 week in the neonatal intensive care unit due to hypoglycemia.
Following the office visit, the patient was admitted to the children’s hospital to investigate his failure to thrive and possible pituitary dysfunction. An ophthalmologic exam in the hospital showed that the patient was unable to follow objects, but did blink to bright light. Intermittent nystagmus was noted. A fundus exam revealed pale, hypoplastic optic nerves, bilaterally. Both nerves were also positive for the “double ring” sign (FIGURE 1).
Magnetic resonance imaging (MRI) of the brain (FIGURE 2) revealed hypoplastic genu of the corpus callosum, cavum septum pellucidum, ectopic posterior pituitary, and small anterior pituitary. There was also enhancement of the inferior hypothalamus.
FIGURE 1
Hypoplastic left optic nerve
FIGURE 2
MRI of the brain
What is your diagnosis?
How would you manage the patient?
Diagnosis: Septo-optic dysplasia
Septo-optic dysplasia is a form of optic nerve hypoplasia, the most common congenital optic nerve anomaly, which results from a decreased number of ganglion cell axons.1,2 By definition the syndrome also includes the absence or dysplasia of the septum pellucidum. In many cases, there are other central nervous system abnormalities, such as thinning of the corpus callosum, pituitary malformation, and schizencephaly.3 Most cases of septo-optic dysplasia are diagnosed in infancy and childhood, and there is an equal gender distribution. While rare (6.3 cases per 100,000), septo-optic dysplasia is potentially fatal.1,4
The exact cause of septo-optic dysplasia is unknown; however, both genetic and environmental factors appear to play a role. It has been linked with a defect in the HESX1 gene, young maternal age, maternal insulin-dependent diabetes mellitus, and a variety of toxins.1,5
Poor vision and the “double ring” sign
Most patients present with visual disturbance secondary to optic nerve hypoplasia. Visual acuity may range from 20/20 to no light perception; however, the majority of patients have vision worse than 20/200.1,3 Severe congenital vision loss often leads to sensory nystagmus and strabismus, as well as absent fixation, visual inattentiveness, and an afferent pupillary defect.1,2,6
On examination of the fundus, you may see a “double ring” sign, the appearance of 2 borders around the optic nerve. This outer ring shows a visible sclera at the outer border of a normal-sized nerve and the inner represents the junction between the retinal pigment epithelium and the actual nerve border.1,2,3,7
From CNS abnormalities to pituitary and adrenal problems
While the absence of a septum pellucidum alone has been shown to be clinically insignificant, the presence of other central nervous system abnormalities—such as schizencephaly, cortical heterotopias, or periventricular leukomalacia—can lead to a variety of deficits.8,9 Three-fourths of patients present with seizures, mental retardation, focal neurological deficits, cerebral palsy, or cortical visual loss.1,9
In addition, 15% of patients have some level of pituitary hormone deficiency. Decreased growth hormone is most common, followed by lack of thyroid-stimulating hormone, corticotropic hormone, and vasopressin. Common presentations include failure to thrive, hypoglycemia, prolonged jaundice, thermoregulatory dysfunction, developmental delay, growth retardation, hypotension, recurrent infection, polydipsia, polyuria, and hyper-natremia.1,4,10
Sudden death has been reported in septo-optic dysplasia patients who exhibit hypocortisolism (adrenal insufficiency), diabetes insipidus, and thermo-regulatory dysfunction. Viral illness and other forms of stress are particularly problematic for these patients, as they are unable to mount an appropriate response and are overwhelmed by hypoglycemia, dehydration, shock, and high fevers.4 As a result, clinicians need to be watch for those infants and neonates who are vulnerable to this stress. Extra care should be taken if they require surgery.4,6
Differentiation from a broad swath of possibilities
Due to the variety of presentations, the differential diagnosis for septo-optic dysplasia is very large. It includes all causes of failure to thrive, pituitary dysfunction, neurodevelopmental delay, and congenital vision loss. However, it’s important to maintain a high suspicion for the condition when the combination of the common signs and symptoms are present.
In addition to a full history and physical with dilated fundus exam, one of the most valuable tools in the diagnosis and prognosis of a patient with septo-optic dysplasia is an MRI of the brain with and without contrast, including the pituitary gland. In addition to detecting severely hypoplastic optic nerves, an MRI may also reveal the condition of the septum pellucidum and corpus callosum, cerebral hemispheric abnormalities, and pituitary ectopia. The presence or absence of these findings can help predict the clinical course in relation to pituitary function and neurodevelopmental delay.9,11
Laboratory testing of the hypothalamic-pituitary axis is important, as well. Referrals to both an ophthalmologist and endocrinologist are also necessary.6
Management
In septo-optic dysplasia, the goals of treatment are to preserve the patient’s vision, normalize hormone levels, and assist with neurodevelopmental delays.
Ophthalmology
Patients should be followed closely by an ophthalmologist. That’s because a patient may have a component of delayed maturation of vision, which may improve as he develops. Also, those with unilateral or asymmetric vision loss must be monitored and treated for a resulting amblyopia. Patching of the unaffected eye can aid toward this end.1,7
Endocrinology
Those patients with documented hormonal insufficiency require supplementation. Any patient at risk for developing a deficiency should also be closely monitored so that a change in hormone levels can be quickly recognized and treated. This will help avoid such complications as impaired growth and development—or even death.1,4
Parent education
It’s very important to teach parents about the critical signs and symptoms of dangerous hormone insufficiencies. In patients with cortisol deficiency or diabetes insipidus, febrile illnesses or extreme dehydration require an immediate stress dose of injectable parenteral corticosteroids and hospitalization.3,4 Parents should also be told to monitor their child for the development of other hormone insufficiencies by paying close attention to his growth pattern.1
Outcome
Our patient had deficiencies of growth hormone, thyroid stimulating hormone, and corticotropic hormone. As a result, we started him on supplements, including somatropin, levothyroxine, and hydrocortisone sodium succinate.
Our patient was also diagnosed with oral aversion, so a gastric tube was placed to ensure adequate nutrition. His parents were instructed to follow-up with ophthalmology, neurology, and endocrinology, as well as his primary care physician.
Five months after discharge, the patient had gained 3 kg and adjustments were made to his hormone therapy.
CORRESPONDENCE
Madhu Agarwal, MD Loma Linda University Department of Ophthalmology, 11370 Anderson, Suite 1800, Loma Linda, CA 92354. [email protected]
1. Smith PM, Rismondo V. Diagnosing septo-optic dysplasia. Eyenet 2006;March:37-39.
2. Zeki SM, Hollman AS, Dutton GN. Neuroradiologic features of patients with optic nerve hypoplasia. J Ped Ophthalmol Strabis 1993;29:107-112.
3. Brodsky MC. Congenital optic disc anomalies. In: Yanoff: Ophthalmogy., 2nd ed. St Louis, Mo: Mosby, Inc; 2004:1255-1256.
4. Brodsky MC, Conte FA, Taylor D, et al. Sudden death in septo-optic dysplasia. Report of 5 cases. Arch Ophthalmol 1997;155:66-70.
5. Oliver SCN, Bennett JL. Genetic disorders and the optic nerve: a clinical survey. Ophthalmol Clin N Am 2004;17:435-445.
6. Siatkowski RM, Sanchez JC, Andrade R, Alvarez A. The clinical, neuroradiographic, and endocrinologic profile of patients with bilateral optic nerve hypoplasia. Ophthalmology 1997;104:493-496.
7. Levin AV. Congenital eye anomalies. Pediatric Clin N Am 2003;50:55-76.
8. Williams J, Brodsky MC, Griebel M, et al. Septo-optic dysplasia: The clinical insignificance of an absent septum pellucidum. Develop Med Child Neurol 1993;35:490-501.
9. Brodsky MC, Glasier CM. Optic nerve hypoplasia: Clinical significance of associated central nervous system abnormalities of magnetic resonance imaging. Arch Ophthalmol 1993;111:66-74.
10. Donahue SP, Lavina A, Najjar J. Infantile infection and diabetes insipidus in children with optic nerve hypoplasia. Br J Ophthalmol 2005;89:1275-1277.
11. Brodsky MC, Glasier CM, Pollock SC, et al. Optic nerve hypoplasia: Identification by magnetic resonance imaging. Arch Ophthalmol 1990;108:1562-1568.
1. Smith PM, Rismondo V. Diagnosing septo-optic dysplasia. Eyenet 2006;March:37-39.
2. Zeki SM, Hollman AS, Dutton GN. Neuroradiologic features of patients with optic nerve hypoplasia. J Ped Ophthalmol Strabis 1993;29:107-112.
3. Brodsky MC. Congenital optic disc anomalies. In: Yanoff: Ophthalmogy., 2nd ed. St Louis, Mo: Mosby, Inc; 2004:1255-1256.
4. Brodsky MC, Conte FA, Taylor D, et al. Sudden death in septo-optic dysplasia. Report of 5 cases. Arch Ophthalmol 1997;155:66-70.
5. Oliver SCN, Bennett JL. Genetic disorders and the optic nerve: a clinical survey. Ophthalmol Clin N Am 2004;17:435-445.
6. Siatkowski RM, Sanchez JC, Andrade R, Alvarez A. The clinical, neuroradiographic, and endocrinologic profile of patients with bilateral optic nerve hypoplasia. Ophthalmology 1997;104:493-496.
7. Levin AV. Congenital eye anomalies. Pediatric Clin N Am 2003;50:55-76.
8. Williams J, Brodsky MC, Griebel M, et al. Septo-optic dysplasia: The clinical insignificance of an absent septum pellucidum. Develop Med Child Neurol 1993;35:490-501.
9. Brodsky MC, Glasier CM. Optic nerve hypoplasia: Clinical significance of associated central nervous system abnormalities of magnetic resonance imaging. Arch Ophthalmol 1993;111:66-74.
10. Donahue SP, Lavina A, Najjar J. Infantile infection and diabetes insipidus in children with optic nerve hypoplasia. Br J Ophthalmol 2005;89:1275-1277.
11. Brodsky MC, Glasier CM, Pollock SC, et al. Optic nerve hypoplasia: Identification by magnetic resonance imaging. Arch Ophthalmol 1990;108:1562-1568.