User login
Helping Seniors Plan for Posthospital Discharge Needs Before a Hospitalization Occurs: Results from the Randomized Control Trial of PlanYourLifespan.org
When seniors are discharged from the hospital, many will require additional support and therapy to regain their independence and return safely home.1,2 Most seniors do not understand what their support needs will entail or the differences between therapy choices.3 To complicate the issue, seniors are often incapacitated and unable to make discharge selections for themselves.
Consequently, discharge planners and social workers often explain options to family members and loved ones, who frequently feel overwhelmed.4,5 While often balancing jobs, loved ones are divided between wanting to stay with the senior in the hospital and driving to area skilled nursing facilities (SNFs) for consideration. Discharges are delayed waiting for families to make visits and choose an SNF. Longer lengths of stay are detrimental to seniors due to the increased risks of infection, functional loss, and cognitive decline.6
Although seniors comprised only 12% of the US population in 2003,7 they accounted for one-third of all hospitalizations, over 13.2 million hospital stays.8 Hospital stays for seniors resulted in hospital charges totaling nearly $329 billion, or 43.6% of national hospital bills in 2003.7 Seniors are also high consumers of postacute care services. By 2050, the number of individuals using long-term care services in any setting (eg, at home, assisted living, or SNFs) will be close to 27 million.9-11 With the knowledge that many seniors will be hospitalized and subsequently require services thereafter, we sought to assist seniors in planning for their hospital discharge needs before they were hospitalized.
Our team developed PlanYourLifespan.org (PYL) to facilitate this planning for postdischarge needs and fill the knowledge gap in understanding postdischarge options. With funding from the Patient Centered Outcomes Research Institute, we aimed to test the effectiveness of PYL on improving knowledge of hospital discharge resources among seniors.
METHODS
PlanYourLifespan.org
PlanYourLifespan.org (PYL) educates users on the health crises that often occur with age and connects them to posthospital and home-based resources available locally and nationally. PYL is personalized, dynamic, and adaptable in that all the information can be changed per the senior’s wishes or changing health needs.
Content of PYL
Previously, we conducted focus groups with seniors about current and perceived home needs and aging-in-place. Major themes of what advanced life events (ALEs) would impact aging-in-place were identified as follows: hospitalizations, falls, and Alzheimer’s.12 We organized PYL around these health-related ALEs. Our multidisciplinary team of researchers, seniors, social workers, caregiver agencies, and Area Agencies on Aging representatives then determined what information and resources should be included.
Each section of PYL starts with a video of a senior discussing their real-life personal experiences, with subsections providing interactive information on what seniors can expect, types of resources available to support home needs, and choices to be made. Descriptions of types of settings for therapy, options available, and links to national/local resources (eg, quality indicators for SNFs) are also included. For example, by entering their zip code, users can identify their neighborhood SNFs, closest Area Agency on Aging, and what home caregiver agencies exist in their area.
Users can save their preferences and revisit their choices at any time. To support communication between seniors and their loved ones, a summary of their choices can be printed or e-mailed to relevant parties. For example, a senior uses PYL and can e-mail these choices to family members, which can stimulate a conversation about future posthospital care expectations.
As inadequate health literacy and cognitive impairment are prevalent among seniors, PYL presents information understandable at all levels of health literacy and sensitive to cognitive load.9 There is simplified, large-font, no mouse scrolling and audio available for the visually impaired.
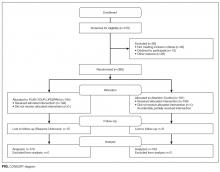
Study Design and Randomization
To test PYL, a 2-armed (attention control [AC] and PYL intervention), parallel, randomized controlled trial was conducted. Participants were randomly assigned to 1 of the 2 conditions via a pregenerated central randomization list using equal (1:1) allocation and random permuted block design to ensure relatively equal allocation throughout the study. The AC condition exposed participants to the National Institute on Aging-sponsored website, Go4Life.nia.nih.gov, an educational website on physical activity for seniors. This website has comparable design and layout to PYL but does not include information about advanced planning. The AC condition controlled for the possibility that regular contact with the study team may improve outcomes in participants randomized to the intervention website.
The trial was conducted from October 2014 to September 2015 in Chicago, Illinois; Fort Wayne, Indiana; and Houston, Texas. Inclusion criteria were as follows: age 65 and older, English-speaking, scoring ≥4 questions correctly on the Brief Cognitive Screen,14 and current self-reported use of a computer or smartphone with internet. Participants were excluded if they had previously participated in the focus groups or beta testing of the PYL website. Community-based patient partners/stakeholders drove subject recruitment in their communities through word of mouth, e-mail bursts, newsletters, and flyers. At the Area Agency on Aging and community centers where services such as food vouchers and case management are provided, participants were recruited on-site and given study information. At the clinical sites, staff referred potential participants. Study materials such as flyers and information sheets were also located in the clinic waiting rooms. The Villages, nonprofit, grassroots, membership organizations that are redefining aging by being a key resource to community members wishing to age in place, heavily relied on electronic recruitment using their regular e-newsletters and e-mail lists to recruit potential participants. Potential subjects were also recruited by distributing flyers at local senior centers and senior housing buildings. Interested seniors contacted research staff who explained the study and assessed their eligibility. If eligible, subjects were scheduled for a face-to-face interview.
At the face-to-face encounter, all study subjects completed a written consent, answered baseline questions, and were randomized to either arm. Next, research staff introduced all study subjects to the website to which they were randomized and provided instructions on its use. Staff were present to assist with questions as needed on navigation but did not assist with decision making for either website. A minimum of 15 minutes and a maximum of 45 minutes was allotted for navigating either website. After navigating their website, participants were administered an immediate in-person posttest survey. One month and 3 months after the face-to-face encounter, research staff contacted all study participants over the phone to complete a follow-up survey. Staff attempted to reach participants up to 3 times by phone. Data were entered into Research Electronic Data Capture survey software.15 This study was approved by the Northwestern University Institutional Review Board.
Understanding of Posthospital Discharge and Home Services
As part of the larger trial, which included behavioural outcomes that will be reported elsewhere, we sought to explore the effects of PYL on participants’ knowledge and understanding of posthospital discharge and home services (UHS). Participants were asked to respond to 6 questions at baseline, immediate posttest, and at the 1- and 3-month follow-up time points. Knowledge items were developed by the study team in conjunction with the patient/partner stakeholders. UHS scores were calculated as the sum of the 6 questions (each scored 0 if incorrect and 1 if correct) with a possible range of 0-6.
Covariates
Demographic information, self-reported health, importance of religion, and existence of a power of attorney, living will, advanced directive (eg, Physician Orders for Life-Sustaining Treatment) were obtained via self-report. Participants were asked about their general and social self-efficacy using the validated Self-efficacy Scale16 and their social support using the Lubben Social Network Scale–6.17 Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine–Short Form.18 To measure burden of disease, participant comorbidities were measured using a nonvalidated 9-item dichotomous response condition list, which included some items adapted from the Charlson Comorbidity Index and the Elixhauser Comorbidity Index.
Statistical Analysis
Data analysis included all available data in the intention-to-treat dataset. As UHS was collected at multiple time points up to 3 months postintervention, we employed linear- mixed modeling with random participant effect and fixed arm, time, and time-by-arm interaction terms. The time-by-arm interaction allows for comparison of UHS slopes (or trajectories) across arms. Analyses explored multiple potential covariates, including current utilization of services, physical function, comorbidities, social support, health literacy, self-efficacy, and sociodemographics. Those covariates found to have a significant association (P < 0.05) with outcome were considered for inclusion in the overall model selection process. Ultimately, we developed a final parsimonious, adjusted longitudinal model with primary predictors of time, arm, and their interaction, controlling for only significant baseline variables following a manual backward selection method. All analyses were conducted in SAS software (version 9.4, copyright 2012, The SAS Institute Inc., Cary, North Carolina).
RESULTS
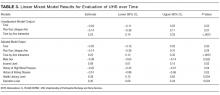
Table 3 illustrates linear mixed model results both failing to adjust and adjusting for potentially influential baseline covariates. In both instances, the interaction term (arm-by-time) was highly significant (P < 0.0001) in predicting UHS score, suggesting that, when compared to the AC arm, the intervention arm exhibited a large mean slope in UHS score over time. That is, understanding home services score tended to increase at a faster rate for those in the active arm. Higher levels of income (P = 0.0191), literacy (P = 0.0036), and education (P = 0.0042) were associated with increased UHS scores; however, male sex (P = 0.0023) and history of high blood pressure (P = 0.0409) or kidney disease (P = 0.0278) were negatively associated with UHS scores.
CONCLUSION/DISCUSSION
The results of our study show that among seniors, PYL improved their understanding of home-based services and the services that may be required following a hospitalization. Educating seniors about what to expect regarding the transition home from a hospital before a hospitalization even occurs may enable seniors and their families to plan ahead instead of reacting to a hospitalization. PYL, a national, publicly available tool with links to local resources may potentially help in advancing transitional discharge care to prior to a hospitalization.
To our knowledge, this is one of the first websites and trials devoted to planning for seniors’ health trajectory as they age into their 70s, 80s, 90s, and 100s. Clinicians regularly discuss code status and powers of attorney during their end-of-life discussions with patients. We encourage clinicians to ask patients, “What about the 10 to 20 years before you die? Have you considered what you will do if you get sick or need help at home?” While not replacing a social worker, the ability of PYL to connect seniors to local resources makes it somewhat of a “virtual social worker.” With many physician practices unable to afford social workers, PYL provides a free-of-charge means of connecting seniors to area resources.
The study participants were in general white, educated, and in reasonably good health. This may be a limitation of this study given that it could impact the generalizability of the study results, as we are unable to know for certain if these same results would be observed with participants who have lower educational levels and are in poor health. Power considerations in this study did not account for comparison of outcomes within specific subgroups so we were unable to assess outcomes in groups such as those with limited health literacy, low social support, or low self-efficacy. The trial was also limited by our inability to collect information on whether or not the knowledge gains observed in the study led to any measureable outcomes. Due to the relatively short follow-up time, we were unable to ascertain whether any study participants were hospitalized during the study follow-up period and if so, if exposure to PYL had any impact on patient anxiety, length of hospital stay, and/or caregiver burden. We were also unable to assess patients’ ability to utilize and carry out their posthospitalization discharge plans if they had one in place. Future studies with longer follow-up are needed to determine these important, measurable outcomes.
Potential implications of planning for a senior’s lifespan are expansive. If hospitalized seniors knew their preferred SNF for subacute rehabilitation on the first day of their hospitalization, hospital lengths of stay could potentially be reduced. If families knew which caregiver agencies, Area Agency on Aging, or Village their senior wished to use, obtaining services would perhaps be easier to accomplish.
Acknowledgments
This work was supported through a Patient-Centered Outcomes Research Institute Award (IH-12-11-4259). Dr. Lindquist and Dr. Ciolino had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Research reported in this publication was also supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR000150.
Disclaimer
All statements in this manuscript, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors or Methodology Committee, or the National Institutes of Health.
Disclosure: The authors have nothing to report.
1. Campbell SE, Seymour DG, Primrose WR, ACMEPLUS Project. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing. 2004;33:110-115. PubMed
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004; 70:345-349. PubMed
3. Kane RL Finding the right level of posthospital care: “We didn’t realize there was any other option for him”. JAMA. 2011;305(3):284-293. PubMed
4. Shepperd S, McClaran J, Phillips CO, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;(1):CD000313. PubMed
5. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173:1715-1722. PubMed
6. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. PubMed
7. U.S. Census Bureau, Population Division, Census 2003. https://www.census.gov/programs-surveys/saipe/data/datasets.2003.html. Originally accessed September 1, 2016.
8. Russo, C. A., Elixhauser, A. Hospitalizations in the Elderly Population, 2003. Statistical Brief #6. May 2006. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb6.pdf. Accessed September 1, 2017.
9 U.S. Department of Health and Human Services, and U.S. Department of Labor. The future supply of long-term care workers in relation to the aging baby boom generation: Report to Congress. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, 2003. http:aspe.hhs.gov/daltcp/reports/ltcwork.htm. Accessed September 1, 2016.
10. The Henry J. Kaiser Foundation. Long-term Care: Medicaid’s role and challenges [Publication #2172]. Washington, DC: 1999.
11. AARP. Beyond 50.2003: A Report to the Nation on Independent Living and Disability, 2003, http://www.aarp.org/research/health/disabilities/aresearch-import-753.html. Accessed September 1, 2016.
12. Lindquist LA, Ramirez-Zohfeld V, Sunkara P, et al. Advanced Life Events (ALEs) that Impede Aging-in-Place among Seniors. Arch Gerontol Geriatrs. 2016;64:90-95. PubMed
13. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. Philadelphia, PA: JB Lippincott Co.; 1996.
14. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771-781. PubMed
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Gonzalez J, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self Efficacy Scale: Construction and Validation. Psychol Rep. 1982;51(3):663-671.
17. Lubben JE. Assessing social networks among elderly populations. Fam Community Health. 1988;11(3):42-52.
18. Arozullah AM, Yarnold PR, Bennett CL, et al. Development and validation of the Rapid Estimate of Adult Literacy in Medicine. Medical Care. 2007;45(11):1026-1033. PubMed
When seniors are discharged from the hospital, many will require additional support and therapy to regain their independence and return safely home.1,2 Most seniors do not understand what their support needs will entail or the differences between therapy choices.3 To complicate the issue, seniors are often incapacitated and unable to make discharge selections for themselves.
Consequently, discharge planners and social workers often explain options to family members and loved ones, who frequently feel overwhelmed.4,5 While often balancing jobs, loved ones are divided between wanting to stay with the senior in the hospital and driving to area skilled nursing facilities (SNFs) for consideration. Discharges are delayed waiting for families to make visits and choose an SNF. Longer lengths of stay are detrimental to seniors due to the increased risks of infection, functional loss, and cognitive decline.6
Although seniors comprised only 12% of the US population in 2003,7 they accounted for one-third of all hospitalizations, over 13.2 million hospital stays.8 Hospital stays for seniors resulted in hospital charges totaling nearly $329 billion, or 43.6% of national hospital bills in 2003.7 Seniors are also high consumers of postacute care services. By 2050, the number of individuals using long-term care services in any setting (eg, at home, assisted living, or SNFs) will be close to 27 million.9-11 With the knowledge that many seniors will be hospitalized and subsequently require services thereafter, we sought to assist seniors in planning for their hospital discharge needs before they were hospitalized.
Our team developed PlanYourLifespan.org (PYL) to facilitate this planning for postdischarge needs and fill the knowledge gap in understanding postdischarge options. With funding from the Patient Centered Outcomes Research Institute, we aimed to test the effectiveness of PYL on improving knowledge of hospital discharge resources among seniors.
METHODS
PlanYourLifespan.org
PlanYourLifespan.org (PYL) educates users on the health crises that often occur with age and connects them to posthospital and home-based resources available locally and nationally. PYL is personalized, dynamic, and adaptable in that all the information can be changed per the senior’s wishes or changing health needs.
Content of PYL
Previously, we conducted focus groups with seniors about current and perceived home needs and aging-in-place. Major themes of what advanced life events (ALEs) would impact aging-in-place were identified as follows: hospitalizations, falls, and Alzheimer’s.12 We organized PYL around these health-related ALEs. Our multidisciplinary team of researchers, seniors, social workers, caregiver agencies, and Area Agencies on Aging representatives then determined what information and resources should be included.
Each section of PYL starts with a video of a senior discussing their real-life personal experiences, with subsections providing interactive information on what seniors can expect, types of resources available to support home needs, and choices to be made. Descriptions of types of settings for therapy, options available, and links to national/local resources (eg, quality indicators for SNFs) are also included. For example, by entering their zip code, users can identify their neighborhood SNFs, closest Area Agency on Aging, and what home caregiver agencies exist in their area.
Users can save their preferences and revisit their choices at any time. To support communication between seniors and their loved ones, a summary of their choices can be printed or e-mailed to relevant parties. For example, a senior uses PYL and can e-mail these choices to family members, which can stimulate a conversation about future posthospital care expectations.
As inadequate health literacy and cognitive impairment are prevalent among seniors, PYL presents information understandable at all levels of health literacy and sensitive to cognitive load.9 There is simplified, large-font, no mouse scrolling and audio available for the visually impaired.
Study Design and Randomization
To test PYL, a 2-armed (attention control [AC] and PYL intervention), parallel, randomized controlled trial was conducted. Participants were randomly assigned to 1 of the 2 conditions via a pregenerated central randomization list using equal (1:1) allocation and random permuted block design to ensure relatively equal allocation throughout the study. The AC condition exposed participants to the National Institute on Aging-sponsored website, Go4Life.nia.nih.gov, an educational website on physical activity for seniors. This website has comparable design and layout to PYL but does not include information about advanced planning. The AC condition controlled for the possibility that regular contact with the study team may improve outcomes in participants randomized to the intervention website.
The trial was conducted from October 2014 to September 2015 in Chicago, Illinois; Fort Wayne, Indiana; and Houston, Texas. Inclusion criteria were as follows: age 65 and older, English-speaking, scoring ≥4 questions correctly on the Brief Cognitive Screen,14 and current self-reported use of a computer or smartphone with internet. Participants were excluded if they had previously participated in the focus groups or beta testing of the PYL website. Community-based patient partners/stakeholders drove subject recruitment in their communities through word of mouth, e-mail bursts, newsletters, and flyers. At the Area Agency on Aging and community centers where services such as food vouchers and case management are provided, participants were recruited on-site and given study information. At the clinical sites, staff referred potential participants. Study materials such as flyers and information sheets were also located in the clinic waiting rooms. The Villages, nonprofit, grassroots, membership organizations that are redefining aging by being a key resource to community members wishing to age in place, heavily relied on electronic recruitment using their regular e-newsletters and e-mail lists to recruit potential participants. Potential subjects were also recruited by distributing flyers at local senior centers and senior housing buildings. Interested seniors contacted research staff who explained the study and assessed their eligibility. If eligible, subjects were scheduled for a face-to-face interview.
At the face-to-face encounter, all study subjects completed a written consent, answered baseline questions, and were randomized to either arm. Next, research staff introduced all study subjects to the website to which they were randomized and provided instructions on its use. Staff were present to assist with questions as needed on navigation but did not assist with decision making for either website. A minimum of 15 minutes and a maximum of 45 minutes was allotted for navigating either website. After navigating their website, participants were administered an immediate in-person posttest survey. One month and 3 months after the face-to-face encounter, research staff contacted all study participants over the phone to complete a follow-up survey. Staff attempted to reach participants up to 3 times by phone. Data were entered into Research Electronic Data Capture survey software.15 This study was approved by the Northwestern University Institutional Review Board.
Understanding of Posthospital Discharge and Home Services
As part of the larger trial, which included behavioural outcomes that will be reported elsewhere, we sought to explore the effects of PYL on participants’ knowledge and understanding of posthospital discharge and home services (UHS). Participants were asked to respond to 6 questions at baseline, immediate posttest, and at the 1- and 3-month follow-up time points. Knowledge items were developed by the study team in conjunction with the patient/partner stakeholders. UHS scores were calculated as the sum of the 6 questions (each scored 0 if incorrect and 1 if correct) with a possible range of 0-6.
Covariates
Demographic information, self-reported health, importance of religion, and existence of a power of attorney, living will, advanced directive (eg, Physician Orders for Life-Sustaining Treatment) were obtained via self-report. Participants were asked about their general and social self-efficacy using the validated Self-efficacy Scale16 and their social support using the Lubben Social Network Scale–6.17 Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine–Short Form.18 To measure burden of disease, participant comorbidities were measured using a nonvalidated 9-item dichotomous response condition list, which included some items adapted from the Charlson Comorbidity Index and the Elixhauser Comorbidity Index.
Statistical Analysis
Data analysis included all available data in the intention-to-treat dataset. As UHS was collected at multiple time points up to 3 months postintervention, we employed linear- mixed modeling with random participant effect and fixed arm, time, and time-by-arm interaction terms. The time-by-arm interaction allows for comparison of UHS slopes (or trajectories) across arms. Analyses explored multiple potential covariates, including current utilization of services, physical function, comorbidities, social support, health literacy, self-efficacy, and sociodemographics. Those covariates found to have a significant association (P < 0.05) with outcome were considered for inclusion in the overall model selection process. Ultimately, we developed a final parsimonious, adjusted longitudinal model with primary predictors of time, arm, and their interaction, controlling for only significant baseline variables following a manual backward selection method. All analyses were conducted in SAS software (version 9.4, copyright 2012, The SAS Institute Inc., Cary, North Carolina).
RESULTS
Table 3 illustrates linear mixed model results both failing to adjust and adjusting for potentially influential baseline covariates. In both instances, the interaction term (arm-by-time) was highly significant (P < 0.0001) in predicting UHS score, suggesting that, when compared to the AC arm, the intervention arm exhibited a large mean slope in UHS score over time. That is, understanding home services score tended to increase at a faster rate for those in the active arm. Higher levels of income (P = 0.0191), literacy (P = 0.0036), and education (P = 0.0042) were associated with increased UHS scores; however, male sex (P = 0.0023) and history of high blood pressure (P = 0.0409) or kidney disease (P = 0.0278) were negatively associated with UHS scores.
CONCLUSION/DISCUSSION
The results of our study show that among seniors, PYL improved their understanding of home-based services and the services that may be required following a hospitalization. Educating seniors about what to expect regarding the transition home from a hospital before a hospitalization even occurs may enable seniors and their families to plan ahead instead of reacting to a hospitalization. PYL, a national, publicly available tool with links to local resources may potentially help in advancing transitional discharge care to prior to a hospitalization.
To our knowledge, this is one of the first websites and trials devoted to planning for seniors’ health trajectory as they age into their 70s, 80s, 90s, and 100s. Clinicians regularly discuss code status and powers of attorney during their end-of-life discussions with patients. We encourage clinicians to ask patients, “What about the 10 to 20 years before you die? Have you considered what you will do if you get sick or need help at home?” While not replacing a social worker, the ability of PYL to connect seniors to local resources makes it somewhat of a “virtual social worker.” With many physician practices unable to afford social workers, PYL provides a free-of-charge means of connecting seniors to area resources.
The study participants were in general white, educated, and in reasonably good health. This may be a limitation of this study given that it could impact the generalizability of the study results, as we are unable to know for certain if these same results would be observed with participants who have lower educational levels and are in poor health. Power considerations in this study did not account for comparison of outcomes within specific subgroups so we were unable to assess outcomes in groups such as those with limited health literacy, low social support, or low self-efficacy. The trial was also limited by our inability to collect information on whether or not the knowledge gains observed in the study led to any measureable outcomes. Due to the relatively short follow-up time, we were unable to ascertain whether any study participants were hospitalized during the study follow-up period and if so, if exposure to PYL had any impact on patient anxiety, length of hospital stay, and/or caregiver burden. We were also unable to assess patients’ ability to utilize and carry out their posthospitalization discharge plans if they had one in place. Future studies with longer follow-up are needed to determine these important, measurable outcomes.
Potential implications of planning for a senior’s lifespan are expansive. If hospitalized seniors knew their preferred SNF for subacute rehabilitation on the first day of their hospitalization, hospital lengths of stay could potentially be reduced. If families knew which caregiver agencies, Area Agency on Aging, or Village their senior wished to use, obtaining services would perhaps be easier to accomplish.
Acknowledgments
This work was supported through a Patient-Centered Outcomes Research Institute Award (IH-12-11-4259). Dr. Lindquist and Dr. Ciolino had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Research reported in this publication was also supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR000150.
Disclaimer
All statements in this manuscript, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors or Methodology Committee, or the National Institutes of Health.
Disclosure: The authors have nothing to report.
When seniors are discharged from the hospital, many will require additional support and therapy to regain their independence and return safely home.1,2 Most seniors do not understand what their support needs will entail or the differences between therapy choices.3 To complicate the issue, seniors are often incapacitated and unable to make discharge selections for themselves.
Consequently, discharge planners and social workers often explain options to family members and loved ones, who frequently feel overwhelmed.4,5 While often balancing jobs, loved ones are divided between wanting to stay with the senior in the hospital and driving to area skilled nursing facilities (SNFs) for consideration. Discharges are delayed waiting for families to make visits and choose an SNF. Longer lengths of stay are detrimental to seniors due to the increased risks of infection, functional loss, and cognitive decline.6
Although seniors comprised only 12% of the US population in 2003,7 they accounted for one-third of all hospitalizations, over 13.2 million hospital stays.8 Hospital stays for seniors resulted in hospital charges totaling nearly $329 billion, or 43.6% of national hospital bills in 2003.7 Seniors are also high consumers of postacute care services. By 2050, the number of individuals using long-term care services in any setting (eg, at home, assisted living, or SNFs) will be close to 27 million.9-11 With the knowledge that many seniors will be hospitalized and subsequently require services thereafter, we sought to assist seniors in planning for their hospital discharge needs before they were hospitalized.
Our team developed PlanYourLifespan.org (PYL) to facilitate this planning for postdischarge needs and fill the knowledge gap in understanding postdischarge options. With funding from the Patient Centered Outcomes Research Institute, we aimed to test the effectiveness of PYL on improving knowledge of hospital discharge resources among seniors.
METHODS
PlanYourLifespan.org
PlanYourLifespan.org (PYL) educates users on the health crises that often occur with age and connects them to posthospital and home-based resources available locally and nationally. PYL is personalized, dynamic, and adaptable in that all the information can be changed per the senior’s wishes or changing health needs.
Content of PYL
Previously, we conducted focus groups with seniors about current and perceived home needs and aging-in-place. Major themes of what advanced life events (ALEs) would impact aging-in-place were identified as follows: hospitalizations, falls, and Alzheimer’s.12 We organized PYL around these health-related ALEs. Our multidisciplinary team of researchers, seniors, social workers, caregiver agencies, and Area Agencies on Aging representatives then determined what information and resources should be included.
Each section of PYL starts with a video of a senior discussing their real-life personal experiences, with subsections providing interactive information on what seniors can expect, types of resources available to support home needs, and choices to be made. Descriptions of types of settings for therapy, options available, and links to national/local resources (eg, quality indicators for SNFs) are also included. For example, by entering their zip code, users can identify their neighborhood SNFs, closest Area Agency on Aging, and what home caregiver agencies exist in their area.
Users can save their preferences and revisit their choices at any time. To support communication between seniors and their loved ones, a summary of their choices can be printed or e-mailed to relevant parties. For example, a senior uses PYL and can e-mail these choices to family members, which can stimulate a conversation about future posthospital care expectations.
As inadequate health literacy and cognitive impairment are prevalent among seniors, PYL presents information understandable at all levels of health literacy and sensitive to cognitive load.9 There is simplified, large-font, no mouse scrolling and audio available for the visually impaired.
Study Design and Randomization
To test PYL, a 2-armed (attention control [AC] and PYL intervention), parallel, randomized controlled trial was conducted. Participants were randomly assigned to 1 of the 2 conditions via a pregenerated central randomization list using equal (1:1) allocation and random permuted block design to ensure relatively equal allocation throughout the study. The AC condition exposed participants to the National Institute on Aging-sponsored website, Go4Life.nia.nih.gov, an educational website on physical activity for seniors. This website has comparable design and layout to PYL but does not include information about advanced planning. The AC condition controlled for the possibility that regular contact with the study team may improve outcomes in participants randomized to the intervention website.
The trial was conducted from October 2014 to September 2015 in Chicago, Illinois; Fort Wayne, Indiana; and Houston, Texas. Inclusion criteria were as follows: age 65 and older, English-speaking, scoring ≥4 questions correctly on the Brief Cognitive Screen,14 and current self-reported use of a computer or smartphone with internet. Participants were excluded if they had previously participated in the focus groups or beta testing of the PYL website. Community-based patient partners/stakeholders drove subject recruitment in their communities through word of mouth, e-mail bursts, newsletters, and flyers. At the Area Agency on Aging and community centers where services such as food vouchers and case management are provided, participants were recruited on-site and given study information. At the clinical sites, staff referred potential participants. Study materials such as flyers and information sheets were also located in the clinic waiting rooms. The Villages, nonprofit, grassroots, membership organizations that are redefining aging by being a key resource to community members wishing to age in place, heavily relied on electronic recruitment using their regular e-newsletters and e-mail lists to recruit potential participants. Potential subjects were also recruited by distributing flyers at local senior centers and senior housing buildings. Interested seniors contacted research staff who explained the study and assessed their eligibility. If eligible, subjects were scheduled for a face-to-face interview.
At the face-to-face encounter, all study subjects completed a written consent, answered baseline questions, and were randomized to either arm. Next, research staff introduced all study subjects to the website to which they were randomized and provided instructions on its use. Staff were present to assist with questions as needed on navigation but did not assist with decision making for either website. A minimum of 15 minutes and a maximum of 45 minutes was allotted for navigating either website. After navigating their website, participants were administered an immediate in-person posttest survey. One month and 3 months after the face-to-face encounter, research staff contacted all study participants over the phone to complete a follow-up survey. Staff attempted to reach participants up to 3 times by phone. Data were entered into Research Electronic Data Capture survey software.15 This study was approved by the Northwestern University Institutional Review Board.
Understanding of Posthospital Discharge and Home Services
As part of the larger trial, which included behavioural outcomes that will be reported elsewhere, we sought to explore the effects of PYL on participants’ knowledge and understanding of posthospital discharge and home services (UHS). Participants were asked to respond to 6 questions at baseline, immediate posttest, and at the 1- and 3-month follow-up time points. Knowledge items were developed by the study team in conjunction with the patient/partner stakeholders. UHS scores were calculated as the sum of the 6 questions (each scored 0 if incorrect and 1 if correct) with a possible range of 0-6.
Covariates
Demographic information, self-reported health, importance of religion, and existence of a power of attorney, living will, advanced directive (eg, Physician Orders for Life-Sustaining Treatment) were obtained via self-report. Participants were asked about their general and social self-efficacy using the validated Self-efficacy Scale16 and their social support using the Lubben Social Network Scale–6.17 Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine–Short Form.18 To measure burden of disease, participant comorbidities were measured using a nonvalidated 9-item dichotomous response condition list, which included some items adapted from the Charlson Comorbidity Index and the Elixhauser Comorbidity Index.
Statistical Analysis
Data analysis included all available data in the intention-to-treat dataset. As UHS was collected at multiple time points up to 3 months postintervention, we employed linear- mixed modeling with random participant effect and fixed arm, time, and time-by-arm interaction terms. The time-by-arm interaction allows for comparison of UHS slopes (or trajectories) across arms. Analyses explored multiple potential covariates, including current utilization of services, physical function, comorbidities, social support, health literacy, self-efficacy, and sociodemographics. Those covariates found to have a significant association (P < 0.05) with outcome were considered for inclusion in the overall model selection process. Ultimately, we developed a final parsimonious, adjusted longitudinal model with primary predictors of time, arm, and their interaction, controlling for only significant baseline variables following a manual backward selection method. All analyses were conducted in SAS software (version 9.4, copyright 2012, The SAS Institute Inc., Cary, North Carolina).
RESULTS
Table 3 illustrates linear mixed model results both failing to adjust and adjusting for potentially influential baseline covariates. In both instances, the interaction term (arm-by-time) was highly significant (P < 0.0001) in predicting UHS score, suggesting that, when compared to the AC arm, the intervention arm exhibited a large mean slope in UHS score over time. That is, understanding home services score tended to increase at a faster rate for those in the active arm. Higher levels of income (P = 0.0191), literacy (P = 0.0036), and education (P = 0.0042) were associated with increased UHS scores; however, male sex (P = 0.0023) and history of high blood pressure (P = 0.0409) or kidney disease (P = 0.0278) were negatively associated with UHS scores.
CONCLUSION/DISCUSSION
The results of our study show that among seniors, PYL improved their understanding of home-based services and the services that may be required following a hospitalization. Educating seniors about what to expect regarding the transition home from a hospital before a hospitalization even occurs may enable seniors and their families to plan ahead instead of reacting to a hospitalization. PYL, a national, publicly available tool with links to local resources may potentially help in advancing transitional discharge care to prior to a hospitalization.
To our knowledge, this is one of the first websites and trials devoted to planning for seniors’ health trajectory as they age into their 70s, 80s, 90s, and 100s. Clinicians regularly discuss code status and powers of attorney during their end-of-life discussions with patients. We encourage clinicians to ask patients, “What about the 10 to 20 years before you die? Have you considered what you will do if you get sick or need help at home?” While not replacing a social worker, the ability of PYL to connect seniors to local resources makes it somewhat of a “virtual social worker.” With many physician practices unable to afford social workers, PYL provides a free-of-charge means of connecting seniors to area resources.
The study participants were in general white, educated, and in reasonably good health. This may be a limitation of this study given that it could impact the generalizability of the study results, as we are unable to know for certain if these same results would be observed with participants who have lower educational levels and are in poor health. Power considerations in this study did not account for comparison of outcomes within specific subgroups so we were unable to assess outcomes in groups such as those with limited health literacy, low social support, or low self-efficacy. The trial was also limited by our inability to collect information on whether or not the knowledge gains observed in the study led to any measureable outcomes. Due to the relatively short follow-up time, we were unable to ascertain whether any study participants were hospitalized during the study follow-up period and if so, if exposure to PYL had any impact on patient anxiety, length of hospital stay, and/or caregiver burden. We were also unable to assess patients’ ability to utilize and carry out their posthospitalization discharge plans if they had one in place. Future studies with longer follow-up are needed to determine these important, measurable outcomes.
Potential implications of planning for a senior’s lifespan are expansive. If hospitalized seniors knew their preferred SNF for subacute rehabilitation on the first day of their hospitalization, hospital lengths of stay could potentially be reduced. If families knew which caregiver agencies, Area Agency on Aging, or Village their senior wished to use, obtaining services would perhaps be easier to accomplish.
Acknowledgments
This work was supported through a Patient-Centered Outcomes Research Institute Award (IH-12-11-4259). Dr. Lindquist and Dr. Ciolino had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Research reported in this publication was also supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR000150.
Disclaimer
All statements in this manuscript, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors or Methodology Committee, or the National Institutes of Health.
Disclosure: The authors have nothing to report.
1. Campbell SE, Seymour DG, Primrose WR, ACMEPLUS Project. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing. 2004;33:110-115. PubMed
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004; 70:345-349. PubMed
3. Kane RL Finding the right level of posthospital care: “We didn’t realize there was any other option for him”. JAMA. 2011;305(3):284-293. PubMed
4. Shepperd S, McClaran J, Phillips CO, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;(1):CD000313. PubMed
5. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173:1715-1722. PubMed
6. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. PubMed
7. U.S. Census Bureau, Population Division, Census 2003. https://www.census.gov/programs-surveys/saipe/data/datasets.2003.html. Originally accessed September 1, 2016.
8. Russo, C. A., Elixhauser, A. Hospitalizations in the Elderly Population, 2003. Statistical Brief #6. May 2006. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb6.pdf. Accessed September 1, 2017.
9 U.S. Department of Health and Human Services, and U.S. Department of Labor. The future supply of long-term care workers in relation to the aging baby boom generation: Report to Congress. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, 2003. http:aspe.hhs.gov/daltcp/reports/ltcwork.htm. Accessed September 1, 2016.
10. The Henry J. Kaiser Foundation. Long-term Care: Medicaid’s role and challenges [Publication #2172]. Washington, DC: 1999.
11. AARP. Beyond 50.2003: A Report to the Nation on Independent Living and Disability, 2003, http://www.aarp.org/research/health/disabilities/aresearch-import-753.html. Accessed September 1, 2016.
12. Lindquist LA, Ramirez-Zohfeld V, Sunkara P, et al. Advanced Life Events (ALEs) that Impede Aging-in-Place among Seniors. Arch Gerontol Geriatrs. 2016;64:90-95. PubMed
13. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. Philadelphia, PA: JB Lippincott Co.; 1996.
14. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771-781. PubMed
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Gonzalez J, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self Efficacy Scale: Construction and Validation. Psychol Rep. 1982;51(3):663-671.
17. Lubben JE. Assessing social networks among elderly populations. Fam Community Health. 1988;11(3):42-52.
18. Arozullah AM, Yarnold PR, Bennett CL, et al. Development and validation of the Rapid Estimate of Adult Literacy in Medicine. Medical Care. 2007;45(11):1026-1033. PubMed
1. Campbell SE, Seymour DG, Primrose WR, ACMEPLUS Project. A systematic literature review of factors affecting outcome in older medical patients admitted to hospital. Age Ageing. 2004;33:110-115. PubMed
2. Forster AJ, Clark HD, Menard A, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004; 70:345-349. PubMed
3. Kane RL Finding the right level of posthospital care: “We didn’t realize there was any other option for him”. JAMA. 2011;305(3):284-293. PubMed
4. Shepperd S, McClaran J, Phillips CO, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev. 2010;(1):CD000313. PubMed
5. Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173:1715-1722. PubMed
6. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219-223. PubMed
7. U.S. Census Bureau, Population Division, Census 2003. https://www.census.gov/programs-surveys/saipe/data/datasets.2003.html. Originally accessed September 1, 2016.
8. Russo, C. A., Elixhauser, A. Hospitalizations in the Elderly Population, 2003. Statistical Brief #6. May 2006. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb6.pdf. Accessed September 1, 2017.
9 U.S. Department of Health and Human Services, and U.S. Department of Labor. The future supply of long-term care workers in relation to the aging baby boom generation: Report to Congress. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, 2003. http:aspe.hhs.gov/daltcp/reports/ltcwork.htm. Accessed September 1, 2016.
10. The Henry J. Kaiser Foundation. Long-term Care: Medicaid’s role and challenges [Publication #2172]. Washington, DC: 1999.
11. AARP. Beyond 50.2003: A Report to the Nation on Independent Living and Disability, 2003, http://www.aarp.org/research/health/disabilities/aresearch-import-753.html. Accessed September 1, 2016.
12. Lindquist LA, Ramirez-Zohfeld V, Sunkara P, et al. Advanced Life Events (ALEs) that Impede Aging-in-Place among Seniors. Arch Gerontol Geriatrs. 2016;64:90-95. PubMed
13. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. Philadelphia, PA: JB Lippincott Co.; 1996.
14. Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771-781. PubMed
15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Gonzalez J, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. PubMed
16. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self Efficacy Scale: Construction and Validation. Psychol Rep. 1982;51(3):663-671.
17. Lubben JE. Assessing social networks among elderly populations. Fam Community Health. 1988;11(3):42-52.
18. Arozullah AM, Yarnold PR, Bennett CL, et al. Development and validation of the Rapid Estimate of Adult Literacy in Medicine. Medical Care. 2007;45(11):1026-1033. PubMed
© 2017 Society of Hospital Medicine
PCP Communication at Hospital Discharge
Medication errors occur frequently when patients transition care between providers, such as the transition from hospital to home.[1] Approximately 50% of about 3 million adults per year over 65 years of age transitioning from hospital to home experience a medication discrepancy.[1] At hospital discharge, patients with complex medical problems are prescribed multiple medications with complex dosing and schedules. To add to this complexity, many patients also have cognitive impairment, variable health literacy, and limited social and financial support. Patients with medication discrepancies have significantly higher rates of rehospitalization compared to those without medication discrepancies.[2] Thus, interventions that focus on patients at greater risk of medication discrepancies may identify those at greater risk of subsequent rehospitalization and potentially reduce the rates of readmissions.[3]
There is limited evidence to date on the effectiveness of interventions to decrease post‐hospitalization medication discrepancies.[3, 4, 5, 6] Previous transitional care interventions have been expensive and difficult to sustain due to the need for multiple additional transitional care personnel (e.g., care managers, nurses, pharmacists, transitional care coaches).[7, 8, 9, 10] Moreover, these additional personnel may further fragment the care of hospitalized patients with additional handoffs.
As both hospitalists and outpatient primary care physicians (PCPs) are being expected to care for larger numbers of increasingly sicker patients, the communication handoff of patient information at discharge remains a challenge.[11] Both patients and PCPs often obtain incomplete or inaccurate information and instructions at discharge. Follow‐up appointments are often missed or delayed.[12] Many hospital‐based interventions do not directly involve the PCP or take advantage of the already established PCPpatient relationship.
We conducted a pilot study examining whether enhancing PCP communication with patients at hospital discharge would impact medication discrepancies and improve the safety of the patient as they transitioned home from the hospital.
METHODS
Recruitment of Subjects
The institutional review board of Northwestern University approved this study. Accessing the hospital electronic health record, research staff queried admission information and contacted the hospital physician to determine potential subject eligibility. Research staff recruited consecutive community‐dwelling adults aged 18 years and older who were hospitalized to the acute medicine services at Northwestern Memorial Hospital and being discharged to their home. The patients recruited had PCPs from practices in the Research and Education for Academic Achievement (REACH) Practice‐Based Research Network. The REACH Practice‐Based Research Network consists of 8 academic, private, and community‐based provider groups affiliated with Northwestern Memorial Hospital and the Northwestern University Feinberg School of Medicine. Subjects were excluded if they (1) were unable to consent to their own procedures while hospitalized, (2) were severely vision impaired that could not be corrected with glasses (because they would be administered tests requiring adequate vision), (3) were reliant on a caregiver or home aide services 8 hours or greater per day, (4) were enrolled in hospice, (5) spoke a language other than English or Spanish, (6) were expected to have a hospital length of stay of <24 hours, or (7) were on <5 outpatient medications prior to hospitalization.
Initial Patient InterviewHospital
Research staff conducted structured in‐person surveys of eligible hospitalized subjects in the private hospital rooms of subjects to maintain confidentiality. Subjects received $20 compensation for their participation. After written informed consent was obtained, research staff obtained demographic information from the subject as well as ascertained their availability in 48 hours, support system, medications, and PCP. Research staff then administered the Short Test of Functional Health Literacy in Adults (sTOFHLA) to determine health literacy.[13] All research staff received the same training on administering the cognitive testing. The survey lasted between 20 and 30 minutes. At hospital discharge, the medication list was obtained from the discharge instructions listed in the patient's electronic medical record.
The PCP‐Enhanced Discharge Communication Intervention
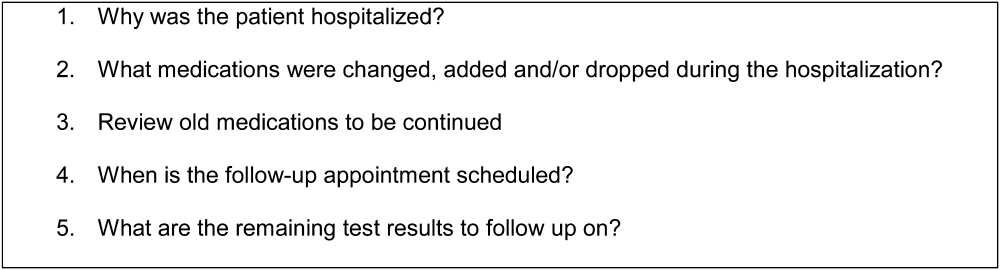
Research staff and the principal investigator met with hospitalists and REACH outpatient physicians in groups to inform them of the study prior to beginning. When the patient was nearing discharge from the hospital, hospitalists were asked to phone the PCP to discuss the patient's discharge plan and facilitate clinical handoffs to the outpatient setting. Research staff paged the hospitalists with the PCP's contact information and reminded them to contact the PCP. Following the hospitalistPCP phone call, the PCP contacted the patient within 24 hours of discharge, either in person while in the hospital or by phone at home. The PCP confirmed medications and clarified any posthospital confusion. The contact flexibility (phone or by person and within 24 hours) was planned as PCPs had other responsibilities that would not allow them to be present at the actual discharge. Physicians were asked to review medications and follow‐up plans, but phone conversations were not recorded. PCPs were given a laminated card that contained points to discuss on discharge (Figure 1). PCPs were compensated with a $5 coffee shop gift card for their time to call patients. This intervention did not involve any additional healthcare personnel.
Postdischarge Phone Interview
During the initial interview, research staff set up a time to contact the subject by phone at 48 hours postdischarge. Research staff contacted the subject at the scheduled time and attempted contact 3 times within 24 hours of scheduled time. During the phone interview, subjects were asked whether they had contact with their PCP to discuss hospital discharge instructions (if so, when) and how satisfied they were with the contact. The subject was also asked whether they were confused with any aspect of the discharge, and if they were, whether the PCP alleviated the confusion. The subjects were asked whether anyone has assisted with their medications, whether they had medication changes, and which medications they were currently taking in the outpatient setting. Both prescription and over‐the‐counter medications were included. Over‐the‐counter medications were included in the study to determine the severity of medication discrepancies if they existed.
The medication list given by the subject was compared with the medical record for the medication list at discharge. Research staff would determine if a discrepancy was present. A discrepancy was considered (1) omission of a medication prescribed at discharge, (2) addition of a medication that was not prescribed at discharge, (3) different dose, (4) different frequency, or (5) duplication of a medication. If discrepancies existed, the subjects were asked for the reason that the discrepancies may have occurred. If discrepancies were identified, subjects were asked to contact their PCP regarding any medication discrepancies and to clarify any issues about medications they had.
Data Analysis
Subjects were categorized into whether they were contacted or not contacted by the PCP within 48 hours of discharge from the hospital. Those who were contacted were defined as those who saw a PCP in person at the time of discharge or within 48 hours of discharge or were called within 48 hours. Those who had an appointment with a PCP after 48 hours of discharge, saw a PCP while hospitalized but did not discuss discharge plan, saw a specialist (such as allergist, urologist, wound care specialist), or who spoke to their PCP but did not discuss their discharge plan were categorized as not contacted.
Reasons for medication discrepancies were categorized into patient‐associated factors (adverse drug effect, intentional nonadherence, unintentional nonadherence) and system‐associated factors (confusion between brand and generic names, discharge instruction incomplete or inaccurate, duplication, incorrect dosage) according to a published medication discrepancy tool.[2] Discrepancies were categorized as intentional nonadherence if patients knew the regimen but decided not to adhere. On the other hand, unintentional nonadherence was used for discrepancies in which patients were unaware of the regimen and thus the discrepancy. Medication discrepancies were classified as mild, moderate, or severe depending on the medication involved. Mild discrepancies were over‐the‐counter medications (eg, acetaminophen, laxatives, multivitamins) and topical creams. Severe discrepancies included medications for heart disease (eg, ‐blockers, calcium channel blockers, angiotensin receptor blockers, diuretics), pulmonary disease (eg, inhalers), diabetes (eg, insulin, glyburide), and antibiotics. Moderate discrepancies were those that did not fit the mild or severe categories (eg, prescription pain medication such as narcotics, anxiety medications, bisphosphonates, muscle relaxants).
Statistical analysis was performed with the SPSS 18.0 (SPSS Inc., Chicago, IL). We analyzed data on study patients to estimate the effect of contact with the PCP within 48 hours of discharge on the frequency of any medication discrepancy. We first examined differences between patients who were contacted or not contacted by patient sociodemographic characteristics. [2] tests were used to analyze the significance of differences in the proportion of medication discrepancies between patients who were contacted and not contacted. Logistic regression analysis was used to test the effect of being contacted on the likelihood of having any prescription medication discrepancy after controlling for patient characteristics (eg, race and ethnicity, age, number of medications, living alone, sex, and TOFHLA score.)
RESULTS
Sample Characteristics
Of the 225 patients who met inclusion criteria, 114 subjects were recruited and interviewed by research staff during the hospital stay and 48 hours after discharge. Due to early discharge and staffing reasons, 27 subjects were not able to be approached during discharge. Of the 84 patients who declined the study, the reasons included: not interested in study (n=58), did not feel well enough to complete or participate (n=16), did not wish study personnel to have access to personal records (n=5), and no reason given (n=5). Of the 114 subjects enrolled in the hospital, 77 subjects completed 48‐hour postdischarge phone interviews with research staff. Two patients had missing data, leaving 75 patients who were included in the analysis.
Study patients' age, race and ethnicity, sex, living situation (alone vs not alone), number of medications, mean sTOFHLA score, and medication discrepancy are summarized in Table 1. Thirty‐six percent of patients (n=27) were contacted by the PCP within 48 hours of discharge. Age, living situation (alone vs not alone), number of medications, and mean sTOFHLA score were similar in both groups of contacted versus noncontacted patients. Of those who were contacted, males made up 48.1% versus 27.1% for those not contacted (P=0.06). Similarly, 44.4% of those who were not contacted were black versus 37.5% among the contacted (P=0.035).
| All Subjects, N=77 | Subject Without PCP Contact, n=50 | Subjects With PCP Contact, n=27 | P Value | |
|---|---|---|---|---|
| ||||
| Mean ageSD, y | 63.012.2 | 63.311.9 | 62.313.1 | 0.74 |
| Race and ethnicity, n (%) | 0.35 | |||
| White/other | 40 (53.5) | 28 (58.3) | 12 (44.4) | |
| Black | 30 (40.0) | 18 (37.5) | 12 (44.4) | |
| Hispanic | 5 (6.7) | 2 (4.2) | 3 (11.1) | |
| Male, n (%) | 26 (34.7) | 13 (27.1) | 13 (48.1) | 0.06 |
| Lives alone, n (%) | 30 (40.0) | 20 (41.7) | 10 (37.0) | 0.69 |
| Mean sTOFHLA scoreSD | 29.67.9 | 29.47.7 | 29.97.8 | 0.75 |
| Mean number of medications | 9.224.9 | 9.064.7 | 9.633.5 | 0.67 |
| Experienced medication discrepancy, n (%) | 39 (52) | 28 (59.3) | 11 (40.7) | 0.14 |
Medication Discrepancies
Of the 75 study patients, 39 patients (50.6%) experienced a total of 84 medication discrepancies. Fifty‐eight medication discrepancies were prescription medications, whereas 25 were over‐the‐counter medications. Of those who had discrepancies, 46.2% (n=18) had 1 discrepancy, 23.1% (n=9) had 2 discrepancies, 12.8% (n=5) had 3 discrepancies, 10.2% (n=4) had 4 discrepancies, and 7.7% (n=3) 5 or more discrepancies. The mean number of discrepancies per patient was 2.15 per patient. Medication discrepancies were categorized by severity based on the safety profile of the medication involved and type discrepancy (Table 2).
| Frequency, n (%) | |
|---|---|
| |
| Type of medication discrepancy | |
| Over the counter | 26 (30.9) |
| Prescription medication | 58 (69.0) |
| Severity of medication discrepancy | |
| Milda | 28 (33.3) |
| Moderateb | 24 (28.6) |
| Severec | 32 (38.1) |
Reasons for Medication Discrepancies
The subject‐provided reasons for medication discrepancies are listed in Table 3 and divided into patient‐ and system‐associated factors. The overall most frequent reason for a discrepancy was the patient's intentional nonadherence. Examples of intentional nonadherence include not sure of purpose of medication, did not recognize drug, did not fill prescription, did not need prescription, and wanted to wait longer, so not taking diuretic daily. The second most frequent reason was inaccurate discharge instructions (e.g., discharge instructions with medication changes denoting no change but incorrect outpatient thyroid medication dosage listed (Table 3).
| Factor | Frequency, n (%) |
|---|---|
| Patient‐associated factors | |
| Adverse drug effects | 8 (9.5) |
| Intentional nonadherence | 50 (59.4) |
| Unintentional nonadherence | 1 (1.2) |
| Subtotal | 59 |
| System‐associated factors | |
| Confusion between brand and generic names | 3 (3.5) |
| Discharge Instructions incomplete or inaccurate | 12 (14.2) |
| Duplication | 3 (3.5) |
| Incorrect dosage | 3 (3.5) |
| Incorrect frequency | 1 (1.2) |
| Conflicting information from different sources | 3 (3.5) |
| Subtotal | 25 |
| Total | 84 |
Logistic Regression Results for the Likelihood of Any Medication Discrepancy
Logistical regression results are shown in Table 4. Patients who were contacted by their PCP at discharge were 70% less likely to have a discrepancy when compared with those who were not contacted (P=0.03). This result was controlled for other possible factors including patient sex. Of interest, men were 3.94 times more likely to have a discrepancy when compared with women (P=0.02). There was also a nonsignificant but potentially important association between higher health literacy, measured continuously (0X) and being more likely to have a discrepancy (P=0.07). Including variables for age, ethnicity, and living alone were nonsignificant and did not change the regression results for contacted patients.
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| ||
| Subject contacted by PCP at Discharge | 0.33 | 0.110.97 |
| Male | 3.98 | 1.2712.49 |
| Number of medications | 1.09 | 0.961.23 |
| TOHFLA score | 1.09 | 1.011.18 |
DISCUSSION
Our results provide evidence that contact with PCPs within 24 hours of hospital discharge can be effective in decreasing medication discrepancies. The PCP‐Enhanced Discharge Communication Intervention was designed to investigate the value of improving existing lines of communication at discharge without involving any additional healthcare personnel. As a lean discharge intervention, the PCP, the hospitalist, and the patient were the main components to this intervention.
This study was limited in that the sample size was small and that we enrolled consecutive patients. Due to the small sample size, we did not examine hospital readmissions. Further studies are needed to examine whether primary care involvement at discharge would affect hospital readmissions. Another limitation of this study was that the control group was not randomized or preselected. Our study compared those subjects who received a phone call from their PCP to those subjects who did not. Although we instructed PCPs with a standardized script, we did not record or ensure that the phone call‐up occurred as such. There is potential variability in how the PCPs conducted their follow‐up with patients, and we are unable to measure what was effective and ineffective in reducing medication discrepancies. Another limitation was that the determination of the severity of the medication discrepancy was done by medication involved as opposed to by physician review and adjudication. The study would have been strengthened by interviewing the outpatient physicians on the amount of harm each discrepancy would or did cause the patient.
The most frequent reason for discrepancy was intentional nonadherence. Prior research has shown that intentional nonadherence of medications at hospital discharge is linked to health literacy.[14] One may postulate that patients with adequate health literacy feel enabled to go against medical advice and chose to not take medications as prescribed.
In our study, patients had the most medication discrepancies in the severe medications category, which involved cardiac, pulmonary, and diabetic medications, compared with the mild and moderate category. This finding may reflect the frequency that these medications are prescribed but are consistent with findings of Coleman et al.[2] The finding highlights the need to ensure adequate education and understanding of medication regimens for these complex patients. Patients with cardiac, pulmonary, and diabetic disease may benefit from personalized discharge instructions and a more structured and organized medication reconciliation process.
Our study found that males were more likely to have a medication discrepancy than females, which has not been found in previous studies on medication discrepancies. One study on Medicare beneficiaries with congestive heart failure found that men were much more likely to be readmitted than woman within 6 months of discharge.[15] The reason for the increased risk of medication discrepancy in males is unknown. Gender differences in health have frequently been reported, with men having higher rates of morbidity and mortality than women.[16, 17] The differences are thought to be due to the reluctance of men to seek medical help and consult medical practitioners when needed. It has been known that women use health services more than men, and are more likely than men to report a chronic illness.[18] When men do present with symptoms, it is often later in the stage of a disease than women and when treatment is less likely to be successful.[19] It may be that men in this study population had more medication discrepancies as they were reluctant to seek help or ask for clarification regarding medications at discharge.
Of those enrolled, 36% of patients were contacted by their PCP within 48 hours of discharge. It is unclear if the PCP attempted but was unable to reach the patient or did not attempt to call the patient. Although PCPs were compensated with a $5 coffee shop gift card, a larger compensation may insure completion of the patient contact. Further research is needed to determine the reasons why PCPs were not able to complete the phone call.
From a policy standpoint, hospitals that focus solely on hospital‐based transition interventions are potentially missing half the problem. The hospital acts as a sender or pitcher, and the PCP acts as a receiver or catcher. The receiver needs to be included in the discharge process for a successful patient transition to home. With recent billing changes for transition coding, the Center for Medicare and Medicaid Services recognizes this relationship.[20] Outpatient PCPs are able to bill for bundled follow‐up phone calls and appointments. Instead of paying additional staff to make 48‐hour postdischarge phone calls, hospitals should consider partnering with PCPs to ensure a more organized discharge.
Our results showed that PCP communication with patients within 24 hours of discharge was associated with decreased medication discrepancies. The PCP is vital to ensuring a safe transition home from the hospital. Because many patients have an established relationship with their PCP, a bond of trust exists that is often missing with hospital‐employed transitional staff. Patients pay attention when a known physician contacts them directly. In our study, patients may have felt comfortable addressing their concerns and questions with their trusted PCP. Subsequently, patients may have been more attuned to the answers their PCP gave and avoided medication errors. Our results further demonstrate the importance of PCP involvement in the hospital discharge process to improve the care of our patients.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , . Posthospital medication discrepancies—prevalence and contributing factors. Arch Intern Med. 2005;165(16):1842–1847.
- , , , et al. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999–1006.
- , , , , . Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee‐for‐service setting. Home Health Care Serv Q. 2009;28(2‐3):84–99.
- , , . Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–1446.
- , , , et al. Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211–218.
- , , , et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187.
- , , , , . A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154(15):1721–1729.
- , , , , , . Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817–1825.
- , , , et al. Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med. 2005;118(10):1148–1153.
- , , , et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385–391.
- , . Hospital readmissions in the Medicare population. N Engl J Med. 1984;311(21):1349–1353.
- , , , , . Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42.
- , , , , , . Relationship of Health Literacy to Intentional and Unintentional Non‐Adherence of Hospital Discharge Medications. J Gen Intern Med. 2012;27(2):173–178.
- , , , et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157(1):99–104.
- . College men's health: an overview and a call to action. J Am Coll Health. 1998;46(6):279–290.
- Gender and the Social Construction of Illness. Thousand Oaks, CA: Sage; 1997.
- Inequalities in Health: The Black Report and the Health Divide. London, UK: Penguin; 1988.
- , , , . Decision making process in people with symptoms of acute myocardial infarction: qualitative study. BMJ. 2002;332:1006–1017.
- Centers for Medicare and Medicaid Services. Transitional Care Management Services. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/PhysicianFeeSched/Downloads/FAQ‐TCMS.pdf. Accessed June 28, 2013.
Medication errors occur frequently when patients transition care between providers, such as the transition from hospital to home.[1] Approximately 50% of about 3 million adults per year over 65 years of age transitioning from hospital to home experience a medication discrepancy.[1] At hospital discharge, patients with complex medical problems are prescribed multiple medications with complex dosing and schedules. To add to this complexity, many patients also have cognitive impairment, variable health literacy, and limited social and financial support. Patients with medication discrepancies have significantly higher rates of rehospitalization compared to those without medication discrepancies.[2] Thus, interventions that focus on patients at greater risk of medication discrepancies may identify those at greater risk of subsequent rehospitalization and potentially reduce the rates of readmissions.[3]
There is limited evidence to date on the effectiveness of interventions to decrease post‐hospitalization medication discrepancies.[3, 4, 5, 6] Previous transitional care interventions have been expensive and difficult to sustain due to the need for multiple additional transitional care personnel (e.g., care managers, nurses, pharmacists, transitional care coaches).[7, 8, 9, 10] Moreover, these additional personnel may further fragment the care of hospitalized patients with additional handoffs.
As both hospitalists and outpatient primary care physicians (PCPs) are being expected to care for larger numbers of increasingly sicker patients, the communication handoff of patient information at discharge remains a challenge.[11] Both patients and PCPs often obtain incomplete or inaccurate information and instructions at discharge. Follow‐up appointments are often missed or delayed.[12] Many hospital‐based interventions do not directly involve the PCP or take advantage of the already established PCPpatient relationship.
We conducted a pilot study examining whether enhancing PCP communication with patients at hospital discharge would impact medication discrepancies and improve the safety of the patient as they transitioned home from the hospital.
METHODS
Recruitment of Subjects
The institutional review board of Northwestern University approved this study. Accessing the hospital electronic health record, research staff queried admission information and contacted the hospital physician to determine potential subject eligibility. Research staff recruited consecutive community‐dwelling adults aged 18 years and older who were hospitalized to the acute medicine services at Northwestern Memorial Hospital and being discharged to their home. The patients recruited had PCPs from practices in the Research and Education for Academic Achievement (REACH) Practice‐Based Research Network. The REACH Practice‐Based Research Network consists of 8 academic, private, and community‐based provider groups affiliated with Northwestern Memorial Hospital and the Northwestern University Feinberg School of Medicine. Subjects were excluded if they (1) were unable to consent to their own procedures while hospitalized, (2) were severely vision impaired that could not be corrected with glasses (because they would be administered tests requiring adequate vision), (3) were reliant on a caregiver or home aide services 8 hours or greater per day, (4) were enrolled in hospice, (5) spoke a language other than English or Spanish, (6) were expected to have a hospital length of stay of <24 hours, or (7) were on <5 outpatient medications prior to hospitalization.
Initial Patient InterviewHospital
Research staff conducted structured in‐person surveys of eligible hospitalized subjects in the private hospital rooms of subjects to maintain confidentiality. Subjects received $20 compensation for their participation. After written informed consent was obtained, research staff obtained demographic information from the subject as well as ascertained their availability in 48 hours, support system, medications, and PCP. Research staff then administered the Short Test of Functional Health Literacy in Adults (sTOFHLA) to determine health literacy.[13] All research staff received the same training on administering the cognitive testing. The survey lasted between 20 and 30 minutes. At hospital discharge, the medication list was obtained from the discharge instructions listed in the patient's electronic medical record.
The PCP‐Enhanced Discharge Communication Intervention
Research staff and the principal investigator met with hospitalists and REACH outpatient physicians in groups to inform them of the study prior to beginning. When the patient was nearing discharge from the hospital, hospitalists were asked to phone the PCP to discuss the patient's discharge plan and facilitate clinical handoffs to the outpatient setting. Research staff paged the hospitalists with the PCP's contact information and reminded them to contact the PCP. Following the hospitalistPCP phone call, the PCP contacted the patient within 24 hours of discharge, either in person while in the hospital or by phone at home. The PCP confirmed medications and clarified any posthospital confusion. The contact flexibility (phone or by person and within 24 hours) was planned as PCPs had other responsibilities that would not allow them to be present at the actual discharge. Physicians were asked to review medications and follow‐up plans, but phone conversations were not recorded. PCPs were given a laminated card that contained points to discuss on discharge (Figure 1). PCPs were compensated with a $5 coffee shop gift card for their time to call patients. This intervention did not involve any additional healthcare personnel.
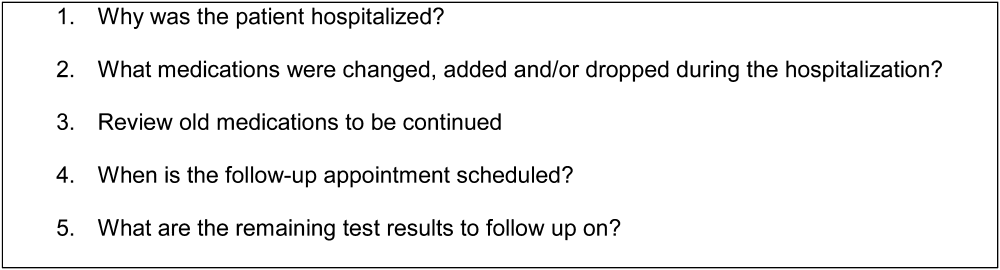
Postdischarge Phone Interview
During the initial interview, research staff set up a time to contact the subject by phone at 48 hours postdischarge. Research staff contacted the subject at the scheduled time and attempted contact 3 times within 24 hours of scheduled time. During the phone interview, subjects were asked whether they had contact with their PCP to discuss hospital discharge instructions (if so, when) and how satisfied they were with the contact. The subject was also asked whether they were confused with any aspect of the discharge, and if they were, whether the PCP alleviated the confusion. The subjects were asked whether anyone has assisted with their medications, whether they had medication changes, and which medications they were currently taking in the outpatient setting. Both prescription and over‐the‐counter medications were included. Over‐the‐counter medications were included in the study to determine the severity of medication discrepancies if they existed.
The medication list given by the subject was compared with the medical record for the medication list at discharge. Research staff would determine if a discrepancy was present. A discrepancy was considered (1) omission of a medication prescribed at discharge, (2) addition of a medication that was not prescribed at discharge, (3) different dose, (4) different frequency, or (5) duplication of a medication. If discrepancies existed, the subjects were asked for the reason that the discrepancies may have occurred. If discrepancies were identified, subjects were asked to contact their PCP regarding any medication discrepancies and to clarify any issues about medications they had.
Data Analysis
Subjects were categorized into whether they were contacted or not contacted by the PCP within 48 hours of discharge from the hospital. Those who were contacted were defined as those who saw a PCP in person at the time of discharge or within 48 hours of discharge or were called within 48 hours. Those who had an appointment with a PCP after 48 hours of discharge, saw a PCP while hospitalized but did not discuss discharge plan, saw a specialist (such as allergist, urologist, wound care specialist), or who spoke to their PCP but did not discuss their discharge plan were categorized as not contacted.
Reasons for medication discrepancies were categorized into patient‐associated factors (adverse drug effect, intentional nonadherence, unintentional nonadherence) and system‐associated factors (confusion between brand and generic names, discharge instruction incomplete or inaccurate, duplication, incorrect dosage) according to a published medication discrepancy tool.[2] Discrepancies were categorized as intentional nonadherence if patients knew the regimen but decided not to adhere. On the other hand, unintentional nonadherence was used for discrepancies in which patients were unaware of the regimen and thus the discrepancy. Medication discrepancies were classified as mild, moderate, or severe depending on the medication involved. Mild discrepancies were over‐the‐counter medications (eg, acetaminophen, laxatives, multivitamins) and topical creams. Severe discrepancies included medications for heart disease (eg, ‐blockers, calcium channel blockers, angiotensin receptor blockers, diuretics), pulmonary disease (eg, inhalers), diabetes (eg, insulin, glyburide), and antibiotics. Moderate discrepancies were those that did not fit the mild or severe categories (eg, prescription pain medication such as narcotics, anxiety medications, bisphosphonates, muscle relaxants).
Statistical analysis was performed with the SPSS 18.0 (SPSS Inc., Chicago, IL). We analyzed data on study patients to estimate the effect of contact with the PCP within 48 hours of discharge on the frequency of any medication discrepancy. We first examined differences between patients who were contacted or not contacted by patient sociodemographic characteristics. [2] tests were used to analyze the significance of differences in the proportion of medication discrepancies between patients who were contacted and not contacted. Logistic regression analysis was used to test the effect of being contacted on the likelihood of having any prescription medication discrepancy after controlling for patient characteristics (eg, race and ethnicity, age, number of medications, living alone, sex, and TOFHLA score.)
RESULTS
Sample Characteristics
Of the 225 patients who met inclusion criteria, 114 subjects were recruited and interviewed by research staff during the hospital stay and 48 hours after discharge. Due to early discharge and staffing reasons, 27 subjects were not able to be approached during discharge. Of the 84 patients who declined the study, the reasons included: not interested in study (n=58), did not feel well enough to complete or participate (n=16), did not wish study personnel to have access to personal records (n=5), and no reason given (n=5). Of the 114 subjects enrolled in the hospital, 77 subjects completed 48‐hour postdischarge phone interviews with research staff. Two patients had missing data, leaving 75 patients who were included in the analysis.
Study patients' age, race and ethnicity, sex, living situation (alone vs not alone), number of medications, mean sTOFHLA score, and medication discrepancy are summarized in Table 1. Thirty‐six percent of patients (n=27) were contacted by the PCP within 48 hours of discharge. Age, living situation (alone vs not alone), number of medications, and mean sTOFHLA score were similar in both groups of contacted versus noncontacted patients. Of those who were contacted, males made up 48.1% versus 27.1% for those not contacted (P=0.06). Similarly, 44.4% of those who were not contacted were black versus 37.5% among the contacted (P=0.035).
| All Subjects, N=77 | Subject Without PCP Contact, n=50 | Subjects With PCP Contact, n=27 | P Value | |
|---|---|---|---|---|
| ||||
| Mean ageSD, y | 63.012.2 | 63.311.9 | 62.313.1 | 0.74 |
| Race and ethnicity, n (%) | 0.35 | |||
| White/other | 40 (53.5) | 28 (58.3) | 12 (44.4) | |
| Black | 30 (40.0) | 18 (37.5) | 12 (44.4) | |
| Hispanic | 5 (6.7) | 2 (4.2) | 3 (11.1) | |
| Male, n (%) | 26 (34.7) | 13 (27.1) | 13 (48.1) | 0.06 |
| Lives alone, n (%) | 30 (40.0) | 20 (41.7) | 10 (37.0) | 0.69 |
| Mean sTOFHLA scoreSD | 29.67.9 | 29.47.7 | 29.97.8 | 0.75 |
| Mean number of medications | 9.224.9 | 9.064.7 | 9.633.5 | 0.67 |
| Experienced medication discrepancy, n (%) | 39 (52) | 28 (59.3) | 11 (40.7) | 0.14 |
Medication Discrepancies
Of the 75 study patients, 39 patients (50.6%) experienced a total of 84 medication discrepancies. Fifty‐eight medication discrepancies were prescription medications, whereas 25 were over‐the‐counter medications. Of those who had discrepancies, 46.2% (n=18) had 1 discrepancy, 23.1% (n=9) had 2 discrepancies, 12.8% (n=5) had 3 discrepancies, 10.2% (n=4) had 4 discrepancies, and 7.7% (n=3) 5 or more discrepancies. The mean number of discrepancies per patient was 2.15 per patient. Medication discrepancies were categorized by severity based on the safety profile of the medication involved and type discrepancy (Table 2).
| Frequency, n (%) | |
|---|---|
| |
| Type of medication discrepancy | |
| Over the counter | 26 (30.9) |
| Prescription medication | 58 (69.0) |
| Severity of medication discrepancy | |
| Milda | 28 (33.3) |
| Moderateb | 24 (28.6) |
| Severec | 32 (38.1) |
Reasons for Medication Discrepancies
The subject‐provided reasons for medication discrepancies are listed in Table 3 and divided into patient‐ and system‐associated factors. The overall most frequent reason for a discrepancy was the patient's intentional nonadherence. Examples of intentional nonadherence include not sure of purpose of medication, did not recognize drug, did not fill prescription, did not need prescription, and wanted to wait longer, so not taking diuretic daily. The second most frequent reason was inaccurate discharge instructions (e.g., discharge instructions with medication changes denoting no change but incorrect outpatient thyroid medication dosage listed (Table 3).
| Factor | Frequency, n (%) |
|---|---|
| Patient‐associated factors | |
| Adverse drug effects | 8 (9.5) |
| Intentional nonadherence | 50 (59.4) |
| Unintentional nonadherence | 1 (1.2) |
| Subtotal | 59 |
| System‐associated factors | |
| Confusion between brand and generic names | 3 (3.5) |
| Discharge Instructions incomplete or inaccurate | 12 (14.2) |
| Duplication | 3 (3.5) |
| Incorrect dosage | 3 (3.5) |
| Incorrect frequency | 1 (1.2) |
| Conflicting information from different sources | 3 (3.5) |
| Subtotal | 25 |
| Total | 84 |
Logistic Regression Results for the Likelihood of Any Medication Discrepancy
Logistical regression results are shown in Table 4. Patients who were contacted by their PCP at discharge were 70% less likely to have a discrepancy when compared with those who were not contacted (P=0.03). This result was controlled for other possible factors including patient sex. Of interest, men were 3.94 times more likely to have a discrepancy when compared with women (P=0.02). There was also a nonsignificant but potentially important association between higher health literacy, measured continuously (0X) and being more likely to have a discrepancy (P=0.07). Including variables for age, ethnicity, and living alone were nonsignificant and did not change the regression results for contacted patients.
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| ||
| Subject contacted by PCP at Discharge | 0.33 | 0.110.97 |
| Male | 3.98 | 1.2712.49 |
| Number of medications | 1.09 | 0.961.23 |
| TOHFLA score | 1.09 | 1.011.18 |
DISCUSSION
Our results provide evidence that contact with PCPs within 24 hours of hospital discharge can be effective in decreasing medication discrepancies. The PCP‐Enhanced Discharge Communication Intervention was designed to investigate the value of improving existing lines of communication at discharge without involving any additional healthcare personnel. As a lean discharge intervention, the PCP, the hospitalist, and the patient were the main components to this intervention.
This study was limited in that the sample size was small and that we enrolled consecutive patients. Due to the small sample size, we did not examine hospital readmissions. Further studies are needed to examine whether primary care involvement at discharge would affect hospital readmissions. Another limitation of this study was that the control group was not randomized or preselected. Our study compared those subjects who received a phone call from their PCP to those subjects who did not. Although we instructed PCPs with a standardized script, we did not record or ensure that the phone call‐up occurred as such. There is potential variability in how the PCPs conducted their follow‐up with patients, and we are unable to measure what was effective and ineffective in reducing medication discrepancies. Another limitation was that the determination of the severity of the medication discrepancy was done by medication involved as opposed to by physician review and adjudication. The study would have been strengthened by interviewing the outpatient physicians on the amount of harm each discrepancy would or did cause the patient.
The most frequent reason for discrepancy was intentional nonadherence. Prior research has shown that intentional nonadherence of medications at hospital discharge is linked to health literacy.[14] One may postulate that patients with adequate health literacy feel enabled to go against medical advice and chose to not take medications as prescribed.
In our study, patients had the most medication discrepancies in the severe medications category, which involved cardiac, pulmonary, and diabetic medications, compared with the mild and moderate category. This finding may reflect the frequency that these medications are prescribed but are consistent with findings of Coleman et al.[2] The finding highlights the need to ensure adequate education and understanding of medication regimens for these complex patients. Patients with cardiac, pulmonary, and diabetic disease may benefit from personalized discharge instructions and a more structured and organized medication reconciliation process.
Our study found that males were more likely to have a medication discrepancy than females, which has not been found in previous studies on medication discrepancies. One study on Medicare beneficiaries with congestive heart failure found that men were much more likely to be readmitted than woman within 6 months of discharge.[15] The reason for the increased risk of medication discrepancy in males is unknown. Gender differences in health have frequently been reported, with men having higher rates of morbidity and mortality than women.[16, 17] The differences are thought to be due to the reluctance of men to seek medical help and consult medical practitioners when needed. It has been known that women use health services more than men, and are more likely than men to report a chronic illness.[18] When men do present with symptoms, it is often later in the stage of a disease than women and when treatment is less likely to be successful.[19] It may be that men in this study population had more medication discrepancies as they were reluctant to seek help or ask for clarification regarding medications at discharge.
Of those enrolled, 36% of patients were contacted by their PCP within 48 hours of discharge. It is unclear if the PCP attempted but was unable to reach the patient or did not attempt to call the patient. Although PCPs were compensated with a $5 coffee shop gift card, a larger compensation may insure completion of the patient contact. Further research is needed to determine the reasons why PCPs were not able to complete the phone call.
From a policy standpoint, hospitals that focus solely on hospital‐based transition interventions are potentially missing half the problem. The hospital acts as a sender or pitcher, and the PCP acts as a receiver or catcher. The receiver needs to be included in the discharge process for a successful patient transition to home. With recent billing changes for transition coding, the Center for Medicare and Medicaid Services recognizes this relationship.[20] Outpatient PCPs are able to bill for bundled follow‐up phone calls and appointments. Instead of paying additional staff to make 48‐hour postdischarge phone calls, hospitals should consider partnering with PCPs to ensure a more organized discharge.
Our results showed that PCP communication with patients within 24 hours of discharge was associated with decreased medication discrepancies. The PCP is vital to ensuring a safe transition home from the hospital. Because many patients have an established relationship with their PCP, a bond of trust exists that is often missing with hospital‐employed transitional staff. Patients pay attention when a known physician contacts them directly. In our study, patients may have felt comfortable addressing their concerns and questions with their trusted PCP. Subsequently, patients may have been more attuned to the answers their PCP gave and avoided medication errors. Our results further demonstrate the importance of PCP involvement in the hospital discharge process to improve the care of our patients.
Medication errors occur frequently when patients transition care between providers, such as the transition from hospital to home.[1] Approximately 50% of about 3 million adults per year over 65 years of age transitioning from hospital to home experience a medication discrepancy.[1] At hospital discharge, patients with complex medical problems are prescribed multiple medications with complex dosing and schedules. To add to this complexity, many patients also have cognitive impairment, variable health literacy, and limited social and financial support. Patients with medication discrepancies have significantly higher rates of rehospitalization compared to those without medication discrepancies.[2] Thus, interventions that focus on patients at greater risk of medication discrepancies may identify those at greater risk of subsequent rehospitalization and potentially reduce the rates of readmissions.[3]
There is limited evidence to date on the effectiveness of interventions to decrease post‐hospitalization medication discrepancies.[3, 4, 5, 6] Previous transitional care interventions have been expensive and difficult to sustain due to the need for multiple additional transitional care personnel (e.g., care managers, nurses, pharmacists, transitional care coaches).[7, 8, 9, 10] Moreover, these additional personnel may further fragment the care of hospitalized patients with additional handoffs.
As both hospitalists and outpatient primary care physicians (PCPs) are being expected to care for larger numbers of increasingly sicker patients, the communication handoff of patient information at discharge remains a challenge.[11] Both patients and PCPs often obtain incomplete or inaccurate information and instructions at discharge. Follow‐up appointments are often missed or delayed.[12] Many hospital‐based interventions do not directly involve the PCP or take advantage of the already established PCPpatient relationship.
We conducted a pilot study examining whether enhancing PCP communication with patients at hospital discharge would impact medication discrepancies and improve the safety of the patient as they transitioned home from the hospital.
METHODS
Recruitment of Subjects
The institutional review board of Northwestern University approved this study. Accessing the hospital electronic health record, research staff queried admission information and contacted the hospital physician to determine potential subject eligibility. Research staff recruited consecutive community‐dwelling adults aged 18 years and older who were hospitalized to the acute medicine services at Northwestern Memorial Hospital and being discharged to their home. The patients recruited had PCPs from practices in the Research and Education for Academic Achievement (REACH) Practice‐Based Research Network. The REACH Practice‐Based Research Network consists of 8 academic, private, and community‐based provider groups affiliated with Northwestern Memorial Hospital and the Northwestern University Feinberg School of Medicine. Subjects were excluded if they (1) were unable to consent to their own procedures while hospitalized, (2) were severely vision impaired that could not be corrected with glasses (because they would be administered tests requiring adequate vision), (3) were reliant on a caregiver or home aide services 8 hours or greater per day, (4) were enrolled in hospice, (5) spoke a language other than English or Spanish, (6) were expected to have a hospital length of stay of <24 hours, or (7) were on <5 outpatient medications prior to hospitalization.
Initial Patient InterviewHospital
Research staff conducted structured in‐person surveys of eligible hospitalized subjects in the private hospital rooms of subjects to maintain confidentiality. Subjects received $20 compensation for their participation. After written informed consent was obtained, research staff obtained demographic information from the subject as well as ascertained their availability in 48 hours, support system, medications, and PCP. Research staff then administered the Short Test of Functional Health Literacy in Adults (sTOFHLA) to determine health literacy.[13] All research staff received the same training on administering the cognitive testing. The survey lasted between 20 and 30 minutes. At hospital discharge, the medication list was obtained from the discharge instructions listed in the patient's electronic medical record.
The PCP‐Enhanced Discharge Communication Intervention
Research staff and the principal investigator met with hospitalists and REACH outpatient physicians in groups to inform them of the study prior to beginning. When the patient was nearing discharge from the hospital, hospitalists were asked to phone the PCP to discuss the patient's discharge plan and facilitate clinical handoffs to the outpatient setting. Research staff paged the hospitalists with the PCP's contact information and reminded them to contact the PCP. Following the hospitalistPCP phone call, the PCP contacted the patient within 24 hours of discharge, either in person while in the hospital or by phone at home. The PCP confirmed medications and clarified any posthospital confusion. The contact flexibility (phone or by person and within 24 hours) was planned as PCPs had other responsibilities that would not allow them to be present at the actual discharge. Physicians were asked to review medications and follow‐up plans, but phone conversations were not recorded. PCPs were given a laminated card that contained points to discuss on discharge (Figure 1). PCPs were compensated with a $5 coffee shop gift card for their time to call patients. This intervention did not involve any additional healthcare personnel.
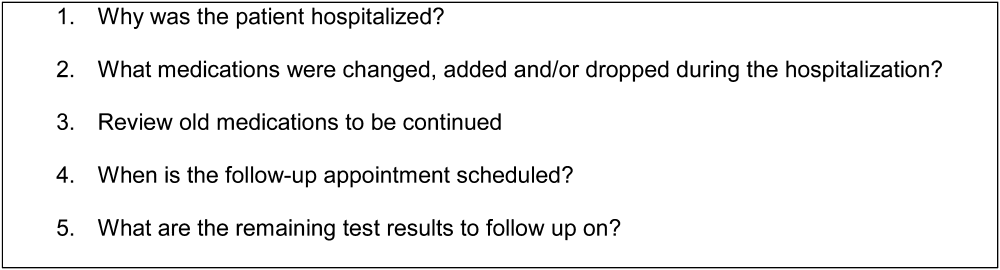
Postdischarge Phone Interview
During the initial interview, research staff set up a time to contact the subject by phone at 48 hours postdischarge. Research staff contacted the subject at the scheduled time and attempted contact 3 times within 24 hours of scheduled time. During the phone interview, subjects were asked whether they had contact with their PCP to discuss hospital discharge instructions (if so, when) and how satisfied they were with the contact. The subject was also asked whether they were confused with any aspect of the discharge, and if they were, whether the PCP alleviated the confusion. The subjects were asked whether anyone has assisted with their medications, whether they had medication changes, and which medications they were currently taking in the outpatient setting. Both prescription and over‐the‐counter medications were included. Over‐the‐counter medications were included in the study to determine the severity of medication discrepancies if they existed.
The medication list given by the subject was compared with the medical record for the medication list at discharge. Research staff would determine if a discrepancy was present. A discrepancy was considered (1) omission of a medication prescribed at discharge, (2) addition of a medication that was not prescribed at discharge, (3) different dose, (4) different frequency, or (5) duplication of a medication. If discrepancies existed, the subjects were asked for the reason that the discrepancies may have occurred. If discrepancies were identified, subjects were asked to contact their PCP regarding any medication discrepancies and to clarify any issues about medications they had.
Data Analysis
Subjects were categorized into whether they were contacted or not contacted by the PCP within 48 hours of discharge from the hospital. Those who were contacted were defined as those who saw a PCP in person at the time of discharge or within 48 hours of discharge or were called within 48 hours. Those who had an appointment with a PCP after 48 hours of discharge, saw a PCP while hospitalized but did not discuss discharge plan, saw a specialist (such as allergist, urologist, wound care specialist), or who spoke to their PCP but did not discuss their discharge plan were categorized as not contacted.
Reasons for medication discrepancies were categorized into patient‐associated factors (adverse drug effect, intentional nonadherence, unintentional nonadherence) and system‐associated factors (confusion between brand and generic names, discharge instruction incomplete or inaccurate, duplication, incorrect dosage) according to a published medication discrepancy tool.[2] Discrepancies were categorized as intentional nonadherence if patients knew the regimen but decided not to adhere. On the other hand, unintentional nonadherence was used for discrepancies in which patients were unaware of the regimen and thus the discrepancy. Medication discrepancies were classified as mild, moderate, or severe depending on the medication involved. Mild discrepancies were over‐the‐counter medications (eg, acetaminophen, laxatives, multivitamins) and topical creams. Severe discrepancies included medications for heart disease (eg, ‐blockers, calcium channel blockers, angiotensin receptor blockers, diuretics), pulmonary disease (eg, inhalers), diabetes (eg, insulin, glyburide), and antibiotics. Moderate discrepancies were those that did not fit the mild or severe categories (eg, prescription pain medication such as narcotics, anxiety medications, bisphosphonates, muscle relaxants).
Statistical analysis was performed with the SPSS 18.0 (SPSS Inc., Chicago, IL). We analyzed data on study patients to estimate the effect of contact with the PCP within 48 hours of discharge on the frequency of any medication discrepancy. We first examined differences between patients who were contacted or not contacted by patient sociodemographic characteristics. [2] tests were used to analyze the significance of differences in the proportion of medication discrepancies between patients who were contacted and not contacted. Logistic regression analysis was used to test the effect of being contacted on the likelihood of having any prescription medication discrepancy after controlling for patient characteristics (eg, race and ethnicity, age, number of medications, living alone, sex, and TOFHLA score.)
RESULTS
Sample Characteristics
Of the 225 patients who met inclusion criteria, 114 subjects were recruited and interviewed by research staff during the hospital stay and 48 hours after discharge. Due to early discharge and staffing reasons, 27 subjects were not able to be approached during discharge. Of the 84 patients who declined the study, the reasons included: not interested in study (n=58), did not feel well enough to complete or participate (n=16), did not wish study personnel to have access to personal records (n=5), and no reason given (n=5). Of the 114 subjects enrolled in the hospital, 77 subjects completed 48‐hour postdischarge phone interviews with research staff. Two patients had missing data, leaving 75 patients who were included in the analysis.
Study patients' age, race and ethnicity, sex, living situation (alone vs not alone), number of medications, mean sTOFHLA score, and medication discrepancy are summarized in Table 1. Thirty‐six percent of patients (n=27) were contacted by the PCP within 48 hours of discharge. Age, living situation (alone vs not alone), number of medications, and mean sTOFHLA score were similar in both groups of contacted versus noncontacted patients. Of those who were contacted, males made up 48.1% versus 27.1% for those not contacted (P=0.06). Similarly, 44.4% of those who were not contacted were black versus 37.5% among the contacted (P=0.035).
| All Subjects, N=77 | Subject Without PCP Contact, n=50 | Subjects With PCP Contact, n=27 | P Value | |
|---|---|---|---|---|
| ||||
| Mean ageSD, y | 63.012.2 | 63.311.9 | 62.313.1 | 0.74 |
| Race and ethnicity, n (%) | 0.35 | |||
| White/other | 40 (53.5) | 28 (58.3) | 12 (44.4) | |
| Black | 30 (40.0) | 18 (37.5) | 12 (44.4) | |
| Hispanic | 5 (6.7) | 2 (4.2) | 3 (11.1) | |
| Male, n (%) | 26 (34.7) | 13 (27.1) | 13 (48.1) | 0.06 |
| Lives alone, n (%) | 30 (40.0) | 20 (41.7) | 10 (37.0) | 0.69 |
| Mean sTOFHLA scoreSD | 29.67.9 | 29.47.7 | 29.97.8 | 0.75 |
| Mean number of medications | 9.224.9 | 9.064.7 | 9.633.5 | 0.67 |
| Experienced medication discrepancy, n (%) | 39 (52) | 28 (59.3) | 11 (40.7) | 0.14 |
Medication Discrepancies
Of the 75 study patients, 39 patients (50.6%) experienced a total of 84 medication discrepancies. Fifty‐eight medication discrepancies were prescription medications, whereas 25 were over‐the‐counter medications. Of those who had discrepancies, 46.2% (n=18) had 1 discrepancy, 23.1% (n=9) had 2 discrepancies, 12.8% (n=5) had 3 discrepancies, 10.2% (n=4) had 4 discrepancies, and 7.7% (n=3) 5 or more discrepancies. The mean number of discrepancies per patient was 2.15 per patient. Medication discrepancies were categorized by severity based on the safety profile of the medication involved and type discrepancy (Table 2).
| Frequency, n (%) | |
|---|---|
| |
| Type of medication discrepancy | |
| Over the counter | 26 (30.9) |
| Prescription medication | 58 (69.0) |
| Severity of medication discrepancy | |
| Milda | 28 (33.3) |
| Moderateb | 24 (28.6) |
| Severec | 32 (38.1) |
Reasons for Medication Discrepancies
The subject‐provided reasons for medication discrepancies are listed in Table 3 and divided into patient‐ and system‐associated factors. The overall most frequent reason for a discrepancy was the patient's intentional nonadherence. Examples of intentional nonadherence include not sure of purpose of medication, did not recognize drug, did not fill prescription, did not need prescription, and wanted to wait longer, so not taking diuretic daily. The second most frequent reason was inaccurate discharge instructions (e.g., discharge instructions with medication changes denoting no change but incorrect outpatient thyroid medication dosage listed (Table 3).
| Factor | Frequency, n (%) |
|---|---|
| Patient‐associated factors | |
| Adverse drug effects | 8 (9.5) |
| Intentional nonadherence | 50 (59.4) |
| Unintentional nonadherence | 1 (1.2) |
| Subtotal | 59 |
| System‐associated factors | |
| Confusion between brand and generic names | 3 (3.5) |
| Discharge Instructions incomplete or inaccurate | 12 (14.2) |
| Duplication | 3 (3.5) |
| Incorrect dosage | 3 (3.5) |
| Incorrect frequency | 1 (1.2) |
| Conflicting information from different sources | 3 (3.5) |
| Subtotal | 25 |
| Total | 84 |
Logistic Regression Results for the Likelihood of Any Medication Discrepancy
Logistical regression results are shown in Table 4. Patients who were contacted by their PCP at discharge were 70% less likely to have a discrepancy when compared with those who were not contacted (P=0.03). This result was controlled for other possible factors including patient sex. Of interest, men were 3.94 times more likely to have a discrepancy when compared with women (P=0.02). There was also a nonsignificant but potentially important association between higher health literacy, measured continuously (0X) and being more likely to have a discrepancy (P=0.07). Including variables for age, ethnicity, and living alone were nonsignificant and did not change the regression results for contacted patients.
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| ||
| Subject contacted by PCP at Discharge | 0.33 | 0.110.97 |
| Male | 3.98 | 1.2712.49 |
| Number of medications | 1.09 | 0.961.23 |
| TOHFLA score | 1.09 | 1.011.18 |
DISCUSSION
Our results provide evidence that contact with PCPs within 24 hours of hospital discharge can be effective in decreasing medication discrepancies. The PCP‐Enhanced Discharge Communication Intervention was designed to investigate the value of improving existing lines of communication at discharge without involving any additional healthcare personnel. As a lean discharge intervention, the PCP, the hospitalist, and the patient were the main components to this intervention.
This study was limited in that the sample size was small and that we enrolled consecutive patients. Due to the small sample size, we did not examine hospital readmissions. Further studies are needed to examine whether primary care involvement at discharge would affect hospital readmissions. Another limitation of this study was that the control group was not randomized or preselected. Our study compared those subjects who received a phone call from their PCP to those subjects who did not. Although we instructed PCPs with a standardized script, we did not record or ensure that the phone call‐up occurred as such. There is potential variability in how the PCPs conducted their follow‐up with patients, and we are unable to measure what was effective and ineffective in reducing medication discrepancies. Another limitation was that the determination of the severity of the medication discrepancy was done by medication involved as opposed to by physician review and adjudication. The study would have been strengthened by interviewing the outpatient physicians on the amount of harm each discrepancy would or did cause the patient.
The most frequent reason for discrepancy was intentional nonadherence. Prior research has shown that intentional nonadherence of medications at hospital discharge is linked to health literacy.[14] One may postulate that patients with adequate health literacy feel enabled to go against medical advice and chose to not take medications as prescribed.
In our study, patients had the most medication discrepancies in the severe medications category, which involved cardiac, pulmonary, and diabetic medications, compared with the mild and moderate category. This finding may reflect the frequency that these medications are prescribed but are consistent with findings of Coleman et al.[2] The finding highlights the need to ensure adequate education and understanding of medication regimens for these complex patients. Patients with cardiac, pulmonary, and diabetic disease may benefit from personalized discharge instructions and a more structured and organized medication reconciliation process.
Our study found that males were more likely to have a medication discrepancy than females, which has not been found in previous studies on medication discrepancies. One study on Medicare beneficiaries with congestive heart failure found that men were much more likely to be readmitted than woman within 6 months of discharge.[15] The reason for the increased risk of medication discrepancy in males is unknown. Gender differences in health have frequently been reported, with men having higher rates of morbidity and mortality than women.[16, 17] The differences are thought to be due to the reluctance of men to seek medical help and consult medical practitioners when needed. It has been known that women use health services more than men, and are more likely than men to report a chronic illness.[18] When men do present with symptoms, it is often later in the stage of a disease than women and when treatment is less likely to be successful.[19] It may be that men in this study population had more medication discrepancies as they were reluctant to seek help or ask for clarification regarding medications at discharge.
Of those enrolled, 36% of patients were contacted by their PCP within 48 hours of discharge. It is unclear if the PCP attempted but was unable to reach the patient or did not attempt to call the patient. Although PCPs were compensated with a $5 coffee shop gift card, a larger compensation may insure completion of the patient contact. Further research is needed to determine the reasons why PCPs were not able to complete the phone call.
From a policy standpoint, hospitals that focus solely on hospital‐based transition interventions are potentially missing half the problem. The hospital acts as a sender or pitcher, and the PCP acts as a receiver or catcher. The receiver needs to be included in the discharge process for a successful patient transition to home. With recent billing changes for transition coding, the Center for Medicare and Medicaid Services recognizes this relationship.[20] Outpatient PCPs are able to bill for bundled follow‐up phone calls and appointments. Instead of paying additional staff to make 48‐hour postdischarge phone calls, hospitals should consider partnering with PCPs to ensure a more organized discharge.
Our results showed that PCP communication with patients within 24 hours of discharge was associated with decreased medication discrepancies. The PCP is vital to ensuring a safe transition home from the hospital. Because many patients have an established relationship with their PCP, a bond of trust exists that is often missing with hospital‐employed transitional staff. Patients pay attention when a known physician contacts them directly. In our study, patients may have felt comfortable addressing their concerns and questions with their trusted PCP. Subsequently, patients may have been more attuned to the answers their PCP gave and avoided medication errors. Our results further demonstrate the importance of PCP involvement in the hospital discharge process to improve the care of our patients.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , . Posthospital medication discrepancies—prevalence and contributing factors. Arch Intern Med. 2005;165(16):1842–1847.
- , , , et al. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999–1006.
- , , , , . Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee‐for‐service setting. Home Health Care Serv Q. 2009;28(2‐3):84–99.
- , , . Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–1446.
- , , , et al. Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211–218.
- , , , et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187.
- , , , , . A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154(15):1721–1729.
- , , , , , . Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817–1825.
- , , , et al. Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med. 2005;118(10):1148–1153.
- , , , et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385–391.
- , . Hospital readmissions in the Medicare population. N Engl J Med. 1984;311(21):1349–1353.
- , , , , . Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42.
- , , , , , . Relationship of Health Literacy to Intentional and Unintentional Non‐Adherence of Hospital Discharge Medications. J Gen Intern Med. 2012;27(2):173–178.
- , , , et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157(1):99–104.
- . College men's health: an overview and a call to action. J Am Coll Health. 1998;46(6):279–290.
- Gender and the Social Construction of Illness. Thousand Oaks, CA: Sage; 1997.
- Inequalities in Health: The Black Report and the Health Divide. London, UK: Penguin; 1988.
- , , , . Decision making process in people with symptoms of acute myocardial infarction: qualitative study. BMJ. 2002;332:1006–1017.
- Centers for Medicare and Medicaid Services. Transitional Care Management Services. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/PhysicianFeeSched/Downloads/FAQ‐TCMS.pdf. Accessed June 28, 2013.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , . Posthospital medication discrepancies—prevalence and contributing factors. Arch Intern Med. 2005;165(16):1842–1847.
- , , , et al. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med. 1994;120(12):999–1006.
- , , , , . Further application of the care transitions intervention: results of a randomized controlled trial conducted in a fee‐for‐service setting. Home Health Care Serv Q. 2009;28(2‐3):84–99.
- , , . Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med. 1996;334(22):1441–1446.
- , , , et al. Reduction of 30‐day postdischarge hospital readmission or emergency department (ED) visit rates in high‐risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211–218.
- , , , et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187.
- , , , , . A case manager intervention to reduce readmissions. Arch Intern Med. 1994;154(15):1721–1729.
- , , , , , . Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817–1825.
- , , , et al. Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. Am J Med. 2005;118(10):1148–1153.
- , , , et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385–391.
- , . Hospital readmissions in the Medicare population. N Engl J Med. 1984;311(21):1349–1353.
- , , , , . Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42.
- , , , , , . Relationship of Health Literacy to Intentional and Unintentional Non‐Adherence of Hospital Discharge Medications. J Gen Intern Med. 2012;27(2):173–178.
- , , , et al. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157(1):99–104.
- . College men's health: an overview and a call to action. J Am Coll Health. 1998;46(6):279–290.
- Gender and the Social Construction of Illness. Thousand Oaks, CA: Sage; 1997.
- Inequalities in Health: The Black Report and the Health Divide. London, UK: Penguin; 1988.
- , , , . Decision making process in people with symptoms of acute myocardial infarction: qualitative study. BMJ. 2002;332:1006–1017.
- Centers for Medicare and Medicaid Services. Transitional Care Management Services. Available at: http://www.cms.gov/Medicare/Medicare‐Fee‐for‐Service‐Payment/PhysicianFeeSched/Downloads/FAQ‐TCMS.pdf. Accessed June 28, 2013.
© 2013 Society of Hospital Medicine