User login
The role of the skin microbiome in skin care
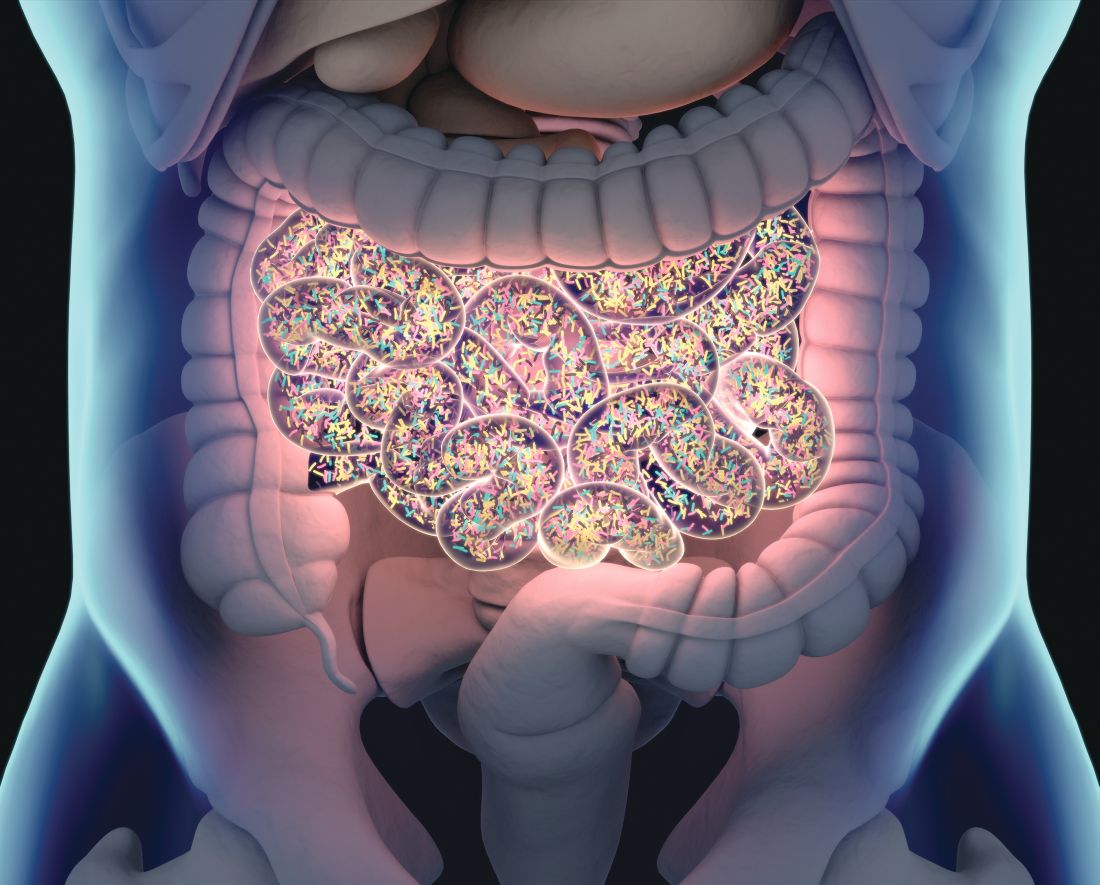
It may not seem intuitive, but to understand some of the new skin care claims, you need to know a bit about the gut microbiome and its role in skin health. The The gut and skin play a balancing act between beneficial, neutral, and harmful flora that are interrelated with the innate and adaptive immune systems.1 The skin and gut seem to be intertwined and express several comorbidities.2 In this column, the focus is on the cutaneous microbiome’s role in skin health. To understand the cosmeceutical claims about pre- and probiotics, you first need to familiarize yourself with skin microbiome science. The skin-gut nexus will be discussed in next month’s column, which will address the role of the skin microbiome in skin diseases.
Why is the microbiome such a hot topic?
Genetic sequencing has spurred advances in the study of the microbiome and has provided intriguing clues that the gut and skin microbiome have influences on each other. Sequencing assays that focus on bacterial 16S ribosomal RNA genes have been used by investigators to distinguish and describe the wide variety of resident and transient microorganisms on the skin and elucidate their roles in skin health and disease.1 Genomic sequencing has identified species in the skin and gut that were not found previously by cultivating microbial isolates.3,4 Advances in technologies such as whole-genome shotgun sequencing, metagenomics, and functional metabolomics will further contribute to our understanding of the effects of the skin microbiome on skin health and skin type. Of course, many supplement and cosmeceutical companies have jumped on this bandwagon prematurely and claim that their products increase “good bacteria while diminishing bad bacteria.” While there are interesting data that have emerged, we still cannot say which bacteria are “good” and ‘bad” as far as the skin is concerned – with a few exceptions that we have known all along. For example, Cutibacterium acnes and Staphylococcus aureus still remain in the undesirable category. (P. acnes has been renamed and now is officially referred to as C. acnes.) While it is premature to recommend probiotic– or prebiotic–containing cosmeceuticals, your patients will ask you about them. New studies about rosacea and the microbiome have generated a lot of patient questions in my practice, so I am writing several blogs about how to answer patient questions, which can be found at STSFranchise.com/blog. I’m also educating consumers on Facebook and Instagram @skintypesolutions so that they will not be taken advantage of by the too early “pseudoscience.” So now that you have heard that it is too early to recommend pre- and probiotic skin care to target skin issues, let’s look at the science that does exist.
Terminology
- Microbiome: Microbes that live in a particular environment or biome.
- Microbiota: The collection of living microbes that live in or on an environment. This term includes the microorganisms only and not the characteristics of their environment.
- Prebiotics: A nondigestible food ingredient that promotes the growth of microorganisms in the intestines. These can promote the growth of beneficial or harmful microorganisms. Think of them as a type of “fertilizer” for the microbiome.
- Probiotics: Living microorganisms that can provide beneficial qualities when used orally or topically. What probiotics are not? Microbes naturally found in your body and on your skin; microbes that are no longer alive; fermented foods that contain an unknown amount of bacteria.
Skin surface area
Richard Gallo, MD, a dermatologist from the University of California, San Diego, who is a leader in the microbiome field of study, says that estimates of the cutaneous microbiome’s impact on human health via skin have failed to acknowledge the inner follicular surface, thus drastically undervaluing the potential of the cutaneous microbiome to influence systemic health.5 He suggests that the surface area of skin has been miscalculated as measuring 2 m2 because it is considered a flat surface. This ignores the plethora of hair follicles and sweat ducts that significantly broaden the epithelial surface to measure closer to 25 m2 and underscores that the expansive skin microbiome is much larger than previously recognized.5 Taking the hair follicle surface area into account, the skin has vast space to harbor various organisms and microbiome environments. What our patients use on their skin certainly influences these environments. The key is trying to figure out how to manipulate the microbiome to our patient’s advantage.
Microbes have environmental preferences
Different microbial species thrive on particular regions of the diverse topography of the expansive surface area and choose their preferred environments from among sebaceous or nonsebaceous, hairy or smooth, moist or dry, and creased or noncreased areas.6,7 Other host factors that affect which microorganisms colonize the skin include hair follicle thickness, age, sex, diet (especially high fat and sugar intake), climate, occupation, and personal hygiene.7-10 Gene sequencing has revealed that these variations are partially because of factors such as ultraviolet exposure, pH, and temperature.4,6,11 For example, C. acnes has been found to be more prevalent in highly sebaceous sites on the head and upper torso.4 In general, Propionibacteriaceae (Cutibacterium) prefer sebaceous areas, whereas Corynebacteriaceae and Staphylococcaceae prevail in moist regions, such as the navel or axilla. Dry areas host the widest diversity of microbes, including Corynebacterium, Staphylococcus, and Streptococcus species.1,7,12
Impact of sebum and skin hydration on microbiome
In 2016, Mukherjee et al. measured sebum and hydration from the forehead and cheeks of 30 healthy female volunteers in a study that tested the hypothesis that differences in sebum and hydration levels in specific facial areas account for interindividual variation in facial skin microbiome. They found that the most significant predictor of microbiome composition was cheek sebum level, followed by forehead hydration level, while cheek hydration and forehead sebum levels were not predictive. The prevalence of Actinobacteria/Propionibacterium rose, while microbiome diversity diminished with an increase in cheek sebum, with such trends reversed in relation to forehead hydration. The investigators concluded that site-specific sebum and water levels impact the nature and diversity of the facial skin microbiome.13
Lability of the cutaneous microbiome
The skin microbiome changes during various times of life. For example, in puberty, more lipophilic species such as Propionibacteriaceae and Cornebacteriaceae predominate, while prior to puberty there is a preponderance of Firmicutes, Bacteroidetes, and Proteobacteria.4,14 However, in the absence of lifestyle changes, cutaneous microbial communities have been found through longitudinal studies to be relatively stable over a 2-year period.6 A person’s skin microbiome is subject to influence from an adjacent skin microbiome, such as between cohabiting couples or the influence of breastfeeding mothers.15 It is never too early to consider the role of the microbiome in health and disease. For example, infant microbiomes play a role in eczema and the atopic march.16 For this reason, those of us who treat children need to be familiar with studies that have demonstrate how the cutaneous microbiome is affected by childbirth delivery method, breastfeeding, the mother’s diet antibiotic use during pregnancy and breastfeeding.4,17
Microbiome effects on skin function
The skin barrier, a bilayer lipid-laden membrane that surrounds keratinocytes and prevents transepidermal water loss, is affected by resident microbial communities and has been shown by research to be influenced by the volume and diversity of such microbes.18 Organisms on the skin’s surface play an important role in communicating with and educating the cutaneous arm of the immune system.19 In 2017, Maguire and Maguire reviewed recent studies of the gut and skin microbiomes and suggested that Nitrobacter, Lactobacillus, and Bifidobacterium can improve skin health and could be useful bacterial adjuvants in a probiotic and prebiotic strategy in homeostatic renormalization when skin health is compromised.20Nitrobacter has displayed antifungal activity against dermatophytes and Staphylococcus; Lactobacillus has exhibited anti-inflammatory effects and was shown to improve adult acne in a small study; Bifidobacterium combined with Lactobacillus lowered the incidence of atopic eczema in early childhood; and Bifidobacterium and the prebiotic galacto-oligosaccharide prevented hydration level losses in the stratum corneum among other beneficial effects in a double-blind, placebo-controlled, randomized trial.20
Microbiome diversity is key
Microbes interact, collaborate, and oppose one another while exerting influence and being affected by the host. Effective communication among the innate and adaptive parts of the immune system, epithelial cells, and cutaneous microbiota is essential for optimal functioning of the skin.6,7 Studies on subjects with atopic dermatitis showed a strong association between decreased diversity and increased disease severity. This suggests that a diverse microbiome is associated with skin health.21 For this reason, use of pre- and probiotics for skin issues is discouraged at this time. If we replace the normal diverse flora with one organism, we do not yet know the consequences. It is much more likely that successful treatments in the future will contain a diverse group of organisms.
Cosmeceutical effects on the skin microbiome
Cleansing and use of emollients certainly affect the skin biome, but we do not yet know to what extent. A study that looked at the effects of emollients on infants with atopic dermatitis showed that the emollient group has a lower skin pH and a more diverse microbiome.22 In a 2016 study on the impact of acute treatment with topical skin cleansers on the cutaneous microbiome, investigators evaluated multiple common skin cleansers in the washing of human forearms. Group A Streptococcus growth was reduced after washing with soaps infused with such antimicrobial compounds as benzalkonium chloride or triclocarban. The researchers stipulated that much more research is necessary to ascertain the effects of chronic washing as well as the that role skin care products may play in skin homeostasis or dysbiosis in some individuals.23
In a 2017 analysis of the effects of cosmetics on the skin microbiome of facial cheeks with high- and low-hydration levels over 4 weeks, Lee et al. found that bacterial diversity was higher in the low-hydration group, with increases in both observed after the use of cosmetics. The high-hydration group showed a greater supply of Propionibacterium. Cosmetic use was found not to have caused a shift in bacterial communities in the low-hydration group.24
Conclusion
We are in the early stages as we strive to learn more about the microbiome to leverage such knowledge to improve skin health. In the meantime, there is not enough evidence to suggest the use of any oral or topical prebiotics or probiotics to improve skin health. In fact, we may be causing harm by lessening diversity. The New York Times recently published an article called “The Problem with Probiotics” that referenced a JAMA Internal Medicine article entitled “Probiotic Safety – No Guarantees.”25 I recommend that you read those. Next month, I will look more closely at microbiome research pertaining to skin disease.
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Dréno B et al. J Eur Acad Dermatol Venereol. 2016 Dec;30(12):2038-47.
2. O’Neill CA et al. Bioessays. 2016 Nov;38(11):1167-76.
3. Kong HH. Trends Mol Med. 2011 Jun;17(6):320-8.
4. Kong HH et al. J Invest Dermatol. 2017 May;137(5):e119-22.
5. Gallo RL. J Invest Dermatol. 2017 Jun;137(6):1213-4.
6. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
7. Grice EA et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
8. Rodrigues Hoffmann A. Vet Dermatol. 2017 Feb;28(1):60-e15.
9. Moestrup KS et al. J Invest Dermatol. 2018 May;138(5):1225-8.
10. Prescott SL et al. World Allergy Organ J. 2017 Aug 22;10(1):29.
11. Costello EK et al. Science. 2009 Dec 18;326(5960):1694-7.
12. Zeeuwen PL et al. Genome Biol. 2012 Nov 15;13(11):R101.
13. Mukherjee S et al. Sci Rep. 2016 Oct 27;6:36062.
14. Oh J et al. Genome Med. 2012 Oct 10;4(10):77.
15. Ross AA et al. mSystems. 2017 Jul 20;2(4).
16. Blázquez AB et al. Transl Res. 2017 Jan;179:199-203.
17. Rock R et al. Open Forum Infect Dis. 2017 Oct;4(1):S232.
18. Baldwin HE et al. J Drugs Dermatol. 2017 Jan 1;16(1):12-8.
19. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
20. Maguire M et al. Arch Dermatol Res. 2017 Aug;309(6):411-21.
21. Kong HH et al. Genome Res. 2012 May;22(5):850-9.
22. Glatz M et al. PLoS One. 2018 Feb 28;13(2):e0192443.
23. Two AM et al. J Invest Dermatol. 2016 Oct;136(10):1950-4.
24. Lee HJ et al. MicrobiologyOpen. 2018 Apr;7(2):e00557. doi: 10.1002/mbo3.557.
25. Cohen PA. JAMA Intern Med. 2018 Sep 17. doi: 10.1001/jamainternmed.2018.5403.
It may not seem intuitive, but to understand some of the new skin care claims, you need to know a bit about the gut microbiome and its role in skin health. The The gut and skin play a balancing act between beneficial, neutral, and harmful flora that are interrelated with the innate and adaptive immune systems.1 The skin and gut seem to be intertwined and express several comorbidities.2 In this column, the focus is on the cutaneous microbiome’s role in skin health. To understand the cosmeceutical claims about pre- and probiotics, you first need to familiarize yourself with skin microbiome science. The skin-gut nexus will be discussed in next month’s column, which will address the role of the skin microbiome in skin diseases.
Why is the microbiome such a hot topic?
Genetic sequencing has spurred advances in the study of the microbiome and has provided intriguing clues that the gut and skin microbiome have influences on each other. Sequencing assays that focus on bacterial 16S ribosomal RNA genes have been used by investigators to distinguish and describe the wide variety of resident and transient microorganisms on the skin and elucidate their roles in skin health and disease.1 Genomic sequencing has identified species in the skin and gut that were not found previously by cultivating microbial isolates.3,4 Advances in technologies such as whole-genome shotgun sequencing, metagenomics, and functional metabolomics will further contribute to our understanding of the effects of the skin microbiome on skin health and skin type. Of course, many supplement and cosmeceutical companies have jumped on this bandwagon prematurely and claim that their products increase “good bacteria while diminishing bad bacteria.” While there are interesting data that have emerged, we still cannot say which bacteria are “good” and ‘bad” as far as the skin is concerned – with a few exceptions that we have known all along. For example, Cutibacterium acnes and Staphylococcus aureus still remain in the undesirable category. (P. acnes has been renamed and now is officially referred to as C. acnes.) While it is premature to recommend probiotic– or prebiotic–containing cosmeceuticals, your patients will ask you about them. New studies about rosacea and the microbiome have generated a lot of patient questions in my practice, so I am writing several blogs about how to answer patient questions, which can be found at STSFranchise.com/blog. I’m also educating consumers on Facebook and Instagram @skintypesolutions so that they will not be taken advantage of by the too early “pseudoscience.” So now that you have heard that it is too early to recommend pre- and probiotic skin care to target skin issues, let’s look at the science that does exist.
Terminology
- Microbiome: Microbes that live in a particular environment or biome.
- Microbiota: The collection of living microbes that live in or on an environment. This term includes the microorganisms only and not the characteristics of their environment.
- Prebiotics: A nondigestible food ingredient that promotes the growth of microorganisms in the intestines. These can promote the growth of beneficial or harmful microorganisms. Think of them as a type of “fertilizer” for the microbiome.
- Probiotics: Living microorganisms that can provide beneficial qualities when used orally or topically. What probiotics are not? Microbes naturally found in your body and on your skin; microbes that are no longer alive; fermented foods that contain an unknown amount of bacteria.
Skin surface area
Richard Gallo, MD, a dermatologist from the University of California, San Diego, who is a leader in the microbiome field of study, says that estimates of the cutaneous microbiome’s impact on human health via skin have failed to acknowledge the inner follicular surface, thus drastically undervaluing the potential of the cutaneous microbiome to influence systemic health.5 He suggests that the surface area of skin has been miscalculated as measuring 2 m2 because it is considered a flat surface. This ignores the plethora of hair follicles and sweat ducts that significantly broaden the epithelial surface to measure closer to 25 m2 and underscores that the expansive skin microbiome is much larger than previously recognized.5 Taking the hair follicle surface area into account, the skin has vast space to harbor various organisms and microbiome environments. What our patients use on their skin certainly influences these environments. The key is trying to figure out how to manipulate the microbiome to our patient’s advantage.
Microbes have environmental preferences
Different microbial species thrive on particular regions of the diverse topography of the expansive surface area and choose their preferred environments from among sebaceous or nonsebaceous, hairy or smooth, moist or dry, and creased or noncreased areas.6,7 Other host factors that affect which microorganisms colonize the skin include hair follicle thickness, age, sex, diet (especially high fat and sugar intake), climate, occupation, and personal hygiene.7-10 Gene sequencing has revealed that these variations are partially because of factors such as ultraviolet exposure, pH, and temperature.4,6,11 For example, C. acnes has been found to be more prevalent in highly sebaceous sites on the head and upper torso.4 In general, Propionibacteriaceae (Cutibacterium) prefer sebaceous areas, whereas Corynebacteriaceae and Staphylococcaceae prevail in moist regions, such as the navel or axilla. Dry areas host the widest diversity of microbes, including Corynebacterium, Staphylococcus, and Streptococcus species.1,7,12
Impact of sebum and skin hydration on microbiome
In 2016, Mukherjee et al. measured sebum and hydration from the forehead and cheeks of 30 healthy female volunteers in a study that tested the hypothesis that differences in sebum and hydration levels in specific facial areas account for interindividual variation in facial skin microbiome. They found that the most significant predictor of microbiome composition was cheek sebum level, followed by forehead hydration level, while cheek hydration and forehead sebum levels were not predictive. The prevalence of Actinobacteria/Propionibacterium rose, while microbiome diversity diminished with an increase in cheek sebum, with such trends reversed in relation to forehead hydration. The investigators concluded that site-specific sebum and water levels impact the nature and diversity of the facial skin microbiome.13
Lability of the cutaneous microbiome
The skin microbiome changes during various times of life. For example, in puberty, more lipophilic species such as Propionibacteriaceae and Cornebacteriaceae predominate, while prior to puberty there is a preponderance of Firmicutes, Bacteroidetes, and Proteobacteria.4,14 However, in the absence of lifestyle changes, cutaneous microbial communities have been found through longitudinal studies to be relatively stable over a 2-year period.6 A person’s skin microbiome is subject to influence from an adjacent skin microbiome, such as between cohabiting couples or the influence of breastfeeding mothers.15 It is never too early to consider the role of the microbiome in health and disease. For example, infant microbiomes play a role in eczema and the atopic march.16 For this reason, those of us who treat children need to be familiar with studies that have demonstrate how the cutaneous microbiome is affected by childbirth delivery method, breastfeeding, the mother’s diet antibiotic use during pregnancy and breastfeeding.4,17
Microbiome effects on skin function
The skin barrier, a bilayer lipid-laden membrane that surrounds keratinocytes and prevents transepidermal water loss, is affected by resident microbial communities and has been shown by research to be influenced by the volume and diversity of such microbes.18 Organisms on the skin’s surface play an important role in communicating with and educating the cutaneous arm of the immune system.19 In 2017, Maguire and Maguire reviewed recent studies of the gut and skin microbiomes and suggested that Nitrobacter, Lactobacillus, and Bifidobacterium can improve skin health and could be useful bacterial adjuvants in a probiotic and prebiotic strategy in homeostatic renormalization when skin health is compromised.20Nitrobacter has displayed antifungal activity against dermatophytes and Staphylococcus; Lactobacillus has exhibited anti-inflammatory effects and was shown to improve adult acne in a small study; Bifidobacterium combined with Lactobacillus lowered the incidence of atopic eczema in early childhood; and Bifidobacterium and the prebiotic galacto-oligosaccharide prevented hydration level losses in the stratum corneum among other beneficial effects in a double-blind, placebo-controlled, randomized trial.20
Microbiome diversity is key
Microbes interact, collaborate, and oppose one another while exerting influence and being affected by the host. Effective communication among the innate and adaptive parts of the immune system, epithelial cells, and cutaneous microbiota is essential for optimal functioning of the skin.6,7 Studies on subjects with atopic dermatitis showed a strong association between decreased diversity and increased disease severity. This suggests that a diverse microbiome is associated with skin health.21 For this reason, use of pre- and probiotics for skin issues is discouraged at this time. If we replace the normal diverse flora with one organism, we do not yet know the consequences. It is much more likely that successful treatments in the future will contain a diverse group of organisms.
Cosmeceutical effects on the skin microbiome
Cleansing and use of emollients certainly affect the skin biome, but we do not yet know to what extent. A study that looked at the effects of emollients on infants with atopic dermatitis showed that the emollient group has a lower skin pH and a more diverse microbiome.22 In a 2016 study on the impact of acute treatment with topical skin cleansers on the cutaneous microbiome, investigators evaluated multiple common skin cleansers in the washing of human forearms. Group A Streptococcus growth was reduced after washing with soaps infused with such antimicrobial compounds as benzalkonium chloride or triclocarban. The researchers stipulated that much more research is necessary to ascertain the effects of chronic washing as well as the that role skin care products may play in skin homeostasis or dysbiosis in some individuals.23
In a 2017 analysis of the effects of cosmetics on the skin microbiome of facial cheeks with high- and low-hydration levels over 4 weeks, Lee et al. found that bacterial diversity was higher in the low-hydration group, with increases in both observed after the use of cosmetics. The high-hydration group showed a greater supply of Propionibacterium. Cosmetic use was found not to have caused a shift in bacterial communities in the low-hydration group.24
Conclusion
We are in the early stages as we strive to learn more about the microbiome to leverage such knowledge to improve skin health. In the meantime, there is not enough evidence to suggest the use of any oral or topical prebiotics or probiotics to improve skin health. In fact, we may be causing harm by lessening diversity. The New York Times recently published an article called “The Problem with Probiotics” that referenced a JAMA Internal Medicine article entitled “Probiotic Safety – No Guarantees.”25 I recommend that you read those. Next month, I will look more closely at microbiome research pertaining to skin disease.
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Dréno B et al. J Eur Acad Dermatol Venereol. 2016 Dec;30(12):2038-47.
2. O’Neill CA et al. Bioessays. 2016 Nov;38(11):1167-76.
3. Kong HH. Trends Mol Med. 2011 Jun;17(6):320-8.
4. Kong HH et al. J Invest Dermatol. 2017 May;137(5):e119-22.
5. Gallo RL. J Invest Dermatol. 2017 Jun;137(6):1213-4.
6. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
7. Grice EA et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
8. Rodrigues Hoffmann A. Vet Dermatol. 2017 Feb;28(1):60-e15.
9. Moestrup KS et al. J Invest Dermatol. 2018 May;138(5):1225-8.
10. Prescott SL et al. World Allergy Organ J. 2017 Aug 22;10(1):29.
11. Costello EK et al. Science. 2009 Dec 18;326(5960):1694-7.
12. Zeeuwen PL et al. Genome Biol. 2012 Nov 15;13(11):R101.
13. Mukherjee S et al. Sci Rep. 2016 Oct 27;6:36062.
14. Oh J et al. Genome Med. 2012 Oct 10;4(10):77.
15. Ross AA et al. mSystems. 2017 Jul 20;2(4).
16. Blázquez AB et al. Transl Res. 2017 Jan;179:199-203.
17. Rock R et al. Open Forum Infect Dis. 2017 Oct;4(1):S232.
18. Baldwin HE et al. J Drugs Dermatol. 2017 Jan 1;16(1):12-8.
19. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
20. Maguire M et al. Arch Dermatol Res. 2017 Aug;309(6):411-21.
21. Kong HH et al. Genome Res. 2012 May;22(5):850-9.
22. Glatz M et al. PLoS One. 2018 Feb 28;13(2):e0192443.
23. Two AM et al. J Invest Dermatol. 2016 Oct;136(10):1950-4.
24. Lee HJ et al. MicrobiologyOpen. 2018 Apr;7(2):e00557. doi: 10.1002/mbo3.557.
25. Cohen PA. JAMA Intern Med. 2018 Sep 17. doi: 10.1001/jamainternmed.2018.5403.
It may not seem intuitive, but to understand some of the new skin care claims, you need to know a bit about the gut microbiome and its role in skin health. The The gut and skin play a balancing act between beneficial, neutral, and harmful flora that are interrelated with the innate and adaptive immune systems.1 The skin and gut seem to be intertwined and express several comorbidities.2 In this column, the focus is on the cutaneous microbiome’s role in skin health. To understand the cosmeceutical claims about pre- and probiotics, you first need to familiarize yourself with skin microbiome science. The skin-gut nexus will be discussed in next month’s column, which will address the role of the skin microbiome in skin diseases.
Why is the microbiome such a hot topic?
Genetic sequencing has spurred advances in the study of the microbiome and has provided intriguing clues that the gut and skin microbiome have influences on each other. Sequencing assays that focus on bacterial 16S ribosomal RNA genes have been used by investigators to distinguish and describe the wide variety of resident and transient microorganisms on the skin and elucidate their roles in skin health and disease.1 Genomic sequencing has identified species in the skin and gut that were not found previously by cultivating microbial isolates.3,4 Advances in technologies such as whole-genome shotgun sequencing, metagenomics, and functional metabolomics will further contribute to our understanding of the effects of the skin microbiome on skin health and skin type. Of course, many supplement and cosmeceutical companies have jumped on this bandwagon prematurely and claim that their products increase “good bacteria while diminishing bad bacteria.” While there are interesting data that have emerged, we still cannot say which bacteria are “good” and ‘bad” as far as the skin is concerned – with a few exceptions that we have known all along. For example, Cutibacterium acnes and Staphylococcus aureus still remain in the undesirable category. (P. acnes has been renamed and now is officially referred to as C. acnes.) While it is premature to recommend probiotic– or prebiotic–containing cosmeceuticals, your patients will ask you about them. New studies about rosacea and the microbiome have generated a lot of patient questions in my practice, so I am writing several blogs about how to answer patient questions, which can be found at STSFranchise.com/blog. I’m also educating consumers on Facebook and Instagram @skintypesolutions so that they will not be taken advantage of by the too early “pseudoscience.” So now that you have heard that it is too early to recommend pre- and probiotic skin care to target skin issues, let’s look at the science that does exist.
Terminology
- Microbiome: Microbes that live in a particular environment or biome.
- Microbiota: The collection of living microbes that live in or on an environment. This term includes the microorganisms only and not the characteristics of their environment.
- Prebiotics: A nondigestible food ingredient that promotes the growth of microorganisms in the intestines. These can promote the growth of beneficial or harmful microorganisms. Think of them as a type of “fertilizer” for the microbiome.
- Probiotics: Living microorganisms that can provide beneficial qualities when used orally or topically. What probiotics are not? Microbes naturally found in your body and on your skin; microbes that are no longer alive; fermented foods that contain an unknown amount of bacteria.
Skin surface area
Richard Gallo, MD, a dermatologist from the University of California, San Diego, who is a leader in the microbiome field of study, says that estimates of the cutaneous microbiome’s impact on human health via skin have failed to acknowledge the inner follicular surface, thus drastically undervaluing the potential of the cutaneous microbiome to influence systemic health.5 He suggests that the surface area of skin has been miscalculated as measuring 2 m2 because it is considered a flat surface. This ignores the plethora of hair follicles and sweat ducts that significantly broaden the epithelial surface to measure closer to 25 m2 and underscores that the expansive skin microbiome is much larger than previously recognized.5 Taking the hair follicle surface area into account, the skin has vast space to harbor various organisms and microbiome environments. What our patients use on their skin certainly influences these environments. The key is trying to figure out how to manipulate the microbiome to our patient’s advantage.
Microbes have environmental preferences
Different microbial species thrive on particular regions of the diverse topography of the expansive surface area and choose their preferred environments from among sebaceous or nonsebaceous, hairy or smooth, moist or dry, and creased or noncreased areas.6,7 Other host factors that affect which microorganisms colonize the skin include hair follicle thickness, age, sex, diet (especially high fat and sugar intake), climate, occupation, and personal hygiene.7-10 Gene sequencing has revealed that these variations are partially because of factors such as ultraviolet exposure, pH, and temperature.4,6,11 For example, C. acnes has been found to be more prevalent in highly sebaceous sites on the head and upper torso.4 In general, Propionibacteriaceae (Cutibacterium) prefer sebaceous areas, whereas Corynebacteriaceae and Staphylococcaceae prevail in moist regions, such as the navel or axilla. Dry areas host the widest diversity of microbes, including Corynebacterium, Staphylococcus, and Streptococcus species.1,7,12
Impact of sebum and skin hydration on microbiome
In 2016, Mukherjee et al. measured sebum and hydration from the forehead and cheeks of 30 healthy female volunteers in a study that tested the hypothesis that differences in sebum and hydration levels in specific facial areas account for interindividual variation in facial skin microbiome. They found that the most significant predictor of microbiome composition was cheek sebum level, followed by forehead hydration level, while cheek hydration and forehead sebum levels were not predictive. The prevalence of Actinobacteria/Propionibacterium rose, while microbiome diversity diminished with an increase in cheek sebum, with such trends reversed in relation to forehead hydration. The investigators concluded that site-specific sebum and water levels impact the nature and diversity of the facial skin microbiome.13
Lability of the cutaneous microbiome
The skin microbiome changes during various times of life. For example, in puberty, more lipophilic species such as Propionibacteriaceae and Cornebacteriaceae predominate, while prior to puberty there is a preponderance of Firmicutes, Bacteroidetes, and Proteobacteria.4,14 However, in the absence of lifestyle changes, cutaneous microbial communities have been found through longitudinal studies to be relatively stable over a 2-year period.6 A person’s skin microbiome is subject to influence from an adjacent skin microbiome, such as between cohabiting couples or the influence of breastfeeding mothers.15 It is never too early to consider the role of the microbiome in health and disease. For example, infant microbiomes play a role in eczema and the atopic march.16 For this reason, those of us who treat children need to be familiar with studies that have demonstrate how the cutaneous microbiome is affected by childbirth delivery method, breastfeeding, the mother’s diet antibiotic use during pregnancy and breastfeeding.4,17
Microbiome effects on skin function
The skin barrier, a bilayer lipid-laden membrane that surrounds keratinocytes and prevents transepidermal water loss, is affected by resident microbial communities and has been shown by research to be influenced by the volume and diversity of such microbes.18 Organisms on the skin’s surface play an important role in communicating with and educating the cutaneous arm of the immune system.19 In 2017, Maguire and Maguire reviewed recent studies of the gut and skin microbiomes and suggested that Nitrobacter, Lactobacillus, and Bifidobacterium can improve skin health and could be useful bacterial adjuvants in a probiotic and prebiotic strategy in homeostatic renormalization when skin health is compromised.20Nitrobacter has displayed antifungal activity against dermatophytes and Staphylococcus; Lactobacillus has exhibited anti-inflammatory effects and was shown to improve adult acne in a small study; Bifidobacterium combined with Lactobacillus lowered the incidence of atopic eczema in early childhood; and Bifidobacterium and the prebiotic galacto-oligosaccharide prevented hydration level losses in the stratum corneum among other beneficial effects in a double-blind, placebo-controlled, randomized trial.20
Microbiome diversity is key
Microbes interact, collaborate, and oppose one another while exerting influence and being affected by the host. Effective communication among the innate and adaptive parts of the immune system, epithelial cells, and cutaneous microbiota is essential for optimal functioning of the skin.6,7 Studies on subjects with atopic dermatitis showed a strong association between decreased diversity and increased disease severity. This suggests that a diverse microbiome is associated with skin health.21 For this reason, use of pre- and probiotics for skin issues is discouraged at this time. If we replace the normal diverse flora with one organism, we do not yet know the consequences. It is much more likely that successful treatments in the future will contain a diverse group of organisms.
Cosmeceutical effects on the skin microbiome
Cleansing and use of emollients certainly affect the skin biome, but we do not yet know to what extent. A study that looked at the effects of emollients on infants with atopic dermatitis showed that the emollient group has a lower skin pH and a more diverse microbiome.22 In a 2016 study on the impact of acute treatment with topical skin cleansers on the cutaneous microbiome, investigators evaluated multiple common skin cleansers in the washing of human forearms. Group A Streptococcus growth was reduced after washing with soaps infused with such antimicrobial compounds as benzalkonium chloride or triclocarban. The researchers stipulated that much more research is necessary to ascertain the effects of chronic washing as well as the that role skin care products may play in skin homeostasis or dysbiosis in some individuals.23
In a 2017 analysis of the effects of cosmetics on the skin microbiome of facial cheeks with high- and low-hydration levels over 4 weeks, Lee et al. found that bacterial diversity was higher in the low-hydration group, with increases in both observed after the use of cosmetics. The high-hydration group showed a greater supply of Propionibacterium. Cosmetic use was found not to have caused a shift in bacterial communities in the low-hydration group.24
Conclusion
We are in the early stages as we strive to learn more about the microbiome to leverage such knowledge to improve skin health. In the meantime, there is not enough evidence to suggest the use of any oral or topical prebiotics or probiotics to improve skin health. In fact, we may be causing harm by lessening diversity. The New York Times recently published an article called “The Problem with Probiotics” that referenced a JAMA Internal Medicine article entitled “Probiotic Safety – No Guarantees.”25 I recommend that you read those. Next month, I will look more closely at microbiome research pertaining to skin disease.
Dr. Baumann is a private practice dermatologist, researcher, author and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients,” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Dréno B et al. J Eur Acad Dermatol Venereol. 2016 Dec;30(12):2038-47.
2. O’Neill CA et al. Bioessays. 2016 Nov;38(11):1167-76.
3. Kong HH. Trends Mol Med. 2011 Jun;17(6):320-8.
4. Kong HH et al. J Invest Dermatol. 2017 May;137(5):e119-22.
5. Gallo RL. J Invest Dermatol. 2017 Jun;137(6):1213-4.
6. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
7. Grice EA et al. Nat Rev Microbiol. 2011 Apr;9(4):244-53.
8. Rodrigues Hoffmann A. Vet Dermatol. 2017 Feb;28(1):60-e15.
9. Moestrup KS et al. J Invest Dermatol. 2018 May;138(5):1225-8.
10. Prescott SL et al. World Allergy Organ J. 2017 Aug 22;10(1):29.
11. Costello EK et al. Science. 2009 Dec 18;326(5960):1694-7.
12. Zeeuwen PL et al. Genome Biol. 2012 Nov 15;13(11):R101.
13. Mukherjee S et al. Sci Rep. 2016 Oct 27;6:36062.
14. Oh J et al. Genome Med. 2012 Oct 10;4(10):77.
15. Ross AA et al. mSystems. 2017 Jul 20;2(4).
16. Blázquez AB et al. Transl Res. 2017 Jan;179:199-203.
17. Rock R et al. Open Forum Infect Dis. 2017 Oct;4(1):S232.
18. Baldwin HE et al. J Drugs Dermatol. 2017 Jan 1;16(1):12-8.
19. Byrd AL et al. Nat Rev Microbiol. 2018 Mar;16(3):143-55.
20. Maguire M et al. Arch Dermatol Res. 2017 Aug;309(6):411-21.
21. Kong HH et al. Genome Res. 2012 May;22(5):850-9.
22. Glatz M et al. PLoS One. 2018 Feb 28;13(2):e0192443.
23. Two AM et al. J Invest Dermatol. 2016 Oct;136(10):1950-4.
24. Lee HJ et al. MicrobiologyOpen. 2018 Apr;7(2):e00557. doi: 10.1002/mbo3.557.
25. Cohen PA. JAMA Intern Med. 2018 Sep 17. doi: 10.1001/jamainternmed.2018.5403.
Buckwheat Extract
Native to North and East Asia, This highly adaptable plant – the most common species of which are Fagopyrum esculentum (common buckwheat or sweet buckwheat), and F. tataricum (which grows in more mountainous regions) – has acclimated to cultivation in North America, as well.1 Increasingly popular as a healthy grain option, buckwheat flour has been touted for beneficial effects on diabetes, obesity, hypertension, hypercholesterolemia, and constipation.1 It has also gained attention for its association with some allergic reactions.
Wound Healing
In 2008, van den Berg et al. performed an in vitro investigation of the antioxidant and anti-inflammatory qualities of buckwheat honey for consideration in wound healing. American buckwheat honey from New York was found to be the source of the most salient activities, with such properties attributed to its abundant phenolic components. The researchers suggested that these phenols might impart antibacterial activity, while the low pH and high free acid content of the buckwheat honey could contribute to healing wounds.4
Antioxidant Activity
The antioxidant capacity, along with other traits, characterizing the sprouts of common buckwheat (F. esculentum) and tartary buckwheat (F. tataricum) was evaluated by Liu et al. in 2008. Rutin is the main flavonoid found in both species, with fivefold higher levels identified in tartary buckwheat in this study. Ethanol extracts of tartary buckwheat also exhibited greater free radical scavenging activity and superoxide scavenging activity, compared with common buckwheat. Both buckwheat species displayed antioxidant activity on human hepatoma HepG2 cells, with tartary buckwheat more effective in diminishing cellular oxidative stress, which the authors attributed to its greater rutin and quercetin levels.5
Zhou et al. studied the protective effects of buckwheat honey on hydroxyl radical-induced DNA damage in 2012, finding that all studied honeys more effectively protected DNA in non–site specific rather than site-specific systems.6
Photoprotection
In a 2005 screening of 47 antioxidant substances and study of their effects on UV-induced lipid peroxidation, Trommer and Neubert reported that buckwheat extract significantly lowered radiation levels, as did extracts of St. John’s Wort, melissa, and sage. They concluded that their in vitro findings supported the inclusion of such ingredients in photoprotective cosmetic formulations or sunscreens pending the results of in vivo experiments with these compounds.7
In 2006, Hinneburg et al. evaluated the antioxidant and photoprotective activity of a buckwheat herb extract, also comparing its photoprotective characteristics to those of a commercial UV absorber. In an assay with 1,1-diphenyl-2-picryl-hydrazyl radical (DPPH), buckwheat extract exhibited significantly more antioxidant activity than did pure rutin, with buckwheat observed to more effectively block UV-induced peroxidation of linoleic acid as compared with rutin and the commercial UV absorber. The researchers concluded that including antioxidants such as buckwheat extract in photoprotective formulations may serve to maximize skin protection in such products.8
Buckwheat Sensitivity
Conclusion
Because it is a popular component in many diets around the world, especially Japan, Korea, Russia, and Poland, as well as other Asian and European countries, South Africa, Australia, and North America,4 it is reasonable to expect that we’ll see more research on buckwheat. For now, there are indications to suggest that more investigations are warranted to determine whether this botanical agent will have a meaningful role in the dermatologic armamentarium.
References
1. Li SQ et al. Crit Rev Food Sci Nutr. 2001 Sep;41(6):451-64.
2. Dattner AM. Dermatol Ther. 2003;16(2):106-13.
3. Hinneburg I et al. J Agric Food Chem. 2005 Jan 12;53(1):3-7.
4. van den Berg AJ et al. J Wound Care. 2008 Apr;17(4):172-4, 176-8.
5. Liu CL et al. J Agric Food Chem. 2008 Jan 9;56(1):173-8.
6. Zhou J et al. Food Chem Toxicol. 2012 Aug;50(8):2766-73.
7. Trommer H et al. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
8. Hinneburg I et al. Pharmazie. 2006 Mar;61(3):237-40.
9. Geiselhart S et al. Clin Exp Allergy. 2018 Feb;48(2):217-24.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
Native to North and East Asia, This highly adaptable plant – the most common species of which are Fagopyrum esculentum (common buckwheat or sweet buckwheat), and F. tataricum (which grows in more mountainous regions) – has acclimated to cultivation in North America, as well.1 Increasingly popular as a healthy grain option, buckwheat flour has been touted for beneficial effects on diabetes, obesity, hypertension, hypercholesterolemia, and constipation.1 It has also gained attention for its association with some allergic reactions.
Wound Healing
In 2008, van den Berg et al. performed an in vitro investigation of the antioxidant and anti-inflammatory qualities of buckwheat honey for consideration in wound healing. American buckwheat honey from New York was found to be the source of the most salient activities, with such properties attributed to its abundant phenolic components. The researchers suggested that these phenols might impart antibacterial activity, while the low pH and high free acid content of the buckwheat honey could contribute to healing wounds.4
Antioxidant Activity
The antioxidant capacity, along with other traits, characterizing the sprouts of common buckwheat (F. esculentum) and tartary buckwheat (F. tataricum) was evaluated by Liu et al. in 2008. Rutin is the main flavonoid found in both species, with fivefold higher levels identified in tartary buckwheat in this study. Ethanol extracts of tartary buckwheat also exhibited greater free radical scavenging activity and superoxide scavenging activity, compared with common buckwheat. Both buckwheat species displayed antioxidant activity on human hepatoma HepG2 cells, with tartary buckwheat more effective in diminishing cellular oxidative stress, which the authors attributed to its greater rutin and quercetin levels.5
Zhou et al. studied the protective effects of buckwheat honey on hydroxyl radical-induced DNA damage in 2012, finding that all studied honeys more effectively protected DNA in non–site specific rather than site-specific systems.6
Photoprotection
In a 2005 screening of 47 antioxidant substances and study of their effects on UV-induced lipid peroxidation, Trommer and Neubert reported that buckwheat extract significantly lowered radiation levels, as did extracts of St. John’s Wort, melissa, and sage. They concluded that their in vitro findings supported the inclusion of such ingredients in photoprotective cosmetic formulations or sunscreens pending the results of in vivo experiments with these compounds.7
In 2006, Hinneburg et al. evaluated the antioxidant and photoprotective activity of a buckwheat herb extract, also comparing its photoprotective characteristics to those of a commercial UV absorber. In an assay with 1,1-diphenyl-2-picryl-hydrazyl radical (DPPH), buckwheat extract exhibited significantly more antioxidant activity than did pure rutin, with buckwheat observed to more effectively block UV-induced peroxidation of linoleic acid as compared with rutin and the commercial UV absorber. The researchers concluded that including antioxidants such as buckwheat extract in photoprotective formulations may serve to maximize skin protection in such products.8
Buckwheat Sensitivity
Conclusion
Because it is a popular component in many diets around the world, especially Japan, Korea, Russia, and Poland, as well as other Asian and European countries, South Africa, Australia, and North America,4 it is reasonable to expect that we’ll see more research on buckwheat. For now, there are indications to suggest that more investigations are warranted to determine whether this botanical agent will have a meaningful role in the dermatologic armamentarium.
References
1. Li SQ et al. Crit Rev Food Sci Nutr. 2001 Sep;41(6):451-64.
2. Dattner AM. Dermatol Ther. 2003;16(2):106-13.
3. Hinneburg I et al. J Agric Food Chem. 2005 Jan 12;53(1):3-7.
4. van den Berg AJ et al. J Wound Care. 2008 Apr;17(4):172-4, 176-8.
5. Liu CL et al. J Agric Food Chem. 2008 Jan 9;56(1):173-8.
6. Zhou J et al. Food Chem Toxicol. 2012 Aug;50(8):2766-73.
7. Trommer H et al. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
8. Hinneburg I et al. Pharmazie. 2006 Mar;61(3):237-40.
9. Geiselhart S et al. Clin Exp Allergy. 2018 Feb;48(2):217-24.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
Native to North and East Asia, This highly adaptable plant – the most common species of which are Fagopyrum esculentum (common buckwheat or sweet buckwheat), and F. tataricum (which grows in more mountainous regions) – has acclimated to cultivation in North America, as well.1 Increasingly popular as a healthy grain option, buckwheat flour has been touted for beneficial effects on diabetes, obesity, hypertension, hypercholesterolemia, and constipation.1 It has also gained attention for its association with some allergic reactions.
Wound Healing
In 2008, van den Berg et al. performed an in vitro investigation of the antioxidant and anti-inflammatory qualities of buckwheat honey for consideration in wound healing. American buckwheat honey from New York was found to be the source of the most salient activities, with such properties attributed to its abundant phenolic components. The researchers suggested that these phenols might impart antibacterial activity, while the low pH and high free acid content of the buckwheat honey could contribute to healing wounds.4
Antioxidant Activity
The antioxidant capacity, along with other traits, characterizing the sprouts of common buckwheat (F. esculentum) and tartary buckwheat (F. tataricum) was evaluated by Liu et al. in 2008. Rutin is the main flavonoid found in both species, with fivefold higher levels identified in tartary buckwheat in this study. Ethanol extracts of tartary buckwheat also exhibited greater free radical scavenging activity and superoxide scavenging activity, compared with common buckwheat. Both buckwheat species displayed antioxidant activity on human hepatoma HepG2 cells, with tartary buckwheat more effective in diminishing cellular oxidative stress, which the authors attributed to its greater rutin and quercetin levels.5
Zhou et al. studied the protective effects of buckwheat honey on hydroxyl radical-induced DNA damage in 2012, finding that all studied honeys more effectively protected DNA in non–site specific rather than site-specific systems.6
Photoprotection
In a 2005 screening of 47 antioxidant substances and study of their effects on UV-induced lipid peroxidation, Trommer and Neubert reported that buckwheat extract significantly lowered radiation levels, as did extracts of St. John’s Wort, melissa, and sage. They concluded that their in vitro findings supported the inclusion of such ingredients in photoprotective cosmetic formulations or sunscreens pending the results of in vivo experiments with these compounds.7
In 2006, Hinneburg et al. evaluated the antioxidant and photoprotective activity of a buckwheat herb extract, also comparing its photoprotective characteristics to those of a commercial UV absorber. In an assay with 1,1-diphenyl-2-picryl-hydrazyl radical (DPPH), buckwheat extract exhibited significantly more antioxidant activity than did pure rutin, with buckwheat observed to more effectively block UV-induced peroxidation of linoleic acid as compared with rutin and the commercial UV absorber. The researchers concluded that including antioxidants such as buckwheat extract in photoprotective formulations may serve to maximize skin protection in such products.8
Buckwheat Sensitivity
Conclusion
Because it is a popular component in many diets around the world, especially Japan, Korea, Russia, and Poland, as well as other Asian and European countries, South Africa, Australia, and North America,4 it is reasonable to expect that we’ll see more research on buckwheat. For now, there are indications to suggest that more investigations are warranted to determine whether this botanical agent will have a meaningful role in the dermatologic armamentarium.
References
1. Li SQ et al. Crit Rev Food Sci Nutr. 2001 Sep;41(6):451-64.
2. Dattner AM. Dermatol Ther. 2003;16(2):106-13.
3. Hinneburg I et al. J Agric Food Chem. 2005 Jan 12;53(1):3-7.
4. van den Berg AJ et al. J Wound Care. 2008 Apr;17(4):172-4, 176-8.
5. Liu CL et al. J Agric Food Chem. 2008 Jan 9;56(1):173-8.
6. Zhou J et al. Food Chem Toxicol. 2012 Aug;50(8):2766-73.
7. Trommer H et al. J Pharm Pharm Sci. 2005 Sep 15;8(3):494-506.
8. Hinneburg I et al. Pharmazie. 2006 Mar;61(3):237-40.
9. Geiselhart S et al. Clin Exp Allergy. 2018 Feb;48(2):217-24.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
The role of defensins in treating skin aging
Most skin-aging treatments work by prodding old fibroblasts and keratinocytes to accelerate the production of important cellular components. For example, retinoids act on retinoic acid receptors to activate collagen genes and deactivate collagenase genes. Glycolic acid, ascorbic acid, and certain growth factors stimulate synthesis of collagen by fibroblasts. Older fibroblasts and keratinocytes are sluggish for many reasons; they do not “hear” signals as well as younger cells do. Glycosaminoglycans such as heparan sulfate can help cells hear these signals. Heparan sulfate, for example, assists in the delivery of growth factors to cells, stabilizes them, and presents them to the receptors on the keratinocytes and fibroblasts, and amplifies cellular response to these factors.
A new angle in antiaging skin care is to create new keratinocytes rather than to stimulate old cells. For the last decade, personal care companies have touted the benefit of putting stem cells in cosmeceuticals, claiming that these cells would rejuvenate skin. However, this proved to be unsubstantiated marketing hype because the stem cells were plant derived (often from apples), had poor shelf life, and could not intercalate between the native skin cells and work with them to have any effect. Stems cells in cosmeceuticals became a point of disdain for savvy scientists.
Stem cells
Wounding the skin stimulates LGR6+ stem cells. This occurs when neutrophils in the immune system release defensins in response to injury, and, in turn, defensins activate LGR6+ stem cells. Situated above the follicular bulge, these cells are reported to have the capacity to synthesize all cutaneous cell lineages, including sebaceous gland and interfollicular epidermal cells.1,2 There are no specific studies that show that the LGR6+ cells generate new fibroblasts, but it seems likely. Transplantation of LGR6+ stem cells into the skin results in increased wound healing, hair follicle genesis, and angiogenesis.3 LGR6+ stem cells repopulate the epidermis by creating new basal stem cells. In regards to skin rejuvenation, it is clear that activated LGR6+ stems cells produce new, younger-acting keratinocytes in the epidermis.
Peptides
Defensin is a peptide. Peptides are short amino acid chains. These important substances are challenging to incorporate into topical formulations for various reasons, including stabilization difficulty, interaction with other molecules, and poor penetration (greater than 500 Dalton molecular weight). For these reasons, many peptide-containing formulations do not have efficacy. Attempts are underway to better develop or modify peptide products to enhance solubility, achieve better penetration, and target increased receptor activity. Defensins are peptides, which makes them difficult to formulate in a topical product. Special steps must be taken in the formulation process to stabilize defensin and allow penetration into the hair follicle where the LGR6+ cells reside. Fortunately, it is easier for a peptide to target the hair follicle because it can traverse through the “pore” – than it is to get a peptide to reach the fibroblasts in the dermis.
Defensins
Defensins, or human beta-defensins, are host defense peptides that exhibit antimicrobial activities against numerous bacteria.4 LGR6+ stem cells, which are dormant until they are activated to respond to damage, are stimulated by defensins. Defensins have been shown to stimulate keratinocyte proliferation, migration, and wound healing. (3) **Human alpha-defensin 5 peptide has also been shown to enhance wound healing, increasing LGR5+ and LGR6+ stem cell migration in the wound bed.(1)***
When formulated in a manner that allows for stability and penetration into the hair follicle where the LGR6+ stem cells reside, defensin formulations can be applied topically. A product sold as DefenAge uses a patented formulation that uses albumin, a large and stable protein, to stabilize defensin and act as a carrier molecule while helping the defensin maintain its integrity and extend shelf life in the serum base. The albumin/defensin complex is incorporated into liposomes to prevent other ingredients in the cosmetic base from interacting with the peptide and to enhance delivery to the LGR6+ target cell.
The role of defensins in treating skin aging
- Old fibroblast and keratinocytes are sluggish and lazy.
- Old cells do not “hear” signals as well as younger cells.
- LGR6+ stem cells repopulate the epidermis with new, young keratinocytes.
- Defensin stimulates LGR6+ stem cells.
- The defensin/LGR6+ pathway plays a role in keratinization.
- Using topical defensin can improve the skin’s appearance.
Studying DefenAge
At this time, there is only one small multicenter, double-blind, placebo-controlled clinical study completed at three locations by investigators who are stockholders in the company and an independent dermatologic histopathologist who has no relation with the company; results have been reported in aesthetic dermatology industry newsletters. Each site had 15 patients for a total of 45 patients; all were women, aged 41-70 years (average age, 60 years), with little or no history of “quality” skin care. The study regimen used a system that contained alpha- and beta-defensins developed by Progenitor Biologics. Thirty patients used the three products in the DefenAge line: the 2-Minute Reveal Masque Exfoliator, 24/7 Barrier Balance Cream, and 8-in-1 BioSerum. The remaining patients received a three-part placebo system. Baseline biopsies were obtained to evaluate underlying conditions in the patients’ skin, and their skin was evaluated at 6 and 12 weeks, when additional biopsies were taken. Data analysis indicated that patients using DefenAge experienced significant improvement in coarse and fine wrinkles, pigmentation, pore prominence, epidermal thickness, as well as skin texture and evenness.
My personal opinion
I have never been a fan of formulations containing stem cells or peptides for the reasons listed above. DefenAge is unique in the way it has been stabilized, by penetrating the hair follicle rather than through the dermis and because defensin has very well-documented effects on the important LGR6+ stem cells. The effects of defensin on LGR6+ stem cells intrigue me. I do not intend to stop recommending retinoids for antiaging, but rather will add DefenAge to the antiaging regimen. In the past year, I have used DefenAge on many patients and have had many observations. I do not recommend starting retinoids and DefenAge at the same time because I have seen increased retinoid dermatitis. I suggest starting one the first month and then introducing the other product during the second month. Although no studies have been performed on this, my impression is that the DefenAge gives a quick result that helps improve patient compliance with the entire skin care regimen, but the effects reach a point at which no further improvement is seen. Combining DefenAge with a skin care regimen (targeted specifically to their Baumann Skin Type of course!) that includes a retinoid will increase efficacy. For wrinkle-prone skin types, I combine DefenAge with a retinoid, vitamin C, and heparan sulfate. After cleansing in the morning, I have them apply vitamin C followed by the DefenAge and an SPF. In the evening after cleansing, I have them apply a retinoid followed by a heparan sulfate analogue.
Conclusion
DefenAge offers a new approach to skin aging. At this time, there is much basic science research about the benefits of LGR6+ and that uses defensin to stimulate these stem cells; however, only one small clinical trial using defensin topically for antiaging has been published. It is doubtful that many studies will be performed because cosmetic companies are not allowed to make biologic claims so they have little incentive to demonstrate biologic changes. For this reason, we have to rely upon anecdotal reports from physicians such as the information that I have shared here.
Conflict of interest note: I have no financial relationship (no honorarium, stocks, or research funding) with Progenitor Biologics. I was asked to lecture in a DefenAge Symposium at the Vegas Cosmetic Surgery meeting but received no compensation. DefenAge products are sold through doctors, with my company, Skin Type Solutions Franchise Systems, as are heparan sulfate analogues, multiple brands of retinol, and 40 other product brands.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Lough D et al. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
2. Snippert HJ et al. Science. 2010 Mar 12;327(5971):1385-9.
3. Lough DM et al. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
4. Kiatsurayanon C et al. J Invest Dermatol. 2014 Aug;134(8):2163-73.
Most skin-aging treatments work by prodding old fibroblasts and keratinocytes to accelerate the production of important cellular components. For example, retinoids act on retinoic acid receptors to activate collagen genes and deactivate collagenase genes. Glycolic acid, ascorbic acid, and certain growth factors stimulate synthesis of collagen by fibroblasts. Older fibroblasts and keratinocytes are sluggish for many reasons; they do not “hear” signals as well as younger cells do. Glycosaminoglycans such as heparan sulfate can help cells hear these signals. Heparan sulfate, for example, assists in the delivery of growth factors to cells, stabilizes them, and presents them to the receptors on the keratinocytes and fibroblasts, and amplifies cellular response to these factors.
A new angle in antiaging skin care is to create new keratinocytes rather than to stimulate old cells. For the last decade, personal care companies have touted the benefit of putting stem cells in cosmeceuticals, claiming that these cells would rejuvenate skin. However, this proved to be unsubstantiated marketing hype because the stem cells were plant derived (often from apples), had poor shelf life, and could not intercalate between the native skin cells and work with them to have any effect. Stems cells in cosmeceuticals became a point of disdain for savvy scientists.
Stem cells
Wounding the skin stimulates LGR6+ stem cells. This occurs when neutrophils in the immune system release defensins in response to injury, and, in turn, defensins activate LGR6+ stem cells. Situated above the follicular bulge, these cells are reported to have the capacity to synthesize all cutaneous cell lineages, including sebaceous gland and interfollicular epidermal cells.1,2 There are no specific studies that show that the LGR6+ cells generate new fibroblasts, but it seems likely. Transplantation of LGR6+ stem cells into the skin results in increased wound healing, hair follicle genesis, and angiogenesis.3 LGR6+ stem cells repopulate the epidermis by creating new basal stem cells. In regards to skin rejuvenation, it is clear that activated LGR6+ stems cells produce new, younger-acting keratinocytes in the epidermis.
Peptides
Defensin is a peptide. Peptides are short amino acid chains. These important substances are challenging to incorporate into topical formulations for various reasons, including stabilization difficulty, interaction with other molecules, and poor penetration (greater than 500 Dalton molecular weight). For these reasons, many peptide-containing formulations do not have efficacy. Attempts are underway to better develop or modify peptide products to enhance solubility, achieve better penetration, and target increased receptor activity. Defensins are peptides, which makes them difficult to formulate in a topical product. Special steps must be taken in the formulation process to stabilize defensin and allow penetration into the hair follicle where the LGR6+ cells reside. Fortunately, it is easier for a peptide to target the hair follicle because it can traverse through the “pore” – than it is to get a peptide to reach the fibroblasts in the dermis.
Defensins
Defensins, or human beta-defensins, are host defense peptides that exhibit antimicrobial activities against numerous bacteria.4 LGR6+ stem cells, which are dormant until they are activated to respond to damage, are stimulated by defensins. Defensins have been shown to stimulate keratinocyte proliferation, migration, and wound healing. (3) **Human alpha-defensin 5 peptide has also been shown to enhance wound healing, increasing LGR5+ and LGR6+ stem cell migration in the wound bed.(1)***
When formulated in a manner that allows for stability and penetration into the hair follicle where the LGR6+ stem cells reside, defensin formulations can be applied topically. A product sold as DefenAge uses a patented formulation that uses albumin, a large and stable protein, to stabilize defensin and act as a carrier molecule while helping the defensin maintain its integrity and extend shelf life in the serum base. The albumin/defensin complex is incorporated into liposomes to prevent other ingredients in the cosmetic base from interacting with the peptide and to enhance delivery to the LGR6+ target cell.
The role of defensins in treating skin aging
- Old fibroblast and keratinocytes are sluggish and lazy.
- Old cells do not “hear” signals as well as younger cells.
- LGR6+ stem cells repopulate the epidermis with new, young keratinocytes.
- Defensin stimulates LGR6+ stem cells.
- The defensin/LGR6+ pathway plays a role in keratinization.
- Using topical defensin can improve the skin’s appearance.
Studying DefenAge
At this time, there is only one small multicenter, double-blind, placebo-controlled clinical study completed at three locations by investigators who are stockholders in the company and an independent dermatologic histopathologist who has no relation with the company; results have been reported in aesthetic dermatology industry newsletters. Each site had 15 patients for a total of 45 patients; all were women, aged 41-70 years (average age, 60 years), with little or no history of “quality” skin care. The study regimen used a system that contained alpha- and beta-defensins developed by Progenitor Biologics. Thirty patients used the three products in the DefenAge line: the 2-Minute Reveal Masque Exfoliator, 24/7 Barrier Balance Cream, and 8-in-1 BioSerum. The remaining patients received a three-part placebo system. Baseline biopsies were obtained to evaluate underlying conditions in the patients’ skin, and their skin was evaluated at 6 and 12 weeks, when additional biopsies were taken. Data analysis indicated that patients using DefenAge experienced significant improvement in coarse and fine wrinkles, pigmentation, pore prominence, epidermal thickness, as well as skin texture and evenness.
My personal opinion
I have never been a fan of formulations containing stem cells or peptides for the reasons listed above. DefenAge is unique in the way it has been stabilized, by penetrating the hair follicle rather than through the dermis and because defensin has very well-documented effects on the important LGR6+ stem cells. The effects of defensin on LGR6+ stem cells intrigue me. I do not intend to stop recommending retinoids for antiaging, but rather will add DefenAge to the antiaging regimen. In the past year, I have used DefenAge on many patients and have had many observations. I do not recommend starting retinoids and DefenAge at the same time because I have seen increased retinoid dermatitis. I suggest starting one the first month and then introducing the other product during the second month. Although no studies have been performed on this, my impression is that the DefenAge gives a quick result that helps improve patient compliance with the entire skin care regimen, but the effects reach a point at which no further improvement is seen. Combining DefenAge with a skin care regimen (targeted specifically to their Baumann Skin Type of course!) that includes a retinoid will increase efficacy. For wrinkle-prone skin types, I combine DefenAge with a retinoid, vitamin C, and heparan sulfate. After cleansing in the morning, I have them apply vitamin C followed by the DefenAge and an SPF. In the evening after cleansing, I have them apply a retinoid followed by a heparan sulfate analogue.
Conclusion
DefenAge offers a new approach to skin aging. At this time, there is much basic science research about the benefits of LGR6+ and that uses defensin to stimulate these stem cells; however, only one small clinical trial using defensin topically for antiaging has been published. It is doubtful that many studies will be performed because cosmetic companies are not allowed to make biologic claims so they have little incentive to demonstrate biologic changes. For this reason, we have to rely upon anecdotal reports from physicians such as the information that I have shared here.
Conflict of interest note: I have no financial relationship (no honorarium, stocks, or research funding) with Progenitor Biologics. I was asked to lecture in a DefenAge Symposium at the Vegas Cosmetic Surgery meeting but received no compensation. DefenAge products are sold through doctors, with my company, Skin Type Solutions Franchise Systems, as are heparan sulfate analogues, multiple brands of retinol, and 40 other product brands.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Lough D et al. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
2. Snippert HJ et al. Science. 2010 Mar 12;327(5971):1385-9.
3. Lough DM et al. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
4. Kiatsurayanon C et al. J Invest Dermatol. 2014 Aug;134(8):2163-73.
Most skin-aging treatments work by prodding old fibroblasts and keratinocytes to accelerate the production of important cellular components. For example, retinoids act on retinoic acid receptors to activate collagen genes and deactivate collagenase genes. Glycolic acid, ascorbic acid, and certain growth factors stimulate synthesis of collagen by fibroblasts. Older fibroblasts and keratinocytes are sluggish for many reasons; they do not “hear” signals as well as younger cells do. Glycosaminoglycans such as heparan sulfate can help cells hear these signals. Heparan sulfate, for example, assists in the delivery of growth factors to cells, stabilizes them, and presents them to the receptors on the keratinocytes and fibroblasts, and amplifies cellular response to these factors.
A new angle in antiaging skin care is to create new keratinocytes rather than to stimulate old cells. For the last decade, personal care companies have touted the benefit of putting stem cells in cosmeceuticals, claiming that these cells would rejuvenate skin. However, this proved to be unsubstantiated marketing hype because the stem cells were plant derived (often from apples), had poor shelf life, and could not intercalate between the native skin cells and work with them to have any effect. Stems cells in cosmeceuticals became a point of disdain for savvy scientists.
Stem cells
Wounding the skin stimulates LGR6+ stem cells. This occurs when neutrophils in the immune system release defensins in response to injury, and, in turn, defensins activate LGR6+ stem cells. Situated above the follicular bulge, these cells are reported to have the capacity to synthesize all cutaneous cell lineages, including sebaceous gland and interfollicular epidermal cells.1,2 There are no specific studies that show that the LGR6+ cells generate new fibroblasts, but it seems likely. Transplantation of LGR6+ stem cells into the skin results in increased wound healing, hair follicle genesis, and angiogenesis.3 LGR6+ stem cells repopulate the epidermis by creating new basal stem cells. In regards to skin rejuvenation, it is clear that activated LGR6+ stems cells produce new, younger-acting keratinocytes in the epidermis.
Peptides
Defensin is a peptide. Peptides are short amino acid chains. These important substances are challenging to incorporate into topical formulations for various reasons, including stabilization difficulty, interaction with other molecules, and poor penetration (greater than 500 Dalton molecular weight). For these reasons, many peptide-containing formulations do not have efficacy. Attempts are underway to better develop or modify peptide products to enhance solubility, achieve better penetration, and target increased receptor activity. Defensins are peptides, which makes them difficult to formulate in a topical product. Special steps must be taken in the formulation process to stabilize defensin and allow penetration into the hair follicle where the LGR6+ cells reside. Fortunately, it is easier for a peptide to target the hair follicle because it can traverse through the “pore” – than it is to get a peptide to reach the fibroblasts in the dermis.
Defensins
Defensins, or human beta-defensins, are host defense peptides that exhibit antimicrobial activities against numerous bacteria.4 LGR6+ stem cells, which are dormant until they are activated to respond to damage, are stimulated by defensins. Defensins have been shown to stimulate keratinocyte proliferation, migration, and wound healing. (3) **Human alpha-defensin 5 peptide has also been shown to enhance wound healing, increasing LGR5+ and LGR6+ stem cell migration in the wound bed.(1)***
When formulated in a manner that allows for stability and penetration into the hair follicle where the LGR6+ stem cells reside, defensin formulations can be applied topically. A product sold as DefenAge uses a patented formulation that uses albumin, a large and stable protein, to stabilize defensin and act as a carrier molecule while helping the defensin maintain its integrity and extend shelf life in the serum base. The albumin/defensin complex is incorporated into liposomes to prevent other ingredients in the cosmetic base from interacting with the peptide and to enhance delivery to the LGR6+ target cell.
The role of defensins in treating skin aging
- Old fibroblast and keratinocytes are sluggish and lazy.
- Old cells do not “hear” signals as well as younger cells.
- LGR6+ stem cells repopulate the epidermis with new, young keratinocytes.
- Defensin stimulates LGR6+ stem cells.
- The defensin/LGR6+ pathway plays a role in keratinization.
- Using topical defensin can improve the skin’s appearance.
Studying DefenAge
At this time, there is only one small multicenter, double-blind, placebo-controlled clinical study completed at three locations by investigators who are stockholders in the company and an independent dermatologic histopathologist who has no relation with the company; results have been reported in aesthetic dermatology industry newsletters. Each site had 15 patients for a total of 45 patients; all were women, aged 41-70 years (average age, 60 years), with little or no history of “quality” skin care. The study regimen used a system that contained alpha- and beta-defensins developed by Progenitor Biologics. Thirty patients used the three products in the DefenAge line: the 2-Minute Reveal Masque Exfoliator, 24/7 Barrier Balance Cream, and 8-in-1 BioSerum. The remaining patients received a three-part placebo system. Baseline biopsies were obtained to evaluate underlying conditions in the patients’ skin, and their skin was evaluated at 6 and 12 weeks, when additional biopsies were taken. Data analysis indicated that patients using DefenAge experienced significant improvement in coarse and fine wrinkles, pigmentation, pore prominence, epidermal thickness, as well as skin texture and evenness.
My personal opinion
I have never been a fan of formulations containing stem cells or peptides for the reasons listed above. DefenAge is unique in the way it has been stabilized, by penetrating the hair follicle rather than through the dermis and because defensin has very well-documented effects on the important LGR6+ stem cells. The effects of defensin on LGR6+ stem cells intrigue me. I do not intend to stop recommending retinoids for antiaging, but rather will add DefenAge to the antiaging regimen. In the past year, I have used DefenAge on many patients and have had many observations. I do not recommend starting retinoids and DefenAge at the same time because I have seen increased retinoid dermatitis. I suggest starting one the first month and then introducing the other product during the second month. Although no studies have been performed on this, my impression is that the DefenAge gives a quick result that helps improve patient compliance with the entire skin care regimen, but the effects reach a point at which no further improvement is seen. Combining DefenAge with a skin care regimen (targeted specifically to their Baumann Skin Type of course!) that includes a retinoid will increase efficacy. For wrinkle-prone skin types, I combine DefenAge with a retinoid, vitamin C, and heparan sulfate. After cleansing in the morning, I have them apply vitamin C followed by the DefenAge and an SPF. In the evening after cleansing, I have them apply a retinoid followed by a heparan sulfate analogue.
Conclusion
DefenAge offers a new approach to skin aging. At this time, there is much basic science research about the benefits of LGR6+ and that uses defensin to stimulate these stem cells; however, only one small clinical trial using defensin topically for antiaging has been published. It is doubtful that many studies will be performed because cosmetic companies are not allowed to make biologic claims so they have little incentive to demonstrate biologic changes. For this reason, we have to rely upon anecdotal reports from physicians such as the information that I have shared here.
Conflict of interest note: I have no financial relationship (no honorarium, stocks, or research funding) with Progenitor Biologics. I was asked to lecture in a DefenAge Symposium at the Vegas Cosmetic Surgery meeting but received no compensation. DefenAge products are sold through doctors, with my company, Skin Type Solutions Franchise Systems, as are heparan sulfate analogues, multiple brands of retinol, and 40 other product brands.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002) and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014); she also authored a New York Times Best Seller for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance Therapeutics. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC.
References
1. Lough D et al. Plast Reconstr Surg. 2013 Nov;132(5):1159-71.
2. Snippert HJ et al. Science. 2010 Mar 12;327(5971):1385-9.
3. Lough DM et al. Plast Reconstr Surg. 2014 Mar;133(3):579-90.
4. Kiatsurayanon C et al. J Invest Dermatol. 2014 Aug;134(8):2163-73.
Vitamin C
Vitamin C (ascorbic acid) is one of the four most important ingredients in skin care products.
• It is proven to increase collagen production when applied topically to skin.
• It inhibits tyrosinase to even skin tone and has a strong antioxidant activity.
• It is absorbed well orally, but not enough gets to the skin.
• It is best absorbed at a pH of 2.0.
• It is unstable when exposed to light and air. Instruct patients to discard 6 months after opening.
In addition, the proper formulation is patented and expensive. Stick with brands you trust. Use vitamin C on skin prior to procedures to speed healing. It will sting when used on inflamed skin because of the low pH.
In my opinion, all patients need to be on the proper skin care regimen for their skin type. This includes a daily sun protection factor (SPF), a cleanser, a retinoid, and an antioxidant. Ascorbic acid is one of my favorite antioxidants because it is the only one shown to increase the production of collagen by fibroblasts and inhibit tyrosinase while scavenging free radicals. Sure it is expensive – but that is because formulating and packaging it properly is expensive. Unfortunately, many subpar brands have entered the market. Ask to see the company’s research data on its formulation before choosing to recommend or sell ascorbic acid/vitamin C in your practice.
An essential water-soluble nutrient for the development of bone and connective tissue, vitamin C is found in citrus fruits and green leafy vegetables. It is produced in most plants and animals, but a mutated gene in humans has resulted in a deficiency of L-gulono-gamma-lactone oxidase, the enzyme required for its production.1,2 Although ascorbic acid cannot be synthesized by the human body, dietary consumption renders it the most abundant antioxidant in human skin and blood, and vitamin C plays an important role in endogenous collagen production and the inhibition of collagen degradation.3-6 Ascorbic acid also is known to regenerate alpha-tocopherol (vitamin E) levels and, therefore, is thought to protect against diseases related to oxidative stress.7
Epidermal vitamin C can be depleted by sunlight and environmental pollution, such as ozone in urban pollution.8,9 Known to exhibit a wide range of biologic activities, ascorbic acid has been shown to deliver rejuvenating effects on skin wrinkles, texture, strength, and evenness of tone through its antioxidant, tyrosinase-inhibiting, and collagen production-promoting activities.10 Indeed, as a topical agent, vitamin C has been used to prevent photodamage, and to treat melasma, striae alba, and postoperative erythema in laser patients.11,12 It is regularly used to treat aging skin, and as a depigmenting agent.2,10,13 This column will discuss the antioxidant, antiaging, and depigmenting activity of vitamin C in the context of recent human studies.
Antioxidant and anti-aging activity
Vitamin C is unique among antioxidants because of its ability to increase collagen production in addition to its free radical scavenging antioxidant activity. Due to its capacity to interfere with the UV-induced generation of reactive oxygen species by reacting with the superoxide anion or the hydroxyl radical, vitamin C has become a popular addition to “after-sun” products,14,15 and been shown to be effective in mitigating the effects of UVB, such as erythema and signs of photoaging, on porcine and human skin.2,16-17
A 2001 study in 10 postmenopausal women by Nusgens et al. found that daily topical application of 5% L-ascorbic acid enhanced the levels of procollagen types I and III, their posttranslational maturation enzymes, and tissue inhibitor of matrix metalloproteinase.18 This led to increased levels of collagen in the skin.
In 2003, Humbert et al. conducted a 6-month, double-blind, vehicle-controlled trial with 20 healthy female volunteers showing that patients treated with 5% vitamin C cream experienced significant improvements in deep furrows on the neck and forearms.19
In a small study of nine adults with Fitzpatrick skin types II or III in 2008, Murray et al. studied whether a stable topical preparation of 15% L-ascorbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid could protect human skin in vivo from UV-induced damage. They found that the antioxidant formulation supplemented the antioxidant pool of the skin and conferred significant photoprotection, guarding the skin against erythema and apoptosis as well as effectively suppressing p53 activation and reducing thymine dimer mutations known to be associated with skin cancer.13
In 2012, Xu et al. evaluated the efficacy and safety of topical 23.8% L-ascorbic acid on photoaged skin in a split-face study of 20 Chinese women. Significant improvements in fine lines, dyspigmentation, and surface roughness were observed, without adverse side effects.20
In a 2015 study of 60 healthy female subjects, Crisan et al. used high-frequency ultrasound to determine that the use of a topical vitamin C formulation yielded significant increases in collagen synthesis, revealing the solution to be an effective rejuvenation therapy.21
Skin lightening activity
Melasma
In 2004, Espinal-Perez et al. conducted a double-blind randomized trial of 5% ascorbic acid, compared with 4% hydroquinone (HQ) water–oil emulsion in 16 female patients with melasma, aged 23-43 years (mean 36 years). Of those treated with vitamin C, 62.5% exhibited good or excellent subjectively assessed skin lightening. There was no statistically significant difference in depigmenting activity in the HQ group, of which 68.7% experienced irritation whereas vitamin C was well tolerated.22
In a randomized, double-blind, placebo-controlled study, researchers used iontophoresis to enhance the penetration of vitamin C into the skin and significantly reduce pigmentation, compared with placebo.23
Although ascorbic acid is viewed by many as ineffective as a depigmenting agent alone, particularly in 5%-10% concentrations, when used in combination with other ingredients such as HQ, it is considered effective.24 In the magnesium-L-ascorbyl-2-phosphate esterified form, however, vitamin C is among the most popular prescribed depigmenting agents around the world, especially in countries where HQ and its derivatives are prohibited.25 In a 2009 16-week open-label study by Hwang et al. of 25% L-ascorbic acid and a chemical penetration enhancer for treating melasma in 40 patients, researchers observed significant reductions in pigmentation.26
In a small split-face study early in 2015, Lee et al. showed that the combination of 1,064-nm Q-switched neodymium-doped yttrium aluminum garnet (QS-Nd:YAG) laser and ultrasonic application of vitamin C was more effective than was the laser treatment alone in achieving a cosmetically acceptable treatment for melasma.27
PIPA
Vitamin C can be used to diminish or prevent post-inflammatory pigment alteration (PIPA) after procedures because it inhibits tyrosinase, lowers inflammation, and quenches free radicals. In a study of 10 patients, the application of topical vitamin C 2 or more weeks after surgery reduced the duration and degree of erythema after skin resurfacing with a carbon dioxide laser.28
Stretch marks
The depigmenting effects of vitamin C can lighten the pigmentation associated with stretch marks and its anti-inflammatory activity can contribute to blunting related redness.12
Conclusion
Although orally administered ascorbic acid is readily bioavailable, ascorbic acid in the skin is quickly depleted and oral supplementation alone does not yield optimal skin levels. Therefore, topical use of vitamin C is desirable. In fact, I tell my patients to use it topically in the morning and add a vitamin C supplement to their diet. Numerous formulation considerations (e.g., packaging, exposure to air or light during use, skin sensitivity, and user preference) are involved in the stabilization and effective penetration of ascorbic acid into the skin, and the process of developing, manufacturing, and packaging of effective, stable vitamin C products is expensive.
Vitamin C, particularly when combined with other ingredients, has been shown to be an integral constituent in topical antioxidant, antiaging, and depigmenting formulations that show promise in the dermatologic armamentarium. It is a great choice for use in a prep-procedure skin care regimen to speed healing. Use after a procedure is prohibited by the stinging associated with the low pH of properly formulated products.
References
1. J Biol Chem. 1994 May 6;269(18):13685-8.
2. Dermatol Surg. 2001 Feb;27(2):137-42.
3. J Invest Dermatol. 1994 Jan;102(1):122-4.
4. Dermatol Surg. 2005 Jul;31(7 Pt 2):814-7.
5. Annu Rev Nutr. 1994;14:371-91.
6. J Drugs Dermatol. 2008 Jul;7(7 Suppl):s2-6.
7. J Am Acad Dermatol. 2003 Jun;48(6):866-74.
8. J Invest Dermatol. 1994 Apr;102(4):470-5.
9. Free Radic Biol Med. 1997;23:85-91.
10. J Drugs Dermatol. 2014 Oct;13(10):1208-13.
11. J Am Acad Dermatol. 1996 Jan;34(1):29-33.
12. Dermatol Surg. 1998 Aug;24(8):849-56.
13. J Am Acad Dermatol. 2008 Sep;59(3):418-25.
14. J Biol Chem. 1983 Jun 10;258(11):6695-7.
15. J Phys Chem. 1983;87:1809-12.
16. Br J Dermatol. 1992 Sep;127(3):247-53.
17. J Invest Dermatol. 1991;96:587.
18. J Invest Dermatol. 2001 Jun;116(6):853-9.
19. Exp Dermatol. 2003 Jun;12(3):237-44.
20. J Drugs Dermatol. 2012 Jan;11(1):51-6.
21. Clin Cosmet Investig Dermatol. 2015 Sep 2;8:463-70
22. Int J Dermatol. 2004 Aug;43(8):604-7.
23. Dermatology. 2003;206(4):316-20.
24. Am J Clin Dermatol. 2011 Apr 1;12(2):87-99.
25. Phytother Res. 2006 Nov;20(11):921-34.
26. J Cutan Med Surg. 2009 Mar-Apr;13(2):74-81.
27. Lasers Med Sci. 2015 Jan;30(1):159-63.
28. Dermatol Surg. 1998 Mar;24(3):331-4.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Vitamin C (ascorbic acid) is one of the four most important ingredients in skin care products.
• It is proven to increase collagen production when applied topically to skin.
• It inhibits tyrosinase to even skin tone and has a strong antioxidant activity.
• It is absorbed well orally, but not enough gets to the skin.
• It is best absorbed at a pH of 2.0.
• It is unstable when exposed to light and air. Instruct patients to discard 6 months after opening.
In addition, the proper formulation is patented and expensive. Stick with brands you trust. Use vitamin C on skin prior to procedures to speed healing. It will sting when used on inflamed skin because of the low pH.
In my opinion, all patients need to be on the proper skin care regimen for their skin type. This includes a daily sun protection factor (SPF), a cleanser, a retinoid, and an antioxidant. Ascorbic acid is one of my favorite antioxidants because it is the only one shown to increase the production of collagen by fibroblasts and inhibit tyrosinase while scavenging free radicals. Sure it is expensive – but that is because formulating and packaging it properly is expensive. Unfortunately, many subpar brands have entered the market. Ask to see the company’s research data on its formulation before choosing to recommend or sell ascorbic acid/vitamin C in your practice.
An essential water-soluble nutrient for the development of bone and connective tissue, vitamin C is found in citrus fruits and green leafy vegetables. It is produced in most plants and animals, but a mutated gene in humans has resulted in a deficiency of L-gulono-gamma-lactone oxidase, the enzyme required for its production.1,2 Although ascorbic acid cannot be synthesized by the human body, dietary consumption renders it the most abundant antioxidant in human skin and blood, and vitamin C plays an important role in endogenous collagen production and the inhibition of collagen degradation.3-6 Ascorbic acid also is known to regenerate alpha-tocopherol (vitamin E) levels and, therefore, is thought to protect against diseases related to oxidative stress.7
Epidermal vitamin C can be depleted by sunlight and environmental pollution, such as ozone in urban pollution.8,9 Known to exhibit a wide range of biologic activities, ascorbic acid has been shown to deliver rejuvenating effects on skin wrinkles, texture, strength, and evenness of tone through its antioxidant, tyrosinase-inhibiting, and collagen production-promoting activities.10 Indeed, as a topical agent, vitamin C has been used to prevent photodamage, and to treat melasma, striae alba, and postoperative erythema in laser patients.11,12 It is regularly used to treat aging skin, and as a depigmenting agent.2,10,13 This column will discuss the antioxidant, antiaging, and depigmenting activity of vitamin C in the context of recent human studies.
Antioxidant and anti-aging activity
Vitamin C is unique among antioxidants because of its ability to increase collagen production in addition to its free radical scavenging antioxidant activity. Due to its capacity to interfere with the UV-induced generation of reactive oxygen species by reacting with the superoxide anion or the hydroxyl radical, vitamin C has become a popular addition to “after-sun” products,14,15 and been shown to be effective in mitigating the effects of UVB, such as erythema and signs of photoaging, on porcine and human skin.2,16-17
A 2001 study in 10 postmenopausal women by Nusgens et al. found that daily topical application of 5% L-ascorbic acid enhanced the levels of procollagen types I and III, their posttranslational maturation enzymes, and tissue inhibitor of matrix metalloproteinase.18 This led to increased levels of collagen in the skin.
In 2003, Humbert et al. conducted a 6-month, double-blind, vehicle-controlled trial with 20 healthy female volunteers showing that patients treated with 5% vitamin C cream experienced significant improvements in deep furrows on the neck and forearms.19
In a small study of nine adults with Fitzpatrick skin types II or III in 2008, Murray et al. studied whether a stable topical preparation of 15% L-ascorbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid could protect human skin in vivo from UV-induced damage. They found that the antioxidant formulation supplemented the antioxidant pool of the skin and conferred significant photoprotection, guarding the skin against erythema and apoptosis as well as effectively suppressing p53 activation and reducing thymine dimer mutations known to be associated with skin cancer.13
In 2012, Xu et al. evaluated the efficacy and safety of topical 23.8% L-ascorbic acid on photoaged skin in a split-face study of 20 Chinese women. Significant improvements in fine lines, dyspigmentation, and surface roughness were observed, without adverse side effects.20
In a 2015 study of 60 healthy female subjects, Crisan et al. used high-frequency ultrasound to determine that the use of a topical vitamin C formulation yielded significant increases in collagen synthesis, revealing the solution to be an effective rejuvenation therapy.21
Skin lightening activity
Melasma
In 2004, Espinal-Perez et al. conducted a double-blind randomized trial of 5% ascorbic acid, compared with 4% hydroquinone (HQ) water–oil emulsion in 16 female patients with melasma, aged 23-43 years (mean 36 years). Of those treated with vitamin C, 62.5% exhibited good or excellent subjectively assessed skin lightening. There was no statistically significant difference in depigmenting activity in the HQ group, of which 68.7% experienced irritation whereas vitamin C was well tolerated.22
In a randomized, double-blind, placebo-controlled study, researchers used iontophoresis to enhance the penetration of vitamin C into the skin and significantly reduce pigmentation, compared with placebo.23
Although ascorbic acid is viewed by many as ineffective as a depigmenting agent alone, particularly in 5%-10% concentrations, when used in combination with other ingredients such as HQ, it is considered effective.24 In the magnesium-L-ascorbyl-2-phosphate esterified form, however, vitamin C is among the most popular prescribed depigmenting agents around the world, especially in countries where HQ and its derivatives are prohibited.25 In a 2009 16-week open-label study by Hwang et al. of 25% L-ascorbic acid and a chemical penetration enhancer for treating melasma in 40 patients, researchers observed significant reductions in pigmentation.26
In a small split-face study early in 2015, Lee et al. showed that the combination of 1,064-nm Q-switched neodymium-doped yttrium aluminum garnet (QS-Nd:YAG) laser and ultrasonic application of vitamin C was more effective than was the laser treatment alone in achieving a cosmetically acceptable treatment for melasma.27
PIPA
Vitamin C can be used to diminish or prevent post-inflammatory pigment alteration (PIPA) after procedures because it inhibits tyrosinase, lowers inflammation, and quenches free radicals. In a study of 10 patients, the application of topical vitamin C 2 or more weeks after surgery reduced the duration and degree of erythema after skin resurfacing with a carbon dioxide laser.28
Stretch marks
The depigmenting effects of vitamin C can lighten the pigmentation associated with stretch marks and its anti-inflammatory activity can contribute to blunting related redness.12
Conclusion
Although orally administered ascorbic acid is readily bioavailable, ascorbic acid in the skin is quickly depleted and oral supplementation alone does not yield optimal skin levels. Therefore, topical use of vitamin C is desirable. In fact, I tell my patients to use it topically in the morning and add a vitamin C supplement to their diet. Numerous formulation considerations (e.g., packaging, exposure to air or light during use, skin sensitivity, and user preference) are involved in the stabilization and effective penetration of ascorbic acid into the skin, and the process of developing, manufacturing, and packaging of effective, stable vitamin C products is expensive.
Vitamin C, particularly when combined with other ingredients, has been shown to be an integral constituent in topical antioxidant, antiaging, and depigmenting formulations that show promise in the dermatologic armamentarium. It is a great choice for use in a prep-procedure skin care regimen to speed healing. Use after a procedure is prohibited by the stinging associated with the low pH of properly formulated products.
References
1. J Biol Chem. 1994 May 6;269(18):13685-8.
2. Dermatol Surg. 2001 Feb;27(2):137-42.
3. J Invest Dermatol. 1994 Jan;102(1):122-4.
4. Dermatol Surg. 2005 Jul;31(7 Pt 2):814-7.
5. Annu Rev Nutr. 1994;14:371-91.
6. J Drugs Dermatol. 2008 Jul;7(7 Suppl):s2-6.
7. J Am Acad Dermatol. 2003 Jun;48(6):866-74.
8. J Invest Dermatol. 1994 Apr;102(4):470-5.
9. Free Radic Biol Med. 1997;23:85-91.
10. J Drugs Dermatol. 2014 Oct;13(10):1208-13.
11. J Am Acad Dermatol. 1996 Jan;34(1):29-33.
12. Dermatol Surg. 1998 Aug;24(8):849-56.
13. J Am Acad Dermatol. 2008 Sep;59(3):418-25.
14. J Biol Chem. 1983 Jun 10;258(11):6695-7.
15. J Phys Chem. 1983;87:1809-12.
16. Br J Dermatol. 1992 Sep;127(3):247-53.
17. J Invest Dermatol. 1991;96:587.
18. J Invest Dermatol. 2001 Jun;116(6):853-9.
19. Exp Dermatol. 2003 Jun;12(3):237-44.
20. J Drugs Dermatol. 2012 Jan;11(1):51-6.
21. Clin Cosmet Investig Dermatol. 2015 Sep 2;8:463-70
22. Int J Dermatol. 2004 Aug;43(8):604-7.
23. Dermatology. 2003;206(4):316-20.
24. Am J Clin Dermatol. 2011 Apr 1;12(2):87-99.
25. Phytother Res. 2006 Nov;20(11):921-34.
26. J Cutan Med Surg. 2009 Mar-Apr;13(2):74-81.
27. Lasers Med Sci. 2015 Jan;30(1):159-63.
28. Dermatol Surg. 1998 Mar;24(3):331-4.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Vitamin C (ascorbic acid) is one of the four most important ingredients in skin care products.
• It is proven to increase collagen production when applied topically to skin.
• It inhibits tyrosinase to even skin tone and has a strong antioxidant activity.
• It is absorbed well orally, but not enough gets to the skin.
• It is best absorbed at a pH of 2.0.
• It is unstable when exposed to light and air. Instruct patients to discard 6 months after opening.
In addition, the proper formulation is patented and expensive. Stick with brands you trust. Use vitamin C on skin prior to procedures to speed healing. It will sting when used on inflamed skin because of the low pH.
In my opinion, all patients need to be on the proper skin care regimen for their skin type. This includes a daily sun protection factor (SPF), a cleanser, a retinoid, and an antioxidant. Ascorbic acid is one of my favorite antioxidants because it is the only one shown to increase the production of collagen by fibroblasts and inhibit tyrosinase while scavenging free radicals. Sure it is expensive – but that is because formulating and packaging it properly is expensive. Unfortunately, many subpar brands have entered the market. Ask to see the company’s research data on its formulation before choosing to recommend or sell ascorbic acid/vitamin C in your practice.
An essential water-soluble nutrient for the development of bone and connective tissue, vitamin C is found in citrus fruits and green leafy vegetables. It is produced in most plants and animals, but a mutated gene in humans has resulted in a deficiency of L-gulono-gamma-lactone oxidase, the enzyme required for its production.1,2 Although ascorbic acid cannot be synthesized by the human body, dietary consumption renders it the most abundant antioxidant in human skin and blood, and vitamin C plays an important role in endogenous collagen production and the inhibition of collagen degradation.3-6 Ascorbic acid also is known to regenerate alpha-tocopherol (vitamin E) levels and, therefore, is thought to protect against diseases related to oxidative stress.7
Epidermal vitamin C can be depleted by sunlight and environmental pollution, such as ozone in urban pollution.8,9 Known to exhibit a wide range of biologic activities, ascorbic acid has been shown to deliver rejuvenating effects on skin wrinkles, texture, strength, and evenness of tone through its antioxidant, tyrosinase-inhibiting, and collagen production-promoting activities.10 Indeed, as a topical agent, vitamin C has been used to prevent photodamage, and to treat melasma, striae alba, and postoperative erythema in laser patients.11,12 It is regularly used to treat aging skin, and as a depigmenting agent.2,10,13 This column will discuss the antioxidant, antiaging, and depigmenting activity of vitamin C in the context of recent human studies.
Antioxidant and anti-aging activity
Vitamin C is unique among antioxidants because of its ability to increase collagen production in addition to its free radical scavenging antioxidant activity. Due to its capacity to interfere with the UV-induced generation of reactive oxygen species by reacting with the superoxide anion or the hydroxyl radical, vitamin C has become a popular addition to “after-sun” products,14,15 and been shown to be effective in mitigating the effects of UVB, such as erythema and signs of photoaging, on porcine and human skin.2,16-17
A 2001 study in 10 postmenopausal women by Nusgens et al. found that daily topical application of 5% L-ascorbic acid enhanced the levels of procollagen types I and III, their posttranslational maturation enzymes, and tissue inhibitor of matrix metalloproteinase.18 This led to increased levels of collagen in the skin.
In 2003, Humbert et al. conducted a 6-month, double-blind, vehicle-controlled trial with 20 healthy female volunteers showing that patients treated with 5% vitamin C cream experienced significant improvements in deep furrows on the neck and forearms.19
In a small study of nine adults with Fitzpatrick skin types II or III in 2008, Murray et al. studied whether a stable topical preparation of 15% L-ascorbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid could protect human skin in vivo from UV-induced damage. They found that the antioxidant formulation supplemented the antioxidant pool of the skin and conferred significant photoprotection, guarding the skin against erythema and apoptosis as well as effectively suppressing p53 activation and reducing thymine dimer mutations known to be associated with skin cancer.13
In 2012, Xu et al. evaluated the efficacy and safety of topical 23.8% L-ascorbic acid on photoaged skin in a split-face study of 20 Chinese women. Significant improvements in fine lines, dyspigmentation, and surface roughness were observed, without adverse side effects.20
In a 2015 study of 60 healthy female subjects, Crisan et al. used high-frequency ultrasound to determine that the use of a topical vitamin C formulation yielded significant increases in collagen synthesis, revealing the solution to be an effective rejuvenation therapy.21
Skin lightening activity
Melasma
In 2004, Espinal-Perez et al. conducted a double-blind randomized trial of 5% ascorbic acid, compared with 4% hydroquinone (HQ) water–oil emulsion in 16 female patients with melasma, aged 23-43 years (mean 36 years). Of those treated with vitamin C, 62.5% exhibited good or excellent subjectively assessed skin lightening. There was no statistically significant difference in depigmenting activity in the HQ group, of which 68.7% experienced irritation whereas vitamin C was well tolerated.22
In a randomized, double-blind, placebo-controlled study, researchers used iontophoresis to enhance the penetration of vitamin C into the skin and significantly reduce pigmentation, compared with placebo.23
Although ascorbic acid is viewed by many as ineffective as a depigmenting agent alone, particularly in 5%-10% concentrations, when used in combination with other ingredients such as HQ, it is considered effective.24 In the magnesium-L-ascorbyl-2-phosphate esterified form, however, vitamin C is among the most popular prescribed depigmenting agents around the world, especially in countries where HQ and its derivatives are prohibited.25 In a 2009 16-week open-label study by Hwang et al. of 25% L-ascorbic acid and a chemical penetration enhancer for treating melasma in 40 patients, researchers observed significant reductions in pigmentation.26
In a small split-face study early in 2015, Lee et al. showed that the combination of 1,064-nm Q-switched neodymium-doped yttrium aluminum garnet (QS-Nd:YAG) laser and ultrasonic application of vitamin C was more effective than was the laser treatment alone in achieving a cosmetically acceptable treatment for melasma.27
PIPA
Vitamin C can be used to diminish or prevent post-inflammatory pigment alteration (PIPA) after procedures because it inhibits tyrosinase, lowers inflammation, and quenches free radicals. In a study of 10 patients, the application of topical vitamin C 2 or more weeks after surgery reduced the duration and degree of erythema after skin resurfacing with a carbon dioxide laser.28
Stretch marks
The depigmenting effects of vitamin C can lighten the pigmentation associated with stretch marks and its anti-inflammatory activity can contribute to blunting related redness.12
Conclusion
Although orally administered ascorbic acid is readily bioavailable, ascorbic acid in the skin is quickly depleted and oral supplementation alone does not yield optimal skin levels. Therefore, topical use of vitamin C is desirable. In fact, I tell my patients to use it topically in the morning and add a vitamin C supplement to their diet. Numerous formulation considerations (e.g., packaging, exposure to air or light during use, skin sensitivity, and user preference) are involved in the stabilization and effective penetration of ascorbic acid into the skin, and the process of developing, manufacturing, and packaging of effective, stable vitamin C products is expensive.
Vitamin C, particularly when combined with other ingredients, has been shown to be an integral constituent in topical antioxidant, antiaging, and depigmenting formulations that show promise in the dermatologic armamentarium. It is a great choice for use in a prep-procedure skin care regimen to speed healing. Use after a procedure is prohibited by the stinging associated with the low pH of properly formulated products.
References
1. J Biol Chem. 1994 May 6;269(18):13685-8.
2. Dermatol Surg. 2001 Feb;27(2):137-42.
3. J Invest Dermatol. 1994 Jan;102(1):122-4.
4. Dermatol Surg. 2005 Jul;31(7 Pt 2):814-7.
5. Annu Rev Nutr. 1994;14:371-91.
6. J Drugs Dermatol. 2008 Jul;7(7 Suppl):s2-6.
7. J Am Acad Dermatol. 2003 Jun;48(6):866-74.
8. J Invest Dermatol. 1994 Apr;102(4):470-5.
9. Free Radic Biol Med. 1997;23:85-91.
10. J Drugs Dermatol. 2014 Oct;13(10):1208-13.
11. J Am Acad Dermatol. 1996 Jan;34(1):29-33.
12. Dermatol Surg. 1998 Aug;24(8):849-56.
13. J Am Acad Dermatol. 2008 Sep;59(3):418-25.
14. J Biol Chem. 1983 Jun 10;258(11):6695-7.
15. J Phys Chem. 1983;87:1809-12.
16. Br J Dermatol. 1992 Sep;127(3):247-53.
17. J Invest Dermatol. 1991;96:587.
18. J Invest Dermatol. 2001 Jun;116(6):853-9.
19. Exp Dermatol. 2003 Jun;12(3):237-44.
20. J Drugs Dermatol. 2012 Jan;11(1):51-6.
21. Clin Cosmet Investig Dermatol. 2015 Sep 2;8:463-70
22. Int J Dermatol. 2004 Aug;43(8):604-7.
23. Dermatology. 2003;206(4):316-20.
24. Am J Clin Dermatol. 2011 Apr 1;12(2):87-99.
25. Phytother Res. 2006 Nov;20(11):921-34.
26. J Cutan Med Surg. 2009 Mar-Apr;13(2):74-81.
27. Lasers Med Sci. 2015 Jan;30(1):159-63.
28. Dermatol Surg. 1998 Mar;24(3):331-4.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in the Design District in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote the textbook “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and a book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Her latest book, “Cosmeceuticals and Cosmetic Ingredients,” was published in November 2014. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Evolus, Galderma, GlaxoSmithKline, Kythera Biopharmaceuticals, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Topix Pharmaceuticals, and Unilever.
Blue light
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Photodynamic light therapies (PDLs) have emerged as significant adjuvant approaches for treating acne. In particular, such therapies have been used for acne refractory to standard retinoid or combined retinoid and antimicrobial regimens. Why write about PDL in a column devoted to topical cosmeceutical products and ingredients? Blue light warrants inclusion because it has been studied in comparison to topical cosmeceutical treatments, and it is used in conjunction with other topical approaches.
Blue light exerts a phototoxic effect on the heme metabolism of Propionibacterium acnes, and it is considered effective by targeting part of the etiologic pathway of acne. It has become a widely used option for inflammatory acne (J. Drugs. Dermatol. 2006;5:605-10).
Early work
In 1990, Meffert et al. were the first to show that a blue light–type, high-pressure lamp could improve acne and seborrhea (10 10-minute treatments, cumulative light dose 325 J/cm2). Given the copious amounts of porphyrins stored in lipophilic P. acnes, the technology could be targeted to destroy propionibacteria, and the researchers observed a decline in the porphyrin content inside acne follicles. They concluded that short-range visible light (400-420 nm) was a viable option for acne treatment during the light-poor season of the year (Dermatol. Monatsschr. 1990;176:597-603). It was subsequently established that treatment with UV-free blue light in the range of 405-420 nm leads to the elimination of acne bacteria by virtue of the effects on the porphyrins generated naturally by P. acnes (J. Cosmet. Laser. Ther. 2003;5:111-7). Notably, blue light appears to photoinactivate P. acnes, but it does not penetrate deeply into the skin (Dermatol. Online J. 2011;17:2).
In an open study of the then-novel high-intensity, enhanced, narrow-band, blue-light phototherapy, Kawada et al. treated 30 acne patients (27 female, 3 male) twice a week for up to 5 weeks. A reduction of 64% was seen in acne lesions, and in vitro data showed a significant decline in P. acnes, but not in Staphylococcus epidermidis (J. Dermatol. Sci. 2002;30:129-35).
Mechanism of action
In 2006, Shnitkind et al. studied the effect of narrow-band blue light on the inflammatory process in the presence and absence of cytokines and ultraviolet B using interleukin-1 alpha (IL-1alpha) and intercellular adhesion molecule 1 (ICAM-1) as markers for inflammation. They found that blue light treatment of HaCaT and hTERT cells decreased levels of IL-1alpha by 82% in HaCaT and by 75% in hTERT. When blue light was combined with ultraviolet B, the respective reductions were 95% and 91%. Similar reductions in ICAM-1 expression were seen in HaCaT, but not in hTERT. The researchers concluded that narrow-band blue light exerts anti-inflammatory effects on keratinocytes by reducing cytokine-induced synthesis of IL-1alpha and ICAM-1. They suggested that these findings imply a broader range of effects is exerted on the inflammatory process by narrow-band blue light than previously understood (J. Drugs. Dermatol. 2006;5:605-10).
Comparison studies
In 2000, Papageorgiou et al. randomized 107 patients with mild to moderate acne to four treatment groups: blue light (peak at 415 nm), mixed blue and red light (peaks at 415 and 660 nm), cool white light, and 5% benzoyl peroxide cream, for 12 weeks of active treatment. Phototherapy using portable light sources was conducted daily for 15 minutes; comparative assessments among the three phototherapy groups were done with observers blinded. The investigators found that the greatest improvement in acne lesions occurred in the blue and red light combined group. The blue/red treatment was significantly superior to blue light alone at 4 and 8 weeks but not 12 weeks, benzoyl peroxide at weeks 8 and 12, and white light at all assessments (Br. J. Dermatol. 2000;142:973-8).
Gold et al. performed a multicenter clinical evaluation comparing blue light to topical 1% clindamycin solution with respect to safety and efficacy. They found that clindamycin was associated with a 14% reduction of inflammatory lesions, but blue light reduced such lesions by an average of 34% (J. Drugs. Dermatol. 2005;4:64-70).
In another study, 20 patients with moderate to severe facial acne were treated in four weekly sessions with topical aminolevulinic acid (ALA)-photodynamic therapy with blue light (415 nm) on the right side of the face, or blue light alone on the left side of the face. At 4, 8, 12, and 16 weeks after the start of treatment, the mean percent reductions in inflamed lesions were higher in the ALA-PDT areas (32%, 50.9%, 65.9%, and 71.1%, respectively) than in the blue light–only treatment areas (20.7%, 27%, 57.7%, and 56.7%), but the differences were not statistically significant. Side effects, which included pain, stinging, erythema, itching, peeling, oozing, and pustules, were more pronounced in the areas treated with ALA-PDT (Photodermatol. Photoimmunol. Photomed. 2007;23:186-90).
However, in a 2007 study of 22 patients with moderate to severe acne randomized to one of three ALA-PDT treatments – intense pulsed light (IPL; 600-850 nm), a combination of IPL (580-980 nm) and bipolar radiofrequency (RF) energies, or blue light (417 nm) – in three sessions at 2-week intervals, ALA-PDT with activation by IPL yielded the most consistent, lasting improvement in moderate to severe acne (J. Drugs Dermatol. 2007;6:1010-6).
In a study of 60 volunteers with facial acne (grades II and III), de Arruda et al. compared the safety and efficacy of blue light to topical benzoyl peroxide 5% over 4 weeks. Thirty patients received blue light treatment twice a week, and the other 30 self-applied the topical formulation twice daily. The improvements were similar in both groups, but side effects were milder in the blue light group (An. Bras. Dermatol. 2009;84:463-8).
Choi et al. compared the bactericidal effects of 5-aminolevulinic acid (ALA) with blue and red light on P. acnes and found that blue light was more effective than red light phototherapy in eliminating the bacteria unless ALA was added, which substantially augmented red light phototherapy efficacy (J. Dermatol. 2011;38:661-6).
In summarizing the off-label uses of light-based treatments and PDT using topical precursors of porphyrins, Sakamoto et al. observed that blue light alone lessens acne severity due to anti-inflammatory effects; PDT using 5-ALA or ALA derivatives provides antimicrobial and anti-inflammatory activity; and, at high doses, red-light PDT may suppress or eradicate sebaceous glands, yielding clinical improvement (J. Am. Acad. Dermatol. 2010;63:183-93).
Combination therapy
In 2011, Wheeland and Dhawan assessed the efficacy and tolerability of treating mild to moderate facial acne using a novel, handheld, light-emitting diode (LED) blue-light device, along with a foam cleanser containing 5% glycolic acid and 2% salicylic acid, plus a serum containing 1.25% salicylic acid, 0.5% niacinamide, 0.08% liposomal-based azelaic acid, and superoxide dismutase. In all, 28 of 35 adults aged 25-45 years completed the 8-week study, in which they used the device twice daily (in addition to the cleanser before treatments and the serum after nighttime treatments). Significant reductions in inflammatory lesion counts were seen from week 1 onward, and significant reductions in noninflammatory lesion counts were seen from week 4 onward compared with baseline counts. The number and severity of flares were significantly reduced from baseline as well.
Therapy was well received by patients, with more than 90% claiming improvement in overall skin appearance and other parameters. In addition, 86% described the treatment as gentler than other therapies. (J. Drugs Dermatol. 2011;10:596-602).
Products
The Skin Clarifying Blue Light device has a power density of 400 mW/cm2, which is 10 times the power of other LED acne devices. This high power density allows the Skin Clarifying Blue Light device to deliver high levels of efficacy with short treatment times. When used as stand-alone treatment, it delivered a 70% reduction in inflammatory lesions in 8 weeks. The success of products designed for self-administration has coincided with the rampant interest in the creation of smart phone applications (J. Cosmet. Laser. Ther. 2011;13:308-14; J. Clin. Aesthet. Dermatol. 2009;2:40-4; J. Clin. Aesthet. Dermatol. 2009;2:44-50). That is, blue-light therapy apps have been developed for the iPhone and the iPod touch. None, however, has been approved by the Food and Drug Administration, although at least one is said to be under investigation in a clinical trial. I am skeptical about the efficacy of these LED-backlit apps and concerned about potentially prolonged magnetic radiation exposure that would be required. The self-administered devices appear to be a more reliable alternative.
Conclusion
Blue light can effectively be used to treat mild to moderate acne by causing photodynamic destruction of P. acnes. It can be used alone or in combination with topical or other light regimens. Additional studies are needed before a consensus protocol can be established, and future research goals should include establishing the optimal incubation time, activating light source, and frequency of treatment.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Blackberry
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Endemic to Europe and North America, the blackberry (Rubus fruticosus) is naturally laden with an abundance of polyphenolic compounds, including ellagic acid, tannins, ellagitannins, quercetin, gallic acid, anthocyanins, and cyanidins, which have been associated with antioxidant and anticarcinogenic activity (J. Med. Food 2007;10:258-65; J. Agric. Food. Chem. 2002;50:3495-500; J. Agric. Food Chem. 2008;56:661-9). Indeed, the health benefits of consuming plants rich in anthocyanins have been known at least since the 1500s (Nat. Prod. Commun. 2011;6:149-56).
It is not surprising, then, that blackberries have long been part of traditional medicine. Rubus extracts have been used in traditional medicine for antimicrobial, anticonvulsant, and muscle relaxant indications, as well as for their ability to detect and inhibit free radicals (Int. J. Antimicrob. Agents. 2009;34:50-9). Rubus has been reported in traditional medicine on Sardinia for hemorrhoids, bleeding gums, and ulcers (J. Ethnobiol. Ethnomed. 2009;5:6). Phytotherapeutic uses have also been noted in Central Italy (Fitoterapia. 2005;76:1-25). Dermatologic applications of blackberry in southern Italy include use of the leaves to treat dog bites, and use of the roots in a hair-wash preparation (J. Ethnobiol. Ethnomed. 2008;4:5).
Data from other studies suggest additional potential uses for blackberry. For example, polyphenols and leaf extract of Rubus ulmifolius exhibited antibacterial activity against two strains of Helicobacter pylori (Int. J. Antimicrob. Agents. 2009;34:50-9). The antimicrobial activity of berries and other anthocyanin-containing fruits, which are typically more effective against Gram-positive than Gram-negative bacteria, is believed to result from various mechanisms and interactions associated with anthocyanins, weak organic acids, phenolic acids, and their mixtures of varying chemical composition (Nat. Prod. Commun. 2011;6:149-56; J. Ethnopharmacol. 2002;79:165-8).
Anti-inflammatory activity
In 2006, Pergola et al. examined whether the pharmacological activity of the anthocyanin fraction of a blackberry extract (cyanidin-3-O-glucoside, approximately 88% of the total anthocyanin content) could be attributed to the inhibition of nitric oxide production. The researchers found that the increased synthesis of nitrites spurred by the treatment of J774 cells with lipopolysaccharide over 24 hours was inhibited by anthocyanin, in a concentration-dependent manner. They concluded that the anti-inflammatory activity associated with blackberry extract can be partially ascribed to the blocking of nitric oxide synthesis by cyanidin-3-O-glucoside, the primary anthocyanin found in the extract (Nitric Oxide 2006;15:30-9).
In another study involving in vivo data and a mouse ear model, investigators assessed the antioxidant and topical anti-inflammatory activity of low- and high-molecular-weight phenolic fractions from three blackberry cultivars (i.e., Navaho, Kiowa, and Ouachita) bred for the warm and humid conditions of the southeastern United States. They found that all three formulations significantly mitigated TPA-induced inflammation. In addition, the researchers investigated mouse ear myeloperoxidase activity, an indicator of polymorphonuclear leukocyte infiltration, and noted that it was substantially diminished after topical application of both blackberry preparations as well as indomethacin (J. Agric. Food. Chem. 2010;58:6102-9).
Antioxidant activity
Blackberries consistently rank highly in oxygen radical absorbance capacity (ORAC), and they showed the strongest antioxidant activity among 1,000 antioxidant foods eaten in the United States in a study by Halvorsen et al. (Am. J. Clin. Nutr. 2006;84:95-135).
Investigators recently evaluated and compared the effect of extraction time (5 and 15 minutes) and hydrolysis on the qualitative and quantitative content of phenolic compounds and antioxidant capacity of six traditional medicinal plants, including blackberry (Rubus fruticosus), lemon balm (Melissa officinalis), thyme (Thymus serpyllum), lavender (Lavandula officinalis), stinging nettle (Urtica dioica), and olive (Olea europea). The distribution of phenolic compounds identified varied widely among the botanicals selected, and the extraction efficiency and antioxidant capacity of the extracts were influenced by prolonged extraction and hydrolysis. The hydrolyzed extract of blackberry leaves, obtained after 15 minutes of extraction, demonstrated the highest phenolic content and antioxidant capacity (Phytochem. Anal. 2011;22:172-80).
In 2007, Dai et al. obtained Hull blackberries grown in Kentucky and analyzed total anthocyanin and phenolic content, polymeric color, as well as anthocyanin composition and antioxidant capacity. Their in vitro cell culture work indicated that the blackberry extract suppressed HT-29 colon tumor cell growth by up to 66% after 72 hours, in a concentration-dependent manner. High-dose and low-dose lipid A-induced interleukin-12 release was also concentration-dependently inhibited from mouse bone marrow–derived dendritic cells by total anthocyanin concentrations (0-40 mcg/mL). The investigators concluded that the blackberry extract exhibits strong antioxidant, antiproliferative, and anti-inflammatory activities, and products based on the extract might be considered for the treatment or prevention of inflammatory conditions as well as cancer (J. Med. Food 2007;10:258-65).
Anticarcinogenic activity
In 2004, Feng et al. studied the effects of fresh blackberry extracts on cancer cell proliferation and neoplastic transformation induced by TPA. They confirmed, using electron spin resonance, that the extract effectively scavenges hydroxyl and superoxide free radicals. They also determined that pretreatment of the human cancer cell line A549 with blackberry extract suppressed cell proliferation and inhibited 8-hydroxy-2\'-deoxyguanosine (8-OHdG) formation induced by UVB. In addition, pretreatment with the extract reduced neoplastic transformation of JB6 P+ cells induced by TPA and blocked UVB- and TPA-induced AP-1 transactivation. The investigators concluded that fresh blackberry extract appears to have anticarcinogenic properties, and that associated activity may be derived from its antioxidant characteristics (Nutr. Cancer 2004;50:80-9).
In 2006, Ding et al. examined the chemopreventive and chemotherapeutic activity of cyanidin-3-glucoside (C3G), a key active ingredient in blackberry. C3G was shown to scavenge UVB-induced hydroxyl and superoxide radicals in cultured JB6 cells. The investigators observed reductions in the number of nonmalignant and malignant skin tumors per mouse induced by TPA in 7,12-dimethylbenz[a]anthracene-initiated mouse skin. In addition, UVB- and TPA-induced transactivation of NF-kappaB and AP-1 and expression of cyclooxygenase-2 and tumor necrosis factor–alpha were suppressed by the pretreatment with C3G of JB6 cells. The researchers suggested that the inhibition of MAPK activity may be important in mediating such effects. TPA-induced neoplastic transformation in JB6 cells was also hindered via C3G pretreatment. Further, C3G suppressed proliferation of the human lung carcinoma cell line A549, diminished the size of A549 tumor xenograft growth, and significantly limited metastasis in nude mice. The investigators concluded that C3G, an important constituent of blackberry, displays significant anticancer activity by dint of its capacity to scavenge free radicals. As such, they suggested that this blackberry derivative, which exhibits scant cytotoxicity to healthy tissue, warrants additional study as a preventive and therapeutic agent in human cancers (J. Biol. Chem. 2006;281:17359-68).
Conclusion
The most recent evidence suggests that blackberry warrants attention for medical applications, including dermatology. In fact, in a small (n = 33) single-center, open-label study led by the author, significant improvement in most metrics of photoaged skin was observed after the use of a day and night regimen containing blackberry leaf extract, dill extract, and Zn-Cu(II) bi-mineral complex in patients with mild to moderate photodamage. (Baumann LS, Figueras KA, Bell M, Flitter CJ. Assessing the efficacy and tolerance of a day and night regimen containing blackberry leaf extract, dill extract, and Cu-Zinc bi-mineral complex in subjects with mild to moderate photoaged skin. Unpublished results.) It remains to be seen if and when blackberry extract alone may be harnessed for dermatologic indications, but present data are promising, and justify continued study.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Nonsteroidal anti-inflammatory drugs (NSAIDs) have therapeutic applications that "have spanned several centuries," according to Rao and Knaus (J. Pharm. Pharm. Sci. 2008;11:81s-110s). NSAIDs are among the increasing number of anti-inflammatory agents used to target bioactive lipids produced from arachidonic acid. Although this drug class is one of the most often used in practice and has been well studied by investigators, the role of NSAIDs for cutaneous purposes has been relatively limited (J. Cutan. Med. Surg. 2002;6:241-56). Indeed, only three topical NSAIDs are approved for use in the United States, for a narrow range of conditions.
Diclofenac sodium 1.5% topical solution (containing dimethyl sulfoxide to enhance penetration) and diclofenac sodium gel 1% are currently approved in the United States for hand and knee osteoarthritis (Postgrad. Med. 2010;122:98-106). The diclofenac hydroxyethylpyrrolidine (epolamine) 1.3% patch was approved by the U.S. Food and Drug Administration for soft-tissue injuries in January 2007, although it has long been available in more than 40 countries (Int. J. Clin. Pract. 2010;64:1546-53; Clin. Ther. 2010;32:1001-14).
A winning adverse event profile
Significantly, topical NSAIDs have not been associated with the adverse events resulting from oral NSAIDs, which engender various dose-related side effects (Semin. Arthritis. Rheum. 2009;39:203-12). Mild and self-limiting local skin reactions are the most common adverse side effects from topical NSAID products. The diclofenac products are approved in the European Union, as are ibuprofen creams and gels, ketoprofen gel, felbinac gel and cutaneous foam, and piroxicam gel.
The efficacy and safety of these products have been established through meta-analyses. In a recent study, researchers cautioned that the patient, the drug, and the drug delivery mechanism should be considered in topical NSAID selection, because the pharmacokinetic absorption from topical preparations can vary with different formulations of the same drug, depending on the agent, the underlying disorder, and the application site (Am. J. Ther. 2012 Feb 22 [Epub ahead of print]).
Easing osteoarthritis
Although oral NSAIDs have been the mainstays of hand and knee osteoarthritis treatment regimens, their dose- and age-related side effect profiles (including adverse effects on the cardiovascular, renal, and gastrointestinal systems) have prompted the use of topical NSAIDs, which yield comparable efficacy with far less systemic risk. Results of a Jan. 1, 2005, to March 31, 2010, literature review showed that topical products exhibited superior efficacy compared with placebo, with similar adverse event profiles. Topicals also showed efficacy comparable to that of oral diclofenac, with side effects seen primarily at the application site and no ulcers, perforations, or bleeding (Postgrad. Med. 2010;122(6):98-106).
In 2009, Barthel et al. evaluated the efficacy and safety of topical diclofenac sodium gel (DSG) 1% in a randomized, double-blind, vehicle-controlled trial of 492 adults (aged 35 years and older) with mild to moderate symptomatic knee osteoarthritis lasting at least 6 months. Patients received 4 g of topical treatment of DSG or vehicle four times daily for 12 weeks. The investigators noted significant reductions in the DSG group compared with the vehicle group according to the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain and physical function subscales, as well as global rating of disease. They also observed significantly better efficacy results with DSG as early as week 1 of treatment. Gastrointestinal reactions occurred in 5.9% of the DSG group and 5.0% of the vehicle group, and application site reactions emerged in 5.1% of the DSG group and 2.5% of the vehicle group (Semin. Arthritis Rheum. 2009;39:203-12).
In 2010, Baraf et al. also conducted a 12-week efficacy and safety study of topical DSG 1% for symptomatic knee osteoarthritis. This randomized, double-blind, parallel-group, multicenter trial of patients at least 35 years of age with symptomatic Kellgren-Lawrence grade (KLG) 1 to 3 osteoarthritis in one or both knees for at least 6 months assigned 208 subjects to DSG treatment and 212 to vehicle. The investigators found significant improvement according to WOMAC metrics in the DSG patients compared with placebo patients. Unlike the Barthel report, no gastrointestinal upset was noted in this study. Application site reactions were the most common side effect, occurring in 4.8% of the DSG group and 0% of the vehicle group (Phys. Sportsmed. 2010;38:19-28).
In 2012, Baraf et al. extended their previous work and assessed the safety of topical DSG 1% for the treatment of knee and hand osteoarthritis in older and younger patients. They also compared the treatment in those with or without comorbid hypertension, type 2 diabetes, or cerebrovascular or cardiovascular disease. This post hoc analysis of pooled data from five randomized, double-blind, placebo-controlled trials included 1,426 patients 35 years of age and older with mild to moderate osteoarthritis of the knee and 783 patients 40 years of age and older with mild to moderate osteoarthritis of the hand. Participants applied 4 g of DSG or vehicle to affected knees q.i.d. for 12 weeks or 2 g of DSG or vehicle to affected hands q.i.d. for 8 weeks. The investigators found that the adverse event profile was similar across comparisons of patients with knee osteoarthritis. Among patients with hand osteoarthritis, the only differences were that the adverse event profile was lower in patients with type 2 diabetes than in patients without the condition, and higher in patients with cerebrovascular or cardiovascular disease than in patients without those conditions. The authors concluded that the rates of adverse side effects were similar and low between the two groups (Am. J. Geriatr. Pharmacother. 2012;10:47-60).
To further examine the efficacy and tolerability of the diclofenac epolamine topical patch (DETP), investigators reviewed data from eight studies from 1984 to 2009, including data on patients with acute pain from soft-tissue injuries or localized periarticular disorders. Significant reductions in spontaneous pain from baseline due to DETP were seen (range, 26%-88% on day 7 and 56%-61% on day 14). In addition, significant decreases in pain scores were linked to DETP use compared with a placebo patch in two studies and compared with diclofenac diethylammonium topical gel in one study. Adverse events were low across studies; reactions at the application site and nausea were the most common events (Clin. Ther. 2010;32:1001-14).
Oral ibuprofen and combination therapy
Notably, ibuprofen has demonstrated effectiveness in the treatment of acne, as inflammatory acne lesions are infiltrated with neutrophils and ibuprofen suppresses leukocyte chemotaxis (Dermatology. 2003;206:68-73). Ibuprofen is generally considered safe, with low potential for causing gastrointestinal, cardiovascular, or renal risks compared with other NSAIDs and selective cyclooxygenase-2 inhibitors (coxibs), which have been removed from the market (Inflammopharmacology 2009;17:275-342; J. Pharm. Pharm. Sci. 2008;11:81s-110s).
In a double-blind study of 60 patients aged 15-35 years with acne vulgaris, patients were randomly assigned to one of four groups: oral ibuprofen (600 mg) plus tetracycline (250 mg) four times daily; ibuprofen (600 mg) plus placebo four times daily; tetracycline (250 mg) plus placebo four times daily; and two placebos four times daily. Interestingly, the combination therapy was the only approach that yielded an effect statistically superior to that of placebo in reducing total lesion counts. The use of ibuprofen alone netted improvements comparable to those afforded by tetracycline but with fewer side effects (J. Am. Acad. Dermatol. 1984;11:1076-81).
NSAIDs are also used for the treatment of sunburn. In 1992, Hughes et al. investigated ameliorating UVB-induced skin injury by nonsteroidal drugs (oral ibuprofen or indomethacin) plus topical betamethasone dipropionate in 24 subjects. Measurements of erythema and increased skin blood flow, performed serially, revealed a synergistic effect of oral NSAIDs combined with topical corticosteroids to repair UVB-induced skin damage (Dermatology 1992;184:54-8).
Conclusion
An ideal anti-inflammatory agent has not yet been developed, but topical NSAIDs appear to fit the bill in terms of reducing or eliminating the adverse side effects associated with oral NSAID regimens. However, topical NSAIDs are approved for only a narrow range of indications, and more research is necessary to determine whether they are appropriate for a wider array of dermatologic conditions.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Alstonia scholaris
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Alstonia scholaris, a tree that grows 50-80 feet high and belongs to the Apocynaceae family, has a long history of use in traditional and homeopathic medicine, including Ayurvedic medicine in India, where it is known as sapthaparna (Integr. Cancer Ther. 2009;8:273-9), in traditional Chinese medicine (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81), and in traditional medicine in Africa and Australia (Integr. Cancer Ther. 2010;9:261-9). The bark contains the alkaloids ditamine, echitamine (or ditaine), and echitanines; and decoctions or other preparations of the bark have been used to treat gastrointestinal conditions (Grieve M. A Modern Herbal (Vol. 1). New York, Dover Publications, 1971, p. 29). Often called the devil’s tree, the bark of A. scholaris also has been used to treat malaria, cutaneous diseases, tumors, ulcers, chronic respiratory conditions (such as asthma and bronchitis), helminthiasis, and agalactia (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]).
In the study of A. scholaris most directly pertinent to potential dermatologic treatment, Lee et al. found that ethanolic bark extracts of A. scholaris significantly suppressed retinoid-induced skin irritation in vitro and in vivo, in human HaCat keratinocytes. The investigators identified echitamine and loganin as the primary components likely responsible for the anti-inflammatory effects.
Data showed that A. scholaris dose-dependently inhibited the all-trans retinoic acid–induced releases of the pro-inflammatory cytokines monocyte chemoattractant protein-1 (MCP-1) and interleukin-8 (IL-8) in vitro. Also in vitro, A. scholaris extract potently suppressed radiation-induced increases in matrix metalloproteinase-1 (MMP-1). Importantly, in a cumulative irritation patch test, the botanical extract diminished retinol-induced skin irritation while enhancing retinoid activity in blocking MMP-1 expression, which is linked closely to cutaneous aging. The authors concluded that A. scholaris appears to have the dual benefits of decreasing irritation associated with retinoids while augmenting their antiaging impact (Evid. Based Complement. Alternat. Med. 2012;2012:190370).
The leaf extract of A. scholaris has been used to treat cold symptoms and tracheitis, and it has been prescribed in hospitals and approved for commercial over-the-counter sale by the State Food and Drugs Administration of China (SFDA) (J. Ethnopharmacol. 2010;129:293-8; J. Ethnopharmacol. 2010;129:174-81). The broad range of biological properties associated with A. scholaris has been ascribed to particular constituent categories, including alkaloids, flavonoids, and terpenoids (specifically, phenolic acids) (Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). These properties include, but are reportedly not limited to, antioxidant, anticancer, anti-inflammatory, antistress, analgesic, antimutagenic, hepatoprotective, immunomodulatory, and chemopreventive activity (Integr. Cancer Ther. 2010;9:261-9; Chin. J. Integr. Med. 2012 Mar 28 [Epub ahead of print]). Antineoplastic effects have been linked directly to phytochemical constituents including echitamine, alstonine, pleiocarpamine, O-methylmacralstonine, macralstonine, and lupeol (Integr. Cancer Ther. 2010;9:261-9).
In 2006, Jagetia and Baliga investigated the anticancer activity of A. scholaris alkaloid fractions in vitro in cultured human neoplastic cell lines. They also conducted in vivo studies in tumor-bearing mice. The in vitro data in HeLa cells revealed a time-dependent rise in antineoplastic activity after 24 hours of exposure (25 mcg/mL). Further, once-daily administration of A. scholaris (240 mg/kg) to tumor-bearing mice yielded dose-dependent remissions, although there were toxic presentations at this dosage. The next-lower dose of 210 mg/kg was found to be most effective, with 20% of the mice surviving for as long as 120 days after tumor cell inoculation, compared with none of the control animals treated with saline (Phytother. Res. 2006;20:103-9).
Using an acute-restraint stress model in mice in 2009, Kulkarni and Juvekar evaluated the effects of stress and the impact of a methanolic extract of A. scholaris bark. Pretreatments with the extract of 100, 250, and 500 mg/kg for 7 days were found to exert significant antistress effects. In addition, nootropic activities were observed, with memory functions clearly enhanced in learning tasks. A. scholaris also was associated with significant antioxidant properties. The extract at 200 mcg/mL exhibited maximum scavenging of the stable radical 1,1-diphenyl-2-picrylhydrazyl at 90.11% and the nitric oxide radical at 62.77% (Indian J. Exp. Biol. 2009;47:47-52).
Later in 2009, Jahan et al. reported on their investigation of potential antioxidant and chemopreventive activity displayed by A. scholaris in a two-stage murine model. Skin carcinogenesis development was initiated in Swiss albino mice through one application of 7, 12-dimethyabenz(a)anthrecene (DMBA) and then promoted two weeks later by repeated application of croton oil three times per week through 16 weeks. The investigators found a lower incidence of tumors, tumor yield, tumor burden, and number of papillomas in mice treated with A. scholaris extract as compared to untreated controls (Integr. Cancer Ther. 2009;8:273-9).
In 2010, Shang et al. conducted multiple studies using A. scholaris. In the first published report, they assessed the anti-inflammatory and analgesic properties of the ethanolic leaf extract to validate its use in traditional Chinese medicine and modern clinical medicine. The investigators first determined that analgesic activity was conferred as the ethyl acetate and alkaloid fractions significantly diminished acetic acid-induced reactions in mice and, along with the ethanolic extract, reduced xylene-induced ear edema.
The researchers also performed in vivo and in vitro assessments of anti-inflammatory activity again on xylene-induced ear edema and carrageenan-induced air pouch formation in mice, as well as cyclooxygenase (COX)-1, -2 and 5-LOX inhibition.
In the air pouch model, A. scholaris alkaloids were found to have significantly spurred superoxide dismutase activity while lowering nitric oxide, prostaglandin E2, and malondialdehyde levels. In vitro tests, supporting evidence from animal models, showed that the three primary alkaloids isolated from A. scholaris leaves (picrinine, vallesamine, and scholaricine) inhibited the inflammatory mediators COX-1, COX-2, and 5-LOX. The researchers also noted that the in vitro anti-inflammatory assay results reinforced the notion of these alkaloids as the bioactive fraction of the plant (J. Ethnopharmacol. 2010;129:174-81).
In their second published report that year, Shang et al. investigated the antitussive and anti-asthmatic activities of the ethanolic extract, fractions, and chief alkaloids of A. scholaris leaf.
The researchers tested for antitussive effects using ammonia-induced or sulfur dioxide-induced coughing in mice and citric acid-induced coughing in guinea pigs. They evaluated anti-asthmatic activity via histamine-induced bronchoconstriction in guinea pigs. They also measured phenol red volume in murine tracheas to assess expectorant activity.
The data indicated antitussive activity, with significant alkaloid suppression of ammonia-induced coughing frequency in mice. Latency periods of sulfur dioxide-induced cough in mice and citric acid-induced cough in guinea pigs increased, and cough frequency in guinea pigs decreased.
Anti-asthmatic effects, such as suppression of convulsion, were observed in guinea pigs. In the expectorant assessment, tracheal phenol red production was increased. The researchers identified picrinine as the primary alkaloid responsible for these activities (J. Ethnopharmacol. 2010;129:293-8).
In addition, Jahan and Goyal showed that pretreatment with A. scholaris bark extract protected the bone marrow of mice against radiation-induced chromosomal damage and micronuclei induction (J Environ. Pathol. Toxicol. Oncol. 2010;29:101-11).
Conclusion
Despite the dearth of research on A. scholaris, the existing data are intriguing, particularly the findings that A. scholaris may have the capacity to amplify the anti-aging activity of retinoids while blunting their irritating effects. Although more research is needed to determine the dermatologic value of A. scholaris, the pursuit may potentially prove fruitful.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Flaxseed
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.
Linum usitatissimum, an annual plant native to the eastern Mediterranean and India and better known as flax (or linseed, several decades ago), was cultivated in ancient Egypt and Ethiopia and used for many purposes, including as an ingredient in medicine, soap, and hair products. The oil from the seeds of the plant is thought to possess significant health benefits. Flaxseed oil is one of the richest sources of omega-3 fatty acids, in particular, alpha-linolenic acid (ALA), which represents more than 50% of its total fatty acid content (Br. J. Nutr. 2009;101:440-5; Medical Herbalism: The science and practice of herbal medicine. Healing Arts Press: Rochester, Vt., 2003, p. 57). In addition, flaxseeds are rich in dietary fiber and lignans, which are phytoestrogens with antioxidant properties.
Antioxidant, anti-inflammatory, and antiapoptotic properties have been associated with flaxseed oil and warrant medical consideration. The substantial anti-inflammatory activity of L. usitatissimum has been ascribed to its primary active constituent, ALA (57%), which suppresses arachidonic acid metabolism, thus inhibiting the synthesis of proinflammatory n-6 eicosanoids and reducing vascular permeability (Inflammopharmacology 2010;18:127-36).
In a randomized, double-blind, placebo-controlled application test in 2009, De Spirt et al. studied the cutaneous effects of supplementation with flaxseed or borage oil for 12 weeks in two groups of women (n = 45) aged 18-65 years with sensitive and dry skin. Fifteen women were included in each group, and 15 were randomized to a placebo control group. The placebo group received medium-chain fatty acids. The flaxseed oil included ALA and linoleic acid, and the borage oil contained linoleic and gamma-linolenic acids. ALA contributed to the significant rise in total fatty acids in plasma seen in the flaxseed oil group at weeks 6 and 12. An increase in gamma-linolenic acid was noted in the borage oil group. Erythema, roughness, and scaling were decreased in both treatment groups compared with baseline, while skin hydration was markedly elevated after 12 weeks. In addition, transepidermal water loss was diminished by 10% after 6 weeks in both oil treatment groups, with further reductions after 12 weeks in the flaxseed oil group. The investigators concluded that intervention with dietary lipids can manifest as skin improvements (Br. J. Nutr. 2009;101:440-5).
In 2010, Kaithwas and Majumdar evaluated the anti-inflammatory potential of flaxseed fixed oil against castor oil–induced diarrhea, turpentine oil–induced joint edema, and formaldehyde-induced and complete Freund’s adjuvant (CFA)-induced arthritis in Wistar albino rats. They found that flaxseed oil dose-dependently inhibited the adverse effects of castor oil and turpentine oil as well as CFA, and a significant inhibitory effect was also exerted by flaxseed oil against formaldehyde-induced proliferation of global edematous arthritis. Flaxseed oil also significantly diminished the secondary lesions engendered by CFA by dint of a delayed hypersensitivity reaction. The authors concluded that the significant anti-inflammatory activity imparted by L. usitatissimum fixed oil suggests its therapeutic viability for inflammatory conditions, such as rheumatoid arthritis (Inflammopharmacology 2010;18:127-36).
Recently, de Souza et al. studied the effects on skin wounds in rats of a semisolid formulation of flaxseed oil (1%, 5%, or 10%). The investigators assessed the contraction/re-epithelialization of the wound and resistance to mechanical traction in incisional and excisional models, respectively. They found that the groups treated with flaxseed oil concentrations of 1% or 5% largely started re-epithelialization earlier than the petroleum jelly control group, and achieved 100% re-epithelialization on the 14th day after injury, as compared to 33% of animals in the petroleum jelly group. The investigators concluded that flaxseed oil, at low concentrations, exhibits potential in a solid pharmaceutical preparation, for use in dermal repair (Evid. Based. Complement. Alternat. Med. 2012;2012:270752).
Early in 2012, Tülüce et al. set out to ascertain the antioxidant and antiapoptotic effects of flaxseed oil exerted against ultraviolet C–induced damage in rats. They divided animals into three groups: control, UVC alone, and UVC and flaxseed oil. UVC light exposure lasted for 1 hour twice daily for four weeks in the two exposure groups. In the flaxseed oil group, the oil was administered by gavage prior to each irradiation (4 mL/kg ). The investigators noted that malondialdehyde and protein carbonyl levels were higher in the UVC group than in the controls, but such levels were reduced in the flaxseed oil group compared with the UVC-only group, in skin, lens, and sera. Also, the activities of glutathione peroxidase and superoxide dismutase were found to be higher in the skin, lens, and sera of the flaxseed oil group as compared to the UVC-only group. In addition, retinal apoptosis was lower in the flaxseed group than in the UVC group. The researchers concluded that flaxseed oil may be useful in conferring a photoprotective effect against UVC-induced damage, as manifested in protein carbonylation and reactive oxygen species generation, in rats (Toxicol. Ind. Health. 2012;28:99-107).
Conclusion
Flaxseed oil has gained recent attention for its salutary effects as part of the diet. Rich in omega-3 essential fatty acids and lignans, flaxseed oil has been found to improve fatty acid profiles. Significantly, emerging evidence points to beneficial cutaneous effects derived from dietary use of flaxseed oil. However, more research is necessary to determine whether the beneficial constituents of flaxseed oil can be harnessed in topical products.
Dr. Baumann is in private practice in Miami Beach.