User login
Probiotics
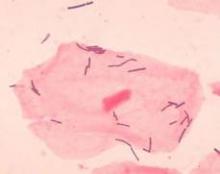
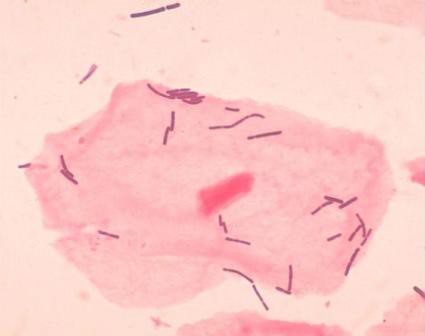
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Probiotics are live microorganisms that impart health benefits to the host when present or administered at appropriate levels (J. Appl. Bacteriol. 1989;66:365-78). Intestinal microflora are better understood and more frequently used than cutaneous microbiota, but researchers have recently applied the concepts underlying the efficacy of intestinal probiotics to investigate potential benefits in the dermatologic realm. This work has also been spurred by the flurry of investigations on probiotics for the treatment of atopic dermatitis (AD).
In one of the earlier studies of possible uses of probiotics for the skin, Ouwehand et al. identified strains that adhere to keratin. However, the tested microbes (Propionibacteria, selected because they are among the normal microbiota of the skin) were not found to inhibit cutaneous pathogen adhesion to human keratin. Nevertheless, the researchers concluded that additional study was warranted to identify strains that adhere in vivo and exhibit activity against potential skin pathogens (Lett. Appl. Microbiol. 2003;36:327-31).
Clearly, some probiotic strains have been shown to exhibit strong immunomodulatory activity at the cutaneous level (Eur. J. Dermatol. 2010;20:731-7). In addition, some topical skin products now contain probiotic strains as active ingredients, including Clinique Medical, which incorporates lactobacillus cultures to yield molecules that help ameliorate skin barrier effects from laser treatments or chemical peels (Facial Plast. Surg. 2009;25:285-9). Probiotics have also been used successively as adjuvant therapy to treat suppurative inflammatory conditions (i.e., boils and abscesses) in the maxilla-facial region (Stomatologiia (Mosk) 2009;88:50-2).
This column will consider some of the most current AD studies as well as other recent research. History is not to be disregarded, though. After all, the notion of topical probiotics conferring cutaneous benefits against acne and seborrhea was considered in 1912 (Gut Pathog. 2011;3:1). Current findings may, indeed, bear this out.
Atopic Dermatitis
The safety of probiotic, as well as prebiotic, treatments for AD in children was established in a long-term, randomized, double-blind trial (Clin. Dermatol. 2010;28:57-61; Pediatrics 2008;122:8-1). But questions remain regarding efficacy, with conflicting data emerging from recent studies. Given increasing interest in the use of probiotics for the treatment of AD, Boyle et al. conducted an extensive literature search up to 2008 and found that 12 trials, including 781 subjects (all children), met their inclusion criteria, with probiotics not emerging as an effective treatment for eczema (Cochrane Database Syst. Rev. 2008;CD006135).
In 2008, Betsi et al. reviewed the results of 13 relevant randomized, placebo-controlled trials, 10 of which assessed probiotics as treatment and 3 for prevention of AD. Overall, they found that probiotics, particularly Lactobacillus rhamnosus GG, appear to be effective for preventing AD, lowering its severity in half of the trials assessed though inflammatory markers were not significantly affected. The authors called for more research to determine the usefulness of probiotics in AD treatment or prevention (Am. J. Clin. Dermatol. 2008;9:93-103).
In a 2010 analysis of systematic reviews indexed between August 2007 and August 2008 covering disease prevention and atopic eczema treatment, Williams and Grindlay found two independent systematic reviews suggesting that ingestion of probiotics by mothers during pregnancy might lower the incidence of subsequent eczema. However, they noted that a review of 13 studies of probiotics for treating established eczema revealed no convincing support for its clinical use, a stance that was buttressed by a later Cochrane Review (Clin. Exp. Dermatol. 2010;35:223-7).
In 2010, Gerasimov et al. conducted a randomized, double-blind, placebo-controlled, prospective study of 90 children (1-3 years old) with moderate to severe AD treated with a mixture of L. acidophilus DDS-1 and Bifidobacterium lactis UABLA-12 with fructo-oligosaccharide (5 billion colony-forming units twice daily for 8 weeks vs. placebo). The researchers found that the use of the probiotic compound correlated with significant clinical improvement in children with AD, and suggested that additional research is necessary to assess the efficacy of probiotics in adults with AD (Am. J. Clin. Dermatol. 2010;11:351-61).
In another recent study, investigators isolated L. plantarum strains from the Korean fermented food kimchi, and found that they hindered the dermatitis promoted by house-dust mites in a mouse model representative of human AD (J. Appl. Microbiol. 2011;110:1195-202). Overall, clinical trials conducted to test the use of probiotics to treat AD over the last 15 years have yielded conflicting results, though it appears that there is not enough evidence to warrant support for such therapy (Clin. Rev. Allergy Immunol. 2011;41:267-71).
Mechanism of Action
Presently, the mechanism of action whereby skin benefits are manifested through the oral ingestion of probiotics is thought to be a downstream result of the boost in systemic immune response, especially T-cell subsets such as Th1 cells that may ultimately enhance immune responses in organs beyond the digestive tract (Clin. Plast. Surg. 2012;39:59-64; Clin. Dermatol. 2008;26:4-11).
In discussing an alternative to antibacterial products for imbalances in cutaneous microorganisms that result in mild acne, xerosis, or AD, Simmering and Breves suggest that "prebiotic actives rebalance the skin microflora while probiotic approaches predominantly consist of applying an inactivated microbial biomass of beneficial bacteria" (Hautarzt. 2009;60:809-14).
Cutaneous Immune Homeostasis
In a 2009 randomized, double-blind, placebo-controlled clinical trial with 54 volunteers, Guéniche et al. set out to ascertain whether the probiotic bacterium L. johnsonii (La1) could influence cutaneous immune homeostasis in humans after solar-simulated UV exposure (twice 1.5 MED [minimal erythema dose]). They showed that La1 consumption contributed to hastening the recovery of allostimulatory function in epidermal cells (Dermatoendocrinol. 2009;1:275-9).
Previously, in 2008, Peguet-Navarro et al. conducted a randomized, double-blind, placebo-controlled clinical trial in 54 healthy volunteers to study the potential impact of oral supplementation with La1 on skin immune status after UV exposure. Subjects received either La1 or placebo during the 6 weeks prior to solar-simulated UV exposure. The investigators found on day 4 after exposure that the allostimulatory capacity of epidermal cells had completely recovered in the La1 group correlating with the normalization of epidermal CD1a expression. They concluded that ingested probiotic bacteria hasten the recovery of skin immune homeostasis after UV-provoked immunosuppression (Eur. J. Dermatol. 2008;18:504-11).
Anti-inflammatory Activity
In 2010, Guéniche et al. demonstrated that B. longum can reduce skin inflammation mediated by substance P (Exp. Dermatol. 2010;19:e1-8). In a separate study, some of the same investigators found that L. paracasei appears to have the capacity to confer benefits related to barrier function and skin reactivity, also blunting the effects of substance P–induced skin inflammation (Eur. J. Dermatol. 2010;20:731-7).
Antiphotoaging Activity
In 2010, Bouilly-Gauthier et al. evaluated the effects of a dietary supplement combining L. johnsonii (La1), which is thought to protect the skin immune system after UV exposure, and nutritional doses of carotenoids on early UV-induced skin damage. They performed three clinical trials using various UV sources (non–extreme UV with a high UVA irradiance, extreme simulated solar radiation, and natural sunlight) in 139 healthy women over age 18 with skin type II-IV. The investigators found over the 10 weeks of the study that the combination of probiotic (La1) and nutritional doses of carotenoids lowered early UV-induced skin damage caused by simulated or natural sun exposure. Further study of the possible long-term effects against UV exposure and photoaging is warranted, they concluded (Br. J. Dermatol. 2010;163:536-43).
Topical Uses
In a study more than a decade ago, Di Marzio et al. showed that the topical application of a cream containing Streptococcus thermophilus, an organism found in most yogurts, raised the production of ceramides, which is notable given the anti-inflammatory activity and antimicrobial activity of some ceramides against Proprionibacterium acnes (J. Invest. Dermatol. 1999;113:98-106;Gut Pathog. 2011;3:1). Two recent in vitro studies have also revealed that probiotics can have antibacterial activity against P. acnes (Int. J. Cosmet. Sci. 2010;32:139-42; J. Microbiol. 2009;47:101-9). The prospects for efficacy of topically applied probiotics in the prevention and treatment of pro-inflammatory immune reactions are considered, by some, to be promising, however (Hautarzt. 2009;60:795-801). And, in fact, Guéniche et al. have found that the topical application of Vitreoscilla filiformis demonstrated efficacy against seborrheic dermatitis and AD (J. Eur. Acad. Dermatol. Venereol. 2008;22:1014-5; Eur. J. Dermatol. 2006;16:380-4).
Conclusion
While still controversial, the findings of probiotics’ effects in the treatment of atopic dermatitis remain compelling. Even more interesting, though, is the current work that suggests additional potential applications of probiotics in the dermatologic armamentarium. The work is in its early stages, but results warrant additional research, at the very least, if not cause for optimism over the prospect of more supportive evidence.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest.
Cosmeceutical Critique: Safflower Oil
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Safflower (Carthamus tinctorius), a thistlelike annual, is one of the oldest cultivated crops, its use dating back to ancient Egypt. It was traditionally grown for its seeds, which were used in foods and folk medicine. Safflower is now primarily cultivated for its vegetable oil, which is extracted from its seeds. Safflower oil has been found to exert notable health benefits when consumed through the diet and also when used in topical formulations.
Linoleic acid is a primary constituent of safflower seeds, and is the component to which the oil’s cutaneous benefits are typically ascribed. In fact, safflower oil is one of the richest sources of linoleic acid, which is necessary for the endogenous production of ceramides, key components of the epidermal layer that play a crucial role in barrier function and help the skin retain water.
In skin care products, safflower oil is incorporated in moisturizing agents for its occlusive properties. Occlusive agents coat the stratum corneum to slow transepidermal water loss. Typically, such substances have the capacity to dissolve fats and are therefore used in many skin care cosmetics.
Research on Topical Applications
In an early study on the antiproliferative potential of C. tinctorius extracts, Yasukawa et al., in 1996, isolated erythro-alkane-6,8-diols from the flowers of C. tinctorius and applied the tumor-promoting agent 12-O-tetradecanoylphorbol-13-acetate (TPA) to the ears of mice (1 mcg/ear) to induce inflammation. The investigators reported that five of the eight alkane-6,8-diols assayed suppressed inflammation, and the mixture of erythro-alkane-6,8-diols significantly inhibited TPA-induced skin tumor formation in mice after initiation with 7,12-dimethylbenz[a]anthracene (Oncology 1996;53:133-6).
In 2004, Roh et al. investigated the melanogenesis-suppressing activity of safflower seeds to develop a novel skin-whitening agent. They reported that an 80% aqueous methanol extract and ethyl acetate fraction from the seeds significantly inhibited mushroom tyrosinase, and the researchers identified three active constituents [N-feruloylserotonin, N-(p-coumaroyl)serotonin, and acacetin]. Of these, N-feruloylserotonin and N-(p-coumaroyl)serotonin were found to more potently suppress the melanin synthesis of Streptomyces bikiniensis and B16 melanoma cells than arbutin, a well-known inhibitor of melanogenesis (Biol. Pharm. Bull. 2004;27:1976-8).
In 2005, Solanki et al. conducted a short, randomized controlled study in a tertiary-care neonatal intensive care unit (NICU) of a large teaching hospital, to assess the transcutaneous absorption of oil traditionally used in massage of newborns, and to compare the effects of safflower oil and coconut oil on fatty acid profiles of massaged babies. The investigators randomly assigned 120 babies to three groups – safflower oil, coconut oil, or no-oil controls (40 in each group). The babies were massaged with 5 mL of oil four times daily for 5 days. Blood triglyceride levels were significantly elevated in all groups, though much more so in the noncontrol groups. Significant increases in essential fatty acids (linolenic and arachidonic) were seen in the safflower oil group, and similar increases in saturated fats were seen in the coconut oil group, with changes more evident in term babies. The researchers concluded that topically applied oil is absorbed in neonates and is likely available nutritionally. Consequently, they deemed the fatty acid constituents of the massage oils significant in potentially impacting the fatty acid profiles of patients (Indian Pediatr. 2005;42:998-1005). Safflower oil is rich in essential fatty acids, and coconut oil is rife with saturated fat.
Potential Dietary Benefits
Safflower oil has also been found, as has olive oil, to confer dietary benefits on diabetic pregnant rats and their embryos, preventing diabetes-induced developmental harm during early organogenesis (Mol. Hum. Reprod. 2010;16:286-95). Supplementation with either oil has also been demonstrated to prevent excessive activity by matrix metalloproteinases (specifically MMP-2 and MMP-9) in the placenta of diabetic rats, with salubrious effects manifesting in the sera (Placenta 2012;33:8-16). In addition, in a recent study, safflower oil and folic acid supplementations were shown to interact, protecting rat embryos from diabetes-induced harm through reductions in proinflammatory mediators (Mol. Hum. Reprod. 2012;18:253-64).
As mentioned above, safflower oil is available in several topical products, but it is more likely beneficial through diet. Topically, safflower oil, as found in a Neutrogena bath oil, for example, contains linoleic acid and may be useful when added to bathwater or applied to wet skin. Of course, oils in general are not suitable for all skin types. Safflower oil is indicated for individuals with dry or damaged skin.
Conclusion
Safflower oil, rich in the essential omega-6 fatty acid linoleic acid, is known to confer health benefits via diet. It is also included in skin care products, such as bath oils, which anecdotally appear to be effective. Nevertheless, there is a dearth of data on the use of safflower oil for dermatologic purposes. Much more research is necessary, including randomized controlled clinical trials in humans, to establish the potential for more extensive uses of safflower oil for skin health.
Dr. Baumann is in private practice in Miami Beach. She did not disclose any conflicts of interest. To respond to this column, or to suggest topics for future columns, write to her at [email protected].
Lignin Peroxidase
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Lignin Peroxidase
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Lignin peroxidase, a novel skin-lightening active agent that is derived from a fungus, is being studied with some interest and is being developed as an ingredient in products to treat pigmentation disorders.
Melanin, the dark pigment in the skin, is produced in the basal layer of the epidermis by melanocytes. Melanocytes make melanin, which is packaged into melanosomes and then transferred to the epidermal cells (keratinocytes). Accumulation of melanin in the epidermis is the main cause of pigmentation disorders, which are observed in all demographic groups but most commonly in people with darker skin types.
Excessive sun exposure in dark and light skin types can lead to unwanted accumulation of pigment (known as solar lentigo) in the skin. Pigmentation disorders are notoriously difficult to treat. Melanin is a very durable compound, and researchers have been largely unsuccessful in finding ways to break down melanin to reduce unwanted skin pigment. The existing topical treatments for skin lightening focus on the prevention of melanin formation by blocking tyrosinase and inhibiting its biosynthesis; by preventing the stimulation of melanocytes by UVA: or by blocking the transfer of melanosomes to keratinocytes via the PAR-2 receptor.
Alternative to Hydroquinone
Historically, the most effective treatments for skin lightening have contained hydroquinone. However, hydroquinone has become controversial, and related safety concerns have prompted research into alternative agents to treat skin pigmentation disorders. In addition, the skin develops tachyphylaxis to hydroquinone requiring 1-month "holidays" in order to maintain effectiveness, and a subset of people may develop contact allergy to hydroquinone. Many other compounds have been studied for the treatment of pigmentation disorders, including retinoids, mequinol, azelaic acid, arbutin, kojic acid, aloesin, licorice extract, ascorbic acid, soy proteins, N-acetyl glucosamine, and most recently, lignin peroxidase.
The enzyme lignin peroxidase (LIP) was first identified in 1984 (Arch. Biochem. Biophys. 1984;234:353-62), and has been researched for many years as a potential agent to break down lignin to whiten wood pulp in paper production. It was later found to break down eumelanin, which has a chemical structure similar to lignin. The development of lignin peroxidase as a skin-lightening agent resulted from these discoveries (U.S. Patent and Trademark Office Patent Application 20060051305). This novel skin-lightening active ingredient is produced extracellularly during submerged fermentation of the fungus Phanerochaete chrysosporium 3 (Biotechnol. Bioproc. E. 2004;9:153-68) and then purified from the fermented liquid medium (Lonza of Switzerland).The LIP enzyme (trademarked as Melanozyme) identifies eumelanin in the epidermis and specifically breaks down the pigment without affecting melanin biosynthesis or blocking tyrosinase. Although there are other types of lignin peroxidase enzymes, at this point, Melanozyme is the only one that has been developed and proved to be effective for skin lightening. Melanozyme is a glycoprotein active at pH 2-4.5 and inactive above that pH level. (The normal pH of skin is around 5.5, with slight variations between 5.0 and 6.5.)
Product Based on Lignin Peroxidase
Melanozyme is currently proprietary and is available only in a new skin-lightening product known on the market as Elure The Elure products are presented in a two-sided dispenser with one side containing the Melanozyme component and the other side an activator. Melanozyme alone has little ability to lighten skin, and first needs to be oxidized by hydrogen peroxide (0.012% in the activator) to enter an "activated state." The activator, which contains a small amount of hydrogen peroxide, is applied to the surface of the skin after the Melanozyme.
When applied to skin, the products that contain the Melanozyme and the activator have to be slightly acidic and buffered in order for the enzyme to perform. In addition, the enzyme is required to be first oxidized by H2O2, and then reduced by a substrate molecule (for example, veratryl alcohol) before the melanin is oxidized. After application of Elure lotion or cream, the skin pH is temporarily reduced to 3.5 but subsequently increases to its normal level of around 5.5. As the skin surface returns to the normal pH level, the enzyme is inactivated. It becomes a simple glycoprotein and is hydrolyzed in the skin by the naturally present proteases and other glycosidases into amino acids.
The safety of lignin peroxidase as a skin-lightening active ingredient has been demonstrated in preclinical studies (data on file at Rakuto Bio Technologies Ltd., 5 Carmel Street, P.O. Box 528, New Industrial Park, Yokneam 20692 Israel) with doses that are 17,000 times the recommended dose without prompting any side effects. LIP is nonmutagenic and nonirritating to eyes. The potential for skin irritation is very low, and in studies of 50 subjects each, there were no reports of skin irritation during acute sensitivity or cumulative sensitivity, or when used in sensitized skin.
Conclusion
Three open-label clinical trials and one double-blind, split-face controlled study (Rakuto Bio Technologies) in subjects with Fitzpatrick skin types II-IV have confirmed the tolerability of Elure. In all clinical studies conducted with Elure, significant improvement in tone, evenness, and dyspigmentation were achieved in most subjects within 1 month of use. Elure has been shown to be better tolerated and more effective than 2% hydroquinone. However, more studies are needed to compare the product against stronger concentrations of hydroquinone and other existing treatments, as well as to demonstrate its effectiveness in the treatment of other pigmentary conditions in a broader range of patients. The use of Elure in a combination skin care regimen with hydroquinone and glycolic acid has not been studied, but there is no reason to believe that these products would be incompatible. In fact, a glycolic cleanser that lowers the pH of the skin prior to application could theoretically enhance the efficacy of the product.
Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, write to her at [email protected]. Dr. Baumann is on the advisory board of Syneron, the manufacturer of Elure.
Sunless Tanners
Coloring the skin with dihydroxyacetone to create an artificial tan was discovered serendipitously in the 1950s by Eva Wittgenstein, whose patients were taking DHA orally. She observed that when patients regurgitated the DHA, pigmented spots remained on the skin (Science 1960;132:894-5).
The change in pigmentation results from the interaction of DHA with amino acids in the stratum corneum (Br. J. Dermatol. 2003;149:332-40).
Although the first product brought to market to exploit this new knowledge in 1959 met with initial success, it fell into disuse because of the poor cosmetic results (J. Am. Acad. Dermatol. 2003;49:1096-106; South. Med. J. 2005;98:1192-5).
Public awareness of sunless tanning has grown in recent years, however, and has been met with formulations that afford a much improved cosmetic performance, with DHA remaining as the main active ingredient in sunless-tanning agents (South. Med. J. 2005;98:1192-5; Am. J. Clin. Dermatol. 2002;3:317-8).
This column will briefly review the role of sunless-tanning lotions and sprays in dermatology, and will try to place recommendations to patients about sunless tanners in the context of sunscreens and tanning attitudes.
Sunless tanners have been used, with varying degrees of popularity, for 50 years; recent evidence suggests that the use of these products has increased in recent years. A long track record of usage and research indicates that sunless-tanning compounds are safe (J. Environ. Pathol. Toxicol. Oncol. 1984;5:349-51; Am. J. Clin. Dermatol. 2002;3:317-8; South. Med. J. 2005;98:1192-5; J. Am. Acad. Dermatol. 2007;56:387-90.) However, there is some debate as to whether the use of these products renders users more inclined to stay in the sun longer. Also, ongoing research has raised some safety issues regarding DHA.
Chemical Protection
In 2004, Petersen et al. investigated the effects of DHA on cell survival and proliferation of a human keratinocyte cell line, HaCaT. Significant genotoxic activity was identified in these cultured cells, as researchers noted dose- and time-dependent morphologic alterations as well as cytoplasmic budding and cell detachment in DHA-treated cells, and apoptosis and marked declines in proliferation 1 day after DHA exposure. Interestingly, the development of DNA strand breaks was prevented via preincubation with antioxidants. The authors suggested that their findings raised concerns about the long-term use of treating the skin with DHA-containing formulations (Mutat. Res. 2004;560:173-86).
A small study by Faurschou et al. showed that DHA provided human skin with modest UVB protection, with a 5% DHA cream applied three times or a 20% DHA cream applied once yielding an effect similar to an SPF 1.6. They acknowledged that most commercial DHA products contain 3%-5% DHA and offer scant protection. A potential advantage of sunless tanners, if they offer protection, suggested the authors, would be that no spots would be left unattended since such gaps would be conspicuous for lack of browning (Arch. Dermatol. 2004;140:886-7).
Howe, Reed, and Dellavalle contended that DHA in self-tanning agents provided enough UVA protection to warrant use as an adjunct to daily sunscreen use for broad-band protection (J. Am. Acad. Dermatol. 2008;58:894). The researchers referenced a 1975 study in which 3% DHA augmented sunlight tolerance among five patients with UVA-sensitive dermatoses (Dermatologica 1975;150:346-51; J. Am. Acad. Dermatol. 2008;58:894).
In 2009, Choquenet et al. assessed the sun protection potency of self-tanners and foundations using an in vitro method to identify indicators such as sun protection factor (SPF), UVA protection factor (PF-UVA), and UVB/UVA ratio. Using seven amino acids in the corneal cells of the epidermis, the investigators identified SPFs virtually equivalent to zero (approximately SPF 2). Conversely, they found foundations to exhibit satisfactory photostability and a non-negligible SPF, noting that such products are safe given their typically once-daily application (J. Dermatol. 2009;36:587-91).
Attitudes and Behavior
Users of sunless-tanning products were found, in a survey of 2,005 randomly selected South Australian adults published in 2001, to be more likely to use sunscreen but less likely to wear a hat or other sun-protective clothing. Sunburns were also linked to the use of sunless tanners in this study (Med. J. Aust. 2001;174:75-8; J. Am. Acad. Dermatol. 2007;56:387-90).
In 2005, Mahler et al. conducted a randomized, controlled trial with 1-month follow-up of 146 Southern California college students to study the impact of UV photoaging photographs and data on the sun protection plans and behaviors of young adults, and whether sunless-tanning lotion might play a role in sun-protective behavior. Of the 146 volunteers, 91.1% completed the "surprise" 1-month follow-up. The intervention consisted of volunteers being shown a UV facial photo and short video illustrating the etiology and results of photoaging. The investigators found that the UV photographic intervention was successful insofar as significantly better sun protection strategies and behaviors were employed by the test group, compared with controls. In addition, they noted that those who used sunless-tanning lotion were more likely to exhibit extensive sun-protective behavior, compared with individuals who received the intervention alone. The authors suggested that such interventions represented a cost-effective approach that might yield behaviors with long-term health benefits in the form of a lower incidence of skin cancer (Arch. Dermatol. 2005;141:373-80).
Later that year, Sheehan and Lesher reported on their anonymous survey of 121 adults (107 women and 14 men) who received spray-on sunless-tanning treatments between February and May 2004. Most reported that sunless tanning had not or would not affect their use of sunscreen or time spent outdoors. Interestingly, though, 73% of the respondents who had used tanning beds indicated that they had reduced or would reduce their use of indoor tanning. The researchers concluded that practitioners should recommend sunless tanning to their patients who use conventional tanning beds as a way to lower their solar exposure and risk of skin cancer (South. Med. J. 2005;98:1192-5).
In 2006, Brooks et al. reported on their July 2004, greater Boston, cross-sectional survey of 448 nonrandomly selected people aged 18-30 years on the subjects of artificial tanning products, recent history of sunburns, and tanning-bed use. During the preceding year, 22% of respondents had used sunless-tanning products and the same percentage hadn’t but would consider using them in the next year. Users of these lotions were more likely to have been severe burners and, after controlling for skin type, the investigators found that previous and potential users were more likely to have experienced sunburns during the summer and to have used tanning beds than were respondents who had neither used nor planned to use sunless tanners. The researchers concluded that the option of sunless tanning did not seem to lower the incidence of sunburn or the use of tanning beds. Further, they urged caution in offering broad support for artificial tanning products, even though looking for alternatives to UV exposure is to be encouraged (J. Am. Acad. Dermatol. 2006;54:1060-6).
A 2007 study using data from 5,491 completed interviews as part of the National Cancer Institute’s HINTS (Health Information National Trends Survey) 2005 set out to determine the prevalence of sunless-tanning formulation use and to understand the relationship between sunless tanning, indoor tanning, and sun-protective behavior. In so doing, the investigators found that the use of sunless-tanning products was relatively rare, with an estimated 11% of U.S. adults claiming to have used such products in the previous year. Of this group, 13% used sunless tanners more than 25 times; 12% used them 11-24 times; 35% used them 3-10 times; and 40% used them just once or twice. Users and exclusive users were more likely to be women, well educated, and living in the West (J. Am. Acad. Dermatol. 2007;56:387-90).
Recent Cause for Pause
In 2008, Jung et al. used the electron spin resonance spectroscopy–based radical sun protection factor, which measures free-radical reactions in skin biopsies during UV exposure and can determine the protective effect of UV filters and sunscreens, to analyze three different self-tanning agents, including DHA. Noting that the reaction of the reducing sugars in such products and amino acids (Maillard reaction) in the skin layer engendered Amadori products that created free radicals during UV irradiation, the investigators reported that in DHA-treated skin, more than 180% additional radicals were produced during sun exposure, compared with untreated skin. They concluded that the use of self-tanners necessitated reducing solar exposure duration (Spectrochim. Acta A. Mol. Biomol Spectrosc. 2008;69:1423-8). Consequently, DHA users would be well advised to wait at least 24 hours before solar exposure following application of sunless lotion or spray (Dermatol. Clin. 2009;27:149-54).
Conclusion
In addition to the need to continually persuade patients to engage in skin-protective behavior – namely, limiting sun exposure, avoiding peak-time exposures, wearing wide-brimmed hats and clothing with SPF value, and using sunscreens (preferably those containing avobenzone, Mexoryl, zinc oxide, or titanium dioxide) every day – it is incumbent upon dermatologists to disabuse our patients of the idea that untanned skin is less attractive or, conversely, that tans should be equated with attractive skin. Although healthy messages (that there is no such thing as a healthy tan, and that a tan indicates skin damage) are slowly spreading, sunless tanners appear to be a medically and cosmetically acceptable intermediary step, far surpassing the patently detrimental effects of indoor tanning. That said, patients should be advised to refrain from solar exposure for a full 24 hours after applying sunless tanners. Furthermore, much more research is necessary to truly establish that DHA delivers even modest protection from UVA or UVB. Accordingly, patients should be counseled that sunless tanners do not suffice as a base, nor do they justify extended solar exposure, and that sunscreens should also be applied.
This column, "Cosmeceutical Critique," regularly appears in Skin & Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann.
Coloring the skin with dihydroxyacetone to create an artificial tan was discovered serendipitously in the 1950s by Eva Wittgenstein, whose patients were taking DHA orally. She observed that when patients regurgitated the DHA, pigmented spots remained on the skin (Science 1960;132:894-5).
The change in pigmentation results from the interaction of DHA with amino acids in the stratum corneum (Br. J. Dermatol. 2003;149:332-40).
Although the first product brought to market to exploit this new knowledge in 1959 met with initial success, it fell into disuse because of the poor cosmetic results (J. Am. Acad. Dermatol. 2003;49:1096-106; South. Med. J. 2005;98:1192-5).
Public awareness of sunless tanning has grown in recent years, however, and has been met with formulations that afford a much improved cosmetic performance, with DHA remaining as the main active ingredient in sunless-tanning agents (South. Med. J. 2005;98:1192-5; Am. J. Clin. Dermatol. 2002;3:317-8).
This column will briefly review the role of sunless-tanning lotions and sprays in dermatology, and will try to place recommendations to patients about sunless tanners in the context of sunscreens and tanning attitudes.
Sunless tanners have been used, with varying degrees of popularity, for 50 years; recent evidence suggests that the use of these products has increased in recent years. A long track record of usage and research indicates that sunless-tanning compounds are safe (J. Environ. Pathol. Toxicol. Oncol. 1984;5:349-51; Am. J. Clin. Dermatol. 2002;3:317-8; South. Med. J. 2005;98:1192-5; J. Am. Acad. Dermatol. 2007;56:387-90.) However, there is some debate as to whether the use of these products renders users more inclined to stay in the sun longer. Also, ongoing research has raised some safety issues regarding DHA.
Chemical Protection
In 2004, Petersen et al. investigated the effects of DHA on cell survival and proliferation of a human keratinocyte cell line, HaCaT. Significant genotoxic activity was identified in these cultured cells, as researchers noted dose- and time-dependent morphologic alterations as well as cytoplasmic budding and cell detachment in DHA-treated cells, and apoptosis and marked declines in proliferation 1 day after DHA exposure. Interestingly, the development of DNA strand breaks was prevented via preincubation with antioxidants. The authors suggested that their findings raised concerns about the long-term use of treating the skin with DHA-containing formulations (Mutat. Res. 2004;560:173-86).
A small study by Faurschou et al. showed that DHA provided human skin with modest UVB protection, with a 5% DHA cream applied three times or a 20% DHA cream applied once yielding an effect similar to an SPF 1.6. They acknowledged that most commercial DHA products contain 3%-5% DHA and offer scant protection. A potential advantage of sunless tanners, if they offer protection, suggested the authors, would be that no spots would be left unattended since such gaps would be conspicuous for lack of browning (Arch. Dermatol. 2004;140:886-7).
Howe, Reed, and Dellavalle contended that DHA in self-tanning agents provided enough UVA protection to warrant use as an adjunct to daily sunscreen use for broad-band protection (J. Am. Acad. Dermatol. 2008;58:894). The researchers referenced a 1975 study in which 3% DHA augmented sunlight tolerance among five patients with UVA-sensitive dermatoses (Dermatologica 1975;150:346-51; J. Am. Acad. Dermatol. 2008;58:894).
In 2009, Choquenet et al. assessed the sun protection potency of self-tanners and foundations using an in vitro method to identify indicators such as sun protection factor (SPF), UVA protection factor (PF-UVA), and UVB/UVA ratio. Using seven amino acids in the corneal cells of the epidermis, the investigators identified SPFs virtually equivalent to zero (approximately SPF 2). Conversely, they found foundations to exhibit satisfactory photostability and a non-negligible SPF, noting that such products are safe given their typically once-daily application (J. Dermatol. 2009;36:587-91).
Attitudes and Behavior
Users of sunless-tanning products were found, in a survey of 2,005 randomly selected South Australian adults published in 2001, to be more likely to use sunscreen but less likely to wear a hat or other sun-protective clothing. Sunburns were also linked to the use of sunless tanners in this study (Med. J. Aust. 2001;174:75-8; J. Am. Acad. Dermatol. 2007;56:387-90).
In 2005, Mahler et al. conducted a randomized, controlled trial with 1-month follow-up of 146 Southern California college students to study the impact of UV photoaging photographs and data on the sun protection plans and behaviors of young adults, and whether sunless-tanning lotion might play a role in sun-protective behavior. Of the 146 volunteers, 91.1% completed the "surprise" 1-month follow-up. The intervention consisted of volunteers being shown a UV facial photo and short video illustrating the etiology and results of photoaging. The investigators found that the UV photographic intervention was successful insofar as significantly better sun protection strategies and behaviors were employed by the test group, compared with controls. In addition, they noted that those who used sunless-tanning lotion were more likely to exhibit extensive sun-protective behavior, compared with individuals who received the intervention alone. The authors suggested that such interventions represented a cost-effective approach that might yield behaviors with long-term health benefits in the form of a lower incidence of skin cancer (Arch. Dermatol. 2005;141:373-80).
Later that year, Sheehan and Lesher reported on their anonymous survey of 121 adults (107 women and 14 men) who received spray-on sunless-tanning treatments between February and May 2004. Most reported that sunless tanning had not or would not affect their use of sunscreen or time spent outdoors. Interestingly, though, 73% of the respondents who had used tanning beds indicated that they had reduced or would reduce their use of indoor tanning. The researchers concluded that practitioners should recommend sunless tanning to their patients who use conventional tanning beds as a way to lower their solar exposure and risk of skin cancer (South. Med. J. 2005;98:1192-5).
In 2006, Brooks et al. reported on their July 2004, greater Boston, cross-sectional survey of 448 nonrandomly selected people aged 18-30 years on the subjects of artificial tanning products, recent history of sunburns, and tanning-bed use. During the preceding year, 22% of respondents had used sunless-tanning products and the same percentage hadn’t but would consider using them in the next year. Users of these lotions were more likely to have been severe burners and, after controlling for skin type, the investigators found that previous and potential users were more likely to have experienced sunburns during the summer and to have used tanning beds than were respondents who had neither used nor planned to use sunless tanners. The researchers concluded that the option of sunless tanning did not seem to lower the incidence of sunburn or the use of tanning beds. Further, they urged caution in offering broad support for artificial tanning products, even though looking for alternatives to UV exposure is to be encouraged (J. Am. Acad. Dermatol. 2006;54:1060-6).
A 2007 study using data from 5,491 completed interviews as part of the National Cancer Institute’s HINTS (Health Information National Trends Survey) 2005 set out to determine the prevalence of sunless-tanning formulation use and to understand the relationship between sunless tanning, indoor tanning, and sun-protective behavior. In so doing, the investigators found that the use of sunless-tanning products was relatively rare, with an estimated 11% of U.S. adults claiming to have used such products in the previous year. Of this group, 13% used sunless tanners more than 25 times; 12% used them 11-24 times; 35% used them 3-10 times; and 40% used them just once or twice. Users and exclusive users were more likely to be women, well educated, and living in the West (J. Am. Acad. Dermatol. 2007;56:387-90).
Recent Cause for Pause
In 2008, Jung et al. used the electron spin resonance spectroscopy–based radical sun protection factor, which measures free-radical reactions in skin biopsies during UV exposure and can determine the protective effect of UV filters and sunscreens, to analyze three different self-tanning agents, including DHA. Noting that the reaction of the reducing sugars in such products and amino acids (Maillard reaction) in the skin layer engendered Amadori products that created free radicals during UV irradiation, the investigators reported that in DHA-treated skin, more than 180% additional radicals were produced during sun exposure, compared with untreated skin. They concluded that the use of self-tanners necessitated reducing solar exposure duration (Spectrochim. Acta A. Mol. Biomol Spectrosc. 2008;69:1423-8). Consequently, DHA users would be well advised to wait at least 24 hours before solar exposure following application of sunless lotion or spray (Dermatol. Clin. 2009;27:149-54).
Conclusion
In addition to the need to continually persuade patients to engage in skin-protective behavior – namely, limiting sun exposure, avoiding peak-time exposures, wearing wide-brimmed hats and clothing with SPF value, and using sunscreens (preferably those containing avobenzone, Mexoryl, zinc oxide, or titanium dioxide) every day – it is incumbent upon dermatologists to disabuse our patients of the idea that untanned skin is less attractive or, conversely, that tans should be equated with attractive skin. Although healthy messages (that there is no such thing as a healthy tan, and that a tan indicates skin damage) are slowly spreading, sunless tanners appear to be a medically and cosmetically acceptable intermediary step, far surpassing the patently detrimental effects of indoor tanning. That said, patients should be advised to refrain from solar exposure for a full 24 hours after applying sunless tanners. Furthermore, much more research is necessary to truly establish that DHA delivers even modest protection from UVA or UVB. Accordingly, patients should be counseled that sunless tanners do not suffice as a base, nor do they justify extended solar exposure, and that sunscreens should also be applied.
This column, "Cosmeceutical Critique," regularly appears in Skin & Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann.
Coloring the skin with dihydroxyacetone to create an artificial tan was discovered serendipitously in the 1950s by Eva Wittgenstein, whose patients were taking DHA orally. She observed that when patients regurgitated the DHA, pigmented spots remained on the skin (Science 1960;132:894-5).
The change in pigmentation results from the interaction of DHA with amino acids in the stratum corneum (Br. J. Dermatol. 2003;149:332-40).
Although the first product brought to market to exploit this new knowledge in 1959 met with initial success, it fell into disuse because of the poor cosmetic results (J. Am. Acad. Dermatol. 2003;49:1096-106; South. Med. J. 2005;98:1192-5).
Public awareness of sunless tanning has grown in recent years, however, and has been met with formulations that afford a much improved cosmetic performance, with DHA remaining as the main active ingredient in sunless-tanning agents (South. Med. J. 2005;98:1192-5; Am. J. Clin. Dermatol. 2002;3:317-8).
This column will briefly review the role of sunless-tanning lotions and sprays in dermatology, and will try to place recommendations to patients about sunless tanners in the context of sunscreens and tanning attitudes.
Sunless tanners have been used, with varying degrees of popularity, for 50 years; recent evidence suggests that the use of these products has increased in recent years. A long track record of usage and research indicates that sunless-tanning compounds are safe (J. Environ. Pathol. Toxicol. Oncol. 1984;5:349-51; Am. J. Clin. Dermatol. 2002;3:317-8; South. Med. J. 2005;98:1192-5; J. Am. Acad. Dermatol. 2007;56:387-90.) However, there is some debate as to whether the use of these products renders users more inclined to stay in the sun longer. Also, ongoing research has raised some safety issues regarding DHA.
Chemical Protection
In 2004, Petersen et al. investigated the effects of DHA on cell survival and proliferation of a human keratinocyte cell line, HaCaT. Significant genotoxic activity was identified in these cultured cells, as researchers noted dose- and time-dependent morphologic alterations as well as cytoplasmic budding and cell detachment in DHA-treated cells, and apoptosis and marked declines in proliferation 1 day after DHA exposure. Interestingly, the development of DNA strand breaks was prevented via preincubation with antioxidants. The authors suggested that their findings raised concerns about the long-term use of treating the skin with DHA-containing formulations (Mutat. Res. 2004;560:173-86).
A small study by Faurschou et al. showed that DHA provided human skin with modest UVB protection, with a 5% DHA cream applied three times or a 20% DHA cream applied once yielding an effect similar to an SPF 1.6. They acknowledged that most commercial DHA products contain 3%-5% DHA and offer scant protection. A potential advantage of sunless tanners, if they offer protection, suggested the authors, would be that no spots would be left unattended since such gaps would be conspicuous for lack of browning (Arch. Dermatol. 2004;140:886-7).
Howe, Reed, and Dellavalle contended that DHA in self-tanning agents provided enough UVA protection to warrant use as an adjunct to daily sunscreen use for broad-band protection (J. Am. Acad. Dermatol. 2008;58:894). The researchers referenced a 1975 study in which 3% DHA augmented sunlight tolerance among five patients with UVA-sensitive dermatoses (Dermatologica 1975;150:346-51; J. Am. Acad. Dermatol. 2008;58:894).
In 2009, Choquenet et al. assessed the sun protection potency of self-tanners and foundations using an in vitro method to identify indicators such as sun protection factor (SPF), UVA protection factor (PF-UVA), and UVB/UVA ratio. Using seven amino acids in the corneal cells of the epidermis, the investigators identified SPFs virtually equivalent to zero (approximately SPF 2). Conversely, they found foundations to exhibit satisfactory photostability and a non-negligible SPF, noting that such products are safe given their typically once-daily application (J. Dermatol. 2009;36:587-91).
Attitudes and Behavior
Users of sunless-tanning products were found, in a survey of 2,005 randomly selected South Australian adults published in 2001, to be more likely to use sunscreen but less likely to wear a hat or other sun-protective clothing. Sunburns were also linked to the use of sunless tanners in this study (Med. J. Aust. 2001;174:75-8; J. Am. Acad. Dermatol. 2007;56:387-90).
In 2005, Mahler et al. conducted a randomized, controlled trial with 1-month follow-up of 146 Southern California college students to study the impact of UV photoaging photographs and data on the sun protection plans and behaviors of young adults, and whether sunless-tanning lotion might play a role in sun-protective behavior. Of the 146 volunteers, 91.1% completed the "surprise" 1-month follow-up. The intervention consisted of volunteers being shown a UV facial photo and short video illustrating the etiology and results of photoaging. The investigators found that the UV photographic intervention was successful insofar as significantly better sun protection strategies and behaviors were employed by the test group, compared with controls. In addition, they noted that those who used sunless-tanning lotion were more likely to exhibit extensive sun-protective behavior, compared with individuals who received the intervention alone. The authors suggested that such interventions represented a cost-effective approach that might yield behaviors with long-term health benefits in the form of a lower incidence of skin cancer (Arch. Dermatol. 2005;141:373-80).
Later that year, Sheehan and Lesher reported on their anonymous survey of 121 adults (107 women and 14 men) who received spray-on sunless-tanning treatments between February and May 2004. Most reported that sunless tanning had not or would not affect their use of sunscreen or time spent outdoors. Interestingly, though, 73% of the respondents who had used tanning beds indicated that they had reduced or would reduce their use of indoor tanning. The researchers concluded that practitioners should recommend sunless tanning to their patients who use conventional tanning beds as a way to lower their solar exposure and risk of skin cancer (South. Med. J. 2005;98:1192-5).
In 2006, Brooks et al. reported on their July 2004, greater Boston, cross-sectional survey of 448 nonrandomly selected people aged 18-30 years on the subjects of artificial tanning products, recent history of sunburns, and tanning-bed use. During the preceding year, 22% of respondents had used sunless-tanning products and the same percentage hadn’t but would consider using them in the next year. Users of these lotions were more likely to have been severe burners and, after controlling for skin type, the investigators found that previous and potential users were more likely to have experienced sunburns during the summer and to have used tanning beds than were respondents who had neither used nor planned to use sunless tanners. The researchers concluded that the option of sunless tanning did not seem to lower the incidence of sunburn or the use of tanning beds. Further, they urged caution in offering broad support for artificial tanning products, even though looking for alternatives to UV exposure is to be encouraged (J. Am. Acad. Dermatol. 2006;54:1060-6).
A 2007 study using data from 5,491 completed interviews as part of the National Cancer Institute’s HINTS (Health Information National Trends Survey) 2005 set out to determine the prevalence of sunless-tanning formulation use and to understand the relationship between sunless tanning, indoor tanning, and sun-protective behavior. In so doing, the investigators found that the use of sunless-tanning products was relatively rare, with an estimated 11% of U.S. adults claiming to have used such products in the previous year. Of this group, 13% used sunless tanners more than 25 times; 12% used them 11-24 times; 35% used them 3-10 times; and 40% used them just once or twice. Users and exclusive users were more likely to be women, well educated, and living in the West (J. Am. Acad. Dermatol. 2007;56:387-90).
Recent Cause for Pause
In 2008, Jung et al. used the electron spin resonance spectroscopy–based radical sun protection factor, which measures free-radical reactions in skin biopsies during UV exposure and can determine the protective effect of UV filters and sunscreens, to analyze three different self-tanning agents, including DHA. Noting that the reaction of the reducing sugars in such products and amino acids (Maillard reaction) in the skin layer engendered Amadori products that created free radicals during UV irradiation, the investigators reported that in DHA-treated skin, more than 180% additional radicals were produced during sun exposure, compared with untreated skin. They concluded that the use of self-tanners necessitated reducing solar exposure duration (Spectrochim. Acta A. Mol. Biomol Spectrosc. 2008;69:1423-8). Consequently, DHA users would be well advised to wait at least 24 hours before solar exposure following application of sunless lotion or spray (Dermatol. Clin. 2009;27:149-54).
Conclusion
In addition to the need to continually persuade patients to engage in skin-protective behavior – namely, limiting sun exposure, avoiding peak-time exposures, wearing wide-brimmed hats and clothing with SPF value, and using sunscreens (preferably those containing avobenzone, Mexoryl, zinc oxide, or titanium dioxide) every day – it is incumbent upon dermatologists to disabuse our patients of the idea that untanned skin is less attractive or, conversely, that tans should be equated with attractive skin. Although healthy messages (that there is no such thing as a healthy tan, and that a tan indicates skin damage) are slowly spreading, sunless tanners appear to be a medically and cosmetically acceptable intermediary step, far surpassing the patently detrimental effects of indoor tanning. That said, patients should be advised to refrain from solar exposure for a full 24 hours after applying sunless tanners. Furthermore, much more research is necessary to truly establish that DHA delivers even modest protection from UVA or UVB. Accordingly, patients should be counseled that sunless tanners do not suffice as a base, nor do they justify extended solar exposure, and that sunscreens should also be applied.
This column, "Cosmeceutical Critique," regularly appears in Skin & Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann.
Perspective: Kojic Acid
Kojic acid has many uses in dermatologic products, primarily as a skin lightener, but concerns about its irritant properties have limited its role in cosmetics. Research on kojic acid shows both its promise and some evidence to support restrictions on its widespread use.
Kojic acid (5-hydroxy-2[hydroxymethyl]-gamma-pyrone, or C6H6O4), a hydrophilic fungal metabolite derived from various species of Aspergillus, Acetobacter, and Penicillium, is commonly used as a treatment for hyperpigmentation disorders (Biochem. Mol. Biol. Int. 1994;32:731-5; Contact Dermatitis 1998;39:86-7), as a food additive for preventing enzymatic browning, and as an agent to promote the reddening of unripe strawberries (J. Sci. Food. Agr. 1977;28:243). It was discovered as a fungal natural product in 1907 (Nat. Prod. Rep. 2006;23:1046-62). Kojic acid exerts a slow-binding inhibition of tyrosinase activity, mainly by chelating copper (Dermatol. Clin. 2007;25:337-42; J. Pharm. Pharmacol. 1994;46:982-5; Phytother. Res. 2006;20:921-34), and the result is a cutaneous whitening effect.
The efficacy of kojic acid in achieving such an effect is similar to that of hydroquinone, the standard and yet still controversial depigmenting agent (Dermatol. Ther. 2004;17:151-7; Skin Therapy Lett. 2004;9:1-3). Used mainly as a skin-lightening agent, kojic acid also exhibits antibiotic, anti-inflammatory, and anodyne properties (Dermatol. Clin. 2007;25:337-42). In addition, it is used in Asia as a dietary antioxidant (Phytother. Res. 2006;20:921-34; Dermatol. Surg. 1999;25:282-4).
Treatment of Hyperpigmentation
Manufacturers, especially in Japan, have used kojic acid since 1988 in cosmetic agents for its capacity to decrease pigmentation (Semin. Cutan. Med. Surg. 2009;28:77-85; J. Pharm. Pharmacol. 1994;46:982-5). In cosmetic formulations, kojic acid enhances the shelf life of products by dint of its preservative and antibiotic activity (Cent. Eur. J. Public Health. 2004;12 [Suppl]:S16-8). Its stability is one of the advantages of kojic acid over hydroquinone and other skin-lightening ingredients (Regul. Toxicol. Pharmacol. 2001;33:80-101).
In two studies, kojic acid combined with glycolic acid was demonstrated to be more effective than 10% glycolic acid combined with 4% hydroquinone for the treatment of hyperpigmentation (Facial Plast. Surg. 1995;11:15-21; Dermatol. Surg. 1996;22:443-7). In one case, Garcia and Fulton set out to assess and compare the effects on melasma and other pigmentary conditions of a glycolic acid/hydroquinone formulation and a glycolic acid/kojic acid formulation. Wood’s light and UV light photography were used to evaluate the effects of the different compounds, one on each side of the face, in 39 patients. The investigators found no statistically significant differences between the reactions; in all, 28% of the patients experienced marked improvements on the kojic acid side, 21% on the hydroquinone side. The responses to each formulation were equal in 51% of the participants. Although the kojic acid formulation was considered more irritating, the investigators found both formulations effective in treating melasma (Dermatol. Surg. 1996;22:443-7).
Treatment for Melasma
Lim studied the effects on melasma of 2% kojic acid in a gel containing 10% glycolic acid and 2% hydroquinone in 40 Chinese women with epidermal melasma. In this 12-week study, subjects were treated with the test formulation, in randomized fashion, on one side of the face and the same formulation minus kojic acid on the other side. Self-assessment questionnaires every 4 weeks, photographs, and clinical evaluations were used to rate the efficacy of the treatment. Lim found that the addition of kojic acid to the glycolic acid/hydroquinone gel improved melasma. Specifically, more than half of the melasma cleared in 24 of 40 patients who received the kojic acid formulation, compared with 19 of 40 who received the kojic acid–free gel. Two patients experienced complete clearance, in both cases on the side of the face on which the kojic acid gel was used (Dermatol. Surg. 1999;25:282-4). Two years later, Ferioli and colleagues found that combining hydroquinone and kojic acid exerted a synergistic effect, with an equimolecular distribution achieving the optimal result (Int. J. Cosmet. Sci. 2001;23:333-40).
As a lone therapy for the treatment of melasma, however, kojic acid is a member of the arsenal but is one of the last options typically selected (Dermatol. Clin. 2007;25:337-42), because it may be irritating to the skin (Skin Therapy Lett. 2006;11:1-6; Dermatol. Nurs. 2004;16:401-6, 413-6). It can be effective, though, in patients who do not tolerate the first-line products, particularly hydroquinone (Dermatol. Nurs. 2004;16:401-6, 413-6). Furthermore, combining a topical corticosteroid with kojic acid can reduce the irritant qualities of the fungal derivative (Int. J. Dermatol. 1998;37:897-903; Phytother. Res. 2006;20:921-34). In the experimental setting, kojic acid is regularly used as a reference or positive control to test the skin-whitening potential of new agents.
Antiwrinkle Properties
Other applications of kojic acid have also been considered. In 2001, Mitani and colleagues investigated the potential antiwrinkle activity of kojic acid given the iron-chelating properties of the acid and the known association between chronic photodamage and cutaneous iron. Over 20 weeks, the investigators topically applied kojic acid prior to exposing hairless mice to UV radiation. The agent successfully inhibited wrinkle development, epidermal hyperplasia, lower dermis fibrosis, and increases in upper dermis extracellular matrix components (Eur. J. Pharmacol. 2001;411:169-74).
Skin-Lightening Properties
The primary use for kojic acid in dermatology, though, remains skin whitening. Kojic acid is second only to hydroquinone in terms of effectiveness as a skin-lightening agent in topical, over-the-counter products (Dermatol. Ther. 2007;20:308-13), and is the most popular agent for treating melasma in East Asia (Dermatol. Surg. 1999;25:282-4; Dermatol. Ther. 2007;20:308-13).This makes sense, given the increasing regulatory scrutiny of hydroquinone, which has been banned in Europe and is tightly regulated in Asia, while remaining available, however tenuously, in the United States. Kojic acid is also a sensitizer. Mild facial erythema is the primary adverse effect reported in association with the typically well-tolerated fungal metabolite (Dermatol. Clin. 2007;25:353-62), which has been banned and then permitted to return to the market as a skin-lightening agent (Dermatol. Ther. 2007;20:308-13).
Kojic acid products are typically used twice daily for 1 to 2 months or until the patient achieves the desired results. Unfortunately, kojic acid has reportedly provoked contact allergies and is considered to exhibit a high sensitizing potential (Contact Dermatitis 1995;32:9-13). Because preparations containing a 2.5% concentration of kojic acid have been associated with facial dermatitis, a concentration of 1% has become more common. However, there have also been some reports of sensitization linked to 1% creams (Contact Dermatitis 1995;32:9-13). As kojic acid has also been extensively used in foods, there have been many reports on its oral safety. In addition, injecting kojic acid has the potential to induce convulsions (Regul. Toxicol. Pharmacol. 2001;33:80-101).
Possible Link With Tumor Promotion
Despite the success of kojic acid at 1% concentrations, particularly in Japan, some studies have indicated that longer term use of the agent may engender contact dermatitis and erythema (Skin Therapy Lett. 2004;9:1-3; Contact Dermatitis 1998;39:86-7; Contact Dermatitis 1995;32:9-13). In addition, an association between hepatic tumors in heterozygous p53-deficient mice and the topical application of kojic acid has been identified (Toxicol. Sci. 2003;73:287-93; Dermatol. Clin. 2007;25:353-62). In 2003, Japan’s health ministry ordered the removal of kojic acid from the market over fears, based on animal studies, that the fungal metabolite might cause cancer (Nature 2004;432:938).
In response to such findings and concerns, specifically the link between potential tumor promotion in mouse and rat livers caused by use of kojic acid, Higa and colleagues examined the presence of initiation activity in rat liver and the potential of photogenotoxicity and carcinogenicity in mouse skin in relation to kojic acid. In one of the team’s multiple experiments, a cream containing 1.0% or 3.0% kojic acid was applied twice to the backs of mice in a 24-hour period, and researchers noted that kojic acid failed to induce epidermal cell micronuclei. In addition, a skin carcinogenesis bioassay for initiation-promotion potential revealed the emergence of no skin nodules that were caused by the topical application of 3.0% kojic acid cream to the backs of mice daily for 7 days or five times a week for 19 weeks, administered during either cancer stage. Overall, the investigators concluded that kojic acid posed a minimal risk of photocarcinogenesis in the skin and did not exhibit skin carcinogenesis initiation nor promotion activity. The findings also lent support to the contention that kojic acid is a safe ingredient in cosmeceuticals (J. Toxicol. Sci. 2007;32:143-59). In addition, Lee and colleagues recently reported on derivatives of kojic acid displaying greater efficiency through increased penetration into the skin (Arch. Pharm. (Weinheim) 2006;339:111-4).
Previously, in 2003, Kim and colleagues studied the effects of a stable kojic acid derivative, 5-[(3-aminopropyl)phosphinooxy]-2-(hydroxymethyl)-4H-pyran-4-one (Kojyl-APPA), on tyrosinase activity and melanin production. The investigators found that Kojyl-APPA is not a direct inhibitor of tyrosinase, but is enzymatically converted to kojic acid in cells. However, the derivative was found to suppress tyrosinase activity markedly 24 hours after treatment in normal human melanocytes and demonstrated a 30% inhibition of tyrosinase in situ (although not in vitro). The kojic acid derivative also lowered melanin content to 75% of control in melanoma cells and neomelanin production to 43% of control in normal human melanocytes. Notably, Kojyl-APPA had an eightfold greater capacity to permeate the skin than did kojic acid (Chem. Pharm. Bull. (Tokyo) 2003;51:113-6). A kojic acid derivative found to be eight times more potent than kojic acid as a tyrosinase inhibitor was also synthesized in 2006. The compound produced by Lee and colleagues also displayed strong inhibitory activity toward melanin production (Arch. Pharm. (Weinheim) 2006;33:111-4).
It is worth noting that although kojic acid yields greater stability than does hydroquinone, the fungal derivative does have labile oxidative properties, which are enhanced by light and heat exposure. For that reason, the inclusion of kojic acid in cosmetic formulations has been through its dipalmitic ester (as kojic dipalmitate) (Talanta 2008;75:407-1).
Conclusion
The fungal derivative kojic acid has maintained a significant role in the dermatologic armamentarium for 2 decades as a skin-whitening agent and is best used in combination with other depigmenting ingredients, which enhance the overall effect of the formulation and blunt the irritating effects of kojic acid. Recent evidence has allayed fears regarding long-term carcinogenic effects, but as always, research is ongoing to develop newer, safer derivatives.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin & Allergy News. She is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail her at [email protected].
Kojic acid has many uses in dermatologic products, primarily as a skin lightener, but concerns about its irritant properties have limited its role in cosmetics. Research on kojic acid shows both its promise and some evidence to support restrictions on its widespread use.
Kojic acid (5-hydroxy-2[hydroxymethyl]-gamma-pyrone, or C6H6O4), a hydrophilic fungal metabolite derived from various species of Aspergillus, Acetobacter, and Penicillium, is commonly used as a treatment for hyperpigmentation disorders (Biochem. Mol. Biol. Int. 1994;32:731-5; Contact Dermatitis 1998;39:86-7), as a food additive for preventing enzymatic browning, and as an agent to promote the reddening of unripe strawberries (J. Sci. Food. Agr. 1977;28:243). It was discovered as a fungal natural product in 1907 (Nat. Prod. Rep. 2006;23:1046-62). Kojic acid exerts a slow-binding inhibition of tyrosinase activity, mainly by chelating copper (Dermatol. Clin. 2007;25:337-42; J. Pharm. Pharmacol. 1994;46:982-5; Phytother. Res. 2006;20:921-34), and the result is a cutaneous whitening effect.
The efficacy of kojic acid in achieving such an effect is similar to that of hydroquinone, the standard and yet still controversial depigmenting agent (Dermatol. Ther. 2004;17:151-7; Skin Therapy Lett. 2004;9:1-3). Used mainly as a skin-lightening agent, kojic acid also exhibits antibiotic, anti-inflammatory, and anodyne properties (Dermatol. Clin. 2007;25:337-42). In addition, it is used in Asia as a dietary antioxidant (Phytother. Res. 2006;20:921-34; Dermatol. Surg. 1999;25:282-4).
Treatment of Hyperpigmentation
Manufacturers, especially in Japan, have used kojic acid since 1988 in cosmetic agents for its capacity to decrease pigmentation (Semin. Cutan. Med. Surg. 2009;28:77-85; J. Pharm. Pharmacol. 1994;46:982-5). In cosmetic formulations, kojic acid enhances the shelf life of products by dint of its preservative and antibiotic activity (Cent. Eur. J. Public Health. 2004;12 [Suppl]:S16-8). Its stability is one of the advantages of kojic acid over hydroquinone and other skin-lightening ingredients (Regul. Toxicol. Pharmacol. 2001;33:80-101).
In two studies, kojic acid combined with glycolic acid was demonstrated to be more effective than 10% glycolic acid combined with 4% hydroquinone for the treatment of hyperpigmentation (Facial Plast. Surg. 1995;11:15-21; Dermatol. Surg. 1996;22:443-7). In one case, Garcia and Fulton set out to assess and compare the effects on melasma and other pigmentary conditions of a glycolic acid/hydroquinone formulation and a glycolic acid/kojic acid formulation. Wood’s light and UV light photography were used to evaluate the effects of the different compounds, one on each side of the face, in 39 patients. The investigators found no statistically significant differences between the reactions; in all, 28% of the patients experienced marked improvements on the kojic acid side, 21% on the hydroquinone side. The responses to each formulation were equal in 51% of the participants. Although the kojic acid formulation was considered more irritating, the investigators found both formulations effective in treating melasma (Dermatol. Surg. 1996;22:443-7).
Treatment for Melasma
Lim studied the effects on melasma of 2% kojic acid in a gel containing 10% glycolic acid and 2% hydroquinone in 40 Chinese women with epidermal melasma. In this 12-week study, subjects were treated with the test formulation, in randomized fashion, on one side of the face and the same formulation minus kojic acid on the other side. Self-assessment questionnaires every 4 weeks, photographs, and clinical evaluations were used to rate the efficacy of the treatment. Lim found that the addition of kojic acid to the glycolic acid/hydroquinone gel improved melasma. Specifically, more than half of the melasma cleared in 24 of 40 patients who received the kojic acid formulation, compared with 19 of 40 who received the kojic acid–free gel. Two patients experienced complete clearance, in both cases on the side of the face on which the kojic acid gel was used (Dermatol. Surg. 1999;25:282-4). Two years later, Ferioli and colleagues found that combining hydroquinone and kojic acid exerted a synergistic effect, with an equimolecular distribution achieving the optimal result (Int. J. Cosmet. Sci. 2001;23:333-40).
As a lone therapy for the treatment of melasma, however, kojic acid is a member of the arsenal but is one of the last options typically selected (Dermatol. Clin. 2007;25:337-42), because it may be irritating to the skin (Skin Therapy Lett. 2006;11:1-6; Dermatol. Nurs. 2004;16:401-6, 413-6). It can be effective, though, in patients who do not tolerate the first-line products, particularly hydroquinone (Dermatol. Nurs. 2004;16:401-6, 413-6). Furthermore, combining a topical corticosteroid with kojic acid can reduce the irritant qualities of the fungal derivative (Int. J. Dermatol. 1998;37:897-903; Phytother. Res. 2006;20:921-34). In the experimental setting, kojic acid is regularly used as a reference or positive control to test the skin-whitening potential of new agents.
Antiwrinkle Properties
Other applications of kojic acid have also been considered. In 2001, Mitani and colleagues investigated the potential antiwrinkle activity of kojic acid given the iron-chelating properties of the acid and the known association between chronic photodamage and cutaneous iron. Over 20 weeks, the investigators topically applied kojic acid prior to exposing hairless mice to UV radiation. The agent successfully inhibited wrinkle development, epidermal hyperplasia, lower dermis fibrosis, and increases in upper dermis extracellular matrix components (Eur. J. Pharmacol. 2001;411:169-74).
Skin-Lightening Properties
The primary use for kojic acid in dermatology, though, remains skin whitening. Kojic acid is second only to hydroquinone in terms of effectiveness as a skin-lightening agent in topical, over-the-counter products (Dermatol. Ther. 2007;20:308-13), and is the most popular agent for treating melasma in East Asia (Dermatol. Surg. 1999;25:282-4; Dermatol. Ther. 2007;20:308-13).This makes sense, given the increasing regulatory scrutiny of hydroquinone, which has been banned in Europe and is tightly regulated in Asia, while remaining available, however tenuously, in the United States. Kojic acid is also a sensitizer. Mild facial erythema is the primary adverse effect reported in association with the typically well-tolerated fungal metabolite (Dermatol. Clin. 2007;25:353-62), which has been banned and then permitted to return to the market as a skin-lightening agent (Dermatol. Ther. 2007;20:308-13).
Kojic acid products are typically used twice daily for 1 to 2 months or until the patient achieves the desired results. Unfortunately, kojic acid has reportedly provoked contact allergies and is considered to exhibit a high sensitizing potential (Contact Dermatitis 1995;32:9-13). Because preparations containing a 2.5% concentration of kojic acid have been associated with facial dermatitis, a concentration of 1% has become more common. However, there have also been some reports of sensitization linked to 1% creams (Contact Dermatitis 1995;32:9-13). As kojic acid has also been extensively used in foods, there have been many reports on its oral safety. In addition, injecting kojic acid has the potential to induce convulsions (Regul. Toxicol. Pharmacol. 2001;33:80-101).
Possible Link With Tumor Promotion
Despite the success of kojic acid at 1% concentrations, particularly in Japan, some studies have indicated that longer term use of the agent may engender contact dermatitis and erythema (Skin Therapy Lett. 2004;9:1-3; Contact Dermatitis 1998;39:86-7; Contact Dermatitis 1995;32:9-13). In addition, an association between hepatic tumors in heterozygous p53-deficient mice and the topical application of kojic acid has been identified (Toxicol. Sci. 2003;73:287-93; Dermatol. Clin. 2007;25:353-62). In 2003, Japan’s health ministry ordered the removal of kojic acid from the market over fears, based on animal studies, that the fungal metabolite might cause cancer (Nature 2004;432:938).
In response to such findings and concerns, specifically the link between potential tumor promotion in mouse and rat livers caused by use of kojic acid, Higa and colleagues examined the presence of initiation activity in rat liver and the potential of photogenotoxicity and carcinogenicity in mouse skin in relation to kojic acid. In one of the team’s multiple experiments, a cream containing 1.0% or 3.0% kojic acid was applied twice to the backs of mice in a 24-hour period, and researchers noted that kojic acid failed to induce epidermal cell micronuclei. In addition, a skin carcinogenesis bioassay for initiation-promotion potential revealed the emergence of no skin nodules that were caused by the topical application of 3.0% kojic acid cream to the backs of mice daily for 7 days or five times a week for 19 weeks, administered during either cancer stage. Overall, the investigators concluded that kojic acid posed a minimal risk of photocarcinogenesis in the skin and did not exhibit skin carcinogenesis initiation nor promotion activity. The findings also lent support to the contention that kojic acid is a safe ingredient in cosmeceuticals (J. Toxicol. Sci. 2007;32:143-59). In addition, Lee and colleagues recently reported on derivatives of kojic acid displaying greater efficiency through increased penetration into the skin (Arch. Pharm. (Weinheim) 2006;339:111-4).
Previously, in 2003, Kim and colleagues studied the effects of a stable kojic acid derivative, 5-[(3-aminopropyl)phosphinooxy]-2-(hydroxymethyl)-4H-pyran-4-one (Kojyl-APPA), on tyrosinase activity and melanin production. The investigators found that Kojyl-APPA is not a direct inhibitor of tyrosinase, but is enzymatically converted to kojic acid in cells. However, the derivative was found to suppress tyrosinase activity markedly 24 hours after treatment in normal human melanocytes and demonstrated a 30% inhibition of tyrosinase in situ (although not in vitro). The kojic acid derivative also lowered melanin content to 75% of control in melanoma cells and neomelanin production to 43% of control in normal human melanocytes. Notably, Kojyl-APPA had an eightfold greater capacity to permeate the skin than did kojic acid (Chem. Pharm. Bull. (Tokyo) 2003;51:113-6). A kojic acid derivative found to be eight times more potent than kojic acid as a tyrosinase inhibitor was also synthesized in 2006. The compound produced by Lee and colleagues also displayed strong inhibitory activity toward melanin production (Arch. Pharm. (Weinheim) 2006;33:111-4).
It is worth noting that although kojic acid yields greater stability than does hydroquinone, the fungal derivative does have labile oxidative properties, which are enhanced by light and heat exposure. For that reason, the inclusion of kojic acid in cosmetic formulations has been through its dipalmitic ester (as kojic dipalmitate) (Talanta 2008;75:407-1).
Conclusion
The fungal derivative kojic acid has maintained a significant role in the dermatologic armamentarium for 2 decades as a skin-whitening agent and is best used in combination with other depigmenting ingredients, which enhance the overall effect of the formulation and blunt the irritating effects of kojic acid. Recent evidence has allayed fears regarding long-term carcinogenic effects, but as always, research is ongoing to develop newer, safer derivatives.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin & Allergy News. She is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail her at [email protected].
Kojic acid has many uses in dermatologic products, primarily as a skin lightener, but concerns about its irritant properties have limited its role in cosmetics. Research on kojic acid shows both its promise and some evidence to support restrictions on its widespread use.
Kojic acid (5-hydroxy-2[hydroxymethyl]-gamma-pyrone, or C6H6O4), a hydrophilic fungal metabolite derived from various species of Aspergillus, Acetobacter, and Penicillium, is commonly used as a treatment for hyperpigmentation disorders (Biochem. Mol. Biol. Int. 1994;32:731-5; Contact Dermatitis 1998;39:86-7), as a food additive for preventing enzymatic browning, and as an agent to promote the reddening of unripe strawberries (J. Sci. Food. Agr. 1977;28:243). It was discovered as a fungal natural product in 1907 (Nat. Prod. Rep. 2006;23:1046-62). Kojic acid exerts a slow-binding inhibition of tyrosinase activity, mainly by chelating copper (Dermatol. Clin. 2007;25:337-42; J. Pharm. Pharmacol. 1994;46:982-5; Phytother. Res. 2006;20:921-34), and the result is a cutaneous whitening effect.
The efficacy of kojic acid in achieving such an effect is similar to that of hydroquinone, the standard and yet still controversial depigmenting agent (Dermatol. Ther. 2004;17:151-7; Skin Therapy Lett. 2004;9:1-3). Used mainly as a skin-lightening agent, kojic acid also exhibits antibiotic, anti-inflammatory, and anodyne properties (Dermatol. Clin. 2007;25:337-42). In addition, it is used in Asia as a dietary antioxidant (Phytother. Res. 2006;20:921-34; Dermatol. Surg. 1999;25:282-4).
Treatment of Hyperpigmentation
Manufacturers, especially in Japan, have used kojic acid since 1988 in cosmetic agents for its capacity to decrease pigmentation (Semin. Cutan. Med. Surg. 2009;28:77-85; J. Pharm. Pharmacol. 1994;46:982-5). In cosmetic formulations, kojic acid enhances the shelf life of products by dint of its preservative and antibiotic activity (Cent. Eur. J. Public Health. 2004;12 [Suppl]:S16-8). Its stability is one of the advantages of kojic acid over hydroquinone and other skin-lightening ingredients (Regul. Toxicol. Pharmacol. 2001;33:80-101).
In two studies, kojic acid combined with glycolic acid was demonstrated to be more effective than 10% glycolic acid combined with 4% hydroquinone for the treatment of hyperpigmentation (Facial Plast. Surg. 1995;11:15-21; Dermatol. Surg. 1996;22:443-7). In one case, Garcia and Fulton set out to assess and compare the effects on melasma and other pigmentary conditions of a glycolic acid/hydroquinone formulation and a glycolic acid/kojic acid formulation. Wood’s light and UV light photography were used to evaluate the effects of the different compounds, one on each side of the face, in 39 patients. The investigators found no statistically significant differences between the reactions; in all, 28% of the patients experienced marked improvements on the kojic acid side, 21% on the hydroquinone side. The responses to each formulation were equal in 51% of the participants. Although the kojic acid formulation was considered more irritating, the investigators found both formulations effective in treating melasma (Dermatol. Surg. 1996;22:443-7).
Treatment for Melasma
Lim studied the effects on melasma of 2% kojic acid in a gel containing 10% glycolic acid and 2% hydroquinone in 40 Chinese women with epidermal melasma. In this 12-week study, subjects were treated with the test formulation, in randomized fashion, on one side of the face and the same formulation minus kojic acid on the other side. Self-assessment questionnaires every 4 weeks, photographs, and clinical evaluations were used to rate the efficacy of the treatment. Lim found that the addition of kojic acid to the glycolic acid/hydroquinone gel improved melasma. Specifically, more than half of the melasma cleared in 24 of 40 patients who received the kojic acid formulation, compared with 19 of 40 who received the kojic acid–free gel. Two patients experienced complete clearance, in both cases on the side of the face on which the kojic acid gel was used (Dermatol. Surg. 1999;25:282-4). Two years later, Ferioli and colleagues found that combining hydroquinone and kojic acid exerted a synergistic effect, with an equimolecular distribution achieving the optimal result (Int. J. Cosmet. Sci. 2001;23:333-40).
As a lone therapy for the treatment of melasma, however, kojic acid is a member of the arsenal but is one of the last options typically selected (Dermatol. Clin. 2007;25:337-42), because it may be irritating to the skin (Skin Therapy Lett. 2006;11:1-6; Dermatol. Nurs. 2004;16:401-6, 413-6). It can be effective, though, in patients who do not tolerate the first-line products, particularly hydroquinone (Dermatol. Nurs. 2004;16:401-6, 413-6). Furthermore, combining a topical corticosteroid with kojic acid can reduce the irritant qualities of the fungal derivative (Int. J. Dermatol. 1998;37:897-903; Phytother. Res. 2006;20:921-34). In the experimental setting, kojic acid is regularly used as a reference or positive control to test the skin-whitening potential of new agents.
Antiwrinkle Properties
Other applications of kojic acid have also been considered. In 2001, Mitani and colleagues investigated the potential antiwrinkle activity of kojic acid given the iron-chelating properties of the acid and the known association between chronic photodamage and cutaneous iron. Over 20 weeks, the investigators topically applied kojic acid prior to exposing hairless mice to UV radiation. The agent successfully inhibited wrinkle development, epidermal hyperplasia, lower dermis fibrosis, and increases in upper dermis extracellular matrix components (Eur. J. Pharmacol. 2001;411:169-74).
Skin-Lightening Properties
The primary use for kojic acid in dermatology, though, remains skin whitening. Kojic acid is second only to hydroquinone in terms of effectiveness as a skin-lightening agent in topical, over-the-counter products (Dermatol. Ther. 2007;20:308-13), and is the most popular agent for treating melasma in East Asia (Dermatol. Surg. 1999;25:282-4; Dermatol. Ther. 2007;20:308-13).This makes sense, given the increasing regulatory scrutiny of hydroquinone, which has been banned in Europe and is tightly regulated in Asia, while remaining available, however tenuously, in the United States. Kojic acid is also a sensitizer. Mild facial erythema is the primary adverse effect reported in association with the typically well-tolerated fungal metabolite (Dermatol. Clin. 2007;25:353-62), which has been banned and then permitted to return to the market as a skin-lightening agent (Dermatol. Ther. 2007;20:308-13).
Kojic acid products are typically used twice daily for 1 to 2 months or until the patient achieves the desired results. Unfortunately, kojic acid has reportedly provoked contact allergies and is considered to exhibit a high sensitizing potential (Contact Dermatitis 1995;32:9-13). Because preparations containing a 2.5% concentration of kojic acid have been associated with facial dermatitis, a concentration of 1% has become more common. However, there have also been some reports of sensitization linked to 1% creams (Contact Dermatitis 1995;32:9-13). As kojic acid has also been extensively used in foods, there have been many reports on its oral safety. In addition, injecting kojic acid has the potential to induce convulsions (Regul. Toxicol. Pharmacol. 2001;33:80-101).
Possible Link With Tumor Promotion
Despite the success of kojic acid at 1% concentrations, particularly in Japan, some studies have indicated that longer term use of the agent may engender contact dermatitis and erythema (Skin Therapy Lett. 2004;9:1-3; Contact Dermatitis 1998;39:86-7; Contact Dermatitis 1995;32:9-13). In addition, an association between hepatic tumors in heterozygous p53-deficient mice and the topical application of kojic acid has been identified (Toxicol. Sci. 2003;73:287-93; Dermatol. Clin. 2007;25:353-62). In 2003, Japan’s health ministry ordered the removal of kojic acid from the market over fears, based on animal studies, that the fungal metabolite might cause cancer (Nature 2004;432:938).
In response to such findings and concerns, specifically the link between potential tumor promotion in mouse and rat livers caused by use of kojic acid, Higa and colleagues examined the presence of initiation activity in rat liver and the potential of photogenotoxicity and carcinogenicity in mouse skin in relation to kojic acid. In one of the team’s multiple experiments, a cream containing 1.0% or 3.0% kojic acid was applied twice to the backs of mice in a 24-hour period, and researchers noted that kojic acid failed to induce epidermal cell micronuclei. In addition, a skin carcinogenesis bioassay for initiation-promotion potential revealed the emergence of no skin nodules that were caused by the topical application of 3.0% kojic acid cream to the backs of mice daily for 7 days or five times a week for 19 weeks, administered during either cancer stage. Overall, the investigators concluded that kojic acid posed a minimal risk of photocarcinogenesis in the skin and did not exhibit skin carcinogenesis initiation nor promotion activity. The findings also lent support to the contention that kojic acid is a safe ingredient in cosmeceuticals (J. Toxicol. Sci. 2007;32:143-59). In addition, Lee and colleagues recently reported on derivatives of kojic acid displaying greater efficiency through increased penetration into the skin (Arch. Pharm. (Weinheim) 2006;339:111-4).
Previously, in 2003, Kim and colleagues studied the effects of a stable kojic acid derivative, 5-[(3-aminopropyl)phosphinooxy]-2-(hydroxymethyl)-4H-pyran-4-one (Kojyl-APPA), on tyrosinase activity and melanin production. The investigators found that Kojyl-APPA is not a direct inhibitor of tyrosinase, but is enzymatically converted to kojic acid in cells. However, the derivative was found to suppress tyrosinase activity markedly 24 hours after treatment in normal human melanocytes and demonstrated a 30% inhibition of tyrosinase in situ (although not in vitro). The kojic acid derivative also lowered melanin content to 75% of control in melanoma cells and neomelanin production to 43% of control in normal human melanocytes. Notably, Kojyl-APPA had an eightfold greater capacity to permeate the skin than did kojic acid (Chem. Pharm. Bull. (Tokyo) 2003;51:113-6). A kojic acid derivative found to be eight times more potent than kojic acid as a tyrosinase inhibitor was also synthesized in 2006. The compound produced by Lee and colleagues also displayed strong inhibitory activity toward melanin production (Arch. Pharm. (Weinheim) 2006;33:111-4).
It is worth noting that although kojic acid yields greater stability than does hydroquinone, the fungal derivative does have labile oxidative properties, which are enhanced by light and heat exposure. For that reason, the inclusion of kojic acid in cosmetic formulations has been through its dipalmitic ester (as kojic dipalmitate) (Talanta 2008;75:407-1).
Conclusion
The fungal derivative kojic acid has maintained a significant role in the dermatologic armamentarium for 2 decades as a skin-whitening agent and is best used in combination with other depigmenting ingredients, which enhance the overall effect of the formulation and blunt the irritating effects of kojic acid. Recent evidence has allayed fears regarding long-term carcinogenic effects, but as always, research is ongoing to develop newer, safer derivatives.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin & Allergy News. She is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail her at [email protected].
Perspective: Jojoba
The jojoba (pronounced ho-ho-ba) plant (Buxus chinensis or Simmondsia chinensis) is a shrub endemic to the Sonoran Desert of northwest Mexico and adjacent areas in Arizona and southern California. This evergreen plant, also known as goat nut or coffeeberry, grows up to 15 feet high and can live for up to 200 years. Clearly, it is well adapted to thrive in the arid heat of the desert. Native Americans are known to have eaten the smooth-skinned, odorless, oil-rich nuts or seeds of the jojoba.
It is the oil of this shrub that is of keen interest as a botanical product for use in cosmetics and cosmeceuticals. The oil from jojoba nuts or seeds has been used for centuries to promote hair growth and alleviate skin conditions. Jojoba is now cultivated for commercial purposes, such as treatment for psoriasis, dry skin, and dandruff, in Argentina, Australia, Mexico, Israel, and India.
Jojoba oil is derived from the cold-pressed seeds, which are the size of peanuts or small olives (Phytother. Res. 2003;17:987-1000). It is actually a polyunsaturated liquid wax. This rich extract is typically used as a humectant in cosmetics and cosmeceuticals and confers a protective film over the skin that aids in moisture retention (Cosmet. Toiletries 1997;112:47-64). The skin’s natural sebum is readily compatible with the wide range of fatty acids (oleic, linoleic, linolenic, and arachidonic) and triglycerides that are key components of jojoba oil (J. Am. Oil Chem. Soc. 2000;77:1325-9; J. Agric. Food Chem. 1997;45:1180-4).
Some authors speculate that its efficacy as a nongreasy lubricant gives the oil, pure or in hydrogenated form, the potential for use in a variety of formulations that are designed for the skin or hair – creams, lotions, soaps, and lipsticks (J. Cosm. Sci. 1998;49:377-83). Jojoba oil has been found to impart significant beneficial properties as an analgesic, antibacterial, anti-inflammatory, antioxidant, antiparasitic, and antipyretic (Phytother. Res. 2003;17:987-1000; J. Cosm. Sci. 1998;49:377-83).
Very similar in consistency to human sebum, jojoba oil is considered to be a natural moisturizer and is thought to be highly conditioning, softening, and healing for all skin types. Although primarily used in skin and hair products now, jojoba oil first gained industry interest and support not for its reputed traditional benefits, but for its viability as a replacement for sperm whale oil, the use of which was banned by the U.S. government in the early 1970s as a result of the Endangered Species Act.
Products
Aubrey Organics (a company that uses botanicals organically grown and processed in accordance with the California Organic Foods Act of 1990) offers two hair products containing jojoba oil. Its J.A.Y. (Jojoba/Aloe/Yucca) Desert Herb Shampoo and Jojoba & Aloe Hair Rejuvenator & Conditioner are said to hydrate and revitalize especially dry and brittle hair. According to the manufacturer, the humectant activity of jojoba oil generates a protective film over the hair and scalp that helps retain moisture. The Swiss company Colos? Beauty also produces a wide array of formulations that contain jojoba oil for the purpose of protecting against dehydration. Colos?’s product line includes Day Cream Sensitive, Day Cream Multi-Active, Cream Egalisante, Miracle Cream, and Night Cream Multi-Active. Jojoba oil is also included in the ReAm Violetta line of moisturizing products. Botanical Buffing Beads from Peter Thomas Roth Labs combine whole-leaf aloe vera with jojoba beads. Shampoos and conditioners comprise the majority of products containing jojoba oil as the primary active ingredient, but the oil is often included among other ingredients in topical skin creams, lotions, and soaps. Olive Oil and Vitamin A Skin Reinforcing Complex from Macrovita includes jojoba oil. Everon Lip Balm from Weleda utilizes jojoba oil for lip protection.
Conclusion
Currently, jojoba oil is used primarily to confer anti-inflammatory benefits to cosmetics and cosmeceuticals. One of the primary challenges in formulating cosmeceutical products from jojoba and other botanicals is to retain the intrinsic benefits of the raw botanical or its extract. Development of jojoba-containing formulations may continue because of the commercial preference for ingredients with known traditional uses that do not require regulatory proof of efficacy.
The versatile botanical extract jojoba oil has not been shown to be harmful or to elicit significant adverse effects. At the very least, then, its presence in over-the-counter products is innocuous. There is a small but growing body of evidence to suggest that the inclusion of jojoba oil in topical formulations does impart salient anti-inflammatory effects. Much research, in the form of blinded, placebo-controlled clinical trials, is needed to compare jojoba-containing products with other formulations established as effective anti-inflammatories.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin and Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann at [email protected].
The jojoba (pronounced ho-ho-ba) plant (Buxus chinensis or Simmondsia chinensis) is a shrub endemic to the Sonoran Desert of northwest Mexico and adjacent areas in Arizona and southern California. This evergreen plant, also known as goat nut or coffeeberry, grows up to 15 feet high and can live for up to 200 years. Clearly, it is well adapted to thrive in the arid heat of the desert. Native Americans are known to have eaten the smooth-skinned, odorless, oil-rich nuts or seeds of the jojoba.
It is the oil of this shrub that is of keen interest as a botanical product for use in cosmetics and cosmeceuticals. The oil from jojoba nuts or seeds has been used for centuries to promote hair growth and alleviate skin conditions. Jojoba is now cultivated for commercial purposes, such as treatment for psoriasis, dry skin, and dandruff, in Argentina, Australia, Mexico, Israel, and India.
Jojoba oil is derived from the cold-pressed seeds, which are the size of peanuts or small olives (Phytother. Res. 2003;17:987-1000). It is actually a polyunsaturated liquid wax. This rich extract is typically used as a humectant in cosmetics and cosmeceuticals and confers a protective film over the skin that aids in moisture retention (Cosmet. Toiletries 1997;112:47-64). The skin’s natural sebum is readily compatible with the wide range of fatty acids (oleic, linoleic, linolenic, and arachidonic) and triglycerides that are key components of jojoba oil (J. Am. Oil Chem. Soc. 2000;77:1325-9; J. Agric. Food Chem. 1997;45:1180-4).
Some authors speculate that its efficacy as a nongreasy lubricant gives the oil, pure or in hydrogenated form, the potential for use in a variety of formulations that are designed for the skin or hair – creams, lotions, soaps, and lipsticks (J. Cosm. Sci. 1998;49:377-83). Jojoba oil has been found to impart significant beneficial properties as an analgesic, antibacterial, anti-inflammatory, antioxidant, antiparasitic, and antipyretic (Phytother. Res. 2003;17:987-1000; J. Cosm. Sci. 1998;49:377-83).
Very similar in consistency to human sebum, jojoba oil is considered to be a natural moisturizer and is thought to be highly conditioning, softening, and healing for all skin types. Although primarily used in skin and hair products now, jojoba oil first gained industry interest and support not for its reputed traditional benefits, but for its viability as a replacement for sperm whale oil, the use of which was banned by the U.S. government in the early 1970s as a result of the Endangered Species Act.
Products
Aubrey Organics (a company that uses botanicals organically grown and processed in accordance with the California Organic Foods Act of 1990) offers two hair products containing jojoba oil. Its J.A.Y. (Jojoba/Aloe/Yucca) Desert Herb Shampoo and Jojoba & Aloe Hair Rejuvenator & Conditioner are said to hydrate and revitalize especially dry and brittle hair. According to the manufacturer, the humectant activity of jojoba oil generates a protective film over the hair and scalp that helps retain moisture. The Swiss company Colos? Beauty also produces a wide array of formulations that contain jojoba oil for the purpose of protecting against dehydration. Colos?’s product line includes Day Cream Sensitive, Day Cream Multi-Active, Cream Egalisante, Miracle Cream, and Night Cream Multi-Active. Jojoba oil is also included in the ReAm Violetta line of moisturizing products. Botanical Buffing Beads from Peter Thomas Roth Labs combine whole-leaf aloe vera with jojoba beads. Shampoos and conditioners comprise the majority of products containing jojoba oil as the primary active ingredient, but the oil is often included among other ingredients in topical skin creams, lotions, and soaps. Olive Oil and Vitamin A Skin Reinforcing Complex from Macrovita includes jojoba oil. Everon Lip Balm from Weleda utilizes jojoba oil for lip protection.
Conclusion
Currently, jojoba oil is used primarily to confer anti-inflammatory benefits to cosmetics and cosmeceuticals. One of the primary challenges in formulating cosmeceutical products from jojoba and other botanicals is to retain the intrinsic benefits of the raw botanical or its extract. Development of jojoba-containing formulations may continue because of the commercial preference for ingredients with known traditional uses that do not require regulatory proof of efficacy.
The versatile botanical extract jojoba oil has not been shown to be harmful or to elicit significant adverse effects. At the very least, then, its presence in over-the-counter products is innocuous. There is a small but growing body of evidence to suggest that the inclusion of jojoba oil in topical formulations does impart salient anti-inflammatory effects. Much research, in the form of blinded, placebo-controlled clinical trials, is needed to compare jojoba-containing products with other formulations established as effective anti-inflammatories.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin and Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann at [email protected].
The jojoba (pronounced ho-ho-ba) plant (Buxus chinensis or Simmondsia chinensis) is a shrub endemic to the Sonoran Desert of northwest Mexico and adjacent areas in Arizona and southern California. This evergreen plant, also known as goat nut or coffeeberry, grows up to 15 feet high and can live for up to 200 years. Clearly, it is well adapted to thrive in the arid heat of the desert. Native Americans are known to have eaten the smooth-skinned, odorless, oil-rich nuts or seeds of the jojoba.
It is the oil of this shrub that is of keen interest as a botanical product for use in cosmetics and cosmeceuticals. The oil from jojoba nuts or seeds has been used for centuries to promote hair growth and alleviate skin conditions. Jojoba is now cultivated for commercial purposes, such as treatment for psoriasis, dry skin, and dandruff, in Argentina, Australia, Mexico, Israel, and India.
Jojoba oil is derived from the cold-pressed seeds, which are the size of peanuts or small olives (Phytother. Res. 2003;17:987-1000). It is actually a polyunsaturated liquid wax. This rich extract is typically used as a humectant in cosmetics and cosmeceuticals and confers a protective film over the skin that aids in moisture retention (Cosmet. Toiletries 1997;112:47-64). The skin’s natural sebum is readily compatible with the wide range of fatty acids (oleic, linoleic, linolenic, and arachidonic) and triglycerides that are key components of jojoba oil (J. Am. Oil Chem. Soc. 2000;77:1325-9; J. Agric. Food Chem. 1997;45:1180-4).
Some authors speculate that its efficacy as a nongreasy lubricant gives the oil, pure or in hydrogenated form, the potential for use in a variety of formulations that are designed for the skin or hair – creams, lotions, soaps, and lipsticks (J. Cosm. Sci. 1998;49:377-83). Jojoba oil has been found to impart significant beneficial properties as an analgesic, antibacterial, anti-inflammatory, antioxidant, antiparasitic, and antipyretic (Phytother. Res. 2003;17:987-1000; J. Cosm. Sci. 1998;49:377-83).
Very similar in consistency to human sebum, jojoba oil is considered to be a natural moisturizer and is thought to be highly conditioning, softening, and healing for all skin types. Although primarily used in skin and hair products now, jojoba oil first gained industry interest and support not for its reputed traditional benefits, but for its viability as a replacement for sperm whale oil, the use of which was banned by the U.S. government in the early 1970s as a result of the Endangered Species Act.
Products
Aubrey Organics (a company that uses botanicals organically grown and processed in accordance with the California Organic Foods Act of 1990) offers two hair products containing jojoba oil. Its J.A.Y. (Jojoba/Aloe/Yucca) Desert Herb Shampoo and Jojoba & Aloe Hair Rejuvenator & Conditioner are said to hydrate and revitalize especially dry and brittle hair. According to the manufacturer, the humectant activity of jojoba oil generates a protective film over the hair and scalp that helps retain moisture. The Swiss company Colos? Beauty also produces a wide array of formulations that contain jojoba oil for the purpose of protecting against dehydration. Colos?’s product line includes Day Cream Sensitive, Day Cream Multi-Active, Cream Egalisante, Miracle Cream, and Night Cream Multi-Active. Jojoba oil is also included in the ReAm Violetta line of moisturizing products. Botanical Buffing Beads from Peter Thomas Roth Labs combine whole-leaf aloe vera with jojoba beads. Shampoos and conditioners comprise the majority of products containing jojoba oil as the primary active ingredient, but the oil is often included among other ingredients in topical skin creams, lotions, and soaps. Olive Oil and Vitamin A Skin Reinforcing Complex from Macrovita includes jojoba oil. Everon Lip Balm from Weleda utilizes jojoba oil for lip protection.
Conclusion
Currently, jojoba oil is used primarily to confer anti-inflammatory benefits to cosmetics and cosmeceuticals. One of the primary challenges in formulating cosmeceutical products from jojoba and other botanicals is to retain the intrinsic benefits of the raw botanical or its extract. Development of jojoba-containing formulations may continue because of the commercial preference for ingredients with known traditional uses that do not require regulatory proof of efficacy.
The versatile botanical extract jojoba oil has not been shown to be harmful or to elicit significant adverse effects. At the very least, then, its presence in over-the-counter products is innocuous. There is a small but growing body of evidence to suggest that the inclusion of jojoba oil in topical formulations does impart salient anti-inflammatory effects. Much research, in the form of blinded, placebo-controlled clinical trials, is needed to compare jojoba-containing products with other formulations established as effective anti-inflammatories.
Dr. Baumann writes the column “Cosmeceutical Critique,” which regularly appears in Skin and Allergy News, an Elsevier publication. Dr. Baumann is in private practice in Miami Beach. To respond to this column, or to suggest topics for future columns, e-mail Dr. Baumann at [email protected].
The Antiaging Potential of Electric Stimulation
Dermatologists have known for years that collagen, hyaluronic acid, and elastin decline in concentration with advancing age. Many products have been convincingly shown to increase synthesis of collagen, such as retinoids, vitamin C, and glycolic acid.
However, elastin production is more elusive. Elastin is of particular interest because its loss is responsible for the sagging of the skin with aging, and it also may play a role in the formation of stretch marks. Although I have been unable to find an original reference proving this, many people say that elastin production ceases after puberty. Obviously, increasing collagen and elastin production would be beneficial to the skin's appearance.
Collagen and elastin are made by fibroblasts. These cells play a vital role in wound healing, as they deliver extracellular matrix components that facilitate the migration of other cell types to the wound site (Exp. Dermatol. 2003;12:396-402). This column will briefly discuss some of the research and concepts pertaining to electric stimulation of fibroblasts as a way of promoting the synthesis of collagen and elastin. In fact, the existence and importance of bioelectricity in the human body have been acknowledged for years in relation to wound healing, insofar as electric fields were measured at the sites of human dermal wounds more than 150 years ago, and modern techniques have verified the existence of endogenous electric fields in wounds (Methods Mol. Biol. 2009;571:77-97).
History
Although German physiologist Emil DuBois-Reymond is credited as being the first to identify endogenous electric fields in wounds (based on his paper in 1843 [Ann. Phys. u. Chem. 1843;58:1-30] and his book in 1860 [DuBois-Reymond E. "Untersuchungen uber Thierische Elektricitat, Zweiter Band, Zweite Abtheilung" (Erste Lieferung) Berlin: Georg Reimer; 1860]) and as a founder of modern electrophysiology, several others made key discoveries along the way.
According to a review of bioelectricity by McCaig et al., in the 1700s Italian physician Luigi Galvani, whose surname is the basis for the word "galvanism," witnessed the bioelectric response while dissecting a frog and performing various related experiments (Physiol. Rev. 2005;85:943-78). He termed the phenomenon "animal electricity."
Notably, Italian physicist Alessandro Volta studied the phenomenon and applied its principles to develop the first battery in 1800. Later, in 1831, Italian physicist and neurophysiologist Carlo Matteucci built on Galvani's work by using a galvanometer (named for Galvani, of course) to measure the injury potential of damaged frog muscle (Physiol. Rev. 2005;85:943-78). In the process, Matteucci became the first to demonstrate the action potential in nerves and muscle. DuBois-Reymond subsequently used these findings as the foundation for his considerable contributions revealing injury currents in the skin.
Given the discovery of the formation of an electrical gradient on the skin, its transmission to neighboring cells might be said to make intuitive sense, given how close cells are in relation to one another.
Wound Healing
Contemporary studies continue to shed light on the role of bioelectricity in cutaneous health. Some recent studies also appear to offer potential implications for antiaging therapies.
In 1997, a review by Beech indicated that the migration of cells into wound sites and the stimulation of quiescent cells at the wound margins can be fostered by exogenous, extremely low frequency fields positioned close to the target site, as well as endogenous tissues with enough zeta potential (Bioelectromagnetics 1997;18:341-8).
In 2009, Zhao concluded that electric fields of physiological strength play an overriding role in directing cell migration during epithelial wound healing (Semin. Cell Dev. Biol. 2009;20:674-82). In 2006, Zhao et al. demonstrated experimentally that electric fields, equal in strength to endogenous ones, direct the migration of inflammatory cells, fibroblasts, and epithelial cells in wound healing as the predominant directional signal. In their experiment, the investigators determined that the tumor suppressor phosphatase and tensin homolog (PTEN) and phosphatidylinositol-3-OH kinase-gamma control electrotaxis. They also identified the first genes that influence cellular movement and are necessary for wound healing prompted by electrical signaling (Nature 2006;442:457-60).
More recently, some of the same investigators, including Zhao and McCaig, noted the inherent vectoral nature of electric fields, and again investigated galvanotaxis/electrotaxis or directional cell migration in wound healing. They established several experimental systems, and found that electric fields of potency equal to those identified at in vivo wounds direct cell migration and supersede other guidance cues (e.g., contact inhibition). They concluded that endogenous electric fields may represent significant signaling mechanisms for guiding cellular movement and migration in vivo, and that exogenously applied electric fields may play a clinical role in guiding cell migration in wound healing, with greater versatility than other guidance cues (such as chemical ones) (Methods Mol. Biol. 2009;571:77-97).
In this context, cutaneous wounds are thought to heal as a result of the bioelectrically stimulated dispersal of positively charged ions and proteins to the wound site. Thus, it is believed that exogenously provoking this process that guides physiological activity at the cellular level can hasten wound healing by facilitating the transportation of repairing cells to the wound (Nature 2006;442:457-60).
The review article by McCaig et al., cited above, details the cellular mechanisms responsible for the effects of small electric fields on cell behavior, and considers the clinical potential for electric field treatment of damaged tissues, including epithelia (Physiol. Rev. 2005;85:943-78). The use of a 10-mV charge is key in the development of new products.
Acupuncture
Interestingly, the principles underlying these new products are at least tangentially related to the practice, though not the philosophy, of acupuncture in achieving facial rejuvenation. Traditional Chinese medicine has been shown to be effective for such a purpose. Acupuncture needles are inserted along particular meridians to tonify the skin. Such treatments have ameliorated some wrinkles, improved facial muscle tone, and produced better skin texture while reducing facial edema, acne, and sagging in different locations (Aesthet. Surg. J. 2005;25:419-24).
In traditional Chinese medicine, needle insertion along various meridians is believed to move or rebalance Qi (pronounced "chee"), the life force. The question of what Qi is, remains open to debate, says licensed acupuncturist Lynn Bondi, LAc. "Qi could very well coincide with or even be tantamount to bioelectric fields. But I'm more inclined to think that modern scientific measurement techniques are tapping into or quantifying some portion of Qi, which encompasses much more" (personal communication, Jan. 5, 2010). She notes, interestingly, that modern acupuncturist practice sometimes includes the use of microcurrents for facial rejuvenation.
New Products
Products poised to enter the market soon will be touted for their capacity to harness electrical currents to stimulate fibroblasts into synthesizing collagen and elastin. Several products from Johnson & Johnson - Aveeno, RoC, and Neutrogena - contain zinc and copper in a grayish cream that is applied to the skin. Zinc and copper exchange an electron, purportedly generating a 10-mV charge, which, as stated above, is believed to stimulate fibroblasts into producing collagen and elastin. Application of the grayish cream is followed by use of a moisturizer. The water in the moisturizer in turn activates the "zinc-copper battery," thus creating the charge, which the patient cannot feel. Studies have shown increased elasticity of the skin (as shown by cutometer measurements) when this "zinc-copper battery" is used in combination with a moisturizer containing ingredients that have been shown to increase elastin production and assembly.
The process of stimulating functional elastin production is more complicated than stimulating collagen production. In the body, collagen is extracted from fibroblasts in a complete and final triple-helix form. No further change in structure is necessary for the collagen to be functional. Elastin, however, is secreted by fibroblasts as tropoelastin, which consists of unbound units of elastin in an immature form. Elastin must assemble on a microfibrillin backbone in order to be functional.
According to unpublished proprietary data, one of the new Aveeno products contains blackberry, which stimulates fibroblasts to produce tropoelastin, and dill, which has been shown to aid in assembling the tropoelastin "building blocks" onto a microfibrillin backbone to yield mature elastin. Aveeno has sponsored a study in which cutometer measurements showed increased skin elasticity after use of its Ageless Vitality product for 8-12 weeks.
In essence, the theory behind these new products is that the topical delivery of energized zinc and copper stimulates cutaneous electrical cues that coax the fibroblast to produce collagen and elastin. This process may lead to dermal changes that rejuvenate the skin.
Conclusions
I have not been involved in any of the trials of these products and have no firsthand knowledge of these studies. Conceptually, I am intrigued with the idea of an electromimetic current being used to stimulate fibroblasts. I have reviewed the wound healing literature, and the scientific concepts and data make sense.
The notion of harnessing the natural electric currents of skin cells to increase collagen and elastin production is fascinating for several reasons, not the least of which is elimination of the issue of penetration of active ingredients. A charge generated on the cells in the top layer will likely propagate to neighboring cells, eliminating the need for actual penetration of the zinc and copper.
Consequently, an enhancement of cell-to-cell communication would seem likely to extend to the lower layers, allowing the cells deeper in the dermis to "get the message." These products launch in March, and it will be interesting to see how they are received by dermatologists and consumers.
Dermatologists have known for years that collagen, hyaluronic acid, and elastin decline in concentration with advancing age. Many products have been convincingly shown to increase synthesis of collagen, such as retinoids, vitamin C, and glycolic acid.
However, elastin production is more elusive. Elastin is of particular interest because its loss is responsible for the sagging of the skin with aging, and it also may play a role in the formation of stretch marks. Although I have been unable to find an original reference proving this, many people say that elastin production ceases after puberty. Obviously, increasing collagen and elastin production would be beneficial to the skin's appearance.
Collagen and elastin are made by fibroblasts. These cells play a vital role in wound healing, as they deliver extracellular matrix components that facilitate the migration of other cell types to the wound site (Exp. Dermatol. 2003;12:396-402). This column will briefly discuss some of the research and concepts pertaining to electric stimulation of fibroblasts as a way of promoting the synthesis of collagen and elastin. In fact, the existence and importance of bioelectricity in the human body have been acknowledged for years in relation to wound healing, insofar as electric fields were measured at the sites of human dermal wounds more than 150 years ago, and modern techniques have verified the existence of endogenous electric fields in wounds (Methods Mol. Biol. 2009;571:77-97).
History
Although German physiologist Emil DuBois-Reymond is credited as being the first to identify endogenous electric fields in wounds (based on his paper in 1843 [Ann. Phys. u. Chem. 1843;58:1-30] and his book in 1860 [DuBois-Reymond E. "Untersuchungen uber Thierische Elektricitat, Zweiter Band, Zweite Abtheilung" (Erste Lieferung) Berlin: Georg Reimer; 1860]) and as a founder of modern electrophysiology, several others made key discoveries along the way.
According to a review of bioelectricity by McCaig et al., in the 1700s Italian physician Luigi Galvani, whose surname is the basis for the word "galvanism," witnessed the bioelectric response while dissecting a frog and performing various related experiments (Physiol. Rev. 2005;85:943-78). He termed the phenomenon "animal electricity."
Notably, Italian physicist Alessandro Volta studied the phenomenon and applied its principles to develop the first battery in 1800. Later, in 1831, Italian physicist and neurophysiologist Carlo Matteucci built on Galvani's work by using a galvanometer (named for Galvani, of course) to measure the injury potential of damaged frog muscle (Physiol. Rev. 2005;85:943-78). In the process, Matteucci became the first to demonstrate the action potential in nerves and muscle. DuBois-Reymond subsequently used these findings as the foundation for his considerable contributions revealing injury currents in the skin.
Given the discovery of the formation of an electrical gradient on the skin, its transmission to neighboring cells might be said to make intuitive sense, given how close cells are in relation to one another.
Wound Healing
Contemporary studies continue to shed light on the role of bioelectricity in cutaneous health. Some recent studies also appear to offer potential implications for antiaging therapies.
In 1997, a review by Beech indicated that the migration of cells into wound sites and the stimulation of quiescent cells at the wound margins can be fostered by exogenous, extremely low frequency fields positioned close to the target site, as well as endogenous tissues with enough zeta potential (Bioelectromagnetics 1997;18:341-8).
In 2009, Zhao concluded that electric fields of physiological strength play an overriding role in directing cell migration during epithelial wound healing (Semin. Cell Dev. Biol. 2009;20:674-82). In 2006, Zhao et al. demonstrated experimentally that electric fields, equal in strength to endogenous ones, direct the migration of inflammatory cells, fibroblasts, and epithelial cells in wound healing as the predominant directional signal. In their experiment, the investigators determined that the tumor suppressor phosphatase and tensin homolog (PTEN) and phosphatidylinositol-3-OH kinase-gamma control electrotaxis. They also identified the first genes that influence cellular movement and are necessary for wound healing prompted by electrical signaling (Nature 2006;442:457-60).
More recently, some of the same investigators, including Zhao and McCaig, noted the inherent vectoral nature of electric fields, and again investigated galvanotaxis/electrotaxis or directional cell migration in wound healing. They established several experimental systems, and found that electric fields of potency equal to those identified at in vivo wounds direct cell migration and supersede other guidance cues (e.g., contact inhibition). They concluded that endogenous electric fields may represent significant signaling mechanisms for guiding cellular movement and migration in vivo, and that exogenously applied electric fields may play a clinical role in guiding cell migration in wound healing, with greater versatility than other guidance cues (such as chemical ones) (Methods Mol. Biol. 2009;571:77-97).
In this context, cutaneous wounds are thought to heal as a result of the bioelectrically stimulated dispersal of positively charged ions and proteins to the wound site. Thus, it is believed that exogenously provoking this process that guides physiological activity at the cellular level can hasten wound healing by facilitating the transportation of repairing cells to the wound (Nature 2006;442:457-60).
The review article by McCaig et al., cited above, details the cellular mechanisms responsible for the effects of small electric fields on cell behavior, and considers the clinical potential for electric field treatment of damaged tissues, including epithelia (Physiol. Rev. 2005;85:943-78). The use of a 10-mV charge is key in the development of new products.
Acupuncture
Interestingly, the principles underlying these new products are at least tangentially related to the practice, though not the philosophy, of acupuncture in achieving facial rejuvenation. Traditional Chinese medicine has been shown to be effective for such a purpose. Acupuncture needles are inserted along particular meridians to tonify the skin. Such treatments have ameliorated some wrinkles, improved facial muscle tone, and produced better skin texture while reducing facial edema, acne, and sagging in different locations (Aesthet. Surg. J. 2005;25:419-24).
In traditional Chinese medicine, needle insertion along various meridians is believed to move or rebalance Qi (pronounced "chee"), the life force. The question of what Qi is, remains open to debate, says licensed acupuncturist Lynn Bondi, LAc. "Qi could very well coincide with or even be tantamount to bioelectric fields. But I'm more inclined to think that modern scientific measurement techniques are tapping into or quantifying some portion of Qi, which encompasses much more" (personal communication, Jan. 5, 2010). She notes, interestingly, that modern acupuncturist practice sometimes includes the use of microcurrents for facial rejuvenation.
New Products
Products poised to enter the market soon will be touted for their capacity to harness electrical currents to stimulate fibroblasts into synthesizing collagen and elastin. Several products from Johnson & Johnson - Aveeno, RoC, and Neutrogena - contain zinc and copper in a grayish cream that is applied to the skin. Zinc and copper exchange an electron, purportedly generating a 10-mV charge, which, as stated above, is believed to stimulate fibroblasts into producing collagen and elastin. Application of the grayish cream is followed by use of a moisturizer. The water in the moisturizer in turn activates the "zinc-copper battery," thus creating the charge, which the patient cannot feel. Studies have shown increased elasticity of the skin (as shown by cutometer measurements) when this "zinc-copper battery" is used in combination with a moisturizer containing ingredients that have been shown to increase elastin production and assembly.
The process of stimulating functional elastin production is more complicated than stimulating collagen production. In the body, collagen is extracted from fibroblasts in a complete and final triple-helix form. No further change in structure is necessary for the collagen to be functional. Elastin, however, is secreted by fibroblasts as tropoelastin, which consists of unbound units of elastin in an immature form. Elastin must assemble on a microfibrillin backbone in order to be functional.
According to unpublished proprietary data, one of the new Aveeno products contains blackberry, which stimulates fibroblasts to produce tropoelastin, and dill, which has been shown to aid in assembling the tropoelastin "building blocks" onto a microfibrillin backbone to yield mature elastin. Aveeno has sponsored a study in which cutometer measurements showed increased skin elasticity after use of its Ageless Vitality product for 8-12 weeks.
In essence, the theory behind these new products is that the topical delivery of energized zinc and copper stimulates cutaneous electrical cues that coax the fibroblast to produce collagen and elastin. This process may lead to dermal changes that rejuvenate the skin.
Conclusions
I have not been involved in any of the trials of these products and have no firsthand knowledge of these studies. Conceptually, I am intrigued with the idea of an electromimetic current being used to stimulate fibroblasts. I have reviewed the wound healing literature, and the scientific concepts and data make sense.
The notion of harnessing the natural electric currents of skin cells to increase collagen and elastin production is fascinating for several reasons, not the least of which is elimination of the issue of penetration of active ingredients. A charge generated on the cells in the top layer will likely propagate to neighboring cells, eliminating the need for actual penetration of the zinc and copper.
Consequently, an enhancement of cell-to-cell communication would seem likely to extend to the lower layers, allowing the cells deeper in the dermis to "get the message." These products launch in March, and it will be interesting to see how they are received by dermatologists and consumers.
Dermatologists have known for years that collagen, hyaluronic acid, and elastin decline in concentration with advancing age. Many products have been convincingly shown to increase synthesis of collagen, such as retinoids, vitamin C, and glycolic acid.
However, elastin production is more elusive. Elastin is of particular interest because its loss is responsible for the sagging of the skin with aging, and it also may play a role in the formation of stretch marks. Although I have been unable to find an original reference proving this, many people say that elastin production ceases after puberty. Obviously, increasing collagen and elastin production would be beneficial to the skin's appearance.
Collagen and elastin are made by fibroblasts. These cells play a vital role in wound healing, as they deliver extracellular matrix components that facilitate the migration of other cell types to the wound site (Exp. Dermatol. 2003;12:396-402). This column will briefly discuss some of the research and concepts pertaining to electric stimulation of fibroblasts as a way of promoting the synthesis of collagen and elastin. In fact, the existence and importance of bioelectricity in the human body have been acknowledged for years in relation to wound healing, insofar as electric fields were measured at the sites of human dermal wounds more than 150 years ago, and modern techniques have verified the existence of endogenous electric fields in wounds (Methods Mol. Biol. 2009;571:77-97).
History
Although German physiologist Emil DuBois-Reymond is credited as being the first to identify endogenous electric fields in wounds (based on his paper in 1843 [Ann. Phys. u. Chem. 1843;58:1-30] and his book in 1860 [DuBois-Reymond E. "Untersuchungen uber Thierische Elektricitat, Zweiter Band, Zweite Abtheilung" (Erste Lieferung) Berlin: Georg Reimer; 1860]) and as a founder of modern electrophysiology, several others made key discoveries along the way.
According to a review of bioelectricity by McCaig et al., in the 1700s Italian physician Luigi Galvani, whose surname is the basis for the word "galvanism," witnessed the bioelectric response while dissecting a frog and performing various related experiments (Physiol. Rev. 2005;85:943-78). He termed the phenomenon "animal electricity."
Notably, Italian physicist Alessandro Volta studied the phenomenon and applied its principles to develop the first battery in 1800. Later, in 1831, Italian physicist and neurophysiologist Carlo Matteucci built on Galvani's work by using a galvanometer (named for Galvani, of course) to measure the injury potential of damaged frog muscle (Physiol. Rev. 2005;85:943-78). In the process, Matteucci became the first to demonstrate the action potential in nerves and muscle. DuBois-Reymond subsequently used these findings as the foundation for his considerable contributions revealing injury currents in the skin.
Given the discovery of the formation of an electrical gradient on the skin, its transmission to neighboring cells might be said to make intuitive sense, given how close cells are in relation to one another.
Wound Healing
Contemporary studies continue to shed light on the role of bioelectricity in cutaneous health. Some recent studies also appear to offer potential implications for antiaging therapies.
In 1997, a review by Beech indicated that the migration of cells into wound sites and the stimulation of quiescent cells at the wound margins can be fostered by exogenous, extremely low frequency fields positioned close to the target site, as well as endogenous tissues with enough zeta potential (Bioelectromagnetics 1997;18:341-8).
In 2009, Zhao concluded that electric fields of physiological strength play an overriding role in directing cell migration during epithelial wound healing (Semin. Cell Dev. Biol. 2009;20:674-82). In 2006, Zhao et al. demonstrated experimentally that electric fields, equal in strength to endogenous ones, direct the migration of inflammatory cells, fibroblasts, and epithelial cells in wound healing as the predominant directional signal. In their experiment, the investigators determined that the tumor suppressor phosphatase and tensin homolog (PTEN) and phosphatidylinositol-3-OH kinase-gamma control electrotaxis. They also identified the first genes that influence cellular movement and are necessary for wound healing prompted by electrical signaling (Nature 2006;442:457-60).
More recently, some of the same investigators, including Zhao and McCaig, noted the inherent vectoral nature of electric fields, and again investigated galvanotaxis/electrotaxis or directional cell migration in wound healing. They established several experimental systems, and found that electric fields of potency equal to those identified at in vivo wounds direct cell migration and supersede other guidance cues (e.g., contact inhibition). They concluded that endogenous electric fields may represent significant signaling mechanisms for guiding cellular movement and migration in vivo, and that exogenously applied electric fields may play a clinical role in guiding cell migration in wound healing, with greater versatility than other guidance cues (such as chemical ones) (Methods Mol. Biol. 2009;571:77-97).
In this context, cutaneous wounds are thought to heal as a result of the bioelectrically stimulated dispersal of positively charged ions and proteins to the wound site. Thus, it is believed that exogenously provoking this process that guides physiological activity at the cellular level can hasten wound healing by facilitating the transportation of repairing cells to the wound (Nature 2006;442:457-60).
The review article by McCaig et al., cited above, details the cellular mechanisms responsible for the effects of small electric fields on cell behavior, and considers the clinical potential for electric field treatment of damaged tissues, including epithelia (Physiol. Rev. 2005;85:943-78). The use of a 10-mV charge is key in the development of new products.
Acupuncture
Interestingly, the principles underlying these new products are at least tangentially related to the practice, though not the philosophy, of acupuncture in achieving facial rejuvenation. Traditional Chinese medicine has been shown to be effective for such a purpose. Acupuncture needles are inserted along particular meridians to tonify the skin. Such treatments have ameliorated some wrinkles, improved facial muscle tone, and produced better skin texture while reducing facial edema, acne, and sagging in different locations (Aesthet. Surg. J. 2005;25:419-24).
In traditional Chinese medicine, needle insertion along various meridians is believed to move or rebalance Qi (pronounced "chee"), the life force. The question of what Qi is, remains open to debate, says licensed acupuncturist Lynn Bondi, LAc. "Qi could very well coincide with or even be tantamount to bioelectric fields. But I'm more inclined to think that modern scientific measurement techniques are tapping into or quantifying some portion of Qi, which encompasses much more" (personal communication, Jan. 5, 2010). She notes, interestingly, that modern acupuncturist practice sometimes includes the use of microcurrents for facial rejuvenation.
New Products
Products poised to enter the market soon will be touted for their capacity to harness electrical currents to stimulate fibroblasts into synthesizing collagen and elastin. Several products from Johnson & Johnson - Aveeno, RoC, and Neutrogena - contain zinc and copper in a grayish cream that is applied to the skin. Zinc and copper exchange an electron, purportedly generating a 10-mV charge, which, as stated above, is believed to stimulate fibroblasts into producing collagen and elastin. Application of the grayish cream is followed by use of a moisturizer. The water in the moisturizer in turn activates the "zinc-copper battery," thus creating the charge, which the patient cannot feel. Studies have shown increased elasticity of the skin (as shown by cutometer measurements) when this "zinc-copper battery" is used in combination with a moisturizer containing ingredients that have been shown to increase elastin production and assembly.
The process of stimulating functional elastin production is more complicated than stimulating collagen production. In the body, collagen is extracted from fibroblasts in a complete and final triple-helix form. No further change in structure is necessary for the collagen to be functional. Elastin, however, is secreted by fibroblasts as tropoelastin, which consists of unbound units of elastin in an immature form. Elastin must assemble on a microfibrillin backbone in order to be functional.
According to unpublished proprietary data, one of the new Aveeno products contains blackberry, which stimulates fibroblasts to produce tropoelastin, and dill, which has been shown to aid in assembling the tropoelastin "building blocks" onto a microfibrillin backbone to yield mature elastin. Aveeno has sponsored a study in which cutometer measurements showed increased skin elasticity after use of its Ageless Vitality product for 8-12 weeks.
In essence, the theory behind these new products is that the topical delivery of energized zinc and copper stimulates cutaneous electrical cues that coax the fibroblast to produce collagen and elastin. This process may lead to dermal changes that rejuvenate the skin.
Conclusions
I have not been involved in any of the trials of these products and have no firsthand knowledge of these studies. Conceptually, I am intrigued with the idea of an electromimetic current being used to stimulate fibroblasts. I have reviewed the wound healing literature, and the scientific concepts and data make sense.
The notion of harnessing the natural electric currents of skin cells to increase collagen and elastin production is fascinating for several reasons, not the least of which is elimination of the issue of penetration of active ingredients. A charge generated on the cells in the top layer will likely propagate to neighboring cells, eliminating the need for actual penetration of the zinc and copper.
Consequently, an enhancement of cell-to-cell communication would seem likely to extend to the lower layers, allowing the cells deeper in the dermis to "get the message." These products launch in March, and it will be interesting to see how they are received by dermatologists and consumers.
The Scoop on Sirtuins
Everyone in the skin care world is talking about sirtuins. Studies have shown that resveratrol activates sirtuins, and sales of resveratrol have risen. Many products claim to contain ingredients that activate sirtuins.
To be up to date on current skin care, you need to know what sirtuins are and why they are a frequent topic at the Society of Cosmetic Chemists meetings. The short explanation is that calorie-restricted mice have been shown to live longer and to have increased expression of sirtuins. It is believed that the upregulation of sirtuin expression is associated with increased longevity. When mice were not calorie restricted but were treated with resveratrol to activate sirtuins, they also lived longer.
The current belief that activating sirtuin is desirable has led to a plethora of products with sirtuin-activating ingredients, including several sold by Avon Products Inc.
Where Are Sirtuins Found?
Role of Sirtuins
Silent mating type information regulator 2 (Sir2) proteins, or sirtuins, are a family of nicotinamide adenine dinucleotide (NAD+)-dependent enzymes known to deacetylate lysine residues on several proteins and, in some cases, to exhibit adenosine diphosphate (ADP)-ribosyltransferase activity (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55). Sirtuins are activated when cellular energy is low and the NAD+ to NADH ratio is high (Genes Nutr. 2006;1:85-93).
This family of enzymes is known to be involved in apoptosis, fatty acid metabolism, gene silencing, and regulation of cellular lifespans. They are also linked to genes that organize and optimize cell functions to resist or survive in stressful environments (J. Drugs Dermatol. 2007;6:s14-9). Sirtuins regulate important biological pathways, such as transcriptional repression, recombination, the cell-division cycle, microtubule organization, and cellular responses to DNA-damaging compounds (Genome Biol. 2004;5:224).
It is believed that the mammalian sirtuins, SIRT1-SIRT7, play an influential role in gene silencing, energy homeostasis, the cell cycle, apoptosis, stress resistance or stress responses, axonal degeneration, and aging (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55; J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x ]). As such, Yamamoto et al. have contended that sirtuins may be appropriate therapeutic targets for a range of disorders, including proliferative, neurodegenerative, and metabolic diseases (Mol. Endocrinol. 2007;21:1745-55).
The Nomenclature
Sirtuin Research in Skin
For the active skin care product portion of the study, the researchers enrolled 33 women between 37 and 64 years old (mean age 51.6 years), who were instructed to apply a formulation enriched in 1% of the yeast biopeptides once daily for 4 weeks to the neck and face. Before and after the first application and after 4 weeks of use, investigating dermatologists assessed fine lines and wrinkles, pigment color intensity, complexion homogeneity, and radiance, as well as skin density, hydration, firmness, and texture on a 1-9 scale. To objectively evaluate skin care efficacy, they used a pixel skin method based on analyzing age-related parameters from numerical pictures of faces.
The investigators identified multiple findings from their study. In particular, the Kluyveromyces biopeptides markedly increased SIRT1 expression in normal human dermal fibroblasts in vitro as well as in healthy human epidermal cells ex vivo while diminishing cellular aging and UVB-induced DNA fragmentation. Among the study participants, improvements were found in all of the assessment parameters, with hydration noted as significantly improving right after the first application.
The authors concluded that the yeast Kluyveromyces biopeptides were efficacious in activating SIRT1 in human skin cells, resulting in the enhancement of DNA resistance and aging. In addition, a formulation featuring Kluyveromyces biopeptides exhibited efficacy in ameliorating various signs of cutaneous aging (J. Drugs Dermatol. 2007;6:s14-9).
In 2008, Cao et al. reported on the role of SIRT1 in UV signaling pathways. With cell culture and Western blot analysis, they found that SIRT1 is expressed in cultured human skin keratinocytes. The investigators observed that SIRT1 is time- and dose-dependently down-regulated by exposure to UV radiation and H2O2, with reactive oxygen species (ROS)-mediated JNK (c-Jun N-terminal kinase) activation involved in the down-regulation. Significantly, resveratrol, an activator of SIRT1, protected against UV- and H2O2-induced apoptosis; SIRT inhibitors such as sirtinol and nicotinamide promoted apoptosis.
The investigators also noted that resveratrol suppresses UV- and H2O2-induced p53 acetylation, while the SIRT inhibitors sirtinol and nicotinamide, as well as SIRT1 small interfering RNA (siRNA), foster it. Overall, the researchers suggested that their work adds to the understanding of the molecular mechanisms of photoaging, and that the SIRT1-activating property of resveratrol might be targeted in agents intended for therapeutic approaches to cutaneous aging (J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x]).
Also in 2008, Pallàs et al. found that increasing SIRT1 protects against amyloid beta-induced ROS synthesis and DNA damage, thus diminishing in vitro apoptosis. In addition, the overexpression of SIRT1, induced by caloric restriction or the use of the antioxidant resveratrol, has been shown to rescue Alzheimer's and Huntington's disease neurons (Recent Pat. CNS Drug Discov. 2008;3:61-9). SIRT1 and SIR2 had already been implicated as the proteins involved in lifespan extension from caloric restriction in various species.
Polyphenols such as quercetin and resveratrol are dietary antioxidants known to confer numerous health benefits and to activate sirtuins, thus playing a role in the caloric restriction longevity extension mechanism; their capacity to influence or extend lifespan has been shown in simple organisms but not consistently, as yet, in humans or other mammals (J. Cosmet. Dermatol. 2008;7:2-7; Genes Nutr. 2006;1:85-93).
However, work in mice (discussed in an episode of the television show "60 Minutes" in early 2009) performed by Sirtris Pharmaceuticals, a research company founded on recent discoveries related to sirtuins, demonstrated that resveratrol fed to mice on a high-fat diet improved insulin resistance, increased mitochondrial content, and prolonged life. In two groups of mice fed a high-fat diet, both groups wound up obese, but the mice administered resveratrol as part of their diet were able to run twice as far and fast, and survived 20% longer. In other studies by Sirtris, mice fed resveratrol as part of a high-fat diet gained less weight than mice administered a high-fat diet without resveratrol. Investigators at Sirtris also have identified small-molecule activators of SIRT1 that are 1,000 times as strong as resveratrol (Nature 2007;450:712-6).
Many other companies, such as Avon, have studied ingredients that upregulate sirtuin expression. By using human skin biopsies and immunohistochemical analysis, Avon has shown that its own proprietary botanical extracts promote the expression of dermal matrix proteins. The company claims that a 12-week clinical study using a product formulated to stimulate sirtuin expression displayed efficacy that warrants use in an antiaging product.
It remains to be seen what such claims - and products - will mean for the skin. For now, I would continue to recommend oral resveratrol and red wine supplements. In particular, I suggest OPC Synergy by Standard Process Inc., which contains grape seed and red wine extracts.
Conclusions
The family of proteins known as sirtuins appears to play an important role in the increased lifespan of various species, particularly, as recent research suggests, in calorie-restricted animals. The polyphenolic antioxidant resveratrol, which is abundant in red wine and is now included in some cosmeceutical agents, upregulates sirtuin expression and may protect cells from DNA damage.
The discovery of the role of sirtuin expression in slowing the pace of aging, in the experimental setting, strikes me as a very significant advance, and may lead to further elucidation of the aging process overall as well as cutaneous aging.
However, it is unknown at this time what role sirtuin and sirtuin activators play in skin care. Early data suggest that the activation of sirtuins may improve the appearance of skin, but the mechanism, if known, is unclear to me. The potential of Avon's botanically derived agent in upregulating sirtuin expression in skin cell cultures appears promising, because the company's study did reveal that patients experienced improvement in wrinkles. I was not the investigator in this study, so it is difficult to comment on the validity of the observations, as I am unsure of the exact study design.
I will be interested to see further work in this area, and it's always good to have a medically sound reason to drink wine.
Recently, investigators attempted to stimulate the expression of sirtuin, specifically SIRT1, in human skin cells in a culture of yeast Kluyveromyces biopetides, and to identify cutaneous benefits from an active skin care product containing such biopeptides. They also tested healthy skin samples ex vivo. Immunostaining, Western blotting, and cytometry were used to assess SIRT1 in culture and in ex vivo samples. Comet assays were used to evaluate cellular aging and integrity. Sir2 protein (Sir2p), present in yeast, is the founding member of the sirtuin family. SIRT1 was the first homolog found in humans and other mammals (Mol. Endocrinol. 2007;21:1745-55; Mol. Cell Biol. 2003;23:3173-85; Biochem. Biophys. Res. Commun. 2000;273:793-8). Now there are seven known mammalian sirtuins: SIRT1-SIRT7. Sirtuins are found in organisms ranging from bacteria to humans. Much sirtuin research has been done in the yeast Saccharomyces cerevisiae, the fruit fly Drosophila melanogaster, and the nematode Caenorhabditis elegans. In these organisms, sirtuins have been identified as molecules that mediate the effects of caloric restriction on aging processes (Genes Nutr. 2006;1:85-93).
Everyone in the skin care world is talking about sirtuins. Studies have shown that resveratrol activates sirtuins, and sales of resveratrol have risen. Many products claim to contain ingredients that activate sirtuins.
To be up to date on current skin care, you need to know what sirtuins are and why they are a frequent topic at the Society of Cosmetic Chemists meetings. The short explanation is that calorie-restricted mice have been shown to live longer and to have increased expression of sirtuins. It is believed that the upregulation of sirtuin expression is associated with increased longevity. When mice were not calorie restricted but were treated with resveratrol to activate sirtuins, they also lived longer.
The current belief that activating sirtuin is desirable has led to a plethora of products with sirtuin-activating ingredients, including several sold by Avon Products Inc.
Where Are Sirtuins Found?
Role of Sirtuins
Silent mating type information regulator 2 (Sir2) proteins, or sirtuins, are a family of nicotinamide adenine dinucleotide (NAD+)-dependent enzymes known to deacetylate lysine residues on several proteins and, in some cases, to exhibit adenosine diphosphate (ADP)-ribosyltransferase activity (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55). Sirtuins are activated when cellular energy is low and the NAD+ to NADH ratio is high (Genes Nutr. 2006;1:85-93).
This family of enzymes is known to be involved in apoptosis, fatty acid metabolism, gene silencing, and regulation of cellular lifespans. They are also linked to genes that organize and optimize cell functions to resist or survive in stressful environments (J. Drugs Dermatol. 2007;6:s14-9). Sirtuins regulate important biological pathways, such as transcriptional repression, recombination, the cell-division cycle, microtubule organization, and cellular responses to DNA-damaging compounds (Genome Biol. 2004;5:224).
It is believed that the mammalian sirtuins, SIRT1-SIRT7, play an influential role in gene silencing, energy homeostasis, the cell cycle, apoptosis, stress resistance or stress responses, axonal degeneration, and aging (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55; J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x ]). As such, Yamamoto et al. have contended that sirtuins may be appropriate therapeutic targets for a range of disorders, including proliferative, neurodegenerative, and metabolic diseases (Mol. Endocrinol. 2007;21:1745-55).
The Nomenclature
Sirtuin Research in Skin
For the active skin care product portion of the study, the researchers enrolled 33 women between 37 and 64 years old (mean age 51.6 years), who were instructed to apply a formulation enriched in 1% of the yeast biopeptides once daily for 4 weeks to the neck and face. Before and after the first application and after 4 weeks of use, investigating dermatologists assessed fine lines and wrinkles, pigment color intensity, complexion homogeneity, and radiance, as well as skin density, hydration, firmness, and texture on a 1-9 scale. To objectively evaluate skin care efficacy, they used a pixel skin method based on analyzing age-related parameters from numerical pictures of faces.
The investigators identified multiple findings from their study. In particular, the Kluyveromyces biopeptides markedly increased SIRT1 expression in normal human dermal fibroblasts in vitro as well as in healthy human epidermal cells ex vivo while diminishing cellular aging and UVB-induced DNA fragmentation. Among the study participants, improvements were found in all of the assessment parameters, with hydration noted as significantly improving right after the first application.
The authors concluded that the yeast Kluyveromyces biopeptides were efficacious in activating SIRT1 in human skin cells, resulting in the enhancement of DNA resistance and aging. In addition, a formulation featuring Kluyveromyces biopeptides exhibited efficacy in ameliorating various signs of cutaneous aging (J. Drugs Dermatol. 2007;6:s14-9).
In 2008, Cao et al. reported on the role of SIRT1 in UV signaling pathways. With cell culture and Western blot analysis, they found that SIRT1 is expressed in cultured human skin keratinocytes. The investigators observed that SIRT1 is time- and dose-dependently down-regulated by exposure to UV radiation and H2O2, with reactive oxygen species (ROS)-mediated JNK (c-Jun N-terminal kinase) activation involved in the down-regulation. Significantly, resveratrol, an activator of SIRT1, protected against UV- and H2O2-induced apoptosis; SIRT inhibitors such as sirtinol and nicotinamide promoted apoptosis.
The investigators also noted that resveratrol suppresses UV- and H2O2-induced p53 acetylation, while the SIRT inhibitors sirtinol and nicotinamide, as well as SIRT1 small interfering RNA (siRNA), foster it. Overall, the researchers suggested that their work adds to the understanding of the molecular mechanisms of photoaging, and that the SIRT1-activating property of resveratrol might be targeted in agents intended for therapeutic approaches to cutaneous aging (J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x]).
Also in 2008, Pallàs et al. found that increasing SIRT1 protects against amyloid beta-induced ROS synthesis and DNA damage, thus diminishing in vitro apoptosis. In addition, the overexpression of SIRT1, induced by caloric restriction or the use of the antioxidant resveratrol, has been shown to rescue Alzheimer's and Huntington's disease neurons (Recent Pat. CNS Drug Discov. 2008;3:61-9). SIRT1 and SIR2 had already been implicated as the proteins involved in lifespan extension from caloric restriction in various species.
Polyphenols such as quercetin and resveratrol are dietary antioxidants known to confer numerous health benefits and to activate sirtuins, thus playing a role in the caloric restriction longevity extension mechanism; their capacity to influence or extend lifespan has been shown in simple organisms but not consistently, as yet, in humans or other mammals (J. Cosmet. Dermatol. 2008;7:2-7; Genes Nutr. 2006;1:85-93).
However, work in mice (discussed in an episode of the television show "60 Minutes" in early 2009) performed by Sirtris Pharmaceuticals, a research company founded on recent discoveries related to sirtuins, demonstrated that resveratrol fed to mice on a high-fat diet improved insulin resistance, increased mitochondrial content, and prolonged life. In two groups of mice fed a high-fat diet, both groups wound up obese, but the mice administered resveratrol as part of their diet were able to run twice as far and fast, and survived 20% longer. In other studies by Sirtris, mice fed resveratrol as part of a high-fat diet gained less weight than mice administered a high-fat diet without resveratrol. Investigators at Sirtris also have identified small-molecule activators of SIRT1 that are 1,000 times as strong as resveratrol (Nature 2007;450:712-6).
Many other companies, such as Avon, have studied ingredients that upregulate sirtuin expression. By using human skin biopsies and immunohistochemical analysis, Avon has shown that its own proprietary botanical extracts promote the expression of dermal matrix proteins. The company claims that a 12-week clinical study using a product formulated to stimulate sirtuin expression displayed efficacy that warrants use in an antiaging product.
It remains to be seen what such claims - and products - will mean for the skin. For now, I would continue to recommend oral resveratrol and red wine supplements. In particular, I suggest OPC Synergy by Standard Process Inc., which contains grape seed and red wine extracts.
Conclusions
The family of proteins known as sirtuins appears to play an important role in the increased lifespan of various species, particularly, as recent research suggests, in calorie-restricted animals. The polyphenolic antioxidant resveratrol, which is abundant in red wine and is now included in some cosmeceutical agents, upregulates sirtuin expression and may protect cells from DNA damage.
The discovery of the role of sirtuin expression in slowing the pace of aging, in the experimental setting, strikes me as a very significant advance, and may lead to further elucidation of the aging process overall as well as cutaneous aging.
However, it is unknown at this time what role sirtuin and sirtuin activators play in skin care. Early data suggest that the activation of sirtuins may improve the appearance of skin, but the mechanism, if known, is unclear to me. The potential of Avon's botanically derived agent in upregulating sirtuin expression in skin cell cultures appears promising, because the company's study did reveal that patients experienced improvement in wrinkles. I was not the investigator in this study, so it is difficult to comment on the validity of the observations, as I am unsure of the exact study design.
I will be interested to see further work in this area, and it's always good to have a medically sound reason to drink wine.
Recently, investigators attempted to stimulate the expression of sirtuin, specifically SIRT1, in human skin cells in a culture of yeast Kluyveromyces biopetides, and to identify cutaneous benefits from an active skin care product containing such biopeptides. They also tested healthy skin samples ex vivo. Immunostaining, Western blotting, and cytometry were used to assess SIRT1 in culture and in ex vivo samples. Comet assays were used to evaluate cellular aging and integrity. Sir2 protein (Sir2p), present in yeast, is the founding member of the sirtuin family. SIRT1 was the first homolog found in humans and other mammals (Mol. Endocrinol. 2007;21:1745-55; Mol. Cell Biol. 2003;23:3173-85; Biochem. Biophys. Res. Commun. 2000;273:793-8). Now there are seven known mammalian sirtuins: SIRT1-SIRT7. Sirtuins are found in organisms ranging from bacteria to humans. Much sirtuin research has been done in the yeast Saccharomyces cerevisiae, the fruit fly Drosophila melanogaster, and the nematode Caenorhabditis elegans. In these organisms, sirtuins have been identified as molecules that mediate the effects of caloric restriction on aging processes (Genes Nutr. 2006;1:85-93).
Everyone in the skin care world is talking about sirtuins. Studies have shown that resveratrol activates sirtuins, and sales of resveratrol have risen. Many products claim to contain ingredients that activate sirtuins.
To be up to date on current skin care, you need to know what sirtuins are and why they are a frequent topic at the Society of Cosmetic Chemists meetings. The short explanation is that calorie-restricted mice have been shown to live longer and to have increased expression of sirtuins. It is believed that the upregulation of sirtuin expression is associated with increased longevity. When mice were not calorie restricted but were treated with resveratrol to activate sirtuins, they also lived longer.
The current belief that activating sirtuin is desirable has led to a plethora of products with sirtuin-activating ingredients, including several sold by Avon Products Inc.
Where Are Sirtuins Found?
Role of Sirtuins
Silent mating type information regulator 2 (Sir2) proteins, or sirtuins, are a family of nicotinamide adenine dinucleotide (NAD+)-dependent enzymes known to deacetylate lysine residues on several proteins and, in some cases, to exhibit adenosine diphosphate (ADP)-ribosyltransferase activity (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55). Sirtuins are activated when cellular energy is low and the NAD+ to NADH ratio is high (Genes Nutr. 2006;1:85-93).
This family of enzymes is known to be involved in apoptosis, fatty acid metabolism, gene silencing, and regulation of cellular lifespans. They are also linked to genes that organize and optimize cell functions to resist or survive in stressful environments (J. Drugs Dermatol. 2007;6:s14-9). Sirtuins regulate important biological pathways, such as transcriptional repression, recombination, the cell-division cycle, microtubule organization, and cellular responses to DNA-damaging compounds (Genome Biol. 2004;5:224).
It is believed that the mammalian sirtuins, SIRT1-SIRT7, play an influential role in gene silencing, energy homeostasis, the cell cycle, apoptosis, stress resistance or stress responses, axonal degeneration, and aging (Genome Biol. 2004;5:224; Mol. Endocrinol. 2007;21:1745-55; J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x ]). As such, Yamamoto et al. have contended that sirtuins may be appropriate therapeutic targets for a range of disorders, including proliferative, neurodegenerative, and metabolic diseases (Mol. Endocrinol. 2007;21:1745-55).
The Nomenclature
Sirtuin Research in Skin
For the active skin care product portion of the study, the researchers enrolled 33 women between 37 and 64 years old (mean age 51.6 years), who were instructed to apply a formulation enriched in 1% of the yeast biopeptides once daily for 4 weeks to the neck and face. Before and after the first application and after 4 weeks of use, investigating dermatologists assessed fine lines and wrinkles, pigment color intensity, complexion homogeneity, and radiance, as well as skin density, hydration, firmness, and texture on a 1-9 scale. To objectively evaluate skin care efficacy, they used a pixel skin method based on analyzing age-related parameters from numerical pictures of faces.
The investigators identified multiple findings from their study. In particular, the Kluyveromyces biopeptides markedly increased SIRT1 expression in normal human dermal fibroblasts in vitro as well as in healthy human epidermal cells ex vivo while diminishing cellular aging and UVB-induced DNA fragmentation. Among the study participants, improvements were found in all of the assessment parameters, with hydration noted as significantly improving right after the first application.
The authors concluded that the yeast Kluyveromyces biopeptides were efficacious in activating SIRT1 in human skin cells, resulting in the enhancement of DNA resistance and aging. In addition, a formulation featuring Kluyveromyces biopeptides exhibited efficacy in ameliorating various signs of cutaneous aging (J. Drugs Dermatol. 2007;6:s14-9).
In 2008, Cao et al. reported on the role of SIRT1 in UV signaling pathways. With cell culture and Western blot analysis, they found that SIRT1 is expressed in cultured human skin keratinocytes. The investigators observed that SIRT1 is time- and dose-dependently down-regulated by exposure to UV radiation and H2O2, with reactive oxygen species (ROS)-mediated JNK (c-Jun N-terminal kinase) activation involved in the down-regulation. Significantly, resveratrol, an activator of SIRT1, protected against UV- and H2O2-induced apoptosis; SIRT inhibitors such as sirtinol and nicotinamide promoted apoptosis.
The investigators also noted that resveratrol suppresses UV- and H2O2-induced p53 acetylation, while the SIRT inhibitors sirtinol and nicotinamide, as well as SIRT1 small interfering RNA (siRNA), foster it. Overall, the researchers suggested that their work adds to the understanding of the molecular mechanisms of photoaging, and that the SIRT1-activating property of resveratrol might be targeted in agents intended for therapeutic approaches to cutaneous aging (J. Cell Mol. Med. 2008 Aug 4 [doi:10.1111/j.1582-4934.2008.00453.x]).
Also in 2008, Pallàs et al. found that increasing SIRT1 protects against amyloid beta-induced ROS synthesis and DNA damage, thus diminishing in vitro apoptosis. In addition, the overexpression of SIRT1, induced by caloric restriction or the use of the antioxidant resveratrol, has been shown to rescue Alzheimer's and Huntington's disease neurons (Recent Pat. CNS Drug Discov. 2008;3:61-9). SIRT1 and SIR2 had already been implicated as the proteins involved in lifespan extension from caloric restriction in various species.
Polyphenols such as quercetin and resveratrol are dietary antioxidants known to confer numerous health benefits and to activate sirtuins, thus playing a role in the caloric restriction longevity extension mechanism; their capacity to influence or extend lifespan has been shown in simple organisms but not consistently, as yet, in humans or other mammals (J. Cosmet. Dermatol. 2008;7:2-7; Genes Nutr. 2006;1:85-93).
However, work in mice (discussed in an episode of the television show "60 Minutes" in early 2009) performed by Sirtris Pharmaceuticals, a research company founded on recent discoveries related to sirtuins, demonstrated that resveratrol fed to mice on a high-fat diet improved insulin resistance, increased mitochondrial content, and prolonged life. In two groups of mice fed a high-fat diet, both groups wound up obese, but the mice administered resveratrol as part of their diet were able to run twice as far and fast, and survived 20% longer. In other studies by Sirtris, mice fed resveratrol as part of a high-fat diet gained less weight than mice administered a high-fat diet without resveratrol. Investigators at Sirtris also have identified small-molecule activators of SIRT1 that are 1,000 times as strong as resveratrol (Nature 2007;450:712-6).
Many other companies, such as Avon, have studied ingredients that upregulate sirtuin expression. By using human skin biopsies and immunohistochemical analysis, Avon has shown that its own proprietary botanical extracts promote the expression of dermal matrix proteins. The company claims that a 12-week clinical study using a product formulated to stimulate sirtuin expression displayed efficacy that warrants use in an antiaging product.
It remains to be seen what such claims - and products - will mean for the skin. For now, I would continue to recommend oral resveratrol and red wine supplements. In particular, I suggest OPC Synergy by Standard Process Inc., which contains grape seed and red wine extracts.
Conclusions
The family of proteins known as sirtuins appears to play an important role in the increased lifespan of various species, particularly, as recent research suggests, in calorie-restricted animals. The polyphenolic antioxidant resveratrol, which is abundant in red wine and is now included in some cosmeceutical agents, upregulates sirtuin expression and may protect cells from DNA damage.
The discovery of the role of sirtuin expression in slowing the pace of aging, in the experimental setting, strikes me as a very significant advance, and may lead to further elucidation of the aging process overall as well as cutaneous aging.
However, it is unknown at this time what role sirtuin and sirtuin activators play in skin care. Early data suggest that the activation of sirtuins may improve the appearance of skin, but the mechanism, if known, is unclear to me. The potential of Avon's botanically derived agent in upregulating sirtuin expression in skin cell cultures appears promising, because the company's study did reveal that patients experienced improvement in wrinkles. I was not the investigator in this study, so it is difficult to comment on the validity of the observations, as I am unsure of the exact study design.
I will be interested to see further work in this area, and it's always good to have a medically sound reason to drink wine.
Recently, investigators attempted to stimulate the expression of sirtuin, specifically SIRT1, in human skin cells in a culture of yeast Kluyveromyces biopetides, and to identify cutaneous benefits from an active skin care product containing such biopeptides. They also tested healthy skin samples ex vivo. Immunostaining, Western blotting, and cytometry were used to assess SIRT1 in culture and in ex vivo samples. Comet assays were used to evaluate cellular aging and integrity. Sir2 protein (Sir2p), present in yeast, is the founding member of the sirtuin family. SIRT1 was the first homolog found in humans and other mammals (Mol. Endocrinol. 2007;21:1745-55; Mol. Cell Biol. 2003;23:3173-85; Biochem. Biophys. Res. Commun. 2000;273:793-8). Now there are seven known mammalian sirtuins: SIRT1-SIRT7. Sirtuins are found in organisms ranging from bacteria to humans. Much sirtuin research has been done in the yeast Saccharomyces cerevisiae, the fruit fly Drosophila melanogaster, and the nematode Caenorhabditis elegans. In these organisms, sirtuins have been identified as molecules that mediate the effects of caloric restriction on aging processes (Genes Nutr. 2006;1:85-93).
Polyphenols Everywhere
Many products that tout antioxidant activity include antioxidant ingredients that contain polyphenols. There are numerous classes of polyphenols, which are the largest group of phytochemicals and the most broadly disseminated among plants (J. Am. Diet. Assoc. 1999;99:213-8). They are secondary plant metabolites represented by more than 8,000 naturally occurring compounds.
These widely divergent substances, which exhibit various levels of antioxidant activity, share a common structural component: a phenol or an aromatic ring, usually two, with at least one hydroxyl group, that are linked via a three-carbon bond to form a six-unit heterocyclic ring (J. Nutr. 2003;133:3248S-54S).
Attention has been increasingly focused on polyphenols, as they are known to be an important part of, and the most abundant source of antioxidants in, the human diet. They are present in many vegetables, fruits, herbs, grains, teas, and beans, as well as coffee, propolis, and red wine (Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2003;147:137-45; J. Nutr. 2000;130:2073S-85S; Annu. Rev. Nutr. 2002;22:19-34; Pharmacol. Ther. 2001;90:157-77; Free Radic. Biol. Med. 2001;30:1213-22).
The most prevalent and frequently studied polyphenols are known as flavonoids. Based on the connection of an aromatic ring to the heterocyclic ring, as well as the oxidation state and functional groups of the heterocyclic ring, flavonoids are further divided into flavones (based on the 2-phenylchromen-4-one skeleton, e.g., apigenin and luteolin); flavonols (based on the 3-hydroxy-2-phenylchromen-4-one skeleton and functional group, e.g., quercetin, kaempferol, myricetin, and fisetin); flavanones (based on the 2,3-dihydro-2-phenylchromen-4-one skeleton and functional group, e.g., naringenin, hesperetin, and eriodictyol); isoflavones (based on the 3-phenylchromen-4-one skeleton, e.g., genistein and daidzein); flavanols or catechins (based on the 2-phenyl-3,4-dihydro-2H-chromen-3-ol skeleton and functional groups, e.g., epicatechin, epicatechin 3-gallate, epigallocatechin, epigallocatechin 3-gallate (EGCG), catechin, gallocatechin); anthocyanins (based on the 2-phenylchromenylium ion skeleton, e.g., cyanidin and pelargonidin); and proanthocyanidins or condensed tannins (which are polymer chains of flavanols, such as catechins, and include pycnogenol, leukocyanidin, and leucoanthocyanidin) (Annu. Rev. Nutr. 2002;22:19-34; Asia Pac. J. Clin. Nutr. 2004;13:S72; J. Nutr. 2000;130:2073S-85S; J. Nutr. 2003;133:3248S-54S).
Tannins, phenolic polymers of high molecular weight, are divided into three classes: hydrolyzable tannins (e.g., ellagic acid, found in pomegranates, raspberries, strawberries, cranberries, and walnuts), derived tannins (created during food handling and processing and present in black and oolong teas), and condensed tannins, described above (J. Am. Diet. Assoc. 1999;99:213-8; J. Nutr. 2003;133:3248S-54S).
Some specific flavonoids can be found in the following food sources: flavonols in apples with skin, broccoli, olives, onions, and green and black tea; flavones in celery and parsley; flavonones in grapefruit, oranges, and their juices; and catechins (flavanols) in apples with or without skin, dark chocolate, cocoa, red wine, and green and black tea (Asia Pac. J. Clin. Nutr. 2004;13:S72).
There are a plethora of other polyphenols, many of which confer health benefits, including stilbenes (e.g., resveratrol, found in red wine), lignans (e.g., enterodiol, found in flaxseed and flaxseed oil), and phenolic acids, such as hydroxybenzoic and hydroxycinnamic acids, among which caffeic and ferulic acids are often present in foods.
Broad health benefits have been associated with hundreds of polyphenolic substances. Notably, some of the best known research results on polyphenols have reported on the success of various topical applications of green tea catechins, ferulic acid, resveratrol, and other related compounds (many of which have been addressed in this column). The rest of this discussion focuses on new information regarding systemic efficacy, topical delivery, or applications of a representative from several subclasses of these compounds.
Flavonols: Quercetin
A water-in-oil microemulsion containing quercetin has been shown, in porcine skin in vitro and hairless mouse skin in vivo, to enhance the penetration of the flavonol into the stratum corneum, epidermis, and dermis. The preparation also was found to significantly inhibit ultraviolet B (UVB)-induced metalloproteinase activity and glutathione reduction (Eur. J. Pharm. Biopharm. 2008;69:948-57).
Flavones: Apigenin
The topical application of 4',5,7-trihydroxyflavone (apigenin) on mouse skin has been shown to decrease skin tumor size and incidence induced by UVB exposure (Cancer Res. 2008:68:3057-65). In a different study, the apigenin glycosides 7-O-glucuronide, 7-O-methylglucuronide, and pectolinarin also have been demonstrated to induce collagen type I synthesis in fibroblasts. The investigators found that all tested compounds promoted the activity of prolidase, which initiates the last stage of collagen degradation and is integral to collagen production (Int. J. Mol. Med. 2007;20:889-95).
Flavonones: Naringenin
The citrus flavonone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. Naringenin has been demonstrated to exert an antiapoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and to facilitate the removal of cyclobutane pyrimidine dimers from the genome (Photochem. Photobiol. 2008;84:307-16).
Isoflavones: Red Clover, Genistein, and Daidzein
Recently, red clover, whose isoflavones had previously been shown to contribute to a low incidence of osteoporosis and menopausal symptoms in high dietary concentrations, was examined for anti-aging effects. Investigators orally administered red clover extract containing 11% isoflavones to ovariectomized rats for 14 weeks, and found that collagen levels increased significantly in the treatment group as compared to the control group. Epidermal thickness and keratinization were normal in the treated group, but were reduced in the control group. The authors concluded that the regular dietary consumption of red clover isoflavones can alleviate cutaneous aging brought on by declines in estrogen (Phytother. Res. 2006;20:1096-9).
In a recent study evaluating the feasibility of skin absorption of the soy isoflavones genistein, daidzein, and glycitein, both genistein and daidzein inhibited UVB-induced hydrogen peroxide synthesis in keratinocytes. Analysis of vehicle effects on in vitro topical delivery revealed that genistein showed better skin absorption than daidzein. The investigators concluded that the topical application of soy isoflavones shows promise as a treatment for photoaging and photodamage (Int. J. Pharm. 2008;364:36-44).
Indeed, the topical application of isoflavones, including genistein and daidzein, has been shown to protect pig skin from photodamage caused by solar-simulated ultraviolet irradiation. Notably, the isoflavone compounds tested were less effective than a topical antioxidant formulation containing vitamins C and E and the phenolic acid ferulic acid (Photodermatol. Photoimmunol. Photomed. 2008;24:61-6).
Catechins (Flavanols): Epigallocatechin 3-gallate
Already considered a potent antioxidant, EGCG continues to receive attention for conferring an expanding range of health benefits. This compound, the most abundant and potent catechin in green tea, has been shown to hinder UVB-induced collagen-degrading matrix metalloproteinases (Food Chem. Toxicol. 2008;46:1298-307).
A different study of EGCG indicated that it hampered the proliferation and migration of keloid fibroblasts in vitro, and also curbed in vivo signs of keloids, by interrupting the signal transducer and activator of the transcription-3 signaling pathway. As a result of these findings, the investigators proposed EGCG as a preventive and therapeutic agent for keloids (J. Invest. Dermatol. 2008;128:2429-41). EGCG also has been suggested as a potential therapeutic approach to atopic dermatitis, given its success against AD-like skin lesions in a murine model (Int. Immunopharmacol. 2008;8:1172-82).
Anthocyanins: Cyanidin
Clearly, all flavonoids are not equal. In a recent study, methanol extracts of black raspberries, strawberries, and blueberries were tested for their capacity to inhibit UV-induced activation of nuclear transcription factor-kappa B (NF-kappaB) and activator protein-1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin 3-rutinoside, were found to time- and dose-dependently inhibit the effects of UV on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin 3-rutinoside (Nutr. Cancer 2007;58:205-12).
Another form of cyanidin has also been shown to impart cutaneous benefits. Specifically, pretreatment of human keratinocytes with the anthocyanin cyanidin 3-O-glucoside has been demonstrated to protect against a wide array of UVB-induced damage (J. Agric. Food Chem. 2006;54:4041-7).
Proanthocyanidins: Pycnogenol
Investigators studied pycnogenol in an antioxidant mixture that also included evening primrose and vitamins C and E. After 10 weeks of oral administration to female SKH-1 hairless mice exposed to UVB irradiation three times weekly, the mixture was found to significantly inhibit wrinkle formation by suppressing UVB-induced matrix metalloproteinase activity while promoting collagen production (Photodermatol. Photoimmunol. Photomed. 2007;23:155-62).
Tannins: Ellagic Acid
In a double-blind, placebo-controlled, 4-week trial, investigators assessed the effects of orally administered ellagic acid-rich pomegranate extract on the pigmentation of 13 women after UV exposure. Healthy volunteers were randomly assigned to high-dose, low-dose, and control groups. The results showed that luminance values decreased by 1.73% in the high-dose group and 1.35% in the low-dose group, compared with the control group, and stains and freckles also were diminished (J. Nutr. Sci. Vitaminol. (Tokyo) 2006;52:383-8).
Stilbenes: Resveratrol
The antioxidant potency of resveratrol has been cited for conferring a wide range of salutary effects, including antitumorigenic and antiaging activity. Recently, a resveratrol-based skin care formulation intended to combat photoaging was reported to exhibit 17-fold greater antioxidant activity than idebenone (J. Cosmet. Dermatol. 2008;7:2-7). In a different study, resveratrol, the primary active polyphenolic constituent in red wine, was assessed in terms of topical/transdermal delivery viability, given the previously established benefits shown via systemic administration. Several hydrogel systems used as resveratrol vehicles were shown to be safe and effective methods for cutaneously delivering the therapeutic effects of this antioxidant (Biol. Pharm. Bull. 2008;31:955-62).
Phenolic Acids: Ferulic Acid
In a small study, a stable formulation of 15% L-corbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid was applied topically to normal-appearing human skin for 4 days, and was found to confer significant photoprotection against solar-simulated UV radiation. The preparation was especially effective at diminishing thymine dimer mutations, which are linked to skin cancer. The authors also noted that the mechanism of action of this antioxidant formulation differs from that of sunscreens and, therefore, may serve as a supplement to such products (J. Am. Acad. Dermatol. 2008;59:418-25). It is worth noting that ferulic acid has been approved as a sunscreen agent in Japan (J. Pharm. Biomed. Anal. 2008;46:645-52).
Conclusion
A brief survey of the polyphenolic landscape obviously cannot do the subject justice. That said, from the dermatologic perspective, it is simply worth noting how often this diverse family of compounds factors occur in to the skin care formulations that are becoming more prevalent in the established armamentarium as well as the direct-to-consumer market.
Given the increasing attention paid here and elsewhere to the impact of diet on the skin, the status of the diverse class of polyphenolic compounds found in a wide array of plants, which includes several antioxidants, appears to be well deserved and warrants much more research.
Many products that tout antioxidant activity include antioxidant ingredients that contain polyphenols. There are numerous classes of polyphenols, which are the largest group of phytochemicals and the most broadly disseminated among plants (J. Am. Diet. Assoc. 1999;99:213-8). They are secondary plant metabolites represented by more than 8,000 naturally occurring compounds.
These widely divergent substances, which exhibit various levels of antioxidant activity, share a common structural component: a phenol or an aromatic ring, usually two, with at least one hydroxyl group, that are linked via a three-carbon bond to form a six-unit heterocyclic ring (J. Nutr. 2003;133:3248S-54S).
Attention has been increasingly focused on polyphenols, as they are known to be an important part of, and the most abundant source of antioxidants in, the human diet. They are present in many vegetables, fruits, herbs, grains, teas, and beans, as well as coffee, propolis, and red wine (Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2003;147:137-45; J. Nutr. 2000;130:2073S-85S; Annu. Rev. Nutr. 2002;22:19-34; Pharmacol. Ther. 2001;90:157-77; Free Radic. Biol. Med. 2001;30:1213-22).
The most prevalent and frequently studied polyphenols are known as flavonoids. Based on the connection of an aromatic ring to the heterocyclic ring, as well as the oxidation state and functional groups of the heterocyclic ring, flavonoids are further divided into flavones (based on the 2-phenylchromen-4-one skeleton, e.g., apigenin and luteolin); flavonols (based on the 3-hydroxy-2-phenylchromen-4-one skeleton and functional group, e.g., quercetin, kaempferol, myricetin, and fisetin); flavanones (based on the 2,3-dihydro-2-phenylchromen-4-one skeleton and functional group, e.g., naringenin, hesperetin, and eriodictyol); isoflavones (based on the 3-phenylchromen-4-one skeleton, e.g., genistein and daidzein); flavanols or catechins (based on the 2-phenyl-3,4-dihydro-2H-chromen-3-ol skeleton and functional groups, e.g., epicatechin, epicatechin 3-gallate, epigallocatechin, epigallocatechin 3-gallate (EGCG), catechin, gallocatechin); anthocyanins (based on the 2-phenylchromenylium ion skeleton, e.g., cyanidin and pelargonidin); and proanthocyanidins or condensed tannins (which are polymer chains of flavanols, such as catechins, and include pycnogenol, leukocyanidin, and leucoanthocyanidin) (Annu. Rev. Nutr. 2002;22:19-34; Asia Pac. J. Clin. Nutr. 2004;13:S72; J. Nutr. 2000;130:2073S-85S; J. Nutr. 2003;133:3248S-54S).
Tannins, phenolic polymers of high molecular weight, are divided into three classes: hydrolyzable tannins (e.g., ellagic acid, found in pomegranates, raspberries, strawberries, cranberries, and walnuts), derived tannins (created during food handling and processing and present in black and oolong teas), and condensed tannins, described above (J. Am. Diet. Assoc. 1999;99:213-8; J. Nutr. 2003;133:3248S-54S).
Some specific flavonoids can be found in the following food sources: flavonols in apples with skin, broccoli, olives, onions, and green and black tea; flavones in celery and parsley; flavonones in grapefruit, oranges, and their juices; and catechins (flavanols) in apples with or without skin, dark chocolate, cocoa, red wine, and green and black tea (Asia Pac. J. Clin. Nutr. 2004;13:S72).
There are a plethora of other polyphenols, many of which confer health benefits, including stilbenes (e.g., resveratrol, found in red wine), lignans (e.g., enterodiol, found in flaxseed and flaxseed oil), and phenolic acids, such as hydroxybenzoic and hydroxycinnamic acids, among which caffeic and ferulic acids are often present in foods.
Broad health benefits have been associated with hundreds of polyphenolic substances. Notably, some of the best known research results on polyphenols have reported on the success of various topical applications of green tea catechins, ferulic acid, resveratrol, and other related compounds (many of which have been addressed in this column). The rest of this discussion focuses on new information regarding systemic efficacy, topical delivery, or applications of a representative from several subclasses of these compounds.
Flavonols: Quercetin
A water-in-oil microemulsion containing quercetin has been shown, in porcine skin in vitro and hairless mouse skin in vivo, to enhance the penetration of the flavonol into the stratum corneum, epidermis, and dermis. The preparation also was found to significantly inhibit ultraviolet B (UVB)-induced metalloproteinase activity and glutathione reduction (Eur. J. Pharm. Biopharm. 2008;69:948-57).
Flavones: Apigenin
The topical application of 4',5,7-trihydroxyflavone (apigenin) on mouse skin has been shown to decrease skin tumor size and incidence induced by UVB exposure (Cancer Res. 2008:68:3057-65). In a different study, the apigenin glycosides 7-O-glucuronide, 7-O-methylglucuronide, and pectolinarin also have been demonstrated to induce collagen type I synthesis in fibroblasts. The investigators found that all tested compounds promoted the activity of prolidase, which initiates the last stage of collagen degradation and is integral to collagen production (Int. J. Mol. Med. 2007;20:889-95).
Flavonones: Naringenin
The citrus flavonone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. Naringenin has been demonstrated to exert an antiapoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and to facilitate the removal of cyclobutane pyrimidine dimers from the genome (Photochem. Photobiol. 2008;84:307-16).
Isoflavones: Red Clover, Genistein, and Daidzein
Recently, red clover, whose isoflavones had previously been shown to contribute to a low incidence of osteoporosis and menopausal symptoms in high dietary concentrations, was examined for anti-aging effects. Investigators orally administered red clover extract containing 11% isoflavones to ovariectomized rats for 14 weeks, and found that collagen levels increased significantly in the treatment group as compared to the control group. Epidermal thickness and keratinization were normal in the treated group, but were reduced in the control group. The authors concluded that the regular dietary consumption of red clover isoflavones can alleviate cutaneous aging brought on by declines in estrogen (Phytother. Res. 2006;20:1096-9).
In a recent study evaluating the feasibility of skin absorption of the soy isoflavones genistein, daidzein, and glycitein, both genistein and daidzein inhibited UVB-induced hydrogen peroxide synthesis in keratinocytes. Analysis of vehicle effects on in vitro topical delivery revealed that genistein showed better skin absorption than daidzein. The investigators concluded that the topical application of soy isoflavones shows promise as a treatment for photoaging and photodamage (Int. J. Pharm. 2008;364:36-44).
Indeed, the topical application of isoflavones, including genistein and daidzein, has been shown to protect pig skin from photodamage caused by solar-simulated ultraviolet irradiation. Notably, the isoflavone compounds tested were less effective than a topical antioxidant formulation containing vitamins C and E and the phenolic acid ferulic acid (Photodermatol. Photoimmunol. Photomed. 2008;24:61-6).
Catechins (Flavanols): Epigallocatechin 3-gallate
Already considered a potent antioxidant, EGCG continues to receive attention for conferring an expanding range of health benefits. This compound, the most abundant and potent catechin in green tea, has been shown to hinder UVB-induced collagen-degrading matrix metalloproteinases (Food Chem. Toxicol. 2008;46:1298-307).
A different study of EGCG indicated that it hampered the proliferation and migration of keloid fibroblasts in vitro, and also curbed in vivo signs of keloids, by interrupting the signal transducer and activator of the transcription-3 signaling pathway. As a result of these findings, the investigators proposed EGCG as a preventive and therapeutic agent for keloids (J. Invest. Dermatol. 2008;128:2429-41). EGCG also has been suggested as a potential therapeutic approach to atopic dermatitis, given its success against AD-like skin lesions in a murine model (Int. Immunopharmacol. 2008;8:1172-82).
Anthocyanins: Cyanidin
Clearly, all flavonoids are not equal. In a recent study, methanol extracts of black raspberries, strawberries, and blueberries were tested for their capacity to inhibit UV-induced activation of nuclear transcription factor-kappa B (NF-kappaB) and activator protein-1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin 3-rutinoside, were found to time- and dose-dependently inhibit the effects of UV on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin 3-rutinoside (Nutr. Cancer 2007;58:205-12).
Another form of cyanidin has also been shown to impart cutaneous benefits. Specifically, pretreatment of human keratinocytes with the anthocyanin cyanidin 3-O-glucoside has been demonstrated to protect against a wide array of UVB-induced damage (J. Agric. Food Chem. 2006;54:4041-7).
Proanthocyanidins: Pycnogenol
Investigators studied pycnogenol in an antioxidant mixture that also included evening primrose and vitamins C and E. After 10 weeks of oral administration to female SKH-1 hairless mice exposed to UVB irradiation three times weekly, the mixture was found to significantly inhibit wrinkle formation by suppressing UVB-induced matrix metalloproteinase activity while promoting collagen production (Photodermatol. Photoimmunol. Photomed. 2007;23:155-62).
Tannins: Ellagic Acid
In a double-blind, placebo-controlled, 4-week trial, investigators assessed the effects of orally administered ellagic acid-rich pomegranate extract on the pigmentation of 13 women after UV exposure. Healthy volunteers were randomly assigned to high-dose, low-dose, and control groups. The results showed that luminance values decreased by 1.73% in the high-dose group and 1.35% in the low-dose group, compared with the control group, and stains and freckles also were diminished (J. Nutr. Sci. Vitaminol. (Tokyo) 2006;52:383-8).
Stilbenes: Resveratrol
The antioxidant potency of resveratrol has been cited for conferring a wide range of salutary effects, including antitumorigenic and antiaging activity. Recently, a resveratrol-based skin care formulation intended to combat photoaging was reported to exhibit 17-fold greater antioxidant activity than idebenone (J. Cosmet. Dermatol. 2008;7:2-7). In a different study, resveratrol, the primary active polyphenolic constituent in red wine, was assessed in terms of topical/transdermal delivery viability, given the previously established benefits shown via systemic administration. Several hydrogel systems used as resveratrol vehicles were shown to be safe and effective methods for cutaneously delivering the therapeutic effects of this antioxidant (Biol. Pharm. Bull. 2008;31:955-62).
Phenolic Acids: Ferulic Acid
In a small study, a stable formulation of 15% L-corbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid was applied topically to normal-appearing human skin for 4 days, and was found to confer significant photoprotection against solar-simulated UV radiation. The preparation was especially effective at diminishing thymine dimer mutations, which are linked to skin cancer. The authors also noted that the mechanism of action of this antioxidant formulation differs from that of sunscreens and, therefore, may serve as a supplement to such products (J. Am. Acad. Dermatol. 2008;59:418-25). It is worth noting that ferulic acid has been approved as a sunscreen agent in Japan (J. Pharm. Biomed. Anal. 2008;46:645-52).
Conclusion
A brief survey of the polyphenolic landscape obviously cannot do the subject justice. That said, from the dermatologic perspective, it is simply worth noting how often this diverse family of compounds factors occur in to the skin care formulations that are becoming more prevalent in the established armamentarium as well as the direct-to-consumer market.
Given the increasing attention paid here and elsewhere to the impact of diet on the skin, the status of the diverse class of polyphenolic compounds found in a wide array of plants, which includes several antioxidants, appears to be well deserved and warrants much more research.
Many products that tout antioxidant activity include antioxidant ingredients that contain polyphenols. There are numerous classes of polyphenols, which are the largest group of phytochemicals and the most broadly disseminated among plants (J. Am. Diet. Assoc. 1999;99:213-8). They are secondary plant metabolites represented by more than 8,000 naturally occurring compounds.
These widely divergent substances, which exhibit various levels of antioxidant activity, share a common structural component: a phenol or an aromatic ring, usually two, with at least one hydroxyl group, that are linked via a three-carbon bond to form a six-unit heterocyclic ring (J. Nutr. 2003;133:3248S-54S).
Attention has been increasingly focused on polyphenols, as they are known to be an important part of, and the most abundant source of antioxidants in, the human diet. They are present in many vegetables, fruits, herbs, grains, teas, and beans, as well as coffee, propolis, and red wine (Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2003;147:137-45; J. Nutr. 2000;130:2073S-85S; Annu. Rev. Nutr. 2002;22:19-34; Pharmacol. Ther. 2001;90:157-77; Free Radic. Biol. Med. 2001;30:1213-22).
The most prevalent and frequently studied polyphenols are known as flavonoids. Based on the connection of an aromatic ring to the heterocyclic ring, as well as the oxidation state and functional groups of the heterocyclic ring, flavonoids are further divided into flavones (based on the 2-phenylchromen-4-one skeleton, e.g., apigenin and luteolin); flavonols (based on the 3-hydroxy-2-phenylchromen-4-one skeleton and functional group, e.g., quercetin, kaempferol, myricetin, and fisetin); flavanones (based on the 2,3-dihydro-2-phenylchromen-4-one skeleton and functional group, e.g., naringenin, hesperetin, and eriodictyol); isoflavones (based on the 3-phenylchromen-4-one skeleton, e.g., genistein and daidzein); flavanols or catechins (based on the 2-phenyl-3,4-dihydro-2H-chromen-3-ol skeleton and functional groups, e.g., epicatechin, epicatechin 3-gallate, epigallocatechin, epigallocatechin 3-gallate (EGCG), catechin, gallocatechin); anthocyanins (based on the 2-phenylchromenylium ion skeleton, e.g., cyanidin and pelargonidin); and proanthocyanidins or condensed tannins (which are polymer chains of flavanols, such as catechins, and include pycnogenol, leukocyanidin, and leucoanthocyanidin) (Annu. Rev. Nutr. 2002;22:19-34; Asia Pac. J. Clin. Nutr. 2004;13:S72; J. Nutr. 2000;130:2073S-85S; J. Nutr. 2003;133:3248S-54S).
Tannins, phenolic polymers of high molecular weight, are divided into three classes: hydrolyzable tannins (e.g., ellagic acid, found in pomegranates, raspberries, strawberries, cranberries, and walnuts), derived tannins (created during food handling and processing and present in black and oolong teas), and condensed tannins, described above (J. Am. Diet. Assoc. 1999;99:213-8; J. Nutr. 2003;133:3248S-54S).
Some specific flavonoids can be found in the following food sources: flavonols in apples with skin, broccoli, olives, onions, and green and black tea; flavones in celery and parsley; flavonones in grapefruit, oranges, and their juices; and catechins (flavanols) in apples with or without skin, dark chocolate, cocoa, red wine, and green and black tea (Asia Pac. J. Clin. Nutr. 2004;13:S72).
There are a plethora of other polyphenols, many of which confer health benefits, including stilbenes (e.g., resveratrol, found in red wine), lignans (e.g., enterodiol, found in flaxseed and flaxseed oil), and phenolic acids, such as hydroxybenzoic and hydroxycinnamic acids, among which caffeic and ferulic acids are often present in foods.
Broad health benefits have been associated with hundreds of polyphenolic substances. Notably, some of the best known research results on polyphenols have reported on the success of various topical applications of green tea catechins, ferulic acid, resveratrol, and other related compounds (many of which have been addressed in this column). The rest of this discussion focuses on new information regarding systemic efficacy, topical delivery, or applications of a representative from several subclasses of these compounds.
Flavonols: Quercetin
A water-in-oil microemulsion containing quercetin has been shown, in porcine skin in vitro and hairless mouse skin in vivo, to enhance the penetration of the flavonol into the stratum corneum, epidermis, and dermis. The preparation also was found to significantly inhibit ultraviolet B (UVB)-induced metalloproteinase activity and glutathione reduction (Eur. J. Pharm. Biopharm. 2008;69:948-57).
Flavones: Apigenin
The topical application of 4',5,7-trihydroxyflavone (apigenin) on mouse skin has been shown to decrease skin tumor size and incidence induced by UVB exposure (Cancer Res. 2008:68:3057-65). In a different study, the apigenin glycosides 7-O-glucuronide, 7-O-methylglucuronide, and pectolinarin also have been demonstrated to induce collagen type I synthesis in fibroblasts. The investigators found that all tested compounds promoted the activity of prolidase, which initiates the last stage of collagen degradation and is integral to collagen production (Int. J. Mol. Med. 2007;20:889-95).
Flavonones: Naringenin
The citrus flavonone naringenin shows promise as a preventive agent against cutaneous aging as well as carcinogenesis. Naringenin has been demonstrated to exert an antiapoptotic effect in UVB-damaged cells, significantly extending long-term cellular survival, and to facilitate the removal of cyclobutane pyrimidine dimers from the genome (Photochem. Photobiol. 2008;84:307-16).
Isoflavones: Red Clover, Genistein, and Daidzein
Recently, red clover, whose isoflavones had previously been shown to contribute to a low incidence of osteoporosis and menopausal symptoms in high dietary concentrations, was examined for anti-aging effects. Investigators orally administered red clover extract containing 11% isoflavones to ovariectomized rats for 14 weeks, and found that collagen levels increased significantly in the treatment group as compared to the control group. Epidermal thickness and keratinization were normal in the treated group, but were reduced in the control group. The authors concluded that the regular dietary consumption of red clover isoflavones can alleviate cutaneous aging brought on by declines in estrogen (Phytother. Res. 2006;20:1096-9).
In a recent study evaluating the feasibility of skin absorption of the soy isoflavones genistein, daidzein, and glycitein, both genistein and daidzein inhibited UVB-induced hydrogen peroxide synthesis in keratinocytes. Analysis of vehicle effects on in vitro topical delivery revealed that genistein showed better skin absorption than daidzein. The investigators concluded that the topical application of soy isoflavones shows promise as a treatment for photoaging and photodamage (Int. J. Pharm. 2008;364:36-44).
Indeed, the topical application of isoflavones, including genistein and daidzein, has been shown to protect pig skin from photodamage caused by solar-simulated ultraviolet irradiation. Notably, the isoflavone compounds tested were less effective than a topical antioxidant formulation containing vitamins C and E and the phenolic acid ferulic acid (Photodermatol. Photoimmunol. Photomed. 2008;24:61-6).
Catechins (Flavanols): Epigallocatechin 3-gallate
Already considered a potent antioxidant, EGCG continues to receive attention for conferring an expanding range of health benefits. This compound, the most abundant and potent catechin in green tea, has been shown to hinder UVB-induced collagen-degrading matrix metalloproteinases (Food Chem. Toxicol. 2008;46:1298-307).
A different study of EGCG indicated that it hampered the proliferation and migration of keloid fibroblasts in vitro, and also curbed in vivo signs of keloids, by interrupting the signal transducer and activator of the transcription-3 signaling pathway. As a result of these findings, the investigators proposed EGCG as a preventive and therapeutic agent for keloids (J. Invest. Dermatol. 2008;128:2429-41). EGCG also has been suggested as a potential therapeutic approach to atopic dermatitis, given its success against AD-like skin lesions in a murine model (Int. Immunopharmacol. 2008;8:1172-82).
Anthocyanins: Cyanidin
Clearly, all flavonoids are not equal. In a recent study, methanol extracts of black raspberries, strawberries, and blueberries were tested for their capacity to inhibit UV-induced activation of nuclear transcription factor-kappa B (NF-kappaB) and activator protein-1 (AP-1) in mouse epidermal cells. The methanol fractions of black raspberries, which contain the anthocyanin cyanidin 3-rutinoside, were found to time- and dose-dependently inhibit the effects of UV on NF-kappaB and AP-1, unlike the other berries, which do not contain cyanidin 3-rutinoside (Nutr. Cancer 2007;58:205-12).
Another form of cyanidin has also been shown to impart cutaneous benefits. Specifically, pretreatment of human keratinocytes with the anthocyanin cyanidin 3-O-glucoside has been demonstrated to protect against a wide array of UVB-induced damage (J. Agric. Food Chem. 2006;54:4041-7).
Proanthocyanidins: Pycnogenol
Investigators studied pycnogenol in an antioxidant mixture that also included evening primrose and vitamins C and E. After 10 weeks of oral administration to female SKH-1 hairless mice exposed to UVB irradiation three times weekly, the mixture was found to significantly inhibit wrinkle formation by suppressing UVB-induced matrix metalloproteinase activity while promoting collagen production (Photodermatol. Photoimmunol. Photomed. 2007;23:155-62).
Tannins: Ellagic Acid
In a double-blind, placebo-controlled, 4-week trial, investigators assessed the effects of orally administered ellagic acid-rich pomegranate extract on the pigmentation of 13 women after UV exposure. Healthy volunteers were randomly assigned to high-dose, low-dose, and control groups. The results showed that luminance values decreased by 1.73% in the high-dose group and 1.35% in the low-dose group, compared with the control group, and stains and freckles also were diminished (J. Nutr. Sci. Vitaminol. (Tokyo) 2006;52:383-8).
Stilbenes: Resveratrol
The antioxidant potency of resveratrol has been cited for conferring a wide range of salutary effects, including antitumorigenic and antiaging activity. Recently, a resveratrol-based skin care formulation intended to combat photoaging was reported to exhibit 17-fold greater antioxidant activity than idebenone (J. Cosmet. Dermatol. 2008;7:2-7). In a different study, resveratrol, the primary active polyphenolic constituent in red wine, was assessed in terms of topical/transdermal delivery viability, given the previously established benefits shown via systemic administration. Several hydrogel systems used as resveratrol vehicles were shown to be safe and effective methods for cutaneously delivering the therapeutic effects of this antioxidant (Biol. Pharm. Bull. 2008;31:955-62).
Phenolic Acids: Ferulic Acid
In a small study, a stable formulation of 15% L-corbic acid, 1% alpha-tocopherol, and 0.5% ferulic acid was applied topically to normal-appearing human skin for 4 days, and was found to confer significant photoprotection against solar-simulated UV radiation. The preparation was especially effective at diminishing thymine dimer mutations, which are linked to skin cancer. The authors also noted that the mechanism of action of this antioxidant formulation differs from that of sunscreens and, therefore, may serve as a supplement to such products (J. Am. Acad. Dermatol. 2008;59:418-25). It is worth noting that ferulic acid has been approved as a sunscreen agent in Japan (J. Pharm. Biomed. Anal. 2008;46:645-52).
Conclusion
A brief survey of the polyphenolic landscape obviously cannot do the subject justice. That said, from the dermatologic perspective, it is simply worth noting how often this diverse family of compounds factors occur in to the skin care formulations that are becoming more prevalent in the established armamentarium as well as the direct-to-consumer market.
Given the increasing attention paid here and elsewhere to the impact of diet on the skin, the status of the diverse class of polyphenolic compounds found in a wide array of plants, which includes several antioxidants, appears to be well deserved and warrants much more research.