User login
Walk the Talk: VA Mental Health Care Professionals’ Role in Promoting Physical Activity
Physical activity is a key determinant of health. Low levels of activity are associated with onset of and poorer outcomes of many chronic health conditions (eg, obesity, coronary artery disease, type 2 diabetes mellitus, chronic pain, hypertension1-4) and with higher rates of mental health conditions (eg, depression, anxiety5-8).
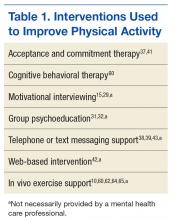
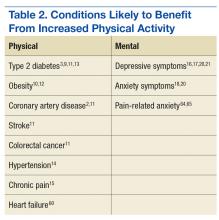
Behavioral interventions (Table 1) can increase activity and improve physical health and mental health (Table 2).9-21 However, only 20% of adults in the U.S. meet federal recommendations for physical activity.22 The situation is particularly grim in the veteran population. Littman and colleagues found that veterans were less likely than nonveterans were to meet physical activity standards, and VA patients were even less likely than were non-VA veterans to meet the recommendations.23
Given that exercise can positively affect physical and mental health and that VA mental health care professionals (MHCPs) have training in motivational enhancement and behavior modification, these clinicians are well positioned to intervene. The question arises, though: How can VA MHCPs do more to effectively promote physical activity in veterans?
Addressing Physical Activity
There are numerous ways in which VA MHCPs can address physical activity with their patients. Several studies have demonstrated that physical activity interventions provided within primary care–mental health integration programs resulted in increased physical activity.28,29 The number of VA health care providers (HCPs) offering such programs is increasing, which could mean that behavioral health support for physical activity promotion could become easier for veterans to access.30
In addition, National Center for Health Promotion and Disease Prevention initiatives have led to an expansion of programs, such as the VA MOVE! Weight Management Program.31 Often cofacilitated by dieticians and MHCPs, MOVE! includes nutrition education, behavior modification, and physical activity promotion.32 Preliminary research suggests that MOVE! helps veterans lose weight and improve their health-related quality of life.33-36
Further, psychological and behavioral interventions can specifically target exercise and have been shown to increase physical activity, improve mood symptoms, and reduce health risk factors.9-21,37 However, little is known about the extent of exercise promotion in VA outpatient mental health services. For instance, some HCPs may educate patients about the benefits of physical activity, while others may facilitate physical activity scheduling, address barriers, and monitor, reinforce, and problem-solve physical activity goals.
Research also has supported the efficacy of technology-based interventions in physical activity promotion by MHCPs. These interventions include phone counseling, text messaging or smartphone application monitoring systems (including the MOVE! Coach mobile app), DVD-based approaches, and web-based interventions.38-42 However, these interventions may be most effective when complemented with face-to-face support (eg, psychotherapy, nutrition/exercise classes).43 Although MHCPs can promote physical activity in various ways, intensive focus on this target is not standard practice in many mental health care settings.
Barriers to Physical Activity
Despite physical activity promotion efforts, patients struggle to implement and maintain physical activity recommendations.22,44,45 For many patients, exercise is a new or long abandoned activity, and instruction on how to exercise properly is needed.46 Lack of financial resources may limit access to a gym, trainer, or physical therapist.47 Some patients avoid exercise because of body image concerns, and many think they lack the self-discipline and time for exercise.46,48,49
Additional barriers to physical activity are pain, fatigue, and other physical symptoms.50-52 Obese patients may find physical activity less enjoyable and more uncomfortable.53 Some patients fear exercise will exacerbate medical problems or have negative physical consequences.51,52
Psychiatric symptoms and medication adverse effects are commonly reported barriers.54 Some patients with anxiety avoid physical activity because the resulting physiologic sensations (eg, rapid heart rate, sweating) are similar to anxiety symptoms.55 Patients with posttraumatic stress disorder (PTSD) are less likely to exercise, secondary to PTSD-related avoidance, even though they were physically active before their trauma.56-58 Some patients with depression avoid exercise and other activities because their symptoms (eg, fatigue, anhedonia) make it difficult for them to take action. Many patients put off exercise while waiting for relief of mental health symptoms, even though evidence suggests that physical activity may help improve those symptoms.5,6
These barriers often render ineffective the approach of simply recommending exercise or encouraging patients to exercise. Counseling alone may not be sufficient to effect meaningful change in exercise habits. Many effective physical activity interventions have both a counseling and exercise components,59-61 and research suggests that such interventions may be most effective when they include a form of experiential exercise.10
Clinician-Assisted Experiential Exercise
Exercise interventions may involve information dissemination, counseling, an experiential exercise program, or a combination of these activities. Research has yet to determine precisely which components are most effective. Given the barriers to adhering to exercise recommendations, however, exercise interventions that include an experiential component may be more likely to affect behavior change.
According to Sime, exercise therapy is the “practice of combining a program of exercise with traditional psychotherapy.”62 Sime outlined a 10-session approach to exercise therapy and suggested that walking with patients while engaging in psychotherapy can reduce barriers to change. This approach may be effective for several reasons. First, it models the recommendation to engage in activity despite not feeling well and often improves mood. Second, the experiential nature of the intervention gives the patient an immediate opportunity to physically feel the benefits of activity. Third, the experiential component is similar to experiential exercise interventions, which have been shown to improve chronic health problems, such as obesity, and it parallels in vivo exposure, which is highly effective in treating anxiety.10,63
Exposure to exercise also has been effective in treating chronic pain in patients who fear physical activity because they anticipate pain or reinjury. In patients with chronic low back pain, in vivo exposure reduced anxiety more than an education-only session did, and the result was improved participation in relevant daily activities.64 Results were sustained at the 6-month follow-up but only for patients who received in vivo exposure.65 Similarly, in vivo exposure to feared movements increased physical activity and reduced pain-related fear, catastrophizing, and disability in patients with chronic low back pain.65 These findings have implications for other chronic health problems. Particularly for patients who fear and avoid exercise, psychoeducation about exercise and opportunities to experience exercise in session may increase physical activity outside of therapy.10
Obstacles to Exercise Promotion
Mental health care providers may be reluctant to use experiential exercise interventions for a variety of reasons. Some fear that they or their patients might sustain an injury or an exacerbation of physical symptoms. In addition, some MHCPs have liability and safety concerns surrounding meetings with patients outside the office. And obtaining medical clearance requires extra time and energy.
Some MHCPs think that this type of experiential activity might cross a professional boundary. Others may wonder whether providing experiential exercise as part of mental health services is sufficiently evidence based or is a breach of standards of practice. Similarly, some MHCPs who use manual-based interventions are hesitant to stray from an evidence-based protocol and include experiential exercise in psychotherapy. Further, some MHCPs do not feel competent to provide such an intervention, given that it is not typically covered in their mental health care training, and they think that providing opportunities for experiential exercise falls outside their MHCP role. Last, some MHCPs are uncomfortable exercising on their own and thus may be particularly uncomfortable exercising in front of patients.
Promoting Physical Activity
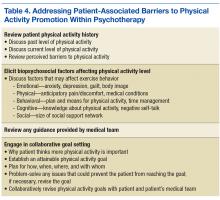
Although significant, barriers to promotion of physical activity can be effectively reduced by taking the steps outlined in Table 3. First, MHCPs must reflect on their own past and present physical activity and on their readiness to provide clinician-assisted experiential exercise. In addition, MHCPs should explore nearby alternative resources for physical activity, share their findings with patients, and encourage patients to use these resources. Next, medical clearance for increased physical activity can be obtained from patients’ primary care physicians, and any physical activity recommendations or limitations can be reviewed and documented. Mental health care providers should then obtain patients’ informed consent, which involves discussing the potential risks and benefits of increased exercise and, if appropriate, collaborate with patients to reach an agreement to focus on physical activity as an important aspect of their work together. Any additional risks and benefits of clinician-assisted experiential exercise can be discussed, and the ways in which physical activity can be used in session (eg, “walk and talk therapy”; other exercises recommended by the medical team) can be reviewed. Further, MHCPs can clarify their role and discuss how clear boundaries will be maintained within the therapeutic relationship. Alternative VA and community services that can help increase physical activity should also be discussed.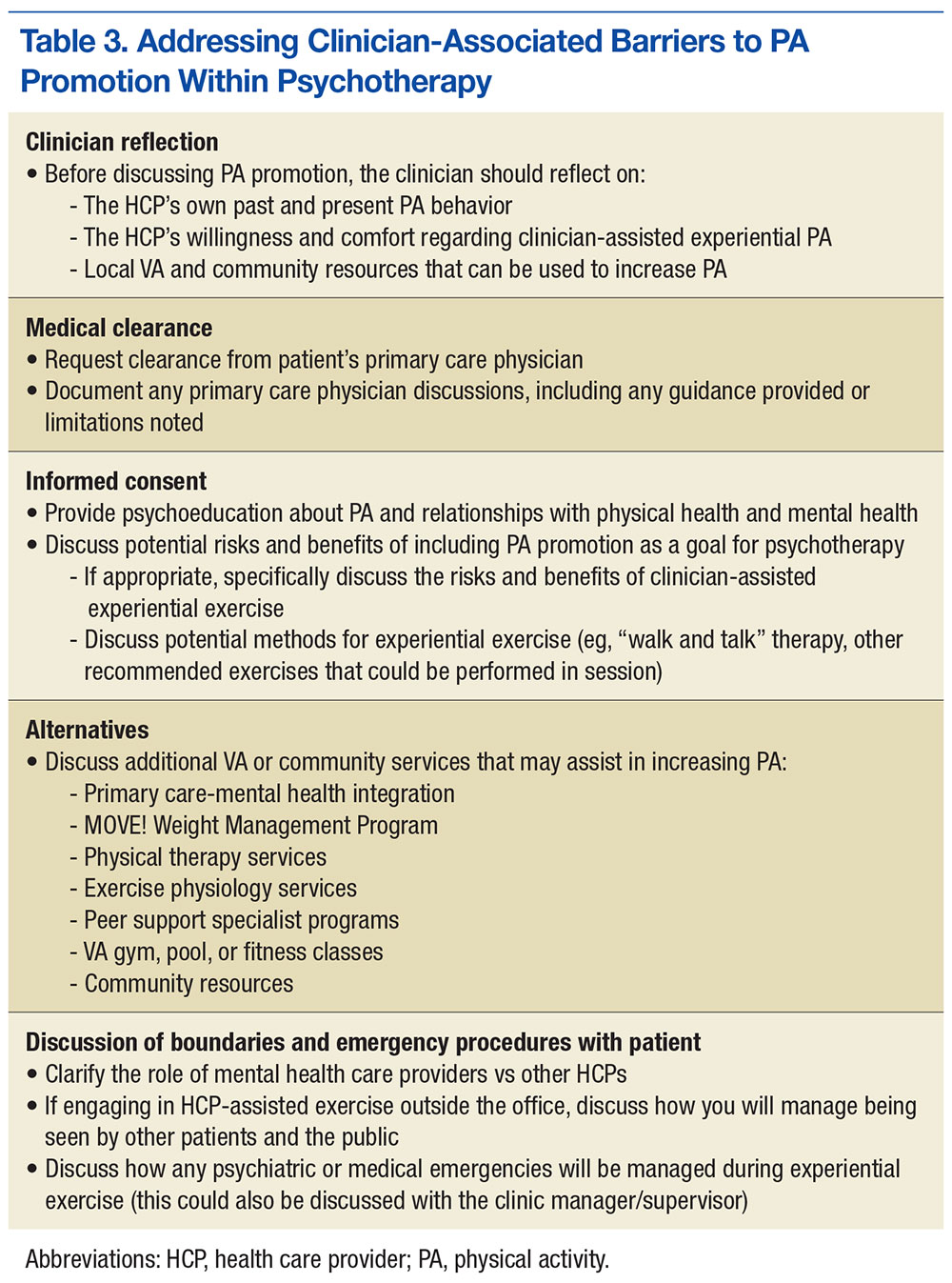
Once these steps are complete, MHCPs can address patient’s barriers to physical activity (Table 4). A discussion of the patient’s physical activity history is a good starting point. Biopsychosocial factors that can affect the ability to engage in and follow through with physical activity can then be explored, and HCPs and patients can set specific attainable physical activity goals. For instance, MHCPs can specify whether in-session clinic-assisted experiential exercise will be used and, if so, in what capacity. Last, physical activity goals can be revised periodically and revisited with the medical team.
Alternate Promotions
Mental health care providers also should consider involving other HCPs. Physical therapists and exercise physiologists are in a unique position to provide experiential exercise training. Some VA facilities include experiential exercise in their MOVE! program—veterans exercise together in the VA’s physical therapy gym while being monitored by a physical therapist.
Peer support specialists (PSPs) also are in a unique position to effectively provide experiential physical activity interventions at VA facilities. These PSPs are veterans who have physical or mental health problems but are far enough along in recovery to provide helpful services to other veterans with similar challenges.66 Recent organizational efforts have increased the presence of PSPs in VA clinics. Peer support specialists use aspects of their recovery to help other veterans, provide supportive counseling, and facilitate activity groups, such as walking, hiking, golfing, and photography groups. Further, PSPs may not have to deal with MHCPs’ concerns regarding scope of practice and clinical boundaries vis-à-vis exercise interventions.
Other VA and community programs provide ways for veterans to engage in experiential physical activities. Some VA facilities have pools and gyms that provide open hours for veterans; some even offer free HCP guidance. Clinics also occasionally provide transportation to community gyms that offer veterans discounted memberships. Team Red, White, and Blue (https://www.teamrwb.org), Veterans Expeditions, (http://www.vetexpeditions.com) and other community organizations promote veterans’ physical activity by organizing events, such as endurance races, fly fishing, and mountaineering. By staying up-to-date on local community services, MHCPs can facilitate opportunities for experiential exercise alongside the psychotherapy services they provide.
Although valuable resources exist, veterans nevertheless encounter obstacles to exercise. For instance, many VA HCPs do not include physical therapy as a standard part of the MOVE! program. Others offer physical therapy not as an integrated service but as a separate, optional service, and attendance requires more initiative. Often, veterans are referred for physical therapy only if they have sustained an injury. Even when physical therapy or exercise physiology services are offered, many veterans have difficulty following through. Reasons include anxiety, time constraints, difficulty managing multiple appointments, and negative beliefs about exercise and physical therapy (eg, it will make me hurt, physical therapy is only for people recovering from an injury). Last, some veterans are reluctant to engage in peer-led or non-VA exercise programs.
Future Research
This article highlights the need for research in several areas. First, it would be helpful to know the extent to which VA MHCPs are already promoting physical activity for their patients and the ways in which they are using experiential exercise interventions. Research also will help determine the extent to which experiential exercise interventions can be effective in treating mental and physical health conditions not listed in Table 2 and any conditions for which exercise interventions may be contraindicated. The effectiveness of exercise therapy, as described by Sime, also warrants more investigation with randomized clinical trials.62 Further, it would be useful to know more about the extent and effectiveness of other experiential exercise available to veterans, whether through the MOVE! program or through other VA or community resources. This would help HCPs understand how to best promote physical activity in veterans with chronic physical and mental health needs.
Conclusion
Most people fall short of recommended levels of physical activity, and this is especially true of veterans, who also are at higher risk for chronic physical and mental health problems.23,24 VA MHCPs are in a unique position to promote physical activity, and therapy programs that include experiential exercise may be particularly effective in helping veterans become and stay active. Other providers are well suited to provide experiential exercise opportunities, but MHCPs can simultaneously address the psychological factors that prevent veterans from engaging in exercise. Although VA MHCPs should continue to collaborate with other resources that can provide experiential exercise, they should also consider the potential benefit of experiential exercise within psychotherapy.
1. Turi BC, Codogno JS, Fernandes RA, Monteiro HL. Physical activity, adiposity and hypertension among patients of public healthcare system [in English, Portuguese]. Rev Bras Epidemiol. 2014;17(4):925-937.
2. Press V, Freestone I, George CF. Physical activity: the evidence of benefit in the prevention of coronary heart disease. QJM. 2003;96(4):245-251.
3. Gill JM, Cooper AR. Physical activity and prevention of type 2 diabetes mellitus. Sports Med. 2008;38(10):807-824.
4. Landmark T, Romundstad P, Borchgrevink PC, Kaasa S, Dale O. Associations between recreational exercise and chronic pain in the general population: evidence from the HUNT 3 study. Pain. 2011;152(10):2241-2247.
5. Brunes A, Augestad L, Gudmundsdottir S. Personality, physical activity, and symptoms of anxiety and depression: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):745-756.
6. De Mello MT, Lemos Vde A, Antunes HK, Bittencourt L, Santos-Silva R, Tufik S. Relationship between physical activity and depression and anxiety symptoms: a population study. J Affect Disord. 2013;149(1-3):241-246.
7. Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698-703.
8. Teixeira CM, Vasconcelos-Raposo J, Fernandes HM, Brustad RJ. Physical activity, depression and anxiety among the elderly. Soc Indic Res. 2013;113(1):307-318.
9. Avery L, Flynn D, Dombrowski SU, van Wersch A, Sniehotta FF, Trenell MI. Successful behavioural strategies to increase physical activity and improve glucose control in adults with type 2 diabetes. Diabet Med. 2015;32(8):1058-1062.
10. Craighead LW, Blum MD. Supervised exercise in behavioral treatment for moderate obesity. Behav Ther. 1989;20(1):49-59.
11. Gulliford MC, Charlton J, Bhattarai N, Charlton C, Rudisill C. Impact and cost-effectiveness of a universal strategy to promote physical activity in primary care: population-based cohort study and Markov model. Eur J Health Econ. 2014;15(4):341-351.
12. Muda SH, Kadir AA. The effectiveness of physical activity counseling in primary care clinic University Science Malaysia Hospital. Int Med J. 2006;13(4):249-253.
13. Plotnikoff RC, Pickering MA, Glenn N, et al. The effects of a supplemental, theory-based physical activity counseling intervention for adults with type 2 diabetes. J Phys Act Health. 2011;8(7):944-954.
14. Semlitsch T, Jeitler K, Hemkens LG, et al. Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis. Sports Med. 2013;43(10):1009-1023.
15. Tse MM, Vong SK, Tang SK. Motivational interviewing and exercise programme for community-dwelling older persons with chronic pain: a randomised controlled study. J Clin Nurs. 2013;22(13-14):1843-1856.
16. Babyak M, Blumenthal JA, Herman S et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
17. Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159(19):2349-2356.
18. Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224-231.
19. Lee C, Russell A. Effects of physical activity on emotional well-being among older Australian women: cross-sectional and longitudinal analyses. J Psychosom Res. 2003;54(2):155-160.
20. Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. 2008;62(suppl 47):25-29.
21. Phillips WT, Kiernan M, King AC. Physical activity as a nonpharmacological treatment for depression: a review. Complement Health Pract Rev. 2003;8(2):1-14.
22. Centers for Disease Control and Prevention. Facts about physical activity. http://www.cdc.gov/physicalactivity/data/facts.htm. Updated May 23, 2014. Accessed August 22, 2016.
23. Littman AJ, Forsberg CW, Koepsell TD. Physical activity in a national sample of veterans. Med Sci Sports Exerc. 2009;41(5):1006-1013.
24. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: United States, 2007–2010. NCHS Data Brief. http://www.cdc.gov/nchs/data/databriefs/db101.pdf. Published August 2012. Accessed August 22, 2016.
25. Zulman DM, Pal Chee C, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open. 2015;5(4):e007771.
26. Yu W, Ravelo A, Wagner TH, et al. Prevalence and costs of chronic conditions in the VA Health Care System. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
27. Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276(18):1473-1479.
28. Gagliardi AR, Abdallah F, Faulkner G, Ciliska D, Hicks A. Factors contributing to the effectiveness of physical activity counselling in primary care: a realist systematic review. Patient Educ Couns. 2015;98(4):412-419.
29. Hardcastle S, Blake N, Hagger M. The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J Behav Med. 2012;35(3):318-333.
30. Johnson-Lawrence V, Zivin K, Szymanski BR, Pfeiffer PN, McCarthy JF. VA primary care–mental health integration: patient characteristics and receipt of mental health services, 2008–2010. Psychiatr Serv. 2012;63(11):1137-1141.
31. U.S. Department of Veterans Affairs. MOVE! weight management program. http://www.move.va.gov. Updated August 1, 2016. Accessed August 22, 2016.
32. Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! Weight-Management Program for veterans. Prev Chronic Dis. 2009;6(3):A98.
33. Dahn JR, Fitzpatrick SL, Llabre MM, et al. Weight management for veterans: examining change in weight before and after MOVE! Obesity (Silver Spring). 2011;19(5):977-981.
34. Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1(4):551-560.
35. Taft TH, Payvar S, Wool L. Effectiveness of the MOVE! program among African American veterans: weight loss and quality of life. Fed Pract. 2011;28(12):17-24.
36. Kahwati LC, Lewis MA, Kane H, et al. Best practices in the Veterans Health Administration’s MOVE! weight management program. Am J Prev Med. 2011;41(5):457-464.
37. Butryn M, Forman E, Hoffman K, Shaw J, Juarascio A. A pilot study of acceptance and commitment therapy for promotion of physical activity. J Phys Act Health. 2011;8(4):516-522.
38. Green BB, McAfee T, Hindmarsh M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med. 2002;22(3):177-183.
39. Prestwich A, Perugini M, Hurling R. Can the effects of implementation intentions on exercise be enhanced using text messages? Psychol Health. 2009;24(6):677-687.
40. U.S. Department of Veterans Affairs. What is MOVE! Coach? http://www.move.va.gov/moveCoachIntro.asp. Updated May 26, 2016. Accessed September 6, 2016.
41. Moffitt R, Mohr P. The efficacy of a self-managed acceptance and commitment therapy intervention DVD for physical activity initiation. Br J Health Psychol. 2015;20(1):115-129.
42. Duncan M, Vandelanotte C, Kolt GS, et al. Effectiveness of a web- and mobile phone–based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. J Med Internet Res. 2014;16(6):e136.
43. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320-329.
44. Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382.
45. Stevinson C, Lydon A, Amir Z. Adherence to physical activity guidelines among cancer support group participants. Eur J Cancer Care (Engl). 2014;23(2):199-205.
46. Spector D, Battaglini C, Groff D. Perceived exercise barriers and facilitators among ethnically diverse breast cancer survivors. Oncol Nurs Forum. 2013;40(5):472-480.
47. Daly JM, Hartz AJ, Xu Y, et al. An assessment of attitudes, behaviors, and outcomes of patients with type 2 diabetes. J Am Board Fam Med. 2009;22(3):280-290.
48. Bautista L, Reininger B, Gay JL, Barroso CS, McCormick JB. Perceived barriers to exercise in Hispanic adults by level of activity. J Phys Act Health. 2011;8(7):916-925.
49. Asano M, Duquette P, Andersen R, Lapierre Y, Mayo N. Exercise barriers and preferences among women and men with multiple sclerosis. Disabil Rehabil. 2013;35(5):353-361.
50. Hefferon K, Murphy H, McLeod J, Mutrie N, Campbell A. Understanding barriers to exercise implementation 5-year post–breast cancer diagnosis: a large-scale qualitative study. Health Educ Res. 2013;28(5):843-856.
51. Crombez G, Vlaeyen J, Heuts P, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1-2):329-339.
52. Rogerson M, Murphy BM, Bird S, Morris T. “I don’t have the heart”: a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140.
53. Leone LA, Ward DS. A mixed methods comparison of perceived benefits and barriers to exercise between obese and nonobese women. J Phys Act Health. 2013;10(4):461-469.
54. Glover C, Ferron J, Whitley R. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J. 2013;36(1):45-47.
55. Sabourin B, Hilchey C, Lefaivre M, Watt M, Stewart S. Why do they exercise less? Barriers to exercise in high-anxiety-sensitive women. Cogn Behav Ther. 2011;40(3):206-215.
56. Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103-115.
57. LeardMann CA, Kelton ML, Smith B, et al; Millennium Cohort Study Team. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126(3):371-383.
58. de Assis MA, de Mello MF, Scorza FA, et al. Evaluation of physical activity habits in patients with posttraumatic stress disorder. Clinics (Sao Paulo). 2008;63(4):473-478.
59. Jimmy G, Martin BW. Implementation and effectiveness of a primary care based physical activity counselling scheme. Patient Educ Couns. 2005;56(3):323-331.
60. Gary RA, Dunbar SB, Higgins MK, Musselman DL, Smith AL. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. J Psychosom Res. 2010;69(2):119-131.
61. van Koulil S, van Lankveld W, Kraaimaat FW, et al. Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res (Hoboken). 2010;62(10):1377-1385.
62. Sime WE. Exercise therapy for stress management. In: Lehrer PM, Woolfolk RL, Sime WE, eds. Principles and Practice of Stress Management. 3rd ed. New York, NY: Guilford Press; 2007:333-359.
63. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences, Therapist Guide. New York, NY: Oxford University Press; 2007.
64. de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21(1):9-17.
65. Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18(4):251-261.
66. Chinman M, Young A, Hassell J, Davidson L. Toward the implementation of mental health consumer provider services. J Behav Health Serv Res. 2006;33(2):176-195.
Physical activity is a key determinant of health. Low levels of activity are associated with onset of and poorer outcomes of many chronic health conditions (eg, obesity, coronary artery disease, type 2 diabetes mellitus, chronic pain, hypertension1-4) and with higher rates of mental health conditions (eg, depression, anxiety5-8).
Behavioral interventions (Table 1) can increase activity and improve physical health and mental health (Table 2).9-21 However, only 20% of adults in the U.S. meet federal recommendations for physical activity.22 The situation is particularly grim in the veteran population. Littman and colleagues found that veterans were less likely than nonveterans were to meet physical activity standards, and VA patients were even less likely than were non-VA veterans to meet the recommendations.23
Given that exercise can positively affect physical and mental health and that VA mental health care professionals (MHCPs) have training in motivational enhancement and behavior modification, these clinicians are well positioned to intervene. The question arises, though: How can VA MHCPs do more to effectively promote physical activity in veterans?
Addressing Physical Activity
There are numerous ways in which VA MHCPs can address physical activity with their patients. Several studies have demonstrated that physical activity interventions provided within primary care–mental health integration programs resulted in increased physical activity.28,29 The number of VA health care providers (HCPs) offering such programs is increasing, which could mean that behavioral health support for physical activity promotion could become easier for veterans to access.30
In addition, National Center for Health Promotion and Disease Prevention initiatives have led to an expansion of programs, such as the VA MOVE! Weight Management Program.31 Often cofacilitated by dieticians and MHCPs, MOVE! includes nutrition education, behavior modification, and physical activity promotion.32 Preliminary research suggests that MOVE! helps veterans lose weight and improve their health-related quality of life.33-36
Further, psychological and behavioral interventions can specifically target exercise and have been shown to increase physical activity, improve mood symptoms, and reduce health risk factors.9-21,37 However, little is known about the extent of exercise promotion in VA outpatient mental health services. For instance, some HCPs may educate patients about the benefits of physical activity, while others may facilitate physical activity scheduling, address barriers, and monitor, reinforce, and problem-solve physical activity goals.
Research also has supported the efficacy of technology-based interventions in physical activity promotion by MHCPs. These interventions include phone counseling, text messaging or smartphone application monitoring systems (including the MOVE! Coach mobile app), DVD-based approaches, and web-based interventions.38-42 However, these interventions may be most effective when complemented with face-to-face support (eg, psychotherapy, nutrition/exercise classes).43 Although MHCPs can promote physical activity in various ways, intensive focus on this target is not standard practice in many mental health care settings.
Barriers to Physical Activity
Despite physical activity promotion efforts, patients struggle to implement and maintain physical activity recommendations.22,44,45 For many patients, exercise is a new or long abandoned activity, and instruction on how to exercise properly is needed.46 Lack of financial resources may limit access to a gym, trainer, or physical therapist.47 Some patients avoid exercise because of body image concerns, and many think they lack the self-discipline and time for exercise.46,48,49
Additional barriers to physical activity are pain, fatigue, and other physical symptoms.50-52 Obese patients may find physical activity less enjoyable and more uncomfortable.53 Some patients fear exercise will exacerbate medical problems or have negative physical consequences.51,52
Psychiatric symptoms and medication adverse effects are commonly reported barriers.54 Some patients with anxiety avoid physical activity because the resulting physiologic sensations (eg, rapid heart rate, sweating) are similar to anxiety symptoms.55 Patients with posttraumatic stress disorder (PTSD) are less likely to exercise, secondary to PTSD-related avoidance, even though they were physically active before their trauma.56-58 Some patients with depression avoid exercise and other activities because their symptoms (eg, fatigue, anhedonia) make it difficult for them to take action. Many patients put off exercise while waiting for relief of mental health symptoms, even though evidence suggests that physical activity may help improve those symptoms.5,6
These barriers often render ineffective the approach of simply recommending exercise or encouraging patients to exercise. Counseling alone may not be sufficient to effect meaningful change in exercise habits. Many effective physical activity interventions have both a counseling and exercise components,59-61 and research suggests that such interventions may be most effective when they include a form of experiential exercise.10
Clinician-Assisted Experiential Exercise
Exercise interventions may involve information dissemination, counseling, an experiential exercise program, or a combination of these activities. Research has yet to determine precisely which components are most effective. Given the barriers to adhering to exercise recommendations, however, exercise interventions that include an experiential component may be more likely to affect behavior change.
According to Sime, exercise therapy is the “practice of combining a program of exercise with traditional psychotherapy.”62 Sime outlined a 10-session approach to exercise therapy and suggested that walking with patients while engaging in psychotherapy can reduce barriers to change. This approach may be effective for several reasons. First, it models the recommendation to engage in activity despite not feeling well and often improves mood. Second, the experiential nature of the intervention gives the patient an immediate opportunity to physically feel the benefits of activity. Third, the experiential component is similar to experiential exercise interventions, which have been shown to improve chronic health problems, such as obesity, and it parallels in vivo exposure, which is highly effective in treating anxiety.10,63
Exposure to exercise also has been effective in treating chronic pain in patients who fear physical activity because they anticipate pain or reinjury. In patients with chronic low back pain, in vivo exposure reduced anxiety more than an education-only session did, and the result was improved participation in relevant daily activities.64 Results were sustained at the 6-month follow-up but only for patients who received in vivo exposure.65 Similarly, in vivo exposure to feared movements increased physical activity and reduced pain-related fear, catastrophizing, and disability in patients with chronic low back pain.65 These findings have implications for other chronic health problems. Particularly for patients who fear and avoid exercise, psychoeducation about exercise and opportunities to experience exercise in session may increase physical activity outside of therapy.10
Obstacles to Exercise Promotion
Mental health care providers may be reluctant to use experiential exercise interventions for a variety of reasons. Some fear that they or their patients might sustain an injury or an exacerbation of physical symptoms. In addition, some MHCPs have liability and safety concerns surrounding meetings with patients outside the office. And obtaining medical clearance requires extra time and energy.
Some MHCPs think that this type of experiential activity might cross a professional boundary. Others may wonder whether providing experiential exercise as part of mental health services is sufficiently evidence based or is a breach of standards of practice. Similarly, some MHCPs who use manual-based interventions are hesitant to stray from an evidence-based protocol and include experiential exercise in psychotherapy. Further, some MHCPs do not feel competent to provide such an intervention, given that it is not typically covered in their mental health care training, and they think that providing opportunities for experiential exercise falls outside their MHCP role. Last, some MHCPs are uncomfortable exercising on their own and thus may be particularly uncomfortable exercising in front of patients.
Promoting Physical Activity
Although significant, barriers to promotion of physical activity can be effectively reduced by taking the steps outlined in Table 3. First, MHCPs must reflect on their own past and present physical activity and on their readiness to provide clinician-assisted experiential exercise. In addition, MHCPs should explore nearby alternative resources for physical activity, share their findings with patients, and encourage patients to use these resources. Next, medical clearance for increased physical activity can be obtained from patients’ primary care physicians, and any physical activity recommendations or limitations can be reviewed and documented. Mental health care providers should then obtain patients’ informed consent, which involves discussing the potential risks and benefits of increased exercise and, if appropriate, collaborate with patients to reach an agreement to focus on physical activity as an important aspect of their work together. Any additional risks and benefits of clinician-assisted experiential exercise can be discussed, and the ways in which physical activity can be used in session (eg, “walk and talk therapy”; other exercises recommended by the medical team) can be reviewed. Further, MHCPs can clarify their role and discuss how clear boundaries will be maintained within the therapeutic relationship. Alternative VA and community services that can help increase physical activity should also be discussed.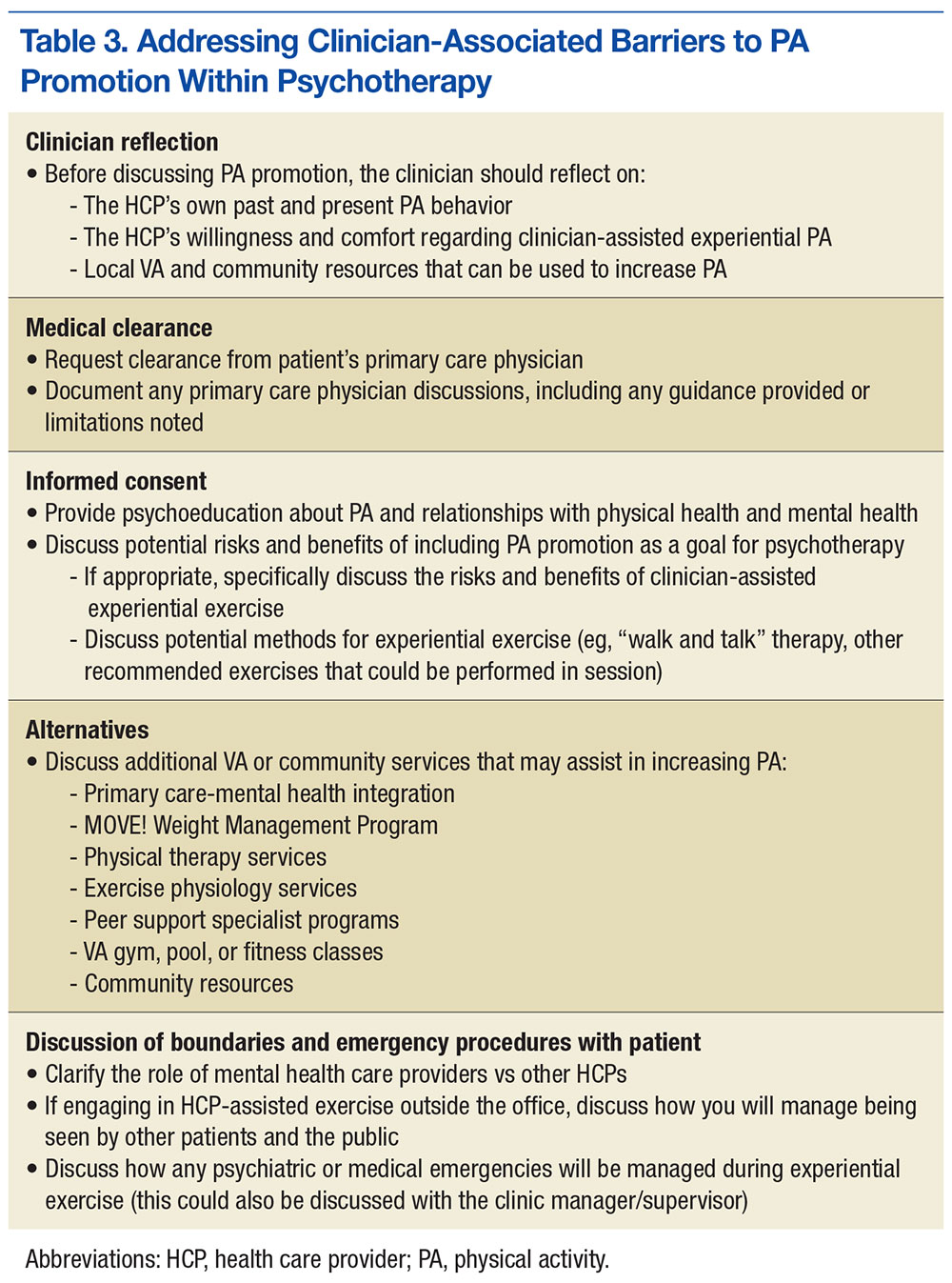
Once these steps are complete, MHCPs can address patient’s barriers to physical activity (Table 4). A discussion of the patient’s physical activity history is a good starting point. Biopsychosocial factors that can affect the ability to engage in and follow through with physical activity can then be explored, and HCPs and patients can set specific attainable physical activity goals. For instance, MHCPs can specify whether in-session clinic-assisted experiential exercise will be used and, if so, in what capacity. Last, physical activity goals can be revised periodically and revisited with the medical team.
Alternate Promotions
Mental health care providers also should consider involving other HCPs. Physical therapists and exercise physiologists are in a unique position to provide experiential exercise training. Some VA facilities include experiential exercise in their MOVE! program—veterans exercise together in the VA’s physical therapy gym while being monitored by a physical therapist.
Peer support specialists (PSPs) also are in a unique position to effectively provide experiential physical activity interventions at VA facilities. These PSPs are veterans who have physical or mental health problems but are far enough along in recovery to provide helpful services to other veterans with similar challenges.66 Recent organizational efforts have increased the presence of PSPs in VA clinics. Peer support specialists use aspects of their recovery to help other veterans, provide supportive counseling, and facilitate activity groups, such as walking, hiking, golfing, and photography groups. Further, PSPs may not have to deal with MHCPs’ concerns regarding scope of practice and clinical boundaries vis-à-vis exercise interventions.
Other VA and community programs provide ways for veterans to engage in experiential physical activities. Some VA facilities have pools and gyms that provide open hours for veterans; some even offer free HCP guidance. Clinics also occasionally provide transportation to community gyms that offer veterans discounted memberships. Team Red, White, and Blue (https://www.teamrwb.org), Veterans Expeditions, (http://www.vetexpeditions.com) and other community organizations promote veterans’ physical activity by organizing events, such as endurance races, fly fishing, and mountaineering. By staying up-to-date on local community services, MHCPs can facilitate opportunities for experiential exercise alongside the psychotherapy services they provide.
Although valuable resources exist, veterans nevertheless encounter obstacles to exercise. For instance, many VA HCPs do not include physical therapy as a standard part of the MOVE! program. Others offer physical therapy not as an integrated service but as a separate, optional service, and attendance requires more initiative. Often, veterans are referred for physical therapy only if they have sustained an injury. Even when physical therapy or exercise physiology services are offered, many veterans have difficulty following through. Reasons include anxiety, time constraints, difficulty managing multiple appointments, and negative beliefs about exercise and physical therapy (eg, it will make me hurt, physical therapy is only for people recovering from an injury). Last, some veterans are reluctant to engage in peer-led or non-VA exercise programs.
Future Research
This article highlights the need for research in several areas. First, it would be helpful to know the extent to which VA MHCPs are already promoting physical activity for their patients and the ways in which they are using experiential exercise interventions. Research also will help determine the extent to which experiential exercise interventions can be effective in treating mental and physical health conditions not listed in Table 2 and any conditions for which exercise interventions may be contraindicated. The effectiveness of exercise therapy, as described by Sime, also warrants more investigation with randomized clinical trials.62 Further, it would be useful to know more about the extent and effectiveness of other experiential exercise available to veterans, whether through the MOVE! program or through other VA or community resources. This would help HCPs understand how to best promote physical activity in veterans with chronic physical and mental health needs.
Conclusion
Most people fall short of recommended levels of physical activity, and this is especially true of veterans, who also are at higher risk for chronic physical and mental health problems.23,24 VA MHCPs are in a unique position to promote physical activity, and therapy programs that include experiential exercise may be particularly effective in helping veterans become and stay active. Other providers are well suited to provide experiential exercise opportunities, but MHCPs can simultaneously address the psychological factors that prevent veterans from engaging in exercise. Although VA MHCPs should continue to collaborate with other resources that can provide experiential exercise, they should also consider the potential benefit of experiential exercise within psychotherapy.
Physical activity is a key determinant of health. Low levels of activity are associated with onset of and poorer outcomes of many chronic health conditions (eg, obesity, coronary artery disease, type 2 diabetes mellitus, chronic pain, hypertension1-4) and with higher rates of mental health conditions (eg, depression, anxiety5-8).
Behavioral interventions (Table 1) can increase activity and improve physical health and mental health (Table 2).9-21 However, only 20% of adults in the U.S. meet federal recommendations for physical activity.22 The situation is particularly grim in the veteran population. Littman and colleagues found that veterans were less likely than nonveterans were to meet physical activity standards, and VA patients were even less likely than were non-VA veterans to meet the recommendations.23
Given that exercise can positively affect physical and mental health and that VA mental health care professionals (MHCPs) have training in motivational enhancement and behavior modification, these clinicians are well positioned to intervene. The question arises, though: How can VA MHCPs do more to effectively promote physical activity in veterans?
Addressing Physical Activity
There are numerous ways in which VA MHCPs can address physical activity with their patients. Several studies have demonstrated that physical activity interventions provided within primary care–mental health integration programs resulted in increased physical activity.28,29 The number of VA health care providers (HCPs) offering such programs is increasing, which could mean that behavioral health support for physical activity promotion could become easier for veterans to access.30
In addition, National Center for Health Promotion and Disease Prevention initiatives have led to an expansion of programs, such as the VA MOVE! Weight Management Program.31 Often cofacilitated by dieticians and MHCPs, MOVE! includes nutrition education, behavior modification, and physical activity promotion.32 Preliminary research suggests that MOVE! helps veterans lose weight and improve their health-related quality of life.33-36
Further, psychological and behavioral interventions can specifically target exercise and have been shown to increase physical activity, improve mood symptoms, and reduce health risk factors.9-21,37 However, little is known about the extent of exercise promotion in VA outpatient mental health services. For instance, some HCPs may educate patients about the benefits of physical activity, while others may facilitate physical activity scheduling, address barriers, and monitor, reinforce, and problem-solve physical activity goals.
Research also has supported the efficacy of technology-based interventions in physical activity promotion by MHCPs. These interventions include phone counseling, text messaging or smartphone application monitoring systems (including the MOVE! Coach mobile app), DVD-based approaches, and web-based interventions.38-42 However, these interventions may be most effective when complemented with face-to-face support (eg, psychotherapy, nutrition/exercise classes).43 Although MHCPs can promote physical activity in various ways, intensive focus on this target is not standard practice in many mental health care settings.
Barriers to Physical Activity
Despite physical activity promotion efforts, patients struggle to implement and maintain physical activity recommendations.22,44,45 For many patients, exercise is a new or long abandoned activity, and instruction on how to exercise properly is needed.46 Lack of financial resources may limit access to a gym, trainer, or physical therapist.47 Some patients avoid exercise because of body image concerns, and many think they lack the self-discipline and time for exercise.46,48,49
Additional barriers to physical activity are pain, fatigue, and other physical symptoms.50-52 Obese patients may find physical activity less enjoyable and more uncomfortable.53 Some patients fear exercise will exacerbate medical problems or have negative physical consequences.51,52
Psychiatric symptoms and medication adverse effects are commonly reported barriers.54 Some patients with anxiety avoid physical activity because the resulting physiologic sensations (eg, rapid heart rate, sweating) are similar to anxiety symptoms.55 Patients with posttraumatic stress disorder (PTSD) are less likely to exercise, secondary to PTSD-related avoidance, even though they were physically active before their trauma.56-58 Some patients with depression avoid exercise and other activities because their symptoms (eg, fatigue, anhedonia) make it difficult for them to take action. Many patients put off exercise while waiting for relief of mental health symptoms, even though evidence suggests that physical activity may help improve those symptoms.5,6
These barriers often render ineffective the approach of simply recommending exercise or encouraging patients to exercise. Counseling alone may not be sufficient to effect meaningful change in exercise habits. Many effective physical activity interventions have both a counseling and exercise components,59-61 and research suggests that such interventions may be most effective when they include a form of experiential exercise.10
Clinician-Assisted Experiential Exercise
Exercise interventions may involve information dissemination, counseling, an experiential exercise program, or a combination of these activities. Research has yet to determine precisely which components are most effective. Given the barriers to adhering to exercise recommendations, however, exercise interventions that include an experiential component may be more likely to affect behavior change.
According to Sime, exercise therapy is the “practice of combining a program of exercise with traditional psychotherapy.”62 Sime outlined a 10-session approach to exercise therapy and suggested that walking with patients while engaging in psychotherapy can reduce barriers to change. This approach may be effective for several reasons. First, it models the recommendation to engage in activity despite not feeling well and often improves mood. Second, the experiential nature of the intervention gives the patient an immediate opportunity to physically feel the benefits of activity. Third, the experiential component is similar to experiential exercise interventions, which have been shown to improve chronic health problems, such as obesity, and it parallels in vivo exposure, which is highly effective in treating anxiety.10,63
Exposure to exercise also has been effective in treating chronic pain in patients who fear physical activity because they anticipate pain or reinjury. In patients with chronic low back pain, in vivo exposure reduced anxiety more than an education-only session did, and the result was improved participation in relevant daily activities.64 Results were sustained at the 6-month follow-up but only for patients who received in vivo exposure.65 Similarly, in vivo exposure to feared movements increased physical activity and reduced pain-related fear, catastrophizing, and disability in patients with chronic low back pain.65 These findings have implications for other chronic health problems. Particularly for patients who fear and avoid exercise, psychoeducation about exercise and opportunities to experience exercise in session may increase physical activity outside of therapy.10
Obstacles to Exercise Promotion
Mental health care providers may be reluctant to use experiential exercise interventions for a variety of reasons. Some fear that they or their patients might sustain an injury or an exacerbation of physical symptoms. In addition, some MHCPs have liability and safety concerns surrounding meetings with patients outside the office. And obtaining medical clearance requires extra time and energy.
Some MHCPs think that this type of experiential activity might cross a professional boundary. Others may wonder whether providing experiential exercise as part of mental health services is sufficiently evidence based or is a breach of standards of practice. Similarly, some MHCPs who use manual-based interventions are hesitant to stray from an evidence-based protocol and include experiential exercise in psychotherapy. Further, some MHCPs do not feel competent to provide such an intervention, given that it is not typically covered in their mental health care training, and they think that providing opportunities for experiential exercise falls outside their MHCP role. Last, some MHCPs are uncomfortable exercising on their own and thus may be particularly uncomfortable exercising in front of patients.
Promoting Physical Activity
Although significant, barriers to promotion of physical activity can be effectively reduced by taking the steps outlined in Table 3. First, MHCPs must reflect on their own past and present physical activity and on their readiness to provide clinician-assisted experiential exercise. In addition, MHCPs should explore nearby alternative resources for physical activity, share their findings with patients, and encourage patients to use these resources. Next, medical clearance for increased physical activity can be obtained from patients’ primary care physicians, and any physical activity recommendations or limitations can be reviewed and documented. Mental health care providers should then obtain patients’ informed consent, which involves discussing the potential risks and benefits of increased exercise and, if appropriate, collaborate with patients to reach an agreement to focus on physical activity as an important aspect of their work together. Any additional risks and benefits of clinician-assisted experiential exercise can be discussed, and the ways in which physical activity can be used in session (eg, “walk and talk therapy”; other exercises recommended by the medical team) can be reviewed. Further, MHCPs can clarify their role and discuss how clear boundaries will be maintained within the therapeutic relationship. Alternative VA and community services that can help increase physical activity should also be discussed.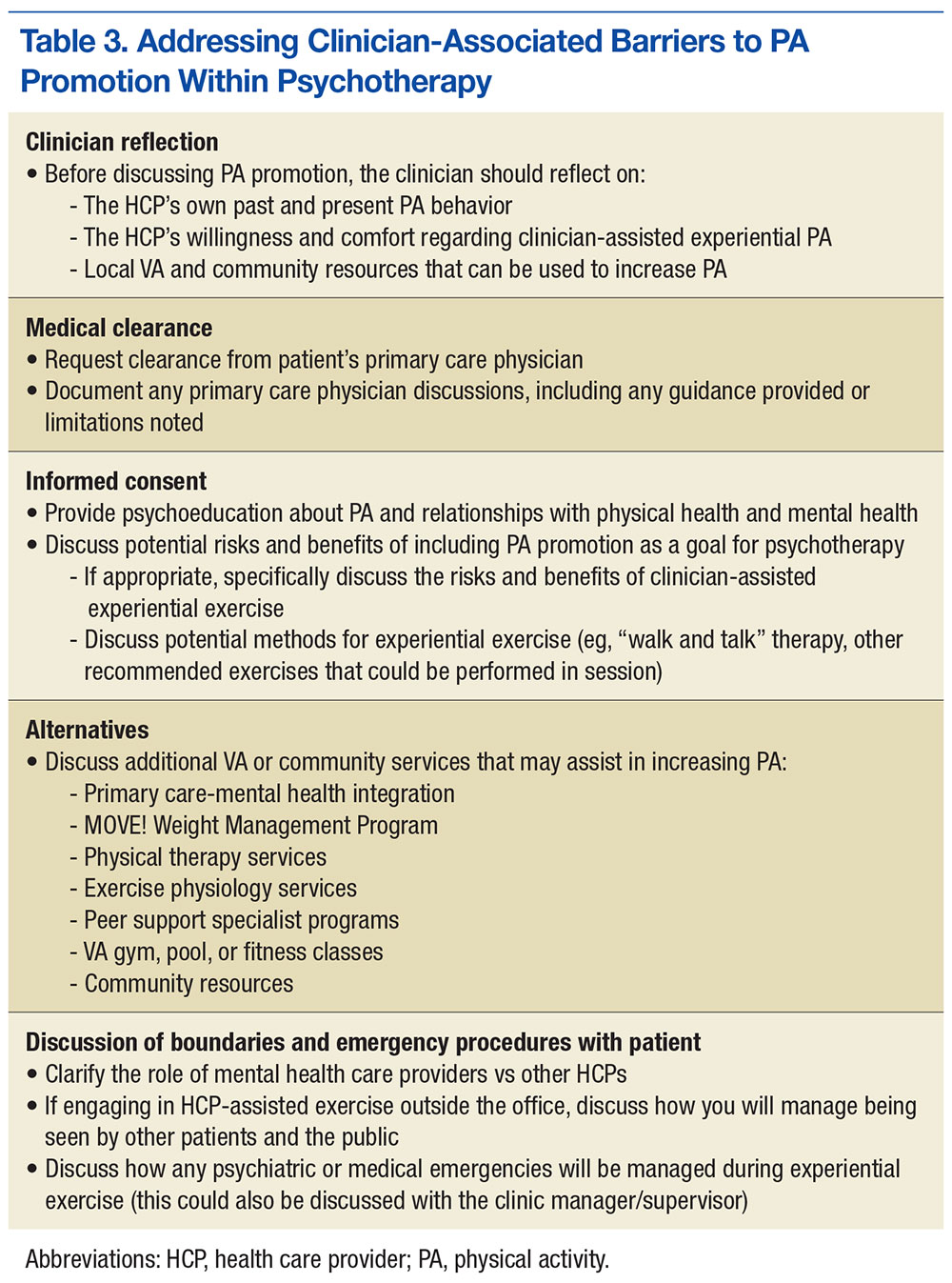
Once these steps are complete, MHCPs can address patient’s barriers to physical activity (Table 4). A discussion of the patient’s physical activity history is a good starting point. Biopsychosocial factors that can affect the ability to engage in and follow through with physical activity can then be explored, and HCPs and patients can set specific attainable physical activity goals. For instance, MHCPs can specify whether in-session clinic-assisted experiential exercise will be used and, if so, in what capacity. Last, physical activity goals can be revised periodically and revisited with the medical team.
Alternate Promotions
Mental health care providers also should consider involving other HCPs. Physical therapists and exercise physiologists are in a unique position to provide experiential exercise training. Some VA facilities include experiential exercise in their MOVE! program—veterans exercise together in the VA’s physical therapy gym while being monitored by a physical therapist.
Peer support specialists (PSPs) also are in a unique position to effectively provide experiential physical activity interventions at VA facilities. These PSPs are veterans who have physical or mental health problems but are far enough along in recovery to provide helpful services to other veterans with similar challenges.66 Recent organizational efforts have increased the presence of PSPs in VA clinics. Peer support specialists use aspects of their recovery to help other veterans, provide supportive counseling, and facilitate activity groups, such as walking, hiking, golfing, and photography groups. Further, PSPs may not have to deal with MHCPs’ concerns regarding scope of practice and clinical boundaries vis-à-vis exercise interventions.
Other VA and community programs provide ways for veterans to engage in experiential physical activities. Some VA facilities have pools and gyms that provide open hours for veterans; some even offer free HCP guidance. Clinics also occasionally provide transportation to community gyms that offer veterans discounted memberships. Team Red, White, and Blue (https://www.teamrwb.org), Veterans Expeditions, (http://www.vetexpeditions.com) and other community organizations promote veterans’ physical activity by organizing events, such as endurance races, fly fishing, and mountaineering. By staying up-to-date on local community services, MHCPs can facilitate opportunities for experiential exercise alongside the psychotherapy services they provide.
Although valuable resources exist, veterans nevertheless encounter obstacles to exercise. For instance, many VA HCPs do not include physical therapy as a standard part of the MOVE! program. Others offer physical therapy not as an integrated service but as a separate, optional service, and attendance requires more initiative. Often, veterans are referred for physical therapy only if they have sustained an injury. Even when physical therapy or exercise physiology services are offered, many veterans have difficulty following through. Reasons include anxiety, time constraints, difficulty managing multiple appointments, and negative beliefs about exercise and physical therapy (eg, it will make me hurt, physical therapy is only for people recovering from an injury). Last, some veterans are reluctant to engage in peer-led or non-VA exercise programs.
Future Research
This article highlights the need for research in several areas. First, it would be helpful to know the extent to which VA MHCPs are already promoting physical activity for their patients and the ways in which they are using experiential exercise interventions. Research also will help determine the extent to which experiential exercise interventions can be effective in treating mental and physical health conditions not listed in Table 2 and any conditions for which exercise interventions may be contraindicated. The effectiveness of exercise therapy, as described by Sime, also warrants more investigation with randomized clinical trials.62 Further, it would be useful to know more about the extent and effectiveness of other experiential exercise available to veterans, whether through the MOVE! program or through other VA or community resources. This would help HCPs understand how to best promote physical activity in veterans with chronic physical and mental health needs.
Conclusion
Most people fall short of recommended levels of physical activity, and this is especially true of veterans, who also are at higher risk for chronic physical and mental health problems.23,24 VA MHCPs are in a unique position to promote physical activity, and therapy programs that include experiential exercise may be particularly effective in helping veterans become and stay active. Other providers are well suited to provide experiential exercise opportunities, but MHCPs can simultaneously address the psychological factors that prevent veterans from engaging in exercise. Although VA MHCPs should continue to collaborate with other resources that can provide experiential exercise, they should also consider the potential benefit of experiential exercise within psychotherapy.
1. Turi BC, Codogno JS, Fernandes RA, Monteiro HL. Physical activity, adiposity and hypertension among patients of public healthcare system [in English, Portuguese]. Rev Bras Epidemiol. 2014;17(4):925-937.
2. Press V, Freestone I, George CF. Physical activity: the evidence of benefit in the prevention of coronary heart disease. QJM. 2003;96(4):245-251.
3. Gill JM, Cooper AR. Physical activity and prevention of type 2 diabetes mellitus. Sports Med. 2008;38(10):807-824.
4. Landmark T, Romundstad P, Borchgrevink PC, Kaasa S, Dale O. Associations between recreational exercise and chronic pain in the general population: evidence from the HUNT 3 study. Pain. 2011;152(10):2241-2247.
5. Brunes A, Augestad L, Gudmundsdottir S. Personality, physical activity, and symptoms of anxiety and depression: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):745-756.
6. De Mello MT, Lemos Vde A, Antunes HK, Bittencourt L, Santos-Silva R, Tufik S. Relationship between physical activity and depression and anxiety symptoms: a population study. J Affect Disord. 2013;149(1-3):241-246.
7. Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698-703.
8. Teixeira CM, Vasconcelos-Raposo J, Fernandes HM, Brustad RJ. Physical activity, depression and anxiety among the elderly. Soc Indic Res. 2013;113(1):307-318.
9. Avery L, Flynn D, Dombrowski SU, van Wersch A, Sniehotta FF, Trenell MI. Successful behavioural strategies to increase physical activity and improve glucose control in adults with type 2 diabetes. Diabet Med. 2015;32(8):1058-1062.
10. Craighead LW, Blum MD. Supervised exercise in behavioral treatment for moderate obesity. Behav Ther. 1989;20(1):49-59.
11. Gulliford MC, Charlton J, Bhattarai N, Charlton C, Rudisill C. Impact and cost-effectiveness of a universal strategy to promote physical activity in primary care: population-based cohort study and Markov model. Eur J Health Econ. 2014;15(4):341-351.
12. Muda SH, Kadir AA. The effectiveness of physical activity counseling in primary care clinic University Science Malaysia Hospital. Int Med J. 2006;13(4):249-253.
13. Plotnikoff RC, Pickering MA, Glenn N, et al. The effects of a supplemental, theory-based physical activity counseling intervention for adults with type 2 diabetes. J Phys Act Health. 2011;8(7):944-954.
14. Semlitsch T, Jeitler K, Hemkens LG, et al. Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis. Sports Med. 2013;43(10):1009-1023.
15. Tse MM, Vong SK, Tang SK. Motivational interviewing and exercise programme for community-dwelling older persons with chronic pain: a randomised controlled study. J Clin Nurs. 2013;22(13-14):1843-1856.
16. Babyak M, Blumenthal JA, Herman S et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
17. Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159(19):2349-2356.
18. Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224-231.
19. Lee C, Russell A. Effects of physical activity on emotional well-being among older Australian women: cross-sectional and longitudinal analyses. J Psychosom Res. 2003;54(2):155-160.
20. Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. 2008;62(suppl 47):25-29.
21. Phillips WT, Kiernan M, King AC. Physical activity as a nonpharmacological treatment for depression: a review. Complement Health Pract Rev. 2003;8(2):1-14.
22. Centers for Disease Control and Prevention. Facts about physical activity. http://www.cdc.gov/physicalactivity/data/facts.htm. Updated May 23, 2014. Accessed August 22, 2016.
23. Littman AJ, Forsberg CW, Koepsell TD. Physical activity in a national sample of veterans. Med Sci Sports Exerc. 2009;41(5):1006-1013.
24. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: United States, 2007–2010. NCHS Data Brief. http://www.cdc.gov/nchs/data/databriefs/db101.pdf. Published August 2012. Accessed August 22, 2016.
25. Zulman DM, Pal Chee C, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open. 2015;5(4):e007771.
26. Yu W, Ravelo A, Wagner TH, et al. Prevalence and costs of chronic conditions in the VA Health Care System. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
27. Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276(18):1473-1479.
28. Gagliardi AR, Abdallah F, Faulkner G, Ciliska D, Hicks A. Factors contributing to the effectiveness of physical activity counselling in primary care: a realist systematic review. Patient Educ Couns. 2015;98(4):412-419.
29. Hardcastle S, Blake N, Hagger M. The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J Behav Med. 2012;35(3):318-333.
30. Johnson-Lawrence V, Zivin K, Szymanski BR, Pfeiffer PN, McCarthy JF. VA primary care–mental health integration: patient characteristics and receipt of mental health services, 2008–2010. Psychiatr Serv. 2012;63(11):1137-1141.
31. U.S. Department of Veterans Affairs. MOVE! weight management program. http://www.move.va.gov. Updated August 1, 2016. Accessed August 22, 2016.
32. Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! Weight-Management Program for veterans. Prev Chronic Dis. 2009;6(3):A98.
33. Dahn JR, Fitzpatrick SL, Llabre MM, et al. Weight management for veterans: examining change in weight before and after MOVE! Obesity (Silver Spring). 2011;19(5):977-981.
34. Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1(4):551-560.
35. Taft TH, Payvar S, Wool L. Effectiveness of the MOVE! program among African American veterans: weight loss and quality of life. Fed Pract. 2011;28(12):17-24.
36. Kahwati LC, Lewis MA, Kane H, et al. Best practices in the Veterans Health Administration’s MOVE! weight management program. Am J Prev Med. 2011;41(5):457-464.
37. Butryn M, Forman E, Hoffman K, Shaw J, Juarascio A. A pilot study of acceptance and commitment therapy for promotion of physical activity. J Phys Act Health. 2011;8(4):516-522.
38. Green BB, McAfee T, Hindmarsh M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med. 2002;22(3):177-183.
39. Prestwich A, Perugini M, Hurling R. Can the effects of implementation intentions on exercise be enhanced using text messages? Psychol Health. 2009;24(6):677-687.
40. U.S. Department of Veterans Affairs. What is MOVE! Coach? http://www.move.va.gov/moveCoachIntro.asp. Updated May 26, 2016. Accessed September 6, 2016.
41. Moffitt R, Mohr P. The efficacy of a self-managed acceptance and commitment therapy intervention DVD for physical activity initiation. Br J Health Psychol. 2015;20(1):115-129.
42. Duncan M, Vandelanotte C, Kolt GS, et al. Effectiveness of a web- and mobile phone–based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. J Med Internet Res. 2014;16(6):e136.
43. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320-329.
44. Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382.
45. Stevinson C, Lydon A, Amir Z. Adherence to physical activity guidelines among cancer support group participants. Eur J Cancer Care (Engl). 2014;23(2):199-205.
46. Spector D, Battaglini C, Groff D. Perceived exercise barriers and facilitators among ethnically diverse breast cancer survivors. Oncol Nurs Forum. 2013;40(5):472-480.
47. Daly JM, Hartz AJ, Xu Y, et al. An assessment of attitudes, behaviors, and outcomes of patients with type 2 diabetes. J Am Board Fam Med. 2009;22(3):280-290.
48. Bautista L, Reininger B, Gay JL, Barroso CS, McCormick JB. Perceived barriers to exercise in Hispanic adults by level of activity. J Phys Act Health. 2011;8(7):916-925.
49. Asano M, Duquette P, Andersen R, Lapierre Y, Mayo N. Exercise barriers and preferences among women and men with multiple sclerosis. Disabil Rehabil. 2013;35(5):353-361.
50. Hefferon K, Murphy H, McLeod J, Mutrie N, Campbell A. Understanding barriers to exercise implementation 5-year post–breast cancer diagnosis: a large-scale qualitative study. Health Educ Res. 2013;28(5):843-856.
51. Crombez G, Vlaeyen J, Heuts P, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1-2):329-339.
52. Rogerson M, Murphy BM, Bird S, Morris T. “I don’t have the heart”: a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140.
53. Leone LA, Ward DS. A mixed methods comparison of perceived benefits and barriers to exercise between obese and nonobese women. J Phys Act Health. 2013;10(4):461-469.
54. Glover C, Ferron J, Whitley R. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J. 2013;36(1):45-47.
55. Sabourin B, Hilchey C, Lefaivre M, Watt M, Stewart S. Why do they exercise less? Barriers to exercise in high-anxiety-sensitive women. Cogn Behav Ther. 2011;40(3):206-215.
56. Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103-115.
57. LeardMann CA, Kelton ML, Smith B, et al; Millennium Cohort Study Team. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126(3):371-383.
58. de Assis MA, de Mello MF, Scorza FA, et al. Evaluation of physical activity habits in patients with posttraumatic stress disorder. Clinics (Sao Paulo). 2008;63(4):473-478.
59. Jimmy G, Martin BW. Implementation and effectiveness of a primary care based physical activity counselling scheme. Patient Educ Couns. 2005;56(3):323-331.
60. Gary RA, Dunbar SB, Higgins MK, Musselman DL, Smith AL. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. J Psychosom Res. 2010;69(2):119-131.
61. van Koulil S, van Lankveld W, Kraaimaat FW, et al. Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res (Hoboken). 2010;62(10):1377-1385.
62. Sime WE. Exercise therapy for stress management. In: Lehrer PM, Woolfolk RL, Sime WE, eds. Principles and Practice of Stress Management. 3rd ed. New York, NY: Guilford Press; 2007:333-359.
63. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences, Therapist Guide. New York, NY: Oxford University Press; 2007.
64. de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21(1):9-17.
65. Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18(4):251-261.
66. Chinman M, Young A, Hassell J, Davidson L. Toward the implementation of mental health consumer provider services. J Behav Health Serv Res. 2006;33(2):176-195.
1. Turi BC, Codogno JS, Fernandes RA, Monteiro HL. Physical activity, adiposity and hypertension among patients of public healthcare system [in English, Portuguese]. Rev Bras Epidemiol. 2014;17(4):925-937.
2. Press V, Freestone I, George CF. Physical activity: the evidence of benefit in the prevention of coronary heart disease. QJM. 2003;96(4):245-251.
3. Gill JM, Cooper AR. Physical activity and prevention of type 2 diabetes mellitus. Sports Med. 2008;38(10):807-824.
4. Landmark T, Romundstad P, Borchgrevink PC, Kaasa S, Dale O. Associations between recreational exercise and chronic pain in the general population: evidence from the HUNT 3 study. Pain. 2011;152(10):2241-2247.
5. Brunes A, Augestad L, Gudmundsdottir S. Personality, physical activity, and symptoms of anxiety and depression: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2013;48(5):745-756.
6. De Mello MT, Lemos Vde A, Antunes HK, Bittencourt L, Santos-Silva R, Tufik S. Relationship between physical activity and depression and anxiety symptoms: a population study. J Affect Disord. 2013;149(1-3):241-246.
7. Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36(6):698-703.
8. Teixeira CM, Vasconcelos-Raposo J, Fernandes HM, Brustad RJ. Physical activity, depression and anxiety among the elderly. Soc Indic Res. 2013;113(1):307-318.
9. Avery L, Flynn D, Dombrowski SU, van Wersch A, Sniehotta FF, Trenell MI. Successful behavioural strategies to increase physical activity and improve glucose control in adults with type 2 diabetes. Diabet Med. 2015;32(8):1058-1062.
10. Craighead LW, Blum MD. Supervised exercise in behavioral treatment for moderate obesity. Behav Ther. 1989;20(1):49-59.
11. Gulliford MC, Charlton J, Bhattarai N, Charlton C, Rudisill C. Impact and cost-effectiveness of a universal strategy to promote physical activity in primary care: population-based cohort study and Markov model. Eur J Health Econ. 2014;15(4):341-351.
12. Muda SH, Kadir AA. The effectiveness of physical activity counseling in primary care clinic University Science Malaysia Hospital. Int Med J. 2006;13(4):249-253.
13. Plotnikoff RC, Pickering MA, Glenn N, et al. The effects of a supplemental, theory-based physical activity counseling intervention for adults with type 2 diabetes. J Phys Act Health. 2011;8(7):944-954.
14. Semlitsch T, Jeitler K, Hemkens LG, et al. Increasing physical activity for the treatment of hypertension: a systematic review and meta-analysis. Sports Med. 2013;43(10):1009-1023.
15. Tse MM, Vong SK, Tang SK. Motivational interviewing and exercise programme for community-dwelling older persons with chronic pain: a randomised controlled study. J Clin Nurs. 2013;22(13-14):1843-1856.
16. Babyak M, Blumenthal JA, Herman S et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62(5):633-638.
17. Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159(19):2349-2356.
18. Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224-231.
19. Lee C, Russell A. Effects of physical activity on emotional well-being among older Australian women: cross-sectional and longitudinal analyses. J Psychosom Res. 2003;54(2):155-160.
20. Martinsen EW. Physical activity in the prevention and treatment of anxiety and depression. Nord J Psychiatry. 2008;62(suppl 47):25-29.
21. Phillips WT, Kiernan M, King AC. Physical activity as a nonpharmacological treatment for depression: a review. Complement Health Pract Rev. 2003;8(2):1-14.
22. Centers for Disease Control and Prevention. Facts about physical activity. http://www.cdc.gov/physicalactivity/data/facts.htm. Updated May 23, 2014. Accessed August 22, 2016.
23. Littman AJ, Forsberg CW, Koepsell TD. Physical activity in a national sample of veterans. Med Sci Sports Exerc. 2009;41(5):1006-1013.
24. Kramarow EA, Pastor PN. The health of male veterans and nonveterans aged 25–64: United States, 2007–2010. NCHS Data Brief. http://www.cdc.gov/nchs/data/databriefs/db101.pdf. Published August 2012. Accessed August 22, 2016.
25. Zulman DM, Pal Chee C, Wagner TH, et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open. 2015;5(4):e007771.
26. Yu W, Ravelo A, Wagner TH, et al. Prevalence and costs of chronic conditions in the VA Health Care System. Med Care Res Rev. 2003;60(suppl 3):146S-167S.
27. Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276(18):1473-1479.
28. Gagliardi AR, Abdallah F, Faulkner G, Ciliska D, Hicks A. Factors contributing to the effectiveness of physical activity counselling in primary care: a realist systematic review. Patient Educ Couns. 2015;98(4):412-419.
29. Hardcastle S, Blake N, Hagger M. The effectiveness of a motivational interviewing primary-care based intervention on physical activity and predictors of change in a disadvantaged community. J Behav Med. 2012;35(3):318-333.
30. Johnson-Lawrence V, Zivin K, Szymanski BR, Pfeiffer PN, McCarthy JF. VA primary care–mental health integration: patient characteristics and receipt of mental health services, 2008–2010. Psychiatr Serv. 2012;63(11):1137-1141.
31. U.S. Department of Veterans Affairs. MOVE! weight management program. http://www.move.va.gov. Updated August 1, 2016. Accessed August 22, 2016.
32. Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! Weight-Management Program for veterans. Prev Chronic Dis. 2009;6(3):A98.
33. Dahn JR, Fitzpatrick SL, Llabre MM, et al. Weight management for veterans: examining change in weight before and after MOVE! Obesity (Silver Spring). 2011;19(5):977-981.
34. Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1(4):551-560.
35. Taft TH, Payvar S, Wool L. Effectiveness of the MOVE! program among African American veterans: weight loss and quality of life. Fed Pract. 2011;28(12):17-24.
36. Kahwati LC, Lewis MA, Kane H, et al. Best practices in the Veterans Health Administration’s MOVE! weight management program. Am J Prev Med. 2011;41(5):457-464.
37. Butryn M, Forman E, Hoffman K, Shaw J, Juarascio A. A pilot study of acceptance and commitment therapy for promotion of physical activity. J Phys Act Health. 2011;8(4):516-522.
38. Green BB, McAfee T, Hindmarsh M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med. 2002;22(3):177-183.
39. Prestwich A, Perugini M, Hurling R. Can the effects of implementation intentions on exercise be enhanced using text messages? Psychol Health. 2009;24(6):677-687.
40. U.S. Department of Veterans Affairs. What is MOVE! Coach? http://www.move.va.gov/moveCoachIntro.asp. Updated May 26, 2016. Accessed September 6, 2016.
41. Moffitt R, Mohr P. The efficacy of a self-managed acceptance and commitment therapy intervention DVD for physical activity initiation. Br J Health Psychol. 2015;20(1):115-129.
42. Duncan M, Vandelanotte C, Kolt GS, et al. Effectiveness of a web- and mobile phone–based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. J Med Internet Res. 2014;16(6):e136.
43. Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320-329.
44. Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382.
45. Stevinson C, Lydon A, Amir Z. Adherence to physical activity guidelines among cancer support group participants. Eur J Cancer Care (Engl). 2014;23(2):199-205.
46. Spector D, Battaglini C, Groff D. Perceived exercise barriers and facilitators among ethnically diverse breast cancer survivors. Oncol Nurs Forum. 2013;40(5):472-480.
47. Daly JM, Hartz AJ, Xu Y, et al. An assessment of attitudes, behaviors, and outcomes of patients with type 2 diabetes. J Am Board Fam Med. 2009;22(3):280-290.
48. Bautista L, Reininger B, Gay JL, Barroso CS, McCormick JB. Perceived barriers to exercise in Hispanic adults by level of activity. J Phys Act Health. 2011;8(7):916-925.
49. Asano M, Duquette P, Andersen R, Lapierre Y, Mayo N. Exercise barriers and preferences among women and men with multiple sclerosis. Disabil Rehabil. 2013;35(5):353-361.
50. Hefferon K, Murphy H, McLeod J, Mutrie N, Campbell A. Understanding barriers to exercise implementation 5-year post–breast cancer diagnosis: a large-scale qualitative study. Health Educ Res. 2013;28(5):843-856.
51. Crombez G, Vlaeyen J, Heuts P, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80(1-2):329-339.
52. Rogerson M, Murphy BM, Bird S, Morris T. “I don’t have the heart”: a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140.
53. Leone LA, Ward DS. A mixed methods comparison of perceived benefits and barriers to exercise between obese and nonobese women. J Phys Act Health. 2013;10(4):461-469.
54. Glover C, Ferron J, Whitley R. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J. 2013;36(1):45-47.
55. Sabourin B, Hilchey C, Lefaivre M, Watt M, Stewart S. Why do they exercise less? Barriers to exercise in high-anxiety-sensitive women. Cogn Behav Ther. 2011;40(3):206-215.
56. Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103-115.
57. LeardMann CA, Kelton ML, Smith B, et al; Millennium Cohort Study Team. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126(3):371-383.
58. de Assis MA, de Mello MF, Scorza FA, et al. Evaluation of physical activity habits in patients with posttraumatic stress disorder. Clinics (Sao Paulo). 2008;63(4):473-478.
59. Jimmy G, Martin BW. Implementation and effectiveness of a primary care based physical activity counselling scheme. Patient Educ Couns. 2005;56(3):323-331.
60. Gary RA, Dunbar SB, Higgins MK, Musselman DL, Smith AL. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. J Psychosom Res. 2010;69(2):119-131.
61. van Koulil S, van Lankveld W, Kraaimaat FW, et al. Tailored cognitive-behavioral therapy and exercise training for high-risk patients with fibromyalgia. Arthritis Care Res (Hoboken). 2010;62(10):1377-1385.
62. Sime WE. Exercise therapy for stress management. In: Lehrer PM, Woolfolk RL, Sime WE, eds. Principles and Practice of Stress Management. 3rd ed. New York, NY: Guilford Press; 2007:333-359.
63. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences, Therapist Guide. New York, NY: Oxford University Press; 2007.
64. de Jong JR, Vlaeyen JW, Onghena P, Goossens ME, Geilen M, Mulder H. Fear of movement/(re)injury in chronic low back pain: education or exposure in vivo as mediator to fear reduction? Clin J Pain. 2005;21(1):9-17.
65. Vlaeyen JW, de Jong J, Geilen M, Heuts PH, van Breukelen G. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain. 2002;18(4):251-261.
66. Chinman M, Young A, Hassell J, Davidson L. Toward the implementation of mental health consumer provider services. J Behav Health Serv Res. 2006;33(2):176-195.