User login
Severe right upper chest pain • tender right sternoclavicular joint • Dx?
THE CASE
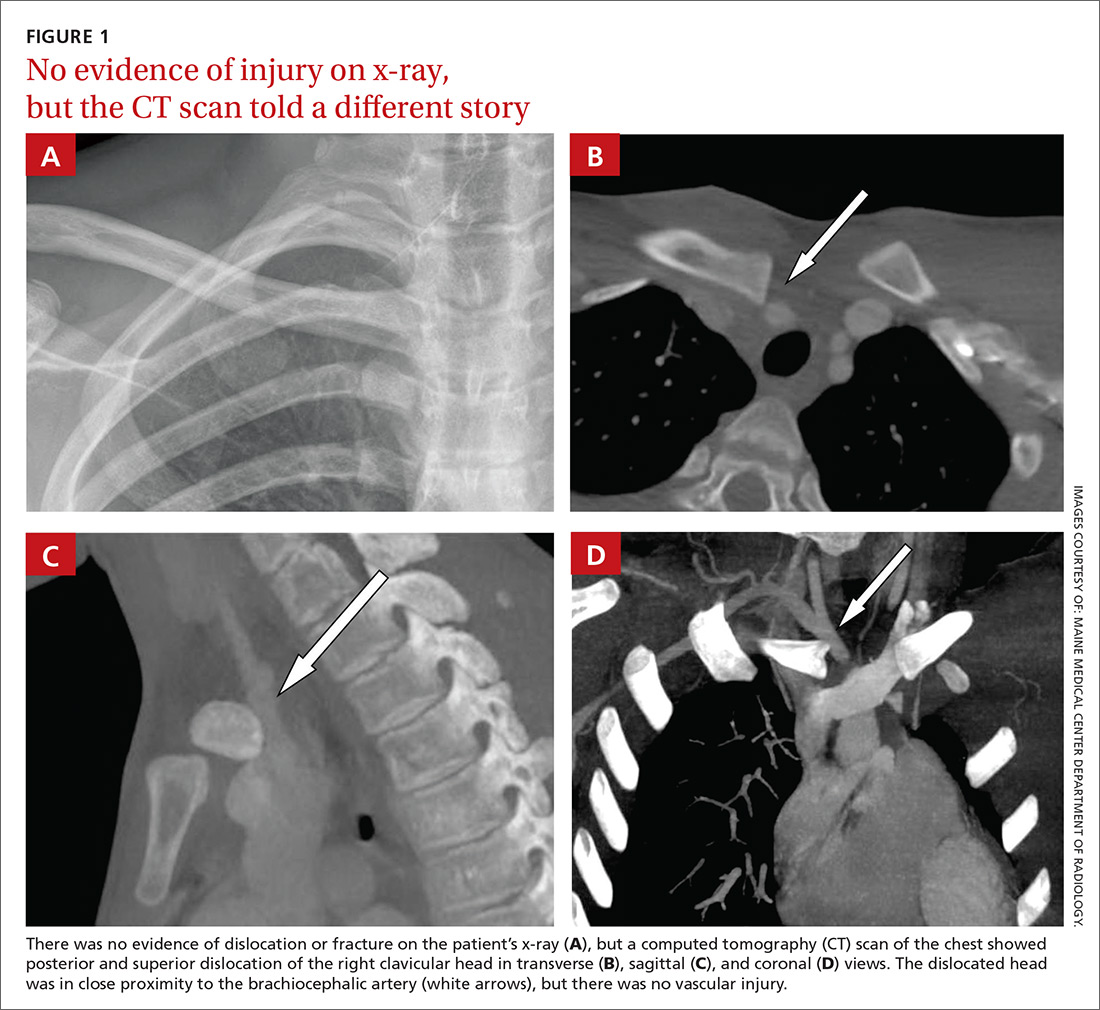
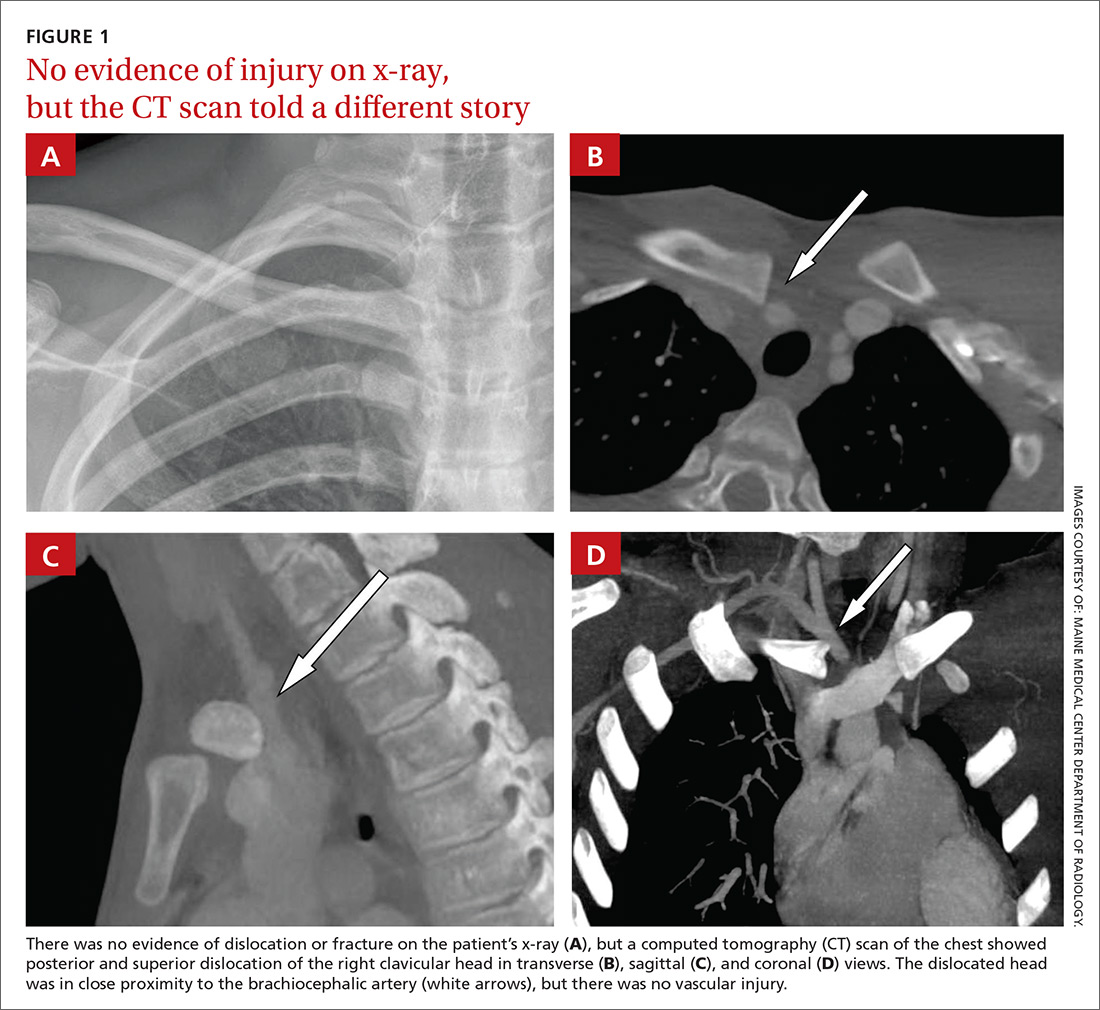
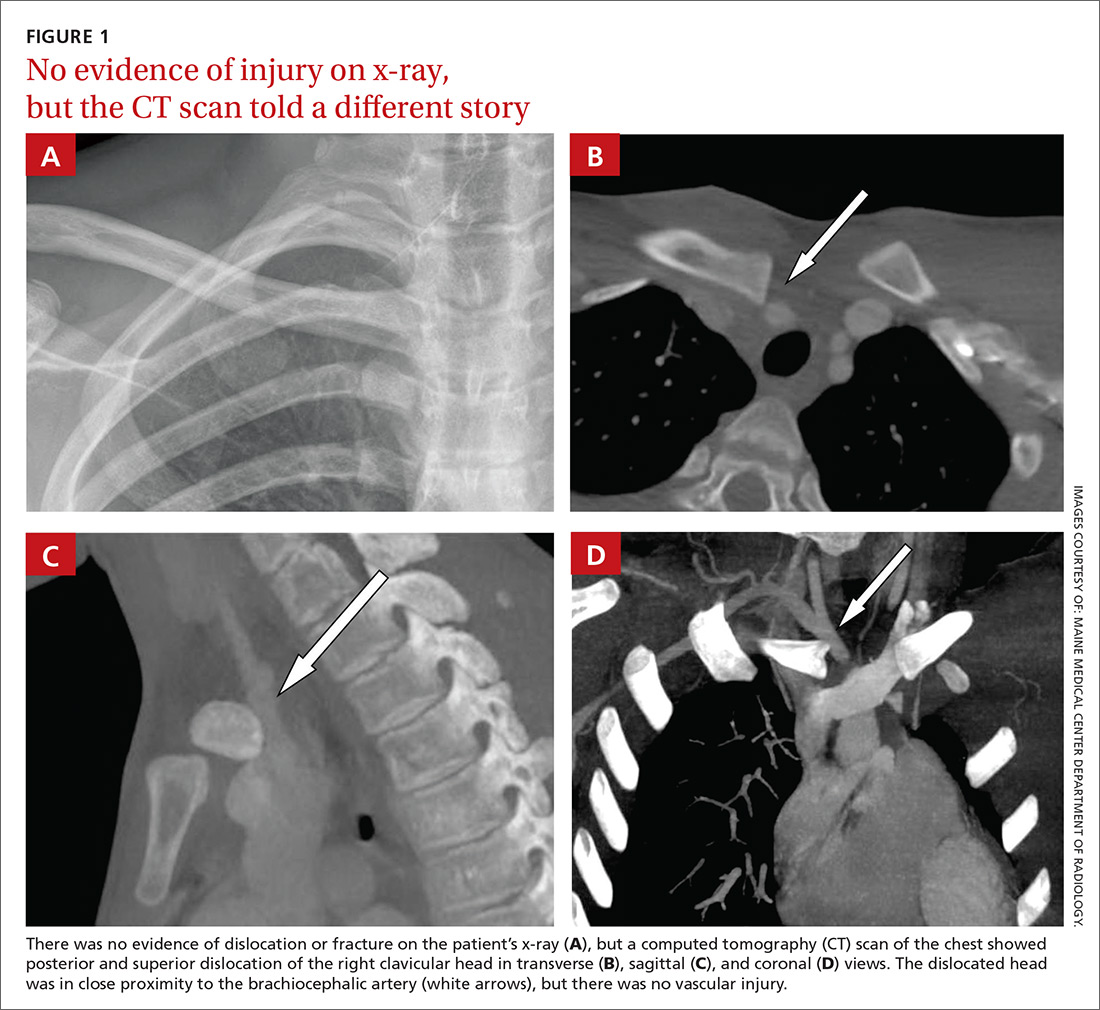
A 16-year-old hockey player presented to our emergency department with sharp pain in his right upper chest after “checking” another player during a game. The pain did not resolve with rest and was worse with movement and breathing. The patient did not have dysphagia, dyspnea, paresthesias, or hoarseness. The physical examination revealed tenderness over the right sternoclavicular joint (SCJ) without swelling or deformity. A distal neurovascular exam was intact, and a chest x-ray showed no evidence of dislocation or fracture (FIGURE 1A). The patient’s pain was refractory to multiple intravenous (IV) pain medications.
THE DIAGNOSIS
A computed tomography (CT) scan with IV contrast of the chest demonstrated posterior and superior dislocation of the right clavicular head. Despite the close proximity of the dislocated head to the brachiocephalic artery (FIGURE 1B-1D), there was no vascular injury.
DISCUSSION
Posterior sternoclavicular dislocations (PSCDs) can be difficult to diagnose. Edema can mask the characteristic skin depression that one would expect with a posterior dislocation.1 Chest radiographs are often normal (as was true in this case). Patients may present with an abnormal pulse, paresthesias, hoarseness, dysphagia, and/or dyspnea. However, for more than half of these patients, their only signs and symptoms will be pain, swelling, and limited range of motion.1 As a result, a PSCD may be misdiagnosed as a ligamentous or soft tissue injury.1
An uncommon injury that can result in serious complications
PSCDs represent 3% to 5% of all SCJ dislocations, which comprise <5% of all shoulder girdle injuries.1 Nevertheless, prompt and accurate diagnosis is critical, as these dislocations involve a high risk for injury to the posterior structures, particularly the brachiocephalic vein, right common carotid artery, and aortic arch.
One study found that nearly 75% of patients had a significant structure <1 cm posterior to the SCJ.2 This proximity can result in neurovascular complications—some of which are devastating—in up to 30% of patients with PSCDs.3 A case report from 2011, for example, describes a 19-year-old man who had an undiagnosed PSCD that caused a pseudoaneurysm in his subclavian artery and a subsequent thrombotic cerebrovascular accident.4
Which injuries should raise your suspicions? Injuries in which lateral compression on the shoulder has caused it to roll forward and those in which a posteriorly directed force has been applied to the medial clavicle (as might occur in tackle sports or motor vehicle rollovers) should increase suspicion of a PSCD.1
Proper diagnosis requires CT angiography of the chest to assess the injury and evaluate the underlying structures. If CT is not available, additional chest film views, such as a serendipity view (anteroposterior view with 40° cephalic tilt) or Heinig view (oblique projection perpendicular to SCJ), may be obtained; an ultrasound is also an option.5
PSCD = surgical emergency
Following diagnosis, immediate orthopedic consultation is required. A PSCD is a surgical emergency. Reduction (open or closed) must be performed under general anesthesia with vascular and/or cardiothoracic surgery specialists available, as the reduction itself could injure one of the great vessels. Fortunately, most patients do quite well following surgery, with the majority achieving good-to-excellent results.6
Our patient was admitted to the hospital and underwent orthopedic surgery the following morning. Vascular and cardiothoracic surgeons were consulted and available in the event of a complication. A Salter-Harris type 2 fracture of the medial clavicle was identified intraoperatively, and an open reduction with internal fixation was performed. The patient had an uneventful recovery and resumed his usual activities, including playing hockey.
THE TAKEAWAY
PSCDs, although uncommon, can be life-threatening. Since the physical exam is unreliable and standard radiographs are often normal, accurate diagnosis relies largely on increased clinical suspicion. When there is a history of shoulder trauma, medial clavicle pain, and SCJ edema or tenderness, a PSCD should be suspected.7
Confirm the diagnosis with CT angiogram, and remember that a PSCD is a surgical emergency that requires coordination with orthopedic and vascular/cardiothoracic surgeons.
1. Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg. 2015;23:468-475.
2. Ponce BA, Kundukulam JA, Pflugner R, et al. Sternoclavicular joint surgery: how far does danger lurk below? J Shoulder Elbow Surg. 2013;22:993-999.
3. Daya MR, Bengtzen RR. Shoulder. In: Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:618-642.
4. Marcus MS, Tan V. Cerebrovascular accident in a 19-year-old patient: a case report of posterior sternoclavicular dislocation. J Shoulder Elbow Surg. 2011;20:e1-e4.
5. Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: a review of the literature. World J Orthop. 2016;7:244-250.
6. Boesmueller S, Wech M, Tiefenboeck TM, et al. Incidence, characteristics, and long-term follow-up of sternoclavicular injuries: an epidemiologic analysis of 92 cases. J Trauma Acute Care Surg. 2016;80:289-295.
7. Roepke C, Kleiner M, Jhun P, et al. Chest pain bounce-back: posterior sternoclavicular dislocation. Ann Emerg Med. 2015;66:559-561.
THE CASE
A 16-year-old hockey player presented to our emergency department with sharp pain in his right upper chest after “checking” another player during a game. The pain did not resolve with rest and was worse with movement and breathing. The patient did not have dysphagia, dyspnea, paresthesias, or hoarseness. The physical examination revealed tenderness over the right sternoclavicular joint (SCJ) without swelling or deformity. A distal neurovascular exam was intact, and a chest x-ray showed no evidence of dislocation or fracture (FIGURE 1A). The patient’s pain was refractory to multiple intravenous (IV) pain medications.
THE DIAGNOSIS
A computed tomography (CT) scan with IV contrast of the chest demonstrated posterior and superior dislocation of the right clavicular head. Despite the close proximity of the dislocated head to the brachiocephalic artery (FIGURE 1B-1D), there was no vascular injury.
DISCUSSION
Posterior sternoclavicular dislocations (PSCDs) can be difficult to diagnose. Edema can mask the characteristic skin depression that one would expect with a posterior dislocation.1 Chest radiographs are often normal (as was true in this case). Patients may present with an abnormal pulse, paresthesias, hoarseness, dysphagia, and/or dyspnea. However, for more than half of these patients, their only signs and symptoms will be pain, swelling, and limited range of motion.1 As a result, a PSCD may be misdiagnosed as a ligamentous or soft tissue injury.1
An uncommon injury that can result in serious complications
PSCDs represent 3% to 5% of all SCJ dislocations, which comprise <5% of all shoulder girdle injuries.1 Nevertheless, prompt and accurate diagnosis is critical, as these dislocations involve a high risk for injury to the posterior structures, particularly the brachiocephalic vein, right common carotid artery, and aortic arch.
One study found that nearly 75% of patients had a significant structure <1 cm posterior to the SCJ.2 This proximity can result in neurovascular complications—some of which are devastating—in up to 30% of patients with PSCDs.3 A case report from 2011, for example, describes a 19-year-old man who had an undiagnosed PSCD that caused a pseudoaneurysm in his subclavian artery and a subsequent thrombotic cerebrovascular accident.4
Which injuries should raise your suspicions? Injuries in which lateral compression on the shoulder has caused it to roll forward and those in which a posteriorly directed force has been applied to the medial clavicle (as might occur in tackle sports or motor vehicle rollovers) should increase suspicion of a PSCD.1
Proper diagnosis requires CT angiography of the chest to assess the injury and evaluate the underlying structures. If CT is not available, additional chest film views, such as a serendipity view (anteroposterior view with 40° cephalic tilt) or Heinig view (oblique projection perpendicular to SCJ), may be obtained; an ultrasound is also an option.5
PSCD = surgical emergency
Following diagnosis, immediate orthopedic consultation is required. A PSCD is a surgical emergency. Reduction (open or closed) must be performed under general anesthesia with vascular and/or cardiothoracic surgery specialists available, as the reduction itself could injure one of the great vessels. Fortunately, most patients do quite well following surgery, with the majority achieving good-to-excellent results.6
Our patient was admitted to the hospital and underwent orthopedic surgery the following morning. Vascular and cardiothoracic surgeons were consulted and available in the event of a complication. A Salter-Harris type 2 fracture of the medial clavicle was identified intraoperatively, and an open reduction with internal fixation was performed. The patient had an uneventful recovery and resumed his usual activities, including playing hockey.
THE TAKEAWAY
PSCDs, although uncommon, can be life-threatening. Since the physical exam is unreliable and standard radiographs are often normal, accurate diagnosis relies largely on increased clinical suspicion. When there is a history of shoulder trauma, medial clavicle pain, and SCJ edema or tenderness, a PSCD should be suspected.7
Confirm the diagnosis with CT angiogram, and remember that a PSCD is a surgical emergency that requires coordination with orthopedic and vascular/cardiothoracic surgeons.
THE CASE
A 16-year-old hockey player presented to our emergency department with sharp pain in his right upper chest after “checking” another player during a game. The pain did not resolve with rest and was worse with movement and breathing. The patient did not have dysphagia, dyspnea, paresthesias, or hoarseness. The physical examination revealed tenderness over the right sternoclavicular joint (SCJ) without swelling or deformity. A distal neurovascular exam was intact, and a chest x-ray showed no evidence of dislocation or fracture (FIGURE 1A). The patient’s pain was refractory to multiple intravenous (IV) pain medications.
THE DIAGNOSIS
A computed tomography (CT) scan with IV contrast of the chest demonstrated posterior and superior dislocation of the right clavicular head. Despite the close proximity of the dislocated head to the brachiocephalic artery (FIGURE 1B-1D), there was no vascular injury.
DISCUSSION
Posterior sternoclavicular dislocations (PSCDs) can be difficult to diagnose. Edema can mask the characteristic skin depression that one would expect with a posterior dislocation.1 Chest radiographs are often normal (as was true in this case). Patients may present with an abnormal pulse, paresthesias, hoarseness, dysphagia, and/or dyspnea. However, for more than half of these patients, their only signs and symptoms will be pain, swelling, and limited range of motion.1 As a result, a PSCD may be misdiagnosed as a ligamentous or soft tissue injury.1
An uncommon injury that can result in serious complications
PSCDs represent 3% to 5% of all SCJ dislocations, which comprise <5% of all shoulder girdle injuries.1 Nevertheless, prompt and accurate diagnosis is critical, as these dislocations involve a high risk for injury to the posterior structures, particularly the brachiocephalic vein, right common carotid artery, and aortic arch.
One study found that nearly 75% of patients had a significant structure <1 cm posterior to the SCJ.2 This proximity can result in neurovascular complications—some of which are devastating—in up to 30% of patients with PSCDs.3 A case report from 2011, for example, describes a 19-year-old man who had an undiagnosed PSCD that caused a pseudoaneurysm in his subclavian artery and a subsequent thrombotic cerebrovascular accident.4
Which injuries should raise your suspicions? Injuries in which lateral compression on the shoulder has caused it to roll forward and those in which a posteriorly directed force has been applied to the medial clavicle (as might occur in tackle sports or motor vehicle rollovers) should increase suspicion of a PSCD.1
Proper diagnosis requires CT angiography of the chest to assess the injury and evaluate the underlying structures. If CT is not available, additional chest film views, such as a serendipity view (anteroposterior view with 40° cephalic tilt) or Heinig view (oblique projection perpendicular to SCJ), may be obtained; an ultrasound is also an option.5
PSCD = surgical emergency
Following diagnosis, immediate orthopedic consultation is required. A PSCD is a surgical emergency. Reduction (open or closed) must be performed under general anesthesia with vascular and/or cardiothoracic surgery specialists available, as the reduction itself could injure one of the great vessels. Fortunately, most patients do quite well following surgery, with the majority achieving good-to-excellent results.6
Our patient was admitted to the hospital and underwent orthopedic surgery the following morning. Vascular and cardiothoracic surgeons were consulted and available in the event of a complication. A Salter-Harris type 2 fracture of the medial clavicle was identified intraoperatively, and an open reduction with internal fixation was performed. The patient had an uneventful recovery and resumed his usual activities, including playing hockey.
THE TAKEAWAY
PSCDs, although uncommon, can be life-threatening. Since the physical exam is unreliable and standard radiographs are often normal, accurate diagnosis relies largely on increased clinical suspicion. When there is a history of shoulder trauma, medial clavicle pain, and SCJ edema or tenderness, a PSCD should be suspected.7
Confirm the diagnosis with CT angiogram, and remember that a PSCD is a surgical emergency that requires coordination with orthopedic and vascular/cardiothoracic surgeons.
1. Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg. 2015;23:468-475.
2. Ponce BA, Kundukulam JA, Pflugner R, et al. Sternoclavicular joint surgery: how far does danger lurk below? J Shoulder Elbow Surg. 2013;22:993-999.
3. Daya MR, Bengtzen RR. Shoulder. In: Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:618-642.
4. Marcus MS, Tan V. Cerebrovascular accident in a 19-year-old patient: a case report of posterior sternoclavicular dislocation. J Shoulder Elbow Surg. 2011;20:e1-e4.
5. Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: a review of the literature. World J Orthop. 2016;7:244-250.
6. Boesmueller S, Wech M, Tiefenboeck TM, et al. Incidence, characteristics, and long-term follow-up of sternoclavicular injuries: an epidemiologic analysis of 92 cases. J Trauma Acute Care Surg. 2016;80:289-295.
7. Roepke C, Kleiner M, Jhun P, et al. Chest pain bounce-back: posterior sternoclavicular dislocation. Ann Emerg Med. 2015;66:559-561.
1. Chaudhry S. Pediatric posterior sternoclavicular joint injuries. J Am Acad Orthop Surg. 2015;23:468-475.
2. Ponce BA, Kundukulam JA, Pflugner R, et al. Sternoclavicular joint surgery: how far does danger lurk below? J Shoulder Elbow Surg. 2013;22:993-999.
3. Daya MR, Bengtzen RR. Shoulder. In: Rosen’s Emergency Medicine: Concepts and Clinical Practice. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:618-642.
4. Marcus MS, Tan V. Cerebrovascular accident in a 19-year-old patient: a case report of posterior sternoclavicular dislocation. J Shoulder Elbow Surg. 2011;20:e1-e4.
5. Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: a review of the literature. World J Orthop. 2016;7:244-250.
6. Boesmueller S, Wech M, Tiefenboeck TM, et al. Incidence, characteristics, and long-term follow-up of sternoclavicular injuries: an epidemiologic analysis of 92 cases. J Trauma Acute Care Surg. 2016;80:289-295.
7. Roepke C, Kleiner M, Jhun P, et al. Chest pain bounce-back: posterior sternoclavicular dislocation. Ann Emerg Med. 2015;66:559-561.
