User login
Chest Pain and Vomiting with Prior Heart Attack
ANSWER
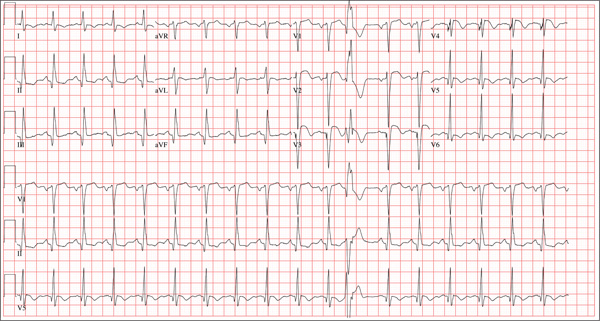
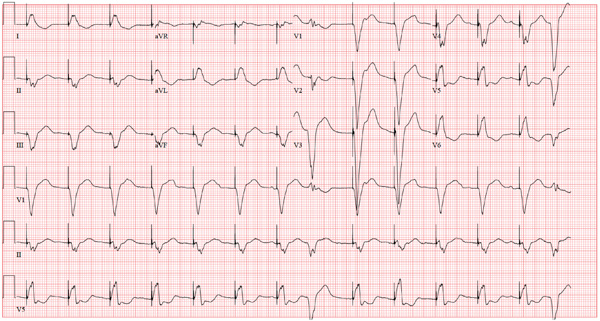
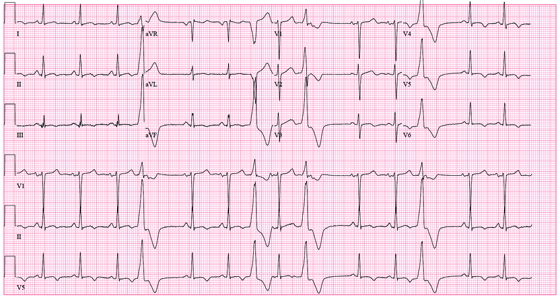
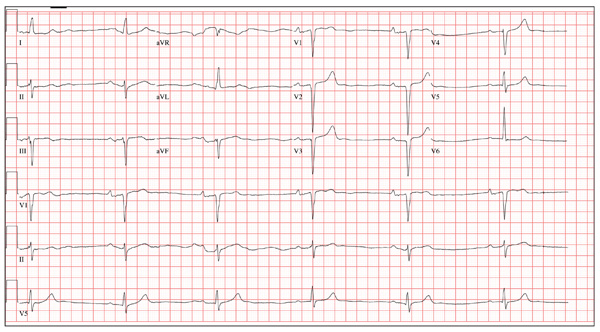
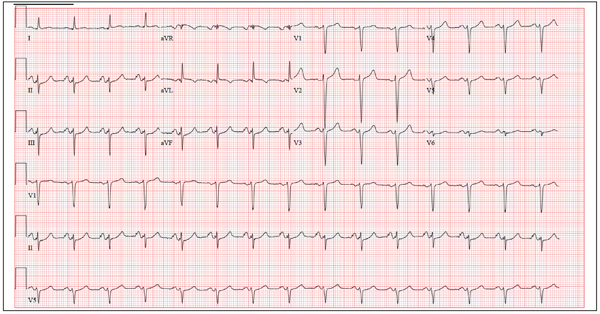
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
Three hours ago, this 69-year-old man started to experience substernal chest pain, nausea, and vomiting. He had stopped for lunch after spending the morning raking leaves; his chest pain began while he was at the drive-through window at a local fast food restaurant. By the time he got home, he was nauseous and had an episode of emesis. The pain is described as a “dull, heavy ache” with radiation to the left neck and arm. The patient states he is diaphoretic, but attributes it to the labor associated with his yardwork. He recalls that his first heart attack started in a similar way and fears he is having another. Following the emesis, his nausea stopped, and he rested in his recliner, hoping his symptoms would resolve. Unfortunately, the chest pain worsened, and he drove himself to the clinic rather than calling 911. (He didn’t want to go to the ED or get billed for the ambulance ride.) Review of his medical history reveals coronary artery disease, evidenced by an inferior MI in 2008. This was treated with coronary artery bypass surgery with reversed saphenous vein grafts placed to the first and second obtuse marginal branches of the circumflex coronary artery, reversed saphenous vein graft to the posterior descending artery, and an internal mammary artery graft placed to the proximal left anterior descending artery. His history is also remarkable for hyperlipidemia, hypertension, and obesity. He is a retired postal worker who has lived alone since his wife died three years ago. He drinks a six-pack of beer daily and continues to smoke one to two packs of cigarettes per day, depending on his activities. His family history includes coronary artery disease, hypertension, diabetes, and stroke. His current medications include aspirin, atorvastatin, clopidogrel, furosemide, isosorbide dinitrate, metoprolol, nicotine patch, potassium chloride, and valsartan. He is intolerant of ACE inhibitors, due to the resulting chronic, dry cough. The review of systems reveals that he has had headaches over the past week and that he recently recovered from the flu. He has had no changes in bowel or bladder function, shortness of breath, or recent weight loss or gain. Vital signs include a blood pressure of 168/100 mm Hg; pulse, 110 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 98% on room air; and temperature, 37.2°C. His weight is 108 kg, and his height is 170 cm. Physical findings show that the lungs are clear to auscultation; his rhythm is regular with no murmurs, rubs, or gallops; and the point of maximum impulse is not displaced. The neck veins are flat, and there is no peripheral edema. A well-healed median sternotomy scar is evident, as are bilateral lower extremity saphenous vein harvest scars. The abdomen is soft and nontender, and peripheral pulses are strong and equal bilaterally. There are no neurologic abnormalities noted. Laboratory samples and an ECG are obtained. The following findings are noted on the ECG: a ventricular rate of 108 beats/min; PR interval, 140 ms; QRS duration, 116 ms; QT/QTc interval, 372/498 ms; P axis, 70°; R axis, 75°; and T axis, 167°. What is your interpretation of this ECG?
The Flu, or a Problem with His Pacemaker?
ANSWER
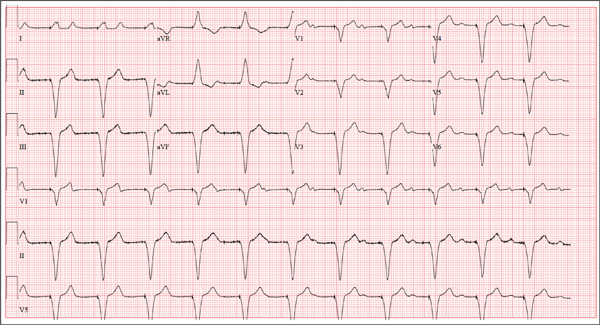
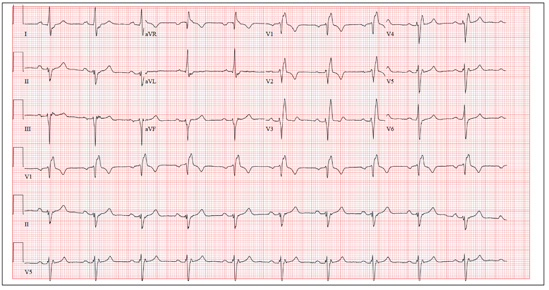
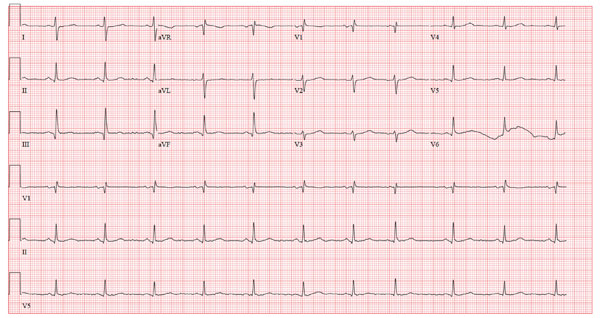
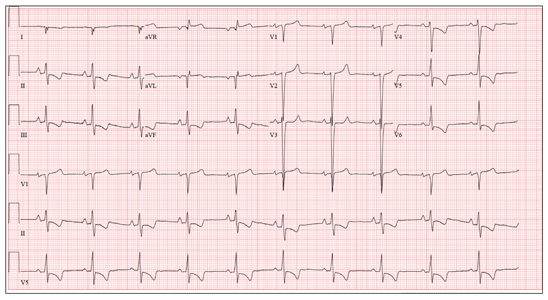
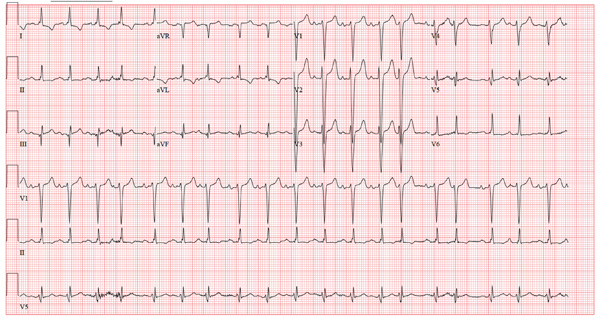
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
ANSWER
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
ANSWER
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
A 75-year-old man presents to your office with complaints of shortness of breath. He states he has had “the flu” for the past week, but it doesn’t seem to be getting any better. His shortness of breath has persisted without change, and he is concerned he may be developing pneumonia. He denies having a productive cough, fevers, chills, or night sweats. Medical history is remarkable for GERD, hyperlipidemia, hypertension, and complete heart block with implantation of a dual-chamber permanent pacemaker in 2010. He has had several surgeries, including a right inguinal hernia repair and an appendectomy. Family history is positive for breast cancer, colon cancer, and stroke. There is no family history of cardiac or pulmonary disease. Social history reveals a retired accountant who lives at home with his wife. He has an occasional brandy in the evening and has never smoked. His current medications include metoprolol, rosu¬\vastatin, and omeprazole. He has no known drug allergies. The review of systems is unremarkable, with the exception of the shortness of breath. The patient is concerned, however, that since his pacemaker was interrogated one week ago, he hasn’t “felt the same.” Physical examination reveals a blood pressure of 130/70 mm Hg; pulse, 70 beats/min; respiratory rate, 16 breaths/min-1; temperature, 36.6°C; and O2 saturation, 97% on room air. The patient’s weight is 105 kg. The cardiovascular exam reveals a regular rate of 70 beats/min, and a grade II/VI early systolic murmur best heard at the left upper sternal border and without radiation. There are no rubs, gallops, or bruits. The pulmonary exam reveals scattered crackles in the right lower chest, which clear with coughing. There are no rhonchi or bronchial breath sounds. All other exams yield normal results. The patient provides a copy of an interrogation report from one year ago, which states his pacemaker is programmed DDDR at a rate of 60 beats/min, with an upper tracking and sensing rate of 130 beats/min, a paced AV delay of 150 ms, and a sensed AV delay of 120 ms. Given the patient’s concern about his most recent interrogation, you call an experienced practitioner to determine whether the patient’s device is functioning appropriately. While waiting, you obtain an ECG, which reveals the following: a ventricular rate of 70 beats/min; PR interval, not measurable; QRS duration, 200 ms; QT/QTc interval, 500/540 ms; no P axis; R axis, –83°; and T axis, 71°. What is your interpretation, and is there any concern regarding his pacemaker function?
Man Waits Until Follow-up to Reveal Chest Pain
ANSWER
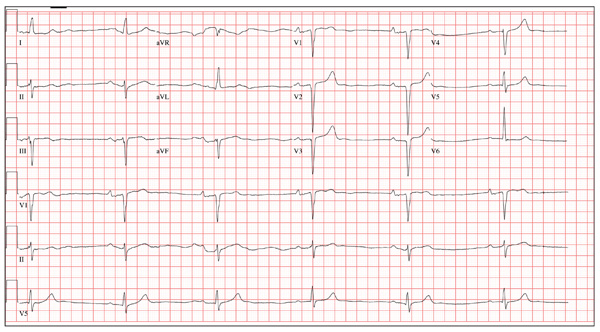
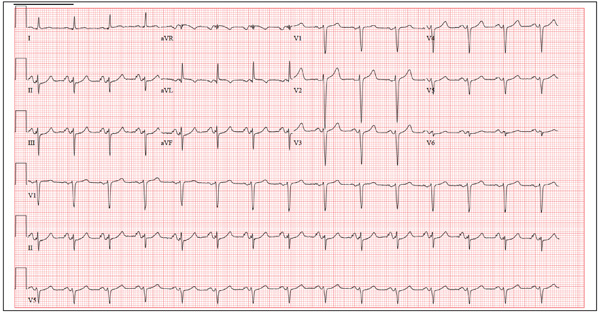
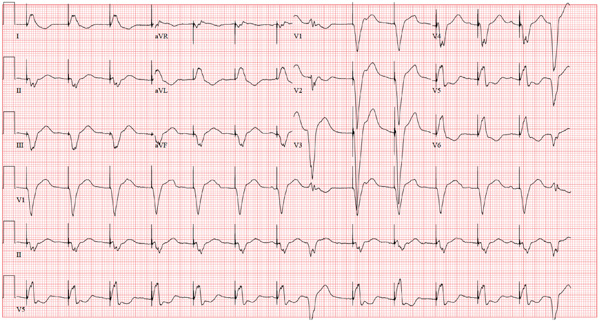
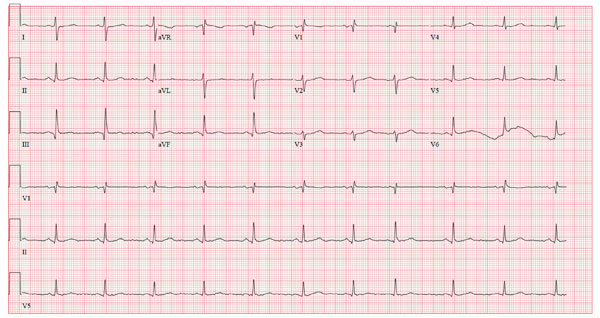
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
A 64-year-old man presents for follow-up to an appointment one month ago in which he reported a history of acute-onset shortness of breath, fatigue, and exercise intolerance. His health prior to that visit was described as “normal”; he had not seen a clinician since having his tonsils out at age 14. At the previous visit, a complete history documented that the patient is a rancher and farmer who makes his living from his crops and animals. He has never been married and lives out in the country. He has a history of several broken bones that he set himself, with no resultant sequelae. Aside from routine colds and flu, he has not been ill. He stopped smoking 10 years ago when it “got to be too expensive,” and he drinks one shot of whiskey at bedtime each night. He denies any drug allergies; he was taking no medications when he presented for that visit. A physical examination during that appointment revealed the presence of an irregularly irregular rhythm with a ventricular rate of 120 beats/min, a grade II/VI decrescendo diastolic murmur best heard at the right upper sternal border, a grade II/VI mid-systolic murmur best heard at the apex, a large point of maximum impulse (PMI) palpable at the anterior axillary line, and 3+ pitting edema to the level of the knees in both lower extremities. Subsequent workup, including an ECG, echocardiogram, chest x-ray, complete blood count, and chemistry panel, was performed—much to the patient’s displeasure. Pertinent results included a diagnosis of atrial fibrillation, a bicuspid aortic valve, aortic insufficiency, and mitral regurgitation. He was prescribed metoprolol and warfarin and referred to a cardiologist. During the current visit, you learn that he did not continue to take his warfarin, because his shortness of breath went away the day after the previous appointment. He states he doesn’t always remember to take his metoprolol, but when he does, he’ll often take enough to “catch up on” his dosage. He did not follow up with a cardiologist as scheduled. Additionally, he reveals that he experienced chest pain two weeks ago, which he describes as a “sharp, sticking” pain in his left chest. He did not come in because he thought he’d wait until this appointment to discuss it. He remembers being “all sweaty” when he had his chest pain, but adds that it hasn’t happened again. His review of symptoms is remarkable for fatigue since his chest pain. Physical exam reveals cardiac changes. His rhythm is now regular, but at a rate of 40 beats/min. His murmurs are unchanged from the previous visit. Another ECG is obtained, which reveals the following: a ventricular rate of 35 beats/min; PR interval, 258 ms; QRS duration, 116 ms; QT/QTc interval, 532/406 ms; P axis, 74°; R axis, –47°; and T axis, 45°. What is your interpretation of this ECG?
Woman with “Dull, Achy” Back Pain and Shortness of Breath
ANSWER
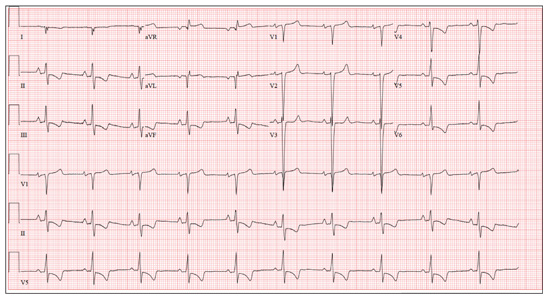
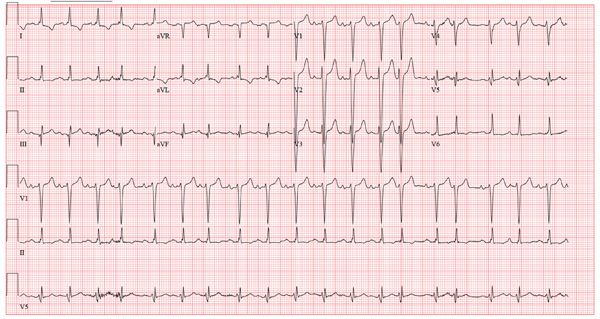
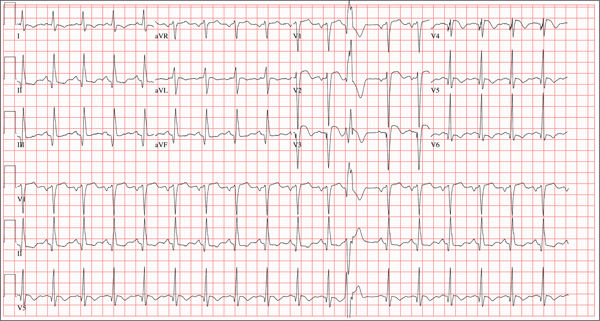
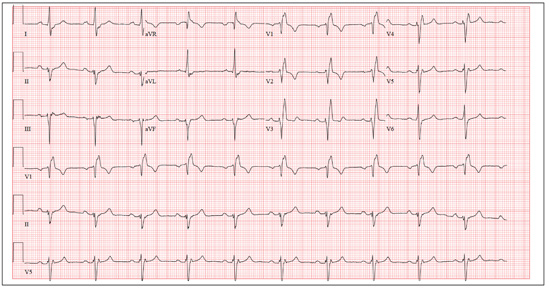
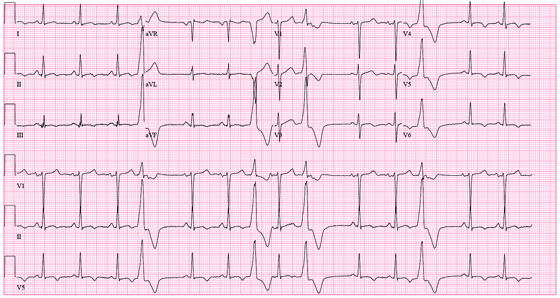
This ECG demonstrates normal sinus rhythm, right-axis deviation, evidence of a lateral MI, and inferolateral ST- and T-wave abnormalities.
Right-axis deviation is indicated by an R-wave axis between 90° and 180° and QS or QR complexes in lead I and/or aVL. While the most common cause of a right-axis deviation is right ventricular hypertrophy, it is also evident in a lateral MI. Evidence for the latter includes the presence of significant Q waves in leads I and aVL. Finally, inferolateral ST- and T-wave changes are evidenced by inverted T waves in leads II, III, aVF, and precordial leads V4 to V6.
ECG evidence of a lateral MI not present on a previous scan (eight months ago), in the presence of a normal troponin level, suggests a recent MI.
ANSWER
This ECG demonstrates normal sinus rhythm, right-axis deviation, evidence of a lateral MI, and inferolateral ST- and T-wave abnormalities.
Right-axis deviation is indicated by an R-wave axis between 90° and 180° and QS or QR complexes in lead I and/or aVL. While the most common cause of a right-axis deviation is right ventricular hypertrophy, it is also evident in a lateral MI. Evidence for the latter includes the presence of significant Q waves in leads I and aVL. Finally, inferolateral ST- and T-wave changes are evidenced by inverted T waves in leads II, III, aVF, and precordial leads V4 to V6.
ECG evidence of a lateral MI not present on a previous scan (eight months ago), in the presence of a normal troponin level, suggests a recent MI.
ANSWER
This ECG demonstrates normal sinus rhythm, right-axis deviation, evidence of a lateral MI, and inferolateral ST- and T-wave abnormalities.
Right-axis deviation is indicated by an R-wave axis between 90° and 180° and QS or QR complexes in lead I and/or aVL. While the most common cause of a right-axis deviation is right ventricular hypertrophy, it is also evident in a lateral MI. Evidence for the latter includes the presence of significant Q waves in leads I and aVL. Finally, inferolateral ST- and T-wave changes are evidenced by inverted T waves in leads II, III, aVF, and precordial leads V4 to V6.
ECG evidence of a lateral MI not present on a previous scan (eight months ago), in the presence of a normal troponin level, suggests a recent MI.
A 70-year-old woman has a 10-year history of a dilated nonischemic cardiomyopathy and New York Heart Association Class II heart failure. She presents with a one-week history of back pain and shortness of breath. She describes the pain as a “dull, achy” pressure, exacerbated by exertion and relieved with rest. She says the pain is localized in the back between her scapulas and does not radiate. She denies substernal chest pain, nausea, vomiting, or diaphoresis; the only associated symptom is dyspnea. Her most recent echocardiogram showed a dilated left ventricle, with a left ventricular ejection fraction of 29%, and a normal right ventricle, with mild hypertrophy and mildly reduced systolic function. She was also noted to have atherosclerotic changes in her ascending and descending thoracic aorta. Medical history is remarkable for diabetes, hypertension, chronic renal insufficiency, hyperlipidemia, and cataracts. Her current medications include aspirin, fer-rous sulfate, furosemide, hydralazine, glargine insulin, isosorbide dinitrate, lisinopril, metoprolol, and raloxifene. She is allergic to codeine, amiodarone, and radi-ographic contrast. Family history is positive for coronary artery disease, diabetes, and stroke. The patient is widowed, does not smoke, and does not consume alcohol. She is very active in her local quilting club. The review of systems is positive for increased weakness and diarrhea. She states that approximately two weeks ago, she experienced vague epigastric pain and diaphoresis; she did not seek medical attention, as it resolved. The physical exam reveals a thin, elderly woman in mild distress. Blood pressure is 139/82 mm Hg; pulse, 66 beats/min; respiratory rate, 21 breaths/¬min-1; and temperature, 35.9°C. Her weight is 108 lb. Pertinent physical findings include a grade II/VI diastolic murmur at the left lower sternal border, 2+ peripheral pulses with a bruit present in the right femoral artery, occasional late expiratory wheezes in both lung bases, vertebral tenderness at the T6-T7 level with no evidence of scoliosis or kyphosis, and no evidence of peripheral edema. She is intact from a neurologic standpoint. Significant laboratory data include a serum glucose level of 294 mg/dL; blood urea nitrogen (BUN), 68 mg/dL; creatinine, 1.75 mg/dL; glomerular filtration rate, 30 mL/min; B-type natriuretic peptide, 984 pg/mL; and serum troponin, 0.11 ng/mL. An ECG is obtained that reveals the following: a ventricular rate of 62 beats/min; PR interval, 160 ms; QRS duration, 94 ms; QT/QTc interval, 404/410 ms; P ax-is, 84°; R axis, 151°; and T axis, 253°. What is your interpretation of this ECG?
Is This Golfer's Pacemaker Malfunctioning?
ANSWER
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
ANSWER
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
ANSWER
The ECG reveals an atrial-sensed and ventricular-paced rhythm of 83 beats/min. In this case, the pacemaker is functioning appropriately as programmed.
Pacemaker code consists of three letters: The first refers to the chamber(s) paced, the second to the chamber(s) sensed, and the third to the pacemaker’s response to a sensed beat. This patient has a pacing lead in the right atrium and one in the right ventricle and is programmed DDD. Each D in this case stands for dual: The first to indicate that both leads are programmed to pace, the second to indicate that both chambers may be sensed, and the third to indicate that the response to sensing can be either to inhibit or trigger a ventricular-paced beat in response to what happens in the atrium. Hence, there are four possible scenarios with a DDD pacemaker: AS-VS (atrial sensed-ventricle sensed; eg, intrinsic AV conduction requiring no pacing), AS-VP (atrial sensed-ventricle paced), AP-VS (atrial paced-ventricle sensed), and AP-VP (atrial paced-ventricle paced).
In this case, the atrial rate (83 beats/min) is faster than the pacemaker’s lower programmed rate. In order to see atrial pacing on the ECG, the intrinsic atrial rate would have to be less than the programmed rate of 60 beats/min. As soon as the pacemaker senses atrial conduction (either spontaneous or paced), it starts a timer (programmed at 130 ms in this case). If there is no spontaneous ventricular depolarization by the end of the timer, the pacemaker delivers an impulse to the ventricle, resulting in a paced ventricular beat. An often-made mistake (as this case illustrates) is the assumption that if one does not see pacing spikes, the pacemaker is not functioning properly.
A 75-year-old man has a history of New York Heart Association Class II congestive heart failure (CHF), coronary artery disease (CAD) with coronary artery by-pass graft (CABG) surgery, and aortic stenosis with a bioprosthetic aortic valve replacement (AVR). He developed second-degree heart block (Mobitz II) following his four-vessel CABG and AVR four years ago, requiring placement of a dual-chamber pacemaker. He has been asymptomatic and plays golf two to three times per week. One week ago, he went to an urgent care center for treatment of a laceration on his leg and was told that part of his pacemaker wasn’t working. He presents to you now for follow-up on the pacemaker. Medical history is also remarkable for COPD, left inguinal hernia repair, hyperlipidemia, and bilateral cataracts. Family history is positive for CAD, diabetes, and stroke. He has a remote history of smoking and drinks one martini after each golf game. His medications include aspirin, lovastatin, and metoprolol. He has no drug allergies. The review of systems is negative except for a recent repair to a 3-cm laceration on the left leg. Physical examination reveals a well-developed, pleasant man in no distress. His height is 74” and weight, 179 lb. Blood pressure is 118/84 mm Hg; pulse, 80 beats/min and regular; respiratory rate, 14 breaths/min; temperature, 98.8°F; and O2 saturation, 97% on room air. Pertinent physical findings include a well-healed pacemaker site without signs of recent trauma. The lungs are clear in all fields, the cardiac exam is within normal limits, and there is no jugular venous distention. The abdomen is benign, and there is no peripheral edema. The laceration repair on his left leg is healing well (no erythema, induration, wound separation, or dehiscence). The pacemaker is programmed DDD at a lower rate of 60 beats/min and an upper rate of 120 beats/min, with paced and sensed atrioventricular (AV) delays programmed at 130 ms. An ECG reveals the following: a ventricular rate of 83 beats/min; PR interval, not measured; QRS duration, 162 ms; QT/QTc interval, 480/564 ms; P axis, unmeasurable; R axis, 254°; and T axis, 56°. What is your interpretation of this ECG? Is there any indication that the pacemaker is not functioning?
Childhood Problem Flares at Age 50
ANSWER
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
ANSWER
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
ANSWER
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
A man, 50, has a history of tetralogy of Fallot (ventricular septal defect [VSD], pulmonary stenosis, right ventricular hypertrophy, and overriding aorta). He underwent surgical correction at age 4, with placement of a Blalock-Taussig shunt and closure of his VSD, and was asymptomatic until one year ago. In the past year, he has developed progressive shortness of breath and dyspnea on exertion. In the past three months, he has developed chest pain that he describes as sharp, nonradiating, and occurring most often with dyspnea on exertion. He denies syncope, near-syncope, palpitations, or tachycardia. He cannot walk more than one-and-a-half blocks before stopping to rest, and he avoids hills and stairs if at all possible. A review of his most recent cardiac work-up (performed six months ago) reveals no significant coronary artery disease or evidence of aortic stenosis; it shows moderate aortic regurgitation, normal systolic aortic pressures, and normal left ventricular end diastolic pressures. The right ventricular pressures were elevated due to pulmonic stenosis; however, the estimated pulmonary artery pressures were normal. A cardiac MRI performed one month ago shows a significantly dilated aortic root with aneurysmal dilatation extending to the aortic arch, with effacement at the sinotubular junction and moderate aortic regurgitation. Additional findings include a markedly dilated right ventricular outflow tract with no pulmonic stenosis, evi-dence of a previous right Blalock-Taussig shunt, and moderate right atrial enlargement. Medical history is remarkable for hypertension. Family history is remarkable for hypertension, diabetes, and coronary artery disease, but not congenital heart disease. The patient does not smoke and drinks socially on the weekends. His medications include amlodipine, aspirin, and lisinopril. He is allergic to penicillin and amox-icillin. A review of systems reveals that he has had flulike symptoms for the past four days, with a dry, nonproductive cough. Physical exam reveals a well-developed, obese male in no distress. His height is 67”and his weight, 208 lb. Blood pressure is 102/70 mm Hg; pulse, 70 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 98.4°F. His oxygen saturation is 98% on room air. Pertinent physical findings include a grade II/VI holosystolic murmur and a grade III/VI diastolic murmur, with a prominent S2 best heard at the left lower sternal border. There is no jugular venous distention, no peripheral edema, and no abnormal pulmonary finding. An ECG previously ordered for today’s visit reveals the following: a ventricular rate of 63 beats/min; PR interval, 196 ms; QRS duration, 174 ms; QT/QTc inter-val, 460/470 ms; P axis, 34°; R axis, –67°; and T axis, 56°. What is your interpretation of this ECG? How does the patient’s history predict the findings?
Dyspnea Confines Woman to Wheelchair
ANSWER
The ECG shows normal sinus rhythm, right atrial enlargement, a left anterior fascicular block, and evidence of an old anterolateral MI. Normal sinus rhythm is evidenced by the presence of a P wave for each QRS complex at a rate of 60 to 100 beats/min. Right atrial enlargement is diagnosed by the presence of tall, peaked P waves ≥ 2.5 mm in leads II, III, and aVF, and is a result of the patient’s pulmonary hypertension (P pulmonale).
A left anterior fascicular block is evidenced by the presence of left-axis deviation (typically between –45° and –90°), small R and large S complexes in leads II, III, and aVF, small Q waves in leads I and aVL, a QRS duration < 120 ms, and poor R-wave progression in leads V1 to V3 and deep S waves in V5 to V6.
The usual criteria for an anterolateral MI include Q, QS, or QRS complexes in leads V4 to V6 with ST-T wave changes. Poor R-wave progression in the absence of Q, QS, or QRS complexes in the anterolateral precordial leads (seen in this ECG) is also consistent with an old anterolateral MI.
ANSWER
The ECG shows normal sinus rhythm, right atrial enlargement, a left anterior fascicular block, and evidence of an old anterolateral MI. Normal sinus rhythm is evidenced by the presence of a P wave for each QRS complex at a rate of 60 to 100 beats/min. Right atrial enlargement is diagnosed by the presence of tall, peaked P waves ≥ 2.5 mm in leads II, III, and aVF, and is a result of the patient’s pulmonary hypertension (P pulmonale).
A left anterior fascicular block is evidenced by the presence of left-axis deviation (typically between –45° and –90°), small R and large S complexes in leads II, III, and aVF, small Q waves in leads I and aVL, a QRS duration < 120 ms, and poor R-wave progression in leads V1 to V3 and deep S waves in V5 to V6.
The usual criteria for an anterolateral MI include Q, QS, or QRS complexes in leads V4 to V6 with ST-T wave changes. Poor R-wave progression in the absence of Q, QS, or QRS complexes in the anterolateral precordial leads (seen in this ECG) is also consistent with an old anterolateral MI.
ANSWER
The ECG shows normal sinus rhythm, right atrial enlargement, a left anterior fascicular block, and evidence of an old anterolateral MI. Normal sinus rhythm is evidenced by the presence of a P wave for each QRS complex at a rate of 60 to 100 beats/min. Right atrial enlargement is diagnosed by the presence of tall, peaked P waves ≥ 2.5 mm in leads II, III, and aVF, and is a result of the patient’s pulmonary hypertension (P pulmonale).
A left anterior fascicular block is evidenced by the presence of left-axis deviation (typically between –45° and –90°), small R and large S complexes in leads II, III, and aVF, small Q waves in leads I and aVL, a QRS duration < 120 ms, and poor R-wave progression in leads V1 to V3 and deep S waves in V5 to V6.
The usual criteria for an anterolateral MI include Q, QS, or QRS complexes in leads V4 to V6 with ST-T wave changes. Poor R-wave progression in the absence of Q, QS, or QRS complexes in the anterolateral precordial leads (seen in this ECG) is also consistent with an old anterolateral MI.
A 46-year-old woman is undergoing evaluation for consideration of heart transplantation versus left ventricular assist device placement as destination therapy. She has had a significant decline in her functional capacity in the past six months (sharpest in the past two months), and now can walk for only half a block be-fore becoming short of breath. For the past month, she has been unable to walk more than 100 feet without dyspnea and now confines herself to a wheelchair. Medical history is remarkable for type 1 diabetes requiring insulin pump therapy; multivessel coronary artery disease (CAD) with angioplasty and stent placement; coronary artery bypass grafting (CABG; left internal thoracic artery graft to left anterior descending artery and reverse saphenous vein graft to the first obtuse marginal branch); an anterior wall myocardial infarction (MI) one year after her CABG; severe ischemic cardiomyopathy with a left ventricular ejection fraction of 18%; implantable defibrillator system for primary prevention of sudden cardiac death; pulmonary hypertension; and hyperlipidemia. Family history is remarkable for diabetes, MI, and sudden death. Social history reveals that despite her ill health, she continues to smoke 1½ packs of cigarettes per day, as she has for the past 30 years. She denies alcohol or illicit drug use. Her medication list is extensive: digoxin, atorvastatin, metoprolol, ramipril, spironolactone, torsemide, aspirin, clopidogrel, omeprazole, ondansetron, insulin pump, sildenafil, and sublingual nitroglycerin. She is allergic to penicillin and cephalosporins. The review of systems is remarkable for early satiety with occasional nausea and vomiting. She states she has difficulty sleeping, and her spouse states she snores very loudly and has witnessed several apneic spells. Physical examination reveals an anxious, obese woman sitting in a wheelchair. Blood pressure is 89/50 mm Hg; pulse, 90 beats/min and regular; respiratory rate, 14 breaths/min; O2 saturation, 94% on room air; and temperature, 36.4°C. Pertinent physical findings include bilateral diabetic retinopathy, jugular venous pressures at 8 to 9 cm, brisk carotid upstrokes without bruits, and late expiratory wheezes in both lung bases. An implantable defibrillator is noted in the infraclavicular area on the left chest. The heart rate is regular, with a 3/6 holosystolic murmur (best heard at the left sternal border) that radiates to the left axilla. The abdomen is large, with the liver span palpable at the right costal margin, and an insulin pump is noted. The extremities reveal 2+ pitting edema to the knees bilaterally, and evidence of recent cellulitis is noted on the left leg below the knee. The neurologic exam is remarkable for diabetic paresthesias in both feet. As part of her work-up, an ECG is obtained and shows the following: a ventricular rate of 90 beats/min; PR interval, 138 ms; QRS duration, 88 ms; QT/QTc inter-val, 370/450 ms; P axis, 81°; R axis, –48°; and T axis, 75°. What is your interpretation of this ECG?
Should This Fitness Instructor Worry About Her Heart?
ANSWER
The ECG shows sinus tachycardia with premature atrial contractions. The premature atrial contractions occur at the 14th and 16th beats on the rhythm strip. They are evident by the shortened R-R interval preceding the beat, with the QRS complex appearing similar to the normal QRS complexes, signifying they propagate through the normal conduction system.
The P waves are hidden from view in the previous T wave. The nonspecific S- and T-wave abnormalities are physiologic in nature and of no consequence. Finally, the large S waves seen in the precordial leads are due to the patient’s thin body habitus and not to ventricular hypertrophy.
The patient was reassured that there were no structural abnormalities of her heart, and that there was no need to treat the premature contractions at this time. She was also asked to monitor her caffeine and energy drink intake to determine whether there was a correlation with her palpitations.
She was relieved to hear that there are no restrictions in her physical activity
ANSWER
The ECG shows sinus tachycardia with premature atrial contractions. The premature atrial contractions occur at the 14th and 16th beats on the rhythm strip. They are evident by the shortened R-R interval preceding the beat, with the QRS complex appearing similar to the normal QRS complexes, signifying they propagate through the normal conduction system.
The P waves are hidden from view in the previous T wave. The nonspecific S- and T-wave abnormalities are physiologic in nature and of no consequence. Finally, the large S waves seen in the precordial leads are due to the patient’s thin body habitus and not to ventricular hypertrophy.
The patient was reassured that there were no structural abnormalities of her heart, and that there was no need to treat the premature contractions at this time. She was also asked to monitor her caffeine and energy drink intake to determine whether there was a correlation with her palpitations.
She was relieved to hear that there are no restrictions in her physical activity
ANSWER
The ECG shows sinus tachycardia with premature atrial contractions. The premature atrial contractions occur at the 14th and 16th beats on the rhythm strip. They are evident by the shortened R-R interval preceding the beat, with the QRS complex appearing similar to the normal QRS complexes, signifying they propagate through the normal conduction system.
The P waves are hidden from view in the previous T wave. The nonspecific S- and T-wave abnormalities are physiologic in nature and of no consequence. Finally, the large S waves seen in the precordial leads are due to the patient’s thin body habitus and not to ventricular hypertrophy.
The patient was reassured that there were no structural abnormalities of her heart, and that there was no need to treat the premature contractions at this time. She was also asked to monitor her caffeine and energy drink intake to determine whether there was a correlation with her palpitations.
She was relieved to hear that there are no restrictions in her physical activity
A 38-year-old woman presents to your clinic with a two-year history of palpitations that have not increased in severity or frequency. Although they are bother-some, she has had no chest pain, shortness of breath, dyspnea on exertion, or peripheral edema. She denies any symptoms of tachycardia, bradycardia, syn-cope, or near syncope. She works at a local health club as a Zumba instructor and teaches four spinning classes per week. She recently learned that the health club will be closing. As a result, until she finds another position, she will be without benefits. She states she wants to “get this checked out” before she loses her medical insurance. Medical history is unremarkable, with the exception of a right clavicle fracture sustained at age 15. She began menses at age 12, has never been pregnant, and has never had surgery. Family history is remarkable for hypertension and diabetes. Her parents and three siblings are alive and well. The patient has no known drug allergies. Her medications include ibuprofen as needed for musculoskeletal pain and an oral contraceptive. She denies recreational drug use. The review of systems is unremarkable, and her last menstrual period was 11 days ago. On physical exam, she is a thin, well-developed, athletic-appearing woman in no distress. Her height is 69”, and her weight is 144 lb. Blood pressure is 108/56 mm Hg; pulse, 58 beats/min and regular; respiratory rate, 14 beats/min; and temperature, 98.4°F. There are no murmurs, gallops, or rubs on her cardiac exam. Her lungs are clear. Her abdomen is flat and nontender, with good bowel tones in all quadrants. There is no peripheral edema. Peripheral pulses are full and bounding bilaterally in all four extremities. The neurologic exam is normal. A chemistry panel, complete blood count, lipid panel, and thyroid function studies are ordered; the results are all within normal limits. A transthoracic echocardiogram shows normal valves, normal wall motion, and a left ventricular ejection fraction of 75%. A baseline ECG shows no ectopic beats. She is placed on a continuous rhythm monitor for 10 minutes, and no ectopic, premature, or dropped beats are seen. At that point, the patient remembers that the palpitations often occur just as she starts exercising, then go away once her heart rate is elevated. You have her do jumping jacks in the examination room for 30 seconds, and she states she can feel the palpitations. You quickly obtain an ECG, which reveals the following: a ventricular rate of 117 beats/min; PR interval, 158 ms; QRS duration, 110 ms; QT/QTc interval, 336/468 ms; P axis, 57°; R axis, 15°; and T axis, 153°. What is your interpretation of this ECG?
Woman with Metabolic Syndrome
ANSWER
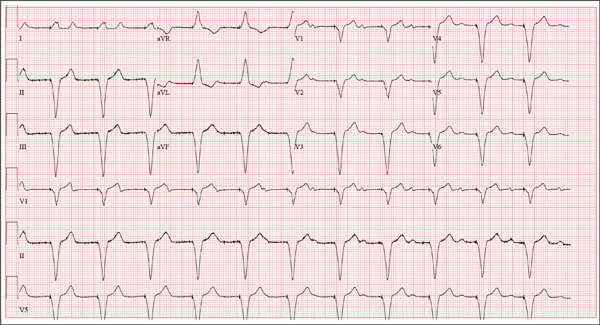
The correct interpretation of this ECG includes sinus rhythm with frequent premature ventricular complexes (PVCs), a T-wave abnormality suggesting lateral ischemia, and a prolonged QT interval.
PVCs occur when conduction of the ventricular myocardium occurs without involving the normal His-Purkinje system. They are responsible for the patient’s irregular pulse.
A prolonged QT interval is evidenced by a QTc interval > 440 ms. The QTc is calculated from Bazett’s formula, which states the QTc = QT interval divided by the square root of the previous R-R interval. The normal range for a QTc is generally considered to be 350 to 440 ms.
Inverted T waves in leads V3 to V6 are suggestive of lateral ischemia. However, they are also seen in subacute or old pericarditis and myocarditis, so clinical correlation is required. The patient has had no recent or remote episodes of chest pain or chest discomfort in the past year.
ANSWER
The correct interpretation of this ECG includes sinus rhythm with frequent premature ventricular complexes (PVCs), a T-wave abnormality suggesting lateral ischemia, and a prolonged QT interval.
PVCs occur when conduction of the ventricular myocardium occurs without involving the normal His-Purkinje system. They are responsible for the patient’s irregular pulse.
A prolonged QT interval is evidenced by a QTc interval > 440 ms. The QTc is calculated from Bazett’s formula, which states the QTc = QT interval divided by the square root of the previous R-R interval. The normal range for a QTc is generally considered to be 350 to 440 ms.
Inverted T waves in leads V3 to V6 are suggestive of lateral ischemia. However, they are also seen in subacute or old pericarditis and myocarditis, so clinical correlation is required. The patient has had no recent or remote episodes of chest pain or chest discomfort in the past year.
ANSWER
The correct interpretation of this ECG includes sinus rhythm with frequent premature ventricular complexes (PVCs), a T-wave abnormality suggesting lateral ischemia, and a prolonged QT interval.
PVCs occur when conduction of the ventricular myocardium occurs without involving the normal His-Purkinje system. They are responsible for the patient’s irregular pulse.
A prolonged QT interval is evidenced by a QTc interval > 440 ms. The QTc is calculated from Bazett’s formula, which states the QTc = QT interval divided by the square root of the previous R-R interval. The normal range for a QTc is generally considered to be 350 to 440 ms.
Inverted T waves in leads V3 to V6 are suggestive of lateral ischemia. However, they are also seen in subacute or old pericarditis and myocarditis, so clinical correlation is required. The patient has had no recent or remote episodes of chest pain or chest discomfort in the past year.
A 50-year-old woman with metabolic syndrome presents for a routine clinic appointment. You quickly review the five criteria of metabolic syndrome: • Fasting blood glucose ≥ 110 mg/dL • Waist circumference ≥ 40” in men or ≥ 35” in women • Triglycerides ≥ 150 mg/dL • HDL cholesterol < 40 ¬mg/dL in men or < 50 mg/dL in women • Blood pressure ≥ 130/85 mm Hg. The patient’s last clinic visit was four months ago; since then, she has done well and has no specific complaints or concerns. She denies angina, palpitations, dizziness, syncope, or dyspnea. Medical history is significant for New York Heart Association class III heart failure and cardiomyopathy secondary to myopericarditis with small-vessel coronary artery disease, as well as depression with anxiety. She also has a history of obstructive sleep apnea, but refuses to use a constant positive airway pressure (CPAP) machine at night due to claustrophobia. She attempts to control her diabetes with diet and exercise but admits she isn’t very compliant. Her medication list includes amlodipine, furosemide, carvedilol, lisinopril, isosorbide dinitrate, hydralazine, spironolactone, simvastatin, citalopram, omeprazole, and oxybutynin. She is allergic to ampicillin, methocarbamol, and codeine. The patient’s family history is unknown, as she was adopted. She works as a comptroller for a municipality in the suburbs, is recently divorced, and does not smoke or drink. Her review of systems is remarkable for headaches, anxiety, and loneliness following her divorce. She denies thoughts of injuring herself or suicide. Physical examination reveals a blood pressure of 118/64 mm Hg; pulse, 88 beats/min and irregular; respiratory rate, 16 breaths/min-1; and temperature, 99.2°F. Her weight is unchanged from her last visit. Her lungs are clear bilaterally, the jugular venous pressure is approximately 4 cm, and her cardiac exam reveals no murmurs, rubs, or extra heart sounds. Her abdomen is benign, and she has strong pulses bilaterally with 1+ pitting edema in both lower extremities, limited to the ankles. Laboratory data demonstrate chemical and lipid profiles and complete blood count within normal limits. An echocardiogram performed at her previous visit showed a left ventricular ejection fraction of 45%, with a mildly enlarged left ventricle, normal right ventricular size and function, and no valvular anomalies. It has been a year since her last ECG, so you decide to order one. It reveals the following: a ventricular rate of 87 beats/min; PR interval, 138 ms; QRS duration, 86 ms; QT/QTc interval, 388/466 ms; P axis, 61°; R axis, 43°; and T axis, 9°. What is your interpretation of this ECG?
Alaskan Man is Concerned About Going Home
ANSWER
The correct interpretation includes normal sinus rhythm with a premature supraventricular complex, a rightward axis, and a QR pattern in V1 suggestive of right ventricular conduction delay.
The eighth beat in the rhythm strip is the premature supraventricular complex. It occurs earlier than the rate of the normal sinus rhythm, and there is a compensatory pause prior to resumption of the next sinus beat.
A right axis is evidenced by an R-wave axis > 100° and is common in chronic obstructive pulmonary disease. Right ventricular conduction delay, or incomplete right bundle branch block, occurs when conduction is slowed through the right bundle. ECG criteria include an RSR’ or QR pattern with a QRS duration of 100 to 120 ms, with similar terminal features of a normal QRS. In this case, the QRS pattern is < 100 ms; however, the QR pattern in lead V1 is suspicious.
ANSWER
The correct interpretation includes normal sinus rhythm with a premature supraventricular complex, a rightward axis, and a QR pattern in V1 suggestive of right ventricular conduction delay.
The eighth beat in the rhythm strip is the premature supraventricular complex. It occurs earlier than the rate of the normal sinus rhythm, and there is a compensatory pause prior to resumption of the next sinus beat.
A right axis is evidenced by an R-wave axis > 100° and is common in chronic obstructive pulmonary disease. Right ventricular conduction delay, or incomplete right bundle branch block, occurs when conduction is slowed through the right bundle. ECG criteria include an RSR’ or QR pattern with a QRS duration of 100 to 120 ms, with similar terminal features of a normal QRS. In this case, the QRS pattern is < 100 ms; however, the QR pattern in lead V1 is suspicious.
ANSWER
The correct interpretation includes normal sinus rhythm with a premature supraventricular complex, a rightward axis, and a QR pattern in V1 suggestive of right ventricular conduction delay.
The eighth beat in the rhythm strip is the premature supraventricular complex. It occurs earlier than the rate of the normal sinus rhythm, and there is a compensatory pause prior to resumption of the next sinus beat.
A right axis is evidenced by an R-wave axis > 100° and is common in chronic obstructive pulmonary disease. Right ventricular conduction delay, or incomplete right bundle branch block, occurs when conduction is slowed through the right bundle. ECG criteria include an RSR’ or QR pattern with a QRS duration of 100 to 120 ms, with similar terminal features of a normal QRS. In this case, the QRS pattern is < 100 ms; however, the QR pattern in lead V1 is suspicious.
A 65-year-old man who lives in a remote village in Alaska is in your area on vacation. He presents to your office stating he has had a cold for the past three weeks that “just won’t go away.” He has tried several OTC medications without success, and he now has a productive cough. You notice as you walk into the examining room that it reeks of cigarette smoke. On questioning the patient, you learn that he has smoked two to three packs of cigarettes a day for most of his life. He is proud to announce that now he is down to 1.5 packs per day. He denies chest pain, fevers, chills, or night sweats, but admits that he is more short of breath than usual and has discomfort in his right chest. He can only walk 25 or 30 feet before he must rest, and he cannot climb one flight of stairs without stopping. He plans to return home in four days and is concerned that he won’t be able to function independently, stating, “You can die up there pretty easily if you’re not up to speed.” His medical history is remarkable for coronary artery disease with three-vessel coronary artery revascularization in 2004, paroxysmal atrial fibrillation, dyslipidemia, chronic obstructive pulmonary disease, and arthritis. Current medications include allopurinol, aspirin, atenolol, fluticasone-salmeterol and albuterol inhalers, folic acid, furosemide, isosorbide mononitrate, lisinopril, potassium chloride, rosuvastatin, and warfarin. He acknowledges that he does not take his warfarin routinely. He is allergic to codeine. Family history is remarkable for a father who died of a myocardial infarction at age 63, and two younger brothers who have had coronary revascularization procedures. He is a retired commercial fisherman who lives alone. He admits to drinking one six-pack of beer per day and occasionally smoking marijuana. A review of systems is remarkable for recurring headaches and a 10-lb weight loss over the past three months. The physical exam reveals a disheveled man in no distress. His blood pressure is 160/94 mm Hg; pulse, 70 beats/min; respirations, 18 breaths/min-1; and temperature, 100.4°F. His teeth are in poor repair, with multiple caries. The lungs reveal diminished vesicular breath sounds throughout with late inspiratory crackles in the right upper lung fields and few breath sounds with late expiratory wheezes in the right lower quadrant. The neck veins are flat, and there are no murmurs, rubs, or extra heart sounds. The abdomen is obese but benign, and there are no neurologic findings. Pertinent laboratory findings include a white blood count of 14,300/mm3 with 75% neutrophils, 20% bands, and 15% lymphocytes. A chest x-ray reveals normal cardiac size, sternotomy wires and surgical clips, and right lower-lobe consolidation consistent with right lower lobe pneumonia. An ECG shows the following: a ventricular rate of 65 beats/min; PR interval, 162 ms; QRS duration, 90 ms; QT/QTc interval, 448/465 ms; P axis, 60°; R axis, 101°; and T axis, 55°. What is your interpretation of this ECG?