User login
Man Gets Burning Sensation in Chest During an Argument
ANSWER
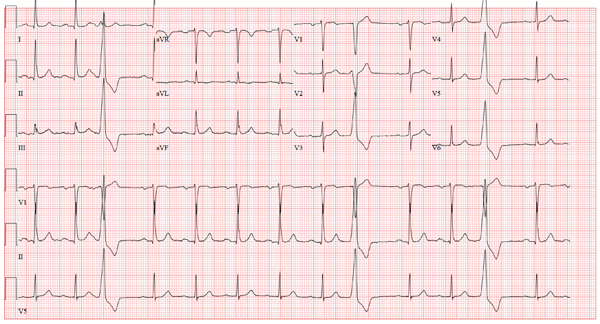
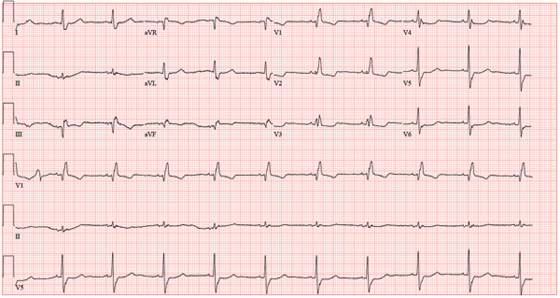
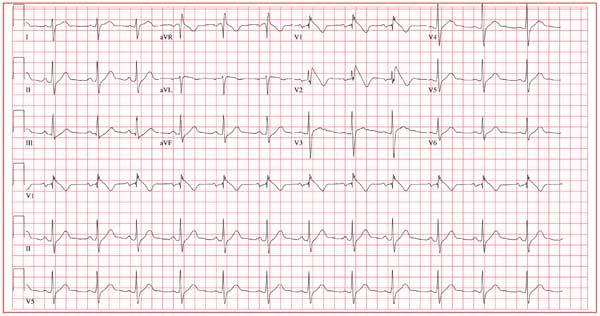
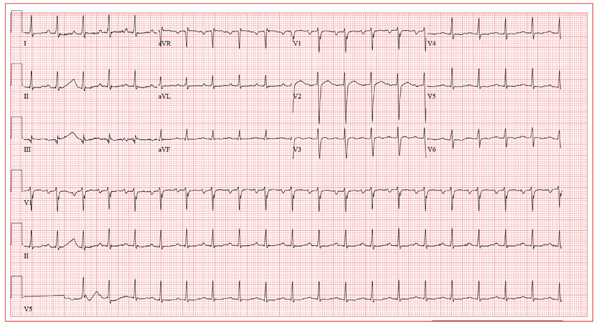
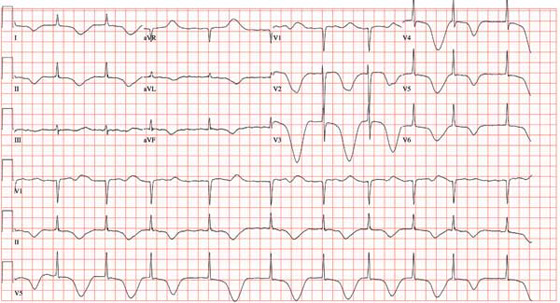
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
ANSWER
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
ANSWER
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
An 80-year-old man presents to your office after having two separate episodes of chest pain. The first occurred two weeks ago, while the patient was arguing with his home health nurse. He describes the pain as a “burning” sensation deep in his chest—similar to that from his long-standing history of esophageal reflux, with the exception that the onset and resolution were much quicker. A second, similar episode occurred two days ago, again during an argument with his nurse. He did not disclose either episode to the nurse. However, he was sufficiently concerned about the possibility of a cardiac cause that he decided to see you. When questioning him about his chest pain, you learn that there was no associated diaphoresis, shortness of breath, or pain radiation to the neck or arm. He denies symptoms of bradycardia, tachycardia, or palpitations. When you question him about the argument with his nurse, you learn that he has been eating chips and salsa, which you have previously advised against, given his history of esophageal reflux, Barrett’s esophagus, and endoscopic confirmation of esophageal dysplasia. The medical history is also significant for bilateral below-knee amputations from trauma sustained during army service in the Korean War. He has had multiple bilateral stump revisions, such that he can no longer wear prostheses and is wheelchair bound. Adenomatous colonic polyps, iron-deficiency anemia, hypothyroidism, asthma, benign prostatic hypertrophy, glaucoma, and Parkinson’s disease complete the medical history. The family history is remarkable for a father who died of a hemorrhagic stroke and a mother who died of renal failure. The patient, a widower, resides at home with a live-in nurse and a housekeeper. His medication list includes aspirin, lisinopril, levothyroxine, carbidopa/levodopa, and travoprost and timolol eye drops. He is allergic to sulfa. The review of symptoms is remarkable for urinary retention and recent resolution of diarrhea. Pertinent physical findings in this pleasant elderly man include audible wheezing and a raspy voice. The lungs are diffusely wheezy on expiration, and there is no conversational dyspnea or accessory muscle use. The neck veins are flat, and while heart sounds are distant, there are no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. A low-amplitude tremor is present in both hands, and there is no cogwheeling. Serum B-type natriuretic peptide is 190 pg/mL and serum troponin levels are negative. An ECG reveals the following: a ventricular rate of 79 beats/min; PR interval, 212 ms; QRS duration, 92 ms; QT/QTc interval, 358/410 ms; P axis, 35°; R axis, 47°; and T axis, 69°. What is your interpretation of this ECG?
Woman Faints During Concert
ANSWER
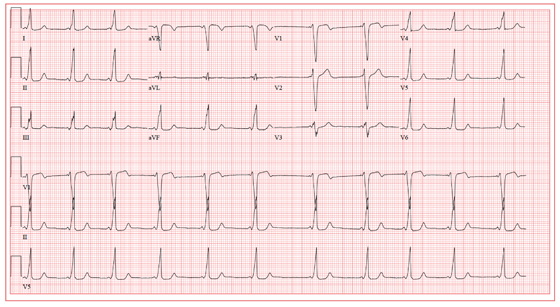
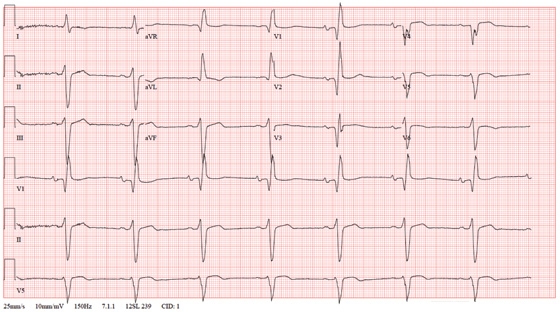
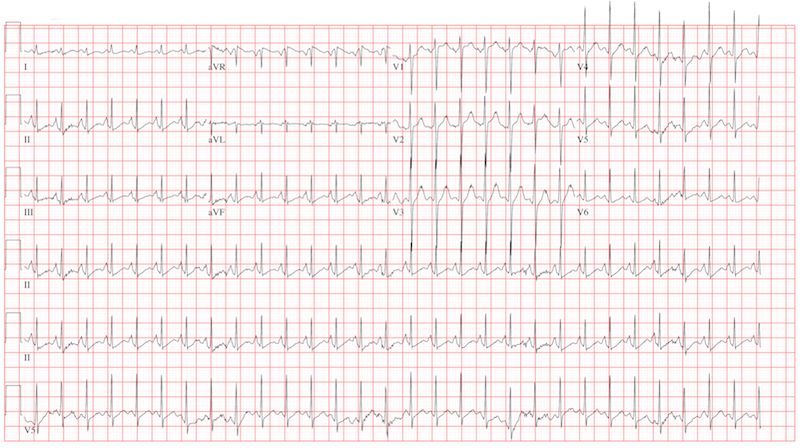
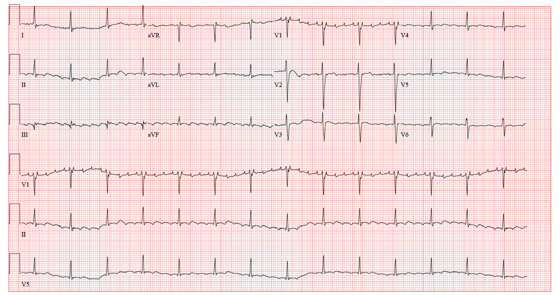
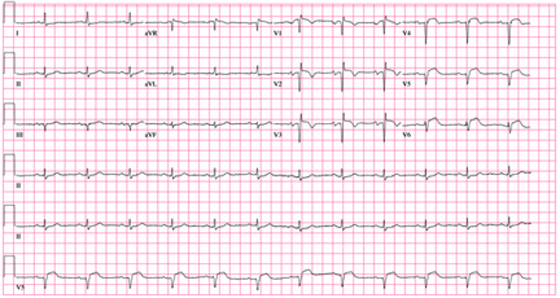
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
ANSWER
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
ANSWER
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
A19-year-old woman is referred from the emergency department (ED) for follow-up. While attending a concert last weekend, she experienced an episode of syncope, was promptly resuscitated by EMTs on site, and was taken by friends to the ED for evaluation. On arrival, she was alert and oriented, albeit embarrassed that she was responsible for her friends missing the remainder of the concert. She admitted having a couple of beers and thought she may have been dehydrated. Following a history, physical exam, lab work, and an ECG, she was discharged in stable condition and asked to follow up in your clinic. As you ask her to remember the episode, she does not recall becoming light-headed or dizzy, and denies having chest pain or palpitations. She says her medical history is unremarkable; however, upon careful questioning, she admits having had several episodes of near-syncope beginning at age 16, with the most recent occurring six months ago. She is a freshman at a local community college and works as a barista at a local coffeehouse. She has no drug allergies and is currently taking no medications. She drinks socially although she is underage, does not smoke, and denies recreational drug use. Her review of systems is negative, and her physical exam is within normal limits for her gender and age. Her last menstrual period was two weeks ago. Reviewing the medical records from the ED, you discover the blood alcohol content was 0.08 and the toxicology screen was negative. A serum beta human chorionic gonadotropin (β-HCG) for pregnancy was negative as well. The ECG reveals a ventricular rate of 64 beats/min; PR interval, 64 ms; QRS duration, 146 ms; QT/QTc interval, 454/468 ms; P axis, unmeasurable; R axis, 60°; and T axis, 92°. What is your interpretation of this ECG, and what do you suspect is the cause of her syncope?
Atrial Flutter Follow-up
ANSWER
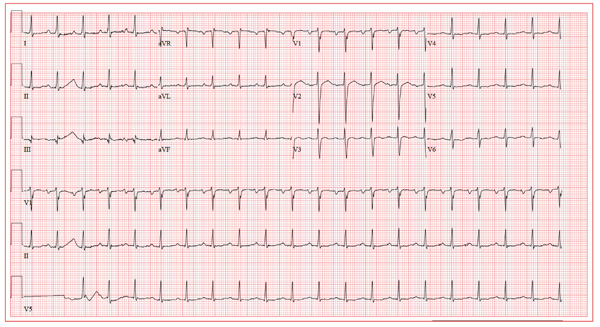
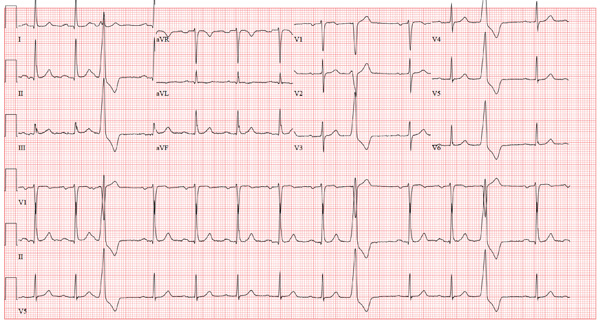
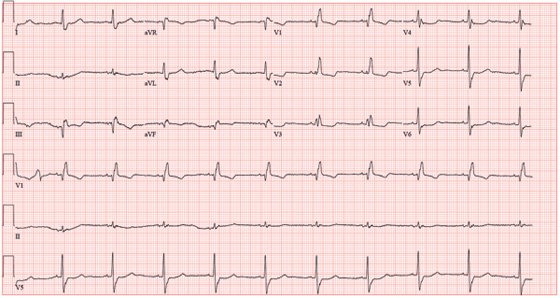
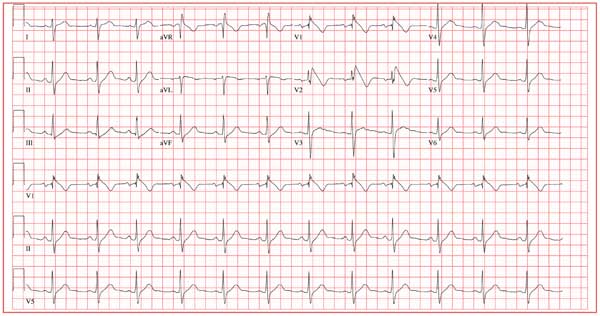
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
ANSWER
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
ANSWER
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
A 39-year-old business professional returns to your clinic for follow-up one month after a synchronized cardioversion to treat abrupt-onset atrial flutter (see January 2012 ECG Challenge). He is slightly short of breath, he says, because he ran up six flights of stairs to see you in clinic after undergoing an echocardiogram. Briefly, he developed atrial flutter presumably as a result of consuming a large quantity of caffeinated coffee along with several energy drinks containing taurine. He has been under a significant amount of stress at work for the past six months, working on a project that he predicted would play a major role in his career. The deadline has come and gone, and his business transaction was a success. He has taken your advice to avoid energy drinks, consume coffee in moderation, stop smoking, get plenty of rest, and exercise. His affect is much improved. He is pleasant, jovial, and relieved that he has had no subsequent episodes of atrial flutter. His medical history is remarkable for that single episode of atrial flutter, as well as childhood cases of chickenpox and mumps. He is taking ibuprofen for a sore knee as a result of “too much basketball.” He has no known drug allergies. Following his cardioversion, his alcohol consumption decreased from two cocktails in the evening and a 12-pack of beer on the weekends to an occasional cocktail during the week and two to four beers on the weekends. He denies illicit drug use. The review of systems is unremarkable. The physical exam reveals a thin, well-developed man in no distress. His weight is 170 lb and his height, 74”. Vital statistics include a blood pressure of 128/72 mm Hg; pulse, 110 beats/min; respiratory rate, 16 breaths/min; temperature, 98.4°F; and O2 saturation, 100% on room air. The chest is clear to auscultation in all lung fields. There are no murmurs, rubs, clicks, or extra heart sounds. The abdomen is soft and nontender. The pulses are equal and bounding bilaterally. The neurologic exam is benign. The echocardiogram performed earlier shows a left ventricular ejection fraction of 68%, normal left and right ventricular volumes and function, normal valvular function, and a left atrial measurement of 3.8 cm (normal, 1.6 to 4.0 cm). An ECG performed just before you entered the exam room reveals the following: a ventricular rate of 122 beats/min; PR interval, 184 ms; QRS duration, 90 ms; QT/QTc interval, 282/401 ms; P axis, 24°; R axis, 28°; and T axis, –45°. What is your interpretation of this ECG?
Are Energy Drinks Causing This Man's Shortness of Breath?
ANSWER
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
ANSWER
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
ANSWER
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
A business professional, age 39, presents with shortness of breath that abruptly began two hours ago. He states he has been under a significant amount of stress at work during the past six months. He is approaching a deadline on a very important contract, which he says will “make or break” his career. As a result, he has been working long hours and often consumes eight to 10 cups of coffee as well as three to five energy drinks per day. After getting only three hours of sleep last night, he had two cups of coffee with a “two–energy-drink chaser.” About one hour after his last energy drink, he felt several palpitations and abruptly became short of breath. There is no history of pulmonary or cardiac illness. The patient’s medical history is unremarkable, with the exception of childhood cases of chickenpox and mumps. He has never had a surgical procedure. He takes ibuprofen on occasion after playing sports and has no known drug allergies. During college, he smoked one pack of cigarettes per day, ceasing at graduation. In response to work-related stress, he has started smoking again and is up to half a pack per day. His alcohol consumption consists of two cocktails in the evening and a 12-pack of beer on the weekends. He denies illicit drug use. The review of systems is remarkable for heartburn, bloating, and frequent indigestion. He denies nausea, vomiting, diarrhea, or constipation. The physical examination reveals a well-developed, anxious male in mild distress. His weight is 174 lb and his height is 74 in. Vital signs include a blood pressure of 90/58 mm Hg; pulse, 88 beats/min; respiratory rate, 18 breaths/min; and temperature, 98°F. His O2 saturation is 99% on room air. The HEENT exam is normal. There is no thyromegaly. The mucous membranes are pink and moist. The chest is clear to auscultation in all lung fields with excellent diaphragmatic excursion. The pulse is regular. There are no murmurs, rubs, clicks, or extra heart sounds. The abdomen is soft and nontender. The liver and spleen are not palpable. The pulses are equal and strong bilaterally. The neurologic exam is unremarkable. A chest x-ray, blood chemistry, complete blood count, and electrocardiogram are ordered. You are handed an ECG tracing that reveals the following: a ventricular rate of 84 beats/min; PR interval, 208 ms; QRS duration, 102 ms; QT/QTc interval, 358/423 ms; R axis, 20°; and T axis, 29°. What is your interpretation of this ECG?
Ederly Woman Experiences Chest Pain While Knitting
ANSWER
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
ANSWER
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
ANSWER
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
An 84-year-old woman presents with left-sided chest pain radiating to the back and neck. The pain began about four hours ago, while she was knitting. She describes it as a “dull ache” that quickly progressed to a “sharp, sticking” pain on a scale of 8/10. She has never experienced pain like this before. She denies nausea, vomiting, diaphoresis, headache, palpitations, orthopnea, or dyspnea on exertion. Her medical history is remarkable for Crohn’s disease, atrial fibrillation, hypertension, and myxomatous mitral valve disease. Surgical history is remarkable for a myocardial infarction 10 years ago, two separate catheter ablations for atrial fibrillation (successful on the second attempt), a mitral valve replacement (bioprosthetic) one year ago, and a hysterectomy/oophorectomy in the remote past. The patient has no known drug allergies. Her medications include atenolol, aspirin, furosemide, estradiol, ferrous sulfate, mesalamine, omeprazole, warfarin, and lisinopril. She is a retired teacher, married, who has never smoked and rarely drinks alcohol. Her family history is remarkable for heart disease in her father and diabetes in her mother. The review of systems is negative, with the exception of frequent episodes of nonbloody diarrhea and abdominal pain associated with her Crohn’s disease. Physical exam reveals a blood pressure of 208/120 mm Hg; pulse, 60 beats/min; respiratory rate, 22 breaths/min-1; temperature, 97.8°F; and O2 saturation, 96% on 2L oxygen. She appears anxious, restless, and unable to find a comfortable position. Pertinent physical findings include jugular venous distention to the angle of the jaw, a regular heart rate with a harsh III/VI systolic murmur at the left upper sternal border, and a soft II/VI diastolic murmur radiating to the apex. Peripheral pulses are brisk and equal bilaterally. There are no neurologic deficits. Laboratory data include a normal complete blood count, an INR of 2.2, normal blood chemistries, normal liver function studies, and negative troponin levels. CT reveals a 5.5-cm dissection of the ascending aorta. An ECG shows the following: a ventricular rate of 61 beats/min; PR interval, 108 ms; QRS duration, 132 ms; QT/QTc interval, 478/481 ms; P axis, 19°; R axis, 0°; and T axis, –13°. What is your interpretation of this ECG?
Widower Experiencing Fatigue
ANSWER
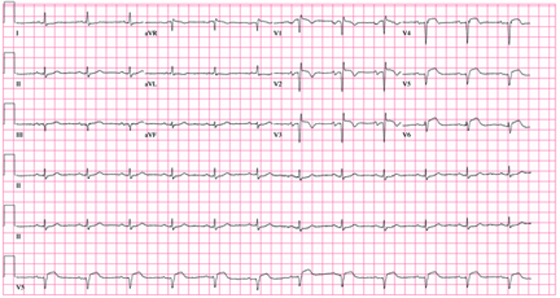
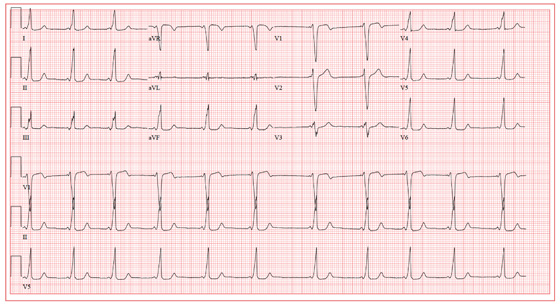
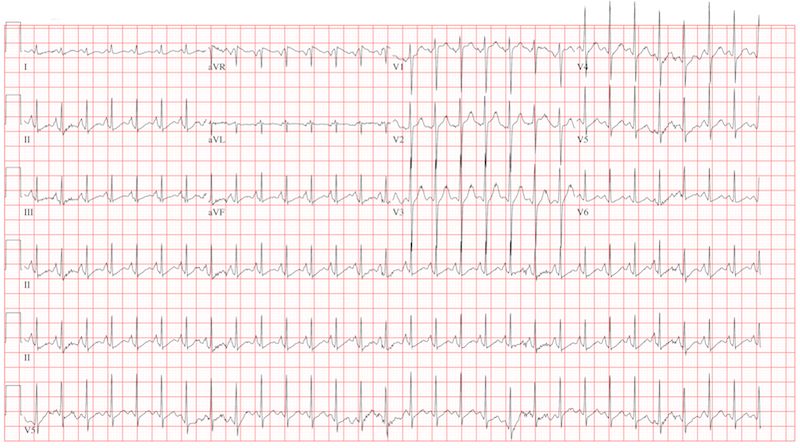
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
ANSWER
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
ANSWER
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
A 72-year-old man presents for a routine appointment. He was doing well until two months ago, when he started to notice that he fatigues easily. He is unable to go up and down stairs at home without pausing and has difficulty working in his garden. He says he does not become short of breath but just feels fatigued. The patient denies chest pain, palpitations, tachycardia, syncope, or near-syncope. He denies recent weight gain or peripheral extremity edema. He has had no recent changes to his medications, and he has not recently been ill. The man’s cardiac history is remarkable for coronary artery disease, a coronary artery bypass graft (CABG) in 2007, paroxysmal atrial fibrillation, and an ischemic cardiomyopathy. His most recent echocardiogram (six months ago) showed global left ventricular dysfunction with inferior akinesis, a left ventricular end-diastolic dimension of 8.1 cm, and a left ventricular ejection fraction of 35%. His pulmonary artery pressure was 25 to 29 mm Hg. A nuclear viability study performed at the same time showed a nonviable myocardial infarction involving the anterior and inferior septal walls of the left ventricle. A cardiac catheterization performed one year ago showed 30% stenosis of the left main coronary artery, an occluded left anterior descending (LAD) artery with myocardial perfusion supplied by right-to-left collateral vessels, 50% stenosis of the left circumflex artery, 70% stenosis of the left circumflex artery, and 70% to 80% stenosis of the mid right coronary artery (RCA). The saphenous vein grafts to the LAD, RCA, circumflex, and diagonal branches were occluded. Medical history is remarkable for dyslipidemia, arthritis, and depression. In addition to CABG, surgical history includes cholecystectomy and a left hip replacement. The patient is a retired beer distributor who has lived alone since his wife’s death three years ago. He drinks two or three glasses of wine in the evenings. Prior to quitting 10 years ago, he had a 30-pack-year history of smoking; however, he started again after his wife’s death and currently smokes half a pack of cigarettes per day. His medication list includes aspirin, atenolol, hydrochlorothiazide, lisinopril, atorvastatin, and trazodone. The review of systems is negative. Vital statistics include a blood pressure of 106/58 mm Hg; pulse, 50 beats/min; temperature, 97.5°F; and O2 saturation, 94% on room air. His weight is 172.4 lb and is unchanged from his last clinic visit. Pertinent findings on the physical exam include clear lung fields, a regular rhythm, and bradycardia with no murmurs or extra heart sounds, no bruits, no jugular venous distention, and no peripheral edema. All pulses are equal and normal. Based on the patient’s symptoms and the finding of bradycardia on physical exam, you order an ECG, which shows the following: a ventricular rate of 46 beats/min; PR interval, 202 ms; QRS duration, 200 ms; QT/QTc interval, 578/505 ms; P axis, 71°; R axis, –77°; and T axis, 109°. What is your interpretation of this ECG?
Man Found Unconscious In a Park
ANSWER
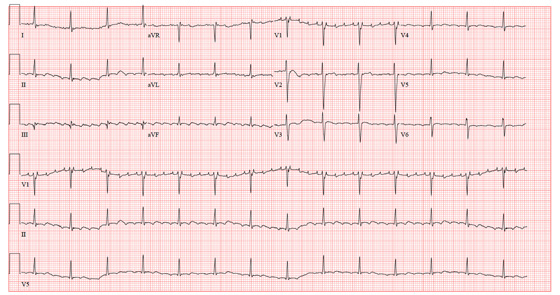
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
ANSWER
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
ANSWER
The ECG shows atrial fibrillation with a controlled ventricular response, a significantly prolonged QTc interval, and deep ST-T wave changes. The patient has chronic atrial fibrillation with a controlled ventricular response, so this arrhythmia is not unusual.
The deep ST-T wave changes and a prolonged QTc interval not seen on the previous ECG are consistent with a central nervous system injury. Cerebral disorders affect ventricular repolarization, as evidenced by depressed ST segments, flat or inverted T waves, and prolongation of the QTc interval. It is important to note that ST-segment elevations and deep T-wave changes do not always signify myocardial ischemia or injury.
This patient’s CT and MRI scans of the head showed no evidence of an intracranial bleed or cerebrovascular accident. A subsequent EEG showed epileptiform discharges, but no seizure activity.
The most likely cause of the ST-T wave changes is global intracranial hypoperfusion as a result of ventricular fibrillation with a prolonged resuscitation period. Over the course of the following two weeks, the ST-T wave changes and QTc prolongation normalized.
A 69-year-old man is found unconscious in a public park by a couple out for a walk. The husband tries to arouse the man to no avail; checking for a pulse and finding none, he asks his wife to call 911 while he begins CPR. His wife joins him after making the call, and they continue CPR for approximately 11 minutes, until paramedics arrive. An automatic external defibrillator is placed on the patient, who is found to be in ventricular fibrillation. The patient is intubated, and epinephrine and lidocaine are administered along with three shocks; the third restores the rhythm to normal sinus. The total resuscitation time is about 17 minutes. The patient is placed on a lidocaine drip and transported to the emergency department. On arrival, the man is unconscious but responsive to deep pain stimuli. An initial ECG shows atrial fibrillation with a controlled ventricular response. His serum troponin measures 2.7 µg/L and peaks at 3.1 µg/L. The medical record shows a history of coronary artery disease with coronary artery revascularization (left internal mammary artery–left anterior descending artery, saphenous vein graft–second diagonal artery) four years ago. The man also has a history of chronic atrial fibrillation, hypertension, hyperlipidemia, peptic ulcer disease, and a pulmonary embolus. The record also indicates that he smokes 1-1/2 packs of cigarettes per day, and drinks shots of tequila on weekends. Family history is remarkable for hypertension, diabetes, coronary artery disease, and breast cancer. He is allergic to aspirin (peptic ulcers), enalapril (cough), and penicillin. His most recent medication list includes atenolol, amlodipine, diltiazem, simvastatin, omeprazole, and warfarin. Because the patient is unconscious, a review of systems cannot be obtained. You assume care of the patient in the ICU. The nurse states that the patient’s vital signs were stable overnight, and there were no new arrhythmias. An abbreviated physical exam reveals no changes to his condition. The patient remains cool, sedated, and intubated. As you finish rounds, his nurse expresses concern that the patient has ongoing ischemia and asks you to review an ECG that was just obtained. The ECG shows the following: a ventricular rate of 62 beats/min; PR interval, indeterminate; QRS duration, 88 ms; QT/QTc interval, 718/728 ms; R axis, 35°; and T axis, 209°. What is your interpretation of this ECG, and what is the explanation for the dramatic changes overnight?
Chest Pain has "Gone On Long Enough"
ANSWER
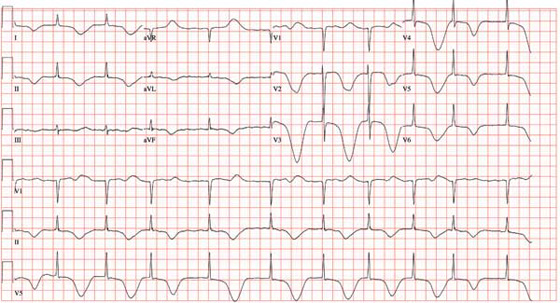
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
ANSWER
The correct interpretation of this ECG includes normal sinus rhythm, left atrial enlargement, and an anteroseptal myocardial infarction.
The diagnostic criteria for left atrial enlargement include a P-wave duration of ≥ 120 ms in lead II and/or a terminal negative component of a biphasic P wave in lead V1. In this example, the biphasic P wave is better seen in lead V2, while a large negative P wave is present in V1.
The diagnostic criteria for anteroseptal myocardial infarction include Q, QS, or QRS complexes in leads V1 through V4 along with evolving ST-T changes. In this example, leads V1 through V3 have large Q waves, while lead V4 has a large QS complex. All precordial leads contain ST-T wave elevations.
A 62-year-old African-American man presents to the urgent care center with a six-hour history of chest pain. He describes the pain as a “burning, achy” sensation with radiation to his left neck and shoulder. The pain started while the man was at rest but did not increase with activity. The patient denies symptoms such as shortness of breath, orthopnea, nausea, or vomiting. He says he had hoped the pain would resolve, but he now thinks it has “gone on long enough.” The patient has a history of similar chest pain four years ago. At that time, cardiac catheterization showed an 80% proximal stenosis of the left anterior descending (LAD) coronary artery. A drug-eluting stent was placed from the origin to the mid vessel of the LAD. Although the patient has a prescription for nitroglycerin, he hasn’t filled it in three months because he hasn’t experienced chest pain in more than a year and wanted to save money. Medical history is remarkable for type 1 diabetes, hypertension, hyperlipidemia, COPD, migraine, and diverticulitis. Surgical history is remarkable for an appendectomy during childhood. The patient is allergic to penicillin and cephalosporins. His current medication list includes insulin glargine, carvedilol, clopidogrel, ezetimibe, fenofibrate, hydrochlorothiazide, and aspirin (in addition to the nitroglycerin), but he has not taken any of these for two weeks due to financial constraints. The patient smokes 1½ packs of cigarettes daily and drinks an average of one case of beer per week. He does not know any details of his family history. The review of systems is remarkable for increased fatigue and weakness during the past week and for a migraine that the patient says is starting now. The physical exam reveals a blood pressure of 188/105 mm Hg; pulse, 70 beats/min; respiratory rate, 20 min-1; and temperature, 99°F. His weight is 119 lb, and his height is 68”. He is anxious, uncomfortable, and chronically ill appearing. Pertinent physical findings include pulmonary crackles in both bases, jugular venous distention to the angle of the jaw, a regular rate and rhythm with an S3 gallop, and a soft early systolic murmur at the left sternal border. He has no lower extremity edema, and his neurologic exam is intact. Abnormal laboratory data include: serum glucose of 318 mg/dL; creatinine, 2.6 mg/dL; troponin, 72 ng/mL; and B-type natriuretic peptide (BNP), 2,499 pg/mL. A stat ECG shows the following: a ventricular rate of 73 beats/min; PR interval, 160 ms; QRS duration, 88 ms; QT/QTc interval, 358/394; P axis, 39°; R axis, -3°; and T axis, 88°. What is your interpretation of this ECG?
Should This Man be Worried About Sudden Death?
ANSWER
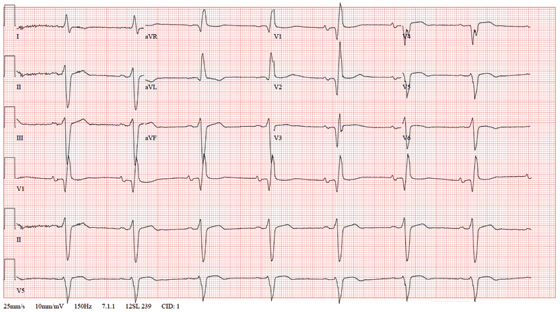
The ECG shows normal sinus rhythm, with a right-axis deviation (R wave axis > 90°) and a significant ST elevation noted in the anterior precordial leads consistent with a type 1 Brugada pattern. In this ECG, the elevated ST segment (≥ 2 mm) descends into an inverted T wave in leads V1 and V2.
The Brugada syndrome is due to a mutation in SCN5A, the alpha subunit of the cardiac sodium channel gene. Any clinical expression of the Brugada syndrome is related to ventricular arrhythmias, which are life-threatening.
Given his family history and his ECG, the patient is correct to be concerned. Genetic testing should be performed, and he should be referred for evaluation, including placement of an implantable defibrillator system for primary prevention of sudden cardiac death.
ANSWER
The ECG shows normal sinus rhythm, with a right-axis deviation (R wave axis > 90°) and a significant ST elevation noted in the anterior precordial leads consistent with a type 1 Brugada pattern. In this ECG, the elevated ST segment (≥ 2 mm) descends into an inverted T wave in leads V1 and V2.
The Brugada syndrome is due to a mutation in SCN5A, the alpha subunit of the cardiac sodium channel gene. Any clinical expression of the Brugada syndrome is related to ventricular arrhythmias, which are life-threatening.
Given his family history and his ECG, the patient is correct to be concerned. Genetic testing should be performed, and he should be referred for evaluation, including placement of an implantable defibrillator system for primary prevention of sudden cardiac death.
ANSWER
The ECG shows normal sinus rhythm, with a right-axis deviation (R wave axis > 90°) and a significant ST elevation noted in the anterior precordial leads consistent with a type 1 Brugada pattern. In this ECG, the elevated ST segment (≥ 2 mm) descends into an inverted T wave in leads V1 and V2.
The Brugada syndrome is due to a mutation in SCN5A, the alpha subunit of the cardiac sodium channel gene. Any clinical expression of the Brugada syndrome is related to ventricular arrhythmias, which are life-threatening.
Given his family history and his ECG, the patient is correct to be concerned. Genetic testing should be performed, and he should be referred for evaluation, including placement of an implantable defibrillator system for primary prevention of sudden cardiac death.
A 25-year-old Vietnamese man has lived in the United States since age 14. He was in his usual state of “excellent” health until one week ago, when he had an episode of syncope while walking along the shore of a lake with a friend. His friend told him that he lost consciousness without warning, fell to the ground, and promptly regained consciousness. He did not lose bowel or bladder control and did not injure himself. He attributed this episode to an insufficient intake of water on a hot, humid afternoon. Two days later, while talking to his father about the episode, he learned that he had a paternal uncle who died suddenly in his late 20s and a maternal aunt who died in her early 30s after similar episodes of syncope. Frightened that he may meet the same end, he presents to your clinic. He has no history of chest pain, palpitations, or dyspnea. Medical history is remarkable for an episode of pneumonia as a child. He has no known drug allergies and is currently taking no medications. He has smoked one pack of cigarettes per day since age 14, and he uses marijuana approximately twice a month. He drinks a six-pack of beer on weekends. He is married with no children and works in the IT department at a local community college. A detailed review of systems reveals no pertinent positive findings. He has had no loss of energy, trouble sleeping, or weight change (loss or gain). Physical examination reveals a blood pressure of 110/72 mm Hg; pulse, 70 beats/min and regular; and respiratory rate, 14 min-1. He is afebrile. His height is 68”, and his weight, 151 lb. He is well nourished and in no acute distress. The HEENT, neck, chest, cardiovascular, abdominal, musculoskeletal, and neurologic exams are all normal. Blood chemistries, complete blood count, lipid profile, liver profile, and thyroid function studies are all normal. You assure the patient that he is in excellent health. He remains concerned, however, and asks that you order an ECG—a request to which you reluctantly agree. The ECG reveals the following: a ventricular rate of 75 beats/min; PR interval, 168 ms; QRS duration, 88 ms; QT/QTc interval, 390/435 ms; P axis, 73°; R axis, 112°; and T axis, 63°. What is your interpretation—and does the patient have a legitimate concern regarding his risk for dying suddenly?
Worsening Symptoms in Woman with Cystic Fibrosis
ANSWER
The correct interpretation is sinus tachycardia with a short PR interval. This ECG illustrates a physiologic sinus rate response to hypercarbic respiratory failure secondary to an infectious exacerbation. A shortened PR interval occurs with an otherwise healthy conduction system in response to a rapid sinus tachycardia.
ANSWER
The correct interpretation is sinus tachycardia with a short PR interval. This ECG illustrates a physiologic sinus rate response to hypercarbic respiratory failure secondary to an infectious exacerbation. A shortened PR interval occurs with an otherwise healthy conduction system in response to a rapid sinus tachycardia.
ANSWER
The correct interpretation is sinus tachycardia with a short PR interval. This ECG illustrates a physiologic sinus rate response to hypercarbic respiratory failure secondary to an infectious exacerbation. A shortened PR interval occurs with an otherwise healthy conduction system in response to a rapid sinus tachycardia.
A 23-year-old woman with cystic fibrosis presents to the pulmonary medicine clinic for follow-up to a hospitalization one month ago for an infectious exacerbation of her condition. She has had four hospital admissions over the past year and is known to be chronically colonized with multidrug resistant Pseudomonas. Two days ago, she began feeling significantly more short of breath, with increasing home oxygen requirements (4 L at baseline, up to 10 L by nasal cannula), as well as increasing phlegm production and a fever of 100°F. She states she feels dehydrated, sleepy, and nauseous. In addition to cystic fibrosis, her medical history is remarkable for pancreatic insufficiency, diabetes, chronic sinus infections, and bronchiolitis obliterans syndrome. Family history is positive for hyperlipidemia and congestive heart failure. No other family members have a diagnosis of cystic fibrosis. Her medication list includes azithromycin, insulin glargine, insulin isophane, insulin lispro sliding scale, insulin regular, loratadine, omeprazole, pancrelipase, prednisone, simvastatin, sulfamethoxazole-trimethoprim, and a tobramycin inhaler. She is allergic to cephalosporin antibiotics. A quick review of systems reveals no other issues. Physical examination reveals a woman in extreme distress who is able to nod to questions and answer briefly but is unable to speak in full sentences. Her blood pressure is 136/82 mm Hg, with a mean arterial pressure of 99 mm Hg; pulse, 170 beats/min and thready; respiratory rate, 40 breaths/min-1; and temperature, 39.2°C. O2 saturation is 89% on 10 L of oxygen via facemask. The pulmonary exam reveals coarse bilateral crackles, worst at the bases, with associated intercostal and supraclavicular muscular retractions. The cardiac exam reveals no jugular venous distention. Her rate is rapid and regular with no murmurs, rubs, or gallops. The abdomen is soft and nontender, with normal bowel sounds. The extremities are warm, well perfused, and without edema. The neurologic exam is grossly normal without focal signs. A stat arterial blood gas reveals respiratory acidosis with a pH of 7.32 and a pCO2 of 83 mm Hg. A complete blood count reveals a white blood cell count of 34 x 109/L. You decide to admit her to the medical intensive care unit. You are concerned that her heart rate of 170 beats/min may be atrial flutter and obtain an ECG, which reveals the following: a ventricular rate of 177 beats/min; PR interval, 88 ms; QRS duration, 60 ms; QT/QTc interval, 238/408 ms; P axis, 67°; R axis, 76°; and T axis, 73°. What is your diagnosis?