User login
Single accreditation for MDs and DOs by 2020
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
Medical home pilot fails to reduce cost, utilization
In a 3-year pilot study, small- and medium-sized primary care practices that had created patient-centered medical homes were not successful in reducing costs or curbing hospital and emergency department visits.
The 32 Pennsylvania practices also had a limited effect on quality of care, improving nephropathy monitoring in diabetes patients, but showing no significant improvement on 10 other quality metrics.
The results come from the southeastern region of the Pennsylvania Chronic Care Initiative, a multipayer pilot study that provided technical assistance and financial incentives to internal medicine, family medicine, and pediatric practices, as well as some nurse-managed health centers that were seeking patient-centered medical home (PCMH) recognition from the National Committee on Quality Assurance (NCQA).
The findings were published Feb. 26 in JAMA (JAMA 2014;311:815-25).
Dr. Mark W. Friedberg, of the RAND Corporation in Boston, and his colleagues compared the performance of the 32 pilot practices to that of 29 similar practices in Pennsylvania. Each of the pilot sites achieved NCQA recognition as a PCMH by the third year of the study, with half achieving level 3 status. They earned performance bonuses averaging $92,000 per physician and were successful in making structural changes to their practices, including using patient registries and electronic prescribing.
But the pilot practices fell short in significantly improving quality, cost, and utilization compared with the practices that did not receive technical assistance and bonuses.
One reason that the pilot sites did not see improvements is that the bonus payments, which were tied to achieving NCQA recognition, might have distracted the practices from other activities that could have improved the quality and efficiency of care, Dr. Friedberg and his colleagues wrote. The pilot sites also had no direct incentives to contain costs, and they didn’t get any information on how their patients were utilizing care.
"Possibly as a consequence of these features of pilot design, we found that few pilot practices increased their night and weekend access capabilities, which could, in theory, have produced short-term savings by offering patients an alternative to more expensive sites of care (such as hospital emergency departments)," they added.
On the quality side, the researchers suggested that the pilot practices, which were all volunteers, may have been performing at a high level at the start, creating a "ceiling effect" that made it hard to achieve significant improvements over the 3-year study period.
The study was sponsored by the Commonwealth Fund and Aetna, which had no role in the study’s design or conduct. The investigators reported no relevant conflicts of interest.
On Twitter @maryellenny
The patient-centered medical home may turn out to be like some expensive biomedical technologies that help high-risk patients but not the broader population of patients, according to Dr. Thomas L. Schwenk.
"The PCMH has been promoted for widespread adoption, using a fairly generic and fixed set of structural practice features, even before being fully developed in targeted high-risk populations or before clearly understanding which features or combination of features are most effective with which patients," he wrote in an editorial accompanying Dr. Friedberg’s study.
"It is time to replace enthusiasm and promotion with scientific rigor and prudence and to better understand what the PCMH is and is not. Widespread implementation of the PCMH with limited data may lead to failure," he wrote (JAMA 2014;311:802-3).
Thomas L. Schwenk, M.D., is the dean of the University of Nevada School of Medicine in Reno. He reported no conflicts of interest.
The patient-centered medical home may turn out to be like some expensive biomedical technologies that help high-risk patients but not the broader population of patients, according to Dr. Thomas L. Schwenk.
"The PCMH has been promoted for widespread adoption, using a fairly generic and fixed set of structural practice features, even before being fully developed in targeted high-risk populations or before clearly understanding which features or combination of features are most effective with which patients," he wrote in an editorial accompanying Dr. Friedberg’s study.
"It is time to replace enthusiasm and promotion with scientific rigor and prudence and to better understand what the PCMH is and is not. Widespread implementation of the PCMH with limited data may lead to failure," he wrote (JAMA 2014;311:802-3).
Thomas L. Schwenk, M.D., is the dean of the University of Nevada School of Medicine in Reno. He reported no conflicts of interest.
The patient-centered medical home may turn out to be like some expensive biomedical technologies that help high-risk patients but not the broader population of patients, according to Dr. Thomas L. Schwenk.
"The PCMH has been promoted for widespread adoption, using a fairly generic and fixed set of structural practice features, even before being fully developed in targeted high-risk populations or before clearly understanding which features or combination of features are most effective with which patients," he wrote in an editorial accompanying Dr. Friedberg’s study.
"It is time to replace enthusiasm and promotion with scientific rigor and prudence and to better understand what the PCMH is and is not. Widespread implementation of the PCMH with limited data may lead to failure," he wrote (JAMA 2014;311:802-3).
Thomas L. Schwenk, M.D., is the dean of the University of Nevada School of Medicine in Reno. He reported no conflicts of interest.
In a 3-year pilot study, small- and medium-sized primary care practices that had created patient-centered medical homes were not successful in reducing costs or curbing hospital and emergency department visits.
The 32 Pennsylvania practices also had a limited effect on quality of care, improving nephropathy monitoring in diabetes patients, but showing no significant improvement on 10 other quality metrics.
The results come from the southeastern region of the Pennsylvania Chronic Care Initiative, a multipayer pilot study that provided technical assistance and financial incentives to internal medicine, family medicine, and pediatric practices, as well as some nurse-managed health centers that were seeking patient-centered medical home (PCMH) recognition from the National Committee on Quality Assurance (NCQA).
The findings were published Feb. 26 in JAMA (JAMA 2014;311:815-25).
Dr. Mark W. Friedberg, of the RAND Corporation in Boston, and his colleagues compared the performance of the 32 pilot practices to that of 29 similar practices in Pennsylvania. Each of the pilot sites achieved NCQA recognition as a PCMH by the third year of the study, with half achieving level 3 status. They earned performance bonuses averaging $92,000 per physician and were successful in making structural changes to their practices, including using patient registries and electronic prescribing.
But the pilot practices fell short in significantly improving quality, cost, and utilization compared with the practices that did not receive technical assistance and bonuses.
One reason that the pilot sites did not see improvements is that the bonus payments, which were tied to achieving NCQA recognition, might have distracted the practices from other activities that could have improved the quality and efficiency of care, Dr. Friedberg and his colleagues wrote. The pilot sites also had no direct incentives to contain costs, and they didn’t get any information on how their patients were utilizing care.
"Possibly as a consequence of these features of pilot design, we found that few pilot practices increased their night and weekend access capabilities, which could, in theory, have produced short-term savings by offering patients an alternative to more expensive sites of care (such as hospital emergency departments)," they added.
On the quality side, the researchers suggested that the pilot practices, which were all volunteers, may have been performing at a high level at the start, creating a "ceiling effect" that made it hard to achieve significant improvements over the 3-year study period.
The study was sponsored by the Commonwealth Fund and Aetna, which had no role in the study’s design or conduct. The investigators reported no relevant conflicts of interest.
On Twitter @maryellenny
In a 3-year pilot study, small- and medium-sized primary care practices that had created patient-centered medical homes were not successful in reducing costs or curbing hospital and emergency department visits.
The 32 Pennsylvania practices also had a limited effect on quality of care, improving nephropathy monitoring in diabetes patients, but showing no significant improvement on 10 other quality metrics.
The results come from the southeastern region of the Pennsylvania Chronic Care Initiative, a multipayer pilot study that provided technical assistance and financial incentives to internal medicine, family medicine, and pediatric practices, as well as some nurse-managed health centers that were seeking patient-centered medical home (PCMH) recognition from the National Committee on Quality Assurance (NCQA).
The findings were published Feb. 26 in JAMA (JAMA 2014;311:815-25).
Dr. Mark W. Friedberg, of the RAND Corporation in Boston, and his colleagues compared the performance of the 32 pilot practices to that of 29 similar practices in Pennsylvania. Each of the pilot sites achieved NCQA recognition as a PCMH by the third year of the study, with half achieving level 3 status. They earned performance bonuses averaging $92,000 per physician and were successful in making structural changes to their practices, including using patient registries and electronic prescribing.
But the pilot practices fell short in significantly improving quality, cost, and utilization compared with the practices that did not receive technical assistance and bonuses.
One reason that the pilot sites did not see improvements is that the bonus payments, which were tied to achieving NCQA recognition, might have distracted the practices from other activities that could have improved the quality and efficiency of care, Dr. Friedberg and his colleagues wrote. The pilot sites also had no direct incentives to contain costs, and they didn’t get any information on how their patients were utilizing care.
"Possibly as a consequence of these features of pilot design, we found that few pilot practices increased their night and weekend access capabilities, which could, in theory, have produced short-term savings by offering patients an alternative to more expensive sites of care (such as hospital emergency departments)," they added.
On the quality side, the researchers suggested that the pilot practices, which were all volunteers, may have been performing at a high level at the start, creating a "ceiling effect" that made it hard to achieve significant improvements over the 3-year study period.
The study was sponsored by the Commonwealth Fund and Aetna, which had no role in the study’s design or conduct. The investigators reported no relevant conflicts of interest.
On Twitter @maryellenny
FROM JAMA
Major finding: Primary care practices in the medical home pilot performed significantly better on only 1 of 11 measures.
Data source: Researchers analyzed claims data, survey responses, and performance on NCQA recognition by the 32 primary care practices in the medical home pilot. They compared their performance to that of 29 practices not in the study.
Disclosures: The study was sponsored by the Commonwealth Fund and Aetna. They had no role in the design or conduct of the study. The investigators reported no relevant conflicts of interest.
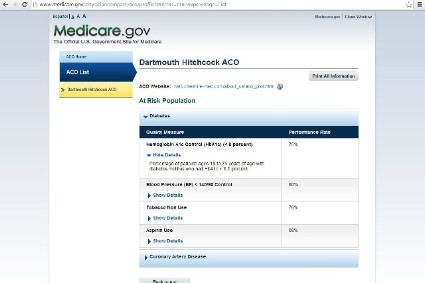
Physician Compare site adds quality scores
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
Physician Compare, Medicare’s online portal for checking on physician qualifications, has added quality scores for physicians in some group practices and Accountable Care Organizations.
The site now displays how a group of physicians has performed on five quality indicators related to management of diabetes and heart disease.
The website will display the ratings using stars, as well as the actual percentage score on the measure.
"This is an important first step in publicly reporting quality measures on Physician Compare," Dr. Patrick Conway, chief medical officer and deputy administrator for innovation and quality at the Centers for Medicare and Medicaid Services, said in a statement. "Offering a strong set of meaningful quality measures on the site will ultimately help consumers make decisions and it will encourage quality improvement among the clinician community, who shares CMS’s strong commitment to the best possible patient care."
The Physician Compare site, which was created under the Affordable Care Act, already displays the specialties offered by physicians, their board certification, and hospital affiliations. It also displays whether physicians participate in Medicare quality programs such as the Physician Quality Reporting System, the Electronic Prescribing Incentive Program, and the Electronic Health Records Incentive Program.
The information comes primarily from the Provider, Enrollment, Chain, and Ownership System (PECOS) and is checked against Medicare claims data. The site includes information on physicians enrolled in the Medicare program only.
This year, CMS is posting quality data from 66 group practices and 141 ACOs. The data is reported at the group practice and ACO level.
The quality measures include:
• Controlling hemoglobin A1c in patients with diabetes.
• Controlling blood pressure in patients with diabetes.
• Prescribing aspirin to patients with diabetes and heart disease.
• Reporting the number of diabetic patients who do not use tobacco.
• Prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
On Twitter @maryellenny
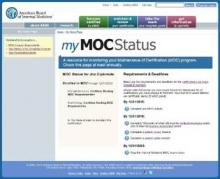
ABIM tightens MOC time frames, reveals docs’ progress
The American Board of Internal Medicine is shortening the time physicians have to earn Maintenance of Certification points, and the board on April 1 will begin publishing online whether physicians are currently meeting requirements for Maintenance of Certification.
The disclosures will appear on ABIM’s website as either "Meeting Maintenance of Certification Requirements: Yes" or "Meeting Maintenance of Certification Requirements: No." Officials at ABIM will update the one-line disclosure based on whether its diplomates have met the requirements for continuous participation in MOC.
Nearly all of the 24 medical specialty boards are already taking similar steps, with every board slated to publish compliance with MOC by the end of 2014, according to the American Board of Medical Specialties.
ABIM is also moving up its MOC program milestones. Every 2 years, physicians who are certified by ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date with MOC. Previously, physicians were given 10 years to earn 100 points.
The schedule for the exam remains the same.
Physicians whose certifications expire this year need to earn 100 points and pass an MOC exam by the end of 2014 to maintain their certification. They will remain certified as long as they continue to meet MOC requirements.
Physicians whose certifications expire in 2015 and beyond must enroll in MOC by April 1 to be considered meeting MOC requirements. They have until Dec. 31, 2015, to earn MOC points to meet the 2-year requirement.
To simplify record-keeping for physicians, ABIM set up an online portal that allows physicians to check their status and find out their next step in MOC.
The new requirements affect all physicians who are certified by ABIM, including those with lifetime certifications, known as "grandfathers." Though those physicians who were certified by ABIM before 1990 can’t lose their certification, they will be marked as not meeting MOC requirements online if they don’t earn the required number of points.
Publishing information about whether grandfathers are participating in MOC is critical, explained Dr. Richard J. Baron, president and CEO of ABIM, because otherwise the board is reporting on decades-old information.
"We’re saying this person is certified, but all we know is something that happened 24 years ago," he said. "We wanted to create a pathway where grandfathers could say they are doing stuff, too. And lots of them are."
Dr. Baron insisted that the board is not breaking its promise to grandfathers by publishing their MOC status. Participation in MOC is voluntary, and they will never lose their certification by opting out, he said.
But not all physicians are happy about the MOC requirements.
Dr. Ron Benbassat, a board-certified internist in Los Angeles, has mounted an effort called Change Board Recertification to roll back the MOC process. The group, which has attracted thousands of physician members from various subspecialties and states, aims to significantly scale back the MOC.
The group wants all time-limited certificates to be converted back to lifetime certification. That’s the only way that MOC can truly be voluntary, Dr. Benbassat said.
"As long as MOC is being tied to hospital privileges, insurance participation, and reimbursement, and the boards continue to pursue linking MOC to state licensure, then it’s clearly no longer voluntary," he said.
The current MOC process is burdensome in terms of both time and money, Dr. Benbassat said, and only serves to enrich ABIM, not produce better doctors.
"The new rules are really no different from what they were before. They completely disregard the cost, the time, and the administrative burdens for completing them. And now it’s also impacting ‘grandfathered’ physicians, as their lifetime certificate status is in jeopardy as well," Dr. Benbassat said. "This is a money grab."
Dr. Ken Lee, an internist in Olympia, Wash., who is also involved with the group, said he thinks that MOC is a burden and doesn’t know any frontline physicians who have found the process useful.
"It doesn’t really help us in daily practice. I can’t really say that I’m using anything now that I learned from those exams," Dr. Lee said. "What they test you on is usually trivia."
ABIM acknowledges that their MOC offerings could be better.
"We can increase the quotient of meaningful, high-value work to busy work," Dr. Baron said. "That’s another thing that we hear a lot about, and we hear that loud and clear."
In addition to fine-tuning their educational products, ABIM is inviting more community physicians to be part of their process and become members of their boards and committees. "It really matters who is in the room," Dr. Baron said. "We’re now committed to having people in community practice in all the rooms."
But ABIM has no intention of rolling back the new continuous certification process, which it views as essential to ensuring for the public, hospitals, and payers that physicians are not falling behind on their medical knowledge and skills.
Dr. Baron said the previous process allowed physicians to cram all of their work into the final 2 years of the 10-year cycle and didn’t guarantee that they were sharpening their skills along the way.
"We knew that it wasn’t functioning as a continuous program, and we also knew that we were basically issuing a certificate and saying it lasts for 10 years," Dr. Baron said. "Our board was uncomfortable with both those things."
While the new process has more requirements and tight time frames, Dr. Baron said the board has worked to make sure that MOC work can also count toward other physician requirements, including CME credit, Medicare’s Physician Quality Reporting System, and Bridges to Excellence. Physicians also may be able to earn rewards or recognition from some health plans, he noted.
[email protected] On Twitter @maryellenny
The American Board of Internal Medicine is shortening the time physicians have to earn Maintenance of Certification points, and the board on April 1 will begin publishing online whether physicians are currently meeting requirements for Maintenance of Certification.
The disclosures will appear on ABIM’s website as either "Meeting Maintenance of Certification Requirements: Yes" or "Meeting Maintenance of Certification Requirements: No." Officials at ABIM will update the one-line disclosure based on whether its diplomates have met the requirements for continuous participation in MOC.
Nearly all of the 24 medical specialty boards are already taking similar steps, with every board slated to publish compliance with MOC by the end of 2014, according to the American Board of Medical Specialties.
ABIM is also moving up its MOC program milestones. Every 2 years, physicians who are certified by ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date with MOC. Previously, physicians were given 10 years to earn 100 points.
The schedule for the exam remains the same.
Physicians whose certifications expire this year need to earn 100 points and pass an MOC exam by the end of 2014 to maintain their certification. They will remain certified as long as they continue to meet MOC requirements.
Physicians whose certifications expire in 2015 and beyond must enroll in MOC by April 1 to be considered meeting MOC requirements. They have until Dec. 31, 2015, to earn MOC points to meet the 2-year requirement.
To simplify record-keeping for physicians, ABIM set up an online portal that allows physicians to check their status and find out their next step in MOC.
The new requirements affect all physicians who are certified by ABIM, including those with lifetime certifications, known as "grandfathers." Though those physicians who were certified by ABIM before 1990 can’t lose their certification, they will be marked as not meeting MOC requirements online if they don’t earn the required number of points.
Publishing information about whether grandfathers are participating in MOC is critical, explained Dr. Richard J. Baron, president and CEO of ABIM, because otherwise the board is reporting on decades-old information.
"We’re saying this person is certified, but all we know is something that happened 24 years ago," he said. "We wanted to create a pathway where grandfathers could say they are doing stuff, too. And lots of them are."
Dr. Baron insisted that the board is not breaking its promise to grandfathers by publishing their MOC status. Participation in MOC is voluntary, and they will never lose their certification by opting out, he said.
But not all physicians are happy about the MOC requirements.
Dr. Ron Benbassat, a board-certified internist in Los Angeles, has mounted an effort called Change Board Recertification to roll back the MOC process. The group, which has attracted thousands of physician members from various subspecialties and states, aims to significantly scale back the MOC.
The group wants all time-limited certificates to be converted back to lifetime certification. That’s the only way that MOC can truly be voluntary, Dr. Benbassat said.
"As long as MOC is being tied to hospital privileges, insurance participation, and reimbursement, and the boards continue to pursue linking MOC to state licensure, then it’s clearly no longer voluntary," he said.
The current MOC process is burdensome in terms of both time and money, Dr. Benbassat said, and only serves to enrich ABIM, not produce better doctors.
"The new rules are really no different from what they were before. They completely disregard the cost, the time, and the administrative burdens for completing them. And now it’s also impacting ‘grandfathered’ physicians, as their lifetime certificate status is in jeopardy as well," Dr. Benbassat said. "This is a money grab."
Dr. Ken Lee, an internist in Olympia, Wash., who is also involved with the group, said he thinks that MOC is a burden and doesn’t know any frontline physicians who have found the process useful.
"It doesn’t really help us in daily practice. I can’t really say that I’m using anything now that I learned from those exams," Dr. Lee said. "What they test you on is usually trivia."
ABIM acknowledges that their MOC offerings could be better.
"We can increase the quotient of meaningful, high-value work to busy work," Dr. Baron said. "That’s another thing that we hear a lot about, and we hear that loud and clear."
In addition to fine-tuning their educational products, ABIM is inviting more community physicians to be part of their process and become members of their boards and committees. "It really matters who is in the room," Dr. Baron said. "We’re now committed to having people in community practice in all the rooms."
But ABIM has no intention of rolling back the new continuous certification process, which it views as essential to ensuring for the public, hospitals, and payers that physicians are not falling behind on their medical knowledge and skills.
Dr. Baron said the previous process allowed physicians to cram all of their work into the final 2 years of the 10-year cycle and didn’t guarantee that they were sharpening their skills along the way.
"We knew that it wasn’t functioning as a continuous program, and we also knew that we were basically issuing a certificate and saying it lasts for 10 years," Dr. Baron said. "Our board was uncomfortable with both those things."
While the new process has more requirements and tight time frames, Dr. Baron said the board has worked to make sure that MOC work can also count toward other physician requirements, including CME credit, Medicare’s Physician Quality Reporting System, and Bridges to Excellence. Physicians also may be able to earn rewards or recognition from some health plans, he noted.
[email protected] On Twitter @maryellenny
The American Board of Internal Medicine is shortening the time physicians have to earn Maintenance of Certification points, and the board on April 1 will begin publishing online whether physicians are currently meeting requirements for Maintenance of Certification.
The disclosures will appear on ABIM’s website as either "Meeting Maintenance of Certification Requirements: Yes" or "Meeting Maintenance of Certification Requirements: No." Officials at ABIM will update the one-line disclosure based on whether its diplomates have met the requirements for continuous participation in MOC.
Nearly all of the 24 medical specialty boards are already taking similar steps, with every board slated to publish compliance with MOC by the end of 2014, according to the American Board of Medical Specialties.
ABIM is also moving up its MOC program milestones. Every 2 years, physicians who are certified by ABIM must earn at least some points by completing some of the educational activities approved for MOC credit. At the 5-year mark, they must earn 100 points, as well as complete patient safety and patient survey activities, to be considered up to date with MOC. Previously, physicians were given 10 years to earn 100 points.
The schedule for the exam remains the same.
Physicians whose certifications expire this year need to earn 100 points and pass an MOC exam by the end of 2014 to maintain their certification. They will remain certified as long as they continue to meet MOC requirements.
Physicians whose certifications expire in 2015 and beyond must enroll in MOC by April 1 to be considered meeting MOC requirements. They have until Dec. 31, 2015, to earn MOC points to meet the 2-year requirement.
To simplify record-keeping for physicians, ABIM set up an online portal that allows physicians to check their status and find out their next step in MOC.
The new requirements affect all physicians who are certified by ABIM, including those with lifetime certifications, known as "grandfathers." Though those physicians who were certified by ABIM before 1990 can’t lose their certification, they will be marked as not meeting MOC requirements online if they don’t earn the required number of points.
Publishing information about whether grandfathers are participating in MOC is critical, explained Dr. Richard J. Baron, president and CEO of ABIM, because otherwise the board is reporting on decades-old information.
"We’re saying this person is certified, but all we know is something that happened 24 years ago," he said. "We wanted to create a pathway where grandfathers could say they are doing stuff, too. And lots of them are."
Dr. Baron insisted that the board is not breaking its promise to grandfathers by publishing their MOC status. Participation in MOC is voluntary, and they will never lose their certification by opting out, he said.
But not all physicians are happy about the MOC requirements.
Dr. Ron Benbassat, a board-certified internist in Los Angeles, has mounted an effort called Change Board Recertification to roll back the MOC process. The group, which has attracted thousands of physician members from various subspecialties and states, aims to significantly scale back the MOC.
The group wants all time-limited certificates to be converted back to lifetime certification. That’s the only way that MOC can truly be voluntary, Dr. Benbassat said.
"As long as MOC is being tied to hospital privileges, insurance participation, and reimbursement, and the boards continue to pursue linking MOC to state licensure, then it’s clearly no longer voluntary," he said.
The current MOC process is burdensome in terms of both time and money, Dr. Benbassat said, and only serves to enrich ABIM, not produce better doctors.
"The new rules are really no different from what they were before. They completely disregard the cost, the time, and the administrative burdens for completing them. And now it’s also impacting ‘grandfathered’ physicians, as their lifetime certificate status is in jeopardy as well," Dr. Benbassat said. "This is a money grab."
Dr. Ken Lee, an internist in Olympia, Wash., who is also involved with the group, said he thinks that MOC is a burden and doesn’t know any frontline physicians who have found the process useful.
"It doesn’t really help us in daily practice. I can’t really say that I’m using anything now that I learned from those exams," Dr. Lee said. "What they test you on is usually trivia."
ABIM acknowledges that their MOC offerings could be better.
"We can increase the quotient of meaningful, high-value work to busy work," Dr. Baron said. "That’s another thing that we hear a lot about, and we hear that loud and clear."
In addition to fine-tuning their educational products, ABIM is inviting more community physicians to be part of their process and become members of their boards and committees. "It really matters who is in the room," Dr. Baron said. "We’re now committed to having people in community practice in all the rooms."
But ABIM has no intention of rolling back the new continuous certification process, which it views as essential to ensuring for the public, hospitals, and payers that physicians are not falling behind on their medical knowledge and skills.
Dr. Baron said the previous process allowed physicians to cram all of their work into the final 2 years of the 10-year cycle and didn’t guarantee that they were sharpening their skills along the way.
"We knew that it wasn’t functioning as a continuous program, and we also knew that we were basically issuing a certificate and saying it lasts for 10 years," Dr. Baron said. "Our board was uncomfortable with both those things."
While the new process has more requirements and tight time frames, Dr. Baron said the board has worked to make sure that MOC work can also count toward other physician requirements, including CME credit, Medicare’s Physician Quality Reporting System, and Bridges to Excellence. Physicians also may be able to earn rewards or recognition from some health plans, he noted.
[email protected] On Twitter @maryellenny
Enrollment in ACA plans exceeds 3 million
More than 3 million Americans signed up for insurance through the Affordable Care Act’s state and federal marketplaces as of Feb. 1, according to the latest official enrollment figures from the Health & Human Services department.
Of the approximately 3.3 million individuals who have enrolled since the online marketplaces launched on Oct. 1, 2013, 1.1 million enrolled in the month of January alone.
Federal officials said the enrollment trends to date are encouraging, especially the interest from young adults, the group most sought after by health insurers.
Overall, about 25% of the 3.3 million enrollees are young adults between the ages of 18 and 34 years. Enrollment from that group grew the fastest of all ages in January, according to the Health & Human Services department.
"The covered population is getting younger," HHS Secretary Kathleen Sebelius said during a Feb. 12 press briefing.
While federal officials cheered the enrollment by younger Americans, they declined to set a goal for how many young adults they want to enroll by the time the Affordable Care Act’s open enrollment closes on March 31.
More women continue to enroll in the marketplaces than men – 55% vs. 45% as of Feb. 1; similar trends were seen in the first 3 months of open enrollment.
Silver plans continue to the most popular types of health plans in the state and federal marketplaces, with 62% of enrollees choosing them. Bronze plans, selected by 19%, were the second most popular choice. Only 1% of enrollees selected catastrophic plans; most of those were young adults, according to HHS.
Most individuals who enrolled in private health plans through the marketplaces also qualified for federal subsidies. Through the first 4 months of enrollment, 82% of people who selected health plans also received financial assistance for their premium, according to the HHS data.
On Twitter @maryellenny
More than 3 million Americans signed up for insurance through the Affordable Care Act’s state and federal marketplaces as of Feb. 1, according to the latest official enrollment figures from the Health & Human Services department.
Of the approximately 3.3 million individuals who have enrolled since the online marketplaces launched on Oct. 1, 2013, 1.1 million enrolled in the month of January alone.
Federal officials said the enrollment trends to date are encouraging, especially the interest from young adults, the group most sought after by health insurers.
Overall, about 25% of the 3.3 million enrollees are young adults between the ages of 18 and 34 years. Enrollment from that group grew the fastest of all ages in January, according to the Health & Human Services department.
"The covered population is getting younger," HHS Secretary Kathleen Sebelius said during a Feb. 12 press briefing.
While federal officials cheered the enrollment by younger Americans, they declined to set a goal for how many young adults they want to enroll by the time the Affordable Care Act’s open enrollment closes on March 31.
More women continue to enroll in the marketplaces than men – 55% vs. 45% as of Feb. 1; similar trends were seen in the first 3 months of open enrollment.
Silver plans continue to the most popular types of health plans in the state and federal marketplaces, with 62% of enrollees choosing them. Bronze plans, selected by 19%, were the second most popular choice. Only 1% of enrollees selected catastrophic plans; most of those were young adults, according to HHS.
Most individuals who enrolled in private health plans through the marketplaces also qualified for federal subsidies. Through the first 4 months of enrollment, 82% of people who selected health plans also received financial assistance for their premium, according to the HHS data.
On Twitter @maryellenny
More than 3 million Americans signed up for insurance through the Affordable Care Act’s state and federal marketplaces as of Feb. 1, according to the latest official enrollment figures from the Health & Human Services department.
Of the approximately 3.3 million individuals who have enrolled since the online marketplaces launched on Oct. 1, 2013, 1.1 million enrolled in the month of January alone.
Federal officials said the enrollment trends to date are encouraging, especially the interest from young adults, the group most sought after by health insurers.
Overall, about 25% of the 3.3 million enrollees are young adults between the ages of 18 and 34 years. Enrollment from that group grew the fastest of all ages in January, according to the Health & Human Services department.
"The covered population is getting younger," HHS Secretary Kathleen Sebelius said during a Feb. 12 press briefing.
While federal officials cheered the enrollment by younger Americans, they declined to set a goal for how many young adults they want to enroll by the time the Affordable Care Act’s open enrollment closes on March 31.
More women continue to enroll in the marketplaces than men – 55% vs. 45% as of Feb. 1; similar trends were seen in the first 3 months of open enrollment.
Silver plans continue to the most popular types of health plans in the state and federal marketplaces, with 62% of enrollees choosing them. Bronze plans, selected by 19%, were the second most popular choice. Only 1% of enrollees selected catastrophic plans; most of those were young adults, according to HHS.
Most individuals who enrolled in private health plans through the marketplaces also qualified for federal subsidies. Through the first 4 months of enrollment, 82% of people who selected health plans also received financial assistance for their premium, according to the HHS data.
On Twitter @maryellenny
ICD-10 price tag going up for doctors
Making the switch from the ICD-9 to the ICD-10 diagnosis code set could cost as much as $225,000 for some small practices and up to $8 million in some large practices, according to a study from the American Medical Association.
Physician offices and hospitals must use the ICD-10 code sets beginning Oct. 1, but the preparation for the switch is taking years and involves hours of staff training, the purchase of new hardware and software, and testing with vendors and payers.
A follow-up report prepared for the AMA by Nachimson Advisors found that in certain cases, implementation costs are nearly three times higher than what the firm predicted in 2008.
In their original report, Nachimson Advisors estimated that it would cost more than $83,000 for a typical small practice (3 physicians, 2 administrative staff) to implement ICD-10, rising to $285,000 for a typical medium-size practice (10 physicians, 1 full-time coder, 6 administrative staff), and about $2.7 million for a typical large practice (100 physicians, 10 full-time coders, 64 administrative staff).
Now those costs are estimated to range from $56,000 to $226,000 for small practices and $213,000 to $824,000 for medium-size practices. And for large practices, implementing ICD-10 could cost anywhere from $2 million to $8 million.
About two-thirds of physician practices are expected to have costs in the upper range of those estimates, according to the AMA.
One reason for the increased cost is new requirements related to the adoption of electronic health records (EHRs). Nachimson Advisors also projects a larger potential for payment disruptions, estimating that 2%-6% of claims could be denied after the Oct. 1 implementation date.
"The markedly higher implementation costs for ICD-10 place a crushing burden on physicians, straining vital resources needed to invest in new health care delivery models and well-developed technology that promotes care coordination with real value to patients," Dr. Ardis Dee Hoven, AMA president, said in a statement. "Continuing to compel physicians to adopt this new coding structure threatens to disrupt innovations by diverting resources away from areas that are expected to help lower costs and improve the quality of care."
The AMA is calling on Health & Human Services secretary Kathleen Sebelius to reconsider ICD-10 implementation. But if the agency sticks to its plan, the AMA has requested several changes to mitigate some of the costs.
For example, the AMA recommends that Medicare provide a 2-year implementation period during which the agency would not be allowed to deny payments based on the specificity of the ICD-10 code provided. And the agency would provide feedback on coding to physicians during this time.
The AMA also is asking Medicare to simplify its claims requirements by adopting a policy that when the most specific ICD-10 code is used, no additional information or attachments will be required before paying the claim.
On Twitter @maryellenny
Making the switch from the ICD-9 to the ICD-10 diagnosis code set could cost as much as $225,000 for some small practices and up to $8 million in some large practices, according to a study from the American Medical Association.
Physician offices and hospitals must use the ICD-10 code sets beginning Oct. 1, but the preparation for the switch is taking years and involves hours of staff training, the purchase of new hardware and software, and testing with vendors and payers.
A follow-up report prepared for the AMA by Nachimson Advisors found that in certain cases, implementation costs are nearly three times higher than what the firm predicted in 2008.
In their original report, Nachimson Advisors estimated that it would cost more than $83,000 for a typical small practice (3 physicians, 2 administrative staff) to implement ICD-10, rising to $285,000 for a typical medium-size practice (10 physicians, 1 full-time coder, 6 administrative staff), and about $2.7 million for a typical large practice (100 physicians, 10 full-time coders, 64 administrative staff).
Now those costs are estimated to range from $56,000 to $226,000 for small practices and $213,000 to $824,000 for medium-size practices. And for large practices, implementing ICD-10 could cost anywhere from $2 million to $8 million.
About two-thirds of physician practices are expected to have costs in the upper range of those estimates, according to the AMA.
One reason for the increased cost is new requirements related to the adoption of electronic health records (EHRs). Nachimson Advisors also projects a larger potential for payment disruptions, estimating that 2%-6% of claims could be denied after the Oct. 1 implementation date.
"The markedly higher implementation costs for ICD-10 place a crushing burden on physicians, straining vital resources needed to invest in new health care delivery models and well-developed technology that promotes care coordination with real value to patients," Dr. Ardis Dee Hoven, AMA president, said in a statement. "Continuing to compel physicians to adopt this new coding structure threatens to disrupt innovations by diverting resources away from areas that are expected to help lower costs and improve the quality of care."
The AMA is calling on Health & Human Services secretary Kathleen Sebelius to reconsider ICD-10 implementation. But if the agency sticks to its plan, the AMA has requested several changes to mitigate some of the costs.
For example, the AMA recommends that Medicare provide a 2-year implementation period during which the agency would not be allowed to deny payments based on the specificity of the ICD-10 code provided. And the agency would provide feedback on coding to physicians during this time.
The AMA also is asking Medicare to simplify its claims requirements by adopting a policy that when the most specific ICD-10 code is used, no additional information or attachments will be required before paying the claim.
On Twitter @maryellenny
Making the switch from the ICD-9 to the ICD-10 diagnosis code set could cost as much as $225,000 for some small practices and up to $8 million in some large practices, according to a study from the American Medical Association.
Physician offices and hospitals must use the ICD-10 code sets beginning Oct. 1, but the preparation for the switch is taking years and involves hours of staff training, the purchase of new hardware and software, and testing with vendors and payers.
A follow-up report prepared for the AMA by Nachimson Advisors found that in certain cases, implementation costs are nearly three times higher than what the firm predicted in 2008.
In their original report, Nachimson Advisors estimated that it would cost more than $83,000 for a typical small practice (3 physicians, 2 administrative staff) to implement ICD-10, rising to $285,000 for a typical medium-size practice (10 physicians, 1 full-time coder, 6 administrative staff), and about $2.7 million for a typical large practice (100 physicians, 10 full-time coders, 64 administrative staff).
Now those costs are estimated to range from $56,000 to $226,000 for small practices and $213,000 to $824,000 for medium-size practices. And for large practices, implementing ICD-10 could cost anywhere from $2 million to $8 million.
About two-thirds of physician practices are expected to have costs in the upper range of those estimates, according to the AMA.
One reason for the increased cost is new requirements related to the adoption of electronic health records (EHRs). Nachimson Advisors also projects a larger potential for payment disruptions, estimating that 2%-6% of claims could be denied after the Oct. 1 implementation date.
"The markedly higher implementation costs for ICD-10 place a crushing burden on physicians, straining vital resources needed to invest in new health care delivery models and well-developed technology that promotes care coordination with real value to patients," Dr. Ardis Dee Hoven, AMA president, said in a statement. "Continuing to compel physicians to adopt this new coding structure threatens to disrupt innovations by diverting resources away from areas that are expected to help lower costs and improve the quality of care."
The AMA is calling on Health & Human Services secretary Kathleen Sebelius to reconsider ICD-10 implementation. But if the agency sticks to its plan, the AMA has requested several changes to mitigate some of the costs.
For example, the AMA recommends that Medicare provide a 2-year implementation period during which the agency would not be allowed to deny payments based on the specificity of the ICD-10 code provided. And the agency would provide feedback on coding to physicians during this time.
The AMA also is asking Medicare to simplify its claims requirements by adopting a policy that when the most specific ICD-10 code is used, no additional information or attachments will be required before paying the claim.
On Twitter @maryellenny
ACP urges monitoring of network adequacy, formularies
Federal and state governments need to do more to ensure patients’ access to physicians under the Affordable Care Act’s new health plans, according to a report from the American College of Physicians.
In its Annual Report on the State of the Nation’s Health Care, issued on Feb. 11, ACP officials said that, even though the Affordable Care Act sets a standard for the adequacy of provider networks, consumers are already complaining that networks are too narrow.
For instance, one California insurer included 204 San Diego–area primary care physicians in its ACA exchange plan network, but its network for employer-sponsored plans in the area is three times larger. In New Hampshire, a hospital was excluded from an exchange-plan contract negotiation despite having lower charges than its competitors and high grades for quality of care, according to the ACP report.
On Feb. 4, the Centers for Medicare & Medicaid Services (CMS) sent a letter to insurers outlining its plans to ensure "reasonable access" to provider networks in 2015 by checking that consumers could access physicians without unreasonable delay. The CMS plans to look specifically at access to hospitals, mental health providers, oncologists, and primary care physicians.
The ACP said that the agency and state regulators should strengthen those requirements in several ways:
• Analyze local patient-to-physician ratios as well as current use of out-of-network clinicians and hospitals.
• Publish network monitoring data.
• Require health plans to provide physicians and patients with advance notice of network changes and the opportunity to appeal.
• Provide real-time access to network directories.
• Allow physicians to apply to any health plan and have their application judged on objective, transparent criteria.
• Bar health plans from excluding clinicians because their practices include patients with expensive medical conditions.
• Provide an additional enrollment period if patients are given an outdated or incorrect network directory.
"The college is not advocating that health plans provide unfettered access to every physician, hospital, or medication. We recognize that some physicians and hospitals have higher and possibly unjustifiably higher utilization rates, poorer outcomes, and higher admission and readmission rates," said Robert Doherty, ACP’s senior vice president of governmental affairs and public policy.
"Rather, we are offering constructive and balanced safeguards that emphasize consideration of additional elements in addressing network adequacy, transparency in network selection criteria and physician performance measures, consumer access to real-time network directories, improvements in the health plan selections shopping experience, and exceptions to ensure continuity of care," he added.
The ACP wants Medicare Advantage plans to be subject to similar requirements.
The ACP also called on federal and state regulators to more closely monitor health plan formularies to ensure that they do not exclude medications to treat complex chronic conditions, including cancer, transplants, mental health conditions, HIV/AIDS, and hepatitis C.
"We call for a balanced, constructive, and transparent approach allowing patients to make informed choices, promoting continuity of care, and ensuring fairness and due process for clinicians and patients, including strengthened federal and state regulatory oversight of qualified health plans," said Dr. Molly Cooke, ACP president.
On Twitter @maryellenny
Federal and state governments need to do more to ensure patients’ access to physicians under the Affordable Care Act’s new health plans, according to a report from the American College of Physicians.
In its Annual Report on the State of the Nation’s Health Care, issued on Feb. 11, ACP officials said that, even though the Affordable Care Act sets a standard for the adequacy of provider networks, consumers are already complaining that networks are too narrow.
For instance, one California insurer included 204 San Diego–area primary care physicians in its ACA exchange plan network, but its network for employer-sponsored plans in the area is three times larger. In New Hampshire, a hospital was excluded from an exchange-plan contract negotiation despite having lower charges than its competitors and high grades for quality of care, according to the ACP report.
On Feb. 4, the Centers for Medicare & Medicaid Services (CMS) sent a letter to insurers outlining its plans to ensure "reasonable access" to provider networks in 2015 by checking that consumers could access physicians without unreasonable delay. The CMS plans to look specifically at access to hospitals, mental health providers, oncologists, and primary care physicians.
The ACP said that the agency and state regulators should strengthen those requirements in several ways:
• Analyze local patient-to-physician ratios as well as current use of out-of-network clinicians and hospitals.
• Publish network monitoring data.
• Require health plans to provide physicians and patients with advance notice of network changes and the opportunity to appeal.
• Provide real-time access to network directories.
• Allow physicians to apply to any health plan and have their application judged on objective, transparent criteria.
• Bar health plans from excluding clinicians because their practices include patients with expensive medical conditions.
• Provide an additional enrollment period if patients are given an outdated or incorrect network directory.
"The college is not advocating that health plans provide unfettered access to every physician, hospital, or medication. We recognize that some physicians and hospitals have higher and possibly unjustifiably higher utilization rates, poorer outcomes, and higher admission and readmission rates," said Robert Doherty, ACP’s senior vice president of governmental affairs and public policy.
"Rather, we are offering constructive and balanced safeguards that emphasize consideration of additional elements in addressing network adequacy, transparency in network selection criteria and physician performance measures, consumer access to real-time network directories, improvements in the health plan selections shopping experience, and exceptions to ensure continuity of care," he added.
The ACP wants Medicare Advantage plans to be subject to similar requirements.
The ACP also called on federal and state regulators to more closely monitor health plan formularies to ensure that they do not exclude medications to treat complex chronic conditions, including cancer, transplants, mental health conditions, HIV/AIDS, and hepatitis C.
"We call for a balanced, constructive, and transparent approach allowing patients to make informed choices, promoting continuity of care, and ensuring fairness and due process for clinicians and patients, including strengthened federal and state regulatory oversight of qualified health plans," said Dr. Molly Cooke, ACP president.
On Twitter @maryellenny
Federal and state governments need to do more to ensure patients’ access to physicians under the Affordable Care Act’s new health plans, according to a report from the American College of Physicians.
In its Annual Report on the State of the Nation’s Health Care, issued on Feb. 11, ACP officials said that, even though the Affordable Care Act sets a standard for the adequacy of provider networks, consumers are already complaining that networks are too narrow.
For instance, one California insurer included 204 San Diego–area primary care physicians in its ACA exchange plan network, but its network for employer-sponsored plans in the area is three times larger. In New Hampshire, a hospital was excluded from an exchange-plan contract negotiation despite having lower charges than its competitors and high grades for quality of care, according to the ACP report.
On Feb. 4, the Centers for Medicare & Medicaid Services (CMS) sent a letter to insurers outlining its plans to ensure "reasonable access" to provider networks in 2015 by checking that consumers could access physicians without unreasonable delay. The CMS plans to look specifically at access to hospitals, mental health providers, oncologists, and primary care physicians.
The ACP said that the agency and state regulators should strengthen those requirements in several ways:
• Analyze local patient-to-physician ratios as well as current use of out-of-network clinicians and hospitals.
• Publish network monitoring data.
• Require health plans to provide physicians and patients with advance notice of network changes and the opportunity to appeal.
• Provide real-time access to network directories.
• Allow physicians to apply to any health plan and have their application judged on objective, transparent criteria.
• Bar health plans from excluding clinicians because their practices include patients with expensive medical conditions.
• Provide an additional enrollment period if patients are given an outdated or incorrect network directory.
"The college is not advocating that health plans provide unfettered access to every physician, hospital, or medication. We recognize that some physicians and hospitals have higher and possibly unjustifiably higher utilization rates, poorer outcomes, and higher admission and readmission rates," said Robert Doherty, ACP’s senior vice president of governmental affairs and public policy.
"Rather, we are offering constructive and balanced safeguards that emphasize consideration of additional elements in addressing network adequacy, transparency in network selection criteria and physician performance measures, consumer access to real-time network directories, improvements in the health plan selections shopping experience, and exceptions to ensure continuity of care," he added.
The ACP wants Medicare Advantage plans to be subject to similar requirements.
The ACP also called on federal and state regulators to more closely monitor health plan formularies to ensure that they do not exclude medications to treat complex chronic conditions, including cancer, transplants, mental health conditions, HIV/AIDS, and hepatitis C.
"We call for a balanced, constructive, and transparent approach allowing patients to make informed choices, promoting continuity of care, and ensuring fairness and due process for clinicians and patients, including strengthened federal and state regulatory oversight of qualified health plans," said Dr. Molly Cooke, ACP president.
On Twitter @maryellenny
Feds spend $19 billion on EHR bonuses
The federal government has spent more than $19 billion over the last 3 years on bonuses to health care providers and hospitals to jump-start the use of electronic health records, according to figures released by the Centers for Medicare & Medicaid Services.
The money, which was paid out as part of the Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs, went to physicians and other health care providers, hospitals, and Medicare Advantage organizations starting in 2011. Under the program, physicians can earn up to $44,000 over 5 years through Medicare or $63,750 over 6 years through Medicaid.
Since its launch in 2011 through the end of last year, more than 268,000 physicians have received incentive payments through the Medicare or Medicaid programs. In total, physicians took home more than $5.5 billion in bonuses over the first 3 years of the program.
But hospitals earned even more. About 4,400 hospitals earned more than $12.2 billion in EHR incentive payments from 2011 through 2013.
The government cut its biggest checks in the first 2 years of the program. And by May 2013, more than half of all physicians and other eligible providers had received bonuses through the program, according to the CMS.
In 2013 alone, more than 28,000 physicians received incentive payments through Medicare or Medicaid totaling more than $421 million.
On Twitter @maryellenny
The federal government has spent more than $19 billion over the last 3 years on bonuses to health care providers and hospitals to jump-start the use of electronic health records, according to figures released by the Centers for Medicare & Medicaid Services.
The money, which was paid out as part of the Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs, went to physicians and other health care providers, hospitals, and Medicare Advantage organizations starting in 2011. Under the program, physicians can earn up to $44,000 over 5 years through Medicare or $63,750 over 6 years through Medicaid.
Since its launch in 2011 through the end of last year, more than 268,000 physicians have received incentive payments through the Medicare or Medicaid programs. In total, physicians took home more than $5.5 billion in bonuses over the first 3 years of the program.
But hospitals earned even more. About 4,400 hospitals earned more than $12.2 billion in EHR incentive payments from 2011 through 2013.
The government cut its biggest checks in the first 2 years of the program. And by May 2013, more than half of all physicians and other eligible providers had received bonuses through the program, according to the CMS.
In 2013 alone, more than 28,000 physicians received incentive payments through Medicare or Medicaid totaling more than $421 million.
On Twitter @maryellenny
The federal government has spent more than $19 billion over the last 3 years on bonuses to health care providers and hospitals to jump-start the use of electronic health records, according to figures released by the Centers for Medicare & Medicaid Services.
The money, which was paid out as part of the Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs, went to physicians and other health care providers, hospitals, and Medicare Advantage organizations starting in 2011. Under the program, physicians can earn up to $44,000 over 5 years through Medicare or $63,750 over 6 years through Medicaid.
Since its launch in 2011 through the end of last year, more than 268,000 physicians have received incentive payments through the Medicare or Medicaid programs. In total, physicians took home more than $5.5 billion in bonuses over the first 3 years of the program.
But hospitals earned even more. About 4,400 hospitals earned more than $12.2 billion in EHR incentive payments from 2011 through 2013.
The government cut its biggest checks in the first 2 years of the program. And by May 2013, more than half of all physicians and other eligible providers had received bonuses through the program, according to the CMS.
In 2013 alone, more than 28,000 physicians received incentive payments through Medicare or Medicaid totaling more than $421 million.
On Twitter @maryellenny
Gov’t. delays ACA employer mandate for some
Businesses with fewer than 100 employees will have until 2016 to offer their workers health insurance or face penalties, according to a regulation released by the Internal Revenue Service.
The Affordable Care Act’s employer mandate had already been delayed until 2015 for all businesses with 50 or more employees. Businesses with fewer than 50 workers are exempt from providing health coverage under the ACA.
Under the new IRS regulation, released on Feb. 10, businesses with 50-99 workers have until 2016 before complying with the mandate, but they must report on their workers and coverage in 2015.
Larger businesses can phase in their health insurance offering starting in 2015. Under the rule, businesses with 100 or more workers must offer coverage to 70% of their full-time employees in 2015, and 95% of full-time workers in 2016.
On Twitter @maryellenny
Businesses with fewer than 100 employees will have until 2016 to offer their workers health insurance or face penalties, according to a regulation released by the Internal Revenue Service.
The Affordable Care Act’s employer mandate had already been delayed until 2015 for all businesses with 50 or more employees. Businesses with fewer than 50 workers are exempt from providing health coverage under the ACA.
Under the new IRS regulation, released on Feb. 10, businesses with 50-99 workers have until 2016 before complying with the mandate, but they must report on their workers and coverage in 2015.
Larger businesses can phase in their health insurance offering starting in 2015. Under the rule, businesses with 100 or more workers must offer coverage to 70% of their full-time employees in 2015, and 95% of full-time workers in 2016.
On Twitter @maryellenny
Businesses with fewer than 100 employees will have until 2016 to offer their workers health insurance or face penalties, according to a regulation released by the Internal Revenue Service.
The Affordable Care Act’s employer mandate had already been delayed until 2015 for all businesses with 50 or more employees. Businesses with fewer than 50 workers are exempt from providing health coverage under the ACA.
Under the new IRS regulation, released on Feb. 10, businesses with 50-99 workers have until 2016 before complying with the mandate, but they must report on their workers and coverage in 2015.
Larger businesses can phase in their health insurance offering starting in 2015. Under the rule, businesses with 100 or more workers must offer coverage to 70% of their full-time employees in 2015, and 95% of full-time workers in 2016.
On Twitter @maryellenny
AMA to Congress: No more SGR patches
The American Medical Association is urging Congress to work quickly to find a way to pay for a permanent repeal of Medicare’s Sustainable Growth Rate formula, before the current short-term patch expires on March 31.
During a press conference on Feb. 10, AMA President Ardis Dee Hoven put the organization’s full support behind the SGR Repeal and Medicare Provider Payment Modernization Act (H.R. 4015/S. 2000), which eliminates the Sustainable Growth Rate (SGR) formula and provides 0.5% physician payment increases for 5 years. The bill, which was introduced simultaneously in the House and Senate on Feb. 6, consolidates Medicare’s quality incentive programs and phases in new payment models.
But the AMA remains opposed to another short-term SGR fix, including a proposal that would avert physician pay cuts under Medicare for another 9 months.
"This whole concept of continued patching is fiscally irresponsible," Dr. Hoven said. "It undermines continually the stability of the program."
Without some type of SGR fix, either short-term or long-term, Medicare physician payments are set to drop about 24% on April 1.
But approving a permanent SGR repeal in the next several weeks hinges on whether lawmakers can agree on how to pay for it. The Congressional Budget Office estimates that the cost could run as high as $150 billion over 10 years.
Dr. Hoven said the AMA would not make recommendations on how to offset the cost of the bill, but they would offer an opinion once lawmakers put a specific proposal on the table.
"Right now, the momentum is there," Dr. Hoven said. "These conversations have been ongoing for years. They simply need to get this done and get it done now."
On Twitter @maryellenny
The American Medical Association is urging Congress to work quickly to find a way to pay for a permanent repeal of Medicare’s Sustainable Growth Rate formula, before the current short-term patch expires on March 31.
During a press conference on Feb. 10, AMA President Ardis Dee Hoven put the organization’s full support behind the SGR Repeal and Medicare Provider Payment Modernization Act (H.R. 4015/S. 2000), which eliminates the Sustainable Growth Rate (SGR) formula and provides 0.5% physician payment increases for 5 years. The bill, which was introduced simultaneously in the House and Senate on Feb. 6, consolidates Medicare’s quality incentive programs and phases in new payment models.
But the AMA remains opposed to another short-term SGR fix, including a proposal that would avert physician pay cuts under Medicare for another 9 months.
"This whole concept of continued patching is fiscally irresponsible," Dr. Hoven said. "It undermines continually the stability of the program."
Without some type of SGR fix, either short-term or long-term, Medicare physician payments are set to drop about 24% on April 1.
But approving a permanent SGR repeal in the next several weeks hinges on whether lawmakers can agree on how to pay for it. The Congressional Budget Office estimates that the cost could run as high as $150 billion over 10 years.
Dr. Hoven said the AMA would not make recommendations on how to offset the cost of the bill, but they would offer an opinion once lawmakers put a specific proposal on the table.
"Right now, the momentum is there," Dr. Hoven said. "These conversations have been ongoing for years. They simply need to get this done and get it done now."
On Twitter @maryellenny
The American Medical Association is urging Congress to work quickly to find a way to pay for a permanent repeal of Medicare’s Sustainable Growth Rate formula, before the current short-term patch expires on March 31.
During a press conference on Feb. 10, AMA President Ardis Dee Hoven put the organization’s full support behind the SGR Repeal and Medicare Provider Payment Modernization Act (H.R. 4015/S. 2000), which eliminates the Sustainable Growth Rate (SGR) formula and provides 0.5% physician payment increases for 5 years. The bill, which was introduced simultaneously in the House and Senate on Feb. 6, consolidates Medicare’s quality incentive programs and phases in new payment models.
But the AMA remains opposed to another short-term SGR fix, including a proposal that would avert physician pay cuts under Medicare for another 9 months.
"This whole concept of continued patching is fiscally irresponsible," Dr. Hoven said. "It undermines continually the stability of the program."
Without some type of SGR fix, either short-term or long-term, Medicare physician payments are set to drop about 24% on April 1.
But approving a permanent SGR repeal in the next several weeks hinges on whether lawmakers can agree on how to pay for it. The Congressional Budget Office estimates that the cost could run as high as $150 billion over 10 years.
Dr. Hoven said the AMA would not make recommendations on how to offset the cost of the bill, but they would offer an opinion once lawmakers put a specific proposal on the table.
"Right now, the momentum is there," Dr. Hoven said. "These conversations have been ongoing for years. They simply need to get this done and get it done now."
On Twitter @maryellenny