User login
Get ready for ICD-10 speed bumps
LAS VEGAS – When it comes to ICD-10 implementation, hospitalists aren’t in for the kind of hassles – or the crushing expenses – that office-based physicians face. But they can expect to spend more time selecting diagnosis codes and to get more questions from hospital coders and other providers, Dr. John Nelson said at the annual meeting of the Society of Hospital Medicine.
All physicians and hospitals begin using the new coding set starting on Oct. 1, 2014, according to the Centers for Medicare & Medicaid Services. And anyone who does not transition to the new system on that date will have their claims rejected.
Private payers, clearinghouses, and IT vendors are rushing to make the switch by Oct. 1.
*But there is a possibility that physicians will get some extra time to prepare for ICD-10. The House voted on March 27 to delay ICD-10 implementation for one year, pushing it back to Oct. 1, 2015. The bill (H.R. 4302) must make it through the Senate for the delay to take effect and it’s unclear if it can pass that chamber. The Senate is scheduled to vote on the issue on March 31.
Most hospitalists won’t need to lead this transition in their groups, but they do need to make sure that someone is making the transition happen, said Dr. Nelson, a hospitalist at Overlake Hospital in Bellevue, Wash., and a principal at Nelson Flores Hospital Medicine Consultants.
That means ensuring that charge capture and billing vendors are compliant, arranging testing for payers well in advance of the Oct. 1 deadline, and scheduling training and practice time for physicians, nurse practitioners, physician assistants, and billing personnel.
The major impact of the switch to ICD-10-CM (the version used by hospitalists and physicians who are not performing procedures) is a significant increase in the number of available codes. There were about 14,500 codes under the ICD-9-CM, but that will jump to more than 69,000 under ICD-10-CM, Dr. Nelson said.
While there are new diagnoses within the set, the bulk of the increase comes from adding greater specificity to the codes. For instance, there are now separate codes for specifying if a condition is "right" or "left" or if the visit is an "initial" or "subsequent" encounter.
"It’s not as bad as you think," Dr. Nelson said.
But some changes could be tricky for hospitalists. The new code set uses combination codes that allow physicians to classify two diagnoses together or a diagnosis with an associated secondary process or complication. For example, under ICD-9, physicians would use one code to denote a pressure ulcer on the ankle and another to indicate that it was stage 1. Under ICD-10, there’s a single code for pressure ulcer of unspecified ankle, stage 1.
All the new options mean it could take longer to choose codes correctly each time, Dr. Nelson predicted. And it’s also likely to mean more time will be spent responding to queries from hospital coders who are looking for more clinical documentation to support those codes.
The goal behind switching from the 30-year-old ICD-9 code set to a new system is to keep up with changes in medical practice and technology, as well as to gain more specific epidemiologic and population health data.
"Assuming we all choose these codes correctly, we will have a very useful data set," Dr. Nelson said.
Supporters of ICD-10 also say that it will cut down on rejected claims because it will provide more information from the start. Dr. Nelson said that he’s supportive of the switch to ICD-10, but is skeptical that it will cut down on the number of rejected claims. In fact, he thinks the opposite will be true, at least at the beginning.
So what can hospitalists do to prepare? If they haven’t heard from their hospital administrators about plans for the ICD-10 transition, it’s time to start asking questions, Dr. Nelson said.
It isn’t necessary for hospitalists to become ICD-10 experts, he said. Instead, lean on the hospital to provide support in the form of coding crosswalks between the two systems, cheat sheets, and even upgraded electronic health record software to aid in appropriate coding.
One potentially positive outcome of the switch is that it could make the process so complex that it will force hospitals to take diagnosis coding out to the hands of physicians.
"I think there’s a possibility that ICD-10 will go badly enough that others will swoop in and say ‘let us take care of that for you,’ " Dr. Nelson said. "That might ultimately be a very good thing for us."
On Twitter @maryellenny
*Updated 3/28/2014
LAS VEGAS – When it comes to ICD-10 implementation, hospitalists aren’t in for the kind of hassles – or the crushing expenses – that office-based physicians face. But they can expect to spend more time selecting diagnosis codes and to get more questions from hospital coders and other providers, Dr. John Nelson said at the annual meeting of the Society of Hospital Medicine.
All physicians and hospitals begin using the new coding set starting on Oct. 1, 2014, according to the Centers for Medicare & Medicaid Services. And anyone who does not transition to the new system on that date will have their claims rejected.
Private payers, clearinghouses, and IT vendors are rushing to make the switch by Oct. 1.
*But there is a possibility that physicians will get some extra time to prepare for ICD-10. The House voted on March 27 to delay ICD-10 implementation for one year, pushing it back to Oct. 1, 2015. The bill (H.R. 4302) must make it through the Senate for the delay to take effect and it’s unclear if it can pass that chamber. The Senate is scheduled to vote on the issue on March 31.
Most hospitalists won’t need to lead this transition in their groups, but they do need to make sure that someone is making the transition happen, said Dr. Nelson, a hospitalist at Overlake Hospital in Bellevue, Wash., and a principal at Nelson Flores Hospital Medicine Consultants.
That means ensuring that charge capture and billing vendors are compliant, arranging testing for payers well in advance of the Oct. 1 deadline, and scheduling training and practice time for physicians, nurse practitioners, physician assistants, and billing personnel.
The major impact of the switch to ICD-10-CM (the version used by hospitalists and physicians who are not performing procedures) is a significant increase in the number of available codes. There were about 14,500 codes under the ICD-9-CM, but that will jump to more than 69,000 under ICD-10-CM, Dr. Nelson said.
While there are new diagnoses within the set, the bulk of the increase comes from adding greater specificity to the codes. For instance, there are now separate codes for specifying if a condition is "right" or "left" or if the visit is an "initial" or "subsequent" encounter.
"It’s not as bad as you think," Dr. Nelson said.
But some changes could be tricky for hospitalists. The new code set uses combination codes that allow physicians to classify two diagnoses together or a diagnosis with an associated secondary process or complication. For example, under ICD-9, physicians would use one code to denote a pressure ulcer on the ankle and another to indicate that it was stage 1. Under ICD-10, there’s a single code for pressure ulcer of unspecified ankle, stage 1.
All the new options mean it could take longer to choose codes correctly each time, Dr. Nelson predicted. And it’s also likely to mean more time will be spent responding to queries from hospital coders who are looking for more clinical documentation to support those codes.
The goal behind switching from the 30-year-old ICD-9 code set to a new system is to keep up with changes in medical practice and technology, as well as to gain more specific epidemiologic and population health data.
"Assuming we all choose these codes correctly, we will have a very useful data set," Dr. Nelson said.
Supporters of ICD-10 also say that it will cut down on rejected claims because it will provide more information from the start. Dr. Nelson said that he’s supportive of the switch to ICD-10, but is skeptical that it will cut down on the number of rejected claims. In fact, he thinks the opposite will be true, at least at the beginning.
So what can hospitalists do to prepare? If they haven’t heard from their hospital administrators about plans for the ICD-10 transition, it’s time to start asking questions, Dr. Nelson said.
It isn’t necessary for hospitalists to become ICD-10 experts, he said. Instead, lean on the hospital to provide support in the form of coding crosswalks between the two systems, cheat sheets, and even upgraded electronic health record software to aid in appropriate coding.
One potentially positive outcome of the switch is that it could make the process so complex that it will force hospitals to take diagnosis coding out to the hands of physicians.
"I think there’s a possibility that ICD-10 will go badly enough that others will swoop in and say ‘let us take care of that for you,’ " Dr. Nelson said. "That might ultimately be a very good thing for us."
On Twitter @maryellenny
*Updated 3/28/2014
LAS VEGAS – When it comes to ICD-10 implementation, hospitalists aren’t in for the kind of hassles – or the crushing expenses – that office-based physicians face. But they can expect to spend more time selecting diagnosis codes and to get more questions from hospital coders and other providers, Dr. John Nelson said at the annual meeting of the Society of Hospital Medicine.
All physicians and hospitals begin using the new coding set starting on Oct. 1, 2014, according to the Centers for Medicare & Medicaid Services. And anyone who does not transition to the new system on that date will have their claims rejected.
Private payers, clearinghouses, and IT vendors are rushing to make the switch by Oct. 1.
*But there is a possibility that physicians will get some extra time to prepare for ICD-10. The House voted on March 27 to delay ICD-10 implementation for one year, pushing it back to Oct. 1, 2015. The bill (H.R. 4302) must make it through the Senate for the delay to take effect and it’s unclear if it can pass that chamber. The Senate is scheduled to vote on the issue on March 31.
Most hospitalists won’t need to lead this transition in their groups, but they do need to make sure that someone is making the transition happen, said Dr. Nelson, a hospitalist at Overlake Hospital in Bellevue, Wash., and a principal at Nelson Flores Hospital Medicine Consultants.
That means ensuring that charge capture and billing vendors are compliant, arranging testing for payers well in advance of the Oct. 1 deadline, and scheduling training and practice time for physicians, nurse practitioners, physician assistants, and billing personnel.
The major impact of the switch to ICD-10-CM (the version used by hospitalists and physicians who are not performing procedures) is a significant increase in the number of available codes. There were about 14,500 codes under the ICD-9-CM, but that will jump to more than 69,000 under ICD-10-CM, Dr. Nelson said.
While there are new diagnoses within the set, the bulk of the increase comes from adding greater specificity to the codes. For instance, there are now separate codes for specifying if a condition is "right" or "left" or if the visit is an "initial" or "subsequent" encounter.
"It’s not as bad as you think," Dr. Nelson said.
But some changes could be tricky for hospitalists. The new code set uses combination codes that allow physicians to classify two diagnoses together or a diagnosis with an associated secondary process or complication. For example, under ICD-9, physicians would use one code to denote a pressure ulcer on the ankle and another to indicate that it was stage 1. Under ICD-10, there’s a single code for pressure ulcer of unspecified ankle, stage 1.
All the new options mean it could take longer to choose codes correctly each time, Dr. Nelson predicted. And it’s also likely to mean more time will be spent responding to queries from hospital coders who are looking for more clinical documentation to support those codes.
The goal behind switching from the 30-year-old ICD-9 code set to a new system is to keep up with changes in medical practice and technology, as well as to gain more specific epidemiologic and population health data.
"Assuming we all choose these codes correctly, we will have a very useful data set," Dr. Nelson said.
Supporters of ICD-10 also say that it will cut down on rejected claims because it will provide more information from the start. Dr. Nelson said that he’s supportive of the switch to ICD-10, but is skeptical that it will cut down on the number of rejected claims. In fact, he thinks the opposite will be true, at least at the beginning.
So what can hospitalists do to prepare? If they haven’t heard from their hospital administrators about plans for the ICD-10 transition, it’s time to start asking questions, Dr. Nelson said.
It isn’t necessary for hospitalists to become ICD-10 experts, he said. Instead, lean on the hospital to provide support in the form of coding crosswalks between the two systems, cheat sheets, and even upgraded electronic health record software to aid in appropriate coding.
One potentially positive outcome of the switch is that it could make the process so complex that it will force hospitals to take diagnosis coding out to the hands of physicians.
"I think there’s a possibility that ICD-10 will go badly enough that others will swoop in and say ‘let us take care of that for you,’ " Dr. Nelson said. "That might ultimately be a very good thing for us."
On Twitter @maryellenny
*Updated 3/28/2014
EXPERT ANALYSIS FROM HOSPITAL MEDICINE 14
CMS preview: Hospital safety up, HAIs and readmissions down
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
LAS VEGAS – Hospital quality and safety are improving across the board, with readmissions and health care–acquired infections falling fast, according to the Centers for Medicare & Medicaid Services.
The official data will be released in April, but Dr. Patrick Conway, chief medical officer and director of the Center for Clinical Standards and Quality at CMS in Baltimore, told attendees at the annual meeting of the Society of Hospital Medicine that the preliminary numbers show "dramatic progress."
Over the last 2 years, U.S. hospitals have reduced harm for hospitalized patients by almost 10% nationally, saving 15,000 lives and more than $4 billion, he said. The estimate comes from chart reviews of all-cause patient harm measures such as central line–associated bloodstream infections, adverse drug events, pressure ulcers, catheter-associated urinary tract infections, and others.
Other quality improvements include:
• Central line–associated bloodstream infections down 40%.
• Surgical site infections down 22%.
• Early elective deliveries down more than 50%.
"You are improving so fast on quality process of care measures for CMS that we actually have to pull them out of the program," Dr. Conway told the audience of hospitalists. "We’ve removed almost half of the measures that were in hospital value-based purchasing in the inpatient quality reporting program over the last 3 years and that’s because the performance has increased so much."
Hospital readmissions – a measure that is getting increasing attention from hospitals now that CMS is tying it to payments – are also dropping. Medicare’s 30-day all-cause hospital readmission rate had been hovering around 19% or 20% nationally through 2011, but it has now dropped below 17.5%, Dr. Conway said.
"This is over 150,000 beneficiaries every year staying home and healthy," he said.
On Twitter @maryellenny
AT HOSPITAL MEDICINE 14
Feds pledge closer scrutiny of provider networks in 2015
Federal health officials will be taking a closer look at the scope of health plan provider networks next year as they decide which plans can be sold on the federally run insurance exchange.
The greater focus on health plan networks comes after reports that many of the plans being sold on the Affordable Care Act’s insurance exchanges have too-narrow networks that have limited access to primary care physicians, area hospitals, and even oncologists and cancer centers.
In a March 14 letter to health plans, officials at the Centers for Medicare and Medicaid Services said that all plans sold in 2015 on the exchange run by the federal government will have to meet a "reasonable access" standard, meaning that they must have a sufficient number and type of providers in their networks to ensure that patients have access to all services without unreasonable delay. The letter doesn’t spell out exactly how the agency plans to define "unreasonable delay."
CMS will focus on areas in which health plans historically have had network adequacy problems, including hospital systems, mental health providers, oncology providers, and primary care providers.
The agency also set a minimum threshold for including "essential community providers," those providers who traditionally treat low-income patients or work in physician shortage areas, such as federally qualified health centers. In 2015, plans must include in their networks at least 30% of available essential community providers in their service area.
CMS officials also plan to monitor network adequacy throughout the year, including tracking complaints.
The American Medical Association, which has raised concerns about the use of narrow networks in the ACA plans, applauded the increased oversight as a "first step."
"Inadequate health plan networks can endanger patients’ health if they cannot access timely, convenient, quality care with their existing physicians and other familiar providers," said Dr. Ardis Dee Hoven, AMA president.
But physicians may have to wait until next year to see if the government’s steps will correct the problem.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said he believes the intent of the CMS letter is to ensure robust provider networks, but there also appears to be some "wiggle room" for insurers. "Whether this letter moves that intent forward or not, we’ll probably have to wait and see," he said.
In a letter to CMS, the American College of Physicians urged additional requirements for insurers and more openness about how networks are designed.
Specifically, the ACP called on CMS to consider patient to physician ratios and the use of out-of-network providers when evaluating networks in addition to time and distance standards. The ACP also wants insurers to rely on performance measures that are based on national standards when assessing physicians for inclusion in their networks. The measures and methodology should also be transparent and understandable by physicians and patients alike, the group said.
The American Cancer Society Cancer Action Network is asking CMS to mandate a standardized exceptions process to allow patients to seek treatment from out-of-network physicians and hospitals when in-network providers are unavailable or too far away. And patients who qualify for the exemption should not have to pay higher out-of-network costs, said Laura Skopec, senior policy analyst for the American Cancer Society Cancer Action Network.
On Twitter @maryellenny
Federal health officials will be taking a closer look at the scope of health plan provider networks next year as they decide which plans can be sold on the federally run insurance exchange.
The greater focus on health plan networks comes after reports that many of the plans being sold on the Affordable Care Act’s insurance exchanges have too-narrow networks that have limited access to primary care physicians, area hospitals, and even oncologists and cancer centers.
In a March 14 letter to health plans, officials at the Centers for Medicare and Medicaid Services said that all plans sold in 2015 on the exchange run by the federal government will have to meet a "reasonable access" standard, meaning that they must have a sufficient number and type of providers in their networks to ensure that patients have access to all services without unreasonable delay. The letter doesn’t spell out exactly how the agency plans to define "unreasonable delay."
CMS will focus on areas in which health plans historically have had network adequacy problems, including hospital systems, mental health providers, oncology providers, and primary care providers.
The agency also set a minimum threshold for including "essential community providers," those providers who traditionally treat low-income patients or work in physician shortage areas, such as federally qualified health centers. In 2015, plans must include in their networks at least 30% of available essential community providers in their service area.
CMS officials also plan to monitor network adequacy throughout the year, including tracking complaints.
The American Medical Association, which has raised concerns about the use of narrow networks in the ACA plans, applauded the increased oversight as a "first step."
"Inadequate health plan networks can endanger patients’ health if they cannot access timely, convenient, quality care with their existing physicians and other familiar providers," said Dr. Ardis Dee Hoven, AMA president.
But physicians may have to wait until next year to see if the government’s steps will correct the problem.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said he believes the intent of the CMS letter is to ensure robust provider networks, but there also appears to be some "wiggle room" for insurers. "Whether this letter moves that intent forward or not, we’ll probably have to wait and see," he said.
In a letter to CMS, the American College of Physicians urged additional requirements for insurers and more openness about how networks are designed.
Specifically, the ACP called on CMS to consider patient to physician ratios and the use of out-of-network providers when evaluating networks in addition to time and distance standards. The ACP also wants insurers to rely on performance measures that are based on national standards when assessing physicians for inclusion in their networks. The measures and methodology should also be transparent and understandable by physicians and patients alike, the group said.
The American Cancer Society Cancer Action Network is asking CMS to mandate a standardized exceptions process to allow patients to seek treatment from out-of-network physicians and hospitals when in-network providers are unavailable or too far away. And patients who qualify for the exemption should not have to pay higher out-of-network costs, said Laura Skopec, senior policy analyst for the American Cancer Society Cancer Action Network.
On Twitter @maryellenny
Federal health officials will be taking a closer look at the scope of health plan provider networks next year as they decide which plans can be sold on the federally run insurance exchange.
The greater focus on health plan networks comes after reports that many of the plans being sold on the Affordable Care Act’s insurance exchanges have too-narrow networks that have limited access to primary care physicians, area hospitals, and even oncologists and cancer centers.
In a March 14 letter to health plans, officials at the Centers for Medicare and Medicaid Services said that all plans sold in 2015 on the exchange run by the federal government will have to meet a "reasonable access" standard, meaning that they must have a sufficient number and type of providers in their networks to ensure that patients have access to all services without unreasonable delay. The letter doesn’t spell out exactly how the agency plans to define "unreasonable delay."
CMS will focus on areas in which health plans historically have had network adequacy problems, including hospital systems, mental health providers, oncology providers, and primary care providers.
The agency also set a minimum threshold for including "essential community providers," those providers who traditionally treat low-income patients or work in physician shortage areas, such as federally qualified health centers. In 2015, plans must include in their networks at least 30% of available essential community providers in their service area.
CMS officials also plan to monitor network adequacy throughout the year, including tracking complaints.
The American Medical Association, which has raised concerns about the use of narrow networks in the ACA plans, applauded the increased oversight as a "first step."
"Inadequate health plan networks can endanger patients’ health if they cannot access timely, convenient, quality care with their existing physicians and other familiar providers," said Dr. Ardis Dee Hoven, AMA president.
But physicians may have to wait until next year to see if the government’s steps will correct the problem.
Dr. Reid Blackwelder, president of the American Academy of Family Physicians, said he believes the intent of the CMS letter is to ensure robust provider networks, but there also appears to be some "wiggle room" for insurers. "Whether this letter moves that intent forward or not, we’ll probably have to wait and see," he said.
In a letter to CMS, the American College of Physicians urged additional requirements for insurers and more openness about how networks are designed.
Specifically, the ACP called on CMS to consider patient to physician ratios and the use of out-of-network providers when evaluating networks in addition to time and distance standards. The ACP also wants insurers to rely on performance measures that are based on national standards when assessing physicians for inclusion in their networks. The measures and methodology should also be transparent and understandable by physicians and patients alike, the group said.
The American Cancer Society Cancer Action Network is asking CMS to mandate a standardized exceptions process to allow patients to seek treatment from out-of-network physicians and hospitals when in-network providers are unavailable or too far away. And patients who qualify for the exemption should not have to pay higher out-of-network costs, said Laura Skopec, senior policy analyst for the American Cancer Society Cancer Action Network.
On Twitter @maryellenny
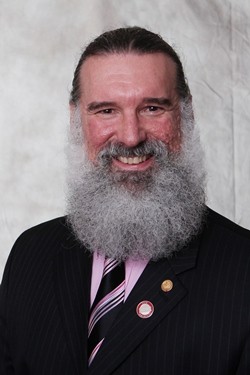
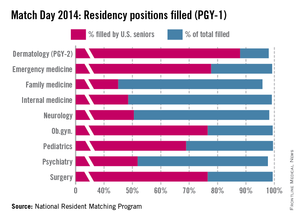
Primary care makes modest gains in 2014 resident match
Primary care specialties continue to gain interest from medical school seniors, according to the results of the 2014 Main Residency Match, but their interest probably isn’t great enough to keep pace with the growing physician workforce demands.
In another record-setting year, the Match offered 29,671 first- and second-year residency positions, up 500 from its previous high in 2013. More than half of the new positions were in internal medicine and family medicine, according to the National Resident Matching Program.
In internal medicine, 247 first-year residency positions were added to the Match. Family medicine offered 72 more spots, and pediatrics offered 24 more positions.
The extra positions added up to gains in the number of U.S. medical school graduates choosing residencies in internal medicine and family medicine. But fewer U.S. seniors matched to pediatrics in 2014 than in the previous year.
In internal medicine, 6,524 positions were offered this year. Of those, 99.1% were filled, with 48.5% taken by U.S. medical graduates.
In 2014, 3,109 family medicine residency positions were offered. Of those, 95.8% were filled, with 45% filled by U.S. medical graduates.
In pediatrics, 99.5% of the total 2,640 positions offered were filled. U.S. medical graduates filled 68.9% of the pediatric positions. Fewer (19) U.S. graduates filled pediatric positions, compared with 2013, reversing a trend of steady increases.
The take-home message from primary care leaders is that it was overall a very good year in the Match. But many more good years are needed to meet growing workforce demands stemming from the Affordable Care Act and the aging population.
"There has been growth in primary care," said Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians. "I’m just concerned that it’s not sufficient to meet the needs of the population as we go forward."
One reason for his concern is that even though more medical students are opting for internal medicine residencies, there’s no guarantee that they will become primary care physicians in the end. Only about 20% to 25% of these residents will stay in general internal medicine, while the rest will subspecialize, Dr. Alguire said.
Pediatrics faces the same situation, said Dr. Reid Blackwelder, president of the American Academy of Family Physicians, as many of the medical students choosing pediatrics on Match Day will end up subspecializing. So projecting the future workforce capacity based on the figures from the Match could lead to "overly optimistic" projections, he said.
"We’re definitely moving in the right direction," Dr. Blackwelder said. "But we really need to have an accelerated increase."
To meet the workforce needs, the AAFP estimates that family medicine residencies must add and fill 65 new positions each year through 2025. They exceeded that goal in 2014, but that trend will need to continue every year for a decade to have an effect, Dr. Blackwelder said.
One way to attract more medical students to primary care is to fix one of the critical issues for physicians in practice: declining payments. The AAFP is advocating for better pay for primary care physicians, by moving away from the current fee-for-service system, which rewards volume of services over quality and efficiency.
High student debt also continues to be a barrier to recruiting young primary care physicians, Dr. Alguire said.
"Any student with an eye to the future would have to be worried about how they’re going to pay the debt off and how quickly they can pay that debt off," he said. "And they may be beginning to wonder if the primary care field is really the answer economically."
Outside of primary care, surgical specialties continued to be popular in this year’s Match. The most competitive specialties in 2014 were neurological surgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. Each of those specialties offered at least 50 positions in the Match program and filled at least 90% of the positions with U.S. medical school seniors.
The top specialties are more competitive than ever, said Mona M. Signer, executive director of the National Resident Matching Program.
"If any applicant is applying to a very competitive specialty, they need to consider what their backup plan is," she said. "Not everyone can be an orthopedic surgeon."
One surprise in this year’s Match was that fewer U.S. seniors participated. There were 89 fewer U.S. seniors registered for the Match, and 113 fewer U.S. seniors submitted rank order lists of program, Ms. Signer said.
Although the marginal drop is likely an anomaly, Ms. Signer said she contacted several medical schools and found that in some cases they were adjusting for overenrollment in the prior year, had dual-degree students delaying graduation, or had students with academic issues.
None of the schools reported that they were reducing enrollment over the long term. "One year never makes a trend," she said.
On Twitter @maryellenny
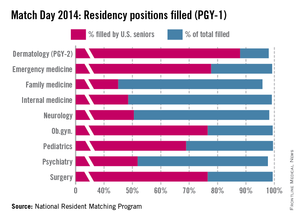
Primary care specialties continue to gain interest from medical school seniors, according to the results of the 2014 Main Residency Match, but their interest probably isn’t great enough to keep pace with the growing physician workforce demands.
In another record-setting year, the Match offered 29,671 first- and second-year residency positions, up 500 from its previous high in 2013. More than half of the new positions were in internal medicine and family medicine, according to the National Resident Matching Program.
In internal medicine, 247 first-year residency positions were added to the Match. Family medicine offered 72 more spots, and pediatrics offered 24 more positions.
The extra positions added up to gains in the number of U.S. medical school graduates choosing residencies in internal medicine and family medicine. But fewer U.S. seniors matched to pediatrics in 2014 than in the previous year.
In internal medicine, 6,524 positions were offered this year. Of those, 99.1% were filled, with 48.5% taken by U.S. medical graduates.
In 2014, 3,109 family medicine residency positions were offered. Of those, 95.8% were filled, with 45% filled by U.S. medical graduates.
In pediatrics, 99.5% of the total 2,640 positions offered were filled. U.S. medical graduates filled 68.9% of the pediatric positions. Fewer (19) U.S. graduates filled pediatric positions, compared with 2013, reversing a trend of steady increases.
The take-home message from primary care leaders is that it was overall a very good year in the Match. But many more good years are needed to meet growing workforce demands stemming from the Affordable Care Act and the aging population.
"There has been growth in primary care," said Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians. "I’m just concerned that it’s not sufficient to meet the needs of the population as we go forward."
One reason for his concern is that even though more medical students are opting for internal medicine residencies, there’s no guarantee that they will become primary care physicians in the end. Only about 20% to 25% of these residents will stay in general internal medicine, while the rest will subspecialize, Dr. Alguire said.
Pediatrics faces the same situation, said Dr. Reid Blackwelder, president of the American Academy of Family Physicians, as many of the medical students choosing pediatrics on Match Day will end up subspecializing. So projecting the future workforce capacity based on the figures from the Match could lead to "overly optimistic" projections, he said.
"We’re definitely moving in the right direction," Dr. Blackwelder said. "But we really need to have an accelerated increase."
To meet the workforce needs, the AAFP estimates that family medicine residencies must add and fill 65 new positions each year through 2025. They exceeded that goal in 2014, but that trend will need to continue every year for a decade to have an effect, Dr. Blackwelder said.
One way to attract more medical students to primary care is to fix one of the critical issues for physicians in practice: declining payments. The AAFP is advocating for better pay for primary care physicians, by moving away from the current fee-for-service system, which rewards volume of services over quality and efficiency.
High student debt also continues to be a barrier to recruiting young primary care physicians, Dr. Alguire said.
"Any student with an eye to the future would have to be worried about how they’re going to pay the debt off and how quickly they can pay that debt off," he said. "And they may be beginning to wonder if the primary care field is really the answer economically."
Outside of primary care, surgical specialties continued to be popular in this year’s Match. The most competitive specialties in 2014 were neurological surgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. Each of those specialties offered at least 50 positions in the Match program and filled at least 90% of the positions with U.S. medical school seniors.
The top specialties are more competitive than ever, said Mona M. Signer, executive director of the National Resident Matching Program.
"If any applicant is applying to a very competitive specialty, they need to consider what their backup plan is," she said. "Not everyone can be an orthopedic surgeon."
One surprise in this year’s Match was that fewer U.S. seniors participated. There were 89 fewer U.S. seniors registered for the Match, and 113 fewer U.S. seniors submitted rank order lists of program, Ms. Signer said.
Although the marginal drop is likely an anomaly, Ms. Signer said she contacted several medical schools and found that in some cases they were adjusting for overenrollment in the prior year, had dual-degree students delaying graduation, or had students with academic issues.
None of the schools reported that they were reducing enrollment over the long term. "One year never makes a trend," she said.
On Twitter @maryellenny
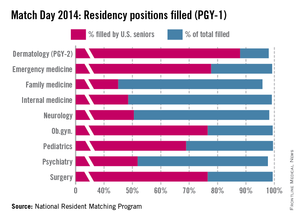
Primary care specialties continue to gain interest from medical school seniors, according to the results of the 2014 Main Residency Match, but their interest probably isn’t great enough to keep pace with the growing physician workforce demands.
In another record-setting year, the Match offered 29,671 first- and second-year residency positions, up 500 from its previous high in 2013. More than half of the new positions were in internal medicine and family medicine, according to the National Resident Matching Program.
In internal medicine, 247 first-year residency positions were added to the Match. Family medicine offered 72 more spots, and pediatrics offered 24 more positions.
The extra positions added up to gains in the number of U.S. medical school graduates choosing residencies in internal medicine and family medicine. But fewer U.S. seniors matched to pediatrics in 2014 than in the previous year.
In internal medicine, 6,524 positions were offered this year. Of those, 99.1% were filled, with 48.5% taken by U.S. medical graduates.
In 2014, 3,109 family medicine residency positions were offered. Of those, 95.8% were filled, with 45% filled by U.S. medical graduates.
In pediatrics, 99.5% of the total 2,640 positions offered were filled. U.S. medical graduates filled 68.9% of the pediatric positions. Fewer (19) U.S. graduates filled pediatric positions, compared with 2013, reversing a trend of steady increases.
The take-home message from primary care leaders is that it was overall a very good year in the Match. But many more good years are needed to meet growing workforce demands stemming from the Affordable Care Act and the aging population.
"There has been growth in primary care," said Dr. Patrick Alguire, senior vice president for medical education at the American College of Physicians. "I’m just concerned that it’s not sufficient to meet the needs of the population as we go forward."
One reason for his concern is that even though more medical students are opting for internal medicine residencies, there’s no guarantee that they will become primary care physicians in the end. Only about 20% to 25% of these residents will stay in general internal medicine, while the rest will subspecialize, Dr. Alguire said.
Pediatrics faces the same situation, said Dr. Reid Blackwelder, president of the American Academy of Family Physicians, as many of the medical students choosing pediatrics on Match Day will end up subspecializing. So projecting the future workforce capacity based on the figures from the Match could lead to "overly optimistic" projections, he said.
"We’re definitely moving in the right direction," Dr. Blackwelder said. "But we really need to have an accelerated increase."
To meet the workforce needs, the AAFP estimates that family medicine residencies must add and fill 65 new positions each year through 2025. They exceeded that goal in 2014, but that trend will need to continue every year for a decade to have an effect, Dr. Blackwelder said.
One way to attract more medical students to primary care is to fix one of the critical issues for physicians in practice: declining payments. The AAFP is advocating for better pay for primary care physicians, by moving away from the current fee-for-service system, which rewards volume of services over quality and efficiency.
High student debt also continues to be a barrier to recruiting young primary care physicians, Dr. Alguire said.
"Any student with an eye to the future would have to be worried about how they’re going to pay the debt off and how quickly they can pay that debt off," he said. "And they may be beginning to wonder if the primary care field is really the answer economically."
Outside of primary care, surgical specialties continued to be popular in this year’s Match. The most competitive specialties in 2014 were neurological surgery, orthopedic surgery, otolaryngology, plastic surgery, and radiation oncology. Each of those specialties offered at least 50 positions in the Match program and filled at least 90% of the positions with U.S. medical school seniors.
The top specialties are more competitive than ever, said Mona M. Signer, executive director of the National Resident Matching Program.
"If any applicant is applying to a very competitive specialty, they need to consider what their backup plan is," she said. "Not everyone can be an orthopedic surgeon."
One surprise in this year’s Match was that fewer U.S. seniors participated. There were 89 fewer U.S. seniors registered for the Match, and 113 fewer U.S. seniors submitted rank order lists of program, Ms. Signer said.
Although the marginal drop is likely an anomaly, Ms. Signer said she contacted several medical schools and found that in some cases they were adjusting for overenrollment in the prior year, had dual-degree students delaying graduation, or had students with academic issues.
None of the schools reported that they were reducing enrollment over the long term. "One year never makes a trend," she said.
On Twitter @maryellenny
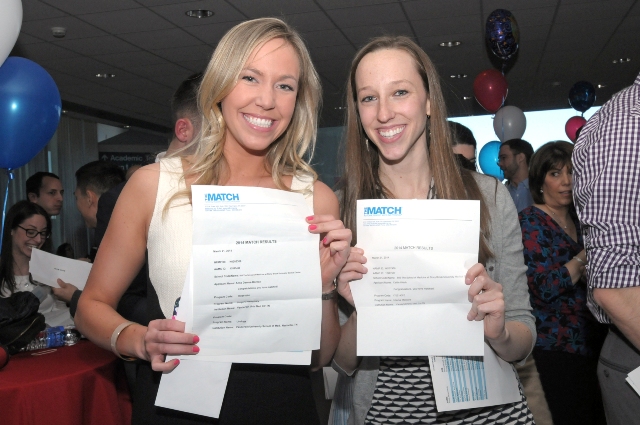
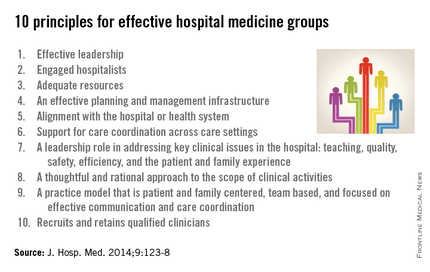
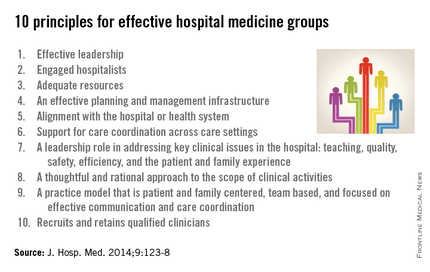
List defines path to an ideal hospital medicine practice
The Society of Hospital Medicine has come up with 10 "basic ingredients" for building and sustaining an effective hospital medicine group.
The list of guiding principles, which was published in the Journal of Hospital Medicine, is meant to help hospital medicine groups perform self-assessments and set goals for improvement, while also providing hospital executives with benchmarks for evaluating those groups. (J. Hosp. Med. 2014;9:123-8).
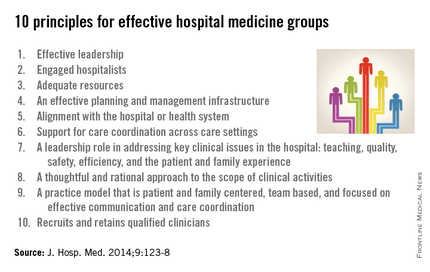
The 10 principles and 47 key characteristics of an effective hospital medicine group address everything from adequate staffing to the scope of clinical activities for the hospitalist.
The biggest challenge in creating the document was identifying characteristics that could apply to all types of hospital medicine groups, given the diversity in practice settings, employment models, and patient populations in hospital medicine, said Dr. John Nelson, a coauthor of the document and cofounder of the Society of Hospital Medicine (SHM).
But it won’t be a perfect fit for everyone, he said. "It’s a little bit like a roadmap for leading a good life," he said. "You put on exercise and eating well and things of that sort, but there are lots of people that have different circumstances."
In the document, the SHM workgroup suggested that the principles and characteristics could be used in variety of ways. For instance, they could be used as a framework for hospital medicine groups and hospital leaders to discuss ongoing issues. They could also be used more formally to guide planning and budget activities for the hospital medicine group. Or hospital leaders could use them to evaluate hospital medicine groups, by calling on them to address 80% of the 47 characteristics, for example.
Dr. Nelson, who is the medical director of the hospitalist medicine group at Overlake Hospital in Bellevue, Wash., and a practice management consultant, said the most important thing is that the list is not ignored.
Spend 20 minutes using the list to grade the group’s performance, he said, and then have other physicians do the same and compare the results.
"It’s a good exercise to think about how your practice is doing, compared with what a large group of people think might be the best way to approach things," Dr. Nelson said.
But the document’s authors admitted that there could be a downside to the publication of the principles. Hospital medicine groups could be held accountable for meeting these criteria without getting the necessary financial support from their hospitals.
"The idea is to encourage good performance," Dr. Nelson said. "No group is doing them all and to use this simply as a tool of punishment will not advance the cause much."
The list of principles and characteristics was created over 18 months by a workgroup of experts selected by the SHM board of directors. The document was also reviewed by focus groups of hospitalists and by health care experts outside of the field of hospital medicine.
On Twitter @maryellenny
The Society of Hospital Medicine has come up with 10 "basic ingredients" for building and sustaining an effective hospital medicine group.
The list of guiding principles, which was published in the Journal of Hospital Medicine, is meant to help hospital medicine groups perform self-assessments and set goals for improvement, while also providing hospital executives with benchmarks for evaluating those groups. (J. Hosp. Med. 2014;9:123-8).
The 10 principles and 47 key characteristics of an effective hospital medicine group address everything from adequate staffing to the scope of clinical activities for the hospitalist.
The biggest challenge in creating the document was identifying characteristics that could apply to all types of hospital medicine groups, given the diversity in practice settings, employment models, and patient populations in hospital medicine, said Dr. John Nelson, a coauthor of the document and cofounder of the Society of Hospital Medicine (SHM).
But it won’t be a perfect fit for everyone, he said. "It’s a little bit like a roadmap for leading a good life," he said. "You put on exercise and eating well and things of that sort, but there are lots of people that have different circumstances."
In the document, the SHM workgroup suggested that the principles and characteristics could be used in variety of ways. For instance, they could be used as a framework for hospital medicine groups and hospital leaders to discuss ongoing issues. They could also be used more formally to guide planning and budget activities for the hospital medicine group. Or hospital leaders could use them to evaluate hospital medicine groups, by calling on them to address 80% of the 47 characteristics, for example.
Dr. Nelson, who is the medical director of the hospitalist medicine group at Overlake Hospital in Bellevue, Wash., and a practice management consultant, said the most important thing is that the list is not ignored.
Spend 20 minutes using the list to grade the group’s performance, he said, and then have other physicians do the same and compare the results.
"It’s a good exercise to think about how your practice is doing, compared with what a large group of people think might be the best way to approach things," Dr. Nelson said.
But the document’s authors admitted that there could be a downside to the publication of the principles. Hospital medicine groups could be held accountable for meeting these criteria without getting the necessary financial support from their hospitals.
"The idea is to encourage good performance," Dr. Nelson said. "No group is doing them all and to use this simply as a tool of punishment will not advance the cause much."
The list of principles and characteristics was created over 18 months by a workgroup of experts selected by the SHM board of directors. The document was also reviewed by focus groups of hospitalists and by health care experts outside of the field of hospital medicine.
On Twitter @maryellenny
The Society of Hospital Medicine has come up with 10 "basic ingredients" for building and sustaining an effective hospital medicine group.
The list of guiding principles, which was published in the Journal of Hospital Medicine, is meant to help hospital medicine groups perform self-assessments and set goals for improvement, while also providing hospital executives with benchmarks for evaluating those groups. (J. Hosp. Med. 2014;9:123-8).
The 10 principles and 47 key characteristics of an effective hospital medicine group address everything from adequate staffing to the scope of clinical activities for the hospitalist.
The biggest challenge in creating the document was identifying characteristics that could apply to all types of hospital medicine groups, given the diversity in practice settings, employment models, and patient populations in hospital medicine, said Dr. John Nelson, a coauthor of the document and cofounder of the Society of Hospital Medicine (SHM).
But it won’t be a perfect fit for everyone, he said. "It’s a little bit like a roadmap for leading a good life," he said. "You put on exercise and eating well and things of that sort, but there are lots of people that have different circumstances."
In the document, the SHM workgroup suggested that the principles and characteristics could be used in variety of ways. For instance, they could be used as a framework for hospital medicine groups and hospital leaders to discuss ongoing issues. They could also be used more formally to guide planning and budget activities for the hospital medicine group. Or hospital leaders could use them to evaluate hospital medicine groups, by calling on them to address 80% of the 47 characteristics, for example.
Dr. Nelson, who is the medical director of the hospitalist medicine group at Overlake Hospital in Bellevue, Wash., and a practice management consultant, said the most important thing is that the list is not ignored.
Spend 20 minutes using the list to grade the group’s performance, he said, and then have other physicians do the same and compare the results.
"It’s a good exercise to think about how your practice is doing, compared with what a large group of people think might be the best way to approach things," Dr. Nelson said.
But the document’s authors admitted that there could be a downside to the publication of the principles. Hospital medicine groups could be held accountable for meeting these criteria without getting the necessary financial support from their hospitals.
"The idea is to encourage good performance," Dr. Nelson said. "No group is doing them all and to use this simply as a tool of punishment will not advance the cause much."
The list of principles and characteristics was created over 18 months by a workgroup of experts selected by the SHM board of directors. The document was also reviewed by focus groups of hospitalists and by health care experts outside of the field of hospital medicine.
On Twitter @maryellenny
FROM THE JOURNAL OF HOSPITAL MEDICINE
Testing now is critical to ICD-10 readiness
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
Still not prepared for the switch over to ICD-10? Experts say there’s still time to catch up before the Oct. 1 compliance date.
In an ideal world, physicians, their coders, and office staff would have already fully assessed the cost of transitioning to ICD-10, would have undergone training about how to improve clinical documentation and appropriate use of the new diagnosis codes, and would have internally tested their upgraded software. That would leave more than half a year to complete external testing with health plans to ensure that they get paid in October.
The reality? Few are on track to meet those milestones on time.
"Everybody is behind, not just practices," said Robert Tennant, senior policy adviser at the Medical Group Management Association (MGMA). For a practice to be ready for ICD-10, the "key trading partners have to be ready and our surveys are indicating that they are not," he said.
Those partners include practice management software vendors, electronic health record (EHR) vendors, clearinghouses, and private and public payers.
So does that mean another ICD-10 delay is likely? The Centers for Medicare and Medicaid Services says no.
Part of the reason may be that health plans, which are investing money in upgrading their own systems, are pushing the agency to move forward on time. They are signaling to the government that they don’t want another delay, Mr. Tennant said.
The MGMA is advising its members to prepare for an Oct. 1 launch of ICD-10. But Mr. Tennant said he’s not entirely convinced that the CMS will stick to the date if much of the health care industry is unprepared to make the switch.
"Claims have to be paid," he said. "The system cannot grind to a halt because practices that aren’t paid can’t see patients."
Start with training
Assuming that most physician offices have assessed which parts of their practice management and EHR systems need to be upgraded, and have determined the cost for upgrades and training, it’s time to get familiar with the new diagnosis coding system.
Coders and billers will need the most training on the new coding methodology, but doctors still need to get familiar with the level of documentation that’s need for their most frequently used codes. In general, the new system calls for great specificity, though it’s not an absolute rule.
For instance, the classification for asthma has changed from ICD-9 to ICD-10. Physicians will need to provide more specific documentation about the severity level (moderately persistent, severely persistent, etc.) for their coders to select the appropriate ICD-10 code, according to Kathryn DeVault, a coding expert at the American Health Information Management Association (AHIMA).
"The good news is that as different as ICD-10 and ICD-9 are, they are similar," Ms. DeVault said. "If there’s a familiarity or comfort level working with ICD-9, it’s a natural transition to ICD-10."
While there are some significant changes, especially related to orthopedic codes, for many subspecialties the differences will be minimal, she said.
Ms. DeVault recommended having the practice manager or lead coder identify the top 20 diagnosis codes for every physician in the practice and build some education around those frequently used codes.
She cautioned doctors not to skimp on the time and money needed to thoroughly train themselves and their staffs. "The key here is to do it right and do it right the first time," she said.
Check the books
Physicians and their staff also need to evaluate their current cash flow and revenue cycle, including the age of account balances, billing lag time, and other issues that may result in delayed or denied claims, said Asia Blunt, practice management strategist at the American Academy of Family Physicians. Correct those problems now, she said, then reevaluate between April and August.
Experts at the AAFP are recommending that physicians put aside a cash reserve, if possible, to cover expenses during the first 3 months of the transition in case large numbers of claims are denied. (See below for more tips on planning for the worst.)
Testing with vendors, payers
Internal and external testing is also key. Before Oct. 1, practices should have completed end-to-end testing of their upgraded systems, ensuring that everything works smoothly from the time they code a claim to when they receive payment from the health insurer.
Practices can begin internal testing as soon as they have upgraded their software. But external testing will depend on when clearinghouses and health plans are ready.
The CMS will provide the first testing opportunity March 3-7. The agency will hold a national ICD-10 testing week allowing practices and clearinghouses to submit claims using the new coding system. Practices will receive an acknowledgement that the claims were either accepted or rejected by the system. Practices must register in advance through their local Medicare Administrative Contractor (MAC) website to test. Find your local MAC here.
But this type of front-end testing is only a first step, Mr. Tennant said. Front-end testing determines whether the claim contains an ICD-10 code and if it is in the right place and the right format. But practices will need to conduct further testing with payers to determine if the code they used is appropriate and whether they will get paid.
For instance, when submitting a claim for a sprained ankle under ICD-10, the coder might specify right or left ankle, or leave it as unspecified. Depending on the health insurer’s policy around the code, the insurer could pay the claim, reject it, or hold or "pend" it while seeking additional information. The complicating factor, Mr. Tennant said, is that each health insurer has different coding policies and those policies have yet to be released for ICD-10.
"It’s very frustrating for everybody," Mr. Tennant said.
To minimize the impact, Mr. Tennant recommended identifying the payers responsible for the majority of your claims. Keep in contact with them about the release of their payment policies and testing schedules, he said.
"Be aggressive in your outreach to those plans," he said.
Contingency plans
Just in case a worst-case scenario develops, Mr. Tennant offered the advice on ICD-10 contingency plans:
• Research back-up options for practice management systems and clearinghouses. If the vendors aren’t providing a clear answer on when they will be ready to offer upgrades and testing, start researching alternatives. Ask colleagues if they have vendors that are prepared for the transition.
• Don’t rely on one coder. Train more than one staff member on how to use the new coding system. That way, if the chief coder leaves 3 weeks before the compliance date, someone else can step in.
• Limit vacations around the Oct. 1 compliance date. This is not a time to operate short staffed.
• Don’t wait around for health plans to start ICD-10 testing. Start with context testing. Take a subset of high-dollar, high-volume ICD-9 claims that have already been paid by the health plan and practice coding them in ICD-10. Similarly, begin to code claims in parallel in both ICD-9 and ICD-10 and move them through your internal workflow. In both of these testing approaches, check if the documentation provided is sufficient to identify the best ICD-10 code. If not, it’s time for more training.
• Ensure you have enough cash to operate in case claims are rejected or delayed. Setting aside cash reserves is a good move. Consider postponing major capital investments for a few months before and after Oct. 1. Obtaining a line of credit to cover a few months of operating expenses is another option.
• Submit as many of claims as possible with ICD-9 codes before Oct. 1.
Free ICD-10 resources
• ICD-10 guide with checklists and timelines (CMS).
• Sample letter to gauge vendors’ ICD-10 readiness (AHIMA).
• Cost calculator and ICD-10 timeline (AAFP).
• Twelve step transition plan, white papers, and practice tool (AMA)
On Twitter @maryellenny
Medicare proposes coverage for hepatitis C screening
Medicare officials propose to cover screening for hepatitis C virus for adults at high risk of infection as well as a one-time screening for Baby Boomers.
The plan, announced in a coverage memo on March 4, would provide Medicare coverage for all screening tests approved by the Food and Drug Administration when they are ordered by a primary care physician or other primary care clinician.
Officials at the Centers for Medicare & Medicaid Services initially floated the idea of hepatitis C (HCV) screening coverage last September. The response was overwhelmingly positive, with nearly all of the 65 public comments advocating in favor of coverage.
HCV screening is already recommended by the U.S. Preventive Services Task Force and the American Academy of Family Physicians. The AAFP recommends screening for HCV infection in high-risk adults. But the 2013 USPSTF recommendation goes further, calling on physicians to screen high-risk adults as well as to provide a one-time screening to all patients born between 1945 and 1965.
The Medicare proposal echoes the USPSTF recommendations.
For the proposal, the CMS deems the following patients as at high risk for HCV infection: adults who use illicit injection drugs or have a history of such drug use, as well as individuals who had blood transfusions before 1992. The proposal calls for coverage of an initial screening test for high-risk adults, followed by annual rescreening for those who continue to use illicit injection drugs after the first test.
“We acknowledge the limited evidence concerning health outcomes of HCV screening,” agency officials wrote in the coverage memo. “However, CMS believes that screening for HCV infection provides an opportunity for appropriate interventions to benefit the infected person by permitting for the early detection of, and potentially the prevention of, HCV-related liver disease.”
Treatment options for hepatitis C are expanding, the CMS noted in its coverage memo. Over the past several years, the FDA has approved three protease inhibitors, boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio), for the treatment of patients with genotype 1 infection. Each of these three drugs can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, the FDA approved sofosbuvir (Sovaldi), which is indicated for the treatment of hepatitis C infection from genotypes 1, 2, 3, or 4. But access to that drug could be impacted by its hefty price tag, which is $1,000 a pill or about $84,000 for a 12-week course of treatment.
Comments on the CMS screening proposal can be made until April 3. The CMS is scheduled to issue a final decision on coverage in June.
On Twitter @maryellenny
Medicare officials propose to cover screening for hepatitis C virus for adults at high risk of infection as well as a one-time screening for Baby Boomers.
The plan, announced in a coverage memo on March 4, would provide Medicare coverage for all screening tests approved by the Food and Drug Administration when they are ordered by a primary care physician or other primary care clinician.
Officials at the Centers for Medicare & Medicaid Services initially floated the idea of hepatitis C (HCV) screening coverage last September. The response was overwhelmingly positive, with nearly all of the 65 public comments advocating in favor of coverage.
HCV screening is already recommended by the U.S. Preventive Services Task Force and the American Academy of Family Physicians. The AAFP recommends screening for HCV infection in high-risk adults. But the 2013 USPSTF recommendation goes further, calling on physicians to screen high-risk adults as well as to provide a one-time screening to all patients born between 1945 and 1965.
The Medicare proposal echoes the USPSTF recommendations.
For the proposal, the CMS deems the following patients as at high risk for HCV infection: adults who use illicit injection drugs or have a history of such drug use, as well as individuals who had blood transfusions before 1992. The proposal calls for coverage of an initial screening test for high-risk adults, followed by annual rescreening for those who continue to use illicit injection drugs after the first test.
“We acknowledge the limited evidence concerning health outcomes of HCV screening,” agency officials wrote in the coverage memo. “However, CMS believes that screening for HCV infection provides an opportunity for appropriate interventions to benefit the infected person by permitting for the early detection of, and potentially the prevention of, HCV-related liver disease.”
Treatment options for hepatitis C are expanding, the CMS noted in its coverage memo. Over the past several years, the FDA has approved three protease inhibitors, boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio), for the treatment of patients with genotype 1 infection. Each of these three drugs can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, the FDA approved sofosbuvir (Sovaldi), which is indicated for the treatment of hepatitis C infection from genotypes 1, 2, 3, or 4. But access to that drug could be impacted by its hefty price tag, which is $1,000 a pill or about $84,000 for a 12-week course of treatment.
Comments on the CMS screening proposal can be made until April 3. The CMS is scheduled to issue a final decision on coverage in June.
On Twitter @maryellenny
Medicare officials propose to cover screening for hepatitis C virus for adults at high risk of infection as well as a one-time screening for Baby Boomers.
The plan, announced in a coverage memo on March 4, would provide Medicare coverage for all screening tests approved by the Food and Drug Administration when they are ordered by a primary care physician or other primary care clinician.
Officials at the Centers for Medicare & Medicaid Services initially floated the idea of hepatitis C (HCV) screening coverage last September. The response was overwhelmingly positive, with nearly all of the 65 public comments advocating in favor of coverage.
HCV screening is already recommended by the U.S. Preventive Services Task Force and the American Academy of Family Physicians. The AAFP recommends screening for HCV infection in high-risk adults. But the 2013 USPSTF recommendation goes further, calling on physicians to screen high-risk adults as well as to provide a one-time screening to all patients born between 1945 and 1965.
The Medicare proposal echoes the USPSTF recommendations.
For the proposal, the CMS deems the following patients as at high risk for HCV infection: adults who use illicit injection drugs or have a history of such drug use, as well as individuals who had blood transfusions before 1992. The proposal calls for coverage of an initial screening test for high-risk adults, followed by annual rescreening for those who continue to use illicit injection drugs after the first test.
“We acknowledge the limited evidence concerning health outcomes of HCV screening,” agency officials wrote in the coverage memo. “However, CMS believes that screening for HCV infection provides an opportunity for appropriate interventions to benefit the infected person by permitting for the early detection of, and potentially the prevention of, HCV-related liver disease.”
Treatment options for hepatitis C are expanding, the CMS noted in its coverage memo. Over the past several years, the FDA has approved three protease inhibitors, boceprevir (Victrelis), telaprevir (Incivek), and simeprevir (Olysio), for the treatment of patients with genotype 1 infection. Each of these three drugs can be used in combination with pegylated interferon and ribavirin for the treatment of genotype 1 infection.
Last year, the FDA approved sofosbuvir (Sovaldi), which is indicated for the treatment of hepatitis C infection from genotypes 1, 2, 3, or 4. But access to that drug could be impacted by its hefty price tag, which is $1,000 a pill or about $84,000 for a 12-week course of treatment.
Comments on the CMS screening proposal can be made until April 3. The CMS is scheduled to issue a final decision on coverage in June.
On Twitter @maryellenny
Obama 2015 budget would extend Medicaid pay bump
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
Primary care physicians would continue to see higher payments for treating Medicaid patients through the end of 2015, under President Obama’s proposed budget for the upcoming fiscal year.
The budget request submitted to Congress March 4 includes $5.4 billion to extend the Affordable Care Act provisions that pay physicians at the higher Medicare levels for providing certain primary care services to Medicaid patients. The ACA sunsets the pay increase at the end of 2014.
Under the budget proposal, nurse practitioners and physician assistants also would be eligible for the higher payment rates.
"Allowing [the higher rates] to expire would result in a deep, across-the-board cut to primary care physicians who are taking care of the most vulnerable populations, at a time when millions more are becoming eligible for Medicaid," Dr. Molly Cooke, president of the American College of Physicians (ACP), said in a statement. ACP is urging Congress to go further and fund the program for at least 2 more years.
The $1 trillion budget proposed for the Health and Human Services (HHS) department includes $77.1 billion in discretionary spending, down $1.3 billion from 2014. The proposal includes investments in the primary care workforce, expanded mental health services, and continued implementation of the ACA insurance marketplaces.
The president’s budget also calls for Medicare cuts that would save the government more than $400 billion over 10 years. The cost-saving measures, which have been proposed in previous budgets, include reduction in Medicare coverage of hospitals’ bad debts; reductions to indirect graduate medical education payments; payment cuts to critical access hospitals; and payment cuts for inpatient rehabilitation facilities, long-term care hospitals, and home health agencies. In addition, the budget would introduce readmission penalties for skilled nursing facilities and strengthen the controversial Independent Payment Advisory Board (IPAB).
As have previous budget requests, the fiscal 2015 proposal would require the IPAB to recommend cost-cutting targets to Congress if the Medicare growth rate exceeds gross domestic product plus 0.5 percentage points. Current law sets that level at GDP plus 1 percentage point.
The 2015 budget proposal would increase investment in the primary care workforce. It requests more than $5 billion over the next decade to train 13,000 new residents as part of a new competitive grant program available to teaching hospitals, children’s hospitals, and community-based consortia of teaching hospitals or other health care institutions. In 2015, the program would provide $100 million for pediatric residents in children’s hospitals.
The budget also beefs up funding for the National Health Service Corps. It includes nearly $4 billion in new funding over 6 years to increase the number of health providers in rural areas and federally funded health centers to 15,000. And it would invest $4.6 billion in community health centers in 2015 and another $8.1 billion for the next 3 years.
For mental health services, the budget includes $55 million for Project AWARE, which encourages community and school officials to work together to keep schools safe, refer students to mental health services, and provide mental health "first aid" training so that teachers can detect early signs of mental illness.
The budget request includes $50 million to train about 5,000 new mental health professionals, $20 million to help young adults aged 16-25 years navigate behavioral health services, and $5 million to change attitudes about people who have behavioral health needs in the workplace.
The budget also provides funding for a demonstration project in Medicaid to help reduce the use of psychotropic medications prescribed to children in foster care by improving access to other mental health services.
The release of the president’s budget request comes just weeks before the end of open enrollment in private health plans through the ACA’s marketplaces. The budget includes $1.8 billion in funding for 2015 to cover the cost of running the federally facilitated marketplace. However, most of the funding – $1.2 billion – would be covered by user fees from health plans in the marketplaces. If Congress fails to provide the remaining funds, HHS officials said they could transfer monies from other agency accounts to cover marketplace costs.
On Twitter @maryellenny
HHS Proposes New Targets for HAI Reduction
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
On Twitter @maryellenny
HHS proposes new targets for HAI reduction
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
HHS is asking the public to comment on the proposed targets by March 27. Comments can be sent by e-mail to [email protected].
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
HHS is asking the public to comment on the proposed targets by March 27. Comments can be sent by e-mail to [email protected].
On Twitter @maryellenny
Federal officials are proposing new targets for reducing health care–associated infections, including a 75% reduction in invasive methicillin-resistant Staphylococcus aureus infections by 2020.
The targets are available at www.health.gov/hai/pdfs/HAI-Targets.pdf and were produced by a committee of experts in the prevention of HAIs, who were charged with updating the federal government’s National Action Plan to Prevent Health Care-Associated Infections. The 5-year goals outlined in that plan, originally released in 2009, expired last year.
The current proposal would make HAI reduction in U.S. hospitals more aggressive in some areas, while dropping five Surgical Care Improvement Project measures from the target list. The process measures, which aim to prevent surgical site infections, are now widely accepted as standards of practice and have adherence rates greater than 95%, according to HHS.
Some of the new targets will be based on 2015 baseline data, which are not yet available.
The seven proposed targets for 2020 are:
• Reduce central line–associated bloodstream infections by 50% from the 2015 baseline. Infections from mucosal barrier injury will be excluded from the calculation.
• Reduce catheter-associated urinary tract infections by 25% from the 2015 baseline.
• Reduce invasive health care–associated MRSA infections by 75% from the 2007 to 2008 baseline (27.08 infections per 100,000 persons).
• Reduce facility-onset MRSA by 50% from the 2015 baseline.
• Reduce facility-onset Clostridium difficile infections by 30% from the 2015 baseline.
• Reduce the rate of C. difficile hospitalizations by 30% from the 2015 baseline.
• Reduce surgical site infection admission and readmission by 30% from the 2015 baseline.
Hospitals and health care providers are seeing mixed results in reducing HAIs so far, according to data from HHS. As of October 2012, there have been steady improvements in reducing central line–associated bloodstream infections, health-care–associated invasive MRSA infections, and surgical site infections. But progress on reducing hospitalizations with C. difficile infection has leveled off, and providers are also not on track to meet targets for catheter-associated urinary tract infections, according to HHS.
HHS is asking the public to comment on the proposed targets by March 27. Comments can be sent by e-mail to [email protected].
On Twitter @maryellenny