User login
Rapid-onset ulcerative hand nodule
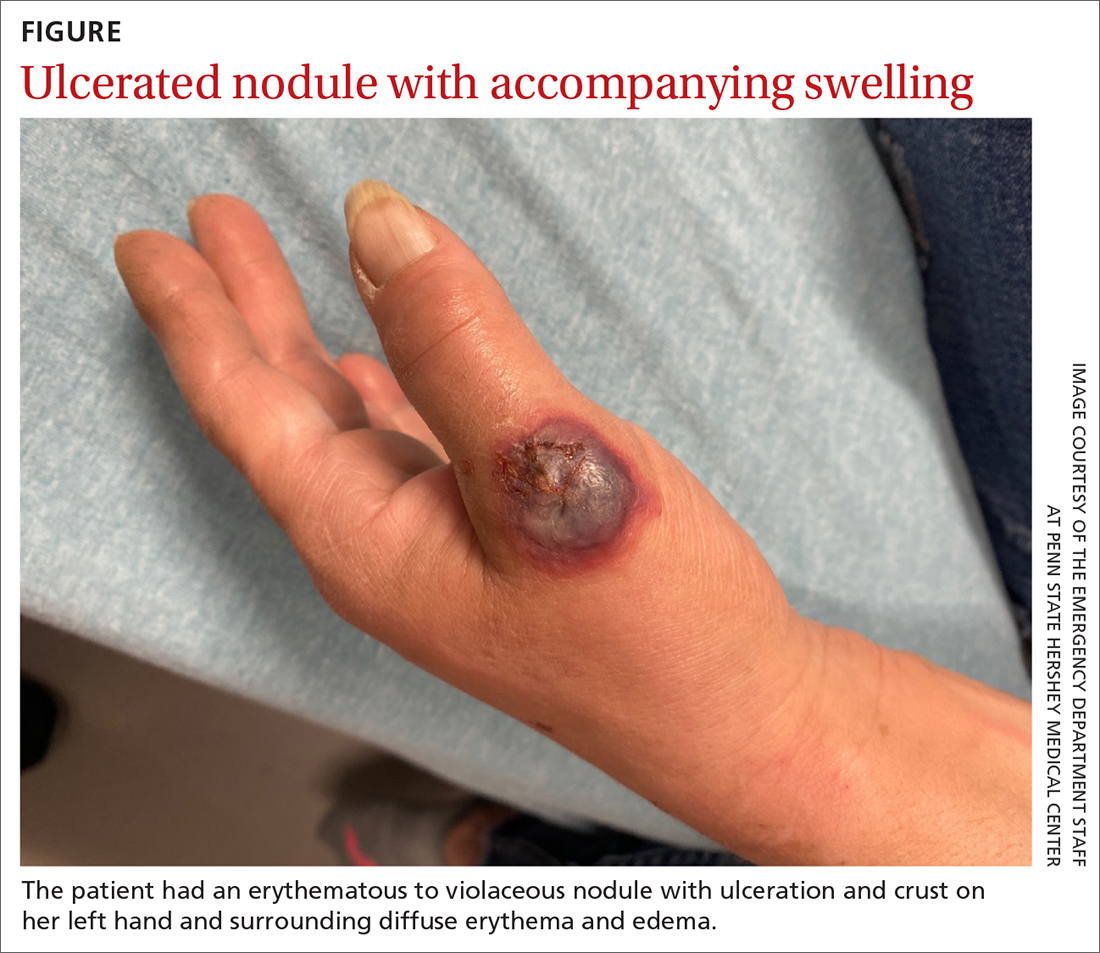
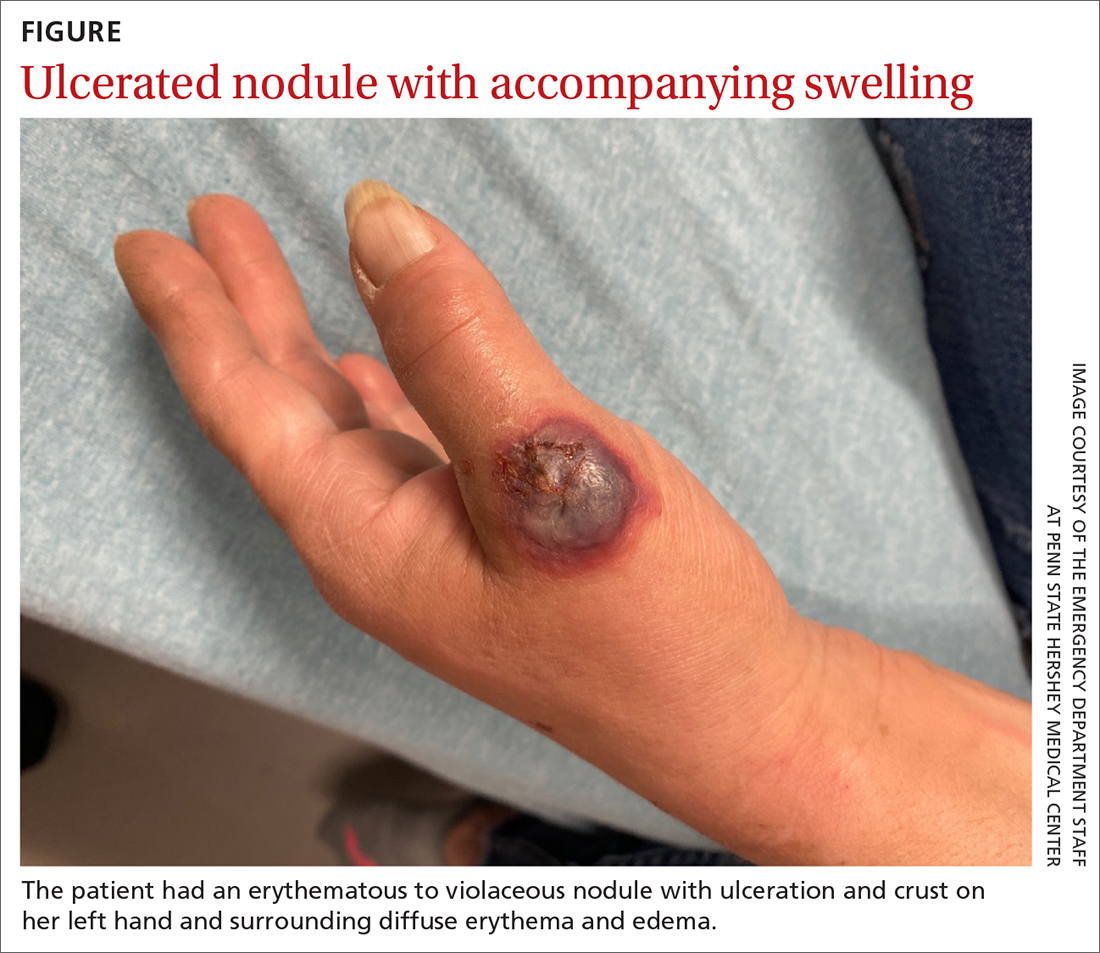
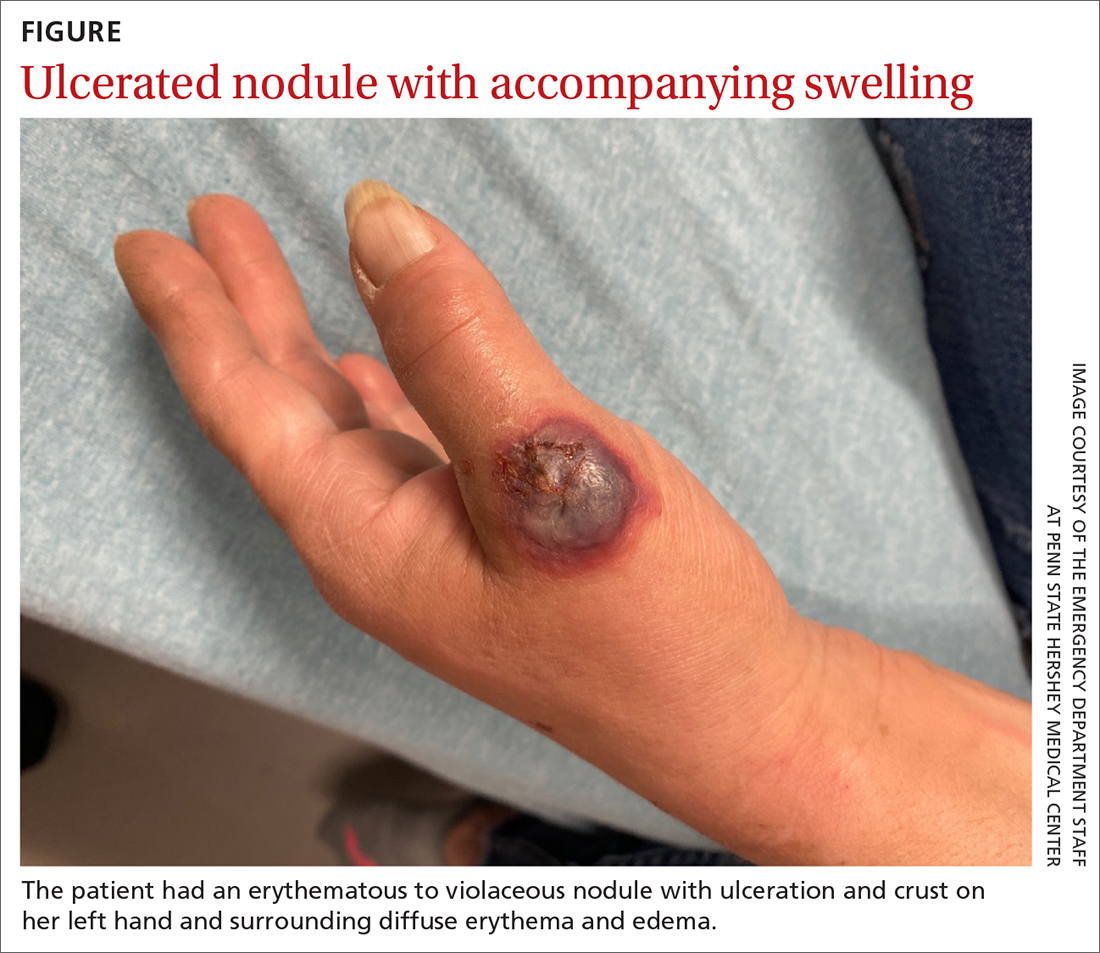
A 55-YEAR-OLD WOMAN developed a small red papule on her left hand that, over the course of a week, progressed rapidly into an ulcerated nodule with accompanying swelling and pain. She reported concomitant fatigue, unintentional weight loss, and swollen axillary lymph nodes. Past medical history included rheumatoid arthritis.
A physical examination of her left hand revealed a tender, erythematous to violaceous nodule with ulceration and crust and surrounding diffuse erythema and edema (FIGURE). She also had several enlarged, nontender right axillary lymph nodes. Initial lab evaluation was significant for leukocytosis (13.8 K/uL) with increased neutrophils, lymphocytes, and eosinophils. Two punch biopsies were performed and the samples submitted for hematoxylin and eosin (H&E) staining and tissue culture.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neutrophilic dermatosis of the dorsal hands
The results of H&E were consistent with neutrophilic dermatosis of the dorsal hands (NDDH). Tissue culture was negative for fungus, bacteria, and atypical mycobacteria, confirming the diagnosis.
NDDH is a neutrophilic dermatosis and considered a localized variant of Sweet syndrome, manifesting on the dorsal hands as suppurative, erythematous to violaceous papules, plaques, or nodules that often undergo necrosis, blistering, and ulceration. The diagnosis can be made clinically, although a biopsy is usually performed for confirmation. It is characterized histologically by a dense dermal neutrophilic infiltrate along with dermal edema.1
The pathogenesis of NDDH is not fully known.2 It is often preceded by trauma and may be associated with recent infection (respiratory, gastrointestinal), inflammatory bowel disease, autoimmune disease (eg, rheumatoid arthritis), or malignancy.1 The most common associated malignancies are hematologic, such as myelodysplastic syndrome, leukemia, or lymphoma, although solid tumors also can be seen.1,3 Therefore, patients who receive a diagnosis of NDDH typically require further work-up to rule out these associated conditions. NDDH is a rare enough entity that incidence/prevalence data aren’t available or likely to be accurate.
The differential includes infection and neoplastic processes
NDDH often is mistaken for an infectious abscess and unsuccessfully treated with antimicrobial agents, such as those commonly used for staphylococcus and streptococcus skin and soft-tissue infections. Thus, wound or tissue culture may be considered to exclude infection from the differential diagnosis. In addition to infectious processes such as sporotrichosis or an atypical mycobacterial infection, the differential includes other neutrophilic dermatoses and neoplastic processes such as lymphoma or leukemia cutis.
Sporotrichosis is caused by Sporothrix schenckii and usually spreads proximally after entering through a wound or cut. Special stains on histology and culture are needed to make the diagnosis.
Continue to: Atypical mycobacterial infections
Atypical mycobacterial infections usually enter through an area of trauma and spread proximally after inoculation. Atypical mycobacterial infections can be diagnosed via biopsy with special stains, culture, and polymerase chain reaction of the tissue.
Neutrophilic dermatoses are a broad category of dermatoses that include NDDH, pyoderma gangrenosum, and Sweet syndrome. This category of dermatoses is differentiated by morphology and distribution of lesions.
Lymphoma can be primary cutaneous or secondary to a systemic lymphoma. A biopsy will show a collection of atypical lymphocytes.
Treatment begins with steroids
Treatment with topical (eg, 0.05% clobetasol ointment bid), intralesional (10 to 40 mg/mL triamcinolone acetonide), or systemic (eg, prednisone 0.5 to 1 mg/kg tapered over the course of 1-2 months) steroids is considered first-line therapy and often results in rapid clinical improvement. Agents such as dapsone (25 to 150 mg/d) and/or colchicine (0.6 mg bid to tid) may be used in recalcitrant cases or in patients for whom steroids are contraindicated.2
Our patient’s NDDH was treated with prednisone (~1.0 mg/kg daily tapered over the course of 6 weeks). She was referred to Hematology/Oncology for further work-up of her constitutional symptoms, lymphadenopathy, and leukocytosis. Ultimately, she received a diagnosis of concomitant chronic lymphocytic leukemia/small lymphocytic lymphoma. The patient required no immediate treatment for her indolent lymphoma and was advised that she would need to get blood work done on a regular basis and have annual check-ups.
1. Walling HW, Snipes CJ, Gerami P, et al. The relationship between neutrophilic dermatosis of the dorsal hands and Sweet syndrome: report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006;142:57-63.
2. Micallef D, Bonnici M, Pisani D, et al. Neutrophilic dermatosis of the dorsal hands: a review of 123 Cases. J Am Acad Dermatol. 2019;S0190-9622(19)32678-7. doi: 10.1016/j.jaad.2019.08.070
3. Mobini N, Sadrolashrafi K, Michaels S. Neutrophilic dermatosis of the dorsal hands: report of a case and review of the literature. Case Rep Dermatol Med. 2019;2019:8301585. doi: 10.1155/2019/8301585
A 55-YEAR-OLD WOMAN developed a small red papule on her left hand that, over the course of a week, progressed rapidly into an ulcerated nodule with accompanying swelling and pain. She reported concomitant fatigue, unintentional weight loss, and swollen axillary lymph nodes. Past medical history included rheumatoid arthritis.
A physical examination of her left hand revealed a tender, erythematous to violaceous nodule with ulceration and crust and surrounding diffuse erythema and edema (FIGURE). She also had several enlarged, nontender right axillary lymph nodes. Initial lab evaluation was significant for leukocytosis (13.8 K/uL) with increased neutrophils, lymphocytes, and eosinophils. Two punch biopsies were performed and the samples submitted for hematoxylin and eosin (H&E) staining and tissue culture.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neutrophilic dermatosis of the dorsal hands
The results of H&E were consistent with neutrophilic dermatosis of the dorsal hands (NDDH). Tissue culture was negative for fungus, bacteria, and atypical mycobacteria, confirming the diagnosis.
NDDH is a neutrophilic dermatosis and considered a localized variant of Sweet syndrome, manifesting on the dorsal hands as suppurative, erythematous to violaceous papules, plaques, or nodules that often undergo necrosis, blistering, and ulceration. The diagnosis can be made clinically, although a biopsy is usually performed for confirmation. It is characterized histologically by a dense dermal neutrophilic infiltrate along with dermal edema.1
The pathogenesis of NDDH is not fully known.2 It is often preceded by trauma and may be associated with recent infection (respiratory, gastrointestinal), inflammatory bowel disease, autoimmune disease (eg, rheumatoid arthritis), or malignancy.1 The most common associated malignancies are hematologic, such as myelodysplastic syndrome, leukemia, or lymphoma, although solid tumors also can be seen.1,3 Therefore, patients who receive a diagnosis of NDDH typically require further work-up to rule out these associated conditions. NDDH is a rare enough entity that incidence/prevalence data aren’t available or likely to be accurate.
The differential includes infection and neoplastic processes
NDDH often is mistaken for an infectious abscess and unsuccessfully treated with antimicrobial agents, such as those commonly used for staphylococcus and streptococcus skin and soft-tissue infections. Thus, wound or tissue culture may be considered to exclude infection from the differential diagnosis. In addition to infectious processes such as sporotrichosis or an atypical mycobacterial infection, the differential includes other neutrophilic dermatoses and neoplastic processes such as lymphoma or leukemia cutis.
Sporotrichosis is caused by Sporothrix schenckii and usually spreads proximally after entering through a wound or cut. Special stains on histology and culture are needed to make the diagnosis.
Continue to: Atypical mycobacterial infections
Atypical mycobacterial infections usually enter through an area of trauma and spread proximally after inoculation. Atypical mycobacterial infections can be diagnosed via biopsy with special stains, culture, and polymerase chain reaction of the tissue.
Neutrophilic dermatoses are a broad category of dermatoses that include NDDH, pyoderma gangrenosum, and Sweet syndrome. This category of dermatoses is differentiated by morphology and distribution of lesions.
Lymphoma can be primary cutaneous or secondary to a systemic lymphoma. A biopsy will show a collection of atypical lymphocytes.
Treatment begins with steroids
Treatment with topical (eg, 0.05% clobetasol ointment bid), intralesional (10 to 40 mg/mL triamcinolone acetonide), or systemic (eg, prednisone 0.5 to 1 mg/kg tapered over the course of 1-2 months) steroids is considered first-line therapy and often results in rapid clinical improvement. Agents such as dapsone (25 to 150 mg/d) and/or colchicine (0.6 mg bid to tid) may be used in recalcitrant cases or in patients for whom steroids are contraindicated.2
Our patient’s NDDH was treated with prednisone (~1.0 mg/kg daily tapered over the course of 6 weeks). She was referred to Hematology/Oncology for further work-up of her constitutional symptoms, lymphadenopathy, and leukocytosis. Ultimately, she received a diagnosis of concomitant chronic lymphocytic leukemia/small lymphocytic lymphoma. The patient required no immediate treatment for her indolent lymphoma and was advised that she would need to get blood work done on a regular basis and have annual check-ups.
A 55-YEAR-OLD WOMAN developed a small red papule on her left hand that, over the course of a week, progressed rapidly into an ulcerated nodule with accompanying swelling and pain. She reported concomitant fatigue, unintentional weight loss, and swollen axillary lymph nodes. Past medical history included rheumatoid arthritis.
A physical examination of her left hand revealed a tender, erythematous to violaceous nodule with ulceration and crust and surrounding diffuse erythema and edema (FIGURE). She also had several enlarged, nontender right axillary lymph nodes. Initial lab evaluation was significant for leukocytosis (13.8 K/uL) with increased neutrophils, lymphocytes, and eosinophils. Two punch biopsies were performed and the samples submitted for hematoxylin and eosin (H&E) staining and tissue culture.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Neutrophilic dermatosis of the dorsal hands
The results of H&E were consistent with neutrophilic dermatosis of the dorsal hands (NDDH). Tissue culture was negative for fungus, bacteria, and atypical mycobacteria, confirming the diagnosis.
NDDH is a neutrophilic dermatosis and considered a localized variant of Sweet syndrome, manifesting on the dorsal hands as suppurative, erythematous to violaceous papules, plaques, or nodules that often undergo necrosis, blistering, and ulceration. The diagnosis can be made clinically, although a biopsy is usually performed for confirmation. It is characterized histologically by a dense dermal neutrophilic infiltrate along with dermal edema.1
The pathogenesis of NDDH is not fully known.2 It is often preceded by trauma and may be associated with recent infection (respiratory, gastrointestinal), inflammatory bowel disease, autoimmune disease (eg, rheumatoid arthritis), or malignancy.1 The most common associated malignancies are hematologic, such as myelodysplastic syndrome, leukemia, or lymphoma, although solid tumors also can be seen.1,3 Therefore, patients who receive a diagnosis of NDDH typically require further work-up to rule out these associated conditions. NDDH is a rare enough entity that incidence/prevalence data aren’t available or likely to be accurate.
The differential includes infection and neoplastic processes
NDDH often is mistaken for an infectious abscess and unsuccessfully treated with antimicrobial agents, such as those commonly used for staphylococcus and streptococcus skin and soft-tissue infections. Thus, wound or tissue culture may be considered to exclude infection from the differential diagnosis. In addition to infectious processes such as sporotrichosis or an atypical mycobacterial infection, the differential includes other neutrophilic dermatoses and neoplastic processes such as lymphoma or leukemia cutis.
Sporotrichosis is caused by Sporothrix schenckii and usually spreads proximally after entering through a wound or cut. Special stains on histology and culture are needed to make the diagnosis.
Continue to: Atypical mycobacterial infections
Atypical mycobacterial infections usually enter through an area of trauma and spread proximally after inoculation. Atypical mycobacterial infections can be diagnosed via biopsy with special stains, culture, and polymerase chain reaction of the tissue.
Neutrophilic dermatoses are a broad category of dermatoses that include NDDH, pyoderma gangrenosum, and Sweet syndrome. This category of dermatoses is differentiated by morphology and distribution of lesions.
Lymphoma can be primary cutaneous or secondary to a systemic lymphoma. A biopsy will show a collection of atypical lymphocytes.
Treatment begins with steroids
Treatment with topical (eg, 0.05% clobetasol ointment bid), intralesional (10 to 40 mg/mL triamcinolone acetonide), or systemic (eg, prednisone 0.5 to 1 mg/kg tapered over the course of 1-2 months) steroids is considered first-line therapy and often results in rapid clinical improvement. Agents such as dapsone (25 to 150 mg/d) and/or colchicine (0.6 mg bid to tid) may be used in recalcitrant cases or in patients for whom steroids are contraindicated.2
Our patient’s NDDH was treated with prednisone (~1.0 mg/kg daily tapered over the course of 6 weeks). She was referred to Hematology/Oncology for further work-up of her constitutional symptoms, lymphadenopathy, and leukocytosis. Ultimately, she received a diagnosis of concomitant chronic lymphocytic leukemia/small lymphocytic lymphoma. The patient required no immediate treatment for her indolent lymphoma and was advised that she would need to get blood work done on a regular basis and have annual check-ups.
1. Walling HW, Snipes CJ, Gerami P, et al. The relationship between neutrophilic dermatosis of the dorsal hands and Sweet syndrome: report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006;142:57-63.
2. Micallef D, Bonnici M, Pisani D, et al. Neutrophilic dermatosis of the dorsal hands: a review of 123 Cases. J Am Acad Dermatol. 2019;S0190-9622(19)32678-7. doi: 10.1016/j.jaad.2019.08.070
3. Mobini N, Sadrolashrafi K, Michaels S. Neutrophilic dermatosis of the dorsal hands: report of a case and review of the literature. Case Rep Dermatol Med. 2019;2019:8301585. doi: 10.1155/2019/8301585
1. Walling HW, Snipes CJ, Gerami P, et al. The relationship between neutrophilic dermatosis of the dorsal hands and Sweet syndrome: report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006;142:57-63.
2. Micallef D, Bonnici M, Pisani D, et al. Neutrophilic dermatosis of the dorsal hands: a review of 123 Cases. J Am Acad Dermatol. 2019;S0190-9622(19)32678-7. doi: 10.1016/j.jaad.2019.08.070
3. Mobini N, Sadrolashrafi K, Michaels S. Neutrophilic dermatosis of the dorsal hands: report of a case and review of the literature. Case Rep Dermatol Med. 2019;2019:8301585. doi: 10.1155/2019/8301585
