User login
Left Ventricular Compression and Hypotension Due to Acute Colonic Pseudo-Obstruction
Acute colonic pseudo-obstruction is a postsurgical dilatation of the colon that presents with abdominal distension, pain, nausea, vomiting, constipation, or diarrhea and may lead to colonic ischemia and bowel perforation.
A cute colonic pseudo-obstruction, or Ogilvie syndrome, is dilatation of the colon without mechanical obstruction. It is often seen postoperatively after cesarean section , pelvic , spinal, or other orthopedic surgery, such as knee arthroplasty. 1 One study demonstrated an incidence of acute colonic pseudo-obstruction of 1.3% following hip replacement surgery. 2
The most common symptoms are abdominal distension, pain, nausea, vomiting, constipation, or diarrhea. Bowel sounds are present in the majority of cases.3 It is important to recognize the varied presentations of ileus in the postoperative setting. The most serious complications of acute colonic pseudo-obstruction are colonic ischemia and bowel perforation.
Case Presentation
An 84-year-old man underwent a total left hip arthroplasty revision. The evening after his surgery, his blood pressure (BP) decreased from 93/54 to 71/47 mm Hg, and his heart rate was 73 beats per minute. He was awake, in no acute distress, but reported loose stools. Results of cardiac and pulmonary examinations were normal, showing a regular rate and rhythm with no murmurs and clear lungs. There was normal jugular venous pressure and chronic pitting edema of the lower extremities bilaterally.
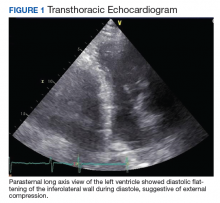
An abdominal examination revealed positive bowel sounds, a large ventral hernia, which was easily reducible, and a distended abdomen. His BP remained unchanged after IV normal saline 4 L, and urine output was 200 cc over 4 hours, which the care team determined represented adequate resuscitation. An infection workup, including chest X-ray, urinalysis, and blood and urine cultures, was unrevealing. Hemoglobin was stable at 8.5 g/dL (normal range 14-18), and creatinine level 0.66 mg/dL (normal range 0.7-1.2) at baseline. A transthoracic echocardiogram showed impaired diastolic filling suggestive of extrinsic compression of the left ventricle by mediastinal contents (Figure 1). An abdominal X-ray revealed diffuse dilatation of large bowel loops up to 10 cm, causing elevation and rightward shift of the heart (Figure 2A). A computed tomography scan of the abdomen showed total colonic dilatation without obstruction (Figure 2B).
The patient was diagnosed with postoperative ileus and acute colonic pseudo-obstruction. Nasogastric and rectal tubes were placed for decompression, and the patient was placed on nothing by mouth status. By postoperative day 3, his hypotension had resolved and his BP had improved to 111/58 mm Hg. The patient was able to resume a regular diet.
Discussion
We present an unusual case of left ventricular compression leading to hypotension due to acute colonic pseudo-obstruction. Our patient presented with the rare complication of hypotension due to cardiac compression, which we have not previously seen reported in the literature. Analogous instance of cardiac compression may arise from hiatal hernias and diaphragmatic paralysis. 4-6
Management of acute colonic pseudo-obstruction is through nothing by mouth status and abdominal decompression. For more severe cases, neostigmine, colonoscopic decompression, and surgery can be considered.
This surgical complication was diagnosed by internal medicine hospitalist consultants on a surgical comanagement service. In the comanagement model, the surgical specialties of orthopedic surgery, neurosurgery, and podiatry at San Francisco Veterans Affairs Medical Center in California have hospitalists who work with the team as active consultants for the medical care of the patients. Hospitalists develop a unique skill set in which they can anticipate new diagnoses, prevent or identify early complications, and individualize a patient’s postoperative care.7 One study found that a surgical comanagement service was associated with a decrease in the number of patients with at least 1 surgical complication, decrease in length of stay and 30-day readmissions for a medical cause, decreased consultant use, and an average cost savings per patient of about $2,600 to $4,300.8
Conclusions
With the increasing prevalence of hospitalist comanagement services, it is important for surgeons and nonsurgeons alike to recognize acute colonic pseudo-obstruction as a possible surgical complication.
1. Bernardi M, Warrier S, Lynch C, Heriot A. Acute and chronic pseudo-obstruction: a current update. ANZ J Surg. 2015;85(10):709-714. doi:10.1111/ans.13148
2. Norwood MGA, Lykostratis H, Garcea G, Berry DP. Acute colonic pseudo-obstruction following major orthopaedic surgery. Colorectal Dis. 2005;7(5):496-499. doi:10.1111/j.1463-1318.2005.00790.x
3. Vanek VW, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome). An analysis of 400 cases. Dis Colon Rectum. 1986;29(3):203-210. doi:10.1007/BF02555027
4. Devabhandari MP, Khan MA, Hooper TL. Cardiac compression following cardiac surgery due to unrecognised hiatus hernia. Eur J Cardiothoracic Surg. 2007;32(5):813-815. doi:10.1016/j.ejcts.2007.08.002
5. Asti E, Bonavina L, Lombardi M, Bandera F, Secchi F, Guazzi M. Reversibility of cardiopulmonary impairment after laparoscopic repair of large hiatal hernia. Int J Surg Case Rep. 2015;14:33-35. doi:10.1016/j.ijscr.2015.07.005
6. Tayyareci Y, Bayazit P, Taştan CP, Aksoy H. Right atrial compression due to idiopathic right diaphragm paralysis detected incidentally by transthoracic echocardiography. Turk Kardiyol Dern Ars. 2008;36(6):412-414.
7. Rohatgi N, Schulman K, Ahuja N. Comanagement by hospitalists: why it makes clinical and fiscal sense. Am J Med. 2020;133(3):257-258. doi:10.1016/j.amjmed.2019.07.053
8. Rohatgi N, Loftus P, Grujic O, Cullen M, Hopkins J, Ahuja N. Surgical comanagement by hospitalists improves patient outcomes: a propensity score analysis. Ann Surg. 2016;264(2):275-282. doi:10.1097/SLA.0000000000001629
Acute colonic pseudo-obstruction is a postsurgical dilatation of the colon that presents with abdominal distension, pain, nausea, vomiting, constipation, or diarrhea and may lead to colonic ischemia and bowel perforation.
Acute colonic pseudo-obstruction is a postsurgical dilatation of the colon that presents with abdominal distension, pain, nausea, vomiting, constipation, or diarrhea and may lead to colonic ischemia and bowel perforation.
A cute colonic pseudo-obstruction, or Ogilvie syndrome, is dilatation of the colon without mechanical obstruction. It is often seen postoperatively after cesarean section , pelvic , spinal, or other orthopedic surgery, such as knee arthroplasty. 1 One study demonstrated an incidence of acute colonic pseudo-obstruction of 1.3% following hip replacement surgery. 2
The most common symptoms are abdominal distension, pain, nausea, vomiting, constipation, or diarrhea. Bowel sounds are present in the majority of cases.3 It is important to recognize the varied presentations of ileus in the postoperative setting. The most serious complications of acute colonic pseudo-obstruction are colonic ischemia and bowel perforation.
Case Presentation
An 84-year-old man underwent a total left hip arthroplasty revision. The evening after his surgery, his blood pressure (BP) decreased from 93/54 to 71/47 mm Hg, and his heart rate was 73 beats per minute. He was awake, in no acute distress, but reported loose stools. Results of cardiac and pulmonary examinations were normal, showing a regular rate and rhythm with no murmurs and clear lungs. There was normal jugular venous pressure and chronic pitting edema of the lower extremities bilaterally.
An abdominal examination revealed positive bowel sounds, a large ventral hernia, which was easily reducible, and a distended abdomen. His BP remained unchanged after IV normal saline 4 L, and urine output was 200 cc over 4 hours, which the care team determined represented adequate resuscitation. An infection workup, including chest X-ray, urinalysis, and blood and urine cultures, was unrevealing. Hemoglobin was stable at 8.5 g/dL (normal range 14-18), and creatinine level 0.66 mg/dL (normal range 0.7-1.2) at baseline. A transthoracic echocardiogram showed impaired diastolic filling suggestive of extrinsic compression of the left ventricle by mediastinal contents (Figure 1). An abdominal X-ray revealed diffuse dilatation of large bowel loops up to 10 cm, causing elevation and rightward shift of the heart (Figure 2A). A computed tomography scan of the abdomen showed total colonic dilatation without obstruction (Figure 2B).
The patient was diagnosed with postoperative ileus and acute colonic pseudo-obstruction. Nasogastric and rectal tubes were placed for decompression, and the patient was placed on nothing by mouth status. By postoperative day 3, his hypotension had resolved and his BP had improved to 111/58 mm Hg. The patient was able to resume a regular diet.
Discussion
We present an unusual case of left ventricular compression leading to hypotension due to acute colonic pseudo-obstruction. Our patient presented with the rare complication of hypotension due to cardiac compression, which we have not previously seen reported in the literature. Analogous instance of cardiac compression may arise from hiatal hernias and diaphragmatic paralysis. 4-6
Management of acute colonic pseudo-obstruction is through nothing by mouth status and abdominal decompression. For more severe cases, neostigmine, colonoscopic decompression, and surgery can be considered.
This surgical complication was diagnosed by internal medicine hospitalist consultants on a surgical comanagement service. In the comanagement model, the surgical specialties of orthopedic surgery, neurosurgery, and podiatry at San Francisco Veterans Affairs Medical Center in California have hospitalists who work with the team as active consultants for the medical care of the patients. Hospitalists develop a unique skill set in which they can anticipate new diagnoses, prevent or identify early complications, and individualize a patient’s postoperative care.7 One study found that a surgical comanagement service was associated with a decrease in the number of patients with at least 1 surgical complication, decrease in length of stay and 30-day readmissions for a medical cause, decreased consultant use, and an average cost savings per patient of about $2,600 to $4,300.8
Conclusions
With the increasing prevalence of hospitalist comanagement services, it is important for surgeons and nonsurgeons alike to recognize acute colonic pseudo-obstruction as a possible surgical complication.
A cute colonic pseudo-obstruction, or Ogilvie syndrome, is dilatation of the colon without mechanical obstruction. It is often seen postoperatively after cesarean section , pelvic , spinal, or other orthopedic surgery, such as knee arthroplasty. 1 One study demonstrated an incidence of acute colonic pseudo-obstruction of 1.3% following hip replacement surgery. 2
The most common symptoms are abdominal distension, pain, nausea, vomiting, constipation, or diarrhea. Bowel sounds are present in the majority of cases.3 It is important to recognize the varied presentations of ileus in the postoperative setting. The most serious complications of acute colonic pseudo-obstruction are colonic ischemia and bowel perforation.
Case Presentation
An 84-year-old man underwent a total left hip arthroplasty revision. The evening after his surgery, his blood pressure (BP) decreased from 93/54 to 71/47 mm Hg, and his heart rate was 73 beats per minute. He was awake, in no acute distress, but reported loose stools. Results of cardiac and pulmonary examinations were normal, showing a regular rate and rhythm with no murmurs and clear lungs. There was normal jugular venous pressure and chronic pitting edema of the lower extremities bilaterally.
An abdominal examination revealed positive bowel sounds, a large ventral hernia, which was easily reducible, and a distended abdomen. His BP remained unchanged after IV normal saline 4 L, and urine output was 200 cc over 4 hours, which the care team determined represented adequate resuscitation. An infection workup, including chest X-ray, urinalysis, and blood and urine cultures, was unrevealing. Hemoglobin was stable at 8.5 g/dL (normal range 14-18), and creatinine level 0.66 mg/dL (normal range 0.7-1.2) at baseline. A transthoracic echocardiogram showed impaired diastolic filling suggestive of extrinsic compression of the left ventricle by mediastinal contents (Figure 1). An abdominal X-ray revealed diffuse dilatation of large bowel loops up to 10 cm, causing elevation and rightward shift of the heart (Figure 2A). A computed tomography scan of the abdomen showed total colonic dilatation without obstruction (Figure 2B).
The patient was diagnosed with postoperative ileus and acute colonic pseudo-obstruction. Nasogastric and rectal tubes were placed for decompression, and the patient was placed on nothing by mouth status. By postoperative day 3, his hypotension had resolved and his BP had improved to 111/58 mm Hg. The patient was able to resume a regular diet.
Discussion
We present an unusual case of left ventricular compression leading to hypotension due to acute colonic pseudo-obstruction. Our patient presented with the rare complication of hypotension due to cardiac compression, which we have not previously seen reported in the literature. Analogous instance of cardiac compression may arise from hiatal hernias and diaphragmatic paralysis. 4-6
Management of acute colonic pseudo-obstruction is through nothing by mouth status and abdominal decompression. For more severe cases, neostigmine, colonoscopic decompression, and surgery can be considered.
This surgical complication was diagnosed by internal medicine hospitalist consultants on a surgical comanagement service. In the comanagement model, the surgical specialties of orthopedic surgery, neurosurgery, and podiatry at San Francisco Veterans Affairs Medical Center in California have hospitalists who work with the team as active consultants for the medical care of the patients. Hospitalists develop a unique skill set in which they can anticipate new diagnoses, prevent or identify early complications, and individualize a patient’s postoperative care.7 One study found that a surgical comanagement service was associated with a decrease in the number of patients with at least 1 surgical complication, decrease in length of stay and 30-day readmissions for a medical cause, decreased consultant use, and an average cost savings per patient of about $2,600 to $4,300.8
Conclusions
With the increasing prevalence of hospitalist comanagement services, it is important for surgeons and nonsurgeons alike to recognize acute colonic pseudo-obstruction as a possible surgical complication.
1. Bernardi M, Warrier S, Lynch C, Heriot A. Acute and chronic pseudo-obstruction: a current update. ANZ J Surg. 2015;85(10):709-714. doi:10.1111/ans.13148
2. Norwood MGA, Lykostratis H, Garcea G, Berry DP. Acute colonic pseudo-obstruction following major orthopaedic surgery. Colorectal Dis. 2005;7(5):496-499. doi:10.1111/j.1463-1318.2005.00790.x
3. Vanek VW, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome). An analysis of 400 cases. Dis Colon Rectum. 1986;29(3):203-210. doi:10.1007/BF02555027
4. Devabhandari MP, Khan MA, Hooper TL. Cardiac compression following cardiac surgery due to unrecognised hiatus hernia. Eur J Cardiothoracic Surg. 2007;32(5):813-815. doi:10.1016/j.ejcts.2007.08.002
5. Asti E, Bonavina L, Lombardi M, Bandera F, Secchi F, Guazzi M. Reversibility of cardiopulmonary impairment after laparoscopic repair of large hiatal hernia. Int J Surg Case Rep. 2015;14:33-35. doi:10.1016/j.ijscr.2015.07.005
6. Tayyareci Y, Bayazit P, Taştan CP, Aksoy H. Right atrial compression due to idiopathic right diaphragm paralysis detected incidentally by transthoracic echocardiography. Turk Kardiyol Dern Ars. 2008;36(6):412-414.
7. Rohatgi N, Schulman K, Ahuja N. Comanagement by hospitalists: why it makes clinical and fiscal sense. Am J Med. 2020;133(3):257-258. doi:10.1016/j.amjmed.2019.07.053
8. Rohatgi N, Loftus P, Grujic O, Cullen M, Hopkins J, Ahuja N. Surgical comanagement by hospitalists improves patient outcomes: a propensity score analysis. Ann Surg. 2016;264(2):275-282. doi:10.1097/SLA.0000000000001629
1. Bernardi M, Warrier S, Lynch C, Heriot A. Acute and chronic pseudo-obstruction: a current update. ANZ J Surg. 2015;85(10):709-714. doi:10.1111/ans.13148
2. Norwood MGA, Lykostratis H, Garcea G, Berry DP. Acute colonic pseudo-obstruction following major orthopaedic surgery. Colorectal Dis. 2005;7(5):496-499. doi:10.1111/j.1463-1318.2005.00790.x
3. Vanek VW, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie’s syndrome). An analysis of 400 cases. Dis Colon Rectum. 1986;29(3):203-210. doi:10.1007/BF02555027
4. Devabhandari MP, Khan MA, Hooper TL. Cardiac compression following cardiac surgery due to unrecognised hiatus hernia. Eur J Cardiothoracic Surg. 2007;32(5):813-815. doi:10.1016/j.ejcts.2007.08.002
5. Asti E, Bonavina L, Lombardi M, Bandera F, Secchi F, Guazzi M. Reversibility of cardiopulmonary impairment after laparoscopic repair of large hiatal hernia. Int J Surg Case Rep. 2015;14:33-35. doi:10.1016/j.ijscr.2015.07.005
6. Tayyareci Y, Bayazit P, Taştan CP, Aksoy H. Right atrial compression due to idiopathic right diaphragm paralysis detected incidentally by transthoracic echocardiography. Turk Kardiyol Dern Ars. 2008;36(6):412-414.
7. Rohatgi N, Schulman K, Ahuja N. Comanagement by hospitalists: why it makes clinical and fiscal sense. Am J Med. 2020;133(3):257-258. doi:10.1016/j.amjmed.2019.07.053
8. Rohatgi N, Loftus P, Grujic O, Cullen M, Hopkins J, Ahuja N. Surgical comanagement by hospitalists improves patient outcomes: a propensity score analysis. Ann Surg. 2016;264(2):275-282. doi:10.1097/SLA.0000000000001629
Hospital Medicine Management in the Time of COVID-19: Preparing for a Sprint and a Marathon
The pandemic of coronavirus disease 2019 (COVID-19) is confronting the modern world like nothing else before. With over 20 million individuals expected to require hospitalization in the US, this health crisis may become a generation-defining moment for healthcare systems and the field of hospital medicine.1 The specific challenges facing hospital medicine are comparable to running a sprint and a marathon—at the same time. For the sprint underway, hospitalists must learn to respond to a rapidly changing environment in which critical decisions are made within hours and days. At the same time, hospitalists need to plan for the marathon of increased clinical needs over the coming months, the possibility of burnout, and concerns about staff well-being. Although runners typically focus on either the sprint or the marathon, healthcare systems and hospital medicine providers will need to simultaneously prepare for both types of races.
GET READY FOR THE SPRINT
Over the past several weeks, hospital medicine leaders have been rapidly responding to an evolving crisis. Leaders and clinicians are quickly learning how to restructure clinical operations, negotiate the short supply of personal protective equipment (PPE), and manage delays in COVID-19 testing. In these areas, our hospitalist group has experienced a steep learning curve. In addition to the strategies outlined in the Table, we will share here our experiences and insights on managing and preparing for the COVID-19 pandemic.
Communication Is Central
During the sprint, focused, regular communication is imperative to ameliorate anxiety and fear. A study of crisis communication after 9/11 found that, for employees, good communication from leadership was one of the most valued factors.2 Communications experts also note that, in times of crisis, leaders have a special role in communication, specifically around demystifying the situation, providing hope, and maintaining transparency.3
Mental bandwidth may be limited in a stressful environment, so efforts should be taken to maximize the value of each communication. Information on hospital metrics should be provided regularly, including the number of COVID-19 cases, the status of clinical services and staffing, hospital capacity, and resource availability.4 Although the ubiquity and ease of email is convenient, recognize that providers are likely receiving email updates from multiple layers within your healthcare organization. To guard against losing important information, we use the same templated format for daily email updates with changes highlighted, which allows busy clinicians to digest pertinent information easily.5 Finally, consider having a single individual be responsible for collating COVID-19–related emails sent to your group. Although clinicians may want to share the most recent studies or their clinical experiences with a group email, instead have them send this information to a single individual who can organize these materials and share them on a regular basis.
To keep two-way communication channels open in a busy, asynchronous environment, consider having a centralized shared document in which providers can give real-time feedback to capture on-the-ground experiences or share questions they would like answered. Within our group, we found that centralizing our conversation in a shared document eliminated redundancy, focused our meetings, and kept everyone up to date. Additionally, regularly scheduled meetings may need to be adapted to a remote format (eg, Zoom, WebEx) as clinicians are asked to work from home when not on clinical service. Finally, recognize that virtual meetings require a different skill set than that required by in-person meetings, including reestablishment of social norms and technology preparation.6
Optimize Your Staffing
Hospital volumes could increase to as high as 270% of current hospital bed capacities during this pandemic.1 This surge is further complicated by the effort involved in caring for these patients, given their increased medical complexity, the use of new protocols, and the extra time needed to update staff and family. As the workload intensifies, staffing models and operations will also need to adapt.
First, optimize your inpatient resources based on the changes your hospital system is making. For instance, as elective surgeries were cancelled, we dissolved our surgical comanagement and consult services to better accommodate our hospitals’ needs. Further, consider using advanced practice providers (eg, physician assistants and nurse practitioners) released from their clinical duties to help with inpatient care in the event of a surge. If your hospital has trainees (eg, residents or fellows), consider reassigning those whose rotations have been postponed to newly created inpatient teams; trainees often have strong institutional knowledge and understanding of hospital protocols and resources.
Second, use hospitalists for their most relevant skills. Hospitalists are pluripotent clinicians who are comfortable with high-acuity patients and can fit into a myriad of clinical positions. The initial instinct at our institution was to mobilize hospitalists across all areas of increasing needs in the hospital (eg, screening clinics,7 advice phone lines for patients, or in the Emergency Department), but we quickly recognized that the hospitalist group is a finite resource. We focused our hospitalists’ clinical work on the expanding inpatient needs and allowed other outpatient or procedure-based specialties that have less inpatient experience to fill the broader institutional gaps.
Finally, consider long-term implications of staffing decisions. Leaders are making challenging coverage decisions that can affect the morale and autonomy of staff. Does backup staffing happen on a volunteer basis? Who fills the need—those with less clinical time or those with fewer personal obligations? When a staffing model is challenged and your group is making such decisions, engaged communication again becomes paramount.
PREPARE FOR THE MARATHON
Experts believe that we are only at the beginning of this crisis, one for which we don’t know what the end looks like or when it will come. With this in mind, hospital medicine leadership must plan for the long-term implications of the lengthy race ahead. Recognizing that morale, motivation, and burnout will be issues to deal with on the horizon, a focus on sustainability and wellness will become increasingly important as the marathon continues. To date, we’ve found the following principles to be helpful.
Delegate Responsibilities
Hospitals will not be able to survive COVID-19 through the efforts of single individuals. Instead, consider creating “operational champion” roles for frontline clinicians. These individuals can lead in specific areas (eg, PPE, updates on COVID-19 testing, discharge protocols) and act as conduits for information, updates, and resources for your group. At our institution, such operational meetings and activities take hours out of each day. By creating a breadth of leadership roles, our group has spread the operational workload while still allowing clinicians to care for patients, avoid burnout, and build autonomy and opportunities for both personal and professional growth. While for most institutions, these positions are temporary and not compensated with salary or time, the contribution to the group should be recognized both now and in the future.
Focus on Wellness
Providers are battling a laundry list of both clinical and personal stressors. The Centers for Disease Control and Prevention has already recognized that stress and mental health are going to be large hurdles for both patients and providers during this crisis.8 From the beginning, hospitalist leadership should be attuned to physician wellness and be aware that burnout, mental and physical exhaustion, and the possibility of contracting COVID-19 will be issues in the coming weeks and months. Volunteerism is built into the physician’s work ethic, but we must be mindful about its cost for long-term staffing demands. In addition, scarce medical resources add an additional moral strain for clinicians as they face tough allocation decisions, as we’ve seen with our Italian colleagues.9
As regular meetings around COVID-19 have become commonplace, we’ve made sure to set aside defined time for staff to discuss and reflect on their experiences. Doing so has allowed our clinicians to feel heard and to acknowledge the difficulties they are facing in their clinical duties. Leaders should also consider frequent check-ins with individual providers. At our institution, the first positive COVID-19 patient did not radically change any protocol that was in place, but a check-in with the hospitalist on service that day proved helpful for a debrief and processing opportunity. Individual conversations can help those on the front lines feel supported and remind them they are not operating alone in an anonymous vacuum.
Continue by celebrating small victories because this marathon is not going to end with an obvious finish line or a singular moment in which everyone can rejoice. A negative test, a patient with a good outcome, and a donation of PPE are all opportunities to celebrate. It may be what keeps us going when there is no end in sight. We have relied on these celebrations and moments of levity as an integral part of our regular group meetings.
CONCLUSION
At the end of this pandemic, just as we hope that our social distancing feels like an overreaction, we similarly hope that our sprint to build capacity ends up being unnecessary as well. As we wrote this Perspectives piece, uncertainty about the extent, length, and impact of this pandemic still existed. By the time it is published it may be that the sprint is over, and the marathon is beginning. Or, if our wildest hopes come true, there will be no marathon to run at all.
1. Tsai TC, Jacobson BH, Jha AK. American Hospital Capacity and Projected Need for COVID-19. Health Affairs. March 17, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/. Accessed April 1, 2020.
2. Argenti PA. Crisis communication: lessons from 9/11. Harvard Business Review. December 2002. https://hbr.org/2002/12/crisis-communication-lessons-from-911. Accessed April 2, 2020.
3. Argenti PA. Communicating through the coronavirus crisis. Harvard Business Review. March 2020. https://hbr.org/2020/03/communicating-through-the-coronavirus-crisis. Accessed April 2, 2020.
4. Chopra V, Toner E, Waldhorn R, Washer L. How should US hospitals prepare for COVID-19? Ann Intern Med. 2020. https://doi.org/10.7326/M20-0907.
5. National Institutes of Health. Formatting and Visual Clarity. Published July 1, 2015. Updated March 27, 2017. https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/plain-language/formatting-visual-clarity. Accessed April 2, 2020.
6. Frisch B, Greene C. What it takes to run a great virtual meeting. Harvard Business Review. March 2020. https://hbr.org/2020/03/what-it-takes-to-run-a-great-virtual-meeting. Accessed April 2, 2020.
7. Yan W. Coronavirus testing goes mobile in Seattle. New York Times. March 13, 2020. https://www.nytimes.com/2020/03/13/us/coronavirus-testing-drive-through-seattle.html. Accessed April 2, 2020.
8. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Stress and Coping. February 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prepare/managing-stress-anxiety.html. Accessed April 2, 2020.
9. Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020. https://doi.org/10.1056/NEJMp2005492.
The pandemic of coronavirus disease 2019 (COVID-19) is confronting the modern world like nothing else before. With over 20 million individuals expected to require hospitalization in the US, this health crisis may become a generation-defining moment for healthcare systems and the field of hospital medicine.1 The specific challenges facing hospital medicine are comparable to running a sprint and a marathon—at the same time. For the sprint underway, hospitalists must learn to respond to a rapidly changing environment in which critical decisions are made within hours and days. At the same time, hospitalists need to plan for the marathon of increased clinical needs over the coming months, the possibility of burnout, and concerns about staff well-being. Although runners typically focus on either the sprint or the marathon, healthcare systems and hospital medicine providers will need to simultaneously prepare for both types of races.
GET READY FOR THE SPRINT
Over the past several weeks, hospital medicine leaders have been rapidly responding to an evolving crisis. Leaders and clinicians are quickly learning how to restructure clinical operations, negotiate the short supply of personal protective equipment (PPE), and manage delays in COVID-19 testing. In these areas, our hospitalist group has experienced a steep learning curve. In addition to the strategies outlined in the Table, we will share here our experiences and insights on managing and preparing for the COVID-19 pandemic.
Communication Is Central
During the sprint, focused, regular communication is imperative to ameliorate anxiety and fear. A study of crisis communication after 9/11 found that, for employees, good communication from leadership was one of the most valued factors.2 Communications experts also note that, in times of crisis, leaders have a special role in communication, specifically around demystifying the situation, providing hope, and maintaining transparency.3
Mental bandwidth may be limited in a stressful environment, so efforts should be taken to maximize the value of each communication. Information on hospital metrics should be provided regularly, including the number of COVID-19 cases, the status of clinical services and staffing, hospital capacity, and resource availability.4 Although the ubiquity and ease of email is convenient, recognize that providers are likely receiving email updates from multiple layers within your healthcare organization. To guard against losing important information, we use the same templated format for daily email updates with changes highlighted, which allows busy clinicians to digest pertinent information easily.5 Finally, consider having a single individual be responsible for collating COVID-19–related emails sent to your group. Although clinicians may want to share the most recent studies or their clinical experiences with a group email, instead have them send this information to a single individual who can organize these materials and share them on a regular basis.
To keep two-way communication channels open in a busy, asynchronous environment, consider having a centralized shared document in which providers can give real-time feedback to capture on-the-ground experiences or share questions they would like answered. Within our group, we found that centralizing our conversation in a shared document eliminated redundancy, focused our meetings, and kept everyone up to date. Additionally, regularly scheduled meetings may need to be adapted to a remote format (eg, Zoom, WebEx) as clinicians are asked to work from home when not on clinical service. Finally, recognize that virtual meetings require a different skill set than that required by in-person meetings, including reestablishment of social norms and technology preparation.6
Optimize Your Staffing
Hospital volumes could increase to as high as 270% of current hospital bed capacities during this pandemic.1 This surge is further complicated by the effort involved in caring for these patients, given their increased medical complexity, the use of new protocols, and the extra time needed to update staff and family. As the workload intensifies, staffing models and operations will also need to adapt.
First, optimize your inpatient resources based on the changes your hospital system is making. For instance, as elective surgeries were cancelled, we dissolved our surgical comanagement and consult services to better accommodate our hospitals’ needs. Further, consider using advanced practice providers (eg, physician assistants and nurse practitioners) released from their clinical duties to help with inpatient care in the event of a surge. If your hospital has trainees (eg, residents or fellows), consider reassigning those whose rotations have been postponed to newly created inpatient teams; trainees often have strong institutional knowledge and understanding of hospital protocols and resources.
Second, use hospitalists for their most relevant skills. Hospitalists are pluripotent clinicians who are comfortable with high-acuity patients and can fit into a myriad of clinical positions. The initial instinct at our institution was to mobilize hospitalists across all areas of increasing needs in the hospital (eg, screening clinics,7 advice phone lines for patients, or in the Emergency Department), but we quickly recognized that the hospitalist group is a finite resource. We focused our hospitalists’ clinical work on the expanding inpatient needs and allowed other outpatient or procedure-based specialties that have less inpatient experience to fill the broader institutional gaps.
Finally, consider long-term implications of staffing decisions. Leaders are making challenging coverage decisions that can affect the morale and autonomy of staff. Does backup staffing happen on a volunteer basis? Who fills the need—those with less clinical time or those with fewer personal obligations? When a staffing model is challenged and your group is making such decisions, engaged communication again becomes paramount.
PREPARE FOR THE MARATHON
Experts believe that we are only at the beginning of this crisis, one for which we don’t know what the end looks like or when it will come. With this in mind, hospital medicine leadership must plan for the long-term implications of the lengthy race ahead. Recognizing that morale, motivation, and burnout will be issues to deal with on the horizon, a focus on sustainability and wellness will become increasingly important as the marathon continues. To date, we’ve found the following principles to be helpful.
Delegate Responsibilities
Hospitals will not be able to survive COVID-19 through the efforts of single individuals. Instead, consider creating “operational champion” roles for frontline clinicians. These individuals can lead in specific areas (eg, PPE, updates on COVID-19 testing, discharge protocols) and act as conduits for information, updates, and resources for your group. At our institution, such operational meetings and activities take hours out of each day. By creating a breadth of leadership roles, our group has spread the operational workload while still allowing clinicians to care for patients, avoid burnout, and build autonomy and opportunities for both personal and professional growth. While for most institutions, these positions are temporary and not compensated with salary or time, the contribution to the group should be recognized both now and in the future.
Focus on Wellness
Providers are battling a laundry list of both clinical and personal stressors. The Centers for Disease Control and Prevention has already recognized that stress and mental health are going to be large hurdles for both patients and providers during this crisis.8 From the beginning, hospitalist leadership should be attuned to physician wellness and be aware that burnout, mental and physical exhaustion, and the possibility of contracting COVID-19 will be issues in the coming weeks and months. Volunteerism is built into the physician’s work ethic, but we must be mindful about its cost for long-term staffing demands. In addition, scarce medical resources add an additional moral strain for clinicians as they face tough allocation decisions, as we’ve seen with our Italian colleagues.9
As regular meetings around COVID-19 have become commonplace, we’ve made sure to set aside defined time for staff to discuss and reflect on their experiences. Doing so has allowed our clinicians to feel heard and to acknowledge the difficulties they are facing in their clinical duties. Leaders should also consider frequent check-ins with individual providers. At our institution, the first positive COVID-19 patient did not radically change any protocol that was in place, but a check-in with the hospitalist on service that day proved helpful for a debrief and processing opportunity. Individual conversations can help those on the front lines feel supported and remind them they are not operating alone in an anonymous vacuum.
Continue by celebrating small victories because this marathon is not going to end with an obvious finish line or a singular moment in which everyone can rejoice. A negative test, a patient with a good outcome, and a donation of PPE are all opportunities to celebrate. It may be what keeps us going when there is no end in sight. We have relied on these celebrations and moments of levity as an integral part of our regular group meetings.
CONCLUSION
At the end of this pandemic, just as we hope that our social distancing feels like an overreaction, we similarly hope that our sprint to build capacity ends up being unnecessary as well. As we wrote this Perspectives piece, uncertainty about the extent, length, and impact of this pandemic still existed. By the time it is published it may be that the sprint is over, and the marathon is beginning. Or, if our wildest hopes come true, there will be no marathon to run at all.
The pandemic of coronavirus disease 2019 (COVID-19) is confronting the modern world like nothing else before. With over 20 million individuals expected to require hospitalization in the US, this health crisis may become a generation-defining moment for healthcare systems and the field of hospital medicine.1 The specific challenges facing hospital medicine are comparable to running a sprint and a marathon—at the same time. For the sprint underway, hospitalists must learn to respond to a rapidly changing environment in which critical decisions are made within hours and days. At the same time, hospitalists need to plan for the marathon of increased clinical needs over the coming months, the possibility of burnout, and concerns about staff well-being. Although runners typically focus on either the sprint or the marathon, healthcare systems and hospital medicine providers will need to simultaneously prepare for both types of races.
GET READY FOR THE SPRINT
Over the past several weeks, hospital medicine leaders have been rapidly responding to an evolving crisis. Leaders and clinicians are quickly learning how to restructure clinical operations, negotiate the short supply of personal protective equipment (PPE), and manage delays in COVID-19 testing. In these areas, our hospitalist group has experienced a steep learning curve. In addition to the strategies outlined in the Table, we will share here our experiences and insights on managing and preparing for the COVID-19 pandemic.
Communication Is Central
During the sprint, focused, regular communication is imperative to ameliorate anxiety and fear. A study of crisis communication after 9/11 found that, for employees, good communication from leadership was one of the most valued factors.2 Communications experts also note that, in times of crisis, leaders have a special role in communication, specifically around demystifying the situation, providing hope, and maintaining transparency.3
Mental bandwidth may be limited in a stressful environment, so efforts should be taken to maximize the value of each communication. Information on hospital metrics should be provided regularly, including the number of COVID-19 cases, the status of clinical services and staffing, hospital capacity, and resource availability.4 Although the ubiquity and ease of email is convenient, recognize that providers are likely receiving email updates from multiple layers within your healthcare organization. To guard against losing important information, we use the same templated format for daily email updates with changes highlighted, which allows busy clinicians to digest pertinent information easily.5 Finally, consider having a single individual be responsible for collating COVID-19–related emails sent to your group. Although clinicians may want to share the most recent studies or their clinical experiences with a group email, instead have them send this information to a single individual who can organize these materials and share them on a regular basis.
To keep two-way communication channels open in a busy, asynchronous environment, consider having a centralized shared document in which providers can give real-time feedback to capture on-the-ground experiences or share questions they would like answered. Within our group, we found that centralizing our conversation in a shared document eliminated redundancy, focused our meetings, and kept everyone up to date. Additionally, regularly scheduled meetings may need to be adapted to a remote format (eg, Zoom, WebEx) as clinicians are asked to work from home when not on clinical service. Finally, recognize that virtual meetings require a different skill set than that required by in-person meetings, including reestablishment of social norms and technology preparation.6
Optimize Your Staffing
Hospital volumes could increase to as high as 270% of current hospital bed capacities during this pandemic.1 This surge is further complicated by the effort involved in caring for these patients, given their increased medical complexity, the use of new protocols, and the extra time needed to update staff and family. As the workload intensifies, staffing models and operations will also need to adapt.
First, optimize your inpatient resources based on the changes your hospital system is making. For instance, as elective surgeries were cancelled, we dissolved our surgical comanagement and consult services to better accommodate our hospitals’ needs. Further, consider using advanced practice providers (eg, physician assistants and nurse practitioners) released from their clinical duties to help with inpatient care in the event of a surge. If your hospital has trainees (eg, residents or fellows), consider reassigning those whose rotations have been postponed to newly created inpatient teams; trainees often have strong institutional knowledge and understanding of hospital protocols and resources.
Second, use hospitalists for their most relevant skills. Hospitalists are pluripotent clinicians who are comfortable with high-acuity patients and can fit into a myriad of clinical positions. The initial instinct at our institution was to mobilize hospitalists across all areas of increasing needs in the hospital (eg, screening clinics,7 advice phone lines for patients, or in the Emergency Department), but we quickly recognized that the hospitalist group is a finite resource. We focused our hospitalists’ clinical work on the expanding inpatient needs and allowed other outpatient or procedure-based specialties that have less inpatient experience to fill the broader institutional gaps.
Finally, consider long-term implications of staffing decisions. Leaders are making challenging coverage decisions that can affect the morale and autonomy of staff. Does backup staffing happen on a volunteer basis? Who fills the need—those with less clinical time or those with fewer personal obligations? When a staffing model is challenged and your group is making such decisions, engaged communication again becomes paramount.
PREPARE FOR THE MARATHON
Experts believe that we are only at the beginning of this crisis, one for which we don’t know what the end looks like or when it will come. With this in mind, hospital medicine leadership must plan for the long-term implications of the lengthy race ahead. Recognizing that morale, motivation, and burnout will be issues to deal with on the horizon, a focus on sustainability and wellness will become increasingly important as the marathon continues. To date, we’ve found the following principles to be helpful.
Delegate Responsibilities
Hospitals will not be able to survive COVID-19 through the efforts of single individuals. Instead, consider creating “operational champion” roles for frontline clinicians. These individuals can lead in specific areas (eg, PPE, updates on COVID-19 testing, discharge protocols) and act as conduits for information, updates, and resources for your group. At our institution, such operational meetings and activities take hours out of each day. By creating a breadth of leadership roles, our group has spread the operational workload while still allowing clinicians to care for patients, avoid burnout, and build autonomy and opportunities for both personal and professional growth. While for most institutions, these positions are temporary and not compensated with salary or time, the contribution to the group should be recognized both now and in the future.
Focus on Wellness
Providers are battling a laundry list of both clinical and personal stressors. The Centers for Disease Control and Prevention has already recognized that stress and mental health are going to be large hurdles for both patients and providers during this crisis.8 From the beginning, hospitalist leadership should be attuned to physician wellness and be aware that burnout, mental and physical exhaustion, and the possibility of contracting COVID-19 will be issues in the coming weeks and months. Volunteerism is built into the physician’s work ethic, but we must be mindful about its cost for long-term staffing demands. In addition, scarce medical resources add an additional moral strain for clinicians as they face tough allocation decisions, as we’ve seen with our Italian colleagues.9
As regular meetings around COVID-19 have become commonplace, we’ve made sure to set aside defined time for staff to discuss and reflect on their experiences. Doing so has allowed our clinicians to feel heard and to acknowledge the difficulties they are facing in their clinical duties. Leaders should also consider frequent check-ins with individual providers. At our institution, the first positive COVID-19 patient did not radically change any protocol that was in place, but a check-in with the hospitalist on service that day proved helpful for a debrief and processing opportunity. Individual conversations can help those on the front lines feel supported and remind them they are not operating alone in an anonymous vacuum.
Continue by celebrating small victories because this marathon is not going to end with an obvious finish line or a singular moment in which everyone can rejoice. A negative test, a patient with a good outcome, and a donation of PPE are all opportunities to celebrate. It may be what keeps us going when there is no end in sight. We have relied on these celebrations and moments of levity as an integral part of our regular group meetings.
CONCLUSION
At the end of this pandemic, just as we hope that our social distancing feels like an overreaction, we similarly hope that our sprint to build capacity ends up being unnecessary as well. As we wrote this Perspectives piece, uncertainty about the extent, length, and impact of this pandemic still existed. By the time it is published it may be that the sprint is over, and the marathon is beginning. Or, if our wildest hopes come true, there will be no marathon to run at all.
1. Tsai TC, Jacobson BH, Jha AK. American Hospital Capacity and Projected Need for COVID-19. Health Affairs. March 17, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/. Accessed April 1, 2020.
2. Argenti PA. Crisis communication: lessons from 9/11. Harvard Business Review. December 2002. https://hbr.org/2002/12/crisis-communication-lessons-from-911. Accessed April 2, 2020.
3. Argenti PA. Communicating through the coronavirus crisis. Harvard Business Review. March 2020. https://hbr.org/2020/03/communicating-through-the-coronavirus-crisis. Accessed April 2, 2020.
4. Chopra V, Toner E, Waldhorn R, Washer L. How should US hospitals prepare for COVID-19? Ann Intern Med. 2020. https://doi.org/10.7326/M20-0907.
5. National Institutes of Health. Formatting and Visual Clarity. Published July 1, 2015. Updated March 27, 2017. https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/plain-language/formatting-visual-clarity. Accessed April 2, 2020.
6. Frisch B, Greene C. What it takes to run a great virtual meeting. Harvard Business Review. March 2020. https://hbr.org/2020/03/what-it-takes-to-run-a-great-virtual-meeting. Accessed April 2, 2020.
7. Yan W. Coronavirus testing goes mobile in Seattle. New York Times. March 13, 2020. https://www.nytimes.com/2020/03/13/us/coronavirus-testing-drive-through-seattle.html. Accessed April 2, 2020.
8. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Stress and Coping. February 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prepare/managing-stress-anxiety.html. Accessed April 2, 2020.
9. Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020. https://doi.org/10.1056/NEJMp2005492.
1. Tsai TC, Jacobson BH, Jha AK. American Hospital Capacity and Projected Need for COVID-19. Health Affairs. March 17, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/. Accessed April 1, 2020.
2. Argenti PA. Crisis communication: lessons from 9/11. Harvard Business Review. December 2002. https://hbr.org/2002/12/crisis-communication-lessons-from-911. Accessed April 2, 2020.
3. Argenti PA. Communicating through the coronavirus crisis. Harvard Business Review. March 2020. https://hbr.org/2020/03/communicating-through-the-coronavirus-crisis. Accessed April 2, 2020.
4. Chopra V, Toner E, Waldhorn R, Washer L. How should US hospitals prepare for COVID-19? Ann Intern Med. 2020. https://doi.org/10.7326/M20-0907.
5. National Institutes of Health. Formatting and Visual Clarity. Published July 1, 2015. Updated March 27, 2017. https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/plain-language/formatting-visual-clarity. Accessed April 2, 2020.
6. Frisch B, Greene C. What it takes to run a great virtual meeting. Harvard Business Review. March 2020. https://hbr.org/2020/03/what-it-takes-to-run-a-great-virtual-meeting. Accessed April 2, 2020.
7. Yan W. Coronavirus testing goes mobile in Seattle. New York Times. March 13, 2020. https://www.nytimes.com/2020/03/13/us/coronavirus-testing-drive-through-seattle.html. Accessed April 2, 2020.
8. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Stress and Coping. February 11, 2020. https://www.cdc.gov/coronavirus/2019-ncov/prepare/managing-stress-anxiety.html. Accessed April 2, 2020.
9. Rosenbaum L. Facing Covid-19 in Italy—ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020. https://doi.org/10.1056/NEJMp2005492.
© 2020 Society of Hospital Medicine