User login
Tuberculous Cellulitis: Diseases Behind Cellulitislike Erythema
Local tender erythema is a typical manifestation of cellulitis, which is commonly seen by dermatologists; however, cutaneous manifestations of other diseases may bear resemblance to the more banal cellulitis. We present the case of a patient with tuberculous cellulitis, a rare variant of cutaneous tuberculosis.
Case Report
An 89-year-old man presented to a local primary care physician with a fever (temperature, 38°C). Infectious disease was suspected. Antibiotic therapy with oral cefaclor and intravenous cefotiam hydrochloride was started, but the patient’s fever did not subside. Six days after initiation of treatment, he was referred to our dermatology department for evaluation of a painful erythematous rash on the left thigh that had suddenly appeared. The patient had a history of pulmonary tuberculosis 71 years prior. He also underwent surgical treatment of pancreatic cancer 14 years prior. Additionally, he had chronic kidney disease (CKD) and polymyalgia rheumatica, which was currently being treated with oral prednisolone 5 mg once daily.
Physical examination revealed a hot and tender erythematous plaque on the left thigh (Figure 1). The edge of the lesion was not well defined and there was no regional lymphadenopathy.

A complete blood cell count revealed anemia (white blood cell count, 8070/μL [reference range, 4000–9,000/μL]; neutrophils, 77.1% [reference range, 44%–74%]; lymphocytes, 13.8% [reference range, 20%–50%]; hemoglobin, 9.3 g/dL [reference range, 13.0–17.0 g/dL]; and platelet count, 329×103/μL [reference range, 150–400×103/μL]). The C-reactive protein level was 7.3 mg/dL (reference range, 0.08–0.3 mg/dL). The creatinine level was 2.93 mg/dL (reference range, 0.6–1.2 mg/dL). There were no signs of liver dysfunction.
A blood culture was negative. A purified protein derivative (tuberculin) skin test was negative (6×7 mm [reference range, ≤9 mm). A chest computed tomography (CT) scan showed small centrilobular nodules that had not changed in number or size since evaluation 3 months prior.
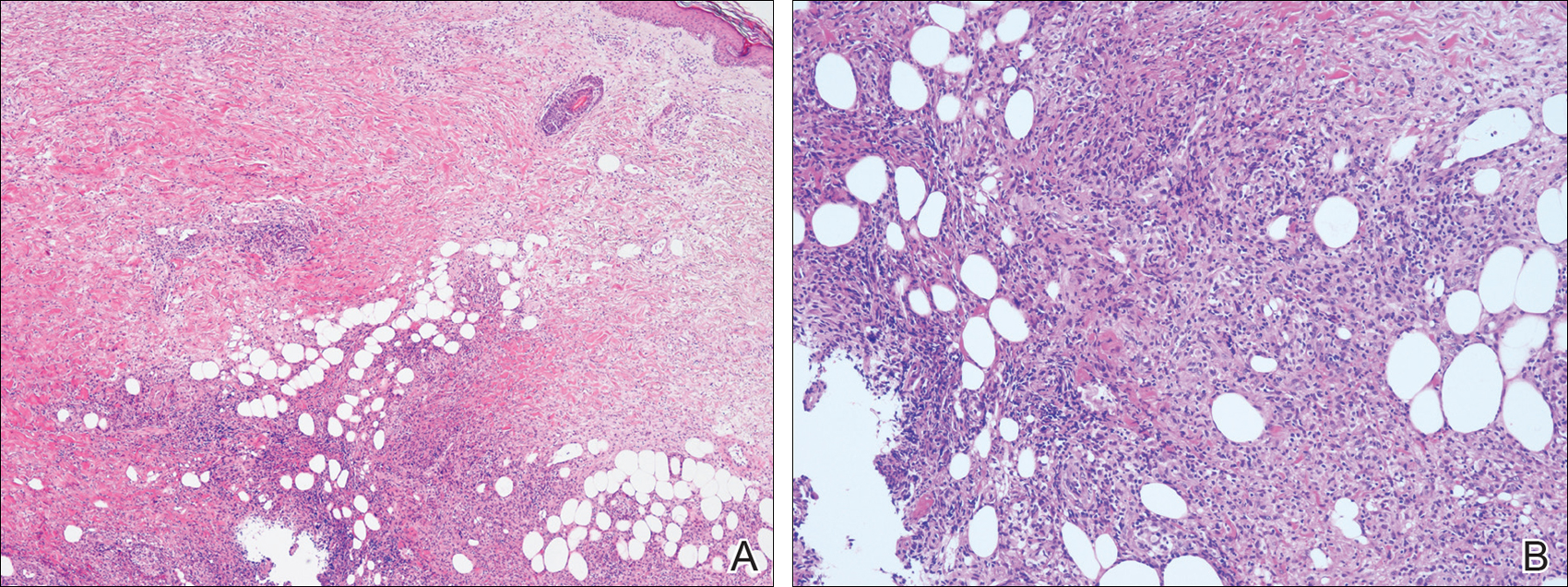
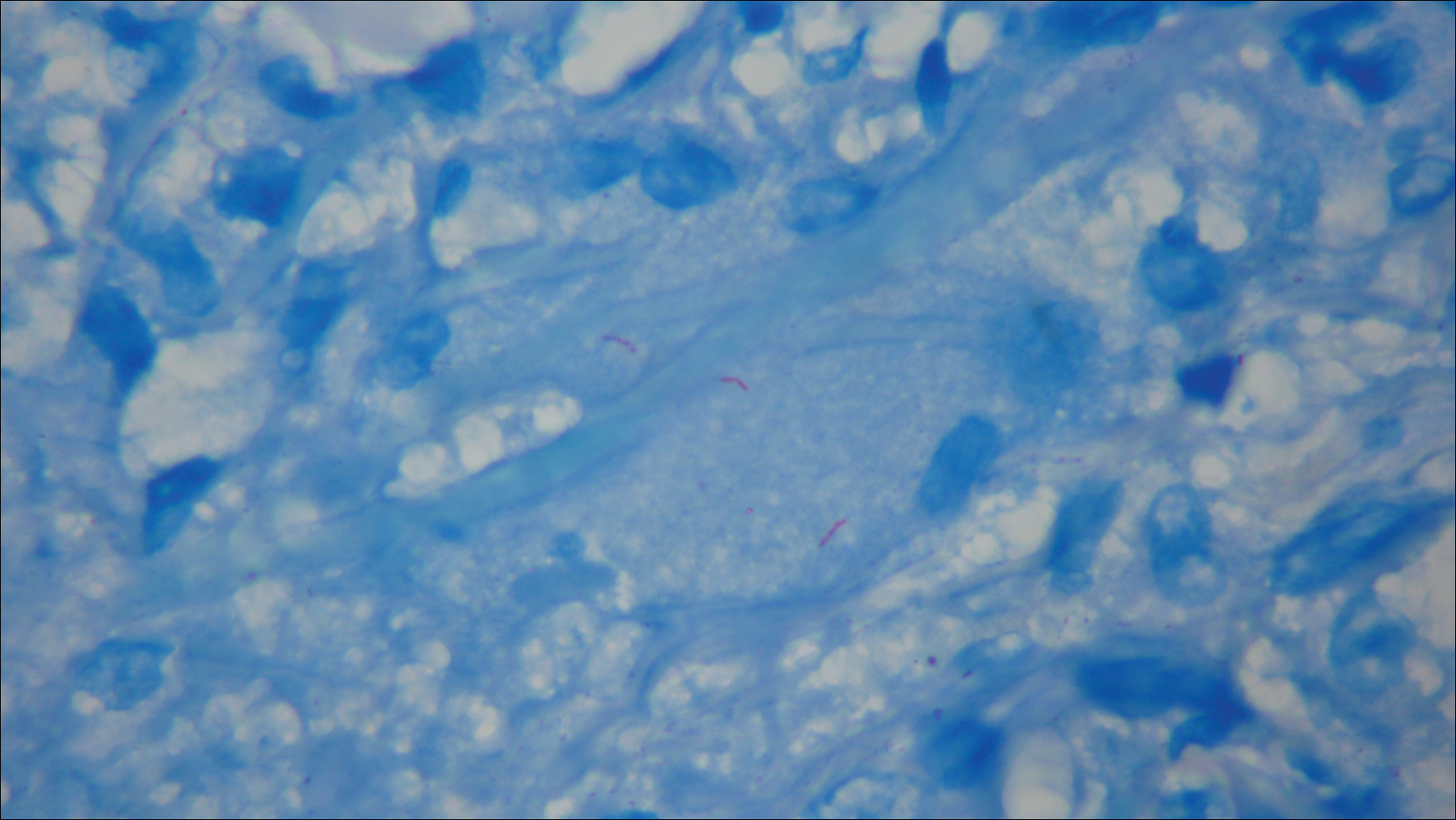
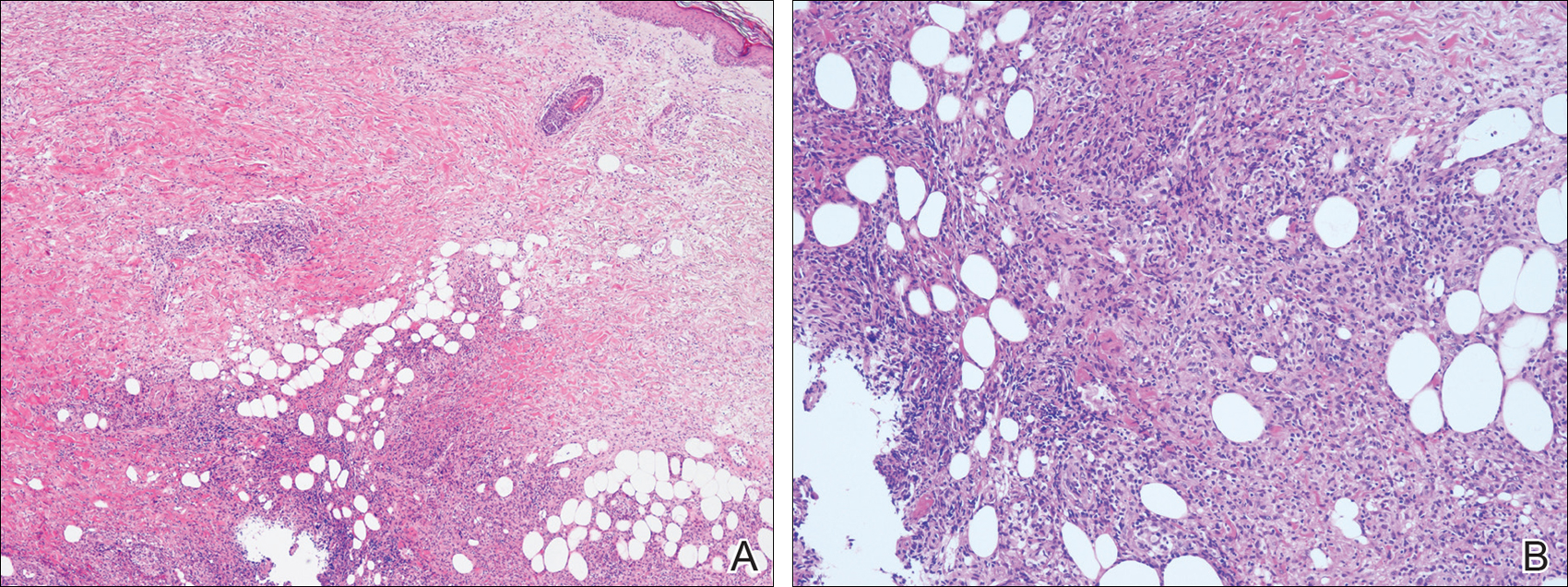
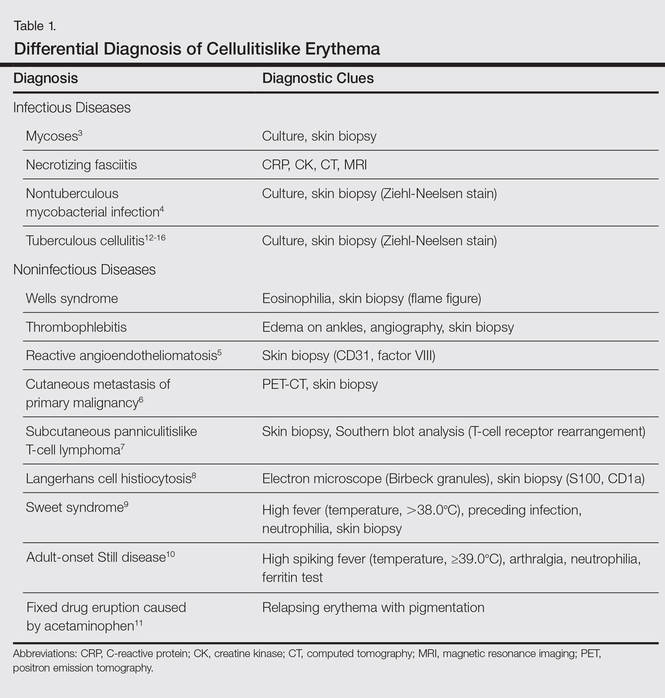
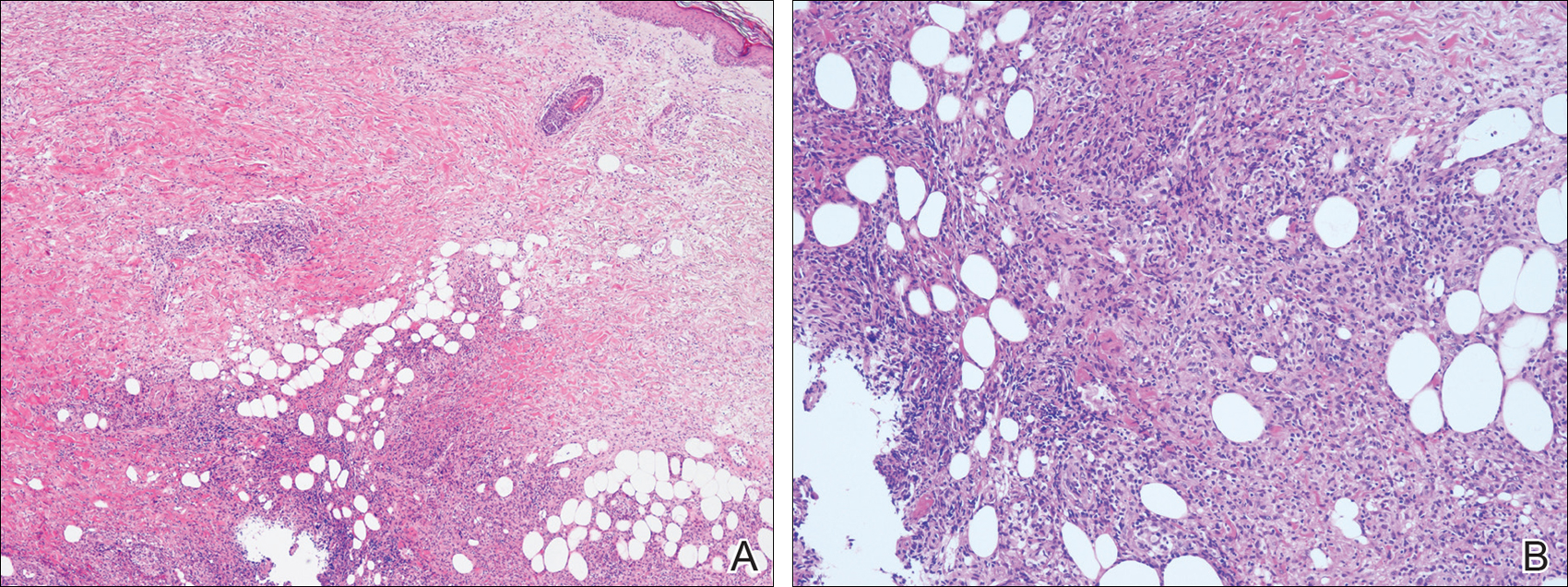
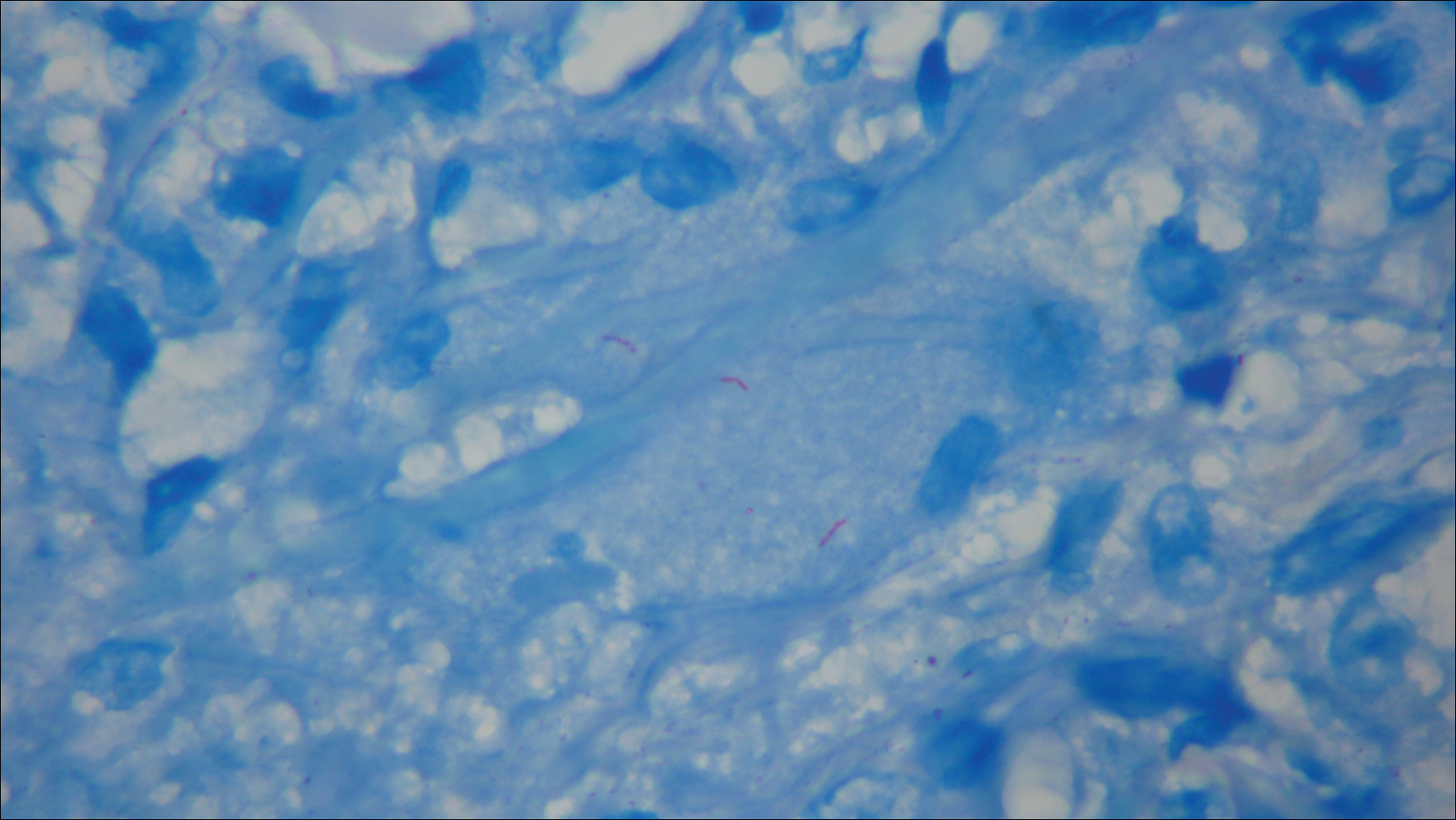
The antibiotics were changed to meropenem hydrate 0.5 g and clindamycin 300 mg twice daily for presumed bacterial cellulitis, then meropenem hydrate 1 g and clindamycin 600 mg daily, but there was still no improvement after about 1 week. Therefore, a skin biopsy was performed on the left thigh. The specimen showed epithelioid cell granulomas throughout the dermis and subcutis (Figure 2). Ziehl-Neelsen stain revealed numerous acid-fast bacilli (Figure 3). Polymerase chain reaction was positive for Mycobacterium tuberculosis in the skin biopsy specimen and gastric fluid. Additionally, M tuberculosis was isolated from the skin biopsy specimen, gastric fluid, and sputum culture. After the series of treatments described above, a remarkable increase in nodule size and number was observed in a follow-up chest CT scan compared with the prior examination. These pulmonary lesions showed bronchogenic spread.
A diagnosis of tuberculous cellulitis with pulmonary tuberculosis was made. Treatment with isoniazid 200 mg once daily, rifampin 300 mg once daily, and ethambutol 500 mg once every other day was started; the dosages were reduced from the standard dose due to the patient’s CKD.1 Four days after initiation of these medications, the patient was transferred to a hospital specifically for the treatment of tuberculosis. Approximately 8 months after treatment with isoniazid, rifampin, and ethambutol, M tuberculosis could not be detected in the sputum and a chest CT revealed that the pulmonary lesions were remarkably improved. However, polymerase chain reaction of the skin biopsy specimen was still positive for M tuberculosis. It was determined that debridement of the skin lesion was needed, but the patient died from complications of deteriorating CKD 10 months after the initiation of the antituberculosis medications.
Comment
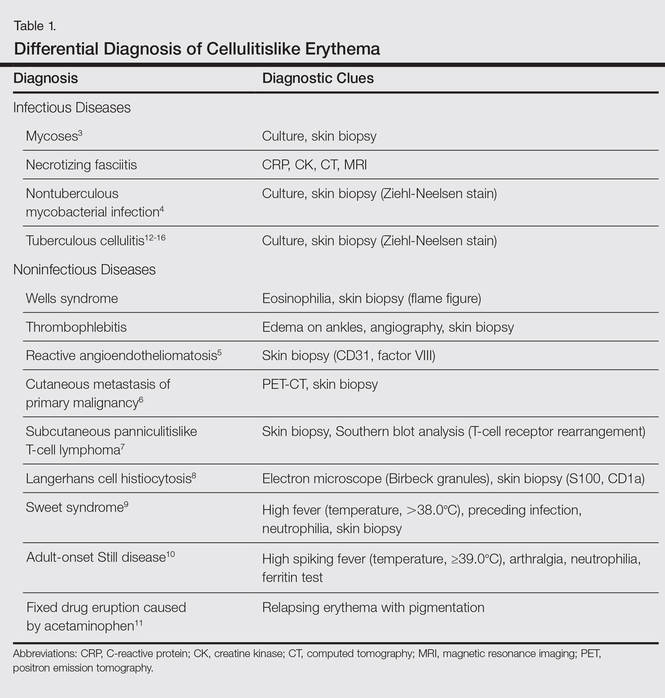
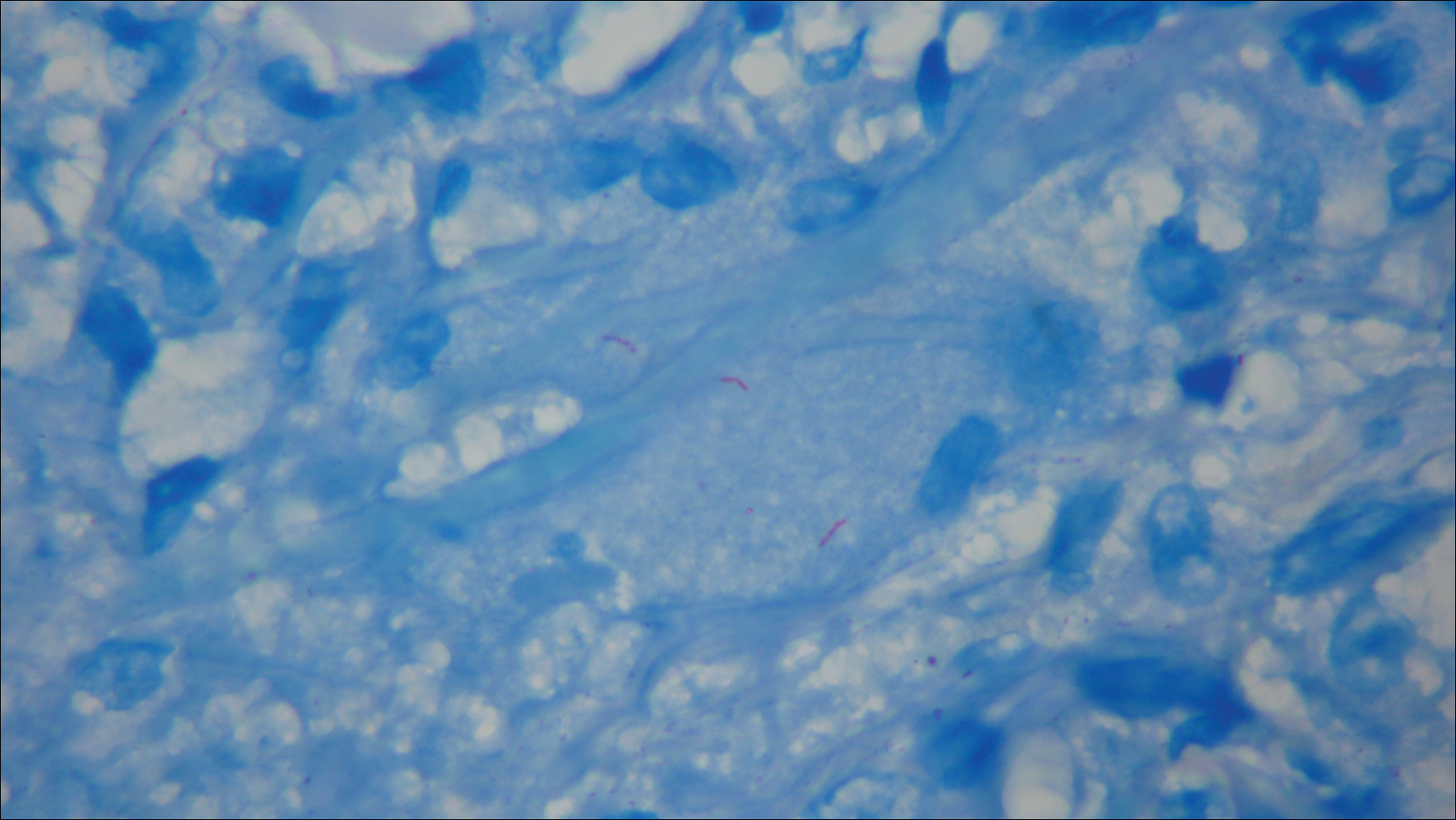
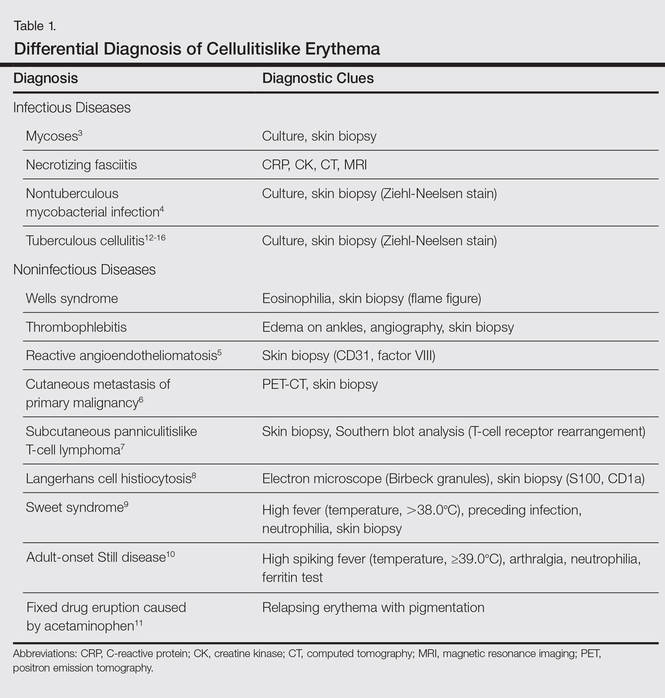
Cellulitis is a suppurative inflammation involving the subcutis.2 Local tender erythema, malaise, chills, and fever may be present at the onset. Cellulitis is commonly seen by dermatologists, and it is well known that other infectious diseases such as necrotizing fasciitis, cutaneous and subcutaneous mycoses,3 and nontuberculous mycobacterial infections4 sometimes present as cellulitislike skin lesions. Moreover, noninfectious diseases, such as Wells syndrome, thrombophlebitis, reactive angioendotheliomatosis,5 cutaneous metastasis of a primary malignancy,6 subcutaneous panniculitislike T-cell lymphoma,7 Langerhans cell histiocytosis,8 Sweet syndrome,9 adult-onset Still disease,10 and fixed drug eruption caused by acetaminophen11 should be excluded. These differential diagnoses and diagnostic clues of cellulitislike erythema are summarized in Table 1.3-16
Cutaneous tuberculosis presenting as cellulitis, so-called tuberculous cellulitis, also is characterized as a clinical mimicker of cellulitis. On the other hand, histologically, it has features of cutaneous tuberculosis (eg, necrotic granuloma).12,14,15 Tuberculous cellulitis is rare and therefore may often be misdiagnosed even in highly endemic areas. We summarized the clinical information of 5 well-documented cases of tuberculous cellulitis along with the current case in Table 2.12-16 All of these cases had an associated disease and involved patients who were currently taking oral corticosteroids. If a patient undergoing immunosuppressive therapy develops cellulitislike erythema, tuberculous cellulitis should be considered in the differential diagnosis.

Cutaneous tuberculosis generally is classified into 4 types according to the mechanism of disease acquisition: (1) inoculation from an exogenous source, (2) endogenous cutaneous spread contiguously or by autoinoculation, (3) hematogenous spread to the skin, and (4) tuberculids. In our case, it was suspected that the cellulitislike erythema may have been caused by hematogenous spread from pulmonary tuberculosis. Considering that negative reactions to purified protein derivative (tuberculin) skin tests often are observed in cases of miliary tuberculosis (widespread dissemination of M tuberculosis to 2 or more organs via hematogenous spread), we suspected that our patient could proceed to miliary tuberculosis; in fact, a case was reported in which miliary tuberculosis emerged approximately 3 weeks after the onset of erythema,13 as observed in the present case. Therefore, erythema in the setting of tuberculosis may be a predictor of miliary tuberculosis. The types of cutaneous lesions caused by tuberculosis infection also are dependent on multiple host factors.2 Cutaneous tuberculosis with an atypical clinical appearance has become more common because of the increasing number of immunocompromised patients.17
In addition, most cases of cutaneous tuberculosis are not associated with pain. Generally, tuberculous cellulitis also causes nontender erythematous plaques or nodules.2 However, in some cases of tuberculous cellulitis, including our case, tender skin lesions have been reported.12-14 Therefore, this symptom is not a sensitive factor for differential diagnosis.
We suggest that tuberculous cellulitis should always be included in the differential diagnosis of a cellulitislike rash with or without pain if the skin lesion is not improved despite antibiotic therapy.
- Daido-Horiuchi Y, Kikuchi Y, Kobayashi S, et al. Tuberculous cellulitis in a patient with chronic kidney disease and polymyalgia rheumatica. Intern Med. 2012;51:3203-3206.
- James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin. 11th ed. Philadelphia, PA: Saunders Elsevier; 2011:322-329.
- Schupbach CW, Wheeler CE Jr, Briggaman RA, et al. Cutaneous manifestations of disseminated cryptococcosis. Arch Dermatol. 1976;112:1734-1740.
- Hsu PY, Yang YH, Hsiao CH, et al. Mycobacterium kansasii infection presenting as cellulitis in a patient with systemic lupus erythematosus. J Formos Med Assoc. 2002;101:581-584.
- Aguayo-Leiva I, Vano-Galván S, Salguero I, et al. Reactive angioendotheliomatosis in a patient with myelodysplastic syndrome presenting as a cellulitis-like plaque. Eur J Dermatol. 2009;19:182-183.
- Yang HI, Lee MC, Kuo TT, et al. Cellulitis-like cutaneous metastasis of uterine cervical carcinoma. J Am Acad Dermatol. 2007;56:S26-S28.
- Tzeng HE, Teng CL, Yang Y, et al. Occult subcutaneous panniculitis-like T-cell lymphoma with initial presentations of cellulitis-like skin lesion and fulminant hemophagocytosis. J Formos Med Assoc. 2007;106:S55-S59.
- Sharma PK, Sabhnani S, Bhardwaj M, et al. Acral, pure cutaneous, self-healing, late-onset, cellulitis-like Langerhans cell histiocytosis. J Cutan Med Surg. 2009;13:43-47.
- Tercedor J, Ródenas JM, Henraz MT, et al. Facial cellulitis-like Sweet’s syndrome in acute myelogenous leukemia. Int J Dermatol. 1992;31:598-599.
- Inaoki M, Nishijima C, Kumada S, et al. Adult-onset Still disease with a cellulitis-like eruption. Eur J Dermatol. 2009;19:80-81.
- Prabhu MM, Prabhu S, Mishra P, et al. Cellulitis-like fixed drug eruption attributed to paracetamol (acetaminophen). Dermatol Online J. 2005;11:24.
- Lee NH, Choi EH, Lee WS, et al. Tuberculous cellulitis. Clin Exp Dermatol. 2000;25:222-223.
- Kim JE, Ko JY, Bae SC, et al. Tuberculous cellulitis as a manifestation of miliary tuberculosis in a patient with malignancy-associated dermatomyositis. J Am Acad Dermatol. 2011;65:450-452.
- Chin PW, Koh CK, Wong KT. Cutaneous tuberculosis mimicking cellulitis in an immunosuppressed patient. Singapore Med J. 1999;40:44-45.
- Seyahi N, Apaydin S, Kahveci A, et al. Cellulitis as a manifestation of miliary tuberculosis in a renal transplant recipient. Transpl Infect Dis. 2005;7:80-85.
- Kato G, Watanabe K, Shibuya Y, et al. A case of cutaneous tuberculosis with cellulitis-like appearance [in Japanese]. Rinsho Hifuka (Jpn J Clin Dermatol). 2010;64:1055-1059.
- Fariña MC, Gegundez MI, Piqué E, et al. Cutaneous tuberculosis: a clinical, histopathologic, and bacteriologic study. J Am Acad Dermatol. 1995;33:433-440.
Local tender erythema is a typical manifestation of cellulitis, which is commonly seen by dermatologists; however, cutaneous manifestations of other diseases may bear resemblance to the more banal cellulitis. We present the case of a patient with tuberculous cellulitis, a rare variant of cutaneous tuberculosis.
Case Report
An 89-year-old man presented to a local primary care physician with a fever (temperature, 38°C). Infectious disease was suspected. Antibiotic therapy with oral cefaclor and intravenous cefotiam hydrochloride was started, but the patient’s fever did not subside. Six days after initiation of treatment, he was referred to our dermatology department for evaluation of a painful erythematous rash on the left thigh that had suddenly appeared. The patient had a history of pulmonary tuberculosis 71 years prior. He also underwent surgical treatment of pancreatic cancer 14 years prior. Additionally, he had chronic kidney disease (CKD) and polymyalgia rheumatica, which was currently being treated with oral prednisolone 5 mg once daily.
Physical examination revealed a hot and tender erythematous plaque on the left thigh (Figure 1). The edge of the lesion was not well defined and there was no regional lymphadenopathy.

A complete blood cell count revealed anemia (white blood cell count, 8070/μL [reference range, 4000–9,000/μL]; neutrophils, 77.1% [reference range, 44%–74%]; lymphocytes, 13.8% [reference range, 20%–50%]; hemoglobin, 9.3 g/dL [reference range, 13.0–17.0 g/dL]; and platelet count, 329×103/μL [reference range, 150–400×103/μL]). The C-reactive protein level was 7.3 mg/dL (reference range, 0.08–0.3 mg/dL). The creatinine level was 2.93 mg/dL (reference range, 0.6–1.2 mg/dL). There were no signs of liver dysfunction.
A blood culture was negative. A purified protein derivative (tuberculin) skin test was negative (6×7 mm [reference range, ≤9 mm). A chest computed tomography (CT) scan showed small centrilobular nodules that had not changed in number or size since evaluation 3 months prior.
The antibiotics were changed to meropenem hydrate 0.5 g and clindamycin 300 mg twice daily for presumed bacterial cellulitis, then meropenem hydrate 1 g and clindamycin 600 mg daily, but there was still no improvement after about 1 week. Therefore, a skin biopsy was performed on the left thigh. The specimen showed epithelioid cell granulomas throughout the dermis and subcutis (Figure 2). Ziehl-Neelsen stain revealed numerous acid-fast bacilli (Figure 3). Polymerase chain reaction was positive for Mycobacterium tuberculosis in the skin biopsy specimen and gastric fluid. Additionally, M tuberculosis was isolated from the skin biopsy specimen, gastric fluid, and sputum culture. After the series of treatments described above, a remarkable increase in nodule size and number was observed in a follow-up chest CT scan compared with the prior examination. These pulmonary lesions showed bronchogenic spread.
A diagnosis of tuberculous cellulitis with pulmonary tuberculosis was made. Treatment with isoniazid 200 mg once daily, rifampin 300 mg once daily, and ethambutol 500 mg once every other day was started; the dosages were reduced from the standard dose due to the patient’s CKD.1 Four days after initiation of these medications, the patient was transferred to a hospital specifically for the treatment of tuberculosis. Approximately 8 months after treatment with isoniazid, rifampin, and ethambutol, M tuberculosis could not be detected in the sputum and a chest CT revealed that the pulmonary lesions were remarkably improved. However, polymerase chain reaction of the skin biopsy specimen was still positive for M tuberculosis. It was determined that debridement of the skin lesion was needed, but the patient died from complications of deteriorating CKD 10 months after the initiation of the antituberculosis medications.
Comment
Cellulitis is a suppurative inflammation involving the subcutis.2 Local tender erythema, malaise, chills, and fever may be present at the onset. Cellulitis is commonly seen by dermatologists, and it is well known that other infectious diseases such as necrotizing fasciitis, cutaneous and subcutaneous mycoses,3 and nontuberculous mycobacterial infections4 sometimes present as cellulitislike skin lesions. Moreover, noninfectious diseases, such as Wells syndrome, thrombophlebitis, reactive angioendotheliomatosis,5 cutaneous metastasis of a primary malignancy,6 subcutaneous panniculitislike T-cell lymphoma,7 Langerhans cell histiocytosis,8 Sweet syndrome,9 adult-onset Still disease,10 and fixed drug eruption caused by acetaminophen11 should be excluded. These differential diagnoses and diagnostic clues of cellulitislike erythema are summarized in Table 1.3-16
Cutaneous tuberculosis presenting as cellulitis, so-called tuberculous cellulitis, also is characterized as a clinical mimicker of cellulitis. On the other hand, histologically, it has features of cutaneous tuberculosis (eg, necrotic granuloma).12,14,15 Tuberculous cellulitis is rare and therefore may often be misdiagnosed even in highly endemic areas. We summarized the clinical information of 5 well-documented cases of tuberculous cellulitis along with the current case in Table 2.12-16 All of these cases had an associated disease and involved patients who were currently taking oral corticosteroids. If a patient undergoing immunosuppressive therapy develops cellulitislike erythema, tuberculous cellulitis should be considered in the differential diagnosis.

Cutaneous tuberculosis generally is classified into 4 types according to the mechanism of disease acquisition: (1) inoculation from an exogenous source, (2) endogenous cutaneous spread contiguously or by autoinoculation, (3) hematogenous spread to the skin, and (4) tuberculids. In our case, it was suspected that the cellulitislike erythema may have been caused by hematogenous spread from pulmonary tuberculosis. Considering that negative reactions to purified protein derivative (tuberculin) skin tests often are observed in cases of miliary tuberculosis (widespread dissemination of M tuberculosis to 2 or more organs via hematogenous spread), we suspected that our patient could proceed to miliary tuberculosis; in fact, a case was reported in which miliary tuberculosis emerged approximately 3 weeks after the onset of erythema,13 as observed in the present case. Therefore, erythema in the setting of tuberculosis may be a predictor of miliary tuberculosis. The types of cutaneous lesions caused by tuberculosis infection also are dependent on multiple host factors.2 Cutaneous tuberculosis with an atypical clinical appearance has become more common because of the increasing number of immunocompromised patients.17
In addition, most cases of cutaneous tuberculosis are not associated with pain. Generally, tuberculous cellulitis also causes nontender erythematous plaques or nodules.2 However, in some cases of tuberculous cellulitis, including our case, tender skin lesions have been reported.12-14 Therefore, this symptom is not a sensitive factor for differential diagnosis.
We suggest that tuberculous cellulitis should always be included in the differential diagnosis of a cellulitislike rash with or without pain if the skin lesion is not improved despite antibiotic therapy.
Local tender erythema is a typical manifestation of cellulitis, which is commonly seen by dermatologists; however, cutaneous manifestations of other diseases may bear resemblance to the more banal cellulitis. We present the case of a patient with tuberculous cellulitis, a rare variant of cutaneous tuberculosis.
Case Report
An 89-year-old man presented to a local primary care physician with a fever (temperature, 38°C). Infectious disease was suspected. Antibiotic therapy with oral cefaclor and intravenous cefotiam hydrochloride was started, but the patient’s fever did not subside. Six days after initiation of treatment, he was referred to our dermatology department for evaluation of a painful erythematous rash on the left thigh that had suddenly appeared. The patient had a history of pulmonary tuberculosis 71 years prior. He also underwent surgical treatment of pancreatic cancer 14 years prior. Additionally, he had chronic kidney disease (CKD) and polymyalgia rheumatica, which was currently being treated with oral prednisolone 5 mg once daily.
Physical examination revealed a hot and tender erythematous plaque on the left thigh (Figure 1). The edge of the lesion was not well defined and there was no regional lymphadenopathy.

A complete blood cell count revealed anemia (white blood cell count, 8070/μL [reference range, 4000–9,000/μL]; neutrophils, 77.1% [reference range, 44%–74%]; lymphocytes, 13.8% [reference range, 20%–50%]; hemoglobin, 9.3 g/dL [reference range, 13.0–17.0 g/dL]; and platelet count, 329×103/μL [reference range, 150–400×103/μL]). The C-reactive protein level was 7.3 mg/dL (reference range, 0.08–0.3 mg/dL). The creatinine level was 2.93 mg/dL (reference range, 0.6–1.2 mg/dL). There were no signs of liver dysfunction.
A blood culture was negative. A purified protein derivative (tuberculin) skin test was negative (6×7 mm [reference range, ≤9 mm). A chest computed tomography (CT) scan showed small centrilobular nodules that had not changed in number or size since evaluation 3 months prior.
The antibiotics were changed to meropenem hydrate 0.5 g and clindamycin 300 mg twice daily for presumed bacterial cellulitis, then meropenem hydrate 1 g and clindamycin 600 mg daily, but there was still no improvement after about 1 week. Therefore, a skin biopsy was performed on the left thigh. The specimen showed epithelioid cell granulomas throughout the dermis and subcutis (Figure 2). Ziehl-Neelsen stain revealed numerous acid-fast bacilli (Figure 3). Polymerase chain reaction was positive for Mycobacterium tuberculosis in the skin biopsy specimen and gastric fluid. Additionally, M tuberculosis was isolated from the skin biopsy specimen, gastric fluid, and sputum culture. After the series of treatments described above, a remarkable increase in nodule size and number was observed in a follow-up chest CT scan compared with the prior examination. These pulmonary lesions showed bronchogenic spread.
A diagnosis of tuberculous cellulitis with pulmonary tuberculosis was made. Treatment with isoniazid 200 mg once daily, rifampin 300 mg once daily, and ethambutol 500 mg once every other day was started; the dosages were reduced from the standard dose due to the patient’s CKD.1 Four days after initiation of these medications, the patient was transferred to a hospital specifically for the treatment of tuberculosis. Approximately 8 months after treatment with isoniazid, rifampin, and ethambutol, M tuberculosis could not be detected in the sputum and a chest CT revealed that the pulmonary lesions were remarkably improved. However, polymerase chain reaction of the skin biopsy specimen was still positive for M tuberculosis. It was determined that debridement of the skin lesion was needed, but the patient died from complications of deteriorating CKD 10 months after the initiation of the antituberculosis medications.
Comment
Cellulitis is a suppurative inflammation involving the subcutis.2 Local tender erythema, malaise, chills, and fever may be present at the onset. Cellulitis is commonly seen by dermatologists, and it is well known that other infectious diseases such as necrotizing fasciitis, cutaneous and subcutaneous mycoses,3 and nontuberculous mycobacterial infections4 sometimes present as cellulitislike skin lesions. Moreover, noninfectious diseases, such as Wells syndrome, thrombophlebitis, reactive angioendotheliomatosis,5 cutaneous metastasis of a primary malignancy,6 subcutaneous panniculitislike T-cell lymphoma,7 Langerhans cell histiocytosis,8 Sweet syndrome,9 adult-onset Still disease,10 and fixed drug eruption caused by acetaminophen11 should be excluded. These differential diagnoses and diagnostic clues of cellulitislike erythema are summarized in Table 1.3-16
Cutaneous tuberculosis presenting as cellulitis, so-called tuberculous cellulitis, also is characterized as a clinical mimicker of cellulitis. On the other hand, histologically, it has features of cutaneous tuberculosis (eg, necrotic granuloma).12,14,15 Tuberculous cellulitis is rare and therefore may often be misdiagnosed even in highly endemic areas. We summarized the clinical information of 5 well-documented cases of tuberculous cellulitis along with the current case in Table 2.12-16 All of these cases had an associated disease and involved patients who were currently taking oral corticosteroids. If a patient undergoing immunosuppressive therapy develops cellulitislike erythema, tuberculous cellulitis should be considered in the differential diagnosis.

Cutaneous tuberculosis generally is classified into 4 types according to the mechanism of disease acquisition: (1) inoculation from an exogenous source, (2) endogenous cutaneous spread contiguously or by autoinoculation, (3) hematogenous spread to the skin, and (4) tuberculids. In our case, it was suspected that the cellulitislike erythema may have been caused by hematogenous spread from pulmonary tuberculosis. Considering that negative reactions to purified protein derivative (tuberculin) skin tests often are observed in cases of miliary tuberculosis (widespread dissemination of M tuberculosis to 2 or more organs via hematogenous spread), we suspected that our patient could proceed to miliary tuberculosis; in fact, a case was reported in which miliary tuberculosis emerged approximately 3 weeks after the onset of erythema,13 as observed in the present case. Therefore, erythema in the setting of tuberculosis may be a predictor of miliary tuberculosis. The types of cutaneous lesions caused by tuberculosis infection also are dependent on multiple host factors.2 Cutaneous tuberculosis with an atypical clinical appearance has become more common because of the increasing number of immunocompromised patients.17
In addition, most cases of cutaneous tuberculosis are not associated with pain. Generally, tuberculous cellulitis also causes nontender erythematous plaques or nodules.2 However, in some cases of tuberculous cellulitis, including our case, tender skin lesions have been reported.12-14 Therefore, this symptom is not a sensitive factor for differential diagnosis.
We suggest that tuberculous cellulitis should always be included in the differential diagnosis of a cellulitislike rash with or without pain if the skin lesion is not improved despite antibiotic therapy.
- Daido-Horiuchi Y, Kikuchi Y, Kobayashi S, et al. Tuberculous cellulitis in a patient with chronic kidney disease and polymyalgia rheumatica. Intern Med. 2012;51:3203-3206.
- James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin. 11th ed. Philadelphia, PA: Saunders Elsevier; 2011:322-329.
- Schupbach CW, Wheeler CE Jr, Briggaman RA, et al. Cutaneous manifestations of disseminated cryptococcosis. Arch Dermatol. 1976;112:1734-1740.
- Hsu PY, Yang YH, Hsiao CH, et al. Mycobacterium kansasii infection presenting as cellulitis in a patient with systemic lupus erythematosus. J Formos Med Assoc. 2002;101:581-584.
- Aguayo-Leiva I, Vano-Galván S, Salguero I, et al. Reactive angioendotheliomatosis in a patient with myelodysplastic syndrome presenting as a cellulitis-like plaque. Eur J Dermatol. 2009;19:182-183.
- Yang HI, Lee MC, Kuo TT, et al. Cellulitis-like cutaneous metastasis of uterine cervical carcinoma. J Am Acad Dermatol. 2007;56:S26-S28.
- Tzeng HE, Teng CL, Yang Y, et al. Occult subcutaneous panniculitis-like T-cell lymphoma with initial presentations of cellulitis-like skin lesion and fulminant hemophagocytosis. J Formos Med Assoc. 2007;106:S55-S59.
- Sharma PK, Sabhnani S, Bhardwaj M, et al. Acral, pure cutaneous, self-healing, late-onset, cellulitis-like Langerhans cell histiocytosis. J Cutan Med Surg. 2009;13:43-47.
- Tercedor J, Ródenas JM, Henraz MT, et al. Facial cellulitis-like Sweet’s syndrome in acute myelogenous leukemia. Int J Dermatol. 1992;31:598-599.
- Inaoki M, Nishijima C, Kumada S, et al. Adult-onset Still disease with a cellulitis-like eruption. Eur J Dermatol. 2009;19:80-81.
- Prabhu MM, Prabhu S, Mishra P, et al. Cellulitis-like fixed drug eruption attributed to paracetamol (acetaminophen). Dermatol Online J. 2005;11:24.
- Lee NH, Choi EH, Lee WS, et al. Tuberculous cellulitis. Clin Exp Dermatol. 2000;25:222-223.
- Kim JE, Ko JY, Bae SC, et al. Tuberculous cellulitis as a manifestation of miliary tuberculosis in a patient with malignancy-associated dermatomyositis. J Am Acad Dermatol. 2011;65:450-452.
- Chin PW, Koh CK, Wong KT. Cutaneous tuberculosis mimicking cellulitis in an immunosuppressed patient. Singapore Med J. 1999;40:44-45.
- Seyahi N, Apaydin S, Kahveci A, et al. Cellulitis as a manifestation of miliary tuberculosis in a renal transplant recipient. Transpl Infect Dis. 2005;7:80-85.
- Kato G, Watanabe K, Shibuya Y, et al. A case of cutaneous tuberculosis with cellulitis-like appearance [in Japanese]. Rinsho Hifuka (Jpn J Clin Dermatol). 2010;64:1055-1059.
- Fariña MC, Gegundez MI, Piqué E, et al. Cutaneous tuberculosis: a clinical, histopathologic, and bacteriologic study. J Am Acad Dermatol. 1995;33:433-440.
- Daido-Horiuchi Y, Kikuchi Y, Kobayashi S, et al. Tuberculous cellulitis in a patient with chronic kidney disease and polymyalgia rheumatica. Intern Med. 2012;51:3203-3206.
- James WD, Berger TG, Elston DM, eds. Andrews’ Diseases of the Skin. 11th ed. Philadelphia, PA: Saunders Elsevier; 2011:322-329.
- Schupbach CW, Wheeler CE Jr, Briggaman RA, et al. Cutaneous manifestations of disseminated cryptococcosis. Arch Dermatol. 1976;112:1734-1740.
- Hsu PY, Yang YH, Hsiao CH, et al. Mycobacterium kansasii infection presenting as cellulitis in a patient with systemic lupus erythematosus. J Formos Med Assoc. 2002;101:581-584.
- Aguayo-Leiva I, Vano-Galván S, Salguero I, et al. Reactive angioendotheliomatosis in a patient with myelodysplastic syndrome presenting as a cellulitis-like plaque. Eur J Dermatol. 2009;19:182-183.
- Yang HI, Lee MC, Kuo TT, et al. Cellulitis-like cutaneous metastasis of uterine cervical carcinoma. J Am Acad Dermatol. 2007;56:S26-S28.
- Tzeng HE, Teng CL, Yang Y, et al. Occult subcutaneous panniculitis-like T-cell lymphoma with initial presentations of cellulitis-like skin lesion and fulminant hemophagocytosis. J Formos Med Assoc. 2007;106:S55-S59.
- Sharma PK, Sabhnani S, Bhardwaj M, et al. Acral, pure cutaneous, self-healing, late-onset, cellulitis-like Langerhans cell histiocytosis. J Cutan Med Surg. 2009;13:43-47.
- Tercedor J, Ródenas JM, Henraz MT, et al. Facial cellulitis-like Sweet’s syndrome in acute myelogenous leukemia. Int J Dermatol. 1992;31:598-599.
- Inaoki M, Nishijima C, Kumada S, et al. Adult-onset Still disease with a cellulitis-like eruption. Eur J Dermatol. 2009;19:80-81.
- Prabhu MM, Prabhu S, Mishra P, et al. Cellulitis-like fixed drug eruption attributed to paracetamol (acetaminophen). Dermatol Online J. 2005;11:24.
- Lee NH, Choi EH, Lee WS, et al. Tuberculous cellulitis. Clin Exp Dermatol. 2000;25:222-223.
- Kim JE, Ko JY, Bae SC, et al. Tuberculous cellulitis as a manifestation of miliary tuberculosis in a patient with malignancy-associated dermatomyositis. J Am Acad Dermatol. 2011;65:450-452.
- Chin PW, Koh CK, Wong KT. Cutaneous tuberculosis mimicking cellulitis in an immunosuppressed patient. Singapore Med J. 1999;40:44-45.
- Seyahi N, Apaydin S, Kahveci A, et al. Cellulitis as a manifestation of miliary tuberculosis in a renal transplant recipient. Transpl Infect Dis. 2005;7:80-85.
- Kato G, Watanabe K, Shibuya Y, et al. A case of cutaneous tuberculosis with cellulitis-like appearance [in Japanese]. Rinsho Hifuka (Jpn J Clin Dermatol). 2010;64:1055-1059.
- Fariña MC, Gegundez MI, Piqué E, et al. Cutaneous tuberculosis: a clinical, histopathologic, and bacteriologic study. J Am Acad Dermatol. 1995;33:433-440.
