User login
Dealing with a difficult boss: A ‘bossectomy’ is rarely the cure
Ms. D is a 48-year-old administrative assistant and married mother of 2 teenagers with a history of adjustment disorder with mixed anxiety and depressed mood. She presents with increasing anxiety, poor sleep, irritability, and occasional feelings of hopelessness in the context of feeling stuck in a “dead-end job.” She describes her main issue as having an uncaring boss with unrealistic expectations. Clearly exasperated, she tells you, “If only I could get rid of my boss, everything would be just fine.”
Ms. D’s situation is common. When confronted with overbearing and demanding supervisors, the natural inclination for some employees is to flee. Symptoms of burnout (eg, emotional exhaustion, depersonalization, and decreased personal accomplishment) often occur, sometimes with more serious symptoms of adjustment disorder or even major depressive disorder or generalized anxiety disorder. To help patients such as Ms. D who are experiencing difficulties with their boss, you can use a simple approach aimed at helping them make the decision to stay at the job or leave for other opportunities, while supporting them along the way.
Clarify, then support and explore
A critical addition to the typical evaluation is a full social history, including prior employment and formative relationships, that may inform current workplace dynamics. Does the patient have a pattern of similar circumstances, or is this unusual for her? How does she view the supervisor-employee relationship, and how do power differentials, potential job loss, and subsequent financial impacts further amplify emotional friction?
Once the dynamics are clarified, support and validate her emotional reaction before exploring potential cognitive distortions and her own contributions to the relationship dysfunction. If her tendency is to lash out in anger, she could fan the flames and risk being fired. If her tendency is to cower or freeze, you can help to gradually empower her. Regardless of relationship dynamics, be careful not to medicalize what may simply be a difficult situation.1 Perhaps she is a perfectionist and minimizes her supervisor’s behaviors that affirm her work and value as a person. In such cases, you can use cognitive-behavioral therapy techniques to help her consider different points of view and nuance. Rarely are people all good or all bad.
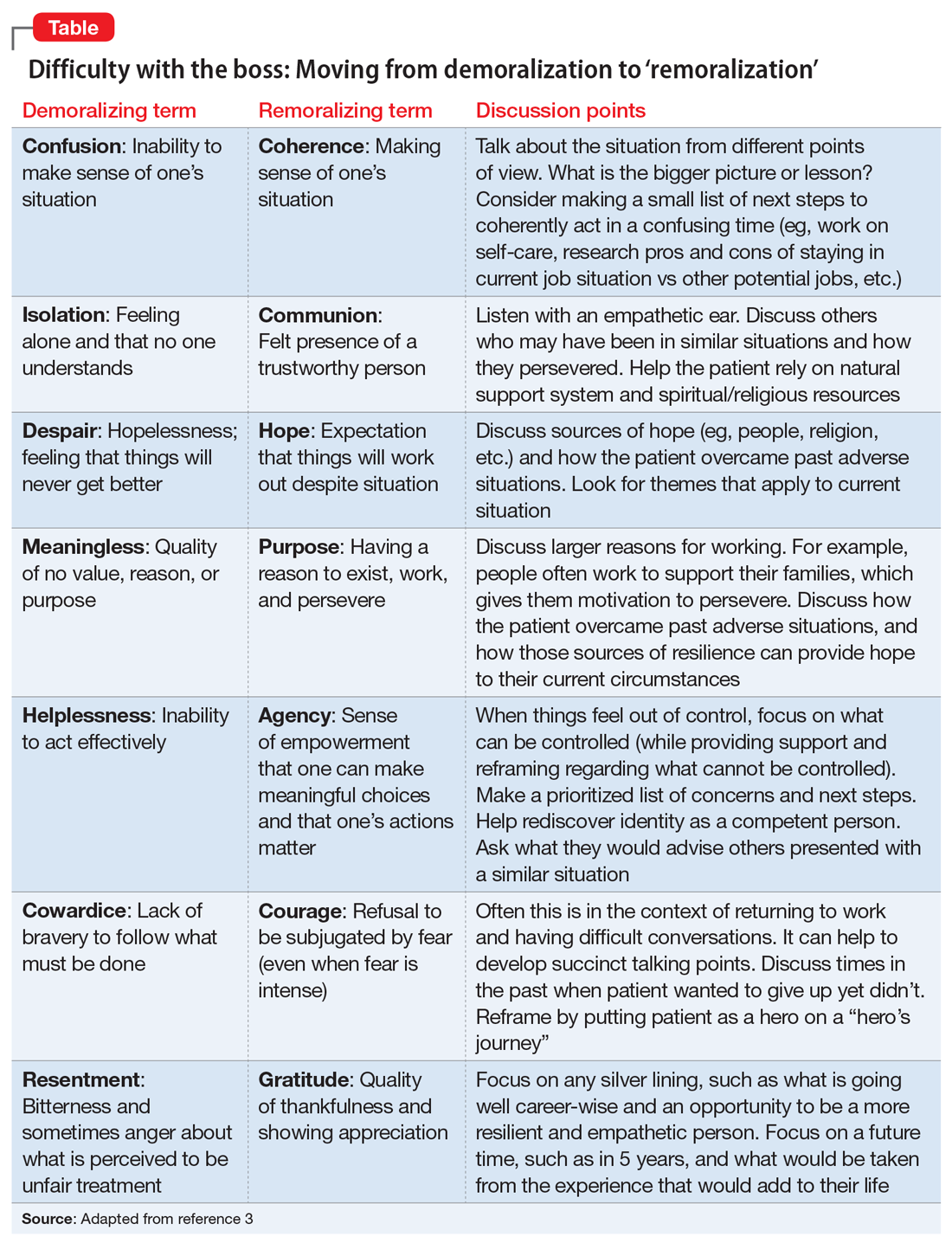
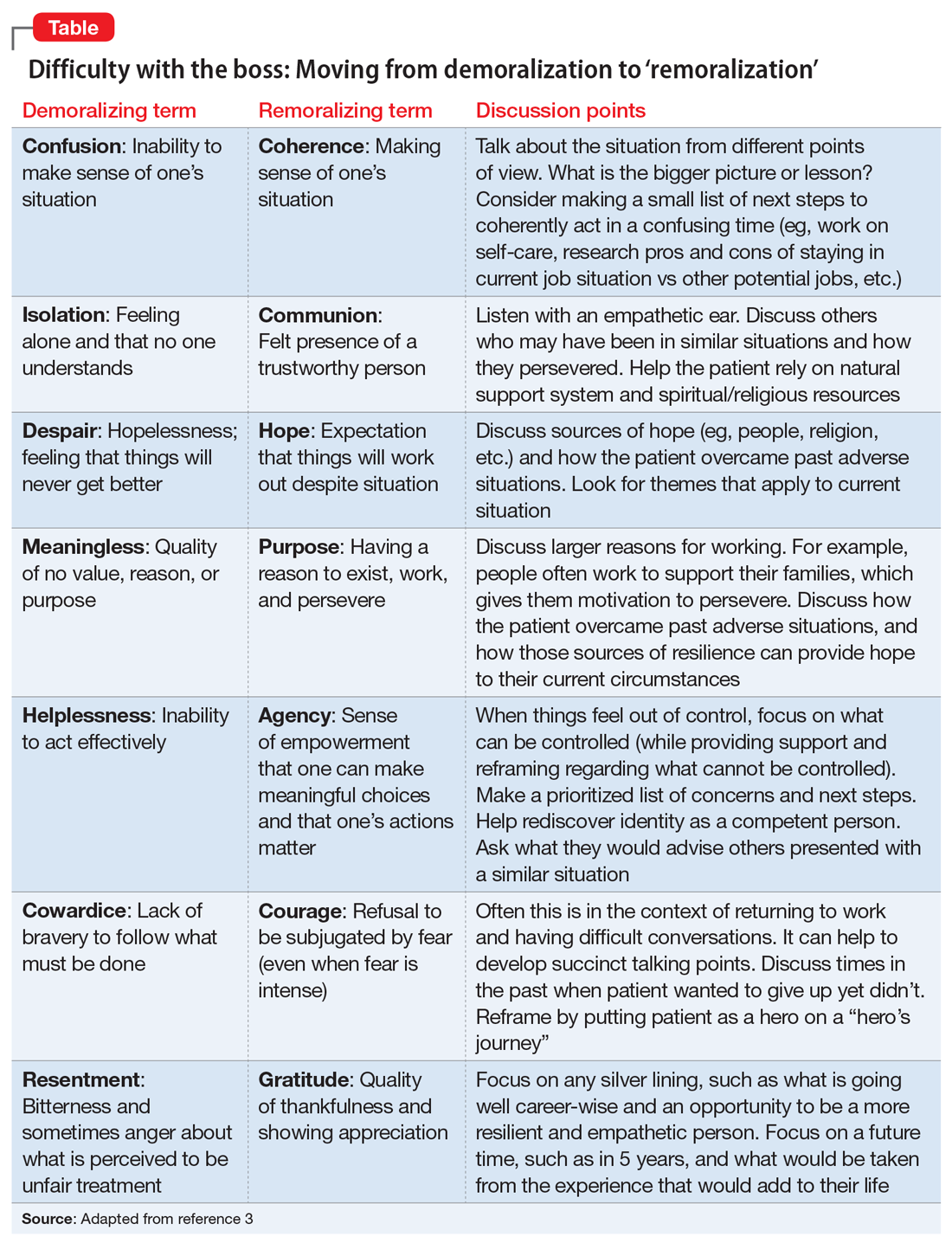
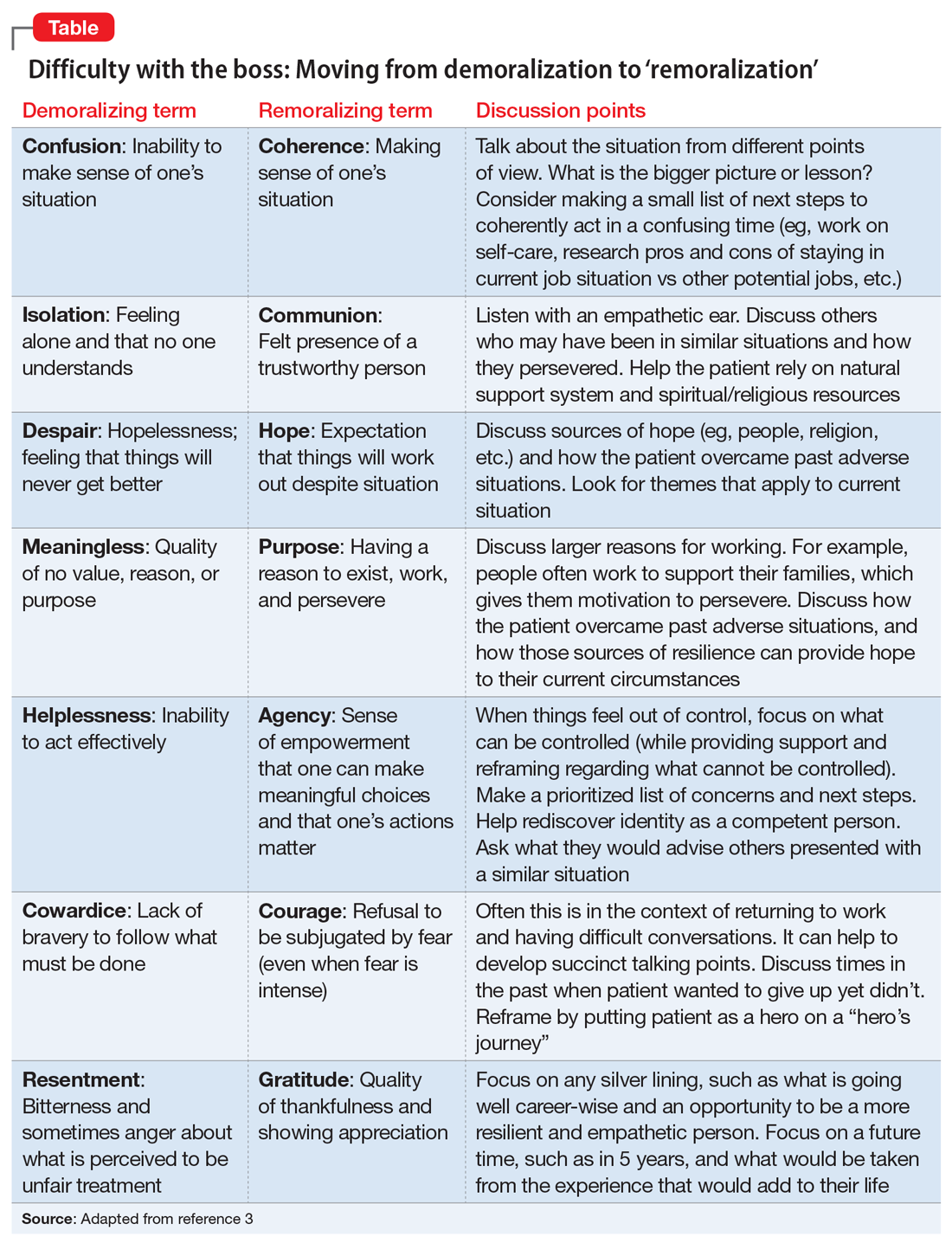
Perhaps her perceptions are accurate, and her boss really is a jerk. If this is the case, she likely feels unfairly and helplessly persecuted. She may be suffering from demoralization, or feelings of impotence, isolation, and despair in which her self-esteem is damaged and she feels rejected because of her failure to meet her boss’s and her own expectations.2 In cases of demoralization, oddly enough, hospice literature lends some tools to help her. The Table3 provides some common terms associated with demoralization and discussion points you can use to help her move toward “remoralization.”
Regardless of the full story, it’s common for people to externalize uncomfortable emotions and attribute symptoms to an external cause. Help her develop self-efficacy by realizing she is in control of how she responds to her emotions. Have her focus on her role in the relationship with her supervisor, looking for common ground and brainstorming practical solutions. Ultimately you can help her realize that she always has choices about whether to stay at the job or look for work elsewhere. Your role is to support her regardless of her decision.
CASE CONTINUED
Over several visits, Ms. D begins to view the relationship with her supervisor in a different light. She has a conversation with him about what she needs to do personally and what she needs professionally from him to be successful at work. Her supervisor acknowledges he has been demanding and could be more supportive. Together they vow to communicate more clearly and regularly assess progress, including celebrating clear victories. Ms. D ultimately decides to stay at the job, and her symptoms resolve without a “bossectomy.”
1. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-e131.
2. Frank JD. Psychotherapy: the restoration of morale. Am J Psychiatry. 1974;131(3):271-274.
3. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116.
Ms. D is a 48-year-old administrative assistant and married mother of 2 teenagers with a history of adjustment disorder with mixed anxiety and depressed mood. She presents with increasing anxiety, poor sleep, irritability, and occasional feelings of hopelessness in the context of feeling stuck in a “dead-end job.” She describes her main issue as having an uncaring boss with unrealistic expectations. Clearly exasperated, she tells you, “If only I could get rid of my boss, everything would be just fine.”
Ms. D’s situation is common. When confronted with overbearing and demanding supervisors, the natural inclination for some employees is to flee. Symptoms of burnout (eg, emotional exhaustion, depersonalization, and decreased personal accomplishment) often occur, sometimes with more serious symptoms of adjustment disorder or even major depressive disorder or generalized anxiety disorder. To help patients such as Ms. D who are experiencing difficulties with their boss, you can use a simple approach aimed at helping them make the decision to stay at the job or leave for other opportunities, while supporting them along the way.
Clarify, then support and explore
A critical addition to the typical evaluation is a full social history, including prior employment and formative relationships, that may inform current workplace dynamics. Does the patient have a pattern of similar circumstances, or is this unusual for her? How does she view the supervisor-employee relationship, and how do power differentials, potential job loss, and subsequent financial impacts further amplify emotional friction?
Once the dynamics are clarified, support and validate her emotional reaction before exploring potential cognitive distortions and her own contributions to the relationship dysfunction. If her tendency is to lash out in anger, she could fan the flames and risk being fired. If her tendency is to cower or freeze, you can help to gradually empower her. Regardless of relationship dynamics, be careful not to medicalize what may simply be a difficult situation.1 Perhaps she is a perfectionist and minimizes her supervisor’s behaviors that affirm her work and value as a person. In such cases, you can use cognitive-behavioral therapy techniques to help her consider different points of view and nuance. Rarely are people all good or all bad.
Perhaps her perceptions are accurate, and her boss really is a jerk. If this is the case, she likely feels unfairly and helplessly persecuted. She may be suffering from demoralization, or feelings of impotence, isolation, and despair in which her self-esteem is damaged and she feels rejected because of her failure to meet her boss’s and her own expectations.2 In cases of demoralization, oddly enough, hospice literature lends some tools to help her. The Table3 provides some common terms associated with demoralization and discussion points you can use to help her move toward “remoralization.”
Regardless of the full story, it’s common for people to externalize uncomfortable emotions and attribute symptoms to an external cause. Help her develop self-efficacy by realizing she is in control of how she responds to her emotions. Have her focus on her role in the relationship with her supervisor, looking for common ground and brainstorming practical solutions. Ultimately you can help her realize that she always has choices about whether to stay at the job or look for work elsewhere. Your role is to support her regardless of her decision.
CASE CONTINUED
Over several visits, Ms. D begins to view the relationship with her supervisor in a different light. She has a conversation with him about what she needs to do personally and what she needs professionally from him to be successful at work. Her supervisor acknowledges he has been demanding and could be more supportive. Together they vow to communicate more clearly and regularly assess progress, including celebrating clear victories. Ms. D ultimately decides to stay at the job, and her symptoms resolve without a “bossectomy.”
Ms. D is a 48-year-old administrative assistant and married mother of 2 teenagers with a history of adjustment disorder with mixed anxiety and depressed mood. She presents with increasing anxiety, poor sleep, irritability, and occasional feelings of hopelessness in the context of feeling stuck in a “dead-end job.” She describes her main issue as having an uncaring boss with unrealistic expectations. Clearly exasperated, she tells you, “If only I could get rid of my boss, everything would be just fine.”
Ms. D’s situation is common. When confronted with overbearing and demanding supervisors, the natural inclination for some employees is to flee. Symptoms of burnout (eg, emotional exhaustion, depersonalization, and decreased personal accomplishment) often occur, sometimes with more serious symptoms of adjustment disorder or even major depressive disorder or generalized anxiety disorder. To help patients such as Ms. D who are experiencing difficulties with their boss, you can use a simple approach aimed at helping them make the decision to stay at the job or leave for other opportunities, while supporting them along the way.
Clarify, then support and explore
A critical addition to the typical evaluation is a full social history, including prior employment and formative relationships, that may inform current workplace dynamics. Does the patient have a pattern of similar circumstances, or is this unusual for her? How does she view the supervisor-employee relationship, and how do power differentials, potential job loss, and subsequent financial impacts further amplify emotional friction?
Once the dynamics are clarified, support and validate her emotional reaction before exploring potential cognitive distortions and her own contributions to the relationship dysfunction. If her tendency is to lash out in anger, she could fan the flames and risk being fired. If her tendency is to cower or freeze, you can help to gradually empower her. Regardless of relationship dynamics, be careful not to medicalize what may simply be a difficult situation.1 Perhaps she is a perfectionist and minimizes her supervisor’s behaviors that affirm her work and value as a person. In such cases, you can use cognitive-behavioral therapy techniques to help her consider different points of view and nuance. Rarely are people all good or all bad.
Perhaps her perceptions are accurate, and her boss really is a jerk. If this is the case, she likely feels unfairly and helplessly persecuted. She may be suffering from demoralization, or feelings of impotence, isolation, and despair in which her self-esteem is damaged and she feels rejected because of her failure to meet her boss’s and her own expectations.2 In cases of demoralization, oddly enough, hospice literature lends some tools to help her. The Table3 provides some common terms associated with demoralization and discussion points you can use to help her move toward “remoralization.”
Regardless of the full story, it’s common for people to externalize uncomfortable emotions and attribute symptoms to an external cause. Help her develop self-efficacy by realizing she is in control of how she responds to her emotions. Have her focus on her role in the relationship with her supervisor, looking for common ground and brainstorming practical solutions. Ultimately you can help her realize that she always has choices about whether to stay at the job or look for work elsewhere. Your role is to support her regardless of her decision.
CASE CONTINUED
Over several visits, Ms. D begins to view the relationship with her supervisor in a different light. She has a conversation with him about what she needs to do personally and what she needs professionally from him to be successful at work. Her supervisor acknowledges he has been demanding and could be more supportive. Together they vow to communicate more clearly and regularly assess progress, including celebrating clear victories. Ms. D ultimately decides to stay at the job, and her symptoms resolve without a “bossectomy.”
1. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-e131.
2. Frank JD. Psychotherapy: the restoration of morale. Am J Psychiatry. 1974;131(3):271-274.
3. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116.
1. Jurisic M, Bean M, Harbaugh J, et al. The personal physician’s role in helping patients with medical conditions stay at work or return to work. J Occup Environ Med. 2017;59(6):e125-e131.
2. Frank JD. Psychotherapy: the restoration of morale. Am J Psychiatry. 1974;131(3):271-274.
3. Griffith JL, Gaby L. Brief psychotherapy at the bedside: countering demoralization from medical illness. Psychosomatics. 2005;46(2):109-116.
