User login
Primary hyperparathyroidism: Labs to order, Tx to consider
Since the advent of multichannel serum chemistry screening in the 1970s, large numbers of asymptomatic cases of primary hyperparathyroidism (PHPT) have been discovered. The clinical spectrum of the disease has changed from the classic “moans, groans, bones, and stones” to an asymptomatic and subtle presentation of hypercalcemia.1,2 PHPT and malignancy are the most common causes for hypercalcemia, accounting for 90% of cases.3 In the United States, the estimated incidence of PHPT between 1998 and 2010 was about 50 per 100,000 person-years. Most patients with PHPT are older women (ages >50 years) who are asymptomatic at the time of diagnosis.1
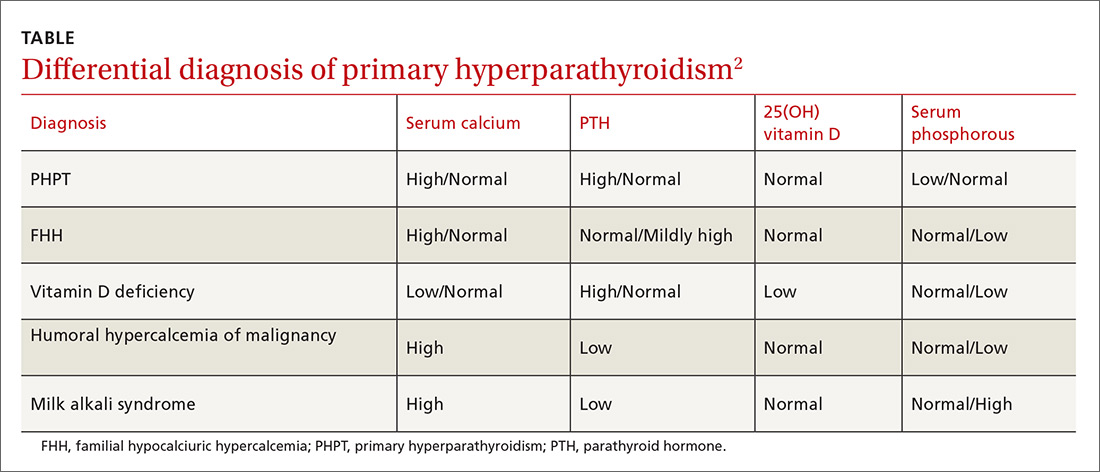
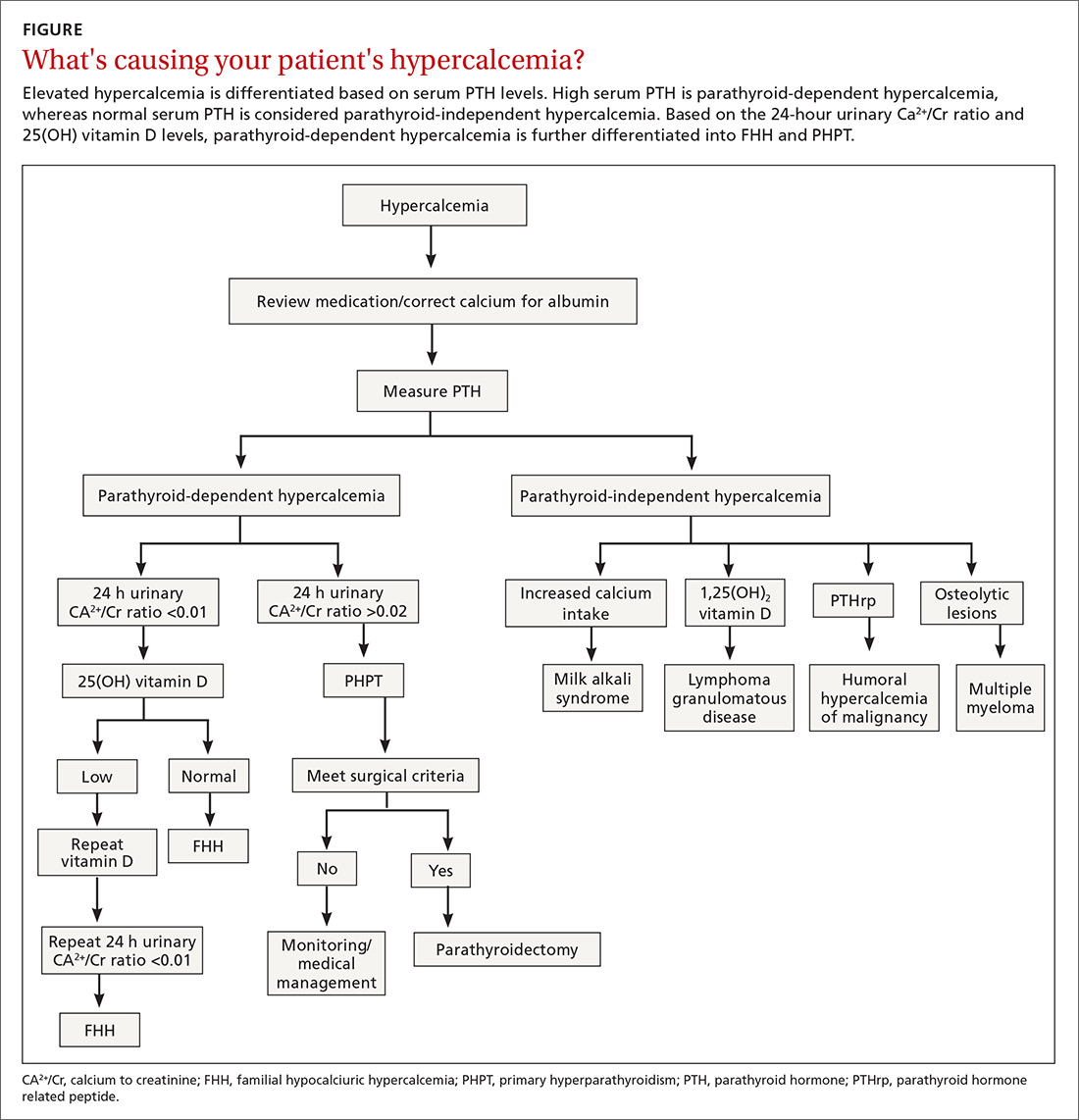
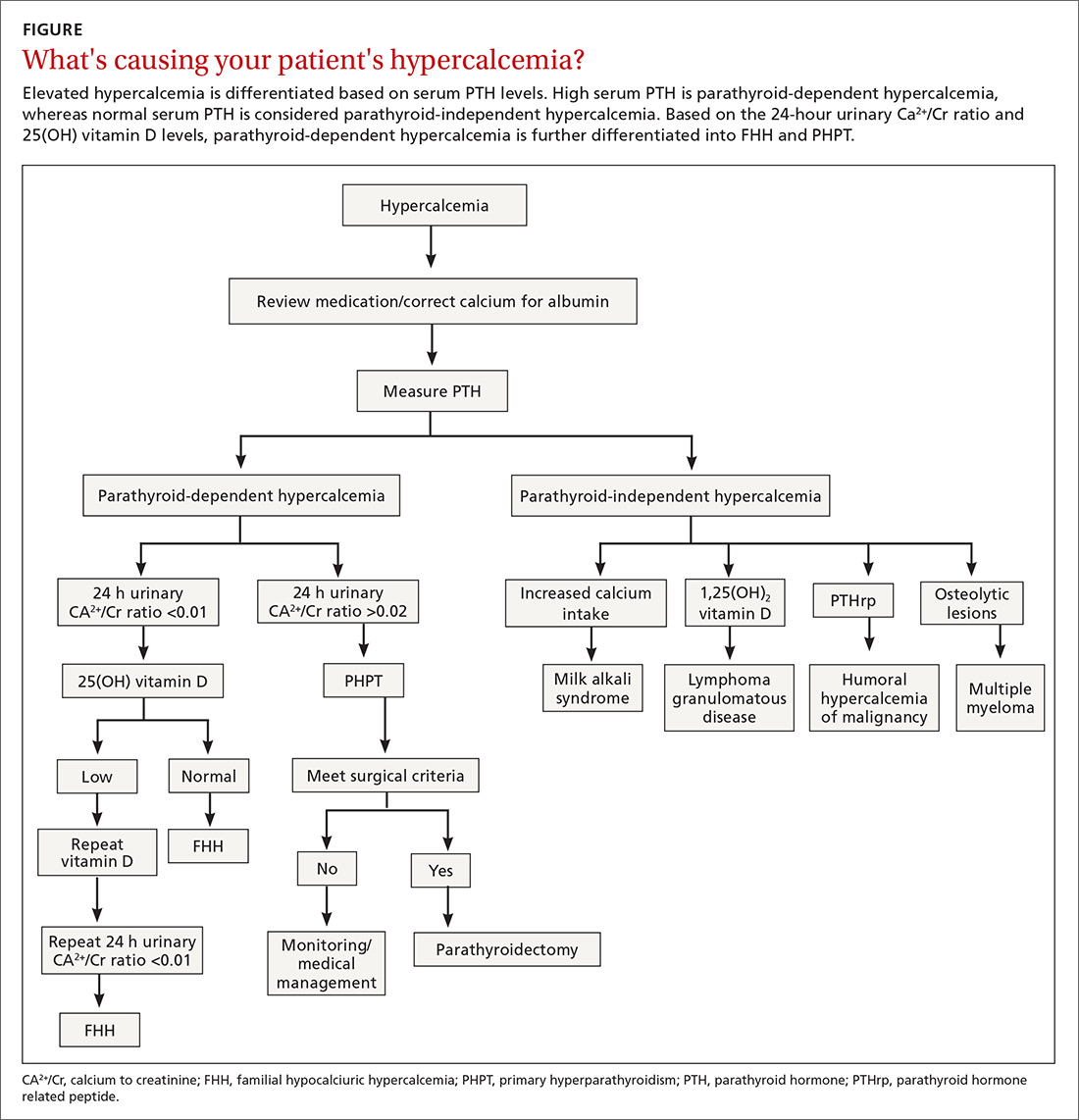
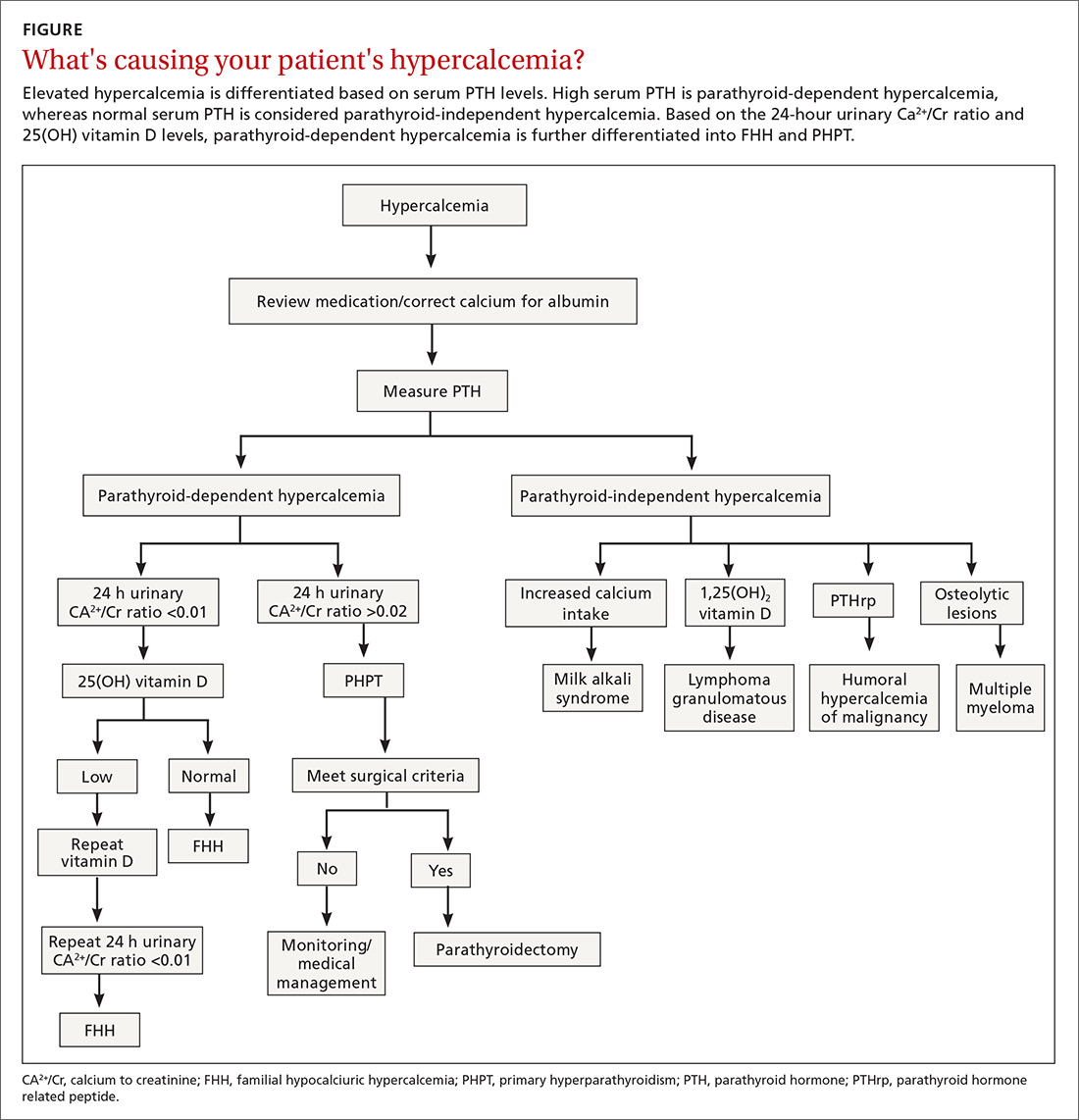
Vigilance needed in primary care. PHPT is slowly progressive, and the patient might accept symptoms as a process of aging. Therefore, it is essential that primary care physicians (PCPs) be aware of the diagnostic and management options. A systematic approach to the diagnosis of PHPT helps differentiate the causes of hypercalcemia (TABLE2; FIGURE2). But before we discuss PHPT diagnostic clues, it’s helpful to quickly review the workings of the parathyroid glands.
How the glands work, what can go wrong
Parathyroid hormone (PTH) is secreted by 4 pea-sized parathyroid glands located posterior to the thyroid. PTH regulates the levels of calcium (Ca2+) and phosphorous and controls the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D by activating the enzyme 1 alpha-hydroxylase.
PHPT is regarded as an abnormal secretion of PTH that does not correlate with the levels of Ca2+ in the blood.1 Eighty percent of PHPT is due to a solitary adenoma in one of the parathyroid glands, 2% to 4% is secondary to multiple parathyroid adenomas, 15% is due to parathyroid hyperplasia, and 0.5% due to parathyroid carcinoma.4
Nonspecific symptomsare subtle clues of PHPT
Patients with PHPT can present with nonspecific symptoms, such as weakness, fatigue, anorexia, polyuria, polydipsia, bone and joint pain, mild depression, and mild cognitive or neuromuscular dysfunction.5 A careful history is essential to elicit these symptoms, as the patient may attribute these to aging or other causes. PHPT should also be considered when patients present with kidney stones, unexplained osteoporosis, or fragility fractures. A physical examination is seldom helpful, as parathyroid adenomas are hardly ever palpable. A slit-lamp examination may reveal corneal diseases in rare cases of hypercalcemia.6
Which lab tests, imaging should you order?
Serum Ca2+
Repeat measurements of serum Ca2+ to confirm hypercalcemia. Volume depletion, underlying malignancy, medications such as hydrochlorothiazide, lithium, and excess intake of Ca2+ carbonate can cause hypercalcemia.7 Therefore, a review of the patients’ home medications and dietary preferences in the evaluation of hypercalcemia is essential. The 2 most common causes of hypercalcemia are hyperparathyroidism and hypercalcemia of malignancy.
For hypercalcemia, establish a differential diagnosis by measuring intact PTH. An increased serum Ca2+ level along with an elevated PTH concentration should suggest PTH-dependent hypercalcemia, whereas hypercalcemia with suppressed or low-normal PTH values should suggest PTH-independent hypercalcemia (granulomatous disorders, hypercalcemia of malignancy).
Continue to: Hypercalcemia of malignancy is due to...
Hypercalcemia of malignancy is due to increased production of parathyroid hormone-related peptide from various tumor cells that initiate bone resorption and increased renal Ca2+ absorption. It can also be due to osteolysis from bone metastasis.7 It is generally severe and is a common cause of hypercalcemia in the inpatient setting.
Meticulous evaluation is vital to diagnose PHPT. Measurement of serum ionized Ca2+ reflects the biologically active Ca2+. Studies by Ong and colleagues suggest that about 24% of patients with the histologically proven parathyroid disease had isolated ionized hypercalcemia.8 It is also an important adjunct to diagnose the presumed normocalcemic PHPT in which both the ionized Ca2+ levels and serum total Ca2+ levels should be normal.9
In patients with hypoalbuminemia, a corrected serum Ca2+ is calculated using the equation: corrected Ca2+ = [0.8 × (normal albumin-patient’s albumin)] + serum Ca2+ level.
Serum PTH
Second-generation PTH assays (intact PTH) and third-generation PTH assays (bioactive PTH) are equally reliable in diagnosing PHPT.10 The results obtained with intact and bioactive PTH assays are highly correlated. Several studies have found no improvement in diagnostic accuracy when using the bioactive PTH assay.11,12
Serum PTH can be low, normal, or elevated in hypercalcemia. Hypercalcemia with a high PTH level is parathyroid-dependent hypercalcemia, whereas hypercalcemia with a suppressed PTH level is considered parathyroid-independent.
Continue to: Serum 25(OH) vitamin D
Serum 25(OH) vitamin D
Vitamin D levels are normal in PHPT and normocalcemic PHPT. However, measuring 25(OH) vitamin D in all patients with suspected PHPT is recommended to evaluate for secondary hyperparathyroidism that is due to hypocalcemia or renal failure, which can occur concomitantly with PHPT.
Normocalcemic PHPT can be differentiated from secondary hyperparathyroidism of chronic kidney disease by measuring the 1,25(OH)2 vitamin D level; it will be low in secondary hyperparathyroidism.4
Serum 1,25(OH)2 vitamin D
1,25(OH)2 vitaminD levels are elevated in about one-third of patients with PHPT, as PTH stimulates the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D.13 Although this is not a routine test, it is useful in the evaluation of parathyroid-independent hypercalcemia caused by granulomatous disease, such as sarcoidosis where there is an autonomous production of 1,25(OH)2 vitamin D leading to hypercalcemia.14
Serum creatinine and estimated glomerular filtration rate
Serum creatinine (Cr) helps assess renal function. Reduction in serum Cr clearance to <60 mL/min with no other underlying cause is an indication for parathyroidectomy.10
Serum phosphorous
PTH increases the excretion of phosphorous by inhibiting reabsorption from the proximal tubule. Therefore, serum phosphorus tends to be in the lower range of normal in PHPT, but hypophosphatemia is present in less than a quarter of patients.4
Continue to: 24-hour urinary Ca2+
24-hour urinary Ca2+
A 24-hour urinary Ca2+ excretion is used to assess the risk of renal stones and to differentiate PHPT from familial hypocalciuric hypercalcemia (FHH). Patients with FHH have an abnormality in Ca2+ receptor gene expression in parathyroid cells and renal tubular cells that could lead to parathyroid-mediated hypercalcemia and hypocalciuria. FHH is differentiated from PHPT by calculating a 24-hour urinary Ca2+/Cr ratio. A value of <0.01 is diagnostic of FHH; whereas values >0.02 indicate PHPT. The test can be more accurate when the patient is on a normal Ca2+ and salt diet, when the estimated glomerular filtration rate is >60 mL/min/1.73 m2, and when the serum 25(OH) vitamin D level is >30 ng/dL.15 Adequate urine volume is necessary for the 24-hour Ca2+/Cr ratio to be valid.
Renal imaging
Kidney stones and high Ca2+ deposits in the kidneys are the common manifestations of PHPT. Renal X-ray, computed tomography (CT), or ultrasonography are recommended in the evaluation of patients with PHPT. An incidental finding of either kidney stones or high Ca2+ deposits in the kidneys is an indication for surgery.10
Bone density/DEXA (dual energy X-ray absorptiometry) scan with a vertebral fracture assessment (VFA)
Asymptomatic PHPT individuals with osteoporosis (T-score < 2.5) or vertebral compression fracture benefit from surgical management.10 It is essential to obtain densitometry at 3 sites: the lumbar spine, the hip, and the distal third of the radius. Due to differing amounts of cortical and cancellous bone at the 3 sites and the differential effects of PTH on the cortical and cancellous bone, measurement at all 3 sites allows a clear estimation of the severity of the hyperparathyroid process on the skeleton.16 Therefore, consider measuring serum PTH if the patient has severe osteoporosis or fragility fractures that cannot be explained or that are unresponsive to treatment.
Management
The primary modality of treatment in PHPT is parathyroidectomy. The benefits are many, including an increase in bone mineral density (BMD) and reduction in fractures and kidney stones.10 With modern imaging and intra-operative PTH measurement, the success of minimally invasive parathyroidectomy is high in experienced hands. Patients with PHPT should be referred to an endocrinologist before surgery.
Surgery
Consider surgery if the patient meets any one of the following criteria:
1) overt clinical manifestations (stones, fractures)
2) serum Ca2+ >1 mg/dL above the upper limit of normal
3) Cr clearance <60 mL/min
4) low BMD with a T score ≤2.5 at any site
5) age <50 years
6) uncertain prospect for follow-up.
Continue to: Perform imaging before surgery to identify...
Perform imaging before surgery to identify the overactive parathyroid glands. Ultrasound can detect enlargement of the parathyroid glands. A sestamibi scan, which measures the uptake of Tc99-sestamibi by the parathyroid glands, reflects the activity of the parathyroid glands. In cases of nonlocalization by these 2 modalities, other imaging techniques like 4D CT scan and contrast-enhanced ultrasound can be used. Of note: Imaging is used for localization, but not for diagnosis.
Intra-operative PTH measurement has added to the efficacy of minimally invasive parathyroidectomy. A drop in PTH of >50% after 10 to 15 minutes of excising the gland is considered to be positive.10
Medication management
Monitor patients who refuse surgery or those who do not meet the criteria after surgery. Serum Ca2+ and PTH are monitored annually. DEXA scan needs to be repeated every 1 to 2 years based on the clinical picture. Also assess patients for any fragility fractures and renal endpoints. Recommend taking vitamin D to keep the level above 20 ng/dL.10 Ca2+ intake should follow normally recommended guidelines.
Bisphosphonates are primarily used for the treatment of osteoporosis accompanying PHPT. They decrease bone resorption and, to a lesser extent, bone formation. Alendronate increases BMD at the lumbar spine, but does not have much effect on Ca2+ and PTH levels.
Calcimimetics act by mimicking the effects of Ca2+ on the Ca2+ receptors present on the surface of the parathyroid cells. Therefore, calcimimetics reduce the level of parathyroid hormone and Ca2+ levels. (Long-term benefits have not been established.) Bisphosphonates are prescribed for osteoporosis and calcimimetics for hypercalcemia.10
Continue to: Conclusion
Conclusion
Although largely asymptomatic, consider PHPT when patients present with unexplained kidney stones, osteoporosis, or any nonspecific symptoms described earlier. PHPT is diagnosed by detecting an inappropriately high or normal PTH in relation to the Ca2+ level. Medications need to be reviewed, and conditions such as FHH that produce similar symptoms need to be ruled out. Measurement of 25(OH) vitamin D levels is recommended in all patients with PHPT.
Parathyroidectomy is the definitive form of treatment and should be offered to patients who meet any one of the surgical criteria, as described earlier. It can also be offered to patients who do not meet the criteria if they prefer. It is known to decrease the risk of kidney stones and osteoporosis. Medical therapy is primarily for patients who do not meet the criteria as mentioned earlier and for those who cannot and/or are unwilling to undergo surgery.
CORRESPONDENCE
Padmaja Sanapureddy, MD, Department of Primary Care and Medicine, G.V. (Sonny) Montgomery VA Medical Center, 1500 E Woodrow Wilson Ave, Jackson, MS 39216; [email protected].
1. Griebeler ML, Kearns AE, Ryu E, et al. Secular trends in the incidence of primary hyperparathyroidism over five decades (1965-2010). Bone. 2015;73:1-7.
2. Melmed S, Polonsky, KS, Larsen PR, et al. Williams Textbook of Endocrinology: Hormones and Disorders of Mineral Metabolism, 12th ed. Philadelphia, PA: Elsevier Inc, 2011:1262-1263.
3. Assadi F. Hypercalcemia: an evidence-based approach to clinical cases. Iran J Kidney Dis. 2009;3(2):71-79.
4. Bilezikian JP, Cusano NE, Khan AA, et al. Primary hyperparathyroidism. Nat Rev Dis Primers. 2016;19;2:16033.
5. Roman S, Sosa JA. Psychiatric and cognitive aspects of primary hyperparathyroidism. Curr Opin Oncol. 2007;19:1-5.
6. Berkow JW, Fine BS, Zimmerman LE. Unusual ocular calcification in hyperparathyroidism. Am J Ophthalmol. 1968;66:812-824.
7. Carroll MF, Schade DS. A practical approach to hypercalcemia. Am Fam Physician. 2003;67:1959-1966.
8. Ong GSY, Walsh JP, Stuckey BGA, et al. The importance of measuring ionized calcium in characterizing calcium status and diagnosing primary hyperparathyroidism. J Clin Endocrinol Metab. 2012;97:3138-3145.
9. Silverberg SJ, Bilezikian JP. “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab. 2003;88:5348-5352.
10. Eastell R, Brandi ML, Costa AG, et al. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99:3570-3579.
11. Boudou P, Ibrahim F, Cormier C, et al. Third- or second-generation parathyroid hormone assays: a remaining debate in the diagnosis of primary hyperparathyroidism. J Clin Endocrinol Metab. 2005;90:6370-6372.
12. Carnevale V, Dionisi S, Nofroni I, et al. Potential clinical utility of a new IRMA for parathyroid hormone in postmenopausal patients with primary hyperparathyroidism. Clin Chem. 2004;50:626-631.
13. Jameson JL, De Groot L. Endocrinology: Adult and Pediatric. 7thed. Philadelphia, PA: Elsevier Inc, 2016:1109.
14. Tebben PJ, Singh RJ, Kumar R. Vitamin d-mediated hypercalcemia: mechanisms, diagnosis and treatment. Endocr Rev. 2016;37:521-547.
15. Shinall MC Jr, Dahir KM, Broome JT. Differentiating familial hypocalciuric hypercalcemia from primary hyperparathyroidism. Endocr Pract. 2013;19:697-702.
16. Castellano E, Attanasio R, Gianotti L, et al. Forearm DXA increases the rate of patients with asymptomatic primary hyperparathyroidism meeting surgical criteria. J Clin Endocrinol Metab. 2016;101:2728-2732.
Since the advent of multichannel serum chemistry screening in the 1970s, large numbers of asymptomatic cases of primary hyperparathyroidism (PHPT) have been discovered. The clinical spectrum of the disease has changed from the classic “moans, groans, bones, and stones” to an asymptomatic and subtle presentation of hypercalcemia.1,2 PHPT and malignancy are the most common causes for hypercalcemia, accounting for 90% of cases.3 In the United States, the estimated incidence of PHPT between 1998 and 2010 was about 50 per 100,000 person-years. Most patients with PHPT are older women (ages >50 years) who are asymptomatic at the time of diagnosis.1
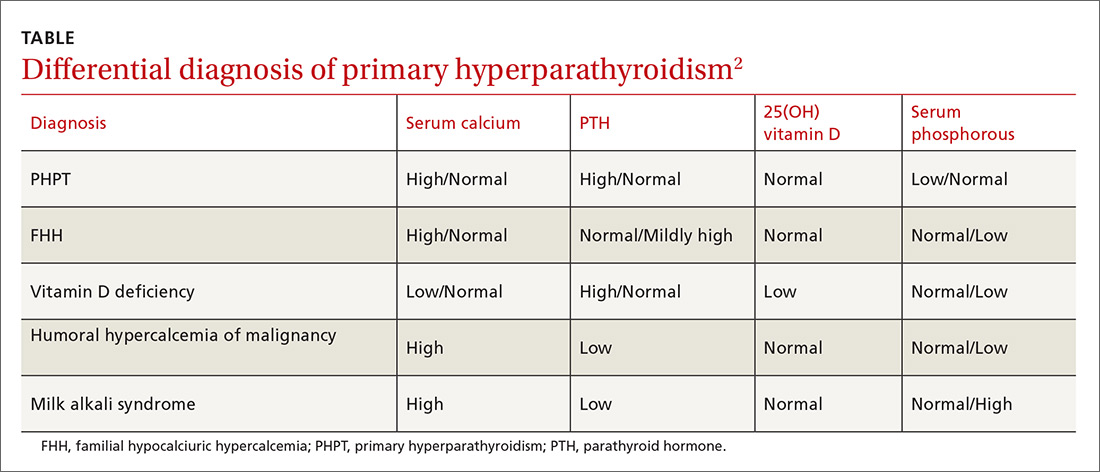
Vigilance needed in primary care. PHPT is slowly progressive, and the patient might accept symptoms as a process of aging. Therefore, it is essential that primary care physicians (PCPs) be aware of the diagnostic and management options. A systematic approach to the diagnosis of PHPT helps differentiate the causes of hypercalcemia (TABLE2; FIGURE2). But before we discuss PHPT diagnostic clues, it’s helpful to quickly review the workings of the parathyroid glands.
How the glands work, what can go wrong
Parathyroid hormone (PTH) is secreted by 4 pea-sized parathyroid glands located posterior to the thyroid. PTH regulates the levels of calcium (Ca2+) and phosphorous and controls the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D by activating the enzyme 1 alpha-hydroxylase.
PHPT is regarded as an abnormal secretion of PTH that does not correlate with the levels of Ca2+ in the blood.1 Eighty percent of PHPT is due to a solitary adenoma in one of the parathyroid glands, 2% to 4% is secondary to multiple parathyroid adenomas, 15% is due to parathyroid hyperplasia, and 0.5% due to parathyroid carcinoma.4
Nonspecific symptomsare subtle clues of PHPT
Patients with PHPT can present with nonspecific symptoms, such as weakness, fatigue, anorexia, polyuria, polydipsia, bone and joint pain, mild depression, and mild cognitive or neuromuscular dysfunction.5 A careful history is essential to elicit these symptoms, as the patient may attribute these to aging or other causes. PHPT should also be considered when patients present with kidney stones, unexplained osteoporosis, or fragility fractures. A physical examination is seldom helpful, as parathyroid adenomas are hardly ever palpable. A slit-lamp examination may reveal corneal diseases in rare cases of hypercalcemia.6
Which lab tests, imaging should you order?
Serum Ca2+
Repeat measurements of serum Ca2+ to confirm hypercalcemia. Volume depletion, underlying malignancy, medications such as hydrochlorothiazide, lithium, and excess intake of Ca2+ carbonate can cause hypercalcemia.7 Therefore, a review of the patients’ home medications and dietary preferences in the evaluation of hypercalcemia is essential. The 2 most common causes of hypercalcemia are hyperparathyroidism and hypercalcemia of malignancy.
For hypercalcemia, establish a differential diagnosis by measuring intact PTH. An increased serum Ca2+ level along with an elevated PTH concentration should suggest PTH-dependent hypercalcemia, whereas hypercalcemia with suppressed or low-normal PTH values should suggest PTH-independent hypercalcemia (granulomatous disorders, hypercalcemia of malignancy).
Continue to: Hypercalcemia of malignancy is due to...
Hypercalcemia of malignancy is due to increased production of parathyroid hormone-related peptide from various tumor cells that initiate bone resorption and increased renal Ca2+ absorption. It can also be due to osteolysis from bone metastasis.7 It is generally severe and is a common cause of hypercalcemia in the inpatient setting.
Meticulous evaluation is vital to diagnose PHPT. Measurement of serum ionized Ca2+ reflects the biologically active Ca2+. Studies by Ong and colleagues suggest that about 24% of patients with the histologically proven parathyroid disease had isolated ionized hypercalcemia.8 It is also an important adjunct to diagnose the presumed normocalcemic PHPT in which both the ionized Ca2+ levels and serum total Ca2+ levels should be normal.9
In patients with hypoalbuminemia, a corrected serum Ca2+ is calculated using the equation: corrected Ca2+ = [0.8 × (normal albumin-patient’s albumin)] + serum Ca2+ level.
Serum PTH
Second-generation PTH assays (intact PTH) and third-generation PTH assays (bioactive PTH) are equally reliable in diagnosing PHPT.10 The results obtained with intact and bioactive PTH assays are highly correlated. Several studies have found no improvement in diagnostic accuracy when using the bioactive PTH assay.11,12
Serum PTH can be low, normal, or elevated in hypercalcemia. Hypercalcemia with a high PTH level is parathyroid-dependent hypercalcemia, whereas hypercalcemia with a suppressed PTH level is considered parathyroid-independent.
Continue to: Serum 25(OH) vitamin D
Serum 25(OH) vitamin D
Vitamin D levels are normal in PHPT and normocalcemic PHPT. However, measuring 25(OH) vitamin D in all patients with suspected PHPT is recommended to evaluate for secondary hyperparathyroidism that is due to hypocalcemia or renal failure, which can occur concomitantly with PHPT.
Normocalcemic PHPT can be differentiated from secondary hyperparathyroidism of chronic kidney disease by measuring the 1,25(OH)2 vitamin D level; it will be low in secondary hyperparathyroidism.4
Serum 1,25(OH)2 vitamin D
1,25(OH)2 vitaminD levels are elevated in about one-third of patients with PHPT, as PTH stimulates the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D.13 Although this is not a routine test, it is useful in the evaluation of parathyroid-independent hypercalcemia caused by granulomatous disease, such as sarcoidosis where there is an autonomous production of 1,25(OH)2 vitamin D leading to hypercalcemia.14
Serum creatinine and estimated glomerular filtration rate
Serum creatinine (Cr) helps assess renal function. Reduction in serum Cr clearance to <60 mL/min with no other underlying cause is an indication for parathyroidectomy.10
Serum phosphorous
PTH increases the excretion of phosphorous by inhibiting reabsorption from the proximal tubule. Therefore, serum phosphorus tends to be in the lower range of normal in PHPT, but hypophosphatemia is present in less than a quarter of patients.4
Continue to: 24-hour urinary Ca2+
24-hour urinary Ca2+
A 24-hour urinary Ca2+ excretion is used to assess the risk of renal stones and to differentiate PHPT from familial hypocalciuric hypercalcemia (FHH). Patients with FHH have an abnormality in Ca2+ receptor gene expression in parathyroid cells and renal tubular cells that could lead to parathyroid-mediated hypercalcemia and hypocalciuria. FHH is differentiated from PHPT by calculating a 24-hour urinary Ca2+/Cr ratio. A value of <0.01 is diagnostic of FHH; whereas values >0.02 indicate PHPT. The test can be more accurate when the patient is on a normal Ca2+ and salt diet, when the estimated glomerular filtration rate is >60 mL/min/1.73 m2, and when the serum 25(OH) vitamin D level is >30 ng/dL.15 Adequate urine volume is necessary for the 24-hour Ca2+/Cr ratio to be valid.
Renal imaging
Kidney stones and high Ca2+ deposits in the kidneys are the common manifestations of PHPT. Renal X-ray, computed tomography (CT), or ultrasonography are recommended in the evaluation of patients with PHPT. An incidental finding of either kidney stones or high Ca2+ deposits in the kidneys is an indication for surgery.10
Bone density/DEXA (dual energy X-ray absorptiometry) scan with a vertebral fracture assessment (VFA)
Asymptomatic PHPT individuals with osteoporosis (T-score < 2.5) or vertebral compression fracture benefit from surgical management.10 It is essential to obtain densitometry at 3 sites: the lumbar spine, the hip, and the distal third of the radius. Due to differing amounts of cortical and cancellous bone at the 3 sites and the differential effects of PTH on the cortical and cancellous bone, measurement at all 3 sites allows a clear estimation of the severity of the hyperparathyroid process on the skeleton.16 Therefore, consider measuring serum PTH if the patient has severe osteoporosis or fragility fractures that cannot be explained or that are unresponsive to treatment.
Management
The primary modality of treatment in PHPT is parathyroidectomy. The benefits are many, including an increase in bone mineral density (BMD) and reduction in fractures and kidney stones.10 With modern imaging and intra-operative PTH measurement, the success of minimally invasive parathyroidectomy is high in experienced hands. Patients with PHPT should be referred to an endocrinologist before surgery.
Surgery
Consider surgery if the patient meets any one of the following criteria:
1) overt clinical manifestations (stones, fractures)
2) serum Ca2+ >1 mg/dL above the upper limit of normal
3) Cr clearance <60 mL/min
4) low BMD with a T score ≤2.5 at any site
5) age <50 years
6) uncertain prospect for follow-up.
Continue to: Perform imaging before surgery to identify...
Perform imaging before surgery to identify the overactive parathyroid glands. Ultrasound can detect enlargement of the parathyroid glands. A sestamibi scan, which measures the uptake of Tc99-sestamibi by the parathyroid glands, reflects the activity of the parathyroid glands. In cases of nonlocalization by these 2 modalities, other imaging techniques like 4D CT scan and contrast-enhanced ultrasound can be used. Of note: Imaging is used for localization, but not for diagnosis.
Intra-operative PTH measurement has added to the efficacy of minimally invasive parathyroidectomy. A drop in PTH of >50% after 10 to 15 minutes of excising the gland is considered to be positive.10
Medication management
Monitor patients who refuse surgery or those who do not meet the criteria after surgery. Serum Ca2+ and PTH are monitored annually. DEXA scan needs to be repeated every 1 to 2 years based on the clinical picture. Also assess patients for any fragility fractures and renal endpoints. Recommend taking vitamin D to keep the level above 20 ng/dL.10 Ca2+ intake should follow normally recommended guidelines.
Bisphosphonates are primarily used for the treatment of osteoporosis accompanying PHPT. They decrease bone resorption and, to a lesser extent, bone formation. Alendronate increases BMD at the lumbar spine, but does not have much effect on Ca2+ and PTH levels.
Calcimimetics act by mimicking the effects of Ca2+ on the Ca2+ receptors present on the surface of the parathyroid cells. Therefore, calcimimetics reduce the level of parathyroid hormone and Ca2+ levels. (Long-term benefits have not been established.) Bisphosphonates are prescribed for osteoporosis and calcimimetics for hypercalcemia.10
Continue to: Conclusion
Conclusion
Although largely asymptomatic, consider PHPT when patients present with unexplained kidney stones, osteoporosis, or any nonspecific symptoms described earlier. PHPT is diagnosed by detecting an inappropriately high or normal PTH in relation to the Ca2+ level. Medications need to be reviewed, and conditions such as FHH that produce similar symptoms need to be ruled out. Measurement of 25(OH) vitamin D levels is recommended in all patients with PHPT.
Parathyroidectomy is the definitive form of treatment and should be offered to patients who meet any one of the surgical criteria, as described earlier. It can also be offered to patients who do not meet the criteria if they prefer. It is known to decrease the risk of kidney stones and osteoporosis. Medical therapy is primarily for patients who do not meet the criteria as mentioned earlier and for those who cannot and/or are unwilling to undergo surgery.
CORRESPONDENCE
Padmaja Sanapureddy, MD, Department of Primary Care and Medicine, G.V. (Sonny) Montgomery VA Medical Center, 1500 E Woodrow Wilson Ave, Jackson, MS 39216; [email protected].
Since the advent of multichannel serum chemistry screening in the 1970s, large numbers of asymptomatic cases of primary hyperparathyroidism (PHPT) have been discovered. The clinical spectrum of the disease has changed from the classic “moans, groans, bones, and stones” to an asymptomatic and subtle presentation of hypercalcemia.1,2 PHPT and malignancy are the most common causes for hypercalcemia, accounting for 90% of cases.3 In the United States, the estimated incidence of PHPT between 1998 and 2010 was about 50 per 100,000 person-years. Most patients with PHPT are older women (ages >50 years) who are asymptomatic at the time of diagnosis.1
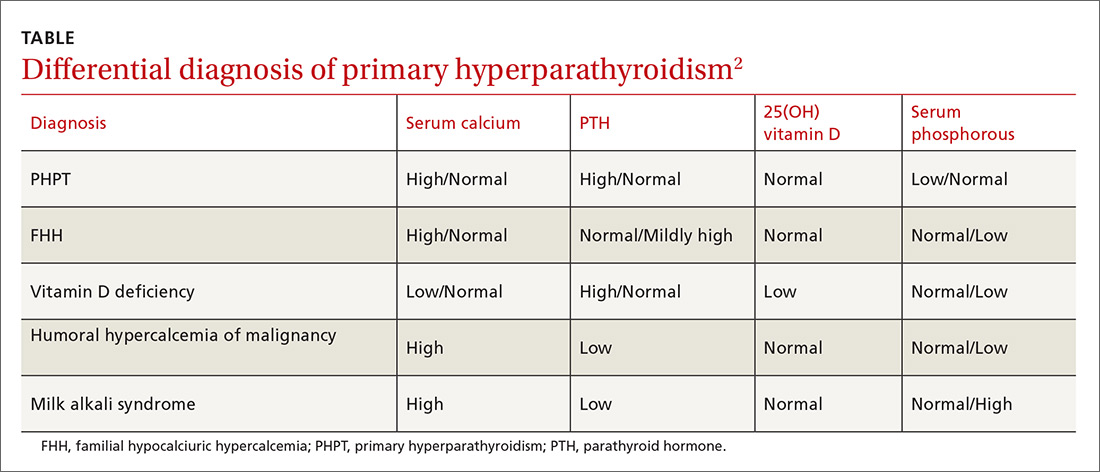
Vigilance needed in primary care. PHPT is slowly progressive, and the patient might accept symptoms as a process of aging. Therefore, it is essential that primary care physicians (PCPs) be aware of the diagnostic and management options. A systematic approach to the diagnosis of PHPT helps differentiate the causes of hypercalcemia (TABLE2; FIGURE2). But before we discuss PHPT diagnostic clues, it’s helpful to quickly review the workings of the parathyroid glands.
How the glands work, what can go wrong
Parathyroid hormone (PTH) is secreted by 4 pea-sized parathyroid glands located posterior to the thyroid. PTH regulates the levels of calcium (Ca2+) and phosphorous and controls the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D by activating the enzyme 1 alpha-hydroxylase.
PHPT is regarded as an abnormal secretion of PTH that does not correlate with the levels of Ca2+ in the blood.1 Eighty percent of PHPT is due to a solitary adenoma in one of the parathyroid glands, 2% to 4% is secondary to multiple parathyroid adenomas, 15% is due to parathyroid hyperplasia, and 0.5% due to parathyroid carcinoma.4
Nonspecific symptomsare subtle clues of PHPT
Patients with PHPT can present with nonspecific symptoms, such as weakness, fatigue, anorexia, polyuria, polydipsia, bone and joint pain, mild depression, and mild cognitive or neuromuscular dysfunction.5 A careful history is essential to elicit these symptoms, as the patient may attribute these to aging or other causes. PHPT should also be considered when patients present with kidney stones, unexplained osteoporosis, or fragility fractures. A physical examination is seldom helpful, as parathyroid adenomas are hardly ever palpable. A slit-lamp examination may reveal corneal diseases in rare cases of hypercalcemia.6
Which lab tests, imaging should you order?
Serum Ca2+
Repeat measurements of serum Ca2+ to confirm hypercalcemia. Volume depletion, underlying malignancy, medications such as hydrochlorothiazide, lithium, and excess intake of Ca2+ carbonate can cause hypercalcemia.7 Therefore, a review of the patients’ home medications and dietary preferences in the evaluation of hypercalcemia is essential. The 2 most common causes of hypercalcemia are hyperparathyroidism and hypercalcemia of malignancy.
For hypercalcemia, establish a differential diagnosis by measuring intact PTH. An increased serum Ca2+ level along with an elevated PTH concentration should suggest PTH-dependent hypercalcemia, whereas hypercalcemia with suppressed or low-normal PTH values should suggest PTH-independent hypercalcemia (granulomatous disorders, hypercalcemia of malignancy).
Continue to: Hypercalcemia of malignancy is due to...
Hypercalcemia of malignancy is due to increased production of parathyroid hormone-related peptide from various tumor cells that initiate bone resorption and increased renal Ca2+ absorption. It can also be due to osteolysis from bone metastasis.7 It is generally severe and is a common cause of hypercalcemia in the inpatient setting.
Meticulous evaluation is vital to diagnose PHPT. Measurement of serum ionized Ca2+ reflects the biologically active Ca2+. Studies by Ong and colleagues suggest that about 24% of patients with the histologically proven parathyroid disease had isolated ionized hypercalcemia.8 It is also an important adjunct to diagnose the presumed normocalcemic PHPT in which both the ionized Ca2+ levels and serum total Ca2+ levels should be normal.9
In patients with hypoalbuminemia, a corrected serum Ca2+ is calculated using the equation: corrected Ca2+ = [0.8 × (normal albumin-patient’s albumin)] + serum Ca2+ level.
Serum PTH
Second-generation PTH assays (intact PTH) and third-generation PTH assays (bioactive PTH) are equally reliable in diagnosing PHPT.10 The results obtained with intact and bioactive PTH assays are highly correlated. Several studies have found no improvement in diagnostic accuracy when using the bioactive PTH assay.11,12
Serum PTH can be low, normal, or elevated in hypercalcemia. Hypercalcemia with a high PTH level is parathyroid-dependent hypercalcemia, whereas hypercalcemia with a suppressed PTH level is considered parathyroid-independent.
Continue to: Serum 25(OH) vitamin D
Serum 25(OH) vitamin D
Vitamin D levels are normal in PHPT and normocalcemic PHPT. However, measuring 25(OH) vitamin D in all patients with suspected PHPT is recommended to evaluate for secondary hyperparathyroidism that is due to hypocalcemia or renal failure, which can occur concomitantly with PHPT.
Normocalcemic PHPT can be differentiated from secondary hyperparathyroidism of chronic kidney disease by measuring the 1,25(OH)2 vitamin D level; it will be low in secondary hyperparathyroidism.4
Serum 1,25(OH)2 vitamin D
1,25(OH)2 vitaminD levels are elevated in about one-third of patients with PHPT, as PTH stimulates the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D.13 Although this is not a routine test, it is useful in the evaluation of parathyroid-independent hypercalcemia caused by granulomatous disease, such as sarcoidosis where there is an autonomous production of 1,25(OH)2 vitamin D leading to hypercalcemia.14
Serum creatinine and estimated glomerular filtration rate
Serum creatinine (Cr) helps assess renal function. Reduction in serum Cr clearance to <60 mL/min with no other underlying cause is an indication for parathyroidectomy.10
Serum phosphorous
PTH increases the excretion of phosphorous by inhibiting reabsorption from the proximal tubule. Therefore, serum phosphorus tends to be in the lower range of normal in PHPT, but hypophosphatemia is present in less than a quarter of patients.4
Continue to: 24-hour urinary Ca2+
24-hour urinary Ca2+
A 24-hour urinary Ca2+ excretion is used to assess the risk of renal stones and to differentiate PHPT from familial hypocalciuric hypercalcemia (FHH). Patients with FHH have an abnormality in Ca2+ receptor gene expression in parathyroid cells and renal tubular cells that could lead to parathyroid-mediated hypercalcemia and hypocalciuria. FHH is differentiated from PHPT by calculating a 24-hour urinary Ca2+/Cr ratio. A value of <0.01 is diagnostic of FHH; whereas values >0.02 indicate PHPT. The test can be more accurate when the patient is on a normal Ca2+ and salt diet, when the estimated glomerular filtration rate is >60 mL/min/1.73 m2, and when the serum 25(OH) vitamin D level is >30 ng/dL.15 Adequate urine volume is necessary for the 24-hour Ca2+/Cr ratio to be valid.
Renal imaging
Kidney stones and high Ca2+ deposits in the kidneys are the common manifestations of PHPT. Renal X-ray, computed tomography (CT), or ultrasonography are recommended in the evaluation of patients with PHPT. An incidental finding of either kidney stones or high Ca2+ deposits in the kidneys is an indication for surgery.10
Bone density/DEXA (dual energy X-ray absorptiometry) scan with a vertebral fracture assessment (VFA)
Asymptomatic PHPT individuals with osteoporosis (T-score < 2.5) or vertebral compression fracture benefit from surgical management.10 It is essential to obtain densitometry at 3 sites: the lumbar spine, the hip, and the distal third of the radius. Due to differing amounts of cortical and cancellous bone at the 3 sites and the differential effects of PTH on the cortical and cancellous bone, measurement at all 3 sites allows a clear estimation of the severity of the hyperparathyroid process on the skeleton.16 Therefore, consider measuring serum PTH if the patient has severe osteoporosis or fragility fractures that cannot be explained or that are unresponsive to treatment.
Management
The primary modality of treatment in PHPT is parathyroidectomy. The benefits are many, including an increase in bone mineral density (BMD) and reduction in fractures and kidney stones.10 With modern imaging and intra-operative PTH measurement, the success of minimally invasive parathyroidectomy is high in experienced hands. Patients with PHPT should be referred to an endocrinologist before surgery.
Surgery
Consider surgery if the patient meets any one of the following criteria:
1) overt clinical manifestations (stones, fractures)
2) serum Ca2+ >1 mg/dL above the upper limit of normal
3) Cr clearance <60 mL/min
4) low BMD with a T score ≤2.5 at any site
5) age <50 years
6) uncertain prospect for follow-up.
Continue to: Perform imaging before surgery to identify...
Perform imaging before surgery to identify the overactive parathyroid glands. Ultrasound can detect enlargement of the parathyroid glands. A sestamibi scan, which measures the uptake of Tc99-sestamibi by the parathyroid glands, reflects the activity of the parathyroid glands. In cases of nonlocalization by these 2 modalities, other imaging techniques like 4D CT scan and contrast-enhanced ultrasound can be used. Of note: Imaging is used for localization, but not for diagnosis.
Intra-operative PTH measurement has added to the efficacy of minimally invasive parathyroidectomy. A drop in PTH of >50% after 10 to 15 minutes of excising the gland is considered to be positive.10
Medication management
Monitor patients who refuse surgery or those who do not meet the criteria after surgery. Serum Ca2+ and PTH are monitored annually. DEXA scan needs to be repeated every 1 to 2 years based on the clinical picture. Also assess patients for any fragility fractures and renal endpoints. Recommend taking vitamin D to keep the level above 20 ng/dL.10 Ca2+ intake should follow normally recommended guidelines.
Bisphosphonates are primarily used for the treatment of osteoporosis accompanying PHPT. They decrease bone resorption and, to a lesser extent, bone formation. Alendronate increases BMD at the lumbar spine, but does not have much effect on Ca2+ and PTH levels.
Calcimimetics act by mimicking the effects of Ca2+ on the Ca2+ receptors present on the surface of the parathyroid cells. Therefore, calcimimetics reduce the level of parathyroid hormone and Ca2+ levels. (Long-term benefits have not been established.) Bisphosphonates are prescribed for osteoporosis and calcimimetics for hypercalcemia.10
Continue to: Conclusion
Conclusion
Although largely asymptomatic, consider PHPT when patients present with unexplained kidney stones, osteoporosis, or any nonspecific symptoms described earlier. PHPT is diagnosed by detecting an inappropriately high or normal PTH in relation to the Ca2+ level. Medications need to be reviewed, and conditions such as FHH that produce similar symptoms need to be ruled out. Measurement of 25(OH) vitamin D levels is recommended in all patients with PHPT.
Parathyroidectomy is the definitive form of treatment and should be offered to patients who meet any one of the surgical criteria, as described earlier. It can also be offered to patients who do not meet the criteria if they prefer. It is known to decrease the risk of kidney stones and osteoporosis. Medical therapy is primarily for patients who do not meet the criteria as mentioned earlier and for those who cannot and/or are unwilling to undergo surgery.
CORRESPONDENCE
Padmaja Sanapureddy, MD, Department of Primary Care and Medicine, G.V. (Sonny) Montgomery VA Medical Center, 1500 E Woodrow Wilson Ave, Jackson, MS 39216; [email protected].
1. Griebeler ML, Kearns AE, Ryu E, et al. Secular trends in the incidence of primary hyperparathyroidism over five decades (1965-2010). Bone. 2015;73:1-7.
2. Melmed S, Polonsky, KS, Larsen PR, et al. Williams Textbook of Endocrinology: Hormones and Disorders of Mineral Metabolism, 12th ed. Philadelphia, PA: Elsevier Inc, 2011:1262-1263.
3. Assadi F. Hypercalcemia: an evidence-based approach to clinical cases. Iran J Kidney Dis. 2009;3(2):71-79.
4. Bilezikian JP, Cusano NE, Khan AA, et al. Primary hyperparathyroidism. Nat Rev Dis Primers. 2016;19;2:16033.
5. Roman S, Sosa JA. Psychiatric and cognitive aspects of primary hyperparathyroidism. Curr Opin Oncol. 2007;19:1-5.
6. Berkow JW, Fine BS, Zimmerman LE. Unusual ocular calcification in hyperparathyroidism. Am J Ophthalmol. 1968;66:812-824.
7. Carroll MF, Schade DS. A practical approach to hypercalcemia. Am Fam Physician. 2003;67:1959-1966.
8. Ong GSY, Walsh JP, Stuckey BGA, et al. The importance of measuring ionized calcium in characterizing calcium status and diagnosing primary hyperparathyroidism. J Clin Endocrinol Metab. 2012;97:3138-3145.
9. Silverberg SJ, Bilezikian JP. “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab. 2003;88:5348-5352.
10. Eastell R, Brandi ML, Costa AG, et al. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99:3570-3579.
11. Boudou P, Ibrahim F, Cormier C, et al. Third- or second-generation parathyroid hormone assays: a remaining debate in the diagnosis of primary hyperparathyroidism. J Clin Endocrinol Metab. 2005;90:6370-6372.
12. Carnevale V, Dionisi S, Nofroni I, et al. Potential clinical utility of a new IRMA for parathyroid hormone in postmenopausal patients with primary hyperparathyroidism. Clin Chem. 2004;50:626-631.
13. Jameson JL, De Groot L. Endocrinology: Adult and Pediatric. 7thed. Philadelphia, PA: Elsevier Inc, 2016:1109.
14. Tebben PJ, Singh RJ, Kumar R. Vitamin d-mediated hypercalcemia: mechanisms, diagnosis and treatment. Endocr Rev. 2016;37:521-547.
15. Shinall MC Jr, Dahir KM, Broome JT. Differentiating familial hypocalciuric hypercalcemia from primary hyperparathyroidism. Endocr Pract. 2013;19:697-702.
16. Castellano E, Attanasio R, Gianotti L, et al. Forearm DXA increases the rate of patients with asymptomatic primary hyperparathyroidism meeting surgical criteria. J Clin Endocrinol Metab. 2016;101:2728-2732.
1. Griebeler ML, Kearns AE, Ryu E, et al. Secular trends in the incidence of primary hyperparathyroidism over five decades (1965-2010). Bone. 2015;73:1-7.
2. Melmed S, Polonsky, KS, Larsen PR, et al. Williams Textbook of Endocrinology: Hormones and Disorders of Mineral Metabolism, 12th ed. Philadelphia, PA: Elsevier Inc, 2011:1262-1263.
3. Assadi F. Hypercalcemia: an evidence-based approach to clinical cases. Iran J Kidney Dis. 2009;3(2):71-79.
4. Bilezikian JP, Cusano NE, Khan AA, et al. Primary hyperparathyroidism. Nat Rev Dis Primers. 2016;19;2:16033.
5. Roman S, Sosa JA. Psychiatric and cognitive aspects of primary hyperparathyroidism. Curr Opin Oncol. 2007;19:1-5.
6. Berkow JW, Fine BS, Zimmerman LE. Unusual ocular calcification in hyperparathyroidism. Am J Ophthalmol. 1968;66:812-824.
7. Carroll MF, Schade DS. A practical approach to hypercalcemia. Am Fam Physician. 2003;67:1959-1966.
8. Ong GSY, Walsh JP, Stuckey BGA, et al. The importance of measuring ionized calcium in characterizing calcium status and diagnosing primary hyperparathyroidism. J Clin Endocrinol Metab. 2012;97:3138-3145.
9. Silverberg SJ, Bilezikian JP. “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab. 2003;88:5348-5352.
10. Eastell R, Brandi ML, Costa AG, et al. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International Workshop. J Clin Endocrinol Metab. 2014;99:3570-3579.
11. Boudou P, Ibrahim F, Cormier C, et al. Third- or second-generation parathyroid hormone assays: a remaining debate in the diagnosis of primary hyperparathyroidism. J Clin Endocrinol Metab. 2005;90:6370-6372.
12. Carnevale V, Dionisi S, Nofroni I, et al. Potential clinical utility of a new IRMA for parathyroid hormone in postmenopausal patients with primary hyperparathyroidism. Clin Chem. 2004;50:626-631.
13. Jameson JL, De Groot L. Endocrinology: Adult and Pediatric. 7thed. Philadelphia, PA: Elsevier Inc, 2016:1109.
14. Tebben PJ, Singh RJ, Kumar R. Vitamin d-mediated hypercalcemia: mechanisms, diagnosis and treatment. Endocr Rev. 2016;37:521-547.
15. Shinall MC Jr, Dahir KM, Broome JT. Differentiating familial hypocalciuric hypercalcemia from primary hyperparathyroidism. Endocr Pract. 2013;19:697-702.
16. Castellano E, Attanasio R, Gianotti L, et al. Forearm DXA increases the rate of patients with asymptomatic primary hyperparathyroidism meeting surgical criteria. J Clin Endocrinol Metab. 2016;101:2728-2732.
PRACTICE RECOMMENDATIONS
› Evaluate suspected cases of primary hyperparathyroidism (PHPT) with serum total calcium, parathyroid hormone (PTH), creatinine, and 25-hydroxy vitamin D levels. A
› Consider 24-hour urine measurement of calcium and creatinine in patients undergoing evaluation for possible PHPT. A
› Obtain bone densitometry at the spine, hip, and distal radius in patients with PHPT. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
