User login
Ovarian teratoma (dermoid cyst) and encephalitis: A link to keep on your radar
CASE. Suspected teratoma-induced encephalitis
You are on call for your practice group, resting comfortably at home, reviewing tomorrow’s office schedule and wondering if your peaceful evening will be interrupted by a call from the hospital. At 9 pm, a neurologist calls and pleads for you to come to the hospital to evaluate a 25-year-old patient with encephalitis who is intubated in the intensive care unit (ICU). You immediately wonder, “Why call me about a case of encephalitis?”
The neurologist reports the following details. Over the 2 weeks preceding hospitalization, the patient developed progressive agitation, irritability, and hallucinations. She then had a seizure. She was brought to the hospital and was observed to be hypoventilating. She was sedated, intubated, and placed on mechanical ventilation.
Imaging studies were consistent with encephalitis. A screen for toxic substances and tests for viral and bacterial infection were negative. A spinal tap showed white blood cells (WBCs) in the cerebrospinal fluid (CSF).
Earlier in the afternoon serum and CSF sent to a reference laboratory returned positive for anti–N-methyl-D-aspartate (anti-NMDA)–receptor antibodies. Emergency pelvic ultrasonography was obtained, showing a 4-cm complex ovarian mass consistent with a teratoma. Based on these findings, the neurologist diagnosed teratoma-induced encephalitis.
The neurologist insists that you immediately operate on the patient to remove the teratoma.
What would you do in this hypothetical case?
OVARIAN TERATOMA AND ENCEPHALITIS—A CAUSAL LINK
Between 2005 and 2009, Dr. Josep Dalmau and colleagues in the Department of Neurology at the University of Pennsylvania published a series of papers documenting a link between encephalitis and ovarian teratomas.1-5 The pathophysiologic connection is thought to be the presence of tissue in the ovarian teratoma that stimulates the immune system to produce anti-NMDA-receptor (anti-NMDAR) antibodies. The anti-NMDAR antibodies, and/or the related B cells, then enter the central nervous system. It is hypothesized that the antibodies deplete cell-surface NMDA receptors on NMDA-receptor–rich neurons in the limbic system. This causes neuronal dysfunction, and over time, may cause permanent loss of neurons.
The antibody-induced abnormality in neuronal function produces a constellation of neuropsychiatric changes, including disturbances of memory, behavior, and cognition, and can trigger the onset of seizures. Hypoventilation may occur, and patients severely affected by the syndrome require sedation, intubation, and mechanical ventilation.
An observational link. Observations that support the mechanistic connection between teratoma-induced production of anti-NMDAR antibodies and encephalitis are as follows:
- In cases of encephalitis associated with an ovarian teratoma, histology often shows an intense WBC infiltrate in areas of the teratoma with neural tissue.6
- Tissue in the teratoma expresses the NMDA receptor.7
- In the syndrome of ovarian teratoma and encephalitis, elevated titers of anti-NMDAR antibodies are often present in serum and CSF.
- The areas of the brain affected by the encephalitis, including limbic and forebrain structures, express the NMDA receptor.
- Interventions that reduce levels of the anti-NMDAR antibody titer, including removal of the teratoma or immunotherapy, are often associated with a marked improvement in the clinical syndrome.
Awareness among ObGyns is valuable
The vast majority of ovarian teratomas never trigger the synthesis of anti-NMDAR antibodies or the development of a disabling encephalitis.8 However, the recognition that teratomas can cause encephalitis suggests that, if a teratoma is expectantly managed, the patient and her family should be alerted to report the new onset of symptoms, such as behavioral change, that may warrant neurologic evaluation.
In the California Encephalitis Project,9 of the 761 cases of encephalitis evaluated, the most common identifiable cause of the condition in women aged 30 years and younger was anti-NMDAR encephalitis. Enterovirus was a close second as a cause of encephalitis. Well-known causes of the condition, such as Herpes simplex 1, Varicella zoster, and West Nile virus were far less common.
HOW IS A DIAGNOSIS REACHED?
In many cases of encephalitis due to an ovarian teratoma, diagnosis is made by history, as well as physical examination consistent with:
- limbic encephalitis
- imaging studies that show encephalitis
- negative test results for viral, bacterial, and toxicologic causes of encephalitis
- evidence of WBCs in the CSF
- the presence of anti–NMDAR antibodies and an ovarian teratoma.
Neuropsychologic changes observed with this disease include agitation, mood lability, speech dysfunction, hallucinations, paranoia, hypersexuality, and seizures. Movement disorders are common in patients with this disease and include orofacial dyskinesias, unilateral dystonia, opisthotonus, chorea, rigidity, and catatonia. In many cases, a prodrome of fever and headache precede the development of the full syndrome. Both mature and immature teratomas can cause the syndrome.
Related Article: Skilled US imaging of the adnexae: Ovarian Neoplasms Ilan Timor-Tritsch, MD, and Steven R. Goldstein, MD (November 2010)
OPTIMAL TREATMENT
Encephalitis due to ovarian teratoma is treated by urgent removal of the teratoma. This is in combination with immune-modulating therapy, which may include intravenous immunoglobulin (IVIG), high-dose glucocorticoids, plasmapheresis, or rituximab (a monoclonal antibody targeted to the CD20 antigen on B lymphocytes).10,11
Although there is little evidence to support this clinical point, most neurologists passionately believe that once the diagnosis of ovarian teratoma–induced encephalitis is made, the teratoma should be urgently removed to help reduce the risk of permanent neurologic injury.
Challenging clinical issues
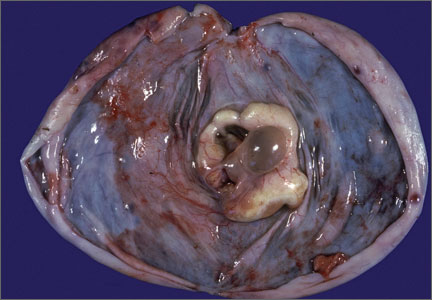
Resect the cyst or remove the ovary? The surgical approach to resecting the teratoma may either be complete ovarian cystectomy or oophorectomy. It is important to resect the teratoma in its entirety and avoid spilling the cyst contents into the peritoneal cavity. Based on these considerations, in women who have completed childbearing, an oophorectomy is often performed (FIGURE). For young patients, an ovarian cystectomy or oophorectomy are both suitable options.12
Intraoperative ultrasound can be helpful in confirming the presence of small teratomas and in guiding the surgeon to the correct location.13
Small teratomas. In cases of encephalitis induced by anti-NMDAR antibodies, the inciting ovarian teratoma can be very small, and not initially detected by ultrasonography.14,15 This creates a clinical challenge as, among women with anti-NMDAR encephalitis, only about half are reported to have ovarian teratomas. However, if microscopic teratomas could precipitate the syndrome, how is the physician to know which women without imaging evidence of a teratoma should have their ovaries surgically explored or removed?
In a case in which an occult teratoma is suspected to be the cause of anti-NMDAR encephalitis, a multidisciplinary team including a neurologist, radiologist, and gynecologist should confer to determine the best course of action. We should minimize the number of cases in which unnecessary oophorectomy is performed in the hope that a teratoma may be the cause of the encephalitis.
Ovarian teratoma but no anti-NMDAR antibodies. Some patients with encephalitis have a teratoma but no detectable anti-NMDAR antibodies. In these patients, teratoma removal may be associated with improvement in the encephalitis; however, the cause of the condition may be another type of anti-neuronal antibody that has yet to be identified.16 Women with encephalitis and an ovarian teratoma, and no evidence of infectious or toxicologic causes for the encephalitis, should be considered for teratoma removal.
CASE RESOLVED. Cyst resection contributes to recovery
You arrive at the hospital’s ICU, perform a physical examination, review the ultrasound, and confirm that the patient has an adnexal mass consistent with a teratoma. The anesthesiologist on call has agreed to provide an anesthetic.
You quickly search PubMed and discover that there are more than 180 publications reporting a link between encephalitis and ovarian teratoma, but only a small number are in the obstetrics and gynecology literature.
You take the patient to the operating room and resect the teratoma. The neurologist treats the patient with high-dose glucocorticoids. She recovers slowly, but her neurologic condition improves each day. On postoperative day 14 she is discharged home with a few remaining neurologic deficits. The patient and her family are amazed and grateful.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] or Dr. Barbieri at [email protected]
- Vitaliani R, Mason W, Ances B, Zwerdling T, Jian Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms and hypoventilation in ovarian teratoma. Ann Neurol. 2005;58(4):594–604.
- Ances BM, Vitaliani R, Taylor RA, et al. Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain. 2005;128(Pt 8):1764–1777.
- Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NDMA-receptor encephalitis: Case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7(12):1091–1098.
- Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66(1):11–18.
- Dabner M, McCluggage W, Bundell C, et al. Ovarian teratoma associated with anti-N-methyl-D-aspartate receptor encephalitis: A report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol. 2012;31(5): 29–37.
- Tachibana N, Shirakawa T, Ishii K, et al.
Expression of various glutamate receptors including N-methyl-D-aspartate receptor (NMDAR) in an ovarian teratoma removed from a young woman with anti-NMDAR encephalitis. Intern Med. 2010;49(19):2167–2173. - Mangler M, Trebesch de Perez I, Teegen B, et al. Seroprevalence of anti-N-methyl-D-aspartate receptor antibodies in women with ovarian teratoma. J Neurol. 2013;260(11):2831–2835.
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California encephalitis project. Clin Infect Dis. 2012;54(7):899–904.
- Pham HP, Daniel-Johnson JA, Stotler BA, Stephens H, Schwartz J. Therapeutic plasma exchange for the treatment of anti-NMDA-receptor encephalitis. J Clin Apher. 2011;26(6):320–325.
- Miya K, Takahashi Y, Mori H. Anti-NMDAR autoimmune encephalitis [published online ahead of print November 5, 2013]. Brain Dev. doi:10.1016/j.braindev.2013.10.005.
- Naoura I, Didelot A, Walker F, Luton D, Koskas M. Anti-N-methyl-D-aspartate receptor encephalitis complications ovarian teratomas: a case report. Am J Obstet Gynecol. 2011;205(4):e6–e8.
- Asai S, Ishimoto H, Yabuno, Asada H, Seki M, Iwata S. Laparoscopic cystectomy of ovarian teratoma in anti-NMDR encephalitis: 2 case reports. J Min Invas Gynecol. 2011;18(1):135–137.
- Tanyi J, Marsh E, Dalmau J, Chu C. Reversible paraneoplastic encephalitis in three patients with ovarian neoplasms. Acta Obstet Gynecol Scand. 2012;91(5):630–634.
- Boeck AL, Logemann F, Kraub T, et al. Ovarectomy despite negative imaging in anti-NMDA receptor encephalitis: Effective even late [published online ahead of print February 26, 2013]. Case Rep Neurol Med. doi:10.1155/2013/843192.
- Armangue T, Titulaer MJ, Sabater L, et al. A novel treatment-responsive encephalitis with frequent opsoclonus and teratoma [published online ahead of print April 24, 2013]. Ann Neurol. doi: 10.1002/ana.23917.
CASE. Suspected teratoma-induced encephalitis
You are on call for your practice group, resting comfortably at home, reviewing tomorrow’s office schedule and wondering if your peaceful evening will be interrupted by a call from the hospital. At 9 pm, a neurologist calls and pleads for you to come to the hospital to evaluate a 25-year-old patient with encephalitis who is intubated in the intensive care unit (ICU). You immediately wonder, “Why call me about a case of encephalitis?”
The neurologist reports the following details. Over the 2 weeks preceding hospitalization, the patient developed progressive agitation, irritability, and hallucinations. She then had a seizure. She was brought to the hospital and was observed to be hypoventilating. She was sedated, intubated, and placed on mechanical ventilation.
Imaging studies were consistent with encephalitis. A screen for toxic substances and tests for viral and bacterial infection were negative. A spinal tap showed white blood cells (WBCs) in the cerebrospinal fluid (CSF).
Earlier in the afternoon serum and CSF sent to a reference laboratory returned positive for anti–N-methyl-D-aspartate (anti-NMDA)–receptor antibodies. Emergency pelvic ultrasonography was obtained, showing a 4-cm complex ovarian mass consistent with a teratoma. Based on these findings, the neurologist diagnosed teratoma-induced encephalitis.
The neurologist insists that you immediately operate on the patient to remove the teratoma.
What would you do in this hypothetical case?
OVARIAN TERATOMA AND ENCEPHALITIS—A CAUSAL LINK
Between 2005 and 2009, Dr. Josep Dalmau and colleagues in the Department of Neurology at the University of Pennsylvania published a series of papers documenting a link between encephalitis and ovarian teratomas.1-5 The pathophysiologic connection is thought to be the presence of tissue in the ovarian teratoma that stimulates the immune system to produce anti-NMDA-receptor (anti-NMDAR) antibodies. The anti-NMDAR antibodies, and/or the related B cells, then enter the central nervous system. It is hypothesized that the antibodies deplete cell-surface NMDA receptors on NMDA-receptor–rich neurons in the limbic system. This causes neuronal dysfunction, and over time, may cause permanent loss of neurons.
The antibody-induced abnormality in neuronal function produces a constellation of neuropsychiatric changes, including disturbances of memory, behavior, and cognition, and can trigger the onset of seizures. Hypoventilation may occur, and patients severely affected by the syndrome require sedation, intubation, and mechanical ventilation.
An observational link. Observations that support the mechanistic connection between teratoma-induced production of anti-NMDAR antibodies and encephalitis are as follows:
- In cases of encephalitis associated with an ovarian teratoma, histology often shows an intense WBC infiltrate in areas of the teratoma with neural tissue.6
- Tissue in the teratoma expresses the NMDA receptor.7
- In the syndrome of ovarian teratoma and encephalitis, elevated titers of anti-NMDAR antibodies are often present in serum and CSF.
- The areas of the brain affected by the encephalitis, including limbic and forebrain structures, express the NMDA receptor.
- Interventions that reduce levels of the anti-NMDAR antibody titer, including removal of the teratoma or immunotherapy, are often associated with a marked improvement in the clinical syndrome.
Awareness among ObGyns is valuable
The vast majority of ovarian teratomas never trigger the synthesis of anti-NMDAR antibodies or the development of a disabling encephalitis.8 However, the recognition that teratomas can cause encephalitis suggests that, if a teratoma is expectantly managed, the patient and her family should be alerted to report the new onset of symptoms, such as behavioral change, that may warrant neurologic evaluation.
In the California Encephalitis Project,9 of the 761 cases of encephalitis evaluated, the most common identifiable cause of the condition in women aged 30 years and younger was anti-NMDAR encephalitis. Enterovirus was a close second as a cause of encephalitis. Well-known causes of the condition, such as Herpes simplex 1, Varicella zoster, and West Nile virus were far less common.
HOW IS A DIAGNOSIS REACHED?
In many cases of encephalitis due to an ovarian teratoma, diagnosis is made by history, as well as physical examination consistent with:
- limbic encephalitis
- imaging studies that show encephalitis
- negative test results for viral, bacterial, and toxicologic causes of encephalitis
- evidence of WBCs in the CSF
- the presence of anti–NMDAR antibodies and an ovarian teratoma.
Neuropsychologic changes observed with this disease include agitation, mood lability, speech dysfunction, hallucinations, paranoia, hypersexuality, and seizures. Movement disorders are common in patients with this disease and include orofacial dyskinesias, unilateral dystonia, opisthotonus, chorea, rigidity, and catatonia. In many cases, a prodrome of fever and headache precede the development of the full syndrome. Both mature and immature teratomas can cause the syndrome.
Related Article: Skilled US imaging of the adnexae: Ovarian Neoplasms Ilan Timor-Tritsch, MD, and Steven R. Goldstein, MD (November 2010)
OPTIMAL TREATMENT
Encephalitis due to ovarian teratoma is treated by urgent removal of the teratoma. This is in combination with immune-modulating therapy, which may include intravenous immunoglobulin (IVIG), high-dose glucocorticoids, plasmapheresis, or rituximab (a monoclonal antibody targeted to the CD20 antigen on B lymphocytes).10,11
Although there is little evidence to support this clinical point, most neurologists passionately believe that once the diagnosis of ovarian teratoma–induced encephalitis is made, the teratoma should be urgently removed to help reduce the risk of permanent neurologic injury.
Challenging clinical issues
Resect the cyst or remove the ovary? The surgical approach to resecting the teratoma may either be complete ovarian cystectomy or oophorectomy. It is important to resect the teratoma in its entirety and avoid spilling the cyst contents into the peritoneal cavity. Based on these considerations, in women who have completed childbearing, an oophorectomy is often performed (FIGURE). For young patients, an ovarian cystectomy or oophorectomy are both suitable options.12
Intraoperative ultrasound can be helpful in confirming the presence of small teratomas and in guiding the surgeon to the correct location.13
Small teratomas. In cases of encephalitis induced by anti-NMDAR antibodies, the inciting ovarian teratoma can be very small, and not initially detected by ultrasonography.14,15 This creates a clinical challenge as, among women with anti-NMDAR encephalitis, only about half are reported to have ovarian teratomas. However, if microscopic teratomas could precipitate the syndrome, how is the physician to know which women without imaging evidence of a teratoma should have their ovaries surgically explored or removed?
In a case in which an occult teratoma is suspected to be the cause of anti-NMDAR encephalitis, a multidisciplinary team including a neurologist, radiologist, and gynecologist should confer to determine the best course of action. We should minimize the number of cases in which unnecessary oophorectomy is performed in the hope that a teratoma may be the cause of the encephalitis.
Ovarian teratoma but no anti-NMDAR antibodies. Some patients with encephalitis have a teratoma but no detectable anti-NMDAR antibodies. In these patients, teratoma removal may be associated with improvement in the encephalitis; however, the cause of the condition may be another type of anti-neuronal antibody that has yet to be identified.16 Women with encephalitis and an ovarian teratoma, and no evidence of infectious or toxicologic causes for the encephalitis, should be considered for teratoma removal.
CASE RESOLVED. Cyst resection contributes to recovery
You arrive at the hospital’s ICU, perform a physical examination, review the ultrasound, and confirm that the patient has an adnexal mass consistent with a teratoma. The anesthesiologist on call has agreed to provide an anesthetic.
You quickly search PubMed and discover that there are more than 180 publications reporting a link between encephalitis and ovarian teratoma, but only a small number are in the obstetrics and gynecology literature.
You take the patient to the operating room and resect the teratoma. The neurologist treats the patient with high-dose glucocorticoids. She recovers slowly, but her neurologic condition improves each day. On postoperative day 14 she is discharged home with a few remaining neurologic deficits. The patient and her family are amazed and grateful.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] or Dr. Barbieri at [email protected]
CASE. Suspected teratoma-induced encephalitis
You are on call for your practice group, resting comfortably at home, reviewing tomorrow’s office schedule and wondering if your peaceful evening will be interrupted by a call from the hospital. At 9 pm, a neurologist calls and pleads for you to come to the hospital to evaluate a 25-year-old patient with encephalitis who is intubated in the intensive care unit (ICU). You immediately wonder, “Why call me about a case of encephalitis?”
The neurologist reports the following details. Over the 2 weeks preceding hospitalization, the patient developed progressive agitation, irritability, and hallucinations. She then had a seizure. She was brought to the hospital and was observed to be hypoventilating. She was sedated, intubated, and placed on mechanical ventilation.
Imaging studies were consistent with encephalitis. A screen for toxic substances and tests for viral and bacterial infection were negative. A spinal tap showed white blood cells (WBCs) in the cerebrospinal fluid (CSF).
Earlier in the afternoon serum and CSF sent to a reference laboratory returned positive for anti–N-methyl-D-aspartate (anti-NMDA)–receptor antibodies. Emergency pelvic ultrasonography was obtained, showing a 4-cm complex ovarian mass consistent with a teratoma. Based on these findings, the neurologist diagnosed teratoma-induced encephalitis.
The neurologist insists that you immediately operate on the patient to remove the teratoma.
What would you do in this hypothetical case?
OVARIAN TERATOMA AND ENCEPHALITIS—A CAUSAL LINK
Between 2005 and 2009, Dr. Josep Dalmau and colleagues in the Department of Neurology at the University of Pennsylvania published a series of papers documenting a link between encephalitis and ovarian teratomas.1-5 The pathophysiologic connection is thought to be the presence of tissue in the ovarian teratoma that stimulates the immune system to produce anti-NMDA-receptor (anti-NMDAR) antibodies. The anti-NMDAR antibodies, and/or the related B cells, then enter the central nervous system. It is hypothesized that the antibodies deplete cell-surface NMDA receptors on NMDA-receptor–rich neurons in the limbic system. This causes neuronal dysfunction, and over time, may cause permanent loss of neurons.
The antibody-induced abnormality in neuronal function produces a constellation of neuropsychiatric changes, including disturbances of memory, behavior, and cognition, and can trigger the onset of seizures. Hypoventilation may occur, and patients severely affected by the syndrome require sedation, intubation, and mechanical ventilation.
An observational link. Observations that support the mechanistic connection between teratoma-induced production of anti-NMDAR antibodies and encephalitis are as follows:
- In cases of encephalitis associated with an ovarian teratoma, histology often shows an intense WBC infiltrate in areas of the teratoma with neural tissue.6
- Tissue in the teratoma expresses the NMDA receptor.7
- In the syndrome of ovarian teratoma and encephalitis, elevated titers of anti-NMDAR antibodies are often present in serum and CSF.
- The areas of the brain affected by the encephalitis, including limbic and forebrain structures, express the NMDA receptor.
- Interventions that reduce levels of the anti-NMDAR antibody titer, including removal of the teratoma or immunotherapy, are often associated with a marked improvement in the clinical syndrome.
Awareness among ObGyns is valuable
The vast majority of ovarian teratomas never trigger the synthesis of anti-NMDAR antibodies or the development of a disabling encephalitis.8 However, the recognition that teratomas can cause encephalitis suggests that, if a teratoma is expectantly managed, the patient and her family should be alerted to report the new onset of symptoms, such as behavioral change, that may warrant neurologic evaluation.
In the California Encephalitis Project,9 of the 761 cases of encephalitis evaluated, the most common identifiable cause of the condition in women aged 30 years and younger was anti-NMDAR encephalitis. Enterovirus was a close second as a cause of encephalitis. Well-known causes of the condition, such as Herpes simplex 1, Varicella zoster, and West Nile virus were far less common.
HOW IS A DIAGNOSIS REACHED?
In many cases of encephalitis due to an ovarian teratoma, diagnosis is made by history, as well as physical examination consistent with:
- limbic encephalitis
- imaging studies that show encephalitis
- negative test results for viral, bacterial, and toxicologic causes of encephalitis
- evidence of WBCs in the CSF
- the presence of anti–NMDAR antibodies and an ovarian teratoma.
Neuropsychologic changes observed with this disease include agitation, mood lability, speech dysfunction, hallucinations, paranoia, hypersexuality, and seizures. Movement disorders are common in patients with this disease and include orofacial dyskinesias, unilateral dystonia, opisthotonus, chorea, rigidity, and catatonia. In many cases, a prodrome of fever and headache precede the development of the full syndrome. Both mature and immature teratomas can cause the syndrome.
Related Article: Skilled US imaging of the adnexae: Ovarian Neoplasms Ilan Timor-Tritsch, MD, and Steven R. Goldstein, MD (November 2010)
OPTIMAL TREATMENT
Encephalitis due to ovarian teratoma is treated by urgent removal of the teratoma. This is in combination with immune-modulating therapy, which may include intravenous immunoglobulin (IVIG), high-dose glucocorticoids, plasmapheresis, or rituximab (a monoclonal antibody targeted to the CD20 antigen on B lymphocytes).10,11
Although there is little evidence to support this clinical point, most neurologists passionately believe that once the diagnosis of ovarian teratoma–induced encephalitis is made, the teratoma should be urgently removed to help reduce the risk of permanent neurologic injury.
Challenging clinical issues
Resect the cyst or remove the ovary? The surgical approach to resecting the teratoma may either be complete ovarian cystectomy or oophorectomy. It is important to resect the teratoma in its entirety and avoid spilling the cyst contents into the peritoneal cavity. Based on these considerations, in women who have completed childbearing, an oophorectomy is often performed (FIGURE). For young patients, an ovarian cystectomy or oophorectomy are both suitable options.12
Intraoperative ultrasound can be helpful in confirming the presence of small teratomas and in guiding the surgeon to the correct location.13
Small teratomas. In cases of encephalitis induced by anti-NMDAR antibodies, the inciting ovarian teratoma can be very small, and not initially detected by ultrasonography.14,15 This creates a clinical challenge as, among women with anti-NMDAR encephalitis, only about half are reported to have ovarian teratomas. However, if microscopic teratomas could precipitate the syndrome, how is the physician to know which women without imaging evidence of a teratoma should have their ovaries surgically explored or removed?
In a case in which an occult teratoma is suspected to be the cause of anti-NMDAR encephalitis, a multidisciplinary team including a neurologist, radiologist, and gynecologist should confer to determine the best course of action. We should minimize the number of cases in which unnecessary oophorectomy is performed in the hope that a teratoma may be the cause of the encephalitis.
Ovarian teratoma but no anti-NMDAR antibodies. Some patients with encephalitis have a teratoma but no detectable anti-NMDAR antibodies. In these patients, teratoma removal may be associated with improvement in the encephalitis; however, the cause of the condition may be another type of anti-neuronal antibody that has yet to be identified.16 Women with encephalitis and an ovarian teratoma, and no evidence of infectious or toxicologic causes for the encephalitis, should be considered for teratoma removal.
CASE RESOLVED. Cyst resection contributes to recovery
You arrive at the hospital’s ICU, perform a physical examination, review the ultrasound, and confirm that the patient has an adnexal mass consistent with a teratoma. The anesthesiologist on call has agreed to provide an anesthetic.
You quickly search PubMed and discover that there are more than 180 publications reporting a link between encephalitis and ovarian teratoma, but only a small number are in the obstetrics and gynecology literature.
You take the patient to the operating room and resect the teratoma. The neurologist treats the patient with high-dose glucocorticoids. She recovers slowly, but her neurologic condition improves each day. On postoperative day 14 she is discharged home with a few remaining neurologic deficits. The patient and her family are amazed and grateful.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] or Dr. Barbieri at [email protected]
- Vitaliani R, Mason W, Ances B, Zwerdling T, Jian Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms and hypoventilation in ovarian teratoma. Ann Neurol. 2005;58(4):594–604.
- Ances BM, Vitaliani R, Taylor RA, et al. Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain. 2005;128(Pt 8):1764–1777.
- Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NDMA-receptor encephalitis: Case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7(12):1091–1098.
- Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66(1):11–18.
- Dabner M, McCluggage W, Bundell C, et al. Ovarian teratoma associated with anti-N-methyl-D-aspartate receptor encephalitis: A report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol. 2012;31(5): 29–37.
- Tachibana N, Shirakawa T, Ishii K, et al.
Expression of various glutamate receptors including N-methyl-D-aspartate receptor (NMDAR) in an ovarian teratoma removed from a young woman with anti-NMDAR encephalitis. Intern Med. 2010;49(19):2167–2173. - Mangler M, Trebesch de Perez I, Teegen B, et al. Seroprevalence of anti-N-methyl-D-aspartate receptor antibodies in women with ovarian teratoma. J Neurol. 2013;260(11):2831–2835.
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California encephalitis project. Clin Infect Dis. 2012;54(7):899–904.
- Pham HP, Daniel-Johnson JA, Stotler BA, Stephens H, Schwartz J. Therapeutic plasma exchange for the treatment of anti-NMDA-receptor encephalitis. J Clin Apher. 2011;26(6):320–325.
- Miya K, Takahashi Y, Mori H. Anti-NMDAR autoimmune encephalitis [published online ahead of print November 5, 2013]. Brain Dev. doi:10.1016/j.braindev.2013.10.005.
- Naoura I, Didelot A, Walker F, Luton D, Koskas M. Anti-N-methyl-D-aspartate receptor encephalitis complications ovarian teratomas: a case report. Am J Obstet Gynecol. 2011;205(4):e6–e8.
- Asai S, Ishimoto H, Yabuno, Asada H, Seki M, Iwata S. Laparoscopic cystectomy of ovarian teratoma in anti-NMDR encephalitis: 2 case reports. J Min Invas Gynecol. 2011;18(1):135–137.
- Tanyi J, Marsh E, Dalmau J, Chu C. Reversible paraneoplastic encephalitis in three patients with ovarian neoplasms. Acta Obstet Gynecol Scand. 2012;91(5):630–634.
- Boeck AL, Logemann F, Kraub T, et al. Ovarectomy despite negative imaging in anti-NMDA receptor encephalitis: Effective even late [published online ahead of print February 26, 2013]. Case Rep Neurol Med. doi:10.1155/2013/843192.
- Armangue T, Titulaer MJ, Sabater L, et al. A novel treatment-responsive encephalitis with frequent opsoclonus and teratoma [published online ahead of print April 24, 2013]. Ann Neurol. doi: 10.1002/ana.23917.
- Vitaliani R, Mason W, Ances B, Zwerdling T, Jian Z, Dalmau J. Paraneoplastic encephalitis, psychiatric symptoms and hypoventilation in ovarian teratoma. Ann Neurol. 2005;58(4):594–604.
- Ances BM, Vitaliani R, Taylor RA, et al. Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain. 2005;128(Pt 8):1764–1777.
- Dalmau J, Tuzun E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36.
- Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NDMA-receptor encephalitis: Case series and analysis of the effects of antibodies. Lancet Neurol. 2008;7(12):1091–1098.
- Florance NR, Davis RL, Lam C, et al. Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol. 2009;66(1):11–18.
- Dabner M, McCluggage W, Bundell C, et al. Ovarian teratoma associated with anti-N-methyl-D-aspartate receptor encephalitis: A report of 5 cases documenting prominent intratumoral lymphoid infiltrates. Int J Gynecol Pathol. 2012;31(5): 29–37.
- Tachibana N, Shirakawa T, Ishii K, et al.
Expression of various glutamate receptors including N-methyl-D-aspartate receptor (NMDAR) in an ovarian teratoma removed from a young woman with anti-NMDAR encephalitis. Intern Med. 2010;49(19):2167–2173. - Mangler M, Trebesch de Perez I, Teegen B, et al. Seroprevalence of anti-N-methyl-D-aspartate receptor antibodies in women with ovarian teratoma. J Neurol. 2013;260(11):2831–2835.
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California encephalitis project. Clin Infect Dis. 2012;54(7):899–904.
- Pham HP, Daniel-Johnson JA, Stotler BA, Stephens H, Schwartz J. Therapeutic plasma exchange for the treatment of anti-NMDA-receptor encephalitis. J Clin Apher. 2011;26(6):320–325.
- Miya K, Takahashi Y, Mori H. Anti-NMDAR autoimmune encephalitis [published online ahead of print November 5, 2013]. Brain Dev. doi:10.1016/j.braindev.2013.10.005.
- Naoura I, Didelot A, Walker F, Luton D, Koskas M. Anti-N-methyl-D-aspartate receptor encephalitis complications ovarian teratomas: a case report. Am J Obstet Gynecol. 2011;205(4):e6–e8.
- Asai S, Ishimoto H, Yabuno, Asada H, Seki M, Iwata S. Laparoscopic cystectomy of ovarian teratoma in anti-NMDR encephalitis: 2 case reports. J Min Invas Gynecol. 2011;18(1):135–137.
- Tanyi J, Marsh E, Dalmau J, Chu C. Reversible paraneoplastic encephalitis in three patients with ovarian neoplasms. Acta Obstet Gynecol Scand. 2012;91(5):630–634.
- Boeck AL, Logemann F, Kraub T, et al. Ovarectomy despite negative imaging in anti-NMDA receptor encephalitis: Effective even late [published online ahead of print February 26, 2013]. Case Rep Neurol Med. doi:10.1155/2013/843192.
- Armangue T, Titulaer MJ, Sabater L, et al. A novel treatment-responsive encephalitis with frequent opsoclonus and teratoma [published online ahead of print April 24, 2013]. Ann Neurol. doi: 10.1002/ana.23917.