User login
What’s the best treatment for CIN 2 or 3?
Excision or ablation of the transformation zone are equally effective for treating an initial diagnosis of cervical intraepithelial neoplasia (CIN) grades 2 or 3 in women with a satisfactory colposcopy and no suggestion of microinvasive or invasive disease (strength of recommendation [SOR]: A, based on randomized controlled trials [RCTs]).
Laser or loop electrosurgical excision procedure (LEEP) are the preferred treatment methods for recurrent CIN 2 and CIN 3 (SOR: B, based on clinical trials without randomization).
For women with an unsatisfactory colposcopy or suspicion of invasive disease, a diagnostic excisional procedure is recommended (SOR: C, based on consensus guidelines).
Observation or deferred treatment may be acceptable for CIN 2 in adolescents with satisfactory colposcopy and negative endocervical sampling (SOR: C, based on consensus guidelines).
Limit diagnostic excisional procedures in pregnancy to cases where suspicion of invasive cancer is high (SOR: C, based on consensus guidelines).
LEEP provides tissue for examination and a short recovery time
Timothy Huber, MD
Oroville, Calif
Close follow-up of observable disease and aggressive intervention continue to drive down the number of cervical cancer deaths each year.
It remains to be seen what the true effect of the HPV vaccine will be, although the presumed result will be a dramatic decline in high-grade lesions (CIN 2 and 3), carcinoma in situ, and invasive disease.
When intervention is necessary, my preferred method is LEEP because it provides tissue for examination and the recovery time is short.
Cryotherapy is an acceptable alternative, but the 4 to 8 weeks of leukorrhea and the lack of a tissue diagnosis often make it a less desirable option for patient and physician.
Evidence summary
Morbidity profile makes LEEP appear best
Similar efficacy. All 7 available surgical techniques were found to have similar efficacy, in a 2005 Cochrane review of 28 randomized trials.1 Resolution of CIN 2 or 3 lesions was 77% to 98%, using knife cone biopsy, laser conization, loop excision, laser ablation, cryotherapy, or 2 techniques not used commonly in the US, cold coagulation and radical diathermy. Surgical techniques were tested in various combinations, but no trial compared all of the techniques with one another. Most studies were underpowered, limiting the results.
Pap test: Good, but underused We’ve made great progress. What was the 2nd leading cancer in US women in incidence and mortality is now 11th in incidence and 13th in mortality. Yet, even with perfect attendance at annual screenings, women still get cervical cancer. And many still do not have screenings—they account for about half of all cervical cancers. The Pap, as good as it is, has flaws. The test is subjective, and sensitivity varies from lab to lab. 9
Dr. J. Thomas cox, university of California. Member, American Cancer society Cervical guidelines Committee, the 2002 Bethesda Workshop; ACS HPV vaccine Advisory Committee; author, ASCCP guidelines Committee
Each year in the united states approximately 500,000 women are diagnosed with high-grade cervical cancer precursor lesions, CIN 2 and CIN III.4 If left untreated, 22% of CIN 2 lesions progress to carcinoma in situ or invasive cervical cancer, 43% regress, and 35% persist at the same level. Fourteen percent of untreated CIN 3 lesions progress, 32% regress, and 56% persist at the same level.
HPV vaccine: Won’t replace prevention or protection Although an effective vaccine is a major advance in the prevention of genital HPV and cervical cancer, it will not replace other prevention strategies, such as cervical cancer screening for women or protective sexual behaviors. Women should continue to get Pap tests as a safeguard against cervical cancer.
Dr. Anne Schuchat, Director, CDC National Center for Immunization and respiratory Diseases, June 29, 2006 press release (www.cdc.gov/od/oc/media/pressrel/r060629.htm)
The HPV vaccine (Gardasil) that prevents the development of lesions caused by HPV types 6, 11, 16, and 18, was approved by the us Food and Drug Administration in June 2006 for use in females 9 to 26 years oof age. Shortly after, the Advisory Committee on Immunization Practices issued guidelines, stating that vaccination is recommended for all women <26 years of age. (www.cdc.gov/vaccines/recs/schedules/adult-schedule.htm).
HPV testing: Adjunct to cytology The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are underway. 10
Dr. Thomas C. Wright, Columbia university. Author, 2001 Consensus guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim guidance for use of HPV DNA testing for Primary screening, and the 2001 Bethesda system
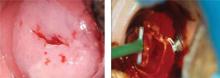
Least morbidity with LEEP. Morbidity was compared with one-on-one trials of different techniques ( TABLE 1 ). The review noted that LEEP has the least morbidity (such as hemorrhage, infection, cervical stenosis, and midtrimester pregnancy loss) while providing the most reliable histology by excising tissue without causing thermal artifact ( FIGURE ).
Higher rate of hemorrhage with cone biopsy. Another systematic review of 21 controlled trials comparing treatments for CIN 2 or 3 found a similar efficacy of all the modalities, including cone biopsy, cryotherapy, laser ablation, and LEEP. However, it also found a trend toward a higher rate of significant hemorrhage among women who received cone biopsies compared with women who received either laser ablation or LEEP.2
FIGURE
CIN 2 and 3 and its treatment by LEEP
TABLE 1
CIN 2 and 3 treatment options: An outcomes comparison
| COMPARISON OF TREATMENTS | OUTCOME/MORBIDITY | ODDS RATIO (95% CI) |
|---|---|---|
| Laser ablation vs cryotherapy | Laser ablation had more perioperative severe bleeding | 7.45 (1.68–33) |
| Laser ablation had higher rates of future adequate colposcopy | 4.64 (2.98–7.27) | |
| Laser conization vs knife conization | Laser conization had higher rates of future adequate colposcopy | 2.73 (1.47–5.08) |
| Laser conization had less cervical stenosis | 0.39 (0.25–0.61) | |
| Laser conization vs LEEP | Laser conization had more severe pain during procedure | 5.36 (1.02–17.2) |
| LEEP had fewer inadequate future colposcopies | 0.27 (0.08–0.89) | |
| Source: Martin-Hirsch et al, Cochrane Database Syst Rev 2000.1 | ||
Surgical treatment raises obstetric risks
There is a concern regarding future obstetric outcomes for women who have undergone surgical treatment of a high-grade cervical lesion. A recent meta-analysis of 27 controlled cohort studies found that cold knife conization and LEEP were associated with increased obstetrical risks, such as delivery at less than 37 weeks’ gestation and a birth weight <2500 g ( TABLE 2 ). Any resection that was more than 10 mm deep increased the risk of prematurity with future pregnancies (pooled relative risk=2.6; 95%] CI, 1.3–5.3).3
TABLE 2
Obstetrical outcomes for CIN 2 and 3 treatment options
| TREATMENT TYPE | OBSTETRICAL OUTCOME | RELATIVE RISK (95% CI) |
|---|---|---|
| Cold knife conization | Preterm delivery | 2.59 (1.80–3.72) |
| Low birth weight | 2.53 (1.19–5.36) | |
| Cesarean delivery | 3.17 (1.07–9.40) | |
| Laser conization | Preterm delivery | 1.71 (0.93–3.14) |
| LEEP | Preterm delivery | 1.70 (1.24–2.35) |
| Low birth weight | 1.82 (1.09–3.06) | |
| Preterm premature rupture of membranes | 2.69 (1.62–4.46) | |
| Source: Kyrgiou et al, Lancet 2006.3 | ||
Recommendations from others
Consensus guidelines from the American Society for Colposcopy and Cervical Pathology (ASCCP) and a practice bulletin from the American College of Obstetricians and Gynecologists (ACOG) both recommend immediate removal of the entire transformation zone, with either ablative or excisional treatment as initial treatment of CIN 2 and 3 for patients who are not pregnant.4,5
Value of excisional treatment. The ASCCP guidelines note that there is a benefit to excisional treatment, as it allows pathologic assessment of the excised tissue. Some of the ASCCP guideline authors recommend excisional procedures for the management of large CIN 2 and 3 lesions, which are at increased risk of having microinvasive disease.4
For women with unsatisfactory colposcopy and biopsy-proven CIN 2 or 3, there is up to a 7% risk for an occult invasive cervical carcinoma.1,4 Performing a diagnostic excisional procedure is recommended on these patients.4,6
ASCCP and ACOG make special recommendations for both adolescents and pregnant women.
For adolescent patients with biopsy-proven CIN 2, a recent ACOG Committee Opinion recommends close follow-up—with Pap smears or colposcopies every 4 to 6 months—due to the high rates of resolution of CIN 2 in adolescents.7
For pregnant patients, diagnostic excisional procedures are associated with complications such as bleeding and preterm delivery, while there is minimal risk of CIN 2 or 3 progressing to invasive cervical cancer.4,8 In pregnancy, follow CIN 2 and 3 with colposcopy each trimester, and reevaluate at 6 to 12 weeks postpartum. Limit any diagnostic excisional procedures to cases where you cannot rule out invasive cancer.4,5
1. Martin-Hirsch PL, Paraskevaidis E, Kitchener H. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev 2000;(2)CD001318.-
2. Nuovo J, Melnikow J, Willan AR, Chan BKS. Treatment outcomes for squamous intraepithelial lesions. Int J gynaecol obstet 2000;68:25-33.
3. Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet 2006;367:489-498.
4. Wright TC, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. 2001 ASCCP-sponsored Consensus Workshop. 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. Am J Obstet Gynecol 2003;189:295-304.
5. American College of obstetricians and gynecologists. ACOG Practice Bulletin number 66, september 2005. Management of abnormal cervical cytology and histology. Obstet Gynecol 2005;106:645-664.
6. Duggan BD, Felix JC, Muderspach LI, et al. Cold-knife conization versus conization by the loop electrosurgical excision procedure: a randomized, prospective study. Am J Obstet Gynecol 1999;180:276-282.
7. American College of obstetricians and gynecologists. ACOG Committee opinion. Evaluation and management of abnormal cervical cytology and histology in the adolescent. Number 330, April 2006. Obstet Gynecol 2006;107:963-968.
8. Economos K, Perez Veridiano N, Delke I, Collado ML, Tancer ML. Abnormal cervical cytology in pregnancy: a 17-year experience. Obstet Gynecol 1993;81:915-918.
9. Cox JT. We’re on the way to ending cervical cancer. OBG Management 2006;18(3):62-72.
10. Wright TC. Cervical disease update. OBG Management 2007;19(3):52-60.
Excision or ablation of the transformation zone are equally effective for treating an initial diagnosis of cervical intraepithelial neoplasia (CIN) grades 2 or 3 in women with a satisfactory colposcopy and no suggestion of microinvasive or invasive disease (strength of recommendation [SOR]: A, based on randomized controlled trials [RCTs]).
Laser or loop electrosurgical excision procedure (LEEP) are the preferred treatment methods for recurrent CIN 2 and CIN 3 (SOR: B, based on clinical trials without randomization).
For women with an unsatisfactory colposcopy or suspicion of invasive disease, a diagnostic excisional procedure is recommended (SOR: C, based on consensus guidelines).
Observation or deferred treatment may be acceptable for CIN 2 in adolescents with satisfactory colposcopy and negative endocervical sampling (SOR: C, based on consensus guidelines).
Limit diagnostic excisional procedures in pregnancy to cases where suspicion of invasive cancer is high (SOR: C, based on consensus guidelines).
LEEP provides tissue for examination and a short recovery time
Timothy Huber, MD
Oroville, Calif
Close follow-up of observable disease and aggressive intervention continue to drive down the number of cervical cancer deaths each year.
It remains to be seen what the true effect of the HPV vaccine will be, although the presumed result will be a dramatic decline in high-grade lesions (CIN 2 and 3), carcinoma in situ, and invasive disease.
When intervention is necessary, my preferred method is LEEP because it provides tissue for examination and the recovery time is short.
Cryotherapy is an acceptable alternative, but the 4 to 8 weeks of leukorrhea and the lack of a tissue diagnosis often make it a less desirable option for patient and physician.
Evidence summary
Morbidity profile makes LEEP appear best
Similar efficacy. All 7 available surgical techniques were found to have similar efficacy, in a 2005 Cochrane review of 28 randomized trials.1 Resolution of CIN 2 or 3 lesions was 77% to 98%, using knife cone biopsy, laser conization, loop excision, laser ablation, cryotherapy, or 2 techniques not used commonly in the US, cold coagulation and radical diathermy. Surgical techniques were tested in various combinations, but no trial compared all of the techniques with one another. Most studies were underpowered, limiting the results.
Pap test: Good, but underused We’ve made great progress. What was the 2nd leading cancer in US women in incidence and mortality is now 11th in incidence and 13th in mortality. Yet, even with perfect attendance at annual screenings, women still get cervical cancer. And many still do not have screenings—they account for about half of all cervical cancers. The Pap, as good as it is, has flaws. The test is subjective, and sensitivity varies from lab to lab. 9
Dr. J. Thomas cox, university of California. Member, American Cancer society Cervical guidelines Committee, the 2002 Bethesda Workshop; ACS HPV vaccine Advisory Committee; author, ASCCP guidelines Committee
Each year in the united states approximately 500,000 women are diagnosed with high-grade cervical cancer precursor lesions, CIN 2 and CIN III.4 If left untreated, 22% of CIN 2 lesions progress to carcinoma in situ or invasive cervical cancer, 43% regress, and 35% persist at the same level. Fourteen percent of untreated CIN 3 lesions progress, 32% regress, and 56% persist at the same level.
HPV vaccine: Won’t replace prevention or protection Although an effective vaccine is a major advance in the prevention of genital HPV and cervical cancer, it will not replace other prevention strategies, such as cervical cancer screening for women or protective sexual behaviors. Women should continue to get Pap tests as a safeguard against cervical cancer.
Dr. Anne Schuchat, Director, CDC National Center for Immunization and respiratory Diseases, June 29, 2006 press release (www.cdc.gov/od/oc/media/pressrel/r060629.htm)
The HPV vaccine (Gardasil) that prevents the development of lesions caused by HPV types 6, 11, 16, and 18, was approved by the us Food and Drug Administration in June 2006 for use in females 9 to 26 years oof age. Shortly after, the Advisory Committee on Immunization Practices issued guidelines, stating that vaccination is recommended for all women <26 years of age. (www.cdc.gov/vaccines/recs/schedules/adult-schedule.htm).
HPV testing: Adjunct to cytology The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are underway. 10
Dr. Thomas C. Wright, Columbia university. Author, 2001 Consensus guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim guidance for use of HPV DNA testing for Primary screening, and the 2001 Bethesda system
Least morbidity with LEEP. Morbidity was compared with one-on-one trials of different techniques ( TABLE 1 ). The review noted that LEEP has the least morbidity (such as hemorrhage, infection, cervical stenosis, and midtrimester pregnancy loss) while providing the most reliable histology by excising tissue without causing thermal artifact ( FIGURE ).
Higher rate of hemorrhage with cone biopsy. Another systematic review of 21 controlled trials comparing treatments for CIN 2 or 3 found a similar efficacy of all the modalities, including cone biopsy, cryotherapy, laser ablation, and LEEP. However, it also found a trend toward a higher rate of significant hemorrhage among women who received cone biopsies compared with women who received either laser ablation or LEEP.2
FIGURE
CIN 2 and 3 and its treatment by LEEP
TABLE 1
CIN 2 and 3 treatment options: An outcomes comparison
| COMPARISON OF TREATMENTS | OUTCOME/MORBIDITY | ODDS RATIO (95% CI) |
|---|---|---|
| Laser ablation vs cryotherapy | Laser ablation had more perioperative severe bleeding | 7.45 (1.68–33) |
| Laser ablation had higher rates of future adequate colposcopy | 4.64 (2.98–7.27) | |
| Laser conization vs knife conization | Laser conization had higher rates of future adequate colposcopy | 2.73 (1.47–5.08) |
| Laser conization had less cervical stenosis | 0.39 (0.25–0.61) | |
| Laser conization vs LEEP | Laser conization had more severe pain during procedure | 5.36 (1.02–17.2) |
| LEEP had fewer inadequate future colposcopies | 0.27 (0.08–0.89) | |
| Source: Martin-Hirsch et al, Cochrane Database Syst Rev 2000.1 | ||
Surgical treatment raises obstetric risks
There is a concern regarding future obstetric outcomes for women who have undergone surgical treatment of a high-grade cervical lesion. A recent meta-analysis of 27 controlled cohort studies found that cold knife conization and LEEP were associated with increased obstetrical risks, such as delivery at less than 37 weeks’ gestation and a birth weight <2500 g ( TABLE 2 ). Any resection that was more than 10 mm deep increased the risk of prematurity with future pregnancies (pooled relative risk=2.6; 95%] CI, 1.3–5.3).3
TABLE 2
Obstetrical outcomes for CIN 2 and 3 treatment options
| TREATMENT TYPE | OBSTETRICAL OUTCOME | RELATIVE RISK (95% CI) |
|---|---|---|
| Cold knife conization | Preterm delivery | 2.59 (1.80–3.72) |
| Low birth weight | 2.53 (1.19–5.36) | |
| Cesarean delivery | 3.17 (1.07–9.40) | |
| Laser conization | Preterm delivery | 1.71 (0.93–3.14) |
| LEEP | Preterm delivery | 1.70 (1.24–2.35) |
| Low birth weight | 1.82 (1.09–3.06) | |
| Preterm premature rupture of membranes | 2.69 (1.62–4.46) | |
| Source: Kyrgiou et al, Lancet 2006.3 | ||
Recommendations from others
Consensus guidelines from the American Society for Colposcopy and Cervical Pathology (ASCCP) and a practice bulletin from the American College of Obstetricians and Gynecologists (ACOG) both recommend immediate removal of the entire transformation zone, with either ablative or excisional treatment as initial treatment of CIN 2 and 3 for patients who are not pregnant.4,5
Value of excisional treatment. The ASCCP guidelines note that there is a benefit to excisional treatment, as it allows pathologic assessment of the excised tissue. Some of the ASCCP guideline authors recommend excisional procedures for the management of large CIN 2 and 3 lesions, which are at increased risk of having microinvasive disease.4
For women with unsatisfactory colposcopy and biopsy-proven CIN 2 or 3, there is up to a 7% risk for an occult invasive cervical carcinoma.1,4 Performing a diagnostic excisional procedure is recommended on these patients.4,6
ASCCP and ACOG make special recommendations for both adolescents and pregnant women.
For adolescent patients with biopsy-proven CIN 2, a recent ACOG Committee Opinion recommends close follow-up—with Pap smears or colposcopies every 4 to 6 months—due to the high rates of resolution of CIN 2 in adolescents.7
For pregnant patients, diagnostic excisional procedures are associated with complications such as bleeding and preterm delivery, while there is minimal risk of CIN 2 or 3 progressing to invasive cervical cancer.4,8 In pregnancy, follow CIN 2 and 3 with colposcopy each trimester, and reevaluate at 6 to 12 weeks postpartum. Limit any diagnostic excisional procedures to cases where you cannot rule out invasive cancer.4,5
Excision or ablation of the transformation zone are equally effective for treating an initial diagnosis of cervical intraepithelial neoplasia (CIN) grades 2 or 3 in women with a satisfactory colposcopy and no suggestion of microinvasive or invasive disease (strength of recommendation [SOR]: A, based on randomized controlled trials [RCTs]).
Laser or loop electrosurgical excision procedure (LEEP) are the preferred treatment methods for recurrent CIN 2 and CIN 3 (SOR: B, based on clinical trials without randomization).
For women with an unsatisfactory colposcopy or suspicion of invasive disease, a diagnostic excisional procedure is recommended (SOR: C, based on consensus guidelines).
Observation or deferred treatment may be acceptable for CIN 2 in adolescents with satisfactory colposcopy and negative endocervical sampling (SOR: C, based on consensus guidelines).
Limit diagnostic excisional procedures in pregnancy to cases where suspicion of invasive cancer is high (SOR: C, based on consensus guidelines).
LEEP provides tissue for examination and a short recovery time
Timothy Huber, MD
Oroville, Calif
Close follow-up of observable disease and aggressive intervention continue to drive down the number of cervical cancer deaths each year.
It remains to be seen what the true effect of the HPV vaccine will be, although the presumed result will be a dramatic decline in high-grade lesions (CIN 2 and 3), carcinoma in situ, and invasive disease.
When intervention is necessary, my preferred method is LEEP because it provides tissue for examination and the recovery time is short.
Cryotherapy is an acceptable alternative, but the 4 to 8 weeks of leukorrhea and the lack of a tissue diagnosis often make it a less desirable option for patient and physician.
Evidence summary
Morbidity profile makes LEEP appear best
Similar efficacy. All 7 available surgical techniques were found to have similar efficacy, in a 2005 Cochrane review of 28 randomized trials.1 Resolution of CIN 2 or 3 lesions was 77% to 98%, using knife cone biopsy, laser conization, loop excision, laser ablation, cryotherapy, or 2 techniques not used commonly in the US, cold coagulation and radical diathermy. Surgical techniques were tested in various combinations, but no trial compared all of the techniques with one another. Most studies were underpowered, limiting the results.
Pap test: Good, but underused We’ve made great progress. What was the 2nd leading cancer in US women in incidence and mortality is now 11th in incidence and 13th in mortality. Yet, even with perfect attendance at annual screenings, women still get cervical cancer. And many still do not have screenings—they account for about half of all cervical cancers. The Pap, as good as it is, has flaws. The test is subjective, and sensitivity varies from lab to lab. 9
Dr. J. Thomas cox, university of California. Member, American Cancer society Cervical guidelines Committee, the 2002 Bethesda Workshop; ACS HPV vaccine Advisory Committee; author, ASCCP guidelines Committee
Each year in the united states approximately 500,000 women are diagnosed with high-grade cervical cancer precursor lesions, CIN 2 and CIN III.4 If left untreated, 22% of CIN 2 lesions progress to carcinoma in situ or invasive cervical cancer, 43% regress, and 35% persist at the same level. Fourteen percent of untreated CIN 3 lesions progress, 32% regress, and 56% persist at the same level.
HPV vaccine: Won’t replace prevention or protection Although an effective vaccine is a major advance in the prevention of genital HPV and cervical cancer, it will not replace other prevention strategies, such as cervical cancer screening for women or protective sexual behaviors. Women should continue to get Pap tests as a safeguard against cervical cancer.
Dr. Anne Schuchat, Director, CDC National Center for Immunization and respiratory Diseases, June 29, 2006 press release (www.cdc.gov/od/oc/media/pressrel/r060629.htm)
The HPV vaccine (Gardasil) that prevents the development of lesions caused by HPV types 6, 11, 16, and 18, was approved by the us Food and Drug Administration in June 2006 for use in females 9 to 26 years oof age. Shortly after, the Advisory Committee on Immunization Practices issued guidelines, stating that vaccination is recommended for all women <26 years of age. (www.cdc.gov/vaccines/recs/schedules/adult-schedule.htm).
HPV testing: Adjunct to cytology The United States is falling behind other countries in assessing how best to utilize HPV testing for screening. Ongoing trials in The Netherlands, Italy, United Kingdom, Canada, and Finland are evaluating whether cytology can be replaced by HPV DNA testing for screening. Currently, HPV testing is only approved as an adjunct to cytology for cervical cancer screening in the United States, and no similar trials are underway. 10
Dr. Thomas C. Wright, Columbia university. Author, 2001 Consensus guidelines on Managing Women with Cytological and Histological Abnormalities, the 2004 Interim guidance for use of HPV DNA testing for Primary screening, and the 2001 Bethesda system
Least morbidity with LEEP. Morbidity was compared with one-on-one trials of different techniques ( TABLE 1 ). The review noted that LEEP has the least morbidity (such as hemorrhage, infection, cervical stenosis, and midtrimester pregnancy loss) while providing the most reliable histology by excising tissue without causing thermal artifact ( FIGURE ).
Higher rate of hemorrhage with cone biopsy. Another systematic review of 21 controlled trials comparing treatments for CIN 2 or 3 found a similar efficacy of all the modalities, including cone biopsy, cryotherapy, laser ablation, and LEEP. However, it also found a trend toward a higher rate of significant hemorrhage among women who received cone biopsies compared with women who received either laser ablation or LEEP.2
FIGURE
CIN 2 and 3 and its treatment by LEEP
TABLE 1
CIN 2 and 3 treatment options: An outcomes comparison
| COMPARISON OF TREATMENTS | OUTCOME/MORBIDITY | ODDS RATIO (95% CI) |
|---|---|---|
| Laser ablation vs cryotherapy | Laser ablation had more perioperative severe bleeding | 7.45 (1.68–33) |
| Laser ablation had higher rates of future adequate colposcopy | 4.64 (2.98–7.27) | |
| Laser conization vs knife conization | Laser conization had higher rates of future adequate colposcopy | 2.73 (1.47–5.08) |
| Laser conization had less cervical stenosis | 0.39 (0.25–0.61) | |
| Laser conization vs LEEP | Laser conization had more severe pain during procedure | 5.36 (1.02–17.2) |
| LEEP had fewer inadequate future colposcopies | 0.27 (0.08–0.89) | |
| Source: Martin-Hirsch et al, Cochrane Database Syst Rev 2000.1 | ||
Surgical treatment raises obstetric risks
There is a concern regarding future obstetric outcomes for women who have undergone surgical treatment of a high-grade cervical lesion. A recent meta-analysis of 27 controlled cohort studies found that cold knife conization and LEEP were associated with increased obstetrical risks, such as delivery at less than 37 weeks’ gestation and a birth weight <2500 g ( TABLE 2 ). Any resection that was more than 10 mm deep increased the risk of prematurity with future pregnancies (pooled relative risk=2.6; 95%] CI, 1.3–5.3).3
TABLE 2
Obstetrical outcomes for CIN 2 and 3 treatment options
| TREATMENT TYPE | OBSTETRICAL OUTCOME | RELATIVE RISK (95% CI) |
|---|---|---|
| Cold knife conization | Preterm delivery | 2.59 (1.80–3.72) |
| Low birth weight | 2.53 (1.19–5.36) | |
| Cesarean delivery | 3.17 (1.07–9.40) | |
| Laser conization | Preterm delivery | 1.71 (0.93–3.14) |
| LEEP | Preterm delivery | 1.70 (1.24–2.35) |
| Low birth weight | 1.82 (1.09–3.06) | |
| Preterm premature rupture of membranes | 2.69 (1.62–4.46) | |
| Source: Kyrgiou et al, Lancet 2006.3 | ||
Recommendations from others
Consensus guidelines from the American Society for Colposcopy and Cervical Pathology (ASCCP) and a practice bulletin from the American College of Obstetricians and Gynecologists (ACOG) both recommend immediate removal of the entire transformation zone, with either ablative or excisional treatment as initial treatment of CIN 2 and 3 for patients who are not pregnant.4,5
Value of excisional treatment. The ASCCP guidelines note that there is a benefit to excisional treatment, as it allows pathologic assessment of the excised tissue. Some of the ASCCP guideline authors recommend excisional procedures for the management of large CIN 2 and 3 lesions, which are at increased risk of having microinvasive disease.4
For women with unsatisfactory colposcopy and biopsy-proven CIN 2 or 3, there is up to a 7% risk for an occult invasive cervical carcinoma.1,4 Performing a diagnostic excisional procedure is recommended on these patients.4,6
ASCCP and ACOG make special recommendations for both adolescents and pregnant women.
For adolescent patients with biopsy-proven CIN 2, a recent ACOG Committee Opinion recommends close follow-up—with Pap smears or colposcopies every 4 to 6 months—due to the high rates of resolution of CIN 2 in adolescents.7
For pregnant patients, diagnostic excisional procedures are associated with complications such as bleeding and preterm delivery, while there is minimal risk of CIN 2 or 3 progressing to invasive cervical cancer.4,8 In pregnancy, follow CIN 2 and 3 with colposcopy each trimester, and reevaluate at 6 to 12 weeks postpartum. Limit any diagnostic excisional procedures to cases where you cannot rule out invasive cancer.4,5
1. Martin-Hirsch PL, Paraskevaidis E, Kitchener H. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev 2000;(2)CD001318.-
2. Nuovo J, Melnikow J, Willan AR, Chan BKS. Treatment outcomes for squamous intraepithelial lesions. Int J gynaecol obstet 2000;68:25-33.
3. Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet 2006;367:489-498.
4. Wright TC, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. 2001 ASCCP-sponsored Consensus Workshop. 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. Am J Obstet Gynecol 2003;189:295-304.
5. American College of obstetricians and gynecologists. ACOG Practice Bulletin number 66, september 2005. Management of abnormal cervical cytology and histology. Obstet Gynecol 2005;106:645-664.
6. Duggan BD, Felix JC, Muderspach LI, et al. Cold-knife conization versus conization by the loop electrosurgical excision procedure: a randomized, prospective study. Am J Obstet Gynecol 1999;180:276-282.
7. American College of obstetricians and gynecologists. ACOG Committee opinion. Evaluation and management of abnormal cervical cytology and histology in the adolescent. Number 330, April 2006. Obstet Gynecol 2006;107:963-968.
8. Economos K, Perez Veridiano N, Delke I, Collado ML, Tancer ML. Abnormal cervical cytology in pregnancy: a 17-year experience. Obstet Gynecol 1993;81:915-918.
9. Cox JT. We’re on the way to ending cervical cancer. OBG Management 2006;18(3):62-72.
10. Wright TC. Cervical disease update. OBG Management 2007;19(3):52-60.
1. Martin-Hirsch PL, Paraskevaidis E, Kitchener H. Surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev 2000;(2)CD001318.-
2. Nuovo J, Melnikow J, Willan AR, Chan BKS. Treatment outcomes for squamous intraepithelial lesions. Int J gynaecol obstet 2000;68:25-33.
3. Kyrgiou M, Koliopoulos G, Martin-Hirsch P, Arbyn M, Prendiville W, Paraskevaidis E. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet 2006;367:489-498.
4. Wright TC, Cox JT, Massad LS, Carlson J, Twiggs LB, Wilkinson EJ. 2001 ASCCP-sponsored Consensus Workshop. 2001 consensus guidelines for the management of women with cervical intraepithelial neoplasia. Am J Obstet Gynecol 2003;189:295-304.
5. American College of obstetricians and gynecologists. ACOG Practice Bulletin number 66, september 2005. Management of abnormal cervical cytology and histology. Obstet Gynecol 2005;106:645-664.
6. Duggan BD, Felix JC, Muderspach LI, et al. Cold-knife conization versus conization by the loop electrosurgical excision procedure: a randomized, prospective study. Am J Obstet Gynecol 1999;180:276-282.
7. American College of obstetricians and gynecologists. ACOG Committee opinion. Evaluation and management of abnormal cervical cytology and histology in the adolescent. Number 330, April 2006. Obstet Gynecol 2006;107:963-968.
8. Economos K, Perez Veridiano N, Delke I, Collado ML, Tancer ML. Abnormal cervical cytology in pregnancy: a 17-year experience. Obstet Gynecol 1993;81:915-918.
9. Cox JT. We’re on the way to ending cervical cancer. OBG Management 2006;18(3):62-72.
10. Wright TC. Cervical disease update. OBG Management 2007;19(3):52-60.
Evidence-based answers from the Family Physicians Inquiries Network