User login
Chronic anterior knee pain
A 14-year-old girl with an unremarkable medical history presented to the family medicine clinic with a 6-month history of right knee pain (episodic locking and anterior pain). Physical examination of the knee ligaments revealed that the knee was stable and pain-free in the frontal and sagittal planes. There was no intra-articular effusion, the joint spaces were not painful, and range of motion was normal.
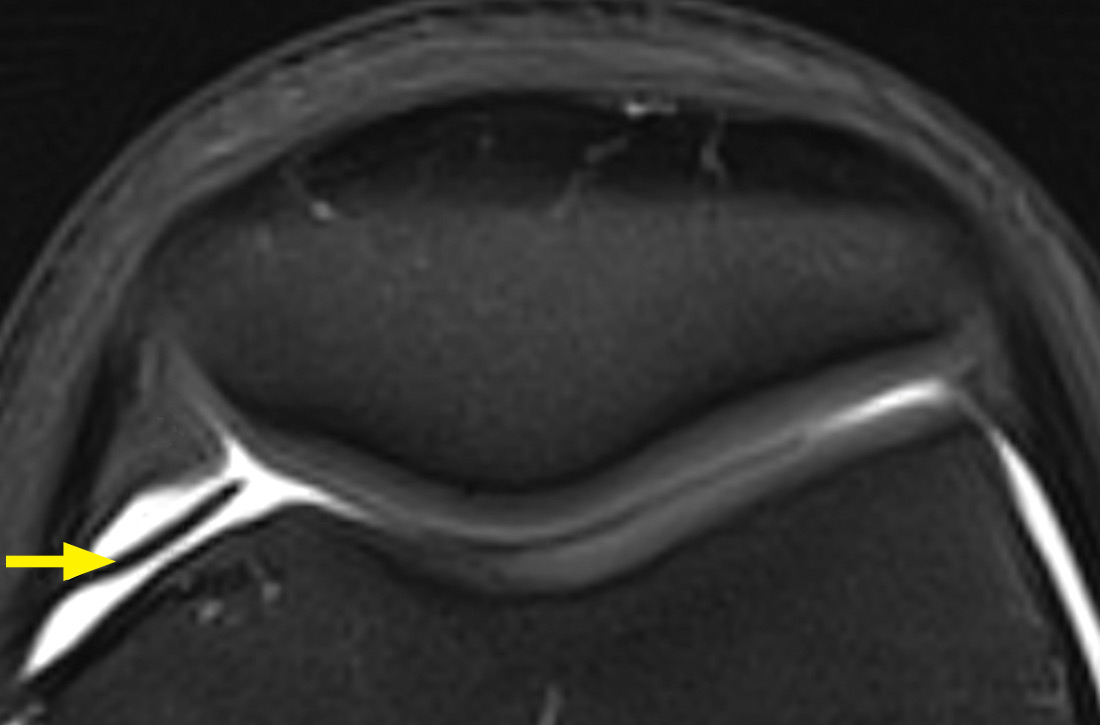
Palpation of the knee elicited pain, notably when the physician rolled his fingers over a “cord” above the internal parapatellar compartment. X-rays of the knee were normal. In light of the patient’s chronic pain, magnetic resonance imaging (MRI) was performed (FIGURE 1).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Synovial plica
The MRI with fat saturation revealed a symptomatic synovial plica between the patellar facet and the condyle (FIGURE 1, arrow). The normal x-ray findings had already ruled out osteochondritis dissecans of the femoral condyles, patellar abnormalities, and trochlear dysplasia; the MRI ruled out several additional items in the differential, such as damage to the meniscus, ligament, and/or cartilage.
The synovial plica is a normal structure that develops during the embryogenic phase; however, involution is incomplete in up to 50% of the population, resulting in persistent plicae.1 The plica is often located in a medial position but can occur lateral to, above, or below the knee cap. Although usually asymptomatic, the plica can become pathologic when irritation (eg, from repetitive motion) causes an inflammatory response.1
Synovial plica syndrome, as this condition is known, is a common cause of anterior knee pain in adolescents and athletes; incidence ranges from 3.8% to 5.5%.2 The patient often reports trauma (a direct impact to the knee) or participation in sports activities that require repeated flexion-extension of the knee.3
Presenting symptoms and MRI findings can unlock the diagnosis
The combination of anterior knee pain and a painful parapatellar “cord” on palpation is the most frequent diagnostic sign of synovial plica syndrome.1 Quadriceps wasting, intra-articular effusion, and reduced range of motion of the knee may also be observed.1,4 Some patients experience particularly disconcerting symptoms, such as knee locking, clicking, or instability.1
In most cases, MRI confirms the clinical diagnosis while ruling out other possible causes of the symptoms and associated pathologies.5 However, MRI may not reveal the plica if it is attached to the articular capsule or if there is no intra-articular effusion. Dynamic ultrasound might be of diagnostic value but is operator dependent.4
Continue to: If conservative treatment fails, consider surgical repair
If conservative treatment fails, consider surgical repair
Conservative treatment—a combination of analgesics, anti-inflammatories, and physiotherapy with vastus medialis strengthening and stretching—is the preferred first-line treatment, with a success rate of 40% to 60%.1 If conservative treatment fails, surgical treatment can be
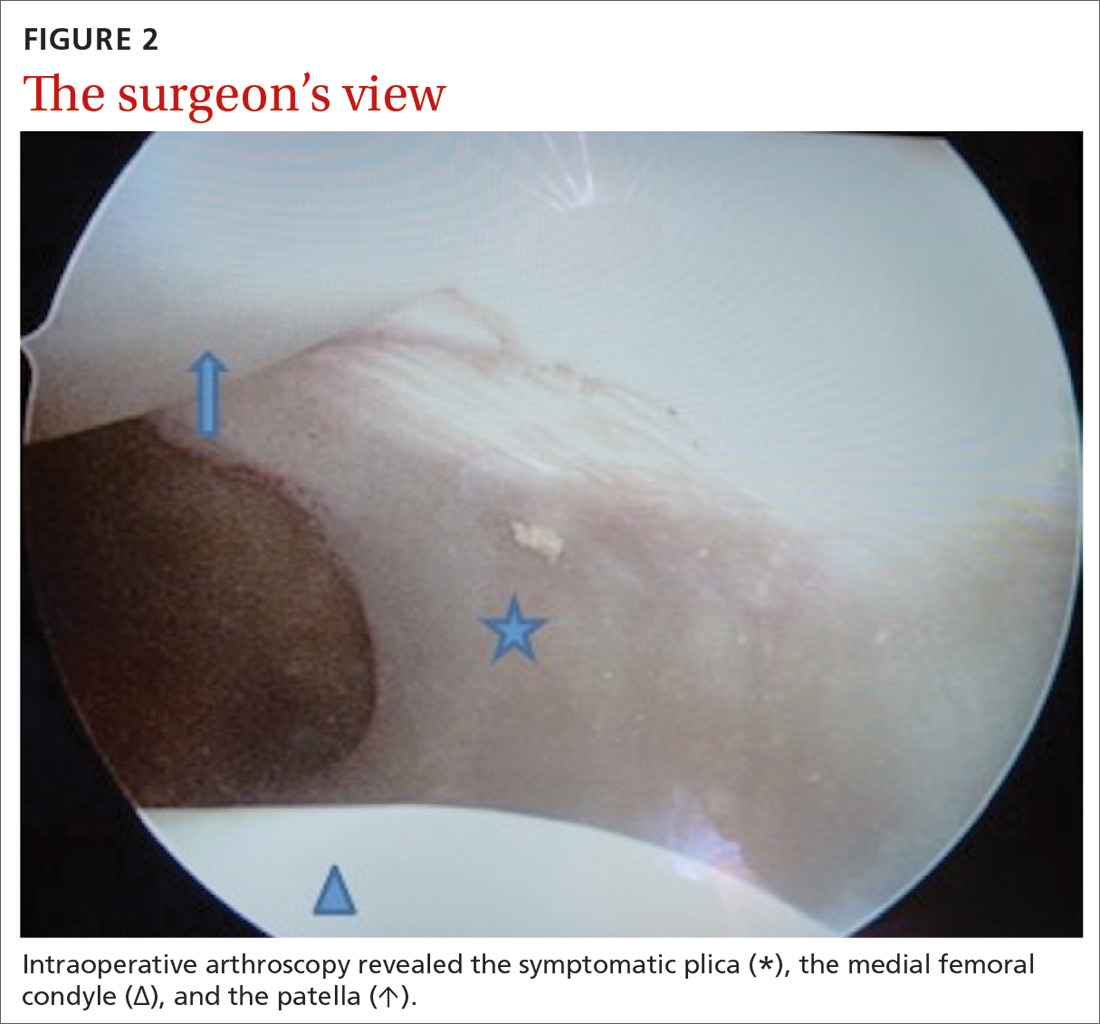
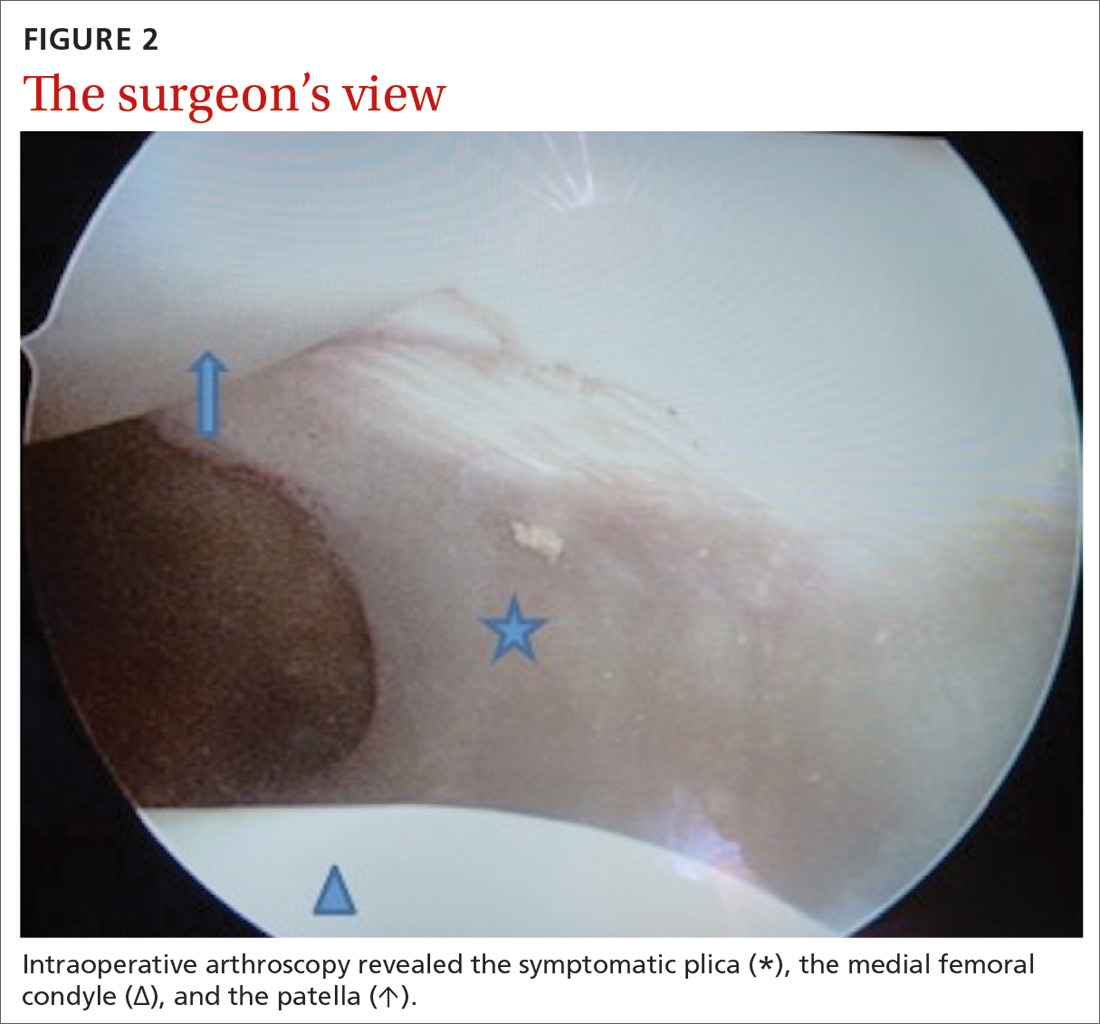
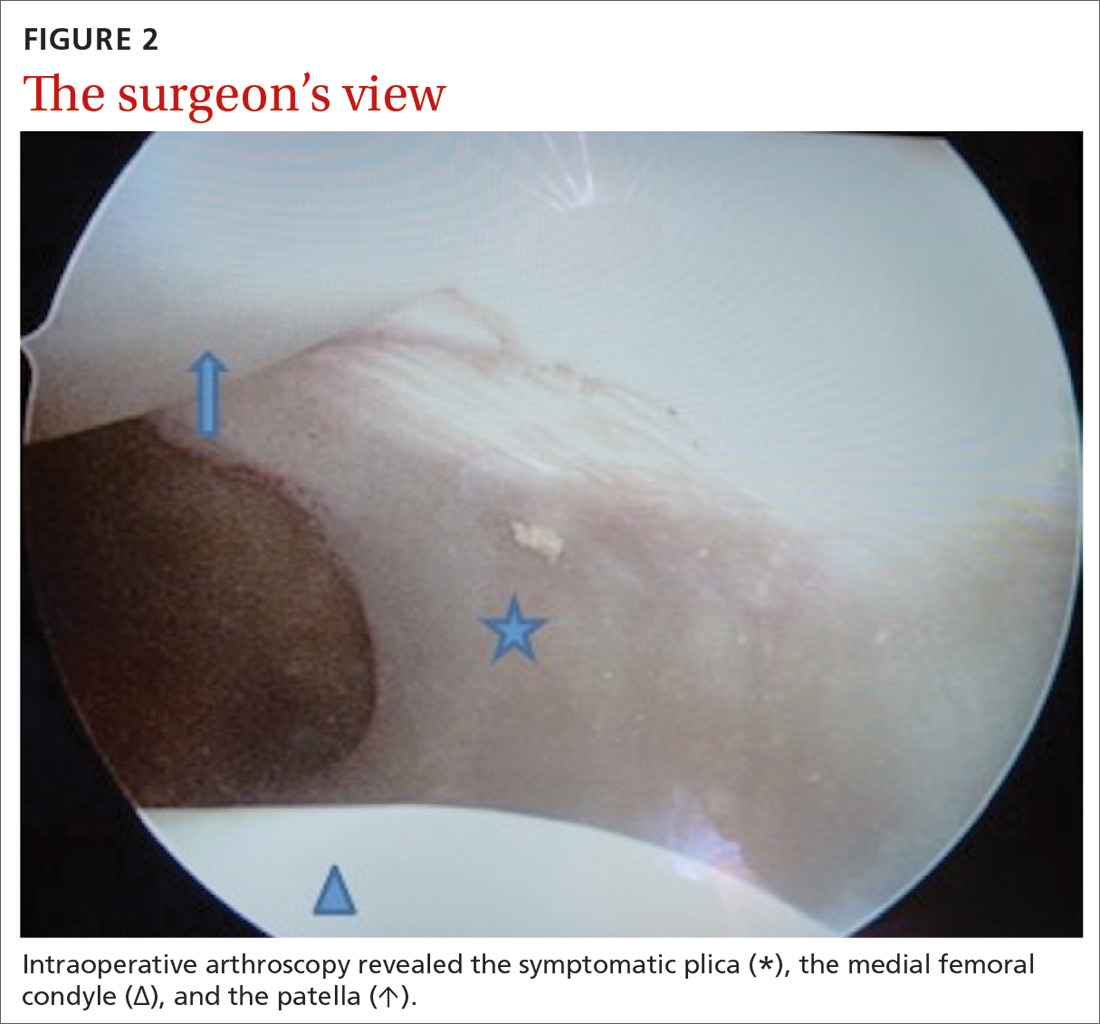
Our patient underwent arthroscopic resection of the plica after 6 months of conservative treatment had failed (FIGURE 2). The patient was able to walk immediately after surgery. The outcome was favorable, since physiotherapy was no longer required 2 months after surgery.
CORRESPONDENCE
Céline Klein, MD, Service d’Orthopédie Pédiatrique, CHU Amiens, Groupe Hospitalier Sud, F-80054 Amiens cedex 1, France; [email protected].
1. Camanho GL. Treatment of pathological synovial plicae of the knee. Clinics (Sao Paolo). 2010;65:247-250.
2. Ewing JW. Plica: pathologic or not? J Am Acad Orthop Surg. 1993;1:117-121.
3. Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr. 2017;6:190-198.
4. Paczesny Ł, Kruczyński J. Medial plica syndrome of the knee: diagnosis with dynamic sonography. Radiology. 2009;251:439-446.
5. Samim M, Smitaman E, Lawrence D, et al. MRI of anterior knee pain. Skeletal Radiol. 2014;43:875-893.
6. Weckström M, Niva MH, Lamminen A, et al. Arthroscopic resection of medial plica of the knee in young adults. Knee. 2010;17:103-107.
7. Kan H, Arai Y, Nakagawa S, et al. Characteristics of medial plica syndrome complicated with cartilage damage. Int Orthop. 2015;39:2489-2494.
A 14-year-old girl with an unremarkable medical history presented to the family medicine clinic with a 6-month history of right knee pain (episodic locking and anterior pain). Physical examination of the knee ligaments revealed that the knee was stable and pain-free in the frontal and sagittal planes. There was no intra-articular effusion, the joint spaces were not painful, and range of motion was normal.
Palpation of the knee elicited pain, notably when the physician rolled his fingers over a “cord” above the internal parapatellar compartment. X-rays of the knee were normal. In light of the patient’s chronic pain, magnetic resonance imaging (MRI) was performed (FIGURE 1).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Synovial plica
The MRI with fat saturation revealed a symptomatic synovial plica between the patellar facet and the condyle (FIGURE 1, arrow). The normal x-ray findings had already ruled out osteochondritis dissecans of the femoral condyles, patellar abnormalities, and trochlear dysplasia; the MRI ruled out several additional items in the differential, such as damage to the meniscus, ligament, and/or cartilage.
The synovial plica is a normal structure that develops during the embryogenic phase; however, involution is incomplete in up to 50% of the population, resulting in persistent plicae.1 The plica is often located in a medial position but can occur lateral to, above, or below the knee cap. Although usually asymptomatic, the plica can become pathologic when irritation (eg, from repetitive motion) causes an inflammatory response.1
Synovial plica syndrome, as this condition is known, is a common cause of anterior knee pain in adolescents and athletes; incidence ranges from 3.8% to 5.5%.2 The patient often reports trauma (a direct impact to the knee) or participation in sports activities that require repeated flexion-extension of the knee.3
Presenting symptoms and MRI findings can unlock the diagnosis
The combination of anterior knee pain and a painful parapatellar “cord” on palpation is the most frequent diagnostic sign of synovial plica syndrome.1 Quadriceps wasting, intra-articular effusion, and reduced range of motion of the knee may also be observed.1,4 Some patients experience particularly disconcerting symptoms, such as knee locking, clicking, or instability.1
In most cases, MRI confirms the clinical diagnosis while ruling out other possible causes of the symptoms and associated pathologies.5 However, MRI may not reveal the plica if it is attached to the articular capsule or if there is no intra-articular effusion. Dynamic ultrasound might be of diagnostic value but is operator dependent.4
Continue to: If conservative treatment fails, consider surgical repair
If conservative treatment fails, consider surgical repair
Conservative treatment—a combination of analgesics, anti-inflammatories, and physiotherapy with vastus medialis strengthening and stretching—is the preferred first-line treatment, with a success rate of 40% to 60%.1 If conservative treatment fails, surgical treatment can be
Our patient underwent arthroscopic resection of the plica after 6 months of conservative treatment had failed (FIGURE 2). The patient was able to walk immediately after surgery. The outcome was favorable, since physiotherapy was no longer required 2 months after surgery.
CORRESPONDENCE
Céline Klein, MD, Service d’Orthopédie Pédiatrique, CHU Amiens, Groupe Hospitalier Sud, F-80054 Amiens cedex 1, France; [email protected].
A 14-year-old girl with an unremarkable medical history presented to the family medicine clinic with a 6-month history of right knee pain (episodic locking and anterior pain). Physical examination of the knee ligaments revealed that the knee was stable and pain-free in the frontal and sagittal planes. There was no intra-articular effusion, the joint spaces were not painful, and range of motion was normal.
Palpation of the knee elicited pain, notably when the physician rolled his fingers over a “cord” above the internal parapatellar compartment. X-rays of the knee were normal. In light of the patient’s chronic pain, magnetic resonance imaging (MRI) was performed (FIGURE 1).

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Synovial plica
The MRI with fat saturation revealed a symptomatic synovial plica between the patellar facet and the condyle (FIGURE 1, arrow). The normal x-ray findings had already ruled out osteochondritis dissecans of the femoral condyles, patellar abnormalities, and trochlear dysplasia; the MRI ruled out several additional items in the differential, such as damage to the meniscus, ligament, and/or cartilage.
The synovial plica is a normal structure that develops during the embryogenic phase; however, involution is incomplete in up to 50% of the population, resulting in persistent plicae.1 The plica is often located in a medial position but can occur lateral to, above, or below the knee cap. Although usually asymptomatic, the plica can become pathologic when irritation (eg, from repetitive motion) causes an inflammatory response.1
Synovial plica syndrome, as this condition is known, is a common cause of anterior knee pain in adolescents and athletes; incidence ranges from 3.8% to 5.5%.2 The patient often reports trauma (a direct impact to the knee) or participation in sports activities that require repeated flexion-extension of the knee.3
Presenting symptoms and MRI findings can unlock the diagnosis
The combination of anterior knee pain and a painful parapatellar “cord” on palpation is the most frequent diagnostic sign of synovial plica syndrome.1 Quadriceps wasting, intra-articular effusion, and reduced range of motion of the knee may also be observed.1,4 Some patients experience particularly disconcerting symptoms, such as knee locking, clicking, or instability.1
In most cases, MRI confirms the clinical diagnosis while ruling out other possible causes of the symptoms and associated pathologies.5 However, MRI may not reveal the plica if it is attached to the articular capsule or if there is no intra-articular effusion. Dynamic ultrasound might be of diagnostic value but is operator dependent.4
Continue to: If conservative treatment fails, consider surgical repair
If conservative treatment fails, consider surgical repair
Conservative treatment—a combination of analgesics, anti-inflammatories, and physiotherapy with vastus medialis strengthening and stretching—is the preferred first-line treatment, with a success rate of 40% to 60%.1 If conservative treatment fails, surgical treatment can be
Our patient underwent arthroscopic resection of the plica after 6 months of conservative treatment had failed (FIGURE 2). The patient was able to walk immediately after surgery. The outcome was favorable, since physiotherapy was no longer required 2 months after surgery.
CORRESPONDENCE
Céline Klein, MD, Service d’Orthopédie Pédiatrique, CHU Amiens, Groupe Hospitalier Sud, F-80054 Amiens cedex 1, France; [email protected].
1. Camanho GL. Treatment of pathological synovial plicae of the knee. Clinics (Sao Paolo). 2010;65:247-250.
2. Ewing JW. Plica: pathologic or not? J Am Acad Orthop Surg. 1993;1:117-121.
3. Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr. 2017;6:190-198.
4. Paczesny Ł, Kruczyński J. Medial plica syndrome of the knee: diagnosis with dynamic sonography. Radiology. 2009;251:439-446.
5. Samim M, Smitaman E, Lawrence D, et al. MRI of anterior knee pain. Skeletal Radiol. 2014;43:875-893.
6. Weckström M, Niva MH, Lamminen A, et al. Arthroscopic resection of medial plica of the knee in young adults. Knee. 2010;17:103-107.
7. Kan H, Arai Y, Nakagawa S, et al. Characteristics of medial plica syndrome complicated with cartilage damage. Int Orthop. 2015;39:2489-2494.
1. Camanho GL. Treatment of pathological synovial plicae of the knee. Clinics (Sao Paolo). 2010;65:247-250.
2. Ewing JW. Plica: pathologic or not? J Am Acad Orthop Surg. 1993;1:117-121.
3. Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr. 2017;6:190-198.
4. Paczesny Ł, Kruczyński J. Medial plica syndrome of the knee: diagnosis with dynamic sonography. Radiology. 2009;251:439-446.
5. Samim M, Smitaman E, Lawrence D, et al. MRI of anterior knee pain. Skeletal Radiol. 2014;43:875-893.
6. Weckström M, Niva MH, Lamminen A, et al. Arthroscopic resection of medial plica of the knee in young adults. Knee. 2010;17:103-107.
7. Kan H, Arai Y, Nakagawa S, et al. Characteristics of medial plica syndrome complicated with cartilage damage. Int Orthop. 2015;39:2489-2494.